Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer

You are here
- Volume 10, Issue 1
- Teaching strategies and outcome assessments targeting critical thinking in bachelor nursing students: a scoping review protocol
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-4086-0086 Frida Westerdahl 1 ,
- Elisabeth Carlson 1 ,
- Anne Wennick 1 ,
- Gunilla Borglin 1 , 2
- 1 Department of Care Science , Malmö University , Malmö , Sweden
- 2 Nursing Education , Lovisenberg Diaconal University College , Oslo , Norway
- Correspondence to Frida Westerdahl; frida.nygren{at}mau.se
Introduction Applying critical thinking is essential for nursing students both in an academic and clinical context. Particularly, as critical thinking is a vital part of nurses’ everyday problem-solving and decision-making processes. Therefore, regardless of the topic taught or the setting in which it is taught, it requires teaching strategies especially targeting students’ critical thinking skills and abilities. One challenge with the latter is the difficulties to assess and evaluate the impact of such teaching strategies on the students’ critical thinking disposition. Hence, our objective will be to review published literature on; existing teaching strategies and outcomes assessments targeting nursing students’ critical thinking skills and abilities.
Methods and analysis Our scoping review will be conducted in accordance with Arksey and O’Malley’s framework for scoping studies. Search strategies will be developed in cooperation with an experienced librarian, and adjusted to each individual database for example, CINAHL, PubMed, PsycINFO, ERIC and ERC. A preliminary search in CINAHL was conducted on the 17 th of July 2019. Peer-reviewed published studies conducted with a qualitative, quantitative or mixed method design and focussing our objectives, will be eligible for inclusion. Included studies will be quality assessed in accordance with their study design. Data will be charted using a standardised extraction form. The qualitative data will be presented through a thematic analyses, and the quantitative data by descriptive numerical analysis. Lastly, nurse educators and nursing students will be consulted for validation of the findings from the scoping review.
Ethics and dissemination Under the Swedish Ethical Review Act (2003:460) this study does not need ethical clearance by a Regional Ethical Review Authority as it not includes any primary empirical data on biological material or sensitive information. The findings will be used to inform the design of a future study aiming to develop an, and subsequently evaluate it, educational intervention targeting teaching strategies focussing on nursing students’ critical thinking skills and abilities.
- critical thinking abilities
- critical thinking skills
- descriptive numerical analysis
- nurse educators
- thematic analysis
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2019-033214
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
To ensure rigour and transparency the upcoming scoping review will be based on (1) a solid methodological framework for scoping studies and (2) the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews checklist.
A minimum of two members of the review team will independently assess study eligibility.
Eligible studies will be quality assessed in accordance with their study design.
To achieve a comprehensive picture of the existing research qualitative, quantitative and mixed methods designs will be included in this scoping review.
One limitation might be the potential risk for publication bias since grey literature will not be included, as this will facilitate charting of teaching strategies and outcome assessments targeting critical thinking skills and abilities as described solely in published research.
Introduction
Applying critical thinking is essential for bachelor nursing students (hereafter nursing students); particularly, considering the complex care situations they regularly will find themselves in after graduation. 1 Care situations that among others require them to work in accordance with established standards 2 to be able to contribute to a safe, evidence based and optimal clinical practice. Given that nursing is based on scientific knowledge, critical thinking is the reasonable reflection to justify nursing actions based on evidence. Skills and abilities in critical thinking have consequently been found to predict nursing competence together with working years, position, title and educational level, that is, Bachelor or Master in Nursing. 3 Critical thinking is, therefore, a crucial component of every registered nurse’s daily activities, aiding problem-solving and decision-making processes. 4
According to Scheffer and Rubenfeld the ability to execute critical thinking in nursing could be seen from two perspectives; habits of the mind (cognition), and skills employed by the critical thinker. 5 Critical thinking can also be seen as a consecutive process including (i) gathering information, (ii) questioning, (iii) analysis and evaluation and (iv) problem-solving and application of theory, that is, the nursing process. 6 This consecutive process of critical thinking needs to be applied both in the clinical area and in the classroom. 7 However, to develop this ability among nursing students is a complex process. To apply critical thinking, the necessary skills and abilities need to be taught and developed during both the students’ clinical placements as well as during their theory courses throughout the nursing education. 4
One challenge with the concept of critical thinking, often highlighted in the literature, and despite its priority within the nursing education, is the interchangeable use of the concepts of critical thinking, clinical reasoning and clinical judgement. 7–9 Concepts that Victor-Chmil describe as; ‘they are not one and the same’ (p 34). It needs to be acknowledged, as the authors of this current protocol do, that critical thinking often is used as a broader term which includes the concepts of clinical reasoning and clinical judgement. 8 According to Alfaro-LeFevre clinical reasoning refers to the process used to solve clinical issues and clinical judgement refers to the outcome or conclusion of this process. 7 Therefore, regardless of the topic taught or the setting in which it is taught, requires teaching strategies especially targeting nursing students’ critical thinking skills and abilities. For these strategies to be favourable, it requires implementation throughout the nursing education, and thereby reflected in all parts of the nursing programmes’ learning objectives and curricula. 10 It has been outlined that teaching strategies such as, problem-based learning, concept-mapping, case-based learning interventions and reflective writing are often used in nursing programmes to support critical thinking. 6 10 11 However, another challenge with critical thinking, besides the interchangeable use of concepts, is the difficulty to assess and evaluate the impact of different teaching strategies on the students’ critical thinking disposition (ie, skills and abilities) as well as the assessment of the different components in the critical thinking process. 8 Previous reviews in the current research area have only included either experimental studies 12 or randomised clinical trials 13 measuring the effectiveness of teaching strategies. Further, other reviews have involved mixed populations including not only nursing students, but also working nurses and nursing managers 14 and midwifery students. 15 Since critical thinking is a vital part of registered nurses’ problem-solving and decision-making, this ability needs to be taught already during the nursing education. It is therefore necessary to focus the educational context of undergraduate nursing taking an extended approach on how teaching strategies targeting critical thinking are described, experienced and assessed. Hence, our overarching objective will be to review published literature on; existing teaching strategies and outcomes assessments targeting nursing students’ critical thinking skills and abilities.
Methods and analysis
The upcoming scoping review will address a broad topic (ie, teaching strategies targeting nursing students’ critical thinking skills and abilities, as well as outcome assessments of such skills and abilities), where a diverse range of study designs can be considered relevant in answering our additionally wide review questions. Our scoping review will therefore be designed in accordance with Arksey and O’Malley’s methodological framework for scoping studies. 16 However, our design will also be informed by other more recent methodological accounts. 17 18 The framework will enable us to identify existing gaps in the literature as well as to summarise, evaluate and disseminate the overall state of research activities within the field. 16 The Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews checklist (PRISMA-ScR) was used to prepare this protocol. 19 PRISMA-ScR will also form the base for the upcoming scoping review as standardised reporting guidelines can according to Colquhoun et al support the critical appraisals of published reviews by expanding on their transparency and reproducibility. 20
Stage 1: identifying the research question
The research questions for the upcoming scoping review aims for comprehensiveness, that is, they will be broad to cover the breadth of research evidence in our field of focus. As scoping is an iterative methodological process, 16 it is possible for us to decide to add supplementary questions based on the findings emerging during the review process. A modified 21 PICOS (Population, Intervention, Comparison, Outcome and Study Setting) framework will aid us in determining the appropriateness of the research questions, as well as guide us in our database searches ( table 1 ).
- View inline
Framework (PICOS) for determination of eligibility of review questions
Since the subsequent goal of the upcoming scoping review is to further the knowledge and understanding about how nurse educators via teaching strategies can target the development of nursing students’ critical thinking skills and abilities we will additionally engage in findings of relevance to this. The following tentative research questions were developed to capture the objectives of the upcoming study:
Which are the teaching strategies described in the literature as targeting critical thinking skills and abilities among nursing students?
How are these teaching strategies conceptualised, described and experienced by students and/or nurse educators for example, pros and cons?
Which outcomes are described in the literature as used to assess critical thinking skills and abilities?
Stage 2: identifying relevant studies
The upcoming scoping review will include primary studies utilising qualitative, quantitative and mixed methods, published in peer-reviewed journals. This strategy will support us to achieve a comprehensive picture of the existing research focussing peer-reviewed studies on teaching strategies targeting critical thinking skills and abilities among nursing students, as well as on existing research focussing on outcome assessments of such skills and abilities. No limits will be applied concerning publication year, since we aim at conducting a comprehensive overview of published studies. Studies will be excluded if the population is not identifiable, qualitative and quantitative data is not possible to extract in case of mixed method design or published in other languages than English. All reasons for exclusion will be documented.
In our upcoming scoping review the term ‘teaching strategies’ will be used. Thus, our focus is not the overall educational organisation of teaching (ie, educational strategies) or the students’ individual general learning process (ie, learning strategies). However, as we are aware of the commonly interchangeable use in the literature of the terms; teaching strategies, educational strategies and learning strategies, they will all be included in our searches. Here the term teaching strategies are operationalised in accordance with Banning, and as encompassing three different perspectives; (i) the didactic perspective, which is teacher centred and mainly involves lectures; (ii) the facilitative perspective, focussing on self-directed learning making the students articulate their knowledge and lastly (iii) the Socratic perspective which is emphasising student-centredness and use objective questioning from the teacher. 22
The following databases; CINAHL, PubMed, PsycInfo, ERIC and ERC will be used to search for eligible studies. These databases are chosen to cover a comprehensive sample of literature from healthcare science and education. A search strategy for each database will be developed by the review team with assistance from an experienced librarian. Our strategies will include both database specific heading that is, Medical Subject Headings, keywords and synonyms. All specific headings and key words will be combined using the Boolean operators OR as well as AND. To ensure comprehensiveness, included studies reference lists will be manually searched. As outlined by Arksey and O’Malley the search strategy should be an iterative process and the search terms could be adjusted while an increased familiarity with the literature is achieved. For this reason, a preliminary pilot search strategy will be applied to the databases and the first 100 search results will be reviewed by the review team to assess validity. 16 During the review team meetings, adjustments will be applied to the search strategy and search terms until full agreement is reached. Grey literature (ie, literature that is not formally published in sources such as journal articles or books) will not, as described elsewhere, be included in our upcoming scoping study. 23 This will support us to focus on and to chart how teaching strategies targeting skills and abilities such as critical thinking is described in published peer-reviewed research. A draft of a preliminary search in CINAHL conducted on the 17 th of July 2019 is attached in online supplementary file 1 .
Supplemental material
Stage 3: study selection.
The study selection will first consist of a title and abstract scan. If the title and abstract are in line with the scoping review’s objectives and questions to the literature or if the relevance of the study is unclear a full-text review will follow. Retrieved studies from each database are going to be divided equally among a minimum of two reviewers, who independently will conduct the selection process. 17 To facilitate the process, we are going to use the data programme Rayyan. The programme is a mobile and web application developed to facilitate the screening of title and/or abstract as well as the collaboration between the reviewers. 24 During the study selection process, the first reviewer (FW) will be responsible for regularly convoking the review team for discussions concerning uncertainties and to refine the study selection process. 17 Criteria for inclusion can also be applied ad hoc during the process when acquaintance with the field of research is increased. 16 If any disagreements on study inclusion occur, an additional reviewer will be consulted to determine the final inclusion. 17 The study selection process ( figure 1 ) will be accounted for by the PRISMA flow diagram. 25
- Download figure
- Open in new tab
- Download powerpoint
Overview study selection process.
Contrary to Arksey and O’Malley’s methodological framework, 16 studies eligible for inclusion in our scoping review are going to be quality assessed. The assessment of the included studies’ quality will allow us to identify where the research itself is of poor quality, that is, identifying gaps in the existing literature review. According to Grant and Booth the lack of quality assessments in scoping reviews are likely to limit the uptake of the findings. 26 Their sentiment is supported by both Levac, Colquhoun and O’Brien 17 and Daudt, van Mossel and Scott 18 who state that a quality assessment of included studies will likely result in findings more useful for practice. The quality assessment will be conducted by a minimum of two reviewers, who will use the relevant study design checklists from the Critical Appraisal Skills Programme (CASP). 27 As, CASP lack a checklist for mixed methods studies, the mixed method appraisal tool will be applied. 28 In the case of any ambiguity concerning a study’s quality assessment, an additional reviewer is going to be consulted. No exclusion of eligible studies will be made on behalf of the quality assessment as studies with limited quality nevertheless can provide a valid rationale as guidance as to where more research is required.
Stage 4: charting data
A data charting form would be developed, and piloted on the first 5 to 10 included studies in this review. The piloting will support the team to reach an agreement on extraction consistency. The latter is especially important, as the extraction will be conducted individually and independently by a minimum of two reviewers. 17 A systematic and analytical approach will be utilised to extract the relevant information of each included study. The variables and themes to be included in order to answer the review’s objective and questions to the literature will be established iteratively ( box 1 ). Thus, the data charting form will be updated throughout the review by one of the reviewers (FW) who will also hold regular discussion with the others in the review team. 17
Tentative data charting form
Author and date.
Study title.
Journal full reference.
Aim, objective and/or research questions.
Study and recruitment context (eg, in what country and where people were recruited).
Participant characteristics (eg, age, gender, education year/semester of study, course (ie, theoretical or clinical placement)).
Sampling method.
Number of study participants.
Study design.
Data collection (eg, what data collection methods were used?).
Data analysis (eg, how was the data analysed?).
Described ethical approval and/or considerations. 29
Described teaching strategies and/or interventions targeting review focus.
Described outcomes and assessments.
Most relevant findings.
Study quality appraisal. 27 28
Tentative ethical requirements influenced by Weingarten, Paul and Leibovici.
Was the study approved by a research ethical committee? (Yes/No)
Was informed consent obtained? (Yes/No)
Were adequate measurements taken to protect personal data? (Yes/No)
Is there a declaration on financial support? (Yes/No)
Is there a declaration on potential conflict of interest? (Yes/No)
Influenced by Weingarten, Paul and Leibovici’s substantial contribution to raise the ethical awareness in reviews, an ethical assess form ( box 2 ) was developed for the upcoming scoping review including five requirements. 29 Included studies valued by the review team as not adhering to the ethical requirements will be excluded at this stage of the scoping review process.
Stage 5: collating, summarising and reporting the results
In the fifth stage, an overview and narrative account of variables and information extracted in stage 4 will be presented, and as highlighted by Arksey and O’Malley no evidence grading will be executed. 16 Levac, Colquhoun and O’Brien 17 and Daudt, Van Mossel and Scott 18 suggest that the extracted qualitative data should be presented through thematic analysis, since no synthesis of data is required. 16 For this purpose, the thematic analysis by Braun and Clarke will be applied which is a flexible method suitable when the data is broad and allowing for a wide range of analytical options. 30 This cohere with the upcoming scoping review, which will include studies with a wide range of research questions and methods. Quantitative data will be reviewed through basic descriptive numerical analysis and presented in tables and charts to highlight the range of data. 16 If studies with a mixed method design are included in stage 3, the qualitative and quantitative data will be extracted and analysed separately. A minimum of two reviewers will be responsible for this stage of the scoping review process. During the process, meetings with the entire review team will be scheduled by the first reviewer (FW) to discuss and come to agreement concerning analysis and presentation of extracted data.
Stage 6: consultation stage
To validate the findings of this scoping study and make it more useful for practice the optional stage consultation will be applied. For this purpose, the findings from the scoping review will be presented to a group of educators and students connected to a nursing programme as a means to contribute with valuable insights on issues connected to the application and implementation of the findings.
Patient and public involvement
No patients have been involved in the design of this study. However, to conduct a study targeting teaching strategies for critical thinking in nursing education will eventually benefit patients since education is the foundation for raising future nurses and improve patient care.
Ethics and dissemination
Under the Swedish Ethical Review Act (2003:460) 31 this study does not need ethical clearance by a Regional Ethical Review Authority as it does not include any primary empirical data on biological material or sensitive information (eg, ethnicity, political or sexual orientation). However, the issue of ethical consideration in the execution of reviews is raised by Vergnes et al 32 as well as by Weingarten, Paul and Leibovici. 29 They state that without an ethical judgement of the included studies it could result in establishing clinical practise and guidelines based on studies with poor ethical quality and even unethical studies. It could further be seen as a way of increasing the awareness and necessity of high ethical standards in research. To meet these requirements one variable in the charting form will be ethical consideration and for that purpose a tentative checklist for ethical requirements was developed ( box 2 ). The checklist will be tested on a minimum of 10 publications, and revised accordingly if necessary.
The upcoming scoping review will contribute to the advancement of research concerning teaching strategies targeting nursing students’ skills and abilities in critical thinking and the outcome assessment of it. It will also provide an indication of the maturity of the literature by identifying research gaps. Gaining more knowledge of the targeted research area can act as a benchmark to implement new teaching strategies facilitating students’ critical thinking disposition within the nursing education. This will better prepare future nurses for the complex care situations they will approach. Our findings will be used to inform the design of a future study aiming to develop and evaluate an educational intervention targeting teaching strategies focussing on nursing students’ critical thinking skills and abilities. The upcoming scoping review will be published in a peer-reviewed journal. We expect to report in late spring 2020.
- Von Colln-Appling C ,
- Cronenwett L ,
- Sherwood G ,
- Barnsteiner J , et al
- Chang Y-J ,
- Kuo S-H , et al
- Andrea Sullivan E ,
- Sullivan EA
- Scheffer BK ,
- Rubenfeld MG
- Alfaro-LeFevre R
- Victor-Chmil J
- Simpson E ,
- Carvalho DPSRP ,
- Azevedo IC ,
- Cruz GKP , et al
- De Oliviera LB ,
- Carbogim FDC , et al
- Zuriguel Pérez E ,
- Lluch Canut MT ,
- Falcó Pegueroles A , et al
- Carter AG ,
- Creedy DK ,
- Sidebotham M
- Colquhoun H ,
- Daudt HML ,
- van Mossel C ,
- Tricco AC ,
- Zarin W , et al
- Colquhoun HL ,
- O'Brien KK , et al
- Mashamba-Thompson TP
- Stoffels M ,
- Peerdeman SM ,
- Daelmans HEM , et al
- Ouzzani M ,
- Hammady H ,
- Fedorowicz Z , et al
- Liberati A ,
- Tetzlaff J , et al
- Fbregues S , et al
- Weingarten MA ,
- Leibovici L
- ↵ Act concerning the ethical review of research involving humans (SFS 2003:460) .
- Vergnes J-N ,
- Marchal-Sixou C ,
- Nabet C , et al
Contributors FW, EC, AW and GB were responsible for the initial design of this study. FW conceptualised the review approach and led the writing of the manuscript. FW, EC, AW and GB contributed to the protocol’s development and approved the final version of this protocol. GB, EC and AW led the supervision of the manuscript preparation.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
Promoting critical thinking through an evidence-based skills fair intervention
Journal of Research in Innovative Teaching & Learning
ISSN : 2397-7604
Article publication date: 23 November 2020
Issue publication date: 1 April 2022
The lack of critical thinking in new graduates has been a concern to the nursing profession. The purpose of this study was to investigate the effects of an innovative, evidence-based skills fair intervention on nursing students' achievements and perceptions of critical thinking skills development.
Design/methodology/approach
The explanatory sequential mixed-methods design was employed for this study.
The findings indicated participants perceived the intervention as a strategy for developing critical thinking.
Originality/value
The study provides educators helpful information in planning their own teaching practice in educating students.
Critical thinking
Evidence-based practice, skills fair intervention.
Gonzalez, H.C. , Hsiao, E.-L. , Dees, D.C. , Noviello, S.R. and Gerber, B.L. (2022), "Promoting critical thinking through an evidence-based skills fair intervention", Journal of Research in Innovative Teaching & Learning , Vol. 15 No. 1, pp. 41-54. https://doi.org/10.1108/JRIT-08-2020-0041
Emerald Publishing Limited
Copyright © 2020, Heidi C. Gonzalez, E-Ling Hsiao, Dianne C. Dees, Sherri R. Noviello and Brian L. Gerber
Published in Journal of Research in Innovative Teaching & Learning . Published by Emerald Publishing Limited. This article is published under the Creative Commons Attribution (CC BY 4.0) licence. Anyone may reproduce, distribute, translate and create derivative works of this article (for both commercial and non-commercial purposes), subject to full attribution to the original publication and authors. The full terms of this licence may be seen at http://creativecommons.org/licences/by/4.0/legalcode
Introduction
Critical thinking (CT) was defined as “cognitive skills of analyzing, applying standards, discriminating, information seeking, logical reasoning, predicting, and transforming knowledge” ( Scheffer and Rubenfeld, 2000 , p. 357). Critical thinking is the basis for all professional decision-making ( Moore, 2007 ). The lack of critical thinking in student nurses and new graduates has been a concern to the nursing profession. It would negatively affect the quality of service and directly relate to the high error rates in novice nurses that influence patient safety ( Arli et al. , 2017 ; Saintsing et al. , 2011 ). It was reported that as many as 88% of novice nurses commit medication errors with 30% of these errors due to a lack of critical thinking ( Ebright et al. , 2004 ). Failure to rescue is another type of error common for novice nurses, reported as high as 37% ( Saintsing et al. , 2011 ). The failure to recognize trends or complications promptly or take action to stabilize the patient occurs when health-care providers do not recognize signs and symptoms of the early warnings of distress ( Garvey and CNE series, 2015 ). Internationally, this lack of preparedness and critical thinking attributes to the reported 35–60% attrition rate of new graduate nurses in their first two years of practice ( Goodare, 2015 ). The high attrition rate of new nurses has expensive professional and economic costs of $82,000 or more per nurse and negatively affects patient care ( Twibell et al. , 2012 ). Facione and Facione (2013) reported the failure to utilize critical thinking skills not only interferes with learning but also results in poor decision-making and unclear communication between health-care professionals, which ultimately leads to patient deaths.
Due to the importance of critical thinking, many nursing programs strive to infuse critical thinking into their curriculum to better prepare graduates for the realities of clinical practice that involves ever-changing, complex clinical situations and bridge the gap between education and practice in nursing ( Benner et al. , 2010 ; Kim et al. , 2019 ; Park et al. , 2016 ; Newton and Moore, 2013 ; Nibert, 2011 ). To help develop students' critical thinking skills, nurse educators must change the way they teach nursing, so they can prepare future nurses to be effective communicators, critical thinkers and creative problem solvers ( Rieger et al. , 2015 ). Nursing leaders also need to redefine teaching practice and educational guidelines that drive innovation in undergraduate nursing programs.
Evidence-based practice has been advocated to promote critical thinking and help reduce the research-practice gap ( Profetto-McGrath, 2005 ; Stanley and Dougherty, 2010 ). Evidence-based practice was defined as “the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of the individual patient” ( Sackett et al. , 1996 , p. 71). Skills fair intervention, one type of evidence-based practice, can be used to engage students, promote active learning and develop critical thinking ( McCausland and Meyers, 2013 ; Roberts et al. , 2009 ). Skills fair intervention helps promote a consistent teaching practice of the psychomotor skills to the novice nurse that decreased anxiety, gave clarity of expectations to the students in the clinical setting and increased students' critical thinking skills ( Roberts et al. , 2009 ). The researchers of this study had an opportunity to create an active, innovative skills fair intervention for a baccalaureate nursing program in one southeastern state. This intervention incorporated evidence-based practice rationale with critical thinking prompts using Socratic questioning, evidence-based practice videos to the psychomotor skill rubrics, group work, guided discussions, expert demonstration followed by guided practice and blended learning in an attempt to promote and develop critical thinking in nursing students ( Hsu and Hsieh, 2013 ; Oermann et al. , 2011 ; Roberts et al. , 2009 ). The effects of an innovative skills fair intervention on senior baccalaureate nursing students' achievements and their perceptions of critical thinking development were examined in the study.
Literature review
The ability to use reasoned opinion focusing equally on processes and outcomes over emotions is called critical thinking ( Paul and Elder, 2008 ). Critical thinking skills are desired in almost every discipline and play a major role in decision-making and daily judgments. The roots of critical thinking date back to Socrates 2,500 years ago and can be traced to the ancient philosopher Aristotle ( Paul and Elder, 2012 ). Socrates challenged others by asking inquisitive questions in an attempt to challenge their knowledge. In the 1980s, critical thinking gained nationwide recognition as a behavioral science concept in the educational system ( Robert and Petersen, 2013 ). Many researchers in both education and nursing have attempted to define, measure and teach critical thinking for decades. However, a theoretical definition has yet to be accepted and established by the nursing profession ( Romeo, 2010 ). The terms critical literacy, CT, reflective thinking, systems thinking, clinical judgment and clinical reasoning are used synonymously in the reviewed literature ( Clarke and Whitney, 2009 ; Dykstra, 2008 ; Jones, 2010 ; Swing, 2014 ; Turner, 2005 ).
Watson and Glaser (1980) viewed critical thinking not only as cognitive skills but also as a combination of skills, knowledge and attitudes. Paul (1993) , the founder of the Foundation for Critical Thinking, offered several definitions of critical thinking and identified three essential components of critical thinking: elements of thought, intellectual standards and affective traits. Brunt (2005) stated critical thinking is a process of being practical and considered it to be “the process of purposeful thinking and reflective reasoning where practitioners examine ideas, assumptions, principles, conclusions, beliefs, and actions in the contexts of nursing practice” (p. 61). In an updated definition, Ennis (2011) described critical thinking as, “reasonable reflective thinking focused on deciding what to believe or do” (para. 1).
The most comprehensive attempt to define critical thinking was under the direction of Facione and sponsored by the American Philosophical Association ( Scheffer and Rubenfeld, 2000 ). Facione (1990) surveyed 53 experts from the arts and sciences using the Delphi method to define critical thinking as a “purposeful, self-regulatory judgment which results in interpretation, analysis, evaluation, and inference, as well as an explanation of the evidential, conceptual, methodological, criteriological, or contextual considerations upon which judgment, is based” (p. 2).
To come to a consensus definition for critical thinking, Scheffer and Rubenfeld (2000) also conducted a Delphi study. Their study consisted of an international panel of nurses who completed five rounds of sequenced questions to arrive at a consensus definition. Critical thinking was defined as “habits of mind” and “cognitive skills.” The elements of habits of mind included “confidence, contextual perspective, creativity, flexibility, inquisitiveness, intellectual integrity, intuition, open-mindedness, perseverance, and reflection” ( Scheffer and Rubenfeld, 2000 , p. 352). The elements of cognitive skills were recognized as “analyzing, applying standards, discriminating, information seeking, logical reasoning, predicting, and transforming knowledge” ( Scheffer and Rubenfeld, 2000 , p. 352). In addition, Ignatavicius (2001) defined the development of critical thinking as a long-term process that must be practiced, nurtured and reinforced over time. Ignatavicius believed that a critical thinker required six cognitive skills: interpretation, analysis, evaluation, inference, explanation and self-regulation ( Chun-Chih et al. , 2015 ). According to Ignatavicius (2001) , the development of critical thinking is difficult to measure or describe because it is a formative rather than summative process.
Fero et al. (2009) noted that patient safety might be compromised if a nurse cannot provide clinically competent care due to a lack of critical thinking. The Institute of Medicine (2001) recommended five health care competencies: patient-centered care, interdisciplinary team care, evidence-based practice, informatics and quality improvement. Understanding the development and attainment of critical thinking is the key for gaining these future competencies ( Scheffer and Rubenfeld, 2000 ). The development of a strong scientific foundation for nursing practice depends on habits such as contextual perspective, inquisitiveness, creativity, analysis and reasoning skills. Therefore, the need to better understand how these critical thinking habits are developed in nursing students needs to be explored through additional research ( Fero et al. , 2009 ). Despite critical thinking being listed since the 1980s as an accreditation outcome criteria for baccalaureate programs by the National League for Nursing, very little improvement has been observed in practice ( McMullen and McMullen, 2009 ). James (2013) reported the number of patient harm incidents associated with hospital care is much higher than previously thought. James' study indicated that between 210,000 and 440,000 patients each year go to the hospital for care and end up suffering some preventable harm that contributes to their death. James' study of preventable errors is attributed to other sources besides nursing care, but having a nurse in place who can advocate and critically think for patients will make a positive impact on improving patient safety ( James, 2013 ; Robert and Peterson, 2013 ).
Adopting teaching practice to promote CT is a crucial component of nursing education. Research by Nadelson and Nadelson (2014) suggested evidence-based practice is best learned when integrated into multiple areas of the curriculum. Evidence-based practice developed its roots through evidence-based medicine, and the philosophical origins extend back to the mid-19th century ( Longton, 2014 ). Florence Nightingale, the pioneer of modern nursing, used evidence-based practice during the Crimean War when she recognized a connection between poor sanitary conditions and rising mortality rates of wounded soldiers ( Rahman and Applebaum, 2011 ). In professional nursing practice today, a commonly used definition of evidence-based practice is derived from Dr. David Sackett: the conscientious, explicit and judicious use of current best evidence in making decisions about the care of the individual patient ( Sackett et al. , 1996 , p. 71). As professional nurses, it is imperative for patient safety to remain inquisitive and ask if the care provided is based on available evidence. One of the core beliefs of the American Nephrology Nurses' Association's (2019) 2019–2020 Strategic Plan is “Anna must support research to develop evidence-based practice, as well as to advance nursing science, and that as individual members, we must support, participate in, and apply evidence-based research that advances our own skills, as well as nursing science” (p. 1). Longton (2014) reported the lack of evidence-based practice in nursing resulted in negative outcomes for patients. In fact, when evidence-based practice was implemented, changes in policies and procedures occurred that resulted in decreased reports of patient harm and associated health-care costs. The Institute of Medicine (2011) recommendations included nurses being leaders in the transformation of the health-care system and achieving higher levels of education that will provide the ability to critically analyze data to improve the quality of care for patients. Student nurses must be taught to connect and integrate CT and evidence-based practice throughout their program of study and continue that practice throughout their careers.
One type of evidence-based practice that can be used to engage students, promote active learning and develop critical thinking is skills fair intervention ( McCausland and Meyers, 2013 ; Roberts et al. , 2009 ). Skills fair intervention promoted a consistent teaching approach of the psychomotor skills to the novice nurse that decreased anxiety, gave clarity of expectations to the students in the clinical setting and increased students' critical thinking skills ( Roberts et al. , 2009 ). The skills fair intervention used in this study is a teaching strategy that incorporated CT prompts, Socratic questioning, group work, guided discussions, return demonstrations and blended learning in an attempt to develop CT in nursing students ( Hsu and Hsieh, 2013 ; Roberts et al. , 2009 ). It melded evidence-based practice with simulated CT opportunities while students practiced essential psychomotor skills.
Research methodology
Context – skills fair intervention.
According to Roberts et al. (2009) , psychomotor skills decline over time even among licensed experienced professionals within as little as two weeks and may need to be relearned within two months without performing a skill. When applying this concept to student nurses for whom each skill is new, it is no wonder their competency result is diminished after having a summer break from nursing school. This skills fair intervention is a one-day event to assist baccalaureate students who had taken the summer off from their studies in nursing and all faculty participated in operating the stations. It incorporated evidence-based practice rationale with critical thinking prompts using Socratic questioning, evidence-based practice videos to the psychomotor skill rubrics, group work, guided discussions, expert demonstration followed by guided practice and blended learning in an attempt to promote and develop critical thinking in baccalaureate students.
Students were scheduled and placed randomly into eight teams based on attributes of critical thinking as described by Wittmann-Price (2013) : Team A – Perseverance, Team B – Flexibility, Team C – Confidence, Team D – Creativity, Team E – Inquisitiveness, Team F – Reflection, Team G – Analyzing and Team H – Intuition. The students rotated every 20 minutes through eight stations: Medication Administration: Intramuscular and Subcutaneous Injections, Initiating Intravenous Therapy, ten-minute Focused Physical Assessment, Foley Catheter Insertion, Nasogastric Intubation, Skin Assessment/Braden Score and Restraints, Vital Signs and a Safety Station. When the students completed all eight stations, they went to the “Check-Out” booth to complete a simple evaluation to determine their perceptions of the effectiveness of the innovative intervention. When the evaluations were complete, each of the eight critical thinking attribute teams placed their index cards into a hat, and a student won a small prize. All Junior 2, Senior 1 and Senior 2 students were required to attend the Skills Fair. The Skills Fair Team strove to make the event as festive as possible, engaging nursing students with balloons, candy, tri-boards, signs and fun pre and postactivities. The Skills Fair rubrics, scheduling and instructions were shared electronically with students and faculty before the skills fair intervention to ensure adequate preparation and continuous resource availability as students move forward into their future clinical settings.
Research design
Institutional review board (IRB) approval was obtained from XXX University to conduct this study and protect human subject rights. The explanatory sequential mixed-methods design was employed for this study. The design was chosen to identify what effects a skills fair intervention that had on senior baccalaureate nursing students' achievements on the Kaplan Critical Thinking Integrated Test (KCTIT) and then follow up with individual interviews to explore those test results in more depth. In total, 52 senior nursing students completed the KCTIT; 30 of them participated in the skills fair intervention and 22 of them did not participate. The KCTIT is a computerized 85-item exam in which 85 equates to 100%, making each question worth one point. It has high reliability and validity ( Kaplan Nursing, 2012 ; Swing, 2014 ). The reliability value of the KCTIT ranged from 0.72 to 0.89. A t -test was used to analyze the test results.
A total of 11 participants were purposefully selected based on a range of six high achievers and five low achievers on the KCTIT for open-ended one-on-one interviews. Each interview was conducted individually and lasted for about 60 minutes. An open-ended interview protocol was used to guide the flow of data collection. The interviewees' ages ranged from 21 to 30 years, with an average of 24 years. One of 11 interviewees was male. Among them, seven were White, three were Black and one was Indian American. The data collected were used to answer the following research questions: (1) What was the difference in achievements on the KCTIT among senior baccalaureate nursing students who participated in the skills fair intervention and students who did not participate? (2) What were the senior baccalaureate nursing students' perceptions of internal and external factors impacting the development of critical thinking skills during the skills fair intervention? and (3) What were the senior baccalaureate nursing students' perceptions of the skills fair intervention as a critical thinking developmental strategy?
Inductive content analysis was used to analyze interview data by starting with the close reading of the transcripts and writing memos for initial coding, followed by an analysis of patterns and relationships among the data for focused coding. The intercoder reliability was established for qualitative data analysis with a nursing expert. The lead researcher and the expert read the transcript several times and assigned a code to significant units of text that corresponded with answering the research questions. The codes were compared based on differences and similarities and sorted into subcategories and categories. Then, headings and subheadings were used based on similar comments to develop central themes and patterns. The process of establishing intercoder reliability helped to increase dependability, conformability and credibility of the findings ( Graneheim and Lundman, 2004 ). In addition, methods of credibility, confirmability, dependability and transferability were applied to increase the trustworthiness of this study ( Graneheim and Lundman, 2004 ). First, reflexivity was observed by keeping journals and memos. This practice allowed the lead researcher to reflect on personal views to minimize bias. Data saturation was reached through following the recommended number of participants as well as repeated immersion in the data during analysis until no new data surfaced. Member checking was accomplished through returning the transcript and the interpretation to the participants to check the accuracy and truthfulness of the findings. Finally, proper documentation was conducted to allow accurate crossreferencing throughout the study.
Quantitative results
Results for the quantitative portion showed there was no difference in scores on the KCTIT between senior nursing students who participated in the skills fair intervention and senior nursing students who did not participate, t (50) = −0.174, p = 0.86 > 0.05. The test scores between the nonparticipant group ( M = 67.59, SD = 5.81) and the participant group ( M = 67.88, SD = 5.99) were almost equal.
Qualitative results
Initial coding.
The results from the initial coding and generated themes are listed in Table 1 . First, the participants perceived the skills fair intervention as “promoting experience” and “confidence” by practicing previously learned knowledge and reinforcing it with active learning strategies. Second, the participants perceived the skills fair intervention as a relaxed, nonthreatening learning environment due to the festive atmosphere, especially in comparison to other learning experiences in the nursing program. The nonthreatening environment of the skills fair intervention allowed students to learn without fear. Third, the majority of participants believed their critical thinking was strengthened after participating. Several participants believed their perception of critical thinking was “enhanced” or “reinforced” rather than significantly changed.
Focused coding results
The final themes were derived from the analysis of patterns and relationships among the content of the data using inductive content analysis ( Saldana, 2009 ). The following was examined across the focused coding process: (1) factors impacting critical thinking skills development during skills fair intervention and (2) skills fair intervention a critical thinking skills developmental strategy.
Factors impacting critical thinking skills development . The factors impacting the development of critical thinking during the skills fair intervention were divided into two themes: internal factors and external factors. The internal factors were characteristics innate to the students. The identified internal factors were (1) confidence and anxiety levels, (2) attitude and (3) age. The external factors were the outside influences that affected the students. The external factors were (1) experience and practice, (2) faculty involvement, (3) positive learning environment and (4) faculty prompts.
I think that confidence and anxiety definitely both have a huge impact on your ability to be able to really critically think. If you start getting anxious and panicking you cannot think through the process like you need too. I do not really think gender or age necessarily would have anything to do with critical thinking.
Definitely the confidence level, I think, the more advanced you get in the program, your confidence just keeps on growing. Level of anxiety, definitely… I think the people who were in the Skills Fair for the first time, had more anxiety because they did not really know to think, they did not know how strict it was going to be, or if they really had to know everything by the book. I think the Skills Fair helped everyone's confidence levels, but especially the Jr. 2's.
Attitude was an important factor in the development of critical thinking skills during the skills fair intervention as participants believed possessing a pleasant and positive attitude meant a student was eager to learn, participate, accept responsibility for completing duties and think seriously. Participant 6 believed attitude contributed to performance in the Skills Fair.
I feel like, certain things bring critical thinking out in you. And since I'm a little bit older than some of the other students, I have had more life experiences and am able to figure stuff out better. Older students have had more time to learn by trial and error, and this and that.
Like when I had clinical with you, you'd always tell us to know our patients' medications. To always know and be prepared to answer questions – because at first as a Junior 1 we did not do that in the clinical setting… and as a Junior 2, I did not really have to know my medications, but with you as a Senior 1, I started to realize that the patients do ask about their meds, so I was making sure that I knew everything before they asked it. And just having more practice with IVs – at first, I was really nervous, but when I got to my preceptorship – I had done so many IVs and with all of the practice, it just built up my confidence with that skill so when I performed that skill during the Fair, I was confident due to my clinical experiences and able to think and perform better.
I think teachers will always affect the ability to critically think just because you want [to] get the right answer because they are there and you want to seem smart to them [Laugh]. Also, if you are leading in the wrong direction of your thinking – they help steer you back to [in] the right direction so I think that was very helpful.
You could tell the faculty really tried to make it more laid back and fun, so everybody would have a good experience. The faculty had a good attitude. I think making it fun and active helped keep people positive. You know if people are negative and not motivated, nothing gets accomplished. The faculty did an amazing job at making the Skills Fair a positive atmosphere.
However, for some of the participants, a positive learning environment depended on their fellow students. The students were randomly assigned alphabetically to groups, and the groups were assigned to starting stations at the Skills Fair. The participants claimed some students did not want to participate and displayed cynicism toward the intervention. The participants believed their cynicism affected the positive learning environment making critical thinking more difficult during the Skills Fair.
Okay, when [instructor name] was demonstrating the Chevron technique right after we inserted the IV catheter and we were trying to secure the catheter, put on the extension set, and flush the line at what seemed to be all at the same time. I forgot about how you do not want to put the tape right over the hub of the catheter because when you go back in and try to assess the IV site – you're trying to assess whether or not it is patent or infiltrated – you have to visualize the insertion site. That was one of the things that I had been doing wrong because I was just so excited that I got the IV in the vein in the first place – that I did not think much about the tape or the tegaderm for sterility. So I think an important part of critical thinking is to be able to recognize when you've made a mistake and stop, stop yourself from doing it in the future (see Table 2 ).
Skills fair intervention as a developmental strategy for critical thinking . The participants identified the skills fair intervention was effective as a developmental strategy for critical thinking, as revealed in two themes: (1) develops alternative thinking and (2) thinking before doing (See Table 3 ).
Develops alternative thinking . The participants perceived the skills fair intervention helped enhance critical thinking and confidence by developing alternative thinking. Alternative thinking was described as quickly thinking of alternative solutions to problems based on the latest evidence and using that information to determine what actions were warranted to prevent complications and prevent injury. It helped make better connections through the learning of rationale between knowledge and skills and then applying that knowledge to prevent complications and errors to ensure the safety of patients. The participants stated the learning of rationale for certain procedures provided during the skills fair intervention such as the evidence and critical thinking prompts included in the rubrics helped reinforce this connection. The participants also shared they developed alternative thinking after participating in the skills fair intervention by noticing trends in data to prevent potential complications from the faculty prompts. Participant 1 stated her instructor prompted her alternative thinking through questioning about noticing trends to prevent potential complications. She said the following:
Another way critical thinking occurred during the skills fair was when [instructor name] was teaching and prompted us about what it would be like to care for a patient with a fractured hip – I think this was at the 10-minute focused assessment station, but I could be wrong. I remember her asking, “What do you need to be on the look-out for? What can go wrong?” I automatically did not think critically very well and was only thinking circulation in the leg, dah, dah, dah. But she was prompting us to think about mobility alterations and its effect on perfusion and oxygenation. She was trying to help us build those connections. And I think that's a lot of the aspects of critical thinking that gets overlooked with the nursing student – trouble making connections between our knowledge and applying it in practice.
Thinking before doing . The participants perceived thinking before doing, included thinking of how and why certain procedures, was necessary through self-examination prior to taking action. The hands-on situational learning allowed the participants in the skills fair intervention to better notice assessment data and think at a higher level as their previous learning of the skills was perceived as memorization of steps. This higher level of learning allowed participants to consider different future outcomes and analyze pertinent data before taking action.
I think what helped me the most is considering outcomes of my actions before I do anything. For instance, if you're thinking, “Okay. Well, I need to check their blood pressure before I administer this blood pressure medication – or the blood pressure could potentially bottom out.” I really do not want my patient to bottom out and get hypotensive because I administered a medication that was ordered, but not safe to give. I could prevent problems from happening if I know what to be on alert for and act accordingly. So ultimately knowing that in the clinical setting, I can prevent complications from happening and I save myself, my license, and promote patient safety. I think knowing that I've seen the importance of critical thinking already in practice has helped me value and understand why I should be critically thinking. Yes, we use the 5-rights of medication safety – but we also have to think. For instance, if I am going to administer insulin – what do I need to know or do to give this safely? What is the current blood sugar? Has the patient been eating? When is the next meal scheduled? Is the patient NPO for a procedure? Those are examples of questions to consider and the level of thinking that needs to take place prior to taking actions in the clinical setting.
Although the results of quantitative data showed no significant difference in scores on the KCTIT between the participant and nonparticipant groups, during the interviews some participants attributed this result to the test not being part of a course grade and believed students “did not try very hard to score well.” However, the participants who attended interviews did identify the skills fair intervention as a developmental strategy for critical thinking by helping them develop alternative thinking and thinking before doing. The findings are supported in the literature as (1) nurses must recognize signs of clinical deterioration and take action promptly to prevent potential complications ( Garvey and CNE series 2015 ) and (2) nurses must analyze pertinent data and consider all possible solutions before deciding on the most appropriate action for each patient ( Papathanasiou et al. , 2014 ).
The skills fair intervention also enhanced the development of self-confidence by participants practicing previously learned skills in a controlled, safe environment. The nonthreatening environment of the skills fair intervention allowed students to learn without fear and the majority of participants believed their critical thinking was strengthened after participating. The interview data also revealed a combination of internal and external factors that influenced the development of critical thinking during the skills fair intervention including confidence and anxiety levels, attitude, age, experience and practice, faculty involvement, positive learning environment and faculty prompts. These factors should be considered when addressing the promotion and development of critical thinking.
Conclusions, limitations and recommendations
A major concern in the nursing profession is the lack of critical thinking in student nurses and new graduates, which influences the decision-making of novice nurses and directly affects patient care and safety ( Saintsing et al. , 2011 ). Nurse educators must use evidence-based practice to prepare students to critically think with the complicated and constantly evolving environment of health care today ( Goodare, 2015 ; Newton and Moore, 2013 ). Evidence-based practice has been advocated to promote critical thinking ( Profetto-McGrath, 2005 ; Stanley and Dougherty, 2010 ). The skills fair intervention can be one type of evidence-based practice used to promote critical thinking ( McCausland and Meyers, 2013 ; Roberts et al. , 2009 ). The Intervention used in this study incorporated evidence-based practice rationale with critical thinking prompts using Socratic questioning, evidence-based practice videos to the psychomotor skill rubrics, group work, guided discussions, expert demonstration followed by guided practice and blended learning in an attempt to promote and develop critical thinking in nursing students.
The explanatory sequential mixed-methods design was employed to investigate the effects of the innovative skills fair intervention on senior baccalaureate nursing students' achievements and their perceptions of critical thinking skills development. Although the quantitative results showed no significant difference in scores on the KCTIT between students who participated in the skills fair intervention and those who did not, those who attended the interviews perceived their critical thinking was reinforced after the skills fair intervention and believed it was an effective developmental strategy for critical thinking, as it developed alternative thinking and thinking before doing. This information is useful for nurse educators who plan their own teaching practice to promote critical thinking and improve patient outcomes. The findings also provide schools and educators information that helps review their current approach in educating nursing students. As evidenced in the findings, the importance of developing critical thinking skills is crucial for becoming a safe, professional nurse. Internal and external factors impacting the development of critical thinking during the skills fair intervention were identified including confidence and anxiety levels, attitude, age, experience and practice, faculty involvement, positive learning environment and faculty prompts. These factors should be considered when addressing the promotion and development of critical thinking.
There were several limitations to this study. One of the major limitations of the study was the limited exposure of students' time of access to the skills fair intervention, as it was a one-day learning intervention. Another limitation was the sample selection and size. The skills fair intervention was limited to only one baccalaureate nursing program in one southeastern state. As such, the findings of the study cannot be generalized as it may not be representative of baccalaureate nursing programs in general. In addition, this study did not consider students' critical thinking achievements prior to the skills fair intervention. Therefore, no baseline measurement of critical thinking was available for a before and after comparison. Other factors in the nursing program could have affected the students' scores on the KCTIT, such as anxiety or motivation that was not taken into account in this study.
The recommendations for future research are to expand the topic by including other regions, larger samples and other baccalaureate nursing programs. In addition, future research should consider other participant perceptions, such as nurse educators, to better understand the development and growth of critical thinking skills among nursing students. Finally, based on participant perceptions, future research should include a more rigorous skills fair intervention to develop critical thinking and explore the link between confidence and critical thinking in nursing students.
Initial coding results
Factors impacting critical thinking skill development during skills fair intervention
Skills fair intervention as a developmental strategy for critical thinking
American Nephrology Nurses Association (ANNA) ( 2019 ), “ Learning, leading, connecting, and playing at the intersection of nephrology and nursing-2019–2020 strategic plan ”, viewed 3 Aug 2019, available at: https://www.annanurse.org/download/reference/association/strategicPlan.pdf .
Arli , S.D. , Bakan , A.B. , Ozturk , S. , Erisik , E. and Yildirim , Z. ( 2017 ), “ Critical thinking and caring in nursing students ”, International Journal of Caring Sciences , Vol. 10 No. 1 , pp. 471 - 478 .
Benner , P. , Sutphen , M. , Leonard , V. and Day , L. ( 2010 ), Educating Nurses: A Call for Radical Transformation , Jossey-Bass , San Francisco .
Brunt , B. ( 2005 ), “ Critical thinking in nursing: an integrated review ”, The Journal of Continuing Education in Nursing , Vol. 36 No. 2 , pp. 60 - 67 .
Chun-Chih , L. , Chin-Yen , H. , I-Ju , P. and Li-Chin , C. ( 2015 ), “ The teaching-learning approach and critical thinking development: a qualitative exploration of Taiwanese nursing students ”, Journal of Professional Nursing , Vol. 31 No. 2 , pp. 149 - 157 , doi: 10.1016/j.profnurs.2014.07.001 .
Clarke , L.W. and Whitney , E. ( 2009 ), “ Walking in their shoes: using multiple-perspectives texts as a bridge to critical literacy ”, The Reading Teacher , Vol. 62 No. 6 , pp. 530 - 534 , doi: 10.1598/RT.62.6.7 .
Dykstra , D. ( 2008 ), “ Integrating critical thinking and memorandum writing into course curriculum using the internet as a research tool ”, College Student Journal , Vol. 42 No. 3 , pp. 920 - 929 , doi: 10.1007/s10551-010-0477-2 .
Ebright , P. , Urden , L. , Patterson , E. and Chalko , B. ( 2004 ), “ Themes surrounding novice nurse near-miss and adverse-event situations ”, The Journal of Nursing Administration: The Journal of Nursing Administration , Vol. 34 , pp. 531 - 538 , doi: 10.1097/00005110-200411000-00010 .
Ennis , R. ( 2011 ), “ The nature of critical thinking: an outline of critical thinking dispositions and abilities ”, viewed 3 May 2017, available at: https://education.illinois.edu/docs/default-source/faculty-documents/robert-ennis/thenatureofcriticalthinking_51711_000.pdf .
Facione , P.A. ( 1990 ), Critical Thinking: A Statement of Expert Consensus for Purposes of Educational Assessment and Instruction , The California Academic Press , Millbrae .
Facione , N.C. and Facione , P.A. ( 2013 ), The Health Sciences Reasoning Test: Test Manual , The California Academic Press , Millbrae .
Fero , L.J. , Witsberger , C.M. , Wesmiller , S.W. , Zullo , T.G. and Hoffman , L.A. ( 2009 ), “ Critical thinking ability of new graduate and experienced nurses ”, Journal of Advanced Nursing , Vol. 65 No. 1 , pp. 139 - 148 , doi: 10.1111/j.1365-2648.2008.04834.x .
Garvey , P.K. and CNE series ( 2015 ), “ Failure to rescue: the nurse's impact ”, Medsurg Nursing , Vol. 24 No. 3 , pp. 145 - 149 .
Goodare , P. ( 2015 ), “ Literature review: ‘are you ok there?’ The socialization of student and graduate nurses: do we have it right? ”, Australian Journal of Advanced Nursing , Vol. 33 No. 1 , pp. 38 - 43 .
Graneheim , U.H. and Lundman , B. ( 2014 ), “ Qualitative content analysis in nursing research: concepts, procedures, and measures to achieve trustworthiness ”, Nurse Education Today , Vol. 24 No. 2 , pp. 105 - 12 , doi: 10.1016/j.nedt.2003.10.001 .
Hsu , L. and Hsieh , S. ( 2013 ), “ Factors affecting metacognition of undergraduate nursing students in a blended learning environment ”, International Journal of Nursing Practice , Vol. 20 No. 3 , pp. 233 - 241 , doi: 10.1111/ijn.12131 .
Ignatavicius , D. ( 2001 ), “ Six critical thinking skills for at-the-bedside success ”, Dimensions of Critical Care Nursing , Vol. 20 No. 2 , pp. 30 - 33 .
Institute of Medicine ( 2001 ), Crossing the Quality Chasm: A New Health System for the 21st Century , National Academy Press , Washington .
James , J. ( 2013 ), “ A new, evidence-based estimate of patient harms associated with hospital care ”, Journal of Patient Safety , Vol. 9 No. 3 , pp. 122 - 128 , doi: 10.1097/PTS.0b013e3182948a69 .
Jones , J.H. ( 2010 ), “ Developing critical thinking in the perioperative environment ”, AORN Journal , Vol. 91 No. 2 , pp. 248 - 256 , doi: 10.1016/j.aorn.2009.09.025 .
Kaplan Nursing ( 2012 ), Kaplan Nursing Integrated Testing Program Faculty Manual , Kaplan Nursing , New York, NY .
Kim , J.S. , Gu , M.O. and Chang , H.K. ( 2019 ), “ Effects of an evidence-based practice education program using multifaceted interventions: a quasi-experimental study with undergraduate nursing students ”, BMC Medical Education , Vol. 19 , doi: 10.1186/s12909-019-1501-6 .
Longton , S. ( 2014 ), “ Utilizing evidence-based practice for patient safety ”, Nephrology Nursing Journal , Vol. 41 No. 4 , pp. 343 - 344 .
McCausland , L.L. and Meyers , C.C. ( 2013 ), “ An interactive skills fair to prepare undergraduate nursing students for clinical experience ”, Nursing Education Perspectives , Vol. 34 No. 6 , pp. 419 - 420 , doi: 10.5480/1536-5026-34.6.419 .
McMullen , M.A. and McMullen , W.F. ( 2009 ), “ Examining patterns of change in the critical thinking skills of graduate nursing students ”, Journal of Nursing Education , Vol. 48 No. 6 , pp. 310 - 318 , doi: 10.3928/01484834-20090515-03 .
Moore , Z.E. ( 2007 ), “ Critical thinking and the evidence-based practice of sport psychology ”, Journal of Clinical Sport Psychology , Vol. 1 , pp. 9 - 22 , doi: 10.1123/jcsp.1.1.9 .
Nadelson , S. and Nadelson , L.S. ( 2014 ), “ Evidence-based practice article reviews using CASP tools: a method for teaching EBP ”, Worldviews on Evidence-Based Nursing , Vol. 11 No. 5 , pp. 344 - 346 , doi: 10.1111/wvn.12059 .
Newton , S.E. and Moore , G. ( 2013 ), “ Critical thinking skills of basic baccalaureate and accelerated second-degree nursing students ”, Nursing Education Perspectives , Vol. 34 No. 3 , pp. 154 - 158 , doi: 10.5480/1536-5026-34.3.154 .
Nibert , A. ( 2011 ), “ Nursing education and practice: bridging the gap ”, Advance Healthcare Network , viewed 3 May 2017, available at: https://www.elitecme.com/resource-center/nursing/nursing-education-practice-bridging-the-gap/ .
Oermann , M.H. , Kardong-Edgren , S. , Odom-Maryon , T. , Hallmark , B.F. , Hurd , D. , Rogers , N. and Smart , D.A. ( 2011 ), “ Deliberate practice of motor skills in nursing education: CPR as exemplar ”, Nursing Education Perspectives , Vol. 32 No. 5 , pp. 311 - 315 , doi: 10.5480/1536-5026-32.5.311 .
Papathanasiou , I.V. , Kleisiaris , C.F. , Fradelos , E.C. , Kakou , K. and Kourkouta , L. ( 2014 ), “ Critical thinking: the development of an essential skill for nursing students ”, Acta Informatica Medica , Vol. 22 No. 4 , pp. 283 - 286 , doi: 10.5455/aim.2014.22.283-286 .
Park , M.Y. , Conway , J. and McMillan , M. ( 2016 ), “ Enhancing critical thinking through simulation ”, Journal of Problem-Based Learning , Vol. 3 No. 1 , pp. 31 - 40 , doi: 10.24313/jpbl.2016.3.1.31 .
Paul , R. ( 1993 ), Critical Thinking: How to Prepare Students for a Rapidly Changing World , The Foundation for Critical Thinking , Santa Rosa .
Paul , R. and Elder , L. ( 2008 ), “ Critical thinking: the art of socratic questioning, part III ”, Journal of Developmental Education , Vol. 31 No. 3 , pp. 34 - 35 .
Paul , R. and Elder , L. ( 2012 ), Critical Thinking: Tools for Taking Charge of Your Learning and Your Life , 3rd ed. , Pearson/Prentice Hall , Boston .
Profetto-McGrath , J. ( 2005 ), “ Critical thinking and evidence-based practice ”, Journal of Professional Nursing , Vol. 21 No. 6 , pp. 364 - 371 , doi: 10.1016/j.profnurs.2005.10.002 .
Rahman , A. and Applebaum , R. ( 2011 ), “ What's all this about evidence-based practice? The roots, the controversies, and why it matters ”, American Society on Aging , viewed 3 May 2017, available at: https://www.asaging.org/blog/whats-all-about-evidence-based-practice-roots-controversies-and-why-it-matters .
Rieger , K. , Chernomas , W. , McMillan , D. , Morin , F. and Demczuk , L. ( 2015 ), “ The effectiveness and experience of arts‐based pedagogy among undergraduate nursing students: a comprehensive systematic review protocol ”, JBI Database of Systematic Reviews and Implementation Reports , Vol. 13 No. 2 , pp. 101 - 124 , doi: 10.11124/jbisrir-2015-1891 .
Robert , R.R. and Petersen , S. ( 2013 ), “ Critical thinking at the bedside: providing safe passage to patients ”, Medsurg Nursing , Vol. 22 No. 2 , pp. 85 - 118 .
Roberts , S.T. , Vignato , J.A. , Moore , J.L. and Madden , C.A. ( 2009 ), “ Promoting skill building and confidence in freshman nursing students with a skills-a-thon ”, Educational Innovations , Vol. 48 No. 8 , pp. 460 - 464 , doi: 10.3928/01484834-20090518-05 .
Romeo , E. ( 2010 ), “ Quantitative research on critical thinking and predicting nursing students' NCLEX-RN performance ”, Journal of Nursing Education , Vol. 49 No. 7 , pp. 378 - 386 , doi: 10.3928/01484834-20100331-05 .
Sackett , D. , Rosenberg , W. , Gray , J. , Haynes , R. and Richardson , W. ( 1996 ), “ Evidence-based medicine: what it is and what it isn't ”, British Medical Journal , Vol. 312 No. 7023 , pp. 71 - 72 , doi: 10.1136/bmj.312.7023.71 .
Saintsing , D. , Gibson , L.M. and Pennington , A.W. ( 2011 ), “ The novice nurse and clinical decision-making: how to avoid errors ”, Journal of Nursing Management , Vol. 19 No. 3 , pp. 354 - 359 .
Saldana , J. ( 2009 ), The Coding Manual for Qualitative Researchers , Sage , Los Angeles .
Scheffer , B. and Rubenfeld , M. ( 2000 ), “ A consensus statement on critical thinking in nursing ”, Journal of Nursing Education , Vol. 39 No. 8 , pp. 352 - 359 .
Stanley , M.C. and Dougherty , J.P. ( 2010 ), “ Nursing education model. A paradigm shift in nursing education: a new model ”, Nursing Education Perspectives , Vol. 31 No. 6 , pp. 378 - 380 , doi: 10.1043/1536-5026-31.6.378 .
Swing , V.K. ( 2014 ), “ Early identification of transformation in the proficiency level of critical thinking skills (CTS) for the first-semester associate degree nursing (ADN) student ”, doctoral thesis , Capella University , Minneapolis , viewed 3 May 2017, ProQuest Dissertations & Theses database .
Turner , P. ( 2005 ), “ Critical thinking in nursing education and practice as defined in the literature ”, Nursing Education Perspectives , Vol. 26 No. 5 , pp. 272 - 277 .
Twibell , R. , St Pierre , J. , Johnson , D. , Barton , D. , Davis , C. and Kidd , M. ( 2012 ), “ Tripping over the welcome mat: why new nurses don't stay and what the evidence says we can do about it ”, American Nurse Today , Vol. 7 No. 6 , pp. 1 - 10 .
Watson , G. and Glaser , E.M. ( 1980 ), Watson Glaser Critical Thinking Appraisal , Psychological Corporation , San Antonio .
Wittmann-Price , R.A. ( 2013 ), “ Facilitating learning in the classroom setting ”, in Wittmann-Price , R.A. , Godshall , M. and Wilson , L. (Eds), Certified Nurse Educator (CNE) Review Manual , Springer Publishing , New York, NY , pp. 19 - 70 .
Corresponding author
Related articles, we’re listening — tell us what you think, something didn’t work….
Report bugs here
All feedback is valuable
Please share your general feedback
Join us on our journey
Platform update page.
Visit emeraldpublishing.com/platformupdate to discover the latest news and updates
Questions & More Information
Answers to the most commonly asked questions here
Florence Nightingale's theory and her contributions to holistic critical thinking in nursing
Affiliations.
- 1 Universidade Federal de Santa Catarina. Florianópolis, Santa Catarina, Brazil.
- 2 Universidade Federal do Rio Grande do Sul. Porto Alegre, Rio Grande do Sul, Brazil.
- 3 Lovisenberg Diakonale Høgskole. Oslo, Noruega.
- PMID: 33950115
- DOI: 10.1590/0034-7167-2020-0139
Objective: to reflect on Florence Nightingale's legacy and describe her contributions to critical holistic thinking in nursing.
Methods: this is a theoretical reflection, for which scientific productions on Florence Nightingale's environmental theory, as published in national and international journals, were based.
Results: Florence Nightingale's philosophy and teachings emphasize that the nurse must use her brain, heart and hands to create healing environments to care for the patient's body, mind and spirit. Nursing, since the time of Nightingale, has been building the holistic paradigm, in all schools of thought, with a view to a humanistic approach to the human being in their indivisible relationship with the environment.
Final considerations: Florence's contributions to holistic critical thinking in nursing are evident, constituting nurses' differential in clinical practice.
Publication types
- Historical Article
- History, 19th Century
- Nursing Theory
The Value of Critical Thinking in Nursing

- How Nurses Use Critical Thinking
- How to Improve Critical Thinking
- Common Mistakes

Some experts describe a person’s ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation.
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as “necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation.”
“This cognitive process is vital for excellent patient outcomes because it requires that nurses make clinical decisions utilizing a variety of different lenses, such as fairness, ethics, and evidence-based practice,” he says.
How Do Nurses Use Critical Thinking?
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Nurses care for many patients during their shifts. Strong critical thinking skills are crucial when juggling various tasks so patient safety and care are not compromised.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
“Nurses must also critically think to determine which patient to see first, which medications to pass first, and the order in which to organize their day caring for patients. Patient conditions and environments are continually in flux, therefore nurses must constantly be evaluating and re-evaluating information they gather (assess) to keep their patients safe.”
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator. She observed critical thinking throughout the pandemic as she watched intensive care nurses test the boundaries of previously held beliefs and master providing excellent care while preserving resources.
“Nurses are at the patient’s bedside and are often the first ones to detect issues. Then, the nurse needs to gather the appropriate subjective and objective data from the patient in order to frame a concise problem statement or question for the physician or advanced practice provider,” she explains.
Top 5 Ways Nurses Can Improve Critical Thinking Skills
We asked our experts for the top five strategies nurses can use to purposefully improve their critical thinking skills.
Case-Based Approach
Slaughter is a fan of the case-based approach to learning critical thinking skills.
In much the same way a detective would approach a mystery, she mentors her students to ask questions about the situation that help determine the information they have and the information they need. “What is going on? What information am I missing? Can I get that information? What does that information mean for the patient? How quickly do I need to act?”
Consider forming a group and working with a mentor who can guide you through case studies. This provides you with a learner-centered environment in which you can analyze data to reach conclusions and develop communication, analytical, and collaborative skills with your colleagues.
Practice Self-Reflection
Rhoads is an advocate for self-reflection. “Nurses should reflect upon what went well or did not go well in their workday and identify areas of improvement or situations in which they should have reached out for help.” Self-reflection is a form of personal analysis to observe and evaluate situations and how you responded.
This gives you the opportunity to discover mistakes you may have made and to establish new behavior patterns that may help you make better decisions. You likely already do this. For example, after a disagreement or contentious meeting, you may go over the conversation in your head and think about ways you could have responded.
It’s important to go through the decisions you made during your day and determine if you should have gotten more information before acting or if you could have asked better questions.
During self-reflection, you may try thinking about the problem in reverse. This may not give you an immediate answer, but can help you see the situation with fresh eyes and a new perspective. How would the outcome of the day be different if you planned the dressing change in reverse with the assumption you would find a wound infection? How does this information change your plan for the next dressing change?
Develop a Questioning Mind
McGowan has learned that “critical thinking is a self-driven process. It isn’t something that can simply be taught. Rather, it is something that you practice and cultivate with experience. To develop critical thinking skills, you have to be curious and inquisitive.”
To gain critical thinking skills, you must undergo a purposeful process of learning strategies and using them consistently so they become a habit. One of those strategies is developing a questioning mind. Meaningful questions lead to useful answers and are at the core of critical thinking .
However, learning to ask insightful questions is a skill you must develop. Faced with staff and nursing shortages , declining patient conditions, and a rising number of tasks to be completed, it may be difficult to do more than finish the task in front of you. Yet, questions drive active learning and train your brain to see the world differently and take nothing for granted.
It is easier to practice questioning in a non-stressful, quiet environment until it becomes a habit. Then, in the moment when your patient’s care depends on your ability to ask the right questions, you can be ready to rise to the occasion.
Practice Self-Awareness in the Moment
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. Passing medication, changing dressings, and hanging intravenous lines all while trying to assess your patient’s mental and emotional status can affect your focus and how you manage stress as a nurse .
Staying present helps you to be proactive in your thinking and anticipate what might happen, such as bringing extra lubricant for a catheterization or extra gloves for a dressing change.
By staying present, you are also better able to practice active listening. This raises your assessment skills and gives you more information as a basis for your interventions and decisions.
Use a Process
As you are developing critical thinking skills, it can be helpful to use a process. For example:
- Ask questions.
- Gather information.
- Implement a strategy.
- Evaluate the results.
- Consider another point of view.
These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
Common Critical Thinking Pitfalls in Nursing
Your brain uses a set of processes to make inferences about what’s happening around you. In some cases, your unreliable biases can lead you down the wrong path. McGowan places personal biases at the top of his list of common pitfalls to critical thinking in nursing.
“We all form biases based on our own experiences. However, nurses have to learn to separate their own biases from each patient encounter to avoid making false assumptions that may interfere with their care,” he says. Successful critical thinkers accept they have personal biases and learn to look out for them. Awareness of your biases is the first step to understanding if your personal bias is contributing to the wrong decision.
New nurses may be overwhelmed by the transition from academics to clinical practice, leading to a task-oriented mindset and a common new nurse mistake ; this conflicts with critical thinking skills.
“Consider a patient whose blood pressure is low but who also needs to take a blood pressure medication at a scheduled time. A task-oriented nurse may provide the medication without regard for the patient’s blood pressure because medication administration is a task that must be completed,” Slaughter says. “A nurse employing critical thinking skills would address the low blood pressure, review the patient’s blood pressure history and trends, and potentially call the physician to discuss whether medication should be withheld.”
Fear and pride may also stand in the way of developing critical thinking skills. Your belief system and worldview provide comfort and guidance, but this can impede your judgment when you are faced with an individual whose belief system or cultural practices are not the same as yours. Fear or pride may prevent you from pursuing a line of questioning that would benefit the patient. Nurses with strong critical thinking skills exhibit:
- Learn from their mistakes and the mistakes of other nurses
- Look forward to integrating changes that improve patient care
- Treat each patient interaction as a part of a whole
- Evaluate new events based on past knowledge and adjust decision-making as needed
- Solve problems with their colleagues
- Are self-confident
- Acknowledge biases and seek to ensure these do not impact patient care
An Essential Skill for All Nurses
Critical thinking in nursing protects patient health and contributes to professional development and career advancement. Administrative and clinical nursing leaders are required to have strong critical thinking skills to be successful in their positions.
By using the strategies in this guide during your daily life and in your nursing role, you can intentionally improve your critical thinking abilities and be rewarded with better patient outcomes and potential career advancement.
Frequently Asked Questions About Critical Thinking in Nursing
How are critical thinking skills utilized in nursing practice.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient’s cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the situation.
How does nursing school develop critical thinking skills?
Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient’s overall well-being. Learners also participate in supervised clinical experiences, where they practice using their critical thinking skills to make decisions in professional settings.
Do only nurse managers use critical thinking?
Nurse managers certainly use critical thinking skills in their daily duties. But when working in a health setting, anyone giving care to patients uses their critical thinking skills. Everyone — including licensed practical nurses, registered nurses, and advanced nurse practitioners —needs to flex their critical thinking skills to make potentially life-saving decisions.
Meet Our Contributors

Crystal Slaughter, DNP, APRN, ACNS-BC, CNE
Crystal Slaughter is a core faculty member in Walden University’s RN-to-BSN program. She has worked as an advanced practice registered nurse with an intensivist/pulmonary service to provide care to hospitalized ICU patients and in inpatient palliative care. Slaughter’s clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care.

Jenna Liphart Rhoads, Ph.D., RN
Jenna Liphart Rhoads is a nurse educator and freelance author and editor. She earned a BSN from Saint Francis Medical Center College of Nursing and an MS in nursing education from Northern Illinois University. Rhoads earned a Ph.D. in education with a concentration in nursing education from Capella University where she researched the moderation effects of emotional intelligence on the relationship of stress and GPA in military veteran nursing students. Her clinical background includes surgical-trauma adult critical care, interventional radiology procedures, and conscious sedation in adult and pediatric populations.

Nicholas McGowan, BSN, RN, CCRN
Nicholas McGowan is a critical care nurse with 10 years of experience in cardiovascular, surgical intensive care, and neurological trauma nursing. McGowan also has a background in education, leadership, and public speaking. He is an online learner who builds on his foundation of critical care nursing, which he uses directly at the bedside where he still practices. In addition, McGowan hosts an online course at Critical Care Academy where he helps nurses achieve critical care (CCRN) certification.
- Open access
- Published: 26 March 2024
The effect of “typical case discussion and scenario simulation” on the critical thinking of midwifery students: Evidence from China
- Yuji Wang 1 na1 ,
- Yijuan Peng 1 na1 &
- Yan Huang 1
BMC Medical Education volume 24 , Article number: 340 ( 2024 ) Cite this article
Metrics details
Assessment ability lies at the core of midwives’ capacity to judge and treat clinical problems effectively. Influenced by the traditional teaching method of “teacher-led and content-based”, that teachers involve imparting a large amount of knowledge to students and students lack active thinking and active practice, the clinical assessment ability of midwifery students in China is mostly at a medium or low level. Improving clinical assessment ability of midwifery students, especially critical thinking, is highly important in practical midwifery education. Therefore, we implemented a new teaching program, “typical case discussion and scenario simulation”, in the Midwifery Health Assessment course. Guided by typical cases, students were organized to actively participate in typical case discussions and to promote active thinking and were encouraged to practice actively through scenario simulation. In this study, we aimed to evaluate the effect of this strategy on the critical thinking ability of midwifery students.
A total of 104 midwifery students in grades 16–19 at the West China School of Nursing, Sichuan University, were included as participants through convenience sampling. All the students completed the Midwifery Health Assessment course in the third year of university. Students in grades 16 and 17 were assigned to the control group, which received routine teaching in the Midwifery Health Assessment, while students in grades 18 and 19 were assigned to the experimental group, for which the “typical case discussion and scenario simulation” teaching mode was employed. The Critical Thinking Disposition Inventory-Chinese Version (CTDI-CV) and Midwifery Health Assessment Course Satisfaction Questionnaire were administered after the intervention.
After the intervention, the critical thinking ability of the experimental group was greater than that of the control group (284.81 ± 27.98 and 300.94 ± 31.67, p = 0.008). Furthermore, the experimental group exhibited higher scores on the four dimensions of Open-Mindedness (40.56 ± 5.60 and 43.59 ± 4.90, p = 0.005), Analyticity (42.83 ± 5.17 and 45.42 ± 5.72, p = 0.020), Systematicity (38.79 ± 4.70 and 41.88 ± 6.11, p = 0.006), and Critical Thinking Self-Confidence (41.35 ± 5.92 and 43.83 ± 5.89, p = 0.039) than did the control group. The course satisfaction exhibited by the experimental group was greater than that exhibited by the control group (84.81 ± 8.49 and 90.19 ± 8.41, p = 0.002).
The “typical case discussion and scenario simulation” class mode can improve the critical thinking ability of midwifery students and enhance their curriculum satisfaction. This approach carries a certain degree of promotional significance in medical education.
Typical case discussion and scenario simulation can improve midwifery students’ critical thinking ability.
Typical case discussion and scenario simulation can enhance students’ learning interest and guide students to learn independently.
Midwifery students were satisfied with the new teaching mode.
Peer Review reports
Maternal and neonatal health are important indicators to measure of the level of development of a country’s economy, culture and health care. The positive impact of quality midwifery education on maternal and newborn health is acknowledged in the publication framework for action strengthening quality midwifery education issued by the World Health Organization (WHO) [ 1 ]. Extensive evidence has shown that skilled midwifery care is crucial for reducing preventable maternal and neonatal mortality [ 2 , 3 , 4 ]. Clinical practice features high requirements for the clinical thinking ability of midwives, which refers to the process by which medical personnel analyze and integrate data with professional medical knowledge in the context of diagnosis and treatment as well as discover and solve problems through logical reasoning [ 5 ]. Critical thinking is a thoughtful process that is purposeful, disciplined, and self-directed and that aims to improve decisions and subsequent actions [ 6 ]. In 1986, the American Association of Colleges of Nursing formulated the “Higher Education Standards for Nursing Specialty”, which emphasize the fact that critical thinking is the primary core competence that nursing graduates should possess [ 7 ]. Many studies have shown that critical thinking can help nurses detect, analyze and solve problems creatively in clinical work and is a key factor in their ability to make correct clinical decisions [ 8 , 9 , 10 ].
However, the traditional teaching method used for midwifery students in China is “teacher-led and content-based”, and it involves efficiently and conveniently imparting a large amount of knowledge to students over a short period. Students have long failed to engage in active thinking and active practice, and the cultivation of critical thinking has long been ignored [ 5 ]. As a result, the critical thinking ability of midwifery students in China is mostly at a medium or low level [ 5 ]. Therefore, it is necessary to develop a new teaching mode to improve the critical thinking ability of midwifery students.
In 2014, Professor Xuexin Zhang of Fudan University, Shanghai, China, proposed a novel teaching method: the divided class mode. The basic idea of this approach is to divide the class time into two parts. The teachers explain the theoretical knowledge in the first lesson, and the students discuss that knowledge in the second lesson. This approach emphasizes the guiding role of teachers and encourages and empowers students to take responsibility for their studies [ 11 ]. Research has shown that the divided class mode can improve students’ enthusiasm and initiative as well as teaching effectiveness [ 12 ].
The problem-originated clinical medical curriculum mode of teaching was first established at McMaster University in Canada in 1965. This model is based on typical clinical cases and a problem-oriented heuristic teaching model [ 13 ]. The process of teaching used in this approach is guided by typical cases with the goal of helping students combine theoretical knowledge and practical skills. This approach can enhance the enthusiasm and initiative of students by establishing an active learning atmosphere. Students are encouraged to discuss and analyze typical cases to promote their ability to digest and absorb theoretical knowledge. Research has shown that the problem-originated clinical medical curriculum teaching mode can enhance students’ confidence and improve their autonomous learning and exploration ability. Scenario simulation teaching can provide students with real scenarios, allowing them to practice and apply their knowledge in a safe environment [ 14 ], which can effectively improve their knowledge and clinical skills and enhance their self-confidence [ 15 , 16 ].
Based on the teaching concept of divided classes, our research team established a new teaching model of “typical case discussion and scenario simulation”. Half of the class time is allocated for students to discuss typical cases and carry out scenario simulations to promote their active thinking and active practice. The Midwifery Health Assessment is the final professional core course that midwifery students must take in our school before clinical practice. All students must complete the course in Grade 3. Teaching this course is important for cultivating the critical thinking and clinical assessment ability of midwifery students. Therefore, our team adopted the new teaching mode of "typical case discussion and scenario simulation" in the teaching of this course. This study explored the teaching mode’s ability to improve the critical thinking ability of midwifery students.
Study design
The study employed a semiexperimental design.
Participants
A convenience sample of 104 third-year midwifery students who were enrolled in the Midwifery Health Assessment course volunteered to participate in this research at a large public university in Sichuan Province from February 2019 to June 2022 (grades 16 to 19). All the students completed the course in the third year of university. Students in grades 16 and 17 were assigned to the control group, which received the traditional teaching mode. Students in grades 18 and 19 were assigned to the experimental group, in which context the “typical case discussion and scenario simulation” class mode was used. The exclusion criteria for midwifery students were as follows: (1) dropped out of school during the study, (2) took continuous leave from school for more than two weeks, or (3) were unable to complete the questionnaire. The elimination criterion for midwifery students was that all the items were answered in the same way. No significant differences in students’ scores in their previous professional courses (Midwifery) were observed between the two groups. Textbooks, teachers, and teaching hours were the same for both groups.
Development of the “typical case discussion and scenario simulation” class mode
This study is based on the implementation of the new century higher education teaching reform project at Sichuan University. With the support of Sichuan University, we first established a “typical case discussion and scenario simulation” class mode team. The author of this paper was the head of the teaching reform project and served as a consultant, and the first author is responsible for supervising the implementation of the project. Second, the teaching team discussed and developed a standard process for the “typical case discussion and scenario simulation” class mode. Third, the entire team received intensive training in the standard process for the “typical case discussion and scenario simulation” class mode.
Implementation of the “typical case discussion and scenario simulation” class mode
Phase i (before class).
Before class, in accordance with the requirements for evaluating different periods of pregnancy, the teacher conceptualized typical cases and then discussed those cases with the teaching team and made any necessary modifications. After the completion of the discussion, the modified cases were released to the students through the class group. To ensure students’ interest, they were guided through the task of discovering and solving relevant problems using an autonomous learning approach.
Phase II (the first week)
Typical case discussion period. The Midwifery Health Assessment course was taught by 5 teachers and covered 5 health assessment periods, namely, the pregnancy preparation, pregnancy, delivery, puerperium and neonatal periods. The health assessment course focused on each period over 2 consecutive teaching weeks, and 2 lessons were taught per week. The first week focused on the discussion of typical cases. In the first lesson, teachers introduced typical cases, taught key knowledge or difficult evaluation content pertaining to the different periods, and explored the relevant knowledge framework. In the second lesson, teachers organized group discussions, case analyses and intergroup communications for the typical cases. They were also responsible for coordinating and encouraging students to participate actively in the discussion. After the discussion, teachers and students reviewed the definitions, treatments and evaluation points associated with the typical cases. The teachers also encouraged students to internalize knowledge by engaging in a process of summary and reflection to achieve the purpose of combining theory with practice.
Phase III (the second week)
Scenario simulation practice period. The second week focused on the scenario simulation practice period. In the first lesson, teachers reviewed the focus of assessment during the different periods and answered students’ questions. In the second lesson, students performed typical case assessment simulations in subgroups. After the simulation, the teachers commented on and summarized the students’ simulation evaluation and reviewed the evaluation points of typical cases to improve the students’ evaluation ability.
The organizational structure and implementation of the “typical case discussion and scenario simulation” class mode showed in Fig. 1 .
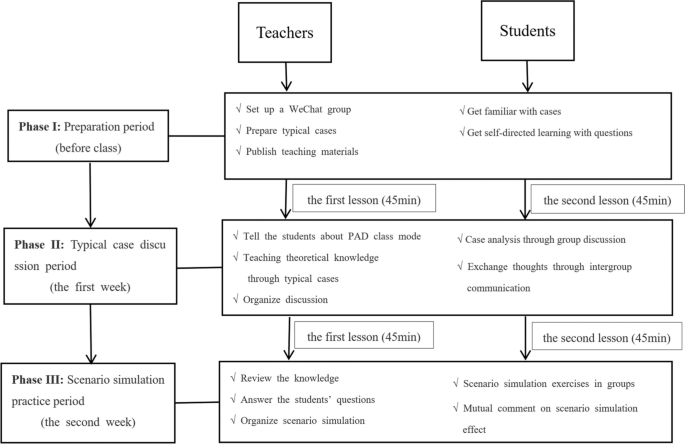
“Typical case discussion and scenario simulation” teaching mode diagram
A demographic questionnaire designed for this purpose was used to collect relevant information from participants, including age, gender, single-child status, family location, experience with typical case discussion or scenario simulation and scores in previous professional courses (Midwifery).
The Critical Thinking Disposition Inventory-Chinese Version (CTDI-CV) was developed by Peng et al. to evaluate the critical thinking ability of midwifery students [ 17 ]. The scale contains 70 items across a total of seven dimensions, namely, open-mindedness, truth-seeking, analytical ability, systematic ability, self-confidence in critical thinking, thirst for knowledge, and cognitive maturity. Each dimension is associated with 10 items, and each item is scored on a 6-point Likert scale, with 1 indicating “extremely agree” and 6 representing “extremely disagree”. The scale includes 30 positive items, which receive scores ranging from “extremely agree” to “extremely disagree” on a scale of 6 to 1, and 40 negative items, which receive scores ranging from “extremely agree” to “extremely disagree” on a scale of 1 to 6. A total score less than 210 indicates negative critical thinking ability, scores between 211 and 279 indicate an unclear meaning, scores of 280 or higher indicate positive critical thinking ability, and scores of 350 or higher indicate strong performance. The score range of each trait is 10–60 points; a score of 30 points or fewer indicates negative trait performance, scores between 31 and 39 points indicate that the trait meaning is incorrect, scores of 40 points or higher indicate positive trait performance, and scores of 50 points or higher indicate extremely positive trait performance. The Cronbach’s α coefficient of the scale was 0.90, thus indicating good content validity and structure. The higher an individual’s score on this measure is, the better that individual’s critical thinking ability.
The evaluation of teaching results was based on a questionnaire used to assess undergraduate course satisfaction, and the researchers deleted and modified items in the questionnaire to suit the context of the “typical case discussion and scenario simulation” teaching mode. Two rounds of discussion were held within the study group to form the final version of the Midwifery Health Assessment satisfaction questionnaire. The questionnaire evaluates the effect of teaching in terms of three dimensions, namely, curriculum content, curriculum teaching and curriculum evaluation. The questionnaire contains 21 items, each of which is scored on a 5-point Likert scale, with 1 indicating “extremely disagree” and 5 representing “extremely agree”. The higher the score is, the better the teaching effect.
Data collection and statistical analysis
We input the survey data into the “Wenjuanxing” platform ( https://www.wjx.cn/ ), which specializes in questionnaire services. At the beginning of the study, an electronic questionnaire was distributed to the students in the control group via student WeChat and QQ groups for data collection. After the intervention, an electronic questionnaire was distributed to the students in the experimental group for data collection in the final class of the Midwifery Health Assessment course. All the data were collected by the first author (Yuji Wang). When students had questions about the survey items, the first author (Yuji Wang) immediately explained the items in detail. To ensure the integrity of the questionnaire, the platform required all the items to be answered before submission.
Statistical Package for Social Sciences Version 26.0 (SPSS 26.0) software was used for data analysis. The Shapiro‒Wilk test was used to test the normality of the data. The measurement data are expressed as the mean ± standard deviation (X ± S), and an independent sample t test was used for comparisons among groups with a normal distribution. The data presented as the number of cases (%), and the chi-square test was performed. A P value < 0.05 indicated that a difference was statistically significant.
Ethical considerations
The study was funded by the New Century Teaching Reform Project of Sichuan University and passed the relevant ethical review. Oral informed consent was obtained from all individual participants in the study.
Characteristics of the participants
A total of 104 third-year midwifery students were enrolled from February 2019 to June 2022, and 98.1% (102/144) of these students completed the survey. Two invalid questionnaires that featured the same answers for each item were eliminated. A total of 100 participants were ultimately included in the analysis. Among the participants, 48 students were assigned to the control group, and 52 students were assigned to the experimental group. The age of the students ranged from 19 to 22 years, and the mean age of the control group was 20.50 years (SD = 0.61). The mean age of the experimental group was 20.63 years (SD = 0.65). Of the 100 students who participated in the study, the majority (96.0%) were women. No significant differences were observed between the intervention and control groups in terms of students’ demographic information (i.e., age, gender, status as an only child, or family location), experience with scenario simulation or typical case discussion and scores in previous Midwifery courses (Table 1 ).

Examining the differences in critical thinking ability between the two groups
The aim of this study was to evaluate the effect of the new teaching mode of “typical case discussion and scenario simulation” on improving the critical thinking ability of midwifery students. Independent sample t tests were used to examine the differences in critical thinking ability between the two groups (Table 2 ). The results showed that the total critical thinking scores obtained by the experimental group were greater than those obtained by the control group (284.81 ± 27.98 and 300.94 ± 31.67, p = 0.008). The differences in four dimensions (Open-Mindedness (40.56 ± 5.60 and 43.59 ± 4.90, p = 0.005), Analyticity (42.83 ± 5.17 and 45.42 ± 5.72, p = 0.020), Systematicity (38.79 ± 4.70 and 41.88 ± 6.11, p = 0.006), and Critical Thinking Self-Confidence (41.35 ± 5.92 and 43.83 ± 5.89, p = 0.039)) were statistically significant.
Examining the differences in curriculum satisfaction between the two groups
To evaluate the effect of the new teaching mode of “the typical case discussion and scenario simulation” on the course satisfaction of midwifery students. Independent sample t tests were used to examine the differences in course satisfaction between the two groups (Table 3 ). The results showed that the curriculum satisfaction of the experimental group was greater than that of the control group (84.81 ± 8.49 and 90.19 ± 8.41, p = 0.002). Independent sample t tests were used to examine the differences in the three dimensions of curriculum satisfaction between the two groups (Table 3 ). The results showed that the average scores of the intervention group on the three dimensions were significantly greater than those of the control group (curricular content: 20.83 ± 1.96 and 22.17 ± 2.23, p = 0.002; curriculum teaching: 34.16 ± 3.89 and 36.59 ± 3.66, p = 0.002; curriculum evaluation: 29.81 ± 3.27 and 31.42 ± 3.19, p = 0.015).
Midwifery is practical and intensive work. To ensure maternal and child safety, midwives must make decisions and take action quickly. Therefore, midwives should have both critical thinking ability and clinical decision-making ability [ 18 ]. In addition, the Australian Nursing and Midwifery Accreditation Council (ANMAC) regulates the educational requirements for the programs required for registration as a midwife. According to these standards, education providers must incorporate learning activities into curricula to encourage the development and application of critical thinking and reflective practice [ 19 ]. Therefore, the challenge of cultivating the critical thinking ability of midwifery students is an urgent problem that must be solved. However, influenced by the traditional teaching method of “teacher-led and content-based”, the critical thinking ability of midwifery students in China is mostly at a medium or low level. In order to improve the critical thinking ability of midwifery students. Our research team has established a new teaching model, the “typical case discussion and scenario simulation” class model. And applied to the midwifery core curriculum Midwifery Health Assessment. This study aimed to investigate the implementation of a novel systematic and structured teaching model for midwifery students and to provide evidence regarding how to improve the critical thinking ability of midwives.
The results showed that the total CTDI-CV score obtained for the experimental group was greater than that obtained for the control group. These findings indicate that the “typical case discussion and scenario simulation” class mode had a positive effect on the cultivation of students’ critical thinking ability, a conclusion which is similar to the findings of Holdsworth et al. [ 20 ], Lapkin et al. [ 21 ] and Demirören M et al. [ 22 ]. We indicate the following reasons that may explain these results.The core aim of the typical case discussion teaching mode is to raise questions based on typical clinical cases and to provide heuristic teaching to students [ 23 ]. This approach emphasizes asking questions based on specific clinical cases, which enables students to engage in targeted learning. Moreover, scenario simulation allows students to attain certain inner experiences and emotions and actively participate in curriculum practice, which can enhance their ability to remember and understand knowledge [ 24 ]. Through the divided class mode, half of the class time was divided into the students. This method emphasizes the guiding role of teachers and encourages and empowers students to assume learning responsibilities. In addition, students can think, communicate and discuss actively [ 22 , 23 ]. Furthermore, this approach created opportunities for students to analyze and consider problems independently and give students sufficient time to internalize and absorb knowledge and deepen their understanding of relevant knowledge, which can increase their confidence in their ability to address such problems and improve their critical thinking ability [ 12 , 25 , 26 ].
In addition, the results showed that except for Truth-Seeking and Systematicity, the other five dimensions were all positive. These findings are similar to the results reported by Atakro et al.. and Sun et al. [ 27 , 28 ]. Through the intervention, the Systematicity scores became positive, suggesting that the new teaching mode can help students deal with problems in an organized and purposeful way. However, Truth-Seeking still did not become positive; this notion focuses on intellectual honesty, i.e., the disposition to be courageous when asking questions and to be honest and objective in the pursuit of knowledge even when the topics under investigation do not support one’s self-interest [ 29 ]. Studies have shown that this factor is related to the traditional teaching mode used [ 30 ]. The traditional teaching mode focuses on knowledge infusion, helps students remember the greatest possible amount of knowledge in a short time, and does not focus on guiding students to seek knowledge with sincerity and objectivity. Therefore, in future educational practice, we should focus on cultivating students’ ability to seek truth and engage in systematization.
Student evaluative feedback is an important way to test the effectiveness teaching mode. Therefore, understanding students’ evaluations of the effects of classroom teaching is key to promoting teaching reform and improving teaching quality. Therefore, we distributed a satisfaction questionnaire pertaining to the midwifery health assessment curriculum, which was based on the “typical case discussion and scenario simulation” class mode, with the goal of investigating curriculum satisfaction in terms of three dimensions (curriculum content, curriculum teaching and curriculum evaluation). The results showed that the satisfaction scores for each dimension increased significantly. This finding suggests that the new teaching method can enrich the teaching content, diversify the teaching mode and improve students’ curriculum evaluations.
In summary, the “typical case discussion and scenario simulation” class mode focuses on typical cases as its main content. Students’ understanding of this content is deepened through group discussion and scenario simulation. The subjectivity of students in curriculum learning should be accounted for. Students can be encouraged to detect, analyze and solve problems with the goal of improving their critical thinking ability. Moreover, this approach can also enhance curriculum satisfaction. It is recommended that these tools should be used continuously in future curriculum teaching.
This study has several limitations. First, the representativeness of the sample may be limited since the participants were recruited from specific universities in China. Second, we used historical controls, which are less effective than simultaneous controlled trials. Third, online self-report surveys are susceptible to response biases, although we included quality control measurements in the process of data collection. Fourth, we did not use the same critical thinking instrument, CTDI-CV, to investigate the critical thinking of the students in the experimental group or the control group before intervention but used professional course grades from the Midwifery for substitution comparison. This may not be a sufficient substitute. However, these comparisons could be helpful since those grades included some sort of evaluation of critical thinking. In light of these limitations, future multicenter simultaneous controlled studies should be conducted. Nonetheless, this study also has several strengths. First, no adjustment of teachers or change in learning materials occurred since the start of the midwifery health assessment, thus ensuring that the experimental and control groups featured the same teaching materials, teachers and teaching hours. In addition, to ensure the quality of the research, the first author of this paper participated in the entirety of the course teaching.
The “typical case discussion and scenario simulation” class mode can improve the critical thinking of midwifery students, which is helpful for ensuring maternal and child safety. Students are highly satisfied with the new teaching mode, and this approach has a certain degree of promotional significance. However, this approach also entails higher requirements for both teachers and students.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
World Health Organisation, Strengthening quality midwifery education for Universal Health Coverage2030,2019, https://www.who.int/maternal_child_adolescent/topics/quality-of-care/midwifery/strengthening-midwifery-education/en/ (accessed 21.01.20).
Akombi BJ, Renzaho AM. Perinatal mortality in Sub-Saharan Africa: a meta-analysis of demographic and health surveys. Ann Glob Health. 2019;85(1):106.
Article Google Scholar
Campbell OM, Graham WJ. Strategies for reducing maternal mortality: getting on with what works. Lancet. 2006;368(9543):1284–99.
Gage AD, Carnes F, Blossom J, Aluvaala J, Amatya A, Mahat K, Malata A, Roder-DeWan S, Twum-Danso N, Yahya T, et al. In low- and middle-income countries, is delivery in high-quality obstetric facilities geographically feasible? Health Aff (Millwood). 2019;38(9):1576–84.
Xing C, Zhou Y, Li M, Wu Q, Zhou Q, Wang Q, Liu X. The effects of CPBL + SBAR teaching mode among the nursing students. Nurse Educ Today. 2021;100:104828.
Carter AG, Creedy DK, Sidebotham M. Critical thinking evaluation in reflective writing: development and testing of Carter assessment of critical thinking in midwifery (Reflection). Midwifery. 2017;54:73–80.
Yeh SL, Lin CT, Wang LH, Lin CC, Ma CT, Han CY. The Outcomes of an Interprofessional simulation program for new graduate nurses. Int J Environ Res Public Health. 2022;19(21):13839.
Chang MJ, Chang YJ, Kuo SH, Yang YH, Chou FH. Relationships between critical thinking ability and nursing competence in clinical nurses. J Clin Nurs. 2011;20(21–22):3224–32.
Shoulders B, Follett C, Eason J. Enhancing critical thinking in clinical practice: implications for critical and acute care nurses. Dimens Crit Care Nurs. 2014;33(4):207–14.
Jalalpour H, Jahani S, Asadizaker M, Sharhani A, Heybar H. The impact of critical thinking training using critical thinking cards on clinical decision-making of CCU nurses. J Family Med Prim Care. 2021;10(10):3650–6.
Xuexin Z. PAD class: a new attempt in university teaching reform. Fudan Educ Forum. 2014;12(5):5–10 [in Chinese].
Google Scholar
Zhai J, Dai L, Peng C, Dong B, Jia Y, Yang C. Application of the presentation-assimilation-discussion class in oral pathology teaching. J Dent Educ. 2022;86(1):4–11.
Colliver JA. Effectiveness of problem-based learning curricula: research and theory. Acad Med. 2000;75(3):259–66.
Bryant K, Aebersold ML, Jeffries PR, Kardong-Edgren S. Innovations in simulation: nursing leaders’ exchange of best practices. Clin Simul Nurs. 2020;41:33-40.e31.
Cicero MX, Whitfill T, Walsh B, Diaz MC, Arteaga G, Scherzer DJ, Goldberg S, Madhok M, Bowen A, Paesano G, et al. 60 seconds to survival: a multisite study of a screen-based simulation to improve prehospital providers disaster triage skills. AEM Educ Train. 2018;2(2):100–6.
Lee J, Lee H, Kim S, Choi M, Ko IS, Bae J, Kim SH. Debriefing methods and learning outcomes in simulation nursing education: a systematic review and meta-analysis. Nurse Educ Today. 2020;87:104345.
Peng G, Wang J, Chen M, Chen H, Bai S, Li J, Li Y, Cai J, Wang L. Yin Validity and reliability of the Chinese critical thinking disposition inventory Chin. J Nurs. 2004;39(09):7–10 [in Chinese].
Papathanasiou IV, Kleisiaris CF, Fradelos EC, Kakou K, Kourkouta L. Critical thinking: the development of an essential skill for nursing students. Acta Inform Med. 2014;22(4):283–6.
Australian Nursing and Midwifery Accreditation Council Midwife accreditation standards, 2014 ANMAC, Canberra. 2014. https://anmac.org.au/document/midwife-accreditation-standards-2014 .
Holdsworth C, Skinner EH, Delany CM. Using simulation pedagogy to teach clinical education skills: a randomized trial. Physiother Theory Pract. 2016;32(4):284–95.
Lapkin S, Fernandez R, Levett-Jones T, Bellchambers H. The effectiveness of using human patient simulation manikins in the teaching of clinical reasoning skills to undergraduate nursing students: a systematic review. JBI Libr Syst Rev. 2010;8(16):661–94.
Demirören M, Turan S, Öztuna D. Medical students’ self-efficacy in problem-based learning and its relationship with self-regulated learning. Med Educ Online. 2016;21:30049.
Spaulding WB, Neufeld VR. Regionalization of medical education at McMaster University. Br Med J. 1973;3(5871):95–8.
Rossler KL, Kimble LP. Capturing readiness to learn and collaboration as explored with an interprofessional simulation scenario: A mixed-methods research study. Nurse Educ Today. 2016;36:348–53.
Yang YL, Luo L, Qian Y, Yang F. Cultivation of undergraduates’ self-regulated learning ability in medical genetics based on PAD class. Yi Chuan. 2020;42(11):1133–9.
Felton A, Wright N. Simulation in mental health nurse education: the development, implementation and evaluation of an educational innovation. Nurse Educ Pract. 2017;26:46–52.
Atakro CA, Armah E, Menlah A, Garti I, Addo SB, Adatara P, Boni GS. Clinical placement experiences by undergraduate nursing students in selected teaching hospitals in Ghana. BMC Nurs. 2019;18:1.
Sun Y, Yin Y, Wang J, Ding Z, Wang D, Zhang Y, Zhang J, Wang Y. Critical thinking abilities among newly graduated nurses: a cross-sectional survey study in China. Nurs Open. 2023;10(3):1383–92.
Wangensteen S, Johansson IS, Björkström ME, Nordström G. Critical thinking dispositions among newly graduated nurses. J Adv Nurs. 2010;66(10):2170–81.
Salsali M, Tajvidi M, Ghiyasvandian S. Critical thinking dispositions of nursing students in Asian and non-Asian countries: a literature review. Glob J Health Sci. 2013;5(6):172–8.
Download references
Acknowledgements
Not applicable.
The study was supported by Sichuan University’s New Century Education and Teaching Reform Project (SCU9316).
Author information
Yuji Wang and Yijuan Peng are co-first authors.
Authors and Affiliations
Department of Nursing, West China Second University Hospital, Sichuan University/West China School of Nursing, Sichuan University/Key Laboratory of Birth Defects and Related Diseases of Women and Children (Sichuan University), No. 20 Third Section, Renmin South Road, Chengdu, Sichuan Province, 610041, China
Yuji Wang, Yijuan Peng & Yan Huang
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Yuji Wang, Yijuan Peng and Yan Huang. The first draft of the manuscript were written by Yuji Wang and Yijuan Peng, and all authors commented on previous versions of the manuscript.
Corresponding author
Correspondence to Yan Huang .
Ethics declarations
Ethics approval and consent to participate.
This study was supported by Sichuan University. And it was approved by the Ethics Review Committee of West China School of Nursing, Sichuan University. As it is a teaching research with no harm to samples, we only obtained oral informed consents from the participants including teachers and midwifery students and it was approved by the Ethics Review Committee of West China School of Nursing, Sichuan University(approval number 2021220). We comfirm that all methods were performed in accordance with the relevant guidelines and regulations in Ethics Approval and Consent to participate in Declarations.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Wang, Y., Peng, Y. & Huang, Y. The effect of “typical case discussion and scenario simulation” on the critical thinking of midwifery students: Evidence from China. BMC Med Educ 24 , 340 (2024). https://doi.org/10.1186/s12909-024-05127-5
Download citation
Received : 19 November 2022
Accepted : 02 February 2024
Published : 26 March 2024
DOI : https://doi.org/10.1186/s12909-024-05127-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical education
- Critical thinking
- Nurse midwives
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 26 March 2024
Evaluation of a new concept to improve and organize clinical practice in nursing education: a pilot-study
- Helle Skou Thomsen 1 ,
- Britt Egeris Jørgensen 1 ,
- Jette Kynde Schøtz 1 , 2 ,
- Line Muff Bech 1 &
- Lea Ladegaard Grønkjær 3
BMC Nursing volume 23 , Article number: 203 ( 2024 ) Cite this article
Metrics details
Nursing students may experience clinical practice as unsafe due to the interactions with patients, fear of making mistakes, lack of clinical experience and supervision, which results in anxiety and stress. Thus, interventions to improve and organize the learning environment in clinical practice for nursing students are warranted, and the aim of this pilot-study was to evaluate a new concept of clinical practice in order to get insight on the different initiatives and gain knowledge for further developing.
The new concept consisted of nursing students being affiliated to the same department during their clinical practices, reflective supervision, and participation in a self-compassion course. Data was collected using questionnaires and focus group interviews of 17 nursing students, 17 clinical supervisors, and 14 head nurses. A mixed-methods strategy was employed to give the study a pragmatic approach. Finding from the questionnaires and focus group interviews were analyzed separately and then weaved together into themes.
The results generated four themes: Information and involvement before and during the new concept, Learning outcomes, safety, and well-being, Impact of reflective supervision and self-compassion course, and Transition from study life to working life. In general, the participating nursing students, clinical supervisors, and head nurses had positives experiences regarding the new concept. They felt well-informed, and they experienced that it contributed to a safe learning environment, increased well-being, strengthened the relationship between nursing students and clinical supervisors and healthcare staff at the department, and prepared the nursing students to working life.
Our results complement the suggestion that improved quality of clinical practice for nursing students is an effective strategy to establish a safe and supportive learning environment that contribute with satisfaction, successful experiences, and attraction of future nurses. However, further intervention studies are needed to compare the effect of the new concept with traditional clinical practice.
Peer Review reports
Introduction
Nurses are vital to the healthcare system and consist of the largest part of healthcare professionals. However, the nursing profession worldwide faces shortages due to the increase in the ageing population and people living with chronic diseases, inequitable workforce distribution with more nurses retiring, high turnover, and a high number of student dropouts at the nursing education [ 1 , 2 ].
Dropout from nursing education is problematic considering the severe shortage of nurses, and it may have severe consequences for the healthcare system. Reasons for dropout include financial problems, personal reasons, but also the educational structure of the nursing education such as theory–practice gap and unpleasant experiences and lack of support during clinical practice. Clinical practice refers to the clinical workplace for example hospitals in which nursing students complete their clinical placements as part of their education [ 3 , 4 ].
Clinical practice is of high importance in nursing education as it is in this context that nursing students acquire clinical skills, apply theoretical knowledge to practice, and develop clinical reasoning and problem-solving skills [ 5 ]. In addition, studies have indicated that the experience of clinical practice influence nursing students learning outcome and, especially in the last part of the education, also facilitate the transition from study to working life, strengths nursing students commitment to the nursing profession, and is important in relation to the choice of future workplace [ 6 , 7 , 8 ]. However, several studies have shown that nursing students experience clinical practice as unsafe due to difficulties in the interactions with patients, fear of making mistakes, lack of clinical experience and supervision, which may result in anxiety and stress [ 9 , 10 , 11 ]. Thus, it appears that there is a need for interventions to improve and organize clinical practice for nursing students as an potentially effective strategy to establish a safe and supportive learning environment that contribute with satisfaction, successful experiences, and attraction of future nurses [ 11 ]. With this background, the aim of this pilot-study was to evaluate a new concept of clinical practice in order to get insight on the different initiatives and gain knowledge for further developing of the concept.
This was a pilot-study to evaluate a new concept to improve and organize clinical practice for nursing students at University Hospital of Southern Denmark, Esbjerg, and the results are reported according to the CONSORT extension to pilot and feasibility trials [ 12 , 13 ].
Setting of the study
The nursing education in Denmark is 3½ years consisting of seven semesters (210 European Credit Transfer System (ECTS) points). Clinical practice are included in all semester and make up 90 ECTS points of the education. Nursing students from the different semesters do a large part of their clinical practice in different departments at the hospitals. In addition, practice is also carried out in primary health care centers, all of them belonging to the same healthcare region.
University Hospital of Southern Denmark, Esbjerg and University College South Denmark have collaborated on developing a new concept of clinical practice to establish a framework for a safe learning environment where it is possible to test new ways of improving and organizing clinical practice. In connection with this concept, nursing students are affiliated at the same department at their clinical practice in both 6th and 7th semester. The aim was to create a clinical learning environment that could support the well-being of the nursing students, increase the feeling of belonging and strengthen the relationship with the healthcare staff at the department. In addition, the intension was to give nursing students confidence to become more independent, which could contribute to facilitating the transition from student to working life. The concept also included initiatives such as reflective supervision during the clinical practice of every semester together with fellow nursing students, a clinical supervisor from the University Hospital of Southern Denmark, Esbjerg, and a nurse educator from University College South Denmark, and participation in a self-compassion course for one hour in six weeks. Figure 1 illustrates the new concept.
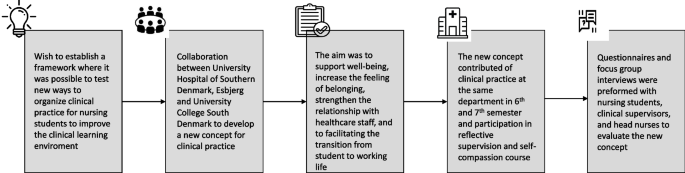
Overview of the new concept for clinical practice
Participants
The new concept was tested at 14 of the 37 departments at University Hospital of Southern Denmark, Esbjerg in February 2023. Thus, the pilot-study included 17 nursing students, 17 clinical supervisors, and 14 head nurses, which were all affiliated to these departments. The choice of departments to test the new concept was random, but aimed to represent both general and specialty wards and outpatient clinics. Nursing students were affiliated to the department using random allocation technique.
Data collection
Data was collected using questionnaires and focus group interviews. Three questionnaires were developed by the authors for this pilot-study. The questionnaires consisted of 15 questions to the nursing students, 13 questions to the clinical supervisors, and 3 questions to the head nurses to evaluate on the new concept for clinical practice (see Supplement Table 1 ). The questionnaires contained questions on the assessment of the new concept in general (nursing students and clinical supervisors), experience of learning outcomes, feeling of well-being (nursing students, clinical supervisors, and head nurses), experience of reflective supervision, the self-compassion course (nursing students and clinical supervisors), and transition from student to working life (nursing students, clinical supervisors, and head nurses). Despite one question regarding participation in an information meeting, the questions were rated using a five point Likert-scale ranging from: to a very low degree, to a low degree, to some extent, to a high degree, and to a very high degree. In all questionnaires, it was possible to write additional comments. The questionnaires were tested for face validity by one nursing student and one educational consultant to determine whether the questions were clear and understandable. Based on the test, only minor linguistic changes were made.
Afterwards, three focus group interviews were carried out with 15 nursing students divided into two groups, and 12 clinical supervisors. Semistructured interview guides were designed for this pilot-study to capture nursing students and clinical supervisors experience of the new concept for clinical practice including the reflective supervision and the self-compassion course with particular focus on elaborating answers from the questionnaires and explore what was good and what could be improved about the new concept (see Supplement Table 2 ). The focus group interviews lasted one hour, and were audio and transcribed verbatim. The questionnaire and focus group interviews were carried out by educational consultants (2th, 3th, and 4th author) from University Hospital of Southern Denmark, Esbjerg. The data collection was conducted in May 2023.
Data analysis
A mixed-methods strategy was employed to give the study a pragmatic approach [ 14 ]. Figure 2 illustrates the data collection and data analysis process. Data from the questionnaires were analyzed using descriptive statistic and were expressed as numbers and percentages, and the statistical analyses were performed by the computer software program, Microsoft Office Excel 2016.
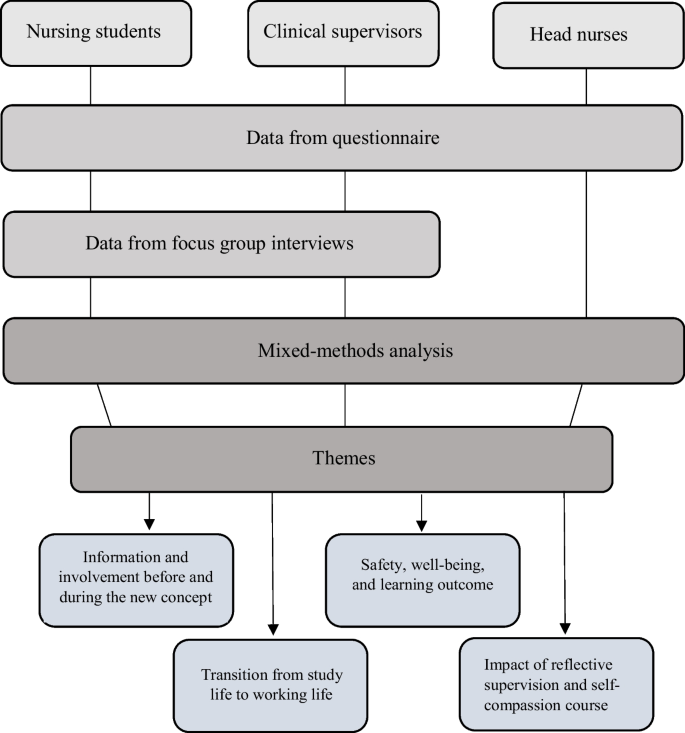
Data collection and data analysis process
Comments from the questionnaire were analyzed with inspiration from the Graneheim and Lundman content analysis method, like the focus group interviews [ 15 ]. To support reliable and valid inferences, content analysis involves a set of systematic and transparent procedures for processing data [ 16 ]. This consist of a stepwise process beginning with several read troughs by the first and last author to obtain an overview of the transcriptions.
Then, the transcriptions were systematically reviewed line by line to identify patterns (i.e. “meaning units”) that expressed segments or quotations that contained information or meaning related to the study aim. Meaning units dealing with the same content were condensed, coded, and organized into categories according to their similarity. The next step involved comparing similarities and differences to reach consensus on the final identified categories. To enhance validity and limit the risk of predetermined interpretation, the first and last author, not having taken part of the data collection earlier, independently performed the analysis. Their preunderstanding consisted of their previous experience as nursing students and present experience as research nurses and knowledge in the field of nursing education from the literature. The analysis and categories were refined and discussed among the whole author group. This made it possible to determine if any preunderstanding could have affected the analysis. The transcripted interviews were reread by the first and last author to ensure that the categories covered all aspect of the data. Representative quotes were chosen and translated into English. Due to the mixed-methods approach, data integration was then performed using a weaving approach. This meant that findings from the questionnaires and focus group interviews were written together on a theme-by-theme basis to present a detailed summary of the results [ 14 ].
Data from the questionnaires and focus group interviews resulted in four themes: Information and involvement before and during the new concept , Learning outcomes, safety, and well-being, Impact of reflective supervision and self-compassion course , and Transition from study life to working life . Answers from the questionnaires are presented in Table 1 .
Information and involvement before and during the new concept
As an introduction to the new concept, two information meetings were held for the nursing students, and almost all participated (83%). Nearly all of the nursing students felt that they to a high or very high degree were informed about the new concept before the start of their clinical practice (85%). Likewise did 76% state that an online information forum kept them informed about the initiatives of the new concept during their clinical practice.
All clinical supervisors had participated in at least one information meeting, and all felt informed about the new concept. However, only 36% reported (to a high or very high degree) to be informed using the online information forum during the clinical practice. Of the clinical supervisors, 63% felt involved in the new concept.
Learning outcomes, safety and well-being
The majority of the nursing students experiences that the affiliation to the same department during clinical practice in 6th and 7th semester contributed to a safe learning environment (80%). Also, 82% felt a high or very high degree of being part of the healthcare staff at the department due to the new concept. Almost all nursing students experiences a high sense of safety, knowing that they were coming back to the same department (95%). However, a concern was raised about the affiliation to the same department in both clinical practices if the nursing students were not interested in the department´s specialty or if the relationship between the nursing student and the clinical supervisor was problematic.
In connection with the focus group interviews with the nursing students, it emerged that they were positive about the collaboration between the hospital and the nursing education. One nursing student reported: “ Nice that the hospital and education are working together. It just does something good and also provides a form of security at the same time. You realize that there are really investing in us .”
All the clinical supervisors and 90% of the head nurses agree that the affiliation to the same department during clinical practice had a positive effect on the nursing students learning and well-being. During the focus group interview, the clinical supervisors expressed that the new concept allowed time to build a strong relationship between the nursing students and the clinical supervisors. In addition, the clinical supervisors thought that the nursing students felt a greater sense of commitment and responsibility to their department, which also contributed to strengthen the relationship with the healthcare staff. The clinical supervisors also described that the nursing students feeling of safety and well-being due to the new concept contributed to professional development and increased responsibility for own learning.
Impact of reflective supervision and self-compassion course
All nursing students had participated in reflective supervision, and 93% reported that it to a high or very high degree contributed to improving their ability to apply theoretical knowledge to practice. In addition, the nursing students stated that reflective supervision brought new perspectives on clinical issues (94%), development of quality (93%), and interdisciplinary and cross-sectoral collaboration in clinical practice (94%). One student reported: “So good to have a bit of theory again because you easily forget when focusing on clinical practice”.
The focus group interviews revealed that the nursing students preferred small groups during reflective supervision as it contributed to a feeling of safety. In addition, the nursing students described that the reflective supervision created a good learning environment with the possibility of feedback, which also prepared the nursing students for their examination and future nursing practice. One nursing student stated: “Why have they not done this before. It all makes more sense now. Now we understand”.
As a suggestion for improvement, the nursing students highlighted a need for more information before attending the reflective supervision so they had the opportunity to be prepared. In addition, a proposal was made to make the reflective supervision online.
Seventy-two percent of the clinical supervisors stated to a high or very high degree that reflective supervision contributed to improve nursing students’ ability to apply theoretical knowledge to practice. In the focus group interviews, the supervisors expressed that the nursing students were excited about the reflective supervision because it contributed to a meaningful learning environment.
All nursing students had participated in the self-compassions course, and 30% stated that the participation to a high or very high degree contributed to their well-being. From the focus group interviews, the nursing students indicated confusion about the purpose of the course and the use in regards to the new concept of clinical practice, and they suggested more information about how to implement self-compassion in practice. This was consistent with the clinical supervisors, they indicated that only 27% of the nursing students to a high or very high degree used elements of the self-compassion course. However, 64% also reported to believe that the compassion approach contributed to the nursing students learning skills and well-being during clinical practice.
Transition from study life to working life
Sixty-five percent of the nursing students thought to a high or very high degree that the new concept would contribute to prepare them from study to working life. One reported: “ I think it is a good concept and I will be better qualified to be a nurse”.
All the clinical supervisors and the head nurses agreed to a high or very high degree that the new concept contributed to develop the nursing students professional identity, and thereby readiness to become a nurse.
The aim of this pilot-study was to evaluate a new concept to improve and organize clinical practice in order to get insight on the different initiatives and gain knowledge to further developing of the concept.
In general, the participating nursing students, clinical supervisors, and head nurses had positives experiences regarding the new concept. They felt well-informed about the concept, and they experienced that the affiliation to the same department during clinical practice in 6th and 7th semester contributed to a safe learning environment, increased well-being among nursing students, strengthen relationship with the clinical supervisors and healthcare staff at the department, and prepared the nursing students to working life. In addition, they were satisfied with initiatives such as reflective supervision but to a lower degree the self-compassion course.
Studies have highlighted that successful changes in healthcare organizations requires clear communication and information to allow for preparation and to increase the chances for success [ 17 ]. This study showed high degree of information to and involvement of nursing students and clinical supervisors, which may be one of the reasons for the positive evaluation of the new concept. However, more information was wanted in connection with the initiatives reflective supervision and the self-compassion course. In addition, changes such as the new concept of clinical practice are more likely to succeed when the involved healthcare professionals have the opportunity to influence the changes, are prepared for the change, and values the changes [ 17 ]. This is in consistent with this pilot-study where the aim is to gain knowledge of the experiences and satisfaction with the concept to further developing.
The results of the evaluation of the pilot-study are consistent with other studies showing that longer clinical practice contributes to the nursing students experience of being part of a workplace, which strengthen the professional recognition and self-confidence, and therefore support the transition from study to working life [ 10 , 18 ]. In addition, a study has shown that the strengthen relationship between nursing students and healthcare staff enables the staff to push the limits of learning [ 19 ]. Concerns about the new concept were raised if the nursing students were not interested in the department´s specialty or if the relationship between the nursing student and the clinical supervisor was problematic. This concern is fair as several studies have shown that a good relationship between nursing students and clinical supervisors is essential for the nursing students learning potential [ 20 , 21 ].
The nursing students experienced the reflective supervision as positive. They thought it improved their ability to apply theoretical knowledge to practice and brought new perspectives on clinical issues, development of quality, and interdisciplinary and cross-sectoral collaboration in clinical practice, which created a good learning environment and increased their understanding of the nursing practice. This was also underlined by the clinical supervisors. This is in accordance with another study, which show how reflective spaces in clinical practice creates an increased understanding of nursing theory and its relevance for clinical practice, and contributes to achieved professional identity [ 22 ]. In addition, a study has highlighted that both situated- and meta learning is necessary in the clinical practice for nursing students to achieve an ultimate learning environment. Situated learning is advice and guidance in nursing to develop and improve clinical skills while meta learning is conceived as advice and guidance about nursing using theoretical and reflective models to interpret different aspects of a situation and discuss it in professional terms [ 19 ].
Studies have shown that nursing students experience clinical practice as unsafe, which may result in anxiety and stress [ 6 , 7 , 8 ]. It is importance to talk to the nursing students about their feelings and reactions as they often feel vulnerable, lonely, and lacks support to deal with their emotions. Thus, the nursing students calls for more support to develop their resilience [ 21 , 23 ]. The challenges of nursing students’ dropout, recruitment and retention of nurses are problematic. Therefore, attention has been made on interventions to emphasize resilience as a positive force for overcoming adversity and improve well-being [ 24 ]. In this study, nursing students participated in a self-compassion course. However, only 30% of the nursing students stated that the participation contributed to their well-being, and clinical supervisors indicated that only 27% of the nursing students used elements of the self-compassion course. This is in contrast to other studies who finds positive health benefits such as burnout prevention, improved nursing care, and stress management from attending a self-compassion course [ 25 , 26 ]. In many of these studies, the effect of self-compassion is measured before and after an intervention using specific self-compassion questionnaires addressing for example burnout, mindfulness, and well-being [ 27 ]. In this pilot-study, only one questions concerning to what extent the self-compassion course has contributed to increased well-being was asked. This may be one reason for the difference. In addition, the nursing students indicated confusion about the purpose of the course and the use in regards to the new concept of clinical practice. Thus, another reason may be lack of understanding of the course and how to implement self-compassion in practice. Another study also highlights the need to help cultivate nursing students´ self-compassion not only during clinical practice but also during classroom teaching at the nursing education [ 28 ].
A review study has investigated the challenges of supporting nursing students in clinical practice. It found that nursing students faced several challenges in connection with clinical practice such as anxiety and fear, ineffective clinical education, organizational-environmental stress, and socio-cultural challenges. However, most studies only highlighted the presence of such challenges, while few studies dealt with their causes [ 29 ]. This pilot-study aimed to evaluate a new concept of clinical practice to create a new clinical learning environment to support nursing students’ independence and well-being, increase the feeling of belonging, strengthen the relationship with the healthcare staff, and facilitate the transition from student to working life. Other studies have also initiated interventions to support nursing student. Thus, a study evaluated initiatives to support the nursing students active learning, engagement, and self-efficacy in clinical practice and found that the Check-in, Check-out process engaged the nursing students as active partners in their learning and teaching in their clinical preparation for practice, and helped them to acknowledge and reflect on their accomplishment [ 30 ]. In addition, another study found that using a matching program to match the nursing students with clinical workplaces in connection with clinical practice at public health agencies increased the nursing students reflection of own competences and needs as well as developed a successful collaboration between the nursing education and clinical workplaces [ 31 ]. Collaboration between nursing educations and clinical workplaces are important for achieving the nursing students learning outcome and facilitate the transition from study to working life. Thus, the higher perceived academic-practice partnership by nursing students, the better interactions with healthcare staff, organizational socialization, and professional self-concept [ 32 ]. In this study, the nursing students also described very positive experiences with the collaboration between the hospital and the nursing education.
Study limitations
The aim of this pilot-study was to evaluate a new concept to improve and organize clinical practice in order to get insight on the different initiatives and gain knowledge to further developing. The objective of a pilot-study is often to assess randomization, recruitment strategies, and sample size calculation, or to test the acceptability of an intervention, the feasibility of a study protocol, or the selection of the most appropriate primary outcomes measure [ 33 ]. In addition, a pilot-study is not perceived as strong evidence [ 12 , 13 ], and this pilot-study do not provide data on the effects of the new concept on nursing students clinical learning environment, feeling of belonging and well-being, relationship with healthcare staff, and facilitation of the transition from student to working life in comparison to traditional clinical practice. This is planned to be investigated in a forthcoming study. In addition, we wish to explore the experience of the new concept among healthcare staff at the departments and nurse educators from the nursing education.
We acknowledge the fact that the results are interpreted in the light of the limitations that might occur in connection with a single-center, pilot-study with a small sample-size. The results are therefore not generalizable and no general conclusion can be drawn from this study. However, we believe our study showing nursing students, clinical supervisors, and head nurses positive experiences regarding the new concept to be a useful contribution to the sparse knowledge on improving and organizing clinical practice of nursing students and may act as an inspiration when planning other intervention studies.
In conclusion, this pilot-study found that affiliation to the same department during clinical practice together with participation in reflective supervision and a self-compassion course was experienced positive among nursing students, clinical supervisors, and head nurses. In addition, the new concept contributed to the experience of a safe learning environment, increased well-being among nursing students, strengthen relationship with the clinical supervisors and healthcare staff at the department, and prepared the nursing students to working life. Our results complement the suggestion that improved quality of clinical practice for nursing students is an effective strategy to establish a safe and supportive learning environment that contribute with satisfaction, successful experiences, and attraction of future nurses. Our results have important implication to strengthen the collaboration between clinical workplaces and nursing educations. However, further intervention studies are needed to compare the effect of the new concept with traditional clinical practice.
Availability of data and materials
Data is provided within the manuscript and supplementary information files. Due to the small sample size, the dataset generated during this study is not available.
Abbreviations
European Credit Transfer System
General Data Protection Regulation
Haddad LM, Annamaraju P, Toney-Butler TJ. Nursing shortage. In: StatPearls [Internet]. Treasure Island: StatPearls Publishing; 2023.
Wismar M, Maier CB, Sagan A, et al. Development in Europe´s Health workforce: addressing the conundrums. Eurohealth Syst Policies. 2018;24:38–42.
Google Scholar
Eick SA, Williamson GR, Heath V. A systematic review of placement-related attrition in nurse education. Int J Nurs Stud. 2012;49:1299–309.
Article PubMed Google Scholar
Bakker EJM, Verhaegh KJ, Kox JHAM, et al. Late dropout from nursing education: an interview study of nursing students´ experience and reasons. Nurse Educ Pract. 2019;39:17–25.
Sellberg M, Palgren PJ, Möller R. A cross-sectional study of clinical learning enviroments across four undergraduate programs using the undergraduate clinical education environment measure. BMC Med Educ. 2021;21:258.
Article PubMed PubMed Central Google Scholar
Fernández-Gardia D, Moreno-Latorre E, Giménez-Espert MDC, et al. Satisfation with the clinical practice among nursing students using regression models and qualitative comparative analysis. Nurs Educ Today. 2021;10:104861.
Article Google Scholar
Kaihlanen A, Gluschkoff K, Koskinen S, et al. Final clinical practicum shapes the trasition experience and occupational commitment of newly graduated nurses in Europe- a longitudinal study. J Adv Nurs. 2021;77:4782–92.
Rodriguez-Garcia MC, Gutierrez-Puertas L, Granados-Gamez G, et al. The connection of the clinical learning environment and supervision of nursing students with student satisfaction and future intention to work in clinical placement hospitals. J Clin Nurs. 2021;30:986–94.
Sheu S, Lin HS, Hwang SL. Perceived stress and physio-psycho-social status of nursing students during their initial period of clinical practice: the effect of coping behaviors. Int J Nurs Stud. 2022;39:165–75.
Sharif F, Masoumi S. A qualitative study of nursing student experiences of clinical practice. BMC Nurs. 2005;4:6.
Ekstedt M, Lindblad M, Löfmark A. Nursing students´ perception of the clinical learning enviroment and supervision in relation to two different supervision models- a comparative cross-sectional study. BMC Nurs. 2019;18:49.
Eldridge SM, Chan CL, Campbell MJ, et al. CONSORT 2010 statement: extension to randomized pilot and feasibility trials. BMJ. 2016;335:i5239.
Lancaster GA, Thabane L. Guidelines for reporting non-randomised pilot and feasibility studies. Pilot Feasibility Stud. 2019;5:114.
Frederiksen M, Toubøl J, Crlse HB. Grundbog i mixed methods. Integration som forskningspraksis. Copenhagen: Djøfs Forlag; 2023.
Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24:105–12.
Article CAS PubMed Google Scholar
Patton MQ. Qualitative research and evaluation methods. Thousand Oaks: Sage; 2015.
Nilsen P, Seing I, Ericsson C, et al. Characteristics of successful changes in health care organizations: an interview study with physicians, registered nurses and assistant nurses. BMC Health Serv Res. 2020;20:147.
Dehlbæk MB, Nielsen ST, Nielsen EM, et al. Nyuddannede sygeplejerskers første år på arbejdsmarkedet: Undersøgelse blandt arbejdsgivere for nyuddannede sygeplejersker. 2023.
Holen M, Lehn S. Meta preceptorship and situated preceptorship in nursing: A conceptual proposal. Klin Sygepleje. 2023;3:193–204.
Kaihlanen A, Haavisto E, Strandell-Laine C, et al. Facilitating the transition from a nursing student to a Registered Nurse in the final clinical practicum: a scoping literature review. Scand J Caring Sci. 2017;32:466–77.
Sørensen J, Nielsen DS, Pihl GT. It’s a hard process – Nursing students’ lived experiences leading to dropping out of their education; a qualitative study. Nurse Educ Today. 2023;122:105724.
Mouritsen EH, Lorentzen V. Reflection on nursing theory reinforces professional identity. Fag & Forskning. 2019;2:70–4.
Günaydin N, Coban SA. Experiences of nursing students during clinical education in mental health clinics: a phenomenological quality study. Nurse Educ Pract. 2021;54:103113.
Kim EY, Chang SO. Exploring nurse perceptions and experiences of resilience: a meta-synthesis study. BMC Nurs. 2022;21:26.
Weingartner LA, Sawning S, Shaw MA, et al. Compassion cultivation training promotes medical student wellness and enhanced clinical care. BMC Med Educ. 2019;19:139.
Scarlet J, Altmeyer N, Knier S, et al. The effects of Compassion Cultivation Training (CCT) on health-care workers. Clin Psychol. 2020;2:116–224.
Kotera Y, Gordon WV. Effects of self-compassion training on wrk-related well-being: a systematic review. Front Psychol. 2021;12:630796.
Kotera Y, Cockerill V, Chircop J, et al. Predicting self-compassion in UK nursing students: relationships with resilience, engagement, motivation, and mental wellbeing. Nurse Educ Pract. 2021;51:102989.
Jafarian-Amiri SR, Zabihi A, Qalehsari MQ. The challenges of supporting nursing students in clinical education. J Educ Health Promot. 2020;9:216.
Henderson A, Harrison P, Rowe J, et al. Students take the lead for learning in practice: a process for building self-efficacy into undergraduate nursing education. Nurse Educ Pract. 2018;31:14–9.
McCullagh MC, Mecomber J, Hubscher JJ, et al. Development and testing of a practicum mathing program for baccalaureate nursing education, a local public health unit. Public Health Nurs. 2020;37:812–7.
Yi YJ, Lee H, Park K. The role of academic-practice partnerships from perspectives of nursing students: a cross-sectional study. Nurse Educ Today. 2020;89:104419.
In J. Introduction of a pilot study. Korean J Anesthesiol. 2017;70:601–5.
Download references
Acknowledgements
The authors would like to thank the nursing students, clinical supervisors, and head nurses who participated in this study.
Open access funding provided by University of Southern Denmark Open access funding provided by University of Southern Denmark.
Author information
Authors and affiliations.
Department of Education, Department of Gastroenterology, University Hospital of Southern Denmark, Esbjerg, Denmark
Helle Skou Thomsen, Britt Egeris Jørgensen, Jette Kynde Schøtz & Line Muff Bech
Nursing Education, University College South Denmark, Esbjerg, Denmark
Jette Kynde Schøtz
Department of Gastroenterology, University Hospital of Southern Denmark, Finsensgade 35, 6700, Esbjerg, Denmark
Lea Ladegaard Grønkjær
You can also search for this author in PubMed Google Scholar
Contributions
Helle Schou Thomsen, Britt Egeris Jørgensen, Jette Kynde Schøtz, Line Muff Bech, and Lea Ladegaard Grønkjær contributed to the conception and design of the study, and the acquisition of data. Helle Schou Thomsen and Lea Ladegaard Grønkjær contributed with analysis and interpretation of data, and of drafting the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Lea Ladegaard Grønkjær .
Ethics declarations
Ethics approval and consent to participate.
This study was performed according to the guidelines of the Helsinki Declaration. Due to the non-biomedical character of the pilot-study, no formal approval was required for questionnaire and interviews studies by the Danish National Center for Ethics (Sect. 14, subsection 2 of the Committees Act), and therefore not applied for during this pilot-study. However, approval to perform the pilot-study was obtained by the management at the University Hospital of Southern Denmark, Esbjerg and University College of South Denmark.
Participation was voluntary, and the participants were informed about the study both orally and in writing. Informed consent in writing was obtained from the participants. All collected data were anonymized and handled accordance with the EU´s General Data Protection Regulation (GDPR), 2016/679.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Thomsen, H.S., Jørgensen, B.E., Kynde Schøtz, J. et al. Evaluation of a new concept to improve and organize clinical practice in nursing education: a pilot-study. BMC Nurs 23 , 203 (2024). https://doi.org/10.1186/s12912-024-01888-y
Download citation
Received : 24 November 2023
Accepted : 21 March 2024
Published : 26 March 2024
DOI : https://doi.org/10.1186/s12912-024-01888-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Clinical practice
- Learning environment
- Nursing education
- Nursing students
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Lifelong learning and nurses’ continuing professional development, a metasynthesis of the literature
Mandlenkosi mlambo.
1 Jersey General Hospital, St Helier, Jersey
2 Department of LIME, Karolinska Institutet, Stockholm, Sweden
Charlotte Silén
Cormac mcgrath.
3 Department of Education, Stockholm University, Stockholm, Sweden
Associated Data
The data in the study is comprised of previous research articles. A full list of articles is included in the Table Table3 3 .
Continuing professional development (CPD) is central to nurses’ lifelong learning and constitutes a vital aspect for keeping nurses’ knowledge and skills up-to-date. While we know about the need for nurses’ continuing professional development, less is known about how nurses experience and perceive continuing professional development. A metasynthesis of how nurses experience and view continuing professional development may provide a basis for planning future continuing professional development interventions more effectively and take advantage of examples from different contexts. The aim of this paper is to conduct such a metasynthesis, investigating the qualitative research on nurses’ experiences of continuing professional development.
A metasynthesis of the qualitative literature was conducted. A total of 25 articles fulfilled the inclusion criteria and were reviewed.
We determined five overarching themes, Organisational culture shapes the conditions, Supportive environment as a prerequisite, Attitudes and motivation reflect nurse’s professional values, Nurses’ perceptions of barriers and Perceived impact on practice as a core value. This metasynthesis highlights that nurses value continuing professional development and believe that it is fundamental to professionalism and lifelong learning. Moreover CPD is identified as important in improving patient care standards.
Conclusions
Based on the metasynthesis, we argue that access to continuing professional development could be made more attainable, realistic and relevant. Expediently, organizations should adequately fund and make continuing professional development accessible. In turn, nurses should continue to actively engage in continuing professional development to maintain high standards of nursing care through competent practice. This paper highlights the perceived benefits and challenges of continuing professional development that nurses face and offers advice and understanding in relation to continuing professional development. We believe that this metasynthesis contributes with insights and suggestions that would be valuable for nurses and policy makers and others who are involved in nurse education and continuing professional development.
Introduction
Health care professionals need to update their skills regularly and continuing education, or continued professional development (CPD) enables the renewal and updating of skills in health care settings. While we know about the need for CPD, less is known about how nurses experience and perceive CPD, and currently, there is no comprehensive global picture of how nurses view and experience CPD. A metasynthesis of the qualitative literature on nurses’ experiences of CPD may provide a basis for planning future CPD interventions more effectively and take advantage of examples from different contexts. This paper is organised in the following way; first we present the notion of CPD, we then use the United Kingdom, (UK) as a setting to offer an overview of the different mechanisms that exist in one specific health care setting, which may impact engagement with CPD. We acknowledge that similar mechanisms may exist in other health care settings and countries too, and identify the UK context, merely as a way to frame the paper. Subsequently, we conduct a metasynthesis of the qualitative literature addressing the topic of how CPD is experienced by nurses.
Continued professional development
This section aims to unpack the notion of CPD, which exists in different forms and is driven, in part, by top-down requirements, but also, bottom-up, from the needs of practitioners. Continuing professional development (CPD) programmes are central to nurses’ lifelong learning and are a vital aspect for keeping nurses’ knowledge and skills up-to-date. The requirement for nurses to participate in CPD differs between European countries and elsewhere in the world and can be mandatory or voluntary [ 1 , 2 ]. For example, CPD is mandatory in the U. K, Belgium, Spain, Australia and in some states in the United States of America, [ 2 – 4 ]. In these countries, nurses engage in CPD because it is a mandatory condition by nurse regulators for remaining registered to practice. However, in Sweden, Netherlands and Ireland nurses participate in CPD of their own volition [ 1 , 3 – 5 ]. Table 1 provides an overview of some of the European countries which provide mandatory and non-mandatory CPD.
Examples of mandatory and non-mandatory CPD in nursing in Europe (EFN, 2012)
In jurisdictions where CPD is mandatory, nurses engage in continuing education by participating in professional development that is relevant to their areas of practice. Mandatory CPD, refers to “… the process of ongoing education and development of healthcare professionals, from initial qualifying education and for the duration of professional life, in order to maintain competence to practice and increase professional proficiency and expertise” ([ 6 ], p.1). CPD can sometimes refer to a learning framework and activities of professional development which contribute to the continual professional effectiveness and competence [ 7 ]. Broadly, CPD is related to continuing education, and continual learning, both formal and informal, which results in the acquisition of knowledge and skills transfer by the practising nurse with the aim of maintaining licensure and competent practice [ 8 ]. Learners can utilise a mixed style approach to learning depending on the circumstances and context of the learning environment [ 9 – 11 ]. To succeed in providing comprehensive care for their patients, nurses need to utilise the best evidence available to them [ 12 – 14 ]. This requires different modes of learning and ways of knowledge acquisition and construction. To achieve this, nurses can engage in different approaches of acquiring knowledge through CPD, through formal learning, courses or workshops as well as workplace informal learning, through self-reflection, appraising literature for best evidence through journal clubs and giving feedback to each other [ 5 , 7 , 15 ]. Informal learning is often volitional and is largely initiated and controlled by individual nurses with the intention to develop their knowledge and skills [ 16 – 18 ]. Due to its unstructured and, at times, unintentional manner, such learning is often acquired during interactions with colleagues and patients [ 19 ]. One of the advantages of on-site learning, both formal and informal is that learners can utilise expertise which are already available on the ward [ 5 , 15 ]. On-site learning occurs often at the discretion and the willingness of managers to facilitate by providing time and space for learning to occur within the clinical areas. Even so, the fact remains that informal on-site learning is not an event but a continuous process, which draws from daily professional experiences. Lack of CPD trained nurses and ward needs, coupled with poor staffing levels, are cited as main barriers to informal workplace learning [ 5 , 15 ]. Evidence from CPD literature indicates that many nurses prefer informal work-based methods of learning, noting that most meaningful learning occurs through interactions with their colleagues [ 20 ]. From a study by Clarke [ 21 ], it was noted that nurses found informal learning methods such as supervision, attending team meetings/briefings, mentoring and observations to be important. Ultimately, whichever delivery method is used for CPD, continuous professional development extends the practitioner’s professional ability beyond pre-registration training, qualification and induction, thereby potentially enhancing the practitioner’s practice.
Continued professional development: the UK example
This next section aims to illustrate the different mechanisms that arise in one specific health care setting when implementing CPD on a national scale. We recognise that other mechanisms will exist in other contexts, and in places where CPD is not a formal requirement.
Today, nurses in the U.K. are required to engage in continuous learning in order to maintain competence as a means of keeping their licensure with their professional body, the Nursing & Midwifery Council (NMC) [ 22 ]. Since the 1980s, UK nurses and other allied health care professionals such as physiotherapists and occupational therapists have been required to engage in continuous professional development [ 23 ]. A justification for CPD has been the need to maintain professional registration to practice. For registered nurses in the UK, the requirement to engage in CPD came to the fore of continuing education in 1995. It was introduced by the then licensing body, the United Kingdom Central Council for Nursing, Midwifery and Health Visiting (UKCC) as post registration education and practice (PREP) [ 24 ]. Further to that, the Agenda for Change Reforms in 2003 introduced a system for linking pay and career progression to competency called the National Health Service Knowledge and Skills Framework [ 25 ]. The framework is linked to the individual nurse’s ability to demonstrate that they possess the necessary knowledge and skills to get promoted and be remunerated accordingly [ 25 ]. In the UK, further reforms to CPD were introduced in 2012 through the introduction of the Health Education England (HEE) in England [ 27 ]. Its mandate was to equip the NHS (National Health Service) workforce, including nurses with appropriate knowledge and skills to deliver high standard care to patients. The HEE’s role was to support workforce development by providing funding largely for nurses’ CPD. In 2016, PREP was replaced with revalidation, which still requires nurses to attend 35 h of CPD every 3 years [ 24 , 26 ]. Revalidation is the process through with nurses and midwives continue as registrants with the Nursing and Midwifery Council (NMC) [ 25 ]. However, comprehensive HEE budget cuts have had a negative effect on nurse CPD initiatives [ 27 ]. CPD funding in UK was cut from 205 million pounds in 2015–16 to 83 million in 2017–18 [ 28 , 29 ]. Consequently, nurses have struggled to fulfil revalidation requirements due to some authorities freezing access and refusing to give nurses time to attend CPD activities [ 27 ].
This previous section offers an insight into different push-pull mechanisms, in the UK alone. Statutory requirements are underpinned by the need for nurses to maintain and develop the knowledge and skills to meet the expected competence standards of practice in response to expanding nursing roles and global trends. Our experience suggests that local governing bodies may enforce similar measures in contexts where CPD measure are not formalised. Nurses may find themselves caught between a patchwork of statutory requirements and a need to develop their skills and knowledge. Consequently, while we know about the need for nurses’ continuing professional development, less is known about how nurses experience and perceive continuing professional development. Therefore we propose that a metasynthesis of the qualitative literature could be a part of forming such a comprehensive view and use the following three questions to examine the literature What is the reported value of CPD for nurses’ lifelong learning and its impact on nursing knowledge?, What are the conditions necessary for CPD?, and, What are the challenges faced by nurses when engaging in CPD?
In this study, a metasynthesis was used to investigate the qualitative literature [ 30 , 31 ]. Metasynthesis is a form of systematic review method used to review qualitative studies in order to develop theory, to explore and understand phenomena or generate new knowledge, thereby creating meaning from that knowledge [ 32 – 36 ]. In this review, we present a metasynthesis based on the interpretation of qualitative results from topically related qualitative reports. In doing so we strive towards theoretical development, which according to Zimmer refers to the synthesis of findings into a product that is ‘thickly descriptive, and comprehensive’ and thus more complete than any of the constituent studies alone ( [ 30 ] p.313).
The results from metasynthesis studies may be used to underpin and inform healthcare policy, nursing practice and patient care. Furthermore, such information can be utilised by health care professionals involved in nursing education to inform planning and designing of training and educational programs. A number of steps are taken when conducting a metasynthesis [ 36 ] and involve;
a) bringing together a multidisciplinary team, in our case the team of three people includes two skilled medical education professional researchers with extensive experience in qualitative studies, including systematic reviews, moreover these two authors have more than 40 years of comprehensive experience of CPD in health care settings, two of the team are registered nurses and afford the team key insights into the context of nursing CPD, the team is spread across three institutions in two countries, finally, the team consisted of a search engine expert,
b) defining inclusive but manageable research questions, see the questions above;
c) conducting the systematic search, in our case this was conducted by the search engine expert, see Table 2 for the search criteria,
Inclusion and exclusion criteria for the review
d) quality assessment of the studies, this was done using the CASP (Critical Appraisal Skills Programme) criteria, weighting three levels (not met, partially met, totally met) where assessment was done by all three authors see Table 4 , e) extracting data from the studies, see Table 3 ,
Summary of articles with location cohort data collection method
Quality assessment according to modified CASP criteria
e) data analysis, which is explained in more detail below, and.
f) expressing the details of the synthesis which is done in the findings sections below.
Search strategy
A comprehensive systematic search of literature was subsequently conducted on Medline (OVID), PubMed and Cumulative Index to Nursing and Allied Health Literature (CINAHL), Web of Science (Clarivate) and ERIC (ProQuest). The literature search was conducted by a librarian. The literature search was conducted in December 2019 and was limited to articles published in English from 2010 to 2019. Inclusion and exclusion criteria for the literature search were established and are presented below in Table Table2. 2 . The inclusion criteria comprise of articles from empirical studies (using qualitative methods), discussing nurse continuing learning and education, professional development, lifelong learning, CPD, motivation and barriers.
Data analysis
A total of 1675 records were identified, and following de-duplication, 1395 articles remained. All 1395 articles were screened. Articles had to address nurses’ CPD and continuing education, using qualitative oriented methods. After the first screening 72 articles remained. These articles were divided into three batches and were divided among the researchers. Each author read one batch to further identify if the articles were to be included. For each batch, a second author read the articles, meaning all articles were read by at least two authors. Any remaining ambiguities were discussed and resolved among the team. Figure 1 is a summary of the literature search and screening and Table Table3 3 presents an overview of each study with its citation, location, cohort size and data collection method. 25 articles were identified for the final metasynthesis. All authors read the final 25 articles. Quality assessment using CASP criteria as outlined by Lachal et al., [ 36 ] is reported in Table Table4. 4 . In the quality assessment we assess the following components; Was there a clear statement of the aims of the research?, Is a qualitative methodology appropriate?, Was the research design appropriate to address the aims of the research?, Was the recruitment strategy appropriate to the aims of the research?, Were the data collected in a way that addressed the research issue?, Has the relationship between researcher and participants been adequately considered and reported?, Have ethical issues been taken into consideration?, Is there a clear statement of findings? We also introduce the question of whether the texts are available in Open Access form or not. We introduce this question, as we believe the outcomes on research on nurses’ perceptions and experiences of CPD is potentially important for their practice, and access via Open Access channels could act as a quality dimension. However, without access to the data and the process of interpretation we choose not to assess; How valuable is the research?, Was the data analysis sufficiently rigorous?

Overview of the steps in the literature screening
For the final analysis enabling the synthesis of the studies in this metasynthesis the articles were read carefully, findings related to the research questions; What is the reported value of CPD for nurses’ lifelong learning and its impact on nursing knowledge?, what are the conditions necessary for CPD? And what are the challenges faced by nurses when engaging in CPD?, were identified. In the next step of the analysis, study findings were examined using constant comparative analysis. The findings and conceptual categories were coded, compared, and sorted, focusing on conditions, strategies, and consequences. Finally, the synthesis, the interpretation of the findings, were described as themes, and these were revised several times until a coherent whole was formed [ 30 , 36 – 38 ] Before the final description of the synthesized themes, all the three authors discussed the content of the themes until consensus concerning credibility was reached.
From the metasynthesis we present five overarching themes, Organisational culture shapes the conditions, Supportive environment as a prerequisite, Attitudes and motivation reflect nurse’s professional values, Nurses’ perceptions of barriers and Perceived impact on practice as a core value. Each theme is further explained below with references to the relevant literature.
Organisational culture shapes the conditions
Organisational culture played an important role towards the professional development of staff. Organisational commitment and support to personal and professional development of its staff was seen as an indication that staff were valued [ 5 , 15 ] Moreover, CPD initiatives contributed to attracting and retaining staff [ 39 ]. Additionally, a culture that was flexible and adaptable to change was perceived by some participants to be favourable towards CPD [ 40 – 42 ]. Flexibility extends to matters such as CPD availability, and also location, but related also to creating opportunities in the work schedule for the nurses to participate [ 43 ]. Other organisational factors such as funding for CPD programs, staff access of CPD learning, role of management in staff CPD, manageable nursing workloads, the design & delivery of CPD activities, communication and collaboration between CPD providers and management are specifically organisational factors seen as crucial to effective staff development [ 44 , 45 ]. Developing a strategy for CPD was also acknowledged as a key element of organisational culture as a way of enabling participation [ 46 ]. In a similar fashion, it was argued that the organisation needs to be focussed on incremental, but constant development of practices, and here CPD was seen to play a key role [ 47 ]. This sentiment was expressed elsewhere too, but from a re-skilling, or keeping up-to-date perspective, where the organisation is seen to have great importance [ 48 , 49 ]. The value of partnerships and shared understanding between managers and nurses as key enabling factors was identified in several studies [ 46 , 50 ]. In a related fashion, Jantzen argues that organisations should actively avoid fragmentation of CPD initiatives [ 51 ]. As more CPD training is digitised IT/ICT (information communication technology) skills were seen as key to successful CPD implementation [ 46 , 52 ]. It was acknowledged that the transformation to online learning does not only affect nurses, it involves change for the whole department [ 52 ].
Supportive environment as a prerequisite
An environment that supports learning was seen as a necessary prerequisite for CPD. Conditions had to include, flexible off-duty patterns to allow time for staff to study, availability of workplace learning, workloads were not excessive and CPD was fully funded or a shared responsibility between employer and staff [ 46 , 52 ]. Other indicators of a supportive environment included staff access to different CPD activities relevant to their career goals, while at the same time meeting organisational goals and where staff felt free to study openly and not secretively [ 15 , 41 ]. Moreover, the development of local and contextual CPD was seen as something that supported and made participation possible [ 43 , 53 , 54 ]. Participants indicated that nurses required financial support and practical support in the form of adequate time to participate in CPD activities and suitable staff cover when colleagues were away attending CPD activities [ 47 ]. Jantzen et al. [ 51 ] suggest there are three catalysts in a supportive environment; mentors, workplace camaraderie and a highly functional workplace team. Moral support or encouragement was identified in more than one study, where it was articulated that learners want to know there is an appreciation for the time and dedication needed to engage in CPD [ 44 , 46 , 50 ]. The value of learning from other health professionals other than nurses, in the day-to-day work was highlighted for professional development [ 54 ]. Similarly, the sense of a supportive environment with a strong team spirit is communicated elsewhere [ 39 ]. Explicit support is noted in several studies; support for novice nurses [ 39 ] but also the importance of explicit managerial support [ 55 ]. Conversely, in one study, respondents noted that there was less support for experienced or late career nurses [ 56 ].
Attitudes and motivation reflect nurse’s professional values
The value and importance of CPD was discussed in many of the studies. In some, CPD was perceived to be key in defining nurse professionalism [ 6 , 15 , 40 , 47 , 49 ]. Engaging in CPD was also viewed by new nurse graduates as an important element of their individual professionalisation in nursing [ 6 , 15 , 40 ]. In addition, CPD was perceived to be important for enhancing and up or re-skilling, keeping knowledge and skills up-to-date, considering that nursing practice has become more evidence based [ 6 , 43 , 46 , 51 , 54 , 56 ]. Furthermore, nurses stated that CPD was important for maintaining licensure, and felt that the responsibility for enrolling and participating in CPD activities was with the individual nurse, not with the employing organisations [ 53 ]. On the other hand, participants felt more motivated to learn if they could easily access CPD programs, if they felt supported and if there were a variety of CPD activities on offer. Here, bedside and informal learning was emphasized as important [ 57 ]. Similarly, contextualising learning and placing it in close proximity to practice was seen to enhance motivation and engagement [ 42 ]. CPD was also viewed as a way to start networking with other peers [ 44 ]. In one study, a competency framework was introduced, here participants felt that such a framework could help them reflect on their own practice and, as it provides a systematic approach to assessing a patient, look at their own strengths and weaknesses [ 58 ]. Such competency frameworks help to harness scarce training more effectively and encourage individuals to take more responsibility for their own development [ 58 ].
Participants’ attitudes towards CPD funding were mixed, with some stating that funding for CPD was the employer’s responsibility, while others felt that the individual practitioner was responsible or that the burden ought to be shared between the organisation and the nurse [ 5 , 15 , 40 ].
Nurses’ perceptions of barriers
Poor staffing levels, heavy workloads, lack of funding, lack of study time and anti-intellectualism were some of the perceived barriers to CPD brought out by this review. Participants in the studies reviewed felt that a lack of organisational support, especially from their managers, was an indication that the organisation did not take professional development of its staff seriously [ 46 ]. Some respondents reasoned that an anti-academic culture and lack of relevant CPD programs was further indication of this [ 5 , 15 , 40 ]. Seeing a connection to patient care was identified as a strong driver and nurses identified that CPD initiatives would be filtered out unless there was such a clear connection to patient care [ 43 , 51 ].
Additionally, some studies indicated that as role models, managers had to show interest in their own CPD, in order to motivate other nurses. In other words, the manager’s knowledge of CPD activities was reflected by their attitude towards work-based study, acceptance of staff who studied openly, the way the manager prioritised funding support and managed staff shift schedules to allow study release time [ 5 , 39 , 54 , 56 ]. Fatigue was identified as a major barrier. For example in Jho et al. [ 53 ], in a context of mandated CPD, respondents felt tired due to the heavy nursing workload in conjunction with CPD. Lack of strategy, and financial initiatives in terms of money, or time off to study was also acknowledged as a barrier [ 5 , 39 , 54 , 56 ]. Lack of transparent career trajectories were also acknowledged as an area of concern [ 44 ].
Other barriers, or de-motivating factors were identified; difficulties in attending CPD and keeping a life-work balance [ 48 ]. Barriers included: formal CPD courses away from the clinical areas were perceived to lack in authenticity [ 47 , 49 ] and a mis-match in expectations and outputs, where nurses viewed themselves as agents of change, but where the organisation was unable to offer means to capitalise on this perception and desire to bring about change [ 50 , 59 ]. As much as competency frameworks were viewed positively in offering a sense of direction, a divergent view was that they were limiting or created set boundaries that participants experienced as limited, for example, if used as prescriptive, hindering nurses to define their own learning needs [ 58 ]. Lack of IT competence was also perceived as a barrier [ 52 ] with more CPD being conducted online.
Perceived impact on practice as a core value
The impact of CPD on nursing practice was perceived as important and valuable in different ways. The impact could be both direct and indirect depending on the organisational culture [ 41 , 45 ]. This mixed perception could be due to the complex nature of health care organisations which can make knowledge sharing difficult [ 45 ] and that some CPD learning was done secretly, results of which were difficult to evaluate [ 41 ]. In the case where a competency framework was studied, participants felt that using the competency framework helped them organise their work and their thought processes [ 58 ]. A common sentiment was that CPD would benefit health care organisation through the provision and enhancement of practitioners’ knowledge and skills [ 46 ]. Sentiments articulating expectations of an impact of CPD could also be seen elsewhere too [ 52 , 55 , 56 , 60 ]. Moreover, CPD is expected to rely on better communication between managers and nurses as a way of informing each other about needs and means of fulfilling those needs [ 48 ]. Direct impact was realised through improved interprofessional collaboration and the idea that new methods could be directly translated into practice [ 47 ]. Others however, raised concerns that CPD programmes or courses may not translate into new practices [ 50 ]. This sentiment was echoed elsewhere too, where a need to situate CPD in close proximity of patients was seen as important for CPD to impact practice [ 49 ] While indirect impact happened through dissemination of knowledge and skills from CPD learning to other nurses at ward level, arguments were put forward that there will be no difference to practice unless organisational processes support and evaluate its effect on practice [ 46 ]. Participants reported that their professional confidence was enhanced, they felt they could challenge medical decisions and the status quo [ 41 ]. Furthermore, participants felt that CPD enhanced their professional knowledge and skills for better patient care through improved care standards, how they communicated and collaborated with other professionals. Participants also believed that learning increased their chances for career progression and reduced work-related anxiety because of enhanced knowledge [ 40 , 41 ].
The aim of this paper is to conduct a metasynthesis investigating the qualitative research on nurses’ experiences of continued professional development. As a result, this metasynthesis revealed a number of overarching themes, which synthesize the findings of previous qualitative oriented research during the period 2010–2019. 2010 was chosen to include the last 10 years of CPD research. The themes are; Organisational culture shapes the conditions, Supportive environment as a prerequisite, Attitudes and motivation reflect nurse’s professional values, Nurses’ perceptions of barriers and Perceived impact on practice as a core value. The themes put focus on important issues that were recurrently put forward by the nurses in the studies reviewed. However, the themes are not isolated from each other, rather, the content of the themes is interrelated. Some of the themes mainly mirror an overarching perspective at the organisational level of health care, while other themes describe the nurses’ experiences and needs on a personal level. The following discussion explores the above themes in relation to the three questions posed earlier; what is the reported value of CPD for nurses’ lifelong learning and its impact on nursing knowledge? What are the conditions necessary for CPD? What are the challenges faced by nurses when engaging in CPD? While we acknowledge that the questions and themes overlap, we have endeavoured to frame the discussion around the three research questions individually.
What is the reported value of CPD for nurses’ lifelong learning and its impact on nursing knowledge?
Nurses reported that CPD raises professional standards through competencies gained, thereby increasing professional performance with positive benefits for patients, organisations and individual nurses [ 40 ]. These outcomes were seen most prominently in the themes Attitudes and motivation reflect nurse’s professional values, and Perceived impact on practice as a core value. Closely aligned to CPD are the nurses’ clinical effectiveness and competence. Maintaining both requires nurses to keep their practice up-to-date highlighting the importance of CPD for nurses. The knowledge and skills gained by nurses through CPD advances the professional status of nursing, which was an idea that was prevalent in some of the studies in this review [ 15 , 40 , 47 , 50 ], but is also illustrated elsewhere in the literature [ 8 , 21 ]. Nurses acknowledged that expectations of professional accountability meant that standards of practice ought to be kept high in order to pass public scrutiny [ 15 , 40 ]. Furthermore, skills acquired through CPD, such as the ability to conduct systematic peer-reviews [ 45 ] and appraise literature for best evidence, provide nurses with essential professional competencies, embeds values such as caring behaviours, influences beliefs and attitudes which in turn shape nurses’ professional conduct [ 61 ]. As such CPD is seen as a tool for nurses to update their skills, and in doing so deliver safe and high-quality health care. As revealed in this review, nurses were willing to fully fund or part-fund their CPD as long as CPD programs were captivating, easily accessible, there was fair allocation of study time and their efforts towards CPD were recognised. The latter implies that nurses want time and space to transfer their CPD learning into practice and for their CPD to be recorded [ 5 , 45 ]. The belief is that, consequently, patient care will improve with positive impact from organisational change [ 15 , 45 ]. However, it is clear that the organisation is key in making CPD work for nurses. The issues brought up in the theme organisational culture shapes the conditions is thus very important in stimulating nurses to engage in CPD. The nurses’ attitudes and motivation to engage in CPD also depends on a supportive environment and engagement may in turn influence the organisational culture.
What are the conditions necessary for CPD?
A disconnect could be seen in relation to the conditions for CPD, where access to CPD training came to the fore as problematic in some of the studies. Nurses had to travel long distances to attend courses [ 15 , 62 , 63 ]. To avoid these challenges, nurses settle for CPD as long as it fulfils mandatory requirements for registration [ 53 ]. If intentions of CPD are to provide a basis for the continual updating of skills, then authentic learning as an expected outcome is seen as a prerequisite for nurses to engage in CPD, whether it occurs at the bedside, at a training facility or through an IT mediated interaction. This calls for accessible CPD, improved design and delivery methods for all nurses [ 52 ]. Nurses’ experiences described in the themes Organisational culture shapes the conditions, Supportive environment as a prerequisite, show that structural and moral support are both important. Structural support in the form of availability, time to engage in CPD, as well as clear expected outcomes [ 46 , 49 ], but also moral support in the form of an understanding management and environment, and also peers and leaders who themselves also prioritise CPD [ 58 ]. Organisational support and commitment towards CPD should mean allocation of study time, support of nurses who study privately, by creating space for knowledge and skills integration and managing poor cultural practices that hinder open study. Funding is seen as a key factor across many of the studies, both in terms of enabling nurses to participate, but also as a way of acknowledging nurses who engage in CPD. Further studies may need to look more closely at how nurses perceive different aspects of funding. For nurses’ lifelong learning to endure, CPD programs need to be more accessible and kept interesting by making them more relevant to nurses’ practice contexts. Here the importance of the organisation for creating a CPD conducive environment is emphasized [ 46 , 51 , 52 ]. As role models, managers need to lead by example and engage in CPD themselves, but also demonstrate explicit support. They also need to influence policy to create environments conducive to CPD. If funding situations do not improve, work-based CPD learning could be one of the alternative ways of CPD delivery for nurses. To promote CPD engagement and cost reduction, eLearning approaches could be utilised for education and training. However, poor IT skills among nurses, but also within organisations continues to be a potential weakness [ 52 ]. A challenge remains here in enabling nurses to get recognition from informal on-site learning [ 16 – 18 ], where elements of meta-cognitive reflection can be used to acknowledge nurses’ continued professional development.
What are the challenges faced by nurses when engaging in CPD?
In some of the literature reviewed, participants lamented their current conditions for CPD, and identified clear barriers and challenges in the form of concerns related to lack of funding for CPD, staffing levels, time allocation for study, lack of organisational support because of negative cultural practices, CPD design & delivery and limited choice of CPD activities. This is articulated within the themes: Organisational culture shapes the conditions, Supportive environment as a prerequisite, Nurses’ perceptions of barriers [ 2 , 11 , 34 , 41 ] . However, studies did not explore the views of nurses on recruitment and retention and its impact on accessing a variety of CPD activities. Evidence from this review indicates that modernising healthcare and simultaneously cutting CPD funding for nurses could lead to a limited number of nurses attaining the skills and competences needed for the modernisation process. In view of the understaffing that is reported elsewhere [ 5 , 15 ], we identify a cause for concern. These perceived barriers may undermine nurses’ professional development [ 23 , 59 ]. Moreover, the findings presented here revealed that nurses face a number of challenges in relation to their CPD participation. The challenges include limited CPD activities to choose from, poor CPD delivery methods, negative organisational culture practices such as anti-intellectualism and lack of support. As a result, nurses were less motivated to participate in CPD training [ 57 ].
It is clear from the review, that IT concerns are becoming more and more prominent, given that more CPD programmes are being offered through digital platforms [ 47 ]. This is a concern for both the individual nurses, but also their organisations. On concerns regarding CPD delivery methods, nurses indicated that they preferred different styles. With these concerns comes the view that learners learn in different ways depending on the context and subject of study [ 61 , 62 ]. This supports the notion that individuals have different learning preferences [ 61 ], where some adult learners learn better in a structured and teacher guided context, while others prefer self-direction.
Limitations
The search was conducted by an experienced search engine expert. Even so, we may still have been unsuccessful in finding all the relevant articles. The study was focussed on qualitative studies, which means that studies using predominantly quantitative or mixed methods were not included, but could hold important insights. In the introduction to the study we used the UK as an example for how CPD might be regulated. However, we have conducted a comprehensive search of the literature and our analysis was not conducted with a UK-centric perspective. While each study needs to be understood in terms of local rules and regulations, the similarities in the findings are striking.
The metasynthesis indicates that differences exist between the nurses’ CPD needs and expectations and organisations’ approaches to nurses’ professional development. The review lays bare a disconnect between the rhetoric of identifying CPD as a way to enhance nurses’ skills, and the reality of CPD interventions, where nurses do not feel support within their organisations or from their immediate supervisors. The review also revealed that CPD is an important element of nursing practice and nurses’ lifelong learning. Furthermore, it suggests that nurses are motivated to take part in CPD to enhance their knowledge, improve skills and keep up- to -date with recent evidence. While evidence from this review indicates that nurses believe that CPD has a positive impact on patient care, there is lack of contemporary research to qualify this claim and there is limited evidence from this review to support this assumption. However, evidence from the review suggests and confirms, that the greatest barriers for CPD in nursing are a lack of funding and time to participate in CPD activities, which are clearly related to organisation structure. It is difficult to envisage how such conditions could be conducive for nurse CPD to flourish. Such perceived barriers undermine nurses’ efforts to keep knowledge and skills up-to-date and provide better patient care while meeting the ever-changing needs and expectations of their patients. This is further exacerbated by negative organisational cultural practices and lack of knowledge on how to facilitate, design and deliver CPD for their staff. We conclude that policy makers and relevant stakeholders need to put in place strategies to support nurse CPD in long term and in doing so tear down the barriers of CPD.
Acknowledgements
We would like to thank Gun Brit Knutssön, at Karolinska Institutet’s University Library, Stockholm, Sweden for the systematic search.
Abbreviations
Authors’ contributions.
MM, CS and CMG designed the study. MM, CS and CMG defined the inclusion and exclusion criteria for the search. MM, CS and CMG conducted an equal share of the analysis work. Versions of the manuscripts were shared, revised and written by all three authors. All authors have read and approved the submitted manuscript.
Open Access funding provided by Stockholm University.
Availability of data and materials
Declarations.
Ethical vetting in Sweden is conducted by a central and national committee, the Swedish Ethical Review Authority. Review articles where research is not conducted on humans, or animals does not require ethical vetting as per Swedish Ethical Review Act (SFS 2003:460).
Not Applicable.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.

VIDEO
COMMENTS
Critical thinking is a complex, dynamic process formed by attitudes and strategic skills, with the aim of achieving a specific goal or objective. The attitudes, including the critical thinking attitudes, constitute an important part of the idea of good care, of the good professional. It could be said that they become a virtue of the nursing ...
Critical thinking is applied by nurses in the process of solving problems of patients and decision-making process with creativity to enhance the effect. It is an essential process for a safe, efficient and skillful nursing intervention. Critical thinking according to Scriven and Paul is the mental active process and subtle perception, analysis ...
Although the literature on critical thinking and transformative learning has remained ... considering perspective-taking readings at the university level. Traditional academic readings - including textbooks, peer-reviewed journal articles, and scholarly books - tend to make objective, evidence-based arguments to support theoretical ...
Lastly, we show that critical thinking constitutes a fundamental component in the research process, and can improve research competencies in nursing. We conclude that future research and actions must go further in the search for new evidence and open new horizons, to ensure a positive effect on clinical practice, patient health, student ...
Critical thinking in nursing; it is a thinking process that includes features such as collecting and organizing the data obtained from the patient/healthy individual, deciding on the needs in parallel with these data, choosing one of the possible approaches based on knowledge and developed with applications, and evaluating the results of the ...
DOI: 10.5455/aim.2014.22.283-286. Critical thinking is defined as the mental process of actively and skillfully perception, analysis, synthesis and evaluation of collected information through observation, experience and communication that leads to a decision for action. In nursing education there is frequent reference to critical th ….
Although previous literature reviews have been conducted relative to CT in nursing education, few recent systematic reviews have been conducted. This systematic review aims to review qualitative studies from 2002 to 2011, in order to explore how critical thinking is perceived in the studies of nursing education, and the obstacles and strategies ...
Critical thinking in acute care nursing education. Active participation and problem-based learning are strategies used to promote critical thinking in the clinical environment ( Distler, 2007 ). Carter et al. (2016) reviewed teaching tools to promote critical thinking in nursing and midwifery students. Seven of the 28 reviewed studies suggest ...
76 nursing programs participated in the study. The Reflective and Critical Thinking was found as a subject, subject content and didactic strategies. Of the 562 subjects reviewed, this type of thinking is found in 46% of the humanities area and 42% in the area of research and professional discipline. It is important to train teachers to achieve ...
Introduction Applying critical thinking is essential for nursing students both in an academic and clinical context. Particularly, as critical thinking is a vital part of nurses' everyday problem-solving and decision-making processes. Therefore, regardless of the topic taught or the setting in which it is taught, it requires teaching strategies especially targeting students' critical ...
Abstract. Critical thinking skills are essential to function in today's complex health care environment and to ensure continuing competence for the future. This article provides a review of ...
Abstract. Critical thinking skills are essential to function in today's complex health care environment and to ensure continuing competence for the future. This article provides a review of various definitions and research studies related to critical thinking. Educators and researchers need to clearly define critical thinking, because there has ...
Some have also defined critical thinking in nursing as "the process of reflective and reasonable thinking about nursing problems without a single solution and is focused on ... Bakalis N. Clinical decision-making in cardiac nursing: a review of the literature. Nurs Stand. 2006; 21 (12):39-46. doi: 10.7748/ns2006.11.21.12.39.c6386. ...
The ability to use reasoned opinion focusing equally on processes and outcomes over emotions is called critical thinking ( Paul and Elder, 2008 ). Critical thinking skills are desired in almost every discipline and play a major role in decision-making and daily judgments. The roots of critical thinking date back to Socrates 2,500 years ago and ...
Data were collected by a questionnaire analyzed using Pearson's correlation test. In this study, nurses had good critical thinking, clinical decision-making abilities and handover quality. There is a strong relationship between critical thinking and clinical decision-making and the quality of nursing handover (p = 0.001; r = 0.384; r = 0.247 ...
The objective of this study is describe the effect of educational intervention on critical thinking, in nursing students of the 2nd year, based on the peer review, using the Cornell test (Level X ...
Objective: to reflect on Florence Nightingale's legacy and describe her contributions to critical holistic thinking in nursing. Methods: this is a theoretical reflection, for which scientific productions on Florence Nightingale's environmental theory, as published in national and international journals, were based. Results: Florence Nightingale's philosophy and teachings emphasize that the ...
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood ...
Other investigators advocate for critical thinking as a model of intelligence specifically designed for addressing real-world problems. Yes, intelligence (i.e., critical thinking) can be enhanced and used for solving a real-world problem such as COVID-19, which we use as an example of contemporary problems that need a new approach. Keywords ...
Peer Review reports. ... Relationships between critical thinking ability and nursing competence in clinical nurses. J Clin Nurs. 2011;20(21-22):3224-32. Article Google Scholar Shoulders B, Follett C, Eason J. Enhancing critical thinking in clinical practice: implications for critical and acute care nurses. Dimens Crit Care Nurs. 2014;33(4 ...
Papastavrou, Hamari, Fuster, Istomina, and Salminen (2016) designed a peer-review activity in which nursing students were asked to review peers' nursing journals written on social media. The experimental results showed that the approach facilitated the students' reflections, knowledge acquisition, and critical thinking.
Formal preceptor development and education for experienced nurses assists them to support new nurses through constructive feedback and encouragement of critical thinking, and in turn, enhances preceptor satisfaction and retention (Rush et al., 2019). Given the valuable role of the preceptor in supporting new nurse transition to practice ...
Clinical reasoning is considered a crucial concept in reaching medical decisions. This paper reviews the reasoning processes involved in clinical reasoning from the perspective of cognitive psychology. To properly use clinical reasoning, one requires not only domain knowledge but also structural knowledge, such as critical thinking skills.
Nursing students may experience clinical practice as unsafe due to the interactions with patients, fear of making mistakes, lack of clinical experience and supervision, which results in anxiety and stress. Thus, interventions to improve and organize the learning environment in clinical practice for nursing students are warranted, and the aim of this pilot-study was to evaluate a new concept of ...
Non-peer reviewed journal articles. Theses or dissertations. Editorials, commentary or opinion articles ... A critical moment: NHS staffing trends, retention and attrition. London: Health Foundation; 2019. 28. House of Commons Health Committee . The nursing workforce, second report of session 2017-19. ... Articles from BMC Nursing are ...