- Research note
- Open access
- Published: 23 September 2021

The pattern of health insurance economic resilience in the Covid 19 pandemic shock
- Erfan Kharazmi ORCID: orcid.org/0000-0002-2138-896X 1 ,
- Shima Bordbar ORCID: orcid.org/0000-0002-0902-6499 1 &
- Hanie Gholampoor ORCID: orcid.org/0000-0002-0569-537X 2
BMC Research Notes volume 14 , Article number: 371 ( 2021 ) Cite this article
1965 Accesses
2 Citations
4 Altmetric
Metrics details
Health insurance is based on people’s significant risks in receiving health services that they cannot afford alone. Since the outbreak of the corona epidemic, the health insurance system has suffered many economic problems. Designing a model of a health insurance system based on the requirements of a resilient economy can improve the functions of this system in the corona crisis.
In this research 12, structural components were obtained in the form of 4 conceptual components. The 4 main conceptual components are Knowledge-based economy, Economic stability, Economic resilience, and justice. The knowledge-based economy is the basis for the formation of economic resilience in the health insurance systems. Health insurance systems will achieve two crucial intermediate results, namely economic resilience, and economic stability, by building the basic infrastructure of a knowledge-based economy. In the long run, maintaining such intermediate results is the foundation of justice in the health insurance system.
Introduction
The World Health Organization considers the right to health as a fundamental right for all [ 1 , 2 ]. Countries are required to ensure the availability of sustainable financial resources alongside other health resources to realize this right [ 3 , 4 , 5 ]. Insurance usually plays the role of an intermediary organization in transferring financial resources from the consumer of health services to its provider [ 6 , 7 ]. Health insurance is based on people’s significant risks in receiving health services that they cannot afford alone. One of the goals of health insurance is to distribute income in favor of people who cannot cope with these risks [ 8 , 9 ].
On the other hand, we live in a century when the economies of the world's countries face various threats and pressures. Each organization reacts differently to stressors according to its position [ 10 , 11 , 12 ]. “Economic resilience” has been introduced as a suitable model for overcoming the general challenges of economic systems in recent years [ 13 , 14 ]. Briguglio uses the idea of “Economic resilience” in two general senses: The first is the ability of the economy to emerge from nasty economic shocks, and the second is the ability of the economy to withstand the effects of these shocks [ 15 , 16 ].
Health insurance systems are also exposed to economic pressures and damage like other economic sectors. One of the damages that have recently severely affected health systems is the occurrence of the Corona pandemic. Health systems and related insurance systems have been involved in many ways as a result of this pandemic. These effects have not only been in the field of essential services of these systems but have also drastically changed the outputs and consequences of these systems [ 17 , 18 , 19 , 20 ].
There is a combination of public and private health insurance programs in the Iranian health system. “Social Security Insurance” and “Health Insurance” are the main insurance organizations in Iran. The Armed Forces Insurance Organization and the IMDAD Committee Insurance Organization also operate in Iran. The last two organizations cover a smaller population [ 21 ]. Iran, among different countries, in addition to severe and risky exposure to Covid 19 disease, has been exposed to various pressures and injuries from the economic point of view for some time. The present research has studied the model of health insurance systems based on Economic resilience that can maintain the stability of insurance services in Iran.
The concepts of Economic resilience in health insurance were extracted using the opinion of experts in the field of health insurance at the beginning of a descriptive and analytical combined study. However, a list of concepts of Economic resilience in health systems, especially in health insurance, was prepared to help experts by referring to studies. Then the semi-structured interview method was used. In this study, researchers have used a questionnaire developed in Heidari's research [ 22 ]. The collective views of 30 key people and experts in the field of Economic resilience and health insurance were extracted, including former and current ministers and deputies of the Ministry of Health, former and current heads and deputies of health insurance organizations, professors of health services management and professors of health economics.
The abovementioned individuals were selected based on the purposive sampling method using the following criteria:
At least ten years of executive and managerial experience at the level of health insurance or the Ministry of Health
Membership in the headquarters of the Economic resilience or similar cases in health insurance or the Ministry of Health
Acquisition of a study and research background on the subject of Economic resilience and insurance systems
People who were reluctant to participate in the study or challenging to reach due to distance or busy schedules were excluded from the study and replaced by new ones. Achieving the final concepts of Economic resilience was done using the content analysis method, and sampling and collecting experts' opinions continued until reaching theoretical saturation of data and not achieving a new theme. The six-step approach of the Clarke & Braun was used, including familiarity with the data, creating the initial code, searching for themes, forming sub-themes, defining and naming the main themes, and preparing a final list at this stage of the research. The last themes were reviewed and validated using the opinion of scientific experts outside the research sample. After identifying and grouping the practical components in the Economic resilience of health insurance systems, Mick Mac's analysis was used to determine the position, influence, dependency, and stability of the designed system. The identified components were scored using a range of numbers from 0 to 3 by a group of experts. Mick Mac matrices were formed in the following four modes: MDI, MII, MPDI, MPII. Then the matrix outputs were categorized and analyzed in the form of graphs and Mick Mac maps.
It was also investigated to calculate the vitality coefficient of each component based on the following formula for more detailed analysis based on the assumptions of the DSM (Design Structure Matrix) technique.
In the first steps of this research, the general components of resistance economy in health insurance systems were identified based on previous studies and expert opinions at three levels of conceptual, structural, and functional features. This study aimed to determine the macro model of the health insurance economic resilience in the critical situation of Covid 19. Therefore, the third-level components were not included in Mick Mac’s analysis. The identified features were summarized as follows (Table 1 ):
Additional file 1 : Table S1 shows the consumption pattern modification component has the highest number of essential elements among the organizing components, and the private sector strengthening component has the lowest fundamental part.
The position of each component to the other features and their role was determined by entering the second-level parts in Mick Mac software. The structural modification component has the most direct and indirect influence, among other features. The components of social justice and deprivation are much more dependent than other components.
The direct influence maps of the components indicate that the independent variables are research and development, structural modification, and modification of consumption patterns.
On the other hand, dependent variables and outputs of the economic resilience system are considered health insurance components of people's purchasing power, endogenous financing, deprivation, and social justice. In the model, no component was identified as a linkage variable (Fig. 1 ).
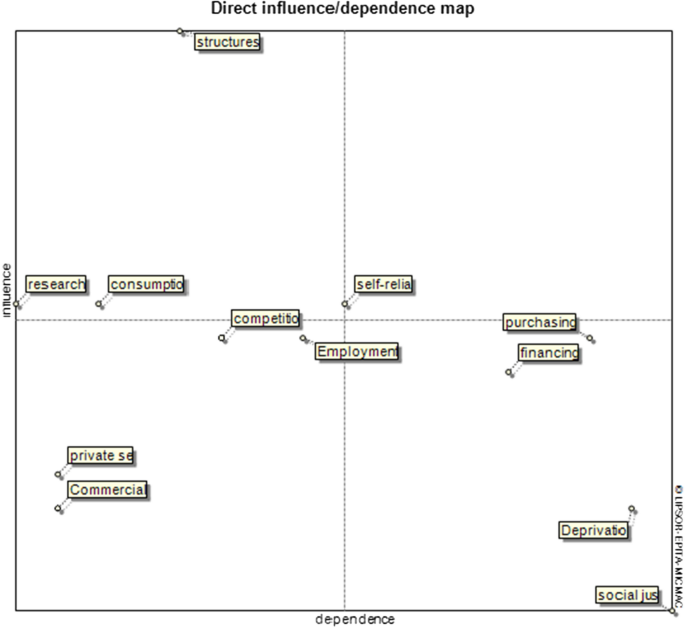
Direct and influence/dependence map of the health insurance economic resilience system
In Fig. 2 , we can see the intensity of the influence of the components on each other. The indirect influence graph of the components clearly shows the strong relationship between structural modification by deprivation and social justice.
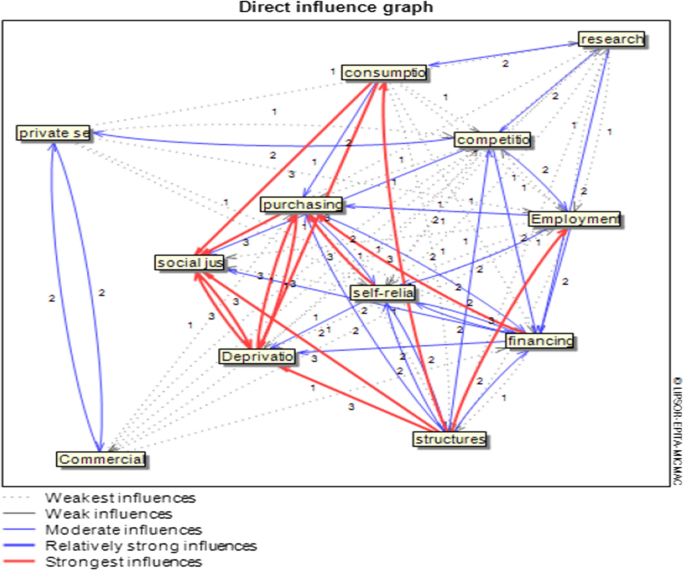
direct influence graph in the health insurance economic resilience system
Many researchers have considered an issue in recent years because of the need for a local model for health insurance in the event of various crises, including economic concerns and epidemiology [ 23 , 24 , 25 , 26 ]. Combining the two analyses of content analysis and Mick Mac analysis can be very effective in modeling complex systems [ 27 , 28 , 29 , 30 , 31 ]. The study aimed to identify appropriate inputs to identify influential variables in the model of the health insurance economic resilience systems using the results of the content analysis method. Then, the position and relationship of these variables are examined using the Mick Mac analysis method.
Three variables set in the second quarter of Mick Mac's direct influence map include Research and Development, consumption pattern modification, and structure modification. These variables are considered the inputs of the system and are affected mainly from outside. Therefore, they can be named as environmental and uncontrollable variables. The occurrence of changes in these three variables can affect the system set under review, and in some cases lead to a crisis in the scheme of the health insurance. The structural modification variable is located above the central diameter of the second quarter, so this variable has a more significant influence on the insurance system than the other two variables of this quarter. The structural modification could strengthen health insurance against environmental tensions and crises, including the Corona epidemic, and guarantee continued services in such circumstances [ 32 , 33 ].
In the third quarter of the map are the variables of empowering the private sector, improving the competitive environment, sustainable employment, and commercialization. These variables are considered independent variables. However, the two variables of sustainable employment and improving the competitive environment can play a regulating role in the health insurance system, given that they are located near the coordinate center. Other sectors of the health insurance economic resilience can perform better by strengthening these two variables. On the one hand, efforts to improve services in the health insurance system will increase with competition between private insurers and innovation will be formed in different parts of health insurance [ 34 , 35 ].
The fourth quarter includes four variables: strengthening people's purchasing power, endogenous financing, deprivation, and social justice. These variables are affected by other variables and are considered the outputs of the health insurance economic resilience system. That is, the occurrence of any event in other variables can change these four variables. The two variables of deprivation and social justice are the ultimate goal of the health insurance system, which are placed at the bottom end of the fourth quarter.
Additional file 2 : Figure S1 shows the two variables of strengthening people's purchasing power and endogenous financing are among the most vital variables of this system. They have a high capacity for influence and dependence at the same time. Health insurance companies must have strategies for endogenous financing to continue and maintain service continuity in the event of various crises. Otherwise, economic resilience in health insurance is problematic [ 36 , 37 ].
No variables were identified in the first quarter of the map in this study, and the map is L-shaped. Therefore, the current system of economic resilience is a stable system with the studied variables. Analysis of variables in the indirect influence map has similar results, but the position of some variables also shows changes. Additional file 3 : Figure S2 shows, the endogenous financing variable is located close to the coordinate center in this case. It has become a regulator. An indirect influence map can also help understand the role and interaction of variables in the long run. For example, the consumption pattern correction variable has lost its regulatory properties in the long run and has become an independent variable. This change of position indicates that in addition to health systems, insurance systems should also be responsible for improving the consumption pattern of health services and constantly monitoring and controlling patients' and society's consumption patterns [ 38 ].
Mick Mac's analysis graph shows the intensity of influences between variables in both direct and indirect modes. It can be seen how the variables of strengthening people's purchasing power, deprivation, and social justice are affected by other variables. Additional file 4 : Figure S3 shows the only variable of structural modification has retained its strong influence on the two variables of deprivation and social justice in the indirect graph. Here, the importance of variable structural modification in a sustainable insurance system is evident. The decrease in density and the number of red lines of decisive influence in changing the direct to indirect graph show that the resilience economy method is mortal in the long run. It means if there is no planning and effort to maintain this system, the effects of variables on each other will gradually decrease, and the achievement of output (justice) will reduce. Therefore, health insurance systems must continuously monitor and control their economic systems and plan and maintain their essential functions.
Health insurance organizations must pay close attention to their organizational structures to maintain their efficiency in times of crisis such as Covid 19. By reforming organizational structures, it will be possible to achieve "endogenous financing" and "internal self-reliance" in insurance systems. These three factors will ultimately lead to social and individual justice in insurance systems. The existence of a stable resistance economy in insurance companies not only prepares them for the crisis, but also causes them to perform better after the crisis.
Limitation.
One of the main limitations of this research was access to experts. Many experts were reluctant to be interviewed due to their busy schedules.
Also due to the prevalence of Covid 19, face-to-face interviews were not possible.
Availability of data and materials
The present research data will be available upon logical request. If anyone wants to request data, they should contact corresponding author.
Abbreviations
Matrix of direct influences
Matrix of indirect influences
Matrix of potential direct influences
Matrix of potential indirect influences
Design structure matrix
Brenes F. Immigrants and the Right to Health Care in the Era of COVID-19. Hisp Health Care Int. 2020;18(4):178–9. https://doi.org/10.1177/1540415320958614 .
Article PubMed Google Scholar
Pūras D, de Mesquita JB, Cabal L, Maleche A, Meier BM. The right to health must guide responses to COVID-19. Lancet. 2020;395(10241):1888–90. https://doi.org/10.1016/S0140-6736(20)31255-1 .
Article PubMed PubMed Central Google Scholar
Watson CR, Watson M, Sell TK. Public health preparedness funding: key programs and trends from 2001 to 2017. Am J Public Health. 2017;107(S2):S165–7. https://doi.org/10.2105/AJPH.2017.303963 .
Nam EW, De Leeuw E, Moon JY, Ikeda N, Dorjsuren B, Park MB. Sustainable funding of health initiatives in Wonju, Republic of Korea via a tobacco consumption tax. Health Promot Int. 2011;26(4):457–64. https://doi.org/10.1093/heapro/dar011 .
Rechel B, Brand H, McKee M. Financing public health in Europe. Gesundheitswesen. 2013;75(5):e28-33. https://doi.org/10.1055/s-0033-1343433 .
Article CAS PubMed Google Scholar
van Kleef RC, van de Ven WP, van Vliet RC. Risk selection in a regulated health insurance market: a review of the concept, possibilities and effects. Expert Rev Pharmacoecon Outcomes Res. 2013;13(6):743–52. https://doi.org/10.1586/14737167.2013.841546 .
Lieber EMJ. Does health insurance coverage fall when nonprofit insurers become for-profits? J Health Econ. 2018;57:75–88. https://doi.org/10.1016/j.jhealeco.2017.09.001 .
Withagen-Koster AA, van Kleef RC, Eijkenaar F. Incorporating self-reported health measures in risk equalization through constrained regression. Eur J Health Econ. 2020;21(4):513–28. https://doi.org/10.1007/s10198-019-01146-y .
Article CAS PubMed PubMed Central Google Scholar
Layton TJ. Imperfect risk adjustment, risk preferences, and sorting in competitive health insurance markets. J Health Econ. 2017;56(259):280. https://doi.org/10.1016/j.jhealeco.2017.04.004 .
Article Google Scholar
Rudmik L, Drummond M. Health economic evaluation: important principles and methodology. Laryngoscope. 2013;123(6):1341–7. https://doi.org/10.1002/lary.23943 .
Mays GP, Atherly AJ, Zaslavsky AM. The economics of public health: missing pieces to the puzzle of health system reform. Health Serv Res. 2017;52(Suppl 2):2275–84. https://doi.org/10.1111/1475-6773.12782 .
Gibson JL, Martin DK, Singer PA. Evidence, economics and ethics: resource allocation in health services organizations. Healthc Q. 2005;8(2):50–9. https://doi.org/10.12927/hcq.17099 .
Murphy K, Koski-Vacirca R, Sharfstein J. Resilience in health care financing. JAMA. 2020;324(2):126–7. https://doi.org/10.1001/jama.2020.10417 .
Fiksel J, Sanjay P, Raman K. Steps toward a resilient circular economy in India. Clean Technol Environ Policy. 2020;11:1–16. https://doi.org/10.1007/s10098-020-01982-0 .
Briguglio L, Cordina G, Farrugia N, Vella S. Conceptualising and measuring economic resilience. In: Briguglio L, Cordina G, Kisanga EJ, editors. Building the economic resilience of small states. Blata I-Bajda: Formatek Ltd; 2006. pp. 265–87.
Google Scholar
Konzelmann SJ. The political economics of austerity. Camb J Econ. 2014;38(4):701–41. https://doi.org/10.1093/cje/bet076 .
Preskorn SH. COVID-19: why has the mortality rate declined? J Psychiatr Pract. 2020;26(5):394–9. https://doi.org/10.1097/PRA.0000000000000494 .
Surkova E, Nikolayevskyy V, Drobniewski F. False-positive COVID-19 results: hidden problems and costs. Lancet Respir Med. 2020;8(12):1167–8. https://doi.org/10.1016/S2213-2600(20)30453-7 .
Rees EM, Nightingale ES, Jafari Y, Waterlow NR, Clifford S, Pearson BCA, Group CW, Jombart T, Procter SR, Knight GM. COVID-19 length of hospital stay: a systematic review and data synthesis. BMC Med. 2020;18(1):270. https://doi.org/10.1186/s12916-020-01726-3 .
Griffin KM, Karas MG, Ivascu NS, Lief L. Hospital preparedness for COVID-19: a practical guide from a critical care perspective. Am J Respir Crit Care Med. 2020;201(11):1337–44. https://doi.org/10.1164/rccm.202004-1037CP .
Kazemi Karyani A, Akbari Sari A, Woldemichael A. Eliciting preferences for health insurance in iran using discrete choice experiment analysis. Int J Health Policy Manag. 2019;8(8):488–97. https://doi.org/10.15171/ijhpm.2019.29 .
Heidari L, Jabbari A, Mohammadi F. Manifestations of economic resilience in hospitals: what do managers say? TB. 2020;19(1):19–31. https://doi.org/10.18502/tbj.v19i1.2814 .
Cuadrado C, Crispi F, Libuy M, Marchildon G, Cid C. National Health Insurance: a conceptual framework from conflicting typologies. Health Policy. 2019;123(7):621–9. https://doi.org/10.1016/j.healthpol.2019.05.013 .
Ruggles BM, Xiong A, Kyle B. Healthcare coverage in the US and Japan: a comparison. Nursing. 2019;49(4):56–60. https://doi.org/10.1097/01.NURSE.0000553277.03472.d8 .
Khetrapal S, Acharya A, Mills A. Assessment of the public-private-partnerships model of a national health insurance scheme in India. Soc Sci Med. 2019;243: 112634. https://doi.org/10.1016/j.socscimed.2019.112634 .
Liao PA, Chang HH, Sun LC. National Health Insurance program and life satisfaction of the elderly. Aging Ment Health. 2012;16(8):983–92. https://doi.org/10.1080/13607863.2012.692765 .
Chandra D, Kumar D. A fuzzy MICMAC analysis for improving supply chain performance of basic vaccines in developing countries. Expert Rev Vaccines. 2018;17(3):263–81. https://doi.org/10.1080/14760584.2018.140332 .
Bian X, Yao G, Shi G. Social and natural risk factor correlation in China’s fresh agricultural product supply. PLoS ONE. 2020;15(6):e0232836. https://doi.org/10.1371/journal.pone.0232836 .
Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nurs Health Sci. 2013;15(3):398–405. https://doi.org/10.1111/nhs.12048 .
Sundler AJ, Lindberg E, Nilsson C, Palmér L. Qualitative thematic analysis based on descriptive phenomenology. Nurs Open. 2019;6(3):733–9. https://doi.org/10.1002/nop2.275 .
Chapman AL, Hadfield M, Chapman CJ. Qualitative research in healthcare: an introduction to grounded theory using thematic analysis. J R Coll Physicians Edinb. 2015;45(3):201–5. https://doi.org/10.4997/JRCPE.2015.305 .
Ku YC, Chou YJ, Lee MC, Pu C. Effects of National Health Insurance on household out-of-pocket expenditure structure. Soc Sci Med. 2019;222:1–10. https://doi.org/10.1016/j.socscimed.2018.12.010 .
Cremer H, Lozachmeur JM, Pestieau P. The design of long-term care insurance contracts. J Health Econ. 2016;50:330–9. https://doi.org/10.1016/j.jhealeco.2016.08.008 .
Gruber J. Delivering public health insurance through private plan choice in the United States. J Econ Perspect. 2017;31(4):3–22. https://doi.org/10.1257/jep.31.4.3 .
Arentz C, Eekhoff J, Kochskämper S. Private health insurance: a role model for European health systems. Eur J Health Econ. 2012;13(5):615–21. https://doi.org/10.1007/s10198-012-0406-7 .
Fawcett J. Thoughts about social justice. Nurs Sci Q. 2019;32(3):250–3. https://doi.org/10.1177/0894318419845385 .
Buettner-Schmidt K, Lobo ML. Social justice: a concept analysis. J Adv Nurs. 2012;68(4):948–58. https://doi.org/10.1111/j.1365-2648.2011.05856.x .
Serván-Mori E, Wirtz VJ. Monetary and nonmonetary household consumption of health services and the role of insurance benefits: An analysis of the Mexico’s National Household Income and Expenditure Survey. Int J Health Plann Manage. 2018;33(4):847–59. https://doi.org/10.1002/hpm.2536 .
Download references
Acknowledgements
We would like to thank all participants and experts in this research.
This study was financially supported by Mashhad University of Medical Sciences (Fund Number: 21280).
Author information
Authors and affiliations.
Health Human Resources Research Center, School of Health Management and Information Sciences, Shiraz University of Medical Sciences, Qasr Al-Dasht St., Alley 29, Between Palestine St. and Mulla Sadra, Diamond Building, 7133654361, Shiraz, Iran
Erfan Kharazmi & Shima Bordbar
Health Economic, Tehran University of Medical Sciences, Tehran, Iran
Hanie Gholampoor
You can also search for this author in PubMed Google Scholar
Contributions
EK designed the experiments, analyzed, and wrote the manuscript. SH gathered data and wrote the manuscript. HG gathered data. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Erfan Kharazmi .
Ethics declarations
Ethics approval and consent to participate.
Written informed consent was obtained from all participants. The code of ethics for this project has been approved by [IR.SUMS.REC.1399.1250] at Shiraz University of Medical Sciences and was conducted in accordance with the ethical standards of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:.
Influence/Dependence Matrix of health insurance factors in economic resilience.
Additional file 2:
Critical coefficient of components of the health insurance economic resilience systems.
Additional file 3:
Indirect influence map in the health insurance economic resilience system.
Additional file 4:
Indirect influence graph in the health insurance economic resilience system.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kharazmi, E., Bordbar, S. & Gholampoor, H. The pattern of health insurance economic resilience in the Covid 19 pandemic shock. BMC Res Notes 14 , 371 (2021). https://doi.org/10.1186/s13104-021-05779-2
Download citation
Received : 17 August 2021
Accepted : 08 September 2021
Published : 23 September 2021
DOI : https://doi.org/10.1186/s13104-021-05779-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health system
- Economic resilience
BMC Research Notes
ISSN: 1756-0500
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 21 November 2023
Lessons from health insurance responses in counteracting COVID-19: a qualitative comparative analysis of South Korea and three influential countries
- Hey Jin Ko 1 ,
- Eunji Yun 2 ,
- Boryung Ahn 3 ,
- Hyejin Lee 4 , 5 ,
- Won Mo Jang 6 , 7 na1 &
- Jin Yong Lee 7 , 8 , 9 na1
Archives of Public Health volume 81 , Article number: 205 ( 2023 ) Cite this article
859 Accesses
1 Altmetric
Metrics details
The COVID-19 pandemic has caused delays and restrictions in providing medical services. In response to the medical surge, countries with social insurance systems provided financial incentives to medical institutions. This study aimed to present the directions for health insurance support by comparing countries in terms of the domains and contents of COVID-19 health insurance support to ensure timely support in case of future pandemics.
An analysis framework was developed to compare health insurance policy interventions for COVID-19 and non-COVID-19 domains, and detailed policy interventions were divided into sub-domains (space, staff, and stuff) for each domain. Data were collected by country from the websites of the Ministry of Health and Social Insurers, Organisation for Economic Co-operation and Development, and European Observatory on Health Systems and Policies and were analyzed using qualitative comparative analysis.
The countries provided comprehensive support for both the COVID-19 and non-COVID-19 domains. In the COVID-19 domain, overall support was provided in all three sub-domains. Additional cost support was provided to prevent infection and provide secure facilities to treat confirmed patients. Outpatient services were mainly supported, and an intensive intervention was developed in the staff sub-domain for the non-COVID-19 domain. The point of policy intervention was the surge of the first confirmed case. Continuous revisions were subsequently made. The government provided financial support through health insurance.
Conclusions
Regarding where policy support through health insurance should be focused, the workload of medical personnel increased according to the change in the service provision environment due to the pandemic, and the medical service delivery system changed to prevent further infection. Consequently, incentives should be provided to aid the provision of stable services to patients and should be an auxiliary means to implement the national quarantine policy more effectively via a health insurance response system that promptly provides additional financial support in case of future crises.
Peer Review reports
The outbreak of coronavirus disease 2019 (COVID-19), the third pandemic declared by the World Health Organization, has led to changes in global healthcare services. COVID-19 is highly contagious and prone to asymptomatic transmission, leading to a rapid increase in infections and a consequent shortage of hospital beds and protective supplies in medical institutions. As a result, a burden was placed on service provision by medical institutions, which included obtaining temporary beds and reallocating existing health care practitioners’ responsibilities to treat COVID-19 patients. The situation has since escalated into a public health crisis due to delays and limitations in the provision of existing medical services (e.g., primary medical services for patients other than those infected with COVID-19) [ 1 ].
The surge in demand for health services during a pandemic makes it difficult to respond using the existing emergency medical system [ 2 ]. A strategy is thus required to strengthen the healthcare system’s resilience. The key inputs of the six building blocks for strengthening the healthcare system (service delivery, health workforce, health information systems, access to essential medicines, financing, and leadership/governance) involve financing and the health workforce [ 3 , 4 ].
For resilience, the most important of these inputs is the financing mechanism [ 5 ]. The main financial resources in the healthcare systems of countries that operate social health insurance are taxes and contributions. The roles and importance of such financing may vary depending on the phase of the disaster. In terms of the preparedness for a pandemic, preparedness can be improved comprehensively and uniformly by using tax funding; and during the stages of disaster response, both taxes and contributions must be coordinated [ 6 ].
To address COVID-19, health insurance systems implemented additional strategies, such as altering their reimbursement systems or additionally reimbursing COVID-19-related claims [ 7 ]. In general, tax funding was provided to support these measures. In Germany, the government provided a tax subsidy when expenditures increased because of COVID-19 to address the shortfall in its social health insurance funds [ 8 ]. South Korea (hereafter “Korea”) also provided financial support through its health insurance system in addition to compensation from the government for medical institution losses in the form of supplier incentives, such as securing and distributing funds to respond to the pandemic [ 9 ].
Many countries, including Korea, have actively leveraged their health insurance systems to ensure surge capacity. However, in Korea, during the pandemic, there were instances of confusion among policymakers and healthcare institutions because of the absence of concrete discussions regarding the decision-making processes, methods, scope, and scale of health insurance policies in public health crises. The health insurance system of Korea is based on the National Health Insurance (NHI) system, which is an integrated, single-insurer system [ 10 ]. The implementation and reform of this system was influenced by countries with social insurance. Among the countries that operate a public health insurance system, Japan, Germany, and the United States have often been mentioned in previous studies as comparisons for the Korean health insurance system [ 10 , 11 , 12 ].
Additionally, the importance of financial support through social insurance has been increasingly emphasized in building a stable financial procurement system with frequent exposure to crises [ 8 ]. However, most discussions about COVID-19 were mainly held from the perspective of the overall health system, including epidemic prevention policy, health system governance, and health service delivery [ 8 , 13 , 14 ]. When it comes to health insurance, there are some studies on payment systems [ 15 , 16 ]; however, a comprehensive review of the intervention areas and contents is lacking.
Therefore, this study aimed to compare and analyze the domains and contents of health insurance policy interventions applied to healthcare service providers in the three countries that have had a significant influence on Korea and the Korean health insurance system to present the directions for health insurance support for establishing response strategies for future pandemics.
Study design and setting
This study comparatively analyzed the insurance domains of four countries (Korea, Japan, Germany, and the United States of America) and the detailed methods and support levels in the first year (January–December 2020) of the COVID-19 pandemic. The analyzed countries, including Korea, are nations that have implemented public health systems. These countries have influenced Korea’s health insurance system reform and development and have similar economic power as members of the Organisation for Economic Co-operation and Development (OECD). Furthermore, these are countries that have actively responded to COVID-19 through their health insurance systems. To examine and analyze each country’s health insurance policies implemented in response to COVID-19, this study employed a case-based approach—qualitative comparative analysis (QCA). QCA is a case-oriented research method that can produce empirically well-grounded and context-sensitive evidence that is useful in decision-making, implementation, and evaluation [ 17 , 18 ]. This methodology is not only widely used in healthcare policy studies [ 19 , 20 , 21 ] but is also being applied in studies on the provision of healthcare services during the COVID-19 pandemic [ 14 , 22 ].
We developed an analytical framework for the analysis of domains in which financial support (in the form of health insurance) was provided in response to COVID-19 (Fig. 1 ). The classification of different response policies for each analyzed country based on this framework ensured the clear identification of the response domains. The analysis was conducted in the following stages: data collection, classification of response domains and timeline, detailed support methods, and comparison by nation.
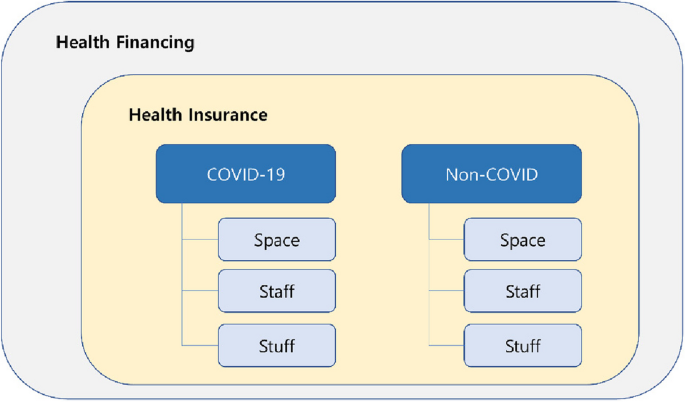
Analytical framework for comparing COVID-19 health insurance response
First, the classification involved health service domains dedicated to treating COVID-19 patients (COVID-19) and non-COVID-19 patients (non-COVID-19) (main domain). Treatments for COVID-19 fell under the “COVID-19” domain. Other treatments were classified under the “non-COVID-19” (hereafter “non-COVID”) domain. Characteristically for an infectious disease, the provision of health services in response to COVID-19 requires a dual-track health system that involves not only treatment and infection prevention but also the recovery of the health service delivery system for other patients [ 5 ]. That is, the provision of prevention-diagnosis-quarantine-treatment services and the management of accumulated health care demand arising from the response to COVID-19 must occur simultaneously. Thus, the “COVID-19” domain identified policies to support the expansion of the health service providers’ capabilities in response to the rapid surge in demand caused by COVID-19. However, the “non-COVID” domain identified the policies supporting the maintenance of existing health service functions and minimizing the impact of the COVID-19 response on pre-existing services.
The main domain was divided into sub-domains based on surge capacity (i.e., the capacity to improve service provision through the management of resources in response to a medical surge) [ 23 , 24 ]. Even in situations with unexpected surges in health service needs, health services must be provided to as many individuals as possible within the population [ 25 ], and the services must be affordable and available to ensure access, which must also be supported with sufficient capacity [ 26 ]. Accordingly, we classified what incentives were offered to maximize surge capacity through health insurance. The main strategies proposed to boost and optimize the healthcare system’s response capacity include mobilizing staff, boosting supplies, and optimizing space [ 26 , 27 , 28 ]. Thus, the sub-domains were space, staff, and stuff. Space included financial support to provide the basic space required for health service provision (e.g., hospital beds). In other words, it referred to the expenses associated with the locations where healthcare services were provided, covering the universal and fundamental patient care provided at those locations. Staff included incentives offered for health services provided by the medical staff. This pertained to the healthcare services offered to patients based on medical judgments considering factors such as the severity of the patients’ conditions, their health status, and their individual needs. Stuff included additional compensation for medical equipment, treatment materials, and pharmaceuticals required to provide health services.
Overview of target countries
Socio-economic status, COVID-19 status, existing health resources, and health insurance system were identified in the four analyzed countries (Table 1 ).
In this study, the four countries are Organisation for Economic Co-operation and Development (OECD) members, with the United States having the largest gross domestic product (GDP) among OECD countries (2020 statistics); Japan, Germany, and South Korea ranked second, third, and eighth, respectively. All four countries have a GDP per capita(current prices, current PPP, 2020 statistics) of more than USD 40,000, which is higher than the OECD average of USD 45,025 for the three countries except Japan [ 29 ].
In Korea, the 3 T strategy (pre-emptive testing, prompt tracing, and proper treatment) was used to effectively reduce the incidence rate of confirmed cases in the early stages of the COVID-19 pandemic [ 38 ]. The Korean health insurance system covers 97% of Koreans, in a single insurer system [ 36 ].
Japan experienced a surge of confirmed cases in major cities, beginning with small mass infections, but was criticized in the initial response stage for the insufficient availability of polymerase chain reaction (PCR) tests and the lack of cooperative efforts between government and medical institutions [ 39 , 40 ]. The nationwide health insurance program was established in 1961, after which all Japanese citizens were eligible for health insurance. Depending on the beneficiary characteristics, employee health insurance and community-based health insurance were implemented [ 41 ].
Germany has been able to reduce its COVID-19 mortality rate presumably due to the relative abundance of its resources, including beds and care providers, and its nationwide health insurance system has enabled the coverage of treatment and diagnostic costs [ 42 ]. Approximately 87% of Germans are enrolled in the national public health insurance system, which individuals who earn less than a certain income are obliged to subscribe to [ 34 ]. Contributions are structured so that the collected contributions of the health insurance association are consolidated into the health fund and distributed to the health insurance association [ 43 ].
The United States has the highest cumulative number of confirmed cases in the world. The American health insurance system is operated under a private health insurance market based on voluntary enrolment along with Medicare—a public health insurance system that provides health services for adults aged 65 years or older and those with a disability—as well as Medicaid—a public welfare system for low-income individuals. This study examined the policy intervention of Medicare, in which approximately 18.6% of Americans are enrolled [ 44 ].
Since private health insurance is at the center of the American health insurance system, the number of public beds per population is among the lowest among OECD countries. As the United States primarily relies on private health insurance, its health system differs from that of the other three countries. However, the relatively low number of public hospital beds resulting in most healthcare services delivered by private providers is similar to the situation in Korea [ 45 ]. Additionally, the Medicare program wields significant influence over the American healthcare system. The Center for Medicare and Medicaid Innovation (Innovation Center) devises and tests new Medicare policies considering the synergy with the private sector [ 46 ]. In fact, the new regulations and incentives introduced by Medicare policies significantly influence provider behavior, affecting not only Medicare patients but also non-Medicare patients [ 47 ]. As we aimed to identify effective incentive-based strategies for providers in response to surge capacity needs, we included both in the analysis.
Data collection
We collected data from the official websites of each nation’s Ministry of Health and social health insurers. Since data could be quickly and reliably obtained from this source in the changing pandemic situation, data collection through websites was carried out first. For comprehensive data collection, additional relevant contents and data were also collected from the OECD and the European Observatory on Health Systems and Policies websites, which offer up-to-date compilations and disclosures of COVID-19-related health service policies (see Additional file 1 ).
We searched for data using keywords related to our topic. The keywords included “COVID-19,” “coronavirus,” “health system,” “health policy,” and “health insurance.” “Medicare” was added to the search in the American context. The collected data included publications from the European Observatory on Health Systems and Policies; publications, web pages, and press releases from governments or health insurers; and an OECD research report (see Additional file 2 ). The collected data were primarily in English, but data from each nation’s Ministry of Health websites were collected in Korean, Japanese, and German languages, respectively. The collected data were primarily based on title and abstract screening to confirm the relevance to the research topic. Only the materials deemed appropriate for the analytical framework of this study were selected, and data unrelated to COVID-19 and health insurance were excluded. We reviewed the contents of the screened articles, and articles meeting the following conditions were excluded from the analysis: 1) support policies that used government financing other than health insurance resources, 2) policy implementation period outside of 2020, and 3) duplicate contents in multiple articles. Articles on changes in administrative regulations related to cost reimbursement for medical institutions were reviewed by considering them as indirect financial support policies even if there was no additional health insurance financial support. Consequently, a total of 16 articles were analyzed.
The final data were analyzed and classified according to the main domains and sub-domains. The data were classified into the corresponding domains after verification and clarification of the data analysis process based on consensus in a meeting of researchers. That is, in case of disagreement on classification among researchers, consensus was reached on whether it was appropriate to classify data under a specific domain via discussion.
COVID-19 wave and timeline of health insurance response
Prior to comparing the financial support policies regarding the COVID-19 pandemic, the current COVID-19 status of each country was examined (Fig. 2 ). The four countries shared a similar pattern in which the first confirmed case of COVID-19 was reported in January 2020 and increases in confirmed case numbers occurred around March to April. Subsequently, a slight decrease was observed in case numbers until the case numbers increased once again at various times in the three countries, excluding Germany (Korea – September, Japan – August, United States – July–August). In November, another wave in confirmed case numbers was observed.
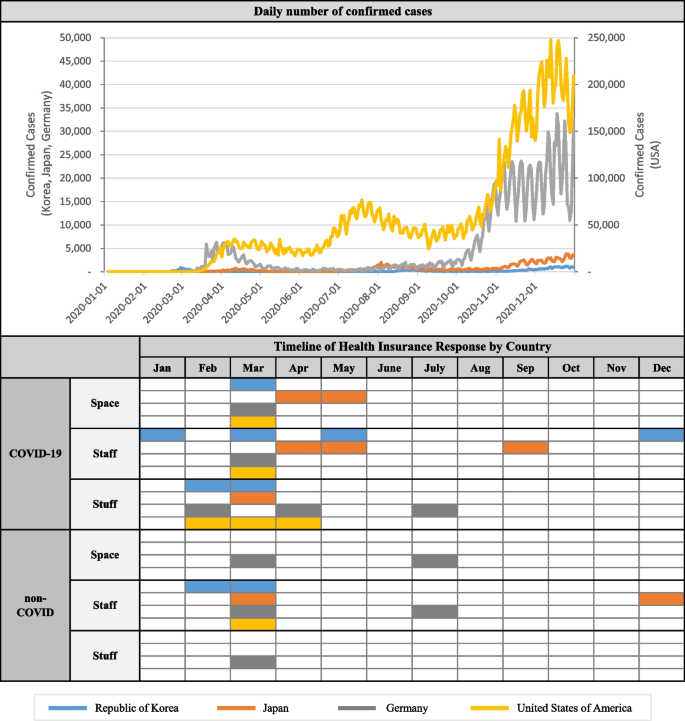
Timeline of Policy Implementation by Country
Examining the pattern of COVID-19 outbreaks and the timing of health insurance intervention implementation reveals that a comprehensive policy implementation of space, staff, and stuff occurred for both the “COVID-19” and “non-COVID” domains in March and April, when the confirmed case numbers rapidly increased.
All four countries implemented simultaneous health insurance policy interventions during the first wave, indicating that social health insurance initiated a response from the early stages of the COVID-19 spread. Therefore, the timing of health insurance system intervention during this major crisis affecting the healthcare systems, namely, the first wave of COVID-19, seemed to be minimally influenced by factors such as the composition of private providers, population coverage, and characteristics of the reimbursement systems.
Among the systems, the implementation of staff was quickest in Korea’s COVID-19 response, as were its responses in the “non-COVID” domain. The single-payer and fee-for-service (FFS) framework of Korea’s incentive system facilitated a relatively smooth increase in testing capacity by healthcare professionals within a short period.
Even after the initial policy intervention, continuous policy intervention efforts, including the supplementation of existing interventions or implementation of additional policies, were observed regardless of the increase pattern of confirmed cases. This trend appeared consistent across all countries, irrespective of the characteristics of their respective health systems. However, the United States concentrated its main support efforts in the COVID-19 domain, with the timing of its interventions tending to align with the first wave. Its degree of health insurance intervention might have been lower than that in the other countries because its Medicare covers a limited population compared with the national insurance in the other countries.
Health insurance response according to analytical framework
We compared the detailed response domains and health insurance implementation targeting COVID-19 and non-COVID patients in each country based on our analytical framework (Table 2 ). Generally, the COVID-19 domain commonly involved additional compensation to address costs related to providing inpatient services for confirmed patients. Given the need for inpatient treatment for highly contagious confirmed COVID-19 patients using negative pressure wards to prevent transmission to other patients, costs pertaining to such services were made eligible to claim. The space sub-domain involved compensation for the hospitalization fees of COVID-19 patients—the most basic of inpatient service costs. In both Korea and the United States, the hospitalization fees for confirmed patients were increased by 20% compared to the existing level of compensation for inpatient care fees [ 9 , 48 ]. In Japan, an additional fee for inpatient care for type-2 infectious disease is charged from patients with an infectious disease to account for the increase (up to four times) in infection risk [ 49 ]. In the United States, hospitalization fees were increased in accordance with the Coronavirus Aid, Relief, and Economic Security Act (hereafter CARES Act), applied retroactively from January 27, before the enforcement date.
As the compensation of hospitalization fees in the United States was based on the diagnosis-related group (hereafter DRG), the increase in fees offered comprehensive support for not only space but also staff and stuff. The hospitalization fees for intensive care units (ICUs) were increased by 6% in Korea [ 9 ] while, in Japan, two revisions led to a fourfold increase in fees [ 50 ]. Such increases in hospitalization fees were made considering the additional need for care providers to treat severe COVID-19 patients who require more extensive management (including equipment such as an extracorporeal membrane oxygenation machines and ventilators) as well as the reduced efficiency of care due to personal protective equipment (PPE). There were no indications of additional increases in existing hospital fees in Germany, but support was provided for the costs involved in gaining access to hospital beds [ 15 ]. The amount of support provided per ICU bed equipped with negative-pressure facilities was equivalent to USD 56,818.18 (EUR 50,000) per bed.
The staff sub-domain involved support similar to that observed in the space sub-domain. This includes compensation for the burden placed on health care practitioners who care for confirmed patients receiving inpatient treatment. In Japan, support was also provided for outpatient services.
A detailed examination of benefits related to hospitalization fees revealed an increase in hospitalization fees in the space sub-domain, concurrent with inpatient management costs in the staff sub-domain [ 9 ]. First, the negative pressure isolation management fee in ICUs had doubled to USD 215.62 (KRW 255,940) while the negative pressure isolation management fee in ICU wards dedicated to severe COVID-19 patients had tripled to USD 431.25 (KRW 511,890). Furthermore, an infection prevention and control fee was newly established (USD 2.86, KRW 3,390) given that COVID-19 patients require isolation and additional efforts to prevent transmission to other patients. Similarly, an additional fee for emergency management was implemented in Japan [ 49 ]. Considering the potential additional treatments and tests needed to identify patient statistics as well as ordering additional drugs and ventilators in the process of caring for critically ill confirmed patients, fees had increased by up to five times. In Germany, compensation of USD 43.18 (EUR 38) was also provided for the increase in nursing work for treating confirmed patients [ 15 ].
Moreover, due to the difficulties in securing hospital beds in Korea, “residential treatment centers” were created for confirmed COVID-19 patients with mild symptoms for monitoring, diagnosing, and testing and for transferring worsening cases to nearby hospitals. Based on the type of service provided in each facility, costs were classified as I, II, or III and compensated accordingly [ 9 ]. Category I included support for patient consultations, monitoring, and chest X-rays through the provision of healthcare practitioners and X-ray equipment. Category II included the same services as under Category I (excluding X-rays), and Category III included greater benefits for patients admitted to one of the main residential treatment centers equipped with better medical facilities or those transferred to a residential treatment center from a medical institution as they required more intensive medical care than under Category I or II.
Among confirmed patients, those requiring specific care received relevant benefits. In Korea, compensations of USD 270.68 (KRW 321,300) were provided for treating dialysis patients [ 9 ] while, in Japan, compensations of USD 26.14 (JPY 2,980) were provided for outpatient dental treatment [ 51 ].
The stuff sub-domain involved compensations to alleviate the economic burden of PPE such as masks. Among the countries analyzed, compensation for PPE was provided in Korea and Germany. In Germany, compensation for PPE was increased from the initial amount of USD 56.82 (EUR 50) in April to USD 113.64 (EUR 100) in July [ 15 ]. Furthermore, compensation was also provided for PCR tests used to confirm COVID-19 infection. This benefit was applied in Korea, Germany, and the United States in February and in Japan in March, more quickly than benefits related to the treatment of confirmed patients [ 9 , 52 , 53 , 54 , 55 ]. Furthermore, in February, the United States first approved a testing kit developed by the Centers for Disease Control and Prevention to confirm COVID-19 diagnoses and extended its insurance benefits to include the usage of such testing kits developed in the private sector to expand supply levels. In April, the insured value for testing kits increased from USD 51 to USD 100 [ 53 , 54 ]. Germany also approved testing kits in February and introduced an insured value of USD 67.05 (EUR 59) [ 26 ].
The non-COVID domain mainly involved policy interventions in the staff sub-domain. No policy interventions were implemented for the space and stuff sub-domains other than the comprehensive benefits in Germany provided for the reduction in patients due to COVID-19 . In Germany, an insurance fee of USD 409.09–863.64 (EURO 360–760) was applied to account for the reduction in patients resulting from postponed treatments or delays due to the treatment of COVID-19 patients [ 15 ].
While support in the COVID-19 domain was focused on inpatient services, support in the non-COVID domain usually involved support for outpatient services. In the staff sub-domain, all countries except Germany expanded benefits for virtual consultations. Telemedicine was implemented in Korea and Japan, where virtual consultations were previously not permitted, for a cost of USD 4.16 (KRW 4,940) and USD 18.77 (JPY 2,140), respectively [ 50 ]. In Korea, the respective fee could be claimed in addition to the basic consultation fee while, in Japan, USD 18.77 (JPY 2,140)—an amount lower than the previous initial consultation fee of USD 25.26 (JPY 2,880)—could be claimed. In the United States, where virtual consultations had already been available, only fees occurring in rural areas or areas with a shortage of healthcare practitioners were covered. Meanwhile, during the public health emergency period due to COVID-19, compensations were made eligible for a greater scope of services, locations, and service methods (e.g., video, telephone, online) [ 56 ]. Furthermore, in Korea, families of patients with a chronic disease requiring long-term prescriptions were granted permission for proxy access to prescriptions with an insurance fee of USD 4.96 (KRW 5,890), approximately 50% of the existing consultation fees.
Furthermore, to create a safe environment for non-COVID patients to receive treatment while preventing infections, compensation was also implemented for such services. In Korea, National Safe Hospitals and clinics dedicated to respiratory diseases, with segregated access, treatment, and care settings, were introduced to enable non-COVID patients to receive in-person treatments without the fear of infection, along with an infection prevention and control fee (USD 17.63, KRW 20,930). An infection prevention and control fee (USD 0.99, KRW 1,170) for implementing infection control protocols such as mask-wearing was also provided for patients in locked wards in mental and long-term care hospitals with many vulnerable elderly patients [ 9 ].
However, in Japan, compensations were offered for all outpatient or inpatient services, drug dispensing, and visiting nursing care without additional conditions [ 57 ]. Furthermore, for the testing of untested suspected COVID-19 patients, the infection prevention and control fee of USD 26.32 (JPY 3,000) was compensated [ 49 ]. Additional benefits included compensations for children under the age of 6 considering the higher likelihood of contact with healthcare practitioners [ 51 ].
Such policy support for health insurance was made possible through health insurance financing as well as national financial support. In Japan, the government budget regularly contributed toward health insurance financing as various support measures were modified or added [ 51 , 58 ]. In Germany, the Hospital Relief Act was enacted in March 2020 to alleviate the financial support and administrative burden of medical institutions through the various aforementioned health insurance policies. Additional funding for this implementation was provided through taxes and contributions [ 59 ]. In the United States, in accordance with the CARES Act enacted in March 2020, matters related to the expansion of Medicare coverage and the like were stipulated along with an announcement that the funds for the changes would be sourced from the national disaster medical system [ 26 ].
Easing administrative regulations of health insurance
Aside from the additional financial compensation, regulations pertaining to health insurance administration procedures were relaxed to increase efficiency in the management of medical institutions (Table 3 ).
In Germany and the United States, the screening of medical expenses during a COVID-19 outbreak, or for COVID-19-related activities, was eased [ 59 , 60 ]. Such measures were enforced in recognition that services were provided based on medical necessity without evaluating the adequacy of the provided medical service to alleviate the time and cost needed for the review process considering the situation’s urgency [ 59 ].
In addition to the easing of the review of medical expenses, the reimbursement period of health insurance claims was shortened in Korea and Germany [ 15 , 61 ]. In Korea, payments were made in advance (90–100% of health insurance benefits for the same month of the previous year paid to the medical institution prior to settlement) or early (90% of the payment is made 10 days after the claim and before the completion of the evaluation). Through this process, the usual period of 22 days that it took medical institutions to receive the payment was reduced to 10 days.
Existing obligations to report staff or facility changes in institutions were also suspended. Although, in Korea, changes in human resource are linked to differential compensation payments and thus must be updated promptly, the duty to report was suspended. Additionally, contents of previous reports were applied in response to the frequent occurrence of unavoidable changes such as the isolation of healthcare practitioners after close contact, treatment of confirmed COVID-19 patients, or dispatch to other medical institutions [ 61 ]. In Japan, although a reduction in medical expenses is applied if the approved number of beds exceeds the number outlined under the Medical Act, the reduction was not applied for beds used to treat COVID-19 patients [ 50 ]. Furthermore, similar to Korea, reports on the changes in human resources due to a temporary surge in patients or the isolation of medical staff were suspended. Moreover, in the context of Korea, although DRG payment is underway for certain diseases or institutions, compensations of COVID-19 patients were based on fee-for-service payment to prevent the likelihood of under-compensation that can occur with bundled payments [ 9 ].
This study revealed that the analyzed countries provided financial support through health insurance from the initial stage of the pandemic. Although there are differences across countries in the detailed response and amount of support, all countries shared a common purpose of maintaining or expanding service providers’ capacity to provide services throughout the pandemic. Comprehensive policy interventions were implemented in both the COVID-19 and non-COVID domains. Among these, support in the COVID-19 domain involved space, staff, and stuff sub-domains while support in the non-COVID domain focused primarily on the staff sub-domain. The support across the three sub-domains can be summarized as follows:
First, financial support in space and staff both served to alleviate the increased workload burden that arose from changes in the service environment. Expansions and changes occurred in the space sub-domain due to the shortage of facilities relative to the number of COVID-19 patients. Aside from COVID-19, pandemics such as the 2009 H1N1 virus outbreak also led to increased healthcare demands due to hospitalizations. During that time, similar to the COVID-19 pandemic, attempts to expand service capacity, such as converting alternative spaces to hospital beds, were employed as strategies [ 62 ]. Thus, changes occurred in healthcare practitioners’ line of service and the management of inpatient services. Additionally, situations arose in which locations not originally used to deliver health services were used due to the increased need for negative pressure isolation rooms given the characteristics of infectious diseases. In these cases, compensation for inpatient services was increased from 20 to 400% of the previous costs to accommodate changes in the workload of healthcare practitioners.
Support for increased workload was also implemented in the staff sub-domain. Compared to the space sub-domain, in which support was focused primarily on inpatient services, support in the staff sub-domain comprised more comprehensive interventions including outpatient services. In the COVID-19 domain, support for infection prevention and control among hospitalized patients was provided in Korea while, in Germany, nurses’ compensation was increased. Moreover, compensation for specialized services, such as dental treatments and hemodialysis, was also reinforced. In the non-COVID domain, additional compensations were made toward healthcare practitioners’ protection during interactions with patients—both in general and those suspected of having COVID-19. In Japan, considerations were also given to additional work involving pediatric care.
The lack of physical space due to increased patient numbers was foreseen, but the staff sub-domain emerged as the most limited domain throughout the pandemic [ 63 ]. Previous research has also demonstrated that, although the service capacity of each country may vary, investments are needed to improve the quantity and quality of healthcare practitioners accompanied by access to sufficient numbers, education, and willingness of practitioners [ 13 ]. During a pandemic, more staff are required than usual for the same type of service due to the need for staff to wear PPE. Thus, support included a comprehensive consideration of the increased workload and the mental and physical burden placed on healthcare practitioners.
Second, financial support in the staff sub-domain was reflected in changes in the healthcare delivery system. Quarantining the sick, contact tracing, and social distancing were employed globally to prevent transmission during the early stages of COVID-19 [ 14 ]. These strategies have also been adopted as measures to ensure effective delivery of health services, and health insurance supported these measures comprehensively.
To prevent the transmission of COVID-19, notable changes in the delivery of outpatient services occurred in the non-COVID domain. First, compensations for virtual consultations, such as telemedicine, were reinforced in the analyzed countries (except Germany). In the case of the United States, although telemedicine was previously authorized, the scope of its application was initially limited. During the COVID-19 pandemic, however, the geographical requirements and scope of application for telemedicine services were expanded, and the level of support was maintained. In Korea and Japan, telemedicine was not previously established, but methods such as telephone consultations and prescription proxies were actively implemented. Such actions helped compensate for the reduced number of patients and service provisions due to COVID-19.
Furthermore, respiratory and non-respiratory patients were instructed to use separate healthcare access and treatment paths in Korea in addition to the establishment of National Safe Hospitals and clinics dedicated to respiratory disease for the safe provision of services. Such institutions were allocated new functions and roles in addition to financial support for the additional work required for patient management and service provision. In Korea, additional compensation was provided for health services in newly established residential treatment centers specifically for COVID-19 patients.
Non-COVID domains have also been threatened by the provision of COVID-19-related services throughout the pandemic [ 7 , 8 ]. Thus, patients were managed to prevent the spread of infection from COVID patients to non-COVID patients and ensure a safe treatment environment. Healthcare professionals’ infection prevention efforts were supported by health insurance.
Third, the stuff sub-domain was focused on prevention of infection among healthcare professionals and patients. PPE, such as masks and protective clothing, worn by healthcare practitioners to prevent infection was compensated for. PPE was required for practitioners when interacting with patients, and, considering the additional costs involved, concerns were raised that a lack of financial support would lead to problems such as the inadequate use of PPE or passivity in treating patients.
Furthermore, extensive support was provided for the use of testing kits. Given the importance of increased testing at the initial stage to contain infections and preemptively treat confirmed cases, expanding diagnostic capacity for quick screening was an important factor of the national public health emergency policy for responding to COVID-19 [ 26 , 64 ].
Fourth, support for healthcare services through health insurance enabled rapid response in the pandemic context and required government budget support. Insurance policies prompted healthcare providers to recognize COVID-19 and to swiftly implement changes to their patient care and patient care facilities. The associated costs to safeguard these providers were also compensated through these policies. Financial support in the form of increased fees for health services was facilitated using the existing insurance fee calculation system and payment process. Nevertheless, such financing required both health insurance financing and the government budget. Support through the government budget required approval from the federal government or the National Assembly to facilitate the smooth implementation of the national public health emergency policy and compensation for financial losses among healthcare practitioners; thus, the government’s role in health insurance financing also expanded during the pandemic [ 8 ]. As the domains of financial support provided through health insurance are determined based on the direction of national public health emergency policy, health insurance financing complements the government budget support rather than relying solely on insurance funds.
According to a recent survey by the NHI Service, Koreans perceive the NHI system as a social safety net that enables access to care without the excessive burden of cost, despite the ongoing COVID-19 crisis [ 65 ]. Thus, it is evident that Koreans regard the NHI system positively and that the health insurance system is highly accepted by its users. Furthermore, support through health insurance has been regarded as one of the success factors of preventive measures against a widespread outbreak of COVID-19 [ 66 ], indicating a need for government support for health insurance policies during this pandemic.

Limitations
This study examined support systems for health service providers in four countries operating social health insurance systems. The study limitations are as follows. Since the spread and severity of COVID-19 vary by country, there are differences in the direction of national public health emergency policy. From a health insurance perspective, however, an emphasis was placed on comparison, and, thus, such national specificities were not considered in detail. Furthermore, due to the varying financial conditions of each country, the financial capacity for health insurance may also differ, influencing policy interventions. Another limitation was that only changes in the initial year of the pandemic were analyzed, thus failing to incorporate the ongoing, long-term policy changes. Nevertheless, this study aimed to derive the common trends in financial support between countries by identifying the specific domains of support in each country.
To overcome the pandemic crisis, policymakers must consider not only quarantine policies but also health service support. Capacity expansion of health systems during the COVID-19 pandemic is a key factor in ensuring health system resilience [ 13 ]. In the COVID-19 pandemic, financial support through health insurance was provided at a higher than usual level with an emphasis on staff in both the COVID-19 and non-COVID domains. Such support enabled health service providers to continue to provide services without concerns regarding reduced profits or additional costs. This allowed for prompt and comprehensive capacity expansion and timely implementation of changed infection control policies.
Based on the lessons learned from COVID-19, decisions regarding health insurance policies in future pandemics should consider the following. First, it is important to recognize the changes that occur in service provision and the corresponding work-related burdens and to provide prompt additional financial support. Second, considering the consistency and relevance to the national public health emergency policy, support should be provided for health insurance plans that align with the goals and direction of the policy. Third, to enable access to sufficient financing in which appropriate financial support can be provided during a pandemic, it is necessary to monitor the financial sustainability of the health insurance system and establish a foundation for receiving governmental support. Fourth, continuous assessment of the response policies and their effects and financial requirements may help to establish the optimal health insurance response system to appropriately manage medical resources and operate a resilient health system.
Availability of data and materials
All data used in this study are publicly available.
Abbreviations
Coronavirus disease 2019
National Health Insurance
Qualitative comparative analysis
Organisation for Economic Co-operation and Development
Gross domestic product
Polymerase chain reaction
Diagnosis-related group
Intensive care unit
Personal protective equipment
World Health Organization. Pulse survey on continuity of essential health services during the COVID-19 pandemic. Interim report: World Health Organization; 2020.
Google Scholar
Casani JAP, Romanosky AJ, et al. Surge capacity. In: Ciottone G, Anderson PD, Heide EAD, Darling RG, Jacoby I, Noji E, et al., editors. Disaster medicine. Mosby Elsevier; 2006. p. 193–202.
Chapter Google Scholar
World Health Organization. Monitoring the building blocks of health systems: A handbook of indicators and their measurement strategies. Geneva, Switzerland: World Health Organization; 2010.
World Health Organization. Everybody business: Strengthening health systems to improve health outcomes: WHO’s framework for action. Geneva, Switzerland: World Health Organization; 2007.
World Health Organization. Strengthening and adjusting public health measures throughout the COVID-19 transition phases: Policy considerations for the WHO European Region, 24 April 2020. Copenhagen, Denmark: WHO Regional Office for Europe; 2020.
Kwon S, Kim E. Sustainable health financing for COVID-19 preparedness and response in Asia and the Pacific. Asian Econ Policy Rev. 2022;17(1):140–56.
Article Google Scholar
Waitzberg R, Gerkens S, Dimova A, Bryndova L, Vrangbaek K, Jervelund SS, et al. Balancing financial incentives during COVID-19: A comparison of provider payment adjustments across 20 countries. Health Policy. 2021. https://doi.org/10.1016/j.healthpol.2021.09.015 .
Schmidt AE, Merkur S, Haindl A, Gerkens S, Gandre C, Or Z, et al. Tackling the COVID-19 pandemic: Initial responses in 2020 in selected social health insurance countries in Europe. Health Policy. 2021;126(5):476–84. https://doi.org/10.1016/j.healthpol.2021.09.011 .
Article PubMed PubMed Central Google Scholar
Ministry of Health and Welfare of Korea. At a Glance: Updated health insurance payments related to COVID-19. 2021.
Lee JC. Health care reform in South Korea: Success or failure? Am J Public Health. 2003;93(1):48–51. https://doi.org/10.2105/ajph.93.1.48 .
Lee SY, Kim CW, Seo NK, Lee SE. Analyzing the historical development and transition of the Korean health care system. Osong Public Health Res Perspect. 2017;8(4):247–54. https://doi.org/10.24171/j.phrp.2017.8.4.03 .
Kim S, Lee S-W. Distorted policy transfer and institutional conflicts: the health insurance reform in South Korea. Japan J Political Sci. 2022;23(1):18–33. https://doi.org/10.1017/S1468109921000384 .
Haldane V, De Foo C, Abdalla SM, Jung A-S, Tan M, Wu S, et al. Health systems resilience in managing the COVID-19 pandemic: Lessons from 28 countries. Nat Med. 2021;27(6):964–80. https://doi.org/10.1038/s41591-021-01381-y .
Article CAS PubMed Google Scholar
Yoo JY, Dutra SVO, Fanfan D, Sniffen S, Wang H, Siddiqui J, et al. Comparative analysis of COVID-19 guidelines from six countries: a qualitative study on the US, China, South Korea, the UK, Brazil, and Haiti. BMC Public Health. 2020;20(1):1853. https://doi.org/10.1186/s12889-020-09924-7 .
Article CAS PubMed PubMed Central Google Scholar
Quentin W, Albreht T, Bezzina A, Bryndova L, Dimova A, Gerkens S, et al. Adjusting hospital inpatient payment systems for COVID-19. Eurohealth. 2020;26(2):88–92.
Yun E, Ko HJ, Ahn B, Lee H, Jang WM, Lee JY. Expanding medical surge capacity to counteract COVID-19: South Korea’s medical fee adjustment through the National Health Insurance System. Risk Manag Healthc Policy. 2022;15:2031–42. https://doi.org/10.2147/RMHP.S375422 .
de Wee G. Comparative policy analysis and the science of conceptual systems: a candidate pathway to a common variable. Found Sci. 2022;27(2):287–304. https://doi.org/10.1007/s10699-021-09782-5 .
Article PubMed Google Scholar
Pattyn V, Molenveld A, Befani B. Qualitative comparative analysis as an evaluation tool: lessons from an application in development cooperation. Am J Eval. 2019;40(1):55–74.
Anderson JE, Aase K, Bal R, Bourrier M, Braithwaite J, Nakajima K, et al. Multilevel influences on resilient healthcare in six countries: An international comparative study protocol. BMJ Open. 2020;10(12):e039158. https://doi.org/10.1136/bmjopen-2020-039158 .
Warren J, Wistow J, Bambra C. Applying qualitative comparative analysis (QCA) in public health: a case study of a health improvement service for long-term incapacity benefit recipients. J Public Health (Oxf). 2014;36(1):126–33. https://doi.org/10.1093/pubmed/fdt047 .
Hanckel B, Petticrew M, Thomas J, Green J. The use of Qualitative Comparative Analysis (QCA) to address causality in complex systems: a systematic review of research on public health interventions. BMC Public Health. 2021;21(1):877. https://doi.org/10.1186/s12889-021-10926-2 .
Awori Hayanga JW, Kakuturu J, Toker A, Asad F, Siler A, Hayanga H, et al. Early trends in ECMO mortality during the first quarters of 2019 and 2020: Could we have predicted the onset of the pandemic? Perfusion. 2022:2676591221114959. https://doi.org/10.1177/02676591221114959 .
Kaji A, Koenig KL, Bey T. Surge capacity for healthcare systems: a conceptual framework. Acad Emerg Med. 2006;13(11):1157–9. https://doi.org/10.1197/j.aem.2006.06.032 .
Barbisch DF, Koenig KL. Understanding surge capacity: essential elements. Acad Emerg Med. 2006;13(11):1098–102. https://doi.org/10.1197/j.aem.2006.06.041 .
Koenig KL, Lim HCS, Tsai S-H. Crisis standard of care: Refocusing health care goals during catastrophic disasters and emergencies. J Exp Clin Med. 2011;3(4):159–65. https://doi.org/10.1016/j.jecm.2011.06.003 .
Organisation for Economic Co-operation and Development. Beyond containment: Health systems responses to COVID-19 in the OECD. 2020.
Abir M, Nelson C, Chan EW, Al-Ibrahim H, Cutter C, Patel KV, et al. Critical care surge response strategies for the 2020 COVID-19 outbreak in the United States. Santa Monica: RAND Corporation; 2020.
Book Google Scholar
Toerper MF, Kelen GD, Sauer LM, Bayram JD, Catlett C, Levin S. Hospital surge capacity: a web-based simulation tool for emergency planners. Disaster Med Public Health Prep. 2018;12(4):513–22. https://doi.org/10.1017/dmp.2017.93 .
OECD. National accounts of OECD countries, Volume 2022 Issue 1. 2022.
OECD Statistics. Organisation for Economic Co-operation and Development. https://stats.oecd.org/ . Accessed 8 Feb 2022.
World Population Prospects 2019. United Nations, Department of Economic and Social Affairs, Population Division. https://population.un.org/wpp/Download/Standard/Population/ . Accessed 1 Dec 2021.
WHO coronavirus online dashboard. World Health Organization. https://covid19.who.int/table . Accessed 8 Feb 2022.
Bohm K, Schmid A, Gotze R, Landwehr C, Rothgang H. Five types of OECD healthcare systems: Empirical results of a deductive classification. Health Policy. 2013;113(3):258–69. https://doi.org/10.1016/j.healthpol.2013.09.003 .
European Observatory on Health S, Policies, Blümel M, Spranger A, Achstetter K, Maresso A, et al. Germany: Health system review. Copenhagen: World Health Organization. Regional Office for Europe; 2020. p. i–273.
Sakamoto H, Rahman M, Nomura S, Okamoto E, Koike S, Yasunaga H, et al. Japan health system review. New Delhi: World Health Organization. Regional Office for South-East Asia; 2018.
World Health Organization. Regional office for the Western P. WHO Regional Office for the Western Pacific: Republic of Korea health system review. Manila; 2015.
European Observatory on Health S, Policies. United States: Health system review. Copenhagen: World Health Organization. Regional Office for Europe; 2020.
Park Y, Huh IS, Lee J, Kang CR, Cho S-i, Ham HJ, et al. Application of Testing-Tracing-Treatment strategy in response to the COVID-19 outbreak in Seoul, Korea. J Korean Med Sci. 2020;35(45). https://doi.org/10.3346/jkms.2020.35.e396 .
Kim S. Japan’s response to COVID-19 and its assessment: Cooperative governance in the fields of health and medicine. Korean J Japanese Stud. 2020;52:6–33.
Shimizu K, Negita M. Lessons learned from Japan’s response to the first wave of COVID-19: a content analysis. Healthcare (Basel). 2020;8(4):426. https://doi.org/10.3390/healthcare8040426 .
Kim KA, Yoo AJ, Kim SY, Lee YJ, Jung HJ. Status of health insurance systems and reform trends in major countries in 2019, Vol. 5 Japan. National Health Insurance Service; 2019.
Kim NS, Song ES, Park EJ, Jeon JA, Byun JH, Moon JH. Comparison and analysis of the impact of European national health care systems on COVID-19 response. Korea Institute for Health and Social Affairs; 2020.
Jung YS, Lee HY, Yang YS, Moon JS. Status of health insurance systems and reform trends in major countries in 2019, vol. 2. Germany: National Health Insurance Service; 2019.
Lee JE, Back JH, Na YK, Byun JO. Status of health insurance systems and reform trends in major countries in major countries in 2019, Vol. 12 The United States of America. National Health Insurance Service; 2014.
Fast Facts on U.S. Hospitals, 2023. American Hospital Association. https://www.aha.org/statistics/fast-facts-us-hospitals . Accessed 23 Aug 2023.
Baron RJ. New pathways for primary care: an update on primary care programs from the innovation center at CMS. Ann Fam Med. 2012;10(2):152–5. https://doi.org/10.1370/afm.1366 .
Geruso M, Richards MR. Trading spaces: Medicare’s regulatory spillovers on treatment setting for non-Medicare patients. J Health Econ. 2022;84:102624. https://doi.org/10.1016/j.jhealeco.2022.102624 .
July 2020 Quarterly Update to the Inpatient Prospective Payment System (IPPS) Fiscal Year (FY) 2020 Pricer: Centers for Medicare & Medicaid Services; 2020. https://www.cms.gov/files/document/mm11764.pdf . Accessed 11 Dec 2021.
Ministry of Health, Labour and Welfare of Japan. Special response to health services compensations related to the acceptance of COVID-19 patients; May 25, 2020. https://www.mhlw.go.jp/content/12404000/000649878.pdf . Accessed 1 Dec 2021.
Ministry of Health, Labour and Welfare of Japan. Special response to health services compensations related to the acceptance of COVID-19 patients; September 14, 2020. https://www.mhlw.go.jp/content/12404000/000671934.pdf . Accessed 1 Dec 2021.
Ministry of Health, Labour and Welfare of Japan. Additional support for medical institutions responding to COVID-19; 2020. https://www.mhlw.go.jp/content/000726525.pdf . Accessed 12 Dec 2021.
Ministry of Health, Labour and Welfare of Japan. Response to COVID-19; 2020. https://www.mhlw.go.jp/content/12404000/000802103.pdf . Accessed 26 Dec 2021.
Centers for Medicare and Medicaid Services. CMS changes medicare payment to support faster COVID-19 diagnostic testing; 2020. https://www.cms.gov/newsroom/press-releases/cms-changes-medicare-payment-support-faster-covid-19-diagnostic-testing . Accessed 2 Jan 2022.
Centers for Medicare and Medicaid Services. CMS develops additional code for coronavirus lab tests; 2020. https://www.cms.gov/newsroom/press-releases/cms-develops-additional-code-coronavirus-lab-tests . Accessed 1 Dec 2021.
LaPointe J. CMS releases medicare reimbursement details for COVID-19 tests: Xtelligent Healthcare Media; 2020. https://revcycleintelligence.com/news/cms-releases-medicare-reimbursement-details-for-covid-19-tests . Accessed 2 Jan 2022.
Centers for Medicare and Medicaid Services. Medicare telemedicine health care provider fact sheet; 2020. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet . Accessed 11 Dec 2021.
Ministry of Health, Labour and Welfare of Japan. Compensation for health services based on the response to COVID-19 and its effects; December 18, 2020 https://www.mhlw.go.jp/content/12404000/000706834.pdf . Accessed 1 Dec 2021.
Ministry of Health, Labour and Welfare of Japan. Additional support for medical institutions responding to COVID-19; 2020. https://www.mhlw.go.jp/content/000690449.pdf . Accessed 12 Dec 2021.
European Observatory. Health financing - COVID-19 Hospital Relief Act: financial support for hospitals; November 9, 2020. https://eurohealthobservatory.who.int/monitors/hsrm/hsrm-countries/hsrm/germany/paying-for-services/health-financing/ . Accessed 17 Feb 2022.
Centers for Medicare & Medicaid Services. COVID-19 emergency declaration blanket waivers for health care providers; 2021. https://www.cms.gov/files/document/covid-19-emergency-declaration-waivers.pdf . Accessed 22 Feb 2022.
Ministry of Health and Welfare of Korea. Guidance for support for medical institutions. 2020.
Scarfone RJ, Coffin S, Fieldston ES, Falkowski G, Cooney MG, Grenfell S. Hospital-based pandemic influenza preparedness and response: Strategies to increase surge capacity. Pediatr Emerg Care. 2011;27(6):565–72. https://doi.org/10.1097/PEC.0b013e31821dc9d1 .
Fiest KM, Krewulak KD. Space, Staff, Stuff, and System. Keys to ICU care organization during the COVID-19 pandemic. Chest. 2021;160(5):1585–6. https://doi.org/10.1016/j.chest.2021.07.001 .
Oh J, Lee J-K, Schwarz D, Ratcliffe HL, Markuns JF, Hirschhorn LR. National response to COVID-19 in the Republic of Korea and lessons learned for other countries. Health Syst Reform. 2020;6(1):e1753464. https://doi.org/10.1080/23288604.2020.1753464 .
National Health Insurance Service. It is worth paying for suitable contributions 87.0% [press release]. 2020.
Kim J, Kim JI. The introduction and development of the national health insurance: Political and economic background and macroeconomic considerations. Korean Econ Forum. 2021;14(3):1–46. https://doi.org/10.22841/kefdoi.2021.14.3.001.
Download references
Acknowledgements
Not applicable.
This research did not receive any funding.
Author information
Won Mo Jang and Jin Yong Lee contributed equally to this work as corresponding authors.
Authors and Affiliations
Human Resource Administration Department, Health Insurance Review & Assessment Service, Wonju-Si, Gangwon-Do, Republic of Korea
Division of Pharmaceutical Policy Research, HIRA Research Institute, Health Insurance Review & Assessment Service, Wonju-Si, Gangwon-Do, Republic of Korea
Division of Review and Assessment Research, HIRA Research Institute, Health Insurance Review & Assessment Service, Wonju-Si, Gangwon-Do, Republic of Korea
Boryung Ahn
Department of Family Medicine, Seoul National University Bundang Hospital, Bundang-Gu, Seongnam-Si, Gyeomggi-Do, Republic of Korea
Department of Family Medicine, Seoul National University College of Medicine, Jongno Gu, Seoul, Republic of Korea
Department of Public Health and Community Medicine, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, 20 Boramae-Ro 5-Gil, Dongjak-Gu, Seoul, 07061, Republic of Korea
Won Mo Jang
Department of Health Policy and Management, Seoul National University College of Medicine, 101 Daehak-Ro, Jongno-Gu, Seoul, 03080, Korea
Won Mo Jang & Jin Yong Lee
Public Health Care Center, Seoul National University Hospital, Jongno-Gu, Seoul, Republic of Korea
Jin Yong Lee
HIRA Research Institute, Health Insurance Review and Assessment Service, Wonju-Si, Gangwon-Do, Republic of Korea
You can also search for this author in PubMed Google Scholar
Contributions
Research conception and design: JYL, WMJ, HJK, HL; Investigation and formal analysis: HJK, EY, BA; Interpretation of data: All authors, Drafting of the manuscript: HJK; Critical review of the manuscript: All authors, Supervision: JYL, WMJ; Approval of final manuscript: All authors.
Corresponding authors
Correspondence to Won Mo Jang or Jin Yong Lee .
Ethics declarations
Ethics approval.
This study was approved by the Institutional Bioethics Committee of the Health Insurance Review and Assessment Service (IRB No. 2021–076).
Consent to participate
Consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Flow Chart of Literature Selection. Figure describing the process of identification, exclusion, and inclusion of relevant data sources.
Additional file 2.
Summary of the Reviewed Literature. Table describing the collected data, including publications from the European Observatory on Health Systems and Policies; publications, web pages, and press releases from governments or health insurers; and an OECD research report.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ko, H.J., Yun, E., Ahn, B. et al. Lessons from health insurance responses in counteracting COVID-19: a qualitative comparative analysis of South Korea and three influential countries. Arch Public Health 81 , 205 (2023). https://doi.org/10.1186/s13690-023-01209-w
Download citation
Received : 20 June 2023
Accepted : 28 October 2023
Published : 21 November 2023
DOI : https://doi.org/10.1186/s13690-023-01209-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health insurance
- Surge capacity
Archives of Public Health
ISSN: 2049-3258
- General enquiries: [email protected]
- Introduction
- Conclusions
- Article Information
ESI indicates employer-sponsored insurance.
Point estimates from regressions are shown, and the error bars indicate 95% CIs. ESI indicates employer-sponsored insurance.
eTable 1. Comparison of the Weighted Estimates of Demographic Characteristics of Respondents in the 2018 and 2019 ACS, 2018 NHIIS, and the 2020 HPS
eFigure 1. Comparison of Distribution of Health Insurance Coverage between the 2019 ACS and the 2020 HPS
eFigure 2A. Comparison of Distribution of Health Insurance Coverage between the 2019 ACS and HPS Spring/Summer 2020 Period by State
eFigure 2B. Comparison of Distribution of Health Insurance Coverage between the 2019 ACS and HPS Fall/Winter 2020 Period by State
eTable 2. Rates of Missing Data from the Household Pulse Survey for Key Study Variables by Week
eFigure 3. Estimates of Insurance Coverage in the HPS by Week and Type of Insurance
eTable 3. Test of Difference in Time Trend of Health Insurance Coverage by Survey Period
eFigure 4A. Sensitivity of Results to Dropping Missing Data, Expansion and Non-Expansion States
eFigure 4B. Sensitivity of Results to Dropping Missing Data, Demographic and Socioeconomic Characteristics
eTable 4A. Underlying Data for Estimates Presented in Figure 2
eTable 4B. Underlying Data for Estimates Presented in Figure 3
eReferences
- Fewer People May Have Become Uninsured in 2020 Than Feared JAMA Health Forum Invited Commentary September 3, 2021 Jessica Banthin, PhD
See More About
Select your interests.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Bundorf MK , Gupta S , Kim C. Trends in US Health Insurance Coverage During the COVID-19 Pandemic. JAMA Health Forum. 2021;2(9):e212487. doi:10.1001/jamahealthforum.2021.2487
Manage citations:
© 2024
- Permissions
Trends in US Health Insurance Coverage During the COVID-19 Pandemic
- 1 Sanford School of Public Policy, Duke University, Durham, North Carolina
- 2 National Bureau of Economic Research, Cambridge, Massachusetts
- 3 Indiana University–Purdue University Indianapolis, Indianapolis
- 4 Stanford University, Stanford, California
- Invited Commentary Fewer People May Have Become Uninsured in 2020 Than Feared Jessica Banthin, PhD JAMA Health Forum
Question How did health insurance coverage change during the COVID-19 pandemic?
Findings In this cross-sectional survey study of more than 1.2 million US adults, rates of employer-sponsored coverage declined and rates of other types of coverage increased after the pandemic began and throughout 2020. Rates of uninsurance increased, particularly during the spring and summer.
Meaning While public programs played an important role in protecting US adults from pandemic-driven declines in employer-sponsored coverage, many people became uninsured during the pandemic.
Importance While most working-age adults in the US obtain health insurance through an employer, little is known about the implications of the massive pandemic-related job loss in March 2020 and subsequent rebound for rates of employer-sponsored coverage and uninsurance.
Objective To determine how health insurance coverage changed during the COVID-19 pandemic.
Design, Setting, and Participants Analysis of trends in insurance coverage based on repeated cross sections of the US Census Bureau’s Household Pulse Survey data, using linear regression to adjust for respondent’s demographic and socioeconomic characteristics and state of residence. More than 1.2 million US adults aged 18 to 64 years were surveyed from April 23 through December 21, 2020.
Exposures The COVID-19 pandemic, separated into spring and summer and fall and winter time periods during 2020, as well as state Medicaid expansion status.
Main Outcomes and Measures Regression-based estimates of the weekly percentage-point change in respondents’ health insurance status, including having any health insurance, any employer-sponsored health insurance, or only nonemployer sponsored coverage. Nonemployer-sponsored coverage is categorized into private, Medicaid, and other public in some analyses.
Results The study population included 1 212 816 US adults (51% female; mean [SD] age, 42 [13] years) across all 50 US states and Washington DC. Among these respondents, rates of employer-sponsored coverage declined by 0.2 percentage points each week during the COVID-19 pandemic. Other types of coverage, particularly from public sources, increased by 0.1 and 0.2 percentage points in the spring and summer and fall and winter periods, respectively. Overall, health insurance coverage of any type declined, particularly during the spring and summer period, during which uninsurance increased by 1.4 percentage points, representing more than 2.7 million newly uninsured people, over a 12-week period.
Conclusions and Relevance In this cross-sectional study of data from the US Census Bureau’s Household Pulse Survey, results showed that while public programs played an important role in protecting US adults from pandemic-driven declines in employment-sponsored coverage, many people became uninsured during 2020.
The COVID-19 pandemic has placed millions of workers at risk of uninsurance. The pandemic’s onset was accompanied by an unprecedentedly large, swift decline in employment, with the unemployment rate peaking at 14.7% in April 2020 and steadily declining to 6.7% in December 2020. These rates do not account for those who had dropped out of the labor force. 1 Because employer-sponsored insurance (ESI) is the primary source of coverage for working-age adults, 2 losing a job not only leads to loss of income, but may also lead to loss of health insurance. The financial risk of COVID-19–related care heightened the potential negative consequences of uninsurance.
The extent of uninsurance during the COVID-19 recession, however, is largely unknown, primarily owing to a lack of comprehensive, real-time data on coverage. 3 Yet, this recession differed in important ways from earlier economic downturns, including the swiftness of the initial economic decline and the sensitivity of the recovery to both policy and the epidemiology of COVID-19. We addressed this gap by analyzing the 2020 Household Pulse Survey (HPS), 4 a US Census Bureau experimental data product intended to provide timely information on the pandemic’s effect on US households. The survey, which has been conducted approximately every 1 to 2 weeks since April 2020, allows us to examine trends in coverage during the pandemic and to provide some of the first evidence on coverage from a large, high-frequency survey designed to be nationally representative. While the HPS has limitations, primarily owing to its low response rate and its lag in data collection relative to the large, initial decline in employment, with 40 000 to 130 000 respondents per week it is perhaps the only source of information on trends in health insurance coverage during the pandemic from a large population-based sample.
We documented the extent to which insurance coverage changed between mid-April and December 2020. The present analysis is based on the premise that pandemic-driven job loss may have led to declines in ESI that lagged the initial employment decline and persisted throughout 2020. In addition, the extent to which declining own ESI was accompanied by rising uninsurance depends on both whether newly unemployed workers had coverage prior to the pandemic and whether people accessed coverage alternatives during the pandemic, including enrolling in coverage through a spouse or other family member, retaining group coverage through COBRA (Consolidated Omnibus Budget Reconciliation Act), 5 purchasing subsidized or unsubsidized private individual coverage, or enrolling in a public program such as Medicaid. Given Medicaid’s safety-net role, we investigated differences between states that did and did not expand Medicaid through the Affordable Care Act (ACA). We also examined differences by prepandemic family income, age, sex, and race and ethnicity based on evidence of the pandemic’s disproportionate labor market effects across groups. 6
We collected data from the US Census Bureau’s 2020 HPS, which was fielded approximately every 1 to 2 weeks beginning April 23, 2020. 7 The HPS randomly selects participants using the US Census Bureau’s Master Address File. Sampled households are contacted by either email or cell phone and then directed to an online survey. 7 The survey, which was designed to produce state-level estimates, includes responses from between approximately 40 000 and 130 000 respondents each week. As anticipated by the survey designers, however, response rates are relatively low at 1.3% to 10.3% per week. 7 - 9 We limited the sample to people aged 18 to 64 years to focus on those reliant on ESI. Herein we present several analyses comparing the HPS with alternative nationally representative surveys (eTable 1 in the Supplement ).
Because this study used deidentified secondary data, it was not deemed human subject research and not subject to review by the institutional review board at Duke University. The study provides information on response rates as advised by the American Association for Public Opinion Research (AAPOR) reporting guideline. 10
We defined any insurance as whether the respondent indicated having any source of coverage. We divided this category into 2 mutually exclusive groups: any ESI and, among those without ESI, any other non-ESI coverage. When comparing expansion and nonexpansion states, we delineated non-ESI into other private, Medicaid, and other public coverage. Details on measure construction and comparisons to other surveys are provided in eFigures 1, 2A, and 2B in the Supplement .
We estimated the weekly percentage-point change in insurance between April 23 and December 21, 2020. For each coverage type, we regressed an indicator on a continuous measure of calendar week, testing for a linear trend in coverage over the survey period. We separately analyzed 2 time periods: April 23 through July 21, 2020 (spring and summer), and August 19 through December 21, 2020 (fall and winter), for 2 reasons. First, the epidemiologic, policy, and economic environments changed dramatically between the periods. Spring and summer were marked by a flatter pandemic curve, gradual reopenings of state economies, and the operation of the federal Paycheck Protection Program. 11 - 14 In contrast, fall and winter saw a resurgence in COVID-19 cases and deaths, the lifting of many state business closures, school reopenings, and termination of the federal Paycheck Protection Program. Second, the survey instrument changed between the 2 periods, with a nearly month-long gap between them, a shift from weekly to biweekly frequency, and, while the health insurance questions were asked in the same way, they appeared later in the questionnaire, resulting in higher nonresponse rates (eTable 2 in the Supplement ).
We estimated linear regression models, adjusting for respondents’ sex, age, race and ethnicity, education, household size, and indicators of any children in the household and state of residence to control for changes over time in sample composition that may not be captured in survey weights (eTable 1 in the Supplement ). We applied the replicate weights developed by the US Census Bureau, which adjusted for nonresponse and coverage of the demographics of the US population, 7 adjusted the standard errors for clustering within state, and reported the coefficient and 95% CIs on the week measure.
We also estimated separate models by state Medicaid expansion status and by respondent sex (male and female), age (18-26, 27-40, 41-50, and 51-64 years), race and ethnicity (Hispanic, non-Hispanic Asian, non-Hispanic Black, and non-Hispanic White), and pretax, prepandemic annual household income reported retrospectively by the respondent (<$50 000, $50 000-99 999, and ≥$100 000). We excluded observations with missing values for health insurance and those from respondents in the state of Nebraska because it underwent ACA Medicaid expansion during the study period. We also excluded those with missing values for family income in analyses by family income (eTable 2 in the Supplement ).
The Supplement provides several analyses supporting our approach. First, models estimated with weekly fixed effects rather than the linear trend demonstrate that the linear trend is an appropriate approximation for health insurance trends (eFigure 3 in the Supplement ). Second, tests of whether the linear trend differed between the 2 time periods guide the interpretation of the findings (eTable 3 in the Supplement ). Finally, rather than dropping those with missing data on insurance, we reestimated the models by coding missing coverage as a separate category, providing evidence that the results were not sensitive to this exclusion (eFigure 4 in the Supplement ). All analyses were conducted using Stata MP, version 16.1 (StataCorp), and statistical significance was defined as P ≤ .05.
The study sample, which included 1 212 816 US adults aged 18 to 64 years (51% female; mean [SD] age, 42 [13] years), is similar to the nationally representative American Community Survey and National Health Interview Survey 15 based on respondent sex, race and ethnicity, and education, but it is slightly older with a larger mean household size (eTable 1 in the Supplement ). The HPS was first fielded on April 23, 2020, just after unemployment had peaked ( Figure 1 ). The unemployment rate steadily declined during the remainder of the calendar year. Unadjusted rates of ESI generally declined throughout the year while other coverage generally increased, resulting in either stable or slightly declining rates of any insurance coverage in both time periods. Figure 1 also demonstrates that there were upward and downward shifts in rates of ESI and other coverage, respectively, between the 2 periods. Analyses were conducted separately for each period because it could not be determined whether these shifts were due to survey changes or true coverage changes.
The proportion of people with any type of health insurance decreased by 0.11 percentage points each week during the 12-week period of spring and summer ( Figure 2 and eTable 4A in the Supplement ), resulting in a 1.36 (0.1137 × 12) percentage-point decline in coverage over the 12-week period. The rise in uninsurance resulted from a 0.21–percentage-point weekly decline in employer-sponsored coverage that was only partly offset by an increase in other coverage.
In contrast, in the fall and winter period the estimate of the decline in any coverage was smaller and not statistically significant; the difference between the 2 periods is statistically significant (eTable 3 in the Supplement ). While rates of ESI continued to decline by 0.19 percentage points weekly, the decline was more fully offset by increases in other coverage, primarily Medicaid.
The decline in insurance during spring and summer was concentrated in states not expanding Medicaid. In nonexpansion states, rates of any coverage declined by 0.23 percentage points weekly; rates of ESI declined by 0.32 percentage points per week, while rates of other coverage increased by 0.09 percentage points. In expansion states, in contrast, the overall decline in coverage was small and not statistically significantly different from zero—the combination of a smaller decline in ESI (0.16 percentage points per week) and a similarly sized increase in other coverage as nonexpansion states. In other words, decline in insurance in nonexpansion states was associated with a large decline in ESI, relative to expansion states, that was less fully offset by increases in non-ESI. The increase in non-ESI represented 28% and 63% of the decline in ESI in nonexpansion and expansion states, respectively, during the spring and summer. In both expansion and nonexpansion states, public rather than private coverage was the primary source of coverage gains.
In contrast, during the fall and winter, the differences between expansion and nonexpansion states were less striking ( Figure 2 ). In both types of states, rates of ESI continued to decline but were nearly fully offset by increases in public coverage.
The trends varied by population subgroups, particularly in the spring and summer ( Figure 3 and eTable 4B in the Supplement ). Early in the pandemic, rising uninsurance was concentrated among men, people aged 27 to 50 years, people of Hispanic ethnicity, and people in families with relatively low prepandemic income. For these groups, the decline in ESI was larger than the increase in other sources. People classified in the HPS as Asian and those in the middle family income category also experienced declines in ESI, but they were nearly fully offset by increases in other coverage. In contrast, in the fall and winter declines in rates of ESI were more similar across demographic and socioeconomic subgroups, with nearly every group with the exception of Asian individuals and high prepandemic income households reporting a statistically significant decline (eTable 4B in the Supplement ). However, there was not evidence of rising uninsurance in any subgroup due to increases in other sources.
Results of this study provide new evidence on how insurance coverage changed during the COVID-19 pandemic. We found that rates of ESI declined throughout much of 2020, even after the initial shock to employment in March. Because ESI declined throughout the 2 study time periods, a time during which employment was increasing, the results suggest either that ESI declines lagged job loss or that people who returned to work did not necessarily recover their employer-sponsored coverage.
While rates of ESI declined, enrollment in other types of coverage increased. Over the spring and summer period, increases in other types of coverage only partially offset declining ESI, resulting in a 1.36–percentage point increase in uninsurance or approximately 2.7 million newly uninsured people over the 12-week period. The 2.7 million estimate is the product of the number of people 18 to 64 years old in the US in 2019 (202 142 110), 16 the weekly change in coverage (0.11 percentage points), and the number of weeks (12).
The results indicate that much of the overall decline in coverage took place within a short 3-month period early in the pandemic. While employer-sponsored coverage declined throughout 2020, the decline was more fully offset by increases in other sources later in the year. This could be due to several factors. People may have delayed pursuing alternative sources of coverage early in the pandemic because of substantial uncertainty in the economic environment, such as likely length of unemployment. In addition, it may have taken people time to identify and enroll in alternative coverage sources, particularly because the enrollment process itself may have slowed, given the widespread disruption to businesses and government offices. Finally, the winter surge of COVID-19 cases may have strengthened incentives to obtain coverage as the risk of infection increased. The cross-sectional nature of the HPS does not allow us to determine whether those losing ESI were the same as those gaining other coverage—indeed the gains in non-ESI coverage we observed in the fall and winter period may be responses to coverage loss earlier in the year.
We found that enrollment in public programs, rather than private insurance such as COBRA or on- or off-exchange individual coverage, increased throughout the year. A large increase in Medicaid enrollment was consistent with documentation of rising Medicaid enrollment during the pandemic, as well as prepandemic evidence that the ACA’s new coverage options have alleviated the negative effect of unemployment on insurance coverage. 17 - 19 The increase in public coverage may also be because of provisions of the Families First Coronavirus Response Act, which prevented states from terminating Medicaid coverage during the pandemic. 20 In other words, rising rates of Medicaid coverage in both expansion and nonexpansion states may have been driven in part by declining disenrollment due to this policy.
Low take-up of private alternatives may have been driven by their high cost, particularly given the uncertainty over the length of job loss. Many people view extending coverage through COBRA as expensive because most are required to pay the full premium paid by the employer—more than $21 000 annually for family coverage in 2020, plus an administrative fee. 21 , 22 People, particularly those without large subsidies, may also view exchange coverage as expensive. Finally, some workers may have been furloughed, retaining coverage until they returned to work. Of course, it is also possible that people either were simply not aware of these options or had private coverage but thought it was public when responding to the survey, particularly in the case of subsidized exchange coverage.
We also documented that, particularly in the early stages, the pandemic had disproportionate associations with coverage across population subgroups. The present results indicate that this issue may be particularly important for Hispanic adults who experienced a decline in ESI without an offsetting increase in non-ESI, resulting in an increase in uninsurance. This raises the concern that the COVID-19 pandemic may have undone some of the reductions in disparities in health insurance generated by the ACA. 23
The COVID-19 recession, which was initiated by a public health crisis rather than a financial crisis, differs in important ways from the most recent major economic downturn, the Great Recession (2007-2010). In the Great Recession, the association between rising unemployment and uninsurance was concentrated among college-educated, white, older men, and public programs served as a key insurance safety net for women and children. 24 The COVID-19 recession’s 2-month employment decline, however, was approximately 50% larger than the 2-year employment decline in the Great Recession. In addition, the types of workers losing jobs differed; workers in construction and manufacturing were most affected in the Great Recession, while job loss was concentrated among low-wage service workers in the COVID-19 recession. 25 Not only did the nature of job loss differ, but newly unemployed workers had more sources of subsidized insurance available to them in the COVID-19 recession. Results of this study suggest that Medicaid, in particular, played an important safety-net role for a broader population, likely because more people are now eligible for Medicaid than in 2007 through 2009. Whether Medicaid coverage continues to expand in 2021 depends on the extent to which employment gains affect Medicaid eligibility. In addition, the American Rescue Plan considerably expanded subsidies for both exchange and COBRA coverage, creating additional alternatives for people without ESI 26 and suggesting that the private plans may begin to play a more important role.
Looking ahead, unemployment rates are currently much lower than the pandemic’s peak (5.8% in May 2021 vs 14.7% in April 2020) but still above the prepandemic levels, and employment recovery has been lagging among racial and ethnic minority subpopulations. 6 , 27 These trends point to the continued importance of safety-net programs both in providing coverage for unemployed workers and in addressing insurance disparities.
This study has several limitations. The HPS’s low response rate, as well as the use of alternative contact modalities including email and texts, raises concern over sample representativeness. The weighted HPS sample is similar to the American Community Survey (eTable 1 in the Supplement ) along some dimensions but not others. While rates of insurance coverage differ from those of other surveys, we note that the differences are consistent across states (eFigures 1 and 2 in the Supplement ). The present analyses also may miss some of the pandemic’s early effect on coverage given the timing of the HPS’s initial wave relative to the timing of pandemic-related job loss ( Figure 1 ). We also emphasize that the analyses are descriptive. We expect that changes in ESI during the COVID recession were driven by changes in employment. However, the present data do not allow us to link insurance coverage and employment at the individual level. Finally, we note that we interpreted the change in coverage between the spring and summer and fall and winter phases of the survey as driven primarily by the change in survey design and the resulting lower response rate for health insurance questions. It is possible that coverage changed in this short time period in ways that the survey does not allow us to track with the result that the findings may not be representative of the total change in coverage over the study period.
Overall, results of this cross-sectional study indicate that while public programs played an important role in insulating US adults from pandemic-driven declines in ESI, many became uninsured. Monitoring and strengthening the health insurance safety net will continue to be a policy challenge during the COVID-19 pandemic and beyond.
Accepted for Publication: July 12, 2021.
Published: September 3, 2021. doi:10.1001/jamahealthforum.2021.2487
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2021 Bundorf MK et al. JAMA Health Forum .
Corresponding Author: M. Kate Bundorf, PhD, MBA, MPH, Sanford School of Public Policy, Duke University, 302 Towerview Rd, PO Box 90311, Durham, NC 27708 ( [email protected] ).
Author Contributions: Prof Bundorf and Dr Gupta had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Bundorf, Gupta.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Bundorf, Gupta.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: All authors.
Administrative, technical, or material support: Bundorf, Gupta.
Supervision: Bundorf, Gupta.
Conflict of Interest Disclosures: None reported.
Additional Contributions: We thank Kosali Simon, PhD, of Indiana University for helpful suggestions in the development of this article, as well as the editor and 2 anonymous reviewers from JAMA Health Forum for their constructive comments. No compensation was provided for the contributions.
Additional Information: The data sources used in this project are publicly available. The programming code used to generate these results is publicly available at github.com/bundorf/doi-10.1001-jamahealthforum.2021.2487 .
- Login To RMS System
- About JETIR URP
- About All Approval and Licence
- Conference/Special Issue Proposal
- Book and Dissertation/Thesis Publication
- How start New Journal & Software
- Best Papers Award
- Mission and Vision
- Reviewer Board
- Join JETIR URP
- Call For Paper
- Research Areas
- Publication Guidelines
- Sample Paper Format
- Submit Paper Online
- Processing Charges
- Hard Copy and DOI Charges
- Check Your Paper Status
- Current Issue
- Past Issues
- Special Issues
- Conference Proposal
- Recent Conference
- Published Thesis
Contact Us Click Here
Whatsapp contact click here, published in:.
Volume 8 Issue 8 September-2021 eISSN: 2349-5162
UGC and ISSN approved 7.95 impact factor UGC Approved Journal no 63975
Unique identifier.
Published Paper ID: JETIR2108615
Registration ID: 314590
Page Number
Post-publication.
- Downlaod eCertificate, Confirmation Letter
- editor board member
- JETIR front page
- Journal Back Page
- UGC Approval 14 June W.e.f of CARE List UGC Approved Journal no 63975
Share This Article
Important links:.
- Call for Paper
- Submit Manuscript online

- Dr. Varsha Agarwal
- Akshaya Kumar M
- Mohammed Saquib Sherief K
- Esha Kothari
Cite This Article
2349-5162 | Impact Factor 7.95 Calculate by Google Scholar An International Scholarly Open Access Journal, Peer-Reviewed, Refereed Journal Impact Factor 7.95 Calculate by Google Scholar and Semantic Scholar | AI-Powered Research Tool, Multidisciplinary, Monthly, Multilanguage Journal Indexing in All Major Database & Metadata, Citation Generator
Publication Details
Download paper / preview article.
Download Paper
Preview this article, download pdf, print this page.
Impact Factor:
Impact factor calculation click here current call for paper, call for paper cilck here for more info important links:.
- Follow Us on
- Developed by JETIR

IMAGES
COMMENTS
Our report re views the profound impact of the current Covid-19 pandemic on an importa nt industry. like the insurance sector and how insurance firms have take n the pandemic to be an opportunity ...
The COVID-19 pandemic has placed millions of workers at risk of uninsurance. The pandemic's onset was accompanied by an unprecedentedly large, swift decline in employment, with the unemployment rate peaking at 14.7% in April 2020 and steadily declining to 6.7% in December 2020.
A Crisis in Public Health. The United States has 4% of the world's population but, as of July 16, approximately 26% of its Covid-19 cases and 24% of its Covid-19 deaths. 17 These startling ...
1. INTRODUCTION. The COVID-19 pandemic has caused an unprecedented policy response from public health. officials and governments. As of September 16, 2021, approximately 4.7 million deaths. worldwide and 669,000 deaths in the United States were attributed to COVID-19 (Johns Hopkins. Coronavirus Resource Center 2022).
The COVID-19 pandemic had the potential to alter patterns of health insurance coverage in the US. Using data from the Medical Expenditure Panel Survey, we found increased stability of Medicaid cove...
The COVID-19 pandemic has posed a sudden and unexpected shock to the insurance industry. The financial impact is huge with profits dropping by 16.6% within the period under review—March to June 2020. Total premiums have dropped by 17.01% while claims have increased by 38.4%.
COVID-19 and the US health insurance conundrum. The devastating efects of the COVID-19 pandemic go far beyond public health; with many industries on hold and unemployment increasing worldwide, the global economy is approaching the deepest recession in living memory. In the USA, where health insurance is largely provided by employers and more ...
The empirical results show that more confirmed COVID-19 cases are associated with greater per capita insurance revenue and the results are robust when considering endogeneity concern, and it is found that the impact of CO VID-19 on insurance revenue only exists in regions with worse medical treatment conditions or higher medical burden. The COVID-19 has been a worldwide pandemic and it needs ...
incentivize getting the COVID-19 vaccine. Some companies have begun charging unvaccinated employees more for health insurance to cover the increased risk of hospitalization with COVID-19. While only 1% of companies surveyed had taken this measure as of September 2021, 13% reported considering it and larger companies comprised one-fifth of that ...
The World Health Organization considers the right to health as a fundamental right for all [1, 2].Countries are required to ensure the availability of sustainable financial resources alongside other health resources to realize this right [3,4,5].Insurance usually plays the role of an intermediary organization in transferring financial resources from the consumer of health services to its ...
The COVID-19 pandemic has caused delays and restrictions in providing medical services. In response to the medical surge, countries with social insurance systems provided financial incentives to medical institutions. This study aimed to present the directions for health insurance support by comparing countries in terms of the domains and contents of COVID-19 health insurance support to ensure ...
This article aims to introduce the inception and operation of the COVID-19 International Collaborative Research Project, the world's first coronavirus disease 2019 (COVID-19) open data project for research, along with its dataset and research method, and to discuss relevant considerations for collaborative research using nationwide real-world data (RWD).
This post approaches this question in a novel way by exploiting a natural experiment—the adoption of the Affordable Care Act Medicaid expansion by some states but not others—to tease out the causal effect of a type of health insurance on COVID-19 intensity. Does health insurance improve health? This question, while apparently a tautology, has been the subject of considerable economic debate.
in the wake of COVID-19, including unemployment, mental illness, and addiction; and, (3) the importance of moderating factors (e.g., age, race and ethnicity, gender, personality, family status, and culture) for which there are likely to be disparate COVID-19 impacts.
COVID-19 Outbreak: Insurance Implications and Response1 March 29, 2020 The COVID-19 Pandemic is significant for the insurance sector, given its contractual coverage of ... Life and health insurance anticipate increased claims, as well as increased costs in providing for the benefits arising per claim, as would be expected.
For example, the UnitedHealth Group's net income during the second quarter grew from $3.4 billion in 2019 to $6.7 billion in 2020 and Anthem Inc's net income increased from $1.1 billion to $2.3 billion. Under the law, insurers must return a large portion of these excess revenues back to individuals, families, and employers.
Key Points. Question How did health insurance coverage change during the COVID-19 pandemic?. Findings In this cross-sectional survey study of more than 1.2 million US adults, rates of employer-sponsored coverage declined and rates of other types of coverage increased after the pandemic began and throughout 2020. Rates of uninsurance increased, particularly during the spring and summer.
Impact of COVID-19 on Cancer-Related Care in the United States: An Overview. I. Jabbal Saad Sabbagh. +4 authors. Z. Nahleh. Medicine. Current oncology. 2023. TLDR. This review provides an overview of the pandemic's impact on cancer care in the United States and suggests measures for tackling similar situations in the future.
Working Paper 580 May 2021. The Impact of the COVID-19 . Pandemic on Social Health Insurance . Claims for High-Burden Diseases in . the Philippines. Abstract. In the Philippines, anecdotes on the dwindling use of essential healthcare services as an indirect . consequence of the COVID-19 pandemic are mounting, but compelling evidence remains scarce.
Impact of Covid-19 Pandemic on Health Insurance Sector According to new research (Dr Niru Sharan, 2021, pp. 14636-14637), India has a long history of underinsured, with health insurance systems covering barely 18% of the urban population and little more than 14% in rural areas. (Dr.
PwC's COVID-19 CFO Pulse Survey (May 2020) shows that 51% of CFOs across sectors expect a decrease in revenue of up to 25% as a result of COVID-19. With respect to the potential impact on their company's revenue and/or profits this year, around 31.7% of the respondents across industries expected a roughly 10-25% decrease in their revenue.
Despite the increase in mortality risk and significant uncertainty, we find limited evidence that life insurance companies increased premiums or decreased policy offerings due to COVID-19. Timothy F. Harris Department of Economics Illinois State University College of Arts and Sciences Stevenson Hall 425 Normal, IL 61790 [email protected] Aaron ...
Unlike a cataclysmic disaster, the COVID-19 pandemic has revealed that global economic and financial activity are inextricably linked. Insurance claims and financial operations have experienced extreme growth in the life and non-life industries, which has put tremendous strain on the sector. Averting pandemic risk has failed miserably in the past.