- Search Menu
- Advance Articles
- Editor's Choice
- Author Guidelines
- Submission Site
- Open Access Options
- Self-Archiving Policy
- About Journal of Molecular Cell Biology
- Society affiliations
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic


Article Contents
Obesity: causes, consequences, treatments, and challenges.
- Article contents
- Figures & tables
- Supplementary Data
Obesity: causes, consequences, treatments, and challenges, Journal of Molecular Cell Biology , Volume 13, Issue 7, July 2021, Pages 463–465, https://doi.org/10.1093/jmcb/mjab056
- Permissions Icon Permissions
Obesity has become a global epidemic and is one of today’s most public health problems worldwide. Obesity poses a major risk for a variety of serious diseases including diabetes mellitus, non-alcoholic liver disease (NAFLD), cardiovascular disease, hypertension and stroke, and certain forms of cancer ( Bluher, 2019 ).
Obesity is mainly caused by imbalanced energy intake and expenditure due to a sedentary lifestyle coupled with overnutrition. Excess nutrients are stored in adipose tissue (AT) in the form of triglycerides, which will be utilized as nutrients by other tissues through lipolysis under nutrient deficit conditions. There are two major types of AT, white AT (WAT) and brown AT, the latter is a specialized form of fat depot that participates in non-shivering thermogenesis through lipid oxidation-mediated heat generation. While WAT has been historically considered merely an energy reservoir, this fat depot is now well known to function as an endocrine organ that produces and secretes various hormones, cytokines, and metabolites (termed as adipokines) to control systemic energy balance. Studies over the past decade also show that WAT, especially subcutaneous WAT, could undergo ‘beiging’ remodeling in response to environmental or hormonal perturbation. In the first paper of this special issue, Cheong and Xu (2021) systematically review the recent progress on the factors, pathways, and mechanisms that regulate the intercellular and inter-organ crosstalks in the beiging of WAT. A critical but still not fully addressed issue in the adipose research field is the origin of the beige cells. Although beige adipocytes are known to have distinct cellular origins from brown and while adipocytes, it remains unclear on whether the cells are from pre-existing mature white adipocytes through a transdifferentiation process or from de novo differentiation of precursor cells. AT is a heterogeneous tissue composed of not only adipocytes but also nonadipocyte cell populations, including fibroblasts, as well as endothelial, blood, stromal, and adipocyte precursor cells ( Ruan, 2020 ). The authors examined evidence to show that heterogeneity contributes to different browning capacities among fat depots and even within the same depot. The local microenvironment in WAT, which is dynamically and coordinately controlled by inputs from the heterogeneous cell types, plays a critical role in the beige adipogenesis process. The authors also examined key regulators of the AT microenvironment, including vascularization, the sympathetic nerve system, immune cells, peptide hormones, exosomes, and gut microbiota-derived metabolites. Given that increasing beige fat function enhances energy expenditure and consequently reduces body weight gain, identification and characterization of novel regulators and understanding their mechanisms of action in the beiging process has a therapeutic potential to combat obesity and its associated diseases. However, as noticed by the authors, most of the current pre-clinical research on ‘beiging’ are done in rodent models, which may not represent the exact phenomenon in humans ( Cheong and Xu, 2021 ). Thus, further investigations will be needed to translate the findings from bench to clinic.
While both social–environmental factors and genetic preposition have been recognized to play important roles in obesity epidemic, Gao et al. (2021) present evidence showing that epigenetic changes may be a key factor to explain interindividual differences in obesity. The authors examined data on the function of DNA methylation in regulating the expression of key genes involved in metabolism. They also summarize the roles of histone modifications as well as various RNAs such as microRNAs, long noncoding RNAs, and circular RNAs in regulating metabolic gene expression in metabolic organs in response to environmental cues. Lastly, the authors discuss the effect of lifestyle modification and therapeutic agents on epigenetic regulation of energy homeostasis. Understanding the mechanisms by which lifestyles such as diet and exercise modulate the expression and function of epigenetic factors in metabolism should be essential for developing novel strategies for the prevention and treatment of obesity and its associated metabolic diseases.
A major consequence of obesity is type 2 diabetes, a chronic disease that occurs when body cannot use and produce insulin effectively. Diabetes profoundly and adversely affects the vasculature, leading to various cardiovascular-related diseases such as atherosclerosis, arteriosclerotic, and microvascular diseases, which have been recognized as the most common causes of death in people with diabetes ( Cho et al., 2018 ). Love et al. (2021) systematically review the roles and regulation of endothelial insulin resistance in diabetes complications, focusing mainly on vascular dysfunction. The authors review the vasoprotective functions and the mechanisms of action of endothelial insulin and insulin-like growth factor 1 signaling pathways. They also examined the contribution and impart of endothelial insulin resistance to diabetes complications from both biochemical and physiological perspectives and evaluated the beneficial roles of many of the medications currently used for T2D treatment in vascular management, including metformin, thiazolidinediones, glucagon-like receptor agonists, dipeptidyl peptidase-4 inhibitors, sodium-glucose cotransporter inhibitors, as well as exercise. The authors present evidence to suggest that sex differences and racial/ethnic disparities contribute significantly to vascular dysfunction in the setting of diabetes. Lastly, the authors raise a number of very important questions with regard to the role and connection of endothelial insulin resistance to metabolic dysfunction in other major metabolic organs/tissues and suggest several insightful directions in this area for future investigation.
Following on from the theme of obesity-induced metabolic dysfunction, Xia et al. (2021) review the latest progresses on the role of membrane-type I matrix metalloproteinase (MT1-MMP), a zinc-dependent endopeptidase that proteolytically cleaves extracellular matrix components and non-matrix proteins, in lipid metabolism. The authors examined data on the transcriptional and post-translational modification regulation of MT1-MMP gene expression and function. They also present evidence showing that the functions of MT1-MMP in lipid metabolism are cell specific as it may either promote or suppress inflammation and atherosclerosis depending on its presence in distinct cells. MT1-MMP appears to exert a complex role in obesity for that the molecule delays the progression of early obesity but exacerbates obesity at the advanced stage. Because inhibition of MT1-MMP can potentially lower the circulating low-density lipoprotein cholesterol levels and reduce the risk of cancer metastasis and atherosclerosis, the protein has been viewed as a very promising therapeutic target. However, challenges remain in developing MT1-MMP-based therapies due to the tissue-specific roles of MT1-MMP and the lack of specific inhibitors for this molecule. Further investigations are needed to address these questions and to develop MT1-MMP-based therapeutic interventions.
Lastly, Huang et al. (2021) present new findings on a critical role of puromycin-sensitive aminopeptidase (PSA), an integral non-transmembrane enzyme that catalyzes the cleavage of amino acids near the N-terminus of polypeptides, in NAFLD. NAFLD, ranging from simple nonalcoholic fatty liver to the more aggressive subtype nonalcoholic steatohepatitis, has now become the leading chronic liver disease worldwide ( Loomba et al., 2021 ). At present, no effective drugs are available for NAFLD management in the clinic mainly due to the lack of a complete understanding of the mechanisms underlying the disease progress, reinforcing the urgent need to identify and validate novel targets and to elucidate their mechanisms of action in NAFLD development and pathogenesis. Huang et al. (2021) found that PSA expression levels were greatly reduced in the livers of obese mouse models and that the decreased PSA expression correlated with the progression of NAFLD in humans. They also found that PSA levels were negatively correlated with triglyceride accumulation in cultured hepatocytes and in the liver of ob/ob mice. Moreover, PSA suppresses steatosis by promoting lipogenesis and attenuating fatty acid β-oxidation in hepatocytes and protects oxidative stress and lipid overload in the liver by activating the nuclear factor erythroid 2-related factor 2, the master regulator of antioxidant response. These studies identify PSA as a pivotal regulator of hepatic lipid metabolism and suggest that PSA may be a potential biomarker and therapeutic target for treating NAFLD.
In summary, papers in this issue review our current knowledge on the causes, consequences, and interventions of obesity and its associated diseases such as type 2 diabetes, NAFLD, and cardiovascular disease ( Cheong and Xu, 2021 ; Gao et al., 2021 ; Love et al., 2021 ). Potential targets for the treatment of dyslipidemia and NAFLD are also discussed, as exemplified by MT1-MMP and PSA ( Huang et al., 2021 ; Xia et al., 2021 ). It is noted that despite enormous effect, few pharmacological interventions are currently available in the clinic to effectively treat obesity. In addition, while enhancing energy expenditure by browning/beiging of WAT has been demonstrated as a promising alternative approach to alleviate obesity in rodent models, it remains to be determined on whether such WAT reprogramming is effective in combating obesity in humans ( Cheong and Xu, 2021 ). Better understanding the mechanisms by which obesity induces various medical consequences and identification and characterization of novel anti-obesity secreted factors/soluble molecules would be helpful for developing effective therapeutic treatments for obesity and its associated medical complications.
Bluher M. ( 2019 ). Obesity: global epidemiology and pathogenesis . Nat. Rev. Endocrinol . 15 , 288 – 298 .
Google Scholar
Cheong L.Y. , Xu A. ( 2021 ). Intercellular and inter-organ crosstalk in browning of white adipose tissue: molecular mechanism and therapeutic complications . J. Mol. Cell Biol . 13 , 466 – 479 .
Cho N.H. , Shaw J.E. , Karuranga S. , et al. ( 2018 ). IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045 . Diabetes Res. Clin. Pract . 138 , 271 – 281 .
Gao W. , Liu J.-L. , Lu X. , et al. ( 2021 ). Epigenetic regulation of energy metabolism in obesity . J. Mol. Cell Biol . 13 , 480 – 499 .
Huang B. , Xiong X. , Zhang L. , et al. ( 2021 ). PSA controls hepatic lipid metabolism by regulating the NRF2 signaling pathway . J. Mol. Cell Biol . 13 , 527 – 539 .
Loomba R. , Friedman S.L. , Shulman G.I. ( 2021 ). Mechanisms and disease consequences of nonalcoholic fatty liver disease . Cell 184 , 2537 – 2564 .
Love K.M. , Barrett E.J. , Malin S.K. , et al. ( 2021 ). Diabetes pathogenesis and management: the endothelium comes of age . J. Mol. Cell Biol . 13 , 500 – 512 .
Ruan H.-B. ( 2020 ). Developmental and functional heterogeneity of thermogenic adipose tissue . J. Mol. Cell Biol . 12 , 775 – 784 .
Xia X.-D. , Alabi A. , Wang M. , et al. ( 2021 ). Membrane-type I matrix metalloproteinase (MT1-MMP), lipid metabolism, and therapeutic implications . J. Mol. Cell Biol . 13 , 513 – 526 .
Author notes
Shanghai Diabetes Institute, Shanghai Key Laboratory of Diabetes Mellitus, Shanghai Clinical Center for Diabetes, Shanghai Jiao Tong University Affiliated Sixth People's Hospital, Shanghai 200233, China E-mail: [email protected]
Email alerts
Citing articles via, affiliations.
- Online ISSN 1759-4685
- Copyright © 2024 Chinese Academy of Sciences
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- About Project
- Testimonials
Business Management Ideas

Essay on Obesity
List of essays on obesity, essay on obesity – short essay (essay 1 – 150 words), essay on obesity (essay 2 – 250 words), essay on obesity – written in english (essay 3 – 300 words), essay on obesity – for school students (class 5, 6, 7, 8, 9, 10, 11 and 12 standard) (essay 4 – 400 words), essay on obesity – for college students (essay 5 – 500 words), essay on obesity – with causes and treatment (essay 6 – 600 words), essay on obesity – for science students (essay 7 – 750 words), essay on obesity – long essay for medical students (essay 8 – 1000 words).
Obesity is a chronic health condition in which the body fat reaches abnormal level. Obesity occurs when we consume much more amount of food than our body really needs on a daily basis. In other words, when the intake of calories is greater than the calories we burn out, it gives rise to obesity.
Audience: The below given essays are exclusively written for school students (Class 5, 6, 7, 8, 9, 10, 11 and 12 Standard), college, science and medical students.
Introduction:
Obesity means being excessively fat. A person would be said to be obese if his or her body mass index is beyond 30. Such a person has a body fat rate that is disproportionate to his body mass.
Obesity and the Body Mass Index:
The body mass index is calculated considering the weight and height of a person. Thus, it is a scientific way of determining the appropriate weight of any person. When the body mass index of a person indicates that he or she is obese, it exposes the person to make health risk.
Stopping Obesity:
There are two major ways to get the body mass index of a person to a moderate rate. The first is to maintain a strict diet. The second is to engage in regular physical exercise. These two approaches are aimed at reducing the amount of fat in the body.
Conclusion:
Obesity can lead to sudden death, heart attack, diabetes and may unwanted illnesses. Stop it by making healthy choices.
Obesity has become a big concern for the youth of today’s generation. Obesity is defined as a medical condition in which an individual gains excessive body fat. When the Body Mass Index (BMI) of a person is over 30, he/ she is termed as obese.
Obesity can be a genetic problem or a disorder that is caused due to unhealthy lifestyle habits of a person. Physical inactivity and the environment in which an individual lives, are also the factors that leads to obesity. It is also seen that when some individuals are in stress or depression, they start cultivating unhealthy eating habits which eventually leads to obesity. Medications like steroids is yet another reason for obesity.
Obesity has several serious health issues associated with it. Some of the impacts of obesity are diabetes, increase of cholesterol level, high blood pressure, etc. Social impacts of obesity includes loss of confidence in an individual, lowering of self-esteem, etc.
The risks of obesity needs to be prevented. This can be done by adopting healthy eating habits, doing some physical exercise regularly, avoiding stress, etc. Individuals should work on weight reduction in order to avoid obesity.
Obesity is indeed a health concern and needs to be prioritized. The management of obesity revolves around healthy eating habits and physical activity. Obesity, if not controlled in its initial stage can cause many severe health issues. So it is wiser to exercise daily and maintain a healthy lifestyle rather than being the victim of obesity.
Obesity can be defined as the clinical condition where accumulation of excessive fat takes place in the adipose tissue leading to worsening of health condition. Usually, the fat is deposited around the trunk and also the waist of the body or even around the periphery.
Obesity is actually a disease that has been spreading far and wide. It is preventable and certain measures are to be taken to curb it to a greater extend. Both in the developing and developed countries, obesity has been growing far and wide affecting the young and the old equally.
The alarming increase in obesity has resulted in stimulated death rate and health issues among the people. There are several methods adopted to lose weight and they include different diet types, physical activity and certain changes in the current lifestyle. Many of the companies are into minting money with the concept of inviting people to fight obesity.
In patients associated with increased risk factor related to obesity, there are certain drug therapies and other procedures adopted to lose weight. There are certain cost effective ways introduced by several companies to enable clinic-based weight loss programs.
Obesity can lead to premature death and even cause Type 2 Diabetes Mellitus. Cardiovascular diseases have also become the part and parcel of obese people. It includes stroke, hypertension, gall bladder disease, coronary heart disease and even cancers like breast cancer, prostate cancer, endometrial cancer and colon cancer. Other less severe arising due to obesity includes osteoarthritis, gastro-esophageal reflux disease and even infertility.
Hence, serious measures are to be taken to fight against this dreadful phenomenon that is spreading its wings far and wide. Giving proper education on benefits of staying fit and mindful eating is as important as curbing this issue. Utmost importance must be given to healthy eating habits right from the small age so that they follow the same until the end of their life.
Obesity is majorly a lifestyle disease attributed to the extra accumulation of fat in the body leading to negative health effects on a person. Ironically, although prevalent at a large scale in many countries, including India, it is one of the most neglect health problems. It is more often ignored even if told by the doctor that the person is obese. Only when people start acquiring other health issues such as heart disease, blood pressure or diabetes, they start taking the problem of obesity seriously.
Obesity Statistics in India:
As per a report, India happens to figure as the third country in the world with the most obese people. This should be a troubling fact for India. However, we are yet to see concrete measures being adopted by the people to remain fit.
Causes of Obesity:
Sedentary lifestyle, alcohol, junk food, medications and some diseases such as hypothyroidism are considered as the factors which lead to obesity. Even children seem to be glued to televisions, laptops and video games which have taken away the urge for physical activities from them. Adding to this, the consumption of junk food has further aggravated the growing problem of obesity in children.
In the case of adults, most of the professions of today make use of computers which again makes people sit for long hours in one place. Also, the hectic lifestyle of today makes it difficult for people to spare time for physical activities and people usually remain stressed most of the times. All this has contributed significantly to the rise of obesity in India.
Obesity and BMI:
Body Mass Index (BMI) is the measure which allows a person to calculate how to fit he or she is. In other words, the BMI tells you if you are obese or not. BMI is calculated by dividing the weight of a person in kg with the square of his / her height in metres. The number thus obtained is called the BMI. A BMI of less than 25 is considered optimal. However, if a person has a BMI over 30 he/she is termed as obese.
What is a matter of concern is that with growing urbanisation there has been a rapid increase of obese people in India? It is of utmost importance to consider this health issue a serious threat to the future of our country as a healthy body is important for a healthy soul. We should all be mindful of what we eat and what effect it has on our body. It is our utmost duty to educate not just ourselves but others as well about this serious health hazard.
Obesity can be defined as a condition (medical) that is the accumulation of body fat to an extent that the excess fat begins to have a lot of negative effects on the health of the individual. Obesity is determined by examining the body mass index (BMI) of the person. The BMI is gotten by dividing the weight of the person in kilogram by the height of the person squared.
When the BMI of a person is more than 30, the person is classified as being obese, when the BMI falls between 25 and 30, the person is said to be overweight. In a few countries in East Asia, lower values for the BMI are used. Obesity has been proven to influence the likelihood and risk of many conditions and disease, most especially diabetes of type 2, cardiovascular diseases, sleeplessness that is obstructive, depression, osteoarthritis and some cancer types.
In most cases, obesity is caused through a combination of genetic susceptibility, a lack of or inadequate physical activity, excessive intake of food. Some cases of obesity are primarily caused by mental disorder, medications, endocrine disorders or genes. There is no medical data to support the fact that people suffering from obesity eat very little but gain a lot of weight because of slower metabolism. It has been discovered that an obese person usually expends much more energy than other people as a result of the required energy that is needed to maintain a body mass that is increased.
It is very possible to prevent obesity with a combination of personal choices and social changes. The major treatments are exercising and a change in diet. We can improve the quality of our diet by reducing our consumption of foods that are energy-dense like those that are high in sugars or fat and by trying to increase our dietary fibre intake.
We can also accompany the appropriate diet with the use of medications to help in reducing appetite and decreasing the absorption of fat. If medication, exercise and diet are not yielding any positive results, surgery or gastric balloon can also be carried out to decrease the volume of the stomach and also reduce the intestines’ length which leads to the feel of the person get full early or a reduction in the ability to get and absorb different nutrients from a food.
Obesity is the leading cause of ill-health and death all over the world that is preventable. The rate of obesity in children and adults has drastically increased. In 2015, a whopping 12 percent of adults which is about 600 million and about 100 million children all around the world were found to be obese.
It has also been discovered that women are more obese than men. A lot of government and private institutions and bodies have stated that obesity is top of the list of the most difficult and serious problems of public health that we have in the world today. In the world we live today, there is a lot of stigmatisation of obese people.
We all know how troubling the problem of obesity truly is. It is mainly a form of a medical condition wherein the body tends to accumulate excessive fat which in turn has negative repercussions on the health of an individual.
Given the current lifestyle and dietary style, it has become more common than ever. More and more people are being diagnosed with obesity. Such is its prevalence that it has been termed as an epidemic in the USA. Those who suffer from obesity are at a much higher risk of diabetes, heart diseases and even cancer.
In order to gain a deeper understanding of obesity, it is important to learn what the key causes of obesity are. In a layman term, if your calorie consumption exceeds what you burn because of daily activities and exercises, it is likely to lead to obesity. It is caused over a prolonged period of time when your calorie intake keeps exceeding the calories burned.
Here are some of the key causes which are known to be the driving factors for obesity.
If your diet tends to be rich in fat and contains massive calorie intake, you are all set to suffer from obesity.
Sedentary Lifestyle:
With most people sticking to their desk jobs and living a sedentary lifestyle, the body tends to get obese easily.
Of course, the genetic framework has a lot to do with obesity. If your parents are obese, the chance of you being obese is quite high.
The weight which women gain during their pregnancy can be very hard to shed and this is often one of the top causes of obesity.
Sleep Cycle:
If you are not getting an adequate amount of sleep, it can have an impact on the hormones which might trigger hunger signals. Overall, these linked events tend to make you obese.
Hormonal Disorder:
There are several hormonal changes which are known to be direct causes of obesity. The imbalance of the thyroid stimulating hormone, for instance, is one of the key factors when it comes to obesity.
Now that we know the key causes, let us look at the possible ways by which you can handle it.
Treatment for Obesity:
As strange as it may sound, the treatment for obesity is really simple. All you need to do is follow the right diet and back it with an adequate amount of exercise. If you can succeed in doing so, it will give you the perfect head-start into your journey of getting in shape and bidding goodbye to obesity.
There are a lot of different kinds and styles of diet plans for obesity which are available. You can choose the one which you deem fit. We recommend not opting for crash dieting as it is known to have several repercussions and can make your body terribly weak.
The key here is to stick to a balanced diet which can help you retain the essential nutrients, minerals, and, vitamins and shed the unwanted fat and carbs.
Just like the diet, there are several workout plans for obesity which are available. It is upon you to find out which of the workout plan seems to be apt for you. Choose cardio exercises and dance routines like Zumba to shed the unwanted body weight. Yoga is yet another method to get rid of obesity.
So, follow a blend of these and you will be able to deal with the trouble of obesity in no time. We believe that following these tips will help you get rid of obesity and stay in shape.
Obesity and overweight is a top health concern in the world due to the impact it has on the lives of individuals. Obesity is defined as a condition in which an individual has excessive body fat and is measured using the body mass index (BMI) such that, when an individual’s BMI is above 30, he or she is termed obese. The BMI is calculated using body weight and height and it is different for all individuals.
Obesity has been determined as a risk factor for many diseases. It results from dietary habits, genetics, and lifestyle habits including physical inactivity. Obesity can be prevented so that individuals do not end up having serious complications and health problems. Chronic illnesses like diabetes, heart diseases and relate to obesity in terms of causes and complications.
Factors Influencing Obesity:
Obesity is not only as a result of lifestyle habits as most people put it. There are other important factors that influence obesity. Genetics is one of those factors. A person could be born with genes that predispose them to obesity and they will also have difficulty in losing weight because it is an inborn factor.
The environment also influences obesity because the diet is similar in certain environs. In certain environments, like school, the food available is fast foods and the chances of getting healthy foods is very low, leading to obesity. Also, physical inactivity is an environmental factor for obesity because some places have no fields or tracks where people can jog or maybe the place is very unsafe and people rarely go out to exercise.
Mental health affects the eating habits of individuals. There is a habit of stress eating when a person is depressed and it could result in overweight or obesity if the person remains unhealthy for long period of time.
The overall health of individuals also matter. If a person is unwell and is prescribed with steroids, they may end up being obese. Steroidal medications enable weight gain as a side effect.
Complications of Obesity:
Obesity is a health concern because its complications are severe. Significant social and health problems are experienced by obese people. Socially, they will be bullied and their self-esteem will be low as they will perceive themselves as unworthy.
Chronic illnesses like diabetes results from obesity. Diabetes type 2 has been directly linked to obesity. This condition involves the increased blood sugars in the body and body cells are not responding to insulin as they should. The insulin in the body could also be inadequate due to decreased production. High blood sugar concentrations result in symptoms like frequent hunger, thirst and urination. The symptoms of complicated stages of diabetes type 2 include loss of vision, renal failure and heart failure and eventually death. The importance of having a normal BMI is the ability of the body to control blood sugars.
Another complication is the heightened blood pressures. Obesity has been defined as excessive body fat. The body fat accumulates in blood vessels making them narrow. Narrow blood vessels cause the blood pressures to rise. Increased blood pressure causes the heart to start failing in its physiological functions. Heart failure is the end result in this condition of increased blood pressures.
There is a significant increase in cholesterol in blood of people who are obese. High blood cholesterol levels causes the deposition of fats in various parts of the body and organs. Deposition of fats in the heart and blood vessels result in heart diseases. There are other conditions that result from hypercholesterolemia.
Other chronic illnesses like cancer can also arise from obesity because inflammation of body cells and tissues occurs in order to store fats in obese people. This could result in abnormal growths and alteration of cell morphology. The abnormal growths could be cancerous.
Management of Obesity:
For the people at risk of developing obesity, prevention methods can be implemented. Prevention included a healthy diet and physical activity. The diet and physical activity patterns should be regular and realizable to avoid strains that could result in complications.
Some risk factors for obesity are non-modifiable for example genetics. When a person in genetically predisposed, the lifestyle modifications may be have help.
For the individuals who are already obese, they can work on weight reduction through healthy diets and physical exercises.
In conclusion, obesity is indeed a major health concern because the health complications are very serious. Factors influencing obesity are both modifiable and non-modifiable. The management of obesity revolves around diet and physical activity and so it is important to remain fit.
In olden days, obesity used to affect only adults. However, in the present time, obesity has become a worldwide problem that hits the kids as well. Let’s find out the most prevalent causes of obesity.
Factors Causing Obesity:
Obesity can be due to genetic factors. If a person’s family has a history of obesity, chances are high that he/ she would also be affected by obesity, sooner or later in life.
The second reason is having a poor lifestyle. Now, there are a variety of factors that fall under the category of poor lifestyle. An excessive diet, i.e., eating more than you need is a definite way to attain the stage of obesity. Needless to say, the extra calories are changed into fat and cause obesity.
Junk foods, fried foods, refined foods with high fats and sugar are also responsible for causing obesity in both adults and kids. Lack of physical activity prevents the burning of extra calories, again, leading us all to the path of obesity.
But sometimes, there may also be some indirect causes of obesity. The secondary reasons could be related to our mental and psychological health. Depression, anxiety, stress, and emotional troubles are well-known factors of obesity.
Physical ailments such as hypothyroidism, ovarian cysts, and diabetes often complicate the physical condition and play a massive role in abnormal weight gain.
Moreover, certain medications, such as steroids, antidepressants, and contraceptive pills, have been seen interfering with the metabolic activities of the body. As a result, the long-term use of such drugs can cause obesity. Adding to that, regular consumption of alcohol and smoking are also connected to the condition of obesity.
Harmful Effects of Obesity:
On the surface, obesity may look like a single problem. But, in reality, it is the mother of several major health issues. Obesity simply means excessive fat depositing into our body including the arteries. The drastic consequence of such high cholesterol levels shows up in the form of heart attacks and other life-threatening cardiac troubles.
The fat deposition also hampers the elasticity of the arteries. That means obesity can cause havoc in our body by altering the blood pressure to an abnormal range. And this is just the tip of the iceberg. Obesity is known to create an endless list of problems.
In extreme cases, this disorder gives birth to acute diseases like diabetes and cancer. The weight gain due to obesity puts a lot of pressure on the bones of the body, especially of the legs. This, in turn, makes our bones weak and disturbs their smooth movement. A person suffering from obesity also has higher chances of developing infertility issues and sleep troubles.
Many obese people are seen to be struggling with breathing problems too. In the chronic form, the condition can grow into asthma. The psychological effects of obesity are another serious topic. You can say that obesity and depression form a loop. The more a person is obese, the worse is his/ her depression stage.
How to Control and Treat Obesity:
The simplest and most effective way, to begin with, is changing our diet. There are two factors to consider in the diet plan. First is what and what not to eat. Second is how much to eat.
If you really want to get rid of obesity, include more and more green vegetables in your diet. Spinach, beans, kale, broccoli, cauliflower, asparagus, etc., have enough vitamins and minerals and quite low calories. Other healthier options are mushrooms, pumpkin, beetroots, and sweet potatoes, etc.
Opt for fresh fruits, especially citrus fruits, and berries. Oranges, grapes, pomegranate, pineapple, cherries, strawberries, lime, and cranberries are good for the body. They have low sugar content and are also helpful in strengthening our immune system. Eating the whole fruits is a more preferable way in comparison to gulping the fruit juices. Fruits, when eaten whole, have more fibers and less sugar.
Consuming a big bowl of salad is also great for dealing with the obesity problem. A salad that includes fibrous foods such as carrots, radish, lettuce, tomatoes, works better at satiating the hunger pangs without the risk of weight gain.
A high protein diet of eggs, fish, lean meats, etc., is an excellent choice to get rid of obesity. Take enough of omega fatty acids. Remember to drink plenty of water. Keeping yourself hydrated is a smart way to avoid overeating. Water also helps in removing the toxins and excess fat from the body.
As much as possible, avoid fats, sugars, refined flours, and oily foods to keep the weight in control. Control your portion size. Replace the three heavy meals with small and frequent meals during the day. Snacking on sugarless smoothies, dry fruits, etc., is much recommended.
Regular exercise plays an indispensable role in tackling the obesity problem. Whenever possible, walk to the market, take stairs instead of a lift. Physical activity can be in any other form. It could be a favorite hobby like swimming, cycling, lawn tennis, or light jogging.
Meditation and yoga are quite powerful practices to drive away the stress, depression and thus, obesity. But in more serious cases, meeting a physician is the most appropriate strategy. Sometimes, the right medicines and surgical procedures are necessary to control the health condition.
Obesity is spreading like an epidemic, haunting both the adults and the kids. Although genetic factors and other physical ailments play a role, the problem is mostly caused by a reckless lifestyle.
By changing our way of living, we can surely take control of our health. In other words, it would be possible to eliminate the condition of obesity from our lives completely by leading a healthy lifestyle.
Health , Obesity
Get FREE Work-at-Home Job Leads Delivered Weekly!

Join more than 50,000 subscribers receiving regular updates! Plus, get a FREE copy of How to Make Money Blogging!
Message from Sophia!
Like this post? Don’t forget to share it!
Here are a few recommended articles for you to read next:
- Essay on Cleanliness
- Essay on Cancer
- Essay on AIDS
- Essay on Health and Fitness
No comments yet.
Leave a reply click here to cancel reply..
You must be logged in to post a comment.
Billionaires
- Donald Trump
- Warren Buffett
- Email Address
- Free Stock Photos
- Keyword Research Tools
- URL Shortener Tools
- WordPress Theme
Book Summaries
- How To Win Friends
- Rich Dad Poor Dad
- The Code of the Extraordinary Mind
- The Luck Factor
- The Millionaire Fastlane
- The ONE Thing
- Think and Grow Rich
- 100 Million Dollar Business
- Business Ideas
Digital Marketing
- Mobile Addiction
- Social Media Addiction
- Computer Addiction
- Drug Addiction
- Internet Addiction
- TV Addiction
- Healthy Habits
- Morning Rituals
- Wake up Early
- Cholesterol
- Reducing Cholesterol
- Fat Loss Diet Plan
- Reducing Hair Fall
- Sleep Apnea
- Weight Loss
Internet Marketing
- Email Marketing
Law of Attraction
- Subconscious Mind
- Vision Board
- Visualization
Law of Vibration
- Professional Life
Motivational Speakers
- Bob Proctor
- Robert Kiyosaki
- Vivek Bindra
- Inner Peace
Productivity
- Not To-do List
- Project Management Software
- Negative Energies
Relationship
- Getting Back Your Ex
Self-help 21 and 14 Days Course
Self-improvement.
- Body Language
- Complainers
- Emotional Intelligence
- Personality
Social Media
- Project Management
- Anik Singal
- Baba Ramdev
- Dwayne Johnson
- Jackie Chan
- Leonardo DiCaprio
- Narendra Modi
- Nikola Tesla
- Sachin Tendulkar
- Sandeep Maheshwari
- Shaqir Hussyin
Website Development
Wisdom post, worlds most.
- Expensive Cars
Our Portals: Gulf Canada USA Italy Gulf UK
Privacy Overview
- Antioxidants
- Weight Management
- Vitamins & Supplements
- Exercise & Mobility
- Cholesterol
- Hypertension
- Improving Memory
- Give a Gift
- Activate My Web Access
- Customer Service
- Free e-newsletter
- Reset Password

- #7213 (no title)
- Contact the Editor
- Content restricted
- Nutrition 101 – Glossary – J
- Nutrition 101 – Glossary – K
- Nutrition 101 – Glossary – L
- Nutrition 101 – Glossary – M
- Nutrition 101 – Glossary – N
- Nutrition 101 – Glossary – O
- Nutrition 101 – Glossary – P
- Nutrition 101 – Glossary – Q
- Nutrition 101 – Glossary – R
- Nutrition 101 – Glossary – S
- Nutrition 101 – Glossary – T
- Nutrition 101 – Glossary – A
- Nutrition 101 – Glossary – B
- Nutrition 101 – Glossary – C
- Nutrition 101 – Glossary – D
- Nutrition 101 – Glossary – E
- Nutrition 101 – Glossary – F
- Nutrition 101 – Glossary – G
- Nutrition 101 – Glossary – H
- Nutrition 101 – Glossary – I
- Nutrition 101 – Glossary – U
- Nutrition 101 – Glossary – V
- Nutrition 101 – Glossary – W
- Nutrition 101 – Glossary – X
- Nutrition 101 – Glossary – Y
- Nutrition 101 – Glossary – Z
- Manage Email
- Current Issue
- OFIE – Subscriber only
- Online Account Activation
- Privacy Policy
- Registration Complete
- Sample Page
- Subscribe Now
- Tufts & Health Nutrition
- Tufts & Health Nutrition | JH Inforce
- Tufts & Health Nutrition | JHV Employee
- Tufts & Health Nutrition | John Hancock
- Tufts & Health Nutrition | Manulife Asia
- Tufts & Health Nutrition | Manulife Vitality
- Tufts & Health Nutrition | NU101
- Tufts & Health Nutrition | Tufts Employees

Alice’s Homemade Pita Chips

Lemon-Garlic Bean Spread

Roman Chicken with Peppers

Eating for the Earth…And Your Health

Dietary Supplements for Sports Performance

Melatonin Supplements

The Truth about “Brain-Boosting” Supplements

Many Herbal Products Found to Have Substantial Quality Issues

Vitamin C Supplements … Processed Meat

Even a Little Physical Activity May Lower the Risks of Sedentary…

How to Stick to Those Resolutions!

Activity—of All Kinds—Can Help Lower Blood Pressure

Eating a Healthy Diet Associated with Better Sleep

Where Does Poultry Fit In?
Understanding Atherosclerosis

Replacing Animal-Based Foods with Plant-Based Benefits Health

Check Your Nutrition Knowledge!
Hear Ye! Hear Ye!

Healthy (But Not Unhealthy) Plant-Based Diets Associated with Lower Parkinson’s Risk

For Prevention of Cognitive Decline, Reduced Calorie MIND Diet Not Superior…

Meta-Analysis Finds One in Four Older Adults Are Dehydrated

Consuming Plant Protein in Midlife Can Help Women Age Well

Is Olive Oil the Best Choice?

Making Time for Healthy Behaviors

Even Healthy, Normal-Weight Older Women May Benefit from a Heart-Healthy Lifestyle
- Healthy Eating
Obesity is a Disease: Why it Happens, and Why it Matters
Scientists now understand weight gain is not simply a problem of willpower..

T here has been a pervasive idea in society that obesity is a sign of personal failure—that it is caused exclusively by lack of willpower, laziness, and “gluttony.” The science does not agree. In 1998, the National Institutes of Health declared obesity a disease and the American Medical Association followed suit in 2013.
Let’s look at three key reasons obesity is more a disease then a personal failing, and how this knowledge can help you control your own weight—or be more understanding of others’ struggles.
Human Biology. The prevalence of obesity (a body mass index over 30) among U.S. adults is 42 percent and rising. Although lifestyle choices (like what we eat and how much we move) are important, our natural biology plays a key role in the current obesity epidemic. “Human biology is designed to encourage us to eat when food is there,” says Susan B. Roberts, PhD, a professor at the Friedman School and senior scientist on the Energy Metabolism Team at the Human Nutrtion Research Center on Aging. “This normal biology combines with an unhealthy food environment and food culture to cause weight gain. So-called ‘low willpower’ is normal human behavior, not some defect.”
What to do: Take control of your food environment. Stocking the house with healthy (whole and minimally processed) foods, watching portion sizes, preparing more food at home, and choosing wisely when eating out or ordering in can all help curb the natural tendency to overeat.
Metabolic Adaptation. In addition to storing energy (calories) for future use, fat (adipose tissue) acts as a powerful endocrine organ, secreting hormones and other molecules into the blood. “Many of the hormones released by adipose tissue are involved in regulating appetite, energy expenditure, and fat storage,” says Leon I. Igel, MD, a Tufts alum who is an endocrinologist and chief medical officer for Intellihealth. For example, adipose tissue releases the hormone leptin to signal we’ve had enough to eat. Individuals with obesity can develop a lack of sensitivity to leptin, or leptin resistance. With this condition, one doesn’t get the normal feelings of fullness and satiety and the body starts to burn less calories at rest. Leptin resistance thus contributes to a vicious cycle of obesity.
Many other hormones are released by fat cells, including those involved in glucose tolerance, insulin sensitivity, cell growth, inflammation, and the formation of blood clots in veins and arteries. “As levels of adipose tissue increase,” Igel explains, “multiple metabolic pathways stop working as they should. This leads to the development of a number of medical conditions associated with obesity.” Metabolic changes are also responsible for making it difficult to maintain weight loss.
What to do: Science suggests specific foods have different effects on weight gain. “Eat more minimally processed fruits, vegetables, nuts, beans, whole grains, fish, and yogurt,” says Dariush Mozaffarian, MD, DrPH, dean of policy for the Friedman School and editor-in-chief of this newsletter. “Foods with live probiotics and fermented foods may also help protect against weigh gain. Eat less refined grains, starches, sugars, and red and processed meat. Avoid soda and other highly sweetened drinks. Alcohol is also associated with weight gain—if you drink, do so moderately. Other animal foods, like milk, cheese, poultry, and eggs, appear, in observational studies, to be relatively neutral for long-term weight gain.”
Getting adequate sleep, increasing physical activity, and finding ways to reduce or deal with stress can also help address some of the physiological reasons we gain weight.
Even metabolic adaptations that slow metabolism and make weight loss maintenance difficult may be responsive to dietary intake. “Recent controlled trials show metabolic adaptation is influenced by diet quality and composition,” says Mozaffarian. “This research found that after weight loss resting metabolic rate was best maintained on a high fat, low carb diet (60 percent energy from fat, 20 percent from carbs) compared to a low fat, high carb diet (20 percent energy from fat, 60 percent from carbs), leading to about 300 more calories of energy expenditure a day.” Effects were in between on a moderate fat, moderate carb diet (40 percent energy from each). All the carbohydrates in these diets emphasized fruits, non-starchy vegetables, beans, and whole and minimally processed grains, rather than refined grains and added sugars.
Health Impacts. Obesity is the root cause for many medical diseases, including heart disease, stroke, type 2 diabetes, and certain types of cancer. It is also a risk factor for poor self-esteem, depression, obstructive sleep apnea, osteoarthritis, gout, female infertility, gallstones, pancreatitis, and non-alcoholic fatty liver disease. “This makes obesity its own complex medical disease,” says Igel. “We treat each of these other weight-associated conditions individually, but if we are able to treat obesity itself, we reduce all of these other medical issues at the same time.”
What to do: As with the treatment of other conditions—like high blood pressure, high cholesterol, and diabetes—medication may be necessary if lifestyle modifications are not enough. New medications, in combination with lifestyle changes, can help overcome the body’s metabolic adaptations and assist with weight loss. However, these tend to be expensive and are not yet widely covered by health insurance programs.
It is important to recognize that people with obesity who struggle to lose weight are fighting a real battle with their own bodies. It’s equally important to understand that we are not entirely helpless in the face of our genes, hormones, and metabolism. Lifestyle modification, including diet and physical activity, is still the cornerstone of obesity treatment. Accepting that obesity is a disease will help reduce stigma and discrimination, increase research dollars and insurance coverage, and move us all toward a healthier future.
LEAVE A REPLY Cancel reply
Save my name, email, and website in this browser for the next time I comment.
- Do Not Sell My Personal Information
Obesity Essay
Last updated on: Feb 9, 2023
Obesity Essay: A Complete Guide and Topics
By: Nova A.
11 min read
Reviewed By: Jacklyn H.
Published on: Aug 31, 2021

Are you assigned to write an essay about obesity? The first step is to define obesity.
The obesity epidemic is a major issue facing our country right now. It's complicated- it could be genetic or due to your environment, but either way, there are ways that you can fix it!
Learn all about what causes weight gain and get tips on how you can get healthy again.

On this Page
What is Obesity
What is obesity? Obesity and BMI (body mass index) are both tools of measurement that are used by doctors to assess body fat according to the height, age, and gender of a person. If the BMI is between 25 to 29.9, that means the person has excess weight and body fat.
If the BMI exceeds 30, that means the person is obese. Obesity is a condition that increases the risk of developing cardiovascular diseases, high blood pressure, and other medical conditions like metabolic syndrome, arthritis, and even some types of cancer.
Obesity Definition
Obesity is defined by the World Health Organization as an accumulation of abnormal and excess body fat that comes with several risk factors. It is measured by the body mass index BMI, body weight (in kilograms) divided by the square of a person’s height (in meters).
Obesity in America
Obesity is on the verge of becoming an epidemic as 1 in every 3 Americans can be categorized as overweight and obese. Currently, America is an obese country, and it continues to get worse.

Paper Due? Why Suffer? That's our Job!
Causes of obesity
Do you see any obese or overweight people around you?
You likely do.
This is because fast-food chains are becoming more and more common, people are less active, and fruits and vegetables are more expensive than processed foods, thus making them less available to the majority of society. These are the primary causes of obesity.
Obesity is a disease that affects all age groups, including children and elderly people.
Now that you are familiar with the topic of obesity, writing an essay won’t be that difficult for you.
How to Write an Obesity Essay
The format of an obesity essay is similar to writing any other essay. If you need help regarding how to write an obesity essay, it is the same as writing any other essay.
Obesity Essay Introduction
The trick is to start your essay with an interesting and catchy sentence. This will help attract the reader's attention and motivate them to read further. You don’t want to lose the reader’s interest in the beginning and leave a bad impression, especially if the reader is your teacher.
A hook sentence is usually used to open the introductory paragraph of an essay in order to make it interesting. When writing an essay on obesity, the hook sentence can be in the form of an interesting fact or statistic.
Head on to this detailed article on hook examples to get a better idea.
Once you have hooked the reader, the next step is to provide them with relevant background information about the topic. Don’t give away too much at this stage or bombard them with excess information that the reader ends up getting bored with. Only share information that is necessary for the reader to understand your topic.
Next, write a strong thesis statement at the end of your essay, be sure that your thesis identifies the purpose of your essay in a clear and concise manner. Also, keep in mind that the thesis statement should be easy to justify as the body of your essay will revolve around it.
Body Paragraphs
The details related to your topic are to be included in the body paragraphs of your essay. You can use statistics, facts, and figures related to obesity to reinforce your thesis throughout your essay.
If you are writing a cause-and-effect obesity essay, you can mention different causes of obesity and how it can affect a person’s overall health. The number of body paragraphs can increase depending on the parameters of the assignment as set forth by your instructor.
Start each body paragraph with a topic sentence that is the crux of its content. It is necessary to write an engaging topic sentence as it helps grab the reader’s interest. Check out this detailed blog on writing a topic sentence to further understand it.
End your essay with a conclusion by restating your research and tying it to your thesis statement. You can also propose possible solutions to control obesity in your conclusion. Make sure that your conclusion is short yet powerful.
Obesity Essay Examples
Essay about Obesity (PDF)
Childhood Obesity Essay (PDF)
Obesity in America Essay (PDF)
Essay about Obesity Cause and Effects (PDF)
Satire Essay on Obesity (PDF)
Obesity Argumentative Essay (PDF)
Obesity Essay Topics
Choosing a topic might seem an overwhelming task as you may have many ideas for your assignment. Brainstorm different ideas and narrow them down to one, quality topic.
If you need some examples to help you with your essay topic related to obesity, dive into this article and choose from the list of obesity essay topics.
Childhood Obesity
As mentioned earlier, obesity can affect any age group, including children. Obesity can cause several future health problems as children age.
Here are a few topics you can choose from and discuss for your childhood obesity essay:
- What are the causes of increasing obesity in children?
- Obese parents may be at risk for having children with obesity.
- What is the ratio of obesity between adults and children?
- What are the possible treatments for obese children?
- Are there any social programs that can help children with combating obesity?
- Has technology boosted the rate of obesity in children?
- Are children spending more time on gadgets instead of playing outside?
- Schools should encourage regular exercises and sports for children.
- How can sports and other physical activities protect children from becoming obese?
- Can childhood abuse be a cause of obesity among children?
- What is the relationship between neglect in childhood and obesity in adulthood?
- Does obesity have any effect on the psychological condition and well-being of a child?
- Are electronic medical records effective in diagnosing obesity among children?
- Obesity can affect the academic performance of your child.
- Do you believe that children who are raised by a single parent can be vulnerable to obesity?
- You can promote interesting exercises to encourage children.
- What is the main cause of obesity, and why is it increasing with every passing day?
- Schools and colleges should work harder to develop methodologies to decrease childhood obesity.
- The government should not allow schools and colleges to include sweet or fatty snacks as a part of their lunch.
- If a mother is obese, can it affect the health of the child?
- Children who gain weight frequently can develop chronic diseases.
Obesity Argumentative Essay Topics
Do you want to write an argumentative essay on the topic of obesity?
The following list can help you with that!
Here are some examples you can choose from for your argumentative essay about obesity:
- Can vegetables and fruits decrease the chances of obesity?
- Should you go for surgery to overcome obesity?
- Are there any harmful side effects?
- Can obesity be related to the mental condition of an individual?
- Are parents responsible for controlling obesity in childhood?
- What are the most effective measures to prevent the increase in the obesity rate?
- Why is the obesity rate increasing in the United States?
- Can the lifestyle of a person be a cause of obesity?
- Does the economic situation of a country affect the obesity rate?
- How is obesity considered an international health issue?
- Can technology and gadgets affect obesity rates?
- What can be the possible reasons for obesity in a school?
- How can we address the issue of obesity?
- Is obesity a chronic disease?
- Is obesity a major cause of heart attacks?
- Are the junk food chains causing an increase in obesity?
- Do nutritional programs help in reducing the obesity rate?
- How can the right type of diet help with obesity?
- Why should we encourage sports activities in schools and colleges?
- Can obesity affect a person’s behavior?
Health Related Topics for Research Paper
If you are writing a research paper, you can explain the cause and effect of obesity.
Here are a few topics that link to the cause and effects of obesity.Review the literature of previous articles related to obesity. Describe the ideas presented in the previous papers.
- Can family history cause obesity in future generations?
- Can we predict obesity through genetic testing?
- What is the cause of the increasing obesity rate?
- Do you think the increase in fast-food restaurants is a cause of the rising obesity rate?
- Is the ratio of obese women greater than obese men?
- Why are women more prone to be obese as compared to men?
- Stress can be a cause of obesity. Mention the reasons how mental health can be related to physical health.
- Is urban life a cause of the increasing obesity rate?
- People from cities are prone to be obese as compared to people from the countryside.
- How obesity affects the life expectancy of people? What are possible solutions to decrease the obesity rate?
- Do family eating habits affect or trigger obesity?
- How do eating habits affect the health of an individual?
- How can obesity affect the future of a child?
- Obese children are more prone to get bullied in high school and college.
- Why should schools encourage more sports and exercise for children?
Tough Essay Due? Hire Tough Writers!
Topics for Essay on Obesity as a Problem
Do you think a rise in obesity rate can affect the economy of a country?
Here are some topics for your assistance regarding your economics related obesity essay.
- Does socioeconomic status affect the possibility of obesity in an individual?
- Analyze the film and write a review on “Fed Up” – an obesity epidemic.
- Share your reviews on the movie “The Weight of The Nation.”
- Should we increase the prices of fast food and decrease the prices of fruits and vegetables to decrease obesity?
- Do you think healthy food prices can be a cause of obesity?
- Describe what measures other countries have taken in order to control obesity?
- The government should play an important role in controlling obesity. What precautions should they take?
- Do you think obesity can be one of the reasons children get bullied?
- Do obese people experience any sort of discrimination or inappropriate behavior due to their weight?
- Are there any legal protections for people who suffer from discrimination due to their weight?
- Which communities have a higher percentage of obesity in the United States?
- Discuss the side effects of the fast-food industry and their advertisements on children.
- Describe how the increasing obesity rate has affected the economic condition of the United States.
- What is the current percentage of obesity all over the world? Is the obesity rate increasing with every passing day?
- Why is the obesity rate higher in the United States as compared to other countries?
- Do Asians have a greater percentage of obese people as compared to Europe?
- Does the cultural difference affect the eating habits of an individual?
- Obesity and body shaming.
- Why is a skinny body considered to be ideal? Is it an effective way to reduce the obesity rate?
Obesity Solution Essay Topics
With all the developments in medicine and technology, we still don’t have exact measures to treat obesity.
Here are some insights you can discuss in your essay:
- How do obese people suffer from metabolic complications?
- Describe the fat distribution in obese people.
- Is type 2 diabetes related to obesity?
- Are obese people more prone to suffer from diabetes in the future?
- How are cardiac diseases related to obesity?
- Can obesity affect a woman’s childbearing time phase?
- Describe the digestive diseases related to obesity.
- Obesity may be genetic.
- Obesity can cause a higher risk of suffering a heart attack.
- What are the causes of obesity? What health problems can be caused if an individual suffers from obesity?
- What are the side effects of surgery to overcome obesity?
- Which drugs are effective when it comes to the treatment of obesity?
- Is there a difference between being obese and overweight?
- Can obesity affect the sociological perspective of an individual?
- Explain how an obesity treatment works.
- How can the government help people to lose weight and improve public health?
Writing an essay is a challenging yet rewarding task. All you need is to be organized and clear when it comes to academic writing.
- Choose a topic you would like to write on.
- Organize your thoughts.
- Pen down your ideas.
- Compose a perfect essay that will help you ace your subject.
- Proofread and revise your paper.
Were the topics useful for you? We hope so!
However, if you are still struggling to write your paper, you can pick any of the topics from this list, and our essay writer will help you craft a perfect essay.
Are you struggling to write an effective essay?
If writing an essay is the actual problem and not just the topic, you can always hire an essay writing service for your help. Essay experts at 5StarEssays can help compose an impressive essay within your deadline.
All you have to do is contact us. We will get started on your paper while you can sit back and relax.
Place your order now to get an A-worthy essay.

Marketing, Thesis
As a Digital Content Strategist, Nova Allison has eight years of experience in writing both technical and scientific content. With a focus on developing online content plans that engage audiences, Nova strives to write pieces that are not only informative but captivating as well.
Was This Blog Helpful?
Keep reading.
- How to Write A Bio – Professional Tips and Examples

- Learn How to Write an Article Review with Examples

- How to Write a Poem Step-by-Step Like a Pro

- How To Write Poetry - 7 Fundamentals and Tips

- Know About Appendix Writing With the Help of Examples

- List of Social Issues Faced By the World

- How To Write A Case Study - Easy Guide

- Learn How to Avoid Plagiarism in 7 Simple Steps

- Writing Guide of Visual Analysis Essay for Beginners

- Learn How to Write a Personal Essay by Experts

- Character Analysis - A Step By Step Guide

- Thematic Statement: Writing Tips and Examples

- Expert Guide on How to Write a Summary

- How to Write an Opinion Essay - Structure, Topics & Examples

- How to Write a Synopsis - Easy Steps and Format Guide

- Learn How To Write An Editorial By Experts

- How to Get Better at Math - Easy Tips and Tricks

- How to Write a Movie Review - Steps and Examples

- Creative Writing - Easy Tips For Beginners

- Types of Plagiarism Every Student Should Know

People Also Read
- informative speech topics
- creative essay writers
- lab report writing
- types of research
- literary analysis essay topics
Burdened With Assignments?
Advertisement
- Homework Services: Essay Topics Generator
© 2024 - All rights reserved

Obesity in America: A Public Health Crisis
Obesity is a public health issue that impacts more than 100 million adults and children in the U.S.
What You Need to Know About Obesity

Getty Images
Obesity has become a public health crisis in the United States. The medical condition, which involves having an excessive amount of body fat, is linked to severe chronic diseases including type 2 diabetes, cardiovascular disease, high blood pressure and cancer. It causes about 1 in 5 deaths in the U.S. each year – nearly as many as smoking, according to a study published in the American Journal of Public Health.
The financial cost of obesity is high as well. According to the U.S. Centers for Disease Control and Prevention , "The estimated annual medical cost of obesity in the United States was $147 billion in 2008 U.S. dollars; the medical cost for people who have obesity was $1,429 higher than those of normal weight."
While researchers say the obesity epidemic began in the U.S. in the 1980s, there has been a sharp increase in obesity rates in the U.S. over the last decade. Nearly 40% of all adults over the age of 20 in the U.S. – about 93.3 million people – are currently obese, according to data published in JAMA in 2018. Every state in the U.S. has more than 20% of adults with obesity, according to the CDC – a significant uptick since 1985, when no state had an obesity rate higher than 15%. Certain states have higher rates than others: there are more obese people living in the South (32.4%) and Midwest (32.3%) than in other parts of the country.
Sugar Taxes and Other Efforts to Reduce Obesity
Federal, state and local governments have moved to address obesity in several ways. On the federal level, several programs – such as the Supplemental Nutrition Assistance Program (SNAP), Women, Infants and Children (WIC) Program, Child and Adult Care Food Program (CACFP) and the Healthy Food FInancing Initiative – as well as the U.S. Departments of Agriculture and Health and Human Services work to make healthier foods affordable and available in underserved communities. To prevent childhood obesity in particular, there are also school and early childhood policies, such as Head Start – a comprehensive early childhood education program – school-based physical education and Safe Routes to School, which promotes walking and biking to and from school and increasing healthy eating and physical activity while reducing the risk of obesity.
In March, the American Academy of Pediatrics and the American Heart Association offered several public policy recommendations , including raising the price of sugary drinks, encouraging federal and state governments to limit the marketing of sugary drinks to kids and teenagers, having vending machines offer water, milk and other healthy beverages, improving nutritional information on labels, restaurant menus and advertisements, and supporting hospitals in establishing policies to discourage the purchase of sugary drinks in their facilities.
Meanwhile, states have implemented laws, largely through early childhood education settings, to improve access to healthy food and increase physical activity in order to promote a healthy weight. These policies stretch from breastfeeding, providing available drinking water and daily physical activity to limited screen time as well as meals and snacks that meet healthy eating standards set by the USDA or CACFP.
City governments have considered, and in some cases implemented, so-called "sin taxes" that aim to make potentially unhealthy food choices less attractive and accessible. Cities including Philadelphia, Boulder, Colorado, and Berkeley, California, levy a tax on sugar-sweetened beverages; The American Public Health Association noted in 2016 that the tax led to a 21% drop in the consumption of sugary drinks in Berkeley alone. (A proposal to expand it to all of California stalled this year .) In Philadelphia , the price of sugary beverages sold in supermarkets, mass merchandisers and pharmacies rose – and sales fell – after the city implemented a tax on those products, but a study found that sales in towns bordering Philadelphia increased.
Some researchers say there's little proof that taxing food or drink choices really changes behavior. In spite of taxes and warnings about the health effects of drinking sugary beverages, eight of every 10 American households buys sodas and other sugary drinks each week, adding up to 2,000 calories per household per week, new research shows .
"Large authoritative systematic reviews of the peer-reviewed scientific literature have failed to illustrate any compelling evidence that economic interventions are effective in promoting any type of dietary behavior change," says Taylor Wallace , principal and CEO of the Think Healthy Group and an adjunct professor in the department of nutrition and food studies at George Mason University.
But others contend that making it more expensive to buy sugary drinks is a step in the right direction.
"We need to ensure that people understand the threat of these products to their health, so they want to reduce their consumption," says Sandra Mullin, senior vice president of policy, advocacy and communication for Vital Strategies, an organization that works to implement health initiatives, and a former public health official in New York City "And [hiking] the price is a prompt for them to do that."
Learn more about obesity:
What is obesity?
Obesity is a chronic disease . It occurs when an excessive amount of body fat affects a person's overall health.
How is obesity diagnosed?
According to the Obesity Action Coalition , a healthcare provider may diagnose a patient with obesity if his or her body mass index, or BMI, is 30 or greater. BMI is a value derived from the weight and height of a person; normal BMI ranges from 20 to 25. There is no lab test, blood screening or other diagnostic used to diagnose obesity.
What is morbid obesity?
Morbid obesity is diagnosed when a person has a BMI of 40 or greater. People can also be diagnosed with morbid obesity if their BMI is 35 if they are also experiencing health complications like high blood pressure or diabetes.
How is being overweight different from being obese?
Obesity has to do with having too much body fat and a Body Mass Index, or BMI, of 30 or more. Being overweight can involve having too much body fat, the Department of Health and Human Services says , but having extra muscle, bone or water can also be a factor.
What causes obesity?
Obesity occurs when a person takes in more calories than he or she burns through normal daily activities and exercise, according to the Mayo Clinic . It is not simply a matter of over-indulgence or a lack of self control, obesity researcher Dr. George Bray said at the first annual U.S. News Combating Childhood Obesity summit , held at Texas Children's Hospital in May.
"Obesity isn't a disease of willpower – it's a biological problem," he said . "Genes load the gun, and environment pulls the trigger."
Certain scientific and societal factors – including genetics, the increased consumption of processed foods and sugar-sweetened beverages, and some medications and medical conditions – can increase a person's risk of becoming obese. Age and pregnancy can also trigger weight gain.
The 10 Fattest States in the U.S.

Diet has an important connection to obesity. Studies show the amount of soybean oil Americans consume spiked in the 1960s and 1970s, most likely as highly processed foods became popular, and American adults and children started to weight more around that time, Bray said.
"The fats in our food supply may well be playing a part in our inability to regulate" food intake, Bray said at the obesity summit . Consumption of sugary soft drinks also skyrocketed between 1950 and 2000, he pointed out, as Americans tripled the amount of sweet beverages they drank each year.
Artificial sweeteners have also been linked to obesity . A study presented at the 2018 Experimental Biology meeting suggests artificial sweeteners alter how bodies process fat and obtain energy.
"Despite the addition of these non-caloric artificial sweeteners to our everyday diets, there has still been a drastic rise in obesity and diabetes," one of the study's authors, Brian Hoffmann, assistant professor in the department of biomedical engineering at the Medical College of Wisconsin and Marquette University , said. "In our studies, both sugar and artificial sweeteners seem to exhibit negative effects linked to obesity and diabetes, albeit through very different mechanisms from each other."
What are some of the risk factors for obesity?
Genetic factors include: the amount of body fat a person stores, where it's distributed and how efficiently his or her body metabolizes food into energy.
Medical conditions include: Prader-Willi syndrome, Cushing's syndrome, arthritis and other diseases that can lead to decreased activity. Certain medications – some antidepressants, anti-seizure, diabetes, antipsychotic medications, steroids and beta blockers – can also cause weight gain.
Lifestyle and behavioral factors include: a lack of physical activity that burns calories, smoking, lack of sleep (which can lead to an increased desire to consume calories), eating an unhealthy diet.
Social and economic factors include: not having a safe space to exercise, not having enough money to afford healthier foods, food deserts where grocery stores that carry fresh fruits and vegetables are not available, lack of transportation to access healthy food options.
Can children be obese?
Obesity can be diagnosed at any age. The prevalence of obesity among children and adolescents between ages 2 and 19 was estimated to be 18.5% – more than one in six – between 2015 and 2016, with 13.7 million impacted, according to the CDC's National Center for Health Statistics .
Children who are obese are at risk for developing premature heart disease , the American Heart Association reports. A study of nearly 2.3 million people monitored over the course of 40 years found that the risk of dying from heart disease was two to three times higher if they had been overweight or obese as teens.
Obesity is a problem in other countries as well. A study published in the Lancet in 2017 found that the number of obese 5 to 19 year olds worldwide increased from 11 million in 1975 and to 124 million in 2016. The researchers projected the number of children and adolescents who are obese will surpass those that are moderately or severly underweight by 2022.
How many adult men and women are obese?
U.S. adult obesity prevalence between 2015 and 2016 was nearly 40% – about 93.3 million people, according to the CDC . The highest rate (42.8%) was among adults between the ages of 40 and 59; the prevalence among adults age 20 to 39 years was 35.7%, and 41% among adults age 60 and older. There was no significant difference between men and women overall or by age group, according to the data brief.
What preventable diseases and health issues are associated with obesity?
Mental and physical health problems involving obesity include:
- Type 2 diabetes
- High blood pressure
- Heart disease
- Gallbladder disease
- Cancers (including breast, liver, pancreas, endometrial, colorectal, prostate and kidney)
- High cholesterol
- Osteoarthritis of weight-bearing joints
- Sleep apnea
- Respiratory problems
- Gastroesophageal reflux disease
- Urinary stress incontinence
- Infertility
- Sexual dysfunction
- Physical disability
- Lower work achievement
- Social isolation
What are the financial costs of obesity in the U.S.?
Researchers from the University of Cincinnati in 2008 estimated the cost of medical care to diagnose and treat obesity and its associated health issues to be about $147 billion annually.
The CDC estimates the indirect costs of obesity-related health issues – including absenteeism, premature disability, declines in productiving and earlier mortality – to range from $3 billion and $6.4 billion annually.
Are certain races more likely to become obese than others?
At 25.8%, Hispanic children and adolescents between the ages of 2 and 19 had the highest prevalence of obesity between 2015 and 2016, according to the National Center for Health Statistics . Meanwhile, obesity prevalence was about 22% among black youths; 14.1% among non-Hispanic whites; and 11% among non-Hispanic Asians. While the report notes that there were no significant differences in the prevalence of obesity between boys and girls by race and Hispanic origin, Hispanic boys in particular had a higher prevalence of obesity than non-Hispanic black boys.
Similarly, non-hispanic black (46.8%) and Hispanic (47%) adults in the U.S. have higher obesity rates than non-Hispanic white (37.9%) and non-Hispanic Asian (12.7%) adults, according to the NCHS. Rates of obesity were especially high among black and Hispanic women, according to the report, surpassing 50%.
How is obesity treated?
Treatment of obesity primarily involves changing a patient's behavior, but surgery to reduce the size of a patient's stomach or alter the digestive tract and medication may also be options for those who have trouble losing weight on their own.
The National Institute of Diabetes and Digestive and Kidney Diseases says common treatments include eating more healthy foods, incorporating more physical activity and changing other habits , such as taking the stairs instead of the elevator. Developing a healthy eating plan with fewer calories, setting realistic and measurable goals, participating in formal weight-management programs and seeking help from family, friends, health professionals and support groups can make it easier to develop healthier habits, though the federal agency warns that setbacks occur and people should be prepared.
Experts say obese patients who lose 5% to 10% of their body weight – about 10 to 20 pounds for a 200-lb person with a BMI indicating obesity, for example – can reduce his or her risk of obesity-related health problems like type 2 diabetes as well as lower blood pressure and cholesterol levels.
Can obesity be prevented?
When it comes to suggestions about how to prevent obesity, common principles stand out across local, state and federal guidelines :
- increase physical activity
- improve nutrition through increased consumption of fruits and vegetables
- encourage breastfeeding
- encourage mobility between work, school and communities.
Some researchers also say that the food industry has a role to play in solving the obesity crisis: Making highly processed and fast food much more expensive could curb consumption and lower the obesity rate in the U.S. over time.
"My former brethren in the soft drink business really fought the issue of obesity early on rather than stepping up and saying, 'OK, we don't wish to be blamed totally for this issue but we still can do something,'" Hank Cardello, a former food company executive who now works as a food policy analyst at the Hudson Institute, a Washington, D.C. think tank, said during the U.S. News Combating Childhood Obesity summit in May. "Larger portions, the whole supersize phenomenon – it's actually proven that that made more money for them" while helping trigger the national obesity epidemic, he explained.
What are the most-obese states in America?
According to the CDC, as of 2017 (the most-recent data available) the most-obese states in America are:
- West Virginia (38.1% of adults)
- Mississippi (37.3%)
- Oklahoma (36.5%)
- Iowa (36.4%)
- Alabama (36.2%)
- Louisiana (36.2%)
- Arkansas (35%)
- Kentucky (34.3%)
- Alaska (34.2%)
- South Carolina (34.1%)
What are the least-obese states in America?
These states have the lowest obesity rates in the U.S., according to the CDC:
- Colorado (22.6% of adults)
- Hawaii (23.8%)
- California (25.1%)
- Utah (25.25%)
- Montana (25.27%)
- New York (25.7%)
- Massachuestts (25.9%)
- Nevada (26.7%)
- Connecticut (26.9%)
- New Jersey (27.3%)
Is obesity a problem in other countries?
The World Health Organization estimates 39% of women and 39% of men ages 18 and older are overweight, with the highest prevalence of obesity on the island of Nauru, at 61%. (The U.S. ranked 12th worldwide, at 36.2%).
Among the 20 most-populous countries worldwide, the United States had the highest level of age-standardized childhood obesity, at 12.7%, while China and India had the highest numbers of obese children in 2015, according to a 2017 University of Washington study . Further, the United States and China had the highest number of obese adults, the study found. That same year, the researchers determined excess body weight to be associated with about 4 million deaths and 120 million disability-adjusted life-years lost.
Rates of adult obesity among the 36 countries in the Organization for Economic Cooperation were highest in the U.S., Mexico, New Zealand and Hungary. They were lowest in Japan and South Korea in 2017, according to an OECD "Obesity Update" report .
Tags: obesity , weight loss , public health
Recommended Articles
Healthiest Communities Health News

Healthiest Communities

- # 1 Los Alamos County, NM
- # 2 Falls Church city, VA
- # 3 Douglas County, CO
- # 4 Morgan County, UT
- # 5 Carver County, MN
You May Also Like
50 years after the former yugoslavia protected abortion rights, that legacy is under threat.
Associated Press March 27, 2024

Senior Doctors in South Korea Submit Resignations, Deepening Dispute Over Medical School Plan
Associated Press March 24, 2024

Kate and William 'Extremely Moved' by Support Since the Princess of Wales' Cancer Revelation

UN Chief Says It's Time to 'Truly Flood' Gaza With Aid and Calls Starvation There an Outrage
Associated Press March 23, 2024

What Is Known About Kate's Cancer Diagnosis
Associated Press March 22, 2024


Prevention, prevention, prevention.
Losing weight is hard to do.
In the U.S., only one in six adults who have dropped excess pounds actually keep off at least 10 percent of their original body weight. The reason: a mismatch between biology and environment. Our bodies are evolutionarily programmed to put on fat to ride out famine and preserve the excess by slowing metabolism and, more important, provoking hunger. People who have slimmed down and then regain their weight don’t lack willpower—their bodies are fighting them every inch of the way.
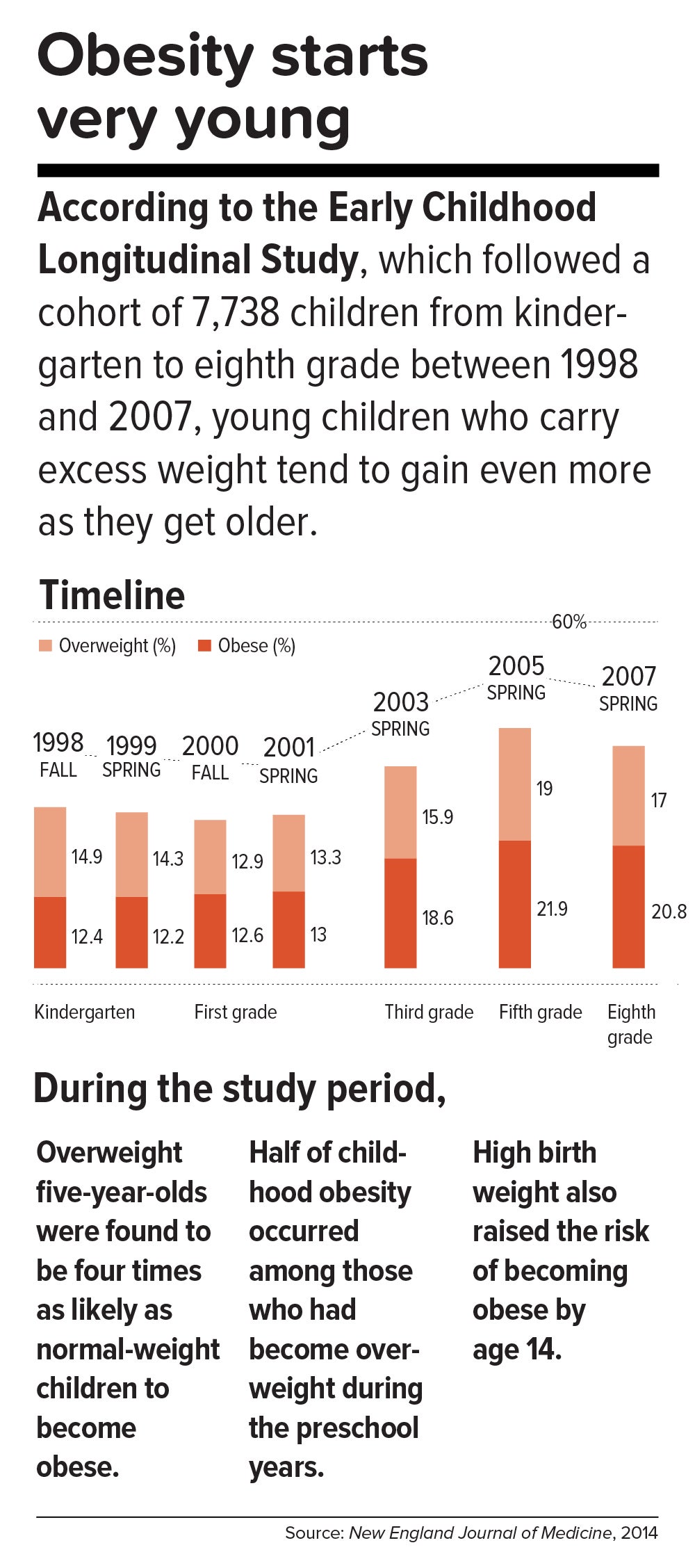
This inborn predisposition to hold on to added weight reverberates down the life course. Few children are born obese, but once they become heavy, they are usually destined to be heavy adolescents and heavy adults. According to a 2016 study in the New England Journal of Medicine , approximately 90 percent of children with severe obesity will become obese adults with a BMI of 35 or higher. Heavy young adults are generally heavy in middle and old age. Obesity also jumps across generations; having a mother who is obese is one of the strongest predictors of obesity in children.
All of which means that preventing child obesity is key to stopping the epidemic. By the time weight piles up in adulthood, it is usually too late. Luckily, preventing obesity in children is easier than in adults, partly because the excess calories they absorb are minimal and can be adjusted by small changes in diet—substituting water, for example, for sugary fruit juices or soda.
Still, the bulk of the obesity problem—literally—is in adults. According to Frank Hu, chair of the Harvard Chan Department of Nutrition, “Most people gain weight during young and middle adulthood. The weight-gain trajectory is less than 1 pound per year, but it creeps up steadily from age 18 to age 55. During this time, people gain fat mass, not muscle mass. When they reach age 55 or so, they begin to lose their existing muscle mass and gain even more fat mass. That’s when all the metabolic problems appear: insulin resistance, high cholesterol, high blood pressure.”
Adds Walter Willett, Frederick John Stare Professor of Epidemiology and Nutrition at Harvard Chan, “The first 5 pounds of weight gain at age 25—that’s the time to be taking action. Because someone is on a trajectory to end up being 30 pounds overweight by the time they’re age 50.”
The most realistic near-term public health goal, therefore, is not to reverse but rather to slow down the trend—and even this will require strong commitment from government at many levels. In May 2017, the Trump administration rolled back recently-enacted standards for school meals, delaying a rule to lower sodium and allowing waivers for regulations requiring cafeterias to serve foods rich in whole grains. If recent expansions in food entitlements and school meals are undermined, “It would be a ‘disaster,’ to use the president’s word,” says Marlene Schwartz, director of the Rudd Center for Obesity & Food Policy at the University of Connecticut. “The federal food programs are incredibly important, not just because of the food and money they provide families, but because supporting better nutrition in child care, schools, and the WIC [Women, Infants, and Children] program has created new social norms. We absolutely cannot undo the progress that we’ve made in helping this generation transition to a healthier diet.”

Get the science right.
It is impossible to prescribe solutions to obesity without reminding ourselves that nutrition scientists botched things decades ago and probably sent the epidemic into overdrive. Beginning in the 1970s, the U.S. government and major professional groups recommended for the first time that people eat a low-fat/high-carbohydrate diet. The advice was codified in 1977 with the first edition of The Dietary Goals for the United States , which aimed to cut diet-related conditions such as heart disease and diabetes. What ensued amounted to arguably the biggest public health experiment in U.S. history, and it backfired.
At the time, saturated fat and dietary cholesterol were believed to be the main factors responsible for cardiovascular disease—an oversimplified theory that ignored the fact that not all fats are created equal. Soon, the public health blitz against saturated fat became a war on all fat. In the American diet, fat calories plummeted and carb calories shot up.
“We can’t blame industry for this. It was a bandwagon effect in the scientific community, despite the lack of evidence—even with evidence to the contrary,” says Willett. “Farmers have known for thousands of years that if you put animals in a pen, don’t let them run around, and load them up with grains, they get fat. That’s basically what has been happening to people: We created the great American feedlot. And we added in sugar, coloring, and seductive promotion for low-fat junk food.”
Scientists now know that whole fruits and vegetables (other than potatoes), whole grains, high-quality proteins (such as from fish, chicken, beans, and nuts), and healthy plant oils (such as olive, peanut, or canola oil) are the foundations of a healthy diet.
But there is also a lot scientists don’t yet know. One unanswered question is why some people with obesity are spared the medical complications of excess weight. Another concerns the major mechanisms by which obesity ushers in disease. Although surplus body weight can itself directly cause problems—such as arthritis due to added load on joints, or breast cancer caused by hormones secreted by fat cells—in general, obesity triggers myriad biological processes. Many of the resulting conditions—such as atherosclerosis, diabetes, and even Alzheimer’s disease—are mediated by inflammation, in which the body’s immune response becomes damagingly self-perpetuating. In this sense, today’s food system is as inflammagenic as it is obesigenic.
Scientists also need to ferret out the nuanced effects of particular foods. For example, do fermented products—such as yogurt, tempeh, or sauerkraut—have beneficial properties? Some studies have found that yogurt protects against weight gain and diabetes, and suggest that healthy live bacteria (known as probiotics) may play a role. Other reports point to fruits being more protective than vegetables in weight control and diabetes prevention, although the types of fruits and vegetables make a difference.
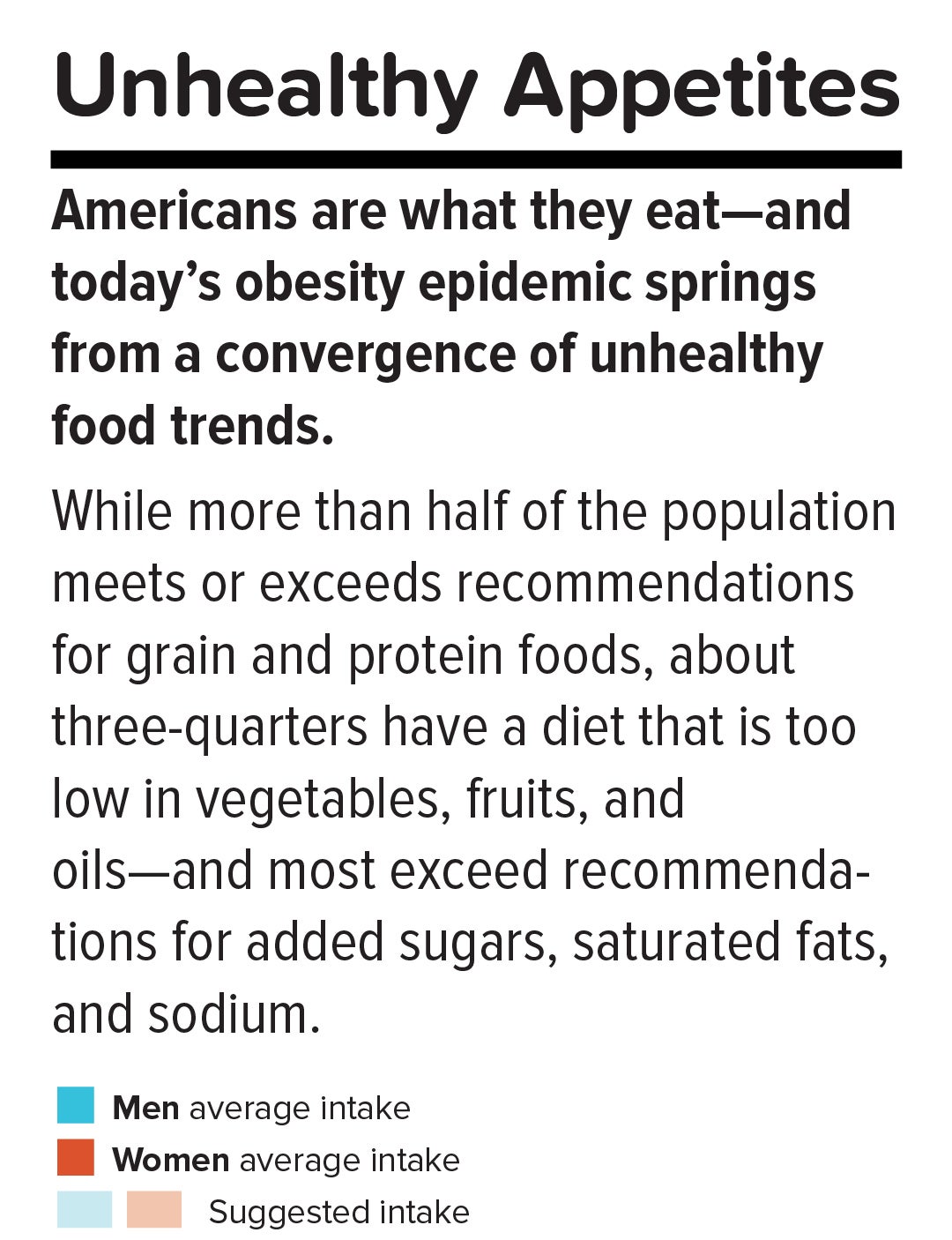
A 2017 article in the American Journal of Clinical Nutrition showed that substituting whole grains for refined grains led to a loss of nearly 100 calories a day—by speeding up metabolism, cutting the number of calories that the body hangs on to, and, more surprisingly, by changing the digestibility of other foods on the plate. That extra energy lost daily—by substituting, say, brown rice for white rice or barley for pita bread—was equivalent to a brisk 30-minute walk. One hundred calories a day, sustained over years, and multiplied by the population is one mathematical equivalent of the obesity epidemic.
A companion study found that adults who ate a whole-grain-rich diet developed healthier gut bacteria and improved immune responses. That particular foods alter the gut microbiome—the dense and vital community of bacteria and other microorganisms that work symbiotically with the body’s own digestive system—is another critical insight. The microbiome helps determine weight by controlling how our bodies extract calories and store fat in the liver, and the microbiomes of obese individuals are startlingly efficient at harvesting calories from food. [To learn more about Harvard Chan research on the gut microbiome, read “ Bugs in the System .”] The hormonal effects of sleep deprivation and stress—two epidemics concurrent and intertwined with the obesity trend—are other promising avenues of research.
And then there are the mystery factors. One recent hypothesis is that an agent known as adenovirus 36 partly accounts for our collective heft. A 2010 article in The Royal Society described a study in which researchers examined samples of more than 20,000 animals from eight species living with or around humans in industrialized nations, a menagerie that included macaques, chimpanzees, vervets, marmosets, lab mice and rats, feral rats, and domestic dogs and cats. Like their Homo sapiens counterparts, all of the study populations had gained weight over the past several decades—wild, domestic, and lab animals alike. The chance that this is a coincidence is, according to the scientists’ estimate, 1 in 10 million. The stumped authors surmise that viruses, gene expression changes, or “as-of-yet unidentified and/or poorly understood factors” are to blame.
Master the art of persuasion.
A 2015 paper in the American Journal of Public Health revealed the philosophical chasm that hampers America’s progress on obesity prevention. It found that 72 to 98 percent of obesity-related media reports emphasize personal responsibility for weight, compared with 40 percent of scientific papers.
A recent study by Drexel University researchers also quantified the political polarization around public health measures. From 1998 through 2013, Democrats voted in line with recommendations from the American Public Health Association 88.3 percent of the time, on average, while Republicans voted for the proposals just 21.3 percent of the time.
Clearly, we can’t count on bipartisan goodwill to stem the obesity crisis. But we can ask what kinds of messages appeal to politically divergent audiences. A stealth strategy may be to avoid even uttering the word “obesity.” On January 1 of this year, Philadelphia’s 1.5-cents-per-ounce excise tax on sugar-sweetened and diet beverages took effect. When Philadelphia Mayor Jim Kenney lobbied voters to approve the tax, his bid centered not on improving health—the unsuccessful pitch of his predecessor—but on raising $91 million annually for prekindergarten programs.
“That’s something lots of people care about and can get behind—it’s a feel-good policy, and it makes sense,” says psychologist Christina Roberto, assistant professor of medical ethics and health policy at the University of Pennsylvania, and a former assistant professor of social and behavioral sciences and nutrition at Harvard Chan. The provision for taxing diet beverages was also shrewd, she adds, because it spread the tax’s pain; since wealthier people are more likely than less-affluent individuals to buy diet drinks, the tax could not be slapped with the label “regressive.”
But Roberto sees a larger lesson in the Philadelphia story. Public health messaging that appeals to values that transcend the individual is less fraught, less stigmatizing, and perhaps more effective. As she puts it, “It’s very different to hear the message, ‘Eat less red meat, help the planet’ versus ‘Eat less red meat, help yourself avoid saturated fat and cardiovascular disease.’”
Supermarket makeovers
Supermarket aisles are other places where public health can shuffle a deck stacked against healthy consumer choices.
With slim profit margins and 50,000-plus products on their shelves, grocery stores depend heavily on food manufacturers’ promotional incentives to make their bottom lines. “Manufacturers pay slotting fees to get their products on the shelf, and they pay promotion allowances: We’ll give you this much off a carton of Coke if you put it on sale for a certain price or if you put it on an end-of-aisle display,” says José Alvarez, former president and chief executive officer of Stop & Shop/Giant-Landover, now senior lecturer of business administration at Harvard Business School. Such promotional payments, Alvarez adds, often exceed retailers’ net profits.
Healthy new products—like flash-frozen dinners prepared with heaps of vegetables and whole grains, and relatively little salt—can’t compete for prized shelf space against boxed mac and cheese or cloying breakfast cereals. One solution, says Alvarez, is for established consumer packaged goods companies to buy out what he calls the “hippie in the basement” firms that have whipped up more nutritious items. The behemoths could apply their production, marketing, and distribution prowess to the new offerings—and indeed, this has started to happen over the last five years.
Another approach is to make nutritious foods more convenient to eat. “We have all of these cooking shows and upscale food magazines, but most people don’t have the time or inclination—or the skills, quite frankly—to cook,” says Alvarez. “Instead, we should focus on creating high-quality, healthy, affordable prepared foods.”
An additional model is suggested by Jeff Dunn, a 20-year veteran of the soft drink industry and former president of Coca-Cola North America, who went on to become an advocate for fresh, healthy food. Dunn served as president and chief executive officer of Bolthouse Farms from 2008 to 2015, where he dramatically increased sales of baby carrots by using marketing techniques common in the junk food business. “We operated on the principles of the three 3 A’s: accessibility, availability, and affordability,” says Dunn. “That, by the way, is Coke’s more-than-70-year-old formula for success.”
Show them the money.
Obesity kills budgets. According to the Campaign to End Obesity, a collaboration of leaders from industry, academia, public health, and policymakers, annual U.S. health costs related to obesity approach $200 billion. In 2010, the nonpartisan Congressional Budget Office reported that nearly 20 percent of the rise in health care spending from 1987 to 2007 was linked to obesity. And the U.S. Centers for Disease Control and Prevention (CDC) found that full-time workers in the U.S. who are overweight or obese and have other chronic health conditions miss an estimated 450 million more days of work each year than do healthy employees—upward of $153 billion in lost productivity annually.
But making the money case for obesity prevention isn’t straightforward. For interventions targeting children and youth, only a small fraction of savings is captured in the first decade, since most serious health complications don’t emerge for many years. Long-term obesity prevention, in other words, doesn’t fit into political timetables for elected officials.
Yet lawmakers are keen to know how “best for the money” obesity-prevention programs can help them in the short run. Over the past two years, Harvard Chan’s Steve Gortmaker and his colleagues have been working with state health departments in Alaska, Mississippi, New Hampshire, Oklahoma, Washington, and West Virginia and with the city of Philadelphia and other locales, building cost-effectiveness models using local data for a wide variety of interventions—from improved early child care to healthy school environments to communitywide campaigns. “We collaborate with health departments and community stakeholders, provide them with the evidence base, help assess how much different options cost, model the results over a decade, and they pick what they want to work on. One constant that we’ve seen—and these are very different political environments—is a strong interest in cost-effectiveness,” he says.
In a 2015 study in Health Affairs , Gortmaker and colleagues outlined three interventions that would more than pay for themselves: an excise tax on sugar-sweetened beverages implemented at the state level; elimination of the tax subsidy for advertising unhealthy food to children; and strong nutrition standards for food and drinks sold in schools outside of school meals. Implemented nationally, these interventions would prevent 576,000, 129,100, and 345,000 cases of childhood obesity, respectively, by 2025. The projected net savings to society in obesity-related health care costs for each dollar invested: $31, $33, and $4.60, respectively.
Gortmaker is one of the leaders of a collaborative modeling effort known as CHOICES—for Childhood Obesity Intervention Cost-Effectiveness Study—an acronym that seems a pointed rebuttal to the reflexive conservative argument that government regulation tramples individual choice. Having grown up not far from Des Plaines, Illinois, site of the first McDonald’s franchise in the country, he emphasizes to policymakers that at this late date, America cannot treat its way out of obesity, given current medical know-how. Only a thoroughgoing investment in prevention will turn the tide. “Clinical interventions produce too small an effect, with too small a population, and at high cost,” Gortmaker says. “The good news is that there are many cost-effective options to choose from.”
While Gortmaker underscores the importance of improving both food choices and options for physical activity, he has shown that upgrading the food environment offers much more benefit for the buck. This is in line with the gathering scientific consensus that what we eat plays a greater role in obesity than does sedentary lifestyle (although exercise protects against many of the metabolic consequences of excess weight). “The easiest way to explain it,” Gortmaker says, “is to talk about a sugary beverage—140 calories. You could quickly change a kid’s risk of excess energy balance by 140 calories a day just by switching from a sugary drink a day to water or sparkling water. But for a 10-year-old boy to burn an extra 140 calories, he’d have to replace an hour-and-a-half of sitting with an hour-and-a-half of walking.”
Small tweaks in adults’ diets can likewise make a big difference in short order. “With adults, health care costs rise rapidly with excess weight gain,” Gortmaker says. “If you can slow the onset of obesity, you slow the onset of diabetes, and potentially not only save health care costs but also boost people’s productivity in the workforce.”
One of Gortmaker’s most intriguing calculations spins off of the food industry’s estimated $633 million spent on television marketing aimed at kids. Currently, federal tax treatment of advertising as an ordinary business expense means that the government, in effect, subsidizes hawking of junk food to children. Gortmaker modeled a national intervention that would eliminate this subsidy of TV ads for nutritionally empty foods and beverages aimed at 2- to 19-year-olds. Drawing on well-delineated relationships between exposure to these advertisements and subsequent weight gain, he found that the intervention would save $260 million in downstream health care costs. Although the effect would probably be small at the individual level, it would be significant at the population level.
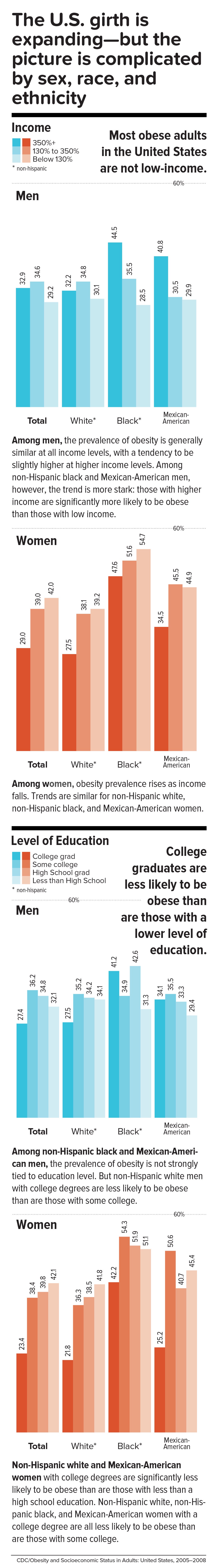
Level the playing field through taxes and regulation.
When public health took on cigarette smoking, starting in the 1960s, it did so with robust policies banning television ads and other marketing, raising taxes to increase prices, making public places smoke-free, and offering people treatment such as the nicotine patch. In 1965, the smoking rate for U.S. adults was 42.2 percent; today, it is 16.8 percent.
Similarly, America reduced the rate of deaths caused by motor vehicle accidents—a 90 percent decrease over the 20th century, according to the CDC—with mandatory seat belt laws, safer car designs, stop signs, speed limits, rumble strips, and the stigmatization of drunk driving.
Change the product. Change the environment. Change the culture. That is also the policy recipe for stopping obesity.
Laws that make healthy behaviors easier are often followed by positive changes in those behaviors. And people who are trying to adopt healthy behaviors tend to support policies that make their personal aspirations achievable, which in turn nudges lawmakers to back the proposals.
One debate today revolves around whether recipients of federal Supplemental Nutrition Assistance Program (SNAP) benefits (formerly known as food stamps) should be restricted from buying sodas or junk food. The largest component of the USDA budget, SNAP feeds one in seven Americans. A USDA report, issued last November, found that the number-one purchase by SNAP households was sweetened beverages, a category that included soft drinks, fruit juices, energy drinks, and sweetened teas, accounting for nearly 10 percent of SNAP money spent on food. Is the USDA therefore underwriting the soda industry and planting the seeds for chronic disease that the government will pay to treat years down the line?
Eric Rimm, a professor in the Departments of Epidemiology and Nutrition at the Harvard Chan School, frames the issue differently. In a 2017 study in the American Journal of Preventive Medicine , he and his colleagues asked SNAP participants whether they would prefer the standard benefits package or a “SNAP-plus” that prohibited the purchase of sugary beverages but offered 50 percent more money for buying fruits and vegetables. Sixty-eight percent of the participants chose the healthy SNAP-plus option.
“A lot of work around SNAP policy is done by academics and politicians, without reaching out to the beneficiaries,” says Rimm. “We haven’t asked participants, ‘What’s your say in this? How can we make this program better for you?’” To be sure, SNAP is riddled with nutritional contradictions. Under current rules, for example, participants can use benefits to buy a 12-pack of Pepsi or a Snickers bar or a giant bag of Lay’s potato chips but not real food that happens to be heated, such as a package of rotisserie chicken. “This is the most vulnerable population in the country,” says Rimm. “We’re not listening well enough to our constituency.”
Other innovative fiscal levers to alter behavior could also drive down obesity. In 2014, a trio of strong voices on food industry practices—Dariush Mozaffarian, DrPH ’06, dean of Tufts University’s Friedman School of Nutrition Science and Policy and former associate professor of epidemiology at the Harvard Chan School; Kenneth Rogoff, professor of economics at Harvard; and David Ludwig, professor in the Department of Nutrition at Harvard Chan and a physician at Boston Children’s Hospital—broached the idea of a “meaningful” tax on nearly all packaged retail foods and many chain restaurants, with the proceeds used to pay for minimally processed foods and healthier meals for school kids. In essence, the tax externalizes the social costs of harmful individual behavior.
“We made a straightforward proposal to tax all processed foods and then use the income to subsidize whole foods in a short-term, revenue-neutral way,” explains Ludwig. “The power of this idea is that, since there is so much processed food consumption, even a modest tax—in the 10 to 15 percent range—is not going to greatly inflate the cost of these foods. Their price would increase moderately, but the proceeds would not disappear into government coffers. Instead, the revenue would make healthy foods affordable for virtually the entire population, and the benefits would be immediately evident. Yes, people will pay moderately more for their Coke or for their cinnamon bear claw but a lot less for nourishing, whole foods.”
Another suggestion comes from Sandro Galea, dean of the Boston University School of Public Health, and Abdulrahman M. El-Sayed, a public health physician and epidemiologist. In a 2015 issue of the American Journal of Public Health , they called for “calorie offsets,” similar to the carbon offsets used to mitigate environmental harm caused by the gas and oil industries. A “calorie offset” scheme could hand the food and beverage industries a chance at redemption by inviting them to invest in such undertakings as city farms, cooking classes for parents, healthy school cafeterias, and urban green spaces.
These ambitious proposals face almost impossibly high hurdles. Political battle lines typically pit public health against corporations, with Big Food casting doubt on solid nutrition science, deeming government regulation a threat to free choice, and making self-policing pledges that it has never kept. On the website for the Americans for Food and Beverage Choice, a group spearheaded by the American Beverage Association, is the admonition: “[W]hether it’s at a restaurant or in a grocery store, it’s never the government’s job to decide what you choose to eat and drink.”
Yet surprisingly, many public health professionals are convinced that the only way to stop obesity is to make common cause with the food industry. “This isn’t like tobacco, where it’s a fight to the death. We need the food industry to make healthier food and to make a profit,” says Mozaffarian. “The food industry is much more diverse and heterogeneous than tobacco or even cars. As long as we can help them—through carrots and sticks, tax incentives and disincentives—to move towards healthier products, then they are part of the solution. But we have to be vigilant, because they use a lot of the same tactics that tobacco did.”
Sow what we want to reap.
Americans overeat what our farmers overproduce.
“The U.S. food system is egregiously terrible for human and planetary health,” says Walter Willett. It’s so terrible, Willett made a pie chart of American grain production consumed domestically. It shows that most of the country’s agricultural land goes to the two giant commodity crops: corn and soy. Most of those crops, in turn, go to animal fodder and ethanol, and are also heavily used in processed snack foods. Today, only about 10 percent of grain grown in the U.S. for domestic use is eaten directly by human beings. According to a 2013 report from the Union of Concerned Scientists, only 2 percent of U.S. farmland is used to grow fruits and vegetables, while 59 percent is devoted to commodity crops.
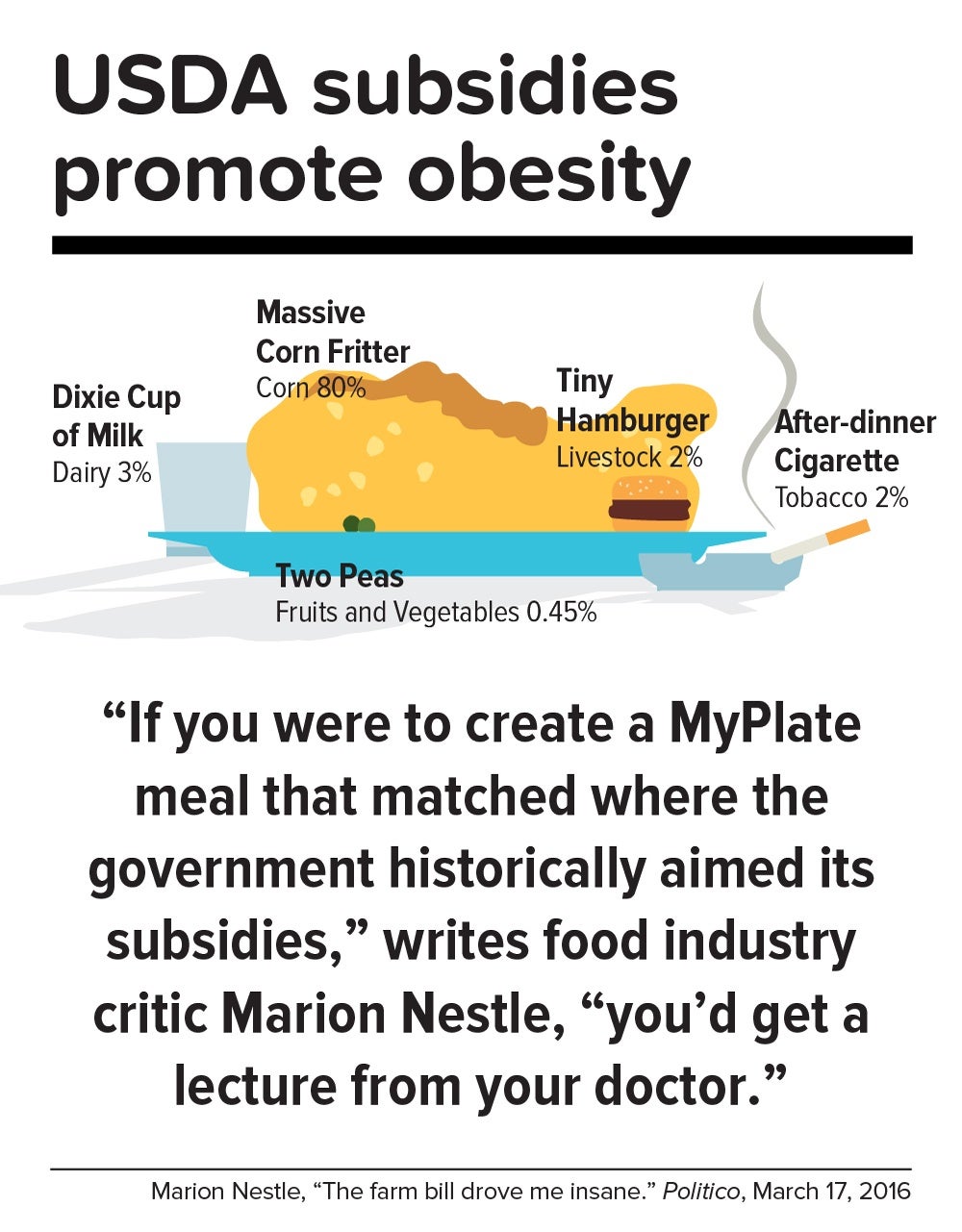
Historically, those skewed proportions made sense. Federal food policies, drafted with the goal of alleviating hunger, preferentially subsidize corn and soy production. And whereas corn or soybeans could be shipped for days on a train, fruits and vegetables had to be grown closer to cities by truck farmers so the produce wouldn’t spoil. But those long-ago constraints don’t explain today’s upside-down agricultural priorities.
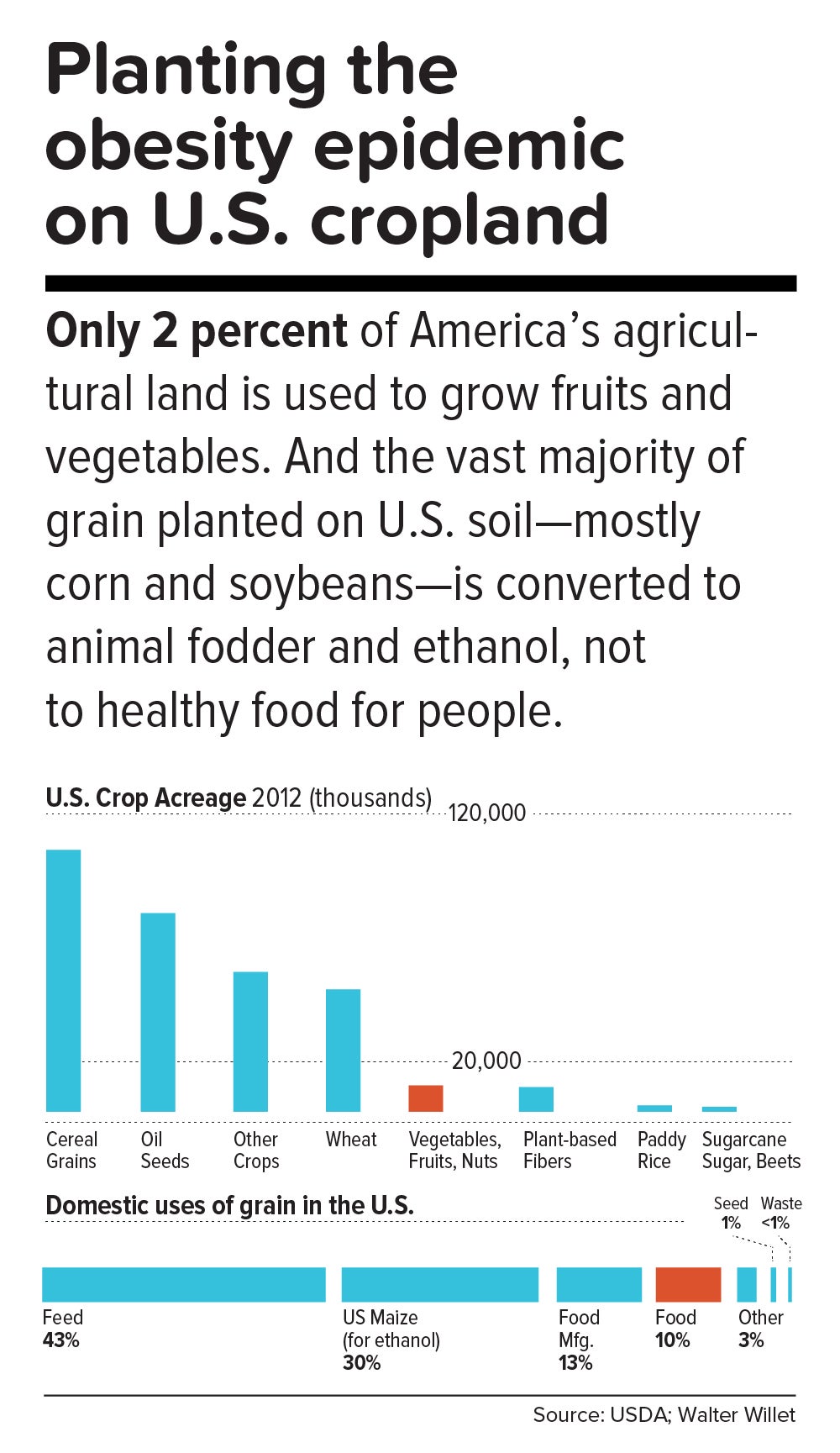
In a now-classic 2016 Politico article titled “The farm bill drove me insane,” Marion Nestle illustrated the irrational gap between what the government recommends we eat and what it subsidizes: “If you were to create a MyPlate meal that matched where the government historically aimed its subsidies, you’d get a lecture from your doctor. More than three-quarters of your plate would be taken up by a massive corn fritter (80 percent of benefits go to corn, grains and soy oil). You’d have a Dixie cup of milk (dairy gets 3 percent), a hamburger the size of a half dollar (livestock: 2 percent), two peas (fruits and vegetables: 0.45 percent) and an after-dinner cigarette (tobacco: 2 percent). Oh, and a really big linen napkin (cotton: 13 percent) to dab your lips.”
In this sense, the USDA marginalizes human health. Many of the foods that nutritionists agree are best for us—notably, fruits, vegetables, and tree nuts—fall under the bureaucratic rubric “specialty crops,” a category that also includes “dried fruits, horticulture, and nursery crops (including floriculture).” Farm bills, which get passed every five years or so, fortify the status quo. The 2014 Farm Bill, for example, provided $73 million for the Specialty Crop Block Grant Program in 2017, out of a total of about $25 billion for the USDA’s discretionary budget. (The next Farm Bill, now under debate, will be coming out in 2018.)
By contrast, a truly anti-obesigenic agricultural system would stimulate USDA support for crop diversity—through technical assistance, research, agricultural training programs, and financial aid for farmers who are newly planting or transitioning their land into produce. It would also enable farmers, most of whom survive on razor-thin profit margins, to make a decent living.
In the early 1970s, Finland’s death rate from coronary heart disease was the highest in the world, and in the eastern region of North Karelia—a pristine, sparsely populated frontier landscape of forest and lakes—the rate was 40 percent worse than the national average. Every family saw physically active men, loggers and farmers who were strong and lean, dying in their prime.
Thus was born the North Karelia Project, which became a model worldwide for saving lives by transforming lifestyles. The project was launched in 1972 and officially ended 25 years later. While its initial goal was to reduce smoking and saturated fat in the diet, it later resolved to increase fruit and vegetable consumption.
The North Karelia Project fulfilled all of these ambitions. When it started, for example, 86 percent of men and 82 percent of women smeared butter on their bread; by the early 2000s, only 10 percent of men and 4 percent of women so indulged. Use of vegetable oil for cooking jumped from virtually zero in 1970 to 50 percent in 2009. Fruit and vegetables, once rare visitors to the dinner plate, became regulars. Over the project’s official quarter-century existence, coronary heart disease deaths in working-age North Karelian men fell 82 percent, and life expectancy rose seven years.
The secret of North Karelia’s success was an all-out philosophy. Team members spent innumerable hours meeting with residents and assuring them that they had the power to improve their own health. The volunteers enlisted the assistance of an influential women’s group, farmers’ unions, homemakers’ organizations, hunting clubs, and church congregations. They redesigned food labels and upgraded health services. Towns competed in cholesterol-cutting contests. The national government passed sweeping legislation (including a total ban on tobacco advertising). Dairy subsidies were thrown out. Farmers were given strong incentives to produce low-fat milk, or to get paid for meat and dairy products based not on high-fat but on high-protein content. And the newly established East Finland Berry and Vegetable Project helped locals switch from dairy farming—which had made up more than two-thirds of agriculture in the region—to cultivation of cold-hardy currants, gooseberries, and strawberries, as well as rapeseed for heart-healthy canola oil.
“A mass epidemic calls for mass action,” says the project’s director, Pekka Puska, “and the changing of lifestyles can only succeed through community action. In this case, the people pulled the government—the government didn’t pull the people.”
Could the United States in 2017 learn from North Karelia’s 1970s grand experiment?
“Americans didn’t become an obese nation overnight. It took a long time—several decades, the same timeline as in individuals,” notes Frank Hu. “What were we doing over the past 20 years or 30 years, before we crossed this threshold? We haven’t asked these questions. We haven’t done this kind of soul-searching, as individuals or society as a whole.”
Today, Americans may finally be willing to take a hard look at how food figures in their lives. In a July 2015 Gallup phone poll of Americans 18 and older, 61 percent said they actively try to avoid regular soda (the figure was 41 percent in 2002); 50 percent try to avoid sugar; and 93 percent try to eat vegetables (but only 57.7 percent in 2013 reported they ate five or more servings of fruits and vegetables at least four days of the previous week).
Individual resolve, of course, counts for little in problems as big as the obesity epidemic. Most successes in public health bank on collective action to support personal responsibility while fighting discrimination against an epidemic’s victims. [To learn more about the perils of stigma against people with obesity, read “ The Scarlet F .”]
Yet many of public health’s legendary successes also took what seems like an agonizingly long time to work. Do we have that luxury?
“Right now, healthy eating in America is like swimming upstream. If you are a strong swimmer and in good shape, you can swim for a little while, but eventually you’re going to get tired and start floating back down,” says Margo Wootan, SD ’93, director of nutrition policy for the Center for Science in the Public Interest. “If you’re distracted for a second—your kid tugs on your pant leg, you had a bad day, you’re tired, you’re worried about paying your bills—the default options push you toward eating too much of the wrong kinds of food.”
But Wootan has not lowered her sights. “What we need is mobilization,” she says. “Mobilize the public to address nutrition and obesity as societal problems—recognizing that each of us makes individual choices throughout the day, but that right now the environment is stacked against us. If we don’t change that, stopping obesity will be impossible.”
The passing of power to younger generations may aid the cause. Millennials are more inclined to view food not merely as nutrition but also as narrative—a trend that leaves Duke University’s Kelly Brownell optimistic. “Younger people have been raised to care about the story of their food. Their interest is in where it came from, who grew it, whether it contributes to sustainable agriculture, its carbon footprint, and other factors. The previous generation paid attention to narrower issues, such as hunger or obesity. The Millennials are attuned to the concept of food systems.”
We are at a public health inflection point. Forty years from now, when we gaze at the high-resolution digital color photos from our own era, what will we think? Will we realize that we failed to address the obesity epidemic, or will we know that we acted wisely?
The question brings us back to the 1970s, and to Pekka Puska, the physician who directed the North Karelia Project during its quarter-century existence. Puska, now 71, was all of 27 and burning with big ideas when he signed up to lead the audacious effort. He knows the promise and the perils of idealism. “Changing the world may have been utopic,” he says, “but changing public health was possible.”
News from the School

Bethany Kotlar, PhD '24, studies how children fare when they're born to incarcerated mothers

Soccer, truffles, and exclamation points: Dean Baccarelli shares his story

Health care transformation in Africa highlighted at conference

COVID, four years in
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

The Epidemiology of Obesity: A Big Picture
The epidemic of overweight and obesity presents a major challenge to chronic disease prevention and health across the life course around the world. Fueled by economic growth, industrialization, mechanized transport, urbanization, an increasingly sedentary lifestyle, and a nutritional transition to processed foods and high calorie diets over the last 30 years, many countries have witnessed the prevalence of obesity in its citizens double, and even quadruple. Rising prevalence of childhood obesity, in particular, forebodes a staggering burden of disease in individuals and healthcare systems in the decades to come. A complex, multifactorial disease, with genetic, behavioral, socioeconomic, and environmental origins, obesity raises risk of debilitating morbidity and mortality. Relying primarily on epidemiologic evidence published within the last decade, this non-exhaustive review discusses the extent of the obesity epidemic, its risk factors—known and novel—, sequelae, and economic impact across the globe.
1. Introduction
Obesity is a complex, multifactorial, and largely preventable disease ( 1 ), affecting, along with overweight, over a third of the world’s population today ( 2 , 3 ). If secular trends continue, by 2030 an estimated 38% of the world’s adult population will be overweight and another 20% will be obese ( 4 ). In the USA, the most dire projections based on earlier secular trends point to over 85% of adults being overweight or obese by 2030 ( 5 ). While growth trends in overall obesity in most developed countries seem to have leveled off ( 2 ), morbid obesity in many of these countries continues to climb, including among children. In addition, obesity prevalence in developing countries continues to trend upwards toward US levels.
Obesity is typically defined quite simply as excess body weight for height, but this simple definition belies an etiologically complex phenotype primarily associated with excess adiposity, or body fatness, that can manifest metabolically and not just in terms of body size ( 6 ). Obesity greatly increases risk of chronic disease morbidity—namely disability, depression, type 2 diabetes, cardiovascular disease, certain cancers—and mortality. Childhood obesity results in the same conditions, with premature onset, or with greater likelihood in adulthood ( 6 ). Thus, the economic and psychosocial costs of obesity alone, as well as when coupled with these comorbidities and sequealae, are striking.
In this article, we outline the prevalence and trends of obesity, then review the myriad risk factors to which a preventive eye must be turned, and finally present the costs of obesity in terms of its morbidity, mortality, and economic burden.
2. Classification of Body Weight in Adults
The current most widely used criteria for classifying obesity is the body mass index (BMI; body weight in kilograms, divided by height in meters squared, Table 1 ), which ranges from underweight or wasting (<18.5 kg/m 2 ) to severe or morbid obesity (≥40 kg/m 2 ). In both clinical and research settings, waist circumference, a measure of abdominal adiposity, has become an increasingly important and discriminating measure of overweight/obesity ( 7 ). Abdominal adiposity is thought to be primarily visceral, metabolically active fat surrounding the organs, and is associated with metabolic dysregulation, predisposing individuals to cardiovascular disease and related conditions ( 8 ). Per internationally used guidelines of metabolic syndrome—a cluster of dysmetabolic conditions that predispose individuals to cardiovascular disease of which abdominal adiposity is one component—a waist circumference resulting in increased cardiovascular risk is defined as ≥94 cm in European men, and ≥80 cm in European women, with different cut points recommended in other races and ethnicities (e.g., ≥90 and ≥80 cm in men and women, respectively, in South Asians, Chinese, and Japanese) ( 8 , 9 ).
Common Classifications of Body Weight in Adults and Children
Abbreviations used: BMI, body mass index; IOTF, International Obesity Task Force; SD, standard deviation; WHO, World Health Organization; WH weight-for-height; Z, z score.
3. Classification of Body Weight in Children
In children, body weight classifications ( Table 1 ) differ from those of adults because body composition varies greatly as a child develops, and further varies between boys and girls primarily owing to differences in sexual development and maturation. The World Health Organization (WHO) Child Growth Standards are the most widely currently used classification system of weight and height status for children from birth to 5 years old, based on data from children in six regions across the globe born and raised in optimal conditions ( 10 ). In 2007, the WHO published updated growth references combining the 1977 National Center for Health Statistics (NCHS)/WHO growth reference and the 2006 WHO Child Growth Standards to create the most recent BMI-for-age references for individuals aged 5–19 years ( 11 ). Thus, the latest WHO guidelines are designed to represent relatively seamless standards and references from birth all the way into late adolescence/early adulthood.
In the USA, the Centers for Disease Control and Prevention (CDC) currently use the 2000 CDC growth references based on 1963–1994 US children’s data, to determine age- and sex-specific BMI percentiles for children aged 2–19 years ( 12 ). Overweight is defined in US children as age- and sex-specific BMI ≥85th and <95th percentile, while obesity is ≥95th percentile ( 13 ). Cut points for severe obesity in childhood have been proposed in recognition of the alarming growing prevalence of this extreme condition, defined as the 99th BMI percentile ( 13 ) or 120% of the 95th percentile ( 14 ). For US children <2 years old, the CDC currently uses the 2006 WHO Child Growth Standards, described above ( 15 ).
4. Prevalence and Trends
4.1. adult obesity—us and europe.
The first indications that obesity was taking on epidemic proportions originated in the USA and Europe. With few restrictions on access to or availability of food, the prevalence of overweight and obesity in the USA climbed virtually unmitigated over the last 50 years. Today, those who are overweight (BMI 25–<30 kg/m 2 ) or obese (BMI ≥30 kg/m 2 ) in the USA eclipse two-fold the numbers of those who are normal weight ( 16 ). In US adults, 1960–1994 trends showed that while levels of overweight hovered at approximately 31% over the time period, in contrast, age-adjusted obesity jumped from 13 to 23%, bringing the crude prevalence of overweight or obesity to 55% of the American population ( 17 ). Unfortunately, 1994 did not represent the endpoint of the upward trend, as the following decade saw adult obesity rise from 23 to 32% by 2003–2004 ( 16 ). In the last 10 years, national estimates of obesity seem to indicate that the steady upward trend of obesity in Americans has leveled off at a prevalence of about 35% ( 16 ) ( Figure 1 ), perhaps having reached some “Malthusian” obesity limit. However, certain subpopulations are faring worse than others, as 2011–2012 obesity rates in Hispanics and non-Hispanic blacks were 43 and 48%, respectively, pointing to a disproportionate burden in differing racial/ethnic and/or socioeconomic status (SES) groups. Gender also plays a role, with women being disproportionately affected by extreme obesity (classes 2–3, BMI ≥35 kg/m 2 ) than men, regardless of age or race/ethnicity ( 16 ).

Trends in age-adjusted prevalence of overweight, obesity, and extreme obesity in US adults, aged 20–74 years, 1960–2012. Trends in prevalence of overweight as BMI 25–<30 kg/m 2 (circles), and upward trends in obesity as BMI ≥30 kg/m 2 (squares), and extreme obesity as BMI ≥40 kg/m 2 (diamonds) in adult males (closed points) and females (open points). The figure is based on data from NHES I (1960–1962), NHANES I (1971–1974), NHANES II (1976–1980), NHANES III (1988–1994), and NHANES (1999–2000, 2001–2002, 2003–2004, 2005–2006, 2007–2008, 2009–2010, 2011–2012). Data derived are derived from Ogden, et al ., and Fryar, et al . ( 16 , 141 ). BMI, body mass index; NHANES, National Health and Nutrition Examination Survey; NHES, National Health Examination Survey.
Meanwhile, in Europe, longitudinal data (1992–1998 to 1998–2005) from participants in five countries involved in the European Prospective Investigation into Cancer and Nutrition (EPIC) study (Italy, the United Kingdom, the Netherlands, Germany, and Denmark), indicate that adult obesity increased modestly from 13 to 17% in that time period ( 18 ). However, were such linear trends were to continue, the overall obesity prevalence in these populations could reach 30% by 2015, paralleling US rates. A more conservative projection suggests a prevalence of just 20% obesity in these populations by 2015, if public awareness and public health measures take hold ( 18 ).
European studies including populations beyond EPIC indicate there is considerable disparity in overweight/obesity between European countries. A systematic review of national and regional surveys conducted between 1990 and 2008 points to obesity rates as low as 4.0 and 6.2% in French men and women, respectively (regional survey, 1994–1996), and as high as 30.0 and 32.0% in Czech men and women, respectively (national survey, 2002–2005) ( 19 ). Regional trends within Europe are apparent, with southern Italy and southern Spain, and Eastern European countries showing higher prevalence of obesity than countries in Western and Northern Europe ( 19 ). As in the USA, these data suggest that socioeconomic disparities and relatively recent/ongoing economic transitions are playing a considerable role in apparent differences across and within countries with respect to obesity risk.
4.2. Child Obesity—USA and Europe
US children may be faring better than their adult counterparts in some ways ( 16 ), potentially offsetting earlier dire predictions of rampant obesity by 2030 ( 5 ). In national surveys, levels of overweight in children, as in adults, seem to have leveled off (or even declined) at approximately 30% of US children aged 2–19 years ( 16 , 20 ). However, this belies a potentially disturbing long-term trend in the rising prevalence of extreme obesity (equivalent to adult class 2 obesity and higher, BMI ≥35 kg/m 2 ). Since 1999–2000, the prevalence of class 2 obesity in children (BMI ≥120% of the 95th percentile) has risen from 3.8 to 5.9% and class 3 obesity (BMI ≥140% of the 95th percentile) has doubled from 0.9 to 2.1%, the latter category jumping 30% since 2009–2010 alone ( 20 ). Again, as in their adult counterparts, certain sub-populations appear to be faring worse than others, notably Hispanic girls and Black boys, in whom overweight, obesity, and class 2 obesity have increased significantly ( 20 ).
Childhood obesity prevalence varies considerably between and within countries as well. Relatively recent estimates based on 2007–2008 data of children aged 6–9-years collected in 12 European countries as a part of the WHO European Childhood Obesity Surveillance Initiative observed overweight/obesity (BMI z score >+1 standard deviation [SD]) prevalence of 19.3–49.0% of boys and 18.4–42.5% of girls, while obesity (BMI z score >+2 SD) affected 6.0–26.6% of boys and 4.6–17.3% of girls. Researchers continued to observe the trend of north-south and west-east gradients evident in adults, with the highest levels of overweight in southern European countries ( 21 ).
4.3. Obesity Beyond North America and Europe
The data discussed above focus on the USA and European countries, many with robust national health surveillance programs. While historical data tends to be scarcer outside of these regions, an alarming picture has emerged over the last decades in low- and middle-income countries around the globe, complicated by rapidly changing socioeconomic environments. While country-specific trends are not discussed in this article, regional and national estimates of long-term changes in child (<20 years old) and adult (>20 years old) overweight and obesity have increased in nearly all countries and regions since 1980 ( Figure 2 ) ( 2 , 3 ). While the USA still may boast the largest absolute numbers of overweight and obese individuals, several other nations exceed the USA in terms of overall prevalence and, moreover, the rate of growth in certain countries is disheartening. For example, the prevalence of overweight and obesity in nationally representative Mexican adults was estimated to be 71.3% overweight/obese, with overweight at 38.8% and obesity at 32.4% ( 22 ). This prevalence represents an increase of 15% since 2000, placing this population among the most rapidly accelerating in terms of obesity prevalence over the last decade. Further, while rates of overweight remained relatively stable since 2000 at approximately 38% overall, extreme obesity (class 3, BMI ≥40 kg/m 2 ) increased by an estimated 76.5% from 2000 to 2012. These trends are also evident in countries outside of the Americas. In China, for example, between 1993 and 2009, overweight (BMI 25 to <27.5 kg/m 2 ) doubled in men (8 to 17%) and increased from 11 to 14% in women. Meanwhile, obesity (BMI ≥27.5 kg/m 2 ) nearly quadrupled in men, from 3 to 11%, and doubled in women, from 5 to 10%. Chinese children are faring as badly as their adult counterparts: overweight/obesity doubled from 6 to 13% in children aged 6–17 years over the same time period, suggesting that the obesity epidemic will continue to deepen in this country ( 23 ).

Prevalence of overweight and obesity in adults aged ≥20 years by global region, 1980–2008. From left to right, each column represents the estimated regional prevalence of overweight and obesity for 1980, 1985, 1990, 1995, 2000, 2005, and 2008. For a given region, a dark gray column indicates the lowest estimated prevalence in the trend, while the highest estimated prevalence is indicated by a black column. As is evident, the vast majority of regions demonstrate the lowest estimated prevalence of overweight and obesity in 1980, and the highest in 2008, demonstrating the global reach of obesity. The scale shows 25, 50, and 100% prevalence columns, for reference. Asterisks denotes high income. Data are sourced from Stevens, et al . ( 3 ).
5. Risk Factors for Obesity
Currently, our greatest gap in knowledge is not regarding the numbers of risk factors, nor in their independent impact on risk, but rather in how they interact with one another—their confluence—to produce today’s aptly if unfortunately named “globesity” epidemic. Obesity arises as the result of an energy imbalance between calories consumed and the calories expended, creating an energy surplus and a state of positive energy balance resulting in excess body weight. This energy imbalance is partially a result of profound social and economic changes at levels well beyond the control of any single individual. These “obesogenic” changes—economic growth, growing availability of abundant, inexpensive, and often nutrient-poor food, industrialization, mechanized transportation, urbanization—have been occurring in high-income countries since the early 20th century, and today these forces are accelerating in low- and middle-income countries. And yet, not all of us living in obesogenic environments experience the same growth in our waistlines. Hereditary factors—genetics, family history, racial/ethnic differences—and our particular socioeconomic and sociocultural milieus have been shown to affect risk of obesity ( Table 2 ) even in ostensibly similar obesogenic environments. So while body weight regulation is and should be viewed as a complex interaction between environmental, socioeconomic, and genetic factors, ultimately, personal behaviors in response to these conditions continue to play a dominant role in preventing obesity. Importantly, apart from genetics, every risk factor discussed below is modifiable .
Risk Factors, Comorbidities, and Sequelae of Obesity
5.1. Genetics of Obesity
To date, over 60 relatively common genetic markers 1 have been implicated in elevated susceptibility to obesity ( 24 , 25 ); however, the 32 most common genetic variants are thought to account for <1.5% of the overall inter-individual variation in BMI ( 24 ). When these 32 “top” genetic hits are combined into a genetic risk of obesity score, those with the highest genetic risk (i.e., carriers of over 38 risk alleles), have just a 2.7 kg/m 2 higher BMI on average than those with a low genetic risk. This translates into about a 15-lb (7-kg) weight difference between two 5’3” (160 cm) individuals with high versus low genetic risk ( 24 ). Although genetics undoubtedly play a role, this relatively small difference in BMI, coupled with the dramatic rise in obesity over the last half century in developed and developing nations alike point to obesity risk factors beyond genetics. A concomitant and rich area of research has therefore evolved investigating gene-environment interaction based on the idea that underlying genetic risk predisposes individuals to particularly adverse (or beneficial) effects of behavioral or environmental exposures such as diet and exercise, a concept scientifically popularized in, for example, the “thrifty gene” hypothesis ( 26 ). In many ways, these types of gene-environment interactions are playing out in population research: for example, a variant in FTO (rs9939609)—the strongest obesity susceptibility locus—increases odds of obesity in risk allele carriers by an estimated 23% per allele; however, this risk is modified by physical activity in adults ( 27 , 28 ) and children ( 29 ), among other factors. Nevertheless, these types of interactions have so far been investigated in relatively few genetic risk loci out of millions, and with just a handful of environmental factors, raising important questions of how to aggregate this complexity for public health and ultimately personalized medicine.
In addition, parental diet, lifestyle, and other exposures have been implicated in subsequent offspring obesity risk, including famine exposure ( 30 ), parental obesity ( 31 – 33 ), smoking ( 34 ), endocrine-disrupting and other chemicals ( 35 , 36 ), and weight gain during gestation and gestational diabetes ( 33 , 37 ). These and other studies point to lasting effects of fetal programming that via differing mechanisms, likely epigenetic, result in substantial repercussions in life course health, with implications across the socioeconomic/food availability spectrum. Careful management of diet and lifestyle in pre- and perinatal periods could exert a considerable impact on the obesity epidemic for generations to come ( 37 ).
5.2. Individual Behaviors
5.2.1. diet.
In the decades preceding the 21st century, the vast majority of research on obesity risk factors focused on individual-level, largely modifiable behaviors. The role of diet and physical activity in mitigating obesity risk and reducing prevalent obesity have received the most attention, and with good reason: 15% of deaths in 2000 in the USA were attributable to excess weight, owing to poor diet and physical inactivity ( 38 ). Caloric intake and expenditure needed for weight maintenance or healthy growth has historically taken center stage ( 39 ), and caloric restriction remains today a primary focus of most popular and clinical weight-management and weight-loss approaches.
Beyond overall caloric intake to regulate body weight, a tremendous amount of research has attempted to resolve the roles of diet quality and dietary patterns, including those specifying combinations of macronutrients ( 40 ). Evidence from clinical trials have almost universally shown that caloric restriction, regardless of dietary pattern, is associated with better weight outcomes ( 40 ). Although the metabolic nuances and relative merits of the differing dietary patterns for various comorbid conditions are still being investigated, the evidence seems to suggest that merely adhering to a diet—nearly irrespective of what type of healthy diet it is—has an impact on weight loss/control ( 41 – 43 ).
For long-term maintenance of healthy weight, evidence from observational cohorts indicate that diets that are considered “healthier” lead to better long-term weight maintenance, or at least mitigate weight gain typically associated with aging through middle age. For example, research in US health professionals pointed to averaged 4-year weight gain throughout middle age as being strongly associated with increasing intake of potato chips and potatoes, sugar-sweetened beverages, and processed and unprocessed red meats, but inversely associated with the intake of vegetables, fruits, whole grains, nuts, and yogurt ( 44 ). Specific food groups, such as sugar-sweetened beverages, have received considerable attention largely because added sugar consumption (primarily as sugar-sweetened beverages) has been rising concomitantly with prevalent obesity ( 45 ). Indeed, the weight of the evidence about the role of sugar-sweetened beverages in obesity ( 46 , 47 ) is a strong impetus for public health interventions and policies, such as limiting advertising on these beverages as in Mexico ( 48 ), attempts to limit beverage sizes permitted for sale as in New York City ( 49 ), taxation, eliminating sale in schools, etc.
5.2.2. Physical Activity, Sedentary Behaviors, and Sleep
Personal behaviors beyond diet (physical activity, sleep, sedentary and screen time, and stress) have also been independently associated with weight change and maintenance in adulthood. Combined with diet, these elements have synergistic and likely cumulative effects on an individual’s ability to maintain or obtain a healthy body weight over the life course. Recently reviewed evidence from randomized trials and observational studies support 2008 US recommendations for weight management ( 50 ), consistently showing that in general, 150–250 minutes per week of moderate intensity activity is required to prevent weight gain, or aid in weight loss when accompanied by dietary restriction ( 51 ). Activity (>250 minutes per week) is associated with weight loss and weight maintenance after weight loss ( 51 ). Leisure-time activities involving sitting, but which are not truly restful behaviors, such as getting <6 or >8 hours of sleep in adults and adolescents ( 44 , 52 – 55 ) or <10–11 hours of sleep in children ( 52 ), television viewing or screen time ( 44 , 56 , 57 ), and other leisure-time sitting ( 58 ) are also associated with weight gain.
5.3. Socioeconomic Risk Factors: Income and Education
Income has had a shifting role in obesity risk over the last century. As late as the mid-20th century, the USA and Europe could link wealth directly with obesity—the wealthier an individual, the more likely to be overweight. Over the last few decades, however, perhaps owing to the abundance of cheap and highly available food, coupled with changing sociocultural norms, this link has flipped. Today, wealth in the USA tends to be inversely correlated with obesity, and it is those who are at or below the level of poverty who appear to have the highest rates of obesity ( 59 ). Indeed, in US cities where the homeless are surveyed, the prevalence of overweight and obesity parallels that of non-homeless populations, contrary to our typical beliefs about thinness accompanying food insecurity or homelessness ( 60 , 61 ).
More broadly, across 11 Organisation for Economic Co-Operation and Development (OECD) countries, SES, whether defined by household income or occupation-based social class, showed an inverse relationship with obesity: women, in particular, had consistently higher prevalence of overweight/obesity the less affluent they were ( 62 ). In men, too, those in low income strata tended to have higher prevalence of obesity, but the gradient for overweight reversed in about half of the countries surveyed. That is, in some countries, poverty was associated with more prevalent overweight than wealth, but in others, lower income was associated with more favorable weight status. The differences between sexes in terms of income status and obesity, in particular the trend reversal in men, may be in part due to low-paying jobs typically involving more physically demanding work performed by men more than by women ( 62 ). Adding complexity to this picture is the role of education: in the 11 OECD countries discussed above, education showed a strong inverse relationship with overweight/obesity, particularly in women, who had consistently higher prevalence of overweight/obesity the less educated they were ( 62 ).
As wealth rises in low- and middle-income countries, it is expected for poverty-obesity patterns to begin more closely mimicking those of high-income countries. Evidence of this transition is already accumulating. In explorations of the role of education and wealth in women and weight status in four middle-income countries (Colombia, Peru, Jordan, and Egypt), authors observed a significant interaction between education and wealth: in women with little or no education, higher income was associated with 9–40% higher odds of obesity, while in those with higher levels of education, the association with income was either not present (Egypt, Peru) or associated with 14–16% lower odds of obesity (Jordan, Colombia) ( 63 ). This suggests that in currently transitioning economies, education may offset the apparently negative effects of increasing purchasing power in emerging obesogenic environments. However, the protective effect of education has yet to be seen in the poorer countries, such as India, Nigeria, and Benin, where both education and wealth were directly associated with increased odds of obesity ( 63 ).This is perhaps unsurprising, as obesity was relatively rare at <6.0% of women in these countries, and >50% of women had little or no education.
The glimmer of hope, then, is that in the context of a paradigm of diseases of affluence, in which the transition to wealth seem to invariably lead to higher obesity and thus greater chronic disease burden, higher education levels may yet offset some of the frightening challenges that lay before us.
5.4. Environmental 2 Risk Factors
5.4.1. the built environment.
Research on the built environment tends to focus on a few measurable characteristics of neighborhoods as they relate to weight status, while holding sociodemographic and other person-level characteristics constant. Such neighborhood characteristics range from more concrete factors (e.g., fast food restaurants, supermarkets, parks, transportation, etc.) to more variably scored factors (e.g., walkability, neighborhood healthiness). Most studies of the built environment have been cross-sectional, tending to focus on one or two characteristics; thus, findings on the relative importance or effects of given characteristics on obesity have been inconsistent ( 66 – 72 ), revealing the fundamental challenge of teasing out whether neighborhood characteristics play a causal role in weight status, or whether health-minded folks inhabit health-friendly areas to begin with (residential selection bias) ( 73 ). However, the emerging picture points to the primacy of diet-related built environments over those associated with physical activity. While presence of neighborhood physical activity or recreational spaces has been associated with increased physical activity levels or energy expenditure ( 71 , 72 ), healthy food environments, characterized by availability of produce or presence of supermarkets over convenience stores or fast food restaurants, play a potentially more important role ( 68 , 70 , 74 , 75 ).
Research on the causality of the built environment as obesity-inducing or health-promoting is critical for municipalities and public health authorities to justify potentially costly improvements to public spaces and/or zoning regulations. There is an unmet need for standardized measures, definitions, and criteria, established residential and occupational geographic radii relevant to health, and research methodologies that can take into account the complexity of something as seemingly simple as a neighborhood.
5.4.2. Environmental “Pathogens”: Viruses, Microbiomes, and Social Networks
Growing evidence from animal and human studies indicates that obesity may be attributable to infection, or that obesity itself may be a contagion. Infectious agents include viruses, the trillions of microbiota inhabiting the human gut, and, of course, obese humans as infectious agents themselves.
Although several viruses have been identified as potentially having a causal role in obesity ( 76 ), Ad-36 is among the most studied, being causally associated with adiposity in animals. Studies in diverse human populations generally support greater Ad-36 viral loads as probably causal of obesity in both children and adults ( 76 – 79 ), with links to other metabolic traits ( 77 , 79 ).
Ground-breaking research in the last decade has emerged on the role of trillions of gut bacteria—the human microbiome—in relation to obesity, energy metabolism, and carbohydrate and lipid digestion, opening promising therapeutic avenues for obesity and disease ( 80 ). Two primary phyla of bacteria differ in their proportions in lean vs. obese populations; these proportions change as obese individuals lose weight and correlate highly with the percentage of body weight lost ( 81 ). Broad and sometimes dramatic changes in microbiome populations have been catalogued following gastric bypass surgery ( 80 ), and in both the short- ( 82 , 83 ) and long-term ( 81 , 83 ) in response to changes in dietary composition ( 80 ). Research in mice indicates that increased adiposity is a transmissible trait via microbiome transplantation ( 84 ), and has prompted similar experimental fecal transplantation research in humans for the promotion of weight loss ( 85 ). In addition, other research has examined the feeding of pre- and probiotics as therapeutic modalities designed to manipulate the gut microbiome; these strategies also show promise for a range of conditions ( 85 ).
Finally, the importance of social networks—real and virtual—in obesity is a fascinating, relatively new area of research that capitalizes on known characteristics of infectious disease transmission. In a landmark 2007 study examining the spread of obesity due to social ties using 32-year prospective data from the Framingham Heart Study, Christakis and Fowler ( 86 ) showed that an individual’s chances of becoming obese increased by 57% if he or she had a friend who became obese in a given 4-year interval. This was a stronger risk ratio than that observed between pairs of adult siblings or even between spouses. Conversely, it may be possible to capitalize on the social contagion of obesity in the reverse direction, that is, in the promotion of healthy weight and behavior. Intervention studies of weight loss often include a social-relational component, although the evidence supporting any single approach or its efficacy is relatively scarce ( 87 ). In theory, a supportive network, community, or coaching relationship is supposed to improve weight loss; despite a lack of strong evidence, it is a key component of many popular commercial (e.g., Weight Watchers), trial/intervention, and online approaches.
6. Costs of Obesity: Co-Morbidities, Mortality, and Economic Burden
Obesity is associated with concomitant or increased risk of nearly every chronic condition, from diabetes, to dyslipidemia, to poor mental health. Its impacts on risk of stroke and cardiovascular disease, certain cancers, and osteoarthritis are significant.
6.1. Overall Mortality
In the year 2000 in the USA, 15% of deaths were attributable to excess weight, owing to poor diet and physical inactivity ( 38 ). Overweight/obesity in middle age shortens life expectancy by an estimated 4–7 years ( 88 ). Many long-term cohort studies, as well as three recent major syntheses of pooled data from established cohorts ( 89 – 91 ), which adequately accounted for history of smoking and chronic disease status, unequivocally show that overweight and obesity over the life course is associated with excess risk of total mortality, death from cardiovascular disease, diabetes, cancer, or accidental death ( 89 – 97 ).
Some studies suggest that excess body weight may be protective against mortality from certain chronic conditions—resulting in a so-called “obesity paradox.” However, most studies that have shown an obesity paradox, or no association between obesity and mortality, have been conducted in groups of older (>65) or elderly patients or in those with chronic conditions, or have inadequately accounted for smoking. Indeed, the role of excess adiposity in old age is unclear. While the protective effects of overweight in specific instances of diseased older populations may be real, these observations are fraught with methodological problems, especially reverse causation, and belie the limitations of generalizing excess adiposity’s supposed benefits to younger populations over the life course, not least because excess body weight leads to higher disease incidence to begin with ( 7 ).
6.2. Diabetes
Excess weight and diabetes are so tightly linked that the American Diabetes Association recommends physicians test for type 2 diabetes and assess risk of future diabetes in asymptomatic people ≥45 years old simply if they are overweight/obese, and regardless of age if they are severely obese ( 98 ). Overweight raises risk of developing type 2 diabetes by a factor of three, and obesity by a factor of seven, compared to normal weight ( 99 ). Excess weight in childhood and in young adulthood, and weight gain through early to mid-adulthood are strong risk factors for diabetes ( 100 – 102 ). While not every overweight/obese individual has diabetes, some 80% of those with diabetes are overweight/obese ( 103 ). Obesity itself raises diabetes risk even in the absence of other metabolic dysregulation (insulin resistance, poor glycemic control, hypertension, dyslipidemia). While metabolically healthy obese individuals are estimated to have half the risk of their metabolically unhealthy counterparts, they still have four times the risk of those who are normal weight and metabolically healthy ( 104 ).
6.3. Heart and Vascular Diseases
Ischemic heart disease and stroke are the leading causes of death in the USA and globally ( 105 ). Excess body weight is a well-known risk factor for heart disease and ischemic stroke, including their typical antecedents—dyslipidemia and hypertension. Recent studies have consistently shown that benign obesity appears to be a myth ( 106 – 108 ); overweight clearly adds to risk of heart disease and stroke beyond its implications for hypertension, dyslipidemia, and dysglycemia.
Given childhood obesity rates, research has lately focused on the role of obesity in early life and subsequent adulthood disease. Obesity in childhood or adolescence has been associated with twofold or higher risk of adult hypertension, coronary heart disease, and stroke ( 100 ). A recent study pooling data from four child cohorts (aged 11 years at baseline with average 23-year follow-up), observed that, compared with individuals who were normal weight in childhood and non-obese as adults, those who were normal weight or overweight but became obese as adults, or who were obese and stayed obese into adulthood, had considerably higher risk of high-risk dyslipidemia, hypertension, and higher carotid intima-media thickness. Notably, those individuals who were overweight/obese as children, but non-obese as adults, had similar risk profiles to those individuals who were never obese, indicating that the potential health effects of childhood obesity can be offset by weight loss prior to or while entering into adulthood ( 109 ).
6.4. Cancer
An estimated 6% of all cancers (4% in men, 7% in women) diagnosed in 2007 were attributable to obesity ( 110 ). Beyond being a major risk factor for diabetes, which itself is a risk factor for most cancers, obesity has long been understood to be associated with increased risk of esophageal, colon, pancreatic, postmenopausal breast, endometrial, and renal cancers ( 111 ). More recently, evidence has accumulated that overweight and/or obesity raise risk of cancers of the gallbladder ( 112 ), liver ( 113 ), ovaries (epithelial) ( 114 ), and advanced cancer of the prostate ( 115 ), as well as leukemia ( 116 ).
6.5. Trauma and Infection
A study in Pennsylvania (USA) trauma centers (2000–2009) showed that in-hospital mortality and risk of major complications of surgery were increased in obese patients as compared to non-obese patients. Severely obese patients had upwards of 30% increased risk of mortality from their trauma than non-obese patients, and double the risk of major complications. Severely obese females also had more than double the risk of developing wound complications, and quadruple the risk of developing decubitus ulcers ( 117 ). A recent meta-analysis of obesity in trauma care concluded that obesity was associated with 45% increased odds of mortality, longer stays in the intensive care unit, and higher rates of complications, and tended to associate with longer durations of mechanical ventilation and longer stays in the hospital overall, compared to non-obese patients, despite equivalent injury severity ( 118 ).
While elevated risk of chronic disease is a seemingly obvious consequence of obesity, increasing attention is being given to increased risk of infection and infectious disease in obesity, including surgical-site, intensive care unit (ICU)-acquired catheter, blood, nosocomial, urinary tract, and cellulitis and other skin infections ( 119 ), community-acquired infections, and poorer recovery outcomes owing to higher risk of influenza, pneumonia, bacteremia, and sepsis ( 119 ). Impaired immunological response may be an underlying mechanism; recent research has demonstrated lower vaccine efficacy and serological response to vaccination in the obese. For example, a recent study estimated an eightfold increase in the odds of non-responsiveness to hepatitis-B vaccination in obese versus normal-weight women ( 120 ).
The consequences of a global obesity epidemic may not merely be greater chronic and infectious disease burden for the obese, but also a greater global burden of infectious disease owing to obesity. Greater infectious disease vigilance may be required in populations with high levels of overweight/obesity, and there is a clear need for better clinical practice guidelines (e.g., use and dosage of antimicrobials, vaccines, other pharmaceuticals) for obese individuals.
6.6. Mental Health
The role of weight in mental health faces causal challenges, but what is clear is that obesity and adiposity are associated with anatomical as well as functional changes in the human brain. Studies in older populations have shown that BMI is inversely correlated with brain volume, and that obese older adults, compared to normal weight counterparts, show atrophy in the frontal lobes, anterior cingulate gyrus, hippocampus, and thalamus ( 121 ). In addition, obesity in children and adolescents (aged >9 years) has been associated with smaller orbitofrontal cortex gray matter volume, along with poorer performance in certain domains of executive function (e.g., inhibitory control) ( 122 ). Being overweight in midlife increases risk of Alzheimer's disease, vascular dementia, or any type of dementia by 35, 33, and 26%, respectively; even higher risk is observed for obesity ( 123 ). Importantly, physical activity, even among overweight individuals, may stave off poor mental functioning: moderately active or highly active adult overweight Finns did not have significantly increased risk of poor mental functioning at a 7-year follow-up compared to those who were normal weight and highly active, but inactive and overweight patients presented a nearly 40% increased risk of poor mental functioning ( 124 ). Thus, exercise may play an important mediating role in the relationship between excess body weight and age-related cognitive decline.
6.7. Economic Burden of Obesity
In the USA, recent estimates indicate that obese men are thought to incur an additional US$1,152 per year in medical spending, particularly due to hospitalizations and prescription drugs, compared to their non-obese counterparts, while obese women incur over double that of obese men, an additional US$3,613 per year in medical spending (year 2005 values). Extrapolating these costs to the national level, authors estimate some US$190 billion per year of healthcare spending, approximately 21% of US healthcare expenditures, is due to treating obesity and obesity-related conditions ( 125 ).
Total hospital costs account for a part of this: another author group studied non-bariatric, non-obstetric hospital procedures for obese patients, finding they were US$648 higher (year 2009 values) per capita than for non-obese patients. The estimated national hospital expenditures for the largest volume surgical procedures was US$160 million higher per year for obese than for their non-obese counterparts ( 126 ).
Employers bear a substantial brunt of obesity-related costs in the USA. Data from the Human Capital Management Services Research Reference Database (2001–2012) on employees and their dependents was used to compare medical, drug, sick leave, short-term disability, and workers’ compensation costs as well as absent days across three BMI strata: <27, ≥27–<30, and ≥30 kg/m 2 . Each of the costs was incrementally higher in ascending BMI categories. For example, total annual costs and total days absent in the highest vs. lowest BMI strata were US$6,313 versus US$4,258 (year 2012 values), and 7.5 versus 4.5 days. In addition, productivity was lowest in the obese group ( 127 ).
Finally, lifetime direct incremental medical costs of obesity in childhood in the USA were estimated to range from US$12,660 to US$19,630 (year 2012 values) for an obese 10-year old compared to a normal-weight 10-year old, if expected weight gain through adulthood among the normal weight child occurs ( 128 ). If normal weight children were to not continue on the typical weight gain trajectory into overweight/obesity, estimated incremental medical costs for today’s 10-year old obese child ranges between US$16,310 and US$39,080. Putting these figures into perspective, multiplying the lifetime medical cost estimate of US$19,000 by the number of obese 10-year-olds today generates a total direct medical cost of obesity of roughly US$14 billion for this 10-year old age group alone. In terms of big picture savings, the upper estimate of US$39,000 per case represents two years of public college tuition for that child ( 128 ).
In Europe, a 2008 review of 13 studies in ten Western European countries estimated the obesity-related healthcare burden had a relatively conservative upper limit of €10.4 billion annually (in Germany, in 1995 € equivalent), and ranging between <0.1 to 0.61% of each country’s gross domestic product (GDP). The review relied on study data from as early as the 1980s in the Netherlands, through 2002 in most of the remaining countries surveyed ( 129 ). A more recent review focused on 19 studies published in 2007–2010 in eight Western European countries (predominantly Germany, Denmark, and the United Kingdom). Excess health care costs of obesity or derivations of excess health care costs by comparisons of mean costs between normal weight and obese individuals in seven of the reviewed studies were between €117 and €1,873 per person (based on the € valuation given in each study year). Excess costs increased particularly due to severe obesity. Approximately 23% of medication costs and 6.9% of out-of-pocket costs were attributable to overweight or obesity. Health economic models estimated that 2.1–4.7% of total health care costs and 2.8% of total hospital costs were due to overweight and obesity. Total (direct and indirect) costs were generally unchanged from the 2008 estimate of the earlier review, accounting for 0.47–0.61% of GDP in these countries ( 130 ).
In the context of the Brazilian Unified Health System (i.e., public hospitals), estimated direct costs of diseases related to overweight/obesity in outpatient and inpatient care based on 2008–2010 data were US$2.1 billion annually (year 2010 values), 68.4% of which was attributable to hospitalizations, and the remainder due to ambulatory procedures ( 131 ). The largest costs of outpatient and inpatient care in both sexes were due to cardiovascular disease (US$747 million) followed by overweight- and obesity-related neoplasms (US$299.8 million), asthma (US$34 million), type 2 diabetes (US$3.7 million), and osteoarthritis (US$3.9 million). Authors estimated that these direct costs were a considerable underestimate of the true burden of overweight/obesity in Brazil, which would include private health care expenditures, as well as indirect costs due to lost productivity, premature death, and home care ( 131 ).
Given the predicted rise in obesity in Brazil, coronary heart disease, stroke, hypertension, cancers, osteoarthritis, and diabetes are projected to at least double by 2050, with concomitant doubling in health care costs, from US$5.8 billion in 2010 to US$10.1 billion per year—totaling US$330 billion over 40 years (year 2010 values). It is estimated that a 5% reduction in mean BMI across the population could save Brazil some US$57 billion over that time frame ( 132 ). A similar analytic approach that substituted Mexican prevalence and trends for the Brazilian ones estimated 2010 costs of obesity at US$806 million (year 2000 values), which were projected to increase to US$1.7 billion by 2050, at which point a mere 1% reduction in BMI prevalence in Mexico could save an estimated US$85 million per year ( 133 ).
Of course, none of these estimates include dollars spent on the weight-loss industry, which is estimated to be over US$60 billion dollars in 2014 in the USA alone ( 134 ), and includes non-prescription drugs and supplements, diet plans, gym memberships, workout videos, and an endless stream of money-making schemes.
7. Touching on Solutions, and Some Conclusions
Obesity is a major contributor to preventable disease and death across the globe, and poses a nearly unprecedented challenge not just to those tasked with addressing it at the public health level, or at the healthcare provider level, but to each of us as individuals, for none of us are immune. Increasing ease of life, owing to reduced physical labor and automated transportation, an increasingly sedentary lifestyle, and liberal access to calorie-dense food, driven by dramatic economic growth in many parts of the world in the last century, have turned a once rare disease of the affluent into one of the most common diseases—increasingly of the poor. That barely one in three people in the USA today are normal weight portends, quite simply, an astounding and frightening future. Significant reductions in public health and healthcare expenditures could occur around the world if we were able to stem the tide of childhood obesity trends, and if young and middle-aged overweight and obese adults lost approximately10% of their body weight, as recommended for a considerably reduced risk of debilitating chronic conditions ( 135 ).
Obesity is complex. Although its risk factors are myriad and compounding, there is an urgent need for deeper understanding of the way risk factors interact with each other, and the potential solutions to the epidemic are as multi-leveled and complex as its causes. There are calls for applying systems-level ( 136 ) and systems epidemiology ( 137 ) approaches to this and related nutrition and metabolic diseases, approaches which attempt to comprehensively address biological, behavioral, and environmental contributors to disease as well as their intricate feedback loops. Additional research on solutions to this epidemic would include, for example, examining the relative cost/benefit to individuals and populations of individual versus systemic policies and/or interventions, concurrently or independently, particularly when individuals and communities must decide between approaches given limited resources, and moreover, with the currently limited evidence in the case of broad industry, agricultural, or public health policies. For example, we could attempt to limit national production and import of sugar-sweetened beverages, tax sugar-sweetened beverages, or restrict fast food restaurant zoning. These largely political acts seem relatively inexpensive, but may have economic impacts in communities and regions beyond what we currently understand. We may push for the increasing medicalization of obesity, including developing an obesity vaccine. While such a “cure” may someday arise, the medicalization of a condition typically improves its treatment rather than its prevention, and prevention is key in the case of obesity. However, preventing and remediating obesity in children and adults—e.g., via health and wellness incorporation into curricula at every educational level from kindergarten through medical school—requires vast resources allocated to educators, as well as earlier diagnosis and treatment of overweight (education, counseling, drug treatment, etc.). Given these resource costs, perhaps greater attention should be given to pregnancy, a condition which is already highly medicalized and which may be an ideal preventive avenue for the provision of nutrition education and intensive monitoring of weight gain, to ensure that children have the most optimal start with respect to their future obesity risk. Clearly, no single approach is optimal, but with limited resources, an evidence base supporting one or more approaches or their combination is needed, as is tenacity and perhaps some audacity by local government and public health authorities in testing some of these approaches within their populations. However, an epidemic of this magnitude needs, quite simply, more resources. One of the reasons why the American Medical Association opted to declare obesity a “disease” was to give obesity the label it needs for greater allocation of resources for research, prevention, and treatment ( 1 ).
Despite the many unknowns, we can be cautiously optimistic about our ability to address the obesity epidemic. Indeed, we have relatively successfully faced similarly daunting public health challenges before: smoking, to name just one. While tobacco can loosely be thought of as a single product, and our food culture is infinitely more complex, as a case study in how to approach obesity, it provides numerous lessons in multi-level solutions to a major health threat in terms of both mitigation and prevention. We began by developing an understanding of smoking’s epidemiological impact and the healthcare costs borne by society, uncovered its biological basis, learned about and applied behavior change, and initiated and carried out vast public health, public policy, political, and economic strategies that ultimately affected whole environments as well as sociocultural norms.
It took over half a century to achieve the immense success we have with regard to smoking in the USA and still we are not yet tobacco-free ( 138 ); other parts of the world continue to wrestle with it to a greater degree. It has only been a couple decades since we first deeply appreciated that obesity was epidemic. We clearly still have a long way to go.
Key Points for Decision Makers
- In 2013, an estimated one in three adults worldwide was overweight or obese, and adult obesity exceeded 50% in several countries around the globe. While the prevalence of adult obesity in the developed world seems to have stabilized, the prevalence of obesity in children and adolescents globally, as well as adults obesity in developing countries, is still increasing. In addition, some developed countries continue to observe increasing prevalence of extreme classes of obesity.
- Overweight and obesity—defined as excess body weight for height—have genetic, behavioral, socioeconomic, and environmental origins.
- Obesity increases risk of major chronic diseases, including heart disease, diabetes, depression, and many cancers, as well as premature death.
- Estimates of annual healthcare costs attributable to obesity are US$190 billion per year in the USA, approximately 21% of US healthcare expenditures.
- Given its complexity, the obesity epidemic requires multilevel and integrated solutions, from individual intervention, to broad food policy, industry, and agriculture initiatives.
Acknowledgements
The authors declare no conflict of interest. AH is supported by an American Diabetes Association Mentor-Based Postdoctoral Fellowship award. FH is supported by NIH grants DK51158, HL60712, P30 DK46200, and U54CA155626. The authors broadly thank the researchers in this field for their consistent and tireless work in illuminating the etiology, sequelae, and solutions to this complex condition.
1 See also http://www.genome.gov/gwastudies/
2 We do not review the impact of food, agriculture, trade, and nutrition policy on obesity in the present paper, but refer interested readers to a recent review ( 64 ). Further, we do not address the body of growing evidence on the role of environmental pollutants–“obesogens”–in obesity, specifically those known as endocrine-disrupting chemicals. We refer readers to recent reviews on the topic ( 35 , 36 , 65 ).
Author Contributions
AH wrote the first draft of the paper. AH and FH contributed to writing, revised, and edited the paper. AH is the final guarantor of this work and takes full responsibility for its contents. Both authors read and approved the final manuscript.

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

7.5: Obesity Epidemic - Causes and Solutions
- Last updated
- Save as PDF
- Page ID 39986

- Alice Callahan, Heather Leonard, & Tamberly Powell
- Lane Community College via OpenOregon

Since the 1980s, the prevalence of obesity in the United States has increased dramatically. Data collected by the Centers for Disease Control and Prevention show rising obesity across the nation, state-by-state. 1
The methods used by the CDC to collect the data changed in 2011, so we can’t make direct comparisons between the periods before and after that change, but the trend has continued. Every year, more and more people in the U.S. are obese.

These trends are unmistakable, and they’re not just occurring in adults. Childhood obesity has seen similar increases over the last few decades—perhaps an even greater concern as the metabolic and health effects of carrying too much weight can be compounded over a person’s entire lifetime.

While obesity is a problem across the United States, it affects some groups of people more than others. Based on 2015-2016 data, obesity rates are higher among Hispanic (47 percent) and Black adults (47 percent) compared with white adults (38 percent). Non-Hispanic Asians have the lowest obesity rate (13 percent). And overall, people who are college-educated and have a higher income are less likely to be obese. 2 These health disparities point to the importance of looking at social context when examining causes and solutions. Not everyone has the same opportunity for good health, or an equal ability to make changes to their circumstances, because of factors like poverty and longstanding inequities in how resources are invested in communities. These factors are called “ social determinants of health. ” 3
The obesity epidemic is also not unique to the United States. Obesity is rising around the globe, and in 2015, it was estimated to affect 2 billion people worldwide, making it one of the largest factors affecting poor health in most countries . 4 Globally, among children aged 5 to 19 years old, the rate of overweight increased from 10.3 percent in 2000 to 18.4 percent in 2018. Previously, overweight and obesity mainly affected high-income countries, but some of the most dramatic increases in childhood overweight over the last decade have been in low income countries, such as those in Africa and South Asia, corresponding to a greater availability of inexpensive, processed foods. 5
Despite the gravity of the problem, no country has yet been able to implement policies that have reversed the trend and brought about a decrease in obesity. This represents “one of the biggest population health failures of our time,” wrote an international group of researchers in the journal The Lancet in 2019. 6 The World Health Organization has set a target of stopping the rise of obesity by 2025. Doing so requires understanding what is causing the obesity epidemic; it is only when these causes are addressed that change can start to occur.
Causes of the Obesity Epidemic
If obesity was an infectious disease sweeping the globe, affecting billions of people’s health, longevity, and productivity, we surely would have addressed it by now. Researchers and pharmaceutical companies would have worked furiously to develop vaccines and medicines to prevent and cure this disease. But the causes of obesity are much more complex than a single bacteria or virus, and solving this problem means recognizing and addressing a multitude of factors that lead to weight gain in a population.
At its core, rising obesity is caused by a chronic shift towards positive energy balance—consuming more energy or calories than one expends each day, leading to an often gradual but persistent increase in body weight. People often assume that this is an individual problem, that those who weigh more simply need to change their behavior to eat less and exercise more, and if this doesn’t work, it must be because of a personal failing, such as a lack of self-control or motivation. While behavior patterns such as diet and exercise can certainly impact a person’s risk of developing obesity (as we’ll cover later in this chapter), the environments where we live also have a big impact on our behavior and can make it much harder to maintain energy balance.
Environment
Many of us live in what researchers and public health experts call “ obesogenic environments. ” That is, the ways in which our neighborhoods are built and our lives are structured influence our physical activity and food intake to encourage weight gain. 7 Human physiology and metabolism evolved in a world where obtaining enough food for survival required significant energy investment in hunting or gathering—very different from today’s world where more people earn their living in sedentary occupations. From household chores, to workplace productivity, to daily transportation, getting things done requires fewer calories than it did in past generations.

Our jobs have become more and more sedentary, with fewer opportunities for non-exercise thermogenesis (NEAT) throughout the day. There’s less time in the school day for recess and physical activity, and fears about neighborhood safety limit kids’ ability to get out and play after the school day is over. Our towns and cities are built more for cars than for walking or biking. We can’t turn back the clock on human progress, and finding a way to stay healthy in obesogenic environments is a significant challenge.
Our environments can also impact our food choices. We’re surrounded by vending machines, fast food restaurants, coffeeshops, and convenience stores that offer quick and inexpensive access to calories. These foods are also heavily advertised, and especially when people are stretched thin by working long hours or multiple jobs, they can be a welcome convenience. However, they tend to be calorie-dense (and less nutrient-dense) and more heavily processed, with amounts of sugar, fat, and salt optimized to make us want to eat more, compared with home-cooked food. In addition, portion sizes at restaurants, especially fast food chains, have increased over the decades, and people are eating at restaurants more and cooking at home less.
Poverty and Food Insecurity
Living in poverty usually means living in a more obesogenic environment. Consider the fact that some of the poorest neighborhoods in the United States—with some of the highest rates of obesity—are often not safe or pleasant places to walk, play, or exercise. They may have busy traffic and polluted air, and they may lack sidewalks, green spaces, and playgrounds. A person living in this type of neighborhood will find it much more challenging to get adequate physical activity compared with someone living in a neighborhood where it’s safe to walk to school or work, play at a park, ride a bike, or go for a run.
In addition, poor neighborhoods often lack a grocery store where people can purchase fresh fruits and vegetables and basic ingredients necessary for cooking at home. Such areas are called “ food deserts ”—where healthy foods simply aren’t available or easily accessible.
Another concept useful in discussions of obesity risk is “food insecurity.” Food security means “access by all people at all times to enough food for an active, healthy life.” 8 Food insecurity means an inability to consistently obtain adequate food. It may seem counter-intuitive, but in the United States, food insecurity is linked to obesity. That is, people who have difficulty obtaining enough food are more likely to become obese and to suffer from diabetes and hypertension. This is likely related to the fact that inexpensive foods tend to be high in calories but low in nutrients, and when these foods form the foundation of a person’s diet, they can cause both obesity and nutrient deficiencies. It’s estimated that 12 percent of U.S. households are food insecure, and food insecurity is higher among Black (22 percent) and Latino (18 percent) households. 3
What about genetics? While it’s true that our genes can influence our susceptibility to becoming obese, researchers say they can’t be a cause of the obesity epidemic. Genes take many generations to evolve, and the obesity epidemic has occurred over just the last 40 to 50 years—only a few generations. When our grandparents were children, they were much less likely to become obese than our own children. That’s not because their genes were different, but rather because they grew up in a different environment. However, it is true that a person’s genes can influence their susceptibility to becoming obese in this obesogenic environment, and obesity is more prevalent in some families. A person’s genetic make-up can make it more difficult to maintain energy balance in an obesogenic environment, because certain genes may make you feel more hungry or slow your energy expenditure. 2
Solutions to the Obesity Epidemic
Given the multiple causes of obesity, solving this problem will also require many solutions at different levels. Because obesity affects people over the lifespan and is difficult to reverse, the focus of many of these efforts is prevention, starting as early as the first years of life. We’ll discuss individual weight management strategies later in this chapter. Here, we’ll review some strategies happening in schools, communities, and at the state and federal levels.
Support Healthy Dietary Patterns
Interventions that support healthy dietary patterns, especially among people more vulnerable because of food insecurity or poverty, may reduce obesity. In some cases, studies have shown that they have an impact, and in other cases, it’s too soon to know. Here are some examples:
- Implement and support better nutrition standards for childcare, schools, hospitals, and worksites. 9
- Limit marketing of processed foods, especially ads targeted towards children.
- Provide incentives for supermarkets or farmers markets to establish businesses in underserved areas. 9

Figure 9.21. Farmers markets can expand healthy food options for neighborhoods and build connections between consumers and local farmers.
- Place nutrition and calorie content on restaurant and fast food menus to raise awareness of food choices. 9 Beginning in 2018, as part of the Affordable Care Act, chain restaurants with more than 20 locations were required to add calorie information to their menus, and some had already done so voluntarily. There isn’t yet enough research to say whether having this information improves customers’ choices; some studies show an effect and others don’t. 10 Many factors influence people’s decisions, and the type of restaurant, customer needs, and menu presentation all likely matter. For example, some studies show that health-conscious consumers choose lower calorie menu items when presented with nutrition information, but people with food insecurity may understandably choose higher calorie items to get more “bang for their buck”. 11 Research has also shown that adding interpretative images—like a stoplight image labeling menu choices as green or red as shorthand for high or low nutrient density—can help. And a 2018 study found that when calorie counts are on the left side of English-language menus, people order lower-calorie menu items. Putting calorie counts on the right side of the menu (as is more common) doesn’t have this effect, likely because the English language is read from left to right. 12 Some studies have also found that restaurants that implement menu labeling offer lower-calorie and more nutrient-dense options, indicating that menu labeling may push restaurants to look more closely at the food they serve. 10,13

- Increase access to food assistance programs and align them with nutrition recommendations. For example, in 2009, the U.S. Department of Agriculture revised the food packages for the Women, Infants, and Children (WIC) program to better align with the Dietary Guidelines for Americans. The new packages emphasized more fruits, vegetables, whole grains, and low-fat dairy and decreased the availability of juice. After this change, there was a decrease in the obesity rate of children in the WIC program. Similar progress may be made by increasing access to the Supplemental Nutrition Assistance Program (SNAP) in order to reduce food insecurity. Many farmers’ markets now accept SNAP benefits for the purchase of fresh fruit and vegetables. 3
- Tax sugary drinks, such as soda and sports drinks, which contribute significant empty calories to the U.S. diet and are associated with childhood obesity. Local taxes on soda and other sugary drinks are often controversial, and soda companies lobby to prevent them from passing. However, early research in U.S. cities with soda taxes show that they do work to decrease soda consumption. 3 In the U.S., soda has only been taxed at the local level, and the tax has been paid by consumers. The United Kingdom has taken a different approach: They started taxing soft drink manufacturers for the sugar content of the products they sell. Between 2015 and 2018, the average sugar content of soda sold in the U.K. dropped by 29 percent. 14
Support Greater Physical Activity
Increasing physical activity increases the energy expended during the day. This can help maintain energy balance, thus preventing weight gain. It may also help to shift a person into negative energy balance and facilitate weight loss if needed. But simply adding an exercise session—a run or a trip to the gym, say—often doesn’t shift energy balance (though it’s certainly good for health). Why? Exercise can increase hunger, and there’s only so many calories a person can burn in 30 or 60 minutes. That’s why it’s also important to look for opportunities for non-exercise activity thermogenesis (NEAT); that is, find ways to increase movement throughout the day.
- P rioritize physical education and recess time in schools. In addition to helping kids stay healthy, movement also helps them learn.
- Make neighborhoods safer and more accessible for walking, cycling, and playing.
- When safe, encourage kids to walk or bike to school.
- Build family and community activities around physical activity, such as trips to the park, walks together, and community walking and exercise groups.
- Facilitate more movement in the workday by encouraging walking meetings, movement breaks, and treadmill desks.
- Find ways to move that are enjoyable to you and fit your life. Yard work, walking your dog, playing tag with your kids, and going out dancing all count!

VIDEO: “ James Levine: ‘I Came Alive as a Person’ “ by NOVA’s Secret Life of Scientists and Engineers, YouTube (April 24, 2014), 3:04 minutes. This short video explains some of the research on NEAT and efforts to increase it in our lives
VIDEO: “ The Weight of the Nation: Poverty and Obesity” by HBO Docs, YouTube (May 14, 2012), 24:05 minutes.
VIDEO: “ The Weight of the Nation: Healthy Foods and Obesity Prevention” by HBO Docs, YouTube (May 14, 2012), 31:11 minutes. These segments from the HBO documentary series, “The Weight of the Nation,” explore some of the causes and potential solutions for obesity.
References:
- 1 CDC. (2019, September 12). New Adult Obesity Maps. Retrieved October 30, 2019, from Centers for Disease Control and Prevention website: https://www.cdc.gov/obesity/data/prevalence-maps.html
- 2 CDC. (2019, January 31). Adult Obesity Facts | Overweight & Obesity | CDC. Retrieved October 30, 2019, from https://www.cdc.gov/obesity/data/adult.html
- 3 Trust for America’s Health. (2019). The State of Obesity: Better Policies for a Healthier America . Retrieved from https://www.tfah.org/report-details/stateofobesity2019/
- 4 Swinburn, B. A., Kraak, V. I., Allender, S., Atkins, V. J., Baker, P. I., Bogard, J. R., … Dietz, W. H. (2019). The Global Syndemic of Obesity, Undernutrition, and Climate Change: The Lancet Commission report. The Lancet , 393 (10173), 791–846. https://doi.org/10.1016/S0140-6736(18)32822-8
- 5 UNICEF. (2019). The State of the World’s Children 2019. Children, Food and Nutrition: Growing well in a changing world . New York.
- 6 Jaacks, L. M., Vandevijvere, S., Pan, A., McGowan, C. J., Wallace, C., Imamura, F., … Ezzati, M. (2019). The obesity transition: Stages of the global epidemic. The Lancet Diabetes & Endocrinology , 7 (3), 231–240. https://doi.org/10.1016/S2213-8587(19)30026-9
- 7 Townshend, T., & Lake, A. (2017). Obesogenic environments: Current evidence of the built and food environments. Perspectives in Public Health , 137 (1), 38–44. https://doi.org/10.1177/1757913916679860
- 8 Pan, L., Sherry, B., Njai, R., & Blanck, H. M. (2012). Food Insecurity Is Associated with Obesity among US Adults in 12 States. Journal of the Academy of Nutrition and Dietetics , 112 (9), 1403–1409. https://doi.org/10.1016/j.jand.2012.06.011
- 9 CDC. (2019, June 18). Community Efforts | Overweight & Obesity | CDC. Retrieved October 30, 2019, from https://www.cdc.gov/obesity/strategies/community.html
- 10 Bleich, S. N., Economos, C. D., Spiker, M. L., Vercammen, K. A., VanEpps, E. M., Block, J. P., … Roberto, C. A. (2017). A Systematic Review of Calorie Labeling and Modified Calorie Labeling Interventions: Impact on Consumer and Restaurant Behavior. Obesity (Silver Spring, Md.) , 25 (12), 2018–2044. https://doi.org/10.1002/oby.21940
- 11 Berry, C., Burton, S., Howlett, E., & Newman, C. L. (2019). Understanding the Calorie Labeling Paradox in Chain Restaurants: Why Menu Calorie Labeling Alone May Not Affect Average Calories Ordered. Journal of Public Policy & Marketing , 38 (2), 192–213. https://doi.org/10.1177/0743915619827013
- 12 Dallas, S. K., Liu, P. J., & Ubel, P. A. (2019). Don’t Count Calorie Labeling Out: Calorie Counts on the Left Side of Menu Items Lead to Lower Calorie Food Choices. Journal of Consumer Psychology, 29(1), 60–69. https://doi.org/10.1002/jcpy.1053
- 13 Theis, D. R. Z., & Adams, J. (2019). Differences in energy and nutritional content of menu items served by popular UK chain restaurants with versus without voluntary menu labelling: A cross-sectional study. PLOS ONE , 14 (10), e0222773. https://doi.org/10.1371/journal.pone.0222773
- 14 Public Health England. (2019). Sugar reduction: Report on progress between 2015 and 2018 . Retrieved from https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/832182/Sugar_reduction__Yr2_progress_report.pdf
Image Credits
- Figure 9.17. “Obesity Trends Among U.S. Adults, BRFSS, 1990-2010” by Division of Nutrition, Physical Activity, and Obesity, National Center for Chronic Disease Prevention and Health Promotion , Centers for Disease Control and Prevention is in the Public Domain
- Figure 9.18. “Prevalence of self-reported obesity among U.S. adults in 2011 and 2018” by Division of Nutrition, Physical Activity, and Obesity, National Center for Chronic Disease Prevention and Health Promotion , Centers for Disease Control and Prevention is in the Public Domain
- Figure 9.19. “Trends in obesity prevalence” by National Center for Health Statistics is in the Public Domain
- Figure 9.20. Elements of obesogenic environment: “wocintech” by WOCinTech Cha is licensed under CC BY 2.0 ; “Perfect timing” by Tamara Menzi , Unsplash is in the Public Domain, CC0 ; “Vending machines” by Purchase College Library is licensed under CC BY-NC 2.0
- Figure 9.21. Farmers markets. “group of people standing near vegetables” by Megan Markham is in the Public Domain, CC0 ; “Veggies at Corvallis Farmers Market” by Friends of Family Farmers is licensed under CC BY-ND 2.0
- Figure 9.22. Menu labeling. “Ballpark Calorie Counting” by Kevin Harber is licensed under CC BY-NC-ND 2.0
- Figure 9.23. Increasing physical activity. “Early bird” by Jorge Vasconez is in the Public Domain, CC0 ; “boy running to the future” by Rafaela Biazi is in the Public Domain, CC0 ; “people riding bicycles inside bicycle lane beside skyscraper” by Steinar Engeland is in the Public Domain, CC0
IELTS Practice.Org
IELTS Practice Tests and Preparation Tips
- Band 9 IELTS Essays
IELTS essay about obesity and its causes and solutions
by Manjusha Nambiar · Published January 24, 2017 · Updated March 24, 2024
Essay topic
The number of people who are at risk of serious health problems due to being overweight is increasing. What is the reason for the growth in overweight people in society? How can this problem be solved?
Sample essay
Over the last few years, there has been a dramatic increase in the number of overweight people in the world. This can be attributed to unhealthy eating habits and lack of physical activity. Obesity is a major health problem. It is a risk factor for diabetes, stroke and heart disease.
Excessive consumption of junk foods is the number one cause of obesity. Junk or fast foods are rich in calories and unhealthy fats. When we consume more calories than our body can burn, it will convert the excess calories into fat. As a result people who consume calorie rich foods on a regular basis gain weight. Late night dinners are another cause of weight gain. When we have a heavy meal immediately before going to bed, the body does not get an opportunity to burn it. Our sedentary lifestyle is also to blame. Most of us have jobs that allow us to spend our entire day in a chair. This lack of physical activity reduces our requirement for calories. Still, we are consuming more calories than we need.
Limiting the consumption of calories and making physical activity an important part of your routine is the only way to combat obesity. Our bodies are designed to move. When we exercise, we not only burn the excess calories but also reduce our risk for a variety of illnesses like diabetes and heart disease. We need to make proper changes to our eating habits too. We must make a conscious effort to stay away from fatty foods. We must also ensure that we are having low calorie healthy meals at regular intervals.
To conclude, while it is true that the number of obese people is on the rise this problem can be tackled by making appropriate changes to our lifestyle and eating habits.
Tags: ielts essay samples
Manjusha Nambiar
Hi, I'm Manjusha. This is my blog where I give IELTS preparation tips.
- Next story IELTS essay sample | The popularity of consumer goods is a reflection of the power of advertising
- Previous story Band 9 essay sample | Keeping pets can cause health problems in children
Leave a Reply Cancel reply
You must be logged in to post a comment.
- Academic Writing Task 1
- Agree Or Disagree
- Band 7 essay samples
- Band 8 Essay Samples
- Band 8 letter samples
- Discuss Both Views
- Grammar exercises
- IELTS Writing
- Learn English
- OET Letters
- Sample Essays
- Sample Letters
- Writing Tips
Enter your email address:
Delivered by FeedBurner
IELTS Practice

Essay on Obesity
Students are often asked to write an essay on Obesity in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Obesity
Understanding obesity.
Obesity is a health condition where a person has excess body fat. It’s often measured using the Body Mass Index (BMI).
Causes of Obesity
Obesity can be caused by eating too much and not exercising enough. Also, genetics and lifestyle can play a role.
Effects of Obesity
Obesity can lead to serious health problems like heart disease, diabetes, and certain types of cancer.
Preventing Obesity
Eating a balanced diet and regular physical activity can help prevent obesity. It’s important to maintain a healthy lifestyle.
Also check:
- Paragraph on Obesity
- Speech on Obesity
250 Words Essay on Obesity
Introduction.
Obesity represents a significant public health issue worldwide, posing detrimental effects to physical health and psychological well-being. It is a complex disorder involving an excessive amount of body fat, often resulting from a combination of genetic, behavioral, and environmental factors.
The primary cause of obesity is an energy imbalance between calories consumed and expended. This disparity is often fueled by unhealthy diets rich in fats and sugars, and a sedentary lifestyle. Genetics also play a critical role, affecting how the body metabolizes food and stores fat.
Implications on Health
Obesity significantly increases the risk of various diseases, including heart disease, diabetes, and certain cancers. Additionally, it can lead to mental health issues like depression and lower quality of life.
Prevention and Management
Preventing obesity requires a multi-faceted approach. It entails adopting a healthier diet, increasing physical activity, and creating supportive environments that promote healthy choices. Management of obesity often involves similar strategies, though in some cases, medication or surgery may be necessary.
In conclusion, obesity is a pressing global health concern that requires immediate attention. It is crucial to promote healthier lifestyles and create supportive environments to combat this epidemic. The battle against obesity is not only about individual responsibility but also about societal commitment to fostering healthful living.
500 Words Essay on Obesity
Obesity, a complex and multifaceted health issue, has become a global epidemic. Characterized by excessive body fat, it poses a significant risk to an individual’s health, leading to numerous chronic illnesses. This essay will delve into the causes, consequences, and potential solutions to this growing health crisis.
The primary cause of obesity is an energy imbalance between calories consumed and expended. This is often due to a combination of excessive dietary intake, lack of physical activity, and genetic susceptibility. However, it is important to recognize the role of socio-economic factors. The availability of high-calorie, low-nutrient food, urbanization, and sedentary lifestyles have all contributed to the rise in obesity rates.
Health Consequences
Obesity significantly increases the risk of various health problems. It is a major risk factor for noncommunicable diseases (NCDs) such as cardiovascular diseases, diabetes, musculoskeletal disorders, and some cancers. Moreover, obesity can lead to psychological issues, including depression, anxiety, and low self-esteem.
Socioeconomic Impact
The socioeconomic impact of obesity is profound. It places a heavy burden on healthcare systems due to the high cost of treating obesity-related diseases. Furthermore, obesity can lead to reduced productivity and increased absenteeism in the workforce, affecting economic growth.
Prevention and Control
Preventing and controlling obesity requires a multifaceted approach. At the individual level, this includes adopting a healthy diet and regular physical activity. However, individual behavior is shaped by the broader socio-environmental context. Therefore, public health interventions are crucial. These may include policies to regulate food advertising, promote active transportation, and ensure access to affordable, nutritious food.
In conclusion, obesity is a complex issue with far-reaching consequences. It is driven by a combination of individual, environmental, and socio-economic factors. Therefore, addressing this problem requires concerted efforts at multiple levels. By implementing comprehensive strategies that promote healthy lifestyles and create supportive environments, we can combat the obesity epidemic and improve public health.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on Nutrition
- Essay on Nursing Profession
- Essay on Nuclear Energy
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Your Article Library
Essay on obesity.
ADVERTISEMENTS:
Read this essay to learn about the meaning, causes, types, treatment, principles of dietary management and complications of overweight/ obesity.
Meaning of Obesity:
Obesity is a big problem of health. Obesity is a condition in which there is excessive weight gain in the body, an increase of 10% over the ideal weight is termed as obesity. Excessive weight gain is generally due to large intake of food.
When excessive amount of energy is consumed and less quantity of it is used up the excess energy gets converted into fat which is deposited as adipose tissue. Excessive weight would predispose a person to cardiovascular diseases, diabetes, gout, arthritis, disease of the liver and gall bladder, etc. Common complaints from an obese person would be fatigue, backaches and foot-aches after a little bit of excretion.
Causes of Obesity:
Genetic Factors:
A genetic base regulates species, difference in body fat and sexual difference within a species. So genetic inheritance to certain extend influences a person’s chance of becoming fat.
Eating Habits:
Certain eating habits of an individual can lead to obesity which are:
1. Snacking in between the meals, common among adolescents and housewives.
2. Eating faster, taking less time for chewing thereby consuming more.
3. The appearance of food or the smell of food turns their appetite on, though internally they would not be hungry.
4. Individuals who frequently attend luncheons hosted by their officials generally lead to consumption of heavy food.
5. Irregular timings, when one would get the time the person would rather.
6. People overeat to suppress their emotions.
Physical Activity:
Persons leading sedentary lives are more prone to be obese. There is hardly any attention given to physical activity.
Endocrine Factors:
Obesity is found in hypothyroidism, hypogonadism and Cushing’s syndrome. Obesity is also common during puberty, pregnancy and menopause, suggesting endocrine glands might be a factor.
An injury to hypothalamus after a head injury may lead to obesity as the hypothalamus cannot regulate appetite or satiety center.
Types of Obesity:
Grade I- These people have Body mass index (BMI) less than 29.9. The excess weight does not affect their health. They generally reduce on their own.
Grade II- The body mass index is between 30-39.9. Though they maintain good health but on little exertion they are fatigued. For reasons unknown they are more at risk for developing diabetes, atherosclerosis, hypertension, fatty liver, gall bladder diseases, hernias, etc.
Grade III- The body mass index is above 40. They have very limited physical activity due to enormous weight. They are more susceptible to all the diseases of grade II.
Body mass Index
(BMI) = Weight [kg]/Height [m]
Grading of obesity can be base on BMI
Grade III >40
Grade II 30-40
Grade I 25-29.9
Not obese <25
Treatment of Obesity:
Reducing Weight:
Losing weight requires careful planning in diet. Reduced intake and regular loss of fat from body in the form of physical activity play a major role as a person grows old. A slight change in ideal weight is normal.
Generally obese persons lead sedentary lives. A low calorie diet with moderate exercise such as walking would be the best in which the time-span can be gradually increased. The grade I type of obese patient can also take part in outdoor games like tennis, badminton, swimming, cycling, etc. Among housewives, household activities like mopping, sweeping the floor, gardening, etc. also forms a pad of good exercise.
Drugs usually act as appetite suppressors which have their own side effects and are no substitute to low calorie diets.
Liposuction:
This is a surgical procedure of removal of excess of fat but is associated with recurrence and a few complications.
Gastric Plication:
By placing surgical staples, across the upper portion of stomach due to which intake capacity of food is reduced.
Principles of Dietary Management:
A low calorie, moderate protein, restricted fat and carbohydrates and liberal fluid and high fibre diets are well preferred.
About 20 kcal per kg body is prescribed for a sedentary person and about 25 kcal per kg body weight for a moderately active person.
The normal protein requirement of 1 gm./kg body is the best suitable.
Fats being concentrated source of energy it has to be restricted. Vegetable oils are permitted [except coconut and palm] to provide the required essential fatty acids.
Carbohydrates:
High Carbohydrate foods like potatoes, refined cereal products are to be avoided. To give satiety feeling and regular bowel movements, green leafy vegetables, fresh fruits and vegetables are preferred.
Fluids should be taken in liberal amounts as they give a filling sensation. A glass of water consumed before a meal reduces the intake.
Complications:
Physical Disability:
As the feet have to bear the load of the whole body they tend to develop problems associated with the joints, knees, spine and the hips.
Metabolic Disorder:
Obesity is closely associated with diabetes. Generally in simple obesity, a patient develops insulin resistance.
Plasma cholesterol levels are high predisposing them to develop gall stones. It can also lead to Gout.
Cardiovascular Disorders:
Apart from atherosclerosis these individuals are prove to develop high blood pressure and varicose veins.
Obstetrical Risk:
Obese ladies when pregnant are greater obstetrical risk due to hypertension, diabetes or postpartum infections.
Psychologic Disturbances:
Obese adolescents have been found to have personality characteristics which are self-created among which the greatest is an inferiority feeling.
Prone to Accidents:
These people are more prone to accidents due to slipping and falling down.
Nursing Diagnosis:
Altered Nutrition-more than Body Requirements:
The patient is at risk of actually consuming more than what is necessary for metabolic needs.
May be related to:
Excessive intake, sedentary life, Cultural preferences, Psychological preferences
Possibly Evidenced by:
10-12% over ideal body weight
Clinical Conditions:
Obesity, Hypothyroidism, Patient on corticosteroids, Prolonged immobility, Cushing’s syndrome.
Expected Outcome:
1. Identifies healthy patterns of nutrition and weight control
2. Plans for future control of weight
3. Weight loss towards desired goal established
Related Articles:
- Nutrition Transition: Extent, Causes, Implications (310 Words)
- How to Calculate the Daily Calorie Requirement ?
Comments are closed.
Read our research on: Abortion | Podcasts | Election 2024
Regions & Countries
As obesity rates rise in the u.s. and worldwide, new weight-loss drugs surge in popularity.
Obesity affects roughly 42% of U.S. adults , according to the Centers for Disease Control and Prevention (CDC). And about two-thirds of Americans (65%) say willpower alone usually isn’t enough for most people who are trying to lose weight and keep it off, according to a new Pew Research Center survey.
Put those two facts together, and it should come as no surprise that a new class of drugs to help people lose weight – including Ozempic, Wegovy and similar medications – has soared in popularity . In the Center survey, about three-quarters of Americans say they have heard or read at least a little about these drugs.
This post analyzes obesity rates and uptake of weight-loss drugs in the United States and worldwide. It uses data from Pew Research Center’s recent report “How Americans View Weight-Loss Drugs and their Potential Impact on Obesity in the U.S.” and other sources.
Data on the prevalence of U.S. adults classified as obese and overweight was obtained from the National Health and Nutrition Examination Survey (NHANES), a project of the Centers for Disease Control and Prevention. The NHANES is normally conducted every two years. Some of our findings come from this most recent dataset, and others are from the 2017-18 NHANES. Data from the 2021-23 survey is not yet available.
Global obesity rates for adults were obtained from the World Health Organization (WHO). The most recent estimates are from 2016. To estimate the number of people worldwide with obesity, we also used 2016 population data for adult men and women from each country from the World Bank. We applied WHO’s gender-specific obesity rates to those population estimates, then totaled them to arrive at a global obesity estimate.
Data on the number of prescriptions for and patients using weight-loss drugs came from ClinCalc.com , an online resource for physicians and other health care practitioners. ClinCalc aggregates data from the Prescribed Medicines File (PMED) of the Medical Expenditure Panel Survey , a project of the U.S. Agency for Healthcare Research and Quality.
We also analyzed recent financial statements from Novo Nordisk, producer of Ozempic and other semaglutide drugs, and Eli Lilly, maker of Mounjaro and Zepbound. We obtained the companies’ financials via the Securities and Exchange Commission’s EDGAR database of corporate filings .
In the case of Novo Nordisk, which as a Danish company reports its financials in Danish kroner rather than U.S. dollars, we converted its reported revenues to dollars at the rate of 1 krone = $0.145, the prevailing exchange rate when we did the analysis.
Obesity patterns in the U.S. and abroad
Over the past three decades, the share of Americans categorized as obese (based on body mass index, or BMI, data from the CDC) has risen considerably.
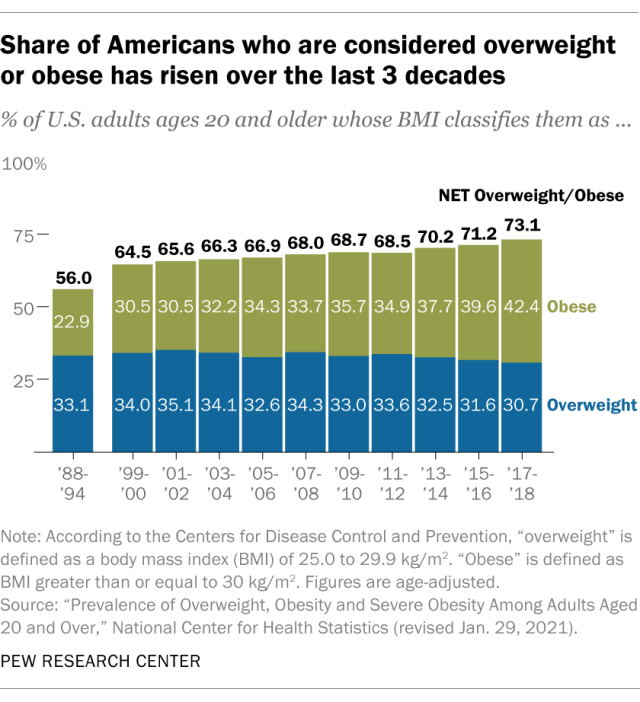
In 2017-18 – the timespan with the most recent data available – about three-quarters of U.S. adults ages 20 and older were considered either overweight (31%) or obese (42%). Just over 9% of adults were considered severely obese. (Note that the CDC survey period spans two years.) About three decades earlier, by comparison, 56% of Americans ages 20 and older were considered overweight or obese, including 3% who were considered severely obese.
The COVID-19 pandemic disrupted the CDC’s data collection, which is why the most recent figures are from 2017-18. However, there’s some evidence from other federal agencies that adult obesity rates rose even higher during the pandemic.
The CDC classifies someone as “overweight” if they have a BMI of 25.0 to 29.9, and “obese” if they have a BMI of 30.0 or greater. People whose BMI is 40.0 or greater are sometimes categorized as “severely obese.” The CDC has more information about BMI , its uses and how to calculate it.
While clinicians and researchers use BMI as a population-level metric and as an individual screening tool to identify potential weight problems, many now advise that BMI alone is an incomplete measure of health . In 2023, for instance, the American Medical Association (AMA) urged doctors to consider additional factors when assessing obesity and health risks, such as body composition, waist circumference and genetic factors. The AMA also noted that health risks differ both between and within demographic groups, and that BMI cutoffs were “based primarily on data collected from previous generations of non-Hispanic White populations and [do] not consider a person’s gender or ethnicity.”
The United States had one of the highest adult obesity rates in the world as of 2016, the most recent year for which the World Health Organization (WHO) has comprehensive data. That year, the U.S. ranked 12th among 191 countries. (Note that the WHO defines adults as those 18 and older, so its figures aren’t directly comparable with the CDC data.)
Worldwide, obesity affected about 663 million adults, or 13% of the global adult population, in 2016. Global obesity rates were 15% for women and 11% for men, based on Center estimates of WHO and World Bank data.
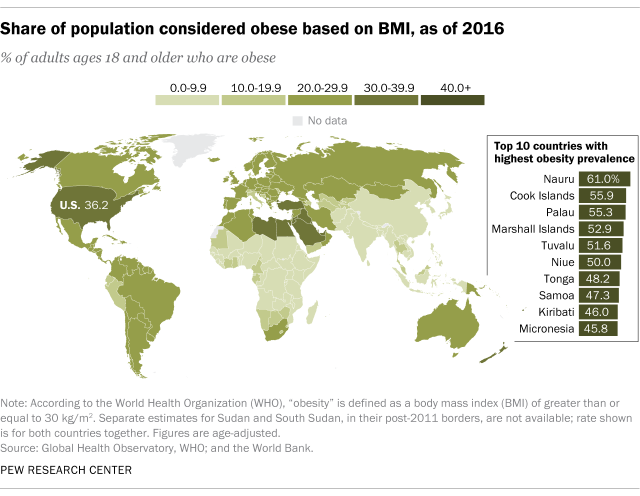
Demand for weight-loss drugs
Americans have only modest expectations that the new weight-loss drugs – formally known as glucagon-like peptide-1 (GLP-1) receptor agonists – will reduce obesity in the U.S. , according to the Center’s new survey. Still, these drugs have taken off in popularity in America, as well as around the world.
Since its 2017 approval as a diabetes treatment, semaglutide (the generic name for Ozempic and its offshoots, Rybelsus and Wegovy) has become one of the most popular prescription drugs in the U.S. It ranked 90th in 2021, the most recent year for which federal data on hundreds of the most commonly prescribed drugs is available. That year, an estimated 8.2 million prescriptions for it were written in the U.S., more than quadruple the number just two years earlier.
Almost 2 million people in the U.S. were taking semaglutide medications in 2021 – more than three times as many as in 2019. (The number of prescriptions exceeds the number of patients because prescription refills and renewals are counted separately.)
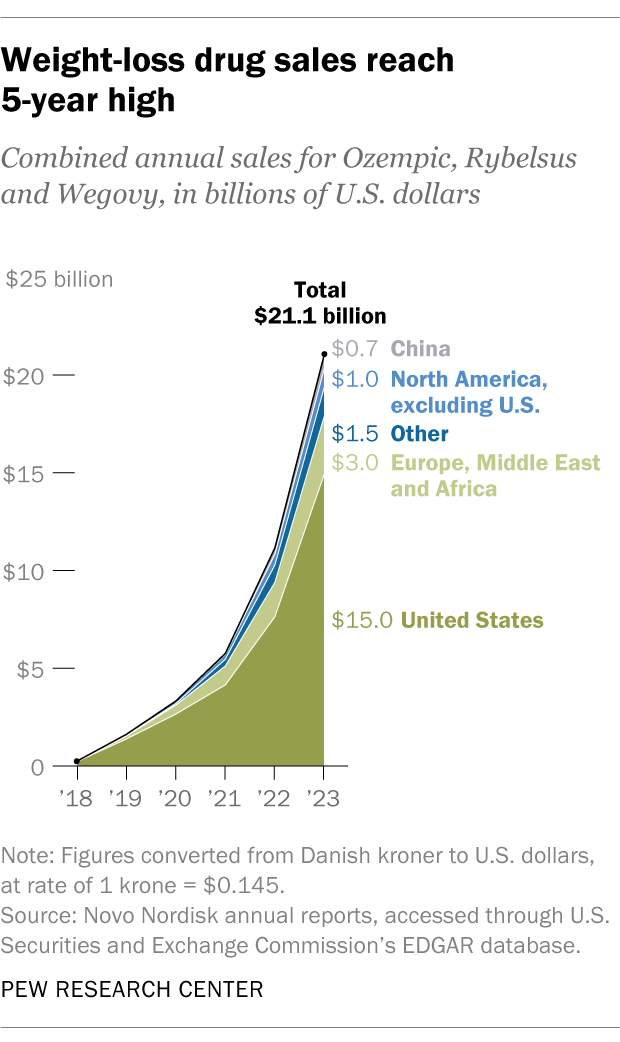
Another indication of weight-loss drugs’ rapid uptake globally comes from the financial statements of their manufacturers. Last year, Ozempic, Rybelsus and Wegovy had combined sales of about $21.1 billion for Novo Nordisk, the Danish company that produces them. That made up nearly two-thirds of Novo Nordisk’s entire revenue that year. The drugs’ combined sales were 89% higher than in 2022. Last year, 71% of semaglutide revenues came from the U.S.
Mounjaro, a similar diabetes drug produced by Eli Lilly with the active ingredient tirzepatide, launched in mid-2022. By the end of 2022, Mounjaro had sales of $482.5 million. In 2023, its first full year on the market, Mounjaro brought in nearly $5.2 billion. In November 2023, the Food and Drug Administration approved a version for weight loss under the name Zepbound.

Sign up for our weekly newsletter
Fresh data delivered Saturday mornings
8 facts about Americans with disabilities
Most patients in u.s. have high praise for their health care providers, health issues topped the list of scientific studies reaching wide audiences in 2016, americans aren’t sold on plastic surgery: few have had it done, opinions mostly mixed, opinions on expanding access to experimental drugs differ by race, income, most popular.
About Pew Research Center Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 11 March 2024
Blockbuster obesity drug leads to better health in people with HIV
- Mariana Lenharo
You can also search for this author in PubMed Google Scholar
You have full access to this article via your institution.
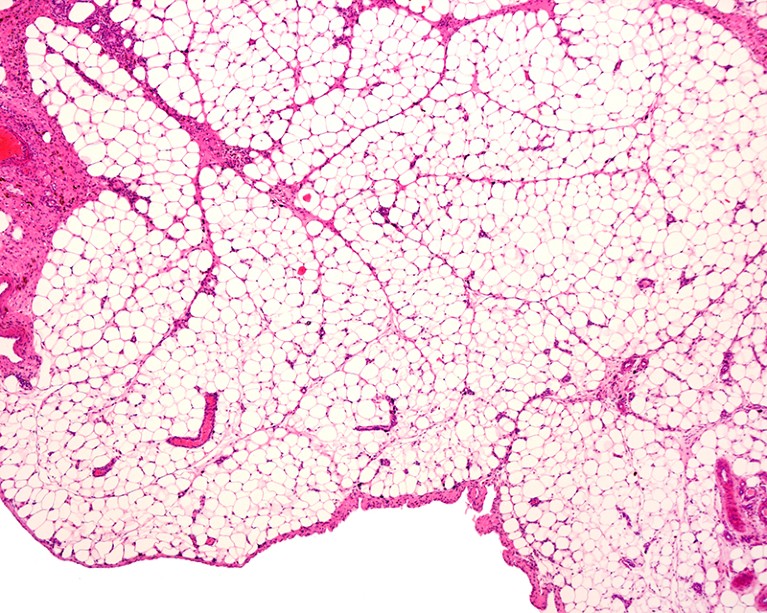
Long-term use of antiretroviral drugs can cause abnormal fat accumulation in people with HIV. Credit: Jose Calvo/SPL
People with HIV are the latest group to benefit from the new generation of anti-obesity drugs . If early data about the treatments’ effects are confirmed, the drugs could become key to controlling the metabolic problems often caused by anti-HIV medications .
Studies presented last week at the Conference on Retroviruses and Opportunistic Infections in Denver, Colorado, suggest that the anti-obesity drug semaglutide not only helps people with HIV to lose weight but also reduces certain conditions associated with fat accumulation that are especially common in people infected with the virus.

Game-changing obesity drugs go mainstream: what scientists are learning
The number of people who are overweight or have obesity is increasing among those with HIV, driving interest among both affected individuals and medical providers in medications such as semaglutide, says Daniel Lee, a physician at the University of California San Diego Medical Center. At his clinic, which treats people with metabolic complications of HIV therapies, around 20% of patients already receive semaglutide or other drugs of the same class.
“For the most part, we’ve had very good experiences with these medications,” Lee says. But, so far, few studies have looked at the effect of the blockbuster anti-obesity drugs on people with HIV.
Unwanted side effects
Although the increasing incidence of obesity in people with HIV is similar to the trend in the general population, certain antiretroviral medications used to suppress HIV could contribute further to weight gain and weight-related conditions in these individuals 1 , 2 .
Semaglutide, marketed as Wegovy for obesity and Ozempic for diabetes, mimics a hormone called glucagon-like peptide 1, which helps to lower blood sugar levels and control appetite. In people who are overweight or have obesity, the drug promotes substantial weight loss 3 .
In a talk on 4 March, researchers at the Centers for AIDS Research Network of Integrated Clinical Systems, a group of HIV clinics across the United States, described their analysis of semaglutide use by 222 individuals receiving HIV care. The drug was associated with an average weight loss of 6.5 kilograms in around one year, or 5.7% of initial body weight.
Helping a fatty liver
Antiretroviral therapies have also been associated with abnormal fat accumulation . One condition affecting 30–40% of people with HIV is metabolic dysfunction-associated steatotic liver disease, which is characterized by the build-up of fat in the liver . As the condition progresses, it can result in liver failure and cardiovascular disease. “We do know that people with HIV have a more aggressive form of fatty liver disease,” says Jordan Lake, an infectious-disease physician at the University of Texas Health Science Center at Houston. But there is currently no approved medication to treat the condition.

Fatty liver disease: turning the tide
She and her colleagues evaluated the use of a weekly injection of semaglutide for around six months in people with both HIV and metabolic dysfunction-associated steatotic liver disease. The results, presented on 5 March, demonstrated that 29% of participants had a complete resolution of the liver disease. “What we saw were really great clinically significant reductions in liver fat even over that short period of time,” Lake said at the conference.
But data from the same study show that participants taking semaglutide lost muscle volume, an effect also observed in other people taking the drug. Individuals who were 60 years of age or older were affected the most. Lee notes that older individuals with HIV are especially vulnerable to semaglutide-linked muscle loss and should be followed closely by health-care providers.
Taming inflammation
Another talk at the conference examined the use of semaglutide for a condition called lipohypertrophy in people with HIV. Characterized by the accumulation of abdominal fat, it “is associated with increased inflammation and carries an increased cardiometabolic risk”, says Allison Eckard, an infectious-disease paediatrician at the Medical University of South Carolina in Charleston. “We have currently few treatments and those treatments often show ineffective response rates.”
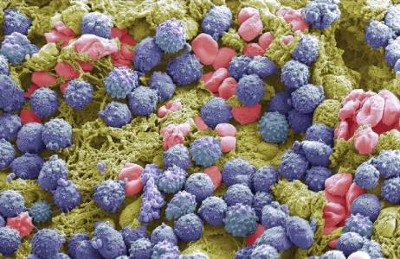
Obesity drugs have another superpower: taming inflammation
In an earlier clinical trial, Eckard and her colleagues scanned the bodies of people with HIV and lipohypertrophy and found that semaglutide helped to reduce abdominal fat. They had presented results from that study in October at IDWeek, a meeting of infectious-disease specialists and epidemiologists in Boston, Massachusetts. And at the conference in Denver, the team showed that a blood marker of inflammation called C-reactive protein fell by almost 40% in study participants who took semaglutide compared with those who did not.
That could be an important effect, because even well-controlled HIV leads to a chronic state of inflammation, Lee says. And, he says, “if there’s increased inflammation, it can lead to end-organ disease of all sorts, including certainly cardiovascular outcomes, but also liver, kidney, brain, cognitive function, you name it”.
Nature 627 , 477-478 (2024)
doi: https://doi.org/10.1038/d41586-024-00691-8
Gómez-Ayerbe, C. et al. Int. J. STD AIDS 33 , 1119–1123 (2022).
Article PubMed Google Scholar
Bansi-Matharu L. et al. Lancet HIV 8 , e711–e722 (2021).
Wilding, J. P. H. et al. N. Engl. J. Med. 384 , 989–1002 (2021).
Download references
Reprints and permissions
Related Articles
- HIV infections
- Medical research

The HIV capsid mimics karyopherin engagement of FG-nucleoporins
Article 24 JAN 24

This is how the world finally ends the HIV/AIDS pandemic
Comment 28 NOV 23

Africa-specific human genetic variation near CHD1L associates with HIV-1 load
Article 02 AUG 23
First US drug approved for a liver disease surging around the world
News 15 MAR 24

Smoking scars the immune system for years after quitting
News 14 FEB 24

No ‘easy’ weight loss: don’t overlook the social cost of anti-obesity drugs
Comment 06 FEB 24

How the body’s cholesterol factory avoids producing too much
Research Highlight 18 MAR 24

Four change-makers seek impact in medical research
Nature Index 13 MAR 24
Professor of Experimental Parasitology (Leishmania)
To develop an innovative and internationally competitive research program, to contribute to educational activities and to provide expert advice.
Belgium (BE)
Institute of Tropical Medicine
PhD Candidate (m/f/d)
We search the candidate for the subproject "P2: targeting cardiac macrophages" as part of the DFG-funded Research Training Group "GRK 2989: Targeti...
Dortmund, Nordrhein-Westfalen (DE)
Leibniz-Institut für Analytische Wissenschaften – ISAS – e.V.
At our location in Dortmund we invite applications for a DFG-funded project. This project will aim to structurally and spatially resolve the altere...
Postdoctoral Fellow
We are seeking a highly motivated PhD and/or MD graduate to work in the Cardiovascular research lab in the Tulane University Department of Medicine.
New Orleans, Louisiana
School of Medicine Tulane University
Posdoctoral Fellow Positions in Epidemiology & Multi-Omics Division of Network Medicine BWH and HMS
Channing Division of Network Medicine, Brigham and Women’s Hospital, and Harvard Medical School are seeking applicants for 3 postdoctoral positions.
Boston, Massachusetts
Brigham and Women's Hospital (BWH)
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
We've detected unusual activity from your computer network
To continue, please click the box below to let us know you're not a robot.
Why did this happen?
Please make sure your browser supports JavaScript and cookies and that you are not blocking them from loading. For more information you can review our Terms of Service and Cookie Policy .
For inquiries related to this message please contact our support team and provide the reference ID below.
Medicare will cover Wegovy to reduce heart disease risk
Medicare will provide coverage for Wegovy for patients with an increased risk of heart attack, stroke or other serious cardiovascular problems , an agency spokesperson said Thursday.
The decision, experts say, could grant millions of patients access to the popular yet expensive weight loss medication.
Medicare, which currently provides health insurance to more than 65 million people in the U.S. , has long been barred from paying for weight loss drugs.
Earlier this month, however, the Food and Drug Administration expanded the approval for Wegovy, saying that it can be prescribed to people who are overweight or have obesity to reduce their risk of heart disease .
The change prompted the Centers for Medicare and Medicaid Services to consider coverage because reducing heart disease risk is a medically accepted use under federal law, the spokesperson said.
Medicare will still not cover Wegovy if it is only being used for weight management, the spokesperson said.
Medicaid, the federal health insurance program for people with low incomes, will also be required to cover Wegovy to reduce heart disease risk.
Lawrence Gostin, director of the O’Neill Institute for National and Global Health Law at Georgetown University, said Medicare providing coverage for Wegovy is “transformational.”
But doing so could undermine Medicare’s “financial stability,” Gostin said. The drug carries a list price of around $1,200 a month, and many patients will likely want a prescription.
A survey from the University of Michigan National Poll on Healthy Aging in December found about 3 in 4 older adults believe Medicare should cover weight loss medications.
A blog post from the Congressional Budget Office last October said that if Medicare did cover weight loss medications such as Wegovy, the net cost to the program “would be significant over the next 10 years.”
“There could be a slippery slope where Medicare ends up paying for the drug to be used for weight loss purposes,” Gostin said. “That would bankrupt Medicare and cause a taxpayer revolt.”
Juliette Cubanski, deputy director of the Medicare policy program at KFF, a nonpartisan group that studies health policy issues, said that while Medicare won't cover the drug solely for weight loss, many people with heart disease are overweight or have obesity.
“We could see Medicare patients with both conditions get coverage of this drug for its heart health benefits,” Cubanski said. “That’s potentially a big deal given the large demand for this drug even in the absence of many insurers covering it.”
The drug will be covered under Medicare Part D, which covers the cost of medications people take at home, the spokesperson said.
It’s not clear how private insurance companies that offer supplemental Part D coverage will respond, Cubanski said, noting that plans do have the ability to add new drugs to the list of drugs they cover in the middle of the year, “but given the cost of this drug, plans might not want to be the first movers.”
Berkeley Lovelace Jr. is a health and medical reporter for NBC News. He covers the Food and Drug Administration, with a special focus on Covid vaccines, prescription drug pricing and health care. He previously covered the biotech and pharmaceutical industry with CNBC.
Obesity: Personal or Social Problem? Essay
Obesity has increased in prevalence and severity over the last few decades. In the US, an estimated 99 million people are obese, which constitutes about 42% of the total adult population (US Centres for Disease Control, 2020). Despite the high and rising prevalence of this health condition, the society has not acknowledged it as an epidemic, and blames the victim for overeating and failure to exercise. However, obesity is both a personal and social problem, and requires a concerted effort to reverse its current trend.
My research on obesity convinced me that preventing obesity goes beyond personal responsibility. Such efforts should include societal initiatives such as promotion of healthy living habits, educating the population on the dangers of obesity, and addressing the systemic constructs that drive people to this condition (Lee, 2016). I learned that placing responsibility on the victims exacerbates the problem, and leads to additional negative outcomes. In contrast, societal involvement in prevention and rehabilitation of obese residents could produce the much needed long-term solution to the condition.
My food journal revealed that I have a strong preference for snacks. These snacks have high-energy and high-sugar density, and a large proportion of saturated fats. In the absence of an intense exercise regimen, I am at risk of becoming obese. Consequently, I have decided to reduce the number and size of snacks taken per day. In addition, I have decided to increase my physical exercises to burn the extra calories. These measures will reduce my risk of developing obesity.
Obesity is a dangerous condition that predisposes individuals to other diseases. The principal responsibility for stemming the condition lies with the individual, but societal interventions are needed to achieve long-term solutions. Engaging in blame game puts the victim at risk and fails to address the systemic problems that result in obesity. These measures will reduce the prevalence of obesity across all age groups and ensure maintenance of healthy lifestyles.
Centers for Disease Control. (2020). National health and nutrition examination survey. US CDC Website. Web.
Lee, B. (2016). The one thing to do to stop the obesity epidemic . Forbes Magazine. Web.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, October 26). Obesity: Personal or Social Problem? https://ivypanda.com/essays/obesity-personal-or-social-problem/
"Obesity: Personal or Social Problem?" IvyPanda , 26 Oct. 2022, ivypanda.com/essays/obesity-personal-or-social-problem/.
IvyPanda . (2022) 'Obesity: Personal or Social Problem'. 26 October.
IvyPanda . 2022. "Obesity: Personal or Social Problem?" October 26, 2022. https://ivypanda.com/essays/obesity-personal-or-social-problem/.
1. IvyPanda . "Obesity: Personal or Social Problem?" October 26, 2022. https://ivypanda.com/essays/obesity-personal-or-social-problem/.
Bibliography
IvyPanda . "Obesity: Personal or Social Problem?" October 26, 2022. https://ivypanda.com/essays/obesity-personal-or-social-problem/.
- The Harmful Effects of Sugar on the Human Body
- Overeating's Causes and Problems
- Eating Disorders: Anorexia, Bulimia and Compulsive Overeating
- Effect of Dietary Protein Content During Overeating
- Coronary Heart Attack and Health Determinants
- The Importance of Mitochondria and Their Purpose
- Weight Loss in an Elderly Male
- Non-Adherence of Diabetic to Their Health Care Regimen
- Social Justice Perspective
- Optimal Foraging Theory in Zoology
- Do Mental Diseases Cause Obesity?
- The Influence of Sleep Deprivation on Human Body
- Reflection “The Spirit Catches You and You Fall Down”
- Red Cell Immunohematology Research
- Disability Discrimination and How to Deal With It
- Election 2024
- Entertainment
- Newsletters
- Photography
- Personal Finance
- AP Buyline Personal Finance
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- March Madness
- AP Top 25 Poll
- Movie reviews
- Book reviews
- Personal finance
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
Medicare can pay for obesity drugs like Wegovy in certain heart patients
FILE - Donna Cooper holds up a dosage of Wegovy, a drug used for weight loss, at her home, March 1, 2024, in Front Royal, Va. The popular weight-loss drug Wegovy may be paid for by Medicare — as long as patients using it also have heart disease and need to reduce the risk of future heart attacks, strokes and other serious problems, federal officials said Thursday, March 21. (AP Photo/Amanda Andrade-Rhoades, File)

- Copy Link copied
Medicare can pay for the popular weight-loss drug Wegovy — as long as the patients using it also have heart disease and need to reduce the risk of future heart attacks, strokes and other serious problems, federal officials said Thursday.
The Centers for Medicare & Medicaid Services issued new guidance that says Medicare Part D drug benefit plans — which are offered through private insurers — could cover anti-obesity drugs that are approved for an additional use.
The move could pave the way for thousands of new prescriptions, resulting in billions of dollars in increased spending, analysts have said.
In practice, the guidance opens the door to wider coverage of Wegovy, the brand name of Novo Nordisk’s obesity medication semaglutide. The U.S. Food and Drug Administration this month approved a label change that allows Wegovy to be used to reduce the risk of cardiovascular events in people who are overweight or have obesity and also have existing heart disease.
Recent research showed that Wegovy cut the risk of heart attack, stroke and other problems by 20% versus a placebo, or dummy drug, in such patients. Cardiologists and other experts said use of semaglutide to reduce the risk of often fatal or disabling conditions could change the way heart patients are treated.
Wegovy carries a price tag of more than $1,300 a month, or $16,000 per year.
Part D plans could begin covering the drug “some time this year,” said Tricia Neuman, a Medicare policy specialist at KFF, a nonprofit that researches health policy.
“Medicare plans may be reluctant to move quickly to cover Wegovy given its relatively high price, particularly because they won’t be able to adjust premiums before next year,” she said.
Even if plans do allow coverage, people who meet the criteria may still face other restrictions. Plans may require higher out-of-pocket fees, prior authorizations or step therapy, in which a patient is required to try a lower-cost drug before proceeding to the new treatment, Neuman said.
Medicare Part D plans are prohibited by law from covering obesity medications used for chronic weight management alone, and that would not change, CMS officials said.
Private insurers are evaluating the guidance — and the new indication for Wegovy — before making coverage decisions, said a spokesperson for AHIP, America’s Health Insurance Plans, an industry trade group.
Drugmakers and obesity advocates have been pushing for expanded coverage, including legislation that would require Medicare to pay for the obesity drugs.
At issue has been whether the cost of the expensive medications will be offset by the savings of reduced spending on medical care related to obesity — and, now, heart disease.
One lingering obstacle to broader use is limited supply of the drug, which has been in shortage for more than a year, according to the FDA. Novo Nordisk officials say they’re working to increase production and access.
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Educational Media Group. The AP is solely responsible for all content.

- Share full article
Advertisement
Supported by
Guest Essay
A Solution on North Korea Is There, if Biden Will Only Grasp It

By John Delury
Dr. Delury is a professor of Chinese studies and an expert on North Korea.
How do you solve a problem like North Korea?
Since the end of the Cold War, it seems that every formula, from threatening war to promising peace, has been tried. And yet, despite being under more sanctions than just about any other country, North Korea developed a nuclear arsenal estimated at 50 warheads and sophisticated missiles that can, in theory, deliver those weapons to targets in the continental United States.
President Biden’s administration has taken a notably more ambivalent approach toward North Korea than his predecessor Donald Trump, who alternately railed at and courted its leader, Kim Jong-un. But we shouldn’t stop trying to come up with bold ways to denuclearize North Korea, improve the lives of its people or lessen the risks of conflict, even if that means making unpalatable choices. On the contrary, there is more urgency now than there has been for years.
As the analyst Robert Carlin and the nuclear scientist Siegfried Hecker, two experienced North Korea watchers, warned in January, Mr. Kim has shifted away from pursuing better relations with the United States and South Korea and closer to President Vladimir Putin of Russia and may be preparing for war. Just days after the two experts issued their warning, Mr. Kim disavowed the long-cherished goal of peaceful reconciliation between the two Koreas, and he called for “completely occupying, subjugating and reclaiming” the South if war breaks out.
It might seem preposterous, even suicidal, for Mr. Kim to seek war. But many people in Ukraine doubted that Mr. Putin would launch a full invasion, right up until the rockets began landing in February 2022, and Hamas caught Israel completely by surprise in October. Both conflicts have had devastating human tolls and are severely taxing America’s ability to manage concurrent crises. The people of both Koreas certainly don’t need war, and neither does the United States.
Mr. Kim’s grandfather started the Korean War, and his father was a master of brinkmanship. Mr. Kim is cut from the same cloth and could instigate a limited conflict by, for example, launching an amphibious assault on South Korean-controlled islands in disputed waters of the Yellow Sea, less than 15 miles off North Korea’s coast. North Korea shelled one of the islands in 2010, killing two South Korean military personnel and two civilians and triggering an exchange of artillery with the South. Just two months ago, Pyongyang fired more than 200 shells into waters near the islands.
Mr. Kim may believe he can manage escalation of such a crisis — threatening missile or even nuclear attack to deter retaliation, perhaps taking the islands, then spinning it as a great propaganda victory and demanding a redrawing of maritime boundaries and other security concessions.
If anything like that scenario came to pass, Mr. Biden would have to explain another outbreak of war on his watch to weary American voters. And it would provide Mr. Trump an opportunity to trumpet his willingness to engage with Mr. Kim.
The mutual distrust between Washington and Pyongyang has only deepened under Mr. Biden, making a breakthrough seem unlikely. Yet there are two underappreciated dynamics at play in North Korea where the United States might find leverage.
The first is China. Despite the veneer of Communist kinship, Mr. Kim and President Xi Jinping of China are nationalists at heart, and they watch each other warily. I have made numerous visits to both nations’ capitals and met with officials and policy shapers. The sense of deep mutual distrust is palpable. Many Chinese look down on neighboring North Korea as backward and are annoyed by its destabilizing behavior. Many North Koreans resent China’s success and resist its influence; Pyongyang could allow much more Chinese investment but doesn’t want to be indebted to Chinese capital. And Mr. Kim seems to delight in timing provocations for maximum embarrassment in Beijing, including testing weapons — prohibited by U.N. sanctions — in the lead-up to sensitive Chinese political events .
Mr. Kim waited six years after becoming the paramount leader in 2011 before making a trip to Beijing to meet Mr. Xi. When Covid emerged, North Korea was among the first countries to shut its borders with China, and ties atrophied during those nearly three years of closure . Last year Mr. Kim chose Mr. Putin, not Mr. Xi, for his first postpandemic summit, skipping China to travel to Russia’s far east. Mr. Kim’s distrust of China is an opening for the United States.
The second point is Mr. Kim’s economic ambitions. For every speech mentioning nukes, he talks at much greater length about the poor state of his nation’s economy while promising to improve it. It was the prospect of American-led economic sanctions being lifted that persuaded him to make the 60-hour train ride from Pyongyang to Hanoi to meet then-President Trump for their second summit in 2019. Mr. Kim explicitly offered to dismantle his main nuclear weapons complex, but Mr. Trump demanded the North also turn over all of its nuclear weapons, material and facilities. The talks collapsed, and Mr. Trump seemed to lose interest in dealing with Mr. Kim. A rare opportunity was wasted, leaving Mr. Kim embittered.
The key to any new overture to North Korea is how it is framed. The White House won’t like to hear this, but success will probably depend on Mr. Biden putting his fingerprints all over the effort, by, for example, nominating a new White House envoy with the stature of someone like John Kerry and announcing a sweeping policy on North Korea and an intelligence review. Only the president can get through to Mr. Kim, and only Mr. Kim can change North Korean policy.
Mr. Biden also would need to use radically different language in framing a new overture as an effort to improve relations and aid North Korea’s economy — not to denuclearize a country that in 2022 passed a law declaring itself a nuclear weapons state. Yes, that would be a bitter pill for America to swallow: Denuclearization has been a guiding principle of U.S. policy toward North Korea for decades. But it is unrealistic to pretend that Pyongyang will surrender its nuclear weapons anytime soon. Disarmament can remain a long-term goal but is impossible if the two sides aren’t even talking.
Mr. Biden’s Republican opponents might accuse him of appeasement by engaging with Mr. Kim, but that is precisely what Mr. Trump tried. Mr. Kim, likewise, might mistake boldness for weakness. But it would be easy enough for the United States to pull back from diplomacy if it goes nowhere.
The United States must be realistic. The world is very different from when the United States, China, Russia, Japan and the two Koreas came together in the 2000s for negotiations to denuclearize North Korea. The country is now a formidable nuclear power, and its leader sounds increasingly belligerent. The president needs to get the wheels of diplomacy turning before it’s too late.
John Delury (@JohnDelury) is a professor of Chinese studies at Yonsei University in Seoul, the Tsao fellow at the American Academy in Rome and the author of “Agents of Subversion: The Fate of John T. Downey and the CIA’s Covert War in China.”
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow The New York Times Opinion section on Facebook , Instagram , TikTok , X and Threads .

IMAGES
COMMENTS
Obesity has become a global epidemic and is one of today's most public health problems worldwide. Obesity poses a major risk for a variety of serious diseases including diabetes mellitus, non-alcoholic liver disease (NAFLD), cardiovascular disease, hypertension and stroke, and certain forms of cancer (Bluher, 2019).Obesity is mainly caused by imbalanced energy intake and expenditure due to a ...
Essay on Obesity - With Causes and Treatment (Essay 6 - 600 Words) We all know how troubling the problem of obesity truly is. It is mainly a form of a medical condition wherein the body tends to accumulate excessive fat which in turn has negative repercussions on the health of an individual.
Health Impacts. Obesity is the root cause for many medical diseases, including heart disease, stroke, type 2 diabetes, and certain types of cancer. It is also a risk factor for poor self-esteem, depression, obstructive sleep apnea, osteoarthritis, gout, female infertility, gallstones, pancreatitis, and non-alcoholic fatty liver disease.
Despite public health efforts, these disorders are on the rise, and their consequences are burgeoning. 1 The Centers for Disease Control and Prevention report that during 2017 to 2018, the prevalence of obesity in the United States was 42.4%, which was increased from the prevalence of 30.5% during 1999 to 2002. 2 Among those afflicted with ...
Obesity and BMI (body mass index) are both tools of measurement that are used by doctors to assess body fat according to the height, age, and gender of a person. If the BMI is between 25 to 29.9, that means the person has excess weight and body fat. If the BMI exceeds 30, that means the person is obese. Obesity is a condition that increases the ...
The obesity epidemic. The World Health Organization (WHO) defines overweight and obesity as abnormal or excessive fat accumulation that presents a risk to health (WHO, 2016a).A body mass index (BMI) ≥25 kg/m 2 is generally considered overweight, while obesity is considered to be a BMI ≥ 30 kg/m 2.It is well known that obesity and overweight are a growing problem globally with high rates in ...
This refers to a medical condition in which a person's body has high accumulation of body fat to the level of being fatal or a cause of serious health complications. Obesity as a Worldwide Problem and Its Solution. A huge sum is spent every year by the government for the welfare of the subjects.
U.S. adult obesity prevalence between 2015 and 2016 was nearly 40% - about 93.3 million people, according to the CDC. The highest rate (42.8%) was among adults between the ages of 40 and 59; the ...
Still, the bulk of the obesity problem—literally—is in adults. According to Frank Hu, chair of the Harvard Chan Department of Nutrition, "Most people gain weight during young and middle adulthood. The weight-gain trajectory is less than 1 pound per year, but it creeps up steadily from age 18 to age 55.
1. Introduction. Obesity is a complex, multifactorial, and largely preventable disease (), affecting, along with overweight, over a third of the world's population today (2,3).If secular trends continue, by 2030 an estimated 38% of the world's adult population will be overweight and another 20% will be obese ().In the USA, the most dire projections based on earlier secular trends point to ...
In 2004, the CDC reported that 66.3% of the adults in the US are overweight or obese. True but unbelievable, a stressful mentally and insufficient sleep could also result in obesity. Genetic reasons seem to be silent killers in this direction. This essay, "Obesity as a Worldwide Problem and Its Solution" is published exclusively on IvyPanda's ...
Between 1999 and 2016, the prevalence of obesity in both children and adults has risen steadily. While obesity is a problem across the United States, it affects some groups of people more than others. Based on 2015-2016 data, obesity rates are higher among Hispanic (47 percent) and Black adults (47 percent) compared with white adults (38 percent).
Obesity is a common health problem caused by genetic factors and a person's lifestyle. Excessive caloric intake in Americans and a decrease in exercise have led to about 35% of the adult population being obese (Kirkwood, 2018). Obesity is diagnosed with a body mass index greater than 30 (Kirkwood, 2018). The morbidity of obesity is high, but ...
Obesity is a major health problem. It is a risk factor for diabetes, stroke and heart disease. Excessive consumption of junk foods is the number one cause of obesity. Junk or fast foods are rich in calories and unhealthy fats. When we consume more calories than our body can burn, it will convert the excess calories into fat.
Accordingly, 93 papers are identified from the review articles as primary studies from an initial pool of over 700 papers addressing obesity. Consequently, this study initially recognized the significant potential factors that influence and cause adult obesity. ... Therefore, ML has been applied to questions and problems in obesity-based ...
Obesity significantly increases the risk of various health problems. It is a major risk factor for noncommunicable diseases (NCDs) such as cardiovascular diseases, diabetes, musculoskeletal disorders, and some cancers. Moreover, obesity can lead to psychological issues, including depression, anxiety, and low self-esteem.
Eating a healthy lifestyle is the main thing to help lose weight. It says that to lose weight it's 80% diet and 20% gym. Along with going to the gym and eating healthy, it is important to drink a lot of water. Water will flush the system of all toxins that could add to weight gain.
Obesity Essay: Obesity is a condition that occurs when a person puts on excess body fat. It is a sudden and unusual increase in body fat. It can lead to heart-related diseases, blood pressure, hypertension, cholesterol, and various other health issues. The main cause of obesity is over-eating. Consuming junk food and staying away for physical ...
Read this essay to learn about the meaning, causes, types, treatment, principles of dietary management and complications of overweight/ obesity. Meaning of Obesity: Obesity is a big problem of health. Obesity is a condition in which there is excessive weight gain in the body, an increase of 10% over the ideal weight is termed as obesity.
As obesity rates rise in the U.S. and worldwide, new weight-loss drugs surge in popularity. By Drew DeSilver. Obesity affects roughly 42% of U.S. adults, according to the Centers for Disease Control and Prevention (CDC). And about two-thirds of Americans (65%) say willpower alone usually isn't enough for most people who are trying to lose ...
Besides health complications, obesity causes an array of psychological effects, including inferiority complex among victims. Obese people suffer from depression, emanating from negative self-esteem and societal rejection. In some cases, people who become obese lose their friends and may get disapproval from teachers and other personalities ...
Clinical trials suggest that they could reduce the risk of heart attacks, kidney disease and perhaps even Alzheimer's. By the end of the decade annual sales of obesity medicines could hit $80bn ...
In people who are overweight or have obesity, the drug promotes substantial weight loss 3. In a talk on 4 March, researchers at the Centers for AIDS Research Network of Integrated Clinical Systems ...
The new obesity drugs might be an exception to a chronic, deadly problem: the failure to stick with medication. Credit...Photo Illustration by Matt Chase Supported by By Gina Kolata Most people ...
Amgen Sees a 2024 Sales Jump, Sets Sights on Obesity Market. In one 68-week trial of semaglutide, the active ingredient in Novo's Ozempic and Wegovy, people on the drug lost an average of about ...
Medicare will provide coverage for Wegovy for patients with an increased risk of heart attack, stroke or other serious cardiovascular problems, an agency spokesperson said Thursday. The decision ...
Obesity has increased in prevalence and severity over the last few decades. In the US, an estimated 99 million people are obese, which constitutes about 42% of the total adult population (US Centres for Disease Control, 2020). Despite the high and rising prevalence of this health condition, the society has not acknowledged it as an epidemic ...
By JONEL ALECCIA. Updated 1:41 PM PDT, March 21, 2024. Medicare can pay for the popular weight-loss drug Wegovy — as long as the patients using it also have heart disease and need to reduce the risk of future heart attacks, strokes and other serious problems, federal officials said Thursday. The Centers for Medicare & Medicaid Services issued ...
March 26, 2024. Illustration by Shoshana Schultz/The New York Times. 901. By Elizabeth Spiers. Ms. Spiers, a contributing Opinion writer, is a journalist and digital media strategist. James and ...
Just days after the two experts issued their warning, Mr. Kim disavowed the long-cherished goal of peaceful reconciliation between the two Koreas, and he called for "completely occupying ...