- Case report
- Open access
- Published: 04 March 2024

Surgical repair of tetralogy of Fallot in a 78-year-old woman: a case report
- Yuzo Katayama ORCID: orcid.org/0000-0002-2206-8212 1 ,
- Sho Isobe 1 ,
- Tsukasa Ozawa 1 &
- Takeshiro Fujii 1
Journal of Medical Case Reports volume 18 , Article number: 128 ( 2024 ) Cite this article
559 Accesses
1 Altmetric
Metrics details
Tetralogy of Fallot is a congenital heart disease mostly diagnosed and treated in early childhood. However, there are some adult cases receiving treatment.
Case presentation
We describe a 78-year-old Japanese woman who presented with severely hypertrophic right ventricle, ventricular septum defect, overriding aorta, and severe infundibular stenosis in the right ventricular outflow tract. As hypoxemia was mild and daily exertion was sufficiently possible, home oxygen therapy was introduced. After 1 month, she was referred because of a positive blood culture. The blood culture test was positive four times, therefore, the antibacterial drug was administered according to active infective endocarditis. SpO 2 repeatedly decreased during hospitalization, thus oxygen was needed. As there were infective endocarditis onset and progressive hypoxemia, we planned a surgical correction.
Tetralogy of Fallot was diagnosed and successfully treated with complete surgical correction, and the development of infective endocarditis was the definitive indication for surgery at this late age.
Peer Review reports
Early surgical correction has been established as the best treatment for tetralogy of Fallot (TOF). Without surgical correction, most patients die during childhood, making adult patients with uncorrected TOF rare. Additionally, surgical indications for untreated adult TOF are mostly due to progression of heart failure [ 1 ]. We report an extremely rare case in which intracardiac repair was performed on an elderly cyanotic patient with infective endocarditis.
Presentation of case
The case involved a 78-year-old Japanese woman diagnosed with ventricular septal defect (VSD) during her elementary school days. In her 40s, she felt exertional dyspnea fatigue, but was followed up without any restrictions. At 77 years, she consulted our adult congenital heart disease clinic for increasing symptoms since her 70s. She had a history of hypertension in her 40s and was taking oral calcium channel blockers (nifedipine; 10 mg) and angiotensin receptor blockers (ARBs; candesartan cilexetil; 4 mg) prescribed by a family doctor, and no other previous medical history. Although she had one pregnancy and birth, there were no special events when she gave birth. There was no history of smoking and drinking and no special cardiovascular events in her family history. She has been working as a typist in an office since her 20s.
Electrocardiography showed sinus rhythm, right bundle-branch block, and right ventricular hypertrophy with secondary ST–T wave abnormalities. Chest radiography showed an enlarged cardiac silhouette and dilated pulmonary arteries. Transthoracic echocardiography and contrast computed tomography (CT) revealed overriding aorta, right ventricular outflow tract (RVOT) stenosis (Fig. 1 ), and right ventricular hypertrophy in addition to VSD. The final diagnosis was tetralogy of Fallot (TOF). As hypoxemia was mild and daily exertion was sufficiently possible, home oxygen therapy was introduced after comprehensively explaining the disease and its prognosis.
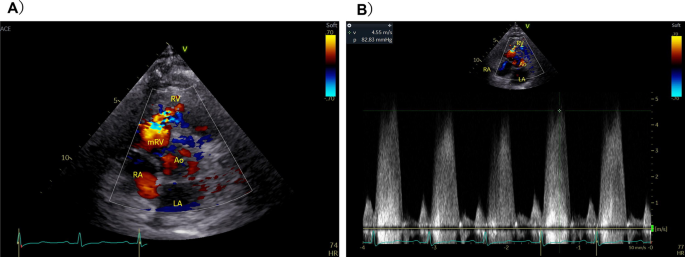
Transthoracic echocardiography revealing a ventricular septum defect in the perimembranous region and right ventricular outflow tract stenosis. A Color Doppler echo showing the short axis view. B Peak pressure gradient was 82 mmHg
After 1 month, she was referred from the family doctor and hospitalized because of a positive blood culture test. The physical findings on admission were as follows: body temperature 38.1 ℃, blood pressure 135/71 mmHg, pulse rate 71 beats per minute and regular, and SpO 2 87%. Systolic murmur was heard at the left sternal border of the second intercostal space, not rales. No special findings were found on the palpebral conjunctiva, fingers and toes, palms, and soles of the feet. No neurological abnormal findings were observed.
Laboratory findings on admission were as follows: WBC 11,000/μL, Hb 17.5 g/dL, Hct 54%, Plt 19.7/μL, CRP 4.1 mg/dL, AST 24 IU/L, ALT 13 IU/L, LDH 240 IU/L, Na 139 mEq/L, K 3.9 mEq/L, Cl 105 mEq/L, TP 7.0 g/dL, Alb 4.1 mg/dL, BUN 14 mg/dL, Cr 0.59 mg/dL, eGFR 73.1, BNP 88.4 pg/dL, urine specific gravity 1.015, PH 7.0, white blood cell count 0. The blood culture test was positive four times (Lactobacillus rhamnosus) and antibiotic susceptibilities of this bacterium were as follows; penicillin G > 2, aminobenzylpenicillin > 2, ceftriaxone 0.5, gentamicin 1, minocycline 0.25, vancomycin > 16, teicoplanin 16, and levofloxacin 2. Therefore, continuous intravenous administration of ceftriaxone 2 g/day was administered for 6 weeks according to active infective endocarditis. At the time of admission, the patient had a fever of 38 °C, but it remained at 36 °C 3 days after the start of administration. The inflammation data also normalized and negative blood cultures were confirmed twice 3 weeks after starting administration. SpO 2 repeatedly decreased to 80% during hospitalization, thus oxygen was started and 3 L was needed to maintain around 90%. Transthoracic echocardiography, thoracic and abdominal CT, head magnetic resonance imaging (MRI), and upper and lower gastrointestinal endoscopy were also performed, but the site or route of infection could not be identified.
Cardiac MRI revealed severe infundibular stenosis and tiny pulmonary valve regurgitation (Additional file 1 : Videos S1 and S2), normal right ventricular contractility, 90% normal left ventricular volume, and 0.67 Qp/Qs (pulmonary blood flow/systemic blood flow ratio). As there were progressive hypoxemia and infective endocarditis onset, we planned a surgical correction after infection control of infective endocarditis.
The operation was performed on full cardiopulmonary bypass. The hypertrophic muscle obstructing the RVOT was resected up to 20 mm and the VSD was closed with a patch. A perforation was found in the left semilunar cusp of pulmonary valve and the lesion accompanied by changes in curability was closed directly. The perforation may have been the source of infection. Intraoperative transesophageal echocardiography showed improvement in the RVOT to 2.5 m per second.
Although all follow-up blood culture tests after surgery were negative, ceftriaxone was administered for 4 weeks. The preoperative BNP level of 79 pg/dL increased to 727 pg/dL on day 8 postoperation, but improved to the same preoperative level after oral diuretic discontinuation, and echocardiography revealed normal cardiac function. The patient was discharged on day 35 postoperation at New York Heart Association (NYHA) class I after removing oxygen. It has now been 2 years since the operation, and she is still doing well.
Discussion and conclusion
Early surgical correction has been established as the best treatment for TOF. Without surgical correction, most patients die during childhood [ 1 ], making adult patients with uncorrected TOF rare. However, there was a report of uncorrected TOF in the oldest patient aged 86 years [ 2 ].
There have been reports of adults with tetralogy of Fallot developing infective endocarditis and brain abscess, but surgical intervention has been avoided [ 3 , 4 ]. There have only been two reports of repair surgery for tetralogy of Fallot in elderly patients aged 75 years or older, but in both cases the chief complaints were cyanosis and dyspnea [ 5 , 6 ]. This case of a 78-year-old patient was an extremely rare case in which surgical intervention was indicated due to cyanosis and infective endocarditis.
Most patients with TOF have cyanosis from birth or the first year of life because of right-to-left shunting. If resistance to flow through the RVOT is less than resistance to flow through the aorta, there will be left-to-right shunt flow across the VSD without peripheral cyanosis and there will be a late presentation similarly to our case. Additionally, the patient has suffered from hypertension since her 40s and had high peripheral vascular resistance, which was one possible reason for the delayed cyanosis appearance. Furthermore, hemodynamic evaluation was performed only with four-dimensional (4D) flow MRI, and blood flow evaluation via collateral blood circulation was not considered. Therefore, there may be a discrepancy with the evaluation by cardiac catheterization. Considering the preoperative clinical findings and postoperative left heart failure, we believe that there may have been a large amount of blood flow from small collateral circulation channels.
There have been several reports on the surgical outcome of intracardiac repair for adult TOF. Sadiq et al . showed acceptable morbidity and mortality rates with good long-term surgical outcome [ 7 ], whereas Hörer et al . showed a high early mortality rate (15.4%) [ 8 ]. Opinions were also divided on the use of transannular patching (TAP), with Sadiq et al . concluding that TAP is not a risk factor, whereas Hörer et al . concluded that TAP is a risk factor [ 7 , 8 ]. Considering the patient’s life expectancy and the preoperative pulmonary valve annulus system being 20 mm, we decided to form an outflow tract of up to 20 mm without TAP.
Despite the sufficient preoperative left ventricular volume and the restriction of RVOT formation, the increase in the left ventricular volume and pleural effusion after surgery required control of left heart failure. Although premised on improving hemodynamics, it appeared that the strategy for outflow tract formation similar to that in childhood should be reconsidered for the elderly. In our case, we performed complete surgical correction of TOF at 78 years of age, and the development of infective endocarditis was the definitive indication for surgery at rare old age.
Availability of data and materials
Not applicable.
Abbreviations
Ventricular septal defect
Right ventricular outflow tract
- Tetralogy of Fallot
Murphy JG, Gersh BJ, Mair DD, Fuster V, McGoon MD, Ilstrup DM, et al . Long-term outcome in patients undergoing surgical repair of tetralogy of Fallot. N Engl J Med. 1993;329:593–9.
Article CAS PubMed Google Scholar
Alonso A, Downey BC, Kuvin JT. Uncorrected tetralogy of Fallot in an 86-year-old patient. Am J Geriatr Cardiol. 2007;16:38–41.
Article PubMed Google Scholar
Sousa P, Santos W, Marques N, Cordeiro P, Ferrinha R, et al . A 72-year-old woman with an uncorrected tetralogy of Fallot presenting with possible pulmonary endocarditis: a case report. J Med Case Rep. 2013;7:150–3.
Article PubMed PubMed Central Google Scholar
Dubey A, Bawiskar N, Kumar S, Lahole S, Somani A. Tetralogy of Fallot—not an innocuous abnormality in adult. J Evolution Med Dent Sci. 2020;16(9):1397–8.
Article Google Scholar
Semeraro O, Scott B, Vermeersch P. Surgical correction of tetralogy of Fallot in a seventy-five year old patient. Int J Cardiol. 2008;128:e98–100.
Hussain FTN, Grogan M, Dearani JA. Surgical repair of tetralogy of Fallot at age 83. World J Pediatr Cong Heart Surg. 2012;3(4):518–20.
Sadiq A, Shyamkrishnan KG, Theodore S, Gopalakrishnan S, Tharakan JM, Karunakaran J. Long-term functional assessment after correction of tetralogy of Fallot in adulthood. Ann Thorac Surg. 2007;83:1790–5.
Hörer J, Friebe J, Schreiber C, Kostolny M, Cleuziou J, Holper K, et al . Correction of tetralogy of Fallot and of pulmonary atresia with ventricular septal defect in adults. Ann Thorac Surg. 2005;80:2285–91.
Download references
Acknowledgements
We thank Dr. Edward Barroga ( https://orcid.org/0000-0002-8920-2607 ) for editing the manuscript.
This study was not funded by any agency or institution.
Author information
Authors and affiliations.
Division of Cardiovascular Surgery, Department of Surgery, Toho University Omori Medical Center, 6-11 Omori-Nishi Ota-Ku, Tokyo, 143-8541, Japan
Yuzo Katayama, Sho Isobe, Tsukasa Ozawa & Takeshiro Fujii
You can also search for this author in PubMed Google Scholar
Contributions
YK drafted the original manuscript. SI, TO, and TF substantially contributed to the revisions of the manuscript drafts. All authors have approved the submitted version of the manuscript and agree to be accountable for any part of the work. All the authors read and approved the final manuscript.
Corresponding author
Correspondence to Yuzo Katayama .
Ethics declarations
Ethics approval and consent to participate.
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Written informed consent was obtained from the patient for the publication of this case report and its accompanying images.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interest associated with this case report.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: video s1:.
Magnetic resonance imaging scan of the heart revealing right ventricular outflow tract stenosis (wall shear stress: RA + RV + PA). Video S2: Magnetic resonance imaging scan of the heart revealing right ventricular outflow tract stenosis (energy loss: RA + RV + PA).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Katayama, Y., Isobe, S., Ozawa, T. et al. Surgical repair of tetralogy of Fallot in a 78-year-old woman: a case report. J Med Case Reports 18 , 128 (2024). https://doi.org/10.1186/s13256-024-04414-5
Download citation
Received : 29 September 2023
Accepted : 26 January 2024
Published : 04 March 2024
DOI : https://doi.org/10.1186/s13256-024-04414-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adult congenital heart disease
- Endocarditis
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Research article
- Open access
- Published: 10 December 2019
Pregnancy outcomes among 31 patients with tetralogy of Fallot, a retrospective study
- Kana Wang 1 , 2 ,
- Junguo Xin 3 ,
- Xiaodong Wang 1 , 2 ,
- Haiyan Yu ORCID: orcid.org/0000-0002-1656-4906 1 , 2 &
- Xinghui Liu 1 , 2
BMC Pregnancy and Childbirth volume 19 , Article number: 486 ( 2019 ) Cite this article
13k Accesses
13 Citations
2 Altmetric
Metrics details
Tetralogy of Fallot (TOF) is a severe type of congenital heart disease (CHD) and it confers substantial risk to mother and fetus for pregnant women. However, the outcome of pregnancy in women with TOF has not been well studied.
Women with TOF who have been seen and/or delivered at our tertiary-care hospital between April 2008 and January 2018 were retrospective reviewed.
A total of 31 pregnant women with TOF were identified during ten-year period. Among these patients, cardiac defects remained uncorrected in 12 women and were surgically repaired in 19 women. The frequency of miscarriages, premature birth, and the percentage of neonates of small for gestational age (SGA) were greater in the uncorrected group than the surgically repaired group (16.67% vs 0, 50% vs 5.26, 41.67% vs 10.53% respectively). The neonatal mortality and fetal mortality were not observed in the surgically repaired group, but were observed in the uncorrected group [3.23% (1/31) and 6.45(2/31) respectively]. Furthermore, the obstetric and cardiac complications in the two groups were stratified and analyzed.
Conclusions
Surgical correction of TOF is associated with improved maternal and perinatal outcome. However, pregnancy in women with uncorrected TOF was still seen and it was observed at a rate of 1.4/10,000 in our medical center during ten year period. The high degree of ventricular dilatation heart, high functional classifications, serious cardiac arrhythmias and pulmonary hypertension appeared to be associated with maternal and neonatal risks.
Peer Review reports
Tetralogy of Fallot (TOF) is a severe type of congenital heart disease (CHD) with an incidence of 10% in all reported CHD, which is characterized by four components: large ventricular septal defect (VSD), overriding aorta, right ventricular hypertrophy, and right ventricular outflow tract obstruction [ 1 ]. In the past decades, the overall prognosis of CHD has been greatly improved and many patients could reach adulthood because of early diagnosis and timely therapy. However, TOF as a complex and cyanotic type of CHD, its prognosis remain poor, especially in those who did not undergo surgical repair, and it remains the leading cause of indirect maternal mortality among CHD patient with pregnancy. There are great variations in cardiac complication rates for maternal mortality among published studies for TOF patients with pregnancy, it ranged from 0 to 17.5% [ 2 ]. It has been thought that it is approximately 1/10,000 in developed countries and may be up to 25 times higher in the developing countries [ 3 ].
After surgical repair, the majority of young women with TOF could survive into their reproductive age. Without repair, TOF patients rarely reach childbearing age and get pregnant. Since pregnancy introduces extra load on the heart, and can damage cardiac functions, resulting in the increase in both maternal and perinatal morbidity [ 4 , 5 ]. Previous studies have demonstrated that cardiac and obstetric complications are more likely to occur in patients without surgical repair [ 6 , 7 , 8 ]. The most common cardiac complications include progressive dilatation of the right ventricle and ventricular failure, thromboembolism, atrial and ventricular arrhythmias, progressive aortic root dilatation and endocarditis [ 1 , 9 ]. The common obstetric complications include the increased risk in miscarriage, premature birth, and low birth weights, postpartum hemorrhage, paradoxical embolism, thromboembolism, congestive cardiac failure, infective endocarditis, and arrhythmias [ 6 ]. Among these complications, the pulmonary hemorrhage, brain abscess and thromboembolism have been thought to be the most common causes of death [ 1 , 10 ].
To date, the outcomes of pregnant women with TOF have not not well characterized due to limited number of studied cases and lack of data for close follow-up. Therefore, the management of TOF pregnant women remains challenging. Here, we present 31 cases of pregnant women with or without surgical repair for TOF.
This is a retrospective study with an approval from the Institutional Review Board of West China Second University Hospital. Between April 2008 and January 2018, a total of 85,184 pregnant women have been seen and gave birth in West China Second University Hospital. A total of 31 pregnant women with TOF were identified, and further reviewed. During analyses, we compared the overall clinical characteristics, cardiac and obstetric complications, outcome of pregnancy complications between the corrected and the uncorrected groups. In addition, we analyzed the maternal hemodynamic features and obstetric outcomes in each individual patients with uncorrected TOF.
All pregnant women with or without surgical repair were evaluated by echocardiography, electrocardiography (ECG), and routine clinical examinations such as blood pressure (BP), and heart rate (HR). Hypertension, diabetes mellitus, and other pregnancy associated diseases were taken into consideration in the clinical characterization of the patients.
Surgical correction for TOF
Among 31 TOF pregnant patients, 12 cases underwent cardiac surgery before juvenile age (< 18 years old), and 6 cases before 25 years old. The median age for cardiac surgery was 15.52 years. The longest interval from the surgical correction to pregnancy was 29 years and the shortest was 1 year. The average interval was 11.84 years. Except one patient received two cardiac operations (cardiopulmonary correction with pulmonary artery valve replacement at 11 years before pregnancy, and atrial septal defect reparation with tricuspid valvuloplasty at 3 years before pregnancy), the remaining studied patients had one-time cardiac surgery.
Echocardiography
During the past ten years, echocardiography for the detection of CHD and the assessment of haemodynamic status has become mature. All of our patients have been evaluated with this reliable technique. The anatomic feature of TOF including the overriding aorta, anterior deviation of the outlet septum, pulmonary stenosis and right ventricular hypertrophy have been identified and characterized by echocardiography in all studied patients [ 1 ]. The diagnosis of TOF by echocardiography has been made by the presence of a ventricular septal defect and a large overriding aorta, as well as the haemodynamic deviation for valvar functions (right ventricular pressure, ventricular dimensions, and ventricular function).
Electrocardiogram
Arrhythmia may become manifest during pregnancy with TOF and other CHD. The 24-h ambulatory ECGs were performed in patients when they had abnormal ECG pattern or in a setting in which the patient was prone to the development of arrhythmia, such as the presence of abnormal electrolyte level.
Pregnancy data
Data related to pregnancy in this study were mainly collected around the delivery. These data included gestational-age of newborn at birth, type of delivery, blood loss at delivery, birthweight, Apgar score and postpartum hemorrhage. Fetal and neonatal echocardiographic data have also been collected for evaluation of CHD.
Descriptive statistics, such as frequency, percentage, mean, standard deviation (SD), and the range were used for the presentation of variables. The normally distributed variables were presented as Means ± SD and they were compared using Student’s t-test for the differences between groups. The distribution of blood loss was presented in the format of Median ± IQR (interquartile ranges) and was compared using Mann–Whitney U test. Categorical variables, such as clinical characteristics and complications, were expressed as proportions and compared using Chi-square test or Fisher’s exact probability test. All statistical analyses were performed in SPSS (version 20.0). An alpha of 0.05 is used as the cutoff for significance.
Patient characteristics
Thirty-one pregnant women with TOF were identified and analyzed in this study. The sociodemographic information for these patients, including age, region, education degree, gravidity and parity, were collected and summarized in the Table 1 . The age of the studied patients ranged from 19 to 39 years. Specifically, the age was between 22 and 35 years (median: 28 years old) in the surgically repaired group and between 19 and 39 years (median age was 26.5 years old) in the uncorrected group. The majority of the patients who did not undergo TOF repair surgery came from remote rural areas and did not have higher education. The frequency of abortion and gestation were higher in uncorrected group than in the surgically repaired group. Of note, 94.74% (18/19) pregnant women in the corrected group were primiparity.
The surgically procedures for TOF repair included the closure of the VSD by insertion of transannular patches, rendering the pulmonary valves incompetent, right ventricle infundibulectomy, and transannular enlargement of the right ventricular outflow tract, as detailed in the Method section. Despite of variation of the surgical procedures, the repair operations reached the goal for correction in the majority of patients, except two patients who still had residual shunt after ventricular patch.
Cardiac and obstetric complications in two groups
Cardiac and obstetric characteristics in 31 pregnant women with TOF are summarized in Table 2 and Table 3 , respectively. Obstetric and cardiac complications were observed more frequently in the uncorrected group. The rate of prematurity was significantly higher in the uncorrected group than in surgically repaired group (50% vs 5.26%, respectively, P = 0.007). The frequency of spontaneous abortion was also greater in the uncorrected group than in the surgically repaired group (16.67% vs none, respectively). The percentage of small-for-gestational-age newborn was 41.67% in the uncorrected group and 10.53% in the surgically repaired group ( P = 0.078). The mean of neonatal birth weight was significantly lower in the uncorrected group than in the surgically repaired group ( P < 0.001). However, the total days of stay in hospital and blood loss at delivery were similar in both groups ( P = 0.866 and 0.586 respectively). The rate of postpartum hemorrhage was 10.53% in the surgically repaired group and 8.33% in the uncorrected group [due to placenta previa in both groups (2 vs 1 case, respectively), instead of abnormal blood coagulation. The CHD [Patent ductus arteriosus (PDA) and patent foramen ovale (PFO)] was observed in one baby from the surgically repaired group (Table 2 ).
Most of patients in the surgically repaired group had good cardiac functional status with NYHA class of I-II, which was significantly better than uncorrected group (63.16% vs 16.67%, respectively, P = 0.031). Ten (83.33%) cases had cardiac function NYHA class III or higher in the uncorrected group. Cardiac diameter and ventricular systolic function were assessed in all patients. The moderate or severe right ventricle dilation was found in all uncorrected patients (12 cases, 100%), but only in 9 cases (47.37%) in the surgically repaired group. The right ventricular dilation was absent or in a very mild degree in the remaining 10 corrected cases (52.63%) ( P = 0.004). Of note, one uncorrected patient showed a limited systolic function (EF = 31%, FS = 16%) and pulmonary arterial hypertension (PAH). In the current study, the most common complications attributable to TOF were outflow tract and valve condition, ventricular shunting with ventricular septal defect and arrhythmias. Pulmonary valve stenosis was seen in all uncorrected patients (100%) and in 4 cases (21.05%) of corrected TOF ( P < 0.001). Pulmonic regurgitation was found in 6 (31.58%) in the surgically repaired patients but none in uncorrected patients ( P = 0.059). According to the ECGs, ventricular hypertrophy was present in all uncorrected patients (100%) but only 5 cases in surgically repaired groups (26.32%, P < 0.001). Following surgical repair, ECG became normal in 5 patients (26.32%), but complete right bundle branch block (CRBB) have been still detected in 9 (47.37%) corrected patients. No other abnormal ECG was found between two groups (Table 3 ).
Maternal and perinatal outcomes in the women with uncorrected TOF
The detailed clinical information concerning maternal and perinatal outcomes in the women with uncorrected TOF is summarized in Table 4 . Among them, five women (41.67%) were primigravidae (G1P0), the remaining 7 women had a history of abortion or childbirth. Except that one patient with intrauterine fetal death who underwent transvaginal complete curettage of uterine cavity, the mode of delivery in remaining patients was cesarean section (C-section). During the operation, 6 patients were under general anesthesia, 4 patients under epidural anesthesia, and 1 patient under combined spinal-epidural anesthesia. Regarding the obstetric complications related to the prematurity including miscarriages, premature labor, small for gestational age (SGA) and low birth weight infant at term (LBWI), half of women (50%) were due to premature rupture of fetal membranes (PROM) and/or prenatal hemorrhage. The rate of SGA was 41.67% ( n = 5). One case with NYHA class IV complicated with severe pulmonary hypertension and limited systolic function had to terminate pregnancy at 27 + 6 weeks. That patient was transferred to the Department of Cardiology for further treatments and survived. Unfortunately, her baby died at the 7th day after birth due to neonatal pneumonia, septicemia and intracranial hemorrhage. The maternal mortality in this study was none. Neonatal mortality and fetal mortality were observed only in the uncorrected group with a rate of 3.23% (1/31) and 6.45% (2/31), respectively (Table 4 ).
Tetralogy of Fallot is a severe type of CHD and it is characterized by the hemodynamic alterations due to anatomic abnormality, with varied degree of comprised cardiac functions, including ventricular dysfunction, right ventricular systolic dysfunction, right ventricular dilation, outflow tract obstruction, and pulmonary hypertension [ 11 ]. After surgical repair of TOF, the majority of young women could survive into their reproductive age. But it is generally known that heart disease constitutes a leading nonobstetric cause of maternal mortality, especially in patients with the cyanotic and complex shunt lesions [ 6 ]. Previous studies for pregnant women with TOF showed that pregnancy confers a considerable risk to these patients. The adverse cardiovascular events may be associated with right ventricular dysfunction, severe pulmonary hypertension, and severe pulmonic regurgitation with RV dysfunction [ 3 , 11 ]. It has been demonstrated that abnormal uteroplacental Doppler flow (UDF) was associated with right ventricular function parameters, suggesting that maternal cardiac dysfunction contributes to defective placentation and/or placental perfusion, which subsequently increases the incidence of obstetric and neonatal complications [ 12 ].
With emerging more advanced diagnostic and therapeutic approaches, the overall prognosis of TOF patients has been remarkably improved in the past decades. However, we occasionally encountered that women with uncorrected TOF got pregnant. Due to the extra cardiac load during pregnancy, women with uncorrected TOF had much higher maternal and perinatal morbidity compared to general population [ 1 , 2 , 3 , 4 , 5 , 9 ]. These cases are relatively rare and almost all of published studies for these patients in the literature were case reports. Thus far, no standard regimen has been established to manage these patients. Accordingly, it will be extremely beneficial to study these cases in a comprehensive manner. This study was for the first time to collect over 30 cases of TOF patients from a single center and perform comparative analysis between uncorrected cases and surgically repaired cases.
It is worthwhile to stress that right ventricular dilation were found in all uncorrected patients but in less than half patients in the surgically repaired group. In addition, no incidence of thromboembolism and endocarditis were found in studied subjects, which may explain the overall good clinical outcomes in spite of different degrees of arrhythmias. Women with NYHA class > III have a relatively poor prognosis during pregnancy [ 13 ]. Of note, one uncorrected patient with NYHA class IV was the only patient with limited left ventricular systolic function and pulmonary arterial hypertension. The pregnancy was terminated in that patient at 27 + 6 weeks due to severe ventricular failure. The data obtained from the current study collectively implied that the high degree of right ventricular dilation and high NYHA classification are the most relevant factors for negative outcomes.
It has been demonstrated that women at childbearing age with surgical repair for TOF have lower pregnancy-related risks, and the changes in ventricular dimensions and NYHA class are consistent with normal pregnancy adaptation [ 14 ]. In the literature, it has been demonstrated that pregnant patients even with corrected TOF still have a higher risk and poorer outcome than otherwise healthy women. The increased risk may be attributed to the extra haemodynamic burden and exacerbation of residual cardiovascular lesions, or recurrence of right ventricular outflow obstruction, right ventricular dilatation, pulmonary regurgitation, the right ventricular dilatation and failure, as well as atrial and ventricular arrhythmia [ 15 , 16 , 17 ]. In the current study, the residual shunt at VSD patches were present in two patients following operations and their NYHA class were grade III. In addition, 6 patients (31.58%) had pulmonary regurgitation and about two-thirds of patients had arrhythmia at different degrees. Our data support the notion that pregnant women with the surgically repaired TOF are still in high risk, depending on the degree of the cardiac functional adaption during pregnancy.
Regarding the functional adaption of pregnant women with corrected TOF, Egidy et al monitored the quantitative volumetric changes, and concluded that that those women with successful pregnancy appeared to experience an accelerated rate of right ventricular remodeling (an increase in end-diastolic volume) [ 14 ]. In our study, the moderate or severe right ventricular dilation was found in all of uncorrected patients (100%), but in less than half of the patients in surgically repaired group (47.37%). In addition, the right ventricular hypertrophy and pulmonary valve stenosis were also been found in all of uncorrected patients (100%), but much less in the surgically repaired patients. The comparisons between the corrected and uncorrected patients revealed that the risk of the women with corrected TOF might be divided to two groups, high-risk and low-risk patient groups according to the degree of right ventricular dilation/hypertrophy and the pulmonary valve stenosis. Further study with a large number of cases that are sufficient to stratify data for high-risk and low-risk patients is necessary to define their actual prognostic value.
Maternal condition and mortality has significant effects on fetal outcome in CHD patients [ 18 ]. Recently, Ramage et al. reported 2114 births to women with adult congenital heart disease (ACHD) and suggested an association between several adverse neonatal/maternal outcomes and ACHD [ 19 ]. Their results showed that preterm births (< 37 weeks gestation) were 1.4 times higher in women with ACHD than those without ACHD. Women with ACHD also had a higher odd of having a preterm birth with a gestation less than 32 weeks. In addition, 12.8% women with ACHD and 8.7% of women without ACHD delivered an SGA infant. Consistent with the study conducted by Ramage, the complications were more frequently present in the uncorrected group in our study. Although all of the patients have survived, most all of them suffered cardiac and obstetric complications at varying degrees. The low maternal cardiac output, intrauterine growth restriction and the SGA may occur even after the surgical repair of TOF [ 20 ].
In consideration of high complication risks, woman with cardiac disease may be safer with a C-section delivery to avoid prolonged laboring time [ 21 ]. In this study, one patient with intrauterine fetal death undergone transvaginal complete curettage of uterine cavity, other uncorrected patients delivered by C-section successfully. Women at highest risk may benefit from preconception counseling and close clinical monitoring during pregnancy [ 19 ]. Careful interdisciplinary management among the cardiologist, obstetrician, anesthetist, and neonatologist, and detailed plans for delivery may improve the prognosis [ 22 , 23 ]. Although the differences of outcomes between 19 surgically repaired and 12 uncorrected cases were significant, the impact of other clinical parameters was not achieved in the current study due to the small number of cases in the subgroups. Further research with a large number of cases to determine the relationship between the outcomes and other clinical parameters may be helpful to establish more beneficial management regimen for TOF patients, especially for those without surgical repair. In addition, it will be beneficial to study the each pregnancy outcome of these TOF patients (with or without repair) in instead of per woman. However, it has not been performed in the current study due to the limitation to retrieve complete medical record for previous pregnancies and no record for new pregnancies in these patients.
In summary, TOF confers a high-risk of cardiac and obstetric complications for pregnant women, especially in those who did not received repair surgery. However, due to economic and regional constraints, patients who did not have a chance to receive timely surgical repair and got pregnancy were occasionally seen in our practice. In the past ten years, 12 such cases among 85,184 pregnancies (1.4 out of 10,000) was seen in our medical center. From our experience, these patients may still be able to have a successful pregnancy, but exclusively depending on professional care from multidisciplinary teams. In addition, while the exact implications of clinical parameters remain to be defined with a larger number of cases, the high degree of ventricular dilatation heart, high functional classifications, serious cardiac arrhythmias and pulmonary hypertension appeared to be associated with maternal and neonatal risks in the patients studied in the current investigation. Routine cardiac examination should be performed before pregnancy to exclude possible cardiac diseases and the cardiac surgery should be performed early. For pregnant women with TOF, close monitoring should be strengthened no matter whether they have received surgical repair or not. Decision for the mode of delivery should be individualized by weighing the risks and benefits in a given clinical situation [ 2 , 23 ].

Availability of data and materials
The raw data supporting this study can be requested via the corresponding author.
Abbreviations
Adult congenital heart disease
Atrial premature beat
Atrioventricular block
Blood pressure
- Congenital heart disease
Complete right bundle branch block
Caesarean section
Electrocardiography
Hospital day (total days in hospital)
Incomplete right bundle branch block
Low birth weight infant at term
Cardiac function grading (New York Heart Association)
Pulmonary arterial hypertension
Patent ductus arteriosus
Patent foramen ovale
Premature rupture of fetal membranes
Small for gestational age
Tetralogy of fallot
Uteroplacental doppler flow
Ventricular premature beat
Ventricular septal defect
Naguib MA, Dob DP, Gatzoulis MA. A functional understanding of moderate to complex congenital heart disease and the impact of pregnancy. Part II: tetralogy of Fallot, Eisenmenger's syndrome and the Fontan operation. Int J Obstet Anesth. 2010;19(3):306–12.
Article CAS Google Scholar
Kampman MA, Siegmund AS, Bilardo CM, van Veldhuisen DJ, Balci A, Oudijk MA, Groen H, Mulder BJ, Roos-Hesselink JW, Sieswerda G, de Laat MW, Sollie-Szarynska KM, Pieper PG. Uteroplacental Doppler flow and pregnancy outcome in women with tetralogy of Fallot. Ultrasound Obstet Gynecol. 2017;49(2):231–9.
Babu-Narayan S V, Li W, Uebing A. Pregnancy in Repaired Tetralogy of Fallot. Pregnancy and Congenital Heart Disease. Springer Int Publishing, 2017: 83–99.
Lu CW, Shih JC, Chen SY, Chiu HH, Wang JK, Chen CA, Chiu SN, Lin MT, Lee CN, Wu MH. Comparison of 3 risk estimation methods for predicting cardiac outcomes in pregnant women with congenital heart disease. Circ J. 2015;79(7):1609–17.
Article Google Scholar
Hink E, Bolte AC. Pregnancy outcomes in women with heart disease: experience of a tertiary center in the Netherlands. Pregnancy Hypertens. 2015;5(2):165–70.
Kaur H, Suri V, Aggarwal N, Chopra S, Vijayvergiya R, Talwar KK. Pregnancy in patients with tetralogy of fallot: outcome and management. World J Pediatr Congenit Heart Surg. 2010;1(2):170–4.
Partana P, Tan JK, Tan JL, Tan LK. Multiple pregnancy in a primigravida with uncorrected Pentalogy of Fallot. BMJ Case Rep. 2017.
Parker JA, Grange C. Anaesthetic management of a parturient with uncorrected tetralogy of Fallot undergoing caesarean section. Int J Obstet Anesth. 2015;24(1):88–90.
Sarikouch S, Boethig D, Peters B, Kropf S, Dubowy KO, Lange P, Kuehne T, Haverich A, Beerbaum P. Poorer right ventricular systolic function and exercise capacity in women after repair of tetralogy of fallot: a sex comparison of standard deviation scores based on sex-specific reference values in healthy control subjects. Circ Cardiovasc Imaging. 2013;6(6):924–33.
Sinto R, Nasution SA. Pregnancy in a woman with uncorrected tetralogy of fallot. Acta Med Indones. 2009;41(2):81–6.
PubMed Google Scholar
Meijer JM, Pieper PG, Drenthen W, Voors AA, Roos-Hesselink JW, van Dijk AP, Mulder BJ, Ebels T, van Veldhuisen DJ. Pregnancy, fertility, and recurrence risk in corrected tetralogy of Fallot. Heart. 2005;91(6):801–5.
Veldtman GR, Connolly HM, Grogan M, Ammash NM, Warnes CA. Outcomes of pregnancy in women with tetralogy of Fallot. J Am Coll Cardiol. 2004;44(1):174–80.
Harris IS. Management of pregnancy in patients with congenital heart disease. Prog Cardiovasc Dis. 2011;53(4):305–11.
Cauldwell M, Quail MA, Smith GS, Heng EL, Ghonim S, Uebing A, Swan L, Li W, Patel RR, Pennell DJ, Steer PJ, Johnson MR, Gatzoulis MA, Babu-Narayan SV. Effect of Pregnancy on Ventricular and Aortic Dimensions in Repaired Tetralogy of Fallot. J Am Heart Assoc. 2017;6(7).
Egidy Assenza G, Cassater D, Landzberg M, Geva T, Schreier J, Graham D, Volpe M, Barker N, Economy K, Valente AM. The effects of pregnancy on right ventricular remodeling in women with repaired tetralogy of Fallot. Int J Cardiol. 2013;168(3):1847–52.
Bowater SE, Thorne SA. Management of pregnancy in women with acquired and congenital heart disease. Postgrad Med J. 2010;86(1012):100–5.
Lee C. Surgical management of chronic pulmonary regurgitation after relief of right ventricular outflow tract obstruction. Korean Circ J. 2012;42(1):1–7.
Warnes CA. Pregnancy and delivery in women with congenital heart disease. Circ J. 2015;79(7):1416–21.
Ramage K, Grabowska K, Silversides C. Association of Adult Congenital Heart Disease with Pregnancy, maternal, and neonatal outcomes. JAMA Netw Open. 2019;2(5):e193667.
Sharma D, Shastri S. Pradeep Sharma intrauterine growth restriction: antenatal and postnatal aspects. Clin Med Insights Pediatr. 2016;10:67–83.
PubMed PubMed Central Google Scholar
Wang K, Wang X, Yu H, Liu X, Xing A, You Y. A single-center experience with 12 consecutive cases of pregnancy among patients with membranous ventricular septal aneurysm. BMC Pregnancy Childbirth. 2018;18(1):8.
Niwa K. Adult congenital heart disease with pregnancy. Korean Circ J. 2018;48(4):251–76.
Hrycyk J, Kaemmerer H, Nagdyman N, Hamann M, Schneider K, Kuschel B. Mode of delivery and pregnancy outcome in women with congenital heart disease. PLoS One. 2016;11(12):e0167820.
Download references
Acknowledgements
We thank Drs. Hannah H Chen and John J Xin (Tufts University School of Medicine, Tufts Medical Center) for discussing and editing manuscript. We feel grateful for the doctors and staff who have been involved in this work.
This study was supported by the Academic and Technical Leader’s Foundation of Sichuan Province (No.2017–919-25), the Science Foundation of Sichuan Province (2018FZ0041) and the Health and Family Planning Commission Foundation of Sichuan Province (17PJ236). With the support of the first two funds (No.2017–919-25 and 2018FZ0041), we were able to design the study, complete the data collection and analysis; with the third fund (17PJ236), we were able to interpret the results, prepare the manuscript. The publishing fee will be also covered by the above fund.
Author information
Authors and affiliations.
Department of Obstetrics and Gynecology, West China Second University Hospital, Sichuan University, No. 20, 3rd section, South Renmin Road, Chengdu, 610041, Sichuan, China
Kana Wang, Xiaodong Wang, Haiyan Yu & Xinghui Liu
Key Laboratory of Birth Defects and Related Diseases of Women and Children, Sichuan University, Ministry of Education, No. 20, 3rd section, South Renmin Road, Chengdu, 610041, Sichuan, China
School of Public Heath, Chengdu Medical College, Chengdu, China
You can also search for this author in PubMed Google Scholar
Contributions
WKN carried out the retrospective review of all cases, participated in the writing and organization of the manuscript. XJG participated in the study’s design and the analysis of cases. HYY and XDW conceived of the whole study, and carried out the study design and correction of the manuscript. LXH participated in the study’s design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Haiyan Yu .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Institutional Review Board of West China Second University Hospital. Written informed consent was obtained from patients or their representatives for participation of this study.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Wang, K., Xin, J., Wang, X. et al. Pregnancy outcomes among 31 patients with tetralogy of Fallot, a retrospective study. BMC Pregnancy Childbirth 19 , 486 (2019). https://doi.org/10.1186/s12884-019-2630-y
Download citation
Received : 09 August 2019
Accepted : 25 November 2019
Published : 10 December 2019
DOI : https://doi.org/10.1186/s12884-019-2630-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Tetralogy of Fallot (TOF)
- Surgical repair
- Uncorrected
- Pregnancy outcome
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Repaired Tetralogy of Fallot: Have We Understood the Right Timing of PVR?
Affiliations.
- 1 Bambino Gesù Children's Hospital, IRCCS, 00165 Rome, Italy.
- 2 Clinical Pathways and Epidemiology Unit, Bambino Gesù Children's Hospital, IRCCS, 00165 Rome, Italy.
- 3 Division of Cardiology and CardioLab, Department of Clinical Sciences and Translational Medicine, University of Rome Tor Vergata, 00133 Rome, Italy.
- 4 Department of Cardiology, University of Palermo, 90133 Palermo, Italy.
- 5 Department of Experimental and Clinical Medicine, Magna Graecia University, 88100 Catanzaro, Italy.
- 6 Paediatric Cardiology and Congenital Heart Disease, University of Padua and Pediatric Research Institute (IRP), Città Della Speranza, 35127 Padua, Italy.
- 7 School of Medicine, University College of Dublin, Mater Misericordiae University Hospital, D07 R2WY Dublin, Ireland.
- 8 Dipartimento di Medicina Clinica e Sperimentale, Università di Messina, 98122 Messina, Italy.
- 9 Institute of Cardiovascular Sciences University College London, London WC1E 6BT, UK and Centre for Inherited Cardiovascular Diseases, Great Ormond Street Hospital, London WC1N 3JH, UK.
- 10 Adult Congenital Heart Disease Unit, AO Dei Colli, Monaldi Hospital, 80131 Naples, Italy.
- 11 Cardiovascular Sciences Department, AOU "Ospedali Riuniti", 60126 Ancona, Italy.
- PMID: 38731211
- PMCID: PMC11084704
- DOI: 10.3390/jcm13092682
Despite many advances in surgical repair during the past few decades, the majority of tetralogy of Fallot patients continue to experience residual hemodynamic and electrophysiological abnormalities. The actual issue, which has yet to be solved, is understanding how this disease evolves in each individual patient and, as a result, who is truly at risk of sudden death, as well as the proper timing of pulmonary valve replacement (PVR). Our responsibility should be to select the most appropriate time for each patient, going above and beyond imaging criteria used up to now to make such a clinically crucial decision. Despite several studies on timing, indications, procedures, and outcomes of PVR, there is still much uncertainty about whether PVR reduces arrhythmia burden or improves survival in these patients and how to appropriately manage this population. This review summarizes the most recent research on the evolution of repaired tetralogy of Fallot (from adolescence onwards) and risk factor variables that may favor or delay PVR.
Keywords: PVR; pulmonary insufficiency; tetralogy of Fallot.
Publication types
Grants and funding.
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Living with a CHD
- Data and Statistics
- Tracking and Research
- Congenital Heart Defects Resources
- How the Heart Works
- CHSTRONG KIDS
- Clinical Testing and Screening
- Congenital Heart Defects Toolkit
About Tetralogy of Fallot
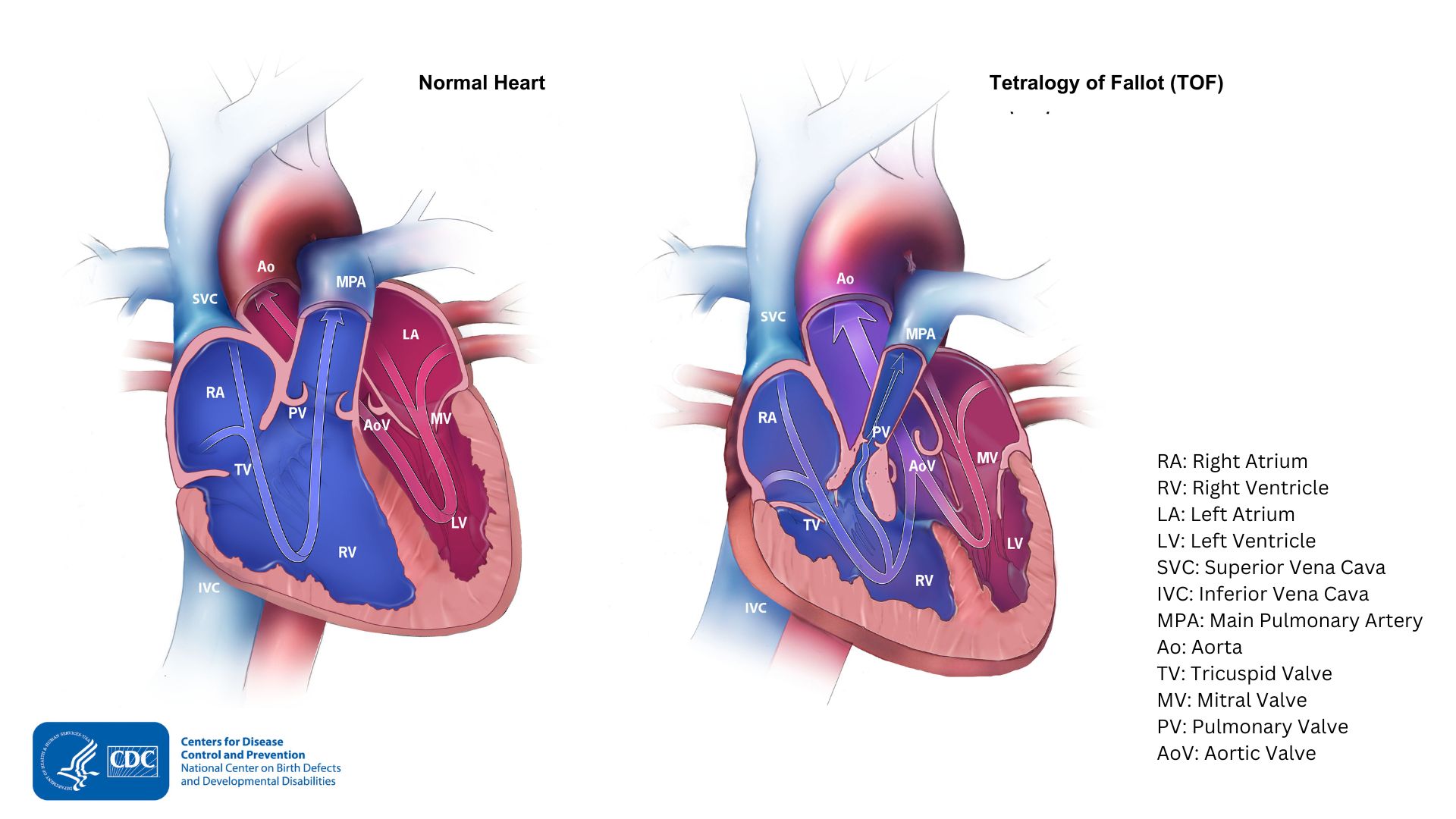
- Tetralogy of Fallot (pronounced te-tral-uh-jee of Fal-oh) is a congenital heart defect. Congenital means present at birth.
- Tetralogy of Fallot occurs when a when a baby’s heart does not form correctly during pregnancy.
- People with this condition should schedule routine checkups with a heart doctor to stay as healthy as possible.

Tetralogy of Fallot is made up of the following four defects of the heart and its blood vessels:
- A hole in the wall between the two lower chambers, or ventricles, of the heart. This condition also is called a Ventricular Septal Defect (VSD).
- A narrowing of the pulmonary valve and main pulmonary artery. This condition also is called pulmonary stenosis.
- The aortic valve, which leads to the aorta, is enlarged and receives blood from both ventricles. In a normal heart, it only receives blood from the left ventricle. In this defect, the aortic valve sits directly on top of the VSD.
- The muscular wall of the lower right chamber of the heart (right ventricle) is thicker than normal. This also is called ventricular hypertrophy .
Because a baby with Tetralogy of Fallot may need surgery or other procedures soon after birth, this condition is considered a critical congenital heart defect (critical CHD).
About 1 in every 2,077 babies in the United States are born with Tetralogy of Fallot 1 . This means that about 1,768 babies are born with Tetralogy of Fallot each year.
Signs and symptoms
Tetralogy of Fallot can cause oxygen in the blood that flows to the rest of the body to be reduced. Babies born with Tetralogy of Fallot may have a bluish looking skin color, called cyanosis, because their blood doesn't carry enough oxygen. At birth, infants might not have blue-looking skin, but may later develop sudden episodes of bluish skin during crying or feeding. These episodes are called tet spells .
Infants with Tetralogy of Fallot or other conditions causing cyanosis can have problems including:
- A higher risk of getting an infection of the layers of the heart, called endocarditis
- A higher risk of having irregular heart rhythms, called arrhythmia
- Dizziness, fainting, or seizures, because of the low oxygen levels in their blood
- Delayed growth and development
Risk factors
The causes of Tetralogy of the Fallot among most babies are unknown. Some babies have heart defects because of changes in their genes or chromosomes. A combination of genes and other risk factors may increase the risk for Tetralogy of the Fallot. These factors can include things in a mother's environment, what she eats or drinks, or the medicines she uses.
Testing and diagnosis
Tetralogy of Fallot may be diagnosed during pregnancy or soon after a baby is born.
During pregnancy
During pregnancy, screening tests (prenatal tests) check for birth defects and other conditions. An ultrasound, a tool that creates pictures of the baby, may detect Tetralogy of the Fallot. If the health care provider suspects Tetralogy of the Fallot from the ultrasound, they can request a fetal echocardiogram to confirm the diagnosis. A fetal echocardiogram is a more detailed ultrasound of the baby's heart. This test can show problems with the structure of the heart and how the heart is working with this defect.
After the baby is born
Tetralogy of Fallot usually is diagnosed after a baby is born, often after the infant has an episode of turning blue during crying or feeding (a tet spell). Findings on a physical exam may make a healthcare provider suspect a baby has Tetralogy of Fallot, including bluish-looking skin or hearing a heart murmur. If these findings are present, the health care provider might request one or more tests to confirm the diagnosis. The most common test is an echocardiogram, which is an ultrasound of the heart.

Tetralogy of Fallot can also be detected with newborn pulse oximetry screening . Newborn screening using pulse oximetry can identify some infants with Tetralogy of Fallot before they show any symptoms.
Tetralogy of Fallot can be treated by surgery soon after the baby is born. During surgery, doctors widen or replace the pulmonary valve and enlarge the passage to the pulmonary artery. They also will place a patch over the VSD to close the hole between the two lower chambers of the heart. These actions will improve blood flow to the lungs and the rest of the body.
What to expect long-term
Most infants will live active, healthy lives after surgery. However, they will need routine checkups with a heart doctor to monitor their progress and check for other health conditions that might develop as they get older. As adults, they may need more surgery or medical care for other possible problems.
- Stallings EB, Isenburg JL, Rutkowski RE et al; for the National Birth Defects Prevention Network. National population-based estimates for major birth defects, 2016–2020. Birth Defects Res. 2024;116(1): https://doi.org/10.1002/bdr2.2301
Congenital Heart Defects (CHDs)
Congenital heart defects (CHDs) are conditions that are present at birth and can affect the structure of a baby’s heart and the way it works. They are the most common type of birth defect.
For Everyone
Health care providers, public health.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Can Med Assoc J
- v.73(1); 1955 Jul 1
Experiences with 180 Cases of Tetralogy of Fallot in Infants and Children *
Full text is available as a scanned copy of the original print version. Get a printable copy (PDF file) of the complete article (2.0M), or click on a page image below to browse page by page. Links to PubMed are also available for Selected References .
Images in this article
Fig. 4 on p.27
Fig. 5 on p.28
Click on the image to see a larger version.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BRINTON WD, CAMPBELL M. Necropsies in some congenital diseases of the heart, mainly Fallot's tetralogy. Br Heart J. 1953 Jul; 15 (3):335–349. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- JOHNS TNP, WILLIAMS GR, BLALOCK A. The anatomy of pulmonary stenosis and atresia with comments on surgical therapy. Surgery. 1953 Feb; 33 (2):161–172. [ PubMed ] [ Google Scholar ]
- DONZELOT E, D'ALLAINES F, DUBOST C, METIANU C, DURAND M. Déductions chirurgicales tirées de l'étude de 54 pièces anatomiques de tétralogie de Fallot. Sem Hop. 1952 Mar 18; 28 (21):877–897. [ PubMed ] [ Google Scholar ]
- BURKE EC, KIRKLIN JW, EDWARDS JE. Sites of obstruction to pulmonary blood flow in the tetralogy of Fallot: and anatomic study. Proc Staff Meet Mayo Clin. 1951 Dec 19; 26 (26):498–504. [ PubMed ] [ Google Scholar ]
- QUER EA, DOCKERTY MB, MAYO CW. Ruptured dermoid cyst of the ovary simulating abdominal carcinomatosis; report of case. Proc Staff Meet Mayo Clin. 1951 Dec 19; 26 (26):489–498. [ PubMed ] [ Google Scholar ]
- BERRI GG, CAPRILE JA, KREUTZER R. Anatomie de la tétrade de Fallot. Arch Mal Coeur Vaiss. 1952 Dec; 45 (12):1082–1091. [ PubMed ] [ Google Scholar ]
- BAFFES TG, JOHNSON FR, POTTS WJ, GIBSON S. Anatomic variations in the tetralogy of Fallot. Am Heart J. 1953 Nov; 46 (5):657–669. [ PubMed ] [ Google Scholar ]
- GARDINER JH, KEITH JD. Prevalence of heart disease in Toronto children; 1948-1949 cardiac registry. Pediatrics. 1951 May; 7 (5):713–721. [ PubMed ] [ Google Scholar ]
- LURIE PR. Postural effects in tetralogy of Fallot. Am J Med. 1953 Sep; 15 (3):297–306. [ PubMed ] [ Google Scholar ]
- LUND GW. Growth study of children with the tetralogy of Fallot. J Pediatr. 1952 Nov; 41 (5):572–577. [ PubMed ] [ Google Scholar ]
- ZIEGLER RF. Some aspects of electrocardiography in infants and children with congenital heart disease. Dis Chest. 1954 May; 25 (5):490–497. [ PubMed ] [ Google Scholar ]
- DONZELOT E, VLAD P, DURAND M, METIANU C. Un nouveau moyen diagnostique dans les cardiopathies congénitales: l'épreuve à l'éther sélective au cours du cathétérisme cardiaque. Arch Mal Coeur Vaiss. 1951 Jul; 44 (7):638–649. [ PubMed ] [ Google Scholar ]
- HILARIO J, LIND J, WEGELIUS C. Rapid biplane angiocardiography in the tetralogy of Fallot. Br Heart J. 1954 Jan; 16 (1):109–119. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- JONSSON G, BRODEN B, KARNELL J. Selective angiocardiography. Acta radiol. 1949 Dec 31; 32 (5-6):486–illust. [ PubMed ] [ Google Scholar ]
- BAIN GO. Tetralogy of fallot: survival to seventieth year; report of a case. AMA Arch Pathol. 1954 Aug; 58 (2):176–179. [ PubMed ] [ Google Scholar ]
- RUDOLPH AM, NADAS AS, BORGES WH. Hematologic adjustments to cyanotic congenital heart disease. Pediatrics. 1953 May; 11 (5):454–465. [ PubMed ] [ Google Scholar ]
- BROCK RC, CAMPBELL M. Infundibular resection or dilatation for infundibular stenosis. Br Heart J. 1950 Oct; 12 (4):403–424. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- BARRETT NR, DALEY R. A method of increasing the lung blood supply in cyanotic congenital heart disease. Br Med J. 1949 Apr 23; 1 (4607):699–702. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- MUSTARD WT, SIREK A. Present status of cardiovascular surgery in infancy and childhood. Surg Clin North Am. 1954 Aug;:903–910. [ PubMed ] [ Google Scholar ]
- CAMPBELL M, DEUCHAR DC, BROCK R. Results of pulmonary valvotomy and infundibular resection in 100 cases of Fallot's tetralogy. Br Med J. 1954 Jul 17; 2 (4880):111–122. [ PMC free article ] [ PubMed ] [ Google Scholar ]

IMAGES
VIDEO
COMMENTS
Tetralogy of Fallot. Tetralogy of Fallot is the most common form of cyanotic congenital heart disease and has 4 main components. The first is a VSD, allowing a right-to-left shunt (Figure 7A and B). The second is RVOT obstruction, constricting blood flow to the pulmonary circuit (Figure 7A). Note that in these patients, the pressure in the RV ...
Tetralogy of Fallot (ToF) is considered the most frequent cyanotic congenital heart abnormality with a low adulthood survival rate if kept untreated. The majority of cases are symptomatic during infancy and mandate early treatment. Few instances of survival to asymptomatic middle-age patients have been reported, and they are decreasing due to ...
Background Tetralogy of Fallot is a congenital heart disease mostly diagnosed and treated in early childhood. However, there are some adult cases receiving treatment. Case presentation We describe a 78-year-old Japanese woman who presented with severely hypertrophic right ventricle, ventricular septum defect, overriding aorta, and severe infundibular stenosis in the right ventricular outflow ...
Tetralogy of Fallot (ToF) is the most common type of cyanotic congenital heart disease. Since the first surgical repair in 1954, treatment has continuously improved. ... A small case-control study found a lower pulmonary valve replacement (PVR) rate following transatrial repair compared with transventricular repair.
cardiac shunt, tetralogy of Fallot Received November 19, 2019. Received revised February 18, 2020. Accepted for publication April 29, 2020. Primary Objective Objective CH3.1: Congenital Heart Disease: Name the most common forms of congenital heart disease and outline their clinical presentation, natural history, and long- and short-term ...
Treatments for Tetralogy of Fallot With Pulmonary Stenosis. Age ... Magnetic resonance imaging is an imaging study done inside a magnet that allows very detailed pictures and measurements of the heart structures. ... Fating T and Dandekar A Rehabilitation in a Pediatric Patient Who Underwent Correction Surgery for Tetralogy of Fallot: A Case ...
Several studies have examined long-term outcomes in TOF3,7,8; however, little is known about early postoperative outcomes of adults undergoing cardiac surgery. In this study, we examined the effect of preop-erative characteristics, type of cardiac sur-gery performed, early postoperative course, and early complications in adults with TOF
Tetralogy of Fallot (ToF) is considered the most frequent cyanotic congenital heart abnormality with a low adulthood survival rate if kept untreated. The majority of cases are symptomatic during infancy and mandate early treatment. Few instances of survival to asymptomatic middle-age patients have been reported, and they are decreasing due to early detection. We reported a case of a middle ...
Tetralogy of Fallot (TOF) is the most common cause of cyanotic heart disease. ... Long-term studies have reported good results with this approach. The case history of a four-year-old male with uncorrected tetralogy of Fallot is presented. The patient required extensive dental treatment prior to scheduled cardiac catheterization. The dental ...
Tetralogy of Fallot Developed by Katie Girgulis, Dr. Andrew Mackie, and Dr. Karen Forbes for PedsCases.com. April 14, 2017 ... Case - Baby Josh Let's start with a clinical case: You are working with Dr. Smith, a family physician, during your family medicine rotation. Josh is a 4-month-old infant who is here for a well-baby check.
Tetralogy of Fallot is a heart condition in which a baby is born with four abnormalities in how their heart developed. These issues make it hard for the baby's heart to send enough oxygen to their entire body. ... In one long-term study, the 36-year survival rate for adults who underwent surgical repair for tetralogy of Fallot was 86%. Living ...
Throughout the study period, a higher percentage of patients with tetralogy of Fallot and pulmonary stenosis (solid line) underwent surgery based on echocardiography alone compared with patients with tetralogy of Fallot and pulmonary atresia (dashed line). PA = pulmonary atresia; PS = pulmonary stenosis; TOF = tetralogy of Fallot.
AbstractIn Brief. The Physician Fee Schedule was updated in 2021 by the Centers for Medicare and Medicaid Services. A case study on Tetralogy of Fallot, the most common cyanotic congenital heart defect, is presented with guidance in billing the office visit to reflect the current guidelines. The Physician Fee Schedule was updated in 2021 by the ...
Tetralogy of Fallot is the most common form of cyanotic congenital heart disease and has 4 main components. The first is a VSD, allowing a right-to-left shunt ( Figure 7A and B ). The second is RVOT obstruction, constricting blood flow to the pulmonary circuit ( Figure 7A ).
Tetralogy of Fallot is the most common cyanotic heart condition in children who have survived untreated beyond neonatal age, with the need for an intervention in the first year of life. It accounts for 7% to 10% of congenital defects, affecting males and females equally and occurring in 3 to 5 of every 10,000 live births.
Summary. This chapter presents an overview of a more common pediatric cardiac lesion; tetralogy of Fallot.The authors provide a description of the anatomic variants that comprise the tetralogy spectrum in addition to a detailed pathophysiology discussion. The surgical/catheter-based interventions are presented in reference to the Tetralogy variant.
Tetralogy of Fallot (TOF) is the most common cyanotic congenital heart disease (CHD) presenting after the neonatal period 1,2. It accounts for between 7% to 10% of all congenital cardiac defects. 3. The word 'tetralogy' refers to something made up of four parts. Therefore, Tetralogy of Fallot is characterised by four defects.
A case study on Tetralogy of Fallot, the most common cyanotic congenital heart defect, is presented with guidance in billing the office visit to reflect the current guidelines. The Physician Fee Schedule was updated in 2021 by the Centers for Medicare and Medicaid Services.
Background Tetralogy of Fallot (TOF) is a severe type of congenital heart disease (CHD) and it confers substantial risk to mother and fetus for pregnant women. However, the outcome of pregnancy in women with TOF has not been well studied. Methods Women with TOF who have been seen and/or delivered at our tertiary-care hospital between April 2008 and January 2018 were retrospective reviewed ...
Abstract. Despite many advances in surgical repair during the past few decades, the majority of tetralogy of Fallot patients continue to experience residual hemodynamic and electrophysiological abnormalities. The actual issue, which has yet to be solved, is understanding how this disease evolves in each individual patient and, as a result, who ...
This decision is made on a case-by-case basis using parameters such as blood pressure, lactate, urine output, and central venous oxygen saturations. The natural longevity of JET ... term outcomes of tetralogy of Fallot: a study from the pediatric cardiac care consortium. J Am Med Assoc Cardiol. (2019) 4(1):34-41. doi: 10.1001/jamacardio.
This is a retrospective study with an approval from the Institutional Review Board of West China Second University Hospital. Between April 2008 and January 2018, a total of 85,184 pregnant women have been seen and gave birth in West China Second University Hospital. A total of 31 pregnant women with TOF were identified, and further reviewed.
Case Studies in Pediatric Critical Care - June 2009. ... Chapter 22 Tetralogy of Fallot; Chapter 23 The child with thermal injury and smoke inhalation; Chapter 24 A child with multiple trauma; Chapter 25 Management of the patient with a failing fontan - morbidities of a palliative procedure;
Key points. Tetralogy of Fallot (pronounced te-tral-uh-jee of Fal-oh) is a congenital heart defect. Congenital means present at birth. Tetralogy of Fallot occurs when a when a baby's heart does not form correctly during pregnancy. People with this condition should schedule routine checkups with a heart doctor to stay as healthy as possible.
Tetralogy of Fallot is characterised by the presence of a ventricular septal defect, overriding aorta, right ventricular outflow tract obstruction and right ventricular hypertrophy. •. Tetralogy of Fallot is one of the commonest cyanotic heart defects. •. The severity of cyanosis is determined by the degree of obstruction to pulmonary blood ...
Tetralogy of Fallot (TOF) is a significant cause of cyanotic congenital heart disease (CHD) encountered in childhood with few cases manifesting in adulthood. It has four classical features (ventricular septal defect, overriding of aorta, hypertrophy of right ventricular hypertrophy, and right ventricular outflow tract obstruction), but the clinical presentation and course can be variable. Due ...
Surgical correction of pulmonary artery stenosis (PAS) is essential to the prognosis of patients with tetralogy of Fallot (TOF). The double-patch method of pulmonary arterioplasty is usually applied in case of multiple stenosis in TOF patients' pulmonary artery (PA) and when PAS cannot be relieved by the single-patch method.
BURKE EC, KIRKLIN JW, EDWARDS JE. Sites of obstruction to pulmonary blood flow in the tetralogy of Fallot: and anatomic study. Proc Staff Meet Mayo Clin. 1951 Dec 19; 26 (26):498-504. [Google Scholar] QUER EA, DOCKERTY MB, MAYO CW. Ruptured dermoid cyst of the ovary simulating abdominal carcinomatosis; report of case. Proc Staff Meet Mayo Clin.