- Ideas for Action
- Join the MAHB
- Why Join the MAHB?
- Current Associates
- Current Nodes
- What is the MAHB?
- Who is the MAHB?
- Acknowledgments

How the world is combating the coronavirus (COVID-19) pandemic
| September 30, 2020 | Leave a Comment
Image by Pete Linforth from Pixabay
Author(s): Gioietta Juo
Since the beginning of 2020 every aspect of our world has changed in an unrecognizable way. Over 200 countries have been affected with the COVID-19 virus. It is in every continent with the exception of the pristine Antarctica. It is now 8 months, what have we achieved? What progress has been made?. It is now time to take stock of the present situation. Are we slowly getting out of the pandemic?? What can we expect the future to look like??
DATA ON CORONAVIRUS WORLDWIDE
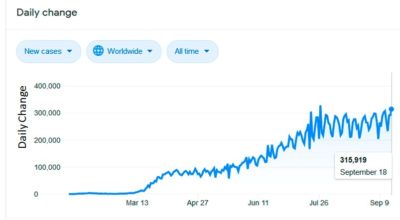
So far, as of September 19, 2020, the. pandemic has caused 30,906,084 cases of coronavirus disease with 959,630 deaths [1].
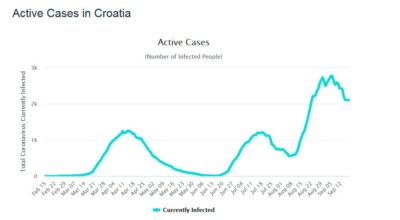
Figure 1 Active Cases in 2020 in millions
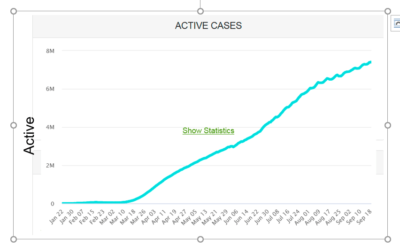
Figure 2 Daily New Cases in 2020 in thousands
It is interesting to note that only 6% of death come from the death of otherwise healthy people. The rest come from those with pre-existing conditions like diabetes, heart and organ weakness and mostly seniors in close contact in places like nursing homes.
Yes, Every aspect of our lives have changed drastically. In order to slow the spread of this highly contagious virus, countries have resorted to a drastic lockdown of ordinary social life as we know it. Schools, shops and many work places have closed. Family is confined to the home. Those who are lucky can work online at home. But others have lost their jobs and depend on government subsistence. But going out means wearing a mask for protection has been mandated.
Even though some countries have slowed down the spread of this virus with social distancing, keeping away from others by more than 6 ft, contact tracing and etc, there are potential down sides. For a start life is lonely not being able to see one’s larger family and friends. Then for those whose marriage is not rock solid, there are emotional risks like child abuse, spouse abuse, drug addictions, alcoholism, and various mental problems even suicides. It has been said that these ills as it happens are worse than the virus itself!! It is imperative that the degree to which these risks have been realized and studied so that health professionals can then develop strategies by which they can be treated. Financial problems can arise, this is where governments have come in to help small businesses and personal problems with stimulus. packages.
There is only a limited time we can lead this dreary life. It is not a permanent solution. Humans are social creatures, we need to go out, meet others, go to schools, have sports, worship in churches and so on……..Most important, schools, the economy cannot be shut down for long.
Now that the season has changed, with the sun beckoning outside, people have the urge to go outside for some fresh air, To the beaches for those living near the coast, to the national parks etc . People cannot be shut indoors forever and it is time to relax the rules.
Most importantly, schools have to open as our children need to go back to their friends and to continue their education. But how?
Social distancing is still necessary. The opening of schools has necessitated a certain closeness in living among the young students, leading to many with low grade fever. In the absence of vaccines what are the solutions? Online teaching is definitely here to stay even though it puts more stress on the families. Then there is nerd immunity [2] where a majority of people who have been exposed and acquired immunity for the virus can impart the immunity to the whole community. That is once a threshold of immune people exist hereby reducing the likelihood of infection for individuals who lack immunity. Immure individuals are unlikely to contribute to disease transmission, They disrupt the chain of infection, which stops or slows the spread of the disease. The greater the proportion of immune individuals in a community, the smaller the probability that that non-immune individuals will come into contact with an immune individual. However, the basic concepts of social distancing, cleanliness of personal hygiene still apply[2].
Definitely, small business – restaurants, hairdressers, stores and workplaces which are the backbone of a country’s economy have to open so long as the basic rules are observed. Innovative ideas such as using the sidewalk for business have sprung up.
PATH TAKEN BY CROATIA TO COMBAT COVID-19
What is happening is Croatia may be an example of what might come [3].
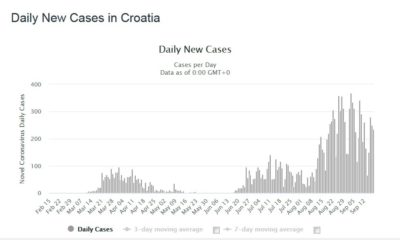
Figure 3 Active Cases in Croatia in 2020
First comes the main peak of active cases. After a mandated social distancing and general lockdown, the number of cases drops drastically. Now is the time to reopen the society and economy? However, after some social mixing, the number of cases rises again. Another lockdown has to happen. Again the number of cases drops. Another attempt of reopening happens followed by an expected rise again of the number of cases. Each time the number of people catching the disease is expected to be lower, Several attempts of reopening will happen until the disease is finally eradicated and society gets back to normal.
Having the confidence that the virus has been licked, the government decided to open up the country completely without restrictions.
This has led to a disastrous sharp rise in new cases in a third wave. See figures 3 and 4. In fact what we are seeing is the second wave followed by the third wave. Not many countries in the world have seen such pronounced multiple waves. Spain is now seeing the second wave. There are signs that the USA is on its second wave.
Figure 4 Daily New Cases in Croatia
TREATMENTS FOR COVID-19 [4]
Although there is no product approved by the US FDA there are many drugs being tested and used. Remdesivir may be prescribed for emergency use. Otherwise the following are actively being tested:
- Antivirial drugs
In addition to Remdesivir, there are favipiravir and merimepodib.
– Dexamethasone
It is a corticosteroid anti – inflammatory drug studied to treat or prevent organ dysfunction and lung injury from inflammation. With people on ventilators or supplemental oxygen. This can reduce death by 30 %.
- Anti- inflammatory therapy
This is in general useful for more severe cases
- I mmune – based therapy[4]
This is a developing therapy which has been found to be highly effective. Recently the US Food and Drug Administration has issued emergency use authorization to treat hospitalized COVID-19 patients with convalescent plasma from people who have recovered from the virus. Convalescent plasma is the liquid portion of the blood that contains the antibodies an individual develops in response to an infection and can be given to patients currently fighting that virus. This treatment has long been a part of the infectious disease arsenal. It has already been in use for COVID-19 for a number of months: The Mayo Clinic has run an “expanded access program for convalescent plasma since March, and more than 70,000 people have received the treatment. It is found that there is a 35% improvement in mortality rate for COVID-19 patients given the plasma.
- Hydroxychloroquine and chloroquine.
This is a long standing anti -malarial drug which has been used for nearly a century. However, there is a fraction of the medical community which maintain this is not an effective solution. In fact there are many people who have used it for long periods just for the prevention of malaria. For them no ill effects have been observed. So this has led to an almost political dialogue. Some say it may cause heart problems but otherwise it has been widely used across all continents with no serious effects.
- Ventilators and oxygen supplements may be used for breathing
VACCINES FOR COVID-19 [5]
It is only natural that we resort to a universal vaccine to solve the pandemic problem. But the scale of the problem given the population size of each country is gigantic. More than 150 companies are desperately competing working drastically to produce a vaccine by the end of 2020. Following are the prominent candidates but which will succeed?
The basic idea of all those vaccines is to instruct one’s immune system to mount a defense, which is sometimes stronger than what would be provided through natural infection and hopefully comes with fewer health consequences.
To do so, some vaccines use the whole coronavirus, but in a killed or weakened state. Others use only part of the virus – whether protein or a fragment. Some transfer the protein into a different virus.
Finally some use pieces of the virus’s genetic material so as to temporarily make the right proteins to stimulate the immune system.
Even when a vaccine has been chemically produced, it faces still a tortuous path to the final usable product. Vaccines have to go through a multi – stage clinical trial process. First phase starts by checking for their safety and whether they trigger an immune response to a small group of healthy individuals. Second phase finds a wider group of those who are likely to catch the virus and to gauge how effective it is. The third phase expands the group to thousands of people to make sure it is safe and effective, given that the immune response varies by age, ethnicity or underlying health conditions.
It then goes to various regulatory agencies for approval. This may take years.
Following are some of the prominent companies. There is much in common between the various companies. Most use the SARS-CoV2 protein to trigger the immune response
== Moderna Therapeutics
Name: mRNA-1273
DNA is the gene and ~RNA gives instructions for certain proteins. A mRNA vaccine is the instruction for the SARS-CoV2 protein. Once inside the cell, the protein is made and that triggers the immune response
Who: A Massachusetts-based biotech company, in collaboration with the US National Institutes of Health.
This vaccine candidate relies on injecting snippets of a virus’s genetic material, in this case mRNA, into human cells. They create viral proteins that mimic the coronavirus, training the immune system to recognize its presence.
STATUS: The third phase has started in a deal with the Swiss company Lonza. It is hoped to manufacture up to one billion doses a year.
Name: BNT162b2
WHO : One of the world’s largest pharmaceutical companies, based in New York in collaboration with German biotech BioNTech.
WHAT: Also an mRNA vaccine based on cancer vaccine.
STATUS : Currently combining phase 2 and 3 on a diverse population in 30,000 people from 39 US states and from Brazil, Argentina, and Germany. Hope to supply 1.3 billion doses by end of 2021.
== University of Oxford
Name: ChAdOx1 nCoV-19
Who: The U.K. university in collaboration with AstraZeneca.
What: Oxford’s candidate is what’s known as a viral vector vaccine, essentially a “Trojan horse ” presented to the immune system. Oxford’s research team has transferred the SARS-CoV-2 spike protein—which helps the coronavirus invade cells—into a weakened version of an adenovirus, which typically causes the common cold. When this adenovirus is injected into humans, the hope is that the spike protein will trigger an immune response. AstraZeneca and Oxford plan to produce a billion doses of vaccine that they’ve agreed to sell at cost.
Status: Preliminary results from this candidate’s first two clinical trial phases revealed that the vaccine had triggered a strong immune response—including increased antibodies and responses from T-cells—with only minor side effects such as fatigue and headache. It has now moved into phase three of clinical trials, aiming to recruit up to 50,000 volunteers in Brazil, the UK, USA and South Africa.
Recently it has been found that one volunteer in the test phase of AstreZeneca has contracted inflammation of the spine. It is not known whether this is related to the vaccine or an independent coincidence. So the whole test phase has been put on hold until further investigation.
==. Sinovac
Name: CoronaVac
Who: A Chinese biopharmaceutical company, in collaboration with Brazilian research center Butantan.
What: CoronaVac is an inactivated vaccine, meaning it uses a non-infectious version of the coronavirus. While inactivated pathogens can no longer produce disease, they can still provoke an immune response, such as with the annual influenza vaccine.
Status: On July 3, Brazil’s regulatory agency granted this vaccine candidate approval to move ahead to phase three, as it continues to monitor the results of the phase two clinical trials. The first phases have so far shown that the vaccine does produce an immune response with no severe adverse effects. Preliminary results of this candidate’s earlier testing in macaque monkeys, published in Science , revealed that the vaccine produced antibodies that neutralized 10 strains of SARS-CoV-2. Phase three will recruit nearly 9,000 healthcare professionals in Brazil.
== Sinopharm
Who: China’s state-run pharmaceutical company, in collaboration with the Wuhan Institute of Biological Products. Wuhan Institute is where the virus initially started. There has been much resentment outside China, especially in the US, that China initially limited the movement of people from Wuhan but failed to let travelers go outside internationally. In this way the virus took hold in Europe and then in USA. The spread of the virus all over the world has led to countless cases and deaths. Not to mention the economic and social disruption it has caused the whole world, China should be made accountable for the gigantic disruption and suffering it has caused to the whole planet!
What: Sinopharm is also using an inactivated SARS-CoV-2 vaccine that it hopes will reach the public by the end of 2020 . Sinopharm has reported that early trials of its vaccine candidate triggered a strong neutralizing antibody response in participants, with no serious adverse effects.
Status: In mid-July, Sinopharm launched its phase three trial among 15,000 volunteers—aged 18 to 60, with no serious underlying conditions—in the United Arab Emirates. The company selected the UAE , as it has a diverse population with approximately 200 different nationalities, making it an ideal testing ground.
==. Murdoch Children’s Research Institute
Name: Bacillus Calmette-Guerin BRACE trial
Who: The largest child health research institute in Australia, in collaboration with the University of Melbourne.
What: For nearly a hundred years, the Bacillus Calmette-Guerin (BCG) vaccine has been used to prevent tuberculosis by exposing patients to a small dose of live bacteria . Evidence has emerged over the years that this vaccine may boost the immune system and help the body fight off other diseases as well. Researchers are investigating whether these benefits may also extend to SARS-CoV-2,
Status: This trial has reached phase three in Australia. It has begun a series of randomized controlled trials that will test whether BCG might work on the coronavirus as well. They aim to recruit 10,000 healthcare workers in the study.
==. CanSino Biologics
Name: Ad5-nCoV
Who: A Chinese biopharmaceutical company.
What: CanSino has also developed a viral vector vaccine, using a weakened version of the adenovirus as a vehicle for introducing the SARS-CoV-2 spike protein to the body. Preliminary results from phase two trials have shown that the vaccine produces “significant immune responses in the majority of recipients after a single immunization.” There were no serious adverse reactions documented.
Status: Though the company is still technically in phase two of its trial, on June 25, CanSino became the first company to receive limited approval to use its vaccine in people. The Chinese government has approved the vaccine for military use only, for a period of one year.
==. The Gamaleya National Center of Epidemiology and Microbiology
Name: Sputnik V
Who: This is the only Russian vaccine research institution which is in collaboration with the state-run Russian Direct Investment Fund.
What: Gamaleya has developed a viral vector vaccine that also uses a weakened version of the common cold-causing adenovirus to introduce the SARS-CoV-2 spike protein to the body. This vaccine uses two strains of adenovirus, and it requires a second injection after 21 days to boost the immune response. Russia has not published any data from its clinical trials, but officials with the institute state that they have completed phases one and two. The researchers also claim the vaccine produced strong antibody and cellular immune responses.
Status: Despite the lack of published evidence, Russia has cleared the Sputnik V vaccine for widespread use and claimed it as the first registered COVID-19 vaccine on the market. Russia reports that it will start phase three clinical trials on August 12 ; the World Health Organization, however, lists the Sputnik V vaccine as being in phase one of clinical trials.
Even when a vaccine is approved, there is the problem of manufacturing, distribution, scaling up of the production and deciding who should get it first. Many vaccines go through the 4th phase of regular study. This can take long time. Then what about the cost? The US government has pledged $10 billion with Pfizer to develop 300 million doses by beginning of 2021, And World Health Organization, WHO, is aiming to deliver 2 billion doses by the end of 2021. It is truly a worldwide effort in the race to produce vaccines to fight and eradicate the pandemic. The companies are located in Australia, Russia, Germany, Brazil, Switzerland, UK, USA and of course China. We hope that the ingenuity of the world’s brilliant scientists and technicians as well as the experience and organized know how of our governments and social systems will lead us through this pandemic by the end of 2020.
Gioietta Kuo, MA at Cambridge, PhD in nuclear physics, Atlas Fellow at St Hilda’s College, Oxford and Princeton University plasma physics lab, is a research physicist. Over 70 professional articles and over 100 articles in environmental problems – in World Future Society-wfs.org, amcips.org, MAHB Stanford and other worldwide think tanks. Also in Chinese in ‘ People’s Daily’ and ‘World Environment’ – Magazine of the Chinese Ministry of Environmental Protection, and others in China. She can be reached at < [email protected] .>
[1] Coronavirus Update (Live): 23,272,847 Cases and 805,907 … https://www.worldometers.info/coronavirus/
[2] Herd immunity and COVID-19 (coronavirus): What you need to … https://www.mayoclinic.org/herd-immunity-and-coronavirus/art-20486808
[3] Croatia Coronavirus: 7,900 Cases and 170 Deaths …
https://www.worldometers.info/coronavirus/country/croatia/
[4] FDA Authorizes Convalescent Plasma As Emergency … https://www.capradio.org/news/npr/story?storyid=905277083 1 day ago … https://www.capradio.org/news/npr/story?storyid=905277083 1 day ago …
[5] https://www.mayoclinic.org/diseases-conditions/coronavirus/expert-answers/coronavirus-drugs
COVID-19 (coronavirus) drugs: Are there any that work …
[6] CORONAVIRUS UPDATE: Here’s what you should know about the vaccines in development
National Geographic 2020
https://www.nationalgeographic.com/science/health-and-human-body/human-diseases/coronavirus-vaccine-tracker-how-they-work-latest-developments-cvd/
How to Write About Coronavirus in a College Essay
Students can share how they navigated life during the coronavirus pandemic in a full-length essay or an optional supplement.
Writing About COVID-19 in College Essays

Getty Images
Experts say students should be honest and not limit themselves to merely their experiences with the pandemic.
The global impact of COVID-19, the disease caused by the novel coronavirus, means colleges and prospective students alike are in for an admissions cycle like no other. Both face unprecedented challenges and questions as they grapple with their respective futures amid the ongoing fallout of the pandemic.
Colleges must examine applicants without the aid of standardized test scores for many – a factor that prompted many schools to go test-optional for now . Even grades, a significant component of a college application, may be hard to interpret with some high schools adopting pass-fail classes last spring due to the pandemic. Major college admissions factors are suddenly skewed.
"I can't help but think other (admissions) factors are going to matter more," says Ethan Sawyer, founder of the College Essay Guy, a website that offers free and paid essay-writing resources.
College essays and letters of recommendation , Sawyer says, are likely to carry more weight than ever in this admissions cycle. And many essays will likely focus on how the pandemic shaped students' lives throughout an often tumultuous 2020.
But before writing a college essay focused on the coronavirus, students should explore whether it's the best topic for them.
Writing About COVID-19 for a College Application
Much of daily life has been colored by the coronavirus. Virtual learning is the norm at many colleges and high schools, many extracurriculars have vanished and social lives have stalled for students complying with measures to stop the spread of COVID-19.
"For some young people, the pandemic took away what they envisioned as their senior year," says Robert Alexander, dean of admissions, financial aid and enrollment management at the University of Rochester in New York. "Maybe that's a spot on a varsity athletic team or the lead role in the fall play. And it's OK for them to mourn what should have been and what they feel like they lost, but more important is how are they making the most of the opportunities they do have?"
That question, Alexander says, is what colleges want answered if students choose to address COVID-19 in their college essay.
But the question of whether a student should write about the coronavirus is tricky. The answer depends largely on the student.
"In general, I don't think students should write about COVID-19 in their main personal statement for their application," Robin Miller, master college admissions counselor at IvyWise, a college counseling company, wrote in an email.
"Certainly, there may be exceptions to this based on a student's individual experience, but since the personal essay is the main place in the application where the student can really allow their voice to be heard and share insight into who they are as an individual, there are likely many other topics they can choose to write about that are more distinctive and unique than COVID-19," Miller says.
Opinions among admissions experts vary on whether to write about the likely popular topic of the pandemic.
"If your essay communicates something positive, unique, and compelling about you in an interesting and eloquent way, go for it," Carolyn Pippen, principal college admissions counselor at IvyWise, wrote in an email. She adds that students shouldn't be dissuaded from writing about a topic merely because it's common, noting that "topics are bound to repeat, no matter how hard we try to avoid it."
Above all, she urges honesty.
"If your experience within the context of the pandemic has been truly unique, then write about that experience, and the standing out will take care of itself," Pippen says. "If your experience has been generally the same as most other students in your context, then trying to find a unique angle can easily cross the line into exploiting a tragedy, or at least appearing as though you have."
But focusing entirely on the pandemic can limit a student to a single story and narrow who they are in an application, Sawyer says. "There are so many wonderful possibilities for what you can say about yourself outside of your experience within the pandemic."
He notes that passions, strengths, career interests and personal identity are among the multitude of essay topic options available to applicants and encourages them to probe their values to help determine the topic that matters most to them – and write about it.
That doesn't mean the pandemic experience has to be ignored if applicants feel the need to write about it.
Writing About Coronavirus in Main and Supplemental Essays
Students can choose to write a full-length college essay on the coronavirus or summarize their experience in a shorter form.
To help students explain how the pandemic affected them, The Common App has added an optional section to address this topic. Applicants have 250 words to describe their pandemic experience and the personal and academic impact of COVID-19.
"That's not a trick question, and there's no right or wrong answer," Alexander says. Colleges want to know, he adds, how students navigated the pandemic, how they prioritized their time, what responsibilities they took on and what they learned along the way.
If students can distill all of the above information into 250 words, there's likely no need to write about it in a full-length college essay, experts say. And applicants whose lives were not heavily altered by the pandemic may even choose to skip the optional COVID-19 question.
"This space is best used to discuss hardship and/or significant challenges that the student and/or the student's family experienced as a result of COVID-19 and how they have responded to those difficulties," Miller notes. Using the section to acknowledge a lack of impact, she adds, "could be perceived as trite and lacking insight, despite the good intentions of the applicant."
To guard against this lack of awareness, Sawyer encourages students to tap someone they trust to review their writing , whether it's the 250-word Common App response or the full-length essay.
Experts tend to agree that the short-form approach to this as an essay topic works better, but there are exceptions. And if a student does have a coronavirus story that he or she feels must be told, Alexander encourages the writer to be authentic in the essay.
"My advice for an essay about COVID-19 is the same as my advice about an essay for any topic – and that is, don't write what you think we want to read or hear," Alexander says. "Write what really changed you and that story that now is yours and yours alone to tell."
Sawyer urges students to ask themselves, "What's the sentence that only I can write?" He also encourages students to remember that the pandemic is only a chapter of their lives and not the whole book.
Miller, who cautions against writing a full-length essay on the coronavirus, says that if students choose to do so they should have a conversation with their high school counselor about whether that's the right move. And if students choose to proceed with COVID-19 as a topic, she says they need to be clear, detailed and insightful about what they learned and how they adapted along the way.
"Approaching the essay in this manner will provide important balance while demonstrating personal growth and vulnerability," Miller says.
Pippen encourages students to remember that they are in an unprecedented time for college admissions.
"It is important to keep in mind with all of these (admission) factors that no colleges have ever had to consider them this way in the selection process, if at all," Pippen says. "They have had very little time to calibrate their evaluations of different application components within their offices, let alone across institutions. This means that colleges will all be handling the admissions process a little bit differently, and their approaches may even evolve over the course of the admissions cycle."
Searching for a college? Get our complete rankings of Best Colleges.
10 Ways to Discover College Essay Ideas

Tags: students , colleges , college admissions , college applications , college search , Coronavirus
2024 Best Colleges

Search for your perfect fit with the U.S. News rankings of colleges and universities.
College Admissions: Get a Step Ahead!
Sign up to receive the latest updates from U.S. News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
Ask an Alum: Making the Most Out of College
You May Also Like
10 destination west coast college towns.
Cole Claybourn May 16, 2024

Scholarships for Lesser-Known Sports
Sarah Wood May 15, 2024

Should Students Submit Test Scores?
Sarah Wood May 13, 2024

Poll: Antisemitism a Problem on Campus
Lauren Camera May 13, 2024

Federal vs. Private Parent Student Loans
Erika Giovanetti May 9, 2024

14 Colleges With Great Food Options
Sarah Wood May 8, 2024

Colleges With Religious Affiliations
Anayat Durrani May 8, 2024

Protests Threaten Campus Graduations
Aneeta Mathur-Ashton May 6, 2024

Protesting on Campus: What to Know
Sarah Wood May 6, 2024

Lawmakers Ramp Up Response to Unrest
Aneeta Mathur-Ashton May 3, 2024

- Open access
- Published: 07 April 2020
Fighting against the common enemy of COVID-19: a practice of building a community with a shared future for mankind
- Xu Qian 1 ,
- Ran Ren 2 ,
- Youfa Wang 3 ,
- Yan Guo 4 ,
- Jing Fang 5 ,
- Zhong-Dao Wu 6 ,
- Pei-Long Liu 4 ,
- Tie-Ru Han 7 &
Members of Steering Committee, Society of Global Health, Chinese Preventive Medicine Association
Infectious Diseases of Poverty volume 9 , Article number: 34 ( 2020 ) Cite this article
196k Accesses
86 Citations
23 Altmetric
Metrics details
The outbreak of coronavirus disease 2019 (COVID-19) has caused more than 80 813 confirmed cases in all provinces of China, and 21 110 cases reported in 93 countries of six continents as of 7 March 2020 since middle December 2019. Due to biological nature of the novel coronavirus, named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) with faster spreading and unknown transmission pattern, it makes us in a difficulty position to contain the disease transmission globally. To date, we have found it is one of the greatest challenges to human beings in fighting against COVID-19 in the history, because SARS-CoV-2 is different from SARS-CoV and MERS-CoV in terms of biological features and transmissibility, and also found the containment strategies including the non-pharmaceutical public health measures implemented in China are effective and successful. In order to prevent a potential pandemic-level outbreak of COVID-19, we, as a community of shared future for mankind, recommend for all international leaders to support preparedness in low and middle income countries especially, take strong global interventions by using old approaches or new tools, mobilize global resources to equip hospital facilities and supplies to protect noisome infections and to provide personal protective tools such as facemask to general population, and quickly initiate research projects on drug and vaccine development. We also recommend for the international community to develop better coordination, cooperation, and strong solidarity in the joint efforts of fighting against COVID-19 spreading recommended by the joint mission report of the WHO-China experts, against violating the International Health Regulation (WHO, 2005), and against stigmatization, in order to eventually win the battle against our common enemy — COVID-19.
A sudden outbreak of coronavirus disease 2019 (COVID-19) caused by infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus has happened since December 2019 in Wuhan City, Hubei Province, a central city in the People’s Republic of China, where transportation is enormously convenient to connecting all other places in China and overseas [ 1 , 2 ]. As of 7 March, 2020, a total of 80 813 confirmed cases reported in all provinces of China, and 21 110 cases reported in 93 countries/territories/areas of six continents [ 3 ]. In particular, some cases have been confirmed in African countries, such as Algeria, Egypt, and Nigeria [ 3 ]. This is the biggest infectious disease outbreak in China ever since 1949, the year of founding the People’s Republic of China. It is the biggest battle since the disease is spreading so fast with high prevalence, and the prevention of the transmission has involved all people in the country [ 4 ]. While at global level, the strategy and coordinating mechanism to control COVID-19 need to be set down as soon as possible [ 5 ], in particular, three questions need to be addressed as (i) how to take the emergency response actions effectively in different countries? (ii) how to mobilize resources quickly with strategic ways? and (iii) how to encourage people proactively and orderly to participate in this battle against COVID-19 from different regions of the world?
Lessons from the battle against COVID-19 in China
In order to address three aforementioned questions, the lessons from China in the battle against COVID-19 need to be understood clearly in the following three aspects:
Traditional epidemiological approaches effectively control the transmission
Professionally speaking, three steps are necessary to taken once an infectious disease outbreaks in certain regions, including controlling infectious sources, blocking the transmission routes, and protecting the susceptive population [ 6 ]. While, as COVID-19 spreading so fast and people’s travelling so frequent during the Chinese New Year (Spring Festival) season, it cannot control effectively if only taking the normal or general countermeasures [ 7 ]. Therefore, the Chinese government has quickly taken actions to contain its transmission inside China, including detecting the disease early, diagnosis and reporting early, isolating and treatment of cases early, tracing all possible contacts, persuading people to stay at home, and promoting social distancing measures commensurate with the risk, etc., based on the current knowledge about epidemiological features and transmission patterns of COVID-19.
Response strategies coping with local conditions
In dealing with the outbreak, China has been adopting the way of tailoring interventions into local settings, from quickly finding each infected person, tracing close contacts and placing them under quarantine, to promoting basic hygiene measures to the public, such as frequent hand washing, cancelling public gathering, closing schools, extending the Spring Festival holiday, delaying return to work, and to the most severe measure of city lockdown of Wuhan [ 8 , 9 ]. By adapting response strategies to the local context, it may avoid blockading the city when it is not needed, and also prevent from a major outbreak without taking any action.
Mobilizing resources quickly to support the emergency responses
Under the strong leadership of the Central Government of China, the mobilization for the emergency responses has been effectively promoted in following ways. Firstly, a Joint Prevention and Control Mechanism of the State Council has established involving 32 Ministries, with subgroups on control of outbreak, medical rescue, scientific research, information and communication, international cooperation, logistics, and frontline coordination [ 10 ]. This multi-sectoral cooperation mechanism at high level is to ensure the facilities and supplies have been well arranged to support the emergency responses in all provinces, with focus on the Hubei Province, for example, more than 10 mobile hospitals and two big hospitals with each one having the capacity of holding more than 1000 beds have been built within 10 days. Secondly, more than 40 000 medical professionals from other provinces or military institutions have been dispatched to Hubei Province to implement emergency responses, including medical care and treatment, epidemiological investigations, environmental sterilization for disinfection, and data and information management to support the policy making.
Encouraging people proactively and orderly participate in this battle against COVID-19
It is important to protect the community from exposure to the infection, all residents in the potential risk areas were encouraged to stay at home, which is an effective way to block the transmission routes. Local community health workers and volunteers, after the specific training, proactively participate in screening the suspicious infections, and help in implementing proper quarantine measures by providing support services, such as driving patients to the mobile hospitals [ 8 ]. All those activities logistically managed at the community level.
At the same time, from medical care side, the medical doctors and nurses worked very hard in the hospitals, to screen the suspected cases, provide medical care for the confirmed cases, and taking emergency response to rescue severe patients to reduce the fatality. While epidemiologists working in centers for disease control and preventions provided the statistical results for the dissemination of epidemiological data correctly, and provide the well-prepared datasets for the decision makers for coordination of necessary resources, and many health workers investigate the suspected contactors for quick medical quarantine of the suspected cases at the community level.
Preventing the pandemic of COVID-19
With the conceptualization on building a community with a shared future for mankind proposed by Chinese President Xi Jinping in 2013 [ 11 ], Chinese people have taken following actions to prevent the pandemic of the diseases: (i) sharing the sequences of SARS-Cov-2 virus with the World Health Organization (WHO) and other countries which are important information for other countries to prepare the tests for screening and diagnosis, (ii) all epidemiological data with clinical treatment in China has been published in the international journals, (iii) prevent spreading of the disease by traveling ban in Wuhan, (iv) medical quarantine has been performed for all suspected contactors, (v) body temperature measuring facilities were equipped in all railway stations and airports, etc. In order to take very strict contain measures for COVID-19 outbreak tailored to local settings, the travelling ban was executed in Wuhan, and encouraging no gathering and less travelling in other cities out of Hubei Province. Those actions were implemented by strong coordinating of the Chinese government in cooperation with local residents. To date, the epidemiological data has showed more than thousands of people have been protected from the infections, and increasing pattern of the transmission has been suppressed significantly in China [ 12 ].
Challenges in fighting against COVID-19
The fighting against COVID-19 has been lasting almost two months, and the time left for people outside of China to prepare the countermeasures has been narrowed quickly. To date, we have found it is one of the greatest challenges to human beings in fighting against COVID-19 in the history, since the pathogen of SARS-CoV-2 is a new coronavirus, differed from either SARS-CoV or MERS-CoV in terms of biological characteristics and transmissibility [ 13 ].
Technically, we have little knowledge on the pathogen and pathogenesis, without specific effectively drugs or vaccine against the virus infection, which cause difficulties in rescuing the severe cases which account for about 20% of the infections. The transmission routes are not clear enough, although we currently understand that the respiratory transmission from human to human is the major transmission route, but other ways for transmission, such as gastrointenstinal transmission or aerosol propagation, is not so clear.
Administratively, implementing the locked down measures in such a big city with over 15 millions of people is not an easy task, with a lot of preparing works from different dimensions of municipal logistic management, to support the emergency response actions. Thus, the multi-administrative systems need to be coordinated collectively, guiding from the central government, with more resources gathering from various places all over the country.
Globally, the information sharing is so important, including patients’ information sharing to trace the suspected cases to protect more people as quickly as possible, genome sequences information sharing to prepare the diagnostics as quickly as possible, and treatment schemes sharing to rescue more severe cases. The WHO declared the Public Health Emergency of International Concern based on the International Health Regulation (2005) in the early time of the outbreak of COVID-19, as it is an extraordinary event to constitute a public health risk to the states through the international spread of disease, and to potentially require a coordinate international response [ 14 ]. All actions to strengthen surveillance and response systems on infectious diseases need to put emphasis on resources limited countries, such as Southeast Asia and African countries [ 15 ].
Recommendations
With understanding more about the nature of COVID-19, it is necessary to understand clearly the current challenges against COVID-19 become increasing, not only to China but also to the world. In order to take quick actions to early prepare the battle against COVID-19 and better allocate enough health resources from the world, the recommendations are as follows:
Coordinating interventions and resources mobilization globally
Preparedness in low and middle income countries.
WHO has identified 13 African countries at the top-risk affected by COVID-19 but with limited resources against COVID-19, including Algeria, Angola, Cote d’Ivoire, the Democratic Republic of the Congo, Ethiopia, Ghana, Kenya, Mauritius, Nigeria, South Africa, Tanzania, Uganda and Zambia. These countries have direct links or greater numbers of people travelling to/from China [ 15 ]. The preparing works on response to the imported cases need initiated as soon as possible with the assistance of WHO as well as developed world. The major preparing works are to prepare enough facilities for use in hospitals, such as test kits, facemasks, and personal protective equipment (PPE), to prepare the quarantine measures in each gate of the traveling venues, and to prepare information communication, etc. The emergency response mechanism on multi-sectoral cooperation needs to be established once the first case has been detected.
Intervention and coordination globally
The fast spreading of COVID-19 to more than 90 countries/territories, with some cluster cases occurred in a few countries, demonstrated that this new disease has higher transmissibility compared with SARS and MERS. The nature of high transmissibility for COVID-19 requires us to (i) prepare the battle globally as soon as possible, by taking the advantage of the time window opened by Chinese battle against COVID-19, (ii) invest more weapons or tools against the diseases by better global coordination, and (iii) take proper quarantine measures globally [ 16 ]. We are able to win the battle only if our actions are coordinated better at a global level.
Resources mobilization globally
One of lessons learnt from the battle in Wuhan is the speed of resources gathering against COVID-19 outbreak could not catch up the speed of the coronavirus spreading in early stage of the outbreak, and it is in need of support or assistances from outside of epicenter, including medical doctors, nurses, and facilities of PPE used in hospitals, and facemasks for residents. The strong support from outside of epicenter quickly to ensure all infectious sources either controlled through quarantine measures or treated in the specialized hospitals. Therefore, for those countries with weak health system, it is so urgent to get help from other parts of the world. WHO needs to mobilize its certified global emergency medical teams to get ready to be dispatched to other countries where health workers are in short supply while an outbreak occurs.
Jointly fighting against common enemy ─ COVID-19
As said by WHO Director-General in the news press on Public Health Emergency of International Concern declaration that “this declaration is not a vote of no confidence in China, our greatest concern is the potential for the virus to spread to countries with weaker health systems.” Therefore, international community needs to work together to prepare for the containment of COVID-19 transmission and spreading in other countries, under the scenario that more countries may be affected by the new coronavirus [ 17 ]. These containment works have to quickly take readiness on active surveillance, early detection, isolation and case management, contact tracing and prevention of onward spread of COVID-19.
Therefore, at this stage, with more countries having confirmed more and more COVID-19 cases, all countries need work together on the following global actions on:
fighting against COVID-19 spreading, including sharing the information of the disease transmission and epidemiological knowledge, sharing the experiences on case management and treatment approaches both for severe cases or light symptoms, and sharing new technologies or strategies to contain the transmission;
fighting against violating International Health Regulation, by following the WHO’s authoritative advices which called on all countries to implement decisions that are evidence-based and convincing. We need to improve our quarantine measures to replace the disconnection of international traveling and trade restrictions, with an assistance of the improved active surveillance systems and AI-based technology to trace the contactors;
fighting against stigmatization, since the stigmatization is always present when the disease outbreak and people facing the sudden attack of this kind of epidemic. These phenomena on stigmatization may be at a scale of epicenter areas, or may be at a country and regional scale, and even at global scale. Thus, we need fight with the real and common enemy which is the new coronavirus, rather than the infected people. The international community needs the solidarity and sympathy to start the battle against the common enemy – the new coronavirus, as well as against stigmatization at the same time.
Global cooperation in priority settings
By considering COVID-19 is spreading so fast which causes difficulties in containing the disease, we, as a community of shared future for mankind, need better coordination in global cooperation and further improvement in the multi-sectoral cooperation in order to quickly take response and prevent from the pandemic [ 18 ]. In addition, we also need better coherence of our resources with more international partners, at least, we can quickly improve our priority settings in sharing information and data, on research priority settings, on surveillance and response to outbreaks at a global level.
Cooperation on sharing information and data
In order to quickly share the information and datasets for countermeasures, the actions on fast and open reporting of outbreak data and sharing of virus samples, genetic information, and research results are encouraged for all international communities, non-governmental organizations (NGOs), as well as governmental institutions around the world. Through regional and country office of WHO, more preventive information against COVID-19 can be disseminated to the public in the vulnerable countries.
Coordination on surveillance and response
With understanding the importance of human health in the planet, multi-sectoral and multi-lateral cooperation against COVID-19 pandemic are recommended at global level. Particularly, the scientific communities, governments and NGOs in different fields, such as public health, agriculture, ecology, epidemiology, governance planning, science, and many others need to collaboratively prevent future outbreaks, with better coordination. The secretary of the United Nations need take the responsibility to coordinate the actions on protecting the planetary health by systematic approaches, such as EcoHealth, One Health, Planetary Health and Urban Health, and making sure public resources are worthwhile investing in strengthening surveillance and response systems for preventing future outbreaks of emerging infectious diseases.
Coherence on research priority settings
We urgently encourage all governments and international foundation to support short-term and emergency response-related research projects to improve our understanding of the causes, risks, infectiousness, and threats of a pandemic [ 19 ]. Health institutions at international level should be encouraged to organize the research priority settings on preventing the pandemic or averting the emergence of the disease. International conservation organizations start to take investigations on types of wildlife-pathogens interactions affecting human health. International environmental agencies can initiate researches on unsustainable transformations of natural environments and ecosystems that provide life-supporting services for our health.
Conclusions
To summarize, COVID-19 is a new disease that has caused great impacts to the people’s daily life extraordinarily. We, as a community of shared future for mankind, need to take collectively and quickly strong emergency responses as a battle against our common enemy, the new coronavirus, not only in China but also in the world. All partners of international community and country leaders are encouraged to proactively take strategic actions as soon as possible to fight the COVID-19 together. Hard times will end finally, and we will meet each other in the blooming spring soon.
Availability of data and materials
All data supporting the findings of this study are included in the article.
Abbreviations
Coronavirus disease 2019
Novel severe acute respiratory syndrome coronavirus
Severe acute respiratory syndrome coronavirus
Middle East respiratory syndrome coronavirus
Non-governmental organizations
World Health Organization
Personal protective equipment
Wu YC, Chen CS, Chan YJ. Overview of the 2019 novel coronavirus (2019-nCoV): the pathogen of severe specific contagious pneumonia (SSCP). J Chin Med Assoc. 2020. https://doi.org/10.1097/JCMA.0000000000000270 .
Wu F, Zhao S, Yu B, Chen YM, Wang W, Song ZG, et al. A new coronavirus associated with human respiratory disease in China. Nature . 2020;579:265–9.
Article CAS Google Scholar
World Health Organization: Coronavirus disease 2019 (COVID-19) situation Report-47. In . Edited by World Health Organization. Geneva. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200307-sitrep-47-covid-19.pdf?sfvrsn=27c364a4_2 . Accessed 8 March 2020.
Zhao S, Lin Q, Ran J, Musa SS, Yang G, Wang W, et al. Preliminary estimation of the basic reproduction number of novel coronavirus (2019-nCoV) in China, from 2019 to 2020: a data-driven analysis in the early phase of the outbreak. Int J Infect Dis. 2020;92:214–7.
Wang FS, Zhang C. What to do next to control the 2019-nCoV epidemic? Lancet . 2020;395(10222):391–3.
Article Google Scholar
TNCPERE. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) — China, 2020. China CDC Weekly. 2020;2(8):113–22.
Google Scholar
Zhao S, Zhuang Z, Ran J, Lin J, Yang G, Yang L, He D. The association between domestic train transportation and novel coronavirus (2019-nCoV) outbreak in China from 2019 to 2020: a data-driven correlational report. Travel Med Infect Dis. 2020;33:101568.
General Administration of Quality Supervision: Inspection and Quarantine of the People’s Republic of China, Standardization Administration of the People’s Republic of China. GB 19193–2015 Beijing: Standards Press of China; 2016.
Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. 2020. https://doi.org/10.1093/jtm/taaa020 .
Joint Prevention and Control Mechanism of the State Council. http://society.people.com.cn/n1/2020/0122/c1008-31559160.html . 2020.
Hu R, Liu R, Hu N. China's belt and road initiative from a global health perspective. Lancet Glob Health. 2017;5(8):e752–3.
China-WHO Expert Team. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). Beijing; 2020.
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–13.
World Health Organization. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). Geneva: World Health Organization. https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) . Accessed 8 March 2020.
Gilbert M, Pullano G, Pinotti F, Valdano E, Poletto C, Boelle PY, et al. Preparedness and vulnerability of African countries against importations of COVID-19: a modelling study. Lancet. 2020;395:871–7.
Chen T, Rui J, Wang Q, Zhao ZY, Cui JA, Yin L. A mathematical model for simulating the phase-based transmissibility of a novel coronavirus. Infect Dis Poverty. 2020;9:24.
Calisher C, Carroll D, Colwell R, Corley RB, Daszak P, Drosten C, et al. Statement in support of the scientists, public health professionals, and medical professionals of China combatting COVID-19. Lancet . 2020;395:E42–3.
Sullivan AD, Strickland CJ, Howard KM. Public health emergency preparedness practices and the management of frontline communicable disease response. J Public Health Manag Pract. 2020;26(2):180–3.
Thompson R. Pandemic potential of 2019-nCoV. Lancet Infect Dis. 2020. https://doi.org/10.1016/S1473-3099(20)30068-2 .
Download references
Acknowledgments
Not applicable.
Author information
Authors and affiliations.
School of Public Health/Global Health Institute, Fudan University, Shanghai, 200032, China
Global Health Center, Dalian Medical University, Dalian, 116021, China
Global Health Institute, School of Public Health, Xi’an Jiaotong University, Xi’an, 710061, China
Global Health Center, School of Public Health, Beijing University, Beijing, 100871, China
Yan Guo & Pei-Long Liu
Kunming Medical University, Yunnan, 650500, China
Zhongshan School of Medicine, Sun Yat-Sen University, Guangzhou, 510080, China
Zhong-Dao Wu
Society of Global Health, Chinese Preventive Medicine Association, Beijing, 100013, China
You can also search for this author in PubMed Google Scholar
- Zong-Fu Mao
- , Tian-Ping Wang
- , Jia-Hui Zhang
- , Qing-Min Zhang
- , Zhao-Yang Zhang
- , Hong-Ning Zhou
- & Feng Chen
Contributions
QX, RR, WYF, GY, FJ, WZD, LPL, and HTR conceived the paper. QX, RR, WYF, and LPL performed the literature search, prepared the figures, and interpreted the data. QX wrote the first version of the manuscript. QX, RR, WYF, GY, and LPL assisted in the restructuring and revision of the manuscript. All authors read, contributed to, and approved the final version.
Corresponding authors
Correspondence to Xu Qian or Tie-Ru Han .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Qian, X., Ren, R., Wang, Y. et al. Fighting against the common enemy of COVID-19: a practice of building a community with a shared future for mankind. Infect Dis Poverty 9 , 34 (2020). https://doi.org/10.1186/s40249-020-00650-1
Download citation
Received : 29 February 2020
Accepted : 20 March 2020
Published : 07 April 2020
DOI : https://doi.org/10.1186/s40249-020-00650-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Preparedness
- International health regulation
Infectious Diseases of Poverty
ISSN: 2049-9957
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
The complexity of managing COVID-19: How important is good governance?
- Download the essay
Subscribe to Global Connection
Alaka m. basu , amb alaka m. basu professor, department of global development - cornell university, senior fellow - united nations foundation kaushik basu , and kaushik basu nonresident senior fellow - global economy and development @kaushikcbasu jose maria u. tapia jmut jose maria u. tapia student - cornell university.
November 17, 2020
- 13 min read
This essay is part of “ Reimagining the global economy: Building back better in a post-COVID-19 world ,” a collection of 12 essays presenting new ideas to guide policies and shape debates in a post-COVID-19 world.
The COVID-19 pandemic has exposed the inadequacy of public health systems worldwide, casting a shadow that we could not have imagined even a year ago. As the fog of confusion lifts and we begin to understand the rudiments of how the virus behaves, the end of the pandemic is nowhere in sight. The number of cases and the deaths continue to rise. The latter breached the 1 million mark a few weeks ago and it looks likely now that, in terms of severity, this pandemic will surpass the Asian Flu of 1957-58 and the Hong Kong Flu of 1968-69.
Moreover, a parallel problem may well exceed the direct death toll from the virus. We are referring to the growing economic crises globally, and the prospect that these may hit emerging economies especially hard.
The economic fall-out is not entirely the direct outcome of the COVID-19 pandemic but a result of how we have responded to it—what measures governments took and how ordinary people, workers, and firms reacted to the crisis. The government activism to contain the virus that we saw this time exceeds that in previous such crises, which may have dampened the spread of the COVID-19 but has extracted a toll from the economy.
This essay takes stock of the policies adopted by governments in emerging economies, and what effect these governance strategies may have had, and then speculates about what the future is likely to look like and what we may do here on.
Nations that build walls to keep out goods, people and talent will get out-competed by other nations in the product market.
It is becoming clear that the scramble among several emerging economies to imitate and outdo European and North American countries was a mistake. We get a glimpse of this by considering two nations continents apart, the economies of which have been among the hardest hit in the world, namely, Peru and India. During the second quarter of 2020, Peru saw an annual growth of -30.2 percent and India -23.9 percent. From the global Q2 data that have emerged thus far, Peru and India are among the four slowest growing economies in the world. Along with U.K and Tunisia these are the only nations that lost more than 20 percent of their GDP. 1
COVID-19-related mortality statistics, and, in particular, the Crude Mortality Rate (CMR), however imperfect, are the most telling indicator of the comparative scale of the pandemic in different countries. At first glance, from the end of October 2020, Peru, with 1039 COVID-19 deaths per million population looks bad by any standard and much worse than India with 88. Peru’s CMR is currently among the highest reported globally.
However, both Peru and India need to be placed in regional perspective. For reasons that are likely to do with the history of past diseases, there are striking regional differences in the lethality of the virus (Figure 11.1). South America is worse hit than any other world region, and Asia and Africa seem to have got it relatively lightly, in contrast to Europe and America. The stark regional difference cries out for more epidemiological analysis. But even as we await that, these are differences that cannot be ignored.
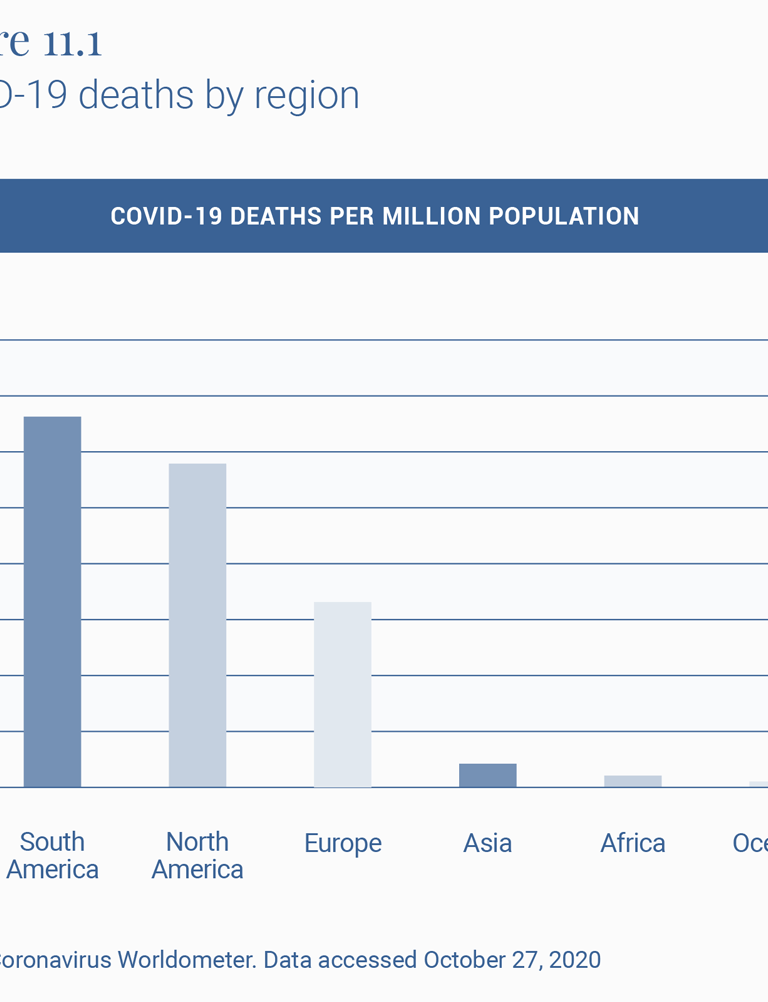
To understand the effect of policy interventions, it is therefore important to look at how these countries fare within their own regions, which have had similar histories of illnesses and viruses (Figure 11.2). Both Peru and India do much worse than the neighbors with whom they largely share their social, economic, ecological and demographic features. Peru’s COVID-19 mortality rate per million population, or CMR, of 1039 is ahead of the second highest, Brazil at 749, and almost twice that of Argentina at 679.
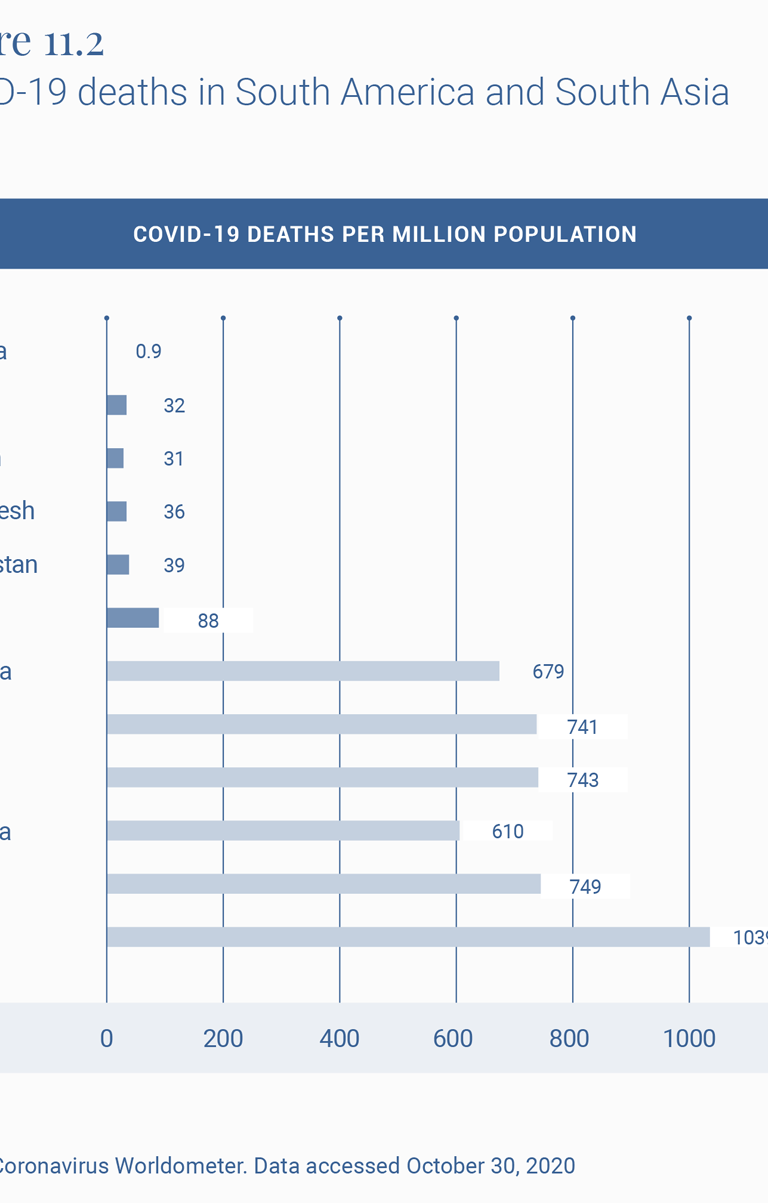
Similarly, India at 88 compares well with Europe and the U.S., as does virtually all of Asia and Africa, but is doing much worse than its neighbors, with the second worst country in the region, Afghanistan, experiencing less than half the death rate of India.
The official Indian statement that up to 78,000 deaths 2 were averted by the lockdown has been criticized 3 for its assumptions. A more reasonable exercise is to estimate the excess deaths experienced by a country that breaks away from the pattern of its regional neighbors. So, for example, if India had experienced Afghanistan’s COVID-19 mortality rate, it would by now have had 54,112 deaths. And if it had the rate reported by Bangladesh, it would have had 49,950 deaths from COVID-19 today. In other words, more than half its current toll of some 122,099 COVID-19 deaths would have been avoided if it had experienced the same virus hit as its neighbors.
What might explain this outlier experience of COVID-19 CMRs and economic downslide in India and Peru? If the regional background conditions are broadly similar, one is left to ask if it is in fact the policy response that differed markedly and might account for these relatively poor outcomes.
Peru and India have performed poorly in terms of GDP growth rate in Q2 2020 among the countries displayed in Table 2, and given that both these countries are often treated as case studies of strong governance, this draws attention to the fact that there may be a dissonance between strong governance and good governance.
The turnaround for India has been especially surprising, given that until a few years ago it was among the three fastest growing economies in the world. The slowdown began in 2016, though the sharp downturn, sharper than virtually all other countries, occurred after the lockdown.
On the COVID-19 policy front, both India and Peru have become known for what the Oxford University’s COVID Policy Tracker 4 calls the “stringency” of the government’s response to the epidemic. At 8 pm on March 24, 2020, the Indian government announced, with four hours’ notice, a complete nationwide shutdown. Virtually all movement outside the perimeter of one’s home was officially sought to be brought to a standstill. Naturally, as described in several papers, such as that of Ray and Subramanian, 5 this meant that most economic life also came to a sudden standstill, which in turn meant that hundreds of millions of workers in the informal, as well as more marginally formal sectors, lost their livelihoods.
In addition, tens of millions of these workers, being migrant workers in places far-flung from their original homes, also lost their temporary homes and their savings with these lost livelihoods, so that the only safe space that beckoned them was their place of origin in small towns and villages often hundreds of miles away from their places of work.
After a few weeks of precarious living in their migrant destinations, they set off, on foot since trains and buses had been stopped, for these towns and villages, creating a “lockdown and scatter” that spread the virus from the city to the town and the town to the village. Indeed, “lockdown” is a bit of a misnomer for what happened in India, since over 20 million people did exactly the opposite of what one does in a lockdown. Thus India had a strange combination of lockdown some and scatter the rest, like in no other country. They spilled out and scattered in ways they would otherwise not do. It is not surprising that the infection, which was marginally present in rural areas (23 percent in April), now makes up some 54 percent of all cases in India. 6
In Peru too, the lockdown was sudden, nationwide, long drawn out and stringent. 7 Jobs were lost, financial aid was difficult to disburse, migrant workers were forced to return home, and the virus has now spread to all parts of the country with death rates from it surpassing almost every other part of the world.
As an aside, to think about ways of implementing lockdowns that are less stringent and geographically as well as functionally less total, an example from yet another continent is instructive. Ethiopia, with a COVID-19 death rate of 13 per million population seems to have bettered the already relatively low African rate of 31 in Table 1. 8
We hope that human beings will emerge from this crisis more aware of the problems of sustainability.
The way forward
We next move from the immediate crisis to the medium term. Where is the world headed and how should we deal with the new world? Arguably, that two sectors that will emerge larger and stronger in the post-pandemic world are: digital technology and outsourcing, and healthcare and pharmaceuticals.
The last 9 months of the pandemic have been a huge training ground for people in the use of digital technology—Zoom, WebEx, digital finance, and many others. This learning-by-doing exercise is likely to give a big boost to outsourcing, which has the potential to help countries like India, the Philippines, and South Africa.
Globalization may see a short-run retreat but, we believe, it will come back with a vengeance. Nations that build walls to keep out goods, people and talent will get out-competed by other nations in the product market. This realization will make most countries reverse their knee-jerk anti-globalization; and the ones that do not will cease to be important global players. Either way, globalization will be back on track and with a much greater amount of outsourcing.
To return, more critically this time, to our earlier aside on Ethiopia, its historical and contemporary record on tampering with internet connectivity 9 in an attempt to muzzle inter-ethnic tensions and political dissent will not serve it well in such a post-pandemic scenario. This is a useful reminder for all emerging market economies.
We hope that human beings will emerge from this crisis more aware of the problems of sustainability. This could divert some demand from luxury goods to better health, and what is best described as “creative consumption”: art, music, and culture. 10 The former will mean much larger healthcare and pharmaceutical sectors.
But to take advantage of these new opportunities, nations will need to navigate the current predicament so that they have a viable economy once the pandemic passes. Thus it is important to be able to control the pandemic while keeping the economy open. There is some emerging literature 11 on this, but much more is needed. This is a governance challenge of a kind rarely faced, because the pandemic has disrupted normal markets and there is need, at least in the short run, for governments to step in to fill the caveat.
Emerging economies will have to devise novel governance strategies for doing this double duty of tamping down on new infections without strident controls on economic behavior and without blindly imitating Europe and America.
Here is an example. One interesting opportunity amidst this chaos is to tap into the “resource” of those who have already had COVID-19 and are immune, even if only in the short-term—we still have no definitive evidence on the length of acquired immunity. These people can be offered a high salary to work in sectors that require physical interaction with others. This will help keep supply chains unbroken. Normally, the market would have on its own caused such a salary increase but in this case, the main benefit of marshaling this labor force is on the aggregate economy and GDP and therefore is a classic case of positive externality, which the free market does not adequately reward. It is more a challenge of governance. As with most economic policy, this will need careful research and design before being implemented. We have to be aware that a policy like this will come with its risk of bribery and corruption. There is also the moral hazard challenge of poor people choosing to get COVID-19 in order to qualify for these special jobs. Safeguards will be needed against these risks. But we believe that any government that succeeds in implementing an intelligently-designed intervention to draw on this huge, under-utilized resource can have a big, positive impact on the economy 12 .
This is just one idea. We must innovate in different ways to survive the crisis and then have the ability to navigate the new world that will emerge, hopefully in the not too distant future.
Related Content
Emiliana Vegas, Rebecca Winthrop
Homi Kharas, John W. McArthur
Anthony F. Pipa, Max Bouchet
Note: We are grateful for financial support from Cornell University’s Hatfield Fund for the research associated with this paper. We also wish to express our gratitude to Homi Kharas for many suggestions and David Batcheck for generous editorial help.
- “GDP Annual Growth Rate – Forecast 2020-2022,” Trading Economics, https://tradingeconomics.com/forecast/gdp-annual-growth-rate.
- “Government Cites Various Statistical Models, Says Averted Between 1.4 Million-2.9 Million Cases Due To Lockdown,” Business World, May 23, 2020, www.businessworld.in/article/Government-Cites-Various-Statistical-Models-Says-Averted-Between-1-4-million-2-9-million-Cases-Due-To-Lockdown/23-05-2020-193002/.
- Suvrat Raju, “Did the Indian lockdown avert deaths?” medRxiv , July 5, 2020, https://europepmc.org/article/ppr/ppr183813#A1.
- “COVID Policy Tracker,” Oxford University, https://github.com/OxCGRT/covid-policy-tracker t.
- Debraj Ray and S. Subramanian, “India’s Lockdown: An Interim Report,” NBER Working Paper, May 2020, https://www.nber.org/papers/w27282.
- Gopika Gopakumar and Shayan Ghosh, “Rural recovery could slow down as cases rise, says Ghosh,” Mint, August 19, 2020, https://www.livemint.com/news/india/rural-recovery-could-slow-down-as-cases-rise-says-ghosh-11597801644015.html.
- Pierina Pighi Bel and Jake Horton, “Coronavirus: What’s happening in Peru?,” BBC, July 9, 2020, https://www.bbc.com/news/world-latin-america-53150808.
- “No lockdown, few ventilators, but Ethiopia is beating Covid-19,” Financial Times, May 27, 2020, https://www.ft.com/content/7c6327ca-a00b-11ea-b65d-489c67b0d85d.
- Cara Anna, “Ethiopia enters 3rd week of internet shutdown after unrest,” Washington Post, July 14, 2020, https://www.washingtonpost.com/world/africa/ethiopia-enters-3rd-week-of-internet-shutdown-after-unrest/2020/07/14/4699c400-c5d6-11ea-a825-8722004e4150_story.html.
- Patrick Kabanda, The Creative Wealth of Nations: Can the Arts Advance Development? (Cambridge: Cambridge University Press, 2018).
- Guanlin Li et al, “Disease-dependent interaction policies to support health and economic outcomes during the COVID-19 epidemic,” medRxiv, August 2020, https://www.medrxiv.org/content/10.1101/2020.08.24.20180752v3.
- For helpful discussion concerning this idea, we are grateful to Turab Hussain, Daksh Walia and Mehr-un-Nisa, during a seminar of South Asian Economics Students’ Meet (SAESM).
Global Economy and Development
Mark Schoeman
May 16, 2024
Ben S. Bernanke, Olivier Blanchard
Joseph Asunka, Landry Signé
May 15, 2024
- Skip to main content
- Keyboard shortcuts for audio player
Goats and Soda
- Infectious Disease
- Development
- Women & Girls
- Coronavirus FAQ
The Coronavirus Crisis
6 solutions to beat covid-19 in countries where the usual advice just won't work.

Malaka Gharib

The fight against coronavirus will not be won until every country in the world can control the disease. But not every country has the same ability to protect people.
For low-income countries that struggle with weak health systems, large populations of impoverished people and crowded megacities, "there needs to be a very major adaptation" to the established measures we've been using to fight COVID-19, says Dr. Wafaa El-Sadr , an epidemiologist and director of ICAP, a global health organization at Columbia University.
The COVID-19 playbook that wealthy nations in Europe, Asia and North America have come to know — stay home as much as possible, keep a six foot distance from others, wash hands often — will be nearly impossible to follow in much of the developing world.
"I think they're trying, but it's not easy," El-Sadr says. "Ministries of health are working, partnering with international organizations to try to innovate — and hopefully, if the innovation works, it can be scaled up."
Here are some of the solutions now being tried.
Fly in tons of medical gear
Problem: Countries in the developing world face massive shortages of medical gear like personal protective equipment, says Avril Benoit, executive director of Doctors Without Borders. And the cutback in commercial flights has made it difficult to bring in equipment.
Solution: The U.N. has launched what it's calling "solidarity flights" – hiring charter planes to airlift millions of face masks, face shields, goggles, gloves, gowns and other supplies. On April 14 , the U.N. dispatched an Ethiopian Airlines charter flight from Addis Ababa full of COVID-19 gear to transport to countries in need.
"This is by far the largest single shipment of supplies since the start of the pandemic, and we will ensure that people living in countries with some of the weakest health systems are able to get tested and treated," said Dr. Ahmed Al-Mandhari, WHO regional director for the Eastern Mediterranean in a statement .
Assessment: "In the short run, a program like this is fine so long as we're dealing with an acute event," says El-Sadr. "Without [supplies like] PPE, you're at risk of losing your scarce and precious health workforce — and you want to protect them at any cost."
But hiring chartered flights to deliver any kind of aid – instead of commercial flights – is expensive, says Manuel Fontaine, director of emergency programs at UNICEF. The U.N. is calling on donors to provide $350 million to continue this program; so far, it has received $84 million.
Create safe havens for the sick and elderly
Problem: How do you protect the most vulnerable individuals in crowded cities and refugee camps? And how do you keep infected individuals from spreading the disease?
Solution: Health authorities are trying out a somewhat controversial strategy: separating the sick and those at high risk, moving them from the homes where they might live alone or with an extended family into vacant homes or taking over facilities previously used for other purposes, such as learning centers. The people being targeted include the elderly and those with preexisting health conditions that make them susceptible to COVID-19 — as well as the homeless.
The strategy has been cited by several health researchers as a practical way to control the spread of disease in densely packed communities. Francesco Checchi of the London School of Tropical Health and Medicine wrote a paper on the subject , and Dr. Paul Spiegel of Johns Hopkins University, in another paper , recommended this as a potential solution in refugee settings.
Assessment: In his paper, Spiegel warns that the strategy of isolating these groups are "novel and untested." And thus far, in parts of the developing world where the strategy has been rolled out, it has had mixed results.
Shah Dedar, an aid worker with the humanitarian group HelpAge, says that religious and community leaders among the Rohingya refugees in Bangladesh don't like the idea of taking the sick or the elderly from the families who might care for them. But "elderly men and women with chronic diseases [who lived alone] were very much keen to the idea and appreciated the initiative," says Dedar.
While HelpAge was able convince local Rohingya leaders to give it a try, Spiegel of Johns Hopkins University says that this may not always be possible. In the case of a severe outbreak, aid workers may have to forcibly separate populations, whether the community approves or not. And he warns that this shielding measure is no guarantee it will keep the virus at bay — it could spread within these facilities, as has happened at some nursing homes in the U.S.
And in Cape Town, South Africa, conditions in a homeless "camp" set up by the government have prompted complaints from the residents about close contact and lack of sanitation — and a call from Doctors Without Borders to shut it down.
Get out of town
Problem: Some citizens are afraid of staying in big cities where social distancing is hard to maintain and outbreaks are more likely to spread.
Solution: Those who have family in ancestral homelands are traveling back to stay in these rural environments – it's happened in countries ranging from Bangladesh to Italy.
Assessment: Both government officials and citizens have criticized this exodus, saying that it puts elderly people in those rural environments at risk if the city dwellers might be contagious yet asymptomatic or presymptomatic.
The other downside of fleeing to these more remote areas, says El-Sadr, is that "health care services are less likely to be available."
That said, El-Sadr notes that this kind of population shift can be a good strategy in an area where transmission within a community has not yet occurred but is deemed likely. This could be a "way that people can have more of an ability to survive, to make a living, get social support [if they are sick], get more access to food, where they can socially distance more readily."
Get the police involved
Problem: Social distancing is hard to enforce in densely populated low-income countries.
Solution: Many governments around the world have turned to the police to ensure that people stay home — and hand out punishments to those who aren't following the lockdown rules. In India, for example, people who violate the lockdown could face up to a year in prison. Others in the country have faced unusual punishments, such as writing "I am very sorry" 500 times, according to an NPR report .
Assessment: Unfortunately, there have been reports of officers using physical violence to keep people in their homes in several countries, including India, Bangladesh and the Philippines. In Kenya, the violence has resulted in public outcry , with citizens calling for more civility from its police force. "This is no way to fight a coronavirus epidemic," tweeted a Kenya-based journalist.
Reinvent factories so they can make medical equipment
Problem: More supplies to fight COVID-19 are needed.
Solution: Get factories to switch gears and respond to the coronavirus.Kenya's textile industry has pivoted to making masks and protective equipment. The Kitui County Textile Center (KICOTEC) has shifted from sewing chef's whites and school uniforms to turning out face masks and scrubs for healthcare workers. Kenya's state-owned oil company is now making hand sanitizer, which it says it is distributing for free.
In South Africa, the state-owned missile manufacturer Denel , has been working to design and build ventilators, and to convert armored trucks into ambulances. The government has launched an initiative called the National Ventilator Project , which calls for companies to build 10,000 ventilators by the end of June, using locally available parts and materials.
Similar efforts are underway in Nigeria, where the government announced that they're working with car companies to manufacture locally-made ventilators.
Assessment:
In Kenya, KICOTEC turning out 30,000 surgical masks a day, according to Kenya's Ministry of Health . Kenya's petroleum company has produced more than 80,000 gallons so far, and plans to make at least 600,000 gallons more.
But WHO projects that countries will need millions of masks, goggles and other supplies to protect healthcare workers and citizens while mounting a response to COVID-19.
So local manufacturing can only partly fill the gap. But local authorities believe it is critical: "We're trying to build up local capacity to ensure that the critical facilities, the beds and ventilators, respirators could be made available within the country," says Adaeze Oreh, a senior official in Nigeria's Ministry of Health, "So we're not constrained by international travel restrictions, border closures and relying on imports."
Set up handwashing stations
Problem: Public health officials globally stress the importance of frequent hand-washing in the fight against COVID-19. In low- and middle-income countries, however, 35% of people lack regular access to soap and water, according to WHO .
"The health workers say we must wash our hands," said Zukwisa Qezo, a 47-year-old mother of two who lives in the Cape Town township to NPR . "But with what?! The city must bring us soap."
Solution: To improve the ability for people to clean their hands, WHO advises that hand hygiene stations — either with soap and water or with alcohol-based hand sanitizer — to be placed at the entrances of buildings, and in transport hubs such as bus and train stations. The system can be as simple as two buckets — one filled with chlorinated water, and one to catch the wastewater.
Assessment: Public hand-washing stations, which were effective in the fight against Ebola, are being resurrected in countries such as Liberia and Sierra Leone, NPR reports . Doctors Without Borders reports that their volunteers are setting up hand washing points in many of the settings they operate in, including migrant camps in Nigeria and health facilities in Mozambique.
- Get involved
How we can overcome the COVID-19 pandemic together
January 4, 2021, lucy ndungu.
Regional Manager, UNV East and Southern Africa Regional Office
For most of the past year, our lives have been disrupted by the COVID-19 pandemic. Lives have been lost, livelihoods disrupted, and education adversely impacted. Poverty levels have increased in some countries, societal bonds have been strained, and the overall trend of development has been reversed. Yet, despite the bleak outlook, we have witnessed stories of hope, courage, triumph and kindness towards one another: the spirit of oneness— Ubuntu, Obuntubulamu, Utu— as is commonly known in East and Southern Africa.
The spirit of volunteerism, innate in all of us, is what drives the selfless people who have during the COVID-19 pandemic, extended kindness to their neighbours, supported access to medical care for those in need, shopped for the elderly and other vulnerable people, among other acts of generosity. This resonates with a quote from former UN Secretary General, the late Kofi Annan: “Behind the progress lie many factors. One is the willingness of many individuals to donate their time, effort, resources and ideas to the well-beings and advancement of all. We call them volunteers.” Volunteers have been at the forefront of medical, community and societal responses across East and Southern Africa. The COVID-19 Strategic Preparedness and Response Plan developed by the WHO identifies community volunteers as key stakeholders for risk communication, community engagement and in provision of health services.
Since joining the UN Volunteers programme for East and Southern Africa in November, I have been humbled by the selflessness shown by volunteers of all ages, races, and genders across the region. In Zambia, more than 800 community youth volunteers have reached about 700,000 households through a door-to-door COVID-19 outreach initiative , debunking myths and spreading life-saving messages. In Kenya, Nicodemus Otieno and Cynthia Wandabwa are two among 50 UN Volunteer health professionals deployed by UNDP Kenya across the country to support the national COVID-19 response. In Mozambique, Ângela Macie, a UN Volunteer serving with the World Food Programme (WFP) , is on the frontlines supporting logistics for food distribution in vulnerable communities. In Somalia , there are many UN Volunteer medical doctors supporting UN clinics in remote regions. In moments like this, these and many other volunteers globally are supporting countries across the region and the world in combating COVID-19.
As countries move to build back better their socio-economic foundations that have been greatly fissured by the pandemic, volunteers will play a vital role. According to the UNV 2018 State of the World’s Volunteerism Report , over a billion people volunteer every year globally , with many more willing to do so if given the opportunity. This translates to one in every seven people, an equivalent of 109 million full-time workers globally. If they constituted a country, the global volunteer workforce would be the fifth largest in the world, roughly equivalent to the number of employed people in Indonesia. The contribution of volunteerism to GDP cannot be underestimated. In Kenya volunteerism contributes to about 3.6 percent of the GDP according to research commissioned by Kenya’s State Department for Social Protection in 2017.
The most recent commemoration of the International Volunteer Day (IVD) recognized the contributions of such volunteers. Across this region, governments, UN partners, academia, civil society and volunteer involving organizations enumerated several benefits of volunteerism including; support building skills and services particularly in far-flung areas and ensuring building community resilience. Noting that volunteers at times work in challenging environments, they also advocated for support and care for volunteers. From lessons of 2020, anecdotes from partners showed that online volunteering works just as well as onsite volunteering where extenuating circumstances limit the latter. Further evidence showed that the nimbleness of local volunteerism in particular flexibility, swiftness to act, the ability to self-organize were attributes that came in handy in response to COVID-19.
UNV ESARO will continue partnering with the UN and member states in the region to promote volunteerism as a “powerful and crosscutting means of implementation of the 2030 Agenda for Sustainable Development” as recognized, for the first time, in the Quadrennial Comprehensive Policy Review of operational activities of the United Nations system, adopted in December 2020.
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
How to Protect Yourself and Others
CDC’s Respiratory Virus Guidance provides strategies you can use to help protect yourself and others from health risks caused by COVID-19 and other respiratory viruses. These actions can help you lower the risk of COVID-19 transmission (spreading or catching COVID-19) and lower the risk of severe illness if you get sick.
Core Prevention Strategies

CDC recommends that all people use core prevention strategies to protect themselves and others from COVID-19:
- Although vaccinated people sometimes get infected with the virus that causes COVID-19, staying up to date on COVID-19 vaccines significantly lowers the risk of getting very sick, being hospitalized, or dying from COVID-19.
- Practice good hygiene (practices that improve cleanliness)
- Take steps for cleaner air
When you are sick:
- Learn when you can go back to your normal activities .
- Seek health care promptly for testing and/or treatment if you have risk factors for severe illness . Treatment may help lower your risk of severe illness, but it needs to be started within a few days of when your symptoms begin.
Additional Prevention Strategies
In addition, there are other prevention strategies that you can choose to further protect yourself and others.
- Wearing a mask and putting distance between yourself and others can help lower the risk of COVID-19 transmission.
- Testing for COVID-19 can help you decide what to do next, like getting treatment to reduce your risk of severe illness and taking steps to lower your chances of spreading COVID-19 to others.
Key Times for Prevention
Using these prevention strategies can be especially helpful when:
- Respiratory viruses, such as COVID-19, flu, and RSV, are causing a lot of illness in your community
- You or those around you have risk factors for severe illness
- You or those around you were recently exposed to a respiratory virus, are sick, or are recovering
Check Your Community
Find out if respiratory viruses are causing a lot of illness in your community. Data updated weekly.
Learn more about all three of these respiratory viruses, who is most at risk, and how they are affecting your state right now. You can use some of the same strategies to protect yourself from all three viruses.
Get the Latest on COVID-19, Flu, and RSV
- COVID-19 Testing
- COVID-19 Vaccines
- COVID-19 Treatments and Medications
- Preventing Respiratory Viruses
- Protect Yourself from COVID-19, Flu, and RSV
Additional Resources
- Respirators and Masks
- Improving Ventilation in Your Home
- Improving Ventilation In Buildings
Search for and find historical COVID-19 pages and files. Please note the content on these pages and files is no longer being updated and may be out of date.
- Visit archive.cdc.gov for a historical snapshot of the COVID-19 website, capturing the end of the Federal Public Health Emergency on June 28, 2023.
- Visit the dynamic COVID-19 collection to search the COVID-19 website as far back as July 30, 2021.
To receive email updates about COVID-19, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
To revisit this article, visit My Profile, then View saved stories .
- Backchannel
- Newsletters
- WIRED Insider
- WIRED Consulting
Adam Rogers
The Perfect Strategy to Fight Covid-19 Is … Everything?

The pandemic has changed—and it’s worse than ever.
Cases of Covid-19 are spiking in nearly every state. The statistics are grim. With more than 100,000 new cases and 2,000 deaths every day, hospital intensive care units are filling up everywhere. It’s an entire country of New-Yorks-in-April. And yet Covid skepticism—over how to fight the disease, and sometimes even the reality of the disease itself—remains a hallmark of right-wing politics.
Read all of our coronavirus coverage here .
There’s a light at the end of the tunnel—vaccines may well be available to millions of people before the end of the year. That’s a scientific triumph, to be sure, but meanwhile, we’re still in the tunnel. Manufacturing and distribution challenges mean that it’ll take until at least June 2021 to vaccinate everyone, according to the head of logistics for the government’s vaccine-goosing Operation Warp Speed program. Until then, the same public health measures that slow the spread of the virus—curve-flattening “non-pharmaceutical interventions” like mask-wearing and canceling gatherings—remain the only tools in the toolbox.
So policymakers and leaders have a stark choice: Force everyone, again, to abide by effective but potentially onerous public health measures, or let hundreds of thousands of people die. It’s a tougher choice than it sounds. Anti-“lockdown” rhetoric and a year of stress has ground people down emotionally and nuked the economy. Plus, it’s a basic tenet of public health that abstinence enjoinders and shame don’t work . If curve-bending efforts aren’t politically and socially viable, they’ll fail—and hundreds of thousands of people will die. As Mike Ryan, executive director of the World Health Organization Health Emergencies Programme, said at a press conference last Friday: “Those countries currently in the fight of their lives, you have got to stick with this. You’ve got to try and control this transmission, or your health systems will not be able to cope.”
What you’d really like to know here is which specific interventions give the most bang for the buck, the greatest reduction in disease transmission with the lightest possible touch on the social fabric and the economy. Is it … a mask mandate? Closing bars and restaurants? Closing schools? Temperature checks at building entrances? It would be very, very good to know this, because all of those things have benefits, but also costs. But scientists and public health experts don’t have answers. They know these things work in the aggregate, but not how they overlap and synergize, how behaviors change in response to new rules, and how politics and sociology affect adherence.
That’s why nothing seems to make sense today—indoor dining open, places of worship closed; outdoor playgrounds closed, gyms open; outdoor dining areas open then closed; curfews implemented on bars. In many countries, early measures combined with financial support and rigorous testing, tracing, and isolation programs squashed the disease. The US and Europe did some of the first thing and almost none of the others, dooming those places to a bloody oscillation: Cases spike, lockdowns come, economies and mental health crash, places reopen, cases spike, repeat. And now, well, we are where we are.
In the initial months of the pandemic, everybody blew it. “Ideally, you want interventions that have maximal effectiveness with the least social and economic downside,” says Lawrence Gostin, director of the O'Neill Institute for National and Global Health Law at Georgetown University. “That’s the rational way of doing it. But there’s been no rationality around fighting this pandemic, particularly in the United States and Europe.”
Public health experts know, in the broadest terms, what measures will bend the curve, but the science of it is really more of an art. Every country around the world rolled out roughly similar sets of public health interventions to fight Covid-19 in roughly the same order, at roughly the same moments in their encounters with the disease. According to research led by Thomas Hale at the Blavatnik School of Government at Oxford, most countries started communicating to their citizens in February about the potential problems to come, and instituted border controls even before they had confirmed cases. About 25 days later, in mid-March, countries started canceling public events and closing schools, and then closing workplaces five days after that. Four days after that, on average, came stay-at-home orders and public transportation closures—lockdowns.
The total portfolio of interventions is familiar, and taken in total they’re still the best and only way to reduce Covid-19’s spread—that portfolio is the basis for new, sweeping recommendations from the Centers for Disease Control and Prevention, for example. But nobody studied those measures closely to see what was working. “I think there has been a missed opportunity to learn from the first-wave experiences,” says Ben Cowling, an epidemiologist at the University of Hong Kong who has tried to assess interventions for Covid-19 and other outbreaks. “A lot of interventions were applied, natural experiments in different places, and it’s been a missed opportunity not to study those more carefully to see what happened, what worked, and what didn’t.”
Take mask-wearing. I’m not going to focus too much on that here, because so many smart reporters already have, and because widespread mask-wearing clearly cuts transmission of Covid-19. But just consider how hard it is to really-and-for-truly test that proposition. It’s possible to, for example, test how well masks reduce the emission of the aerosolized particles that seem to be a major contributor to the spread of the virus. You can also compare places with mask mandates to places without and see what the virus does. In Kansas , for example, counties that put a mask mandate in place last summer saw Covid-19 incidence decline; counties that didn’t mandate masks saw incidence increase. The same correlation held in Germany; regions with mask mandates for transit and shops saw reductions in cases while non-mandate regions did not, leading researchers there to conclude that 20 days after mask mandates go into force, infections go down by about 45 percent.
That’s great, and those new CDC guidelines are all-in on masking, recommending people wear them everywhere other than their household, including indoors. President-elect Joe Biden told CNN that he’ll ask all citizens to wear masks for the first 100 days of his term—quite the turn from Donald Trump’s derisive attitude . Mask not what your country can do for you, I guess.
But mask studies still have some gaps. Was it really the masks themselves blocking enough virus emitted from the mouth and nose? That’s almost certainly true, but what if the population-scale effect of masking also includes more subtle effects? “Mask mandates usually arise when cases are rising. Does a mask mandate reduce transmission because masks actually stop transmission by blocking virus when we breathe out, or because wearing masks reminds us that there is a pandemic going on, and we don't socialize?” says A. Marm Kilpatrick, an infectious disease researcher at the University of California, Santa Cruz. “Or, are masks completely irrelevant and the decrease in transmission that sometimes follows mask wearing is just because people were freaked out by news reports of cases rising? Disentangling these effects is extremely difficult.” It’d be good to know those things, if for no other reason than to be able to convince people to wear their damn masks.
A gold-standard, randomized controlled trial of mask use would answer these questions—you’d think. A recent Danish study attempted that. One group of people got told to wear masks outside their homes, and another group didn’t. According to the study, masks didn’t really help; the reduction in Covid-19 infections wasn’t significant. But as other analysts have written, the study wasn’t enforcing actual mask wearing. So it wasn’t actually a study of masks versus no masks; it was a study of the effect of telling people to wear masks. If anything, it was a study of mask mandates, not mask effectiveness. Even the lead author acknowledged that it didn’t really say anything about whether masks worked. And it wasn’t really a gold-standard trial. For one thing, it’s impossible to blind which people were doing masks or no-masks. For another, the study didn’t actually isolate the thing it set out to test.
Actually isolating the right variable and getting statistical power out of a double-blinded RCT on masks would be nearly impossible. “Doing a mask RCT with 30,000 people would be very, very challenging, and one would need to somehow measure mask usage, since a substantial fraction of people wouldn't wear their mask all the time,” Kilpatrick says.
Masks are relatively cheap, and mask mandates are relatively easy to implement—especially if you’re not trying to put any power of enforcement behind them, like fines. Harder, society-level interventions with bigger economic and social implications are even tougher to study.
People have tried. When you can’t run an RCT, you have to be satisfied with natural experiments, observational and retrospective analyses, and computer models. In mid-November, The New York Times correlated Hale’s Oxford countermeasure data for US states with the extents of their outbreaks—new cases per 100,000 people and hospitalizations per 100,000 people. Sure enough, the states with the fewest and least potent restrictions—North Dakota and South Dakota, it turned out—had the worst outbreaks. Hawaii’s rules were the most stringent, and the state had the fewest cases.
That analysis makes intuitive sense, and it supports the everything-all-at-once strategy. But it isn’t perfect. Time plays a role here—tests were hard to come by early in the pandemic, which means states could have had thousands of cases that went undetected. Hawaii is a lot easier to keep potentially infected travelers away from than, say, Iowa or Kansas, so maybe the Aloha state had fewer patient zeroes to begin with.
Just a couple of days before the Times analysis, the journal Nature Human Behaviour published another attempt at developing a heuristic for non-pharmaceutical interventions. An international team led by Austrian network scientists looked at the rise of nearly 7,000 different countermeasures in March and April in 79 different countries. They found a pattern similar to the one that Hale’s team discovered. But then things got tricky. “Many countries implemented bunches of measures simultaneously, and this is statistically challenging, because if you have 10 interventions implanted the same day, it’s hard to disentangle the effects,” says Peter Klimek, a data scientist at the Medical University of Vienna who led the research. “And these individual interventions are closely related to each other. You can’t shut down schools without shutting down other areas of life in parallel. There is no such thing as the effectiveness of a single intervention.”
Klimek’s team tried anyway. They looked at the kinds of interventions that the countries ran and their concurrent reductions, if any, in the effective reproduction number, R t —how fast the disease moves from person to person. Then the team ran four different kinds of analyses: They ran a complex regression model, basically comparing countries with specific interventions to countries that didn’t do the same thing; a time-series regression that assumed the interventions had specific effects they could find in the numbers; and a couple of machine-learning algorithms to look for patterns, too. (They also tried to build in ways to account for socioeconomic and political differences in the countries themselves.) “For some measures, these four different methods gave us completely different results. But there was a core of interventions on which they could agree,” Klimek says, “where they were implementing a measure and observing a reduction of the effective reproduction number.”
The winners? The most effective move was canceling small gatherings like weddings and parties, and closing shops, bars, and restaurants. Number two: school closures, which is controversial because Covid-19 seems to spread differently among younger kids, and because closing schools has all kinds of knock-on effects—developmental impact on kids, forcing caregivers to stay home as well. Klimek says his team saw hints in their data that closing high schools was more effective than closing elementary schools in terms of reducing disease transmission.
Making sure that health care facilities had enough personal protective equipment was number three, and good communication strategies were number four. Airport restrictions also helped, but only if countries put them in place in the very early days of the pandemic (so no help there, really). Mask-wearing showed up in some of the statistical approaches but not all, and might be subsumed in some of the other broad descriptors, like social distancing.
The losers? Improvements in testing and tracing didn’t seem to help—maybe because they weren’t implemented soon enough or at grand enough scale. Closing intracity public transit didn’t move the needle, either. “These are just not places where a lot of transmission happened,” Klimek says.
But as appealing as this assessment might seem, it’s not straightforward. All of those “winners” that Klimek laid out might (or might not) be part of a “lockdown” or stay-at-home order like the ones coming into force in California. Instituting one or several might enhance or limit the effects of others. “The measures do not associate in a linear way. They overlap partly,” Klimek says. On the plus side, that means removing a single intervention from the set doesn’t necessarily knock over the whole Jenga tower. Places could open schools, for example, but keep bars and restaurants closed and prohibit small gatherings, and still get a good effect. Maybe. “We’re starting to see this in many European countries,” Klimek says. “It’s not only black and white. We can do this now in a more differentiated way.”
It’s a good thought, and Klimek is working with the Austrian government to put it into effect. It’s also not clear-cut. “I’d caution you that regression analysis and modeling are very unreliable,” Gostin says. “You really need to do rigorous retrospective analyses to try to figure out what works and what doesn’t, which we’ve never really done.”
Worse, though, as the paper itself acknowledges, when it comes to population-level public health interventions during a crisis, subtext is everything. It’s the unmeasured changes in people’s behavior that confound work like Klimek’s, the second-order consequences of the rules—like caregivers staying home because their kids don’t have school to go to. If the government doesn’t subsidize staying home, let’s say, those people could lose their jobs, which crushes their finances and harms the overall economy. So school closures don’t “work,” as such, without all kinds of other supporting efforts. “When we think about other NPIs, like school closures, the effect of that kind of intervention could vary from one place to another,” Cowling says. “So I don’t think it’s possible to have an estimate of the effect of school closures on Covid. You could have the effect of school closures on Covid in April 2020 in the UK—in a particular place, at a particular time, with an intervention described in a certain way.”
That means research like Klimek’s faces a huge task in trying to disentangle what public health rules say from what they actually do. “What they are actually measuring is the direct effect of these interventions, plus the indirect effect of these interventions, plus the direct and indirect effects of other things happening at the same time,” Kilpatrick says. “None of the papers I’ve seen tries to quantify media coverage of local epidemics, even though I'd bet that's one of the largest effects on peoples’ behavior.”
(It does seem to be true that perception of the seriousness of the pandemic changes how people respond to it. Simple perception of the threat—understanding that Covid-19 is dangerous—makes people more willing to comply with interventions, or more cautious overall, and so indirectly reduces R t , or infections or death rates. This, too, makes intuitive sense. People who hear that their local hospitals are full or have Facebook feeds full of posts from sick friends and relatives might be more likely to simply stay home. In one model —so, caveats apply—a greater awareness of Covid-19 deaths reduced, in the short term, death rates overall. I tried to hint at this a little more bluntly last April, in a story that tried to figure out how many people would have to die of Covid-19 in the United States before everyone knew at least one person, and so might be more open to behavioral interventions. It turns out to be a harder math problem than it sounds, but the range was between about 500,000 and 1.6 million people, which seemed much less possible nine months ago than it does today.)
And the converse might be true too. Maybe people who don’t buy it, who get their information from sources that downplay Covid-19 or think that a laissez-faire herd-immunity strategy would work ( it wouldn’t ), might not respond to any interventions. They’d put themselves at risk, and since Covid-19 has significant transmission by people who have no symptoms , put others at risk as well. That could look like the intervention itself was failing, when the real problem was compliance, or lack of synergistic effects with other subtler, cautious behaviors. So which thing actually cut R t ?
No, seriously, I’m asking. Because no one really knows.
Even worse, different places and conditions might lessen or increase how well Covid-19 spreads. It’s “spatiotemporally heterogenous,” meaning the disease moves in spikes through populations, with super-spreading events having a disproportionate effect on where and when it crops up. One study , from researchers in Canada and England in the journal Proceedings of the National Academy of Sciences in September, even hypothesized that different interventions would affect the reproductive number differently at different kinds of events—smaller or larger, longer or shorter, and so on. The trick is knowing which kind of event you’re at, and getting people there to believe they should do the safest thing.
A catastrophic year of inconsistencies has led, in the US, to millions of sick people, a quarter million deaths, and mounting frustration. Even influential public health voices, like former White House Covid-19 task force leader Scott Atlas, seemed to be arguing for a “herd immunity” strategy that involved letting everyone get sick and hoping for the best. If nothing seems to work, why bother trying?
Of course, it’s not that nothing works. It’s that everything does, a model that some public-health-minded scientists liken to stacking slices of Swiss cheese . Layer enough of them, and all the holes get blocked. The sum is greater than the holes of the parts.
If the government wants people to keep building cheese barriers (if you see what I mean), the cheese has to come with social and financial support for staying home, for wearing masks—money to keep businesses and homes together until the pandemic ends—and clear, transparent communication from officials (and maybe some famous people, too) to explain what’s going on and why. None of that has happened. “The most effective interventions are population-wide risk mitigation measures based on changing the public’s risk profiles. That’s why the United States has failed so abysmally—because very simple behavioral mitigations have become politicized,” Gostin says.
Back in April I wrote that the point of communal public health measures was to hold the line , to keep cases and deaths low, to keep the hospital system from being overwhelmed until research scientists could get us out of this mess. I thought, perhaps naively, it would take months. It took a year, and cases and deaths are worse than they’ve ever been. But we’re almost there—months away from getting a shot that looks likely to stop the pandemic. Holding on is the only option. “It’s not the expressed goal, but that’s the absolute hidden goal,” Gostin says. “That’s literally all we’ve got left. We’ve failed at everything else.” Non-pharmaceutical interventions are the only tools in the toolbox, and they only work if you take them out and use them—even if you don’t know how to use them well. They work, and they’re the only way the country will get from here to the After Times. But it’s going to be a muddle, not a march.
- 📩 Want the latest on tech, science, and more? Sign up for our newsletters !
- Two global efforts try to trace the origin of the Covid virus
- Warp speed, atomic structure, and the future of vaccines
- The free-market approach to this pandemic isn't working
- Winter is coming. Could humidifiers help ?
- The vulnerable can wait. Vaccinate the super-spreaders first
- Read all of our coronavirus coverage here

Emily Mullin

John Timmer, Ars Technica

Beth Mole, Ars Technica

Maanvi Singh

Lyndie Chiou
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- International...
International collaboration and covid-19: what are we doing and where are we going?
Read our covid-19: the road to equity and solidarity collection.
- Related content
- Peer review
- Jesse B Bump , executive director 1 2 ,
- Peter Friberg , professor 3 4 ,
- David R Harper , senior consulting fellow 5
- 1 Takemi Program in International Health, Harvard TH Chan School of Public Health, USA
- 2 Bergen Centre for Ethics and Priority Setting, University of Bergen, Norway
- 3 Department of Public Health and Community Medicine, Sahlgrenska Academy at Gothenburg University, Gothenburg, Sweden
- 4 Swedish Institute for Global Health Transformation, Royal Swedish Academy of Sciences, Stockholm, Sweden
- 5 Chatham House, London, UK
- Correspondence to: J B Bump bump{at}hsph.harvard.edu
The mixed patchwork of achievements and mis-steps in responding to covid-19 show powerful nations are not living up to their commitment to solidarity and equity, argue Jesse Bump and colleagues
The 19th century pandemics that followed the globalisation of commercial and military activities led to a series of sanitary conferences, at which countries agreed to fight infectious diseases by working together. 1 In the nearly two centuries since the Ottoman Empire convened the initial gathering, 2 formal collaboration in health has been institutionalised through the World Health Organization, founded in 1948 as the specialised agency of the United Nations and granted international responsibilities and a legal mandate over international public health matters such as the cross-border spread of disease. 3 4
The covid-19 pandemic has once again shown the value of international cooperation and collaboration. Its importance is intuitive and widely supported. When the World Health Assembly convened in May 2020, member states passed a resolution emphasising the need for solidarity, resource redistribution, and collective action. 5 Many individuals agree, and most want their countries to increase collaboration. A poll in 14 countries showed that about 60% of respondents believe that even greater international collaboration would further reduce the number of covid-19 cases. 6 And in public opinion polls the European parliament found that most citizens believed that their governments should show greater solidarity in the covid-19 era. 7
Logic of collaboration
The reasons for collaboration remain clear, logical, and have endured essentially unchanged from their original conceptualisation in the 1800s. Three of the most central are as follows. Firstly, the many ties between nations create collective health risks that are difficult to manage independently. The rapid spread of SARS-CoV-2 shows the close connections between countries, and the poorly managed economic and social costs are further evidence of their shared fate. Secondly, sharing knowledge and experience accelerates learning and facilitates more rapid progress. Information and knowledge on pathogens, their transmission, the diseases they provoke, and possible interventions are all areas in which researchers and public health professionals can benefit from the experience of others. Thirdly, agreeing on rules and standards supports comparability of information, helps establish good practices, and underpins shared understanding and mutual trust. All three reasons drive nations to collaborate and are reflected in their creation of WHO, a central authority, and its World Health Assembly (WHA), which serves as a forum for countries to share information, debate issues, and take collective decisions.
Reality of collaboration in covid-19 pandemic
Despite the logical imperative to collaborate and the long heritage of attempts to do so, one year into the covid-19 pandemic and transmission rages on, with nearly 100 million cases and over two million deaths by January 2021. The ongoing devastation has raised questions about the effectiveness of international collaboration in health and shone a powerful spotlight on WHO and other multilateral agencies with interests in disease control. Member states have ordered an inquiry into WHO’s response, 8 and interim findings have been critical of the institution. 9
Meanwhile, WHO has warned that vaccine nationalism by members states is leading to “catastrophic moral failure.” 10 One of its independent oversight committees has added that the “rising politicisation of pandemic response” is a “material impediment” to WHO’s work, and has warned that WHO cannot succeed without greater collaboration by member states. 11 These realities call for close scrutiny of collaboration in international health and demand fresh attention to its problems.
Member states and collaboration at WHO
If international collaboration through WHO meets with criticisms on many fronts, then the next question is why. One of WHO’s most crucial responsibilities is to notify its member states about the emergence and spread of infectious diseases, and it has been criticised for reacting too slowly at the beginning of the covid-19 outbreak in Wuhan, China. 12 13 Detailed reviews of the timing are available, 14 but some of WHO’s initial actions seem to have been prompt. On 31 December 2019, WHO’s China office picked up a media statement by the Wuhan Municipal Health Commission mentioning viral pneumonia. After seeking more information, WHO notified partners in the Global Outbreak Alert and Response Network (GOARN), which includes major public health institutes and laboratories around the world, on 2 January. Chinese officials formally reported on the viral pneumonia of unknown cause on 3 January. WHO alerted the global community through Twitter on 4 January and provided detailed information to all countries through the international event communication system on 5 January. 15 Where there were delays, one important reason was that national governments seemed reluctant to provide information. 16
WHO is a manifestation of the advantages of cooperation and collaboration, and it consistently leads member states in ways that uphold its mission to advance the highest standard of health for all. In the pandemic, WHO has shown leadership in sharing information and in co-launching the Access to COVID-19 Tools (ACT) Accelerator, a global collaboration to accelerate development and equitable access to diagnostic tests, treatments, and vaccines. 17 WHO advocated for global financial solidarity by establishing the Covid-19 Solidarity Response Fund in April 2020 and the external independent WHO Foundation in May 2020. 18 19 In addition, WHO has produced a wide range of technical guidance together with cost estimates for responding to the pandemic, 20 decried vaccine nationalism, and exhorted its members to increase their solidarity. 10
But WHO also exemplifies the reluctance of member states to fully trust one another. For example, member states do not grant WHO powers to scrutinise national data, even when they are widely questioned, 21 22 or to conduct investigations into infectious diseases if national authorities do not agree, 23 or to compel participation in its initiatives. 24 Despite passing a resolution on the need for solidarity in response to covid-19, many member states have chosen self-centred paths instead. Against WHO’s strongest advice, vaccine nationalism has risen to the fore, with nations and regional blocks seeking to monopolise promising candidates. 25 Similarly, nationalistic competition has arisen over existing medicines with the potential to benefit patients with covid-19. 26 27 Forgoing cooperation for selfishness, some nations have been slow to support the WHO organised common vaccine development pool, 24 with some flatly refusing to join. 28
The tensions between what member states say and do is reflected in inequalities in the international governance of health that have been exploited to weaken WHO systematically, particularly after it identified the prevailing world economic order as a major threat to health and wellbeing in its 1978 Health for All declaration. 29 WHO’s work on a code of marketing of breastmilk substitutes around the same time 30 increased concern among major trade powers that WHO would use its health authority to curtail private industry. Starting in 1981, the US and aligned countries began interfering with WHO’s budget, announcing a policy of “zero growth” to freeze the assessed contributions that underpinned its independence and reorienting its activities through earmarked funds. 31 The result is a WHO shaped by nations that can pay for their own priorities. This includes the preference that WHO focus on specific diseases rather than the large social, political, and commercial determinants of health or the broad public health capacities in surveillance, preparedness, and other areas needed for pandemic prevention and management. 32 33
Health cooperation at other multilaterals
As member states have constrained WHO, practical, economic, and ethical imperatives have led other multilaterals to embrace aspects of the health agenda. The World Bank, for example, has directly engaged with global infectious disease control through its pandemic emergency financing facility, supported by issuing “pandemic bonds.” 34 When the first pandemic bonds were sold in 2017 as a mechanism for speeding financing, coronaviruses were mentioned specifically, along with five other viruses deemed most likely to cause a pandemic. The bond offering was oversubscribed by 200%, and would, the bank claimed, “channel surge funding to developing countries facing the risk of a pandemic” and “potentially save millions of lives.” 35
Even before the arrival of covid-19, the bonds were controversial in health circles because of their very high payout thresholds, 36 but with more expertise in finance than health, the World Bank persisted. As the covid-19 pandemic built in early 2020 many investors believed the bonds would pay out, but they did not. 37 The bonds were issued in two tranches, one of which was not eligible for payout until three months after the beginning of any outbreak, and both tranches had thresholds for mortality and spread, along with a requirement for exponential growth of cases in low income countries. 38 Essentially, the payout conditions required a pandemic to be well established before funds could be released, leading to wide condemnation. 39 When the bonds did pay out, the allocation for each country was capped at a maximum of $15m (£11m; €12m). Too little, too late concluded many analysts. 40 Plans for future pandemic bonds were quietly abandoned. 41
In other cases, major UN member states have found it easier to establish new organisations with narrowly defined missions than to strengthen or broaden WHO. Both Gavi the Vaccine Alliance and the Global Fund to fight AIDS, TB, and Malaria were established in the early 2000s around health priorities reflected in their names. Both institutions have governance structures that are more inclusive and flexible than the member states model of the UN agencies, and both are focused on areas of specific agreement among major donors.
Gavi is a public-private partnership for increasing vaccine access in low income countries, including through pooled procurement and advance market commitments. 42 The expectation of a vaccine for covid-19 suggested a clear role for Gavi, which co-leads the vaccine pillar of the ACT Accelerator, Covax. 17 43 Although Covax membership is optional, 189 countries have joined, including China, all members of the EU, and 92 low income countries. 44 The Covax facility should therefore be well placed to cross-subsidise vaccines for all low income countries, but uncertainty in its terms have led some to explore independent options. 45 Additionally, there are questions about whether Gavi’s market focused perspective can manage the ethical and regulatory issues threatening equitable access and distribution at a time of nationalistic competition.
The Global Fund is a public-private partnership that emerged from uncertainty about how to raise and manage the unprecedented resources required to combat HIV/AIDS and disagreements about which diseases should be included and what organisation would be in charge of the funds. 46 With the arrival of covid-19, the Global Fund has sought to support eligible countries by allowing them to divert up to 5% of existing grants and allocating an additional $665m for ad hoc requests to “reinforce the response to covid-19, mitigate the impact of the pandemic on HIV, TB, and malaria programmes, and make urgent improvements in health and community systems.” 47 However, covid-19 reopens many questions about how global health initiatives are financed and delivered, including whether the Global Fund should be constrained to three diseases and how it should relate to WHO.
Shared future
The covid-19 pandemic painfully shows the reasons why nations are better off when they cooperate and collaborate in health, and also reveals the hazards of their incomplete commitment to doing so. Member states have prioritised themselves by restricting WHO from meaningful oversight of national information and endangered global health security by competing for vaccines rather than allocating them equitably. The inability to verify national data or advance its own estimates is just one of the many crucial dimensions in which WHO is prevented from maintaining the primacy of technical competence over the self-interested obfuscations of some member states. WHO’s independence is compromised also through the manipulation of its budget. The patchwork of institutions active in health reflects the limited, ad hoc agreement among powerful countries. Although generally global institutions have performed well in their missions, their often limited mandates leave the world’s people inadequately protected from new threats. In a pandemic, the cost is expressed in lives and livelihoods. More than 10 000 people were dying daily at end of 2020, 48 and the world economy was forecast to lose $5tn or more in 2020 alone. 49 The imperative of finding collaborative and collective solutions—solidarity—has never been more obvious, or more urgent, for covid-19, climate change, non-communicable diseases, and the many other pressing and grave challenges that hinge on collective action.
Meaningful international collaboration is a critical part of the road ahead and calls for immediate action in three areas. Firstly, member states must end the systematic weakening of WHO—end ad hoc institutional fragmentation in global health and end budgetary manipulation. Secondly, they must support the independence of WHO—increase its core budget and build its authority over trade and travel related issues, including compulsory licensure for pharmaceuticals. Thirdly, states must uphold fairness, participation, and accountability by granting WHO powers to hold members accountable, including for overcoming deficiencies in national data, and by decolonising its governance to address the undue influence of a small number of powerful member states.
Key messages
Shared objectives draw nations to collaborate on international health challenges
Poor performance against covid-19, however, reflects patterns of self-interested nationalism that undermine WHO and other international institutions
Although these institutions have performed reasonably well, the pandemic reveals limitations in their mandates that reflect some member states’ unwillingness to fully collaborate
Addressing these deficits in collaboration is essential to resolving global collective action challenges, including covid-19, climate change, and non-communicable diseases
Advance global health by ending the institutional fragmentation and budgetary manipulation that weaken WHO, strengthen its authority over trade and travel issues, and decolonise its governance
Acknowledgments
We thank Emily Coles for her help.
Contributors and sources: JBB is a historian of medicine and public health who has reported widely on current global health policy. PF is a physician and public health researcher with special interest in evidence informed policy. DRH is a global public health policy consultant and has worked as an expert at the top levels of national government and internationally. The article was conceptualised jointly by JBB, PF, and DRH. JBB wrote the initial draft using inputs from PF and DRH. All three authors revised and edited the article to produce a final draft. JBB is the guarantor.
Competing interests: We have read and understood BMJ policy on declaration of interests and have no relevant interests to declare.
Provenance and peer review: Commissioned; externally peer reviewed.
This article is part of a collection launched at the Prince Mahidol Awards Conference (PMAC) in January 2021. Funding for the articles, including open access fees, was provided by PMAC. The BMJ commissioned, peer reviewed, edited, and made the decision to publish these articles. David Harper and an expert panel that included PMAC advised on commissioning for the collection. Rachael Hinton and Kamran Abbasi were the lead editors for The BMJ.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- ↵ Howard-Jones N. The scientific background of the International Sanitary Conferences, 1851-1938. World Health Organization, 1975.
- ↵ UN. The global guardian of public health. https://www.un.org/en/sections/issues-depth/health/
- ↵ WHO. Covid-19 response. Seventy third World Health Assembly 2020. https://apps.who.int/gb/ebwha/pdf_files/WHA73/A73_CONF1Rev1-en.pdf
- ↵ Devlin K, Connaughton A. Most approve of national response to covid-19 in 14 advanced economies. PEW Research Center, 2020. https://www.pewresearch.org/global/2020/08/27/most-approve-of-national-response-to-covid-19-in-14-advanced-economies/
- ↵ European Parliament. Uncertainty/EU/Hope: public opinion in times of covid-19: 2020. https://www.europarl.europa.eu/at-your-service/files/be-heard/eurobarometer/2020/public_opinion_in_the_eu_in_time_of_coronavirus_crisis_2/en-covid19-survey2-report.pdf .
- ↵ Coronavirus: World Health Organization members agree response probe. BBC News 2020 May 19. https://www.bbc.co.uk/news/world-52726017
- ↵ Nebehay S. WHO pandemic review panel critical of China, WHO delays. Reuters 2021 Jan 18. euters.com/article/us-health-coronavirus-who-panel/independent-pandemic-review-panel-critical-of-china-who-delays-idUSKBN29N1V1
- ↵ Schemm P, Hassan J. WHO chief warns of “catastrophic moral failure” as rich countries dominate vaccine supplies. Washington Post 2021 Jan 18. https://www.washingtonpost.com/world/who-chief-warns-of-catastrophic-moral-failure-as-rich-countries-dominate-vaccine-supplies/2021/01/18/033644a0-5978-11eb-a849-6f9423a75ffd_story.html .
- ↵ Independent Oversight and Advisory Committee for the WHO Health Emergencies Programme. Interim report on WHO’s response to COVID-19, January-April 2020. https://www.who.int/about/who_reform/emergency-capacities/oversight-committee/IOAC-interim-report-on-COVID-19.pdf?ua=1
- ↵ Peel M, Gross A, Cookson C. WHO struggles to prove itself in the face of COVID-19. Financial Times 2020 Jul 11. https://www.ft.com/content/c2809c99-594f-4649-968a-0560966c11e0
- ↵ Hernandez J. Trump slammed the WHO over coronavirus. He’s not alone. New York Times 2020 Apr 8. https://www.nytimes.com/2020/04/08/world/asia/trump-who-coronavirus-china.html
- ↵ WHO. Timeline: WHO’s COVID-19 response. 2020 https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline :
- ↵ Associated Press. China delayed releasing coronavirus info, frustrating WHO. 2 Jun 2020. https://apnews.com/article/3c061794970661042b18d5aeaaed9fae .
- ↵ WHO. The access to covid-19 tools (ACT) accelerator. 2020 https://www.who.int/initiatives/act-accelerator
- ↵ WHO. WHO foundation established to support critical global health needs, 2020. https://www.who.int/news/item/27-05-2020-who-foundation-established-to-support-critical-global-health-needs#:~:text=The%20World%20Health%20Organization%20provides,safe%20and%20serve%20the%20vulnerable
- ↵ WHO. Coronavirus disease (COVID-19) donors & partners: WHO says thank you! 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/donors-and-partners/funding .
- ↵ Winter L. Data fog: Why some countries’ coronavirus numbers do not add up. AlJazeera 2020 Jun 17. https://www.aljazeera.com/features/2020/6/17/data-fog-why-some-countries-coronavirus-numbers-do-not-add-up
- ↵ Stolberg SG. Trump administration strips CDC of control of coronavirus data. New York Times 2020 Jul 14. https://www.nytimes.com/2020/07/14/us/politics/trump-cdc-coronavirus.html
- ↵ Hernandez J. Two members of WHO team on trail of virus are denied entry to China. New York Times 2021 Jan 13. https://www.nytimes.com/2021/01/13/world/asia/china-who-wuhan-covid.html
- ↵ Mancini DM, Peel M. “Vaccine nationalism” delays WHO’s struggling Covax scheme. Financial Times 2020 Sep 1. https://www.ft.com/content/502df709-25ac-48f6-aee1-aec7ac03c759
- ↵ Buranyi S. ‘Vaccine nationalism’ stands in the way of an end to the Covid-19 crisis. Guardian , 2020 Aug 14. https://www.theguardian.com/commentisfree/2020/aug/14/vaccine-nationalism-stands-in-the-way-of-an-end-to-the-covid-19-crisis
- ↵ US Department of Health and Human Services. Trump administration secures new supplies of remdesivir for the United States. Press release, 29 Jun 2020.
- ↵ Taylor A. Why vaccine nationalism is winning. Washington Post , 2020 Sep 3. https://www.washingtonpost.com/world/2020/09/03/why-coronavirus-vaccine-nationalism-is-winning/
- ↵ WHO. Declaration of Alma-Ata. International Conference on Primary Health Care. Alma-Ata, USSR, 1978.
- ↵ WHO. International code of marketing breast-milk substitutes. WHO, 1981.
- ↵ WHO. Verbatim records of plenary meetings reports of committees, WHA/34/1981/REC/2 Thirty-Fourth World Health Assembly. 1981. https://apps.who.int/iris/bitstream/handle/10665/155680/WHA34_1981-REC-2_eng.pdf?sequence=1&isAllowed=y .
- Vaughan JP ,
- Mogedal S ,
- ↵ World Bank. World Bank group launches groundbreaking financing facility to protect poorest countries against pandemics. 2016. https://www.worldbank.org/en/news/press-release/2016/05/21/world-bank-group-launches-groundbreaking-financing-facility-to-protect-poorest-countries-against-pandemics
- ↵ World Bank. World Bank launches first-ever pandemic bonds to support $500 million pandemic emergency financing facility. 2017. https://www.worldbank.org/en/news/press-release/2017/06/28/world-bank-launches-first-ever-pandemic-bonds-to-support-500-million-pandemic-emergency-financing-facility [
- ↵ Gross A. World Bank’s pandemic bonds sink as coronavirus spreads. Financial Times 2020 Feb 24. https://www.ft.com/content/70dd05ac-54d8-11ea-8841-482eed0038b1
- ↵ Vossos T, Lauerman J. Deadly virus fails to trigger world bank’s pandemic bonds. Bloomberg 2020 Apr 10. https://www.bloomberg.com/news/articles/2020-04-10/deadly-virus-fails-to-trigger-world-bank-s-pandemic-bonds
- Erikson SL ,
- ↵ Winck B. Coronavirus triggers $133 million worth of the World Bank's pandemic bonds, releasing aid to developing nations hammered by the outbreak. Market Insider 2020 10 Apr. https://markets.businessinsider.com/news/stocks/coronavirus-triggers-world-bank-pandemic-bonds-release-aid-poor-nations-2020-4-1029108864?utm_source=markets&utm_medium=ingest
- ↵ Hodgson C. World Bank ditches second round of pandemic bonds. Financial Times 2020 Jul 5. https://www.ft.com/content/949adc20-5303-494b-9cf1-4eb4c8b6aa6b :
- ↵ GAVI. Phase V (2021-2025). https://www.gavi.org/our-alliance/strategy/phase-5-2021-2025
- ↵ Berkley S. Covax explained. 2020. https://www.gavi.org/vaccineswork/covax-explained [
- ↵ GAVI. Covax commitment agreements. 2020. https://www.gavi.org/sites/default/files/covid/pr/COVAX_CA_COIP_List_COVAX_PR_24-11.pdf
- ↵ Guarascio F. WHO vaccine drive bedevilled by familiar question: who pays if things go wrong? Reuters 2020 Oct 15. https://www.reuters.com/article/health-coronavirus-who-vaccine-insight/who-vaccine-drive-bedevilled-by-familiar-question-who-pays-if-things-go-wrong-idUSKBN2701PO .
- ↵ Copson R, Salaam T. The Global Fund to Fight AIDS, Tuberculosis, and Malaria, background and current issues. Foreign Affairs, Defense, and Trade Division, US Department of State, 2003. https://www.everycrsreport.com/files/20030127_RL31712_6d8aac204fb47a7dffc6368c461b99953d5afa37.pdf
- ↵ Global Fund. Covid-19 operational response. https://www.theglobalfund.org/en/covid-19
- ↵ WHO. Coronovirus disease dashboard. https://covid19.who.int/
- Dobson AP ,

Search the United Nations
- Policy and Funding
- Recover Better
- Disability Inclusion
- Secretary-General
- Financing for Development
- ACT-Accelerator
- Member States
- Health and Wellbeing
- Policy and Guidance
- Vaccination
- COVID-19 Medevac
- i-Seek (requires login)
- Awake at Night podcast

COVID-19 photo essay: We’re all in this together
About the author, department of global communications.
The United Nations Department of Global Communications (DGC) promotes global awareness and understanding of the work of the United Nations.
23 June 2020 – The COVID-19 pandemic has demonstrated the interconnected nature of our world – and that no one is safe until everyone is safe. Only by acting in solidarity can communities save lives and overcome the devastating socio-economic impacts of the virus. In partnership with the United Nations, people around the world are showing acts of humanity, inspiring hope for a better future.
Everyone can do something

Rauf Salem, a volunteer, instructs children on the right way to wash their hands, in Sana'a, Yemen. Simple measures, such as maintaining physical distance, washing hands frequently and wearing a mask are imperative if the fight against COVID-19 is to be won. Photo: UNICEF/UNI341697
Creating hope

Venezuelan refugee Juan Batista Ramos, 69, plays guitar in front of a mural he painted at the Tancredo Neves temporary shelter in Boa Vista, Brazil to help lift COVID-19 quarantine blues. “Now, everywhere you look you will see a landscape to remind us that there is beauty in the world,” he says. Ramos is among the many artists around the world using the power of culture to inspire hope and solidarity during the pandemic. Photo: UNHCR/Allana Ferreira
Inclusive solutions

Wendy Schellemans, an education assistant at the Royal Woluwe Institute in Brussels, models a transparent face mask designed to help the hard of hearing. The United Nations and partners are working to ensure that responses to COVID-19 leave no one behind. Photo courtesy of Royal Woluwe Institute
Humanity at its best

Maryna, a community worker at the Arts Centre for Children and Youth in Chasiv Yar village, Ukraine, makes face masks on a sewing machine donated by the Office of the United Nations High Commissioner for Refugees (UNHCR) and civil society partner, Proliska. She is among the many people around the world who are voluntarily addressing the shortage of masks on the market. Photo: UNHCR/Artem Hetman
Keep future leaders learning

A mother helps her daughter Ange, 8, take classes on television at home in Man, Côte d'Ivoire. Since the COVID-19 pandemic began, caregivers and educators have responded in stride and have been instrumental in finding ways to keep children learning. In Côte d'Ivoire, the United Nations Children’s Fund (UNICEF) partnered with the Ministry of Education on a ‘school at home’ initiative, which includes taping lessons to be aired on national TV and radio. Ange says: “I like to study at home. My mum is a teacher and helps me a lot. Of course, I miss my friends, but I can sleep a bit longer in the morning. Later I want to become a lawyer or judge." Photo: UNICEF/UNI320749
Global solidarity

People in Nigeria’s Lagos State simulate sneezing into their elbows during a coronavirus prevention campaign. Many African countries do not have strong health care systems. “Global solidarity with Africa is an imperative – now and for recovering better,” said United Nations Secretary-General António Guterres. “Ending the pandemic in Africa is essential for ending it across the world.” Photo: UNICEF Nigeria/2020/Ojo
A new way of working

Henri Abued Manzano, a tour guide at the United Nations Information Service (UNIS) in Vienna, speaks from his apartment. COVID-19 upended the way people work, but they can be creative while in quarantine. “We quickly decided that if visitors can’t come to us, we will have to come to them,” says Johanna Kleinert, Chief of the UNIS Visitors Service in Vienna. Photo courtesy of Kevin Kühn
Life goes on

Hundreds of millions of babies are expected to be born during the COVID-19 pandemic. Fionn, son of Chloe O'Doherty and her husband Patrick, is among them. The couple says: “It's all over. We did it. Brought life into the world at a time when everything is so uncertain. The relief and love are palpable. Nothing else matters.” Photo: UNICEF/UNI321984/Bopape
Putting meals on the table

Sudanese refugee Halima, in Tripoli, Libya, says food assistance is making her life better. COVID-19 is exacerbating the existing hunger crisis. Globally, 6 million more people could be pushed into extreme poverty unless the international community acts now. United Nations aid agencies are appealing for more funding to reach vulnerable populations. Photo: UNHCR
Supporting the frontlines

The United Nations Air Service, run by the World Food Programme (WFP), distributes protective gear donated by the Jack Ma Foundation and Alibaba Group, in Somalia. The United Nations is using its supply chain capacity to rapidly move badly needed personal protective equipment, such as medical masks, gloves, gowns and face-shields to the frontline of the battle against COVID-19. Photo: WFP/Jama Hassan

S7-Episode 2: Bringing Health to the World
“You see, we're not doing this work to make ourselves feel better. That sort of conventional notion of what a do-gooder is. We're doing this work because we are totally convinced that it's not necessary in today's wealthy world for so many people to be experiencing discomfort, for so many people to be experiencing hardship, for so many people to have their lives and their livelihoods imperiled.”
Dr. David Nabarro has dedicated his life to global health. After a long career that’s taken him from the horrors of war torn Iraq, to the devastating aftermath of the Indian Ocean tsunami, he is still spurred to action by the tremendous inequalities in global access to medical care.
“The thing that keeps me awake most at night is the rampant inequities in our world…We see an awful lot of needless suffering.”
:: David Nabarro interviewed by Melissa Fleming

Brazilian ballet pirouettes during pandemic
Ballet Manguinhos, named for its favela in Rio de Janeiro, returns to the stage after a long absence during the COVID-19 pandemic. It counts 250 children and teenagers from the favela as its performers. The ballet group provides social support in a community where poverty, hunger and teen pregnancy are constant issues.

Radio journalist gives the facts on COVID-19 in Uzbekistan
The pandemic has put many people to the test, and journalists are no exception. Coronavirus has waged war not only against people's lives and well-being but has also spawned countless hoaxes and scientific falsehoods.
How to stop the spread of COVID-19
COVID-19 - Prevention; 2019 Novel Coronavirus - Prevention; SARS CoV 2 - Prevention
Coronavirus disease 2019 (COVID-19) is a serious disease, mainly of the respiratory system, affecting many people around the globe. It can cause mild to severe illness and even death. COVID-19 spreads easily between people. Learn how to protect yourself and others from this illness.
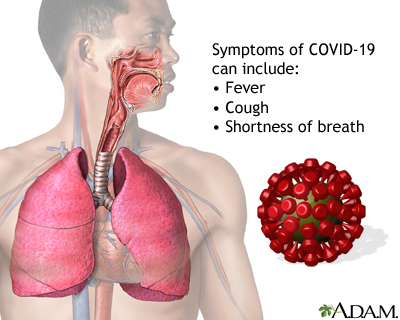
Infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causes COVID-19, a respiratory illness that ranges from mild symptoms to pneumonia or even death. Symptoms occur within 2 to 14 days from exposure to the virus and may include fever, cough, shortness of breath, chills, muscle pain, headache, sore throat, and new loss of sense of taste or smell. COVID-19 may be more severe in people who are older or who have chronic health conditions, such as heart disease or diabetes.

Steps for proper handwashing include: 1. Take off any jewelry. 2. Wet your hands with clean water. 3. Apply soap and lather your hands by rubbing them together for at least 20 seconds. 4. Make sure you also lather the back of the hands, between the fingers, the thumb, and under the nails. Rinse well. 5. Dry with a clean towel or air dry. Proper handwashing is the best way to avoid spreading germs to help prevent infection.

Using face masks in public settings helps reduce the spread of COVID-19. COVID-19 spreads to people within close contact via small droplets sprayed into the air by someone with the disease who coughs, sneezes, sings, talks, or breathes. Wearing face masks or cloth face coverings helps reduce the spray of respiratory droplets from the nose and mouth. Wearing a face mask may also protect you from infection.

Wearing face masks or cloth face coverings helps prevent the spread of COVID-19. For masks to work, they have to be worn properly. Choose a mask with two or more layers of washable, breathable fabric that completely covers your mouth and nose and fits snugly against the sides of your face, leaving no gaps. Do not wear a mask that is too loose on the sides. Do not pull the mask low on your nose, below your nose, or below your mouth or chin. Do not leave your chin or your mouth exposed or dangle the mask from one ear. Do not wear the mask in any other way that does not entirely cover your mouth and nose. Wash your hands before and after wearing the mask and use only the loops of the mask to put it on and take it off. Do not touch the front of the mask while wearing it. If you use a cloth mask, wash it and dry it daily and keep it in a clean, dry place.

COVID-19 vaccines protect people from getting COVID-19. They are a vital tool to help stop the COVID-19 pandemic. The vaccine works with your body’s immune system against the SARS-CoV-2 virus, which causes COVID-19.While COVID-19 vaccines will not make you sick, they may cause certain side effects and flu-like symptoms. This is to be expected. These symptoms may be a sign that your body is making antibodies against the virus. Even after you receive both doses of the COVID-19 vaccine, you will still need to continue to wear a mask with at least 2 layers that fits snugly over your nose and mouth and is secured under your chin, stay at least 6 feet away from others, and wash your hands often.
Information
HOW COVID-19 SPREADS
COVID-19 is an illness caused by infection with the SARS-CoV-2 virus. COVID-19 most commonly spreads between people with close contact (about 6 feet or 2 meters). When someone with the illness coughs, sneezes, sings, talks, or breathes, droplets carrying the virus spray into the air. You can catch the illness if you breathe in these droplets or they get in your eyes.
In some instances, COVID-19 may spread through the air and infect people who are more than 6 feet away. Small droplets and particles can remain in the air for minutes to hours. This is called airborne (or aerosol) transmission, and it occurs mainly in enclosed spaces with poor ventilation. However, it is more common for COVID-19 to spread through close contact.
Less often, the illness can spread if you touch a surface with the virus on it, and then touch your eyes, nose, mouth, or face. But this is a much less common way the virus spreads.
HOW TO PREVENT COVID-19
You can spread COVID-19 before you show symptoms . Some people with the illness never have symptoms, but can still spread the disease. However, there are ways to protect yourself and others from getting COVID-19. These tips can help you and others stay safe:
- Get an updated COVID-19 vaccine . Being vaccinated helps protect you from getting and spreading COVID-19. Being vaccinated can also help protect you from serious illness if you do get the virus.
- Make sure children ages 6 months and older get the COVID-19 vaccine . Getting children and teens vaccinated helps prevent them from spreading COVID-19 to older relatives and young siblings and friends who can't or don't get the vaccine. It also helps protect children and teens from serious illness.
- If you are vaccinated, and in an area where COVID-19 hospital admission rates are high, you can wear a face mask or respirator that fits well without gaps when you are indoors in public.
- If you have a weakened immune system, you may want to wear a face mask indoors in public regardless of how active COVID-19 is in your community.
- Avoid poorly ventilated indoor spaces and crowded areas, even if you are vaccinated. If you are indoors, open windows and doors and use fans to help bring in outdoor air, when possible. Use a portable high-efficiency particulate air (HEPA) cleaner. Spending time outdoors or in well-ventilated spaces can help reduce your exposure to respiratory droplets.
- COVID-19 tests can help prevent the spread to others. You can use COVID-19 self-tests at home and get quick results whether or not you have symptoms.
- Wash your hands many times a day with soap and running water for at least 20 seconds. In general, this is a good practice to help prevent the spread of germs. Do this before eating or preparing food, after using the toilet, and after coughing, sneezing, or blowing your nose. Use an alcohol-based hand sanitizer (at least 60% alcohol) if soap and water are not available.
- Cover your mouth and nose with a tissue or your sleeve (not your hands) when coughing or sneezing. Droplets that are released when a person sneezes or coughs are infectious. Throw away the tissue after use.
- Avoid touching your face, eyes, nose, and mouth with unwashed hands.
- Do not share personal items such as cups, eating utensils, towels, or bedding. Wash anything you have used in soap and water.
- Know the symptoms of COVID-19. If you develop any symptoms, contact your health care provider.
- Stay home if you think you have COVID-19 or test positive for the virus. Follow guidance for how long to stay away from others and when you can safely resume normal activities, as listed below.
WHAT TO DO IF YOU GET COVID-19
If you have COVID-19 or have symptoms of it, you must stay at home and avoid contact with other people , both inside and outside your home, to avoid spreading the illness.
Once you start to feel better, you can go back to your normal activities if BOTH of the following things are true:
- For at least 24 hours, your symptoms have improved AND
- You have not had a fever for at least 24 hours, and you are not using fever-reducing medicine
Even though you feel better, you may still be able to spread the virus to others for several days. For this reason, once you go back to your normal activities, continue to protect others from illness by taking these steps for 5 days:
- Practice good hygiene by washing your hands and cleaning "high touch" areas around your home.
- Take steps to bring cleaner air inside your home by opening windows and using exhaust fans.
- Wear a mask around others.
- Practice physical distancing by avoiding close contact and avoiding crowds.
- Self-test for COVID-19 before being indoors with others.
You should also practice these steps for 5 days if you tested positive for COVID-19, but did not have any symptoms. Even though you have no symptoms, you can still spread the virus to others. Doing so will protect people at risk for serious illness, such as people who are immunocompromised.
If your fever returns after resuming normal activities, you should go back to staying home and away from others. Once your fever and symptoms improve for more than 24 hours, you can resume activities while taking steps to protect others for 5 more days.
Centers for Disease Control and Prevention website. COVID-19: How COVID-19 spreads. www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html . Updated August 11, 2022. Accessed March 10, 2024.
Centers for Disease Control and Prevention website. COVID-19: How to protect yourself and others. www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html . Updated July 6, 2023. Accessed March 10, 2024.
Centers for Disease Control and Prevention website. COVID-19: Masks. www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/masks.html . Updated August 12, 2021. Accessed March 10, 2024.
Centers for Disease Control and Prevention website. COVID-19: Use and care of masks. www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/about-face-coverings.html . Updated May 11, 2023. Accessed March 10, 2024.
Centers for Disease Control and Prevention website. Respiratory virus guidance. www.cdc.gov/respiratory-viruses/guidance/respiratory-virus-guidance.html . Updated March 1, 2024. Accessed March 10, 2024.
Centers for Disease Control and Prevention website. Stay up to date with COVID-19 vaccines. www.cdc.gov/coronavirus/2019-ncov/vaccines/stay-up-to-date.html . Updated March 7, 2024. Accessed March 10, 2024.
Version Info
Last reviewed on: 2/22/2023
Reviewed by: Frank D. Brodkey, MD, FCCM, Associate Professor, Section of Pulmonary and Critical Care Medicine, University of Wisconsin School of Medicine and Public Health, Madison, WI. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 03/12/2024.
Students’ Essays on Infectious Disease Prevention, COVID-19 Published Nationwide
As part of the BIO 173: Global Change and Infectious Disease course, Professor Fred Cohan assigns students to write an essay persuading others to prevent future and mitigate present infectious diseases. If students submit their essay to a news outlet—and it’s published—Cohan awards them with extra credit.
As a result of this assignment, more than 25 students have had their work published in newspapers across the United States. Many of these essays cite and applaud the University’s Keep Wes Safe campaign and its COVID-19 testing protocols.
Cohan, professor of biology and Huffington Foundation Professor in the College of the Environment (COE), began teaching the Global Change and Infectious Disease course in 2009, when the COE was established. “I wanted very much to contribute a course to what I saw as a real game-changer in Wesleyan’s interest in the environment. The course is about all the ways that human demands on the environment have brought us infectious diseases, over past millennia and in the present, and why our environmental disturbances will continue to bring us infections into the future.”
Over the years, Cohan learned that he can sustainably teach about 170 students every year without running out of interested students. This fall, he had 207. Although he didn’t change the overall structure of his course to accommodate COVID-19 topics, he did add material on the current pandemic to various sections of the course.
“I wouldn’t say that the population of the class increased tremendously as a result of COVID-19, but I think the enthusiasm of the students for the material has increased substantially,” he said.
To accommodate online learning, Cohan shaved off 15 minutes from his normal 80-minute lectures to allow for discussion sections, led by Cohan and teaching assistants. “While the lectures mostly dealt with biology, the discussions focused on how changes in behavior and policy can solve the infectious disease problems brought by human disturbance of the environment,” he said.
Based on student responses to an introspective exam question, Cohan learned that many students enjoyed a new hope that we could each contribute to fighting infectious disease. “They discovered that the solution to infectious disease is not entirely a waiting game for the right technologies to come along,” he said. “Many enjoyed learning about fighting infectious disease from a moral and social perspective. And especially, the students enjoyed learning about the ‘socialism of the microbe,’ how preventing and curing others’ infections will prevent others’ infections from becoming our own. The students enjoyed seeing how this idea can drive both domestic and international health policies.”
A sampling of the published student essays are below:
Alexander Giummo ’22 and Mike Dunderdale’s ’23 op-ed titled “ A National Testing Proposal: Let’s Fight Back Against COVID-19 ” was published in the Journal Inquirer in Manchester, Conn.
They wrote: “With an expansive and increased testing plan for U.S. citizens, those who are COVID-positive could limit the number of contacts they have, and this would also help to enable more effective contact tracing. Testing could also allow for the return of some ‘normal’ events, such as small social gatherings, sports, and in-person class and work schedules.
“We propose a national testing strategy in line with the one that has kept Wesleyan students safe this year. The plan would require a strong push by the federal government to fund the initiative, but it is vital to successful containment of the virus.
“Twice a week, all people living in the U.S. should report to a local testing site staffed with professionals where the anterior nasal swab Polymerase Chain Reaction (PCR) test, used by Wesleyan and supported by the Broad Institute, would be implemented.”
Kalyani Mohan ’22 and Kalli Jackson ’22 penned an essay titled “ Where Public Health Meets Politics: COVID-19 in the United States ,” which was published in Wesleyan’s Arcadia Political Review .
They wrote: “While the U.S. would certainly benefit from a strengthened pandemic response team and structural changes to public health systems, that alone isn’t enough, as American society is immensely stratified, socially and culturally. The politicization of the COVID-19 pandemic shows that individualism, libertarianism and capitalism are deeply ingrained in American culture, to the extent that Americans often blind to the fact community welfare can be equivalent to personal welfare. Pandemics are multifaceted, and preventing them requires not just a cultural shift but an emotional one amongst the American people, one guided by empathy—towards other people, different communities and the planet. Politics should be a tool, not a weapon against its people.”
Sydnee Goyer ’21 and Marcel Thompson’s ’22 essay “ This Flu Season Will Be Decisive in the Fight Against COVID-19 ” also was published in Arcadia Political Review .
“With winter approaching all around the Northern Hemisphere, people are preparing for what has already been named a “twindemic,” meaning the joint threat of the coronavirus and the seasonal flu,” they wrote. “While it is known that seasonal vaccinations reduce the risk of getting the flu by up to 60% and also reduce the severity of the illness after the contamination, additional research has been conducted in order to know whether or not flu shots could reduce the risk of people getting COVID-19. In addition to the flu shot, it is essential that people remain vigilant in maintaining proper social distancing, washing your hands thoroughly, and continuing to wear masks in public spaces.”
An op-ed titled “ The Pandemic Has Shown Us How Workplace Culture Needs to Change ,” written by Adam Hickey ’22 and George Fuss ’21, was published in Park City, Utah’s The Park Record .
They wrote: “One review of academic surveys (most of which were conducted in the United States) conducted in 2019 found that between 35% and 97% of respondents in those surveys reported having attended work while they were ill, often because of workplace culture or policy which generated pressure to do so. Choosing to ignore sickness and return to the workplace while one is ill puts colleagues at risk, regardless of the perceived severity of your own illness; COVID-19 is an overbearing reminder that a disease that may cause mild, even cold-like symptoms for some can still carry fatal consequences for others.
“A mandatory paid sick leave policy for every worker, ideally across the globe, would allow essential workers to return to work when necessary while still providing enough wiggle room for economically impoverished employees to take time off without going broke if they believe they’ve contracted an illness so as not to infect the rest of their workplace and the public at large.”

Women’s cross country team members and classmates Jane Hollander ’23 and Sara Greene ’23 wrote a sports-themed essay titled “ This Season, High School Winter Sports Aren’t Worth the Risk ,” which was published in Tap into Scotch Plains/Fanwood , based in Scotch Plains, N.J. Their essay focused on the risks high school sports pose on student-athletes, their families, and the greater community.
“We don’t propose cutting off sports entirely— rather, we need to be realistic about the levels at which athletes should be participating. There are ways to make practices safer,” they wrote. “At [Wesleyan], we began the season in ‘cohorts,’ so the amount of people exposed to one another would be smaller. For non-contact sports, social distancing can be easily implemented, and for others, teams can focus on drills, strength and conditioning workouts, and skill-building exercises. Racing sports such as swim and track can compete virtually, comparing times with other schools, and team sports can focus their competition on intra-team scrimmages. These changes can allow for the continuation of a sense of normalcy and team camaraderie without the exposure to students from different geographic areas in confined, indoor spaces.”
Brook Guiffre ’23 and Maddie Clarke’s ’22 op-ed titled “ On the Pandemic ” was published in Hometown Weekly, based in Medfield, Mass.
“The first case of COVID-19 in the United States was recorded on January 20th, 2020. For the next month and a half, the U.S. continued operating normally, while many other countries began their lockdown,” they wrote. “One month later, on February 29th, 2020, the federal government approved a national testing program, but it was too little too late. The U.S. was already in pandemic mode, and completely unprepared. Frontline workers lacked access to N-95 masks, infected patients struggled to get tested, and national leaders informed the public that COVID-19 was nothing more than the common flu. Ultimately, this unpreparedness led to thousands of avoidable deaths and long-term changes to daily life. With the risk of novel infectious diseases emerging in the future being high, it is imperative that the U.S. learn from its failure and better prepare for future pandemics now. By strengthening our public health response and re-establishing government organizations specialized in disease control, we have the ability to prevent more years spent masked and six feet apart.”
In addition, their other essay, “ On Mass Extinction ,” was also published by Hometown Weekly .
“The sixth mass extinction—which scientists have coined as the Holocene Extinction—is upon us. According to the United Nations, around one million plant and animal species are currently in danger of extinction, and many more within the next decade. While other extinctions have occurred in Earth’s history, none have occurred at such a rapid rate,” they wrote. “For the sake of both biodiversity and infectious diseases, it is in our best interest to stop pushing this Holocene Extinction further.”
An essay titled “ Learning from Our Mistakes: How to Protect Ourselves and Our Communities from Diseases ,” written by Nicole Veru ’21 and Zoe Darmon ’21, was published in My Hometown Bronxville, based in Bronxville, N.Y.
“We can protect ourselves and others from future infectious diseases by ensuring that we are vaccinated,” they wrote. “Vaccines have high levels of success if enough people get them. Due to vaccines, society is no longer ravaged by childhood diseases such as mumps, rubella, measles, and smallpox. We have been able to eradicate diseases through vaccines; smallpox, one of the world’s most consequential diseases, was eradicated from the world in the 1970s.
“In 2000, the U.S. was nearly free of measles, yet, due to hesitations by anti-vaxxers, there continues to be cases. From 2000–2015 there were over 18 measles outbreaks in the U.S. This is because unless a disease is completely eradicated, there will be a new generation susceptible.
“Although vaccines are not 100% effective at preventing infection, if we continue to get vaccinated, we protect ourselves and those around us. If enough people are vaccinated, societies can develop herd immunity. The amount of people vaccinated to obtain herd immunity depends on the disease, but if this fraction is obtained, the spread of disease is contained. Through herd immunity, we protect those who may not be able to get vaccinated, such as people who are immunocompromised and the tiny portion of people for whom the vaccine is not effective.”
Dhruvi Rana ’22 and Bryce Gillis ’22 co-authored an op-ed titled “ We Must Educate Those Who Remain Skeptical of the Dangers of COVID-19 ,” which was published in Rhode Island Central .
“As Rhode Island enters the winter season, temperatures are beginning to drop and many studies have demonstrated that colder weather and lower humidity are correlated with higher transmissibility of SARS-CoV-2, the virus that causes COVID-19,” they wrote. “By simply talking or breathing, we release respiratory droplets and aerosols (tiny fluid particles which could carry the coronavirus pathogen), which can remain in the air for minutes to hours.
“In order to establish herd immunity in the US, we must educate those who remain skeptical of the dangers of COVID-19. Whether community-driven or state-funded, educational campaigns are needed to ensure that everyone fully comprehends how severe COVID-19 is and the significance of airborne transmission. While we await a vaccine, it is necessary now more than ever that we social distance, avoid crowds, and wear masks, given that colder temperatures will likely yield increased transmission of the virus.”
Danielle Rinaldi ’21 and Verónica Matos Socorro ’21 published their op-ed titled “ Community Forum: How Mask-Wearing Demands a Cultural Reset ” in the Ewing Observer , based in Lawrence, N.J.
“In their own attempt to change personal behavior during the pandemic, Wesleyan University has mandated mask-wearing in almost every facet of campus life,” they wrote. “As members of our community, we must recognize that mask-wearing is something we are all responsible and accountable for, not only because it is a form of protection for us, but just as important for others as well. However, it seems as though both Covid fatigue and complacency are dominating the mindsets of Americans, leading to even more unwillingness to mask up. Ultimately, it is inevitable that this pandemic will not be the last in our lifespan due to global warming creating irreversible losses in biodiversity. As a result, it is imperative that we adopt the norm of mask-wearing now and undergo a culture shift of the abandonment of an individualistic mindset, and instead, create a society that prioritizes taking care of others for the benefit of all.”

Shayna Dollinger ’22 and Hayley Lipson ’21 wrote an essay titled “ My Pandemic Year in College Has Brought Pride and Purpose. ” Dollinger submitted the piece, rewritten in first person, to Jewish News of Northern California . Read more about Dollinger’s publication in this News @ Wesleyan article .
“I lay in the dead grass, a 6-by-6-foot square all to myself. I cheer for my best friend, who is on the stage constructed at the bottom of Foss hill, dancing with her Bollywood dance group. Masks cover their ordinarily smiling faces as their bodies move in sync. Looking around at friends and classmates, each in their own 6-by-6 world, I feel an overwhelming sense of normalcy.
“One of the ways in which Wesleyan has prevented outbreaks on campus is by holding safe, socially distanced events that students want to attend. By giving us places to be and things to do on the weekends, we are discouraged from breaking rules and causing outbreaks at ‘super-spreader’ events.”
An op-ed written by Luna Mac-Williams ’22 and Daëlle Coriolan ’24 titled “ Collectivist Practices to Combat COVID-19 ” was published in the Wesleyan Argus .
“We are embroiled in a global pandemic that disproportionately affects poor communities of color, and in the midst of a higher cultural consciousness of systemic inequities,” they wrote. “A cultural shift to center collectivist thought and action not only would prove helpful in disease prevention, but also belongs in conversation with the Black Lives Matter movement. Collectivist models of thinking effectively target the needs of vulnerable populations including the sick, the disenfranchised, the systematically marginalized. Collectivist systems provide care, decentering the capitalist, individualist system, and focusing on how communities can work to be self-sufficient and uplift our own neighbors.”
An essay written by Maria Noto ’21 , titled “ U.S. Individualism Has Deadly Consequences ,” is published in the Oneonta Daily Star , based in Oneonta, N.Y.
She wrote, “When analyzing the cultures of certain East Asian countries, several differences stand out. For instance, when people are sick and during the cold and flu season, many East Asian cultures, including South Korea, use mask-wearing. What is considered a threat to freedom by some Americans is a preventive action and community obligation in this example. This, along with many other cultural differences, is insightful in understanding their ability to contain the virus.
“These differences are deeply seeded in the values of a culture. However, there is hope for the U.S. and other individualistic cultures in recognizing and adopting these community-centered approaches. Our mindset needs to be revolutionized with the help of federal and local assistance: mandating masks, passing another stimulus package, contact tracing, etc… However, these measures will be unsuccessful unless everyone participates for the good of a community.”

A published op-ed by Madison Szabo ’23 , Caitlyn Ferrante ’23 ran in the Two Rivers Times . The piece is titled “ Anxiety and Aspiration: Analyzing the Politicization of the Pandemic .”
John Lee ’21 and Taylor Goodman-Leong ’21 have published their op-ed titled “ Reassessing the media’s approach to COVID-19 ” in Weekly Monday Cafe 24 (Page 2).
An essay by Eleanor Raab ’21 and Elizabeth Nefferdorf ’22 titled “ Preventing the Next Epidemic ” was published in The Almanac .
- Keep Wes Safe
- student publications
- Teaching during the pandemic
Related Articles
Gallery: Students Enjoy Spring Fling 2024 Festivities
Patricelli center awards funding to three new student ventures, wesleyan in the news: may 2024, previous matesan's new book explores political violence, islamist mobilization in egypt and indonesia, next students launch fun, interactive virtual program for school-aged kids.
- Find a Doctor
- Our Services
- More at NYP.org

Prevent COVID-19: How to Protect Yourself from the Coronavirus
Follow these simple precautions to reduce your chances of contracting covid-19..
Save this to read later.
The COVID-19 pandemic has been a part of our daily lives since March 2020, but with about 151,000 new cases a day in the United States, it remains as important as ever to stay vigilant and know how to protect yourself from coronavirus.
According to the Centers for Disease Control and Prevention (CDC) , “The best way to prevent illness is to avoid being exposed to this virus.” As the vaccines continue their roll out, here are the simple steps you can take to help prevent the spread of COVID-19 and protect yourself and others.
Know how it spreads
Scientists are still learning about COVID-19, the disease caused by the coronavirus, but according to the CDC, this highly contagious virus appears to be most commonly spread during close (within 6 feet) person-to-person contact through respiratory droplets.
“The means of transmission can be through respiratory droplets produced when a person coughs or sneezes, or by direct physical contact with an infected person, such as shaking hands,” says Dr. David Goldberg , an internist and infectious disease specialist at NewYork-Presbyterian Medical Group Westchester and an assistant professor of medicine at Columbia University Vagelos College of Physicians and Surgeons.
The CDC also notes that COVID-19 can spread by airborne transmission , although this is less common than close contact with a person. “Some infections can be spread by exposure to virus in small droplets and particles that can linger in the air for minutes to hours,” the CDC states. “These viruses may be able to infect people who are further than 6 feet away from the person who is infected or after that person has left the space. These transmissions occurred within enclosed spaces that had inadequate ventilation.”
Finally, it’s possible for coronavirus to spread through contaminated surfaces, but this is also less likely. According to the CDC, “Based on data from lab studies on COVID-19 and what we know about similar respiratory diseases, it may be possible that a person can get COVID-19 by touching a surface or object that has the virus on it and then touching their own mouth, nose, or possibly their eyes, but this isn’t thought to be the main way the virus spreads.”
Practice social distancing
Since close person-to-person contact appears to be the main source of transmission, social distancing remains a key way to mitigate spread. The CDC recommends maintaining a distance of approximately 6 feet from others in public places. This distance will help you avoid direct contact with respiratory droplets produced by coughing or sneezing.
In addition, studies have found that outdoor settings with enough space to distance and good ventilation will reduce risk of exposure. “There is up to 80% less transmission of the virus happening outdoors versus indoors,” says Dr. Ashwin Vasan , an assistant attending physician in the Department of Medicine at NewYork-Presbyterian/Columbia University Irving Medical Center and an assistant professor at the Mailman School of Public Health and Columbia University Vagelos College of Physicians and Surgeons. “One study found that of 318 outbreaks that accounted for 1,245 confirmed cases in China, only one outbreak occurred outdoors. That’s significant. I recommend spending time with others outside. We’re not talking about going to a sporting event or a concert. We’re talking about going for a walk or going to the park, or even having a conversation at a safe distance with someone outside.”
Wash your hands
Practicing good hygiene is an important habit that helps prevent the spread of COVID-19. Make these CDC recommendations part of your routine:
- Wash your hands often with soap and water for at least 20 seconds, especially after you have been in a public place, or after blowing your nose, coughing, or sneezing.
- Before eating or preparing food
- Before touching your face
- After using the restroom
- After leaving a public place
- After blowing your nose, coughing, or sneezing
- After handling your mask
- After changing a diaper
- After caring for someone who’s sick
- After touching animals or pets
- If soap and water are not readily available, use a hand sanitizer that contains at least 60% alcohol. Cover all surfaces of your hands with the sanitizer and rub them together until they feel dry.
- Avoid touching your eyes, nose, and mouth with unwashed hands.
Visit the CDC website for guidelines on how to properly wash your hands and use hand sanitizer . And see our video below on how soap kills the coronavirus. There’s plenty of science behind this basic habit. “Soap molecules disrupt the fatty layer or coat surrounding the virus, ” says Dr. Goldberg. “Once the viral coat is broken down, the virus is no longer able to function.”
In addition to hand-washing, disinfect frequently touched surfaces daily. This includes tables, doorknobs, light switches, countertops, handles, desks, phones, keyboards, toilets, faucets, and sinks.
Wear a mask
Face masks have become essential accessories in protecting yourself and others from contracting COVID-19. The CDC recommends that people wear face coverings in public settings, especially since studies have shown that individuals with the novel coronavirus could be asymptomatic or presymptomatic. (Face masks, however, do not replace social distancing recommendations.)
“Face masks are designed to provide a barrier between your airway and the outside world,” says Dr. Ole Vielemeyer , medical director of Weill Cornell ID Associates and Travel Medicine in the Division of Infectious Diseases at NewYork-Presbyterian/Weill Cornell Medical Center and Weill Cornell Medicine. “By wearing a mask that covers your mouth and nose, you will reduce the risk of serving as the source of disease spread by trapping your own droplets in the mask, and also reduce the risk of getting sick via droplets that contain the coronavirus by blocking access to your own airways.”

Restrict your travel
Traveling can increase the spread of COVID-19 and put you at risk for contracting the disease. The CDC recommends avoiding non-essential travel to many international destinations during the pandemic. It also advises people to weigh the risks when it comes to domestic travel: “Travel increases your chance of getting and spreading COVID-19,” states the CDC. “Staying home is the best way to protect yourself and others from COVID-19.”
“For people at risk for the complications of COVID-19, such as those with underlying medical conditions or those who are older, it’s prudent to avoid travel,” says Dr. Goldberg.
If you must travel, take safety measures, consider your mode of transportation, and stay up to date on the restrictions that are in place at your destination. Adhering to your state’s quarantine rules after traveling will help prevent the spread of COVID-19.
Watch for symptoms
The symptoms of infection for the coronavirus are often similar to those of other respiratory virus infections, such as influenza. Symptoms can include:
- Fever or chills
- Shortness of breath or difficulty breathing
- Muscle or body aches
- New loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
With the COVID-19 pandemic now coinciding with flu season, it’s important to recognize the differences in symptoms — as well as get a flu shot. “The medical community is concerned that if we have an increased number of influenza cases, it will strain the hospital system on top of what’s already going on with the COVID-19 pandemic,” says Dr. Ting Ting Wong , an attending physician and infectious disease specialist at NewYork-Presbyterian Brooklyn Methodist Hospital.
If you think you may have been exposed to a person with COVID-19 and have symptoms, call ahead to a doctor’s office to see if you can get tested. You can also use a virtual care platform, such as NewYork-Presbyterian’s NYP OnDemand, to meet with a healthcare professional by videoconference. Avoid contact with others and wear a face mask if you need to leave your home when you are sick.
How NewYork-Presbyterian is prepared
NewYork-Presbyterian continues to follow the situation closely and implement the recommendations provided by our local and state departments of health and the CDC. Our medical staff is trained to recognize patients who may have the virus and will help prevent COVID-19 from spreading.
We understand how important the support of loved ones and friends is to patients during their hospital stay. Stay up to date with NewYork-Presbyterian’s visitor guidelines . It’s our priority to keep patients and visitors safe from infection.
For more information on the evolving situation and how to protect yourself from coronavirus, visit the CDC and check NewYork-Presbyterian for more updates.
View all of our COVID-19 outbreak articles here .
Additional Resources
If you have concerns regarding COVID-19, please call NewYork-Presbyterian’s hotline at 646-697-4000. This hotline is available as a public service to provide information only and not diagnose, treat, or render a medical opinion.
If you are not feeling well, consider using NewYork-Presbyterian’s Virtual Urgent Care for non-life-threatening symptoms such as fever, cough, upset stomach, or nausea. Learn more by visiting nyp.org/urgentcare .
At a Glance
Featured experts.
Internal Medicine, Infectious Disease
Internal Medicine
Infectious Disease
Share This Story
Get the latest health and wellness news.
Keep in touch with NewYork-Presbyterian and subscribe to our newsletter.
- Privacy Notice

Get health information you can use, fact-checked by Nebraska Medicine experts.
How to fight COVID-19 at home

Critical care physician and pulmonologist Brian Boer, MD , has been treating COVID-19 patients since the beginning of the pandemic. Here he shares his expertise on fighting COVID-19 at home – some of it different from what's shared online.
How to rest
First, if you're fighting COVID-19 at home, you don't need to sleep in a certain position. "We know that sleeping on your stomach can improve your oxygenation if you need supplemental oxygen in the hospital. If you don't have severe COVID-19, lying on your stomach or side is not going to affect your disease," says Dr. Boer.
You should move around somewhat during the day, but you don't need to wake up every two hours to walk around. "Maintain your mobility, meaning don't lay on the couch all day, but that isn't specific to COVID-19," says Dr. Boer. "It's more to avoid blood clots and similar issues." Also, moving your arms around doesn't open up your lungs. "Just being mobile and active helps you take a deep breath," he says.
What to take and what to avoid
Maintain a healthy, well-balanced diet. Stay hydrated, especially if you're throwing up or have diarrhea.
No supplements or vitamins have shown any proven benefit for treating COVID-19. If you want to take a normal dose of a vitamin, that's fine. It won't hurt, but there's no evidence that it will help you recover from COVID-19 faster.
Treat your symptoms like you would for other infections, like the common cold. If you have a fever or muscle aches, you can take over-the-counter medications like acetaminophen, naproxen or ibuprofen.
Some drugs will do more harm than good, such as antibiotics. "Antibiotics, in general, do not help COVID-19," says Dr. Boer. Antibiotics combat bacteria, not viruses. So you're left with the side effects of the antibiotics while getting no benefit at all. "Hydroxychloroquine and its derivatives have also shown no benefit to treating COVID-19. A lot of the data shows that it could lead to cardiac events or other secondary outcomes."
When to seek care
The majority of people with COVID-19 have mild symptoms and can treat it at home. Seek medical attention if you have chest pain or shortness of breath .
It's essential to avoid spreading COVID-19 to others. Find out how to keep others safe if you test positive .
Related articles

Can zinc, oregano oil, vitamin C or D prevent or treat COVID-19?
Want to support your immune system? Better sleep on it

You asked, we answered: What to do if you test positive for COVID-19
In this article.
Browse our doctors or call 800.922.0000
- Link to share on Twitter
- Link to share on Facebook
- Share via email
Stay connected with the Nebraska Medicine app
Subscribe to advancing health.
By signing up, you are consenting to receive electronic messages from Nebraska Medicine.
Links you might like

How loneliness affects your health

Can medications like Ozempic® and Wegovy® decrease your stroke risk?

What should you look for in a multivitamin?
May 7, 2024
A Fight About Viruses in the Air Is Finally Over. Now It’s Time for Healthy Venting
WHO now admits the COVID virus and other germs spread “through the air.” This plain language may help improve research and action to fight disease
By Maggie Fox
Science Photo Library/Alamy Stock Photo
After four years of fighting about it, the World Health Organization has finally proclaimed that viruses, including the SARS-CoV-2 virus that causes COVID, can be spread through the air .
The operative phrase here is “through the air.” It’s plain language that anyone can understand, and this switch from jargon such as “airborne” and “aerosol” may finally clear the way for researchers to get funding to study better, real-life ways to protect people from a range of infectious diseases.
And just maybe governments, retailers, school authorities and others can now start to get solid information about ways they can clean indoor air. While it is going to take more than a wordy WHO statement to persuade gym owners that fogged-up windows mean too many people are huffing out potentially infectious air, the new wording does provide a better explanation of why it’s gross and unhealthy.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
It took four years to get here because some leaders in public health, medicine and science clung too tightly to precision and semantics . No one disputes that respiratory viruses are spread by droplets. The disagreements were over what sized droplets really counted as droplets, whether they hung in the air and how far they traveled. There were debates over the definition of “aerosol” and what sized droplet that meant. Some experts refused to say—or to let anyone else say—that a droplet could remain suspended in air or travel over a distance unless it was, technically, an aerosol. They said that meant it had to be five microns or less in size—a definition that itself did not have a basis in modern science.
One particular moment of shame came on March 28, 2020, when WHO tweeted : “FACT: #COVID19 is NOT airborne.”
So the initial guidance for people was that the virus was carried in droplets that fell to surfaces. It is transported that way, as are other viruses, and cleaning and disinfecting surfaces is useful in fighting a range of microbes.
But it’s not the only way they spread. In the battle over what “aerosol” and “airborne” meant, public health officials lost sight of what was right in front of them: people were catching COVID by breathing contaminated air.
“It’s terrible that it took them years,” José-Luis Jiménez , a chemistry professor and aerosol expert at the University of Colorado, said. “By the end of March 2020, a lot of scientists had contacted them. It’s not like they didn’t have access to the information,” added Jiménez, who has detailed the history of mainstream public health resistance to the idea of airborne spread.
WHO and other agencies such as the Centers for Disease Control and Prevention did come around eventually, and it’s now broadly agreed that, along with measles, smallpox and tuberculosis, other infectious diseases can linger in the air and spread across rooms. “The descriptor ‘through the air’ can be used in a general way to characterize an infectious disease where the main mode of transmission involves the pathogen travelling through or being suspended in the air,” WHO now says .
The agency also states: “These potentially infectious particles are carried by expired airflow, exit the infectious person’s mouth/nose through breathing, talking, singing, spitting, coughing or sneezing and enter the surrounding air. From this point, these particles are known as ‘infectious respiratory particles’ or IRPs.” There’s no definition of particle size and no cutoff for when these germy expectorations will end with a splat on the floor instead of making their way into someone else’s eyes, nose or mouth.
This should clear the way for funding more and better research on the transmission of infectious diseases—not just COVID, but influenza, respiratory syncytial virus (RSV) and viruses that cause the common cold. That, in turn, should give managers of schools, retailers, airports and other public spaces the information they need to help keep air and surfacers cleaner. Because if people understand the physics of disease transmission, they can find ways to safely keep schools, shops and restaurants open during outbreaks and epidemics with better practices in ventilation, air and surface cleaning and foot traffic control.
Cases of influenza, RSV and other respiratory infections plummeted during the height of the COVID pandemic . Researchers are still studying why, but closures of schools and restaurants, remote working, handwashing, distancing and mask use all played strong roles. Flu, RSV and other respiratory infections came roaring back in 2024 as people returned to offices, schools, restaurants and large gatherings, largely without masks.
Could restaurants with ultraviolet lights and fans in the ceilings offer safer spaces to eat out during flu season? Can schools stay open even during disease outbreaks with upgrades to HVAC systems and low-tech fixes like windows that actually open? Ananya Iyengar of the Johns Hopkins Center for Health Security and colleagues took a look at how one New York school kept infections down during the pandemic, for example, and found better ventilation improved indoor air quality . The cost? Along with a suite of other measures, about $880 per student per year.
Words matter. When people heard that COVID might spread on surfaces, they wasted time wiping down groceries. People who misunderstood airborne spread needlessly wore masks on outdoor walks and veered off sidewalks to avoid their neighbors. Stores spent countless dollars and employee-hours pasting “keep six feet apart” signs on the floor and routing one-way traffic through aisles in what was almost certainly a futile effort to limit disease spread.
Instead, an understanding of how viruses can drift out of an infected person’s nose or mouth and then transmit infections for more than four hours can encourage a teacher to air out a classroom in between classes or a bar owner to serve drinks on the patio instead of forcing customers to jam together inside.
Another potential benefit: clearing air of germs will also cleanse it of pollen, spores and other particles that cause allergies and worsen asthma. Better circulation can also help clear out potentially toxic chemical fumes and dust . Residents of Louisiana still remember the noxious formaldehyde found polluting trailers FEMA supplied to Hurricane Katrina survivors. Better ventilation standards for new homes could reassure homeowners that they are not only at less risk for catching something nasty from their school-aged children, but also potentially safer from off-gassing carpets and furniture or mold spores. If people had cleaner indoor air all year long, would that cut annual cases of flu, the common cold and even asthma and allergies?
There’s no guarantee a future administration won’t once again mix up the messaging, but there will be much less excuse for government officials telling Americans they do not need to wear masks , as then surgeon general Jerome Adams did in a February 2020 post on Twitter . It will take years if not decades to win back the trust lost by the conflicting advice, but at least now some understandable language is available to use.
The new federal health research agency, the Advanced Research Projects Agency for Health or ARPA-H, has launched an effort called BREATHE , short for Building Resilient Environments for Air and Total HEalth , that promises to fund studies aimed at improving indoor air in buildings. The agency is asking for ideas and bids for ways to clean up indoor air in the same way water treatment and sewer systems revolutionized public health a century ago. It’s a worthwhile area of study that deserves adequate funding.
“It’s now respectable to do this research,” Jiménez said. “People can get funding to do some research about indoor air and engineering systems. They are stepping into fields that they really wouldn’t work on before. So you see some encouraging changes.”
This is an opinion and analysis article, and the views expressed by the author or authors are not necessarily those of Scientific American.
Persuasive Essay Guide
Persuasive Essay About Covid19
How to Write a Persuasive Essay About Covid19 | Examples & Tips
11 min read

People also read
A Comprehensive Guide to Writing an Effective Persuasive Essay
200+ Persuasive Essay Topics to Help You Out
Learn How to Create a Persuasive Essay Outline
30+ Free Persuasive Essay Examples To Get You Started
Read Excellent Examples of Persuasive Essay About Gun Control
Crafting a Convincing Persuasive Essay About Abortion
Learn to Write Persuasive Essay About Business With Examples and Tips
Check Out 12 Persuasive Essay About Online Education Examples
Persuasive Essay About Smoking - Making a Powerful Argument with Examples
Are you looking to write a persuasive essay about the Covid-19 pandemic?
Writing a compelling and informative essay about this global crisis can be challenging. It requires researching the latest information, understanding the facts, and presenting your argument persuasively.
But don’t worry! with some guidance from experts, you’ll be able to write an effective and persuasive essay about Covid-19.
In this blog post, we’ll outline the basics of writing a persuasive essay . We’ll provide clear examples, helpful tips, and essential information for crafting your own persuasive piece on Covid-19.
Read on to get started on your essay.
- 1. Steps to Write a Persuasive Essay About Covid-19
- 2. Examples of Persuasive Essay About Covid19
- 3. Examples of Persuasive Essay About Covid-19 Vaccine
- 4. Examples of Persuasive Essay About Covid-19 Integration
- 5. Examples of Argumentative Essay About Covid 19
- 6. Examples of Persuasive Speeches About Covid-19
- 7. Tips to Write a Persuasive Essay About Covid-19
- 8. Common Topics for a Persuasive Essay on COVID-19
Steps to Write a Persuasive Essay About Covid-19
Here are the steps to help you write a persuasive essay on this topic, along with an example essay:
Step 1: Choose a Specific Thesis Statement
Your thesis statement should clearly state your position on a specific aspect of COVID-19. It should be debatable and clear. For example:
Step 2: Research and Gather Information
Collect reliable and up-to-date information from reputable sources to support your thesis statement. This may include statistics, expert opinions, and scientific studies. For instance:
- COVID-19 vaccination effectiveness data
- Information on vaccine mandates in different countries
- Expert statements from health organizations like the WHO or CDC
Step 3: Outline Your Essay
Create a clear and organized outline to structure your essay. A persuasive essay typically follows this structure:
- Introduction
- Background Information
- Body Paragraphs (with supporting evidence)
- Counterarguments (addressing opposing views)
Step 4: Write the Introduction
In the introduction, grab your reader's attention and present your thesis statement. For example:
Step 5: Provide Background Information
Offer context and background information to help your readers understand the issue better. For instance:
Step 6: Develop Body Paragraphs
Each body paragraph should present a single point or piece of evidence that supports your thesis statement. Use clear topic sentences, evidence, and analysis. Here's an example:
Step 7: Address Counterarguments
Acknowledge opposing viewpoints and refute them with strong counterarguments. This demonstrates that you've considered different perspectives. For example:
Step 8: Write the Conclusion
Summarize your main points and restate your thesis statement in the conclusion. End with a strong call to action or thought-provoking statement. For instance:
Step 9: Revise and Proofread
Edit your essay for clarity, coherence, grammar, and spelling errors. Ensure that your argument flows logically.
Step 10: Cite Your Sources
Include proper citations and a bibliography page to give credit to your sources.
Remember to adjust your approach and arguments based on your target audience and the specific angle you want to take in your persuasive essay about COVID-19.
Paper Due? Why Suffer? That's our Job!
Examples of Persuasive Essay About Covid19
When writing a persuasive essay about the Covid-19 pandemic, it’s important to consider how you want to present your argument. To help you get started, here are some example essays for you to read:
Check out some more PDF examples below:
Persuasive Essay About Covid-19 Pandemic
Sample Of Persuasive Essay About Covid-19
Persuasive Essay About Covid-19 In The Philippines - Example
If you're in search of a compelling persuasive essay on business, don't miss out on our “ persuasive essay about business ” blog!
Examples of Persuasive Essay About Covid-19 Vaccine
Covid19 vaccines are one of the ways to prevent the spread of Covid-19, but they have been a source of controversy. Different sides argue about the benefits or dangers of the new vaccines. Whatever your point of view is, writing a persuasive essay about it is a good way of organizing your thoughts and persuading others.
A persuasive essay about the Covid-19 vaccine could consider the benefits of getting vaccinated as well as the potential side effects.
Below are some examples of persuasive essays on getting vaccinated for Covid-19.
Covid19 Vaccine Persuasive Essay
Persuasive Essay on Covid Vaccines
Interested in thought-provoking discussions on abortion? Read our persuasive essay about abortion blog to eplore arguments!
Examples of Persuasive Essay About Covid-19 Integration
Covid19 has drastically changed the way people interact in schools, markets, and workplaces. In short, it has affected all aspects of life. However, people have started to learn to live with Covid19.
Writing a persuasive essay about it shouldn't be stressful. Read the sample essay below to get idea for your own essay about Covid19 integration.
Persuasive Essay About Working From Home During Covid19
Searching for the topic of Online Education? Our persuasive essay about online education is a must-read.
Examples of Argumentative Essay About Covid 19
Covid-19 has been an ever-evolving issue, with new developments and discoveries being made on a daily basis.
Writing an argumentative essay about such an issue is both interesting and challenging. It allows you to evaluate different aspects of the pandemic, as well as consider potential solutions.
Here are some examples of argumentative essays on Covid19.
Argumentative Essay About Covid19 Sample
Argumentative Essay About Covid19 With Introduction Body and Conclusion
Looking for a persuasive take on the topic of smoking? You'll find it all related arguments in out Persuasive Essay About Smoking blog!
Examples of Persuasive Speeches About Covid-19
Do you need to prepare a speech about Covid19 and need examples? We have them for you!
Persuasive speeches about Covid-19 can provide the audience with valuable insights on how to best handle the pandemic. They can be used to advocate for specific changes in policies or simply raise awareness about the virus.
Check out some examples of persuasive speeches on Covid-19:
Persuasive Speech About Covid-19 Example
Persuasive Speech About Vaccine For Covid-19
You can also read persuasive essay examples on other topics to master your persuasive techniques!
Tips to Write a Persuasive Essay About Covid-19
Writing a persuasive essay about COVID-19 requires a thoughtful approach to present your arguments effectively.
Here are some tips to help you craft a compelling persuasive essay on this topic:
Choose a Specific Angle
Start by narrowing down your focus. COVID-19 is a broad topic, so selecting a specific aspect or issue related to it will make your essay more persuasive and manageable. For example, you could focus on vaccination, public health measures, the economic impact, or misinformation.
Provide Credible Sources
Support your arguments with credible sources such as scientific studies, government reports, and reputable news outlets. Reliable sources enhance the credibility of your essay.
Use Persuasive Language
Employ persuasive techniques, such as ethos (establishing credibility), pathos (appealing to emotions), and logos (using logic and evidence). Use vivid examples and anecdotes to make your points relatable.
Organize Your Essay
Structure your essay involves creating a persuasive essay outline and establishing a logical flow from one point to the next. Each paragraph should focus on a single point, and transitions between paragraphs should be smooth and logical.
Emphasize Benefits
Highlight the benefits of your proposed actions or viewpoints. Explain how your suggestions can improve public health, safety, or well-being. Make it clear why your audience should support your position.
Use Visuals -H3
Incorporate graphs, charts, and statistics when applicable. Visual aids can reinforce your arguments and make complex data more accessible to your readers.
Call to Action
End your essay with a strong call to action. Encourage your readers to take a specific step or consider your viewpoint. Make it clear what you want them to do or think after reading your essay.
Revise and Edit
Proofread your essay for grammar, spelling, and clarity. Make sure your arguments are well-structured and that your writing flows smoothly.
Seek Feedback
Have someone else read your essay to get feedback. They may offer valuable insights and help you identify areas where your persuasive techniques can be improved.
Tough Essay Due? Hire Tough Writers!
Common Topics for a Persuasive Essay on COVID-19
Here are some persuasive essay topics on COVID-19:
- The Importance of Vaccination Mandates for COVID-19 Control
- Balancing Public Health and Personal Freedom During a Pandemic
- The Economic Impact of Lockdowns vs. Public Health Benefits
- The Role of Misinformation in Fueling Vaccine Hesitancy
- Remote Learning vs. In-Person Education: What's Best for Students?
- The Ethics of Vaccine Distribution: Prioritizing Vulnerable Populations
- The Mental Health Crisis Amidst the COVID-19 Pandemic
- The Long-Term Effects of COVID-19 on Healthcare Systems
- Global Cooperation vs. Vaccine Nationalism in Fighting the Pandemic
- The Future of Telemedicine: Expanding Healthcare Access Post-COVID-19
In search of more inspiring topics for your next persuasive essay? Our persuasive essay topics blog has plenty of ideas!
To sum it up,
You have read good sample essays and got some helpful tips. You now have the tools you needed to write a persuasive essay about Covid-19. So don't let the doubts stop you, start writing!
If you need professional writing help, don't worry! We've got that for you as well.
MyPerfectWords.com is a professional persuasive essay writing service that can help you craft an excellent persuasive essay on Covid-19. Our experienced essay writer will create a well-structured, insightful paper in no time!
So don't hesitate and place your ' write my essay online ' request today!
Frequently Asked Questions
Are there any ethical considerations when writing a persuasive essay about covid-19.
Yes, there are ethical considerations when writing a persuasive essay about COVID-19. It's essential to ensure the information is accurate, not contribute to misinformation, and be sensitive to the pandemic's impact on individuals and communities. Additionally, respecting diverse viewpoints and emphasizing public health benefits can promote ethical communication.
What impact does COVID-19 have on society?
The impact of COVID-19 on society is far-reaching. It has led to job and economic losses, an increase in stress and mental health disorders, and changes in education systems. It has also had a negative effect on social interactions, as people have been asked to limit their contact with others.

Write Essay Within 60 Seconds!

Caleb S. has been providing writing services for over five years and has a Masters degree from Oxford University. He is an expert in his craft and takes great pride in helping students achieve their academic goals. Caleb is a dedicated professional who always puts his clients first.

Paper Due? Why Suffer? That’s our Job!
Keep reading


Vitamin D: The New Weapon in the Fight Against COVID-19?
Vitamin D therapy has recently emerged as a new method of boosting the immune system. While vitamin D injections are going viral, it is important to consider whether it is safe for everyone to take them. Instead of blindly following the crowd because it’s said to be good or necessary, it’s crucial to do some research and determine the most suitable method of Vitamin D treatment based on your current health status. In particular, assessing whether injections are more effective is important.
Can It Also Prevent COVID-19?
Recent research from a team in Argentina showed that vitamin D supplementation could enhance the preventive effects of the COVID-19 vaccine. Researchers stated people with low vitamin D levels have a lower serum protection rate after flu vaccination than those with normal levels. They claimed that vitamin D supplementation can maximize the ability of the immune system to respond to the COVID-19 vaccine.
Oral Supplements VS. Injections
Vitamin D injections have the advantage of being efficient and convenient. If you’re diagnosed with a vitamin D deficiency in a test, you can also benefit from insurance. However, opinions are divided on whether injections or oral supplements are better. Injections cannot be administered to young children. In addition, according to some study results, injecting a high dose of 200,000 IU at once can interfere with enzymes, reducing the effect of vitamin D.
High-Dose Injections Can Cause Adverse Events
Vitamin D injections can cause adverse events by introducing a large dose at once. When you get an injection, vitamin D stays in the muscles and is slowly secreted into the blood over two to three months. The problem is that instead of consistent release, a significant amount is initially secreted, which could lead to adverse events from overdosing.
Read more: Hong Kong to Dazzle Visitors with Monthly Firework and Drone Shows
How to Avoid Vitamin D Deficiency?
Unlike other vitamins , vitamin D can be synthesized in the body. However, if the latitude is higher than 35 degrees, the sun’s ultraviolet rays do not reach the earth’s surface well in winter. Consequently, vitamin D is not sufficiently synthesized. It’s important to get a lot of sun in the spring, summer, and fall when the sun’s rays reach the ground well. On sunny days, it’s good to be outside at least three times a week.
Recommended to be Taken Through Food
To reach the daily recommended intake through food, it’s good to eat oily fish, such as mackerel, herring, salmon, and tuna, which are rich in vitamin D. Eggs, mushrooms, and milk also contain small amounts of vitamin D. If it’s hard to get enough from food, you can also take oral vitamin D supplements.
Editor's Pick
- 10 Foods You Should NEVER Mix with Medicine
- Feeling Tired This Spring? Here’s Why and What to Do About It
- The Surprising Health Benefits of Sleep
- Revolutionary Tech Predicts Atrial Fibrillation 30 Minutes in Advance
Excess is Better Than Deficiency
Even though vitamin D injections can cause adverse events, some people need to get them. Most oral vitamin D supplements contain calcium, which can upset your stomach when taken. If you have poor digestion or find it difficult to swallow pills due to aging, injections can be a good option. This is because problems caused by deficiency are more likely to occur than adverse events from excess.
How to Increase Natural Synthesis
To increase the natural synthesis of vitamin D, it’s good to expose your arms and legs to the sun for about 20 to 30 minutes a day. If that’s difficult, choosing oral supplements or injections as a secondary option is one method. However, if you’re someone who normally synthesizes enough vitamin D, additional intake can be harmful, so be careful.
How Sunlight Helps You Synthesize Vitamin D
It’s often said that it’s good to sunbathe to produce vitamin D. That’s because the ultraviolet rays from the sun help make vitamin D. Among the ultraviolet rays, UVB is used as the main component for synthesizing vitamin D. When the skin is exposed to UVB, 7D-hydrocholesterol in the skin converts into a vitamin D precursor. This then converts into vitamin D.
Vitamin D and Magnesium: A Dynamic Duo
The health benefits of vitamin D and magnesium are well known. Vitamin D, whether taken in tablet form or produced in the skin from sunlight, is in an inactive form. For vitamin D to perform its important functions, it must be activated through a two-step process. What’s needed for this two-step process is magnesium. Magnesium helps vitamin D bind to transport proteins to move through the blood and activates the receptors necessary for cells to use vitamin D. Conversely, vitamin D helps improve the absorption of magnesium in the intestines of people with low magnesium levels, helping it to be used more efficiently in the body.
Symptoms of Vitamin D Deficiency and Age-Specific Dosage
If you’re deficient in vitamin D, you may feel depressed and the quality of your sleep may decline. If the deficiency is severe, your bone density may decrease, increasing the risk of fractures. You may also experience symptoms of eye twitching. The daily recommended dosage of vitamin D for adults is 600-800 IU, while for the elderly it’s 800 IU. For children and adolescents, it’s about 400-600 IU. If a child is not regularly exposed to sunlight or doesn’t consume enough vitamin D through food, the recommended amount may increase slightly. Pregnant women with a vitamin D deficiency may have an increased risk of gestational diabetes and preeclampsia.
Unauthorized reproduction and redistribution are prohibited.
Most Viewed in ViewusGlobal
- Turning Over a New Leaf: Plant-Based Diets Help Alleviate Prostate Cancer Symptoms
- Unlocking the Power of Arachidonic Acid in Battling Bipolar Disorder
- Depression More Likely to Occur During Menopause Transition

Advertisement
Supported by
There’s a New Covid Variant. What Will That Mean for Spring and Summer?
Experts are closely watching KP.2, now the leading variant.
- Share full article

By Dani Blum
For most of this year, the JN.1 variant of the coronavirus accounted for an overwhelming majority of Covid cases . But now, an offshoot variant called KP.2 is taking off. The variant, which made up just one percent of cases in the United States in mid-March, now makes up over a quarter.
KP.2 belongs to a subset of Covid variants that scientists have cheekily nicknamed “FLiRT,” drawn from the letters in the names of their mutations. They are descendants of JN.1, and KP.2 is “very, very close” to JN.1, said Dr. David Ho, a virologist at Columbia University. But Dr. Ho has conducted early lab tests in cells that suggest that slight differences in KP.2’s spike protein might make it better at evading our immune defenses and slightly more infectious than JN.1.
While cases currently don’t appear to be on the rise, researchers and physicians are closely watching whether the variant will drive a summer surge.
“I don’t think anybody’s expecting things to change abruptly, necessarily,” said Dr. Marc Sala, co-director of the Northwestern Medicine Comprehensive Covid-19 Center in Chicago. But KP.2 will most likely “be our new norm,’” he said. Here’s what to know.
The current spread of Covid
Experts said it would take several weeks to see whether KP.2 might lead to a rise in Covid cases, and noted that we have only a limited understanding of how the virus is spreading. Since the public health emergency ended , there is less robust data available on cases, and doctors said fewer people were using Covid tests.
But what we do know is reassuring: Despite the shift in variants, data from the C.D.C. suggests there are only “minimal ” levels of the virus circulating in wastewater nationally, and emergency department visits and hospitalizations fell between early March and late April.
“I don’t want to say that we already know everything about KP.2,” said Dr. Ziyad Al-Aly, the chief of research and development at the Veterans Affairs St. Louis Healthcare System. “But at this time, I’m not seeing any major indications of anything ominous.”
Protection from vaccines and past infections
Experts said that even if you had JN.1, you may still get reinfected with KP.2 — particularly if it’s been several months or longer since your last bout of Covid.
KP.2 could infect even people who got the most updated vaccine, Dr. Ho said, since that shot targets XBB.1.5, a variant that is notably different from JN.1 and its descendants. An early version of a paper released in April by researchers in Japan suggested that KP.2 might be more adept than JN.1 at infecting people who received the most recent Covid vaccine. (The research has not yet been peer-reviewed or published.) A spokesperson for the C.D.C. said the agency was continuing to monitor how vaccines perform against KP.2.
Still, the shot does provide some protection, especially against severe disease, doctors said, as do previous infections. At this point, there isn’t reason to believe that KP.2 would cause more severe illness than other strains, the C.D.C. spokesperson said. But people who are 65 and older, pregnant or immunocompromised remain at higher risk of serious complications from Covid.
Those groups, in particular, may want to get the updated vaccine if they haven’t yet, said Dr. Peter Chin-Hong, an infectious disease specialist at the University of California, San Francisco. The C.D.C. has recommended t hat people 65 and older who already received one dose of the updated vaccine get an additional shot at least four months later.
“Even though it’s the lowest level of deaths and hospitalizations we’ve seen, I’m still taking care of sick people with Covid,” he said. “And they all have one unifying theme, which is that they’re older and they didn’t get the latest shot.”
The latest on symptoms and long Covid
Doctors said that the symptoms of both KP.2 and JN.1 — which now makes up around 16 percent of cases — are most likely similar to those seen with other variants . These include sore throat, runny nose, coughing, head and body aches, fever, congestion, fatigue and in severe cases, shortness of breath. Fewer people lose their sense of taste and smell now than did at the start of the pandemic, but some people will still experience those symptoms.
Dr. Chin-Hong said that patients were often surprised that diarrhea, nausea and vomiting could be Covid symptoms as well, and that they sometimes confused those issues as signs that they had norovirus .
For many people who’ve already had Covid, a reinfection is often as mild or milder than their first case. While new cases of long Covid are less common now than they were at the start of the pandemic, repeat infections do raise the risk of developing long Covid, said Fikadu Tafesse, a virologist at Oregon Health & Science University. But researchers are still trying to determine by how much — one of many issues scientists are trying to untangle as the pandemic continues to evolve.
“That’s the nature of the virus,” Dr. Tafesse said. “It keeps mutating.”
Dani Blum is a health reporter for The Times. More about Dani Blum

Featured News - Current News - Archived News - News Categories
Northwell Health deploying nurses to fight COVID-19 surge in Western New York
Gov. Kathy Hochul on Saturday announced Northwell Health , New York state's largest health system, has dispatched a team of skilled nurses to Western New York to answer the call for more medical personnel to help a region overburdened with a surge in COVID-19 cases.
The Northwell team of 16 clinical professionals and two team leads, which includes intensive care, emergency department and medical-surgical nurses, were deployed to Erie County Medical Center in Buffalo and the University of Rochester's Strong Memorial Hospital in Rochester.
The two-week mission comes as the entire state sees a rise in COVID-19 infections and hospitalizations.
"Fighting the winter surge requires a statewide team effort from partners across New York state," Hochul said. "I want to thank Northwell Health for answering the call to action and partnering with us to send a team of extraordinarily skilled nurses that will boost hospital capacity and help us bring the numbers down in Western New York."
Northwell employees nearly 19,000 nurses at its 22 hospitals and more than 800 outpatient facilities, including the team of nurses who volunteered for the mission to New York's latest COVID-19 hotspot. The health system will continue to track patient volume and staffing needs internally as it extends help elsewhere.
Acting State Health Commissioner Dr. Mary T. Bassett said, "As we approach the holidays, we'll need community-minded solutions and cooperation with partners like Northwell Health to respond to the rise in COVID-19. We are so much stronger when we work together, so we thank Northwell for sending staff support from downstate to Western New York. We have the tools – and resources – we need to prevent infection. Vaccination protects you and wearing a mask is how we protect each other."
President and CEO of Northwell Health Michael Dowling said, "We offered to send nurses there after hearing about a staffing crunch in the region and seeing COVID-19 cases peaking there. While COVID cases downstate have increased, they are nowhere near the burden currently faced by health systems elsewhere in New York. There's a natural collaboration among health care organizations. In this time of crisis, we have the ability to help and so will continue to do so. We remember when the pandemic hit us hardest and we were at our worst."
Thomas J. Quatroche Jr., Ph.D., president and CEO of Erie County Medical Center, said, "We are thankful to Gov. Hochul and Northwell Health for coordinating this effort to assist ECMC while we experience extremely high patient volumes and continue to address our staffing shortages. This is an example of how we can all collaborate to provide lifesaving patient care."
Northwell Chief Nursing Officer Maureen White, R.N., said, "New York City and Long Island were overrun with COVID cases in March 2020. It was an ordeal the frontline team at Northwell – and all New Yorkers – won't soon forget. Our nurses received a helping hand then from other health systems. We want to be mindful to pay it forward and provide assistance now as others face a renewed assault by the virus."
Buffalo Mayor Byron Brown said, "I thank Gov. Kathy Hochul and Northwell Health for dispatching medical professionals to assist Erie County Medical Center staff, as our region responds to this latest COVID-19 surge. On behalf of all of the residents of the City of Buffalo, I am grateful for the partnership and support from across New York state."
The University of Rochester and Intermountain Healthcare in Utah sent medical help to Northwell during the first coronavirus wave in 2020. Northwell reciprocated by aiding Intermountain during its surge and now gets the chance to repay the University of Rochester in its time of need. Northwell has also deployed medical teams to the Henry Ford System in Michigan during the pandemic, as well as Houston and Puerto Rico after hurricanes devastated those regions.
Hometown News

View All News
Follow Us On

Niagara Frontier Publications
1859 Whitehaven Road, Grand Island, NY 14072 Phone: 716-773-7676 Fax: 716-773-7190
Get an Email Update!
All materials appearing on this Web page and website © copyright 2024 Niagara Frontier Publications. No materials may be reproduced without the express written consent of Niagara Frontier Publications.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Springer Nature - PMC COVID-19 Collection

Understanding and combating COVID-19 using the biology and chemistry of SARS-CoV-2
Mohammad mansoob khan.
1 Chemical Sciences, Faculty of Science, Universiti Brunei Darussalam, Jalan Tungku Link, Gadong, 1410 BE Brunei Darussalam
Yea-Wen Goh
Norhayati ahmad.
2 Environmental and Life Sciences, Faculty of Science, Universiti Brunei Darussalam, Jalan Tungku Link, Gadong, 1410 BE Brunei Darussalam
3 Institute for Biodiversity and Environmental Research, Universiti Brunei Darussalam, Jalan Tunku Link, Gadong, 1410 BE Brunei Darussalam
Monowarul Mobin Siddique
The coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Symptoms of COVID-19 can range from asymptomatic to severe, which could lead to fatality. Like other pathogenic viruses, the infection of SARS-CoV-2 relies on binding its spike glycoprotein to the host receptor angiotensin-converting enzyme 2 (ACE 2). Molecular studies suggested that there is a high affinity between the spike glycoprotein and ACE 2 that might arise due to their hydrophobic interaction. This property is mainly responsible for making this virus highly infectious. Apart from this, the transmissibility of the virus, prolonged viability in certain circumstances, and rapid mutations also contributed to the current pandemic situation. Nanotechnology provides potential alternative solutions to combat COVID-19 with the development of i. nanomaterial-based COVID-19 detection technology, ii. nanomaterial-based disinfectants, iii. nanoparticle-based vaccines, and iv. nanoparticle-based drug delivery. Hence, this review provides diverse insight into understanding COVID-19.
Introduction
Coronaviruses (CoVs) belong to the family Coronaviridae in the order of Nidovirales, which are positive-sensed single-stranded RNA viruses (+ ssRNA) surrounded by an envelope [ 1 – 4 ]. The name “Corona” stands for ‘crown’ in Latin, given due to the distinctive crown-like appearance of their spike proteins, which allow the virus to interact with the host cell receptors, a key step necessary to penetrate the host cell surface. This group of viruses is sub-divided based on the difference in the protein sequence into four genera: Alphacoronavirus, Betacoronavirus, Gammacoronavirus, and Deltacoronavirus (Fig. 1 ) [ 3 – 6 ].

Classification of human coronaviruses, SARS-CoV, MERS-CoV, and SARS-CoV-2
Alpha- and Betacoronaviruses are known to infect humans that include seven types of coronaviruses: i. HCoV-229E, ii. HCoV-NL63, iii. HCoV-OC43, iv. HCoV-HKU1, v. SARS-CoV, vi. MERS-CoV, and vii. SARS-CoV-2 [ 3 , 4 , 7 ]. HCoV stands for human coronavirus where HCoV-229E and HCoV-NL63 are alpha-CoVs while HCoV-OC43 and HCoV-HKU1 are beta-CoVs. These human coronaviruses usually cause mild symptoms such as the common cold (or acute rhinitis) or gastrointestinal infection, which causes diarrhea [ 3 ]. In contrast, SARS-CoV, MERS-CoV, and SARS-CoV-2, which are beta-CoVs, are highly transmittable and pathogenic, causing a higher chance for patients to develop severe acute respiratory infections like pneumonia [ 3 ]. According to epidemiological data, SARS-CoV and MERS-CoV are zoonotic pathogens that can be transmitted between animals and humans during close interaction [ 3 , 6 ]. In 2002, the severe acute respiratory syndrome (SARS) outbreak caused by SARS-CoV in Guangdong Province of China was identified to be transmitted from bats to humans via civet cats as the intermediate host [ 8 ]. A decade later in 2012, the Middle East respiratory syndrome (MERS) outbreak caused by MERS-CoV from Saudi Arabia was investigated to be from camels to humans [ 3 , 6 ].
In December 2019, Wuhan, the capital of Hubei Province of China, experienced an outbreak of unidentified pneumonia disease associated with a novel coronavirus (nCoV) [ 4 ]. The term nCoV is a provisional name given to the new strain of coronavirus, which has not previously been identified in humans. This new strain of the virus was initially referred to as 2019-nCoV before it was named severe acute respiratory syndrome coronavirus 2 (SAR-CoV-2) by the International Committee on Taxonomy of Viruses (ICTV) [ 1 , 6 ]. This name was chosen because the virus is genetically related to SAR-CoV which caused the SARS outbreak back in 2002. On the 11th of February 2020, the name of the disease caused by SAR-CoV-2 was announced as coronavirus disease 2019 (COVID-19) by the World Health Organization (WHO). The World Health Organization (WHO) then declared the coronavirus disease 2019 (COVID-19) outbreak a pandemic on the 11th March 2020. Coming from the beta-CoV genus, SAR-CoV-2, the seventh strain of human coronavirus, is the third zoonotic CoV after SARS-CoV and MERS-CoV [ 1 , 8 ]. The source of COVID-19, however, is still actively being investigated, although initial studies have shown that the CoVs found in bats and pangolins are highly related to SAR-CoV-2 [ 8 ]. This is because neither of the CoVs found in these mammals is sufficiently genetically similar to serve as its direct reservoir [ 8 ].
According to WHO, as of 1st July 2022, there have been more than 545 million confirmed COVID-19 cases, including more than 6 million deaths. Previously, there were four SARS-CoV-2 variants of concern (VOC) which are i. Alpha (B.1.1.7), ii. Beta (B.1.351), iii. Gamma (P.1), and iv. Delta (B.1.617.2) (Table (Table1). 1 ). However, on 26th November 2021, WHO classified a new variant of concern which was first reported by scientists in South Africa, known as the Omicron variant (B.1.1.529). Subsequently, Omicron is currently the dominant variant circulating globally. These are caused by mutations, especially in the spike protein receptor-binding domain (RBD) that enhances viral replication in the upper respiratory tract and in vivo transmission [ 9 ]. It was reported that Omicron possesses the most mutation sites and the mutations in its spike protein were approximately three to four times greater than the four previously circulating VOCs [ 10 , 11 ]. Weng et al . reported that the Omicron variant had 50 consensus mutations, while Alpha, Beta, Gamma, and Delta had 22, 18, 23, and 29 mutations, respectively [ 11 , 12 ]. These mutations have also shown increased infectivity and antibody resistance [ 13 ]. In addition, variants that were previously classified as variants of interest (VOI) include i. Epsilon (B.1.427 and B.1.429), ii. Zeta (P.2), iii. Eta (B.1.525), iv. Theta (P.3), v. Iota (B.1.526), vi. Kappa (B.1.617.1), vii. Lambda (C.37), and viii. Mu (B.1.621) (Table (Table1 1 ).
Classification of SARS-CoV-2 variants as of 7th June 2022 by the World Health Organization [ 14 ]
The current estimated incubation period for SARS-CoV-2 is 5–6 days [ 15 ] or even shorter for the Omicron variant [ 16 ]. However, it can also take up to 14 days for an infected individual to develop symptoms [ 15 ]. Symptoms of COVID-19 can range from asymptomatic to severe (acute respiratory infections and intestinal infections), which could lead to fatality. However, the most common symptoms reported are i. fever, ii. fatigue, iii. dry cough, iv. loss of smell or taste, and v. sore throat [ 17 ]. Researchers have found that pre-existing health conditions such as high blood pressure, obesity, and diabetes in patients can enhance the severity of the disease and susceptibility to infection. Furthermore, post-COVID-19 symptoms or long COVID was also reported by a significant number of patients who have recovered from COVID-19 infection [ 17 , 18 ]. These are symptoms such as i. fatigue, ii. shortness of breath, and iii. cognitive dysfunction (e.g., lack of mental focus and clarity, confusion, and forgetfulness) which persist for more than 12 weeks from initial symptoms [ 17 , 18 ].
Different areas of chemistry and biology play a key role in understanding everything from the structure and pathogenesis of SARS-CoV-2 to preventive measures and treatment for COVID-19. Biochemistry, for instance, helps us understand the structure of SARS-CoV-2, its viral proteins, viral genome, and pathogenic mechanisms [ 19 ]. On the other hand, organic and pharmaceutical chemistry plays a crucial role in identifying potential antiviral drugs, synthesizing antiviral compounds, and developing effective antiviral drugs against COVID-19 [ 19 ]. Furthermore, biomaterial chemistry and nanotechnology aid in the research and development of better diagnosis, preventive measures, and drug delivery system using nanomaterials for the prevention and treatment of COVID-19 [ 19 , 20 ]. The efficiency of drug delivery, for instance, can be improved with the different types of nanostructures which include i. metallic nanoparticles, ii. liposomes, iii. fullerenes, iv. graphene, v. carbon nanoparticles, and vi. polymeric nanoparticles [ 20 ].
Structure of SARS-CoV-2
Biochemistry plays a crucial role in understanding the structure of SARS-CoV-2. The structure of SARS-CoV-2 consists of i. a positive-sensed single-stranded RNA genome (+ ssRNA), ii. a lipid-bilayer viral membrane, iii. nucleocapsid (N) proteins, iv. membrane (M) proteins, v. spike (S) glycoproteins, and vi. envelope (E) proteins (Fig. 2 ) [ 19 , 21 ]. The single-stranded RNA genome is composed of 30,000 nucleotides which encode for four structural proteins (N protein, M protein, E protein, and S glycoprotein) and non-structural proteins (NsPs) such as 3-chymotrypsin-like protease (3CL pro ), papain-like protease (PL pro ), helicase (H), and RNA-dependent RNA polymerase (RdRp) [ 2 , 5 , 19 ]. N protein functions to encapsulate and protect the single-stranded RNA genome. M protein supports the viral assembly and is responsible for the shape of the viral membrane. In contrast, E protein has a crucial role in virus assembly, envelope formation, host cell membrane permeability and virulence [ 5 , 19 ]. The S glycoprotein comprises an S1 and S2 subunit in each spike monomer which is responsible for binding to the host cell receptor and fusion of the viral and cellular membranes, respectively [ 22 – 24 ]. Therefore, the S1 subunit which recognizes the protein receptor is called the receptor-binding domain (RBD) [ 19 ]. Furthermore, S protein is the main antigen component in all structural proteins that interact with the host cell receptors angiotensin-converting enzyme 2 (ACE 2) [ 22 – 24 ]. ACE 2 is a zinc-dependent metalloenzyme present in the lungs (type II alveoli cells), gastrointestinal (GI) tract, kidneys, and blood vessels [ 25 ]. This may suggest that enhanced binding between S protein of SARS-CoV-2 and ACE 2 may be responsible for increased disease severity (respiratory infection or GI infection) and high transmission rate of COVID-19.

Schematic drawing of the SARS-CoV-2 structure showing the single-stranded RNA genome (ssRNA), nucleocapsid (N) protein, membrane (M) protein, envelope (E) protein, spike (S) protein, and lipid-bilayer viral membrane
Mechanism of SARS-CoV-2 pathogenesis
As illustrated in Fig. 3 , the S1 subunit of the spike (S) protein of SARS-CoV-2 mediates binding to the receptors’ angiotensin-converting enzyme 2 (ACE 2) to enter the host cell [ 22 – 24 ]. The transmembrane serine protease TMPRSS2 then releases the S2 subunit of the S protein to fuse SARS-CoV-2 with the host cellular membrane [ 21 , 26 ]. After the entry into the host cell (endocytosis), the viral positive-sense single-stranded RNA (+ ssRNA) is released into the cytosol, where ribosomes translate it into two large polypeptides known as pp1a and pp1ab [ 2 , 19 , 27 ]. These two large polypeptides are then transformed into mature non-structural proteins (NsPs) such as RNA-dependent RNA polymerase (RdRp) and structural viral proteins (S, M, N, and E proteins) by two viral proteases: i. 3-chymotrypsin-like cysteine protease (3CL pro ) which is the main protease and ii. papain-like protease (PL pro ) [ 19 , 21 ]. RdRp mediates RNA replication, which causes multiple copies of the genome to be produced. Hence, more SARS-CoV-2 is generated as NsPs and the replicated viral genome self-assembles. Lastly, these synthesized virions are then secreted out (by exocytosis) from the infected cell, infecting other host cells.

Molecular interaction between SARS-CoV-2 and ACE2 receptor
Physical forces like i. hydrophobic effect, ii. electrostatic forces, iii. van der Waals forces, iv. hydrogen bonding, v. ionic bonding, and vi. entropy plays a crucial role in understanding protein–protein interactions. The binding interactions between the S protein of SARS-CoV-2 and ACE 2 receptor can be studied by using molecular dynamics (MD) simulations, which is a computer simulation method to analyze the physical movements of atoms and molecules, and the Monte Carlo (MC) sampling approach. Research by Li et al . has found that hydrogen bond pairing does not dominate the interaction between SARS-CoV-2 and ACE 2, as only several hydrogen bonds were identified [ 28 ]. However, simulation results of the hydration layer by using the MD method showed the existence of a large area of hydrophobic surfaces on SARS-CoV-2 RBD and ACE 2 [ 28 ]. This result suggests that the high affinity between SARS-CoV-2 and ACE 2 may be due to the hydrophobic effect among the hydrophobic surface areas of these two proteins at the binding site. Furthermore, a study by a group of computational chemists led by Amin showed that ACE 2 exhibited a negative electrostatic potential at the RBD, while SARS-CoV-2 showed positive electrostatic potential. This study has also found that mutations in the S protein of SAR-CoV-2 cause enhanced affinity toward ACE 2 due to the increase in electrostatic interactions [ 19 , 22 , 29 ].
Transmission routes of SARS-CoV-2
The transmission of SARS-CoV-2 can be spread through three major routes: i. droplet transmission, ii. aerosol transmission, and iii. contact transmission [ 5 , 30 ]. Droplet transmission is the spread caused by respiratory water droplets carrying the virus via coughing and sneezing. Similarly, aerosol transmission spreads fine, infectious respiratory water droplet nuclei that sustain in the air and can be inhaled directly into the lower respiratory tract. On the other hand, contact transmission can be either direct (direct contact with an infected person) or indirect (contact with virus-contaminated surfaces). Door knobs, handrails, and lift buttons, for instance, are common virus-contaminated surfaces that may cause indirect contact transmission. Adsorption of SARS-CoV-2 to these surfaces can be further facilitated by van der Waals and electrostatic attractions [ 31 ].
Persistence and viability of SARS-CoV-2 on different surfaces
Enveloped viruses such as SARS-CoV-2 can survive on inanimate surfaces. The quantity of adsorbed viruses is influenced by surface charge, size, stability, and steric conformation of the virus’s outer surface proteins. Moreover, the persistence and viability of SARS-CoV-2 differ with the characteristics of the inanimate surfaces, surface proteins, and environmental conditions such as relative humidity, pH, and temperature [ 5 , 31 ]. Studies have shown that SARS-CoV-2 has longer viability on plastics, glass, metals (stainless steel and zinc), latex, paper, and cardboard pieces [ 5 , 31 , 32 ]. Regarding this, Chin et al . reported that at 22 °C and 65% relative humidity, SARS-CoV-2 retained its infectivity for 4 days on plastics and stainless steel [ 33 ]. However, under the same temperature and relative humidity, SARS-CoV-2 retained its infectivity on paper for only 30 min (Table (Table2) 2 ) [ 33 ]. On the other hand, SARS-CoV-2 could also have different survivability on a single surface at different temperatures and relative humidity. Research by Biryukov et al . observed that SARS-CoV-2 decayed more rapidly when temperature and relative humidity increased, and the type of inanimate surface did not impact the decay rate [ 32 ].
Persistence and time for complete inactivation of SARS-CoV-2 on different surfaces at 22 °C and 65% relative humidity [ 33 ]
Diagnostic testing for SARS-CoV-2
Detection of SARS-CoV-2 is part of a necessary process to reduce community spread, especially by identifying asymptomatic infected individuals to be isolated. The types of specimens to be collected for SARS-CoV-2 diagnostic testing are i. upper respiratory specimen (e.g., nasopharyngeal or oropharyngeal), ii. lower respiratory specimen (e.g., sputum or lavage), iii. rectal swabs, or iv. blood (including serum and plasma). According to WHO and the Centers for Disease Control and Prevention (CDC) guidelines, a nasopharyngeal swab (upper respiratory specimen) is the preferred specimen required for detecting SARS-CoV-2 [ 34 ]. However, saliva is also an alternative specimen that has been considered for SARS-CoV-2 detection [ 34 ]. Nasopharyngeal specimen is the mucous secretion collected by cotton swab from the nasopharynx. Upon collection, the swab is placed immediately into a sterile tube containing a viral transport medium. Currently, there are several types of diagnostic testing methods, which include i. nucleic acid amplification test (NAAT) such as real-time reverse transcription-polymerase chain reaction (RT-PCR), ii. rapid antigen tests (RATs), and iii. SARS-CoV-2 antibody tests [ 21 , 34 ].
Reverse transcription-polymerase chain reaction
Reverse transcription-polymerase chain reaction (RT-PCR) is a type of nucleic acid amplification test (NAAT) that amplifies viral nucleic acids until they are at detectable levels. Hence, it is the most reliable and standard diagnostic method for SARS-CoV-2 due to its high sensitivity, specificity, and accuracy. However, RT-PCR testing is time-consuming and requires expensive laboratory instruments, reagents, and skilled laboratory personnel [ 34 ]. In addition, this technique detects the presence of SARS-CoV-2 nucleic acids based on specific genes such as S, E, N, and RdRP genes in specimens of the infected individual [ 35 , 36 ]. RT-PCR involves five steps which include i. specimen collection, ii. sample storage at 2–8 °C, iii. RNA extraction and purification using silica or magnetic particle-based methods, iv. reverse transcription of the viral RNA to a single-stranded complementary DNA (cDNA) using reverse transcriptase enzyme, and v. real-time detection of the fluorescent signals during the amplification of the specific genes of gene fragments [ 34 , 35 ].
Rapid antigen test
Rapid antigen test (RATs), detects the presence of viral proteins (antigens) expressed by SARS-CoV-2 in nasopharyngeal or oropharyngeal specimens of the infected individual [ 35 ]. The technology for RATs is similar to that of a pregnancy test, as the presence of these antigens will be shown by a fluorescent or colored band on the test strip (Fig. 4 ) [ 34 ]. Since it is a cheap and rapid technique, this diagnostic method is currently available as at-home test kits. However, this method produces a higher rate of false negative results, as it can only detect antigens (viral protein) if the virus is actively replicating [ 35 ].

Rapid antigen test kit showing negative and positive signs
Antibody test
On the other hand, an antibody test which is a serology test is a method to test for past infections. It is an indirect test in detecting SARS-CoV-2, as this technique detects the antibodies produced specifically in response to fight with SARS-CoV-2. This is a quick method to detect the presence of SARS-CoV-2 antibodies, but this cannot confirm the active infection status of an individual.
Preventive measures
Prevention of infection is a major strategy to slow down the spread of COVID-19. Interventions such as social distancing, personal protective equipment (PPE), and chemical sanitizations are examples of COVID-19 preventive measures. PPE is a garment or equipment that protects the user against any health or safety risk. The most commonly used PPE for respiratory and body protection during the pandemic includes masks or respirators, gloves, gown/aprons, goggles, and face shields [ 37 ]. However, the choice of PPE and level of protection for the general public and health-care workers during this COVID-19 pandemic is based on the risk of exposure. On the other hand, usage of soap water, hand sanitizers, and disinfecting inanimate surfaces with chemicals (e.g., bleach and hydrogen peroxide) are examples of chemical inactivation and preventive measures.
Face masks cover the users’ nose and mouth, which act as physical barriers that prevent respiratory droplets transmission. It protects a healthy person from getting infected and also prevents onward transmission by an infected person. Therefore, the usage of face masks has become a worldwide health-care necessity during this COVID-19 pandemic. Masks are divided into three categories which include i. fabric face masks, ii. medical or surgical masks, and iii. respirators. Polymers such as polypropylene (PP), polyethylene, polyesters, polyamides, polycarbonates, and polyphenylene oxide are usually used for fibers in medical masks and medical respirators due to their hydrophobic and nonabsorbent properties [ 38 ]. Furthermore, WHO has developed specific guidelines and strategies on infection prevention and control (IPC). According to WHO, medical masks are recommended for health-care workers in clinical settings, people with mild symptoms (e.g., fatigue, slight cough, and sore throat), people with chronic health conditions (e.g., obesity, diabetes, cancer, chronic respiratory disease, and cardiovascular disease), patients with suspected or confirmed COVID-19, and home caregivers for suspected or confirmed COVID-19 patients. On the other hand, non-medical or fabric masks can be used by the general public under the age of 60 years with no health conditions. In general, face masks should possess five characteristics: i. particulate filtration efficiency (PFE), ii. bacterial filtration efficiency (BFE), iii. fluid resistance, iv. differential pressure, and v. flammability [ 30 ]. In addition, the four main characteristics which determine the mask performance are i. filtration, ii. breathability, iii. fit, and iv. performance under different environmental conditions [ 39 ].
A medical/surgical mask is most widely and commonly used by health-care workers and the general public. Medical/surgical masks are fluid-resistant disposable masks that can filter particles of size 0.04–1.3 μm [ 40 ]. It covers the nose and mouth of the user, but is not designed to seal tightly against the user’s face [ 30 , 37 , 41 ]. As a result, they are not able to completely protect the user against airborne infectious agents such as coronavirus. Surgical masks usually consist of either three layers (3-ply) or four layers (4-ply). A three-ply surgical mask consists of three layers: i. an exterior hydrophobic layer, ii. a central filter layer, and iii. internal tender moisture-absorbing layer [ 41 ]. The function of the first layer is to repel water droplets; the second layer filters out germs and aerosols, while the third layer absorbs moisture from the user. A four-ply surgical mask is similar to a three-ply surgical mask, but with an additional central filtering layer or activated carbon filter [ 41 ]. In addition, the most commonly used material to make these medical masks is non-woven polypropylene (PP) as it is hydrophobic, nontoxic, breathable, inexpensive, provides filtration, and does not absorb humidity [ 30 , 38 ]. Furthermore, its filtering mechanism is based on Brownian diffusion, entrapment, inertial collision, gravity sedimentation, and electrostatic adsorption [ 42 ].
Respirators, which are also known as filtering facepiece respirators (FFR), seal tightly against the user’s face and are capable of protecting the user from infectious agents [ 41 ]. Surgical N95 respirators, for instance, is the most widely used surgical respirators, especially by health-care workers. It is a CDC/National Institute for Occupational Safety and Health (NIOSH)-certified disposable half-mask filtering facepiece respirator that has 95% or above filtering efficiency for particle size of about 0.3 μm [ 38 , 40 ]. Furthermore, it is effective in filtering non-oily particles such as coronaviruses as “N” means that the respirator is not resistant to oil [ 41 ]. It compises four layers which include i. a hydrophobic non-woven polypropylene (PP) outer later, ii. two layers of melt-blown non-woven PP, iii. a modacrylic support layer, and iv. a hydrophobic non-woven PP (Fig. 5 ) [ 30 , 38 ]. The filter layers operate on four principles, which are i. inertial impaction, ii. interception, iii. diffusion, and iv. electrostatic attraction [ 30 ].

Four layers of an N95 mask
Chemicals used for prevention of SARS-CoV-2
Usage of soap which is a surfactant is an effective way of killing SARS-CoV-2. Surfactant (surface-active agents) molecules are sodium salt with a long chain of fatty acids known as amphiphile [ 19 ]. Amphiphile consists of two parts: i. fat-like long-chain tail, which is hydrophobic, and ii. a COO − Na + head, which is hydrophilic or lyophobic. Due to hydrophobic interactions, when soap is dissolved in water, the molecules would arrange in such a way as to form micelles (Fig. 6 a) [ 19 ]. As the lipophilic tails are oriented inward, any dirt on our skin will be trapped to be rinsed away along with water. As shown in Fig. 6 b, the lipid-bilayer membrane of SARS-CoV-2 is structurally similar to amphiphiles found on surfactant molecules. The connection of lipids in the viral membrane is the weakest connection due to the structure of the virus being self-assembled [ 19 ]. Hence, some surfactant molecules will compete with the lipids and attach to the viral membrane. This is done by bonding its hydrophilic head with water, while its lipophilic tail bonds to the lipid resulting in push–pull interactions that eventually break the viral membrane [ 19 ]. As SARS-CoV-2 structurally falls apart, the fragments of the virus get trapped in the micelle and get washed away with water. Furthermore, WHO guidelines recommend frequent hand washing with soap and water for at least 20 s to effectively prevent the disease [ 43 ].

a Hydrophobic tails of amphiphile faces inward to form micelle which traps dirt and b structure of amphiphile and lipid on the lipid-bilayer membrane of SARS-CoV-2
Alcohol-based hand sanitizers
In addition to soap and water, the usage of rubbing alcohol or alcohol-based hand sanitizer is also an effective alternative way to kill SARS-CoV-2 when soap water is inaccessible. The components of alcohol-based hand sanitizers are i. alcohol (ethyl alcohol or isopropanol), ii. water, iii. glycerol, and iv. hydrogen peroxide. Among the four components, alcohol plays a crucial role in destroying SARS-CoV-2. In a recent study, two standardized World Health Organization formulae are known as WHO formulation 1, which consists of 85% ethanol, and WHO formulation 2, which consists of 75% isopropanol, were proven to be efficient in inactivating SARS-CoV-2 [ 44 – 46 ]. This is because enveloped viruses like SARS-CoV-2 are highly sensitive toward these alcohols, as they can dissolve the lipid molecules of the viral membrane which inactivates the virus as its structure collapses (Fig. 7 ) [ 19 , 43 , 44 , 47 ]. Alcohols are also amphiphilic compounds similar to lipid molecules. Therefore, they possess both hydrophilic and hydrophobic (or lipophilic) properties, allowing them to enter through the lipid-bilayer viral envelope, which leads to alteration in its fluidity. This is because the presence of polar oxygen atoms from alcohols increases the internal affinity of the membrane for water [ 43 ]. Thus, its protein structures are also destabilized and denatured, causing the virus to lose its biological activities and hence inactivated [ 19 , 43 ].

Antiviral action and mechanism of alcohol against enveloped viruses like SARS-CoV-2 [ 43 ]
Vaccines against COVID-19
Seven different classes of vaccines developed against SARS-CoV-2, which are i. messenger RNA (mRNA), ii. DNA, iii. inactivated viruses, iv. viral vector (non-replicating and replicating), v. protein subunit, vi. viral-like particles, and, vii. live attenuated [ 48 , 49 ]. Currently, there are different types of authorized vaccines used against SARS-CoV-2, which include i. BNT162b2 vaccine by Pfizer and BioNTech, ii. mRNA-1273 vaccine by Moderna, iii . AZD1222 by AstraZeneca and University of Oxford, iv. CoronaVac by Sinovac, v. BBIBP-CorV by Sinopharm, and, vi. JNJ-78436735 by Janssen Pharmaceuticals Companies of Johnson and Johnson (Table (Table3) 3 ) [ 49 , 50 ]. These vaccines remove the ability of SARS-CoV-2 to cause severe symptoms of COVID-19, hospitalization, intensive care unit admission, and death. However, these vaccines may cause short-lived side effects such as i. pain at the injection site, ii. headache, iii. mild fever, iv. fatigue, and v. chills. These side effects could be more pronounced after the second dose, but usually resolve within 24–72 h. In addition, these vaccines should also be given to individuals who had a history of asymptomatic or symptomatic SARS-CoV-2 infection after 90 days [ 48 ].
Authorized COVID-19 vaccines [ 48 – 50 ]
Messenger RNA
Messenger RNA (mRNA) vaccines are a new type of vaccine technology that has been scientifically relevant since early in the twenty-first century. These vaccines can be developed rapidly and are cost efficient. Both BNT162b2 by Pfizer and BioNTech and mRNA-1273 by Moderna are examples of authorized mRNA vaccines against SARS-CoV-2 [ 48 , 51 ]. These vaccines are cationic lipid nanoparticles-encapsulated (LNP) mRNA of the SARS-CoV-2 expressing spike (S) proteins, which are unable to cause disease [ 48 , 49 , 52 ]. The lipid nanoparticle barrier functions to protect the mRNA, which is easily broken down. Next, these modified mRNA provide genetic instructions for human cells to produce the spike (S) proteins that cause an immune response, eliciting the production of antibodies, CD4 + and CD8 + T cells [ 51 ]. Hence, the body will be able to develop a certain degree of immunity against SARS-CoV-2. BNT162b2 vaccine, for instance, requires two doses given 3 weeks apart and has an efficacy rate of 95%, 7 days after a double dose [ 48 , 49 , 52 , 53 ]. However, dealing with BNT162b2 is challenging in rural areas, since the storage temperature of this vaccine is − 70 °C and the undiluted vials can only be stored at room temperature for not more than 2 h [ 48 , 54 ]. In addition, the BNT162b2 vaccine is approved for the age group of 16 years and older [ 48 ]. mRNA-1273, on the other hand, also requires two doses given 4 weeks apart. It has an efficacy rate of 94.1%, 14 days after the second dose [ 48 , 52 ]. mRNA-1273 is recommended for the age group of 18 years and above [ 54 ]. Furthermore, mRNA-1273 can be stored for 30 days between 2 and 8 °C [ 54 ].
There are differences in the number of doses required for different COVID-19 vaccines to reach their maximum level of protection against the virus. Two doses of these mRNA vaccines have been shown to significantly reduce the risk of SARS-CoV-2 infections and severe COVID-19 symptoms. However, COVID-19 vaccine boosters or additional doses are also required to further enhance and restore protection, which has been decreased over time after previous primary vaccinations, especially when Omicron is currently causing surges around the world. A study conducted by Edara et al . using serum from mRNA-vaccinated individuals showed that at 2–4 weeks after the primary series of vaccinations, a 30-fold reduction in neutralizing activity against Omicron (B.1.1.529) was observed [ 55 ]. In addition, their findings also showed that the majority of the naive vaccinated individuals have lost detectable neutralizing antibodies against Omicron (B1.1.529) after 6 months [ 55 ]. Hence, CDC recommends a booster of either BNT162b2 by Pfizer and BioNTech or mRNA-1273 by Moderna for the age group of 5 years and older after completing their primary series of vaccinations. A second booster, on the other hand, is recommended for adults of age 50 years and older and individuals of age 12 years and older with moderately or severely impaired immune systems. However, a study by Korves et al . reported that booster vaccine effectiveness for mRNA vaccines has shown lower vaccine effectiveness against infection with Omicron than Delta with 54% and 70% reduction in infection during Omicron and Delta predominance, respectively [ 56 ].
Inactivated virus
Inactivated virus vaccines against COVID-19 are a type of vaccine which contains inactivated SARS-CoV-2 through physical, chemical, or radiation processes, and hence are unable to replicate and cause disease [ 52 , 57 ]. BBIBP-CorV manufactured by Sinopharm Group in association with Beijing Institute of Biological Products and CoronaVac vaccine by Sinovac Biotech are both approved inactivated vaccines used by many countries against SARS-CoV-2 [ 48 , 49 , 57 ]. BBIBP-CorV, for instance, requires two doses to be given 3 weeks apart. It has an efficacy rate of 79.34% and 86% in China and the UAE, respectively [ 48 ]. The CoronaVac vaccine is a formalin-inactivated and alum adjuvanted vaccine [ 49 ]. It also requires two doses to be given 2 weeks apart and has been reported to have 50.38% efficacy. In addition, both vaccines should be stored and transported in the refrigerator at 2–8 °C.
Viral vector
The AZD1222 vaccine manufactured by AstraZeneca in collaboration with Oxford University is one of the authorized vector vaccines against COVID-19. It utilizes the non-replicating chimpanzee adenoviral vector ChAdOx1 with the double-stranded DNA segment of the RNA, which codes for the S protein antigen of SARS-CoV-2 [ 48 , 49 , 52 , 58 ]. AZD1222 should be given to individuals of age 18 years and older in two doses with an interval of 4–12 weeks [ 48 ]. JNJ-78436735 manufactured by Janssen Pharmaceuticals Companies of Johnson and Johnson, on the other hand, utilizes adenovirus type 26 (Ad26) vector carrying the S gene of SARS-CoV-2, which was also used for the development of Ebola vaccine [ 48 , 52 ]. It is a one-dose vaccine for individuals aged > 18 years old with 66% efficacy globally [ 48 ]. Furthermore, this vaccine is safe to be administered for pregnant women who may develop more severe COVID-19 symptoms [ 50 ].
Therapeutic approaches
Although vaccines are developed and authorized for protection against hospitalizations and deaths, there have still been major vaccine breakthroughs due to the constant viral mutations. Therefore, there is an urgent need to develop more effective treatments and drugs to mitigate the current pandemic. Currently, some repurposed drugs are being used to reduce the complications of COVID-19 based on their symptoms. Research has suggested that antiviral medicines such as remdesivir (RDV) are most effective in the early stages of COVID-19 when the patient’s immune system is challenged to prevent the replication of SARS-CoV-2 [ 50 ]. In contrast, immunosuppressive or anti-inflammatory drugs are more effective in the acute stages of COVID-19 when the patient is experiencing tissue damages due to severe immune or inflammatory reactions [ 50 ]. Hence, certain promising antiviral drugs have been authorized for the treatment of COVID-19, which include i. remdesivir, ii. molnupiravir, and iii. PAXLOVID™.
Remdesivir (RDV), which was developed to treat Ebola, is an antiviral drug act as a nucleoside analog and inhibits the RNA-dependent RNA polymerase (RdRp) enzyme of SARS-CoV-2 [ 21 , 59 ]. It is the first antiviral drug approved by the United States Food and Drug Administration (FDA) to treat COVID-19 patients [ 59 ]. Remdesivir is given to patients by intravenous (IV) administration. The recommended dosage for remdesivir is 200 mg IV once, followed by 100 mg IV once daily for 4 days [ 60 ]. However, treatment may be extended to 10 days if there is no improvement in recovery by day 5 [ 60 ]. Furthermore, its structure is composed of three fragments which include i. nucleobase (adenine) derivative, ii. pentose sugar, and iii. phosphoramidate unit (Fig. 8 ) [ 19 ].

Structure of remdesivir (molecular formula: C 27 H 35 N 6 O 8 P)
In the host cell, remdesivir (prodrug) is converted into the nucleoside derivate GS-441524 (Fig. 9 ). {"type":"entrez-nucleotide","attrs":{"text":"GS441524","term_id":"257561308","term_text":"GS441524"}} GS441524 is an active compound of remdesivir, which targets RdRp and competes with endogenous nucleotides (ATP) at the RdRp for incorporation into viral RNA [ 61 ]. Incorporation of the triphosphate form of remdesivir instead of ATP interrupts viral RNA replication and, thus, inhibits SARS-CoV-2 viral replication [ 61 ].

Structure of GS-441524 (molecular formula: C 12 H 13 N 5 O 4 )
Molnupiravir
Molnupiravir is an orally administered and directly acting antiviral interventional drug developed by Emory University (USA), Ridgeback Biotherapeutics, and Merck [ 62 ]. It was originally developed for the treatment of influenza [ 62 ]. However, molnupiravir, which is a pyrimidine ribonucleoside analog, also acts by inhibiting RdRp of SARS-CoV-2 to induce RNA mutagenesis. First, molnupiravir (C 13 H 19 N 3 O 7 ) (Fig. 10 a) is converted to EIDD-1931 (C 9 H 13 N 3 O 6 ) (Fig. 10 b) in the body and then to EIDD-1931-triphosphate (C 9 H 16 N 3 O 15 P 3 ) (Fig. 10 c) through phosphorylation by the host kinases [ 62 ]. Next, EIDD-1931-triphosphate acts as an alternate substrate and competes with the endogenous nucleotides at the RdRp enzyme of SARS-CoV-2 [ 62 ]. This causes inhibition of the normal functions of RdRp, causing it to generate mutated RNA copies of SARS-CoV-2 [ 62 ]. Hence, this prevents SARS-CoV-2 to reproduce and spread. Moreover, the reducing property (better electron donor than electron acceptor) of molnupiravir also contributes to its antiviral activity, as it affects the conditions required for viral infection [ 62 ].

a Structure of molnupiravir (molecular formula: C 13 H 19 N 3 O 7 ), b structure of EIDD-1931 (molecular formula: C 9 H 13 N 3 O 6 ), and c structure of EIDD-1931-triphosphate (molecular formula: C 9 H 16 N 3 O 15 P 3 )
PAXLOVID™
PAXLOVID™ is an orally administered antiviral drug developed by Pfizer Inc. It contains nirmatrelvir (PF-07321332) (Fig. 11 a) and ritonavir (Fig. 11 b) [ 63 ]. Both PF-07321332 and ritonavir are protease inhibitors. PF-073321332 works by interacting with 3CL pro , the main protease of SARS-CoV-2. It blocks its ability to transform pp1a and pp1ab into non-structural and structural proteins, which eventually stops the replication process of SARS-CoV-2 [ 64 ]. Furthermore, ritonavir functions as a booster as it slows down the metabolism of PF-073321332 and, hence, allows a higher concentration to remain active in the body for a longer period [ 64 ].

a Structure of nirmatrelvir (PF-07321332) (molecular formula: C 23 H 32 F 3 N 5 O 4 ), and b structure of ritonavir (molecular formula: C 37 H 48 N 6 O 5 S 2 )
Nature-based agents as possible COVID-19 inhibitors
Apart from well-established antiviral drugs in the treatment and inhibition of COVID-19, the possible naturally sourced agents should also be given some attention. Natural products are known to contain a multitude of metabolites with a wide range of therapeutic actions. These natural compounds are known to possess medicinal properties including antiviral activities. The bioactive components reportedly found in plants have been shown to exhibit robust antiviral activity. The isolation, purification, and identification of several phytochemicals from crude extracts have demonstrated antiviral activities such as against POLIO, HIV-1, adenoviruses, hepatitis, and influenza [ 65 ]. Natural products have been tested for coronaviruses and have been shown to show potential in coronavirus treatment [ 66 ].
More recently the BA.5 and BA.4 variants from the Omicron lineage have continued to increase, with the proportion of BA.5 variants increasing globally [ 67 ]. The highly contagious new subvariants BA.4 and BA.5 are driving the next waves of Omicron infections in several countries. There should be a multifaceted strategy to combat this global health pandemic including sourcing drugs from natural products, as they can work through multitargets and elicit their actions via different biochemical mechanisms [ 68 ].
Compounds such as quercetin have been reported to reduce the viral replication of rhinoviruses in infected mice [ 69 ]. More recently, preliminary randomized clinical studies involving quercetin have reported that following treatment of COVID-19 patients with quercetin, a proportion of the patients tested negative for the SARS-CoV-2 virus following a week of treatments with a protein of these patients having their symptoms diminished indicating the [ 70 ]. An in silico study involving about 8000 small molecule candidates has shown that quercetin was among the top candidates for binding with the ACE 2 interface on the S protein. Such binding will eventually reduce the ability of the virus to interact with host cells and thereby reduce the infectability of the virus. Quercetin is known to possess anti-inflammatory activities that might also help to prevent the consequences of the COVID-19 infection. COVID-19 infection triggers a cascade of inflammatory reactions as evident from reports on the elevated levels of cytokines and inflammatory indices such as IL-1β, IL-6, IL-10, and D-dimer in severely ill COVID-19 patients compared to those with moderate symptoms [ 71 ].
In addition, quercetin is a flavonoid that is widely found in several foods, and as some preliminary studies have shown has the potential to be further explored as a potentially useful compound to add to the COVID-19 treatment regime.
Nanotechnology-based approaches for the diagnosis, prevention, and treatment of COVID-19
Nanotechnology is a study that encompasses the understanding of diverse disciplines including chemistry, biology, and technology of nanomaterials, which are at dimensions between approximately 1–100 nm [ 20 ]. According to dimensions in the nanoscale, nanostructures are classified into four categories: i. zero-dimensional nanostructures (e.g., fullerene), ii. one-dimensional nanostructures (e.g., nanofibers), iii. two-dimensional nanostructures (e.g., nanofilms, nanolayers, and nanocoatings), and iv. three-dimensional nanostructures (e.g., nanoparticles) [ 20 , 72 ]. The dimensions of these nanostructures determine their functions and applications in nanotechnology [ 72 ]. Nanotechnology has a range of applications such as i. biomolecular detection and diagnostics, ii. therapeutics, iii. DNA sequencing, iv. pharmaceuticals, and v. sensors [ 20 ]. Therefore, it is established that the different fields in nanotechnology can contribute to providing alternative solutions to combat COVID-19. This includes the development of i. nanomaterial-based COVID-19 detection technology, ii. nanomaterial-based disinfectants, iii. new nanoparticle-based vaccines, and iv. nanoparticle-based drug delivery [ 20 , 73 ].
Gold nanoparticles (AuNPs) for instance, are nanomaterials that have been investigated for COVID-19 detection. AuNP-based nano-devices use an AuNP-based electrochemical immunosensor for COVID-19 detection [ 73 ]. The biosensor comprises a competitive immunoassay, performed on an array of nanostructured electrodes that are capable of immobilization of different antigens for multiplexed detection [ 73 ]. In addition, an increase in the number of nanostructured electrodes per array chip can also facilitate high-throughput screening of hundreds of samples in a single step which reduces the time and cost associated with the overall assay [ 73 ].
Furthermore, it has been established that SARS-CoV-2 can survive on objects and surfaces ranging from a few hours to a few days. However, currently, the available chemical disinfectants provide only a temporary solution and are harmful and toxic substances to humans. Therefore, the unique physicochemical properties of silver nanoparticles (AgNPs) have been widely investigated for their antiviral activity against SARS-CoV-2. AgNPs work by releasing Ag + ions, which are nontoxic to humans and have good long-term stability that curbs the growth of viruses such as SARS-CoV-2 and prevents proliferation by prohibiting the activity of respiratory system enzymes [ 73 ]. Therefore, Ag + can be sprayed on surfaces such as doorknobs, handrails, and wound dressing for disinfection.
The application of nanoparticles (NPs) in vaccine formulations has a crucial role in the structuring and delivery of vaccines, as they can act as assistants and carriers to deliver antigens to their intended targets [ 73 ]. In addition, NPs also speed up the development of COVID-19 vaccines. Nanoparticle-based delivery approaches have been used in the current mRNA-based COVID-19 vaccines such as BNT162b2 and mRNA-1273, as the mRNAs are embedded in lipid nanoparticles (LNPs) [ 48 , 49 , 52 ]. However, these developed vaccines are normally treated through intramuscular injections that can only be operated by health-care professionals and must be stored at low temperature which causes storage and distribution difficulties. Therefore, self-administered nanoparticle-based vaccines (nanovaccines) such as micro-needle patches offer a new approach for protection against SARS-CoV-2 [ 73 ]. Micro-needle patches for COVID-19 are polymer-encapsulated S and N protein-encoding DNA vaccines to stimulate an immune response for SARS-CoV-2 [ 74 ].
There are different types of nanostructured materials that can be used for drug delivery vesicles such as i. metallic nanoparticles, ii. liposomes, iii. fullerenes, iv. graphene, v. carbon nanoparticles, and vi. polymeric nanoparticles [ 20 ]. Liposomes and polymeric nanoparticles, for instance, prolong the drug half-life, improve the solubility of hydrophobic drugs, and reduce potential immunogenicity [ 20 ].
Future outlook
The COVID-19 pandemic has led to an unprecedented loss of human lives worldwide. Despite the continuous global research to understand COVID-19, it has yet to be eradicated. Furthermore, it is well known that the COVID-19 pandemic will not be the last, as there is still a possibility that another zoonotic coronavirus may emerge in the future. Therefore, it is crucial to strengthen global research and development in science and technology with interdisciplinary collaborations. The following are the main future outlooks to understand SARS-CoV-2 better, advance in detecting and preventing SARS-CoV-2 infections, and develop effective treatments for COVID-19.
- SARS-CoV-2 is the third zoonotic coronavirus after SARS-CoV and MERS-CoV. Therefore, for future early detection, prevention, and treatment of novel coronaviruses, more research is required to identify and describe the mechanism of these viral mutations to infect humans and their ability to persist in the human population. Especially, information on the mutational trend in the spike protein is important to develop future effective vaccines.
- The knowledge of the origin and reservoir of SARS-CoV-2 remains scarce. Therefore, it is crucial to comprehensively investigate the zoonotic origin and reservoir through multidisciplinary collaboration and carefully coordinated studies to help prepare for future destructive outbreaks caused by novel viruses.
- The ability of asymptomatic patients to spread SARS-CoV-2 has been proven. Therefore, further study on these asymptomatic patients is crucial to discover effective, reliable, and rapid screening methods and improve the accuracy of early diagnosis. Current COVID screening methods imply identifying more reliable early detection markers for such viruses.
- Single-use PPE, which is mostly made of highly hydrophobic and non-degradable materials like polypropylene, causes environmental pollution and ecosystem damage. Hence, to address the impacts of single-use PPE on the environment, more research on sustainable materials should be carried out to develop PPE that can be disinfected and reused without losing its protective properties.
- Traditional disinfecting method (e.g., soap water and alcohol-based sanitizers) is a temporary solution to prevent indirect contact transmission from virus-contaminated surfaces. Hence, more research on nanocoating materials plays a leading role in developing a novel surface disinfection approach. The use of environmentally friendly natural products is an alternative to the existing disinfectants.
- Majority of the vaccines available or under development target the healthy population of age group 18 years and older. Multidisciplinary collaboration between material science, chemistry, and biomedical science plays an essential role in developing vaccines for different populations such as infants, children below the age of 5 years, and individuals with underlying medical conditions.
- The main target for current vaccines against COVID-19 is mostly based on the spike (S) glycoprotein of SARS-CoV-2, which constantly develops mutations. Therefore, vaccine research and development should focus on different approaches to maintain its effectiveness.
- Mammals including dogs, cats, tigers, and lions were reported to be infected with SARS-CoV-2 after close contact with a human that is infected with COVID-19. Although there is no evidence that these infected mammals can spread SARS-CoV-2 and infect people, more studies in this area are required.
- Amphiphilic molecules such as soap were shown to be effective in breaking the lipid-bilayer membrane of SARS-CoV-2, causing its structure to fall apart. Therefore, identifying antiviral compounds that target the lipid-bilayer membrane of SARS-CoV-2 may be a viable therapeutic strategy.
- Since the long-term side effect of the existing vaccines is a major concern, it is necessary to develop an appropriate animal model to address this issue.
This review has provided an overview of all aspects of COVID-19, such as i. the structure of SARS-CoV-2, ii. molecular interaction between SARS-CoV-2 and ACE 2 receptor, iii. mechanism of SARS-CoV-2 pathogenesis, iv. transmission routes of SARS-CoV-2, v. persistence and viability of SARS-CoV-2 on different surfaces, vi. the materials and methods currently used for diagnosis, prevention, vaccines, and treatment for COVID-19, and vii. different approaches for the diagnosis, prevention, and treatment of COVID-19 using nanotechnology. The chemistry perspective has helped to understand different aspects of COVID-19. A study using molecular dynamics simulations suggested that the high affinity between the S glycoprotein and ACE 2 may be due to the hydrophobic effect among the hydrophobic surface areas of S glycoprotein and ACE 2 at the binding site. In addition, another study also found that the enhanced affinity of SARS-CoV-2 toward ACE 2 is due to the increase in electrostatic interactions caused by mutations in the S glycoprotein. Furthermore, the study of the persistence and viability of SARS-CoV-2 on different surfaces showed that it has longer persistence and viability on materials such as plastics, glass, and stainless steel compared to copper, paper, and cardboard. Another research has also shown that the increase in temperature and relative humidity increases the decay rate of SARS-CoV-2. The mechanism of cleansing action of soaps involves two steps: i. destruction of the lipid-bilayer viral membrane by surfactant molecules, and ii. micelle formation. On the other hand, alcohols found in alcohol-based hand sanitizers, which are also amphiphilic compounds, inactivate SARS-CoV-2 by destabilizing and denaturing its protein structures. Lastly, using nanomaterials such as gold nanoparticles (AuNPs) and silver nanoparticles (AgNPs) has been found to be a potential alternative detection and preventive method, respectively. Hence, in conclusion, research collaborations between biology and chemistry with other disciplines such as material science, biomedical science, and nanotechnology play an important role in understanding all aspects of COVID-19 to develop an effective diagnosis, prevention, and treatments for this infectious disease caused by SARS-CoV-2.
Acknowledgements
The authors would like to acknowledge the FIC block grant (UBD/RSCH/1.4/FICBF(b)/2022/046) received from Universiti Brunei Darussalam, Brunei Darussalam.
Abbreviations
Author contributions.
M.M.K.: supervision, conceptualization, funding acquisition, and writing—review and editing. G. Y. W.: methodology, data curation, and writing—original draft preparation. N. A.: writing—review and editing, and conceptualization. M. M. S.: writing—review and editing, and conceptualization.
Declarations
The authors declare that there are no conflicts of interest.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.

IMAGES
VIDEO
COMMENTS
DATA ON CORONAVIRUS WORLDWIDE. So far, as of September 19, 2020, the. pandemic has caused 30,906,084 cases of coronavirus disease with 959,630 deaths [1]. Figure 1 Active Cases in 2020 in millions. Figure 2 Daily New Cases in 2020 in thousands. It is interesting to note that only 6% of death come from the death of otherwise healthy people.
Students can choose to write a full-length college essay on the coronavirus or summarize their experience in a shorter form. To help students explain how the pandemic affected them, The Common App ...
Our challenge is great. Together, forward in the fight against COVID-19. The WHO South-East Asia Region is entering a new phase in its pandemic response. In recent weeks the spread of COVID-19 in the Region has slowed, due in large part to the unprecedented physical distancing measures that countries implemented early and aggressively.
Keep physical distance of at least 1 metre from others, even if they don't appear to be sick. Avoid crowds and close contact. Wear a properly fitted mask when physical distancing is not possible and in poorly ventilated settings. Clean your hands frequently with alcohol-based hand rub or soap and water.
Go to: The coronavirus disease-2019 (COVID-19) pandemic, caused by the new coronavirus SARS-CoV-2, has spread around the globe with unprecedented consequences for the health of millions of people. While the pandemic is still in progress, with new incidents being reported every day, the resilience of the global society is constantly being ...
Even in the lead up to the COVID-19 pandemic, U.S. resource allocation for combating infectious diseases and developing biodefense was woefully inadequate. In 2014, the U.S. allocated $6 billion ...
The outbreak of coronavirus disease 2019 (COVID-19) has caused more than 80 813 confirmed cases in all provinces of China, and 21 110 cases reported in 93 countries of six continents as of 7 March 2020 since middle December 2019. Due to biological nature of the novel coronavirus, named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) with faster spreading and unknown transmission ...
This essay is part of "Reimagining the global economy: Building back better in a post-COVID-19 world," a collection of 12 essays presenting new ideas to guide policies and shape debates in a ...
Problem: More supplies to fight COVID-19 are needed. Solution: Get factories to switch gears and respond to the coronavirus.Kenya's textile industry has pivoted to making masks and protective ...
This article is part of Harvard Medical School's continuing coverage of COVID-19.. As SARS-CoV-2 seems to settle into the background of our lives, transitioning from an unprecedented crisis to a routine threat alongside influenza and other, more familiar viruses, scientists have begun to turn their attention to the future of the COVID-19 pandemic as the virus continues to change and, just as ...
The COVID-19 Strategic Preparedness and Response Plan developed by the WHO identifies community volunteers as key stakeholders for risk communication, community engagement and in provision of health services. Since joining the UN Volunteers programme for East and Southern Africa in November, I have been humbled by the selflessness shown by ...
In addition, there are other prevention strategies that you can choose to further protect yourself and others. Wearing a mask and putting distance between yourself and others can help lower the risk of COVID-19 transmission. Testing for COVID-19 can help you decide what to do next, like getting treatment to reduce your risk of severe illness ...
Emergency funding provided by different countries to fight the COVID-19 is mentioned in this chapter. Lastly, artificial intelligence, data science and technological solutions like public health surveillance, remote biosignal measurement, IoT and wearables, chatbots and communication, social media and open data, automated diagnostics, drug ...
Avoid all fizzy, carbonated, concentrated juices, and all drinks which contain sugar. Maintain a healthy lifestyle of exercise, meditation, and regular sleep. Adequate sleep will help to support immune functioning. Eat at home to avoid contact with other people and try to reduce the chance of being exposed to COVID-19.
Cases of Covid-19 are spiking in nearly every state. The statistics are grim. With more than 100,000 new cases and 2,000 deaths every day, hospital intensive care units are filling up everywhere ...
The mixed patchwork of achievements and mis-steps in responding to covid-19 show powerful nations are not living up to their commitment to solidarity and equity, argue Jesse Bump and colleagues The 19th century pandemics that followed the globalisation of commercial and military activities led to a series of sanitary conferences, at which countries agreed to fight infectious diseases by ...
Hundreds of millions of babies are expected to be born during the COVID-19 pandemic. Fionn, son of Chloe O'Doherty and her husband Patrick, is among them. The couple says: "It's all over. We did ...
COVID-19 tests can help prevent the spread to others. You can use COVID-19 self-tests at home and get quick results whether or not you have symptoms. Wash your hands many times a day with soap and running water for at least 20 seconds. In general, this is a good practice to help prevent the spread of germs.
Sydnee Goyer '21 and Marcel Thompson's '22 essay "This Flu Season Will Be Decisive in the Fight Against COVID-19" also was published in Arcadia Political Review. "With winter approaching all around the Northern Hemisphere, people are preparing for what has already been named a "twindemic," meaning the joint threat of the ...
Scientists are still learning about COVID-19, the disease caused by the coronavirus, but according to the CDC, this highly contagious virus appears to be most commonly spread during close (within 6 feet) person-to-person contact through respiratory droplets. "The means of transmission can be through respiratory droplets produced when a person coughs or sneezes, or by direct physical contact ...
How to rest. First, if you're fighting COVID-19 at home, you don't need to sleep in a certain position. "We know that sleeping on your stomach can improve your oxygenation if you need supplemental oxygen in the hospital. If you don't have severe COVID-19, lying on your stomach or side is not going to affect your disease," says Dr. Boer.
This plain language may help improve research and action to fight disease. WHO now admits the COVID virus and other germs spread "through the air." This plain language may help improve ...
Writing a persuasive essay about COVID-19 requires a thoughtful approach to present your arguments effectively. Here are some tips to help you craft a compelling persuasive essay on this topic: Choose a Specific Angle. Start by narrowing down your focus. COVID-19 is a broad topic, so selecting a specific aspect or issue related to it will make ...
As they do, they must be cautious about the lessons they might think Covid-19 left behind. We need to be prepared to fight the next war, not the last one. We need to be prepared to fight the next ...
Researchers stated people with low vitamin D levels have a lower serum protection rate after flu vaccination than those with normal levels. They claimed that vitamin D supplementation can maximize ...
The latest on symptoms and long Covid. Doctors said that the symptoms of both KP.2 and JN.1 — which now makes up around 16 percent of cases — are most likely similar to those seen with other ...
As Porter played the video of the fight, he pointed out that Jackson was standing with his back to the man and woman accosting them, appearing to try and ignore them and that Hooks remained seated ...
Gov. Kathy Hochul on Saturday announced Northwell Health, New York state's largest health system, has dispatched a team of skilled nurses to Western New York to answer the call for more medical ...
The COVID-19 pandemic has led to an unprecedented loss of human lives worldwide. Despite the continuous global research to understand COVID-19, it has yet to be eradicated. Furthermore, it is well known that the COVID-19 pandemic will not be the last, as there is still a possibility that another zoonotic coronavirus may emerge in the future.
A jury trial of a Little Rock couple accusing the management of a local Saltgrass Steakhouse of standing by on June 27, 2020, as they were attacked by other patrons in the restaurant over covid-19 ...