- Practice task 1
- Practice task 2
- Practice task 3

Practice task 4
- Practice task 5
Read the case study, then answer the questions that follow.
Ingrid is a community services worker in a large team. Ingrid’s team attends a weekly team meeting to discuss important service changes and give an area report.
Ingrid was offended by something her supervisor Sandra said as this week’s meeting. She felt like Sandra was saying that all the other service areas were doing well and that Ingrid’s service area was under performing.
When Ingrid was giving her service update she felt like Sandra wasn’t even listening and that when Sandra did respond her responses were not related to the information Ingrid was providing.
At the end of the meeting Ingrid was unsure what follow up actions she should do next and didn’t even know what the point of the meeting was.
There are three questions.
CHCCOM005 Release 2, Aspire v1.1 © 2015 Aspire Training & Consulting Ltd trading as Aspire Learning Resources

Snapsolve any problem by taking a picture. Try it in the Numerade app?

Public perception of vets rooted in romanticised James Herriot fiction rather than fact
Bucolic fantasy world in which male vet gets paid in slices of cake still informs expectations of profession, say vet leaders
The public perception of vets is rooted in romanticised James Herriot fiction rather than the commercial realities of modern day practice, say vet leaders, in this week’s issue of the Vet Record .
The popular and much loved James Herriot novels, which were also televised in the 1970s and 1980s, depict a bucolic fantasy world in which a male vet gets paid in slices of cake--a misguided image that still informs expectations of the profession today, they say.
Herriot, the nom de plume of real life Yorkshire vet Alf Wight, practised in the 1940s and 1950s. He was often portrayed as working long hours, doing favours for clients for free, and with scarcely any mention of how he made ends meet.
Speaking to Vet Record about Herriot’s legacy, Henry Tremaine, a specialist in equine surgery and dentistry, said: “The nostalgic thing is of this romantic life driving around in an old car being appreciated by the clients - but actually the reality is working very long hours in stressful conditions with poor reward, being poorly equipped, and with unappreciative clients.”
He added: “That’s being consigned to history - gradually - but I think the public still cling onto the notion that that’s what a vet’s life is.”
His comments echo those of British Small Animal Veterinary Association president, Sue Patterson, who earlier this year blamed James Herriot for the assumption among some clients that vets’ love of animals would make them prepared to work for nothing.
“I think James Herriot is to blame because we’re all supposed to love animals and work for nothing, but we all run businesses,” she pointed out.
And at the British Equine Veterinary Association (BEVA) Congress earlier this month, another vet, who graduated in 1992, criticised the Herriot legacy for making it harder for vets to achieve a good work-life balance.
“We’ve been left in that Herriot mentality, and it was a nightmare,” said equine vet and congress speaker, Ben Mayes. He didn’t want the next generation of vets to suffer the same fate, he said.
A series of six case studies in this week’s issue show just how outdated the Herriot depiction of a vet’s life is, although “there is still clearly some way to go before it [the profession] is truly representative of the client population it serves,” acknowledges Vet Record senior reporter, Josh Loeb, who spoke to all the vets featured in the series.
The case studies, which reflect vets who have pursued their careers through non-traditional routes, include Peter Harlech Jones. He was the British Veterinary Association’s (BVA) first openly gay president and the first head of the veterinary unit at the medicines regulator, the European Medicines Agency.
Daniella Dos Santos, the BVA’s new, and youngest ever president, grew up in a working class immigrant family in inner city London and had to fund her own studies.
Enrique Vega uprooted from his native Spain to work in England. He now sits on the Veterinary Products Committee and is a member of the Veterinary Public Health Association’s Council.
“James Herriot continues to inspire vets and future vets, and we know from our own research that he along with other vets in literature is still very popular across the profession,” comments Daniella Dos Santos.
“At the same time, the profession is very different to what was depicted in the age of Herriot and it continues to undergo significant change,” she says. “We need to make sure that there is a diverse range of role models in place that reflect modern demographics and modern ways of working while continuing to inspire future generations of vets.”
Adele waters, Vet Record editor, added: “James Herriot may be a popular cultural figure, but he is 70 years out of date and we should retire him gracefully. With 60 per cent of UK vets being female, Herriot is no longer representative of the modern working vet, and today we should really be talking about Jane Herriot instead.” [Ends] 20/09/2019
Notes for editors News: Vets labouring under legacy of bygone era Feature: Herriot is no longer the face of the profession News: Herriot’s way not fit for modern practice
BMJ Expert Media Panel
If you are a journalist needing to speak to an expert, please click here.
BMJ IN THE NEWS
Latest coverage of BMJ in the national and international media
JOIN OUR MEDIA LIST
If you are a journalist who would like to receive our press releases, please provide your details.
CONTACT OUR MEDIA RELATIONS TEAM
Email the UK media relations team for more information.
James Herriot.org
Making Flop-bott a Household Word Since 2002
Category: Chapter Summaries
Every living thing chapter summaries.
Chapter 1 James Herriot reminisces about the cold winter days in Yorkshire. He treats a horse with a new medicine and supplements it with an older type, just to help. Instead, the horse collapses, and he and the owner both worry that the horse has died. Herriot fears he added one medicine too many, but just then the horse regains his footing, and the spots he was suffering from are nearly gone. Herriot learns a lesson about using too much technology when the new drugs are more effective.
Chapter 2 Every sense heightened by his near-loss of the lovely horse, Herriot notices everything around him more fully. He walks in heather with his dog, wondering anew at the countryside where he works, with all of its wonders and natural beauty. Sadly, he has to head along to his other farm calls for the day. Herriot treats a dog who has been eating the chips from fish and chips, which is what his owner always feeds him. When Herriot has found a medication to help him, he realizes that the tender beef they keep to hide pills in doesn’t tempt this dog. So, he writes the prescription order for the meds to be given with chips.
Chapter 3 Herriot has just endured three nights of lambing, and is feeling the effects. He heads to the local confectioner for some cough drops, and enjoys watching the way the man interacts with his candies and with his customers. The confectioner’s cat sits on the counter and is as much a part of the show as the owner of the shop. When the cat takes ill, Herriot is sad to see that it affects the owner as well. He loses weight, and his banter with his customers. After Herriot heals the cat, the owner is soon himself once again.
Chapter 4 Herriot gets a newer vehicle since his Austin can’t be driven anymore, and this brings some of his less charitable clients to accuse him of overcharging them, to be able to afford a newer car. Herriot never overcharges people, and even treats some animals without pay, so these taunts affect him. His spirits are lifted when he visits his “nephewâ€, Tricki-Woo, a Pekingese whose owner dotes on him. They talk about a new Chinese restaurant in Darrowby, and Herriot determines to visit it more often, since it’s just a small, new business.
Chapter 5 Tricki-Woo’s owner has given Herriot a suit that her late husband had ordered, but Herriot and his wife laugh when he tries it on, since the man was obviously much bigger than he. They decide to try and have it altered, since it’s a very expensive suit. Herriot delivers a difficult calf, using an epidural to slow the cow from pushing so hard, so that he can get a hand in to get the calf’s legs. As he drives away from the farm, he recalls how much more difficult the farmer’s life is than his.
Chapter 6 Herriot is speaking to the local dairy board on behalf of a farmer friend, who wants his dairy TB-test license. He wears his newly-altered suit, and sweats the whole way to the meeting, and during the meeting’s first two hours until it’s his turn to speak. The committee enthusiastically agrees to the license, and mentions after he leaves how dapper he looked.
Chapter 7 Herriot recalls farm visits with his then-young son Jimmy along as his helper. Jimmy doesn’t get in the way, and shines the flashlight beam right where it is needed. His daughter Rosie is the self-appointed gate-opener, which saves Herriot a lot of work. They both take their jobs seriously. Jimmy even second-guesses his father about a possible case of mastitis, and Herriot is embarrassed that his son is right, but pleased, too. Jimmy disappears after school one day, and everyone is worried until they find him in farmer Suggett’s barn, where he has just learned to milk a cow. Herriot looks on his children now, and Jimmy is a vet, and Rosie is a doctor. He ponders that she could have been a good vet, too.
Chapter 8 Herriot is called dishonest in this chapter, and he is stunned by the statement. He has always tried to do his honest best. A veterinarian from a nearby town thinks that Herriot and Farnon are stealing his clients, when actually they only do what is asked, and always talk to him when a client of his shows up at their office. Things look worse when that veterinarian is out of town and his prized hunter colic’s. Siegfried and James cure the horse, but are worried what will happen when the other veterinarian finds out. But they needn’t have worried. The veterinarian is thankful for their help and even invites them to dinner.
Chapter 9 Herriot recalls a woman and her dog, and she always thought something was wrong with the dog. He was the healthiest dog one could want, but she always found something she thought was wrong, and the vets at Skeldale House gave him shots or vitamins to make his owner feel better. One night, Herriot has been ill and is in a delusional state when this woman comes into surgery. He tells her there is nothing wrong with her dog and there hasn’t been anything wrong with him for all her visits. She is quite shocked. He fears after he is himself again, that she will file charges, but instead she thanks him for explaining that she had been pestering the practice for unneeded services.
Chapter 10 John Crooks, who has helped at the practice before, has been hired as a full-time assistant. Herriot worries about him, but as it turns out, he is a splendid veterinarian, good with the animals and very confident and cool with the clients, as well. As much as Herriot is happy for John, he knows he is bound for bigger and better things.
Chapter 11 John introduces Herriot to his girlfriend Heather, whom he will ask to be his wife. She lives in his home town of Beverley. One day shortly after that, John is on a farm call and gets word that Heather is sick. His vehicle is stuck, so he gets a ride to the train station and leaves to be with her. Happily, her illness is not serious. Herriot realizes that John is a man who makes decisions quickly and correctly. John will eventually become the President of the British Veterinary Association.
Chapter 12 Herriot is determined to get a smaller place to live for himself, Helen and the kids. Skeldale House is too damp and drafty, and there is too much work to be done to keep it up. He feels badly that Helen has to do that. He meets a widow who is selling her house, but it goes to auction, and Herriot bids 1000 pounds more than he can afford, and still doesn’t get the house for Helen. But he finds out it wasn’t all a lost cause, since the widow appreciates the additional funds the auction brought to her.
Chapter 13 Mr. Dowson is a vet’s best friend. He thinks every medication that Herriot has used has been like a magic potion, that instantly has restored his animals to good health. His newest case is a calf that keeps knocking over the milk bucket instead of drinking. Herriot doesn’t want to leave the man with no hope of ridding the calf of the habit, so he gives the calf a shot and the calf no longer knocks his bucket over. Another miracle for Herriot, or at least Mr. Dowson thinks so.
Chapter 14 Old Dick Fawcett has no one in the world except his cat, “Friskâ€. The cat has brought laughter into a sad house. Fawcett brings the cat into the surgery, feeling he is dead, or near dead. Herriot finds a heartbeat, and gives the cat a stimulant. The next day the cat is fine, but every other day he collapses again. As it turns out, the cat has been licking the saucer of medications that Mr. Fawcett is taking for late stage cancer. Herriot sees Frisk and his owner in the man’s bed and the man is calling the cat’s name softly. Dick Fawcett dies later that day.
Chapter 15 Calum Buchanan arrives at the Darrowby train station for his new job as assistant veterinarian with his pets – a massive dog and a badger. They get quite a few looks, as one might imagine. They’re not sure what to think of him, so when they get a call in for someone to help with a calving, Siegfried sends Calum to the farm. After a few hours, he and Herriot start to worry, but Calum returns and tells them he did a successful Caesarean section. They check the farm, to be sure, and the cow is neatly stitched and the calf looks fat and happy. They still think Calum is odd, but there is no doubt that he is a good veterinarian, so far.
Chapter 16 Mrs. Coates brings a big dog into surgery to have his anal glands cleaned out, and Herriot thinks the dog is not objecting to the procedure, because his tail is wagging. But the dog comes at him with teeth bared, and Herriot is quite surprised that he would come so close to a successful attack while wagging his tail. Later, worried about robbers in Mrs. Coates’ neighborhood, he visits she and her dog Wolfie at home. As it turns out, someone did try to rob her – but Wolfie attacked one of the men and chased them away.
Chapter 17 Herriot works on a Clydesdale with a hoof abscess in this chapter. The horse kicks and bites at him, so he decides to bring back the blacksmith to help, since the horse is shod. Herriot picks up Denny, the farrier, and tries to warn him about the ill-mannered horse. Denny is afraid of the farmers’ dogs, but he catches the Clydesdale’s foot, and uses the hoof knife to pare away until he has drained the abscess. They head along to the next farm, where Denny worries about bad dogs again, even though he has no trouble with horses.
Chapter 18 Herriot and Calum head to a bar after a farm call, but Calum’s pet badger brings pandemonium to the place. Calum also meets the Herriot family, including Dinah, their overweight beagle. Dinah likes Calum right away, as Herriot is to learn most animals do. Calum plays their piano and harmonica, and their concertina. Marilyn the badger gets chimney soot all over the Herriot’s furniture, so even while the children had enjoyed her, Herriot isn’t sure about Calum and the badger.
Chapter 19 Herriot recalls the tailor, Mr. Bendelow, in this chapter. The man speaks more than he stitches, and the customer he is speaking to left her coat at his shop three months ago and it still isn’t done. Herriot just has some pants he wants fixed, as they are frayed at the bottom. Mr. Bendelow talks Herriot’s ears off, but doesn’t look at the pants to be fixed. An irate customer comes in, but the tailor’s big dog keeps him at bay. The dog is seen at the surgery soon afterward, but the pants are still not done. The man is quite a talker, but not so much a tailor.
Chapter 20 Herriot is called out to a lambing in the middle of the night. It’s cold, and he doesn’t want to go out. The ewe is out in a field, and the one lamb inside is very large. He delivers the big lamb and washes up. He gets to be home to eat breakfast, but then has to go out to remove a cow’s afterbirth. Each of these procedures involves soaping up the arms, and his arms are nearly raw from the scrubbing and the cold. At the Birrell farm, however, the grandmother takes care of him, with expensive soap and fluffy towels. The grandmother has passed away now, though. As it turns out, she has trained her grand-daughter to do the same thing for Herriot.
Chapter 21 Herriot remembers the day his partially-built house blew down. He had bid on another house for Helen, still feeling badly about her keeping up with all the chores at Skeldale House, but the bidding once again went too high for his budget. He and Helen design a house, but progress is slow. The house is rebuilt after the wind storm, and they have the house of their dreams.
Chapter 22 Calum has bought a badger friend for Marilyn, and he has the run of Skeldale House. Siegfried is not pleased, but is interrupted by a farm call for a horse. Calum and Herriot work on a ewe with ringwomb. Calum sees a cage of cats when they finish, and wonders why they are being sent to another vet to be spayed. Calum tries to spay a cat and can’t find the uterus, and Herriot is called away on an emergency farm call. Calum spays three cats while no one is watching, and then more are admitted, and he calls Herriot to watch, but cannot find the uterus once again. The piece of tissue he keeps grabbing is nick-named Herriot’s duct.
Chapter 23 Herriot is pondering the changes in their new home, and not missing the drafty cold of Skeldale House. The kids are enjoying playing practical jokes on their dad. Yet he remembers more fond things about Skeldale House, too, the times with Tristan and Siegfried. James wonders if they will ever be as happy as in their days at Skeldale.
Chapter 24 People are starting to ask for Calum when they call into the practice, in this chapter. He is a good vet, just as John Crooks was. Calum is harder to keep track of, though, and Herriot needs to know when he is available between farm calls. Calum begins to call in, asking permission to eat, and that becomes a standing line at the practice.
Chapter 25 Herriot is planning to build a grass tennis court in his back yard for the children, and for he and Helen. He buys a bunch of netting from a retiring fishermen. Helen fears that he has been taken in, and sure enough, there are many large holes in the netting. Herriot looks for other ways to spruce up the back yard, and he orders some protective cloches for the plants. These arrive in a small envelope, and look to be worthless. Helen arranges to buy a rug of dubious origin, and says that the seller is on his way back, to see James. Now James has something to keep over Helen, because the rug is a fake.
Chapter 26 Herriot speaks in this chapter about Bouncer, a border collie who is a true gamesman. His owner is a bit of an exaggerator. Later, Bouncer has taken ill, and Herriot is shocked by his appearance. Bouncer has diabetes. Herriot gives Bouncer shots of insulin to stabilize him, and he begins to look a bit more like himself. He will get better. And, as it turns out, Bouncer’s owner does know nearly as many famous cricket players as he has always said.
Chapter 27 Herriot believes that most of his clients see him as capable, but not brilliant. And he is relatively sure that at least one client thinks he’s not right in the head. The Hardwicks are that family. He has taken their father’s eyeglasses by accident, and locked his keys in his car at their farm, among other things. In addition, he asks the farmers to get extra help to slip a cow’s hip back into place, and she does it herself when she rolls over.
Chapter 28 Herriot helps with medications for an elderly man’s equally elderly dog. While he is there, he gets the man’s television to show a proper picture. When the man calls him back three days later, he is afraid the old dog has died. Instead, the man needs help with his television again.
Chapter 29 Herriot meets Farmer Whitehead’s new hand, a young man named Basil. Herriot is checking a lame cow for Whitehead. He cleans out the cow’s abscess, and Basil invites him in to wash up. Herriot notices that Basil does things differently than most barn hands. He is elegant and graceful, but not too much like the average farmer. Herriot checks on some of Whitehead’s calves that have the scours. He leaves medication for them, but they don’t look any better on his next visit. After an overnight snow, Herriot stops in, and there are no tracks in the snow outside the barns at Whitehead’s farm. Basil has not given the calves their medications. Later, Herriot and Helen travel to Brawton, where Basil is now working as a waiter, and he seems much more at home.
Chapter 30 Calum asks Herriot if he would like to do some nature-walking with him. Herriot knows he doesn’t know as much about the flora and fauna of the area as he should. Herriot doesn’t know that accepting Calum’s invitation will mean riding bareback draft horses to the lookout site. They would see many deer, after Herriot bangs his leg on a gate post. Afterwards, Calum invites Herriot to dinner, which is a not-fully-plucked duck. It has been a Calum day.
Chapter 31 Herriot and Siegfried head out to call on a local man’s horse and an ailing calf. William Hawley has a sick calf, but Siegfried is his hero, so he has hope that all will be well. Siegfried asks for a length of string, and the farmer thinks it’s to help cure the calf. Instead, it’s for Siegfried’s coat. He injects the calf with a B-vitamin for a brain anomaly, and the calf is better the next day. Herriot thinks that the farmer wistfully wishes that the string had been part of the cure, so it would have been more magical.
Chapter 32 Herriot visits Siegfried at his home in the evening after a farm call nearby. They talk about televisions and the farmers of the area. Siegfried points out a few things that Herriot has forgotten to attend to of late. This is ironic, because Siegfried forgets more things than anyone Herriot knows. In fact, as they speak, the phone rings, and it is someone who is waiting for Siegfried, at a speaking engagement that Siegfried has missed.
Chapter 33 Calum wants to bring another dog to his flat, and Siegfried is upset, since the man already has two badgers and a dog now. Finally, Siegfried breaks down and says that it’s alright for Calum to get another dog, from his mother’s house. Instead, Calum has two more dogs when Siegfried next sees him. The Dobermans block Siegfried in the outhouse when he needs the loo in a hurry, and Calum has to call them off. Herriot feels guilty, because he helped talk Siegfried into letting Calum bring in “one†more dog.
Chapter 34 Herriot prepares to head out to see a sick calf and a dog who is ill. The Labrador is in a basket and the family completely ignores him as they watch the television. The dog has mange, and Herriot gives the medication to the father. Herriot leaves for the Farrow’s farm, to check their calf. He injects the calf and the farmer wraps the calf’s chest to keep him warm. Herriot feels good for the future health of the calf, but worries about the dog, that he won’t get his proper treatments. Herriot visits the dog’s home, and the family has done no treatments on their poor dog. Herriot treats the dog himself, as a neighbor watches, and the next Monday, the neighbor is giving the dog his medicinal bath. As it turns out, the neighbor has taken on the dog, by convincing the original owners that his vet bills will be high. A few weeks later, Herriot sees Jet, the dog, with his new owners, and his coat is healthy and shiny.
Chapter 35 Mr. Busby calls Herriot out to work on his cow, and is upset when Herriot is delayed at surgery working on a dog. He feels that the cow is his livelihood, and is more important than a pet. A few weeks later, Helen gives James a message from a client that is bringing in a dog, but he has an emergency farm call for a bull, which he attends to first. When he comes back, the client in his office with a dog is Mr. Busby, who is now chastising Herriot for dealing with farm stock before pets.
Chapter 36 Herriot receives a call from the police about a possible robber, but he knows it’s just Bernard, the younger brother of a sister who runs a farm outside Darrowby. He is always being berated by his sister, and he is not really from farmer stock. When he has to assist with anything that smells, he puts on a bandana. The veterinarians at Skeldale House have taken to calling him Cisco Kid, and that’s who the police thought was a robber.
Chapter 37 Herriot muses that sometimes he works figurative miracles at some farms, with little acknowledgment or appreciation. At one farm, he constantly has excellent luck with bringing animals back to health, but the barn hands never even look at him. One day, he happens to take out his winnings from the football pool, which he occasionally bets on successfully. Suddenly the barn hands are all ears, and he does several coupons for them, and they all win. He tells them he won’t do that anymore, but he does win over 77 pounds on the pool, and he tells Siegfried that if he’d only had one more draw, he would have won sixteen thousand pounds. Siegfried spreads the rumor that Herriot won sixteen thousand pounds, and suddenly all the barn hands look at him with what he feels he earns at his job – respect.
Chapter 38 Herriot is having trouble with a calving, but can’t quite reach as far into the heifer as he needs to. He recalls that Calum is at a neighboring farm, and they call him over. He and Herriot work on the calf together, with no initial luck. While they rest, Calum tells Herriot that he is getting married soon. They deliver the calf, and Herriot gets to meet Calum’s fiance, but there will be no public wedding. They are married in a private ceremony. They have a brief honeymoon, and Herriot thinks that the new wife would make Calum’s quarters less spartan, but she doesn’t. She is exactly in tune with him, and that is with nature and the outdoors.
Chapter 39 Calum acquires another badger named Bill in this chapter. He conveniently doesn’t tell Siegfried. Siegfried asks Calum to release an owl that Calum has worked on, since it has regained its health. There is also a family of foxes living in Skeldale House. Then it turns out that he is also babysitting a monkey while his owner is on holiday. Later, Herriot walks in on Calum and his zoo of animals. In addition, Calum tells Herriot that his Doberman is pregnant. Herriot knows this will not be a good thing for Siegfried, since it looks like all the animals will be staying.
Chapter 40 Herriot discovers an igloo-type shelter by the gate of a farm where he is to do some TB testing. A man and his cat come from the shelter, greet Herriot, and head off walking toward town. He tells the farmer what he has seen, and the farmer says that he’s met Eugene, then. He’s been living there for some time, and Herriot has only just now visited the farm, so he hasn’t seen him before. He is the brother of a millionaire. A few days later, Herriot returns to check the TB test results, and Eugene is sitting in a chair outside his structure. His cat makes friends with Herriot. Herriot is a cat lover, and it appears that the cat can sense this. Herriot accepts an invitation to tea, after checking the TB tests. They have tea in the igloo, for lack of a better term. From then on, Herriot visits Eugene whenever he goes to the Carless farm. He talks to Eugene about having Emily the cat spayed, since she may encounter Tom cats in her wanderings. Eugene is worried about his cat having an operation. Next time Herriot visits, though, the cat is already pregnant. Herriot sees someone he thinks is Eugene at a formal meeting not long afterward, and he is surprised at the man’s elegant dress. As it turns out, it is the millionaire brother he sees. Later, Herriot sees that Emily the cat is having a hard time delivering her kittens, so he takes her to the surgery. As it turns out, she is only having one huge kitten. Herriot realizes that it will be difficult for Eugene to make his usual rounds with two cats, and he has found a home for the kitten, which Eugene accepts.
Chapter 41 Nat Briggs is accidentally stuck with Herriot’s vaccine needle, and the other farm help are having a good laugh about it. Nat worries about having gotten some of the vaccine, but he didn’t. He complains about the event during subsequent visits by Herriot to the farm where they work. Later on, Nat tells Herriot that the vaccine (which he didn’t get any of) is preventing he and his wife from becoming pregnant. On a later farm call, the other workers, or the movements of the animal they are wrestling with, put Briggs on the business end of a needle again. The joke, after Nat and his wife are expecting, is that the second shot was the antidote for the first one.
Chapter 42 Siegfried tells Herriot about a house coming up for sale outside Darrowby. Herriot has always liked to think about living in a tiny village in the countryside. Hannerly is a quiet, very small town with no pubs or street lights. Herriot and Helen visit the house and enjoy relaxing in the grass by the brook. They buy the house, and enjoy living like they are on the edge of the “real†world.
Chapter 43 Herriot and Albert Budd have been roped into Calum’s Highland dance class, and they are exhausted – and Albert is gassy. The dances are fun to learn or re-learn, and Albert is pulled back to the floor for another dance. Herriot reflects that Calum has brought many changes to the town, including the dancing that is presently not going well for Albert.
Chapter 44 Helen puts out some milk and food for a stray cat and her kittens, at their new house in Hannerly. They watch, and it appears that the mother is a feral cat, and she won’t allow her kittens to come to the porch – she grabs the food and takes it back to them. They make their new home in the log shed, but a few days later, the mother cat disappears. The kittens are accepting of the food and milk. Herbert Platt, a local dustman, comes to visit and says he has known the family of cats for a long time, and they won’t be domesticated. Herriot wants to alter the animals, so they won’t be breeding more feral cats. He catches them in a cat cage, and takes them to surgery. The cats struggle, but don’t scratch or bite, like even some of their domestic cats do in surgery. He lets them loose back at home after they have recovered. Eventually, Helen can pet them as they eat, but they won’t come inside, regardless of the weather. They will disappear for a few days at a time, but once they are gone for a week, and the Herriots think they have lost them. When the cats return, they are sick. Helen calls to them and they come right into the kitchen. Herriot gets drugs from the boot of his car, and treats them, but they don’t want to stay in the house. They allow themselves to be treated, though, and when they feel better, James has to put medication in their food, since they aren’t fully recovered yet. When they are fully recovered, they will no longer let James handle them.
Chapter 45 Siegfried wants Herriot to go home from the surgery, since Herriot is sick. Siegfried tells Herriot that he cannot work, but that he can ride along with Calum on his rounds if he wants to. They have to walk a long way at their first farm, and Herriot introduces the farmer to Calum. The farmer Mr. Stott, thinks he is always right about everything. Calum asks the farmer what the sick cow’s symptoms are. The farmer rattles off some, and watches as Calum soaps up and inserts his arm into vagina and then rectum, but can’t find nothing wrong. Turns out that cow isn’t the one that was sick, and the farmer gets a good laugh. Calum keeps laughing, and then heads to the cow who is sick. He makes up symptoms and tells the farmer it will take two veterinarians and a great deal of money to cure her. The farmer is upset, and then Calum tells him it was all a joke, since he knows how much the farmer likes a good joke.
Chapter 46 The Herriot’s “wild†cats are becoming more tame, but not toward James. Olly has long hair, and it gets matted, since he can’t be caught to be combed. He won’t let Helen trim his knots, either. Herriot drugs Olly’s food to anesthetize him, but he has to watch everywhere the cat walks, so that he won’t be sedated somewhere in the wild, where a predator could get at him. The cat isn’t completely drugged, and watches James as he clips the knots out. The cat looks better, but when he sees James the next morning, he runs away from their food.
Chapter 47 Herriot is checking out a little dog that looks very afraid, and is shaking. The dog has a 105 temperature but no other symptoms. Herriot gives the dog a shot of an antibiotic, glad to be able to help, and sends the owner home with pills. The next day, he rechecks the dog and Robbie is no better. His temperature was still 105. A urine test also shows nothing. More tests, a different antibiotic and Robbie is no better. Herriot gives the dog a shot of dexamethasone and the dog is more himself the same afternoon. But a month later, Robbie has the same symptoms again. He treats him until he is better, but this same scenario plays out over years. Finally, the attacks worsen, and Robbie’s owner asks Herriot to put the dog down. He does as she asks, and she pats Robbie’s fur. Herriot’s memories of Robbie will not leave him. Molly, Robbie’s owner, dies only a few weeks after the dog did. Herriot has a bad day shortly afterward, when all the farmers he visits seem to be calling him a failure. He mentions his feelings to Helen, and she brings in something that has been recovered at Molly’s home sale. It is a framed photograph with “My Favorite Men†written across the top. In the photo are John Wayne, Sir Charles Armitage and James Herriot.
Chapter 48 Herriot is called to the cottage of the Colwells, and the gas man, who is leaving, tells him that the family has fleas, on his way off the porch. Herriot thinks the man is daft, but he seems happy enough. He enters the house to see the family’s dog Roopy, who has been hit by a van. There is dust thick everywhere, and the house seems in disarray. The dog has no broken bones, but some acute discomfort, so Herriot gives him a shot for pain and an antibiotic. Mrs Colwell invites Herriot to stay for tea, and he does. When he gets back in the car, he feels prickles around his ankles. The gas man wasn’t daft, after all. He rushes home for a bath, and has Helen throw his clothes in the washer. They head out for their afternoon together, but James is feeling like he has fleas again, and it distracts him during their lunch. Surely enough, several fleas land on the tablecloth from his collar, and they finish, quickly pay and head out. They are going to be attending a concert with friends, so James bathes again and puts on a different suit. In the concert hall, he feels a flea once more. He is fairly sure there is only one, as he sits between their guests, and he tries to squash it, but draws their attention, since they are seated on either side of him. He makes it through the night, but a few days later, the Colwell’s call for him to clip a snagged nail on Roopy’s paw. He can’t get out of it, so he plans to go by a bicyclist’s house first, to get clips for his trousers.
Chapter 49 Sister Rose has a terrier that Herriot is checking over. She takes in dogs whose owners have dumped them. Herriot feels rage for those people and pity for the dogs. He is at Sister Rose’s to check on the animals, and give them their required shots. The terrier has a broken hind leg that was never set, and he trembles when Herriot and Sister Rose speak. He is emaciated and needs love. Another dog has an infected foot. A man walks down the rows of cages. Herriot knows the man, a grocer who used to bring his dog in for routine treatment, until it died a few days back. Rupe, the grocer, is having trouble deciding on which one dog to take home. Herriot reassures him that Sister Rose won’t put down any unadopted animals – hers is a no-kill shelter. He seems to fancy the terrier that they have just been working on. The grocer and his dog arrive at Skeldale House a week later for inoculations. The terrier, Tritch, no longer looks emaciated and is no longer afraid of everything. The grocer would like Herriot to fix the little dog’s leg, if he can. Calum will help, as he appreciates new methods of surgery. Tritch’s leg heals nicely, but he still won’t bear any weight on it. Later, they travel to see the grocer’s induction as the mayor, and he has the little dog beside him, happily trotting on all four legs. Calum smiles at Herriot. Sometimes you win.
Chapter 50 Herriot heads into a bar, The Lord Nelson Inn, to get a drink, passing Bob Stockdale at the bar. The inn used to be a quiet place where few gentlemen sat and drank, but now it is a raucous and busy place. Bob Stockdale still frequents the bar, and sits with his dog Meg. The dog is his cattle dog, and she is aging. They drink together for a bit, and Herriot watches Bob’s show as he tries to get on his bicycle after having too much to drink. Herriot sees Bob at the bar a few months later, but Meg isn’t with him. Herriot asks why not, and is told that she has cancer. He hasn’t consulted a vet, because he doesn’t want her put down, but she has a growth. Herriot explains that not all growths are cancerous. Herriot goes to Bob’s house, that he shares with his brother Adam, and checks Meg. He is reasonably sure he can remove the growth, and that it’s not cancerous. Bob doesn’t want to bring her in, so Herriot tells him that he can do the surgery there in Bob’s house. Bob can’t watch, once the surgery starts, but his brother helps. The tumor is removed and they share a cup of tea, Bob still a bit queasy from all the blood. Herriot sees Bob – and Meg – a month later, and both are themselves once more.
Chapter 51 Calum is ready to head on to a new place to work, in Nova Scotia. It has a lot of desolated country, just the type of place Herriot feels that Calum will like. Siegfried bids Calum a fond farewell, too, but as they speak, a heron walks past in the hall. Once Calum leaves, the surgery is a quiet place, with none of his menagerie there. Calum opens an auction mart in addition to his veterinary practice, and trains Border Collies. He has six children, and still decides to leave his new practice, and move to Papua, New Guinea. He adds to his menagerie there, and soon has more animals than he did at Skeldale House.
Chapter 52 Herriot still cannot get their stray cats to come to him, as Helen can. And he needs to trim Olly’s matted hair again. He catches him by hiding behind Helen when she feeds them. He and Siegfried work to remove the mats after they anesthetize the cat. The next day, Olly looks even better than his sister Ginny. But he flees at the first sight of Herriot. This weighs on Herriot, since his life is devoted to helping animals. Helen explains that they only see him when something they perceive as bad is going to happen, so he helps with the feeding and brings them milk. One day he is able to gently pet Olly on his chin. But sadly, less than two days later, Olly dies. It is perhaps a stroke, or some other brain problem. Ginny will not eat for days and it is obvious that she misses Olly as much or more than Helen and James do. It takes months for Ginny to befriend James as Olly had, since she was always more skittish. But it finally happens, and Herriot regards it as one of his greatest triumphs.
The Lord God Made Them All Chapter Summaries
Chapter 1 James Herriot is happy to be home from war, but he remembers some of the harder times he has spent in his veterinary practice, too, like the gates (seven of them) at a local farmer’s spread. The last gate gets him every time, and it’s no different now. The farmer promises to set appointments for castrating his bulls when they are younger and to fix the gate, but of course nothing was done the whole time Herriot was off to war.
Chapter 2 This chapter tells the story of an older man who dotes on his precious dog, but feels guilty when he goes off drinking at the track one day a week, and calls Herriot in the wee hours of Sunday mornings. There is never anything wrong with his dog, but Herriot always gives her a vitamin so that the farmer believes something needed to be done. When Herriot finally refuses to go out on an early Sunday morning, he realizes that the dog is sick, and he flies to the farm, where the dog has eclampsia. He is able to save her.
Chapter 3 Herriot relaxes by the side of the road, remembering the dells fondly, and overlooking the landscape he missed so much when he was off at war. Many things have changed for veterinary medicine, but he is happy to see that the dales have not changed. He misses the times when he had to do more than poke animals with a needle to treat them, but he admits to himself that he appreciates being able to cure more animals than he used to be able to.
Chapter 4 Herriot heads for Russia, on a trip everyone has advised him not to go on. He is taking care of expensive sheep on the journey, and he marvels at their health and vigor, even on a moving ship. He is worried that the ship is not larger, but all in all, he is excited about the journey ahead of him.
Chapter 5 Herriot remembers his then-young son in this chapter, and how he always wanted to go on farm calls with his father. Helen Herriot bought him real boots like the farmers of the day wore, and he could not have been more pleased. Herriot also has memories about one day when he was working on removing a thorn from an animal’s paw, and he saw his son outside the window, climbing the wisteria, which he had been forbidden to do. Eventually, his son climbed higher, than hung upside down, and then fell. Fortunately, he was not seriously injured.
Chapter 6 Mongolian Russians who helped Herriot on his rounds are the subject of this chapter. These men were taken prisoner during the war, but they were good workers and treated well by the farmers where they were living after the war. One of them actually catches a bull and holds him by the ear, so that he can be worked on. Neither Siegfried nor Herriot has even been able to do that, although they have tried.
Chapter 7 Herriot speaks again about his trip to Russia in this chapter. He treats a couple minor injuries in the sheep, but worries that they may have husk. He is afraid that his meals, meanwhile, will be small, after he sees the tiny galley, but actually he is served chef-quality foods.
Chapter 8 In this chapter, Herriot works with a student, who leads him to believe he knows how to do a c-section on a cow in hard labor. He cuts into one of the stomachs instead of the uterus, and Herriot fears that the animal will die, since it took so long to get her organs back in, and since they might become infected. However, the cow is fine, and has eight more calves over time. Herriot berates the student when he learns that he doesn’t know the operation, but later apologizes.
Chapter 9 Herriot speaks in his journal about one of his days onboard the ship to Russia. The crew member, Raun, who has been helping him recalls that cattle died on one trip since there was no vet along to help them. Herriot and Raun check on the sheep with the wounded hoof, and isolate it in a separate pen. Herriot hopes he will be able to earn his wages for the trip by taking good care of the sheep.
Chapter 10 In this chapter, Herriot uses a new medication to treat foul of the foot in cattle. It is injected into the neck, and old-time farmers are hard to convince that a shot in their cow’s neck will fix a foul foot problem. In one animal, a clot develops at the injection site, and the cow dies. Still, the farmer calls him out for another sick cow, and he is able to help that cow back to health.
Chapter 11 Herriot talks about a client of their veterinary practice in this chapter. She sends her goat droppings to be examined by whichever vet she has taken a shine to on that day. It’s a humorous chapter, but Herriot talks about the lady in a way such that it doesn’t seem he is making fun of her.
Chapter 12 Herriot remembers his Russian trip once more. The seas are rough and his wards, the sheep, are sick. Herriot realizes that they are ill from the stress of the trip, and he injects them with prednisone. The sheep recover, and Herriot recalls that some of the new ways of practicing veterinary medicine are a positive thing for veterinarians
Chapter 13 Herriot talks about the town barber in this chapter. He gives proper cuts in his barber shop, but when he is drunk on the weekend, he gives free – and very bad – haircuts. Herriot meets Josh’s new dog, who has a chicken bone stuck in his throat. He gets the bone out while the dog is under anesthesia, but the dog’s breathing stops and Herriot has to whirl him around to restart his breathing, and it works. When Josh comes back, he mentions the dog probably felt like he was flying, which puzzles Herriot, since Josh wasn’t there during the surgery. He recalls that people say Josh can read your mind when he runs your hair through his fingers, so Herriot makes a mental note not to think about the incident when he gets his hair cut.
Chapter 14 Herriot tells the reader more about his trip to Russia. The ship docks, and he introduces us to the Russians who check the sheep feed to make sure it’s alright. He also talks about the lady who takes each sheep’s temperature, which takes an entire five hours. Then he recounts how he and the captain are almost attacked by guard dogs, trying to find a short cut to the local club.
Chapter 15 Herriot sometimes becomes too close to his patients, and one is a local Sister’s dog, named Amber. He is treating the dog, but she is not responding, and he keeps treating her anyway. When he sees how thin she has become in his headlights, he decides he must do the right thing, and needs to put her to sleep.
Chapter 16 Herriot travels out in a blizzard to try to treat a local animal. He drives as far as he can drive, and then takes off on skis. But nothing is familiar in the swirling snow, and he heads back to his vehicle, rather than to get lost. Back home, he calls the farmer and tells him how to get his pig’s milk flowing, and his plan works.
Chapter 17 Herriot tells us about the birth of his daughter Rosie in this chapter. Helen is patient and waits until the proper time for them to go to the hospital. He hears his daughter’s cries, and goes in to see her, and is appalled at how bloated she looks. It’s strange that he has seen so many animals born, yet doesn’t expect that a human birth might not be a lovely thing.
Chapter 18 Herriot’s curiosity almost gets him into trouble, in Russia. He and the captain wander into a school, because Herriot wants to see what they are like. He walks into a teachers’ meeting and is almost arrested, before the captain can explain that they are simply visitors. Herriot enjoys talking to the school’s English teacher, but he almost went to jail – something the folks in Darrowby had warned him about.
Chapter 19 We meet Mr. Biggins in this chapter. Although he is a long-time client, he lets his animals’ maladies go, until it becomes an emergency, and then calls the veterinarian A cow that Herriot is called to treat dies, since it was too far along to save, and the man wants to know why, but then complains at the cost of the testing. He also refuses to use the newer method of treatment on one cow, until Siegfried gives the cow a shot (actually just vitamins) which he tells Biggins will kill the cow if he doesn’t give her the right medication. Biggins does as told and the cow survives.
Chapter 20 Herriot writes in this chapter about two brothers who are unwittingly committing insurance fraud. They have many accidents at their farm, and they take the money that should be used to pay others do their work, and pocket it, doing the work themselves. They don’t seem to understand fraud; rather they see having accidents as a way to make money.
Chapter 21 Herriot recalls his return from Russia and high seas where the ship is sailing. Even the seasoned seamen get sick, but Herriot is fine, and he attributes this to the seafaring men in his family. On the trip, the chef makes sure he is kept fed with excellent delicacies.
Chapter 22 Herriot talks about his daughter in this chapter. He enjoys spending time with her, and taking her on calls with him. He also fondly recalls the same type of trips he made with his son, when he was younger. She came close to injury on one farm call, when an ill-behaved cow got away from the farmer, but she just stood there and said “mama†very softly, and the cow ignored her and went the other way. Rosie also worried about her dad when school started, and he didn’t have her help for farm calls anymore.
Chapter 23 Herriot remembers talking with farmers who are not at all well-read. He once made a comment about a cow with a broken leg, since he had read in the newspaper that George Bernard Shaw had broken his leg as well. The farmer ended up believing that Shaw was a friend of Herriot’s, and the veterinarian believes that there was probably an amused comment at the farmer’s dinner table that evening.
Chapter 24 Herriot talks more about his return trip from Russia in this chapter. He had wondered why the tablecloth was wet every day, and as it turns out, it’s done so that it doesn’t slide off the table when the ship rolls. He takes a pleasant exploratory walking trip while the ship is docked in Poland, and checks his return cargo of pigs, happy that they are getting along. The men are kind to him since his anniversary is celebrated while he is on board, and when he arrives home, he thinks the ship’s cook will miss him more than the others, since he was the only one who felt well enough to eat for the whole return trip.
Chapter 25 Herriot starts this chapter talking about how he wants to speak with a client about putting off calling the vet until Sunday, when the vet needs his rest that day, too. But he is drawn into the story of a little Dachshund, who is suffering from what Herriot believes is a progressive paralysis. The owner gives the dog what Herriot calls “quack†meds, but the dog recovers. Of course, the clients think their “quack†medicine healed the dog, but Herriot is more inclined to believe that the dog had a spontaneous recovery. Nevertheless, he offers a toast to the man who suggested the quack medicine, since Herriot has grown close to the family by this time.
Chapter 26 Artificial inseminations are new to the veterinary world of Herriot’s time, and he meets up with his old friend Tristan, while Herriot is trying to get sperm from a bull. Although the sessions does not go easily, Tristan handles it with his usual grace, and retrieves the device after the bull falls. Previous to this, Herriot himself was nearly trampled trying to get the sperm into the artificial vagina.
Chapter 27 Herriot introduces us to Jack Scott in this chapter. He gives all of his animals a chance, even if they appear to be too ill to recover. Scott’s dog Rip suffers two injuries to a hind leg, and the next time Herriot sees the dog, he is still herding, just on three legs. He also tells of a cow of Jack’s that walks in circles all the time. She doesn’t get better rapidly, but over a period of years, there is little trace left of her circling, and she even wins first prize at a farm show.
Chapter 28 Herriot talks about various people he has met in his work in and around Darrowby. On one farm call, a goat ate prized tomatoes, but when Herriot arrives at their house, he feels more like he has been called to referee a marital spat. Herriot tells of clients who seem to know what is wrong with their animals, and some that actually have no idea. He meets quite a variety of people in his farm calls.
Chapter 29 Herriot is excited about another trip as a ship’s vet – until he finds out that they are flying, not sailing. The plane is old, and he is afraid it won’t make the journey in one piece. As if reading his mind, the plane has an engine catch on fire. Nevertheless, they make it to Istanbul. Herriot feels that this was certainly not the leisurely trip he signed on for.
Chapter 30 Herriot remembers a piano recital his son is in, that doesn’t go well, in this chapter. The piano teacher gives him another chance at the end of the recital, since he can’t make it through his piece at his assigned time, and this time he makes it all the way through. Afterwards, Herriot finds it ironic that his son thinks music is soothing, but the recital made his father a nervous wreck.
Chapter 31 Herriot teaches us a lesson in this chapter. A crotchety old scrap metal dealer has a cat that he is fond of. Someone puts rubber bands on the cat’s leg and even his neck. The owner is worried about the cat, but it heals from these ills. Later on, the cat becomes ill with distemper, and Herriot can’t save him. The old man cries, even though he thinks this will make Herriot think less of him. Instead, Herriot understands his feelings for the cat.
Chapter 32 Herriot’s Istanbul trip continues in this chapter. He had wanted to travel, but they wait for hours to unload the cattle. There seems to be a cow # 15 not on the charter the buyers have, but eventually, they take that cow, too. On top of that, the plane needs repairs and cannot take passengers to Copenhagen, where the repairs will be done. Herriot and the crew get stuck in a lousy hotel, and end up crashing a wedding reception when they can’t find a pub. Back at the hotel, noisy partiers keep them awake all night.
Chapter 33 Dehorning is the main subject of this chapter. A friend helps Herriot dehorn bulls, and although he says he is jealous of Herriot’s freedom and outdoor job at the beginning of the day, he doesn’t envy him by the end of the day. Siegfried thinks that maybe hedge clippers will work to dehorn cattle, but doesn’t have any luck when he tries them out.
Chapter 34 We meet Brandy the Labrador Retriever in this chapter. He is forever getting into things, like getting his nose stuck in food cans in the garbage. He develops pneumonia, and although he recovers, he doesn’t act like the dog he used to be. After a period of time, though, Brandy visits Herriot at his office, and he is happy and running again, like he used to.
Chapter 35 Herriot and the crew in Istanbul decide that since he can’t write a check to British Airways, that they will sign a waiver and ride on the plane with the bad engine, to Copenhagen. They fly low, but that gives Herriot a chance to take in the view. Months later, he hears a rumor that the plane crashed in the ocean, with the loss of the crew. He doesn’t know for sure if this is true, but he clings to hopes that it’s false.
Chapter 36 Herriot recalls two terrible Westies owned by clients of their practice. The owners let the dogs do whatever they like, and the dogs have no manners. They always nip and bite at the veterinarian who is unlucky enough to be on call that day. After this pair of terrors die, the owners get two Westie pups, and they end up being the same way – until one day one of them bites their owner. Herriot thinks they may be easier to handle if the owners practice simple discipline.
Chapter 37 In this chapter, Herriot tells of a farmer who had a ragtag pen made of all sorts of materials, and many animals. He decides to raise pigs, and has a brand new piggery built. But his pigs develop swine fever, and many of them die. The remaining pigs have to be sold at lower prices. He has the piggery cleaned and tries again. This time the pipes stop up and the pigs are without water for a time. They recover, but after this second bad experience, the farmer decides not to raise pigs anymore. Now that he is a smalltime farmer again, the man is happy, like he was before he started the piggery.
Chapter 38 Herriot and Siegfried share thoughts in the final chapter of this book. They opine that these may be the best times of their lives, with their families growing up and their practice doing well. Siegfried assures Herriot that there are still good times ahead, as well.
All Things Wise and Wonderful Chapter Summaries
Chapter 1 This book begins with James Herriot, the country veterinarian, beginning his life in England’s military. He desperately wants to go home to his wife and their home. He remembers an old cow named Blossom, who was due to be sold since she was old, but she kept eluding the fatstock driver. She was quite creative in her means of escaping her inevitable fate. Her owner eventually lets her stay at his farm.
Chapter 2 In Chapter 2, Herriot remembers heading for a Lord’s manor to test his cattle for TB. The Lord liked to make a show of helping Herriot, even though, truth be told, he was actually not very much help. Later, James receives a call from the Lord about a sick pig. Herriot has tried to save pigs with this ailment, a prolapsed uterus before, and both times he has failed. This time, happily he succeeds.
Chapter 3 Chapter 3 has James remembering his terror of dentists, and the military dentist now has to work on him. He is even more scared when he learns that the military dentist is called “The Butcherâ€. When he is finally done with Herriot, after a lot of pain, Herriot is reminded of the many wolf teeth he has pulled from horses, and so he tells the military dentist that he pulls teeth the same way – on animals.
Chapter 4 In Chapter 4, Herriot hears various types of gas and other emanations from his fellow military men. It leads him to remember the gas problem that a bulldog had in their home town. The dog’s owner was petite and feminine, and couldn’t have a dog “behaving” that way. Herriot eventually paired the dog up with a man who had lost his sense of smell, and all was well.
Chapter 5 In Chapter 5, Herriot notices a policeman chasing a young street urchin, which reminds him of a boy back home. Many pranks are blamed on Wesley Binks, that young boy. One day, Wesley adopts a dog who has distemper, and takes on an actual job to pay Herriot for treatment. Sadly, the dog dies, bringing Wesley to tears. Then he goes right back to his life of mischief.
Chapter 6 James remembers Skeldale House in Chapter 6 with humor, and a time when Tristan was filling in for the housekeeper. They don’t know that there is only one dish he can cook. At the same time, James and his boss-turned-partner, Siegfried, were confused over a rash of deaths at a local cattle farm. As it turned out, the cattle were eating bits of antlers that had fallen into their feed. As Tristan prepares yet another meal of the same thing, Siegfried says he can empathize with the cattle, and heads out to eat.
Chapter 7 Chapter 7 finds Herriot reflecting on how little attention veterinarians are given, even when they are called to a farm. He especially recalls an incident where a family’s collie had swallowed a ball, and he was able to dislodge it from outside the throat, since he couldn’t reach it from the dog’s mouth. The family wrote a thank you note that began with a greeting to the vet with a bandage on his finger.
Chapter 8 Winters in Darrowby are on James’ mind, in the military. He especially remembers his first winter there, when one of his clients is dressed like he is ill-prepared for the weather, even though James is bundled up. But the client is comfortable and James is not. The farmer’s skillful, calm manner is one of James’ first indications of how much he has to learn as a veterinarian.
Chapter 9 James remembers another Christmas back home in Darrowby in Chapter 9. One particular client is the type he enjoys, since she lovingly cares for her animals and calls even with smaller concerns. A stray cat brings a kitten to live at the client’s house, and then the cat herself dies of cancer. The following Christmas, James visits her house again, and sees the little kitten, now a cat, playing with the client’s Basset Hounds.
Chapter 10 Times are especially hard for Herriot right now, since his wife is almost ready to deliver their baby, back home. He experiences queasiness, like her morning sickness, and pseudo-contractions. James goes AWOL and home to see his wife, then returns to duty. He is not one to break many rules, but he feels that Helen’s pregnancy was worth the visit.
Chapter 11 Herriot is at the lowest rank in the military. It’s a feeling he is used to, since for a long time in his practice, he would reach a farm for a vet call, only to find the owner upset that Siegfried hadn’t been the veterinarian to respond to the call. But one of the horses of such a client is choking while Herriot is there, and he realizes it’s an allergic reaction, and cures the horse with one shot. After that, the farmer respects him more.
Chapter 12 Herriot is guarding a hotel in this chapter, which he finds as humorous, since the hotel doesn’t seem to need guarding. It reminds him of a battle he had with a local man’s sheep dog, Shep. Shep leaps onto unsuspecting visitors from a hiding place in the garden, and he does so to Herriot, when the veterinarian is deep in thought. He is worried about a cow he is treating, who ends up being cured by an idea the postman has, of all people. James takes his frustration out on Shep, not allowing him to scare him, but later sees that Shep is still himself, scaring a local tinker.
Chapter 13 James goes AWOL once again in this chapter, as Helen prepares to give birth to their baby. He gets home in time to see his new son. He is unaccustomed to the look of newborn humans, and the others are amused at his reaction. He is more used to seeing animal babies. James fakes a telegram and gets more time off, to spend with Helen and their son.
Chapter 14 James remembers some of the harder parts of being a country veterinarian in this chapter. He recalls a time in a pub after a hard farm call, and how he saw another customer’s dog, who needed surgery. The patrons pitched in money and he performed the surgery on the dog, but the owner just treated the fact as though the dog’s illness had cleared up by itself.
Chapter 15 In this chapter, Herriot finds out just how not in control he is, in the RAF. The men are ordered to nail the windows shut for a bad storm, and the incidence of lung infections rises alarmingly. In addition, they have to take up shadow-boxing, to keep themselves alert and on the ready. The men feel demoralized and out of control of their own lives.
Chapter 16 Herriot remembers a sad outbreak of dog poisonings in this chapter. He feels that he needs to better the lives of the animals in his area, and purposeful injury makes him especially upset. One of the dogs that is poisoned is a seeing-eye dog, which is especially painful for Herriot. He gives it one last chance at life by using a risky drug, and this dog is the only one of the poisoned dogs who survives. Herriot is glad that if only one dog could be saved it was one who has such an important task in life.
Chapter 17 Herriot recalls an older women who was very good at not paying bills, back in Darrowby. Rumor had it that she was rich, she just didn’t pay her bills. She wants her cat spayed, and cries until James says he’ll do it for half price. They end up having to transport the difficult cat to and from the old woman’s house, and then she won’t pay until the stitches are taken out.
Chapter 18 Chapter 18 finds Herriot thinking about how the war has changed life for everyone. He is a Leading Aircraftsman now, a higher rank. The promotion has also brought with it a pay raise. As he is marching away from the Grand Hotel, he promises himself to return after the war, to see it as it should be seen.
Chapter 19 James recalls in Chapter 19 that the ways of speaking in different areas are much different. His understanding of coarse and sexual language has become more clear since he has been in the RAF. At home, it’s hard to get a farmer to explain what is the problem with an animal, if it is in any way a sexual problem. He finds it rather amusing that particularly the Methodist clients he has won’t say anything about any body part in that area, even if a cow runs into them there.
Chapter 20 In Chapter 20, Herriot remembers a time before he met Helen, when he was sent along to Hensfield so that he could cover for his former boss, Siegfried. Hensfield is a dreary, dark mill town, and the vet he is covering for generally works on animals for poor owners, for low pay. The veterinary facilities are not what he is accustomed to, and when a Golden Retriever comes in with a severed leg, Herriot has no idea how to treat the dog.
Chapter 21 In this chapter, Herriot does the best he can, with what he has available, to put the Golden Retriever’s broken body back together. He worries about infection, but does everything he can think of doing, to save the dog. He plasters the dog in a cast, in a way they did in the Spanish Civil War, when they would allow the limb to heal in its own fluids. After a week, the dog is better, and James cleans the leg and applies a new cast.
Chapter 22 In this chapter, Herriot inspects dogs at a Greyhound track. It is a low quality track, and he finds many problems with the health of the animals. This puts him on the outs with the track owner, but James won’t compromise his standards for the man. At the end of his stay, the Golden Retriever, Kim, comes back for a visit, and Herriot is happy to see how well the dog is doing.
Chapter 23 James hears a lot of shouting while on duty in the RAF, but none that compares to one farmer back in Darrowby, Len Hampson, who it is said could be heard from farms away when he shouted. James cannot save Len’s pig, but he does save his soft-spoken neighbor’s bull. Later, they all meet up at the local pub, and of course, the soft-spoken man who tells of his bull being healed is sorely drowned out by the big mouthed man whose pig died.
Chapter 24 Herriot remembers a small animal vet, Granville Bennett, who always drank him under the table, back home. James just cannot seem to get out of socializing with Bennett, and on one visit, he is so drunk that he forgets that he should not eat hot dogs, and he eats entirely too many of them. He pays for that, later on.
Chapter 25 James thinks about his successful business partnership with Siegfried Farnon, in this chapter. He feels that they work well together because they are opposites, since he is more traditional, while Siegfried likes to try new methods. However, he has noticed that Siegfried doesn’t tell him when some of his newer contraptions don’t work. Siegfried also occasionally chastises Herriot for giving away services to poor clients, even though he does at least as much of that, if not more.
Chapter 26 James helps farmers bring in their crops in this chapter. He has trouble, and he doesn’t have the skills he needs. The farmer says he just needs to learn how to do it right. Later on in the day, the farmer has trouble delivering a calf, and James helps, and has little problem with the delivery. So he learns that it isn’t a matter of brute strength at all, but of knowing the proper procedure.
Chapter 27 James heads off to flight school in this chapter. Throughout all the journeys, he sleeps a lot and dreams about Helen. During training, though, all the men are instructed to always have their ID discs with them, since this will be the only way their bodies can be identified if they happen to be shot down. That brings the war more realistically into Herriot’s mind.
Chapter 28 James is in flight school in this chapter, and his instructor is not very good with trainees. He is rough on Herriot, but no harder than Herriot was on himself, as a veterinarian. He remembers a night when there was an animal who had eaten too much fallen fruit and was in distress. Although he would have preferred to stay at home, he went out in the cold to help the animal, and in the process exposed him to the coughs and chills of the owners.
Chapter 29 In this chapter we meet one of Siegfried’s pharmaceutical reps, who believes he is seldom wrong. He pitches a new sedative, and they buy some, but they find out that it doesn’t work as a sedative. Herriot and Siegfried try, but they cannot bring themselves to tell the pharmaceutical rep that the product performed so badly.
Chapter 30 Tristan answer’s the practice phone with a funny accent, until he realizes the caller is a serious man. He would end up dating the man’s daughter. Mr. Mount has a horse with canker, and they stable the horse for six weeks at Skeldale House, to treat him. Tristan continues with his characteristic pranks, but he is caught twice by Mr. Mount, who is not a man of good humor. He is happy with the way his horse was treated and cured, though.
Chapter 31 This chapter speaks of comradeship, and how necessary it is between men and also between animals. One dog comes in for treatment, and his friend-dog must be in the treatment room with him. You cannot separate the two dogs. When the sick dog dies, the dog’s friend is heartbroken, but when the owners buy a new puppy, the same breed as the dog’s lost friend, he returns to his former happy self.
Chapter 32 Herriot’s flight instructor talks constantly while he is learning to fly. This reminds him of a family he knows back home, the Birtwhistles. They all try to explain what their animal’s ailment is, with the end result that he can’t hear any of them. One of the sons in the family can’t tolerate the sight of blood, and knocks James out by accidentally hitting him in the head.
Chapter 33 Herriot remembers a trip to the local market with Siegfried, where they see a dog, begging for food. After a time, the dog is hit by a car and they spend an evening patiently stitching him back together, but if no one adopts him in a week, he will be put down. Luckily, the policeman who called in the accident adopts the dog, and this is a happy thing for the vets.
Chapter 34 Herriot remembers, in this chapter, a time when tuberculosis was common in their area back in Darrowby, and the veterinarians had to check many herds of cattle. Herriot usually goofs up the forms that they have to send to the Ministry of Agriculture. He recalls that he is a much better veterinarian than a clerical person.
Chapter 35 In this chapter, Herriot is sent to fly a plane with only nine hours of learning. He fears a crash or at least getting lost, but he does much better than he thought he would. Even though this realization temporarily throws him off a bit, he flies well and finds his way back to the airfield, where congratulations await him, even from his flight instructor.
Chapter 36 Herriot remembers a farmer whose dairy farm has been automated. One day a cow is having a difficult time calving, and James assists her. He doesn’t know her name, only her number, but it is refreshing for him to see that veterinarians are still needed even with more machines taking the place of other aspects of farming.
Chapter 37 At the Drovers Arms, he talks to Paul Cotterell who has Theo, the pub terrier. He looks at Theo’s paw and snips the broken claw which has been bothering him. Paul also asks about Theo getting a little thin and they think it might be worms. James gives him some pills but that doesn’t work and James realizes the dog has Hodgkin’s disease. They put the dog down and Paul doesn’t seem that bothered by it but ends up committing suicide.
Chapter 38 Andrew Vine has a dog, Digger, who has eye problems. He is given lotion, but his vision keeps getting worse. James and Sam see them them on walks while Digger slowly goes blind. Andrew is depressed and James is worried he will end up like Paul and commit suicide. James convinces him that Digger needs him more than ever and eventually, Andrew gets over it and realized James is right.
Chapter 39 James has David, a 15 year old, coming on rounds with him. They go on three calls which are all false pregnancies and then the last call is a cow who calves and then hides the calf. David thinks James has quite a funny job.
Chapter 40 In the RAF, James has surgery and the anesthesiologist is from his vet school days. James remembers Judy, Eric Abbot’s sheepdog, who used to watch James fix up the farm’s animals, almost like his own personal nurse.
Chapter 41 Siegfried is tired of Tristan’s womanizing and partying ways, so he tells him to stay in and study. Then he leaves for Brawton for the night. Tristan has a date with Lydia but has to watch Hamish, a Scottie. He invites Lydia over but when James comes home he hurriedly kicks her out thinking James is Siegfried and in the process he loses Hammish. James and Tristan spent the night looking for the dog which eventually is found on its own front porch, Lydia comes back a few times to yell at Tristan in the process, but by the time Siegfried comes home, Tristan is hard at work studying.
Chapter 42 James learns he will be discharged. He remembers Mr. Potts, a retired farmer who always likes to talk about animals with James. Sam and Mr. Potts’ dog, Nip used to play and when Mr. Potts dies, James continues to go around to his house so Nip can play with Sam.
Chapter 43 In the RAF, James gets assigned to laundry and the boot repairs store. The other guy who is also working there doesn’t organize anything, so James doesn’t either. This ends up causing a huge mess when other military people want their clothes or boots back.
Chapter 44 James sees Roddy Travers, who pushes his dog Jake around in a pram. He does odd jobs around town and when Jake has fainting spells, James thinks it is epilepsy. While James is looking at him in the surgery, he has a fainting episode and James realizes there is something choking him. He operates right then and discovers a pebble that had been causing it. After removing it, Jake is perfectly healthy.
Chapter 45 Mr. Duggleby is a big cricket fan and talks about it the whole time James is looking at his lame pigs. James thinks it may be Foot and Mouth disease and has to send samples away. Foot and Mouth is confirmed and there are a few anxious weeks while James waits to see if any other farmers get it. He thinks Terence Baileys cow has it but it turns out it just has cowpox which is has gotten from the baby who was just vaccinated for smallpox.
Chapter 46 Mr. Daggett, a farmer, has a farmhand named Ned Finch that he is always complaining about. They live a hard life on a spartan farm and Mr. Daggett doesn’t like the fact that Ned stays at the pub until ten o’clock and doesn’t get up until seven some days. James then goes to a wonderful rebuilt manor house owned by Miss Treymayne. James discovers that her housekeeper, Elsie, is getting married to Ned. James is happy to hear that Ned will get to leave the hard farm and live in the nice manor house.
Chapter 47 Marjorie Simpson, brings in a cat with his intestines hanging out. Tristan and James patch him up and up and he starts purring. Helen decides to keep him, names him Oscar and he spends his time going around to social gatherings in town. Then the Gibbons family comes to claim him and confirm it is their cat by saying how much he likes to visit people. They rename him Tiger. Helen is sad, but eventually James and Helen go and visit him.
Chapter 48 James is finally discharged from the RAF. The bus brings him back home and he is excited about getting back to his life and all the wonderful experiences that come along with it.
All Things Bright and Beautiful Chapter Summaries
Chapter 1 Herriot checks on a ewe who has just had a lamb. The owner of the ewe is drunk, and Herriot freezes in the cold while the owner finds the animal for him. As it turns out, the ewe has another lamb to be born. This is an exciting time for Herriot.
Chapter 2 Herriot describes some of the daily details of his life since his marriage. They are low on usable furniture, but they are happy. Herriot works on a foal’s leg at a nearby farm, and their dog Jock chases his car as he leaves. Jock’s puppies are soon overtaking him in the chasing department, but after they are sold, Jock is the best car-chaser once again.
Chapter 3 At a farm, busy helping ewes who are lambing, Herriot notices one lamb whose mother won’t let him drink. Later, he returns to the farm because the lambs have been chased by a local dog. Later, a ewe who lost her lamb is depressed, so they take dead skins and use them on the ewe whose mother won’t let him drink. So the mother with no baby adopts Henry, whose own mother wouldn’t feed him.
Chapter 4 In this chapter we meet a dog named Clancy, who is sick, and no one can figure out why, unless it’s his habit of eating trash. They make a plan to hold the dog down for an exam, but the owner is late for the appointment. So the vets all take the chance and leave. They don’t relish having to deal with the dog, since he is ill-tempered.
Chapter 5 Mr. Pickersgill is introduced in Chapter Five. He feels educated because of a two week college course. He actually knows very little. Herriot has to deal with these feelings while getting Mr. Pickersgill to realize the real problems he has.
Chapter 6 Siegfried, who is Herriot’s partner and who used to be his boss, lectures Herriot and Tristan, since they are forever forgetting surgical equipment at the farms where they visit. He removes a cow’s tumor, only to be reminded that he left the forceps at the farm. He is very hesitant to admit this, since he has preached about not losing track of one’s equipment.
Chapter 7 Chapter 7 tells the reader of an encounter between Herriot and Helen, and her family, prior to their marriage. Helen’s father seems to take an instant dislike to Herriot, and the veterinarian thinks he will impress the man when his cow becomes ill. Instead, despite his treatment, the cow dies.
Chapter 8 In Chapter 8, Herriot recalls an embarrassing time in his life. While attempting to befriend a client, he drinks too much wine, and then he’s called to Bamford’s farm to deliver a calf. The next day, Siegfried is not at all pleased that Herriot had shown up at the Bamford’s farm so fully intoxicated. Siegfried hopes they couldn’t tell he was drunk, as they are strict Methodists, but Herriot knows that they could tell.
Chapter 9 We meet Mrs. Donovan in Chapter 9. She enjoys showing up at farms where Herriot is treating an animal, and treating them herself. The farm people of the community sometimes trust her treatment more than they trust that of Herriot. When her dog Rex dies after being hit by a car, she vows never to own another dog. Nonetheless, a month or so later, she is witness to a dog cruelty intervention by Herriot, and asks to take the Golden Retriever home. The dog has a happy home with Mrs. Donovan for many years.
Chapter 10 Herriot writes about serving the Darrowby Fair as their veterinarian, in Chapter 10. He sees Helen there, with her other male friend. Herriot spends some time with Tristan, then is called to see to an injured heifer. He cannot clamp the blood vessel, and is forced to simply cover it over with gauze. Helen and her other beau are watching. Herriot next sees a dog who should not be showing, since it is exhibiting signs of distemper. He also has to measure ponies to make sure they are of correct height for their classes. He is interrupted to check the dog’s temperature again by the dog’s owner, and then he continues measuring ponies, and listening to arguments by owners whose ponies are not the correct size for their classes. He notices that Helen and her other boyfriend are watching him once more.
Chapter 11 Still at the fair, Herriot must judge the Family Pets divisions. He judges them based on the knowledge of the owners about how to care for them. First prize goes to a goldfish. As Helen and her beau leave, his car won’t start and he must crank start it.
Chapter 12 In Chapter 12, we meet the widow Dalby, and learn of her fight to keep her family’s farm. Herriot arrives to see to some coughing cattle. They are sick, and must be kept inside and fed, instead of pastured. Twelve of her cattle die, and Herriot fears that her continued bad luck will result in her losing the family farm.
Chapter 13 Herriot must go to the Dalby farm again in this chapter, for more sick cattle. He tests the cattle, and it turns out that they are deficient in copper. The animals’ conditions improve with treatment. The widow Dalby still runs the farm, with her sons, and she still gives Herriot special treatment and tea when he comes to see to her animals.
Chapter 14 In this chapter, Herriot is looking at purchasing furnishings for Helen’s room, and his as well. He has a history of bringing home useless things from sales, but he resolves not to do that when he makes a trip to the Leed’s Laboratory, and attends a sale nearby. So what does he do? He buys a set of books. He can’t get them on the bus, so he finally gets them home, but they smell. At home, Helen isn’t mad, but won’t let them stay in the house because of the odor. They end up in the basement of Skeldale House.
Chapter 15 We meet the Raynes ghost in Chapter 15. It is reportedly the ghost of a monk who was murdered, and one night, after working on a pony, Herriot stops by the abbey. He gets spooked, but doesn’t see a ghost. He’s still feeling uncomfortable at home, when Tristan appears in his room, dressed as a monk. He has been the “ghost†all along. A couple days later, Siegfried and Herriot have a farm call for a cow, and Herriot rides home with a local policeman. The policeman sees the ghost and takes chase, but loses him. Tristan has to spend the night inside a drainage pipe, though, and he gives up his “haunting†ways.
Chapter 16 Granville Bennett is a small animal veterinarian, called in sometimes by Herriot for complicated small animal cases. Granville’s skilled assistants and spic and span operating room impress Herriot. He remembers, now, that he really wanted to work with small animals, when he originally went to veterinary school. He and Bennett share a beer as their small animal patient recovers.
Chapter 17 In Chapter 17, Herriot is pushed to have more beer than he should, by Bennett. At Bennett’s house, he has even more to drink, and pickled onions that upset his stomach. He is more than a little amused to see that Bennett’s last patient is already feeling better than he does.
Chapter 18 Chapter 18 tells us about Monty the bull. He is a pedigreed Newton bull, and the farmer who has purchased him feels he will be worth a lot of money. He falls ill, and Herriot treats and heals him with a miraculous surgery, and thereafter, the two have a special bond. Herriot never leaves the farm without petting the bull. When Monty the bull is fully grown, he has become mean. Herriot must get a blood sample, and does, but is then knocked to the floor. He scrambles away before the bull can gore him. The farmer finds this amusing, as Herriot leaves the farm.
Chapter 19 There are many fewer horses working on farms, as Herriot tells us in Chapter 19. He remembers a time when he was nearly kicked by a horse who is later subdued with the farmer’s voice, not needing a sedative to finish his work. The next time Herriot is at that farm, only one old horse is left. This horse has tetanus, and the antitoxin doesn’t work, so Herriot has to put the aged horse down.
Chapter 20 Christmas arrives in Chapter 20. Herriot wants a light business day so that he can relax. But he gets called to a farm in the early hours of the morning. The farmer is ungrateful and rude, and Herriot gets home only to see another call. Helen makes him breakfast while she relays the information on the second call. Herriot’s second Christmas call is a choking goat, whose owner is apologetic. As it turns out, the goat has swallowed a pair of underwear belonging to the farmer. Herriot is able to pull it back out because the elastic was stuck on the goat’s tongue. After they’re done, the wife of the farmer has Herriot in for cake and a drink. In this way, the veterinarian’s love of farmers and spirit of Christmas is renewed.
Chapter 21 Herriot gets to see Marmaduke Skelton in Chapter 21. Duke is a quack as far as medicine is concerned, and he attempts to treat animal diseases. In the case of a cow with a prolapsed uterus, one of Herriot’s veterinarian friends, Ross, arrives only to find Duke already trying to treat the animal. Ross is ready to leave but the farmer wants him to stay. Ross puts the uterus back in easily, and Duke assumes he was part of the cure.
Chapter 22 We meet Mrs. Bond’s cats in Chapter 22. She has many cats, both inside and outside. Boris the cat dislikes Herriot, since he had to give him a worm tablet once. On one day, Tristan accompanies Herriot to Mrs. Bond’s house, since one of her cats has a bone stuck in its teeth. Of course, as fate would have it, that cat is Boris. Tristan lets him out of the basket, and then chases the cat, trying to catch him. This stirs up all the other cats, who also scatter and run. Tristan actually has fun on the chase, but Mrs. Bond tells Herriot to please leave Tristan behind, next time.
Chapter 23 Herriot visits Bennett in Chapter 23. He takes along Maudie, who is a cat owned by Colonel Bosworth. Maudie was struck by a car and injured her face, but Herriot thinks Bennett can help her. After the surgery, Bennett takes Herriot along to a veterinarian meeting. Since Herriot has dressed up for the day, he agrees to go along.
Chapter 24 The snow is flying as they drive to the meeting, and Herriot fears that they will be late. They do arrive as the meeting is just ending, but as it turns out, this is what Bennett intended to do. Herriot didn’t want to meet Zoe Granville again unless he was sober and not filled with food, but they have food and drink after the meeting. Herriot starts feeling poorly on the way back to Granville’s house. The sliding of the car in the snow doesn’t help his stomach at all. They make it back to Bennett’s house safely, and Herriot is once again drunk and ill when he says good-night to Zoe.
Chapter 25 Herriot meets a dog with a testicular tumor in Chapter 25. The owner, Mr. Partridge, is afraid that his dog Percy might die in surgery, so he lets it go much too long before addressing the problem. The owner is quite enamored of his dog, to the point of not having his tail docked when all his friends ridiculed him for the decision. He cannot bring himself to allow Herriot to cut his little dog.
Chapter 26 Herriot finally gets to operate on the little dog in Chapter 26. But it was there for so long that it grows back. Herriot uses a new drug to help stop the regrowth, and it works, but causes the little dog to give off a scent much like a female dog in heat. Soon Partridge’s house is flocked by avid male dogs. But the tumors on Percy the dog do shrink, and the male dogs leave after Herriot takes the dog off those particular meds.
Chapter 27 Herriot remembers some unique ways that clients have sought his services, in Chapter 27. One particular client was in the office but drunk, and thought he was talking on the phone. Some of his clients were not always sure they needed a vet, and some wanted him to decide without even seeing the animal, if a farm call was needed. Often, his clients will give him descriptions that are not clear when they call, so Herriot sometimes doesn’t know what he’ll find when he gets to the farm.
Chapter 28 Herriot reminisces about Richard Carmody in Chapter 28. He was a student observer. He seems financially secure, and educated when Herriot first meets him. For his part, the observer is not impressed with the Skeldale House clinic, and the usage of old remedies. On his first day of farm calls with Herriot, he disagrees often and answers questions condescendingly. But a dog bites Carmody on the back-side, which does cause him to lose his poise.
Chapter 29 Carmody has decided he wants to work on the animals himself in Chapter 29, and Herriot allows it. Carmody, for all his book learning, hasn’t any common sense. Herriot watches him chase pigs, drench a horse and bleed a pig. The last task must be taken over by Herriot. Later that day, Herriot watches a bull drag Carmody across a field covered with manure. Many years later, Herriot sees Carmody once more, and they share a minute together, during which Herriot believes he sees some warm emotion.
Chapter 30 In Chapter 30, we meet Mr. Kitson, who used to attempt to deliver his lambs himself, so as not to have to pay a veterinarian. By the time Herriot arrives, there is one dead lamb, and the rest are more difficult to birth. Herriot also notices a sick ewe while he is there, but Kitson doesn’t want him to treat her. Knowing she will die, Herriot secretly gives her some anesthetic so that she can die in her sleep. As it turns out, when Herriot returns to the farm several days later, the sick ewe is better, having slept for a couple days. Herriot rightfully believes her days without pain allowed her to recover.
Chapter 31 Herriot treats a poodle with gastroenteritis in Chapter 31. He uses various remedies, but none of them work. When they are so far along that euthanasia is discussed, Herriot puts the poodle into a deep sleep for several days, which gives her body time to recover. The dog recovers, to everyone’s delight.
Chapter 32 We get to meet Sam in Chapter 32. He is Helen’s dog, a beagle, who accompanies Herriot on his farm calls. Next, the veterinarian remembers a time he was nearly smashed by a bull who just had an itch, and another time he attempts to treat a budgie’s beak, and the bird dies of fright. He cannot bring himself to tell the older owner, so he buys a new bird to replace the dead budgie.
Chapter 33 Herriot attends to a worried owner whose dog is pregnant in Chapter 33. The dog isn’t near her due date yet, but the owner insists it’s time. Herriot attempts to explain that the dog’s cervix is not dilated, so she can’t have the pups yet. Siegfried makes the next call to the lady’s house, and by this time, the dog is ready to have her pups, so he administers the shot to give her contractions. The owner scolds Herriot the next time she sees him, saying he doesn’t know his job.
Chapter 34 Mr. Wilkins’ dog, Gyp, has unexplained periodic convulsions. He recovers, but James tells the owner it will be a lifelong issue. Gyp also never barks, but his brother Sweep, who was given away turns into a great sheepdog for George Crossley. At the Mellerton Agricultural Show, Gyp sees Sweep running sheep and lets out one bark. After this, he never barks again.
Chaper 35 James reminisces about the Daffodil Ball at the Drovers Arms. He sees Helen there dancing with Richard Edmundson and wants to ask her to dance but doesn’t get the chance and gets called away. On the way out, he runs into her and tells her to come with him. They kiss and then go up to Bert Chapman’s place where Susie, his dog is having puppies. James delivers the puppies and realizes that Helen is now his girlfriend.
Chapter 36 James meets the Dimmocks, who bring him their dog Bonzo, who has been hit by a car. He patches him up and that begins a relationship with the entire Dimmock family. Then, the young daughter, Nellie brings in her puppy, Toby who can’t keep his food down. James realizes he has pyloric stenosis and calls Granville Bennet, who says he would be happy to operate.
Chapter 37 Granville comes and operates on the dog and invites James to lunch at the Old Oak Tree Inn. Once there, James has a few whiskey and sodas. Then he goes to Granville’s house where his wife, Zoe makes them lunch. James has a hard time keeping himself together from all the alcohol he has consumed. The dog ends up recovering after the surgery.
Chapter 38 Former steel worker, Frank Metcalfe, shows off his new barn and dairy to James. He has a cow that develops brucellosis, which may have infected the other cows. When they all start aborting, James’ fears are confirmed. Another farmer, Mr. Bagely says he has a cure, Professor Driscoll’s Abortion Cure. After giving it to the cows, some heifers have calves and Mr. Bagley say it is because of him. But then there are five more abortions, causing Metcalfe to have to sell everything and move.
Chapter 39 James revels in his marriage to Helen and the domestic bliss she brings to Skeldale House. After a calving, Mr. Horner invites him into a breakfast of bread, butter, jam and 100% fat bacon that is eaten cold. Only by spooning tons of piccalilli on it, is James is able to gag it down.
Chapter 40 Walt Barnett demands a horse be gelded and when James gets upset, Siegfried tries to calm him down and tells him he stresses out too much. Then Barnett calls again and irritates Siegfried and now it is James’ turn to laugh. Siegfried agrres to do the job but tells James he will overcharge him. He does the job, asks for 10 pounds and after a long period of silence, Barnett pays. Siegfried then manages to lose the check and makes James go back and get another one.
Chapter 41 James comes back late from a job and ends up chatting and drinking all night with Siegfried who is leaving for the RAF in the morning. Siegfried says he owes James money, 50 pounds, and gives it to him before leaving. James only realizes years later that it was a gift.
Chapter 42 Helen and James are invited to the Hodgsons for dinner. James has three jobs before dinner and he assumes they will not take that long. First, he goes to Edward Wiggins farm to give some vaccinations. While Wiggins fumbles around trying to catch a bullock, James gets angrier and angrier. He eventually gets run over and while he is resting, James and Wilf, the farmhand, catch and vaccinate the bull. Next, James has to go stitch up a pig who has a minor cut at the Misses Dunn’s farm. To get the pig to walk to where James can stitch it, they have to throw digestive biscuits in front if it. This takes forever because the pig will only walk if the biscuit is thrown close to him, so they have to throw a lot of biscuits to get the pig to where James wants it to go.
Chapter 43 After James is done with the pig, it’s off to Ted buckle’s farm to put a ring in a bull’s nose. As he is about to the put in the ring, the bull jumps the gate and runs out into the field. James is panicking and he can’t even call Helen because the farm doesn’t have a phone. The farmer says it isn’t a problem and sends a cow out into the field and when he calls the cow back in the bull is following her. James is amazed and the farmer tell him his secret, the cow is the bull’s mother.
Chapter 44 James sees Tristan’s car at a farm and wonders how he is doing. Tristan always seems to get along with the farmers, although this farmer is Mark Dowson, who can be difficult. Tristan puts on such a performance helping a cow give birth that he is invited in for brandy much to James’ amazement.
Chapter 45 White scour infects Mr. Clark’s cows and they have to call out Jeff Mallock, the knacker. He says he will give them a day and James ends up curing the cows with a new drug, sulphapyridine. James thinks back about how this was the start of a drug revolution in antibiotics.
Chapter 46 James is having a pint at the Drovers Arms and Magnus, a mini daschund barks at him. He remembers how he had to bandage his mouth shut the first time they met just to get his nails clipped. Magnus has obviously not forgotten. In contrast, James remembers Mrs. Hammond’s Irish Setter, Rock, who gets his foot stuck in a animal trap. Even though it is completely swollen and James has to clean and dress it for a week, Rock never minds. Another dog, Timmy Buttermark, a wire haired fox terrier, eats poison and James has to make him throw up by giving him lots of mustard. Much like Magnus, he never forgets and eyes James whenever he sees him.
Chapter 47 James gets called up to military service on his birthday. He goes to help a Old English sheepdog, Benjmain who has a dislocated elbow. James manages to pop it back into place, amazing the farmer. He revels in the moment, knowing he will be back after the RAF.
Chapter 48 James leaves for the RAF while Helen waves once more from the window.
All Creatures Great and Small Chapter Summaries
Chapter 1 Herriot is having a hard time with a calving in the dead of winter. The calf is not properly presented for delivery, and Herriot has to endure much nay-saying and second-guessing from the farmer’s uncle. After hours of struggling with the calf within the cow, Herriot is ready to give up, but then he gets the rope around the calf’s jaw and delivers a healthy calf. “Uncle” is sure that his veterinarian could have performed the task better.
Chapter 2 Herriot remembers the day he came to talk to his would-be boss, Siegfried Farnon, with only a little hope that he would get a paid position. Times are bad in England, and most students that graduated with Herriot are lucky to find work just to pay their board. Herriot very much enjoys the English countryside, and is surprised when he meets Farnon that he’s not German, as Herriot expected, but a regular Englishman.
Chapter 3 Herriot goes on farm calls with Farnon in this chapter. He is grateful to be doing real work, and feels that this is the best way to show Farnon that he is qualified for the position. Herriot has a draft horse lean on him for untold minutes, while he digs for an abscess in the animal’s hoof. At their last call he gets kicked by a cow. But he has survived his first day.
Chapter 4 Farnon and Herriot stop at a pub after finishing their rounds, and Farnon hires the young vet, for wages plus board. After a talk with a local farmer who imparts a secret about marshmallow cream being the heal-all for hoof ailments, Herriot joins Farnon at the house where he will live, Skeldale House.
Chapter 5 Herriot is anxious to go on a farm call by himself, and he does get that chance, but the horse he goes to see has a twisted intestine, and needs to be put down. The problem is that the stable manager expected that he could be made well, especially if Farnon had come. Soames calls later to complain about Herriot, but Farnon backs Herriot up.
Chapter 6 Farnon performs a necropsy on the valuable hunter that Herriot put down in the last chapter. He finds that Herriot was correct in his diagnosis. Herriot meets Tristan, Farnon’s younger brother, who is not like his older brother at all. Tristan has flunked both of his veterinary courses, which Farnon is paying for, and is sternly lectured. He accepts it graciously.
Chapter 7 With Tristan and Herriot both on board, the practice settles into a stable routine. Tristan is a bit lazy about taking morning calls, which earns him more chastising by Siegfried. After working on some nearly-wild cattle, Herriot relaxes and enjoys the countryside he has found himself in, and thinks he will do well here.
Chapter 8 In this chapter, Herriot learns that the elder Farnon is a lady’s man and someone who constantly contradicts himself. The contradictions fluster Herriot, and in this chapter, Farnon tells Herriot the wrong farm to drive to, then insists he didn’t, and then mildly berates Herriot for abusing his fine car, which is actually an old and junky car.
Chapter 9 Tristan and Siegfried play jokes on each other, but whereas Tristan’s usually work, his older brother cannot often get Tristan to fall for any of his pranks. Later, Herriot himself tricks Tristan, telling him that a uterus they spent all afternoon pushing back into a cow has worked its way out again.
Chapter 10 Herriot is settling into the life in Darrowby, and the townspeople and farmers are becoming more accepting of him, since he does know how to do his job. Still, he is not at all used to the laid back pace of the farmers. One family has asked him to take them to a concert he is also attending, but they proceed to eat a sumptuous lunch, and eventually Herriot is late to the concert, and has to endure the irritation of the other audience members.
Chapter 11 This chapter tells the sad story of an elderly man in a poor section of town, whose old dog is sick. Herriot checks the dog and finds a tumor that is not operable. As much as he hates to tell the man, the dog must be put down. The old man agrees, and kneels down to tell his old dog good-bye. Herriot injects the dog, and refuses to accept money for the shot. The dog dies peacefully, and the old man gives Herriot a cigar in thanks.
Chapter 12 In this chapter, Siegfried assigns Tristan to collect money on the day everyone comes in to pay. He seems to do well, and is congenial with the patrons, but has not yet recorded any transactions in the ledger when the payment book goes missing. So, the customers who have already paid still are billed the next month, and this does not generate any good will for the practice.
Chapter 13 One of Herriot’s easy patients is Tricki Woo, a little dog who is owned by a rich older lady. She spends lots of money on the dog, but feeds him too much fat, which Herriot is always trying to get her to stop. Tricki Woo sends treats to Skeldale House, and Herriot learns that he must talk to the dog just like he would a person.
Chapter 14 Farnon hires a book-keeper, to avoid another debacle with the books, but she is harsh with him when she finds out that they just stuff the receipts into a pot on a shelf. She tells them they will need to be more organized, and she is a tough lady.
Chapter 15 Siegfried decides he’d like to have fresh eggs and bacon for breakfast, so he gets some hens and pigs and tells Tristan it’s his job to look after them. The group ends up with hens up in the trees and Siegfried sells them. Although they never laid one egg at Skeldale house, they are excellent layers at the next farm, because Tristan was not careful about what he fed them.
Chapter 16 Tristan does better with the piglets than the hens, but they grow very large, and are always knocking him down when he tries to feed them. One time, he left the gate open, and they trampled him and escaped. They are all rounded up except one, but then Tristan finds that Siegfried’s new hunter mare got loose, and they have to travel to a neighbors house to pick her up.
Chapter 17 The new book-keeper is very upset with Siegfried, because he keeps taking money out of petty cash whenever he needs it, but doesn’t leave a note as to how much he took or what it was for. In addition, she describes his poor receipt penmanship, and those are only on the few occasions when he actually remembers to write them down.
Chapter 18 Herriot recalls a lesson learned, in this chapter. After having only seen a diagram of a horse in veterinary school, he decides he knows everything about horses. He sees an old, sway-backed coal cart horse, and attempts to soothe him. The horse picks him up and hangs onto him by his fancy coat until the owner returns. Herriot is properly humbled.
Chapter 19 Herriot attends a party for Tricki Woo, and discovers just how much he is being overfed by his loving owner. He gently chastises her and shows her the correct amount to feed the dog. Herriot drinks too much at the party, and then gets called out on a farm call in the middle of the night. He falls asleep trying to deliver a pig, since he is still tipsy from the drinking, and the farmer has to wake him up. The rest of the pigs are soon delivered.
Chapter 20 The new book-keeper is the latest to be flustered by Siegfried’s contradictions. He tells her the money box has to be kept full, even though he empties it at will, and tells her all the bills need to go out the first of the month, even though he doesn’t give her many receipts for the work he has done himself. She is truly on the receiving end of this frustrating phenomenon.
Chapter 21 A dog is slow in coming around after surgery in this chapter. Farnon and Herriot go on their rounds, leaving Tristan to watch the dog, who is howling constantly. He is still howling when they return from their rounds, and Tristan is drunk. The dog wakes up, and Siegfried tells Tristan to take him to his room, where it’s safe, and then the dog paces all night. Tristan is fit to be tied, and the next day, the dog finally gets to go home.
Chapter 22 Herriot takes a dog to another vet’s office, since it is his patient, and the vet performs surgery. He wants Herriot to take the dog back, but not until the anesthesia wears off. So Herriot is stuck going on a farm call with the other vet, who has none of the pleasant characteristics that most Scotsmen do. The vet asks for his help, but he is dressed in a suit. The vet gives him a black coverall to wear, so that he can help, but he doesn’t end up needing to do much. The other vet has a good laugh at Herriot’s expense.
Chapter 23 Herriot treats a cow with a calcium deficiency, even though the owner thinks she is dying. There are newer injectables now, and they work very well. They take the cow and her calf back to the barn, from the stream where she had been laying. Herriot is invited for breakfast, and has an excellent meal. Later, the book-keeper at Skeldale House and Farnon are arguing again, and she is winning until he takes a note she wrote for him and shreds it.
Chapter 24 Siegfried wants Tristan to leave the house for a night, but Tristan wants to go to a dance in the village. Siegfried picks the worst task he can think of for Tristan, working on the ear of a mean old sow. Tristan makes several trips to the farm, and returns with different excuses about why he couldn’t take care of the sow. Siegfried sends him out yet again. Finally, Tristan tells Herriot that the sow wouldn’t let him in her pen, but he finally got so mad that he chased her around. As it turns out, the sow is a coward, and burst her ear growth on the wall.
Chapter 25 Spring finally comes to the Dales after a long and bitter winter. Herriot learns about lambing, and also about how quickly the lambs can find their ewes after being corralled for vaccinations. Then he learns about foaling, which is a lot harder than delivering lambs. Even harder is the castration of the male horses that will not be used at stud. They used to drug and throw the colts and do the procedure on the ground, but the new method leaves the colts standing up. Herriot is supposed to work on a horse that turns out to be a six year old stallion, and he is afraid to do it. He hopes that Farnon will do the horse, but he doesn’t. Finally, Herriot has to work on the horse, and the horse kicks him in the leg. Herriot realizes that fear is worse than the hurt leg.
Chapter 26 Herriot calls on a farmer with six sick steers. The farmer is waiting for some new-fangled diagnosis and treatment, since Herriot is young and fresh out of veterinary school. Instead, Herriot tells him the animals have lead poisoning, and to give them Epsom salts. The farmer is disappointed at the old-school remedy, but it works. Later, the man has a bull who is down and has a temperature of 110. Once again, he expects a new remedy, but the bull has heat stroke, so Herriot has the men spray him with water, which effectively cures him. Once again, the man is disappointed that he never got to see newer methods used.
Chapter 27 Farnon wants the vets to display more professionalism, so he takes them along on a farm call, after donning a white lab coat. Time and again, Farnon tries to get the wire from a cow’s second stomach. Finally, he decides to lance the stomach, since there is a build up of gas. He is thoroughly sprayed and quite ill-smelling all the way home. Tristan and Herriot hang their heads out the car windows, but Farnon declares that the day was a success.
Chapter 28 We meet the knacker in this chapter. He is the man who hauls away dead animals and renders them. He also checks for cause of death. One farmer wants to collect on insurance for a cow that he says was struck by lightning, but Herriot says the animal died of heart failure. The farmer goes to the knacker for a second opinion, and he finds a tumor that caused the heart to fail. The farmer is left with neither expert able or willing to help him get insurance money for the dead cow.
Chapter 29 The farmer who couldn’t get the insurance money still uses the practice at Skeldale House, after complaining to Farnon about the cow’s cause of death. Siegfried sends Tristan to deliver ointment to Cranford, the cow farmer, and he also tells him to drop a fecal sample off at a local laboratory. Instead, Tristan accidentally mixes up the packages and Cranford is rubbing fecal matter onto his cows, which gives everyone at the practice a laugh.
Chapter 30 Tricki Woo is very ill in this chapter, having been overfed to the point of being near death. Herriot decides he needs two weeks away from his owner to regain his health, which worries her to no end. After with-holding food for two days, they bring him up to one meal a day, and he loses weight playing with Siegfried’s dogs, as well. When he recovers, his owner thinks it is a miracle of modern science, when it was just proper feeding.
Chapter 31 Herriot is called out in the middle of the night, for a mare who is having trouble foaling. He goes out in his pajamas, with a coat over them. He repositions the foal properly inside the mare, and it is born without any further issues. Herriot drives to the local cafe, forgetting he is wearing only pajamas and a coat. He orders coffee and a sandwich, but hasn’t brought his wallet, so the waitress gives him his coffee on the house. The other people in the cafe joke about his clothing, thinking him possibly a prison escapee.
Chapter 32 Herriot goes out to check a cow that is down, and despite some help, she will not rise. He hears a noise in her bones and decides that she has a broken pelvis and probably will not walk again. Of course, as these things go, the cow gets up the next day, and Farnon explains to Herriot that sometimes cows have a weakening of the ligaments after they have a calf, and of course the farmer tells anyone who will listen about the cow that Herriot said would never get up again, but who did.
Chapter 33 Tricki Woo’s owner has bought a pig, and she keeps it in the kitchen, much to the chagrin of her cooks, since pigs definitely have their own odor. Herriot convinces her that the place for pigs is outdoors. He checks the pig once because the owner thinks he is sick, stopping and starting during urination, which is normal for pigs. Now Herriot has two nephews, and Farnon gives him some grief at having a pig for a nephew, but he gets more treats and gifts.
Chapter 34 Dr. Grier, the other vet in the area, needs help at his practice, and Herriot goes, but is not happy about it. He gets plain porridge three meals a day. He is called out for a cow who has a prolapsed uterus, and Grier tells him not to put in retention sutures. Herriot does as he is told, even though he normally puts in the sutures. Predictably, they get a call that her uterus is back out, and Dr. Grier reinserts her uterus and then puts in the stitches he told Herriot not to, while Herriot must listen to comments about his less than adequate veterinary skills.
Chapter 35 Dr. Grier falls sick again, so Herriot must help him once more. A client calls and says her dog has a bone in his throat, but Grier tells Herriot that it will actually be pharyngitis. Herriot examines the dog, who appears fine, and tells the owner what Dr. Grier told him to tell her. As it turns out, Dr. Grier is having an affair with the woman who owns the dog, and there is nothing wrong with the dog. An assistant is hired by Dr. Grier, and Herriot happily returns to Skeldale House, even though the first thing he hears there is the Farnon brothers arguing.
Chapter 36 Herriot works on the cow of a poor farmer. The cow has mastitis, and even after treatment and cleaning, she will never produce milk from all of her teats. The farmer gladly says he will clean her out if it means he can still milk her at all. The next morning, Herriot stops by to check on the cow, and the farmer has spent the whole night cleaning his cow out, and she is doing better. The farmer, dead on his feet, nevertheless goes on to his other job.
Chapter 37 Farnon watches Herriot stitching up a dog at Skeldale House, and tells him he’s using too much suture material. Farnon finishes himself, using the bare minimum. When they go to suture up a foal together, Herriot remembers the lecture and only uses a bit of catgut at a time. Farnon is frustrated, and pulls off a huge length, so much that he must stand to stitch. Farnon chastises Herriot in front of the farmer about not being so thrifty, and Herriot just grumbles at this latest contradiction.
Chapter 38 We learn about Mr. Worley, a pig-breeder, in this chapter. He is very successful, contrary to what the locals believe he should be. Herriot becomes one of Mr. Worley’s favorites when he works on a sow’s foot, and the breeder has him over to his inn for liquor, against local regulations. Worley has a pig give birth and then not produce milk, but Herriot gives her a shot that helps almost immediately. He shares a round at the inn, not realizing he bought the round. After he leaves, the bar is raided by a visiting constable, and they are fined. It doesn’t seem to bother anyone, though.
Chapter 39 Tristan drives Herriot to a farm call in this chapter, since Herriot has an infection in his arm. They are driving the older Austin, since Tristan had an accident in his car the same week. After the call, they are relaxing, until they see the Austin rolling down the hill, since Tristan forgot to set the parking brake. The car spews veterinary instruments all over and crashes into a shed. The car is none the worse for wear, but the shed is destroyed. It was leased by a local golf club. The farmer says he won’t tell anyone what happened. The next day, Farnon is still ill and Tristan and Herriot have to use his Land Rover. Someone sideswipes them, and the Land Rover is damaged. Tristan tells Siegfried and the elder Farnon fires the younger again, but they both know he doesn’t really mean it.
Chapter 40 Herriot is called to look at an injured calf, and he can’t find it at the farm, so he knocks at the house. A young lady named Helen takes him to the place where the cow is. Herriot puts a cast on the calf’s leg, and has a pleasant talk with Helen. He learns from the Farnons that Helen is popular with the men, but picky about who she dates.
Chapter 41 Herriot does a spell of work as a veterinary inspector, which means checking all the local cattle for tuberculosis. At the first farm, six calves cannot be caught, until a neighbor with a unique skill imitates a fly, and all the cows come running.
Chapter 42 Herriot is already behind on time on his TB testing, after that first farm. At the second farm, he has to clean all the ears of the cattle, because the farmers can’t remember which is which. Herriot realizes he needs to schedule fewer farms per day to check, and the rest of the farmers this day are angry with him. Some have even turned their cows back out, since they think he’s not coming. They don’t like to clean the barns, so the cows are usually left outside in the summer. At the next farm, no one is there but the cows are in, so Herriot starts checking them. One particular cow keeps pummeling him and kicking him, so he pulls his way into the hayloft. The farmer is amused. At the last farm, Herriot checks the last cow in line, only to find he’s checking a bull, instead. This farmer is also amused by Herriot.
Chapter 43 Miss Stubbs is a poor, older woman, who has five animals, all but one of which is ill. Herriot visits her often, helping the sick animals. After a favorite dog, Ben, dies, she says that she’ll be next. She passes away and Herriot hears about it second-hand. He rushes to her house, fearing for her animals. But they have been taken in by her housekeeper, and they greet him like the old friend he is.
Chapter 44 Herriot is trying to woo Helen Alderson, whom he met on a farm call. He goes to concerts she attends, since she likes music, but he is too shy to make much headway. When they clean up after a concert, he asks her out and she agrees. But he is worried that he might have pressured her into accepting.
Chapter 45 After discussing an article that says small animal breeders love their animals more than do breeders of large animals, Herriot goes out to float the teeth of two horses, at a successful farm owned by John Skipton. Herriot discovers the horses are older, with so much white hair that they look like roans. They are indeed older horses, who need their teeth kept floated and smooth, so that they can digest their food. Skipton says the horses were slaves when he was. He obviously cares very much for them. One horse has two long, sharp teeth, and he doesn’t even react when Herriot is able to snap them off, since he is used to good care.
Chapter 46 Herriot’s assistant passes out during a bloody surgery, and this reaffirms his belief that large men are more prone to this. He remembers another occasion when he asked for help and a big man volunteered. He, too, passed out, and the small farm owner came to assist Herriot. He has one farmer pay him money before his work begins, and he will wait until after the castrations to give the man his change. The man faints, so Herriot leaves the change, which wakes the man up, and he says he’s short on his change.
Chapter 47 Mr. Sidlow always waits until the last minute to call the veterinarian, causing his animals to be in pain for longer than they need to be. This man has been a client of Siegfried’s, but now Herriot has him. The current call is for a bullock that swallowed something, and the farmer has tried to push it down his throat, and in the process cut his windpipe. Herriot tells him that the bullock must be put down, but the man does not agree. Herriot signs a form stating that the meat is alright to buy for butchering. Later, Herriot is called to a local track to stitch up a horse, and he is nervous, since the horse’s usual vet is very well-known as an excellent veterinarian. The stable boy gives him a tip on a good bet, and Herriot goes to the bank and gets out money to bet, then changes clothes and is ready to head back to the track when Mr. Sidlow calls Skeldale House. He has a gravely ill cow, and by the time Herriot gets to the track, the race is over, and the 10-1 horse he had a tip on has won.
Chapter 48 Herriot will take Helen on their first date today. Herriot has a quickly-altered suit that is out of style and fits poorly and then after he picks Helen up, their car ends up on a road that is washed out. They go to her house for shoes, and he has to wear an ill-fitting pair of her father’s shoes. Add to this a flat tire, and the fact that he needed a hotel reservation to eat at the hotel restaurant. The date feels uncomfortable to Herriot, and he’s sure that Helen hadn’t wanted to go, anyway.
Chapter 49 The brakes in the Austin are shot, and Herriot has to drive it for some time like this, since Siegfried always forgets to have it done. Finally Siegfried has to drive the car, with Herriot along, and he has a very hard time stopping the car. Afterwards, he chides Herriot for “not telling him†about the brakes. Herriot just remains silent.
Chapter 50 Mr. Denham is a millionaire but still plays football pools. He makes vet calls to Siegfried, since he won a pool once, on betting days, but they are always non-serious issues. He just wants to know who to pick in the pool. When Herriot is called to see Denham’s Great Dane, she is afraid he is there to steal her newborn pups, and she bites him nastily in the leg. Siegfried jokes about it until he sees how badly the dog bit Herriot.
Chapter 51 It is Herriot’s second winter in Yorkshire, and there is more snow than the previous year. Herriot drives as close as he can to his farm call, but has to get out and walk. The snowfall picks up and he wanders around, quite lost, until he ends up at the right farm. The farmer says it seems like a plain day.
Chapter 52 Farnon half-listens to Herriot detailing a case, and he hears the details wrong. Herriot repeats himself, but Farnon still doesn’t catch it. He tells Herriot that after he has been a vet for awhile, he won’t be so easily confused. This irritates Herriot. Herriot speaks to Tristan afterward, and the younger Farnon says it’s probably not Siegfried who is bothering Herriot, but the events with Helen. Herriot suspects that Tristan is right.
Chapter 53 A poor farmer named Rudd has finally saved up enough money to buy a cow, and he is pleased when he can finally get her. Herriot gets along well with the family, and discovers that the way Mrs. Rudd feeds all 7 kids is feeding lots of pudding so they’re not as hungry for the main course. Sadly, the new cow develops a throat abscess, and while he treats it, she steadily gets worse. The family appreciates his efforts, but this just makes him feel guilty.
Chapter 54 Herriot finally decides to lance the abscess on the cow’s neck, but fears she is too far gone. Instead, she recovers, and he and the Rudds are very happy that she is back to her regular self again. Herriot looks back now, knowing how much harder everything was back then, and wishes he had some of our techniques and medicines in earlier years.
Chapter 55 The worst problem at Skeldale House practice is customers that won’t pay. The non-payers are usually quite charming, but they don’t pay their bills. Farnon’s favorite non-payer is a man called The Major, who lived in Darrowby for three years and never paid anyone anything. He was so charming that he just got away with it.
Chapter 56 There are also non-payers who are not charming. One such man is the local butcher. He always expects the veterinarians to drop whatever they are doing and attend to his animals, but he doesn’t pay his bills. Herriot helps deliver twin calves for the man, and they both live, which is unusual. The butcher offers some sausage for Herriot’s efforts, but Herriot asks him how much they are and pays for them, to try to prove a point.
Chapter 57 Herriot double-dates with Tristan in this chapter, but although his date is nice, he only thinks of Helen. Herriot and his date, Connie, get drunk and then eat too much filling food. They end up outside in the mud, sine they feel sick. Later, back inside, he and Connie run into Helen, and Herriot is completely mortified.
Chapter 58 In this chapter, Herriot recalls stories about some of the people who live in the Yorkshire area. He remembers farmers who had extraordinary animals, as well as farmers who seemed unable to get along with anyone, and farmers who tried to live life on the land but couldn’t make it. One lady from a farm brings Herriot kittens to heal, and he is happy to be able to help her with a new vaccines and equally happy to hear from the farmer later on, that they are now cats.
Chapter 59 Herriot meets gypsy’s who have a foundering black and white pinto pony in this chapter. Founder is serious and can easily kill a horse even today, but Herriot and Farnon bleed the pony and tell the owners to let him stand in a stream a few minutes at a time, many times each day. Days later, they see the gypsy’s leaving, and the pony is fine.
Chapter 60 Helen brings her dog Dan into the practice and asks for Herriot. The dog has a dislocated hip, and he and Helen work together to pop it back into place. Mrs. Hall makes tea for Herriot and Helen, and Herriot calls later that day to check on the dog, who is better. While on the phone, he asks Helen out and she happily agrees.
Chapter 61 Rich and poor families are recalled in this chapter. In the rich family, the wife and daughter blame the father for their dog’s condition, which he could not have caused. Herriot notices the man’s hands shaking, and decides he may have Parkinson’s, or he may be an alcoholic. Later Herriot sees a poor family, where everyone pitches in to help, and the daughter is headed to town to get her father something, with money she saved herself. The difference between the two families is striking to Herriot.
Chapter 62 Herriot and Helen’s second date begins at the cinema, where the usher laughs at the veterinarian since he’s there with a date. A man in the theater berates Herriot for supposedly misdiagnosing an animal, and then a drunk collapses in the chair next to Herriot, and snores for the rest of the movie. Instead of a Scottish film as the second half of the double-feature, it’s a western, and Helen laughs in amusement. She suggests that on the next date they go for a walk, and Herriot is happy because she said “next time”.
Chapter 63 Farnon has a chance to go to work as the supervising veterinarian for a racing circuit, but he would have to leave his home behind. They are at the track, checking over a horse, when a veterinarian that Farnon knows comes up. Farnon and Herriot drag the other vet away from the area.
Chapter 64 The visiting vet, Herriot and Farnon go to a club and have a meal and drinks. But then Farnon remembers the people waiting for him, and they are quite angry. Farnon has made a horrible impression on the people from the Racing Circuit, and he says that’s OK, because he really didn’t want to leave Darrowby.
Chapter 65 Herriot and Helen are getting along famously, but her father seems to dislike him. Back at Skeldale House, Farnon tells Herriot that if he marries Helen, they can live in a private room upstairs. Farnon is afraid that Herriot’s timidity will result in them never marrying. Herriot will soon be a partner in the practice, and he decides he will ask Helen. She says yes, but now they have to tell her father.
Chapter 66 Herriot has cleaned a cow and smells awful, so he borrows Mrs. Hall’s bath salts, which are very flowery. After his bath, he falls asleep upstairs. He is called out early in the morning on a farm call to Helen’s father’s farm, and Mr. Alderson notices the weird flowery smell on Herriot. Herriot helps the cow to have her calf, and then tells Mr. Alderson of his plan to marry Helen. They go in Alderson’s house and share some drinks, and the man opens up about how much he loved and misses his deceased wife. Alderson drinks too much and Herriot has to help him upstairs, and he feels they are getting along better.
Chapter 67 It’s TB testing time, but also Herriot and Helen’s wedding and honeymoon time. Farnon complains about having to do all the testing himself, so they honeymoon close by, so Herriot can help. As they are leaving their wedding, they see a new shingle at Skeldale House. Farnon has made Herriot a full partner. Helen and Herriot spend their honeymoon inspecting cows and enjoying each other’s company.
CHCCOM005 Communicate and CHCLEG001 Work Legally Ethically
Student assessment booklet, chc33015 certificate iii in individual support, working in community support, for class room-based students, chccom005 communicate and work in health and community services, chcleg001 work legally and ethically, assessment task 1: written questions .
T ASK SUMMARY :
- This is an open book test – you can use the Internet, textbooks and other documents to help you with your answers if required.
- You must answer all 21 questions correctly.
- Write your answers in the space provided.
- If you need more space, you can use extra paper. All extra pieces of paper must include your name and the question number/s you are answering.
- You may like to use a computer to type your answers. Your assessor will tell you if you can email them the file or if you need to print a hard copy and submit it. W HAT DO I NEED IN ORDER TO COMPLETE THIS ASSESSMENT ? ▪ Access to textbooks and other learning materials.
- Access to a computer and the Internet (if you prefer to type your answers). W HEN DO I DO THIS TASK ?
- You will do this task in the classroom or for homework – your assessor will advise.
- Write in your due date as advised by your assessor:
WHAT DO I NEED TO DO IF I GET SOMETHING WRONG ?
If your assessor marks any of your answers as incorrect, they will talk to you about resubmission. You will need to do one of the following: ▪ Answer the questions that were incorrect in writing.
- Answer the questions that were incorrect verbally.
Q UESTION 1
What are the Australian Privacy Principles and what do they cover?
Q UESTION 2
Provide an example to explain informed consent.
Q UESTION 3
Provide three examples of how you would protect client or customer information.
Q UESTION 4
- What is the Universal Declaration of Human Rights? Who uses this?
- What is meant by ‘human needs’? What are the basic needs?
- What is meant by ‘human rights’?
Q UESTION 5
Bridgette, a registered nurse, is being harassed by a male senior staff member, Alex. He constantly mocks her because she is overweight. Bridget works with Alex on a daily basis and he constantly make jokes and comments about the quality of her work. He also mocks her when she has to do any physical tasks – saying she will probably have a heart attack because she is so fat. When an opportunity to take on a project comes up Alex tells Bridgette that she should not attempt to apply for it because she wouldn’t be fit enough to do the job.
- What legislation and policies are being breached?
- Describe an effective complaints management process that Bridgette could follow if she wanted to formally lodge a complaint. (Provide a step-by-step process.)
Q UESTION 6
- Describe the difference between a code of conduct and a code of practice.
- Name two codes of practice that a health and community services worker would work under.
Q UESTION 7
80 year old Mr Johnson has been diagnosed with Alzheimer’s disease and is rapidly declining in his overall state of health and wellbeing although he is still able to function at a functional capacity. His doctors have informed his daughter Ellen she needs to move him into a better care facility who are able to strictly monitor her father on a daily basis. Ellen suggests this as an option to her father however he is adamant that he can continue living in his own home with minor support. His doctors consider this unsafe for Mr Johnson however he feels strongly about his decision and refuses to change his mind. Ellen is not comfortable with her father’s decision and advises his doctors that he will move out in to the recommended facility the following Friday. On the Friday morning Mr Johnson is taken unwillingly to the care facility.
Would you consider Ellen’s choices unlawful? Why/Why not?
Q UESTION 8
In the following table briefly describe each of the legal and ethical considerations, their importance in health and community services area and a possible consequence of a breach of each.
Q UESTION 9
Jessie works in a Home and Community Care environment. One of Jessie’s elderly clients lives at home with her daughter and granddaughter. Lately you have been concerned that the granddaughter has bruises on her arms and face. Her bruising patterns lead Jessie to suspect the child is being abused. The mother always seems to avoid you and the grandmother says the child keeps falling off her bike. When you talk to the child she does not answer. The child is not your client.
- Does Jessie have a duty of care to report this suspected abuse? Why/why not?
- List five other indicators that might suggest that a child is being abused physically or psychologically.
Q UESTION 10
Harry is working in Home and Community Care. One of the clients, Arnold has taken a liking to Harry as he reminds him of his son. He often gives Harry small presents and has now offered to pay for a season ticket to the football (they both follow the same team).
What should Harry consider before he accepts this gift?
Q UESTION 11
Joan and John are having a conversation about a client:
Joan: I have given Mr Fisher his meds. I helped him take them as he sometimes forgets if we just leave them with him. Can you look in on him in the next half hour as he needs his bandaging done?
John: Oh yes – I agree that we should be assisting him to take his meds as you are right – he’s getting a bit forgetful. Yes I will do Mr Fisher’s bandages straightaway.
- Interactive
- Transactional
- Does John use an affirming statement in his response? If so, what does he say?
- How does John summarise Joan’s communication to show that he has understood?
Q UESTION 12
- Write an example of an open-ended question.
- Write an example of a closed question.
Q UESTION 13
Joan would like Mr Fisher to use a walking frame instead of his walking stick as he is getting unsteady on his feet. To do this she would like to use a motivational approach rather than a coercive approach.
In a paragraph, explain what Joan could say to Mr Fisher to motivate him to use the walking frame.
Q UESTION 14
Mr Fisher’s daughter, Matilda charges up to Joan. ‘Why isn’t my father being looked after properly? You let him fall over – he could have been badly injured. I’ve a good mind to take him out of this facility!’
How could Matilda have used a more collaborative approach? How would this have been an advantage to her father?
Q UESTION 15
When working with a diverse range of people we are bound to come across situations where we need to consider our communication approach. In the following table describe how you would respond to each situation.
Q UESTION 16
Giuseppe is a 70 year old man. Today he is looking very uncomfortable. You notice that he is fidgety and keeps getting up to use the toilet. He must have gone 10 times in the last 30 minutes. When you ask him if he is okay, he says, ‘Yes I’m fine’.
It turns out that Giuseppe has an enlarged prostrate and is not able to urinate properly.
- Why do you think that Giuseppe said he was “fine” when he clearly wasn’t?
A friend comes to visit Giuseppe. She comes to you after the visit and says ‘What’s wrong with Giuseppe?
Does he have prostate cancer? What treatment is he having?’
- How should you answer Giuseppe’s friend?
Question 17
Choose a health and/or community services service that you are interested in.
- What is the function of this service?
Explain how this service interacts with at least two other services.
- Is this service funded? What is one major source of funding?
Q UESTION 18
Describe two ways in which each of the following digital media could be used effectively in a health and community services environment.
Q UESTION 19
- Describe the relationship between legal and ethical frameworks.
- Provide one example of a legal requirement.
- Provide one example of an ethical requirement.
Q UESTION 20
A client discloses to you in confidence that they are considering harming another person. Are you obliged to keep this matter to yourself due to confidentiality requirements? Why or why not?
Q UESTION 21
- Provide an example of person-centred service delivery.
- Provide an example of a multi-disciplinary team and how this team would be used.
- What are two support services that could be accessed by a disability client?
ASSESSMENT TASK 2: CASE STUDIES
- Complete the questions that follow each case study.
W HAT DO I NEED IN ORDER TO COMPLETE THIS ASSESSMENT ?
- Access to textbooks and other learning materials
- Access to a computer and the Internet (if you prefer to type your responses).
W HEN DO I DO THIS TASK ?
- You will do this task in the classroom or as homework – your assessor will advise.
- Write in your due date as advised by your assessor:
W HAT DO I NEED TO HAND IN ?
- Your answers to the questions in each case study.
If your assessor marks any of your answers as incorrect, they will talk to you about resubmission. You will need to do one of the following:
- Answer the questions that were incorrect in writing. ▪ Answer the questions that were incorrect verbally.
- How has the personal care worker breached ethical requirements?
- What would have been the ramifications if Jim had been given antibiotics against the instructions of his wife?
- How did the personal care worker’s values differ from those of Norni, Jim and the doctor?
- What action should be taken by the person who heard the personal care worker’s comments?
Norni is very sad after her husband’s death. She confides in you that she misses him terribly. She is glad that he is finally at peace but is also struggling with her decision to refuse treatment. She knows that is what Jim wanted but wishes he was still with her. She tells you that she can’t sleep at night and does not feel like eating at all. She thanks you for the care that you provided to Jim in his last weeks of life.
- What would you say to comfort Norni?
Norni is so thankful to you for all the support you have given to Jim and her that she presents you with Jim’s gold watch and says she wants you to have it. It is old and looks very valuable.
- Would it be a conflict of interest to accept this gift? Explain your answer.
- What would you say to Norni in regards to the gift she has offered?
- What issues does Maya face regarding communication with staff?
- What issues does Maya face in communication with other residents?
- What assistance can Benny give to other staff to assist them to communicate with Maya?
- Is Maya being rude when she doesn’t look people in the face when talking to them? Explain your answer.
Benny explains the process that will happen when Maya is near death. Various members of her family will gather to be with her. On her death they will conduct a smoking ceremony to purify the room and remove bad spirits. The body will then be taken back to her homeland to be buried.
The health and safety officer says that he understands this is Maya’s custom, but the smoking ceremony cannot be undertaken in her room. This would set off the smoke detectors and other residents may complain about the smoke. He suggests they do the smoking ceremony when her body is back at home.
Benny rolls his eyes and walks out of the room in disgust.
- What are Maya’s rights to the smoking ceremony?
- List two things that Benny can do to support Maya to ensure that her rights are met.
- List three things that Benny and the health and safety officer should do to resolve their differences.
Advise what you would do in Maria’s position.
James is a member of the local hospital board. His father is getting old and frail and has had some medical problems lately. The family is looking for a prioritised place in the local aged care facility. As member of the board, James will have some say in whether his father is offered a prioritised place or not.
- What is the problem in this case study?
- What should be done?
In this situation, nothing is done and James influences the board to approve the priority place for his father. He justifies his action by saying that his father was a clear priority and that the decision would have been the same whether he was on the board or not.
- If this is the case, has James and the rest of the board made an ethical decision? Why/why not?
- What should the rest of the board have done?
- What legislation covers the protection of children against abuse in your state?
- Herriot has a reputation for lying. Does this mean you should decide whether or not she is telling the truth before reporting the allegation? How may the code of ethics assist you with this decision?
- Where can you find information about how to deal with allegations of client abuse inside and outside of your organisation?
- What guidance does a code of ethics give in relation to confidentiality in this case?
- Is Herriot right when she says her mother has no rights because she is not her real mother?
- You realise you will need to report this to your supervisor. When should you do this and what would you do if your supervisor was not available?
- What communication and interpersonal techniques would you use when talking with Herriot?
- You may have personal values that conflict with those of Herriot’s family. How would you deal with this?
ASSESSMENT TASK 3: ROLE PLAYS
There are four role plays in this task. Some role plays have background information that you will need to read and there are also some questions to complete.
- Your assessor will play the role of the client/colleague in each role play.
- You do not have to submit anything for these role plays
If your assessor sees that you have not shown the right skills/techniques during any of the role plays, they will give you some feedback and you will need to do the role play again.
If your assessor marks any of your written answers as incorrect, you will need to either:
- Answer the questions that were incorrect in writing.
R OLE PLAY 1: H ERRIOT AND THE CARE WORKER
This role play is a continuation of Case Study 5 from Assessment Task 2.
In this role play your assessor will play the role of Herriot.
Herriot is going to tell you some things.
You will need to take notes about what Herriot says to you, as you will need to discuss her situation with your supervisor in Role Play 2.
As part of this role play you should:
- Listen to what Herriot has to say. Use verbal and non-verbal communication techniques to show Herriot your concern, show respect, and to make sure you have understood her correctly
- Respond appropriately to what Herriot tells you
- Ask for permission to take notes
- Explain what you will do with the information that Herriot has given you.
Your assessor will refer to the following checklist when observing your performance:
- Demonstrate effective communication skills
- Check understanding and demonstrate empathy and respect
- Respond appropriately
- Respect the confidentiality of the disclosure
- Explain duty of care to client and mandatory reporting requirements
R OLE PLAY 2: H ERRIOT ’ S CARE WORKER AND THEIR SUPERVISOR
This role play is a continuation of Role Play 1 above.
In this role play your assessor will play the role of your supervisor, Ian.
You need to give Ian a verbal report of what Herriot told you. You can refer to your notes during this discussion. You will need to talk about what further action should be taken.
Ian will ask you questions.
- Provide a full, accurate and non-judgmental verbal report of what Herriot has disclosed
- Detail your own responsibilities in this situation
- Describe what actions should be taken next by your organisation, including timeframes
- Listen to your supervisor’s instructions and confirm that you have understood what you need to do and what timeframes you have to do it in.
You are to role play a telephone conversation with Jenienne. She is the daughter of a potential client of your residential aged care facility.
Jenienne is concerned about her father’s rights within the home and the type of care that they will receive. She is also concerned about how information is kept (both electronically and in hard copy) and who will have access to her father’s information.
Your assessor will play the role of Jenienne.
R OLE PLAY 4: E LANA
There are two parts to this task:
- Role playing a discussion with Elana about the storeroom.
- Answering a set of verbal questions related to this scenario.
You have been asked by your supervisor to clean out the storeroom – it has become a workplace hazard. Nothing has been sorted and there is stuff all over the floor.
You are a little concerned because your supervisor has told you to ask Elana to assist you. You know Elana hates doing jobs like this – and the last time you worked with her, she basically told you to get lost!
Your assessor will play the part of Elana. You must ask her to assist you with the storeroom, and try to avoid a conflict. Ian, your supervisor, has asked you to get this done immediately because it is a health and safety hazard.
Following the role play, you will need to answer a set of verbal questions.
ASSESSMENT TASK 4: WORKPLACE TASK
You will need to locate and discuss a number of workplace policies and procedures, and a job description.
W HAT DO I NEED IN ORDER TO COMPLETE THIS ASSESSMENT ? ▪ Access to your work placement service.
- Access to your work placement’s policies and procedures. ▪ A job description for a position in your work placement service
- During one of your assessor’s visits to your work placement service.
- Write in the date of your assessor’s work placement visit:
If your assessor sees that you have not shown appropriate skills or knowledge during any of these tasks, they will give you some feedback and you will need to do the specific task again.
- Answer the questions that were incorrect in writing. Answer the questions that were incorrect verbally.
Instructions: For this task you must to locate the following policies, procedures and codes at your work placement service: Privacy and confidentiality, Access and equity, Reporting of abuse, Code of ethics. You must also locate a job description for a position that you would be interested in. You will discuss each policy and procedure with your assessor – they will ask you questions. Your assessor will ask how each policy and procedure relates to the work you have been doing, or how it relates to the work you have seen others do. Your assessor will ask you a number of questions about the job description you have chosen. Make sure you answer all of their questions to the best of your ability.
ASSESSMENT TASK 5: WORKPLACE TASK – COMMUNICATE WITH CLIENTS
- Students are to be observed communicating with clients in their work placement service.
W HAT DO I NEED IN ORDER TO COMPLETE THIS ASSESSMENT ? ▪ Access to their work placement service ▪ Access to clients. W HEN DO I DO THIS TASK ?
- Write in the date of your assessor’s work placement visit:
If your assessor sees that you have not shown appropriate skills or knowledge during any of these tasks, they will give you some feedback and you will need to do the specific task again. I NSTRUCTIONS :
For this task your assessor will observe you during their visit to your work placement service as you communicate with at least two clients.
This observation may be undertaken in any situation that is relevant to your workplace. For example, you could be assisting the client with activities of daily living, providing assistance to a client, or just having a friendly conversation.
ASSESSMENT TASK 6: WORKPLACE IMPROVEMENTS
For this task you are required to identify and discuss two work practice improvements.
- Access to your organisation’s policies and procedures.
- Access to a computer,
- Access to your supervisor for the meeting (or your assessor will play the role if your supervisor is unavailable). W HEN DO I DO THIS TASK ?
- You will do this while you are on your work placement.
- Write in your due date as advised by your assessor: OR:
- During one of your assessor’s visits to your work placement service (if your supervisor cannot take part in this task). ▪ Write in the date of your assessor’s work placement visit (if applicable):
INSTRUCTIONS:
- Identify two improvements that would enhance work practices within your organisation.
You may choose any types of work practices for this task. Some examples include such things as:
- Redesigning a checklist to make it more user friendly
- Suggesting a change to a work practice to make it more efficient
- Providing additional information to staff (such as using a meeting to share information or putting into a poster or flyer format) ▪ Improving work flow
- Improving communication with clients and carers or family.
- Now you need to write an email to your supervisor that proposes your two suggestions for improvement.
Your email must be written in a professional manner and must include the following information:
- Your description of the improvements.
- The reasons you are suggesting each improvement.
- How each improvement will help staff do their job – including meeting legal and ethical requirements.
- Attach any documents you have designed or redesigned (for example, a revised checklist, revised procedure, poster, work flow chart etc) if appropriate.
You can write your suggestions in dot point form if you wish.
Send your email to your supervisor (or your assessor if your supervisor cannot participate).
- Organise a time to discuss your email and suggestions with your supervisor. If your supervisor is not available, or does not have time to meet with you, you may meet with your assessor instead who will play the role of your workplace supervisor.
You will need to talk about the following in your meeting:
- Why you think each work practice can be improved.
- Each suggestion for improvement.
You must take notes during this meeting.
You must also ask your supervisor for feedback on your suggestions. Ask them:
- If they think your suggestions are a good idea.
- If there other things that need to be thought about.
- If they can suggest any improvements to your suggestions.
- After your meeting with your supervisor (or your assessor), write a short report that provides details about the meeting. Include in your report: ▪ the feedback from your supervisor (or assessor) about your suggestions ▪ any changes that you will need to make to your original suggestions.
ASSESSMENT TASK 7: FEEDBACK AND SKILLS DEVELOPMENT
For this task you are required to obtain feedback on knowledge and skills development.
- Access to your organisation’s policies and procedures. Access to your supervisor for the meeting. When do I do this task? ▪ You will do this while you are on your work placement. Write in your due date as advised by your assessor:
If your assessor marks any of your answers as incorrect, they will talk to you about resubmission. You will need to do one of the following: Answer the questions that were incorrect in writing. Answer the questions that were incorrect verbally. I NSTRUCTIONS :
- You are to meet with your supervisor and ask for advice about what types of skills and knowledge development you will need to pursue a career in community services. Get feedback on your performance during your work placement – what are your strengths and what are your areas for improvement? What advice can your supervisor give you in regards to enhancing your skills and knowledge? How can you get this professional development?
Diploma Universities Assignments
Laureate international universities assignment, holmes institute assignment, yes college australia, acc508 informatics and financial applications task 2 t2, 2019, acc512 accounting, acc520 legal regulation of business structures semester 2, 2019, acct20074 contemporary accounting theory term 2 assessment 3, aero2463 computational engineering analysis : assignment 4, b01dbfn212 database fundamentals assessment 1, be01106 - business statistics assignment, bfa301 advanced financial accounting, bfa504 accounting systems assessment 3, bsb61015 advanced diploma of leadership and management, bsbadv602 develop an advertising campaign, bsbcom603 plan and establish compliance management systems case study, bsbcom603 plan and establish compliance management systems assessment task 1, bsbcom603 plan and establish compliance management systems assessment task 2, bsbcom603 plan and establish compliance management systems assessment task 3, bsbfim501 manage budgets and financial plans assessment task 1, bsbhrm602 manage human resources strategic planning, bsbinm601 manage knowledge and information, bsbwor501 assessment task 3 plan personal development plan project, bsbmgt517 manage operational plan, bsbwhs521 ensure a safe workplace for a work area, bsbwrk510 manage employee relations, buss1030 accounting, business and society, cab202 microprocessors and digital systems assignment help, chc40213 certificate iv in education support, chcage001 facilitate the empowerment of older people, chcage005 provide support to people living with dementia, chcccs023 support independence and wellbeing, chcccs025 support relationships with carers and families, chcdis002 follow established person-centred behaviour supports, chcece019 early childhood education and care, chchcs001 provide home and community support services, comp10002 foundations of algorithms, comp90038 algorithms and complexity, cosc2633/2637 big data processing, cosc473 introduction to computer systems, cpccbc5011a manage environmental management practices and processes in building and construction, cpccbc5018a apply structural principles medium rise construction, cse3osa assignment 2019, elec242 2019 session 2, enn543 data analytics and optimisation, enn543 data analytics and optimisation semester 2, 2019, finm202 financial management assessment 3 group report, forensic investigation case assignment ecu university, ha2042 accounting information systems t2 2019, hc1010 holmes institute accounting for business, hc2112 service marketing and relationship marketing individual assignment t2 2019, hc2121 comparative business ethics & social responsibility t2 2019, hi5002 holmes institute finance for business, hi5003 economics for business trimester 2 2019, hi5004 marketing management t1 2020 individual report, hi5004 marketing management t1 2020 group report, hi5004 holmes institute marketing management, hi5014 international business across borders assignment 1, hi5014 international business across borders, hi5017 managerial accounting t2 2019, hi5017 managerial accounting t1 2019, hi5019 tutorial questions 1, hi5019 strategic information systems for business and enterprise t1 2020, hi5019 holmes institute strategic information systems t2, hi5019 t2 2019, hi5019 t1 2019, hi5020 corporate accounting t3 2019, hi5020 corporate accounting t2 2019, hi6005: management and organisations in a global environment, hi6006 tutorial questions, hi6006 competitive strategy individual t1 2020, hi6006 holmes institute competitive strategy, hi6006 competitive strategy t3 2019, hi6007 statistics for business decisions, hi6007 assessment 2 t1 2020, hi6007 t1 2019, hi6008 t2 2019, hi6008 holmes institute research project, hi6025 accounting theory and current issues, hi6026 audit, assurance and compliance assignment help, hi6026 audit, assurance and compliance, hi6027 business and corporate law tutorial assignment t1 2021, hi6027 business and corporate law t3 2019, hi6027 business and corporate law t2 2019, hi6028 taxation theory, practice and law t2 2021, hi6028 taxation theory, practice and law final assessment t1 2021, hi6028 taxation theory, practice and law t2 2019, hi6028 taxation theory t1 2019, hi6028 taxation law holmes, hltaap001 recognise healthy body systems, hltwhs002 follow safe practices for direct client care, hotl5003 hotel property and operations, hps771 - research methods in psychology a, hs2021 database design, ictict307 customise packaged software applications for clients, ifn619 data analytics for strategic decision makers, inf80028 business process management swinburne university, isy2005 case assignment assessment 2, isys326: information systems security assignment 2, semester 2, 2019, itap3010 developing data access solutions project, itech1103- big data and analytics – lab 3 – working with data items, itech1103- big data and analytics assignment semester 1, 2020, itech 5500 professional research and communication, kent institute australia assignment, ma5830 data visualisation assignment 2, mgmt7020 project management plan, mgt 301 assessment 3, mgt215 project management individual assignment, mis102 data and networking assignment help, mits4002 object oriented software development, mits5002 software engineering methodology, mkt01760 tourism planning environments assessment 4, mkt01760 tourism planning environments, mkt01906 international tourism systems, mkt5000 marketing management s2 2019, mng03236 report writing scu, mre5003 industrial techniques in maintenance management assignment 4, mre5003 industrial techniques in maintenance management assignment 3, mre5003 industrial techniques in maintenance management, network security and mitigation strategies answers, nit2213 software engineering assignment, nsb231 integrated nursing practice assessment task 1, science literacy assessment 4, sit323 practical software development t 2, 2019, sit718 using aggregation functions for data analysis, sitxcom002 show social and cultural sensitivity, tlil5055 manage a supply chain, tlir5014 manage suppliers, usq acc5502 accounting and financial management, uts: 48370 road and transport engineering assessment 2, chcccs011 meet personal support needs, chcccs015 provide individualised support, chccom005 communicate and work in health or community services, chcdis001 contribute to ongoing skills development, chcdis003 support community participation and social inclusion, chcdis005 develop and provide person-centred service responses, chcdis007 facilitate the empowerment of people with disability, chcdis008 facilitate community participation and social inclusion, chcdis009 facilitate ongoing skills development, chcdis010 provide person-centred services, chcdiv001 work with diverse people, chcleg003 manage legal and ethical compliance, hltaid003 provide first aid, hlthps007 administer and monitor medications, hltwhs002 follow safe work practices for direct client care, assignment 2 introduction to digital forensics, mgt603 systems thinking assessment 1, mgt603 systems thinking assessment 2, hi5017 managerial accounting t1 2021, hi6028 taxation theory, practice and law t1 2021, oodp101 assessment task 3 t1 2021, itne2003r network configuration and management project, australia universities, australian catholic university, australian national university, bond university, central queensland university, charles darwin university, charles sturt university, curtin university of technology, deakin university, edith cowan university, flinders university, griffith university, holmes institute, james cook university, la trobe university, macquarie university, monash university, murdoch university, queensland university of technology, rmit university, southern cross university, swinburne university of technology, university of adelaide, university of ballarat, university of canberra, university of melbourne, university of newcastle, university of new england, university of new south wales, university of notre dame australia, university of queensland, university of south australia, university of southern queensland, university of sydney, university of tasmania, university of technology sydney, university of the sunshine coast, university of western australia, university of wollongong, victoria university, western sydney university, year 11 - 12 certification assignment, australian capital territory year 12 certificate, hsc - higher school certificate, ntce - northern territory certificate of education, qce - queensland certificate of education, sace - south australian certificate of education, tce - tasmanian certificate of education, vce - victorian certificate of education, wace - western australia certificate of education.
Assignment Service Australia | CDR Writing Help | TAFE Assignment Help | Perth Assignment Help | Melbourne Assignment Help | Darwin Assignment Help | Adelaide Assignment Help | Assignment Help Victoria | Sydney Assignment Help | Canberra Assignment Help | Brisbane Assignment Help | CDR for Australian immigration | Course For Australian History
- MassiveMark Playground
- Transliteration Playground
- Professional Practice Test
- Assignmenthelp Services
- Custom Writing help
- Free Assignment Samples
- Free Homework Help Samples
- Terms of Use
- Refund Policy
- 🇸🇪 Svenska ›
- 🇫🇮 Suomeksi ›
- 🇩🇪 Deutsch ›
- 🇫🇷 Français ›
- 🇺🇸 English (US) ›
- +44 20 8133 4551
- +44 151 808 2343

Heriot-Watt University
Fed up of time-consuming health and safety reporting, Herriot-Watt University uses Info Exchange to digitise and simplify it's processes.
About Herriot-Watt University
Founded in 1821, Heriot-Watt has a rich heritage and is valued for its pioneering research informed by the global needs of business and industry. The university hosts over 7,000 students and prides itself on being one of the leading universities in the UK.
Increasing visibility and scope across all business processes
Before Heriot-Watt implemented a digital system, they faced the same challenges as many other organisations when trying to manage many processes using paper-based systems.
"Info Exchange has enabled us to have access to the right information, in the right place and at the right time. This is the functionality we need to be able to react to things and resolve any issues that may occur."
Before they implemented a digital health and safety process, the victim of an accident would complete a paper form that would then be sent to their local safety officer to review and add comments. This would then have to be passed to their health and safety team as a physical document. As a result, the time it took to complete this process could range from a few days to a few weeks and there were often times where the paper forms would be lost. A similar, cumbersome process was involved with the security teams at the university. If an incident happened, the team had to search through over 50 paper forms to find the right one to complete and then pass to various people. As a result of this, the visibility of the accidents and incidents across the university was poor, the paper forms resulted in a duplication of effort and there were delayed response times. In 2014, Heriot-Watt decided to digitise their processes. Lorraine commented that “students are constantly on their phones, so using the new technology means we have direct access to communicate with them.”
The software platform enabled Heriot-Watt to have the right information, in the right place and at the right time which is imperative to the immediate response to any accidents or incidents.
It enabled them to save time as they had the functionality to report accident rates and trends at the touch of a button, something that would normally take Lorraine and her team weeks to complete. The use of remote forms means that everyone has access to the system instantly, improving the data collection to all. Since implementing the system, Heriot-Watt have extended their use to include travel declarations. This was a key feature for Lorraine when students were caught up in the terrorist attack that took place in Strasbourg in December 2018. They were able to locate all their students within 20 minutes and communicate with them to ensure they were safe. Historically, this was something that would have previously taken up to 48 hours to complete when they didn’t have a digitised solution to enable this. Lorraine has been so impressed with Info Exchange that she has extended the scope of the software to include driver declarations and even supply chain management.
Discover more about Info Exchange
See exactly how our software can work within your current processes to help you grow a positive safety culture.
.png)
Hannah Daly
Account Manager, EcoOnline Ireland
Trusted by 10,000+ customers worldwide
With the knowledge from 90 different industries we have developed our platform to make sure it tailors to your needs. Don't take our word for it.

Select your location
- North America English
- Brazil Português
- Latin America Español
Asia Pacific
- Australia English
- Germany Deutsch
- Spain Español
- United Kingdom English
- Benelux Dutch
- Italy Italiano
Canvas by Instructure
Heriot-Watt Case Study
Heriot-Watt move from Blackboard to Canvas to increase student engagement and support Responsive Blended Learning

UK, Dubai, Malaysia
30,000 Users
Adopted Canvas 2020
Heriot-Watt is a global university focused on delivering innovative, worldwide education. Since 1821 the community of scholars that founded the institution have been ‘developing transformational solutions to specific global problems.’ With campuses in the UK as well as Dubai and Malaysia, Heriot-Watt specialises in STEM subjects, producing leaders in engineering, business and science.
The Challenge
Following the introduction of Responsive Blended Learning across Heriot-Watt University, the need for a fresh, updated VLE, with greater consistency across navigation, was identified to help support the move to online and blended learning and meet Heriot-Watt’s ambitions for the future. Heriot-Watt’s top drivers included ensuring a smooth integration between the Student Information System (SIS) and the VLE, achieving a level of consistency across all campuses and having more methods of delivering feedback. Staff and student satisfaction were key and both groups were involved in the transition process.
Key Insights
Staff at Heriot-Watt have enthusiastically adopted Canvas, with students being equally engaged.
The introduction of Responsive Blended Learning, and the support of Canvas in delivering this, has proved very successful.
Feedback from Heriot-Watt's Digital Capabilities survey highlights Canvas as a favourite learning tool, adding that students appreciate the consistency between courses.
The Solution
Heriot-Watt chose Canvas as the appropriate technology to support the implementation of the Learning and Teaching Strategy to deliver inspiring learning for all students. After selecting Canvas, Heriot-Watt engaged with other institutions using the platform to draw on sector experience and maximise positive outcomes. The University has benefitted from Canvas tools that support student engagement, receiving positive feedback on assessment tools and feedback functionality within the Canvas Speedgrader. Canvas Discussions is also a great way for promoting engagement as students can reply in threads, comments can be moderated by academics, and responses can also be hidden until a student posts their own response, encouraging everyone to participate.
The key to an effective implementation is building trust with staff. The Canvas project team responding quickly and with compassion to staff queries made staff feel supported and engaged with the system.
Rosemarie Mcllwhan, Associate Professor of Learning and Teaching Enhancement
Collaboration is Key
To ensure a successful Canvas implementation, Heriot-Watt prioritised collaboration across teams within the University. A strong partnership between the Information Services Team (IS) and the Learning and Teaching Academy (LTA) ensured appropriate technological implementation informed by effective learning and teaching practice and pedagogy. Collaboration between the Canvas Project Team and the Schools across the University was also crucial to ensuring that the implementation of Canvas met the needs of staff and students. Heriot-Watt used K16 to help migrate content from their previous VLE, Blackboard, to Canvas, carrying out the entire implementation during the lockdown. The smooth transition across campuses in different time zones, while staff adapted to delivering courses completely online due to Covid-19, is a testament to the hard work, dedication and collaboration across several teams
Driving Adoption
Ensuring staff and student buy-in was identified as vital to Canvas implementation so Heriot-Watt worked hard to ensure staff and students were included and engaged at every step of the process. Firstly, the Canvas Academic Reference Group (CARG) comprising of representatives from all Schools, academic programmes and Student Associations, chaired by the Canvas Academic Lead from the LTA gave staff and student a direct route to influence decisions and policy. CARG also advised on the design and use of Canvas course sites and ensured that training and guidance were fit-for purpose to meet everyone’s needs. A series of townhall meetings were held in the University’s Schools which were co-presented by the Canvas Academic Lead and representatives from the Information Services team. These sessions were useful in identifying key needs, issues and answering questions. They also enabled rapid response and direct communication, helping build trust with staff. Thirdly, engagement through the University senior management group ensured senior buy-in and support. A key success was the ongoing communication via CARG enabling both academic and professional services staff to buy-in and feel they had options to shape the implementation of Canvas throughout the process.
Student adoption was supported through targeted communications for new and existing students, a peer-led training project and use of the Canvas Student Guides. With Canvas being easy to use, few students required additional training and were happy with the consistent and up-to-date guidance displayed in the Canvas Student Guides.
The Results
The biggest change across the University has been consistency in the use of VLE, making it easier for students and staff to access relevant learning resources. Staff are also keen to maximise the features of a VLE to improve teaching and learning. Heriot-Watt aim to maintain the consistency they have implemented globally by introducing VLE benchmarks which provide a baseline for the use of Canvas. They also plan to continue support the adoption of Canvas features which are pedagogically appropriate and will help the University to achieve its vision of delivering inspiring learning.
Heriot-Watt move from Blackboard to Canvas
Download Case Study
Discover More Topics:

- Request new password
- Create a new account
Introduction to Abnormal Child and Adolescent Psychology
Instructor resources, case studies.
Teaching notes for cases, designed to help instructors expand questions to students or initiate class discussion, include a brief summary of each case, and sample answers to case questions.
› Case Study Contents
Chapter 1: The Science and Practice of Abnormal Child Psychology
Normality vs. abnormality across development.
Mental health professionals have long struggled with the best way to differentiate mental disorders from mental health. The DSM-5 conceptualization of mental disorders borrows heavily from Jerome Wakefield’s (1992) notion of “harmful dysfunction.” According to Wakefield, disorders reflect an underlying genetic, biological, or psychological dysfunction that causes harm to the individual. The DSM-5 definition of a mental disorder is reproduced below:
A mental disorder is a syndrome characterized by clinically significant disturbance in an individual’s cognition, emotion regulation, or behavior that reflects a dysfunction in the psychological, biological, or developmental processes underlying mental functioning. Mental disorders are usually associated with significant distress or disability in social, occupational, or other important activities. An expectable or culturally approved response to a common stressor or loss, such as the death of a loved one, is not a mental disorder. Socially deviant behavior (e.g., political, religious, sexual) and conflicts that are primarily between the individual and society are not mental disorders unless the deviance or conflict results from a dysfunction in the individual, as described above. (American Psychiatric Association, 2013, p. 20)
Read each of the brief case studies below. Using the DSM-5 definition above, determine if the child in each case study has a mental disorder. If there’s not enough information in the case study, identify any other information would you need to determine if he or she meets the DSM-5 definition.
- Margaret wets the bed at night. Her parents discover her wet the next morning and spend a great deal of time and energy washing her pajamas and bedding.
Margaret may meet the DSM-5 definition of a mental disorder, but we would need additional information. Some information that would be helpful includes the following:
- How old is Margaret? DSM-5 requires clinicians to consider children’s age when diagnosing mental disorders. If Margaret was a 2-year-old, wetting the bed would be developmentally normative and not an indicator of a disorder. However, if Margaret was 8 years old, wetting the bed might be developmentally atypical and a clinically significant problem.
- Does Margaret experience distress or impairment associated with her bedwetting? Some children wet the bed but do not experience distress (e.g., embarrassment, guilt) or impairment (e.g., limitations in daily functioning). If Margaret felt shame because she wet the bed or if she could not attend a sleepover at a friend’s house because of her bedwetting, she might have sufficient distress or impairment to merit a diagnosis.
Note that DSM-5 adopts a medical conceptualization of mental disorders. Like medical illnesses, mental disorders are believed to exist within individuals. Margaret’s bedwetting might cause her parents distress (e.g., anger) or impairment (e.g., lost sleep and daytime fatigue). Technically, distress or impairment in others is not sufficient to merit a diagnosis for most DSM-5 disorders. However, most clinicians who work with children emphasize the effects of the child’s behavior problem on the entire family, rather than on the child alone.
- Is Margaret’s bedwetting better explained by a medical condition? DSM-5 differentiates problems caused by medical conditions from problems caused by mental disorders. In some sense, this dichotomy is artificial because nearly all mental disorders have genetic and biological factors that cause or maintain them over time. (See Chapter 2.) Nevertheless, we would not diagnose Margaret with a mental disorder if her bedwetting is likely caused by a medical condition (e.g., a urinary tract infection), or a medication (e.g., a diuretic). Chapter 16 provides more information about how clinicians work with medical professionals to help children with health-related problems such as elimination disorders, sleep disorders, and chronic medical conditions.
- Shawn is afraid to ride elevators. Every time he is in an elevator, he experiences intense feelings of panic. He tries to avoid elevators whenever he can.
In order to determine if Shawn has a mental disorder we need evidence that he experiences distress or disability/impairment. Many children have fears that do not merit diagnosis or treatment. For example, many youths (and college students) are afraid of spiders and snakes, but very few seek treatment. Although these stimuli produce considerable distress, they usually do not lead to marked impairment in daily functioning.
In the case of Shawn, we’d need to know if his fear and avoidance of elevators limits his life in any significant way. For example, if Shawn lives in a rural area, he probably doesn’t encounter elevators very often. When he does, he can probably take the stairs to avoid them with little trouble. On the other hand, if Shawn lives in an urban area, and his apartment is on the 15th floor of a large building, his avoidance of elevators probably has a major impact on his daily life.
Chapter 11 provides more information about differentiating adaptive anxiety from anxiety disorders.
- Charlotte is a teenage girl whose father died of a heart attack. Charlotte isn’t eating or sleeping well. She can’t concentrate on her homework or activities at school. Sometimes, at night, she talks with her father about her day before she falls asleep. She also thinks a lot about death.
Charlotte is clearly exhibiting distress and impairment. However, we would need additional information before diagnosing her with a mood disorder, such as major depressive disorder. DSM-5 differentiates mental disorders from bereavement, that is, a culturally expected response to the death of a loved one.
Differentiating bereavement from depression and other mental health problems can be tricky. Three bits of additional information might help us differentiate the two conditions:
- How recently did Charlotte’s father die? If his death was sudden, and it occurred only a few weeks ago, most clinicians would regard Charlotte’s response as bereavement. If his death occurred several years ago, and Charlotte continues to experience such high levels of distress and impairment, we might consider her behavior an indicator of a mood disorder.
- Does Charlotte experience thoughts about suicide? According to DSM-5 , it is not uncommon for people who are experiencing bereavement to have thoughts about death and dying. For example, an adolescent might wonder what it is like to die or if anyone would mourn her if she died. However, suicidal ideation is usually an indicator of a mental disorder rather than bereavement. Does Charlotte have thoughts about killing herself? Does she have a suicide plan? Would she like to die?
- Does Charlotte experience auditory or visual hallucinations? Hallucinations are perceptions (e.g., sounds, visions) that do not correspond to reality. Most adolescents with schizophrenia experience hallucinations and problems with self-care, like Charlotte. Although it is unlikely that Charlotte has schizophrenia, we would need to rule out that possibility by asking her if she hears or sees images of her father when she talks with him.
- indicates that hearing or seeing recently deceased loves ones may be an indicator of bereavement rather than schizophrenia. To differentiate the two conditions, we would need to determine if Charlotte has other hallucinations (i.e., not involving her father), if she has delusions (i.e., bizarre thoughts that do not correspond to reality), or other signs and symptoms of schizophrenia such as disorganized speech, disorganized actions, or flat affect. The presence of these other signs and symptoms might suggest a mental disorder rather than bereavement. Even if Charlotte is experiencing bereavement, rather than a mental disorder per se, most clinicians would recommend psychotherapy to prevent the emergence of more lasting distress or impairment. Interpersonal psychotherapy, discussed in Chapter 4, is designed to help individuals cope with the loss of a loved one. It might be a particularly useful treatment for Charlotte.
Chapter 13 discusses the features of depressive disorders in adolescents, methods to assess suicidal ideation and suicide risk, and techniques to prevent and treat depression and suicidal behavior. Chapter 14 discusses the signs and symptoms of schizophrenia in adolescents.
References:
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders, fifth edition. Washington, DC: Author.
Wakefield, J. (1992). Disorder as harmful dysfunction. Psychological Review , 99 , 232–247.
______________________________________________________________________________
Weis, R. (2017). Introduction to Abnormal child and adolescent psychology, Third Edition. Thousand Oaks, CA: Sage.
Continuity vs. Change Across Development
Developmental psychopathology is a multidisciplinary approach to understanding normal and abnormal development over the lifespan. It conceptualizes development in terms of risk and protective factors that place individuals on developmental pathways toward adaptation or maladaptation.
Developmental psychopathologists are interested in stability versus change in development. Almost a century ago, Sigmund Freud wrote about the difficulty in predicting children’s development:
So long as we trace development from its final outcome backwards, the chain of events appears continuous. . . . But if we proceed the reverse way, if we start from the premises and try to follow these up to the final result, we notice at once that there might have been another result and we might have been just as well able to understand and explain the latter. Hence the chain of causation can always be recognized with certainty if we follow the line of analysis backwards, whereas to predict it is impossible. (from Sroufe & Rutter, 1984)
Read the scenarios below and answer each question. What principle of developmental psychopathology does each scenario illustrate?
1. Sebastian is a 14-year-old boy with a longstanding history of attention-deficit/hyperactivity disorder (ADHD). He began to show problems with hyperactivity and impulsivity as a preschooler. In early elementary school, he also began exhibiting poor attention and concentration. Now in the eighth grade, Sebastian continues to show problems with restlessness, talkativeness, and impulse control as well as inattention, forgetfulness, and distractibility. He manages these symptoms with medication and behavioral interventions administered by his parents and teachers.
What principle of developmental psychopathology does Sebastian illustrate?
Sebastian illustrates homotypic continuity , the tendency of certain disorders to persist, relatively unchanged, from childhood through adolescence or adulthood. Certain disorders such as ADHD, autism spectrum disorder, and intellectual disability often show homotypic continuity. The article by Reinke and Ostrander (2008) examines stability and change from childhood through adolescence for the major childhood disorders.
Reinke, W. M., & Ostrander, R. (2008). Heterotyic and homotypic continuity: The moderating effects of age and gender. Journal of Abnormal Child Psychology , 36 , 1109–1121.
2. Haley is a 17-year-old high school student with a history of separation anxiety disorder. In early childhood, she followed her parents around the house and cried when they left her with a babysitter. Haley refused to attend preschool and was resistant to begin kindergarten when she turned 6 years old. In early elementary school, Haley’s separation anxiety decreased, but she continued to worry about “bad things” happening to her parents when she was separated from them.
Now in high school, Haley reports no significant problems with separation anxiety. However, in the past 6 months, she has experienced several panic attacks—intense episodes of fear characterized by rapid heart rate, shallow breathing, and intense distress. Her pediatrician confirmed that these attacks are not caused by a medical problem. Her mother has sought help from a psychologist who specializes in adolescent anxiety disorders.
What principle of developmental psychopathology does Haley illustrate?
Haley illustrates heterotypic continuity , the phenomenon in which children’s symptoms change over time, but their underlying behavioral or social-emotional problems remain the same. Like many adolescents with recurrent panic attacks, Haley has a history of separation anxiety disorder in childhood. Both problems reflect underlying difficulty with anxiety. Indeed, Kossowsky and colleagues (2013) showed that children with separation anxiety disorder are three times more likely to develop panic disorder in adolescence or adulthood than children without separation anxiety disorder.
Kossowsky, J., Pfaltz, M. C., Schneider, S., Taeymans, J., Locher, C., & Gaab, J. (2013). The separation anxiety hypothesis of panic disorder revisited: A meta-analysis. American Journal of Psychiatry , 170 , 768–781.
3. The juvenile court in one county hears cases for approximately 75 youths and families each month. Most cases involve older children and adolescents with substance use problems and antisocial behavior. What causes these problems? What principle of developmental psychopathology does this scenario illustrate?
It is not possible to point to a single cause of adolescent substance use problems and antisocial behavior. This scenario illustrates the principle of equifinality . Two youths who experience the same developmental outcomes (e.g., arrest because of substance use problems and antisocial behavior) can have different histories. For example, some youths develop substance use problems because they inherit a genetic susceptibility to such problems, others use alcohol and other drugs to alleviate anxiety or depression, and still others are introduced to alcohol and other drugs by deviant peers. These, and other, pathways to adolescent substance use problems are presented in Chapter 10.
4. You are a social worker who works for children’s protective services in your county. You are assigned a new case, an 11-year-old girl who experienced repeated sexual abuse by her stepfather. What is her prognosis? What principle of developmental psychopathology does she illustrate?
Even if we had much more information, it would be challenging to predict the girl’s long-term outcome. The scenario illustrates the developmental principle of multifinality . Two children exposed to the same psychosocial stressor (e.g., sexual abuse) can have different developmental outcomes.
It is likely that this girl’s developmental outcome will depend on risk and protective factors through her life. Possible risk factors include the severity of the abuse, duration of the abuse, and other psychosocial stressors in her childhood (e.g., poverty, neighborhood disadvantage). Possible protective factors include a supportive nonoffending parent, access to high-quality medical treatment and psychotherapy, and supportive relationships with other family members and peers. For example, Godbout and colleagues (2014) showed that the long-term outcomes of children exposed to sexual abuse depended on the level of support they received from a nonoffending parent.
Godbout, N., Briere, J., Sabourin, S., & Lussier, Y. (2014). Child sexual abuse and subsequent relational and personal functioning: The role of parental support. Child Abuse and Neglect , 38 , 317–325.
Sroufe, L. A., & Rutter, M. (1984). The domain of developmental psychopathology. Child Development , 55 , 17–29.
Weis, R. (2017). Introduction to Abnormal Child and Adolescent Psychology, Third Edition . Thousand Oaks, CA: Sage.
Chapter 2: The Causes of Childhood Disorders: A Levels of Analysis Approach
Opioid use disorder across multiple levels of analysis.
Just like the characters in The Blind Men and the Elephant , we obtain a more complete picture of something when we look at it from multiple perspectives. Developmental psychopathologists look at childhood disorders across multiple levels of analysis: genetic, biological, psychological, familial, and social–cultural. Then, they combine information from across these levels to explain how disorders emerge over time.
Now it’s your turn to apply the various levels of analysis presented in the text to a clinical case. Read the case study and briefly explain how Valerie’s disorder can be explained in terms of each level, and how the levels might interact with each other, over time, to shape development.
Description:
Valerie Connell was a 16-year-old girl who was referred to an inpatient residential treatment program for adolescents with substance use disorders. Val was ordered to participate in treatment by the juvenile court after she was arrested for opioid possession and distribution.
Val grew up in a western suburb of Chicago. Her father was a musician with a history of alcohol and marijuana use problems. He left Val and her mother when Val was 5-years-old. Although he continued to live in the Chicago area, he had only occasional contact with Val. Val had mixed feelings about her father. On one hand, she was attracted to his glamorous lifestyle: performing, traveling, and socializing. On the other hand, she resented his decision to abandon his family when she was so young and harbored anger toward him because of the many times he disappointed her over the years. “If your own dad doesn’t care about you, no one will,” said Val. “I saw myself as pretty worthless—like no one will ever really love me.”
Val’s mother also had a history of alcohol use. She became pregnant with Val when she was 17, a single parent by the time she was 22, and a recovering alcoholic by the time she was 26. Mrs. Connell attends Alcoholics Anonymous meetings to maintain her sobriety and supports herself and Val by working two jobs. Long hours limit her ability to be involved in Val’s school or extracurricular activities. Although she says, “Val means the world to me—the one thing I live for,” she admits that stress at work and concerns about her ability to pay the bills “sometimes cause me to lose my temper with her.”
Val exhibited problems with hyperactivity and oppositional behavior as a preschooler. “She was a handful,” recalled her mother. “She’d always be on the go, she never wanted to be quiet and listen to me. If I would tell her to do something, she’d ignore me, yell, or scream.” Val’s disruptive behavior persisted into elementary school. Her pediatrician prescribed stimulant medication to manage her hyperactive-impulsive behavior, but it had little effect on her defiance and tantrums. By the time Val was in the third grade, she was behind her classmates in reading and math and had gained a reputation as a troublemaker.
Val’s substance use began with her transition to middle school. She was referred to a special education program for children with behavior problems and learning disabilities. She quickly made friends with several girls who introduced her to smoking (age 12) and marijuana (age 13). Although she tried alcohol at approximately the same age, she did not like its taste and limited its use to parties and social gatherings. By the time Val was 14 years old, she was using marijuana several times per week and drinking five to six sweet alcoholic drinks at parties on the weekends. She found it relatively easy to hide her substance use from her mother.
Val transitioned to an alternative high school during her freshman year. “All of the kids there used drugs,” Val recalled. Her 17-year-old boyfriend introduced her to prescription pain medication. Val’s favorite combination was OxyContin in the morning followed by Roxicodone periodically throughout the school day. She quickly became known as the “Oxy and Roxy” girl. “I’d sleep during class, slur my speech, didn’t care about anything,” she recalled. “The teachers didn’t say anything to me because I didn’t cause trouble, so I kept on going.” Val obtained $10 pills from her boyfriend and sold them to classmates for $25, pocketing the profits to support her own drug use.
“I first used heroin with my boyfriend—a different boyfriend—during my sophomore year,” Val reported. “I was afraid of needles so I snorted it. The feeling was excellent, like all the pain in my life was taken away. I could relax, stay still, and not worry about school or family. Snorting worked much faster than taking pills and the effects of heroin were much better.” Within 6 months, Val was using heroin approximately four times per day to sustain its positive effects and avoid withdrawal symptoms such as anxiety, nausea, and agitation. Her use became expensive and she engaged in prostitution several times to support her habit.
“It might seem crazy, but I’m kind of glad that I got caught,” Val reported. “I’ve been to the funerals of two friends who died from heroin. My life was on the wrong track.” In residential treatment, Val was prescribed a medication called Suboxone, a combination of buprenorphine (an opiate substitute that reduces cravings) and naloxone (a medication that blocks the positive effects of heroin). The physician and psychologist at the residential treatment facility hope that it will help her reduce her opioid use (see Fiellin et al., 2014).
“I’m not sure what I’m going to do when I get out of here,” reported Val. “My mom wants me to come back home, but I can’t go back. Everyone I know uses. I need a clean break.”
Discussion Questions:
1. How might you explain Val’s substance use disorder in terms of behavioral genetics and epigenetics?
Behavioral geneticists are interested in the degree to which genetic factors contribute to the emergence of psychological disorders. They would be interested in determining whether individuals with high genetic similarity have greater behavioral concordance than individuals with lower genetic similarity. It is possible that Val inherited a genetic diathesis toward substance use disorder from her parents, both of whom have histories of substance use problems themselves.
Epigenetics refers to the degree to which environmental factors can influence the expression of specific genes. For example, Val might inherit a genetic diathesis toward a substance use disorder. However, early environmental risk factors may have influenced the expression of this risk. For example, her father’s decision to leave his family when Val was a child, her mother’s high level of parenting stress, or the family’s socioeconomic hardships could have placed Val at greater risk for a substance use disorder later in life.
2. How might you explain Val’s problems with (1) hyperactivity-impulsivity and (2) substance use in terms of the brain and neurotransmitters?
Val was diagnosed with ADHD in childhood. ADHD is a neurodevelopmental disorder that is associated with underactivity in brain regions associated with attention and behavioral inhibition (e.g., prefrontal cortex). The neurotransmitter involved in these brain regions is dopamine, a major excitatory neurotransmitter. It is possible that dysregulation of dopaminergic pathways in these brain regions underlies her ADHD symptoms. These ADHD symptoms, in turn, may contribute to her substance use problems. Detailed information about the brain’s involvement in ADHD is presented in Chapter 8.
Other brain regions play a role in the emergence and maintenance of substance use disorders. Specifically, a neural pathway that runs from the midbrain (e.g., nucleus accumbens, ventral tegmental area) to the frontal lobe operates as the brain’s “reinforcement center” and is associated with feelings of pleasure in humans. The neurotransmitter involved in this pathway is also dopamine. Most addictive substances stimulate the release of dopamine along this pathway, producing feelings of euphoria. Unfortunately, prolonged use of these substances can cause a reduction in the release of dopamine, the number of dopamine receptors, or the sensitivity of dopamine receptors over time. Consequently, individuals who use these substances for long periods of time (like Val) must take more of the substance to experience the same effects (i.e., tolerance). If they discontinue using the substance, they will likely experience withdrawal symptoms. Detailed information about the brain’s involvement in substance use disorders is presented in Chapter 10.
3. How might you use learning theory to explain Val’s substance use disorder?
Operant conditioning can be used to explain the cause and maintenance of substance use disorders. Opioids initially cause euphoria, which can be positively reinforcing. Furthermore, they can reduce feelings of physical pain and negative affect, which can be negatively reinforcing.
Observational learning (modeling) may also play a role in Val’s substance use problems. It is likely that Val learned to use substances, or overcame her fear of using substances such as heroin, by observing peers use these substances. Vicarious reinforcement, therefore, strengthened her own substance use.
Finally, classical conditioning might interfere with Val’s ability to abstain from opioid use after she completes inpatient treatment. Specifically, Val stated that she is reluctant to return to her old neighborhood and school because many of her former friends use substances. Through classical conditioning, Val may associate these people and places with opioids. Consequently, she may experience cravings when she returns to her old surroundings.
4. How might problems with cognition or emotion regulation contribute to Val’s substance use problems?
Social cognition refers to the capacity to think about social situations in objective, flexible ways. Val seems to have developed a schema for relationships in which she sees other people as disappointing or rejecting and sees herself as worthless and unlovable. This schema may contribute to feelings of dysphoria that might prompt her substance use. A primary goal of cognitive therapy is to challenge maladaptive or distorted cognitions that can contribute to dysphoria in this manner.
Emotion regulation refers to the ability to recognize, label, and control the expression of emotions in adaptive ways. She may also use substances, such as marijuana and opioids, to reduce negative affect and regulate her emotions.
5. How might Val’s parents and peers contribute to her substance use problems?
Based on the information in the case study, we might speculate that Val had a “difficult” temperament early in life. Her high-rate behavior probably provided a poor fit with her father’s absence and her mother’s substance use problems and work-related stress. The result of this poor fit between Val’s temperament and her parents’ capacity for care likely contributed to Val’s disruptive behavior problems.
Val’s mother shows low responsiveness and demandingness, the essential characteristics of an “uninvolved” parent. It is likely that her own substance use history and work-related stress compromised her ability to attend to her daughter. Although she dearly loves Val, she lacks the resources to provide sensitive and responsive care and to monitor Val’s activities. Prospective studies indicate that children of uninvolved parents often have the poorest developmental outcomes. Like Val, they tend to show low academic achievement, behavior problems, and dysphoria.
Val was rejected by prosocial peers in early elementary school. Consequently, she encountered a deviant peer group that introduced her to progressively more serious substances. It is likely that Val used these substances to gain acceptance into this new peer group who modeled and reinforced continued substance use. Chapter 10 presents additional information about the deviance-prone model for adolescent substance use disorders, the theoretical model that seems to apply to Val.
6. How might social–cultural factors contribute to Val’s substance use problem?
Social–cultural influences are usually thought of as distal risk factors for child and adolescent disorders. They contribute to the emergence or development of these disorders indirectly, by adversely impacting the family, peer group, school, neighborhood, or broader society. In Bronfenbrenner’s bioecological systems theory (presented in this chapter), these influences often fall within the exosystem.
Two social–cultural factors that likely contributed to Val’s substance use problems are (1) socioeconomic disadvantage and (2) low-quality schools. Socioeconomic disadvantage likely prompted Val’s mother to work long hours, which added to her chronic stress and compromised her ability to be involved in Val’s schooling and to monitor Val’s behavior. Similarly, Val’s school system seems to have failed her. School officials largely overlooked Val’s emerging behavior and substance use problems until it was too late.
Bronfenbrenner also recognized how the overall social–cultural climate in which children live (i.e., the macrosystem) can contribute to the development of mental health problems. The increased use of prescription pain medications in our culture has led to a corresponding increase in opioid use disorders more generally. Many individuals who are initially prescribed opioids to manage pain caused by illness or injury, eventually become dependent on opioids. Some turn to heroin, a less costly and more plentiful alternative to prescription pain medication in many communities.
Fiellin, D. A., Schottenfeld, R. S., Cutter, C. J., Moore, B. A., Barry, D. T., & O’Connor, P. G. (2014). Primary care–based buprenorphine taper vs. maintenance therapy for prescription opioid dependence: A randomized clinical trial. JAMA, 174 , 1947–1954.
Weis, R. (2017). Introduction to Abnormal Child and Adolescent Psychology, Third Edition . Thousand Oaks, CA: Sage. The case study is based on interviews conducted by Paul Grondahl for the Albany Times Union .
Butterfly Di: A Case of Gene-Environment Correlation
Scarr and McCartney’s (1983) notion of gene–environment correlation can be used explain the way genotype and environment affect each other to shape development. The text presents the case study of Kirby, a boy with emerging disruptive behavior problems. However, gene–environment correlation can also be applied to children whose development seems to be coming along “swimmingly.” Read the case study below and identify how the theory of gene–environment correlation can be applied to Diana’s development.
Diana was born to swim. Her mother was an Olympic athlete whose relay medley team won the bronze medal in Atlanta. Today, she is the head swim coach at a Division II college in Diana’s hometown. Although not a swimmer, her father was a Division I baseball player who currently works as a personal trainer. Diana also has two older sisters who earned college scholarships for swimming and diving, respectively.
Diana was a healthy baby who enjoyed all of the benefits of a health-conscious family. Her father, who studied nutrition in college, was extremely conscientious about his family’s eating habits. Diana and her sisters ate a largely vegetarian diet and received excellent medical care. Her mother decorated Diana’s room in an aquatic theme: blue walls, fish-patterned bedsheets, an octopus pillow, and a dolphin nightlight.
Diana began taking swim lessons at the age of 18 months. She was more agile in the pool than on land. Her mother would swim with her and her sisters several times per week. Diana also attended her older sisters’ swim lessons and, later in her childhood, she would also attend their swim meets.
Diana began to swim competitively at the age of 5 for a summer aquatic league. By the time she was 7, she was swimming year-round for a 10 and under recreational team at the YMCA and winning many of her events. One of the coaches recognized her raw talent and invited her to join his travel team that practiced at the local college. Diana joined the team several months later, practiced 5 days per week, and received individual lessons from the head coach.
Diana swam on the varsity team during her freshman year of high school. She excelled in all events, especially the butterfly. Diana bonded with other girls on the team and had success in the pool and in the classroom.
Now 17-year-old Diana is beginning her final year as a high school swimmer. A shoulder injury sustained in a car accident earlier in the year slowed down her stroke and probably eliminated her chances of a Division I scholarship. However, Diana has visited several Division III schools with excellent swimming programs that would provide her with a good education and an opportunity to swim competitively for 4 more years. “Swimming’s not the only thing important in my life, but it’s a major part of it,” Diana said. “I can’t imagine giving it up just yet.”
1. How does Diana illustrate passive gene–environment correlation?
Diana likely inherited genes that predispose her toward a high degree of athleticism. At the same time, her parents provided her with early environmental experiences that are conducive to healthfulness and athletic ability. For example, they gave her access to high quality nutrition and health care, encouraged physical activity, and promoted an interest in swimming by decorating her room in a swim motif and giving her swim lessons early in life. This type of correlation is called “passive” because Diana receives her genes and her early experiences passively from her parents.
2. How does Diana illustrate evocative gene–environment correlation?
Diana’s emerging athletic abilities evoke certain reactions from others. For example, Diana’s skills as a swimmer are recognized by a coach who invites her to participate on a more competitive travel team. Diana receives intensive, high-quality instruction that helps her develop her skills even more.
3. How does Diana illustrate active gene–environment correlation?
As an adolescent, Diana actively selects environmental experiences that are conducive to her genes. For example, most of her friends in high school are on the swim team. Furthermore, Diana will likely select a college that will allow her to continue to swim competitively. Active gene–environment correlation is sometimes described as “niche-picking” because youths actively select niches (e.g., surroundings) that are conducive to their genotype and emerging abilities.
Scarr, S., & McCartney, K. (1983). How people make their own environments: A theory of genotype–environment effects. Child Development , 54 , 424–435.
Weis, R. (2017). Introduction to Abnormal child and adolescent psychology. Thousand Oaks, CA: Sage.
Chapter 3: Assessment and Diagnosis
Functional analysis of behavior.
For each of these scenarios, explain how you might perform a functional analysis of behavior. Specifically, answer the following questions: {C}{C}{C}{C}{C}{C}
{C}{C}{C}{C}{C}{C}
- How might you operationally define the behavior problem?
- What might be an antecedent of the behavior? How might this antecedent elicit the behavior?
- What might be a consequence of the behavior? How might this consequence reinforce the behavior and maintain it over time?
{C}{C}{C}{C}{C}{C}{C}
1. {C}{C}{C}{C}{C}{C}
You are a psychologist working in an elementary school. You have been asked by one of the teachers at the school to deal with a fifth grade student who bullies other children. She says his behavior is getting worse and she is growing very frustrated with him.
- Intervention: One method of treatment is to alter the antecedents. For example, the psychologist might recommend that teachers closely monitoring the boy during recess or restrict his access to younger students. Another approach to treatment is to alter the consequences. For example, the psychologist might encourage teachers to give the boy activities so that he is less likely to experience boredom; alternatively, the psychologist might teach social problem-solving skills so the boy is less likely to use physical harm to solve interpersonal problems.
2. You are a psychologist assigned to work with an extremely shy, 7-year-old girl. She refuses to go to school, because she fears criticism from her teacher and classmates. She has no friends and only seems comfortable at home.
- Possible consequences: The girl’s mother likely gives in to her demands to stay home. The girl then avoids anxiety associated with school attendance; her behavior is maintained through negative reinforcement. It is also possible that her mother gives her attention when she refuses to attend school or attention when she stays home from school. In either case, her school refusal might be maintained through positive reinforcement as well.
- Intervention: One way to intervene would be to alter the environmental contingencies for her school refusal. First, she must always attend school so that her refusal is not negatively reinforced. Attending school may also decrease her anxiety through repeated exposure. The therapist might work with the girl’s teacher to make sure that the girl’s experiences at the school are positive. Second, the girl’s parents must avoid giving unnecessary attention to the girl when she refuses to attend school. Instead, they can approach the problem in a matter-of-fact way and insist on school attendance.
3. Your client is a 34-year-old woman with a disrespectful son. He never does what she says, deliberately defies her, throws tantrums, and ignores her commands. She reports considerable stress in her role as a mother. She loves her son, but doesn’t enjoy spending time with him.
- Operationally define “disrespectful” so that it is an observable, measurable behavior. For example, disrespectful might be defined as “does not comply with parental requests within 10 seconds” (i.e., noncompliance) or “whines, complains, or says ‘no’ when parents issue a clear command” (i.e., defiance).
- Possible antecedents might include (1) a vague or unclear command that the child does not understand; (2) a command to engage in a behavior that is beyond the child’s developmental level, such as asking a 2-year-old to clean his room by himself; (3) hostile-coercive parenting strategies such as yelling; or (4) asking a child to comply when the child is hungry or tired.
- One possible consequence of ignoring a parent’s command or actively refusing to comply with a command might be that the parent backs down from the command. In this instance, the child is negatively reinforced for ignoring his mother because the mother withdraws her command. Alternatively, a child might tantrum to obtain something he wants (e.g., candy, to stay up late). If the parent gives in to the child’s demand, the child’s tantrum may be positively reinforced over time. (Note that these interactions reflect coercive family process, which is discussed in Chapter 9.)
- One intervention is to alter the antecedents of children’s noncompliant or defiant behavior. Parents might be taught to issue clear, developmentally appropriate commands at times when their child is not hungry or tired. A second intervention is to alter the consequences of the child’s noncompliant actions. If a child is noncompliant or defiant, the parent administers time out in a matter-of-fact manner until the child complies. The parent refrains from inadvertently positively reinforcing the child’s noncompliant or defiant behavior by yelling, threatening, or spanking the child and avoids backing down from her initial command.
4. Your client is an 8-year-old boy with autism spectrum disorder and below average intellectual functioning. He attends a regular second-grade classroom with help from an aide. Several times each day, the boy engages in stereotypies: rocking back and forth and flapping his arms. His stereotyped behaviors are disruptive and distract his classmates during lessons.
- Operationally define one stereotyped behavior so that it is an observable, measurable action. For example, hand flapping might be defined as “rapidly moving hands back and forth or up and down for more than three seconds.”
- Possible antecedents might include (1) certain classes, teachers, nearby students, or times of day; or (2) certain emotional states such as boredom or frustration.
- Possible consequences include (1) gaining attention from teacher and classmates, which is positively reinforcing; (2) avoiding boredom or schoolwork, which is negatively reinforcing; or (3) self-stimulation (i.e., pleasurable sensations associated with the action), which is also positively reinforcing. Chapter 5 describes how psychologists conduct functional analyses of problem behavior in children with intellectual disabilities, and how functional analysis can be used to differentiate among these three consequences.
- One possible intervention would be to alter the child’s antecedents. For example, if hand flapping is elicited only when the child is bored, the therapist might teach the child to communicate that he is bored, so that the aide can intervene before the child engages in hand flapping. A second intervention might be to alter the consequences of the boy’s classroom behavior. For example, Chapter 5 discusses how a clinician might use differential reinforcement of incompatible behavior (DRI) to reduce stereotypies. The boy might be positively reinforced for engaging in a behavior that is incompatible with hand flapping, such as keeping his hands at his sides or in his pockets. If the boy engages in hand flapping, the therapist can work with teachers to make sure the boy is not inadvertently reinforced by attention from teachers or classmates.
5. Your teenage client reports problems with depression that have lasted approximately four months. She feels sad and lethargic most of the time, has dropped out of her favorite activities like the school pep and jazz bands, has a hard time getting out of bed in the morning, and can’t concentrate on her schoolwork. She wants antidepressant medication and is furious when she finds out that you can’t prescribe them because you’re not a “real doctor.”
- Operationally define “depressed” so that it is an observable, measurable behavior. One possibility is to ask the client to identify one sign or symptom of depression that is most distressing. Some possibilities include (1) not participating in band, (2) problems getting up in the morning, or (3) difficulty concentrating on homework. An initial goal of behavior therapy might be to decrease the frequency or severity of these signs/symptoms.
- If the adolescent experiences a reluctance to attend band practice, possible antecedents might include (1) the time of day that practice occurs; (2) tangible obstacles to attend band practice, such as a lack of transportation to and from practice; or (3) a lack of encouragement from peers or parents to attend practice. If the adolescent has problems getting up in the morning, possible antecedents include (1) going to bed too late the night before, (2) a lack of enjoyable activities to look forward to later in the day, or (3) unpleasant activities scheduled for later that day.
- Consequences for dropping out of band or staying in bed might include temporary satisfaction with staying at home (i.e., positive reinforcement) or avoidance of anxiety or other negative emotions associated with attending band or school (i.e., negative reinforcement).
- Behavioral interventions would likely alter antecedent events to encourage more social contact and physical activity. For example, the client might schedule activities like band practice, lunch with a friend, or attending a social event and reinforce herself for engaging in these activities afterward. Alternatively, the client might structure her bedroom in a way that increases her likelihood of getting out of bed in the morning. For example, she might place her alarm clock on the other side of the room so that she must leave her bed in the morning to turn it off.
6. You are a family therapist. One of your clients is a couple who has been married for 6 years. They have two young children. The wife complains that her husband doesn’t listen to her or appreciate her. The husband complains that his wife is emotionally distant and frigid. They each say that the other one is argumentative. They are seeing you as a last-ditch effort before seeking a divorce.
- Operationally define “argumentative” so that it is an observable, measurable behavior. For example, argumentative might be defined as “blames the other person” or “yells, screams, or uses sarcasm when speaking.”
- Antecedents might include (1) a particular time of day when the couple tends to argue (e.g., immediately after work), (2) an emotional state that often elicits an argument (e.g., feeling tired, hungry, lonely), and (3) a topic that often elicits an argument (e.g., childcare, family finances).
- Consequences for arguments might include temporarily feeling like one has “won” the argument (e.g., positive reinforcement) or alleviating stress by disclosing negative affect or anger (e.g., negative reinforcement).
- One way to intervene would be to alter the antecedents by teaching the couple more effective communication skills. Components of communication training might include (1) avoiding discussions when one member of the dyad is tired, hungry, or experiencing negative emotions; (2) communicating one’s own feelings accurately in a nonjudgmental manner; (3) listening to the partner’s feelings and accurately reflecting that feeling; and (4) engaging in positive social interactions with the partner.
Reliability, Validity, and Predictive Power
The Screen for Child Anxiety Related Emotional Disorders (SCARED) is one of the most widely used and well-validated measures of anxiety for children and adolescents (Birmaher et al., 1997). The current version of the SCARED is a questionnaire that assesses all of the major DSM-5 anxiety disorders, obsessive–compulsive disorder, posttraumatic stress disorder, and school refusal (Bodden, Bogels, & Muris, 2009). It can be administered to parents or youths ages 8 to 18 years. Here are some sample items:
- When frightened, I feel dizzy . . . (panic disorder)
- I worry about the future . . . (generalized anxiety disorder)
- I don’t like being away from my family . . . (separation anxiety disorder)
- It’s hard for me to talk with people I don’t know . . . (social phobia)
- I’m scared to go to school . . . (school refusal)
Let’s imagine that it’s 1997 and we have been asked to evaluate the reliability, validity, and utility of the SCARED as a diagnostic instrument. The Spice Girls and Backstreet Boys are playing on a CD in the background and we’re ready to get to work.
1. The developers of the SCARED wanted to create a brief questionnaire that might identify children at risk for anxiety and related disorders. At that time, there were already several structured interviews that clinicians could use to identify anxiety disorders in children. Why did the researchers want to create the SCARED, too?
One of the four principles of psychological assessment is multimethod assessment . Clinicians obtain a more complete picture of children’s functioning when they rely on multiple methods to gather data. The SCARED would allow clinicians to gather information about children’s anxiety using a different method than a structured interview. For example, children might be more willing to report anxiety problems on a questionnaire rather than during a face-to-face interview.
Another benefit of the SCARED questionnaire is that it is easier to administer than a structured interview. Typically, structured interviews take a long time to administer and must be conducted by trained clinicians. In contrast, questionnaires like the SCARED take only a few minutes to administer and can be scored by paraprofessionals.
2. The SCARED is a questionnaire that can be administered to both parents and children separately. Why was it important for the test’s authors to develop a screening instrument that could be administered to both adults and children? One of the four principles of psychological assessment is multi-informant assessment . Clinicians can obtain a more complete picture of children’s functioning if they obtain information from multiple people. The correlation between parents’ and children’s ratings on the SCARED is significant, but rather modest ( r = .33). This modest correlation is probably due to the fact that parents might be more accurate reporters of children’s overt actions whereas children might be more accurate reporters of their own subjective feelings. For example, parents and children showed the highest agreement on the separation anxiety and school refusal dimensions of the SCARED ( r = .47), perhaps because parents could easily observe children’s reluctance to leave their side or attend school, respectively.
The SCARED is a norm-referenced test. What does it mean when we say that a test is “norm-referenced”? If we wanted to create the SCARED as a norm-referenced test, what would we need to do?
Norm-referenced tests allow clinicians to determine the degree to which the child they are assessing is typical of other children of the same age and/or gender. These tests are called norm-referenced because they compare the child to a normative sample of other children. The developers of the SCARED administered the questionnaire to more than 300 children referred to an outpatient clinic and their parents. Later researchers gathered normative data from boys and girls separately and for younger children and adolescents separately. Consequently, a clinician who is assessing a 10-year-old girl can compare her SCARED score with the average SCARED score of girls roughly her age.
4. How might we assess the test-retest reliability of the SCARED?
Reliability refers to the consistency of test scores. Test–retest reliability refers to the temporal stability of scores. The developers of the SCARED administered the test to the same group of children and parents at time 1 and then at time 2 (approximately five weeks later). The average correlation across the administrations was .86, which indicated fairly strong test–retest reliability over this time period.
5. How might we assess the internal consistency of the SCARED?
Internal consistency is a form of reliability that concerns the consistency of test items. Ideally, children should answer items that measure the same construct (e.g., anxiety) in the same way. Coefficient alpha is a statistic usually used to assess internal consistency. In the original development of the SCARED, coefficient alpha was .93. This indicates that children with high levels of anxiety tended to rate most items highly whereas children with low anxiety tended to assign low ratings to the test items.
We might expect coefficient alpha to be slightly lower because the SCARED assesses a wide range of anxiety and related disorders. For example, children with generalized anxiety disorder might endorse items related to “worry,” “tension,” or “sadness,” but not endorse items related to obsessive–compulsive disorder or posttraumatic stress disorder.
Similarly, we would not want a coefficient alpha that is too high. A coefficient alpha of .99 would indicate that respondents were answering almost all items the same way and that test items were redundant with one another.
6. What is validity? Can a test be valid without being reliable?
Validity refers to the accuracy of the test, that is, whether the test measures the construct it is intended to measure. Technically speaking, validity is not a property of the test itself, but rather, it is a property of the test used for a specific purpose. For example, the SCARED might be a valid test of childhood anxiety (the construct it is designed to measure), but it should not be used to assess childhood depression.
Reliability is necessary for validity. Test scores must be consistent in order for them to accurately reflect the construct of interest. In contrast, a test can be reliable without being valid. A test can yield consistent scores over time, but it may not accurately measure the desired construct.
7. How might we assess the content validity of the SCARED?
Content validity refers to the degree to which the test items reflect the construct of interest. The SCARED has excellent content validity because items on the SCARED map onto the DSM’s signs and symptoms of the anxiety and related disorders.
8. How might we assess the construct validity of the SCARED?
Construct validity refers to the degree to which test scores reflect the construct of interest. Two components of construct validity are convergent and discriminant validity.
Convergent validity refers to the degree to which SCARED scores correlate with other, theoretically related constructs. For example, the researchers showed significant correlations between children’s SCARED scores and other self-report measures of anxiety.
Discriminant validity refers to the degree to which SCARED scores do not correlate with other, theoretically dissimilar constructs. For example, SCARED scores correlate more highly with other measures of anxiety than with measures of depression (a theoretically less similar construct).
9. How might we assess the criterion-related validity of the SCARED?
Criterion-related validity refers to the degree to which test scores can be used to infer an examinee’s probable standing on some external benchmark. In clinical psychology, criterion-related validity is usually established by showing that test scores can be used to infer something about client’s diagnostic status or real-world functioning.
For example, the researchers administered the SCARED to three groups of children: children with anxiety disorders, children with depression, and children with disruptive behavior problems. Results showed that children with anxiety disorders ( M = 22.9, SD = 12.2) reported higher SCARED scores than children with depression ( M = 18.9, SD = 11.8) and children with disruptive behavior problems ( M = 11.1, SD = 11.2). This finding supports the concurrent validity of the SCARED. It is also noteworthy that SCARED scores were higher in children with depression (which is often comorbid with anxiety) than in children with disruptive behavior problems (which is less often comorbid with anxiety).
10. How might we assess the predictive power of the SCARED?
Predictive power refers to the ability of the test results to predict the actual presence or absence of a disorder. Positive predictive power (PPP) is the likelihood that a child with a high SCARED score (above the normative cutoff) actually has an anxiety disorder. Negative predictive power (NPP) is the likelihood that a child with a low SCARED score (below the normative cutoff) does not have an anxiety disorder. Ideally, tests have high PPP and NPP, indicating that they are useful in screening individuals for disorders.
In a recent study (Bodden et al., 2009), researchers administered the SCARED to a large sample of clinic-referred children. Then, they classified children based on their SCARED score (i.e., high or low) and their diagnostic status (i.e., anxiety disorder or no disorder). Results are shown below:
- is the number of people with high scared scores who actually have an anxiety disorder (A) divided by the total number of people with a high SCARED score (A + B). The PPP in this study was .97, which indicates that a high SCARED score strongly indicates the presence of an anxiety disorder.
- is the number of people with low SCARED scores who do not have an anxiety disorder (D) divided by the total number of people with low SCARED scores (C + D). The NPP in this study was .69, which is somewhat low. This NPP indicates that a low score on the SCARED does not necessarily mean the child is anxiety free; approximately 31% of youths with low SCARED scores actually have anxiety problems. Altogether, these findings indicate that a high scared score likely indicates the presence of anxiety; however, children who earn low SCARED scores should be assessed using another instrument if they (or their parents) report ongoing problems with anxiety.
The text does not discuss sensitivity and specificity because predictive power is usually more important in clinical diagnosis. Instructors can use this example to present sensitivity and specificity too, if they would like.
Sensitivity refers to the degree with which children with an anxiety disorder earn high SCARED scores. It is calculated by taking the number of children with anxiety disorders and high SCARED scores (A) divided by the total number of children with anxiety disorders (A + C). Sensitivity in this study was .89, indicating that the test is very sensitive to detecting anxiety in children.
Specificity refers to the degree with which children without an anxiety disorder earn low SCARED scores. It is calculated by taking the number of children without anxiety disorders and low SCARED scores (B) divided by the total number of children without anxiety disorders (B + D). Specificity in this study was also .89, indicating that children without anxiety disorders test to score low on the SCARED.
Birmaher, B., Khetarpal, S., Brent, D., Cully, M., Balach, L., Kaufman, J., & Neer, S. M. (1997). The screen for child anxiety related emotional disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child and Adolescent Psychiatry , 36 , 545–553.
Bodden, D. H., Bögels, S. M., & Muris, P. (2009). The diagnostic utility of the screen for child anxiety related emotional disorders-71. Behavior Research and Therapy , 47 , 418–425.

Chapter 4: Treating Children, Adolescents, and Families
Systems of psychotherapy.
There are hundreds of different systems or “schools” of psychotherapy. The text presents five, broad approaches that are most often used with children and adolescents. In addition, medication is frequently used to augment treatment.
Let’s look at the case of Val once again, the adolescent with an opioid use disorder. If you were Val’s therapist, what approach to treatment would you recommend? If you were Val, what approach would you prefer?
Val’s substance use began with her transition to middle school. She was referred to a special education program for children with behavior problems and learning disabilities. She quickly made friends with several girls who introduced her to smoking (age 12) and marijuana (age 13). Although she tried alcohol at approximately the same age, she did not like its taste and limited its use to parties and social gatherings. By the time Val was 14-years-old, she was using marijuana several times per week and drinking five to six sweet alcoholic drinks at parties on the weekends. She found it relatively easy to hide her substance use from her mother.
“I’m not sure what I’m going to do when I get out of here,” reported Val. My mom wants me to come back home, but I can’t go back. Everyone I know uses. I need a clean break.”
1. What medications might be effective to treat Val’s symptoms of hyperactivity and impulsivity?
Psychostimulants (e.g., Adderall, Ritalin) are effective in reducing hyperactivity-impulsivity and increasing attention in children and adolescents. They increase dopaminergic activity in brain regions responsible for inhibition. Unfortunately, there are few studies investigating the use of psychostimulants for adolescents with ADHD who also have an opioid use disorder.
Some youths with substance use problems may engage in diversion, that is, the practice of distributing prescription medication to other individuals. Val’s history of obtaining and selling prescription pain medication likely increases the likelihood that she might engage in a similar practice with medication for ADHD. Consequently, some physicians may wish to prescribe the nonstimulant ADHD medication atomoxetine (Strattera). Atomoxetine is a specific norepinephrine reuptake inhibitor. Because it does not directly affect dopamine in the central nervous system, it has lower risk for misuse and diversion.
2. According to Carl Rogers, what three necessary and sufficient factors might the therapist provide to help Val overcome her substance use problems?
Rogers’s three “necessary and sufficient” conditions for therapeutic change are (1) unconditional positive regard, (2) congruence, and (3) empathy. Most therapists would see these factors as necessary for building an effective therapeutic alliance, although most would not regard them as sufficient for helping an adolescent overcome an opioid use disorder.
3. How might a behavior therapist attempt to help Val with her opioid use disorder?
Exposure therapy would likely be used during inpatient treatment. Currently, Val’s opioid use is maintained through negative reinforcement. By taking opioids, she avoids unpleasant withdrawal symptoms. The medication Suboxone will allow her to abstain from heroin during inpatient treatment and endure these withdrawal symptoms.
Principles of behavior therapy would also be important in planning Val’s return to the community. Through classical conditioning, she has learned to associate certain people and places with opioid use. If she returns to those people or places, they might serve as conditioned stimuli, prompt cravings, and contribute to relapse. A behavior therapist would likely work with Val and her mother to develop a strategy to avoid these environmental triggers. Also, they might help Val plan for relapse if it occurs after she returns home. If she begins to use heroin again, what should she do? Who can she contact for help?
4. How might a cognitive therapist attempt to help Val with her opioid use disorder?
Cognitive therapists believe that there is a close association between people’s thoughts, feelings, and actions. Although we cannot easily change the way we feel, we often can control the way we think and act. If we think or act differently, our feelings might improve.
A cognitive therapist who adopts Aaron Beck’s theory would likely try to identify and challenge Val’s cognitive biases or distortions. For example, one source of dysphoria for Val is her poor relationship with her father. Val said, “If your own dad doesn’t care about you, no one will.” A cognitive therapist might challenge this belief. What is the evidence that no one cares for Val? Is there any evidence that her mother cares about her? That her therapist cares about her? The goal of therapy is to help Val think more realistically and flexibly about events in her life.
Alternatively, a cognitive therapist who adopts Albert Ellis’s theory might identify and challenge Val’s irrational beliefs that contribute to her dysphoria. For example, it is likely that Val believes that her father “should” have been a better father and not have abandoned her when she was a child. Although this belief seems reasonable to most people, Ellis would argue that it is irrational: There is no rule that says that people must act in a way that pleases us. It is likely that Val’s belief that her father “should” have been a better dad contributes to her anger and resentment toward him. Perhaps her father abandoned her at the time because he (like Val) had a substance use problem and was largely unable to care for his family. By changing her thoughts about her father’s actions, Val might feel disappointment or sorrow toward her father rather than anger and resentment.
5. How might an interpersonal therapist attempt to help Val with her opioid use disorder?
Interpersonal therapists believe that disturbances in relationships tend to prompt mental health problems. An interpersonal therapist might help Val identify one of the following interpersonal problems that contributed to her low self-esteem and substance use disorder: (1) death or loss, (2) interpersonal transition, (3) interpersonal conflict, or (4) interpersonal deficits.
For example, the abandonment by her father seems to be a source of Val’s dysphoria. An interpersonal therapist might help Val grieve this loss and help Val identify her feelings about him. Alternatively, Val may have interpersonal deficits that interfere with her ability to make and keep satisfying relationships. Indeed, all of her friendships in recent years seem to be based around drug distribution or use. An interpersonal therapist might help her find ways to develop more prosocial friendships, perhaps through a part-time job, participation in a GED program, or through a sport or hobby.
6. How might a family therapist attempt to help Val with her opioid use disorder?
Although there are many different types of family therapy, all adopt a systems approach to treatment. Family systems therapists believe that that the family together is more than the sum of its parts. Changing one member in the family will necessarily change all of the family relationships and, hence, all members. A family therapist would view both Val and her mother as the “client” in need of treatment.
Structural family therapy focuses on the quality of relationships among family members. Val and her mother seem to have a relationship characterized by disengagement. A family therapist would likely work with Val and her mother to open lines of communication between them. The therapist would likely pay special attention to helping Val’s mother cope with psychosocial stress in her own life so that she might be better able to monitor Val’s activities and support her as she participates in treatment.
An Adlerian family therapist would try to identify the function that Val’s substance use problem has on the family as a whole. For example, it is possible that Val uses drugs to avoid her family and be left alone. A family therapist would try to strengthen the relationship between Val and her mother so that Val can derive greater satisfaction from her interactions with her.
7. How might a psychodynamic therapist attempt to help Val with her opioid use disorder?
A psychodynamic therapist would attempt to identify an unconscious motive for Val’s substance use problem. According to classic Freudian theory, her opioid use is likely a symptom of unconscious mental conflicts that are unknown to her and unresolved. For example, Val might have directed anger and resentment toward her father upon herself. Her history of substance use and other dangerous behaviors (e.g., prostitution) may express an unconscious wish to punish herself.
A psychodynamic therapist would pay attention to transference in the therapeutic relationship. Val might act toward the therapist in a manner that reflects her unconscious feelings toward her father or other important figures in her life. The goal of psychodynamic therapy is to interpret the transference relationship and to help Val gain insight. If Val could recognize the source of her conscious feelings, her symptoms might decrease.
Ethical Dilemmas in Child and Adolescent Psychotherapy
In one study, researchers surveyed psychologists about ethical dilemmas that they encountered in their practice. Some of the most troubling cases involved questions about maintaining confidentiality (#1), multiple relationships or potential conflicts of interest (#2), when and how to provide informed consent (#3), and practicing within one’s boundaries of competence (#10; Pope & Vasquez, 2016). Ethical issues are especially difficult in psychotherapy with children and families.
Read each of the ethical scenarios below. Identify the ethical principle that is most relevant to the scenario. Then use this ethical principle to determine how you might act in that situation.
Ethics scenario 1: You are a therapist in private practice who has been providing counseling to Aimee, a 15-year-old girl with anxiety and depression. Over the last few weeks, Aimee has disclosed a worsening of her symptoms and admitted to engaging in self-injury. Her mother wants to know what is wrong. What should you do to act in an ethical manner?
This scenario illustrates the importance of confidentiality in psychotherapy. It is subsumed under the American Psychological Association (APA, 2010) ethical principle of fidelity . Confidentiality refers to clients’ expectations that information that they disclose in therapy will remain private. Confidentiality promotes trust between therapists and clients. Issues of confidentiality are the primary source of ethical dilemmas among clinicians.
Confidentiality can be particularly tricky with adolescents. In most instances, adolescents do not have a legal right to confidentiality apart from their parents. Consequently, if a parent insists on reviewing her adolescent’s medical records, the clinician is usually legally obligated to provide them to the parent. Such disclosure respects parental autonomy, but it can jeopardize the therapeutic relationship between the adolescent and clinician.
In the scenario above, the clinician must assess the risk that the adolescent’s self-injury places to her health and welfare. Clinicians have a legal and ethical responsibility to protect their clients. If the adolescent’s self-injury is serious, the clinician would need to disclose the injury in order to protect the client. If the injuries are superficial, the clinician might talk with the parent about her desire to know “what’s wrong” and emphasize the importance that some information remains private.
Obviously, the clinician is in a tricky situation. Perhaps the best way to deal with this situation is to prevent it. Most clinicians who work with adolescents and family discuss the importance of confidentiality and its limitations early in therapy, before such issues arise. Chapter 4 presents one way a therapist might approach this topic with an adolescent and parent.
Ethics scenario 2: You are an undergraduate psychology major who is participating in a summer internship at a residential treatment facility for adolescents with conduct problems. One of the social workers at the facility asks you to lead a group therapy session with five or six residents each week. The focus of the therapy session will be to help the adolescents develop emotion regulation and social skills. What should you do?
This scenario illustrates the importance of practicing within one’s boundaries of competence . It is subsumed under the APA ethical principle of nonmaleficence , that is, “do no harm.” Mental health practitioners should only deliver services they are competent to perform. For example, a clinician who has no experience delivering a particular form of therapy, or who is experiencing mental health problems himself, should refrain from providing such services.
In this scenario, it is unlikely that an undergraduate student is competent to lead group therapy. The student should seek supervision from a licensed mental health provider who has experience leading such a group. Ideally, the student would observe several sessions before helping to facilitate the group herself, and then, only under direct supervision.
Ethics scenario 3: You are a behavior therapist working at a special needs preschool. You’ve been assigned to work with Meredith, a 6-year-old girl who has low intellectual functioning and autism spectrum disorder. Meredith becomes angry and tantrums when she must brush her teeth or her hair in the morning. Your task is to reduce the frequency and severity of these tantrums. What must you do to proceed in an ethical manner?
This scenario illustrates the importance of informed consent and child assent in psychotherapy. It is subsumed under the APA ethical principle of autonomy . All patients have the right to make informed decisions regarding their treatment. For example, patients should know the potential benefits and risks of treatment, the duration and costs of treatment, the general approach to therapy, and alternative interventions that might be available. Consent is a process in which therapists also take time to answer questions from patients throughout the course of treatment.
Because children cannot consent to treatment themselves, parents or legal guardians usually provide proxy consent for their children. Before treatment begins, however, clinicians also gain children’s assent to treatment. Specifically, clinicians describe treatment to children in a manner they are likely to understand and ask for permission to help them.
In the scenario, the clinician should obtain parental consent prior to beginning behavior therapy. The clinician should attempt to use positive reinforcement to modify Meredith’s behavior whenever possible. The clinician should also try to obtain the assent of Meredith by explaining or demonstrating the therapy in simple terms.
Ethics scenario 4: You are a psychologist working at a local high school. One of your friends, a teacher at the high school, asks you to help her daughter, a 14-year-old middle school student, who has been acting very depressed and withdrawn in recent weeks. After meeting with the girl for a few sessions, you learn that she is sexually active and may be pregnant. What must you do to act in an ethical manner?
This scenario illustrates the importance of being aware of potential conflicts of interest in psychotherapy. It is subsumed under the APA ethical principle of beneficence , that is, putting the client’s welfare before the interests of others. (The scenario also illustrates the importance of confidentiality, for the same reason as scenario 1 above.)
The school psychologist has entered in to a multiple relationship. She is not only the therapist for the 14-year-old girl, but she is also a good friend and coworker of the girl’s mother. The school psychologist’s relationship with the mother might adversely affect the care the psychologist gives the girl during the course of therapy.
Ideally, the psychologist would have avoided the multiple relationship by referring the girl and her mother to another clinician. At this point, however, the psychologist should make known the multiple relationship to the mother and seek consultation about how best to resolve the situation. Another psychologist, who serves as consultant, might be able to look at the situation more objectively.
American Psychological Association. (2010). Ethical principles of psychologists and code of conduct. Washington, DC: Author.
Pope, K. S., & Vasquez, M. J. (2016). Ethics in psychotherapy and counseling: A practical guide . New York, NY: Wiley.
Chapter 5: Intellectual Disability and Developmental Disorders
Cheerful robin.
Intellectual Disability (Down Syndrome)
Milena was a 6-year-old girl who was referred to her school psychologist by her pediatrician. Milena was diagnosed with Down syndrome when she was an infant. Her pediatrician wanted Milena’s cognitive and academic achievement skills to be reassessed before she began kindergarten this academic year.
Milena’s gestation and delivery were uncomplicated. However, Milena was born with a congenital heart defect that required several surgeries. Milena showed physical features associated with Down syndrome. For example, she had a small nose with a flat nasal bridge, almond-shaped eyes, and broad hands with short fingers. Each of her palms had a single transverse crease rather than the many folds seen in most children.
Milena showed delays in achieving developmental milestones, especially in the areas of gross motor functioning (e.g., sitting up, walking), fine motor skills (e.g., feeding and dressing herself), and expressive communication (e.g., saying her first words, using two- or three-word phrases). Fortunately, Milena’s parents became active in her education and in a local support group for the caregivers of children with Down syndrome. Milena participated in occupational therapy and speech–language therapy as a toddler and attended a full-day enrichment preschool for children with special needs.
Results of the WISC-V indicated that Milena’s full scale IQ was 57, falling in the low range of intellectual functioning. Milena performed better on tests assessing her visual–spatial reasoning and nonverbal fluid reasoning than tests assessing her verbal comprehension skills. Her preschool teacher said that she often learned better through demonstrations and “hands-on” learning than from verbal instruction.
Milena showed good eye contact when speaking with others, obeyed classroom rules, and enjoyed playing with other children. Also, with extensive practice, she learned to perform most self-care skills such as bathing, dressing, and cleaning her room. On the other hand, Milena continued to show problems learning her numbers, the alphabet, and the value of money. Her reading skills were poor and her handwriting was mostly illegible.
Interpersonally, Milena presented as a charming girl who loved to play with her classmates and spend time with her parents. Her favorite hobbies included soccer, playing with her dog, and helping her parents cook meals. Her parents called her “the cheerful robin” because of her tendency to get up early in the morning and her friendly, social disposition.
1. List the three DSM-5 domains of adaptive functioning. Then, describe Milena’s functioning on each of these three domains.
Conceptual: Expressive language, reading, writing, counting, telling time, using and understanding money seem delayed
Social: Interpersonal skills, rule-following, social problem-solving, and making friends seem within normal limits
Practical: Daily living skills, safety skills, home activities, and recreational activities seem within normal limits
2. DSM-5 identifies four levels of severity for children with intellectual disability. Which level of severity best describes Milena’s functioning?
Severity is determined by Milena’s adaptive functioning. If her adaptive functioning in the conceptual domain is similar to her FSIQ (57), Milena would be diagnosed with mild intellectual disability. Many children with Down syndrome fall further behind their classmates over time. Therefore, Milena’s severity might fall into the moderate intellectual disability range later in childhood or adolescence.
3. According to Zigler’s classification system, what is the difference between organic and cultural–familial intellectual disability? Which classification best describes youths with Down syndrome like Milena?
Youths with organic intellectual disability, like Milena, typically have a known cause for their disability, low IQ, parents with normal intellectual functioning, and characteristic cognitive and physical features associated with their disability. In contrast, youths with cultural–familial intellectual disability tend to have no clear cause for their disability, borderline IQ, parents who also have borderline IQ, and no obviously physical anomalies.
4. How do Milena’s delays in gross motor, fine motor, and communication skills support the similar sequence hypothesis?
Milena’s skills lag behind those of typically developing children. However, Milena shows the same order/sequence of developing these skills as typically developing children, albeit at a slower rate.
5. What is the behavioral phenotype for children with Down syndrome? How many aspects of this phenotype does Milena show?
Many youths with Down syndrome, like Milena, earn FSIQ scores in the 50 to 65 range with relative strengths in nonverbal problem-solving and relative weaknesses in verbal comprehension and language. They tend to learn best through manipulation and demonstration rather than through verbal instruction. Expressive language, reading, and writing tend to be difficult for these children. On the other hand, these children are usually described as friendly or affectionate, especially in elementary school. Like Milena, many youths with Down syndrome have characteristic physical features and medical problems.
6. What caused Milena’s disability? Did she inherit Down syndrome from her parents?
In most (95%) cases, Down syndrome is caused by a nondisjunction, in which the 21st chromosome fails to separate during meiosis. The result is that the child inherits three 21st chromosomes rather than two. This is a genetic error and it is not heritable. Only about 3% to 5% of children with Down syndrome have a heritable condition.
7. What prenatal tests might Milena’s mother have taken to determine the risk that Milena would be born with Down syndrome? Which of these tests carries the greatest risk to the fetus?
- Serum screening (15–18 weeks)
- Amniocentesis (15–20 weeks)
- Chorionic villus sampling (8–12 weeks) * greatest risk
- Ultrasound screening (11–14 weeks)
8. Milena’s school psychologist would likely use the results of her assessment to generate an IEP for Milena. What is an IEP?
The Individuals with Disabilities Education Improvement Act (IDEIA) requires that school districts identify youths with disabilities and provide them with an Individualized Education Plan (IEP) in consultation with their parents. This plan describes the services and accommodations the child will receive to help her achieve her highest potential.
9. If you were Milena’s teacher, how might you use principles of universal design to help Milena learn to read and perform mathematics?
Universal design involves the use of educational materials and activities that allow all children (with and without disabilities) to achieve learning goals. For example, the teacher might use manipulatives (e.g., blocks, beads) to help all children learn to count, add, and subtract rather than rely on verbal counting only. Similarly, the teacher might use computer software that allows children to read text silently while the computer reads text aloud, to assist children with decoding and fluency. These techniques would help Milena overcome her weaknesses, but they would also likely benefit the typically developing children in her class.
10. In what way might having a child with a known genetic disorder, like Down syndrome, be easier than having child with a developmental disability of unknown origin?
The parents of children with developmental disabilities can benefit from the social support of other caregivers, teachers, and advocates. Some disabilities are more easily recognized than others and have extensive advocacy and support groups, whereas other disabilities are less clearly recognized and understood by others, including teachers and mental health professionals. The caregivers of children with these lesser known disabilities may experience reduced support and greater stress or isolation in their caregiving roles. ______________________________________________________________________________
Case Study: Intellectual Disability (Fragile X Syndrome)
New Challenges
Logan was a 7-year-old boy referred to our clinic by his mother because of problems with hyperarousal and stereotyped behaviors at home and school. Logan was diagnosed with Fragile X syndrome at the age of 3½ years and attended a special needs preschool for children with neurodevelopmental disorders. This year, Logan began first grade at his local public school and attends most regular classes with the help of a classroom aide.
Logan reached developmental milestones at a much slower pace than other, typically developing children. Most notably, he showed marked delays in fine and gross motor skills and generally poor muscle tone and coordination. He was very slow to develop receptive and expressive language and, even today, speaks in simple sentences. His speech is often perseverative and tangential; he often repeats words, phrases, and sounds that he hears in real life or on videos. Logan was initially diagnosed with global developmental delay. Subsequent genetic testing confirmed the existence of Fragile X.
Results of cognitive testing at the beginning of first grade showed that Logan’s full scale IQ was approximately 50. He showed relative strengths on tasks assessing visual–spatial processing and rote memory, but relative weaknesses on tasks measuring verbal abilities, abstract reasoning, and attention, even compared to other children at his developmental level.
Logan’s mother was most concerned with his social behavior. Logan became easily excited in his new classroom. He often had difficulty with transitions from one activity to the next, became anxious and overwhelmed during loud games or assemblies, and refused to participate in most group activities. Logan also seldom made eye contact with teachers or peers. Logan seemed to want to make friends and join groups but was extremely reticent to interact with others.
When anxious or excited, Logan would show signs of physiological arousal, like a flushed face and sweating. He would appear agitated and show hyperactive behavior, such as leaving his seat, pacing about the room, and repeating words and phrases. Logan also showed stereotypies at these times; usually, he would rock or sway his body and flap his hands repeatedly. On one occasion, his teacher tried to calm by holding him in his seat by his shoulders and talking with him gently. Her actions made Logan more agitated, however, and elicited a severe tantrum.
Logan’s mother was also concerned about similar problems with hyperarousal and social anxiety at home. Besides his siblings, Logan has few friends in his neighborhood. His poor eye contact, reluctance to engage others, and stereotypies limit his mother’s ability to participate in community activities with peers. Despite his interpersonal challenges, Logan’s mother described him as a “loving and affectionate little guy” who she “cherishes with all my heart.”
1. Logan has Fragile X syndrome. Can he also be diagnosed with intellectual disability? If he meets diagnostic criteria for autism spectrum disorder (ASD), can he also be diagnosed with that condition, too?
Yes. Most children with Fragile X syndrome also have intellectual disability. Logan can also be diagnosed with ASD if he meets diagnostic criteria for that disorder. The term dual diagnosis is used to describe individuals with intellectual disability who have another, comorbid disorder like ASD, depression, or anxiety. Approximately 40% of children with Fragile X also have ASD.
2. Why was Logan diagnosed with global developmental delay as a toddler?
Global developmental delay is diagnosed in young children, like Logan, who show significant delays in adaptive functioning but who are too young for formal IQ testing. Logan’s delays in gross and fine motor functioning and language likely qualify him of the global developmental delay diagnosis. Once he is diagnosed with intellectual disability, this new diagnosis will replace his older global developmental delay diagnosis.
3. Logan displays stereotypies, especially when overaroused. What other challenging behaviors are sometimes shown by children with intellectual disability?
Other challenging behaviors include (1) self-injurious behaviors, (2) physical aggression, and (3) other comorbid mental disorders.
4. Do Logan’s weakness in verbal abilities, abstract reasoning, and attention support the similar structure hypothesis?
The similar structure hypothesis posits that two children at the same developmental level (one with and the other without intellectual disability) will show similar abilities. This hypothesis is often not supported by children with genetic disorders like Logan. Logan shows specific deficits that are characteristic of his genetic condition. This suggests that Fragile X (like many other genetic disorders) is associated with behavioral phenotypes (i.e., cognitive and behavioral characteristics) that are unique to that disorder.
5. What causes Fragile X syndrome?
Fragile X syndrome is an X-linked genetic disorder. It occurs when there is a mutation on a gene of the X chromosome (the FMR1 gene) that produces a protein that aids brain development. Children with the mutation produce less of this protein and typically show intellectual disability and other impairments.
6. Why are girls much less likely than boys to show Fragile X syndrome?
Girls have two X chromosomes. Usually, only one has the mutation; the other X chromosome is healthy. Consequently, girls can usually produce sufficient amounts of the protein to aid brain development and they show less severe symptoms.
7. Imagine that you want to observe Logan’s behavior at school in order to record the number of times he flaps his hands in a given class period. What method of observation might you use to record this frequency?
Hand flapping is a discrete action that can be observed and recorded. A therapist might observe the number of flaps during class, during recess, and during transition times (e.g., going from recess to class) using event recording.
8. If you were Logan’s parent or classroom aide, how might you use positive reinforcement to help him keep his hands at his side and reduce hand flapping?
A behavior therapist might use differential reinforcement to increase Logan’s appropriate behavior and decrease hand flapping. For example, differential reinforcement of incompatible behavior (DRI) could be used by reinforcing Logan for keeping his hands on his desk or at his side.
9. Are any medications effective in reducing challenging behaviors in youths with developmental disabilities?
Atypical antipsychotic medications, such as risperidone (Risperdal), are useful in reducing challenging behaviors in children with intellectual disabilities. Behavior therapy is typically seen as a first-line treatment, however.
Chapter 6: Autism Spectrum Disorder (ASD)
Our miracle.
Autism Spectrum Disorder w/ Intellectual Impairment
Joel was a 33-month-old boy referred to the developmental disabilities clinic of a large children’s hospital. Joel’s pediatrician had assigned a provisional diagnosis of autism spectrum disorder (ASD) and requested that the psychologists at the clinic perform a more thorough assessment and determine the best avenue for treatment.
Joel was born premature, weighing only 3½pounds upon delivery. Moreover, he was diagnosed with neonatal anemia shortly after birth, a condition that limited the amount of oxygen in his bloodstream. He spent the first 6 weeks in-and-out of the hospital; his parents called him “their miracle” when he finally was deemed healthy enough to come home.
Joel was diagnosed with global developmental delay 18 months ago when he displayed marked delays in gross motor skills, fine motor skills, and language. His pediatrician attributed these early delays to his perinatal medical problems.
Today, however, Joel is largely unable to feed, dress, or otherwise care for himself, has limited receptive language skills, and no functional expressive language. Joel also shows very little shared attention, rarely initiates interactions with other people besides his parents, and does not engage in pretend or symbolic play. Indeed, Joel seldom maintains eye contact with others and shows little interest in games or activities enjoyed by most children his age. Although Joel has many toys, his favorite pastime is to arrange and rearrange common household objects, to drop items onto the floor from his chair and observe the sounds they make, and to listen to music. His parents reported that he would engage in these activities “all day long” if they would let him.
“We’ve tried to improve Joel’s self-care skills and use of language, but it’s been very difficult,” admitted his father. “When we make him use a spoon to eat, or require him to make eye contact with us, he cries terribly. We know it’s in his interest in the long term to do these things, but he fights us every time so we eventually just give in and let him do things his way.”
Joel’s mother added, “On a few occasions, he’s become very upset. Once we tried to brush his teeth. At first he just cried, but then he tried to hit and bite us. We need help teaching him some skills so that he can function effectively when he starts school.”
The psychologist at the clinic attempted to assess Joel’s intellectual functioning, but he refused to participate in testing. Results of the Autism Diagnostic Interview-Revised and the Autism Diagnostic Observation Schedule, Second Edition confirmed Joel’s diagnosis of ASD.
“We’re hoping that you can help us obtain services from our school district,” Joel’s father said to the psychologist. “We also need help improving his behavior at home.”
1. List four problem areas or deficits shown by Joel.
Some problem areas include
- deficits in social communication,
- repetitive, perseverative activities and interests,
- low intellectual functioning and adaptive behavior, and
- poor receptive and expressive language skills
2. Which problem areas reflect his DSM-5 ASD diagnosis and which problem areas are associated with ASD but are not part of the diagnosis itself?
The first two problem areas are characteristic of ASD. Intellectual disability (i.e., low IQ and adaptive functioning) and limited communication skills are sometimes comorbid with ASD but they are not part of the ASD disorder itself. Approximately 44% of children with ASD earn IQ scores < 70 and 25% lack language, like Joel.
3. What deficits in social cognition did Joel show as a toddler that preceded his ASD diagnosis?
Many toddlers later diagnosed with ASD, like Joel, show deficits in (1) joint attention, (2) social orientation, and (3) pretend/symbolic play. These early deficits may interfere with the development of later social communication and language skills.
4. What evidence-based psychosocial treatments might you recommend for Joel to help improve his social communication and language skills?
Two evidence-based treatments for a preschool-age child like Joel are (1) EIBI and (2) pivotal response training. Both interventions rely heavily on discrete trial training and behavioral prompts. Pivotal response training also attempts to help children generalize skills to new people and settings.
5. If Joel was lucky enough to live in a community where TEACCH was available, what might this intervention look like?
TEACCH is a school-based, behavioral intervention for children with ASD and other developmental disorders. Teachers and therapists rely on structured teaching, scaffolding, visual schedules, and hand-over-hand assistance to prompt children’s appropriate behavior in the classroom, maximize their likelihood of success, and reinforce the development of skills.
6. The psychologist at the clinic recommends that Joel’s family use an augmentative and alternative communication (AAC) system to help Joel communicate. What is an AAC system? Will an AAC system limit Joel’s use of verbal language?
AAC systems compensate for the language deficits shown by some children with ASD, like Joel. Examples are PECS and electronic speech generating devices. They can either be used to supplement children’s emerging spoken language or compensate for permanent language deficits. They are not designed to replace the use of verbal language and have not been shown to hinder verbal language acquisition in children with ASD.
7. When Joel’s parents try to brush Joel’s teeth, he cries and sometimes becomes aggressive. His parents back down and let him go without brushing his teeth. Over time, Joel learns that crying is an effective way to avoid activities he dislikes. In behavioral terms, what sort of reinforcement has occurred?
Joel’s parents negatively reinforced him for crying and biting. Joel’s behavior (crying) was followed by the withdrawal of a stimulus (the toothbrush) making Joel more likely to cry in the future when he’s asked to brush his teeth.
8. BONUS: In Chapter 5, we learned about Iwata and colleagues’ (1994) method of conducting a functional analysis of problem behavior in children with developmental disabilities. How might you use this method to determine the function of Joel’s crying, hitting, and biting?
You could observe Joel’s behavior in four conditions: (1) attention, (2) demand, (3) alone, and (4) play and record the frequency of his problematic behavior in each condition. The case study suggests that he cries, hits, and bites mostly when forced to do activities he dislikes (i.e., the demand condition). Therefore, it is likely that his behavior problems are maintained through negative reinforcement.
Iwata, B. A., Pace, G. M., Dorsey, M. F., Zarcone, J. R., Vollmer, T. R., Smith, R. G., . . . & Goh, H. L. (1994). The functions of self‐injurious behavior: An experimental‐epidemiological analysis. Journal of Applied Behavior Analysis , 27 , 215–240.
A Second Opinion
Autism Spectrum Disorder w/o Intellectual Impairment
Noah Favero was a 9-year-old boy referred to our clinic by his parents. Approximately six months ago, Noah’s pediatrician diagnosed him with attention-deficit/hyperactivity disorder (ADHD) and began prescribing stimulant medication to help manage episodes of hyperactivity and impulsivity at school. Noah’s parents reported that the medication was largely ineffective in reducing these episodes and they felt that ADHD did not adequately reflect Noah’s functioning.
Noah was a full-term, healthy infant who met early developmental milestones in an age-expected fashion. His parents began having concerns about his development at age 18 months, when Noah still did not show any spoken language. Also, Noah did not seem to interact with his parents like other toddlers his age. For example, he was content to play with toy trains and dinosaurs, lining them up and then rearranging them, for hours at a time. He seldom engaged his parents in play and rarely (if ever) engaged in pretend play with his toys. Noah also showed little interest in imitative games like peak-a-boo and the itsy-bitsy-spider. Because Noah was their first child, his parents attributed these behaviors to the fact that Noah was a “late bloomer.”
Noah’s expressive vocabulary developed rapidly between 30 and 36 months. By age 4, Noah was a talkative preschooler. His speech was characterized by two peculiarities, however. First, it had an odd, pedantic quality, as if Noah was lecturing to others rather than talking with others. Second, Noah was preoccupied with reptiles. Although such a fascination is not uncommon for a 4-year-old boy, Noah could not deviate from the subject. Indeed, he exhausted his parents, relatives, and neighbors with information about lizards, snakes, and turtles.
Noah’s behavior became more problematic when he began preschool. He seldom initiated interactions with other children, except to talk about his favorite topic. He avoided group games and activities, especially when they were unstructured. Instead, Noah preferred to watch other children from the sidelines or to play by himself. Needless to say, Noah had few friends in preschool or in his neighborhood. Moreover, he did not seem bothered by his social isolation or aware of the fact that his behavior caused classmates to avoid him.
Noah displayed episodes of hyperactivity at school. His teacher reported that he would easily become overwhelmed by noisy activities and transitions from one activity to the next. During these instances, he would pace about the classroom, talk incessantly, or rock in his seat. More concerning, Noah would become irritable or angry when forced to engage in certain high-rate group activities. During one class assembly, for example, he yelled and threw a chair when he was asked to accompany his class on stage to sing. On another occasion, Noah became belligerent when his daily schedule was changed to accommodate a Halloween party.
On the WISC-V, Noah earned a full scale IQ in the average range. He showed above-average scores on measures of verbal comprehension and visual–spatial reasoning domains, but below-average scores on measures of working memory and processing speed. His academic skills were also within the average range.
“We’re hoping that you might be able to give us a second opinion about Noah,” said his father. “The school psychologist recommended that we have him evaluated more thoroughly.” Noah’s mother added, “She said that many of his behaviors resemble the features of autism, but that doesn’t seem right. He’s a really smart, articulate kid!”
1. Review the DSM-5 diagnostic criteria for ASD. Which features does Noah display?
A. Noah shows deficits in social communication. First, he shows problems with social-emotional reciprocity, that is, the natural give-and-take of conversations. Second, he has deficits in nonverbal communication skills, especially eye contact. Third, he has a history of imaginative/pretend play and current problems making friends.
B. Noah shows restricted, repetitive interests and activities. First, he becomes distressed when his daily routine is changed. Second, he is preoccupied with reptiles. Third, he may have hypersensitivity to certain loud, boisterous settings although more information on this diagnostic criterion is necessary.
C. Noah’s symptoms emerged in toddlerhood and fully manifested themselves by the preschool years.
D. Noah’s symptoms cause impairment in his social relationships.
E. Noah’s symptoms are not better explained by intellectual disability or global developmental delay. His cognitive functioning is average.
2. Can Noah be diagnosed with ASD despite the fact that his FSIQ is within the average range and he has good verbal skills?
Yes, children can be diagnosed with ASD despite having average intelligence. A national survey of 8-year-old children with ASD showed that 32% earned FSIQ scores in the average or above average range.
In the past, Noah would likely have been diagnosed with Asperger Disorder, a condition characterized by problems with social communication, fixated interests, and average language skills. Asperger disorder was removed from DSM-5 , however, and Noah would probably be diagnosed with ASD today.
3. How does Noah display problems with the pragmatics of language?
Pragmatics refers to the use of language in specific social contexts. Noah has difficulty adjusting his use of language to suit his classmates. He also seems unable to recognize when his lectures about reptiles irritate or annoy others. He seems to talk “at” others rather than “with” others.
If Noah only showed deficits in pragmatic language and did not show problems with restrictive or repetitive interests or activities, he would be diagnosed with social (pragmatic) communication disorder, a DSM-5 communication disorder presented in Chapter 7.
4. Many toddlers later diagnosed with ASD show early deficits in social communication. What deficits did Noah show as a toddler?
Noah showed deficits in social orientation as a toddler. For example, he would not initiate interactions with his parents or other children or “share” objects that he enjoyed with them.
Noah also showed a lack of pretend/symbolic play as a toddler. His play was rigid rather than elaborate and imaginative. These deficits in pretend/symbolic play may also be related to his delays in language acquisition.
5. Why might early intensive behavioral intervention (EIBI) probably not be the first-line treatment for Noah? If you were Noah’s therapist, what skills would you target for treatment?
EIBI is most effective for preschool-age children with ASD, intellectual impairments, and/or poor language skills. Instead, Noah would likely benefit from training to help develop his social communication skills: how to initiate conversations with peers, how to engage in reciprocal interactions with others, for example. Ideally, these would be taught individually (in discrete trial training), in a group setting (to generalize skills), and then in real-life settings like school.
6. BONUS: Although some youths with ASD also have ADHD, the case study does not support the existence of comorbid ADHD. Why not?
By definition, children with ADHD show problems with hyperactivity-impulsivity and/or inattention across multiple settings (e.g., home, school, with peers). In contrast, Noah shows hyperactivity only at school and only in certain situations. It is likely that his hyperactive and irritable behavior is an indication that he is overwhelmed by social situations. His therapist might help him develop techniques to cope with these situations. For example, Noah might have a “code word” that he can tell his teacher when he feels upset or overwhelmed. He can use this “code word” to indicate that he needs to be temporarily excused from the activity.
Chapter 7: Communication and Learning Disorders
Animal noises.
Language Disorder (Late Language Emergence)
Josie is a 24-month-old girl who shows speech and language problems. Josie’s parents brought her to you, her pediatrician. “Josie’s vocabulary seems very underdeveloped,” her mother reported. “She doesn’t know very many words. She can make the correct noises for several animals when she sees them in a picture book, but she doesn’t know the names of any of the animals.” Her father added, “Josie also doesn’t seem to understand simple questions, like ‘Do you want juice?’ or obey simple commands like, ‘Give me your doll.’”
You quickly determine that Josie is physically healthy with vision and hearing within normal limits. She is able to point to her eyes and ears when you ask her to do so, but isn’t able or willing to follow more complex, two-step commands (e.g., get the ball and throw it into the basket ). Josie said “hi” and “bye” but was otherwise nonverbal. Her eye contact was ample during your assessment, and she seldom strayed from her parents.
After the session, Josie’s parents ask you, “So, do you think something is wrong with Josie? If so, what should we do about it?”
1. How would you assess Josie’s language skills?
A psychologist or speech–language therapist would probably want to assess Josie’s receptive vocabulary and expressive vocabulary. The scenario suggests deficits in both language domains.
2. What DSM-5 diagnosis best describes Josie’s communication problems?
Josie likely meets diagnostic criteria for language disorder (late language emergence). She shows
marked difficulties with the acquisition of language,
- language skills that are delayed compared to other children her age,
- the onset in childhood, and
- that she is otherwise healthy.
3. What other (differential) diagnoses might you want to rule out?
Information in the scenario rules out hearing problems as a cause of Josie’s language impairment. We would also want to make sure Josie does not have intellectual disability (Chapter 5) or autism spectrum disorder (ASD; Chapter 6) that can sometimes interfere with the acquisition of language in young children.
4. What is Josie’s prognosis?
Longitudinal data indicate that most children with late language emergence eventually catch up to their peers. However, 22% show persistent language problems or show other neurodevelopmental disorders, such as ASD. Josie’s language skills should be monitored carefully over the next 12 months and language therapy is warranted if her skills do not improve.
5. How might you use discrete trial training to increase Josie’s language production?
Discrete trial training to teach individual words, requests, comments, and statements is described extensively in the text. Most importantly, discrete trial training involves (1) the presentation of the linguistic stimulus, (2) the child’s utterance, and (3) immediate feedback and/or reinforcement by the therapist.
Production Problems
Language Disorder (Specific Language Impairment)
You are a speech–language therapist at a local elementary school. One of the kindergarten teachers at your school referred her student to you, a 6-year-old-boy named Jack. Jack had a history of language delays as a preschooler and had received speech therapy for problems with articulation prior to beginning school. Currently, his language skills are still poor.
“I can’t understand what Jack is saying most of the time,” his teacher reported. “He often says ‘gar’ for car and ‘gook’ for book . Jack often makes simple mistakes when speaking. For example, today he said, ‘Me got two gars’ instead of I have two cars . Yesterday, he described a classmate running in the hallway, saying, ‘Him run in gall.’ In general, Jack talks like a 3-year-old rather than a boy his age.”
You meet with Jack and briefly screen his receptive and expressive vocabulary. You notice that Jack has difficulty finding the right words to label objects. For example, when shown a picture of a watch, he called it a “tock” (i.e., clock). When shown a picture of a purse, he called it “Dat ting mom has. I not know what.” You also discover that Jack’s prereading skills, such as his ability to recognize letters and word–sounds (i.e., phonemes) are deficient. For example, he was only able to correctly identify 14 letters and he was unable to generate the sounds for the letters f , l , and s .
“What should we do?” Jack’s teacher asks.
1. What DSM-5 diagnosis best fits Jack?
Jack likely meets diagnostic criteria for language disorder (specific language impairment). He shows
- marked difficulties with the use of language due to deficits in both production and comprehension,
- language skills that are delayed compared to other children his age,
- that he is (probably) otherwise healthy.
2. Describe Jack’s phonology, morphology, grammar, and semantics.
Like many children with specific language impairment (SLI), Jack has problems in all four areas. First, Jack has poor phonemic awareness and lacks the ability to sound out even single letters. Most notably, he substitutes phonemes, such as /g/ for /c/. Second, he omits certain morphemes, such as when he drops word endings. Third, he makes grammatical errors when speaking, such as when he says, “Him run in gall.” Fourth, his semantic knowledge is somewhat limited; for example, he could not identify a watch or a purse. These errors suggest more pervasive underlying language problems than children with late language emergence alone (like Josie in the scenario before).
3. Identify three possible causes for Jack’s language problems.
Possible causes include the following:
- Genetics: Heritability estimates range from .50 to .75
- Brain abnormalities: Lack of left hemisphere enlargement of the lateral sulcus (near speech centers such as Broca’s area and Wernicke’s area)
- Auditory perception problems
- Deficits in rapid temporal processing
- Delays in short-term memory
- (Possibly) impoverished parent–child communication
4. How might you use conversational recast training to help Jack?
Conversational recast training is described in the text. The therapist structures the child’s environment to elicit the desired verbal behavior. Then the therapist provides feedback regarding the child’s utterances and reinforces correct language use.
5. How might you use milieu training to help Jack?
Milieu training is also described in the text. The therapist (or caregiver) tries to generalize the child’s language skills to real-world situations (e.g., home, school). When situations present themselves, the therapist prompts the child’s use of language and provides reinforcement contingent on correct language use.
Speech Therapy
Speech Sound Disorder (Articulation Deficits)
Doria is a first-grade student who was referred to you because of problems with speech and language. As the speech–language therapist at the school, it is your job to assess Doria and plan treatment, if you think it is appropriate.
Doria’s main problem is speech production. Specifically, she has great difficulty pronouncing the /r/ and /l/ phonemes. To informally assess her speech, you ask Doria what she likes to do on the weekends. She replies, “I weally wike to visit my dad. We wike to go to the movies or to the pawk.”
You question Doria’s mother about her speech problems. She replies, “Doria’s been talking this way since the age of 2. She has a wonderful vocabulary and is very expressive. However, people have a hard time understanding her. They often ask her to repeat herself. Doria doesn’t seem to mind too much.”
1. What is Doria’s primary DSM-5 diagnosis?
Doria likely meets criteria for speech sound disorder (SSD):
- She has persistent difficulty with speech production that interferes with communication.
- Her problems limit her ability to interact with others.
- Onset is in childhood.
- These difficulties are not attributable to other, medical causes.
2. What is the chance that Doria will “grow out of” her speech problem? Does she need therapy?
Longitudinal data indicate that 75% of young children with articulation problems learn to speak clearly on their own, without formal therapy. If her parents want speech therapy, it could begin immediately. Therapy is also warranted if Doria’s speech problems become upsetting to her or limit her academic functioning. Her parents could also simply monitor Doria’s speech over the next year to see if her articulation problems resolve on their own.
3. Identify the most common reason for her speech problem.
Doria’s articulation problems probably reflect immature speech production strategies. She likely adopted immature speech production when she first acquired expressive language (e.g., ages 1 to 3 years) and continues to use these strategies today despite the fact that they are developmentally nonnormative.
4. If you were to provide speech therapy, what would you do?
The text describes and provides examples of how a speech therapist might improve articulation using direct instruction. Important elements of treatment include (1) demonstrating correct lip, tongue, and teeth positioning when uttering the phoneme; (2) correcting mistakes immediately; and (3) repeatedly providing reinforcement contingent on clear articulation.
Just Baby Talk?
Speech Sound Disorder (Phonological Deficits)
You meet Geoffrey while volunteering at a local preschool. Geoffrey, an attractive, 5-year-old boy immediately likes you and wants to play. Although social and outgoing, Geoffrey’s speech is poor. It is very difficult for you to understand Geoffrey and you frequently need to ask him to repeat himself. After talking with him for a while, you realize that he tends to omit or reverse the sounds in certain words. For example, when you ask him about his favorite games, he answers, “I lie do blay wi my drober. We blay babbetba by da hou.” When you ask him about his favorite foods, he answers, “My pravite poods are mambergers, hotdas, an ide ream.”
You share your observations with Geoffrey’s preschool teacher. She comments, “Geoffrey has always had articulation problems. He has excellent receptive vocabulary and knows what he wants to say. He is just very difficult to understand. Many kids his age have articulation problems or engage in baby talk; we are not too worried. His speech will improve when he starts school.”
- What DSM-5 diagnosis best describes Geoffrey’s condition?
Geoffrey likely meets criteria for speech sound disorder (SSD).
A. He has persistent difficulty with speech production that interferes with communication.
B. His problems limit his ability to interact with others.
C. Onset is in childhood.
D. These difficulties are (probably) not attributable to other, medical causes (although we would need more information to confirm this criterion).
2. Identify one possible cause of his speech problem.
Unlike Doria, in the case above, Geoffrey’s has underlying problems with phonology that cause his articulation problems. Whereas Doria’s poor articulation likely reflects immature speech production (e.g., the way she positions her tongue or lips), Geoffrey’s poor articulation is probably caused by the way he mentally represents and uses phonemes (i.e., speech sounds). According to the phonological theory of SSD, subtle neurological impairments can cause children to perceive, differentiate, and use phonemes incorrectly while speaking, causing sound omissions, reversals, or substitutions.
3. What is Geoffrey’s prognosis? Will he improve without therapy?
Geoffrey’s articulation problems are probably more serious that Doria’s articulation problems. Approximately 40% to 80% of children like Geoffrey develop language disorder (specific language impairment; SLI). These children are also at risk for reading problems, given that phonemic awareness and phonics skills are important to reading acquisition. Most experts would recommend speech–language therapy without delay.
4. If you were a speech–language therapist, how might you help Geoffrey?
The text describes the use of direct instruction to help children with speech disorders. In addition, Geoffrey might benefit from several of the interventions designed for children with SLI, to help him develop greater phonemic awareness.
Teased in School
Childhood-Onset Fluency Disorder
Mark is a 9-year-old boy enrolled in the fourth grade at a local elementary school. Several years ago, Mark began stuttering. “Mark began having problems repeating certain letter sounds and syllables,” his mother recalled. “It was amazing how quickly the problem began. Over the course of a few weeks, it became very noticeable. Then, he would have trouble spitting words out. He would take long pauses, like he knew what he wanted to say, but couldn’t actually articulate the words.” She added, “Then, we noticed that he would tense up or grimace a little while trying to find the word he wanted. This became very noticeable to everyone. I think other kids teased him about it.”
With his mother present, you interview Mark in order to get a sample of his speech. When asked to talk about school, Mark said, “I-I-I-I reall-lly like school. I-I-I-I lllll-ike art and mmm-usic the b-b-b-est. Ssss-.”
His mother interrupted, “Don’t worry honey. Take your time.”
Mark continued, “Ssss-sometimes I have a hard ttt-ime in rrrrr-eading in class.”
After Mark left the room, his mother added, “Mark’s dad stuttered as a kid. He doesn’t stutter now. We’re hoping that Mark will outgrow this problem. What do you think?”
1. What is the official DSM-5 diagnosis for problems associated with stuttering?
Childhood-onset fluency disorder
2. What is the evidence that stuttering is heritable?
Stuttering is one of the most heritable communication disorders. For example, 28% of children who stutter have a parent with a childhood history of stuttering, like Mark.
3. What brain differences are observable in children who do and do not stutter?
Typically developing children show increased activity in left hemisphere brain regions responsible for language, especially Broca’s and Wernicke’s areas. Some children who stutter, however, show greater activation in the right hemisphere rather than the left hemisphere.
4. How might learning theory, emotion theory, and psycholinguistic theory be used to explain the causes of stuttering?
Learning theory: The two-factor theory of stuttering posits that children acquire stuttering through classical conditioning, as occasional disfluencies are paired with parental disapproval. Stuttering is maintained by operant conditioning when adults give attention to children when they stutter or excuse children from activities because of stuttering.
Emotion theory: Children who stutter often experience greater anxiety and apprehension while speaking, which can exacerbate their disfluent speech. The anticipatory-struggle theory posits that these children expect speaking to be anxiety provoking; this anxiety in turn compromises their fluency.
Psycholinguistic theory: The covert-repair hypothesis posits that children who stutter are very sensitive to minor speech disruptions. They closely monitor their speech and try to correct even small disfluencies while speaking, leading to pauses and repetitions.
5. What is the likelihood that Mark will overcome his stuttering problem on his own?
As many as 75% of children who stutter overcome this problem on their own. However, Mark might merit treatment immediately if his stuttering causes him great concern or interferes with his social functioning.
7. How might a therapist improve speech fluency in a boy like Mark?
The text describes and gives examples of speech therapy for children who stutter. Some important components of treatment include (1) using a soft/easy voice while speaking, (2) speaking at a slower rate, and (3) relaxing the muscles of the mouth and throat to control breathing. Treatment might also involve helping Mark cope with anxiety while speaking or responding to teasing from peers.
Problems Making Friends
Social (Pragmatic) Communication Disorder
Thirteen–year-old Ethan was referred by his parents, who were concerned with his social functioning. His father began, “I asked to meet with you because you are the psychologist at Ethan’s school. Ethan’s a great kid. He’s really bright and musically gifted. He does well in school and especially likes art, math, and science. All the time, he tells me how much he wants to be an engineer, like me, and work in my company when he grows up. But, Ethan has problems making friends. He really wants friends and he’s invited several other kids from school over to the house. But, he doesn’t seem to know how to play with the other kids. For example, when other kids are playing a game, Ethan doesn’t know how to join in. Then, if he sometimes manages to join the game, he insists on directing everything—being in charge.”
Ethan’s mother added, “He’s also pretty pedantic. He goes on and on about topics no other kid really cares about. I think it turns them off or wears them out over time. Kids come to the house to play maybe once or twice but they seldom return.”
You agree to meet with Ethan in your office the following day. With an awkward gait, Ethan enters your office, sits down on your chair and comments, “You would have really enjoyed it.”
“Enjoyed what?” you ask.
Ethan responds, “My little brother and I loved it, but my mom said it was too violent. I knew you would have loved it because you like those kind of things and because you’re young, not like my mom and dad. Besides, the Annihilation comics came out in 2014 and that was only a few years ago. You don’t look old enough to have read the original Marvel comics but you probably read the newer version when you were in school.” Ethan looks over at the Guardians of the Galaxy figurine on your desk.
You respond, “Do you mean that I would have liked the Guardians of the Galaxy movie? I saw it. I liked it a lot. What did you like about it?”
Ethan replies, “The original Marvel comics came out when my dad was a kid—about my age. Things were a lot different back then. Rocket had a different name.”
You ask, “They had rockets in the original?”
Ethan replies in a disgusted tone, “I thought you said you saw the movie? Not ‘rockets.’ I mean ‘Rocket’ the raccoon.”
“Oh, right. I forgot his name until you mentioned it,” you respond. “My favorite character was actually Groot, the plant-man. Didn’t you think he was funny?”
Ethan replies, “Then, maybe 20 years passed before they resurrected the series and produced the new comics. Most people say that the original was better but I like the newer ones . . .”
1. What DSM-5 communication disorder best describes Ethan’s behavior?
Ethan may meet diagnostic criteria for social (pragmatic) communication disorder.
- He has marked deficits in verbal (and probably) nonverbal communication.
- These social communication deficits limit his social interactions and ability to make friends.
- Onset is in childhood or adolescence.
- Symptoms are not better explained by another disorder such as intellectual disability or autism spectrum disorder (although we would need additional data to rule out autism).
2. What other (differential) diagnoses might you want to rule out?
We would need to gather information from parents and teachers to rule out autism spectrum disorder (ASD). Social (pragmatic) communication disorder is characterized by social communication deficits only . In contrast, ASD is characterized by deficits in social communication and repetitive behaviors or interests.
3. How might you encourage Ethan to show better turn-taking skills?
A therapist might use a verbal prompt (e.g., “It’s your turn now . . .”) or a physical prompt (e.g., a gesture) to help children learn turn-taking skills.
4. What is conversational repair and how might you improve Ethan’s conversational repair skills?
Conversational repair skills allow children to recognize when listeners cannot follow their stories and take steps to clarify or provide additional information to help listeners’ understanding. One technique to improve conversational repair skills is to help children with social (pragmatic) communication disorder recognize puzzled facial expressions that indicate a listener is confused or lost.
5. What are narratives and how might you improve Ethan’s narrative skills?
Narratives refer to coherent, logically organized stories that relate information to other people. Initially, a therapist might model appropriate storytelling using a familiar story. Then, the child can retell the story as the therapist gives feedback. Later, the therapist might introduce a structured way for the child to relate an autobiographical story (e.g., First, I did this; then I did that . . .). Finally, the therapist and child can practice scripts to organize stories about common, real-life situations (e.g., ordering food at a restaurant, going to the movies).
Delays or Deficits?
Specific Learning Disorder w/ Impairment in Reading
Sebastián is a 9-year-old third-grade student referred to you for a psychological evaluation to determine whether he has a learning disability and might qualify for special education services.
Information about Sebastián’s early development is limited. His parents, both migrant workers, moved to the United States when Sebastián was a toddler. His mother and father speak Spanish exclusively at home and have limited English-speaking skills. Sebastián acquired English during his preschool years through his interactions with other children, involvement in his church, summer programs for the children of migrant workers, and one year of formal kindergarten. A recent physical exam indicated that he is healthy and has no sensory problems.
Sebastián began showing delays in reading acquisition when he enrolled in his current school as a first-grade student. Although his receptive and expressive vocabulary were similar to other children his age, Sebastián could recognize only 16 of his letters and lacked the ability to phonetically decode (i.e., “sound-out”) letter combinations (such as th, st, tr ) or simple words (such as fish, pet, stop ). Recurrent colds and flu caused Sebastián to miss a lot of school later that academic year. Consequently, his teacher was uncertain whether his reading delays were attributable to missed learning opportunities at school, his history of impoverished educational opportunities, the fact that English is his second language, or an underlying learning disability.
In second grade, Sebastián’s reading skills fell further behind his classmates. Curriculum-based assessment using the DIBELS indicated the need for additional tutoring. Consequently, Sebastián progressed through Tier I and II interventions of the school’s RTI program. Although he showed some improvement in response to Tier II, small-group instruction, his reading skills continued to lag behind his peers at the end of second grade.
You decide to conduct a comprehensive assessment of Sebastián’s cognitive and academic functioning. Because his English-speaking skills are excellent, you administer the English versions of all tests. On the WISC-V, Sebastián earned a FSIQ of 103, squarely within the average range. His verbal comprehension score was slightly lower than his fluid and visual–spatial reasoning scores, but all three scores were within normal limits. However, Sebastián earned a score of 82 in processing speed, indicating below-average ability to process information quickly and easily.
On the Woodcock-Johnson-IV achievement tests, Sebastián’s Math score of 101 fell within the average range. However, his performance on the Broad Written Language (85) and Broad Reading (78) composites were below average to borderline compared to other children his age. In fact, Sebastián’s Broad Reading score exceeded only 7% of children his age in the standardization sample. Follow-up testing indicated basic reading skills similar to those of a typically developing first-grade student.
1. Does Sebastián meet DSM-5 diagnostic criteria for a specific learning disorder?
The information in the scenario suggests that Sebastián does meet diagnostic criteria for specific learning disorder with impairment in reading.
- He has longstanding problems with inaccurate word reading.
- His reading problems are substantially below those of other children his age (i.e., >1 SD below the mean).
- His reading problems emerged during his school years.
- His problems are likely not attributable to intellectual disability, sensory impairments, language differences or impairments, or inadequate educational instruction.
The scenario allows us to rule out intellectual disability, sensory impairments, and inadequate education as causes for his reading problems. However, some clinicians would want additional information to rule out language differences as a cause of Sebastián’s reading deficits.
2. How did Sebastián’s teachers use response to intervention (RTI) to identify and mitigate his early reading deficits?
RTI involves a tiered approach to intervention in which children with academic skill deficits receive progressively more intensive treatment. Sebastián received Tier I and II interventions, which likely consisted of large-group and small-group tutoring sessions, respectively. When these interventions did not allow him to make adequate progress, he was referred for comprehensive assessment.
3. What is the difference between curriculum-based assessment and norm-referenced assessment? Which type of assessment did Sebastián receive?
Curriculum-based assessment involves measuring children’s academic progress toward benchmarks established by the school. Children who fail to reach these benchmarks at certain ages may be referred for more intensive intervention.
Norm-referenced testing compares children to other youths of the same age, to determine their relative standing (i.e., average, above average, below average). Sebastián received both types of assessment: the DIBELS is a curriculum-based test often used in RTI whereas the WISC-V and WJ-IV are norm-referenced tests often used in comprehensive assessment.
4. Are children whose primary language is not English at greater risk for learning disabilities than native English-language speakers?
Empirical data indicate that children whose primary language is not English are not at increased risk for learning disabilities. However, children who are not proficient with spoken English by the time they begin school or who are referred to English as a Second Language (ESL) programs are at risk for learning disabilities.
5. What is phonemic mediation and why might it be important to explaining Sebastián’s reading problems?
Phonemic mediation is the ability to use phonemic awareness and phonics skills to sound out novel words. Children with learning disabilities in reading often have poor phonemic awareness and phonics skills and have problems with phonemic mediation. Consequently, they have difficulty sounding out words they do not know.
Youths with poor phonemic mediation skills often memorize words based on their appearance or use context cues to infer words. These strategies eventually prove problematic as words become more complex and context cues, like pictures, become less frequent. Sebastián showed poor phonemic awareness, indicating this might be an underlying cause of his reading problems.
6. What intervention has the greatest empirical support for children with reading deficits like Sebastián?
Systematic instruction in phonemic awareness and phonics is effective in improving children’s reading skills if implemented before the end of the third grade. The textbook describes and illustrates the use of direct instruction as an evidence-based method to teach and reinforce these skills.
Not Adding Up
Specific Learning Disorder w/ Impairment in Mathematics
Maddie is an 11-year-old girl who was referred to you by her parents because of her recent decline in math at school.
“Maddie’s a great kid. She’s very conscientious, always tries her best, and loves to read and write,” reported her father.
Her mother added, “She used to like math too. She learned to count, add, and subtract without much trouble. She started to stumble when she tried to learn multiplication. It took FOREVER for her to learn her times tables. I think she still has problems with some of them.”
“Since that time, about third or fourth grade, Maddie has really struggled in math,” said her father. “Initially, her teacher provided after-school tutoring for her. When that didn’t work, she was placed in a special class for kids who had difficulty with math. We didn’t notice much improvement, so we hired a tutor on our own. The tutor helps Maddie with her homework, but I’m not sure it has really helped her acquire the skills she needs.”
“Maddie, how do you feel about math?” you ask. With an embarrassed look, Maddie begins to speak, pauses, and then starts to cry. “I hate it,” eventually escapes from her mouth. “Nothing I do is ever right.”
You decide to conduct a comprehensive evaluation to assess Maddie’s intellectual abilities and academic achievement. Results of the WISC-V indicated a FSIQ of 115, above average compared to other children her age. Maddie showed a significant relative strength in verbal comprehension (standard score = 119) but a significant weakness in working memory (standard score = 81). Follow-up testing confirmed that Maddie has marked deficits in both her verbal and nonverbal working memory compared to other youths her age.
As you expected, Maddie’s reading and written language scores on the WJ-IV were well above average. Unfortunately, her score on the Broad Math domain was below average (standard score = 80). Interestingly, Maddie earned an average score on a test of math fluency, indicating that she could solve simple arithmetic problems quickly and efficiently. However, her ability to perform higher-level math calculations and story problems was much delayed, exceeding only about 5% of youths her age in the norm group.
1. Does Maddie meet DSM-5 diagnostic criteria for a specific learning disorder?
The information in the scenario suggests that Maddie does meet diagnostic criteria for specific learning disorder with impairment in mathematics.
- She has longstanding problems with mathematics. We would need more information to know exactly where her deficits are, but the scenario suggests problems memorizing math facts (i.e., times tables) and performing math calculations.
- Her math skills are substantially below those of other children her age (i.e., >1 SD below the mean).
- Her math difficulties emerged during her school years.
- Her problems are likely not attributable to intellectual disability, sensory impairments, language, or inadequate educational instruction.
2. Maddie earned a very low score on the WISC-V working memory index. What is working memory and why might it be important to understanding the cause of Maddie’s problems with math?
Working memory is the ability to hold information in short-term memory, manipulate or process the information in some way, and use the information to solve problems. Youths with learning disabilities in the domain of mathematics often show deficits in working memory. These deficits can interfere with their ability to recall and apply math facts, remember and synthesize different bits of information to solve a problem, or perform multistep calculations. Memory problems can also interfere with children’s ability to recall and apply math procedures, such as how to do long division or how to “borrow” numbers in a multidigit subtraction problem.
3. Neither Maddie nor her parents reported problems with her reading skills. Why was it important to assess Maddie’s reading skills when assessing her for a learning disability?
Some children with math disabilities experience difficulties solving math story problems because they have poor basic reading or reading comprehension skills. By assessing Maddie’s reading skills, we can rule out reading deficits as a cause for her difficulty solving math story problems.
4. What three interventions are likely effective in helping students with math disabilities, like Maddie?
The textbook outlines three evidence-based techniques to improve children’s math skills: (1) direct instruction, (2) self-instruction, and (3) mediated/assisted instruction. Meta-analyses indicate that all three methods yield moderate to large benefits for school-age children.
5. BONUS: How might Maddie’s thoughts about math interfere with her ability to accurately solve math problems and do well in math class? If you were her parent, teacher, or therapist, how could you help Maddie think differently about math?
Cognitive therapists believe that people’s feelings are influenced by their thoughts about events rather than by the events themselves (see Chapter 4). Maddie views math negatively and sees herself as unable to do well in math class. A cognitive therapist might view her beliefs as a cognitive distortion, that is, Maddie may twist reality to make math seem more difficult than it really is and herself as less capable than she really is. Her maladaptive thoughts about math probably lead her to avoid practicing math and getting better at it. Consequently, she falls further behind her peers.
One intervention strategy is to help Maddie challenge her maladaptive ways of thinking. Is it really true that “ nothing ” she does is ever right? It is likely that Maddie is a good student in most subjects besides math, such as language arts. Even in math class, there might be some aspects of math that she is better at than others (e.g., math fluency). Perhaps she and adults in her life can find ways to compensate for her weaknesses in math so that she can feel better about math class and school more generally.
Chapter 8: Attention-Deficit/Hyperactivity Disorder
Little red rooster.
ADHD, Predominantly Hyperactive-Impulsive Presentation
Tricia Newsome slumped into the large chair in my office, looking much older than the 35 years she indicated on the new patient information sheet. “I’m at my wits end,” she began. “I’m coming to you because I don’t know where else to go.” With downcast eyes, outlined by dark circles, she explained the reason for her visit: her 6-year-old son, Bennett.
Mr. and Mrs. Newsome were overjoyed when they discovered that they would finally have a child after many years of infertility. Mr. Newsome was an ecologist, whose job allowed him to work outdoors most of the year, trapping, tagging, and monitoring animals for the fish and wildlife service. Mrs. Newsome was a pharmaceutical representative who decided shortly after Bennett’s birth to stay home with her newborn baby. The couple doted upon Bennett who they described as a healthy, bouncing baby boy.
The problem, according to Mrs. Newsome, was that Bennett never stopped bouncing. “Even as an infant, Bennett was restless. He never wanted to eat and I had to force him to take a bottle. Later, when he began to eat solids, I had to fight to keep him in the high chair or at the table. He was also an erratic sleeper. He didn’t sleep through the night until he was over 12 months of age—if you call sleeping 6 hours ‘sleeping through the night.’ Every morning, he’d wake up before sunrise and get into mischief. My husband called him ‘the little red rooster’ because of his early morning waking, but I prayed that one day he might sleep later and let me rest.”
“Bennett is a handful. He’s always moving—his legs, his arms, his middle. He can’t sit still for more than a few minutes at a time and he has absolutely no attention span. He’ll begin one activity, like playing with toy cars, and then move onto another activity after only a few minutes.
My home is a mess because he leaves his toys everywhere. Bennett’s also a chatterbox. He never stops talking. It doesn’t really matter if I’m listening or not; he’ll even talk to himself. He’ll interrupt me when I’m talking to other people, on the telephone, or doing work on the computer. He demands constant attention.”
“Does Bennett act the same way at school?” I asked.
Mrs. Newsome replied, “That’s why I’m here. His teacher wants me to take him to his pediatrician and have him receive medication for ADHD. Apparently, Bennett engages in the same high-rate behavior at school as at home. He doesn’t listen to directions, can’t wait his turn, and frequently interrupts lessons. His classmates have started to avoid him because even they find his behavior aversive.”
I asked, “Is Bennett ever deliberately disrespectful to you or your husband? For example, does he talk back to you, refuse to do chores, or lose his temper?”
She replied, “Not any more than other first graders. His teacher says that he tries hard to be good at school, but can’t seem to help himself. It’s as if he has more energy than most kids his age and doesn’t know what to do with it.”
Mrs. Newsome added, “Do you think Bennett has ADHD? He seems to have all of the features—according to Web MD. I really don’t want to put him on medication. He’s so young.”
1. Review the DSM-5 signs and symptoms of ADHD. Which signs or symptoms does Bennett show, based on his mother’s and teacher’s reports?
Bennett’s symptoms fall mostly within the hyperactive-impulsive domain:
- fidgets or squirms
- leaves his seat
- unable to play quietly
- talks excessively
- blurts out answers
- difficulty waiting his turn
- interrupts others
Bennett shows some inattentive symptoms, but not enough to meet the > six symptoms diagnostic threshold:
- difficulty sustaining attention on play activities
- does not follow instructions
2. What DSM-5 diagnosis best describes Bennett’s behavior, based on the available information?
3. Imagine that Bennett showed hyperactive-impulsive behavior only at home, but not at school. Could he still be diagnosed with ADHD? Why or why not?
DSM-5 requires children to show several ADHD symptoms in at least two domains (e.g., home and school). If Bennett only experienced symptoms at home, he would not qualify for the ADHD diagnosis. Because ADHD is a neurodevelopmental disorder, children with the disorder should show signs and symptoms in all settings that require attention and/or behavioral inhibition.
4. Why did the psychologist ask Bennett’s mother if Bennett was deliberately disrespectful to adults?
The psychologist is assessing whether Bennett also engages in oppositional-defiant behavior and might meet diagnostic criteria for oppositional defiant disorder (ODD; see Chapter 9). ADHD and ODD often co-occur; between 54% and 67% of children with ADHD also have ODD.
Children with ADHD alone do not deliberately misbehave. According to Russell Barkley, children with ADHD know how they should act, but they have difficulty regulating their attention and inhibiting their overt actions to follow the rules at home and at school. Bennett seems to have ADHD without comorbid ODD.
5. How common is it for a young child, like Bennett, to exhibit mostly hyperactive-impulsive symptoms, but not inattentive symptoms?
Longitudinal research shows that the ADHD hyperactive-impulsive symptoms usually emerge first, between 3 and 4 years of age. Most children who initially show these hyperactive-impulsive symptoms will also experience inattentive symptoms, sometime between the ages of 6 and 12 years.
6. Why might the psychologist who conducted the evaluation want to assess Bennett’s cognitive and academic skills?
On average, children with ADHD show cognitive deficits in areas of attention and memory. These deficits can interfere with the acquisition of academic skills. On average, children with ADHD score lower than typically developing children on standardized measures of reading, math, and written language. Children with ADHD are also more likely than typically developing children to be classified with a learning disability, to be referred for special education, to repeat a grade in school, or to withdraw from school before graduation.
7. How common are sleep problems among children with ADHD? Identify two sleep disorders typically shown by these children.
Approximately 50% of youths with ADHD, like Bennett, experience sleep problems. Two common sleep problems are (1) dyssomnias, such as refusing to go to sleep or problems staying asleep; and (2) sleep movement disorders, such as excessive tossing and turning during sleep. Bennett seems to have the most problem with dyssomnias such as sleep refusal and early morning waking.
8. The psychologist did not ask whether Bennett’s mother or father had problems with attention or hyperactivity-impulsivity as children or if they experience similar problems today. Why might assessing the family’s history for ADHD be important?
ADHD is heritable; genetic factors explain 70% to 90% of the variance in children’s ADHD symptoms. It is possible that one of Bennett’s parents has a history of ADHD symptoms, although he or she might not have been formally diagnosed or treated. For example, his father’s job allows him to work outdoors and be active most days. Perhaps he sought this type of employment because it demands less sustained attention and behavioral inhibition.
9. Mrs. Newsome is reluctant to allow Bennett to take medication to manage his symptoms. What evidence-based, psychosocial treatments are available for children his age?
The book describes several evidence-based, behavioral treatments for young, school-age children with ADHD. They include (1) clinical behavior therapy, (2) summer treatment programs, and (3) behavioral classroom management.
10. The psychologist wants Mrs. Newsome to make an informed decision regarding the best form of treatment for Bennett: medication, psychosocial treatment, or combined medication/psychosocial treatment. Based on the available empirical evidence, what should he tell her?
Results of the multimodal treatment of ADHD (and similar) studies indicate that combined treatment is slightly more effective than either medication or psychosocial treatment alone in managing children’s ADHD symptoms. Furthermore, medication alone is typically more effective than psychosocial treatment alone. Therefore, most experts recommend medication as a component of treatment. However, if Mrs. Newsome wants to pursue psychosocial treatment only, several evidence-based interventions are available (see question 9 above).
Forgotten Faith
ADHD, Predominantly Inattentive Presentation
Eleven-year-old Faith sat in the front row of her fifth-grade classroom, listening to her teacher explain the difference between proper and common nouns. Except, Faith wasn’t really listening. Anyone visiting her class that day would have thought that Faith was a model student. She sat in her desk quietly, eyes forward, feet solidly on the floor, chewing on the side of her pencil. Her teacher knew better.
“Faith,” Mrs. Kline said, abruptly pausing her language arts lesson. “Are you with us?”
Faith’s eyes suddenly widened. She shook her head, oriented herself to her teacher, and glanced quickly around the room at her classmates who were beginning to snicker. Of course, Faith had no idea what the subject of today’s lesson was. For at least the last 15 minutes, her mind had wandered from language arts, to crows outside her classroom window, to last night’s soccer game, to a friend’s upcoming birthday party, to whatever. Her teacher’s reprimand brought Faith back to earth.
Faith began to show problems with inattention and mind wandering only in the past academic year. Mrs. Kline initially thought that she was sick or she was not getting sufficient sleep at home. She seemed to be chronically tired, slow, and lethargic. After Faith’s parents (and pediatrician) confirmed that she was healthy, Mrs. Kline looked for other explanations for Faith’s inattentiveness. Maybe she was depressed or preoccupied by troubles at home? Maybe she had a learning disability and simply had trouble following lessons? Maybe she couldn’t see the board?
Assessment by the school psychologist and school nurse ruled out these possibilities however. Moving Faith’s desk to the front row of the classroom, periodically calling on her to direct her attention, and pasting sticky notes to her desk to remind her of important assignments did not help. Faith still couldn’t focus on lessons, made careless mistakes on assignments and tests, and didn’t complete activities that lasted for more than a few minutes. Her desk and locker were a mess because of her poor organizational skills.
As Mrs. Kline returned to her lesson, Faith’s eyes gradually began to glaze over. She tried very hard to focus on which nouns need to be capitalized and which do not. She knew that information would be important for the test tomorrow. But, for some reason, it was no longer important. Faith’s attention was now on the scarf around Mrs. Kline’s waist. How had she not noticed it before? It had a butterfly pattern that resembled a monarch. She wondered if the milkweed would grow in the field near her house again this year, what other kinds of foods monarchs might eat if milkweed was not available, and what she might eat for dinner tonight . . .
1. What DSM-5 signs or symptoms of ADHD does Faith show?
Faith shows predominantly inattentive signs and symptoms:
- makes careless mistakes in schoolwork
- difficulty sustaining attention
- does not seem to listen when spoken to
- difficulty organizing activities
- loses things
- easily distracted
2. What additional information would we need to know in order to diagnose Faith with ADHD, predominantly inattentive presentation?
We would need to confirm that Faith experiences some inattentive symptoms in other settings, not only at school. To do this, we would likely want to interview her parents and administer norm-referenced behavior rating scales, like the Conners 3, to her parents and her teacher.
3. What features of “sluggish cognitive tempo” does Faith display?
The features of “sluggish cognitive tempo” overlap somewhat with the inattentive symptoms of ADHD. In addition, sluggish cognitive tempo is characterized by the following:
- daydreaming
- mentally foggy
- acting spacey/mind is elsewhere
- Having a drowsy/sleepy appearance
- lost in thoughts
It is noteworthy that sluggish cognitive tempo is not a DSM-5 disorder. However, some researchers believe it reflects a distinct ADHD subtype or qualitatively different attention disorder.
4. In samples of clinic-referred children, the gender ratio for ADHD favors boys, approximately 10:1. In samples of children from the community, the gender ratio is only 3:1. What might explain this difference?
Girls, like Faith, disproportionately show ADHD, predominantly inattentive presentation, which is likely to emerge later in childhood and is less likely to elicit a referral for treatment by parents and teachers. Often, children with inattentive symptoms only are overlooked because they do not engage in disruptive behavior at home or school.
5. What is the default mode network and why might it be important in explaining Faith’s attention problems at school?
The default mode network is active when we engage in mind wandering or daydreaming. Brain regions in this network include the prefrontal, parietal, and temporal cortices. Children with inattention may have difficulty inhibiting this neural network and focusing their attention on tasks.
6. Can improving children’s duration and/or quality of sleep reduce their inattentive symptoms?
Randomized controlled studies indicate that improving children’s sleep duration and quality or increasing children’s cardiovascular exercise can reduce signs and symptoms of ADHD. Although insufficient sleep or exercise likely does not cause ADHD, symptom reduction can occur if sleep or exercise levels are improved. Medication and behavior therapy, however, are first-line treatments for ADHD in children.
Chapter 9: Conduct Problems in Children and Adolescents
Choose your own (parenting) adventure.
Coercive Family Process
Amanda looked at her phone. It was already 9:15 p.m., her 5-year-old daughter’s usual bedtime. Work had run late, she didn’t get home until 7:30 p.m., and traffic was worse than she expected. After picking up Jamie from her sister’s house, she had time to grab a salad at the supermarket deli and a few items that she needed for Jamie’s lunch the next day. Luckily, the market was not too busy on a Wednesday night and she quickly led Jamie to the checkout isle.
“Hey, mom, can I have one of these peanut bars?” Jamie asked.
Amanda almost didn’t hear Jamie. She was thinking about tomorrow’s schedule. Looking down at the tired girl, she said, “No sweetie. It’s late and you already brushed your teeth at Aunt Tara’s house.”
Jamie begged, “But I’m hungry. I didn’t eat much dinner. And you got something to eat.”
Sheepishly, Amanda looked at the salad in her basket. Then she remembered the time and could only think about getting Jamie to bed as soon as possible. The last thing she needed was a sugared-up, five-year-old insomniac on her hands. “No baby. I’m just getting a few things and then we’re going home to bed.”
Jamie didn’t link that answer. She repeated her request. Then, she began to complain, then whine, then cry. “I’m so hungry. Why can’t I? Please???” Jamie kicked the shopping cart in time with her protests for added emphasis. Amanda was sure that Jamie was acting this way deliberately to annoy her. Jamie knew how to press her buttons, especially at the end of the day.
The checkout person, clearly annoyed, narrowed her eyes on Amanda. Amanda could read the checkout person’s mind, “Don’t you have any control over your kid? Why didn’t you feed her a decent meal? What are you doing at the supermarket with a 5-year-old at 9:30 on a school night in the first place?” Amanda felt a flood of emotions: anger, despair, fatigue.
If you were Amanda, what would you do and why?
- Buy Jamie the peanut bar. After all, peanuts are healthy, right?
- Stand firm, even if that means yelling or threatening Jamie with punishment. You need to show her who’s the parent and who’s the child.
- Ignore her. Let her protest all she wants. She might tantrum in the middle of the supermarket, but hey, it’s Walmart. She won’t be the first kid to do that.
The case study illustrates Patterson’s coercive family process. According to this process, parents often model and reinforce oppositional, defiant, and aggressive behavior to their children although they are usually unaware that they are doing so. The case study also illustrates how parent’s cognitions about their children and their own parenting skills can affect their quality of parent–child interactions. It is likely that students will know that option C is probably the best course of action for Amanda. However, students should explain the problems with options A and B in order to review concepts presented in the text.
Option A: If Amanda gives in, she will complete the cycle of reinforcement that defines the coercive family process. Although she initially denies Jamie’s request for the peanut bar, Jamie protests and escalates her aversive behavior by complaining and whining (an extinction burst). If Amanda backs down and buys Jamie the candy, Jamie will likely be positively reinforced for whining and complaining; she is more likely to whine and complain to get what she wants in the future. At the same time, Amanda is negatively reinforced for acquiescing to Jamie’s demands. Amanda learns that she can get Jamie to stop whining and complaining by backing down. This coercive process underlies many oppositional-defiant behaviors in young children.
Option B: Let’s assume that Amanda yells, threatens, or spanks Jamie. Amanda has used hostile-coercive behavior to gain her daughter’s compliance. Amanda is negatively reinforced for engaging in hostile-coercive behavior to silence her daughter. Amanda may be more likely to yell, threaten, or spank Jamie in the future. Amanda has also modeled hostile-coercive behavior to Jamie. Jamie might learn, through her observations, that yelling, threatening, or hitting another person is an effective way to gain his or her compliance. Hostile-coercive parenting behaviors, such as yelling, threatening, and spanking, (although reinforcing in the short-term) often underlie defiant and aggressive behavior.
Note also how Amanda’s attributions for her child’s behavior and other parenting cognitions contribute to her negative emotions. She attributes Jamie’s tantrums to internal, volitional causes and she views herself as powerless. She also engages in the cognitive distortion of “mind-reading” in which she assumes the checkout person thinks that she is a bad parent. These thoughts may make it more likely that she will engage in hostile-coercive parenting behavior.
Option C: This option illustrates the use of planned ignoring in a naturalistic setting. Amanda will tell Jamie “no” in a clear, firm voice and then ignore her bids for attention. Jamie might protest, but Amanda will attempt to extinguish Jamie’s aversive behavior by denying any positive reinforcement. (Even yells, threats, and spanks can be positively reinforcing to some children.) Amanda will likely be embarrassed, but she avoids giving into Jamie’s demands and the use of hostile-coercive actions toward her child. If you see a parent in the supermarket use planned ignoring, you should buy that parent a candy bar!
Social Information Processing Model
Twelve-year-old Aiden loved soccer. That’s why it was sheer torture for him to miss even a minute of recess. All morning long, he waited for the chance to escape his classroom and run to the field outside his school to play during lunchtime. Unfortunately, today Aiden was late for recess because he had “lunch duty” and it was his responsibility to make sure the tables were clean after everyone had eaten.
When he was finished, Aiden dashed to the soccer field. Dismayed, he discovered that the other boys had already started and were in the middle of a close game.
“Which team should I be on?” Aiden asked one of the boys.
The boy responded curtly, “Neither. Take a seat.”
Another boy said, “Yeah. The game’s too close.” Several other boys snickered and then ran off after the ball.
Aiden felt a rush of warmth spread from the middle of his chest to the center of his face. He didn’t know exactly how he felt. Was it pain? Disappointment? Rejection? Anger? Whatever the feeling, it was not good and Aiden knew he needed to do something about it.
1. Identify the six main components of Crick and Dodge’s (1994, 1996) social-information processing model.
This model is presented in the text and reproduced below. The stages include (1) encoding cues, (2) interpreting cues, (3) clarifying goals, (4) response access, (5) response decision, and (6) behavioral enactment and peer evaluation.
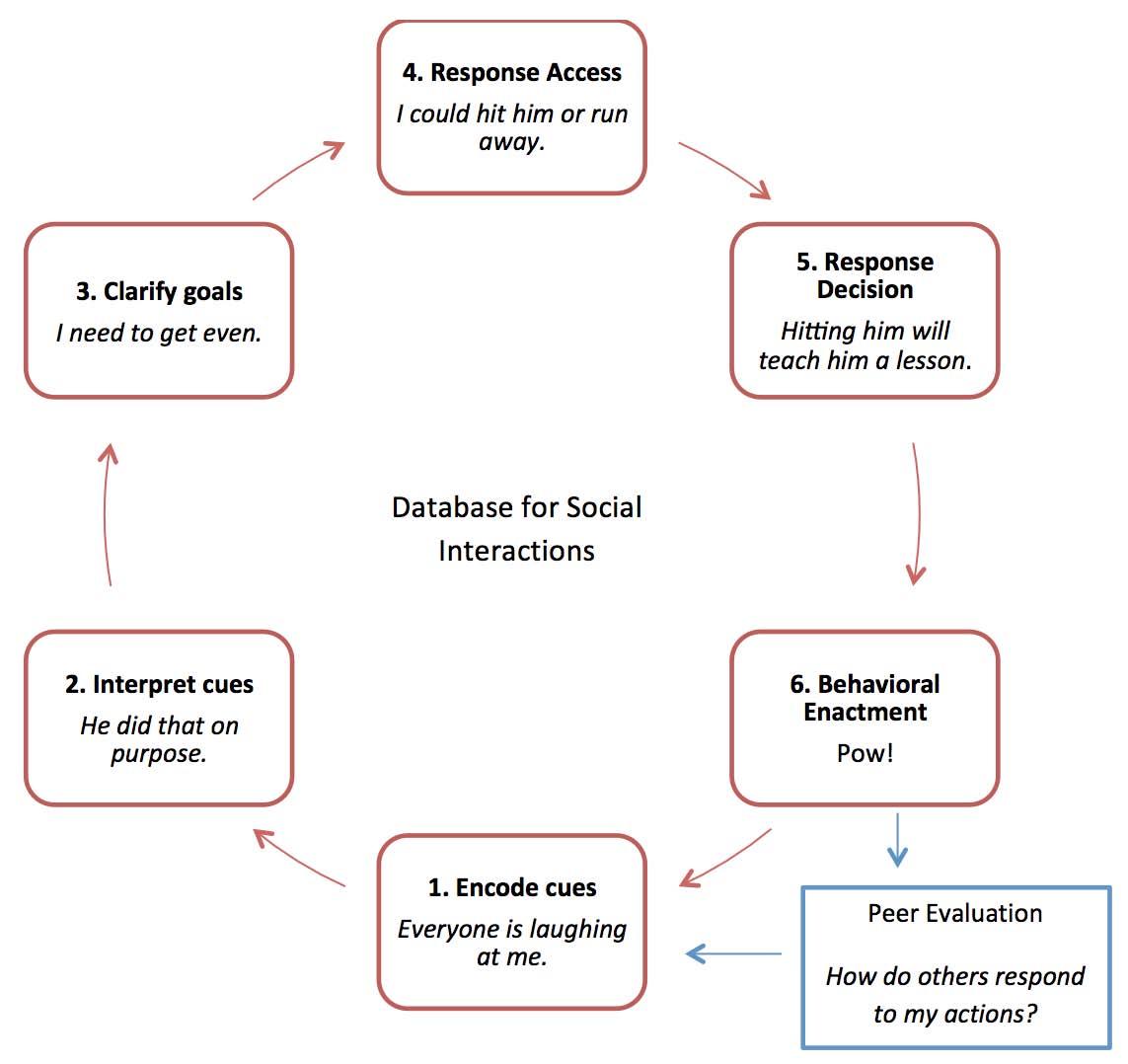
2. If Aiden was a boy with a history of reactive aggression, what sort of biases might he show in his social information processing?
Children who engage in reactive aggression tended to have hostile attributional biases for others’ behaviors. Specifically, they exhibit biased problem-solving in steps (1) encoding cues and (2) interpreting cues. In step 1, Aiden might focus chiefly on his negative emotions (internal cues) or the other boys’ negative words or expressions (external cues). In step 2, Aiden might believe that the boys were excluding him from the game to be deliberately hurtful or because they do not like him. Aiden might not pay attention to alternative causes for the boys’ behavior. For example, perhaps the boys did not want him to join because the game was close and Aiden might make the teams unbalanced or unfair if he joined the game. Alternatively, perhaps the boys’ actions were hurtful because they were angry about losing the game, and not because they disliked Aiden.
3. If Aiden was a boy with a history of proactive aggression, what sort of biases might he show in his social information processing?
Children who engage in proactive aggression often show biased problem solving in steps 3 through 5. In step 3 (clarifying goals), Aiden might immediately identify an aggressive goal for the social dilemma. For example, he might impulsively decide that he wants to “get even” with the boys for being mean to him or excluding him from the game. An alternative, nonaggressive goal might be for Aiden to “remain friends” with the boys by being patient. Perhaps they will let him join the game later.
In step 4 (response access), Aiden might have difficulty generating or recalling a large number of possible ways to respond in this social situation. Instead, he might be able to generate only one or two possible solutions and these solutions will likely be aggressive in nature (i.e., yell, shove, hit). The ability to generate possible solutions partially depends on Aiden’s “database for social interactions,” that is, his history of interpersonal dilemmas. If he has seldom seen or used prosocial methods to solve problems in the past, it is unlikely that he will be able to access prosocial methods to solve this current social dilemma.
In step 5 (response decision), Aiden will likely select an aggressive course of action. Many children with histories of proactive aggression overestimate the reinforcement and underestimate the punishment that aggressive actions bring.
4. After Aiden enacts his solution to this social problem, how does the social information-processing model repeat itself?
According to Crick and Dodge (1994, 1996), after Aiden enacts his solution to the social dilemma, his peers will respond to his behavior. For example, the other boys might make fun of Aiden, ignore him, or allow him to join the game after all. Their behavior, in turn, provides a new set of cues that must be encoded, interpreted, and responded to—setting the model in motion again.
5. If you were Aiden’s therapist, how might you use problem-solving skills training (PSST) to help him avoid conflicts with peers?
In PSST, the therapist teaches children the social problem-solving steps in order to (1) avoid hostile attributional biases and (2) generate and select more prosocial solutions. The problem-solving steps include the following:
- What am I supposed to do?
- What are all my possibilities?
- I’d better concentrate and focus in.
- I need to make a choice.
- Evaluate: I did a good job or I made a mistake.
Crick, N. R., & Dodge, K. A. (1994). A review and reformulation of social information-processing mechanisms in children's social adjustment. Psychological Bulletin , 115 , 74–101.
Crick, N. R., & Dodge, K. A. (1996). Social information‐processing mechanisms in reactive and proactive aggression. Child Development , 67 , 993–1002.
Chapter 10: Substance Use Disorders in Adolescents
Pathways to substance use problems.
Various Substance Use Disorders
Preston Allen was referred to the Montgomery County rehabilitation center because of chronic problems with heroin use. Although Preston was only 17-years-old, he had a longstanding history of psychosocial stress, disruptive behavior, and substance use problems.
Preston’s mother, Gina Herriot, worked as a medical assistant in a local clinic. Preston’s father, Mark Allen, held various semiskilled jobs over Preston’s childhood and is currently employed in a food processing plant. The couple divorced when Preston was 15 years old, following a tumultuous relationship characterized by frequent verbal arguments and (on two occasions) physical altercations requiring police involvement. Indeed, Preston’s father has a history of arrests ranging from physical assault, breaking and entering, driving while intoxicated, and possession of marijuana with intent to distribute. Preston has little contact with his father today.
As a preschooler, Preston added to his parents’ troublesome family life by showing emerging problems with hyperactivity, impulsivity, and inattention. His mother described him as a “risk-taker” and “dare-devil” who “couldn’t sit still or take no for an answer.” Preston always seemed to be in motion, up to mischief, or doing things to gain the attention of others (either good or bad). A psychological evaluation, conducted when Preston was 6-years-old also indicated significant oppositional and defiant behavior toward his mother who reported feeling “totally stressed out” by his hyperactive and noncompliant behavior.
Preston’s behavior problems continued into elementary school. He was frequently reprimanded by teachers for talking, leaving his seat, and breaking class rules. He would deliberately annoy classmates, largely to escape the monotony and boredom of the classroom. His classmates came to fear and despise him. He was referred to a special education program for children with learning delays and “emotional disturbance.” The school counselor’s report described him as “a boy whose behavior problems mask underlying feelings of sadness and loneliness.” The counselor suggested that his mother become more involved in Preston’s schooling, but her hectic work schedule and marital stress interfered with her ability to devote more time to her son.
In junior high school, Preston had been rejected by most youths his age and began associating with older adolescents from the adjacent high school. These new friends, who had behavior problems themselves, introduced Preston to more serious, antisocial behaviors. Preston began skipping classes, staying out late without his mother’s permission, and using cigarettes and alcohol. Preston noticed that cigarettes increased his concentration while, at the same time, reduced tension and anxiety. He used alcohol (and later marijuana) to get “messed up” and enjoy himself with his friends. For the first time in his life, Preston felt like he had a group of friends who liked him “for who he was.” Unfortunately, Preston spent considerable time and effort trying to access these substances. As his substance use increased, his school attendance and performance plummeted.
In high school, Preston had begun stealing prescription pain medications from his father and paternal grandmother. He initially used these medications recreationally with his friends. However, he soon noticed that he developed pharmacological tolerance for these medications and began taking them daily to alleviate anxiety and avoid withdrawal symptoms (e.g., headache, nausea, tension). When his father moved out, Preston lost access to these medications. He began using heroin which he obtained from the “friends of friends” in his neighborhood. Preston became dependent on heroin relatively quickly and used nearly any means necessary to obtain it. At the age of 16, he and two young men were arrested for stealing items from parked cars with the intention to sell these items to purchase drugs. Preston was also found in possession of marijuana and prescription medication, which he often sold to high school students to help support his own drug habit.
Now 17, Preston was referred for inpatient treatment to help him discontinue heroin and other substances in a controlled, medical environment. “I really want to change,” he told the substance abuse counselor who conducted his initial interview. “I’m ready to turn over a new leaf. I hope that you’ll give me one more chance to turn my life around.”
The counselor reviewed Preston’s psychological and medical records. He noticed that Preston had used these same words to describe his situation many times before.
1. Review the DSM-5 diagnostic criteria for substance use disorders. Which signs and symptoms does Preston show?
Preston shows the following signs and symptoms:
- use in large amounts
- problems cutting down
- time spent obtaining the substance
- failure to fulfill major role obligations (school)
It is likely that we can infer that he shows other signs and symptoms (e.g., use in potentially harmful situations) too, although these are not explicitly mentioned in the case study.
2. How does Preston’s psychosocial history reflect the deviance-prone model for substance use disorders?
The deviance-prone model (shown below) is the most common pathway for the emergence of substance use problems in adolescents. According to this model, children inherit a genetic diathesis toward psychological problems. Preston seems to have been at genetic risk for both disruptive behavior problems (as evidenced by ADHD in childhood and his father’s history of antisocial behavior) and substance use problems (as evidenced by his father’s substance use problems). Preston also showed problems with neurobehavioral disinhibition in early childhood characterized by (1) impulse control, (2) anger, and (3) ADHD signs and symptoms. These problems caused prosocial peers to reject him and older, deviant peers to introduce him to antisocial behavior and substance use. His father’s absence and his mother’s high level of stress likely compromised their ability to monitor and control his behavior. Over time, the frequency and severity of Preston’s antisocial actions and substance use increased, resulting in arrest and referral for substance abuse treatment.
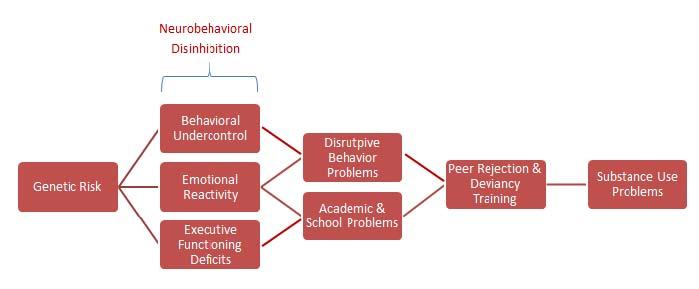
3. How does Preston’s psychosocial history reflect the negative affect model for substance use disorders?
The negative affect model (shown below) is often helpful in explaining the emergence of substance use problems in adults. However, aspects of the model can be seen in Preston’s psychosocial history. Preston’s tumultuous family life likely caused considerable psychological distress (e.g., anger, anxiety, tension). Similarly, Preston experienced problems with attention and concentration related to ADHD. He found that various substances were useful in alleviating anxiety or inattention (i.e., nicotine in cigarettes), reducing psychological distress or emotional pain (i.e., marijuana, prescription opioids), or avoiding withdrawal symptoms (e.g., heroin). Negative reinforcement, therefore, can be used to explain the maintenance of Preston’s substance use problems over time.

4. How does Preston’s psychosocial history reflect the enhanced reinforcement model for substance use disorders?
At the heart of the enhanced reinforcement model (shown below) is a genetic diathesis toward substance use problems. We can infer that Preston has such a genetic risk given his father’s extensive history of substance use. In some individuals, like Preston, genetic risk makes individuals highly sensitive to the positive effects of the substance; in fact, they anticipate these positive effects. Preston experiences marijuana as pleasurable and looks forward to using marijuana recreationally with his friends. In turn, his deviant peer group models and reinforces continued substance use. Over time, these behaviors escalate and resulte in Preston’s arrest and referral for treatment.

5. How might medication be used as part of Preston’s inpatient treatment for opioid (heroin) use disorder?
Substitution therapy involves administering a medication that reduces cravings for the substance. Preston might be prescribed methadone, a synthetic opioid, which binds to opioid receptors and produces mild analgesia and anxiety reduction. This medication might be gradually tapered off to reduce the severity of withdrawal symptoms.
Detoxification therapy involves administering a medication to help manage negative, physiological symptoms of withdrawal. For example, clonidine is a medication that reduces heart rate and blood pressure. It can reduce these arousal symptoms and make opioid withdrawal symptoms less severe.
Note that Preston also seems to be involved in the diversion of ADHD medication, that is, he seems to be selling his own stimulant medication to high school students to support his opioid use.
6. What evidence-based psychosocial treatment might be helpful to adolescents like Preston, who have serious substance use problems caused by multiple environmental factors?
Multidimensional family therapy (MDFT) is an evidence-based psychosocial treatment that is presented in the text. Targets of MDFT include (1) the adolescent’s immediate substance use, (2) the caregiving practices of the adolescent’s parents, (3) the quality of the parent–adolescent relationship, and (4) peers and school involvement.
Motivational Interviewing: Theory and Practice
Alcohol and Cannabis Use Disorder
Irene was a 15-year-old girl referred to mandatory substance abuse counseling by the juvenile court after being arrested for marijuana possession. Approximately one month ago, Irene and her friends were caught drinking after a football game in a field a few miles away from her school. Although Irene was not intoxicated, she was questioned by police who discovered a small amount of cannabis in her purse. Whereas her friends were sent home to their parents, Irene was detained by police and ordered to participate in 8 weeks of therapy by a juvenile court judge.
“This is total crap,” as Irene began her first therapy session with Rebecca, her substance use counselor. “Everyone else got to go home, but they arrested me, probably because I was the only Latina there. Everyone drinks and uses a little, you know, just to have some fun. God knows we don’t go to the games to watch football!”
Rebecca began, cautiously, “Sometimes, adults overreact or do things that are just not fair.”
Irene replied, “Yeah, like with me. There were seven of us and a few boys. All of us drove out there to party and relax. I was the only one who got arrested.”
Rebecca commented, “They singled you out.”
“Right. Just me.” Irene continued, “And now I’m stuck going to this place. I can think of a dozen kids who drink a lot more than me. Kids who are addicted. Kids who I know sell drugs. But they don’t get into trouble. Well, if I have to be here, fine. But the judge can’t make me talk.” Irene crossed her arms in defiance.
Rebecca took a deep breath, looked away from Irene, out the window, and said, “Your dad tells me you’re a good swimmer.”
“What?” Irene asked.
Rebecca said, “When I talked to your dad on the telephone, before you came here, he mentioned that you swim on the varsity team. He said that you’re pretty good and that he’s really proud of you.”
Puzzled, Irene looked up and relied, “What’s that got to do with anything?”
“I was wondering,” explained Rebecca, “are you still eligible to swim if you get in trouble with the police?”
Irene replied with a sarcastic tone, “The school swim season doesn’t start for two months.”
“Oh, right,” Rebecca said. “But if you get in trouble again, you probably couldn’t swim.”
Irene paused, digesting Rebecca’s words, then responded, “No, probably not.”
Rebecca added, “I wonder how your dad would feel if you couldn’t swim.”
“He’d probably be more hurt by it than I would. He comes to every meet. He was a college swimmer and really wants me to swim in college too.”
Rebecca added, “And you probably like swimming yourself, at least a little? And being on the team?”
Irene answered, “Of course.”
Rebecca said, “So even if the police, or the school administrators, or the judge is unfair, or overreacting, or singling you out for whatever reason, it’s still in your best interests to NOT get into trouble with alcohol or drugs—at least until swim season is over.”
Irene, “I guess not.”
1. What are the six steps in the stages of change model? Which stage best describes Irene?
The stages are presented in the text. They are (1) precontemplation, (2) contemplation, (3) action, (4) maintenance, (5) relapse, and (6) termination. Irene is probably in the precontemplation stage, because she does not believe that she has a substance use problem and resents being ordered to attend therapy.
2. What are the five principles of motivational interviewing? Which principles did Rebecca illustrate?
Students can remember the five principles using the DRESS acronym: Develop discrepancies, Roll with resistance, Express empathy, Support change no matter how small, and Success should be acknowledged.
Rebecca tried to show empathy by initially reflecting Irene’s feelings of resentment and anger for being ordered to therapy.
Rebecca rolled with resistance and avoided arguing with Irene by agreeing with her that sometimes adults overreact to situations. Rebecca also changed topics when Irene refused to participate in therapy.
Rebecca tried to develop discrepancies between Irene’s use of alcohol and her desire to swim and please her father.
3. What is harm reduction? In what way did Rebecca use a harm reduction approach with Irene?
Harm reduction is an approach to treatment in which the therapist encourages the client to reduce substance use in problematic situations (i.e., reduce the likelihood of harm) rather than insist on complete abstinence. Harm reduction approaches are an alternative to abstinence-based treatment programs such as 12-step interventions (e.g., Alcoholics Anonymous). Rebecca suggested that it is important that Irene “not get into trouble” with alcohol or marijuana in the future to maintain her sports eligibility. Rebecca did not insist that Rebecca abstain from alcohol and marijuana altogether.
4. Imagine that you were Irene’s therapist. You want to help her perform a cost–benefit analysis for (1) continuing her current alcohol and marijuana use versus (2) reducing her substance use. What might be the costs and benefits of each behavior?
The text illustrates a cost–benefit analysis for substance use problems in adolescents. An example for Irene is shown below.
5. Irene asserted that most kids her age use alcohol and marijuana fairly regularly. Based on data from the Monitoring the Future studies, is Irene’s assertion true?
The most recent Monitoring the Future data (presented in the text) show that <20% of 10th graders have used marijuana in the past month and < 45% of 10th graders have used alcohol in the past month. Irene seems to overestimate the frequency with which youths her age use these substances. It is likely that she overestimates adolescent alcohol and marijuana use because her immediate peer group uses these substances more regularly than adolescents in the general population.
6. What is the prevalence of substance use problems among Latino adolescents compared to non-Latino White and African American adolescents?
The most recent Monitoring the Future data (presented in the text) show that Latino adolescents are slightly less likely than non-Latino White adolescents to use alcohol and marijuana, but more likely than African American adolescents to use these substances.
Chapter 11: Anxiety Disorders and Obsessive–Compulsive Disorder
Listless liesel.
Separation Anxiety Disorder
Liesel Brandt was a 7-year-old girl referred by her pediatrician because of problems with school refusal, anxiety, and social withdrawal. Liesel’s mother worked as an interior designer; her father was employed as a mechanical engineer. Liesel’s parents separated approximately one year ago and are in the process of divorcing. Her parents live in the same small town, so Liesel splits her time with her mother and father. Liesel has one brother who is 3½ years old.
Liesel’s developmental history is unremarkable. She was born healthy and full term with no complications associated with delivery. She reached developmental milestones in an age-expected fashion. Her mother reported that Liesel was a “fussy” baby who cried often and had difficulty eating and sleeping. She often needed her mother to cuddle with her before she was able to go to sleep. Liesel was also described as a shy and “clingy” toddler who was reluctant to talk with others or wander too far away from her mother.
Last year, Liesel began attending preschool approximately three mornings each week while her mother worked part time. Initially, Liesel was reticent to separate from her mother. However, by the third week of school, she attended preschool without complaining and began to make friends with other girls in her class.
Liesel’s school refusal returned at the beginning of this school year, however. The night before the first day of kindergarten, Liesel complained of nausea and stomach pain. When her illness did not subside by the next morning, her mother allowed her to stay home. The following day, when her mother insisted that she attend school, Liesel tantrummed and locked herself in the bathroom. Her mother drove her to school despite protests and crying. Liesel’s teacher said that she continued to cry most of the morning and remained tearful and reclusive the rest of the day. When her mother picked her up in the afternoon, Liesel looked hurt and exhausted. She clung to her mother and vowed never to return to school again.
Nevertheless, Liesel’s mother continued to insist that Liesel attend school. Liesel often reported stomach problems, headaches, and other vague illnesses. At school, she behaved in a withdrawn, listless fashion, rarely participating in class activities. Liesel also reported transient fears that something bad might happen to her mother or father while she was at school, that terrorists would attack her school, or that her mother might forget to pick her up and that she would have to spend the night alone in the school building.
Liesel’s mother reported a significant increase in family stress within the past 6 months, about the time Liesel’s school refusal and mood problems emerged. First, she and her husband are in the process of divorcing, which causes her considerable stress and financial hardship. She is struggling to care for her children while, at the same time, building her interior design business to make ends meet. Liesel’s mother admitted to longstanding problems with anxiety and insomnia which have increased markedly since separation from her husband. A second stressor in Liesel’s life has been the death of her cat, Tobbie, who was hit by a car outside the family home. Liesel was unusually attached to Tobbie; she would often hug and pet Tobbie when she was upset. Her mother is considering adopting another cat to replace Tobbie, but wondered whether she would have sufficient time and money to care for it.
1. What DSM-5 anxiety (or related) disorder best describes Liesel’s behavior?
Separation anxiety disorder
2. Review the DSM-5 criteria for this disorder. Describe how Liesel meets diagnostic criteria for this condition.
A. Liesel has the following signs/symptoms:
1. Excessive distress upon separation from her mother
2. Worry about harm befalling parents
3. Worry about being abandoned at school by her mother
4. School refusal
5. Nightmares involving the theme of separation
6. Physical complaints when separation is anticipated
B. Duration is > 4 weeks
C. Experiences distress and impaired functioning
D. Not better explained by other disorders
3. Liesel is 7 years old. At what age is her problem developmentally normative? Can adolescents experience problems similar to Liesel’s?
Separation anxiety is developmentally expected in infancy, particularly between the ages of 9 and 18 months. After 24 to 36 months of age, separation anxiety decreases. Separation anxiety disorder can be diagnosed in preschoolers who continue to show separation anxiety beyond this period of typical development if their anxiety causes distress and/or impairment. Typical age of onset is between 7 and 9 years.
Adolescents (and adults) can also be diagnosed with separation anxiety disorder, although they might manifest symptoms differently than younger children. For example, adolescents may have more realistic fears that harm might befall their caregivers (e.g., mom might get into a car accident on the way to work) and they may need more subtle forms of reassurance (e.g., texts, phone calls) instead of following their caregivers around the house.
4. The diathesis stress model is often used to explain the emergence of anxiety disorders. How might the diathesis stress model be used to explain the development of Liesel’s problems with school refusal?
The diathesis stress model posits that individuals develop disorders if they experience (1) a genetic risk for the disorder and (2) an environmental stressor to trigger its onset. It is difficult to determine if Liesel has a genetic risk for anxiety without gathering more information about her psychosocial history. However, her mother reported problems with both anxiety and insomnia. Liesel has also experienced several significant stressors at about the same time as the emergence of her school refusal: separation of her parents, death of her cat, stress in her mother’s work that could impact her ability to care for Liesel. These stressors are largely interpersonal in nature and might threaten her sense of security. Although we cannot be certain that these stressors caused her disorder, providing consistent, sensitive, and responsive care to Liesel might be an important component of treatment.
5. What evidence-based treatment might you recommend for Liesel?
The evidence-based treatment of all anxiety disorders typically involves exposure therapy. Liesel must attend school and (ideally) experience her participation at school as pleasant. Behavioral interventions (presented in the text) include contingency management, systematic desensitization, and peer modeling.
In addition, cognitive–behavior interventions can be useful to challenge Liesel’s fears that she might be abandoned at school by her mother or that harm might befall her mother when she is separated from her. The text illustrates the use of the Coping Cat program and the development of a FEAR plan—two cognitive interventions that might be helpful for Liesel. Liesel’s parents should also be encouraged to provide more consistent, sensitive, and responsive care to Liesel and to avoid conflicts during the divorce process.
Taciturn Tessa
Selective Mutism
Mrs. Miller sat awkwardly in the small desk of her daughter’s kindergarten classroom. Shifting her weight, she waited for her daughter’s teacher, Ms. Shafer, to speak.
“Thank you for meeting with me today,” said Ms. Shafer. “I’m glad that we can talk about your daughter, Tessa.”
“Of course,” Mrs. Miller responded. “Is there a problem?”
The teacher responded, “Tessa’s a delight to have in class. She’s always attentive and completes her work in a neat organized way. Her writing and math are coming along nicely, too. There’s just one concern—she doesn’t talk much.”
This report was not what Mrs. Miller was expecting. Confused, she asked, “What do you mean? She talks all the time at home.”
Ms. Shafer answered, “We’ve been in school for 6 weeks. Tessa’s never said a word. She’s definitely gotten better since the first day of school. In August, she wouldn’t even make eye contact with me. She’d just sit at her desk or stand on the fringes of group activities and refuse to participate. Now, she’ll look me in the eye when I talk to her and answer questions by nodding or shaking her head. I still can’t assess her reading skills because she refuses to read aloud in class or in her reading circle.” Ms. Shafer paused and then asked, “Is anything wrong at home? Is she under a lot of stress or did something bad happen?”
Mrs. Miller looked stunned. Then she responded, “No. Nothing’s really changed at our house.” Thinking to herself for a while, she added, “Tessa’s always been a very shy girl. My husband called her ‘shadow’ because she’s constantly by our side. She even dislikes being in the living or family room alone and insists that one of us is with her. She’s also had a hard time making friends, but has a few younger kids in the neighborhood that she likes.”
Ms. Shafer questioned, “What was Tessa like last year in school?”
“Actually,” Mrs. Miller began, “Tessa didn’t attend formal school because our family was traveling due to my husband’s work. He’s a petroleum engineer and our family spent last year in South America. I homeschooled Tessa because other schooling options were limited. Maybe that was a mistake.”
Ms. Shafer replied, “Like I said, Tessa is making progress—although it’s not as fast as I would like. I think we can help her overcome this problem, but we need to work together.”
1. What DSM-5 anxiety (or related) disorder best describes Tessa’s behavior?
Selective mutism
2. Review the DSM-5 criteria for this disorder. Describe how Tessa meets diagnostic criteria for this condition.
A. Tessa shows persistent failure to speak at school.
B. Her mutism interferes with her academic and social functioning.
C. Duration is > 1 month.
D. It is not attributable to underlying language differences.
E. It is not better explained by a communication disorder or other psychiatric condition.
3. Tessa is a kindergarten student. At what age do problems like hers typically emerge? If untreated, is she likely to get better by herself?
Selective mutism typically develops during the preschool or early school-age years, when children begin formal schooling. Without treatment, the average duration of selective mutism is several years. Consequently, some type of intervention is warranted.
4. How might temperament play a role in Tessa’s difficulty at school?
Children with selective mutism often have temperaments characterized by high behavioral inhibition. These children often become distressed when presented with novel stimuli; consequently, they learn to avoid novel people, places, and situations to modulate their level of arousal. Children with selective mutism are at particular risk for developing social anxiety disorder later in life. In fact, some researchers see selective mutism as an early variant of social anxiety.
5. How might we use learning theory to explain the cause and maintenance of Tessa’s problem?
According to Mowrer’s two-factor theory, anxiety disorders often emerge through classical conditioning and are maintained through operant conditioning (negative reinforcement). Tessa may have associated speaking at school with anxiety or panic. Then, she might learn that by avoiding speaking at school, she could reduce her level of anxiety or panic, making her more likely to remain mute in the future.
6. What evidence-based treatment might you recommend for Tessa?
The evidence-based treatment of all anxiety disorders typically involves exposure therapy. Tessa must speak at school and (ideally) experience her participation as pleasant. Behavioral interventions (presented in the text) include contingency management, systematic desensitization, and peer modeling. Graded exposure might be especially useful; perhaps Tessa could initially mouth responses, then whisper responses, then say responses while being reinforced amply by the teacher.
Dental Plan
Specific Phobia
Nora was a 10-year-old girl who was referred to our outpatient anxiety clinic because of persistent fears about going to the dentist. Nora’s problems began approximately six months ago following a routine dental procedure that ended up in disaster.
Nora was a typically developing fourth-grade student who was generally compliant toward her mother, respected her teachers, and was well-liked by her peers. She also had no history of anxiety or mood disorders in her family and was considered physically healthy. Consequently, when Nora’s mother took her to the dentist to fill a small cavity, she did not expect the visit to go so poorly.
As the dentist began drilling to remove portions of the decayed tooth, Nora felt the dull pressure of the machine against her jaw and inhaled the burnt aroma of bone against the drill tip. As the scent assailed her nostrils, she experienced saliva filling the lower portion of her mouth, sliding rapidly toward her throat. She thought, “I need to swallow. I‘m going to drown in my own spit. I need to get it out, but I can’t.” Nora was too embarrassed to ask the dentist to pause and allow her to swallow. She felt her eyes tear, her face and neck break out in a cold sweat, and her heart thump. Then, she began to choke. The drill slipped and injured her tooth, saliva flew in all directions, and Nora vomited a little on her clothes. An overwhelming sense of embarrassment flooded Nora. She felt a terrible impulse to run from the exam room and, without thinking, she bolted. Her mother watched her run down the hallway, past her seat in the waiting room, and out the door. After 20 minutes of heavy sobbing, Nora explained what happened.
Nora has since refused to visit the dentist. Her mother has tried to take her to different offices, but Nora either cries, tantrums, or stubbornly refuses to enter. Her mother is concerned because Nora’s cavity was never filled and she is still in need of dental work. Her mother is hoping that a psychologist might develop a plan to help Nora muster the courage to visit the dentist.
1. What DSM-5 anxiety (or related) disorder best describes Nora’s behavior?
Specific phobia: Other type (i.e., fear of choking, vomiting)
(You might also argue that it is a “situational type” phobia with avoidance of dentists’ offices as the situation.)
2. Review the DSM-5 criteria for this disorder. Describe how Nora meets diagnostic criteria for this condition.
A. Nora has a marked fear of visiting the dentist. She seems to be especially afraid about choking, vomiting, or embarrassing herself during a dental procedure.
B. Thoughts of visiting the dentist elicit immediate fear.
C. She avoids going back to the dentist.
D. Her fear is out of proportion to the actual risk involved in going to the dentist.
E. Her fear has persisted for at least 6 months. (Technically, we don’t know its duration. DSM-5 says the fear “typically” lasts for at least 6 months. Because her avoidance of the dentist prohibits her to fill a cavity, we probably wouldn’t want to wait several months before addressing the problem.)
F. The fear causes distress and the avoidance risks further tooth decay (impairment).
G. The disorder is not caused by another psychiatric disorder.
3. How do older children and adolescents’ fears differ from the fears of preschool and young school-age children?
Children’s fears reflect their level of cognitive development and salient developmental tasks. Younger children often fear concrete objects (e.g., animals) and monsters. Older children, like Nora, tend to fear natural disasters or real places and situations (e.g., the dentist). Adolescents often fear social interactions and situations where they might be negatively evaluated by others (e.g., recitals, sporting events, exams).
4. How might Nora’s cognitions mediate the relationship between her situation (i.e., the dental procedure) and her emotional and behavioral consequence (e.g., fear/panic and fleeing the office)?
Children with specific phobias often make negative self-statements that emphasize the danger of situations and minimize their ability to cope with that danger. Nora thought that she might drown in her own spit and believed that she needed to get up and swallow. However, she also believed that she couldn’t ask the dentist to pause so that she could swallow or get up from the dentist’s chair. It is likely that Nora also had negative automatic thoughts after vomiting, such as “The dentist thinks I’m a terrible patient. Everyone is staring at me or making fun of me.” These thoughts may have prompted her desire to flee the office.
5. How might we use learning theory to explain the cause and maintenance of Nora’s problem?
According to Mowrer’s two-factor theory, anxiety disorders often emerge through classical conditioning and are maintained through operant conditioning (negative reinforcement). Nora associated the dental procedure with choking and vomiting (i.e., classical conditioning). This association generalized to dentists’ offices in general. She learned that by avoiding dentists’ offices, she could avoid fear and anxiety (i.e., negative reinforcement).
6. What evidence-based treatment might you recommend for Nora?
The evidence-based treatment of all anxiety disorders typically involves exposure therapy. Nora must visit the dentist’s office and have a cavity filled without experiencing a negative consequence (e.g., choking, vomiting). Behavioral interventions (presented in the text) include contingency management, systematic desensitization, and modeling. In vivo, graded exposure might be especially useful. For example, on separate occasions, Nora might (1) walk past the dentist’s office, (2) enter the waiting room and sit for 10 minutes, (3) sit in the dentist’s chair for 10 minutes, (4) have a hygienist brush her teeth in the chair, and (5) gradually engage in the necessary procedures.
Relaxation techniques (e.g., deep breathing, guided imagery, muscle relaxation) or distraction (e.g., listening to music or watching a video) might also be used to help her regulate her anxiety.
Some therapists might allow Nora to have a signal that she might use (e.g., raise her right hand) if she wants the dentist to pause. A signal might allow Nora to experience greater self-efficacy during the procedure.
Finally, cognitive interventions might be useful to challenge negative automatic thoughts that might exacerbate Nora’s fears of dental procedures. For example, Nora might believe that the dentist or hygienist makes fun of her for choking or vomiting. A therapist might ask Nora, “If you worked in the dental office and you saw a girl choke, what would you think? Would you make fun of her or think she was terrible?” It is likely that Nora would be sympathetic and understanding. The therapist might then ask Nora, “Why would you expect the staff at the dentist’s office to be any less sympathetic or understanding than you would be if placed in the same situation?”
Gun Shy Guy
Social Anxiety Disorder
Logan Wright was a handsome, intelligent, 10th-grade student at Watkins High School. Although somewhat quiet and reserved, he had a small circle of close friends and was involved in the school’s marching band. Logan was also an excellent student, earning mostly As in advanced courses in math and science. Overall, Logan was successfully navigating the world of adolescence, except for one small problem: He could not urinate in a public restroom.
Logan’s problem was discovered by his teacher several days ago when he left his classroom during a test without permission. Apparently, Logan had refrained from using the bathroom all day, and drank too much fluid to delay urination any longer. After 20 minutes of uncomfortable fidgeting, Logan darted from the classroom down the hall to the bathroom. Although no one stood at the urinals, one student occupied a nearby stall. Logan quickly closed the bathroom door and dashed to a different bathroom at the other end of the school, attracting the attention of several teachers and the dean of students. Luckily, no one was inside the second bathroom and Logan could relieve his bladder. However, he had some explaining to do.
“How long have you had this problem?” his guidance counselor asked.
Logan replied, “Forever. At first, it wasn’t much of a problem. I would always just pee in a stall. Then, about three or four years ago, it became worse and I couldn’t pee if anyone was in the bathroom.”
The counselor asked, “What is it about peeing in public that bothers you?”
Logan laughed, nervously, and then replied, “I don’t know. I guess I’m worried that someone will hear me. I know it’s really dumb, but I think that they might be making fun of me.”
“What might they think?” the counselor asked.
“I don’t know. Maybe that I pee really loud or that I pee different from others or maybe that they’ll be looking at me funny. I know it’s silly, but when I have these thoughts I tense up and can’t go.”
The counselor asked, “Have you ever told anyone about this problem, like your dad?”
Logan laughed, cynically, and then said, “No. He’s not the type of person to go to with a problem like this.”
“What do you mean?” asked the counselor.
“I mean, he’s not the most understanding person in the world,” Logan explained. “Let’s just say we don’t have a good relationship.”
“And I don’t suppose you can talk to your mom about a problem like this,” said the counselor.
Logan replied, “Not really. Besides, she’s a bundle of nerves herself. She’s been taking anxiety medication for years.”
The counselor responded, “Well, I’m glad that we can talk about it. Let’s see if we can find a way to help you get over this problem.”
1. What DSM-5 anxiety (or related) disorder best describes Logan’s behavior?
Social anxiety disorder (social phobia)
2. Review the DSM-5 criteria for this disorder. Describe how Logan meets diagnostic criteria for this condition.
A. Logan experiences marked anxiety about a social situation in which he might be exposed to scrutiny (e.g., urinating in a public restroom).
B. Logan fears that his behavior will be negatively evaluated by others.
C. The social situation always causes anxiety.
D. Logan avoids urinating in a public restroom.
E. Logan’s fear is out of proportion to the actual threat posed by the situation.
F. The problem has persisted for > 6 months.
G. The problem causes significant impairment (and distress).
H. Logan’s problem is (probably) not attributable to a substance or medical condition (although we would need a physical exam to confirm that this criterion is met).
I. The problem is not explained by another mental disorder.
J. No other medical condition better explains Logan’s problem.
3. Logan is a 10th-grade student, perhaps 15 years of age. At what age do youths with his disorder typically manifest symptoms?
Social anxiety disorder typically emerges in early adolescence. It is rare before age 10 years. Preoccupation and minor concerns about being negatively evaluated by others are developmentally normative in early adolescence (e.g., the imaginary audience). However, excessive concerns about being subjected to scrutiny or negative evaluation, which cause significant distress or impairment in functioning, are not normative and may be a sign of social anxiety disorder.
4. Logan seems to have a negative attitude toward his father and his mother. According to the research literature, how can parents contribute to the development of anxiety disorders in children?
Empirical studies suggest that the parents of children with social anxiety disorder are often described as follows:
- controlling
- overprotective
- hostile and critical
5. How might a behavior therapist use graded exposure to help Logan overcome his problem?
Graded exposure involves repeated exposure to the feared stimulus without escape or avoidance until anxiety dissipates. A behavior therapist might work with Logan on establishing a fear hierarchy, that is, a list of situations that elicit anxiety from least to greatest. Then, Logan would engage in activities on the hierarchy. For example, early activities might involve entering (but not using) an empty bathroom or a bathroom with one other occupant. Midrange activities might be urinating in an occupied bathroom while using a stall after flushing the toilet (i.e., to mask any embarrassing sounds) or urinating in a bathroom urinal while the therapist is also in the bathroom standing at the sink. High-range activities might involve urinating at a urinal while others are in the bathroom and urinating at a urinal while another person is using another adjacent urinal.
6. What cognitive distortions might contribute to Logan’s anxiety problem? How might a cognitive therapist address these distortions?
Cognitive therapists believe that a person’s thoughts about events, not the events themselves, largely determine the person’s actions and feelings. Logan likely believes that others will make fun of him for urinating in a public bathroom. Although he says that he knows this belief is “silly,” it may exacerbate his anxiety. A cognitive therapist would likely ask Logan to engage in collaborative empiricism, that is, to provide evidence supporting or refuting his belief. For example, has anyone ever commented on his urinating in the past?
Perhaps Logan is engaging in a cognitive distortion known as “mind-reading”—the tendency to assume that others are evaluating him negatively without any supporting evidence. Alternatively, Logan might adopt the cognitive distortion of “catastrophizing”—the tendency to anticipate the worst possible outcome. To challenge this distortion, the therapist might ask Logan to (1) describe the worst thing that could happen if he used a public restroom and then (2) realistically estimate the chance that this terrible outcome would occur. Then, the therapist might ask Logan to assume that this terrible outcome did occur and reevaluate how terrible it might actually be. For example, the likelihood that someone might make fun of the way he urinates is very low. Furthermore, even if someone did make fun of him, he might feel embarrassed, but the event would certainly not be catastrophic.
Cardio Consult
Panic Disorder
Sivan sat in the cardiologist’s office with her parents. Her mother sat by her side with her arm around the back of Sivan’s chair. Her father sat nervously across from them, periodically rubbing his forehead and brushing back his hair. Sivan was their only child. Sixteen years ago, she was born with a congenital heart defect that threatened her life and necessitated a series of operations that kept her in and out of hospitals for most of her infancy. Her parents thought that all of these medical problems were in Sivan’s past. Sivan had not experienced any irregularities in years and had even been cleared to play tennis and ride horses (an activity that she adored). Then, several months ago, all of that changed.
Sivan was completing an important chemistry exam when she experienced severe heart palpitations. The palpitations came on suddenly, as if her heart skipped a beat. They were accompanied with a curious “sinking feeling” like she was going to faint. She later described it as similar to the time when she was pulled over by the police for speeding. She felt dizzy and lightheaded, experienced shortness of breath, and her skin became clammy. Sivan left the classroom without permission, ran to an empty adjacent room, and curled into a ball on the floor waiting to feel better. After about 20 minutes, she felt able to walk to the bathroom and wash her face. She returned to her classroom, explained to her teacher that she felt sick, and put the event behind her.
Unfortunately, Sivan experienced similar episodes over the subsequent 3 months. Three episodes occurred at school, usually before or during exams. One episode, however, happened in the school parking as she was walking to her car to drive home. This last episode greatly upset Sivan because it came “out of the blue,” it did not seem prompted by stress, and it could have been dangerous if it had occurred while she was driving. Worried about their recurrence, Sivan told her parents about these events and they immediately contacted her pediatrician who ordered testing.
“I have the results of Sivan’s EEG,” said the cardiologist. “The good news is that it looks completely normal. I don’t think she’s experiencing any return of the problems she’s had in the past.”
Her father let out a sigh of relief, followed by the inevitable question, “Well, that’s good news. But then why is Sivan having these episodes?”
“And how can we stop them?” added her mother.
Discussion Questions:
1. What DSM-5 anxiety (or related) disorder best describes Sivan’s behavior?
Panic disorder
2. Review the DSM-5 criteria for this disorder. Describe how Sivan meets diagnostic criteria for this condition.
A. Sivan seems to be experiencing recurrent panic attacks. These attacks are characterized by intense fear and discomfort as well as the following signs and symptoms: heart palpitations, sweating, shortness of breath, and dizziness/faintness.
B. Sivan experiences persistent worry about additional attacks for at least one month.
C.Her attacks are not caused by a substance or medical condition.
D. Her attacks are probably not due to another mental disorder.
3. How might expectancy theory be used to explain the development of Sivan’s symptoms?
The expectancy theory of panic posits that people with panic disorder often have high anxiety sensitivity, that is, they are unusually attentive to the physiological symptoms of anxious arousal and find these symptoms distressing. People with high anxiety sensitivity, like Sivan, might pay extra attention to any fluctuations in their heart rate, breathing, or other signs of arousal. This extra attention might cause them to misperceive these normal fluctuations as something problematic and, consequently, exacerbate these symptoms.
4. According to a cognitive therapist, how might Sivan’s thoughts contribute to her recurrent problem?
Youths with panic disorder often engage in catastrophic thinking, a cognitive distortion characterized by expecting the worst possible outcomes. When these youths experience minor (and normative) fluctuations in autonomic arousal they might interpret this arousal as something catastrophic, such as an indicator that they are having a heart attack or are “going crazy.” It is likely that Sivan misinterpreted her panic attacks as indicators that her chronic heart problems have returned. This catastrophic attribution is understandable given her history and likely increased the amount of attention (and worry) she paid to the possibility of future attacks.
5. What evidence-based interventions might a therapist use to help Sivan?
Three evidence-based behavioral interventions for youths with panic disorder include (1) relaxation training, (2) interoceptive exposure, and (3) cognitive restructuring. Relaxation training is helpful in reducing initial arousal and anxiety sensitivity. Interoceptive exposure involves intentionally producing panic symptoms and establishing the fact that these symptoms can be controlled. Cognitive restructuring often targets catastrophic thoughts that exacerbate panic.
Stomach Problems
Agoraphobia
Luke Atkins was a 13-year-old boy referred to our outpatient clinic because of problems with social avoidance. Luke’s mother, Margaret Atkins, works as a defense attorney. His father, Bill Atkins, works as an accountant. Luke has two younger sisters and no family history of mental health problems. Prior to the onset of his current anxiety problem, Luke had been a friendly, although somewhat introverted boy, who did well in school, liked to play soccer, and had a close group of friends at school.
Approximately six months ago, however, Luke’s mother received a telephone call from the school nurse who reported that Luke was involved in an “incident” at school. Apparently, after lunch, Luke experienced upset stomach, cramping, and heartburn. He attempted to cope with these symptoms by sitting quietly at his desk. When the discomfort increased, Luke decided to ask his teacher if he could be excused because he was not feeling well. As Luke rose from his desk, Luke felt a surge of stomach acid and partially undigested food enter the back of his mouth. He gagged and, embarrassingly, regurgitated some of the contents onto his shirt and the floor. Luke ran from the room to the nurse’s office.
The following day, Luke refused to go to school, claiming that he was too embarrassed to show his face to his classmates. Only after much coaxing were his parents able to persuade him to go. Unfortunately, later that week, Luke experienced another attack of upset stomach that almost caused him to vomit in the same classroom. This time, however, Luke left the classroom in time and received antacids from the school nurse, which alleviated his symptoms.
Luke’s pediatrician prescribed medication for acid reflux and recommended that he carry antacids with him during the day at school. Unfortunately, these precautions did not help Luke. He refused to attend his afternoon math class, so school personnel rearranged his schedule. Unfortunately, Luke experienced subsequent acid reflux problems over the next few weeks: at first period physical education class, immediately after lunch in his new language arts class, and one the bus ride home. This last incident was especially problematic. Luke, who was formerly so self-reliant, insisted that his mother pick him up from school in case he experienced another stomach problem on the bus and could not get to the bathroom or otherwise obtain help.
Currently, Luke complains about going to school each morning. He refuses to eat lunch at school because he is afraid of more attacks. School personnel have rearranged his schedule a third time so that his “important” classes (e.g., math, language arts) are in the morning when he is likely to feel well. Luke attends his afternoon classes very reluctantly and insists that he sit near the door in case he needs to leave in an emergency. He refuses to attend physical education class altogether. His parents have rearranged their work schedules so they can drive him home each afternoon.
Luke denies other symptoms of anxiety or mood problems. He says that he has never experienced a panic attack and is not afraid of social situations. His chief worry is that his stomach problems will become worse, thus limiting his functioning even more.
1. What DSM-5 anxiety (or related) disorder best describes Luke’s behavior?
2. Review the DSM-5 criteria for this disorder. Describe how Luke meets diagnostic criteria for this condition.
A. Luke experiences anxiety (1) being in enclosed places like his classroom and (2) riding the bus home from school.
B. Luke fears these situations because he thinks escape or help might be difficult if he developed panic-like or embarrassing symptoms (i.e., acid reflux).
C. These situations almost always elicit anxiety.
D. Luke avoids riding the bus home from school. He is able to attend some classes, but only after his schedule has been rearranged several times. He refuses to attend physical education class which may be required for graduation. He attends classes with considerable distress or worry about future stomach problems.
E. Luke’s fear is out of proportion to the actual danger of the situation.
F. Duration > 6 months.
G. Luke’s symptoms cause distress and impairment.
H. Although Luke’s anxiety was initially caused by gastroesophageal reflux disease (GERD), his agoraphobic avoidance of classrooms and the bus is excessive and impairing.
I. His symptoms are not better explained by another mental disorder.
3. How common are problems like the kind experienced by Luke (e.g., avoiding school, the bus)? At what age do problems like Luke’s tend to develop?
The overall prevalence of agoraphobia is 1.7%; prevalence among adolescents is < 0.5%. The typical age of onset for agoraphobia is between 18 and 29 years. This condition is rare among younger adolescents like Luke.
4. Approximately what percentage of youths has problems like Luke without a history of panic attacks?
As many as 50% of youths with agoraphobia do not have a history of panic attacks. These youths tend to develop agoraphobic avoidance in one of three ways: (1) because they experience panic-like symptoms in specific locations where help is unavailable or embarrassing, (2) they experience an external negative event in specific locations and then avoid those locations, or (3) they show high dependency and need reassurance from others when entering specific locations or situations. The first option seems to explain Luke’s agoraphobic avoidance.
5. According to Mowrer’s two-factor theory of anxiety, how did Luke’s avoidance of class and the bus emerge? Why has it persisted over time?
According to the two-factor theory of anxiety, agoraphobic avoidance can develop through classical conditioning and can be maintained through operant conditioning, especially negative reinforcement. Luke associates specific classrooms or situations (i.e., the bus) with GERD symptoms that cause discomfort and embarrassment. He now avoids these situations. His agoraphobic avoidance is maintained through negative reinforcement; he learns that by avoiding these places and situations, he can avoid or reduce anxiety.
6. Imagine that you are a cognitive therapist working in the clinic. How might you help Luke?
Cognitive therapists believe that the way Luke thinks about situations, rather than the situations themselves, influence his actions and emotions. A cognitive therapist would likely help Luke identify negative automatic thoughts or cognitive distortions that might exacerbate his fear of the classroom or bus.
For example, Luke may engage in mindreading, a cognitive distortion in which people think they know what other people are thinking, without having sufficient evidence. Luke might be certain that other students are making fun of him for being sick in class or on the bus. This cognitive distortion likely exacerbates his feelings of embarrassment. A cognitive therapist might help Luke challenge that distortion by looking for evidence to support it or refute it. Did Luke actually see students laugh at him? If Luke saw another student become sick during class would he make fun of that student? Wouldn’t he, instead, feel sorry for that student and try to help?
The Talented Musician
Generalized Anxiety Disorder
Chloe McGovern was referred to the pediatric headache clinic at a children’s hospital in a metropolitan area. Chloe was a 13-year-old, eighth-grade student with tension headaches of moderate intensity. The headaches began approximately 18 months ago and have gradually worsened, especially over the past 6 months. These headaches occurred approximately three times per week, with duration of approximately one to three hours each. Over-the-counter medications (e.g., acetaminophen, ibuprofen) are generally effective in shortening their duration, but Chloe’s parents are worried given the headaches’ increasing frequency and severity.
A neurological examination revealed no apparent structural or functional abnormalities of Chloe’s nervous system. She appeared to be perfect except for her headaches. Consequently, Chloe and her family were referred to a pediatric psychologist at the clinic to explore psychosocial causes for her problem.
The psychologist, Dr. Witten, learned that the onset of Chloe’s headaches coincided with her transition to middle school. Chloe’s mother explained, “Chloe’s always been a perfectionist. She was in accelerated programs throughout elementary school: math, language arts, music. When she started middle school, she tested into the gifted program, meaning that she could skip seventh-grade classes and begin immediately to eighth-grade work for most subjects.” Her father added, “And she’s also a very good musician. They asked her to play for both the seventh- and eighth-grade orchestras. She plays the oboe, which is somewhat rare. Both orchestras needed her.”
Dr. Witten looked up from her notes, “And is all this work hard to manage, Chloe? I mean, you essentially skipped seventh grade.”
Chloe answered, “Not really.” Then crossed her arms and remained silent.
Chloe’s mother elaborated, “Chloe’s a really hard worker. I drive her to school each morning a little early because she’s on the student council. She tries to do as much homework as possible during study hall. Then, after school, she has orchestra or archery practice. She also takes private oboe lessons twice a week.”
“That seems like a busy schedule,” commented Dr. Witten. Chloe remained silent.
Later, Dr. Witten interviewed Chloe privately. She said, “ Chloe, I know that you’re a good musician. I wonder if you’re a good artist, too. I want you to draw me a picture of yourself just when your headache is about to begin. Draw how you feel.” Reluctantly, Chloe sketched the image of a teenage girl with taut shoulders, stiff neck, bulging forehead and eyes, and a worried expression on her face. Dr. Witten responded, “That’s a really good picture. The girl looks so tense! I wonder what’s going through her mind right now.” Dr. Witten drew a bubble above the image of the girl and then asked, “Write some words that describe what she’s thinking.”
Chloe hesitated, reached for the pencil, paused again and then began writing. The words flowed from her, like water breaking through an old dam that was no longer able to bear the strain: math test, language arts presentation, student council service project, science fair, string ensemble, dad’s cholesterol, mom’s work schedule, friends, another headache, getting enough sleep, grandma’s sick . . .
“Do you think about these things before you have a headache?” asked Dr. Witten.
Chloe looked up from the paper, then answered, “I think about these things all of the time. There’s always something going on in my life, something to worry about. I tell myself, ‘Relax. Nobody else worries about things like you do.’ But it doesn’t do any good. I feel tense all the time. I can’t control it. It’s the worst at night, before I fall asleep. All the things I need to do and should have done come to my mind and they don’t stop.”
Dr. Witten responded, “All the things that you’re good at, like school and music?”
“Right,” Chloe sighed. As a tear trickled down her cheek, she added, “That’s just it. I think that if I didn’t worry so much, you know—make sure I’ve planned for everything, I might not get good grades, or do well in my ensembles, or let my parents down.”
Pointing to her head, Dr. Witten replied, “You carry all this pressure up here.” Your problem is not the headaches, though—it’s that you think too much! I’d like to work with you to find a way to stop all that worrying. Would you like that?”
For the first time in a long time, Chloe smiled.
1. What DSM-5 anxiety (or associated) disorder best describes Chloe’s behavior?
Generalized anxiety disorder (GAD)
2. How does Chloe meet DSM-5 criteria for this disorder?
- Chloe experiences excessive anxiety and worry (apprehensive expectation) occurring most days for at least 6 months.
- Chloe finds it difficult to control her worrying.
- She experiences the following symptoms: (1) restlessness, tension, (2) fatigue, (3) muscle tension, and (4) sleep disturbance. We would need to question her or her parents about other symptoms: (5) concentration problems and (6) irritability.
- Chloe’s symptoms cause distress and impairment (headaches).
- Her symptoms are not better explained by a medical condition.
- Her symptoms are not better explained by another psychiatric disorder.
3. When do problems with worrying tend to emerge? Is Chloe’s age on onset developmentally atypical?
Children develop the capacity to worry about future events at approximately age 4 or 5 years. However, most children are unable to dwell on their worrying until after age 8 years. Consequently, GAD does not tend to emerge until age 10 or later. Chloe began experiencing problems with worrying at age 11 or 12 years, which is a typical age of onset for GAD in children.
4. Chloe seems to worry about mundane things: school, extracurricular activities, family. How does the worrying of children with anxiety disorders differ from the worrying of typically developing children?
Children with and without GAD worry about the same things; the content of their worrying is similar. However, children with GAD differ from children without GAD in three ways: (1) they have a greater number of worries, (2) they experience worrying as more intense or distressing, and (3) they spend a greater percentage of their day worrying.
5. Chloe seems to be a high-achieving girl who is rather mature for her age. Is this typical of children with anxiety disorders?
Kendall and colleagues have argued that youths with GAD create an “illusion of maturity” in which they appear more behaviorally and emotionally competent than they really are. Beneath this façade, youths like Chloe harbor a strong need for perfectionism and strong feelings of self-doubt, self-criticism, and uncertainty about future events and their ability to cope.
6. Based on the results of longitudinal studies, what disorder is Chloe at particular risk for developing as she enters later adolescence and early adulthood?
Youths with GAD are at increased risk for major depressive disorder later in life. The anxious-misery symptoms of GAD and major depressive disorder are highly comorbid and distinct from the fear/panic symptoms that characterize other DSM-5 anxiety disorders.
7. How can cognitive avoidance theory be used to explain Chloe’s problem with chronic worrying?
According to cognitive avoidance theory, worry is maintained through negative reinforcement. Worrying allows individuals to replace emotionally laden images of imminent danger or misfortune (e.g., failing a test, embarrassing oneself at a recital) with more abstract, analytical thoughts about possible future misfortune. As long as Chloe worries, she can avoid fear and panic.
8. If you were Chloe’s clinician, what evidence-based psychotherapies or pharmacological interventions might you recommend?
Cognitive therapy for GAD might focus on three cognitive distortions often shown by youths with this disorder. These distortions are catastrophizing (i.e., anticipating the worst possible future outcomes), overgeneralizing (i.e., believing that a single adverse event is a sign of terrible future misfortune), and personalizing (i.e., assuming personal blame for others’ mistakes or misfortune). A cognitive therapist would help Chloe identify and challenge these beliefs by evaluating evidence that support or refute them.
Results of Child/Adolescent Anxiety Multimodal Study (described in the textbook) showed that combined SSRI and CBT was more effective than either treatment alone for older children and adolescents with GAD. Medication alone is more efficacious than psychotherapy; however, youths prescribed medication alone still tend to experience clinically significant GAD symptoms and relapse is high when medication is discontinued.
* Note that the case study titled Thoughts Before Bedtime presents an older adolescent with GAD who also experiences insomnia associated with this condition.
Sibling Rivalry
Obsessive–Compulsive Disorder
Isabella Hague was an 11-year-old girl referred to an outpatient mental health clinic by her mother because of “a curious preoccupation about harming her infant brother.” Isabella’s immediate family consisted of herself, her father and mother, and her 12-month-old baby brother, Manuel. Isabella’s mother, a sales executive, and her father, a store manager, had been thrilled when Isabella was born 12 years ago. The couple had difficulty conceiving a child and viewed Isabella as “their miracle.” Although they thought Isabella would be their only child, Mrs. Hague was surprised to learn that she was pregnant with Manual last year. Mrs. Hague reduced her work hours to stay at home with Manuel and the family soon adjusted to being a group of four.
Or so it seemed. Approximately three months after Manuel’s birth, Mrs. Hague noticed Isabella’s mood change. The formerly cheerful girl who loved to spend time with her parents became irritable and reclusive.
“Isabella would often snap at us, for no reason,” described her mother. “She’d seldom smile and was often crabby or disrespectful. We knew something was different about her. She’d also spend a lot of time by herself, usually in her room or in her tree house in the back yard.”
Mr. Hague added, “We figured that Isabella was having a bad case of sibling rivalry. For 11 years, she was our only child—our baby. Now she has to share attention with Manny. And, to be honest, Manny demands a lot of attention. We tried to make sure that Isabella didn’t feel neglected, so we’d take her on special outings, like to the movies or to dinner, you know, one-on-one.”
On one such outing, Mrs. Hague discovered the source of Isabella’s change in mood. While eating frozen custard, Mrs. Hague raised the possibility that Isabella might be jealous of Manny. Isabella burst into tears. After a long while, she admitted that she often had “strange thoughts” about hurting Manny. Once, while watching Manny in his crib, Isabella thought about how easy it would be to smother him with a blanket or pillow. Another time, when her mother was bathing Manny, Isabella imaged drowning him in the tub. Such thoughts began shortly after his birth and gradually increased in frequency and severity.
Later, the psychologist at the clinic questioned Isabella about her “strange thoughts.”
Isabella explained, “I love Manny so much. I’ve always wanted a baby brother or sister. I’d never do anything to hurt him. I feel so guilty!”
“Guilty?” the psychologist asked.
“Like maybe I might actually do something that could hurt him,” Isabella explained. “I know I never will but I still think it.” She paused and then added, “Like maybe if I think it, it might actually come true.”
The psychologist asked, “So if you don’t act upon these thoughts, how do you get rid of them?”
Isabella responded, hesitantly, “I pray. I ask God to get rid of these bad thoughts and to help me love my brother. I know I shouldn’t have these thoughts, but I do, so I pray to get rid of them.”
“Do you say specific prayers?” asked the psychologist.
“At first I would say three Our Fathers,” said Isabella. “That helped a lot. Then I started adding other prayers to get the thoughts out of my mind and to make me feel better. This all took a lot of time and if I messed up, I’d think, ‘I need to start over and get it right’ otherwise it wouldn’t work.”
“You mean, if you didn’t say the prayers right, it wouldn’t help you get rid of the bad thoughts?” asked the psychologist.
“Yes,” responded Isabella. “Or it wouldn’t stop bad things from happening to Manny. Sometimes, I would spend a lot of time praying, getting it right until I felt like everything was OK. I wish there was some way I could stop.”
1. What DSM-5 anxiety (or related) disorder best describes Isabella’s behavior?
Obsessive–compulsive disorder (OCD)
2. Review the DSM-5 criteria for this disorder. Describe how Isabella meets diagnostic criteria for this condition.
A. Isabella experiences obsessions and compulsions (although only one is required for the DSM-5 diagnosis).
- Obsessions: Recurrent thoughts about harming Manuel which are unwanted and cause distress. These thoughts are suppressed and neutralized by compulsions (see below).
- Compulsions: Repetitive mental acts (i.e., praying) that Isabella feels driven to perform according to certain rules in response to her unwanted thoughts about harming Manuel. The mental acts reduce guilt and appear excessive.
B. The obsessions cause clinically significant distress and impair Isabella’s emotional functioning and interactions with her parents (e.g., increased irritability and reclusive behavior).
C. Symptoms are not attributable to a substance.
D. Symptoms are not better explained by another mental disorder.
3. How might you characterize Isabella’s insight regarding her problem?
Using the DSM-5 , Isabella’s insight would likely be described as “good or fair.” She reports that she loves her brother and does not wish him harm. She also feels guilty about having thoughts about killing him. On the other hand, Isabella worries that simply having ill thoughts about her brother might somehow magically cause harm to him.
4. What two cognitive distortions often characterized the thoughts of children and adolescents with Isabella’s condition? Does Isabella experience these cognitive distortions?
Inflated responsibility for misfortune: Youths with OCD often believe that if something bad happens to a loved one, they are somehow responsible for this negative event. Although there is no evidence of this distortion in the case study, a clinician might want to assess further to see if Isabella exhibits this cognitive distortion.
Thought–action fusion: Youths with OCD often believe that merely thinking about a negative event will increase its chance of occurring. Isabella adopts this distortion when she thinks that imaging harm befalling Manuel might actually cause real harm to befall him.
5. What is PANDAS? Is it applicable to Isabella?
PANDAS (Pediatric Autoimmune Neuropsychiatric Disorder Associated with Streptococcus) is a neurological disorder in which a child exhibits OCD-like behaviors immediately following a strep infection. A clinician would need to assess Isabella’s physical health prior to the onset of her OCD symptoms to rule out PANDAS.
Recently, some researchers have developed guidelines for PANS (Pediatric Acute-onset Neuropsychiatric Syndrome) in which youths develop OCD-like behaviors triggered by unknown infections, not only strep. Therefore, any serious infection prior to Isabella’s symptoms should be assessed as a possible cause for her disorder.
Can’t Fight This Feeling
Tourette’s Disorder
David Simons was an 8-year-old boy referred to an outpatient mental health clinic by his pediatrician because of chronic anxiety problems and “nervous habits.” David is the only child of Joseph and Margaret Simons. Mr. Simons works as a house painter whereas Mrs. Simons recently returned to work as a medical technician after several years caring for David at home.
Approximately 18 months ago, David’s parents brought him to his pediatrician because of an upper respiratory infection. Although David recovered from this illness, his parents noticed lingering problems with sniffling, wrinkling and wiping his nose, and a persistent, dry cough. A follow-up appointment showed David to be healthy. His physician suggested that David might have merely developed some “bad habits” during his illness that would likely go away over time.
Indeed, David’s strange mannerisms subsided over the following weeks, only to return with greater intensity at the beginning of the school year. During his first weeks of kindergarten, David began coughing again, approximately 30 to 40 times per hour. His coughs were accompanied with head turns, rapid blinking, and a grimace that resembled a combination of a smirk and a wink. These mannerisms also waned gradually over the first 3 months of school.
David’s cough and repetitive facial movements returned yet a third time several months ago. This time, their onset coincided with his mother’s return to full-time employment and David’s enrollment in an after-school program. David’s classmates began to tease him, calling him names like “coffee” and “sicky” and running away from him as if he had a contagious disease. David’s teacher allowed David to leave the classroom or excuse himself from class activities when he felt the need to cough or engage in any of his other behaviors. This strategy reduced class disruptions, but caused David to miss out on learning opportunities.
The psychologist who conducted the evaluation learned that Mr. Simons had a history of obsessive–compulsive behavior in early adolescence. His condition was never diagnosed and gradually improved on its own. Mrs. Simons denied obsessions or compulsions, but admitted to chronic problems with anxiety and insomnia for which she takes medication.
David told the psychologist that he “can’t help (him)self” when he coughs, turns his head, wrinkles his nose, blinks, or winks. Just before he coughs, he gets a “strange feeling, like something building up inside” that he “just has to let go.” David says that if he tries to “fight” the urge, it gets worse until he “can’t hold it back.” David denied having any thoughts, ideas, or images before coughing or other behaviors. He admitted that he felt “very bad” about disrupting class and reported that he felt sad and lonely at school. Neither David’s parents nor his teacher reported problems with hyperactivity or inattention. However, both parents and his teacher noticed increased problems with sadness and social withdrawal.
1. What DSM-5 anxiety (or related) disorder best describes David’s behavior?
Tourette’s disorder
2. Explain how David meets DSM-5 diagnostic criteria for this condition.
- David has multiple motor tics (e.g., wrinkling nose, head turning, grimacing) and at least one vocal tic (i.e., coughing).
- David’s tics have waxed and waned, yet have persisted for more than one year since their onset.
- Onset is prior to age 18 years.
- The problem is not better explained by a substance or medical condition.
3. How might a clinician differentiate David’s condition from OCD?
Children with OCD almost always perform their compulsion in response to an obsessive thought or image. In contrast, less than 50% of children with Tourette’s disorder report an obsession prior to their tics. More commonly, children with Tourette’s disorder report a vague premonitory urge (analogous to an itch) prior to the tic.
4. Does David still meet diagnostic criteria for this disorder, despite the absence of coprolalia?
Coprolalia, the involuntary utterance of obscene words, is seen in only 10% of patients with Tourette’s disorder. Coprolalia, therefore, is not necessary for the disorder and occurs in only a minority of patients.
5. Is it typical for children to show a waxing and waning of symptoms over time, as displayed by David? What causes this waxing and waning?
Yes. Onset tends to occur around age 5½ years with a waxing and waning of severity over time. The type of tics that children show can also change across development, as shown by David. Tics tend to be exacerbated by psychosocial stressors. For example, the stress of beginning school or the adjustment to his mother transitioning to the workforce may have increased the severity of David’s tics.
6. In the case study, the psychologist assessed David for OCD. Is it possible for David to also have OCD?
Yes, approximately 25% to 50% of children with tic disorders also have OCD. Clinicians should routinely assess the presence of OCD and ADHD (another frequently co-occurring disorder) in children like David. The case study suggests that David probably does not have obsessions or ADHD-related behaviors, however.
7. If you were David’s psychologist, what evidence-based treatments might you recommend?
Comprehensive Behavioral Intervention for Tics (CBIT) is a first-line treatment for children like David. It has three components: (1) education about tics and Tourette’s disorder; (2) self-monitoring, to help David and his family record the frequency and severity of his tics; and (3) habit reversal training in which David’s parents might reinforce David for engaging in a behavior that is incompatible with the tics. For example, David might be taught to inhale slowly through his nose whenever he experiences the urge to cough.
A behavior therapist would also use contingency management to alter environmental factors that might exacerbate David’s tics. For example, David’s teacher might be negatively reinforcing the tics by allowing David to leave the classroom whenever he experiences the urge to cough. Instead, his teacher might reinforce him for using habit reversal techniques at school.
Chapter 12: Trauma-Related Disorders and Child Maltreatment
Family problems.
Posttraumatic Stress Disorder (PTSD)
Henry Evans was an 11-year-old boy referred to outpatient therapy through the Department of Children and Family Services. Henry is the oldest of four children born to Mark Evans and Julia Bryers. His younger sisters (ages 6 and 9 years, respectively) and brother (age 3⅓years) lived in the same single-family home prior to their involvement with protective services.
Henry’s home had never been a happy one. Mr. Evans worked several part-time jobs to make ends meet. The family never seemed to have enough money and, consequently, were forced to rent a small, two-bedroom home in a bad neighborhood. Mrs. Bryers had also worked part time before the birth of her most recent baby. Now a stay-at-home mom, Mrs. Bryers struggles to keep up with household tasks and the responsibilities of raising four children during her husband’s frequent absences. The couple’s relationship was strained by Mr. Evan’s frequent alcohol use and Mrs. Bryer’s history of anxiety and chronic stomach ailments that often left her incapacitated. Indeed, the couple frequently argued and occasionally hit and shoved each other. Their loud altercations were well known to neighbors and (on two occasions) the police.
Several months ago, Henry and his siblings were removed from his parent’s custody following a particularly violent interaction. The police report indicated that Henry’s father hit his mother with a fireplace poker while intoxicated. The attack left Mrs. Bryers with a large gash on her forehead that produced copious amounts of blood. Unfortunately, Henry and his three older siblings awoke in time to witness the injury. They also saw Mrs. Bryers defend herself by shooting at her husband with a handgun. Mrs. Bryers had poor aim, and left a large bullet hole on the living room wall.
Henry adjusted poorly to living with his maternal aunt, Jocelyn. Separated from his three siblings and his parents for several weeks, Henry acted sad and emotionally withdrawn, “like he had lost all sense of joy” according to his aunt. He did not want to play games or interact with other children in the neighborhood. Although Henry was known as a troublemaker before the incident, his behavior at school worsened. He seemed to have no attention span, could not concentrate on assignments, and was often moody, irritable, and easily “set off” by others. On two occasions, Henry reacted aggressively to classmates—once by biting and the second time by hitting a classmate on the playground.
Jocelyn was most troubled by Henry’s sleep problems. Henry often had problems falling asleep and would frequently ask Jocelyn if he could sleep on the floor of her bedroom at night. He was especially reluctant to sleep by himself at night because he expected “bad things” to happen. (He was initially in bed at the time the incident with his parents occurred.) Henry also experienced nightmares, approximately two or three times each week. Henry refused to tell Jocelyn about these dreams, claiming that he “didn’t want to talk about them.” Jocelyn suspected that these dreams involved his parents because Henry said words like “mom” “no” and “stop” in his sleep but she could not be sure.
Henry’s father is currently incarcerated for felonious assault. Henry has biweekly, supervised visitation with his mother. However, Henry refuses to visit his mother at their home and insists that he will remain living with his aunt. His social worker says that family reunification is planned for next month.
1. What DSM-5 disorder best describes Henry’s behavior?
Posttraumatic stress disorder (PTSD) for children older than 6 years of age
2. How does Henry meet DSM-5 diagnostic criteria for this condition?
- Henry directly witnessed serious injury (i.e., domestic violence) to his mother and the threat of death/injury to his father.
- Henry has one or more intrusion symptoms associated with the trauma:
He has recurrent, distressing dreams that may be about the trauma. Note that DSM-5 recognizes that children’s dreams may not have recognizable content.
- Henry has one or more avoidance symptoms associated with the trauma:
He avoids going back to his house where the trauma occurred (i.e., an external reminder of the trauma).
- Henry has two or more negative alterations in cognitions or mood associated with the trauma:
He shows a persistently negative emotional state (anxiety), diminished activity in activities with others, possible feelings of detachment or estrangement from others, and a lack of positive emotions. These symptoms would need to be confirmed by Henry during an interview.
- Henry has two or more alterations in arousal and activity associated with the trauma:
He shows irritability with angry outbursts, problems with concentration, and sleep disturbance.
- Duration is likely > 1 month.
- The disturbance causes Henry significant distress and is impairing his social and educational functioning.
- The disturbance is not attributable to a substance or medical condition.
3. The case study does not describe Henry’s immediate reaction to observing his parents’ fight. Is his reaction important to determine his DSM-5 diagnosis?
In the past, PTSD was considered an anxiety disorder. People diagnosed with PTSD were required to react to traumatic events with fear, helplessness, or horror. In DSM-5 , however, PTSD is considered a trauma-related disorder and a specific anxiety response is not needed for the PTSD diagnosis. A recent survey of children with PTSD showed that many youths did not react with fear or anxiety and approximately 11% showed no emotional response to the trauma whatsoever.
4. In what way might Henry’s functioning before witnessing his parents’ fight predict his behavior and emotions after the incident?
Children’s functioning before exposure to a traumatic event predicts their likelihood of developing PTSD. The case study suggests that Henry’s family is experiencing significant psychosocial stress, perhaps caused by relationship problems between Henry’s parents, parental substance use and psychological problems, and low socioeconomic status. It is possible that these stressors made Henry vulnerable to PTSD upon exposure to his parents’ fight and relocation to his aunt’s home.
5. If you were a police officer or other first responder called to Henry’s house at the time of his parents’ fight, how might you use psychological first aid to help Henry and his siblings?
Psychological first aid (PFA) is an evidence-based intervention that is administered to individuals shortly after exposure to a traumatic event. A first responder would try to implement the following steps: (1) foster a sense that Henry is safe from physical harm, (2) remain calm, (3) increase Henry’s self-efficacy by giving him as much control over the situation as possible, (4) achieve connectedness and social support by uniting him with his aunt or other supportive family members, and (5) remain hopeful about the future. A first responder would emphasize safety and empathy and would likely not encourage children to discuss the traumatic event immediately.
6. What evidence-based interventions might a psychologist use to help Henry?
Trauma-focused cognitive-behavioral therapy (TF-CBT) is presented in the text. It includes the following components: (1) education about PTSD; (2) relaxation training or other coping skills; (3) imagined or in vivo exposure, such as encouraging Henry to talk about the trauma or visit his home where the trauma occurred; and (4) challenging maladaptive thoughts or cognitive distortions that can contribute to feelings of self-blame, anxiety, or anger.
Eye movement desensitization and reprocessing (EMDR) involves asking individuals to recall traumatic events, relaxation training, and the use of repeated, rapid, lateral eye movements tracking specific stimuli (e.g., lights, therapist’s finger). Imagined exposure seems to be a critical component of treatment.
Hurt Inside
Disinhibited Social Engagement Disorder (DSED)
Ivy Minton was a 24-month-old toddler referred to our clinic by her foster mother, Jennifer Spence. Ms. Spence is a middle-aged, experienced foster parent who had been caring for Ivy for the past 3months alongside her three other foster children. Ivy was removed from her parents’ custody approximately three months earlier due to child endangerment and neglect. Ivy was discovered, unsupervised in a dilapidated apartment. Her mother had a history of opioid dependence. The paramedics were called to the apartment by Ivy’s “aunt” who reported that Ivy’s mother had overdosed on heroin.
Child protective services sought an emergency foster placement for Ivy with her maternal grandmother. However, chronic health problems interfered with her grandmother’s ability to care for Ivy. After 6 weeks in her grandmother’s care, Ivy was again relocated, this time to Ms. Spence’s foster home. Although her long-term treatment plan involves parental reunification, Ivy’s mother has experienced problems recovering from her substance use problem.
Developmental rating scales, completed by Ms. Spence, indicated that Ivy’s motor, cognitive, and adaptive functioning was within normal limits for a child her age. Physically, Ivy was healthy. Although she exhibited minor problems with insomnia and occasional picky eating, her foster mother reported no problems with her affect and mood. Similarly, Ivy showed no problems with hyperactivity or impulsive behavior at home. Her social functioning, however, caused her foster mother concern.
“Two weeks ago was the final straw. Me, Ivy, and two of the other kids were playing in the park. I was helping Ivy down the little slide and she scraped her leg as she came down. She screamed something awful! Then, she walked past me and ran toward another mom, begging to be picked up. The other mom gave me a strange look, bent down, and picked up Ivy to comfort her. I thought, ‘Why didn’t Ivy come to me? Aren’t I the one who’s been caring for her all these months? What am I doing wrong?’ What surprised me even more is when the other mom tried to return Ivy to me. Ivy fussed, like she didn’t want to leave the other mom. My initial feeling of embarrassment was replaced by a deep hurt inside.”
Ms. Spence described similar episodes of Ivy’s overly social behavior. During playdates and church activities, Ivy seemed just as content sitting in other parents’ laps as her foster mother’s. On one occasion, she hopped onto the youth pastor’s lap and began stroking his beard in an affectionate way, much to his surprise and embarrassment. Ivy also wandered off with adults she did not know on two occasions. “She gave me quite a scare,” commented Ms. Spence. “I need to watch her like a hawk because she’ll go off with anyone—even strangers—without checking with me first.”
Observations of Ms. Spence and Ivy in the clinic playroom largely confirmed her foster mother’s reports. Ivy was an active, verbal, 2-year-old who took delight in social engagement. She maintained good eye contact and showed appropriate imitation and imaginary play. She also displayed adequate reciprocity in her social interactions and a high degree of positive affect. Ivy’s motor skills were within normal limits. Although she fussed slightly when Ms. Spence told her it was time to clean up, Ivy responded well to her foster mother’s directions. Curiously, Ivy showed no anxiety when she first met the psychologist and readily went off with the receptionist to another room when the psychologist and Ms. Spence discussed treatment options.
1. What DSM-5 disorder best describes Ivy’s behavior?
Disinhibited social engagement disorder (DSED)
2. How does Ivy meet diagnostic criteria for this condition?
- Ivy shows (1) reduced reticence in approaching unfamiliar adults, (2) overly familiar behavior with others (e.g., sitting on strangers’ laps, stroking beard), (3) failure to check back with caregiver, and (4) willingness to go off with a stranger.
- Ivy’s behavior reflects socially disinhibited behavior and not general problems with impulsivity.
- Ivy has a history of early deprivations and disruptions to her caregiving, including placement with multiple foster caregivers.
- She is older than 9 months of age (and should, therefore, exhibit wariness of strangers).
3. How does Ivy exhibit both risk and resilience?
Ivy has several risk factors that place her on a negative developmental trajectory with respect to her social-emotional functioning. These risks include parent substance use problems, experiences of neglect and deprivation during infancy and toddlerhood, separation from primary caregivers, and multiple placements in foster homes. Despite these risks, Ivy shows some resilience. Although she shows disinhibited social behavior, her motor, cognitive, language, and adaptive skills are within normal limits. Chapter 1 presents a more detailed discussion of risk and resilience across development.
4. What is an underlying cause of Ivy’s problems in social functioning?
It is likely that Ivy’s indiscriminately social behavior was caused by deprivation and disruptions in her caregiving history. Prospective longitudinal studies, described in the text, indicate that DSED does not necessarily reflect a disturbance in caregiver–child attachment. Even infants who exhibit secure attachment toward their primary caregivers can develop DSED if exposed to deprivation during a sensitive period in their development.
Most data indicate that DSED reflects an underlying problem with social inhibition, that is, the ability to regulate one’s actions in social situations with adults. This lack of social inhibition is associated with social-emotional deprivation in late infancy or toddlerhood, a developmental period in which children’s capacity for social inhibition typically develops. Therefore, DSED is often caused by a lack of inhibitory control rather than a lack of attachment.
5. What is Ivy’s prognosis, assuming she receives treatment?
DSED is a relatively new disorder; therefore, prospective longitudinal studies examining its course are limited. However, three studies described in the text indicate that social disinhibition decreases with age but continues to persist and interfere with social functioning.
6. What evidence-based treatments are effective for youths like Ivy?
Ideally, Ivy will be reunited with her parents. A stable home environment, characterized by sensitive and responsive caregiving, will increase the chance of optimal development. If Ivy cannot be reunited with her parents soon, a stable foster placement would be the next best option for her. It would be important for Ms. Spence to know that Ivy’s behavior likely reflects her caregiving history and are not an indicator that Ivy does not love her or that she is doing something wrong.
Unfortunately, there are few evidence-based treatments for DSED. Attachment and Biobehavioral Catch-Up (ABC) is one option, presented in the text. Although it is designed for children with attachment disorders, rather than DSED, it may be helpful to either Ms. Spence or Ivy’s mother to facilitate sensitive and responsive caregiver–child interactions. Several researchers have suggested that social disinhibition might be improved with behavioral training or medication, but data supporting these claims are limited. Clearly, more research needs to be directed at developing an evidence-based treatment for youths with DSED.
Chapter 13: Depressive Disorders and Suicide
Irritable isaac.
Disruptive Mood Dysregulation Disorder (DMDD)
Isaac Morgan was an 11-year-old boy brought to the emergency department (ED) of our hospital by the police. Earlier that evening, Isaac’s mother, Mrs. Morgan, told Isaac that she would not take him to soccer practice until he cleaned his room. Isaac whined, but Mrs. Morgan insisted that he clean his room. Isaac became belligerent, ran upstairs to his room, and began breaking toys and other objects. His mother chased him upstairs and ordered him to stop. Screaming, Isaac grabbed a pair of scissors and waived them at his mother, ordering her to leave him alone. With some difficulty, Mrs. Morgan was able to wrestle the scissors from Isaac’s hands. Isaac continued to scream and tried to scratch her with his fingernails. Exasperated and frightened, Mrs. Morgan returned downstairs to call her husband. While she telephoned, Isaac began banging his head against his bedroom wall, wailing in a loud voice, “I need to go. I need to go. You can’t make me clean my room!” Mrs. Morgan immediately called 911 and the police arrived shortly thereafter.
Mrs. Morgan provided background information to the psychologist at the hospital. Isaac had a history of violent temper tantrums beginning approximately five years ago. At first, the tantrums occurred only at home when Isaac’s parents would make him perform a chore or punish him with time out. Later, the tantrums became more violent and arose with little provocation. For example, Isaac would scream and throw objects when he learned that he could not go out to play or when he would lose a game of checkers. Two years ago, Isaac also began showing similar tantrums in class and on the playground at school. Last year, he was suspended for throwing a book at a teacher. This year, he began attending a special education class for students with “emotional disturbance.” On average, Isaac tantrums four to five times per week with each tantrum lasting between 30 minutes and 2 hours.
When not having tantrums, Isaac presents as a disruptive and moody child. His mother describes him as “irritable, grouchy, or cranky” most of the time. His father calls him “a pain in the ass who is set off by the smallest setbacks or disappointments.” Both parents admit that Isaac has had longstanding problems with oppositional and defiant behavior. “Isaac never listens to us and seems to take delight in pushing our buttons,” said his father.
Although physically healthy, Isaac has a longstanding psychiatric history. He showed early delays in gross motor skills (e.g., walking), fine motor skills (e.g., using utensils), and spoken language. In school, he showed deficits in reading acquisition and math. His academic problems were compounded by problems with hyperactivity and impulsivity beginning at age 4 and inattention and poor concentration at age 6. He was formally diagnosed with ADHD at age 7 and has been prescribed a litany of stimulant medications that have yielded only limited benefits.
Last year, a psychiatrist diagnosed Isaac with bipolar I disorder because of his longstanding problems with irritability, distractibility, and talkativeness combined with his recurrent (and often violent) tantrums or “rages.” Isaac has no family history of bipolar disorder and lithium had little effect on his behavior.
Isaac’s parents report that Isaac’s behavior has placed considerable stain on their marriage. They frequently argue about him and have contemplated separating. They also admit that they often neglect their other two boys, Noah (7) and Asher (4), because Isaac demands so much attention. Mrs. Morgan reported a longstanding history of major depression that has worsened considerably in the past 2 years. Mr. Morgan reported a mixture of depression, anxiety, insomnia, and alcohol use problems.
Isaac was reluctant to talk with the psychologist and provide additional information regarding his thoughts and feelings. The psychologist offered to meet with him individually the next day. Isaac replied, “Why? There’s nothing wrong with me.”
1. What DSM-5 disorder best describes Isaac’s current problems with irritability and tantrums?
Disruptive mood dysregulation disorder (DMDD)
2. Provide a rationale for your primary diagnosis.
- Isaac has recurrent temper outbursts that are physically aggressive toward people and destructive to objects. His tantrums are also out of proportion to the situation.
- His outbursts are inconsistent with his developmental level.
- They occur, on average, at least 3 days per week.
- Between outbursts, he shows persistently irritable or angry mood that is observable by others.
- Signs and symptoms of the disorder have existed for at least 12 months.
- Signs and symptoms exist in at least two settings (e.g., home, school).
- Isaac is first diagnosed between 6 and 18 years of age.
- Onset of symptoms began before age 10 years.
3. Assuming Isaac meets DSM-5 criteria for ADHD, can he also be diagnosed with this disorder?
Yes. Most children with DMDD also meet diagnostic criteria for ADHD and should be diagnosed with both conditions. However, most children with ADHD do not have DMDD. Youths with ADHD should only be diagnosed with DMDD also if they show persistent irritability/anger and recurrent outbursts in addition to their ADHD symptoms.
4. Assuming Isaac meets DSM-5 criteria for oppositional defiant disorder (ODD), can he also be diagnosed with this disorder?
No. DSM-5 instructs clinicians to diagnose DMDD only in children who meet diagnostic criteria for both DMDD and ODD. DMDD is considered the more severe disorder and is given diagnostic preference.
5. Why is bipolar I disorder probably not an accurate diagnosis for Isaac?
Several years ago, children who showed chronic problems with irritability, moodiness, and affective “rages” were often assigned the bipolar I diagnosis. Children with irritability and comorbid ADHD (like Isaac) were especially prone to receiving the bipolar diagnostic label because irritability and several symptoms of ADHD (i.e., decreased need for sleep, talkativeness, distractibility, psychomotor agitation) are also features of mania.
Isaac probably does not have a bipolar disorder, however. He does not show classic episodes of mania or hypomania required for the bipolar I diagnosis. Instead, his irritable mood is persistent rather than episodic. Furthermore, Isaac seems to lack an episode of major depression, which is usually seen in people with bipolar disorders. Other evidence against the bipolar I diagnosis include (1) he has no family history of bipolar disorders, (2) both parents have histories of depression and anxiety, and (3) Isaac was nonresponsive to lithium.
6. What psychiatric problems is Isaac most at risk for developing in adulthood?
Longitudinal studies indicate that youths with DMDD, like Isaac, are at risk for developing anxiety and depression in adulthood. In contrast, risk for bipolar disorders is relatively low. Indeed, both parents have histories of anxiety and/or depression.
7. What brain areas may be responsible for the problems with emotional regulation shown by children like Isaac?
Overactivity of the medial frontal gyrus and anterior cingulate is associated with problems regulating emotions and controlling temper. Youths with DMDD may selectively attend to negative social cues (e.g., being reprimanded by a parent or teacher, losing a game with a friend) and, because of this overactivity, exhibit severe tantrums that are difficult to control.
8. Identify two psychosocial treatments that might be effective for Isaac.
Traditional parent training is often ineffective for youths with DMDD because it does not specifically target children’s angry outbursts and longstanding mood problems.
Comprehensive family therapy, in which children and parents learn to manage children’s tantrums and irritability, may be more effective. Key components of treatment might involve helping parents identify triggers for Isaac’s tantrums, helping the family diffuse tantrums early before they escalate, and improving Mr. and Mrs. Morgan’s relationship so that they can more effectively address their children’s social-emotional needs.
Emerging data indicate that youths with DMDD may benefit from a more consistent sleep–wake cycle. Sleep hygiene and chronotherapy can be helpful to regulate this cycle.
The New Kid
Major Depressive Disorder
Danielle is a 16-year-old high school student who recently moved from a small town in Minnesota to Santa Barbara, California. Danielle’s soccer coach referred her to the school psychologist because he was concerned about her sad affect and withdrawn behavior. Although Danielle is a good midfielder, and has been on the soccer team since transferring to the school last semester, she has repeatedly commented that she “no longer enjoys playing” and feels like she “doesn’t fit in” with the other girls on her team. Danielle admitted to problems making friends at her new school. She feels terribly homesick, missing her former classmates and teammates.
Danielle was a straight-A student and star soccer player at her high school in Minnesota. She repeatedly made the high honor roll and started as a center midfielder on both her school varsity soccer team and a competitive travel team during the summer. In California, however, Danielle found her classes much more difficult. Although she would study incessantly, she found herself unable to earn anything higher than Bs and was struggling to pass language arts. Moreover, she was unable to gain a starting position on her school soccer team, which already had many players who were more talented and experienced than Danielle. Although Danielle put countless hours into practicing, she seldom played more than a few minutes each game and had yet to score or assist in a goal.
The school psychologist asked Danielle to describe a typical school day. Danielle explained that she had a difficult time waking in the morning, can’t concentrate on her classes during the day, and usually eats lunch alone. “After school,” she explained, “I try to get enough energy together to go to soccer practice, but my heart is not in it. Anyway, what’s the point? I’m not as good as the other girls on the team and I’ll never get to play as much as I did back home.”
The school psychologist asked, “Have you thought about getting a tutor, to help you with language arts?” Danielle replied, “No. It’s just no use. I’m no good at anything. I’m a total loser.”
“What about friends?” asked the school psychologist. “Have you tried to make friends with the girls on your team?” Danielle answered, “At first I did. But I could tell that they didn’t like me. They already have their own friends. Who wants to be friends with the new kid?”
1. What DSM-5 disorder best describes Danielle’s behavior?
Major depressive disorder
2. How does Danielle meet diagnostic criteria for this disorder?
- Danielle shows the following signs and symptoms:
- Depressed or irritable mood most days
- Anhedonia (giving up activities that she formerly enjoyed)
- Sleep problems
- Fatigue/loss of energy
- Feelings of worthlessness
- Concentration problems
- She experiences significant distress and social/academic impairment.
- Problems are not attributable to a medical condition.
- Problems are not better explained by another psychiatric disorder.
- There is no evidence of a history of mania or hypomania.
3. How might a cognitive therapist, like Aaron Beck, explain Danielle’s mood disorder?
Beck would argue that Danielle’s mood problems are caused by the way she thinks about stressful life events. Her thoughts about these events, rather than the events themselves, influence her actions and feelings. Beck would pay special attention to cognitive biases and distortions that Danielle might have regarding negative life events. A possible bias might be her tendency to attend to negative events and minimize or ignore positive events. A possible distortion might be twisting reality to fit her negative view of herself, others, and the world.
4. How might a behavior therapist, like Martin Seligman, explain Danielle’s mood disorder?
Seligman developed the theory of learned helplessness. This theory posits that individuals became depressed when they are unable to control their experiences. Another behavior therapist, Lewinsohn, believed that people become depressed when they are unable to derive positive reinforcement from their surroundings. In both cases, individuals (like Danielle) experience very little pleasure and (often) much discomfort from life.
Seligman revised his original theory. The revised learned helplessness theory of depression posits that people become depressed when they attribute negative events to internal, stable, and global causes. Danielle attributes her failures to internal (herself), stable (dispositional), and global (pervasive) causes.
5. How might an interpersonal therapist, like Myrna Weissman, explain Danielle’s mood disorder?
Klerman and Weissman posited that depression is a medical disorder that interferes with an individual’s psychosocial functioning. Although relationship problems do not necessarily cause depression, they can exacerbate mood problems. Interpersonal therapists believe that depression is exacerbated by one (or more) of the following relationship problems: (1) grief/loss of a loved one, (2) role transitions, (3) role disputes, and (4) interpersonal deficits. Danielle seems to be having difficulty adjusting to her new interpersonal role (i.e., student in a new school) and may be grieving the loss of her old peer network.
Suicidal Behavior
Melody O’Neil was born to dance. Her mother enrolled her in ballet at the age of 4. When Melody was 6, she began Irish dance lessons at the insistence of her grandmother, who emigrated from Ireland when she was a girl. Melody instantly fell in love with everything about Irish dance: the steps, the music, the incessant practice, and the close connection it had with her family’s ancestry. Melody also proved to be a very good dancer, winning local competitions and being featured in several recitals.
Dance lessons, costumes, and wigs were expensive. So were the entry fees and travel costs associated with competitions. Her mother began working a second, part-time job to help pay for individual lessons in addition to group instruction. Her father spent many weekends remodeling the family’s basement into a dance studio so Melody could practice at home. Melody’s younger sisters often were carted to Melody’s practices, recitals, and competitions. Melody’s room was decorated with Irish paraphernalia, recital brochures, ribbons, and trophies.
Now 15, Melody auditioned for a spot in the best Irish dance company in the region. Although it would place even greater burden on her family, her parents agreed that if she was going to “make it” as a professional dancer, she needed to be trained by the best instructors. During the audition, Melody gave it her all. Her mother commented afterward, “You danced beautifully—the best I have ever seen you dance. I’m sure you’ll get a spot.”
Melody’s mother was wrong. She was not selected for a spot. “Melody is a good dancer,” commented the leader for the dance company, “but she doesn’t have the skills that we expect from a girl her age.”
Melody took the news hard, but not as hard as her parents. Although they did not say so, their actions indicated that they began to regret the sacrifices they made for Melody. Melody’s mother quit her second job and cut back on the extra lessons and special recitals for Melody. Both parents seemed to spend more time with the other children in the family. Her dad began coaching one daughter’s basketball team; her mother volunteered to lead the other daughter’s Girl Scout troop. Melody began to feel less “special” than before and she hated it.
One year later, Melody was referred to counseling after attempting suicide. The police report indicated that she had tried to kill herself by taking her mother’s antidepressant medication and alcohol. Luckily, her younger sister discovered her lying unconscious in her bedroom, and Melody was able to receive medical treatment. The physician who treated Melody also noticed superficial cuts on her thighs that were likely self-inflicted.
During an interview with a psychologist at the hospital, Melody admitted to severe depression and suicidal ideation with intent to die. “No one loves me anymore,” she reported. “My mom and dad sacrificed so much for me—all for nothing. I tried my best, but my best just wasn’t good enough. I was a little fish doing well in a small pond, but I couldn’t advance beyond that.”
For a long while, Melody sobbed into her arm. She added, “My family will be better off without me. They can spend more time with my sisters. Maybe they can make something of themselves.”
1. Use the hopelessness theory of suicide to explain the possible causes of Melody’s suicidal behavior.
Hopelessness theory asserts that hopeless depression predicts suicidal ideation and actions. Hopelessness arises from three causes, each possibly shown by Melody:
- Negative events are attributed to stable and global causes. Melody believes that she is a failure at Irish dance because (1) she is a poor dancer and (2) she always will be; she could never be good enough to gain admission to the best dance company.
- The consequences of the negative event are deemed highly important. Melody had her heart set on becoming a top-quality Irish dancer. When she was not selected for the dance company, she was devastated.
- The negative event is an indicator of worthlessness. Melody’s identity was based on her skills as an Irish dancer. When those skills were called into question, she saw herself as worthless. Her parents’ actions toward her may have contributed to this sense of worthlessness.
2. Use the interpersonal–psychological theory of suicide to explain the possible causes of Melody’s suicidal behavior.
The interpersonal–psychological theory of suicide posits that disturbances in interpersonal relationships predict the emergence of suicidal thoughts and actions. Specifically, three factors prompt suicidal behavior, each possibly shown by Melody:
- Perceived burdensomeness: Melody sees herself as a burden on her family. She knows that her parents sacrificed time and money so that she could pursue a dance career. She also recognizes that her younger sisters’ needs may have been placed second to her own. Melody believes all of their efforts came to naught because she was not selected for the dance company.
- Thwarted belongingness: Melody likely experienced a loss of connection toward her family (especially her parents) after her potential dance career ended. She perceived them as taking less interest in her and favoring her sisters instead.
- Capability for suicide: Self-injurious behavior may desensitize Melody to self-harm and increase the likelihood of suicidal actions.
3. Imagine that you are the psychologist at the hospital who interviews Melody. After staying in the hospital overnight, you decide that she can return home under her parents’ supervision. What three components might you include in a safety plan for Melody?
Safety plans vary, but most have the following three components:
- Means restriction: The psychologist helps the family identify means for suicide and ways to reduce the risk of a future suicide attempt. For example, if the family has a firearm, it should be locked securely. If Mrs. O’Neil has other prescription medication in the house, it should be secured in a place that Melody cannot access and should be regularly monitored.
- Identify triggers and coping mechanisms: The psychologist helps Melody identify thoughts, feelings, or situations that might prompt a suicide attempt, such as an argument with a parent or intense feelings of loneliness or rejection. Melody might identify several ways to cope with these situations or feelings.
- Identify sources of social support: The psychologist would help Melody identify family members or friends who she might contact in case of future suicidal ideation. The psychologist might also give Melody his/her own contact number in case of an emergency and the number of a suicide crisis line.
4. Family-focused treatment might be especially helpful for Melody to help prevent future suicidal thoughts and actions. Briefly describe two evidence-based family-focused therapies that a psychologist might recommend.
Safe Alternatives for Teens and Youths (SAFETY) is a family-focused treatment that involves (1) means restriction, (2) improving communication and connectedness within the family, (3) identifying triggers for suicidal thoughts and actions, (4) improving coping mechanisms for negative thoughts and (5) improving coping mechanisms for negative feelings. Initially, adolescents and parents learn skills separately. Later, they practice skills together. Melody might especially benefit from sessions that focus on improving connectedness with family members.
The Resourceful Adolescent Parent Program (RAP-P) consist of four sessions for parents: (1) practical strategies to reduce adolescent suicidal thoughts and actions, (2) positive aspects of parenting behavior and ways to reduce parenting stress; (3) techniques to improve adolescents’ self-esteem and achieve closeness with the family, and (4) strategies for reducing family conflict. Melody and her parents might benefit especially from session 3, which focuses on self-esteem and connectedness in the family.
Chapter 14: Pediatric Bipolar Disorders and Schizophrenia
Bipolar I Disorder
Nolan Mitchell was a 9-year-old boy referred to the school psychologist for “inappropriate behavior” in his fourth-grade classroom. Earlier that day, Nolan had been sent to the principal’s office for repeatedly making “animal noises” in class, despite his teacher’s reprimands. “Nolan’s snorting, chirping, and grunting was finally too much,” his teacher reported. “I’m not sure what’s gotten into him lately. In the last few months, he’s gone from being an active, but generally compliant, boy to a class clown and troublemaker.”
Indeed, Nolan was now known as “the Joker,” a moniker given to him by several classmates because of his frequent antics during school. Nolan had a history of hyperactive and inattentive behavior, beginning in preschool. He was always talkative, had a hard time remaining seated during class, and was easily distracted by even minor extraneous stimuli. Recently, however, his impulsivity and attention problems at school worsened. Nolan couldn’t seem to resist the urge to blurt out funny comments during class, make rude noises, disrupt classmates’ activities, and perform various stunts or pranks (e.g., attempting to climb out the classroom window onto the building’s roof; releasing the class’ pet turtles in the bathroom). Most salient was Nolan’s frequent laughs, giggles, and chuckles, sometimes for no apparent reason.
None of Nolan’s antics were deliberately malicious or disrespectful to others. His teacher commented, “When I reprimand Nolan, he’s very apologetic. He’s a good boy deep down, it’s just that he loses control a lot.”
Nolan’s mother reported a similar exacerbation with his behavioral and emotional regulation at home. Approximately three months ago, Nolan began experiencing increased problems attending to his schoolwork, remaining seated at dinner, and carrying on quiet conversations with family members. “He began talking very rapidly—so fast that we often had to ask him to repeat himself,” recalled his mother. “He was like a recording being played at twice the speed. It was also sometimes difficult for us to follow his train of thought. He’s always had trouble staying on topic, but now it was worse than usual. It was like he couldn’t focus at all.”
Most problematic was a change in Nolan’s sleep. He would resist going to bed at his usual time, claiming that he was not tired. His mother reported, “I caught him playing on his iPod, assembling Legos, or coloring several hours after he was supposed to be asleep. When I told him to go to bed, he became very upset and cried for an hour in his room claiming that he couldn’t.” Nolan also woke early in the morning, approximately two or three hours before the rest of his family. Although he averaged only 4 or 5 hours of sleep each night, he never reported fatigue.
Nolan’s change in sleep–wake cycle was accompanied by a change in mood. His energetic, high-rate behavior was sometimes peppered by instances of moodiness and irritability. “We noticed that little things would set him off,” recalled his stepfather. “I’d tell him to help with the dishes or to turn off the TV and eat dinner, and he’d become argumentative. On two occasions, he swore right in front of us, which he has never done before.” Nolan’s mother added, “He’s also had a couple of meltdowns: once after basketball practice when I told him that we didn’t have time to stay late, and once in the morning, when I told him that I wouldn’t drive him to school and he needed to take the bus. Nolan screamed, kicked at the walls and furniture, and generally behaved like a 2-year old. He didn’t settle down for hours and only because he was exhausted.”
Although Nolan was a young boy, he had an extensive psychiatric history. He was diagnosed with ADHD at age 6. His symptoms were managed relatively well with stimulant medication, although he still showed overactivity at school and problems sustaining attention on homework. Nolan also had a history of major depression, during his parents’ separation and divorce when he was 7. His depressive episode lasted approximately nine months and was characterized by sadness, a lack of interest in play and sports, social withdrawal, and extreme irritability and temper tantrums. The episode resolved without treatment.
More recently, Nolan began reporting problems with chronic worrying: about school, friends, sports, his family—all sorts of topics. His increase in worrying was accompanied by more frequent headaches, stomachaches, and other vague physical complaints that sometimes caused him to miss school. Nolan’s problems with anxiety predated the onset of his sleep problems by approximately one year. An SSRI, prescribed by his pediatrician, reduced the frequency of his worrying, but seemed to exacerbate the severity of his hyperactivity, impulsivity, and inattention. His parents also noticed that the medication immediately preceded the onset of Nolan’s antics at school.
During an interview, Nolan’s mother reported longstanding problems with generalized anxiety, recurrent panic attacks, and depression. She also admitted to a history of alcohol use problems. She continued to participate in Alcoholics Anonymous meetings to maintain sobriety. Nolan’s biological father has a history of bipolar disorder that required hospitalization on two occasions because of self-injury during manic episodes.
During an initial (albeit brief) interview with the school psychologist, Nolan said that he was sorry for disrupting class. He had problems remaining seated, was repeatedly distracted by noises and other activity in the hallway outside the office, and talked very rapidly. Nolan denied feelings of sadness and described his mood as “good.” When asked if he had noticed a change in his behavior in the past few weeks, Nolan responded, “I guess so. I never used to get into so much trouble.”
1. What DSM-5 disorder best describes Nolan’s behavior?
Bipolar I disorder
2. How does Nolan meet DSM-5 diagnostic criteria for this condition?
Nolan is likely experiencing a manic episode, the essential feature of bipolar I disorder. Mania is characterized by the following:
- A distinct period of abnormal and persistently elevated, expansive, or irritable mood and abnormal and persistently increased goal-directed activity or energy lasting at least 1 week. Nolan’s mood is predominantly elevated and irritable and he clearly shows increased activity above and beyond his history of ADHD.
- During the episode, Nolan shows the following signs/symptoms:
- decreased need for sleep
- more talkative than usual
- flight of ideas (although we would need additional information to confirm)
- distractibility
- increased activity or agitation
- The disturbance causes impairment (at home and school).
- It is not attributable to the effects of a substance.
It appears that the SSRI exacerbated Nolan’s manic symptoms. DSM-5 allows individuals to be diagnosed with bipolar I disorder if symptoms emerge after antidepressant treatment as long as symptoms persist after treatment is discontinued.
3. If Nolan did not have a history of major depression, could he still receive the same primary diagnosis that you assigned in question #1 above?
Yes. The essential diagnostic criterion for bipolar I disorder is a manic episode. Although most people with bipolar I disorder also experience episodes of depression, depressive episodes are not required for the bipolar I diagnosis.
4. Why doesn’t Nolan meet diagnostic criteria for bipolar II disorder?
Nolan fails to meet diagnostic criteria for bipolar II disorder because
- the duration of his manic symptoms exceed four days and
- His signs/symptoms have caused impairment at home and school.
5. Is there evidence that Nolan exhibits psychotic features during his mood disturbance?
The most common psychotic features shown by individuals with bipolar I disorder are delusions and hallucinations. There is no evidence in the scenario to support the presence of these features, although the psychologist would want to assess whether they occur. The presence of psychotic features is associated with a poorer prognosis and a possible need for medication to address these features.
6. Is there evidence that Nolan exhibits mixed features in his mood disturbance?
Mixed features are characterized by the presence of subthreshold depressive symptoms during a manic episode or subthreshold manic symptoms during a depressive episode. Although Nolan is currently experiencing a manic episode, the only depressive symptom that he shows (at home) is irritability. Because irritability is also a symptom of mania and is not unique to depression, there seems to be little evidence of a mixed mood episode.
7. Can Nolan also be diagnosed with ADHD?
Yes, approximately 70% of children with bipolar I disorder also have ADHD. Mania and ADHD have several diagnostic features in common: talkativeness, distractibility, and excessive motor activity. In Nolan’s case, these problems exist above and beyond his usual ADHD signs and symptoms, and they occur alongside an elevated and irritable mood, general silliness and disruptive behavior, and decreased need for sleep. Consequently, he seems to have both ADHD and bipolar I disorder.
8. Why is disruptive mood dysregulation disorder (DMDD) probably not the best diagnostic label for Nolan?
DMDD is characterized by (1) recurrent and severe temper outbursts that are out of proportion to the provocation or situation, and (2) persistently irritable or angry mood between temper outbursts. Furthermore, the duration of symptoms must be 12 months or longer and the outbursts must occur, on average, three or more times per week.
Nolan does show temper outbursts, but their frequency does not seem to meet the requirement of three or more times per week. Furthermore, Nolan shows some signs of irritability, but his mood problems are episodic rather than chronic and they exist alongside other manic symptoms such as distractibility, talkativeness, and decreased need for sleep. His other manic symptoms and their episodic (rather than chronic) nature suggests bipolar I disorder rather than DMDD.
9. Based on the results of the Course and Outcomes of Bipolar Youth (COBY) study, what is Nolan’s prognosis if he participates in treatment?
Most youths in the COBY study recovered with an average time to recovery of approximately two years. Unfortunately, within 1½ years of recovery, most youths experienced another mood episode (usually depression). Even after recovery, most youths continued to experience subthreshold mood problems, such as sadness, irritability, or insomnia.
10. What medications might be effective for Nolan?
Most physicians would recommend either a mood stabilizing medication like lithium (Eskalith) or an atypical antipsychotic medication like aripiprazole (Abilify) to manage Nolan’s current manic episode. Youths with bipolar I disorder are more likely to respond to atypical antipsychotics than lithium, although both medications are effective and frequently prescribed for this condition.
Most physicians would treat Nolan’s ADHD symptoms after his mood is stabilized. Stimulant medication is usually the treatment of choice for ADHD. Antidepressant medications, especially SSRIs, can exacerbate manic symptoms (as was the case for Nolan) and must be used cautiously.
11. What psychosocial treatments might you recommend for Nolan and his parents?
Two evidence-based psychosocial treatments are effective for children with bipolar I disorder, when used in combination with medication.
Child- and Family-Focused CBT is designed for youths 7 to 13 years of age and their caregivers. It has three components: (1) emotional monitoring and regulation, (2) improving parent–child interactions, and (3) managing disruptive child behavior.
Psychoeducational Psychotherapy (PEP) is designed for youths 8 to 12 years of age with mood disturbances, and their caregivers. It can be administered to individual families or to groups of families together. It teaches families about depressive and bipolar disorders and fosters emotion-regulation and problem-solving skills.
Weis, R. (2017). Introduction to Abnormal Child and Adolescent Psychology, Third Edition . Thousand Oaks, CA: Sage
God’s Servant
Adolescence-Onset Schizophrenia
Our patient was an unidentified adolescent girl brought to the emergency department of the hospital by the police after receiving lacerations from a physical altercation with a homeless man in a city park. An initial mental status examination indicated that the girl was not oriented to time or place; furthermore, she refused to provide her name or other identifying information. Instead, the girl remained largely unresponsive, lying in the hospital bed, wrapped in blankets and curled into a ball like a pill bug. Witnesses saw the girl attempting to care for homeless adults in the park. Although one man resisted her help, the girl insisted on providing it. One thing led to another, a fight ensued, and the girl sustained minor injuries to her arms and right leg.
Identification found in the girl’s coat revealed that her name was Julianna McCall, a 16-year-old high school student from a nearby, affluent suburb. Her parents were contacted, immediately drove to the hospital, and provided additional background information.
Julianna had disappeared approximately 24 hours earlier. Her parents were surprised when she did not come home immediately from school on Friday afternoon, because she seldom left the house and never socialized with friends on weekends. After several hours, they filed a police report, organized an informal search, and spent the night worried sick about their daughter.
Julianna was born full term. Although her gestation and delivery were unremarkable, she showed delays in gross motor, fine motor, and expressive language skills. By the time she began school, however, she had largely caught up with her peers. Throughout primary school, she was generally well liked, earned average grades, and participated in several extracurricular activities such as swimming, 4-H, and horseback riding.
Julianna showed problems transitioning to high school, however. She became more “moody” at home and began spending less time with her parents and younger siblings. She dropped out of many activities, except for horseback riding (which she loved), and withdrew from her former friends. By her sophomore year in high school, Julianna was a recluse. She would usually come home from school, lock herself in her room, and occupy her time watching movies or perusing social media. Her grades in school plummeted. Her parents met with the school guidance counselor who suggested that Julianna’s difficulties reflected “typical adolescent adjustment problems.”
Not so. Within the last few months, Julianna’s functioning changed dramatically. She began refusing to go to school, rarely left her room upon returning home, and never interacted with family members. Her teachers described her as “withdrawn and emotionally distant” at school. On at least two occasions, she missed entire school days, hiding in the school bathroom or a supply closet.
Perhaps more concerning was Julianna’s increased preoccupation with religion. Although her family was religious, Julianna spent much of her time praying. When she did talk to others, she made comments about “saving her soul” and “resisting the devil” and “helping God’s children.” Her speech was noticeably rapid and her train of thought became difficult to follow. Once, her father directly confronted her about her preoccupation with praying. Julianna responded in an angry manner, claimed that he would not lead her astray from her “work,” and that she was “God’s servant.”
Julianna was admitted to the hospital for observation. The next day, she was responsive and answered questions from the psychologist. In a lethargic and unemotional manner, she reported that she went to the park “to help the homeless men and women as expiation for her sins.”
“What did you do that was sinful?” asked the psychologist.
“Everything I do is sinful,” Julianna replied. “That is what he tells me. That’s what he’s telling me now.”
“You hear a voice now?” asked the psychologist.
After a long pause, with downcast eyes, Julianna explained. “It’s more like a raspy whisper. Right now it’s quiet but it gets louder sometimes.”
“What does it say?” asked the psychologist.
“It says,” Julianna paused and then continued, “It says that my soul is evil, that others can smell its evilness, and that I am going to go to hell.”
“Whose whisper is it?” asked the psychologist.
For the first time during the interview, Juliana looked into the psychologist’s eyes, allowed a small tear to trickle down her cheek, and answered, “The devil’s.”
1. What DSM-5 disorder best describes Julianna’s behavior?
Schizophrenia
2. How does Julianna meet diagnostic criteria for this condition?
- She experiences the following signs/symptoms during a 1-month time period:
- Delusions of grandiosity (that she has a special calling from God) and possible delusions of persecution (that she is being tormented by the devil)
- Auditory hallucinations
- Disorganized speech (rapid, sometimes derailed or incoherent)
- Social withdrawal with brief catatonic behavior
- Negative symptoms (irritability, anger, limited emotional expression)
- She shows marked deterioration in academic and social functioning at home and school.
- Signs and symptoms (including prodromal signs/symptoms) have lasted at least 6 months with at least 1 month of active symptoms (e.g., delusions/hallucinations).
- Not better explained by another psychotic disorder (although this would need to be confirmed by further assessment)
- Not attributable to the effects of a substance (although, again, we would need additional information to confirm that this criterion is met, but there is no mention of substance use in the scenario)
- Not explained by other psychiatric disorder such as autism spectrum disorder or a communication disorder
A clinician might also specify “first episode, currently in acute episode” because this appears to be Julianna’s first psychotic episode.
3. Many youths show premorbid or prodromal signs and symptoms prior to their first psychotic episode. What premorbid or prodromal signs and symptoms did Julianna experience?
Premorbid: She showed motor and speech delays in infancy and toddlerhood. She also displayed moderate deficits in academic skill acquisition in elementary school. Often, youths who develop schizophrenia show below-average cognitive abilities, although the scenario only mentions “average” grades in primary school.
Prodromal: Approximately one to two years prior to her current psychotic episode, Julianna experienced a marked deterioration in her academic and social-emotional functioning. Behaviors included problems with attention and concentration at school, a marked drop in grades, moodiness and irritability, withdrawal from friends, and reduced interest in extracurricular and social activities with friends and family.
4. What is Julianna’s prognosis?
Julianna’s prognosis is variable. The outcome of youths with schizophrenia can be predicted based on three factors:
- Age of onset: Individuals with later age of onset are more likely to recover than individuals with earlier age of onset. Julianna’s age of onset (16) is somewhat early; less than 15% of individuals who develop schizophrenia experience their first psychotic episode prior to age 18 years.
- Duration between the onset of prodromal symptoms and treatment: On average, prognosis is best when prodromal symptoms are recognized and treatment is administered before the initiation of an acute psychotic episode. In Julianna’s case, the prodromal signs/symptoms of her illness were not recognized prior to her psychotic episode. However, her hospitalization (although unfortunate) will enable her to access treatment, thus improving her prognosis.
- The presence of positive symptoms: Julianna presents with predominantly positive symptoms of psychosis (e.g., delusions, hallucinations). Individuals with predominantly positive symptoms often show better prognoses than individuals with predominantly negative symptoms because positive symptoms respond better to antipsychotic medication than do negative symptoms, on average.
5. What two brain pathways are implicated in schizophrenia?
Excessive dopaminergic activity in the mesolimbic pathway is believed to underlie many of the positive signs/symptoms of schizophrenia. In contrast, underactivity of the mesocortical pathway is believed to be responsible for many of the negative signs/symptoms of schizophrenia.
6. What is attenuated psychosis syndrome? Did Julianna meet diagnostic criteria for this condition immediately prior to her first psychotic episode?
Attenuated psychosis syndrome is a DSM-5 condition for future study. It is diagnosed in youths who experience the first signs and symptoms of psychosis, before the onset of a full-blown psychotic episode. To be diagnosed, the individual must show at least one of the following:
- delusions or delusional ideas,
- hallucinations or perceptual abnormalities, or
- disorganized speech or communication.
One or more of these features must occur at least once per week for at least 1 month and have worsened in the previous year. Furthermore, they must have caused enough distress or impairment for their family members to seek help.
It appears that Julianna met criteria for attenuated psychosis syndrome. She likely exhibited delusional ideas about God and the devil (as evidenced by her preoccupation with religion), showed speech and thought problems at home and at school, and was referred to the guidance counselor because of impairment in academic and social functioning. Unfortunately, she was not identified as being in a prodromal stage and did not receive treatment at that time.
It is noteworthy that the developers of DSM-5 included attenuated psychosis syndrome so that clinicians might be better able to identify and treat the early signs/symptoms of psychosis in youths like Julianna, and to encourage additional research. The developers listed attenuated psychosis syndrome as a “condition for future study” rather than as an official diagnosis because of limited empirical data regarding the emergence of schizophrenia in children and adolescents and to avoid potentially stigmatizing youths with this diagnostic label who might not develop a psychotic disorder.
7. Is medication effective to help youths like Julianna? What are some limitations of medication as a first-line therapy?
Results of the Treatment of Early-Onset Schizophrenia Spectrum Disorders (TEOSS) Study showed that youths with schizophrenia respond to both conventional and atypical antipsychotics. On average, approximately 20% to 34% respond to these medications. Furthermore, neither class of medication seems to be superior. Usually, atypical antipsychotics are prescribed as a first-line treatment because they are associated with fewer side effects.
Side effects for conventional antipsychotics include extrapyramidal side effects (especially motor problems), tardive dyskinesia, sedation, and in rare instances neuroleptic malignant syndrome. The most common side effects associated with the atypical antipsychotics are sedation and weight gain.
8. How might psychotherapy be used to help Julianna and her family?
Although medication is considered the first-line treatment for psychotic disorders in youths, nearly all practitioners also recommend psychotherapy for youths and their families. Psychosocial interventions might include the following components:
- psychoeducation about schizophrenia and medication,
- helping families increase the youth’s adherence to medication,
- cognitive–behavioral interventions to improve coping skills and reality testing,
- communication skills training to reduce expressed emotion in the family, and
- rehabilitation and integration back to the community (e.g., school, peers).
Chapter 15: Feeding and Eating Disorders
Nothing by mouth.
Avoidant/Restrictive Food Intake Disorder (ARFID)
Demarco Johnson was a beautiful baby who was born approximately five weeks premature. His mother had a difficult pregnancy, marked by preeclampsia beginning at 32 weeks gestation. She experienced high blood pressure, severe headaches, and recurrent nausea and weight loss. She needed to be hospitalized and delivered Demarco early. Demarco was 5 lbs., 2 oz. at birth (low birth weight) with low blood oxygen levels.
After Demarco was medically stable, his mother attempted to feed him by breast and bottle. Although he was able to latch onto the nipple, his suck reflex was very weak and he was unable to ingest sufficient nutrition. After 2 days of attempted feeding, his mother, nurses, and lactation expert grew more worried about his ability to eat. Mrs. Johnson, in particular, recognized the importance that a premature baby like Demarco gain weight and she grew increasingly frustrated and angry with his passivity. By the time Mrs. Johnson was scheduled to be discharged, the nurse had written NPO in large letters on Demarco’s patient board. The abbreviation stood for the Latin words nil per os (“nothing by mouth”).
Demoralized, Mr. and Mrs. Johnson reluctantly agreed to feed Demarco by a NG (nasogastric) tube, that is, a long tube that delivers nutrients through the baby’s nostrils, down his esophagus, and into his stomach. When Demarco failed to gain sufficient weight by his 1-month checkup, his parents agreed to switch to a more permanent G (gastric) tube that delivered food directly into Demarco’s stomach though a button-like opening on his abdomen. Although Demarco remained at approximately the 15th percentile for weight, he was able to ingest sufficient nutrition through this method.
The main drawback with Demarco’s G tube was that he never learned to eat solids. When he was 6-months old, his parents attempted to feed him liquefied and pureed foods orally: rice cereal with formula, apricots, peas, applesauce. Demarco resisted everything. Initially, he accepted food into his mouth, but then thrust the food out with his tongue. When his parents insisted that he eat, Demarco became obstinate. He would arch his back, turn his head, flail his arms, and cry uncontrollably. If he ingested a little, Demarco would gag or spit up. Eventually, the mere sight of the spoon, bowl, and bib caused him to panic.
Now a 30-month-old toddler, Demarco continues to receive nearly all his nutrients and fluids by G tube. He continues to lag behind other toddlers in weight (26 lbs.). His pediatrician recommended surgery and behavior therapy to help wean him off the G tube, but his parents are not sure he (or they) are ready.
1. What DSM-5 disorder best describes Demarco’s eating behavior?
Avoidant/restrictive food intake disorder (posttraumatic feeding)
2. How does Demarco’s resistance toward solid foods illustrate Chatoor’s (2009) transactional model for feeding disorders?
According to the transactional model, feeding disorders develop in the context of caregiver–infant interactions. Demarco’s initial problems sucking and swallowing likely elicited anxiety and frustration in his parents. These negative emotions, in turn, may have caused them to be excessively demanding or intrusive during feeding and exacerbated his feeding problems. Although neither infant nor parents are to blame, the infant’s feeding problem reflects the gradual unfolding of these interactions over time.
3. How might classical conditioning be used to partially explain Demarco’s refusal to eat solid foods?
Demarco missed the sensitive period during which most infants develop the capacity to ingest solids, usually between 6 and 12 months. Consequently, he never learned to inhibit a prominent tongue thrust, to accept food of different tastes and textures into his mouth, and to swallow solids. When presented solids at 30 months, he coughed, gagged, or vomited. Through classical conditioning, he associated solid foods with these negative experiences. He has also generalized these conditioned responses to stimuli associated with eating, such as his bowl, spoon, and bib.
4. How might negative reinforcement be used to partially explain Demarco’s refusal to eat solid foods?
Demarco has learned that by refusing solid foods, he can avoid coughing, gagging, and vomiting. He also has low motivation to recognize hunger signals and accept solids, because his nutrition is provided by his G tube. Consequently, his food refusal is maintained over time.
5. How might extinction be used to treat Demarco?
Treatment of posttraumatic feeding is similar to the treatment of PTSD. The individual must be presented with the stimulus that elicits the negative emotional reaction (solid foods) and must not be allowed to escape the presentation. Over time and with repeated exposures, the negative emotional reaction will decrease in severity.
6. How might a behavior therapist help Demarco and his parents overcome his problem with feeding?
The book outlines components of behavior therapy for ARFID. These components include the following:
- Appetite manipulation: A physician will reduce the amount of nutrients Demarco receives from his G tube. Hunger will increase his motivation to accept solids.
- Contingency management: The therapist uses escape conditioning in which Demarco is presented with food on a spoon, the spoon is not withdrawn until he accepts the food, and physical guidance is used to increase his acceptance. Reinforcement (e.g., access to toys, movies) is contingent on acceptance. Time out (e.g., screening) is used if Demarco continues to refuse solids.
- Parent counseling: The therapist teaches parents to implement the contingency management program, to avoid negative interactions that might exacerbate Demarco’s food refusal, and to manage parents’ own stress as caregivers to a child with special medical needs.
Chatoor, I. (2009). Diagnosing and treating feeding disorders. Washington, DC: National Center for Clinical Infant Programs
The Apple Doesn’t Fall Far
Anorexia Nervosa
Miranda Richeson, a 16-year-old girl, was referred to our eating disorders clinic for assessment and inpatient treatment. Two days ago, Miranda had passed out during physical education class, apparently from dehydration. The hospital report indicated that Miranda was significantly underweight compared to girls her height and age, lacked sufficient hydration, and had an electrolyte imbalance. After she was medically stable, they released Miranda to her mother’s supervision and set up an intake appointment at our clinic.
Miranda presented as an extremely attractive, well-kempt girl. Perhaps her most striking features were her height (5’ 8’’) and stylish clothes that hung on her frame. Although Miranda reported her mood as “fine,” her general disposition seemed to be one of irritability. She resented being questioned by the psychologist. Miranda tended to answer questions using curt, one- or two-word utterances with her eyes fixated on some unseen object on the floor. Occasionally, she glanced at the psychologist, narrowing her eyes with a mixture of scorn and contempt. Her speech suggested above-average intelligence and ample vocabulary, supporting her mother’s report that she was an honors student. Thought contact focused largely on her desire to leave the treatment facility and return home, feelings of anger toward her mother who insisted that she receive treatment, and preoccupation with friends “back home.” When asked specifically about her weight, Miranda reported a preoccupation with her appearance and a desire for perfection. Her insight was poor; although Miranda recognized the need for medical treatment after she passed out during school, she said inpatient treatment was “a big waste of time and money.” Nevertheless, Miranda agreed to a “trial run” at the facility for 2 weeks.
Miranda eventually admitted to a history or bingeing and purging beginning approximately two years ago, when she was 13. At that time, she had moved from her local public junior high school to a new, private college preparatory school near her mother’s workplace in the city. Although Miranda was an excellent student and had many friends at her old school, she initially had difficulty performing well academically and fitting in socially.
Miranda began dieting in order to lose weight. Although she was never overweight, she often felt guilty when she would indulge in forbidden foods such as pizza, ice cream, and chocolate. Unfortunately, Miranda lacked the willpower to sustain her diets for long. After breaking a diet, she would give in to despair, indulge, and regret her weakness later. Several of her new friends introduced her to purging as a mean to avoid weight gain. Miranda soon learned that purging not only allowed her to avoid gaining weight, it also allowed her to reduce feelings of guilt for occasionally indulging in her favorite foods. Eventually, she developed a pattern of bingeing and purging that occurred several times per week. She felt out of control, emotionally vulnerable, and guilty for hiding her bingeing and purging from her family.
Miranda’s parents knew Miranda had an eating problem, but they never raised their concerns with her. Mrs. Richeson had a history of bulimia beginning in college. “I could see myself in Miranda,” she said. “All of the insecurity, the need for perfection, the lack of control. I felt that way for years. Some of her eating habits are probably my fault. Before I got help, I used to always diet and was obsessed with calories. It probably rubbed off on Miranda.”
1. What DSM-5 disorder best describes her behavior?
Anorexia nervosa, binge eating/purging type
Note: We would need to calculate Miranda’s BMI to confirm this diagnosis and determine its severity.
2. How does Miranda meet diagnostic criteria for that disorder?
- Miranda restricts energy intake causing significantly low body weight for her gender and age.
- She likely has a fear of gaining weight and she engages in bingeing and purging behavior despite her low weight.
- Her shape/weight has undue influence on her self-evaluation.
3. How might a clinician differentiate between the various eating disorders?
Miranda has anorexia nervosa because she exhibits significantly low body weight. Significantly low body weight differentiates anorexia nervosa from the other eating disorders.
Bulimia nervosa is characterized by binge eating and some compensatory behavior to avoid weight gain. Miranda shows both bingeing and purging. However, she is not diagnosed with bulimia nervosa because she meets diagnostic criteria for anorexia nervosa. DSM-5 does not allow individuals to be diagnosed with bulimia nervosa if they also meet criteria for anorexia nervosa because anorexia nervosa is believed to be the more serious condition.
Binge eating disorder is characterized by binge eating without some compensatory behavior to avoid weight gain. Because Miranda purges, she does not meet criteria for binge eating disorder.
4. Identify several health-related problems that Miranda may experience because of her maladaptive eating behavior.
Problems include malnutrition, dehydration, electrolyte imbalance, cardiac arrhythmia, hypokalemia, osteopenia, growth suppression, lanugo, and problems associated with purging (e.g., dental enamel erosion, enlarged salivary glands, Russell’s signs).
5. How might a psychologist use the cognitive–behavioral model for eating disorders to explain the cause and maintenance of Miranda’s problematic eating?
The text presents the cognitive–behavioral theory for bingeing and purging (see below). Miranda likely inherited a genetic risk for developing eating problems or psychological distress. She also seems to overvalue a slim body shape or low body weight.
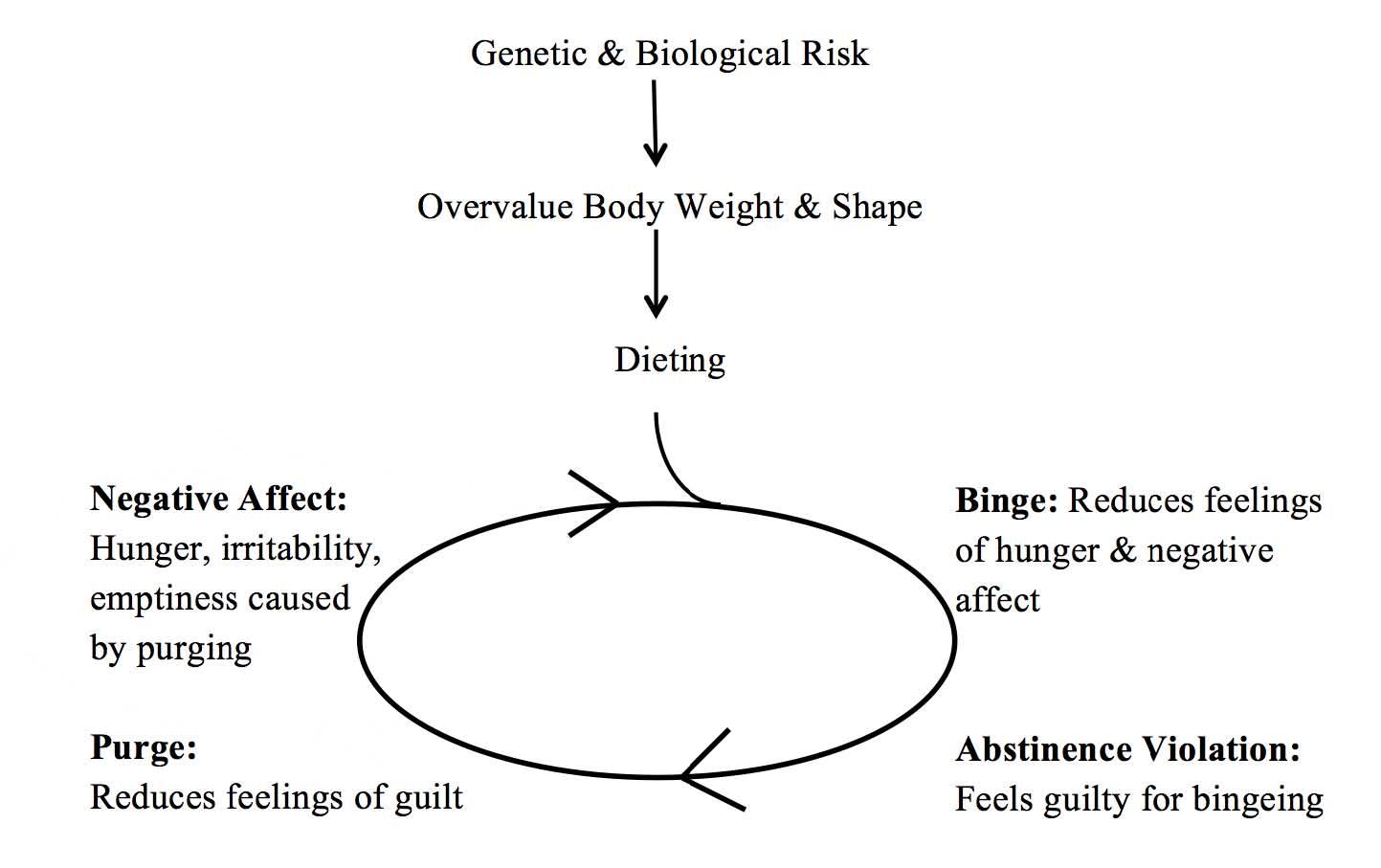
Her maladaptive eating behavior began when she dieted to lose weight or avoid weight gain. Dieting caused feelings of hunger, irritability, and emptiness. Breaking her diet (and bingeing) temporarily reduced these feelings and is maintained by negative reinforcement. However, breaking her diet (and bingeing) elicits feelings of guilt. Purging temporarily reduces feelings of guilt because it allows Miranda to avoid weight gain and is maintained by negative reinforcement. However, purging elicits feelings of hunger, irritability, and emptiness. The cycle, therefore, continues with binging negatively reinforced by a reduction of hunger and negative affect and purging negatively reinforced by a reduction of guilt and fear of weight gain.
6. How might a psychologist use the tripartite influence model to explain the cause and maintenance of Miranda’s problematic eating?
The text describes the tripartite influence model, a social–cultural theory for the emergence of eating disorders. This model identifies three factors that can contribute to eating problems in adolescents: (1) parents, (2) peers, and (3) the media.
Miranda’s mother admitted that she has a history of maladaptive eating behavior and body image problems. Miranda may have inherited a genetic diathesis toward disordered eating behavior, anxiety, or psychological distress. Miranda’s mother also may have modeled maladaptive eating, emphasized a thin body, or inadvertently reinforced unhealthy eating in Miranda.
Miranda’s new classmates also may have modeled unhealthy eating habits, critiqued others’ body shape or weight, or reinforced an unrealistic “thin ideal” body. Miranda might have adopted unhealthy eating habits in a desire to achieve this unrealistic ideal and gain acceptance by these peers.
The model posits that unrealistic standards for thinness and beauty perpetuated by the media also contribute to the development of eating disorders. Although media influences are not described in the case study, it is reasonable that Miranda is a consumer of these influences, which could affect her desire for thinness and her eating behavior.
7. How might a psychologist use interpersonal theory to explain the cause and maintenance of Miranda’s problematic eating?
Interpersonal theory views eating disorders as a medical illness that typically arises because of (1) a genetic diathesis toward psychological distress and (2) an environmental stressor that elicits maladaptive eating. Although interpersonal problems do not cause eating disorders, they are often associated with their onset and maintenance over time. Specifically, eating disorders are associated with one or more of the following interpersonal problems:
- grief or loss
- role disputes
- role transitions
- interpersonal deficits
Miranda’s history of dieting, bingeing, and purging is associated with a major role transition: adjustment to a new college preparatory school. It is likely that problems adjusting to this new environment elicited negative affect which was reduced (in the short term) by maladaptive eating and acceptance by her new group of friends.
8. Identify one way a psychologist might help Miranda, according to (1) cognitive–behavioral theory, (2) the tripartite influence model, and (3) interpersonal theory, respectively.
Cognitive–behavioral theory: A psychologist might use exposure-based treatment to help Miranda. Miranda must consume increasingly greater amounts of food and avoid compensatory behaviors to reduce weight gain (e.g., purging). Over time, her anxiety about weight gain should decrease. This treatment is similar to exposure-based treatments for anxiety disorders. A therapist would also likely challenge maladaptive beliefs that contribute to Miranda’s unrealistic desires for perfection or thinness.
Tripartite-influence model: A psychologist might target any of the three factors believed to underlie maladaptive eating. For example, a therapist might encourage Miranda’s mother to avoid comments about her (or Miranda’s) body weight or shape.
Interpersonal theory: A psychologist might help Miranda mourn the loss of her old school and peer group, and then facilitate her transition to her new school. A critical component of treatment might be to help Miranda establish a network of friends who will not model and reinforce unhealthy eating.
Chapter 16: Health-Related Disorders and Pediatric Psychology
Lawrence: a little late.
Enuresis (Polysymptomatic)
“My son has a problem controlling his bladder.” That is how Mrs. Handler began our first session.
She continued, “I thought I might explain the situation to you first, before you interview Lawrence himself. He’d probably be very embarrassed if he was in the room with us.”
“Lawrence is 10-years-old. He’s a great kid. He’s excellent in just about any sport he plays. He’s extraverted, has an infectious smile, and loves to play with his little brothers. The only problem is his accidents.”
“Tell me about them,” I said.
Mrs. Handler continued, “My husband and I call him ‘Little Late Larry.’ He’ll be playing a game, or watching TV, or doing something else in the house. Then, he’ll get this sudden urge to go. He’ll rush over to the bathroom and not make it in time. The funny thing is, when he does wet himself, he doesn’t tend to go very much.”
I asked, “Do you mean he doesn’t void much urine when he has an accident?”
“Yes. Well sometimes he does. But usually it’s just enough that it is noticeable.”
“Does he wet at night too?” I asked.
“Yes. He wets about two or three nights a week. We’ve tried to use a urine alarm to get him to stop, but it hasn’t helped. Lawrence wakes up when he wets the bed even without the alarm.”
I asked, “And at night, when he has an accident, does he also void only a little amount of urine or does he soak the bed?”
Mrs. Handler responded, “It’s usually just enough to wake him up. He’s such a good kid, he runs to the bathroom and empties whatever is left. He even helps us clean up. Bill (his father) and I let him wear disposable underpants to help manage.”
I commented, “If it’s OK with you, I’d like to talk with Lawrence to get his perspective on this problem. I’d also like to talk with his pediatrician, to make sure there’s no medication or illness that might be contributing to this problem. How does that sound?”
1. How does Lawrence meet DSM-5 diagnostic criteria for enuresis?
- Lawrence shows repeated voiding of urine into his bed and clothes.
- Frequency is at least twice weekly for at least 3 months or it causes distress/impairment in functioning.
- He is > 5 years old.
- His bedwetting is not attributable to a substance (medication) or general medical condition.
(Note that we would need to confirm the last criterion by consulting Lawrence’s pediatrician.)
2. When does bedwetting become a disorder that merits treatment?
- indicates that bedwetting becomes a disorder when (1) it is developmentally unexpected (i.e., > age 5 years), and (2) it occurs frequently ( > twice weekly for > 3 months) OR causes distress or impairment.
3. What kind of enuresis does Lawrence likely have? Why is knowing his kind of enuresis important?
Lawrence likely has polysymptomatic nocturnal enuresis (PSNE). Youths with PSNE tend to wet the bed throughout the night, void small amounts of urine when they wet, and wake after wetting. These youths also typically wet during the day and report sudden urges to void. PSNE is often associated with bladder instability or low functional bladder capacity. In contrast, monosymptomatic primary enuresis (MPE), the kind experienced by most youths, is associated with failure to respond to a full bladder. Whereas urine alarm training is highly effective for MPE, it is often less effective for PSNE. (A case of MPE is presented in the textbook.)
4. Approximately how many children Lawrence’s age experience enuresis?
In any given year, approximately 4.5% of children ages 8 to 11 years have enuresis. Prevalence is higher in boys (6.2%) than in girls (2.5%).
5. What are the two primary causes for Lawrence’s type of nocturnal enuresis?
Approximately one third of youths with PSNE have bladder instability; that is, they have involuntary bladder contractions during sleep that make them void small amounts of urine. They usually wake up when they void.
Some youths with PSNE have small functional bladder capacities; that is, they cannot hold as much urine before they experience an urge to void.
6. Lawrence also wets during the day. Why do most boys show daytime wetting?
Lawrence may wet during the day because of bladder instability. However, most boys who wet during the day engage in voiding postponement; that is, they become engrossed in other activities and hold urine too long until they wet involuntarily.
7. Imagine that you were Lawrence’s therapist. Outline a psychosocial treatment plan to decrease his daytime wetting.
A treatment plan might have the following components, each described in the text:
- consultation with Lawrence’s pediatrician to rule out a medical illness or medication as a cause of his enuresis;
- scheduled bathroom breaks during the day, to reduce voiding postponement (if necessary) and recognize feelings of a full bladder;
- Kegel exercises, to strengthen pelvic floor muscles and increase retention; and
- retention control training and overlearning, to increase functional bladder capacity.
8. What medication might be used to treat Lawrence? What are the limitations of medication to treat enuresis?
Approximately 25% to 60% of youths who receive desmopressin (DDVAP), a synthetic vasopressin, are able to stay dry while taking the medication.
Atomoxetine (Strattera) can increase arousal in some children with nocturnal enuresis and help them respond to sensations of a full bladder. This medication may not be effective for Lawrence, however, who seems to wake when he wets at night already.
Oxybutynin (Ditropan) is an antispasmic medication that can reduce involuntary bladder contractions in children with diurnal and nocturnal enuresis.
Unfortunately, relapse is high with these medications; only 15% to 20% of youths continue to stay dry at night after discontinuing them.
An Embarrassing Problem
Encopresis (Primary)
Brad was referred to our outpatient clinic by his school guidance counselor. Brad, a cute fourth-grader, was having problems with teasing.
“To put it bluntly, Brad has fecal incontinence,” the guidance counselor explained. “He often smells very badly, but I don’t think he’s even aware of it. The more polite kids in his class simply avoid him. The less polite kids make fun of him behind his back.”
One week later, Brad’s mother met with me in my office. She explained the situation.
“It’s ironic. Brad’s always had problems with constipation. As a preschooler, I’d need to use laxative suppositories to help him go. His stool would be very hard and it would be so painful. He’d sit on the toilet and cry. He began avoiding the toilet, probably because he hurt so much.”
“So what’s the problem now?” I asked.
She responded, “Now, it’s the opposite problem. Brad has accidents throughout the day, almost every day. It’s usually just a little bit, but it’s watery and,” she paused, “it doesn’t smell so good.”
I questioned, “So what have you tried to do to solve the problem?”
She replied, “At first, I tried over-the-counter medication for diarrhea. That didn’t work at all. I actually think it made the problem worse.”
“Then,” she continued, “I tried rewarding him for each day he didn’t have an accident, but there were so few of them. Then, I started punishing him—taking away privileges—whenever he had an accident. But, honestly, this just made him upset and didn’t correct the problem. I think he’s just gotten in the habit of having these accidents. He doesn’t seem to even realize when he has to go. He doesn’t seem to care.”
I commented, “It sounds like Brad has a really common, but really embarrassing, problem. His colon is stretched out and flabby, like a boxer who’s taken a beating for many years and is now old and out of shape. We need to get it back into shape so that it can do its job.”
Brad’s mother replied, “OK. Whatever it takes.”
1. How does Brad meet DSM-5 criteria for encopresis?
- He engages in the repeated passage of feces into inappropriate places, whether voluntary or unintentional.
- He defecates inappropriately each month for at least 3 months.
- He is at least 4 years of age.
- His behavior is not attributable to a substance or medical condition besides constipation. (Note that we would need to confirm that this criterion is met by consulting Brad’s pediatrician.)
2. When does soiling become a disorder that merits treatment?
Note that DSM-5 does not require distress or impairment for the diagnosis of encopresis. However, Brad is currently experiencing impairment in his social functioning because of this problem.
3. Does Brad show primary or secondary encopresis? Why is this distinction important?
Brad shows primary encopresis because it does not seem that he has learned to stay continent for an extended period of time. Youths with primary encopresis, like Brad, often benefit from systematic toilet training and other behavioral interventions. In contrast, youths with secondary encopresis might respond to interventions designed to improve coping skills or reduce psychosocial stress and/or oppositional behavior that might be associated with their soiling.
4. Approximately how many children Brad’s age experience encopresis? How many children with encopresis also have enuresis?
Approximately 3% of school-age children meet DSM-5 criteria for encopresis. Boys are 4 to 6 times more likely to have this condition than girls. Approximately 30% of youths with encopresis also have enuresis. Comorbid enuresis is often seen in children with encopresis caused by constipation. Constipation can put pressure on the child’s bladder, reducing functional bladder capacity and increasing his or her urge to urinate.
5. What is probably the cause of encopresis? (How might learning theory be used to explain Brad’s symptoms?)
Brad’s encopresis is probably caused by constipation with overflow incontinence. Through classical conditioning, Brad associated the toilet with painful elimination. Over time, he came to avoid toileting in order to reduce pain. His avoidance of the toilet was negatively reinforced and maintained over time through pain avoidance/reduction. Unfortunately, toileting avoidance caused constipation that reduced his sensitivity to a full bowel. Now, fecal matter has hardened into a mass in his colon. Liquid waste seeps around the fecal mass without Brad’s volition (or awareness). It is likely that Brad has no control over this fecal leakage.
Taking an over-the-counter medication for diarrhea probably exacerbated Brad’s problem by increasing his constipation. Punishing Brad for inappropriate soiling will also be ineffective because the leakage that Brad experiences is involuntary.
6. Imagine that you were Brad’s therapist. Outline a psychosocial treatment plan to decrease his encopresis.
A psychosocial treatment plan might have the following components, each presented in the text: (1) a medical evaluation to rule out an illness (besides constipation); (2) education; (3) medical treatment to clean Brad’s colon of constipated fecal matter, usually with a laxative; (4) scheduled toilet sitting with positive reinforcement; and (5) cleanliness training/response cost to reduce future accidents.
Why is it important to refer Brad to a pediatrician prior to psychosocial treatment?
It is important that a physician rule out a medical cause for Brad’s encopresis (besides constipation). Medical supervision is also necessary to clean Brad’s colon prior to psychosocial treatment.
Encopresis (Secondary)
David was a 7-year-old boy who was referred to our clinic for children with elimination disorders. One day each week, a team of psychologists and pediatricians met with children experiencing enuresis and encopresis and their families. We assessed children’s problems with elimination, arrived at a diagnosis, and provided recommendations for treatment so the family could get started correcting the problem right away. David was different from most of the kids we tended to see.
“The problem began about six months ago,” his mother explained. “I was doing the laundry in the basement of our house. I noticed a funny smell and then I saw it. Somebody had defecated in the middle of the pile of dirty clothes. I must have screamed or something. All of the kids came running – all except David. It didn’t take long to figure out who the culprit was.”
I asked, “Did this happen again?”
She continued, “I punished him pretty hard. He’s always been a bit of a troublemaker, but nothing like this! Everything was fine for a while, and then it occurred twice in one week. Well, to be honest, I only noticed his droppings twice in one week – I am not really sure when he left them. I found both of them in the basement, one in the basement shower (which we rarely use) and one in the closet that holds the hot water heater.”
“How did you respond?” I asked.
“I was livid,” she replied. “How could he do such a thing? I spanked him and took away all of his games and privileges. I was really worried he would start doing this at school!”
“Does he ever have accidents, like soil his pants or wet the bed?” I questioned.
She answered, “No. He’s never had problems with soiling or wetting like that. He’s a pretty healthy kid. I just don’t know what to do. I’ve got three kids at home and David’s the oldest, but he’s the one acting like a baby! It’s hard enough being a single mom and now I have to deal with this.”
“It sounds like you have a lot on your plate. You don’t have anyone who can help you?” I asked.
She replied, “Not since their dad left several months ago. I suppose I could ask my sister to help, but she’s got kids of her own.”
1. How does David meet DSM-5 diagnostic criteria for encopresis?
- He defecates inappropriately each month for at least 3 months. (Note that this would need to be confirmed by David’s mother.)
- His behavior is not attributable to a substance or medical condition besides constipation. (Note that we would need to confirm that this criterion is met by consulting David’s pediatrician.)
DSM-5 does not require distress or impairment for the diagnosis of encopresis. However, David’s behavior is currently causing distress to his family. It also may indicate problems with his psychosocial functioning.
3. Does David show primary or secondary encopresis? Why is this distinction important?
David shows secondary, nonretentive encopresis. David has been able to remain continent prior to this time. Furthermore, his encopresis is not caused by retention or constipation. Instead, it may be deliberate as suggested by evidence of defecation in specific places rather than on his clothes.
Youths with primary encopresis often benefit from medical treatment to reduce constipation and systematic toilet training. In contrast, youths with secondary encopresis, like David, might respond to interventions designed to improve coping skills or to reduce psychosocial stress and/or oppositional behavior that might be associated with their soiling.
4. Approximately how many children David’s age experience encopresis? How many children with encopresis also have enuresis?
5. What is the cause of David’s encopresis?
Only about 15% of youths with encopresis have nonretentive encopresis. Of these 15%, very few defecate inappropriately on purpose. Voluntary encopresis is usually associated with problems coping with a psychosocial stressor, such as a family disruption, hospitalization, or episode of maltreatment. The clinician might want to explore the possibility that David’s encopresis might be associated his parents’ separation
6. What other symptoms or comorbid disorders might you want to investigate in David?
Although this is unlikely, the clinician might assess whether David has evidence of constipation with overflow incontinence. If David’s encopresis is voluntary, the clinician might explore possible symptoms of oppositional defiant disorder or mood problems.
7. Imagine that you were David’s therapist. Outline a psychosocial treatment plan to decrease his encopresis.
Treatment for voluntary, secondary encopresis should address the psychosocial stressors associated with this behavior. For example, parent management training is effective for youths with oppositional defiant disorder whereas cognitive–behavioral interventions are effective for youths with depressive disorders associated with parental separation.
Enfamil and Insomnia
Insomnia Disorder in Infancy
“If I hear another mom talk about how her baby is sleeping through the night, I am going to scream!”
Mrs. Drumm brought her 1-year-old son, Benedict, to his pediatrician because of chronic insomnia. His pediatrician had examined Benedict and determined that there was nothing medically wrong with him. Consequently, she suggested that Mrs. Drumm seek out a psychologist to help with her son’s sleep problems.
Mrs. Drumm continued, “Every night it’s the same song-and-dance. He doesn’t want to go to sleep unless we carry him in our arms and feed him. When he was a newborn it was not a big deal. I would support him with my right arm and hold the bottle for him with my left. Then, when he got older he would insist on holding the bottle. But, when he starts to drift off, he drops the bottle and wakes up. Then, we have to start the whole routine again. Also, he’s getting to be so heavy . Do you see these?” Mrs. Drumm rolled up the sleeve of her right arm displaying her bicep. “Pretty nice arms for a 38-year-old woman don’t you think? The problem is my right arm’s bigger around than my left. And I can’t sit down. I need to hold him and feed him while walking around the room. If I stop walking or sit down, he wakes up again crying.”
“It sounds exhausting!” I said.
She continued, not seeming to hear my comment. “Then, when Ben wakes in the middle of the night, I have to do the same thing all over. He won’t go to sleep on his own.”
“What would you like to be different?” I asked.
Mrs. Drumm rolled her eyes and replied, “You’ve got to be kidding me? What do I want to be different? I want to get some sleep! I want this kid to sleep through the night like a normal kid his age. I’m too old for this.”
1. How does Ben meet DSM-5 diagnostic criteria for insomnia disorder?
- The presenting problem is inadequate quality of sleep characterized by difficulty initiating sleep without a caregiver’s intervention.
- The sleep problem causes significant distress (in mother) and disturbance in family functioning.
- Occurs > 3 nights per week.
- Present for > 3 months.
- The problem persists despite adequate opportunity to sleep.
- The problem is not better explained by another sleep–wake disorder.
- The problem is not attributable to a medication. (Note that we would need to confirm this with Ben’s pediatrician.)
- The problem is not better explained by another medical or mental disorder. (Again, we would need to consult Ben’s pediatrician to rule out a medical disorder that might explain Ben’s sleep refusal.)
2. When does a child’s sleep problem become a disorder that merits treatment?
DSM-5 requires significant distress or impairment for the diagnosis of insomnia disorder. Curiously, DSM-5 is not clear who must experience this distress or impairment: the child or the caregiver? For example, DSM-5 reads, “A diagnosis of Insomnia Disorder should be reserved for those individuals with significant daytime distress or impairment related to their nighttime sleep difficulties” (p. 364), which implies that the individual himself or herself must experience distress or impairment. However, most clinicians would believe that Ben merits treatment, given the distress and impairment his family is experiencing because of his sleep refusal.
3. At what age do most infants go to sleep on their own and sleep through the night? Is Ben’s behavior typical for a 12-month-old?
Insomnia also must be differentiated from developmentally typical patterns of sleep and wakefulness. For example, children less than 6 months of age are usually unable to sleep more than 6 hours at a time. The ability to soothe oneself to sleep, a skill that Ben lacks, develops between 5 and 7 months. By age 9 months, most infants can sleep in 6 to 8 hour durations. However, as many as 25% of 1-year-olds, like Ben, can’t fall sleep on their own or return to sleep independently.
4. How many hours of sleep should Ben get, if he is typically developing?
A 12-month-old infant like Ben should get approximately 12 to 14 hours each day including a daytime nap.
5. How might learning theory be used to explain Ben’s insomnia?
Ben’s parents have conditioned him to fall asleep when being held and fed by a bottle. Consequently, he is unable to achieve sleep when these environmental conditions are not present. Ben also lacks self-soothing skills—skills that typically develop between 5 and 7 months of age. Consequently, when he wakes during the night, he requires his parents to return to sleep.
Ben’s parents have positively reinforced his crying by responding to his bids for comfort and attention. Ben has also negatively reinforced his parents’ tendency to provide him with comfort and attention by stopping his crying when they pick him up and soothe him back to sleep.
6. Imagine that you are the therapist for Ben and his mother. How might improved sleep hygiene help reduce Ben’s insomnia?
Ben should have a regular bedtime and bedtime ritual prior to sleep (e.g., bath, feeding). His parents should place him in his crib when he is fed, dry, and drowsy but still awake. They might give him a transitional object, such as a small blanket, to help him soothe himself to sleep.
How might planned ignoring improve Ben’s insomnia?
The text describes the procedures that might be used for planned ignoring. Ben’s parents will attempt to extinguish Ben’s crying and other bids for attention prior to bedtime and in the middle of the night by withdrawing all positive reinforcement from him when he protests. They may check on him using a fixed interval reinforcement schedule (e.g., every 10 minutes), but they do not respond contingent on his crying.
7. Some parents are unable to used planned ignoring with their infants or toddlers. What alternative treatment might you recommend to Ben and his mother?
Two other behavioral interventions are (1) graduated ignoring, and (2) bedtime fading. They are also described in the text.
8. How effective are behavioral interventions to treat infant insomnia?
More than 90% of healthy infants respond to behavioral interventions like these.
Thoughts Before Bedtime
Insomnia Disorder in Adolescence
Alex Molnar was a 15-year-old boy who was referred to the sleep disorders clinic of our hospital because of sleep-onset insomnia. For the past 6 months, Alex has experienced problems falling asleep at night. His insomnia had an insidious onset and has grown progressively worse, especially in the past two months. Initially, Alex would toss and turn in bed, finally falling asleep after an hour-long struggle to rest. Currently, however, Alex spends several hours, several nights each week, trying to fall asleep. Needless to say, his sleep problems have caused him considerable frustration.
“We tried to get an appointment for the sleep clinic over 6 weeks ago,” explained Alex’s mother. “I noticed Alex acting like a zombie most of the time. I had to yell and scream at him to get him out of bed in the morning. He’d often be late for the bus and I’d have to drive him to school. Then, when he’d get home, he’d only want to lounge on the couch or watch TV. He was crabby all of the time.”
Alex’s father added, “What really prompted us to seek help was his performance in school. We noticed a marked drop in his grades from last year, even in subjects that he used to enjoy like math and science. At first, we attributed this drop in grades to problems transitioning from middle school to high school, but then we talked with his math teacher. She commented about his concentration problems and drowsiness in school. She thought Alex might be depressed or have ADHD.”
Alex readily admitted to having insomnia. He said that he typically went to bed between 10:00 p.m. and 11:30 p.m. Initially, he would feel exhausted when his head hit the pillow. However, soon after laying down, his mind would fill with events that occurred that day. Alex admitted to disproportionately reflecting on bad events: things he said to friends that he later regretted, mistakes he made on tests, silly things he did that caused embarrassment. He would often chastise himself thinking, “How could I have been so stupid?” These thoughts caused muscle tension and “a warm feeling in his chest” making him toss and turn in his bed.
Eventually, his thoughts would turn to the next day: homework that he still needed to complete before class, an important invitational for cross country, his dad’s chronic health problems. As he thought about each problem, both little hassles and major stressors, Alex felt more helpless. “It’s like I’m running in a narrow valley and the cliffs on each side are closing in on me. I can feel tightness in my body, in my chest, everywhere. At that point, I tell myself, ‘C’mon man. You’ve got to get to sleep. It’s midnight already and you need to get up at 6:30 for school.’”
Of course, statements like these never helped. Frustrated and angry with himself, Alex would often leave his bedroom, have a snack, and watch TV. TV distracted him from his worries, eventually lulling him to sleep. Coffee in the morning, three or four diet sodas during the day, and Red Bull after school would help him through the next day.
A medical examination revealed no health problems that would likely cause Alex’s sleep disorder. Furthermore, Alex was not taking any medication that might cause insomnia. The neurologist suggested that his family try a psychosocial intervention before participating in a formal sleep study.
1. How does Alex meet DSM-5 diagnostic criteria for insomnia disorder?
- Alex has problems falling asleep.
- His sleep disturbance causes him distress (e.g., frustration) and impairment (i.e., daytime fatigue, concentration problems).
- His sleep difficulties occur at least three nights per week.
- Duration is > 3 months.
- Alex has adequate opportunities for sleep but cannot fall asleep.
- Alex’s problem is not better explained by another sleep–wake disorder.
- Alex’s problem is not attributable to the effects of a substance (although his caffeine consumption may contribute to his problem).
- Co-existing mental disorders or medical conditions do not adequately explain Alex’s insomnia (although symptoms of GAD likely contribute to his sleep problems).
A clinician would likely diagnose Alex with insomnia disorder with non-sleep disorder mental comorbidity because of his co-occurring generalized anxiety disorder. (See question 2 below.)
2. Does Alex meet criteria for any other mental disorder that might exacerbate his insomnia?
Alex would likely be diagnosed with co-occurring generalized anxiety disorder (GAD). GAD is an anxiety disorder characterized by excessive worry. He meets the following diagnostic criteria:
- He shows excessive worry (apprehensive expectation), more days than not, for at least 6 months.
- He finds it difficult to control his worry.
- He shows the following signs/symptoms (at least one is required in children):
- restlessness
- easily fatigued
- difficulty concentrating
- irritability
- muscle tension
- sleep disturbance
- The worry and physical symptoms cause distress or impairment.
- The problem is not attributable to a substance or medical condition.
- The problem is not better explained by another mental disorder.
We might wonder if some of the signs/symptoms of GAD are caused by Alex’s insomnia rather than GAD itself. For example, lack of sleep might cause fatigue, difficulty concentrating, and irritability. However, Alex’s chronic worrying at night, combined with his restlessness and muscle tension, suggest the presence of GAD in addition to insomnia. Furthermore, only one sign/symptom of GAD is required for youths. For these reasons, many clinicians would diagnose Alex with both disorders.
3. Identify three cognitive distortions that might contribute to Alex’s excessive worrying and insomnia.
Three cognitive distortions are mentioned in the text.
- catastrophizing: expecting the worst possible outcomes, even if their probability of occurring is low
- selective abstraction: emphasizing negative events and downplaying positive events that occurred during the day
- personalization: attributing negative events to one’s own shortcomings when, in fact, there is no relationship between one’s actions and the negative event
Alex seems to engage in selective abstraction and personalization when he reflects on events that occurred that day. In contrast, when Alex thinks about the next day’s events, he may catastrophize.
4. What cognitive interventions might be useful to treat Alex’s problems?
A cognitive therapist would likely help Alex identify and challenge these negative automatic thoughts and cognitive distortions that contribute to his worrying and insomnia. For each belief, the therapist would likely ask Alex to produce evidence to support it. Alternatively, the therapist might encourage Alex to think more flexibly and realistically and then to test his new (realistic) way of thinking the next day.
For example, Alex might believe, “I need to get to bed right now. If I don’t, I’ll be a mess tomorrow and run poorly (in cross country).” A therapist might help Alex look at the situation more objectively and flexibly. Is it really true that Alex needs to get to bed immediately after he lies down to sleep? Don’t most adolescents take, on average, about 20 to 30 minutes to sleep? Even if Alex takes much longer, would that be so terrible? Couldn’t he survive the next day if he slept only 4 or 5 hours? Besides, what is the likelihood that he only gets 4 hours of sleep? The likelihood is probably pretty low.
5. What behavioral interventions might be useful to treat Alex’s problems?
A behavioral intervention that would likely be helpful to alleviate Alex’s insomnia would be to improve his sleep hygiene. At the very least, Alex would likely benefit from a more consistent bedtime, a routine or ritual before bed (e.g., a relaxing shower), reduced access to nighttime stimulation (e.g., avoiding television or other electronic media), and decreased caffeine consumption, especially in the late afternoon and evening. Exercise shortly before bedtime might also be problematic, but the case study does not tell us when Alex runs. Finally, if Alex experiences continued sleep-onset problems, he might benefit from leaving his bedroom and reading (or listening to music or a podcast) in another room for 20 to 30 minutes. Leaving one’s bed during an episode of insomnia is important so that the bed is associated with sleep rather than with anxiety, worry, or frustration.
A behavioral intervention that might help Alex reduce his chronic worrying is exposure therapy. Recall that Borkovec’s model for GAD posits that people engage in chronic worrying so they can avoid panic. Worry, therefore, is negatively reinforcing. A therapist might encourage Alex to keep a “worry journal” in which he can jot down his worries. Alex might set aside 10 minutes during the day to write his worries in the journal. A designated “worry time” can help Alex gain control over his worrying and lead to a decrease in overall worrying because of repeated exposure. If Alex finds himself worrying at bedtime, he can give himself permission to stop worrying because he has already set aside time for worrying earlier in the day.
Exposure-based therapy might also be combined with relaxation techniques, such as deep breathing exercises, progressive muscle relaxation, or guided imagery. These techniques might be useful to reduce worrying and promote sleep.
6. What medications might be useful to treat Alex’s problems?
There is limited information regarding the efficacy of medications to treat insomnia in children and adolescents. The most frequently used over-the-counter medications are antihistamines, such as diphenhydramine (Benadryl), which cause drowsiness. Prescription medications include alpha-2 agonists (e.g., Catapres) and traditional benzodiazepines (e.g., Doral), and hypnotics (e.g., Ambien). These medications are associated with reduced sleep quality and may promote dependency if used for long durations.
Selective serotonin reuptake inhibitors (SSRIs; Prozac, Zoloft) are efficacious in reducing anxiety in adolescents. It is possible that an initial trial of an SSRI might alleviate Alex’s GAD symptoms and improve his sleep onset.
Daytime Fatigue
Circadian Rhythm Sleep–Wake Disorder
Sixteen-year-old Lindsay was referred to our sleep clinic because of chronic fatigue. Lindsay was a perfectionist. She earned high grades, was a star on the cross country and track teams, and popular with other kids at school. Lindsay was excellent at everything she did—everything except for sleeping.
Despite her best efforts, Lindsay had terrible problems going to sleep. Lindsay tried to go to sleep early each night, so that she could get up early the next morning and attend writing club before school. Often, however, she would lie in bed for hours before finally falling asleep.
“You know what they say. ‘Early to bed, early to rise . . .,” Lindsay said to me during her first visit. “The problem is, I’ll finish studying or come home from some activity and try to get to bed at a reasonable hour. But then, I’d toss and turn in bed, unable to get to sleep.”
“What do you do when you can’t sleep?” I asked.
“Sometimes, I’ll get up and watch TV for a while or text someone. Usually, I just tell myself, ‘C’mon Lind, you know you need to get to sleep’ which makes me even more frustrated because I can’t.”
I asked, “So what is it like, when you’re lying in bed, trying to sleep?”
She answered, “It’s like I can’t shut off my brain. Instead of relaxing, I’ll be thinking of things that happened that day or things that are scheduled for tomorrow.”
“I’ve caught Lindsay up at 2 and 3 in the morning,” added her mother. Lindsay admitted, “Sometimes I watch videos, or have something to eat, or whatever.”
Her mother interjected, “The problem is the next day. It’s nearly impossible to get her out of bed.”
“I want to get up and go to school but just can’t,” Lindsay reported. “Then, when I get to school, I’m tired all of the time. I have a hard time concentrating.”
“How long have you had this problem?” I asked.
“It started when I was in middle school,” Lindsay reported. “At first it wasn’t too bad, but now it takes me several hours to fall asleep.”
“And what about on weekends?” I asked. “Do you have trouble falling asleep on Friday and Saturday nights too?”
“On weekends I know that I don’t need to get up early the next day, so I just go to sleep whenever I want, usually about 1 or 2 a.m.,” she replied. “Then I sleep most of the next morning.”
From the look on her face, I could tell that Lindsay was exasperated. Trying to give her hope, I said, “Maybe I can help you—teach you strategies that could help you get to sleep.”
1. What DSM-5 sleep-wake disorder best describes Lindsay’s condition?
2. How does Lindsay meet diagnostic criteria for this condition?
- Lindsay has a persistent pattern of sleep disruption caused by a misalignment between her endogenous circadian rhythm and the sleep–wake cycle required by her daily schedule.
- The sleep disturbance causes excessive sleepiness and/or insomnia.
- The sleep disturbance causes clinically significant distress or impairment in social (and perhaps) academic functioning.
Lindsay would probably be diagnosed with circadian rhythm sleep–wake disorder: delayed sleep phase type. If allowed to set her own sleep–wake cycle, she would go to sleep much later and wake up much later than she currently does.
2. When does an adolescent’s sleep problem become a disorder that merits treatment?
DSM-5 requires individuals to experience significant distress or impairment in order to merit a sleep disorder diagnosis. Lindsay clearly experiences distress and impairment (daytime fatigue).
3. How many hours of sleep should Lindsay get, if she is typically developing?
A healthy adolescent should receive between 9 and 10 hours of sleep per night.
4. Many adolescents show a phase delay in melatonin production after puberty. Why might this be important for Lindsay?
Phase delay production of melatonin can cause Lindsay to want to go to sleep later in the evening and wake later in the morning. This might cause a mismatch between her desired sleep–wake cycle and the sleep–wake cycle that she must achieve in order to attend school and early morning extracurricular activities (i.e., writing club).
5. What associated symptoms or comorbid disorders would you want to assess prior to treating Lindsay?
Lindsay is at greatest risk for major depressive disorder, a condition that is often associated with sleep–wake disorders. A clinician might always want to explore the possibility that she has symptoms of generalized anxiety disorder (GAD). When she lies in bed at night, does she worry?
6. Imagine that you are Lindsay’s therapist. How might you improve Lindsay’s sleep hygiene to reduce her sleep problems?
The text describes principles of sleep hygiene. For example, Lindsay may wish to adopt a bedtime ritual prior to going to sleep, establish a regular bedtime each night, and avoid stimulation prior to bed (e.g., television).
How might you use stimulus control and sleep restriction to help Lindsay?
Stimulus control: If Lindsay is unable to sleep, she should leave her bed so that she does not associate worrying with her bed or bedroom through classical conditioning.
Sleep restriction: Similarly, Lindsay should not spend more time in bed than necessary. Instead of remaining in bed and worrying, she should leave her bed and engage in another quiet activity, such as reading for 20 minutes. Restricted sleep, especially through reading, will increase fatigue and make sleep easier to achieve.
How might you use cognitive restructuring to help Lindsay?
The text describes the use of cognitive restructuring for adolescents experiencing sleep problems. A critical component of cognitive restructuring is to help Lindsay identify maladaptive or irrational beliefs that might contribute to her problems falling asleep. For example, Lindsay might believe that she “needs” to get to sleep at a certain hour to function well the next day. Although she would “like to” get to sleep at a reasonable hour, it is probably not true that she “needs” to get to sleep at a certain hour. She can likely function pretty well with fairly little sleep, at least in the short term. Her high level of achievement supports this assertion.
7. Most physicians treat pediatric sleep problems with medication. Identify one medication that might be used to help Lindsay fall asleep. What are the side effects of this medication? Would you want your child to take this medication?
Medications for insomnia include (1) antihistamines, (2) alpha-2 agonists, and (3) benzodiazepines. Antihistamines are associated with the fewest risks, although they can interfere with the overall quality of sleep and cause daytime drowsiness. Children can overdose on alpha-2 agonists and benzodiazepines. Consequently, their use must be monitored by parents and physicians. Benzodiazepines are also associated with tolerance over time. All of these medications are generally regarded as short-term treatments for sleep problems in adolescents rather than long-term solutions to pediatric sleep problems.
A Normal Life
Pediatric Sickle Cell Disease
Caleb Johnson was a 10-year-old boy who was referred to a pediatric psychologist at a large children’s hospital. Caleb was diagnosed with sickle cell disease shortly after birth and has an extensive medical history related to this condition.
Caleb’s disorder, hemoglobin SS disease, is a recessive genetic disorder. Both his mother and father were carriers of the disease and Caleb was unlucky enough to inherit the recessive gene from each parent. The disease is especially prevalent among African American children, like Caleb.
The disorder causes red blood cells to have a sickle shape, rather than the round shape shown by healthy children. The sickle shape limits the amount of oxygen the blood cells can carry and can cause occlusion (blockages) in children’s blood stream. Sickle cells also have a much shorter lifespan (10–20 days) than healthy red blood cells (120 days) causing children with the disease to experience anemia, that is, a low red blood cell count.
Caleb had experienced the most common effects of sickle cell disease. First, because of his anemia, he was frequently tired and often experienced weakness and fatigue. These symptoms often reduced the amount of time that he could play with other children and limited his participation in certain high-intensity sports, like soccer and football (two sports that he enjoyed watching).
Second, Caleb experienced frequent, intense episode of pain associated with occlusions. Usually, these painful crises occurred in his chest, arms, and legs and lasted for several hours or days. Sometimes, the pain was severe and caused him to miss school and other daily activities. Painful crises often occurred when he was dehydrated (e.g., after playing sports), when he experienced a sudden change in temperature (e.g., playing in the snow, swimming in a cold pool), or when he was under stress (e.g., listening to his parents argue).
Third, Caleb has a history of infections and hospitalizations associated with his disorder. As a toddler, he was diagnosed with acute chest syndrome, a condition characterized by occlusions of vesicles in the lungs, resulting in severe chest pain, coughing, and breathing problems. In preschool, he experienced splenic sequestration syndrome, a serious condition in which his sickle-shaped cells became trapped (i.e., sequestered) in his spleen, causing severe anemia and abdominal pain. He has also been hospitalized on several other occasions because of recurrent fevers. Currently, Caleb takes a medication called hydroxyurea (Droxia) that increases hemoglobin and reduces the frequency and intensity of his pain.
During the initial interview with the pediatric psychologist, Caleb’s parents reported significant symptoms of irritability and dysphoria in Caleb. Over the past 6 months, Caleb has shown an increase in moodiness, lethargy, and overall feelings of hopelessness, associated with his sickle cell symptoms. On one occasion, during a painful episode, he commented that “he wished he had never been born.” He has also grown angry at being limited in his ability to play sports, run and swim, and do many other physical activities because of chronic fatigue and recurrent pain. Although many of his friends and classmates are sympathetic to his medical problems, his parents have noticed that Caleb is less often invited to others’ homes to play.
Caleb’s medical condition has also taken its toll on the Johnson family more generally. His parents reported very high levels of stress associated with caring for a child with a chronic medical problem. Stressors include (1) making sure that Caleb takes his medication regularly, (2) coordinating Caleb’s medical care with his schooling, (3) working with teachers to help Caleb make up missed schoolwork, (4) transportation to and from medical appointments, (5) medical bills, and (6) missed work. Mr. and Mrs. Johnson are also concerned that they may be neglecting Caleb’s two younger brothers. These stressors have led to increased marital conflict that, in turn, exacerbates Caleb’s symptoms.
When interviewed alone, Caleb denied suicidal ideation, but readily admitted to feelings of hopelessness and helplessness regarding his illness. “No one understands what it’s like . . .” he repeatedly said. “I can’t do all the things that I want to do, all the things even my little brothers can do. I can’t have a normal life.”
1. What is a pediatric psychologist and what are his or her three main professional activities?
Pediatric psychology is a subdivision of clinical child psychology that focuses on the interaction between children’s physical and mental health. Pediatric psychologists often work in hospitals, medical clinics, or outpatient facilities to address behavioral factors that might impact children’s health outcomes.
The three main professional activities of pediatric psychologists are (1) inpatient consultation–liaison; (2) helping children with chronic medical conditions; and (3) specialized care for specific disorders such as feeding and eating disorders, sleep–wake disorders, or elimination disorders. The pediatric psychologist who interviewed Caleb and his family may work with medical professionals to help youths with sickle cell disease.
2. What mental health problem(s) might Caleb experience?
Caleb might meet diagnostic criteria for major depressive disorder. He shows the following signs and symptoms: (1) depressed and irritable mood (observed by others), (2) loss of interest in activities he formerly enjoyed, (3) fatigue/loss of energy, (4) feelings of worthlessness, (5) concentration problems, and (6) thoughts of death. These symptoms have lasted more than 2 weeks and are associated with impairment and distress.
To diagnose Caleb with major depressive disorder we would need to confirm with his physicians that his symptoms are not entirely due to his medical condition. For example, sickle cell anemia can cause fatigue and concentration problems. The case study suggests that Caleb’s mood problems, decreased energy, and concentration problems are in excess of what might be expected of sickle cell anemia alone and may reflect a depressive response to the disorder.
3. If you were Caleb’s therapist, how might you address adherence in therapy?
Adherence refers to Caleb’s willingness and ability to follow through with his physicians’ recommendations regarding medical treatment. Specifically, Caleb must remember to take his medication to manage his disorder and keep pain levels low.
Adherence might be a problem for at least three reasons. First, children like Caleb might have difficulty remembering to take their medication regularly because of immature executive functioning skills. Second, Caleb might not take his medication because he experiences depression, hopelessness, and helplessness. He might feel “What’s the use?” and refuse to take medication. Third, his parents’ high levels of stress might compromise their ability to monitor Caleb’s medication use.
The therapist might work with Caleb’s family to increase adherence. For example, she might challenge Caleb’s negative thoughts about the hopelessness of his condition. Alternatively, she might help Caleb’s parents establish a token economy to reinforce regular medication use. Finally, she might work with parents to reduce stress that interferes with their ability to care for Caleb and monitor/reinforce his adherence to medication.
4. In what way might behavioral factors (besides adherence) exacerbate Caleb’s sickle cell symptoms? How might a therapist address these factors?
Certain actions can exacerbate Caleb’s pain. For example, a lack of hydration, excessive physical activity, or exposure to very cold or warm temperatures can cause a pain crisis. The therapist might work with Caleb to identify the association between these actions and increased pain. The therapist might also target maladaptive thoughts that prompt Caleb to engage in these actions. For example, Caleb might think, “I’m getting really tired playing soccer, but I don’t want to stop. If I stop, everyone will think I’m weak.” The therapist might challenge Caleb’s belief that others will think he is weak or make fun of him if he stops playing. The therapist might ask, “If a classmate said that he needed to stop playing, because he was getting tired or didn’t feel well, would you make fun of him?” The therapist might role-play situations in which Caleb uses humor or other adaptive coping mechanisms to withdraw from activities when he feels fatigue or discomfort.
5. In what way might emotional factors exacerbate Caleb’s sickle cell symptoms? How might a therapist address these factors?
It is likely that Caleb’s experience of pain is exacerbated by psychosocial stress and problems with emotion regulation. Treating his depressive symptoms and increasing his sense of self-efficacy in managing his symptoms will likely improve his overall functioning. Pediatric psychologists would likely teach children like Caleb relaxation skills to help them reduce psychosocial stress and manage discomfort. Techniques might include controlled breathing, progressive muscle relaxation, and guided imagery. Although not mentioned in the text, biofeedback might also be used to help children manage chronic pain.
Many children with chronic health problems, and their parents, participate in support groups. A support group for children with sickle cell disease might be especially helpful to Caleb who feels that none of the other children at his school can empathize with him. One option might be to enroll Caleb in a summer camp for children with sickle cell disease and similar chronic medical problems.

IMAGES
VIDEO
COMMENTS
Subject to that exception, any mandatory reporter who fails to report the issue within 24 hours will be fined up to $500 for the first failure and more than $1000 for subsequent failures. In cases of rape, sodomy, or object sexual penetration, a mandatory reporter who knowingly and intentionally fails to make the report is guilty of a Class 1 ...
CASE STUDY 4-HERRIOT. You are working in a community health service which is run in conjunction with a youth drop-in' progranm. known. as Youth in Front. Herriot Malini is a 14-year-old girl who has been attending the program for some time. Herriot. has a mild intellectual disability with sub-average intellectual functioning and lack of social ...
Case Study - Herriot You are working in a community health service which is run in conjunction with a youth 'drop-in' program known as Youth in Front. Herriot Malini is a 14-year-old girl who has been attending the program for some time. Herriot has a mild intellectual disability with sub-average intellectual functioning and a lack of social ...
You will need to take notes about what Herriot says to you, Certificate III IN INDIVIDUAL SUPPORT- CHCCOM005 ASSESSMENT TASK 3 ROLE PLAYS: ROLE PLAY 1: HERRIOT AND THE CARE WORKER: This role play is a continuation of Case Study 5 from Assessment Task 2. In this role play your assessor will play the role of Herriot.
Case Study - Herriot. You are working in a community health service which is run in conjunction with a youth 'drop-in' program known as Youth in Front. Herriot Malini is a 14-year-old girl who has been attending the program for some time. Herriot has a mild intellectual disability with sub-average intellectual functioning and lack of social ...
CASE STUDY 5: HERRIOT. You are working in a community health service which is run in conjunction with a youth 'drop-in' program known as Youth in Front. Herriot Malini is a 14-year-old girl who has been attending the program for some time. Herriot has a mild intellectual disability with sub-average intellectual functioning and a lack of social ...
Practice task 4. Read the case study, then answer the questions that follow. Case study. Ingrid is a community services worker in a large team. Ingrid's team attends a weekly team meeting to discuss important service changes and give an area report. Ingrid was offended by something her supervisor Sandra said as this week's meeting.
5. Read the case study regarding Herriot. How would you support Herriot to make her own decision about this purchase? There are 2 steps to solve this one. Who are the experts? Experts have been vetted by Chegg as specialists in this subject. Expert-verified. Step 1.
using the information that you have discovered about Herriot's reported abuse in Herriot's case study and role plays (Assessment Tasks 2 and 3), complete the Report of a Reasonable Suspicion of Child Abuse and/or Neglect form to report the suspected abuse to the appropriate authorities
VIDEO ANSWER: All right so you're looking for some opinions on bio ethics cases i'll do what i can to help so first case in forming the wife. Mister s is marry the father of 2 school children. Basically, mister s has h.
The public perception of vets is rooted in romanticised James Herriot fiction rather than the commercial realities of modern day practice, say vet leaders, in this week's issue of the Vet Record. The popular and much loved James Herriot novels, which were also televised in the 1970s and 1980s, depict a bucolic fantasy world in which a male ...
Posted onNovember 23, 2010November 2, 2010. Every Living Thing Chapter Summaries. Chapter 1. James Herriot reminisces about the cold winter days in Yorkshire. He treats a horse with a new medicine and supplements it with an older type, just to help. Instead, the horse collapses, and he and the owner both worry that the horse has died.
This role play is a continuation of Case Study 5 from Assessment Task 2. In this role play your assessor will play the role of Herriot. Herriot is going to tell you some things. You will need to take notes about what Herriot says to you, as you will need to discuss her situation with your supervisor in Role Play 2.
A literary biography with an overview of critical response to Herriot's work. Rossi, Michael John. James Herriot: A Critical Companion. Westport, Conn.: Greenwood Press, 1997. A study of Herriot ...
Case Study Heriot-Watt University Fed up of time-consuming health and safety reporting, Herriot-Watt University uses Info Exchange to digitise and simplify it's processes. About Herriot-Watt University Founded in 1821, Heriot-Watt has a rich heritage and is valued for its pioneering research informed by the global needs of business and industry
#lowcode #nocode Sign up to a free trial of LiveCodehttps://livecode.com/trialJames Heriot Museum and LiveCode | A Case StudyCheck out our other videos by cl...
Get four FREE subscriptions included with Chegg Study or Chegg Study Pack, and keep your school days running smoothly. 1. ^ Chegg survey fielded between Sept. 24-Oct 12, 2023 among a random sample of U.S. customers who used Chegg Study or Chegg Study Pack in Q2 2023 and Q3 2023. Respondent base (n=611) among approximately 837K invites.
Finally, there have been several single-case studies of CFT for psychosis (Ellerby, 2013a, 2013b, 2014a, 2014b; Heriot-Maitland & Levey, 2021; Heriot-Maitland & Russell, 2018). These involved individual CFT formulations and longer-term interventions utilizing multiple CFT techniques.
Heriot-Watt Case Study. Heriot-Watt move from Blackboard to Canvas to increase student engagement and support Responsive Blended Learning. UK, Dubai, Malaysia. 30,000 Users. Adopted Canvas 2020. download Share. Heriot-Watt is a global university focused on delivering innovative, worldwide education. Since 1821 the community of scholars that ...
By Peter Herriot. Edition 1st Edition. First Published 2008. eBook Published 12 September 2008. Pub. Location London. ... Each chapter is followed by a lengthy case study, and these range from a close textual analysis of George W. Bush's second inaugural speech through to a treatment of Al-Qaida as a global media event. ... 5 Howick Place ...
Read each of the brief case studies below. Using the DSM-5 definition above, determine if the child in each case study has a mental disorder. If there's not enough information in the case study, identify any other information would you need to determine if he or she meets the DSM-5 definition. Margaret wets the bed at night.