A brief history of vaccines and how they changed the world

Child deaths have halved since Gavi, the Vaccine Alliance, was launched in 2000. Image: REUTERS/Hereward Holland

.chakra .wef-1c7l3mo{-webkit-transition:all 0.15s ease-out;transition:all 0.15s ease-out;cursor:pointer;-webkit-text-decoration:none;text-decoration:none;outline:none;color:inherit;}.chakra .wef-1c7l3mo:hover,.chakra .wef-1c7l3mo[data-hover]{-webkit-text-decoration:underline;text-decoration:underline;}.chakra .wef-1c7l3mo:focus,.chakra .wef-1c7l3mo[data-focus]{box-shadow:0 0 0 3px rgba(168,203,251,0.5);} Greta Keenan

.chakra .wef-9dduvl{margin-top:16px;margin-bottom:16px;line-height:1.388;font-size:1.25rem;}@media screen and (min-width:56.5rem){.chakra .wef-9dduvl{font-size:1.125rem;}} Explore and monitor how .chakra .wef-15eoq1r{margin-top:16px;margin-bottom:16px;line-height:1.388;font-size:1.25rem;color:#F7DB5E;}@media screen and (min-width:56.5rem){.chakra .wef-15eoq1r{font-size:1.125rem;}} COVID-19 is affecting economies, industries and global issues

.chakra .wef-1nk5u5d{margin-top:16px;margin-bottom:16px;line-height:1.388;color:#2846F8;font-size:1.25rem;}@media screen and (min-width:56.5rem){.chakra .wef-1nk5u5d{font-size:1.125rem;}} Get involved with our crowdsourced digital platform to deliver impact at scale
Stay up to date:.
- Edward Jenner developed the first vaccination to prevent smallpox.
- Gavi, the Vaccine Alliance, aims to lower vaccine prices for the poorest countries.
- The Coalition for Epidemic Preparedness Innovation (CEPI) works to accelerate the development of vaccines against emerging diseases.
It is no secret that vaccinations have revolutionized global health. Arguably the single most life-saving innovation in the history of medicine, vaccines have eradicated smallpox, slashed child mortality rates, and prevented lifelong disabilities.
Have you read?
Why a coronavirus vaccine takes over a year to produce – and why that is incredibly fast, why we need to start a new pro-vaccine movement.
Possibly lesser known, however, are the historic events and pioneers we can today thank for not only saving millions of lives each year, but for laying the foundations of future vaccine development – something that is front-of-mind as the world rushes to make a viable coronavirus vaccine.
Early attempts to inoculate people against smallpox – one of history’s most feared illnesses, with a death rate of 30% – were reported in China as early as the 16th Century. Smallpox scabs could be ground up and blown into the recipient’s nostrils or scratched into their skin.
The practice, known as “variolation”, came into fashion in Europe in 1721, with the endorsement of English aristocrat Lady Mary Wortley Montagu, but was later met with public outcry after it transpired 2-3% of people died after inoculation, and further outbreaks were triggered.
The next iteration of inoculation, which turned out to be much safer than variolation, originated from the observation that dairy farmers did not catch smallpox. The 18th Century English physician, Edward Jenner, hypothesised that prior infection with cowpox – a mild illness spread from cattle – might be responsible for the suspected protection against smallpox. And so, he set to work on a series of experiments, now considered the birth of immunology, vaccine therapy, and preventive health.
In 1796, Jenner inoculated an eight-year-old boy by taking pus from the cowpox lesions on a milkmaid’s hands and introducing the fluid into a cut he made in the boy’s arm. Six weeks later, Jenner exposed the boy to smallpox, but he did not develop the infection then, or on 20 subsequent exposures.
In the years that followed, Jenner collected evidence from a further 23 patients infected or inoculated with the cowpox virus, to support his theory that immunity to cowpox did indeed provide protection against smallpox.
The earliest vaccination – the origin of the term coming from the Latin for cow (“vacca”) – was born. Jenner’s vaccination quickly became the major means of preventing smallpox around the world, even becoming mandatory in some countries.

Almost a century after Jenner developed his technique, in 1885, the French biologist, Louis Pasteur, saved a nine-year-old boy’s life after he was bitten by a rabid dog, by injecting him with a weakened form of the rabies virus each day for 13 days. The boy never developed rabies and the treatment was heralded a success. Pasteur coined his therapy a “rabies vaccine”, expanding the meaning of vaccine beyond its origin.
The global influence of Louis Pasteur led to the expansion of the term vaccine to include a long list of treatments containing live, weakened or killed viruses, typically given in the form of an injection, to produce immunity against an infectious disease.
Scientific advances in the first half of the 20th Century led to an explosion of vaccines that protected against whooping cough (1914), diphtheria (1926), tetanus (1938), influenza (1945) and mumps (1948). Thanks to new manufacturing techniques, vaccine production could be scaled up by the late 1940s, setting global vaccination and disease eradication efforts in motion.
Vaccines against polio (1955), measles (1963), rubella (1969) and other viruses were added to the list over the decades that followed, and worldwide vaccination rates shot up dramatically thanks to successful global health campaigns. The world was announced smallpox-free in 1980, the first of many big vaccine success stories, but there was still a long way to go with other infectious diseases.
By the late 1990s, the progress of international immunization programmes was stalling. Nearly 30 million children in developing countries were not fully immunized against deadly diseases, and many others weren’t immunized at all. The problem was that new vaccines were becoming available but developing countries simply could not afford them.
In response, the Bill and Melinda Gates Foundation and partners came together in 2000 to set up the Global Alliance for Vaccines and immunization, now called Gavi, the Vaccine Alliance . The aim was to encourage manufacturers to lower vaccine prices for the poorest countries in return for long-term, high-volume and predictable demand from those countries. Since its launch, child deaths have halved, and 13 million deaths have been prevented.
Responding to the COVID-19 pandemic requires global cooperation among governments, international organizations and the business community , which is at the centre of the World Economic Forum’s mission as the International Organization for Public-Private Cooperation.
Since its launch on 11 March, the Forum’s COVID Action Platform has brought together 1,667 stakeholders from 1,106 businesses and organizations to mitigate the risk and impact of the unprecedented global health emergency that is COVID-19.
The platform is created with the support of the World Health Organization and is open to all businesses and industry groups, as well as other stakeholders, aiming to integrate and inform joint action.
As an organization, the Forum has a track record of supporting efforts to contain epidemics. In 2017, at our Annual Meeting, the Coalition for Epidemic Preparedness Innovations (CEPI) was launched – bringing together experts from government, business, health, academia and civil society to accelerate the development of vaccines. CEPI is currently supporting the race to develop a vaccine against this strand of the coronavirus.
Protecting against long-standing illnesses will continue to be important in the decades and centuries ahead, but the work is not complete. In order to protect the world against infectious diseases, we need a mechanism to monitor new viruses, and rapidly develop vaccines against the most dangerous emerging infections. The devastating 2014/2015 Ebola virus was a wake up call for how ill-prepared the world was to handle such an epidemic. A vaccine was eventually approved but came too late for the thousands of people who lost their lives.
In response, the Coalition for Epidemic Preparedness Innovation (CEPI) was launched at Davos in 2017, a global partnership between public, private, philanthropic, and civil society organizations working to accelerate the development of vaccines against emerging infectious diseases and enable equitable access to these vaccines for affected populations during outbreaks.
We’ve come a long way since the risky and gruesome early inoculation efforts five centuries ago. Scientific innovation, widespread global health campaigns, and new public-private partnerships are literally lifesavers. Finding a vaccine to protect the world against the new coronavirus is an enormous challenge, but if there’s one thing we can learn from history, it’s that there is reason for hope.
Don't miss any update on this topic
Create a free account and access your personalized content collection with our latest publications and analyses.
License and Republishing
World Economic Forum articles may be republished in accordance with the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Public License, and in accordance with our Terms of Use.
The views expressed in this article are those of the author alone and not the World Economic Forum.
Related topics:
The agenda .chakra .wef-n7bacu{margin-top:16px;margin-bottom:16px;line-height:1.388;font-weight:400;} weekly.
A weekly update of the most important issues driving the global agenda
.chakra .wef-1dtnjt5{display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;-webkit-flex-wrap:wrap;-ms-flex-wrap:wrap;flex-wrap:wrap;} More on COVID-19 .chakra .wef-17xejub{-webkit-flex:1;-ms-flex:1;flex:1;justify-self:stretch;-webkit-align-self:stretch;-ms-flex-item-align:stretch;align-self:stretch;} .chakra .wef-nr1rr4{display:-webkit-inline-box;display:-webkit-inline-flex;display:-ms-inline-flexbox;display:inline-flex;white-space:normal;vertical-align:middle;text-transform:uppercase;font-size:0.75rem;border-radius:0.25rem;font-weight:700;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;line-height:1.2;-webkit-letter-spacing:1.25px;-moz-letter-spacing:1.25px;-ms-letter-spacing:1.25px;letter-spacing:1.25px;background:none;padding:0px;color:#B3B3B3;-webkit-box-decoration-break:clone;box-decoration-break:clone;-webkit-box-decoration-break:clone;}@media screen and (min-width:37.5rem){.chakra .wef-nr1rr4{font-size:0.875rem;}}@media screen and (min-width:56.5rem){.chakra .wef-nr1rr4{font-size:1rem;}} See all
Winding down COVAX – lessons learnt from delivering 2 billion COVID-19 vaccinations to lower-income countries
Charlotte Edmond
January 8, 2024
Here’s what to know about the new COVID-19 Pirola variant
October 11, 2023

How the cost of living crisis affects young people around the world
Douglas Broom
August 8, 2023
From smallpox to COVID: the medical inventions that have seen off infectious diseases over the past century
Andrea Willige
May 11, 2023

COVID-19 is no longer a global health emergency. Here's what it means
Simon Nicholas Williams
May 9, 2023

New research shows the significant health harms of the pandemic
Philip Clarke, Jack Pollard and Mara Violato
April 17, 2023
Organization Menu
Additional organization links, search and explore, primary menu.
Vaccines 101
The Future of Immunization
Last updated 20 April 2022
Vaccines have been a part of the human fight against disease for more than 200 years. The worldwide vaccination campaign eradicated smallpox, and immunization has eliminated polio in all but a handful of countries. Childhood vaccination has substantially reduced the morbidity and mortality of infectious diseases in much of the developed world, and yearly influenza vaccination is a commonly accepted practice worldwide to reduce the impact of the seasonal influenza infection.
While we can attribute many public health successes to vaccination, the future presents continued challenges. Diseases remain for which researchers have been unable to find effective vaccines (such as HIV/AIDS, malaria, and leishmaniasis) or that flourish in areas of the world where infrastructures for vaccination are poor or nonexistent, and even the currently available vaccines cannot be delivered. In other cases, the cost of vaccines is too high for poorer countries to afford, even though this is often where they are most needed. And, of course, although many current vaccines are highly effective, efforts continue to develop vaccines that are more effective than those available today. Thus, researchers continue to explore new possibilities. Higher effectiveness, lower cost, and convenient delivery are some of the main goals.
New Development Techniques
The first vaccine—the smallpox vaccine—consisted of a live, attenuated virus. “Attenuation” means weakening a virus to the point where it can still provoke an immune response, but doesn’t cause illness in a human host.
Many of the vaccines used today, including those for measles and some influenza vaccines, use live, attenuated viruses. Others used killed forms of viruses, pieces of bacteria, or inactivated forms of toxins that the bacteria create. Killed viruses, pieces of bacteria and inactivated toxins can’t cause illness, but can still provoke an immune response that protects against future infection.
However, new techniques are also being employed to create different types of vaccines. Some of these new types include:
- Live recombinant vaccines
- DNA vaccines
- mRNA vaccines
Live recombinant vaccines use attenuated viruses (or bacterial strains) as vectors: a virus or bacterium from one disease essentially acts as a delivery device for an immunogenic protein from another infectious agent. In some cases, this approach is used to enhance the immune response; in others, it is used when giving the actual agent as a vaccine would cause disease. For example, HIV cannot be attenuated enough to be given as a vaccine in humans—the risk of disease is too high.
Starting with a complete virus, researchers identify a section of the virus’s DNA that is not necessary for replication. One or more genes that code for immunogens of other pathogens are then inserted into this region. (Each gene essentially contains instructions that tell the body how to make a certain protein. In this case, researchers select genes that code for a protein specific to the target pathogen: an immunogen that will generate an immune response to that pathogen.) For example, a baculovirus (a virus that only infects insects) can be used as a vector, and the gene for a particular immunogenic surface protein of an influenza virus may be inserted.
When the modified virus is introduced into a person’s body, the immunogen is expressed and presented, generating an immune response against the immunogen—and therefore, against the pathogen it originates from. In addition to insect viruses, human adenoviruses have been considered potential vectors for use in recombinant vaccines, particularly against diseases such as AIDS. The vaccinia virus, which is the basis for the smallpox vaccine, was the first used in live recombinant vaccine approaches. Experimental recombinant vaccinia strains have been designed to protect against influenza, rabies, and hepatitis B, among other diseases.
DNA vaccines consist of DNA coding for a particular antigen, which is directly injected into the muscle. The DNA itself inserts into the individual’s cells, which then produce the antigen from the infectious agent. Since this antigen is foreign, it generates an immune response. This type of vaccine is relatively easy to produce, since DNA is stable and easy to manufacture, but is still experimental, because no DNA-based vaccines have been shown to elicit the substantial immune response required to prevent infection. Researchers hope DNA vaccines can generate immunity against parasitic diseases, such as malaria—currently, there is no human vaccine in use against a parasite.
mRNA vaccines aim to deliver a snippet of messenger RNA (ribonucleic acid) to a cell, so that the cell's protein-producing machinery can create a protein. That protein created from the mRNA code resembles the protein of a pathogen (virus, bacteria, fungus, or parasite) that triggers an immune response. The protein is then "presented" to immune cells to kick off the immune response consisting of killer cells and antibody-producing cells. All of this allows vaccines to include no part of the pathogen for which the vaccine is created. All researchers would need is the genetic code of the protein to be created by the recipient's cells. As of April 2020, the only licensed mRNA vaccines in the world are against SARS CoV-2, the virus causing the COVID-19 pandemic.[5, 6]
New Delivery Techniques
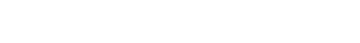
When you think of vaccination, you probably think of a doctor or nurse administering a shot. Future immunization delivery methods, however, may differ from what we use today.
Inhaled vaccines, for example, are already used in some cases: influenza vaccines have been made in a nasal spray. One of these vaccines is available every year for seasonal flu. Other possibilities include a patch application, where a patch containing a matrix of extremely tiny needles delivers a vaccine without the use of a syringe. This method of delivery could be particularly useful in remote areas, as its application would not require a trained medical person, which is generally needed for vaccines delivered as a shot by syringe.
Another issue researchers are trying to address is the so-called cold chain problem. Many vaccines require cool storage temperatures to remain viable. Unfortunately, temperature-controlled storage is often unavailable in parts of the world where vaccination is vital for disease control. One of the reasons smallpox eradication was successful was that the smallpox vaccine could be stored at relatively high temperatures and remain viable for reasonable periods. However, some contemporary vaccines cannot withstand such temperatures. The eruption of the Eyjafjallaajokull volcano in Iceland in April 2010 brought air traffic to a standstill in Northern Europe, including planes carrying 15 million doses of polio vaccine bound for West Africa. Officials feared the delay in delivering the vaccines would allow polio to spread, or that temperatures in the cargo holds of the grounded planes would render the vaccines ineffective.
Such situations highlight the need for vaccine materials that can be easily transported in various conditions and still remain viable. One possible approach to this problem was studied in early 2010 by researchers at the Jenner Institute of the University of Oxford. Starting with a small filter-like membrane, the researchers coated it with an ultrathin layer of sugar glass, with viral particles trapped inside it. In this form, the viruses the researchers used could be stored at temperatures of up to 113°F for six months, without losing their ability to provoke an immune response. By comparison, when stored in liquid storage at 113°F for just one week, one of the two viruses tested was essentially destroyed.
The researchers also demonstrated that the vaccine material could be placed in a holder designed to attach to a syringe, allowing a vaccinator to prepare the vaccine material (with a fluid medium inside the syringe) and administer the vaccine almost simultaneously.
Although this research was preliminary, it offers a promising new avenue for vaccine storage and delivery. With a stabilization method like this, widespread vaccination campaigns may be possible in areas previously difficult or impossible to reach.
The future of immunization depends on the success of medical research for vaccines that are simpler to administer, survive transport even without refrigeration, and provide a more substantial and long-lasting immune response. And in parallel, the continuing success of vaccines against so many infectious diseases has inspired scientists to use similar methods to combat diseases that remain lethal to many people, such as malaria, HIV/AIDS, and other diseases for which there are not yet effective vaccines.
- Plotkin, S., Mortimer, E. Vaccines . New York: Harper Perennial; 1988.
- Fominyen, G. . Updated April 20, 2010. Accessed 01/10/2018.
- Carvalho, J.A., Rodgers, J., Atouguia, J., Prazeres, D.M., Monteiro, G.A. DNA vaccines: a rational design against parasitic diseases. Expert Rev Vaccines . 2010 Feb;9(2):175-91.
- Alcock, R., Cottingham, M., Rollier, C., et al. Long-Term Thermostabilization of Live Poxviral and Adenoviral Vaccine Vectors at Supraphysiological Temperatures in Carbohydrate Glass. Sci. Transl. Med. 2010; 2(19), 19ra12.
Jain S, Venkataraman A, Wechsler ME, Peppas NA. Messenger RNA-based vaccines: Past, present, and future directions in the context of the COVID-19 pandemic. Adv Drug Deliv Rev. 2021 Oct 9;179:114000. doi: 10.1016/j.addr.2021.114000. Epub ahead of print. PMID: 34637846; PMCID: PMC8502079.
Verbeke R, Lentacker I, De Smedt SC, Dewitte H. The dawn of mRNA vaccines: The COVID-19 case. J Control Release. 2021 May 10;333:511-520. doi: 10.1016/j.jconrel.2021.03.043. Epub 2021 Mar 30. PMID: 33798667; PMCID: PMC8008785.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- How are vaccines being...
How are vaccines being adapted to meet the changing face of SARS-CoV-2?
- Related content
- Peer review
- Chris Stokel-Walker , freelance journalist
- Newcastle upon Tyne
- stokel{at}gmail.com
The vaccines’ development was a miracle of modern science—but as SARS-CoV-2 adapts, how are manufacturers and researchers responding? Chris Stokel-Walker learns more
It seems like a lifetime ago, but the first clinically approved vaccine against SARS-CoV-2 was given to a patient just 17 months ago, on 8 December 2020. Since that first vaccine dose, developed by the drug company Pfizer, a number of vaccines have been developed. Ten are approved by the World Health Organization, and scores more are still undergoing trials.
However, just as vaccine development hasn’t stood still, neither has the virus itself. The changing face of the novel coronavirus has challenged scientists to modify existing vaccines to better tackle the changing characteristics of SARS-CoV-2. Yet, despite much talk of modified vaccines for variants, the world is still using largely the same original vaccines for initial rollouts and booster doses.
“It seems as if the dominant things I’m hearing about at the moment are updates to existing vaccines,” says Paul Bieniasz, virologist at the Rockefeller University, New York. Those updates modify how a vaccine works to make it better match the circulating strains of SARS-CoV-2 around the world, much like the existing system for vaccinating against influenza (see below). National and international groups analyse which strains are circulating worldwide and then decide strains are the most likely to require updates to existing vaccines.
A key question at this phase of the covid pandemic is whether it’s better to continue playing catch-up with the virus and its variants or to try to develop multivalent vaccines, based on a mixture of strains that could prime the immune system against potential future variants. “We haven’t yet got a consensus agreement on what strains manufacturers should put in their vaccines,” says Penny Ward, visiting professor in pharmaceutical medicine at King’s College, London. “In part, that’s because of the rather rapid emergence of novel strains of this virus, and the fact we’re learning about the disease it causes as we’re going.”
What modified or updated covid vaccines are in development?
Many of the original main vaccines against SARS-CoV-2 are the subject of ongoing clinical trials looking at the immune response to different variants, says Ward. Not many findings have been publicly released, but Moderna released a preprint paper in April looking at a modified vaccine variant raised against the spike protein of the beta variant. 1 Reassuringly, “it showed a superior immune response when they use the variant vaccine in an already immunised population,” says Ward.
Some more experimental vaccines in development aim to invoke a broader immune response—not just to variants we’ve encountered so far or could see in the near future, says Bieniasz, but to sarbecoviruses, the group of viruses that gave rise to SARS-CoV-2 and the original SARS-CoV. One early trial, 2 which began in September 2021, has reported promising initial results from a multivariant vaccine, albeit one that triggers the production of neutralising antibodies at a similar rate to approved mRNA vaccines.
The most widely used of these experimental approaches is based on nanoparticles that contain mixtures of parts of the spike protein from various sarbecoviruses. “It’s somewhat clear these vaccines can induce a broader antibody response that would give broader protection,” says Bieniasz. One such drug, developed by researchers at the University of Cambridge, entered clinical trials in December 2021. 3
How do these approaches compare to the adaptation of flu vaccines each year?
The first bivalent flu vaccine, which can neutralise the effects of influenza types A and B, has its 80th birthday this year. But the key difference with SARS-CoV-2 is time, says Ward. She explains, “We’re not in the same position we’re at with the flu vaccines, where there are two yearly updates of the vaccines: one for the southern hemisphere and one for the northern hemisphere seasons, based on the types that have been circulating the preceding seasons.”
Although flu also adapts and spreads significantly, SARS-CoV-2 does so while being a relatively unknown quantity. “With the omicron variant, within three months, pretty much everybody on the planet has had the infection, whether or not you’ve been vaccinated,” says Paul Hunter, professor of medicine at the University of East Anglia. “The value in developing new variant vaccines is always mitigated against the time taken to find a new variant, figure out if it’s an important one, [and then] develop, modify the vaccine, check it’s worked, and approve.”
With SARS-CoV-2 the emergence and spread of new variants—globally and whatever the season—has been frighteningly fast.
Should we ignore variant specific vaccine development and aim instead for a pan-coronavirus vaccine?
A pan-coronavirus vaccine would certainly be ideal, says Bieniasz. But it’s easier said than done. Ward points out that we still have no pan-influenza vaccine, “and we’ve been at it for 80 years.”
In fact, no such pan-virus vaccine exists. “We don’t really have anything that has the breadth of protection we are envisaging for the current effort in pan-coronavirus vaccines,” says Bieniasz.
What we do have are extraordinarily effective vaccines against diseases such as measles, where we’ve been using the same vaccine for a long time. Yet for every success there are also big misses. HIV still has no effective vaccine.
“The difference there is the genetic diversity of the two viruses,” says Bieniasz. “Measles just doesn’t change very much, whereas with HIV there are more variants in a single individual at any given time point than that individual’s immune system can cope with.” The fear is that SARS-CoV-2 is closer to HIV’s continual series of variants.
One key issue is the brief immunity that seems to exist after SARS-CoV-2 infection. The fact that people are being reinfected with different variants of the novel coronavirus suggests that it would be difficult to develop a vaccine with broad enough coverage and long enough lasting immunity to be effective at stopping viral infection and transmission.
“The sort of breadth that might be achievable with a pan-coronavirus perhaps won’t be as ‘pan’ as many people imagine,” warns Bieniasz. Pan-sarbecovirus vaccines may be possible, he says—his laboratory is one of those working on it—but coronaviruses in general, whether SARS, MERS, or others, are so different that catching them all under one net is a challenge.
Still, WHO’s chief scientific officer, Soumya Swaminathan, finds it “scientifically quite feasible” that such a vaccine may be developed within the next two years. She told The BMJ in April, 4 “That’s partly because of the huge amount of research that’s gone into SARS-CoV-2 and also the understanding of immunology, as well as on the virus itself. So, we’re in a good position to be optimistic about a pan-coronavirus vaccine.”
What alternative preventive treatments are there?
“Not much, in terms of vaccinology, unfortunately,” says Ward. Monoclonal antibodies can be generated against less mutated parts of the viral genome that help prevent disease when given to patients who have contracted the novel coronavirus.
Antivirals are also being developed at pace, which is important but expensive. Ward says, “Generally speaking, we all believe that vaccines are the least expensive way of protecting a population.”
Competing interests: I have read and understood BMJ policy on declaration of interests and have no relevant interests to declare.
Provenance and peer review: Commissioned; not externally peer reviewed.
This article is made freely available for personal use in accordance with BMJ's website terms and conditions for the duration of the covid-19 pandemic or until otherwise determined by BMJ. You may download and print the article for any lawful, non-commercial purpose (including text and data mining) provided that all copyright notices and trade marks are retained.
- ↵ Moderna. Moderna announces clinical update on bivalent covid-19 booster platform. 19 Apr 2022. https://investors.modernatx.com/news/news-details/2022/Moderna-Announces-Clinical-Update-on-Bivalent-COVID-19-Booster-Platform/default.aspx
- ↵ Manchester University NHS Foundation Trust. Early data for multivariant COVID-19 vaccine booster shows promise. 6 Jan 2022. https://mft.nhs.uk/2022/01/06/early-data-for-multivariant-covid-19-vaccine-booster-shows-promise/
- ↵ Brierley C. Cambridge coronavirus vaccine enters clinical trial. University of Cambridge. 14 Dec 2021. https://www.cam.ac.uk/stories/DIOSCoVax_safetytrial
Vaccination explained in 60 seconds: ideas that changed the world
How a medical breakthrough has saved countless millions of lives
- Newsletter sign up Newsletter

In this series , The Week looks at the ideas and innovations that permanently changed the way we see the world.
Vaccination in 60 seconds
Vaccination trains the immune system to recognise and protect the body against pathogens from viruses or bacteria. Molecules from or similar to the pathogens are introduced into the body, usually through an injection.
Feminism explained in 60 seconds: ideas that changed the world The printing press explained in 60 seconds: ideas that changed the world Colonialism explained in 60 seconds: ideas that changed the world
The process may sound counter-intuitive, but vaccination can “confer active immunity against a specific harmful agent by stimulating the immune system to attack the agent”, explained Encyclopaedia Britannica . Once stimulated, “the antibody-producing cells, called B lymphocytes, remain sensitised and ready to respond to the agent should it ever gain entry to the body”, the reference website continued.
Subscribe to The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.
Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
You cannot catch a disease through vaccination, added the NHS website. That’s because the pathogens inside vaccines have been “weakened or destroyed in a laboratory first”.
If the vaccinated individual then comes into contact with the targeted disease, their immune system should be able to quickly recognise and fight it.
How did vaccination come about?
The first vaccine was developed by English surgeon Edward Jenner in 1796, to inoculate against smallpox, a leading cause of death in the 18th century that left many survivors permanently disfigured.
Prior to Jenner’s breakthrough, some doctors tried to protect their patients from smallpox by deliberately exposing them to smallpox scabs, a process originating in China called variolation, but this system often proved ineffective and made the recipient temporarily infectious to others.
Jenner observed that people who had previously caught cowpox, a relatively harmless virus passed on from close contact with cows, appeared to be immune to smallpox.
To test his theory, he obtained permission from his gardener to inoculate his eight-year-old son, applying lesions from a dairymaid with cowpox to a scratch on the boy’s skin. The child was mildly ill for a few days, but soon recovered – and when later subjected to variolation, he did not experience any symptoms of smallpox.
Initially, “Jenner’s newly proven technique for protecting people from smallpox did not catch on as he anticipated”, meeting with resistance from the medical establishment and sceptical patients, said Oxford-based research organisation The Jenner Institute .
But his technique was quickly adopted across Europe and in the US and Russia. By the time of Jenner’s death, in 1823, the significance of his work was recognised in countries worldwide and he was feted as a hero. Exactly 30 years later, it became mandatory in Britain to vaccinate children against smallpox, with parents who failed to do so fined or imprisoned.
Further major vaccines were developed in the following decades. In 1881, French biologist Louis Pasteur refined techniques to immunise sheep against anthrax, with his vaccine for rabies following four years later.
And an early typhoid vaccine developed by British bacteriologist Almroth Edward Wright was used successfully by the British military during the Boer War in South Africa between 1899 and 1902.
The following century would bring vaccines for diseases including mumps, measles, cholera, plague, tuberculosis, tetanus, influenza, yellow fever and some types of hepatitis.
The world watched in real time, the rapid development and deployment of new life-saving vaccines in 2020 when the Covid-19 virus was infecting millions and sparked a global pandemic. By 2022, nearly two-thirds of the global population had received at least one dose of a Covid vaccine, and the Imperial College London estimated the vaccines had prevented about 20 million deaths worldwide.
How did it change the world?
Vaccination has led to the eradication of the smallpox virus and some types of polio. Other diseases have been dramatically brought under control, including mumps, diphtheria, rubella and hepatitis.
The Measles, Mumps, Rubella (MMR) vaccine has been particularly successful in curbing the spread of measles, the most infectious disease on the planet and still a leading cause of childhood mortality in the developing world.
Public Health England estimated that in the UK alone, “20 million measles cases and 4,500 deaths have been averted” since the introduction of the measles vaccine in 1968. The disease was considered to be eliminated in the UK, but in 2018 cases began to rise, and about 50 cases were confirmed in England in the early part of 2023, The Guardian reported. Experts believe the recent decline in MMR uptake in children is due in part to a rise in vaccine hesitancy among parents, said The Lancet .
The Covid pandemic ushered in a new era for vaccination. The messenger ribonucleic acid (mRNA) technology used in some of the most popular vaccines, including those made by Pfizer-BioNTech and Moderna, paved the way “for a whole new class of mRNA vaccines with the potential to eradicate countless other diseases, even cancer”, said Penn Medicine .
Sign up for Today's Best Articles in your inbox
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com

Under The Radar Brexit and wage ruling are threatening the 'mutually beneficial arrangement'
By Chas Newkey-Burden, The Week UK Published 18 April 24

Instant Opinion Opinion, comment and editorials of the day
By Harold Maass, The Week US Published 17 April 24

Cartoons Wednesday's cartoons - political anxiety, jury sorting hat, and more
By The Week US Published 17 April 24
In Depth This emotive but hard-to-define art form has played a pivotal role in human evolution
By Gabriel Power, The Week UK Last updated 3 October 23
In Depth How meat-free diets went from religious abstention to global sustainability trend
By Rebecca Gillie Last updated 22 September 23
In Depth How a new understanding of bacteria revolutionised medicine
By Sorcha Bradley Last updated 15 September 23
In Depth How a new way of portraying existence transformed literature
By Rebecca Gillie Last updated 11 August 23

In Depth How the international community brought humanity to warfare
By Rebecca Gillie Last updated 4 August 23
In Depth How paying farmers fairly went from niche to necessary
By James Ashford Last updated 14 July 23

In Depth How women fought for social and political liberation
By Rebecca Gillie Last updated 30 June 23

In Depth How a German goldsmith revolutionised the way we share ideas
By Rebecca Gillie Last updated 23 June 23
- Contact Future's experts
- Terms and Conditions
- Privacy Policy
- Cookie Policy
- Advertise With Us
The Week is part of Future plc, an international media group and leading digital publisher. Visit our corporate site . © Future US, Inc. Full 7th Floor, 130 West 42nd Street, New York, NY 10036.
The changing health impact of vaccines in the COVID-19 pandemic: A modeling study
Affiliations.
- 1 Institute for Disease Modeling, Global Health Division, Bill & Melinda Gates Foundation, Seattle, WA, USA. Electronic address: [email protected].
- 2 Gender Equality Division (contractor), Bill Melinda Gates Foundation, Seattle, WA, USA.
- 3 The Big Data Institute and the Pandemic Sciences Institute, University of Oxford, Oxford, UK; The Queen's College, University of Oxford, Oxford, UK.
- 4 University of South Africa, Pretoria, South Africa.
- 5 Burnet Institute, Melbourne, VIC, Australia.
- 6 Institute for Disease Modeling, Global Health Division, Bill & Melinda Gates Foundation, Seattle, WA, USA.
- PMID: 36976678
- PMCID: PMC10015104
- DOI: 10.1016/j.celrep.2023.112308
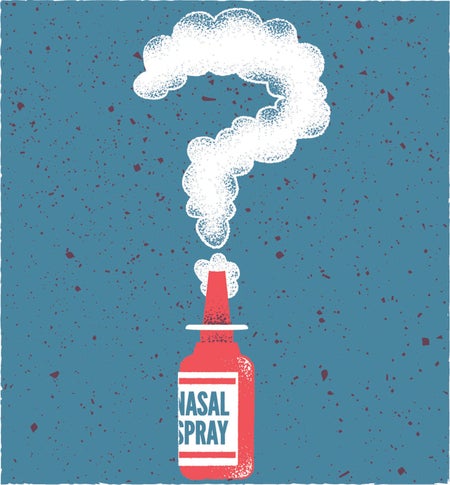
Much of the world's population had already been infected with COVID-19 by the time the Omicron variant emerged at the end of 2021, but the scale of the Omicron wave was larger than any that had come before or has happened since, and it left a global imprinting of immunity that changed the COVID-19 landscape. In this study, we simulate a South African population and demonstrate how population-level vaccine effectiveness and efficiency changed over the course of the first 2 years of the pandemic. We then introduce three hypothetical variants and evaluate the impact of vaccines with different properties. We find that variant-chasing vaccines have a narrow window of dominating pre-existing vaccines but that a variant-chasing vaccine strategy may have global utility, depending on the rate of spread from setting to setting. Next-generation vaccines might be able to overcome uncertainty in pace and degree of viral evolution.
Keywords: COVID-19; CP: Immunology; infectious disease modeling; vaccines.
Copyright © 2023 The Author(s). Published by Elsevier Inc. All rights reserved.
- COVID-19* / prevention & control
- Pandemics / prevention & control
Supplementary concepts
- SARS-CoV-2 variants
Search form
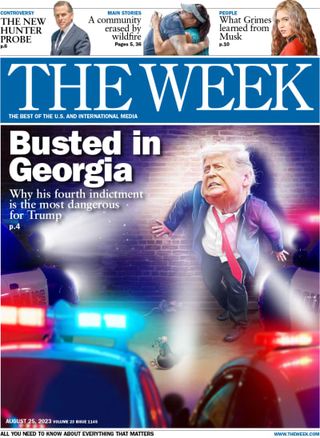
Omnia q&a: shots fired: the controversy surrounding vaccinations, then and now, robert aronowitz, walter h. and leonore c. annenberg professor in the social sciences, reflects on vaccine hesitancy today compared to the past, and the politicization of public health..
Thursday, October 21, 2021
By Katelyn Silva

Robert A. Aronowitz, Walter H. and Leonore C. Annenberg Professor in the Social Sciences
The story of the COVID-19 vaccines is a winding one. Never in the world’s history has a vaccine been developed and deemed safe and effective so quickly—in less than 12 months. For many, it felt like a miracle. For others, it brought trepidation. In the United States—where vaccines are widely available—about 23 percent of eligible individuals have chosen to not get a jab. The ongoing controversy around vaccination uptake has left many Americans on opposite sides of a fiery debate which has significant implications for public health.
Robert Aronowitz, Walter H. and Leonore C. Annenberg Professor in the Social Sciences, has extensively researched vaccines related to HPV and Lyme disease and says, “Every vaccine has a unique history. How the public reacts to a vaccine is based on the target condition it’s treating, the concerns and fears that are raised, and the era in which it comes up. No vaccine story is the same.”
We asked Aronowitz, a professor in the Department of History and Socology of Science and co-editor of Three Shots at Prevention: The HPV Vaccine and the Politics of Medicine’s Simple Solutions, his thoughts on how vaccine hesitancy today compares to the past, the politicization of public health, and the power of vaccination mandates.
How does current vaccine hesitancy and controversy look either familiar or different compared to the past?
The resistance to COVID-19 vaccinations is by no means the first instance of vaccine hesitancy. There has been opposition to vaccinations throughout history. For example, the controversies around the MMR vaccine to protect against measles, mumps, and rubella and the erroneous belief that it causes autism is one example. My HPV research looked at, among other points of contention, how the overreach of pharmaceutical companies—in underhanded lobbying of state legislatures, high pricing, and aggressive marketing that created and exploited fear—undermined the trust necessary for many ordinary people to get jabbed.
I would say that the controversy around the COVID-19 vaccines has more of a left-right political quality to the opposition than existed with some of the other vaccines of the past. Certainly, some of the opposition to older vaccines did arise from a feeling that there was overreach of the local, state, and federal government, which is a political point of view. However, the left-right dimension to the COVID skepticism seems more extreme. As a historian, I would say this is about a moment in time and the politics of that moment. Perhaps if we had had better leadership and direction under the Trump administration, this would have played out differently.
There have been some COVID vaccine mandates for healthcare workers, within private corporations, and soon, within the federal government. Are mandates historically a useful tool to increase vaccine uptake?
I’m on sabbatical in California right now and there is a mandate for healthcare workers here to be vaccinated, and compliance is really high. Mandates can work to get people who are on the fence or dragging their feet to get it done.
Based on the research of other experts, I’d mention the effectiveness of leverage points. A good example of this is the vaccinations that children are required to receive to begin schooling. The push for school mandates for childhood vaccinations came about because of the awareness that lots of people were not getting vaccinated because they had substandard access to healthcare, particularly the poor and minorities. There were social and racial inequalities in vaccine uptake, which was threatening herd immunity and the health of children not vaccinated. The basic idea was that by mandating vaccination for entry into school, you could create a powerful leverage point to influence people and put pressure on localities to find ways of providing and paying for vaccines.
Many people choose not to vaccinate because it’s inconvenient to do so, not necessarily because of ideological reasons. Everyone wants their kids in school—it’s a powerful incentive. Every state in the union eventually had school vaccine mandates and that went hand-in-hand with other programs like CHIP, the expansion of Medicaid’s service to children, and programs to subsidize what families pay for vaccinations. The approach was quite effective.
You’ve extensively studied vaccinations for HPV and Lyme Disease. How does your research dovetail with the current COVID landscape?
My research emphasizes that we have to look closely at the particular circumstances in which vaccines are developed, what the target disease is, and the peculiarities of its preexisting controversies. For example, vaccine hesitancy around Lyme disease had little to do with the kind of concerns or politics that surrounded vaccines like the MMR or others of the time, and everything to do with the problematic nature of what Lyme disease is.
There was a preexisting and ongoing fight over whether Lyme disease is a relatively straightforward tick-borne disease that doesn’t usually cause long-term, serious problems even if left untreated, that is relatively easily treated when identified, doesn’t require multiple courses of antibiotics, and only very rarely leads to chronic symptoms. That’s the sort of mainstream expert medical view of the disease, but a lot of other people believe that Lyme disease is much more serious: That it’s not easily treated by oral antibiotics, that it requires multiple courses of intravenous antibiotics, and that it can cause all kinds of symptomatology, including chronic fatigue, weakness, and various other neurological manifestations. This group originally supported a Lyme disease vaccine, but they turned against it when the success of the vaccine seemed to undermine their alternative view of Lyme disease. The very definition of the disease used in the clinical trials was this narrow acute problem version.
Before introducing the vaccine, there was some issues with the immunological criteria to diagnose Lyme disease. Because clinicians use immunological tests to diagnose the disease, there was concern that there would be overlap between people who were vaccinated and people who looked like they had the disease. So, they changed their criteria and some people in the Lyme disease community got really angry about the narrowing of immunological criteria for diagnosis. Additionally, the more lay oppositional view posited a possible immunological mechanism for the chronic symptoms of Lyme disease, basically a kind of autoimmune reaction to the offending spirochete. If you believe that theory, then you worry that a vaccine could cause long-term problems because vaccines work by inducing immunity. As of today, there is no Lyme disease vaccine for humans currently available largely because of this particular context and other factors such as medical ambivalence about a vaccine against a treatable, non-deadly disease in comparison to, say, the often untreatable and potentially deadly consequences of HPV infection, which does have a vaccine. Ultimately, the context and the details surrounding vaccines matter when talking about the vaccine hesitancy that may arise in each case.
Read More from Omnia
New faculty.
Penn Arts & Sciences welcomed 18 new faculty members for the 2023–24 academic year.
How the Modern Story of Postwar Anti-Racism Ignored the Global South
Science historian Sebastián Gil-Riaño explores the lives of scientists who shaped one of the first international efforts to combat racism—and then got left out of the story.
60-Second Lectures | Fall 2023 Roundup (Video)
This fall’s 60-Second Lectures included a special Constitution Day edition and 1.5 Minute Climate Lectures during Climate Week at Penn.
About OMNIA
Editorial Offices
School of Arts & Sciences University of Pennsylvania 3600 Market Street, Suite 300 Philadelphia, PA 19104-3284 Phone: 215-573-4981 Fax: 215-573-2096 Email: [email protected]
Subscribe to the Podcast

- Penn WebLogin
How COVID Changed the World
Lessons from two years of emergency science, upheaval and loss

Olena Shmahalo
Nasal Spray COVID Preventives Are Finally in Development
Different methods of drug delivery give us more tools to fight disease
Megha Satyanarayana
COVID’s Uneven Toll Captured in Data
Visualizing ongoing stories of loss, adaptation and inequality
Amanda Montañez, Jen Christiansen, Sabine Devins, Mariana Surillo, Ashley P. Taylor
The Pandemic Showed the Promise of Cities with Fewer Cars
Residents learned what was possible. Some politicians fought to keep it that way
Andrea Thompson
How a Virus Exposed the Myth of Rugged Individualism
Humans evolved to be interdependent, not self-sufficient
Robin G. Nelson

The Pandemic Deepened Fault Lines in American Society
COVID energized the Black Lives Matter movement—and provoked a dangerous backlash
Aldon Morris

COVID Disrupted Everything—Even Rocket Launches
Surprising supply chain breakdowns

Vaccine Inequality Has Shut Vulnerable People Out of Plans to Save the Planet
Those with the most at stake were heard the least
Nnimmo Bassey

COVID Is Here to Stay
How do we live with it?
Christine Crudo Blackburn

Messenger RNA Therapies Are Finally Fulfilling Their Promise
Instructing our cells to make specific proteins could control influenza, autoimmune diseases, even cancer
Drew Weissman

We’re No More Serious about the Climate Crisis Than We Were before the Pandemic
Emergency managers are stuck reacting to a constant march of disasters
Samantha Montano

Introducing 21 Ways COVID Changed the World
The pandemic didn’t bring us together, but it did show us what we need to change the most
Jen Schwartz

COVID Long Haulers Are Calling Attention to Chronic Illnesses
But society is not prepared for the growing crisis of long COVID
Meghan O'Rourke
- Ethics & Leadership
- Fact-Checking
- Media Literacy
- The Craig Newmark Center
- Reporting & Editing
- Ethics & Trust
- Tech & Tools
- Business & Work
- Educators & Students
- Training Catalog
- Custom Teaching
- For ACES Members
- All Categories
- Broadcast & Visual Journalism
- Fact-Checking & Media Literacy
- In-newsroom
- Memphis, Tenn.
- Minneapolis, Minn.
- St. Petersburg, Fla.
- Washington, D.C.
- Poynter ACES Introductory Certificate in Editing
- Poynter ACES Intermediate Certificate in Editing
- Ethics & Trust Articles
- Get Ethics Advice
- Fact-Checking Articles
- International Fact-Checking Day
- Teen Fact-Checking Network
- International
- Media Literacy Training
- MediaWise Resources
- Ambassadors
- MediaWise in the News
Support responsible news and fact-based information today!
What makes vaccine skeptics change their minds?
Here are some of the main motivators for people who were opposed to taking the covid-19 vaccine to change their minds..

The Kaiser Family Foundation wanted to know what motivates people who were opposed to taking the COVID-19 vaccine to change their minds and obtained some insightful data.
Here are some of the main motivators (which I edited for length). You really should go to the KFF website to pull the data to develop this story. It might also give you insight into what messages resonate with people who need to hear it most.
One-fifth of adults (21%) now report being vaccinated after saying in January they planned on waiting to get vaccinated, would only get it if required, or would definitely not get vaccinated. Many of these individuals noted the role of their friends and family members as well as their personal doctors in persuading them to get a vaccine. Seeing their friends and family members get vaccinated without serious side effects, talking to family members about being able to safely visit, and conversations with their personal doctors about their own risks were all persuasive factors for these individuals.

(Kaiser Family Foundation)
A small but meaningful share also say the easing of restrictions for vaccinated people was a factor in their decision to get a vaccine.

When asked to name the feeling that best describes how they feel now that they have been vaccinated, nearly a quarter of vaccinated adults offer responses around feeling safe (24%) and relieved (22%). Other positive feelings reported were freedom, confidence, and more certainty that if they did get COVID-19 it would be less serious or they were less likely to die from it. Conversations with family members and friends have played a major role in persuading people to get vaccinated. 17% of adults who are now vaccinated (after saying in January they planned on waiting to get vaccinated, would only get it if required, or would definitely not get vaccinated) say they were persuaded to do so by a family member and 5% say they were persuaded by a friend.

Others cite protecting friends and family members as the main reason for getting vaccinated and others offer being able to see their friends and family members as well as family pressure or encouragement as the main reasons why they chose to receive a vaccine. When asked what would motivate them to get vaccinated against COVID-19, most in the “wait and see” group say they just want more time to see how the vaccine affects others who have already gotten it.
The Kaiser polling shows that a substantial number of people are concerned about the side effects of the vaccination. They say they can’t afford to be sick for a few days. They say they want to wait until the vaccine has been in use for a year, then they will consider it.
Another research project involving vaccine skeptics by Echelon Insights involved millions of social media posts, as well as tracking polls. It even takes a global view of why people turn down vaccines. It found that among vaccine skeptics or opponents, one of the most persuasive messages would be that former President Donald Trump took the vaccine and supported its rapid development.
This article originally appeared in Covering COVID-19 , a daily Poynter briefing of story ideas about the coronavirus and other timely topics for journalists. Sign up here to have it delivered to your inbox every weekday morning.

Opinion | NPR suspends an editor for his essay blasting … NPR
The firestorm caused by Uri Berliner’s critical essay in The Free Press continues to rage

Taylor Swift has not endorsed Joe Biden for president
As of mid-April 2024, Swift has not issued a public endorsement for the 2024 presidential election, despite social posts claiming otherwise

Opinion | Reaching its limits: CNN’s Gayle King-Charles Barkley show ends
A once-a-week show on Wednesday at 10 p.m. Eastern? Who thought this was a good idea?

Two new books are essential reading for anyone considering a news startup
One tells the stories of entrepreneurs taking the plunge. The other focuses on the tools, techniques and trends across an evolving media landscape


‘I’m seeing on a very personal level how challenging it is to be a younger reporter these days.’
The Dallas Morning News’ Tom Huang on why he’s championing this Poynter training for early-career journalists
Start your day informed and inspired.
Get the Poynter newsletter that's right for you.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Hum Vaccin Immunother
- v.17(12); 2021
Vaccines and vaccination: history and emerging issues
Veysel kayser.
Sydney Pharmacy School, Faculty of Medicine and Health, The University of Sydney, Sydney, NSW, Australia
Iqbal Ramzan
Prophylactic vaccines are crucial in modern healthcare and have been used successfully to combat bacterial and viral infectious diseases. Infections like polio and smallpox, which were dreaded historically, and which devastated the human race over many centuries, are now rare. Smallpox has been eradicated completely and polio is nearly eradicated because of vaccines. Vaccines differ fundamentally from other classes of medicines in that they are usually administered as a preventive measure to a healthy individual rather than to a sick person already with an infection, although exceptions to this practice exist. Most currently used prophylactic vaccines are based on established platforms, but many vaccine candidates, in late development stages, including several COVID-19 vaccines, use highly novel vaccine platforms not available historically. History of infectious diseases and prophylactic vaccines are filled with important scientific lessons, and thus provide valuable insights for the future. With hindsight, historically there were some ethically questionable approaches to testing vaccines and the germ warfare against native populations in the Americas and other regions. In this review, we examine key historical lessons learned with prophylactic vaccines with reflections on current healthcare dilemmas and controversies with respect to influenza and COVID-19 vaccines.
Introduction
Vaccination has been relatively successful in preventing many childhood-related infections and saving millions of lives. Well in excess of 10 million lives were saved between mid-1960s and 2015 with viral vaccines 1 , 2 such as measles, mumps, rubella, chickenpox and hepatitis A, produced from acceptable cell culture substrates. However, approximately 1.5 million children under 5 years still die annually from vaccine-preventable diseases, mainly due to the lack of access to essential childhood vaccines. 3 , 4 By contrast, major pathogens, including smallpox, polio, rabies that killed hundreds of millions of individuals in the last few centuries, are largely under control because of availability of safe and effective prophylactic vaccines. The WHO estimates that currently available vaccines prevent 2–3 million deaths worldwide annually. 3 Smallpox was eradicated formally about 40 years ago and animal borne virus, rinderpest, was the second pathogen to be eradicated, in 2011. Remarkable progress has been made toward eradicating Polio due to global vaccination efforts since 1960s and relatively recent more effective single antigen vaccine or various combination vaccines 1 that contain inactivated polio virus. Polio is set to become the second human infectious virus that will be fully eradicated. Other vaccine preventable diseases are largely under control with more than 90% to 100% decrease in morbidity compared to 20 th Century annual cases because of protection that vaccines offer in conferring herd immunity 1 .
Early developments in inoculation (precursor to vaccination) were due to the efforts in Asia Minor, Africa and East Asian societies, in particular Chinese and Muslim countries. Later vaccine developments, particularly by British, French and German scientists contributed significantly to vaccine development between the 17 th –20 th Centuries. Spain was the first country to undertake a general public health vaccination program by transporting vaccines from Europe to the Americas to vaccinate millions of people against smallpox. 5
History provides many lessons in dealing with infectious diseases. It is also obvious that current efforts to combat COVID-19 as well as other potential future pandemics requires us to work in close collaborations globally since “no one is safe until everyone is safe.” This review critically examines key past successes with vaccine developments, as well as key mistakes made in the past in vaccine discovery and vaccination. The focus of this review is on active immunization using commercially developed vaccines rather than on passive immunization where an individual receives antibodies from another infected individual (or animal). We also highlight how certain human actions with respect to vaccines and vaccinations have affected indigenous populations in the colonized world with the goal that current vaccination efforts do not lead to similar catastrophic outcomes for marginalized populations.
Inoculation, Edward Jenner and Lady Montague – eradication of “Angel of Death”
Start of modern vaccination refers to the study by English physician, Edward Jenner, in the 18 th century. Jenner recognized that milkmaids infected with cowpox virus were immune to the smallpox virus. He injected pus from a pustule of a cowpox patient to his gardener’s son and subsequently challenged him with smallpox virus and observed that the child survived. His 1798 published findings is one of the most influential studies in medical history. 6 He named this practice Variolae vaccinae denoting cowpox; the term vaccine originates from the Latin word vacca for cow.
By today’s norms, Jenner’s experiment would be considered unethical, and his experiment had many flaws. However, this study was a precursor to the development of smallpox vaccine and paved the way for the discovery and development of many vaccines used currently. Smallpox was eventually eradicated in 1979 and children are no longer vaccinated against smallpox. However, smallpox vaccines are still stockpiled by various countries for threats against bioterrorism.
Prior to vaccines and vaccination, inoculation (also referred to as variolation or engrafting) was common globally; cultures in Asia Minor, Middle East, Africa, India and China, were already using inoculation to immunize children. 7 , 8 This practice firmly established the concept that an individual who recovered from a disease generally did not catch the same disease again.
Well before Jenner’s time, inoculation was widely used in Britain, New England, and Russia due to the efforts of Lady Montague (1689–1762), who learnt about inoculation in Istanbul. Lady Montague was herself disfigured by smallpox and her children were inoculated in Istanbul; she mentioned in her letters home how old women would inoculate children with attenuated/ inactivated smallpox viruses from prior mild cases. The practice also became widespread in Russia after Catherine the Great was inoculated, well before Jenner’s milkmaid and cowpox observation.
Similar developments were evolving in other regions; in Boston, an African slave, Onesimus (circa 1600s–1700s), detailed an inoculation that he had undergone which he claimed protected him from smallpox for life. This led to inoculation of many Bostonians once smallpox emerged as a major cause of death (1,000 deaths of the estimated population of 10,000 in the 1700s). 9 , 10
An alternative inoculation process, involving nasal insufflation of cotton buds that contained a small amount of powdered substance from smallpox, very likely from smallpox scabs, was also common in China and India. 11–13
Aftermath of the first vaccine
Inoculation, however, worked partially and occasionally caused serious complications or even death. Jenner’s success, therefore, was a major achievement and his results and related later experiments by Pasteur, Toussaint 2 and others, in animals and subsequently in humans for other infectious diseases, by transferring an artificially weakened (attenuated) pathogen (e.g., anthrax, rabies) from the same species (i.e., from animal to animal or human to human), were pioneering projects in modern vaccine discovery and development. These successes collectively led to vaccination as the major public health initiative to combat infectious diseases globally.
Colonization – consequences of infectious diseases in the colonies
Colonization by Spanish, British, French, Dutch and other European nations with the consequent spread of new European diseases like smallpox in the new colonies, drastically changed human history. This had a cataclysmic effect on many indigenous populations, causing precipitous declines in their populations due to lack of natural immunity. It is estimated that more than 20 million natives died in the 16 th Century not long after the Spanish established a new colony in Mexico because of previously unknown infections that Europeans brought to the continent. 14–17 This rapid decline in the native population had a subsequent effect on much needed workforce as new settlements required expanded workforce. In turn, the colonizers needed to identify new cheap workforce sources which resulted in massive slavery of Africans by European nations.
Similar outcomes were noted in other parts of the world where native populations suffered similar consequences of colonialism. The First Australians suffered 80–96% population loss during the first 10 years of European settlement in the 18 th Century; smallpox, measles and other diseases played a significant role. 18
There was also intentional spread of infections in the new colonies with similar catastrophic consequences, as a crude and primary form of biological warfare. One example is the deliberate attempt to spread smallpox in Massachusetts to native Americans via infected blankets and other material; mentioned in the letters of Sir Jeffery Amherst (chief of British forces in North America in the mid-18 th Century). 19 , 20 Deliberate spread of smallpox and perhaps other infectious diseases amongst native Australians was also suggested during European settlement in the late 18 th Century. 21
Vaccination in the Americas by the Spanish
The first mass vaccination campaign was probably the vaccination of millions of individuals in the Americas against smallpox by the Spanish in the early 19 th Century. Transporting vaccines to long destinations over many months, especially by sea was however, extremely difficult in the 19 th Century. The Spanish found a solution; creating a human chain, akin to cold chain that is used currently, to carry the vaccine to the New World. For this highly unethical and immoral chain, 22 orphans were taken on the voyage and one after another were infected until the expedition reached the colonies in the Americas. Several trips were then made to major settlements in North and South America, and subsequently millions were vaccinated against smallpox. 22–25
Eradication of “Angel of Death”
Variola viruses causing smallpox are of two major types: variola minor and variola major. Variola minor was a strain of smallpox that was less common and only caused mild infection. Variola major , however, was commonly known as the smallpox strain that originated approximately 3000 years ago either in Egypt or India and caused global havoc over many centuries. It bore many names like the Angel of Death and speckled monster. In the 20 th Century alone, smallpox caused 100–300 million deaths. 26 , 27
Victor Zhdanov (1914–1987), a highly influential Russian epidemiologist and deputy health minister of the Soviet Union advocated for the total eradication of the smallpox virus. Many were skeptical since previous eradication programs for malaria, yellow fever, hookworm and other infections had not been feasible. In 1959, the World Health Organization (WHO) undertook this challenge; progress was very slow until 1966, when an annual US$2.4 million funding was secured the appointment of well-known epidemiologist, Dr Donald A. Henderson (1928–2016), as the head of WHO’s Smallpox Eradication Unit. 27 Other relatively simple and novel approaches, such as the introduction of the bifurcated needle for vaccine administration, expedited the eradication program and it was easy to teach vaccinators who were not medically trained, the bifurcated needle also required much less vaccine so the production capacity was no longer the critical issue.
In 1975, “Operation Smallpox Zero” program was launched by WHO which was treated with skepticism by many experts. In 1980, the WHO officially declared that smallpox was eradicated due largely to a globally successful vaccination campaign that lasted many decades. It required international collaborative public health measures, adopting rigorous scientific principles and pragmatically adopting other methods as required, providing appropriate monetary support, and public involvement at many levels of society. Smallpox eradication is probably the greatest public health achievements in history. A similar eradication of polio is close to being achieved.
Summary of lessons from history
The preceding discussion on the history of vaccines and vaccination has provided useful lessons for the future of vaccines. These include:
- Colonization and its effects on emergence of infectious diseases especially in Indigenous populations and how to protect vulnerable native peoples.
- Importance of critical observations to document ways of protecting individuals as well as the general population against infectious diseases.
- Use of ethical testing practices for testing vaccine efficacy and safety.
- Importance of childhood and adult mass-vaccination programs to confer herd immunity in the population (e.g., lessons recently learned from outbreaks of mumps and pertussis) and to eradicate specific infections linked to specific contagions.
- Collaborative targeted international efforts, and injection of appropriate funds to bring about stepwise and rapid changes in vaccine development.
- The importance of political will, leadership and role models to promote greater acceptance of vaccines quickly especially in an era of vaccine hesitancy.
Keeping these lessons from the history of vaccines and vaccination in mind this review now moves to more contemporary considerations facing society in the era of recurrent influenza outbreaks and the current pandemic.
Types and classes of vaccines
Many vaccine types have been developed since Jenner’s historic breakthrough and majority of these vaccines are summarized in Table 1 and depicted in Figure 1 . Most of these vaccines, however, use established discovery/development platforms, where the pathogen is grown using cell culture. Globally, most of these vaccines are provided as pediatric vaccines. However, since Jenner’s time, and as a result of the many lessons learnt, novel methods and vaccine discovery strategies have evolved to arrive at safe and effective vaccines.
Vaccine immunization programs *
*This is not an exhaustive list. Adapted from the National Immunization Program Schedule of Australia, NWS Immunization Schedule and WHO. 28–32 Many other countries (like the US, UK) have specific lists to suit the vaccination programs in their individual countries.
**Vaccine brands are for Australia only; these may differ in other countries. Adapted from the Australian Immunization Handbook and NPS MedicineWise. 33 , 34

Different types/classes of vaccines. Vaccines are produced using different processes. Vaccines may contain live attenuated pathogens (usually viruses), inactivated whole pathogens, toxoids (an inactivated form of the toxin produced by bacteria that causes the disease), or parts of pathogens (e.g., natural or recombinant proteins, polysaccharides, conjugated polysaccharide or virus-like particles). Adapted from. 35
Conjugate vaccines, where a specific bacterial surface sugar group (i.e., polysaccharide) that is conjugated covalently to a toxoid (a chemically modified pathogen toxin, which is no longer toxic but is still antigenic and can be used as a vaccine), usually diphtheria or tetanus protein, have emerged. Conjugation is necessary since polysaccharides are weakly immunogenic, but toxoids elicit good immunogenicity while displaying fewer side effects. Combined conjugate toxoid vaccines have been developed against Haemophilus influenzae type b (Hib) and pneumococcus which are used as combination vaccines for childhood immunization ( Table 1 ). Recently new conjugated pneumococcal vaccines have been developed with additional pneumococcal capsular polysaccharide from different serotypes to provide broader coverage for different regions of the world.
Other childhood vaccines including diphtheria, tetanus, pertussis, polio, hepatitis B plus HibCV are constituents of the hexavalent pediatric vaccine ( Table 1 ).
Attenuated or inactivated viral vaccines are another vaccine class that use established platforms to prepare vaccines. In the attenuated vaccine, a pathogen is passed many times through cells until it is not infectious/ virulent in humans. Some of the influenza and polio vaccines are examples of attenuated vaccines. In such vaccines, the virus is inactivated chemically or using elevated temperature so that it cannot reproduce anymore. Chemical inactivation uses either formalin, β-mercapto-ethanol or other similar chemicals, Rabies vaccine is an example. 36 Occasionally, further processing is needed to split the virus to prepare a subunit vaccine with fewer side effects. Some influenza vaccines are examples of this kind of vaccine. Usually, a surfactant, like Triton-100, is used to split the virus. Exposing the virus to a surfactant induces splitting by dissolving the viral membrane and exposing inner regions of the virus. This process is used for most annual seasonal influenza vaccines. Formulation stability is a major issue with this process since splitting generates a non-homogeneous mixture.
Novel vaccine platforms have emerged in recent years including nucleic acid-based (e.g., mRNA), nanoparticle complex formation or viral vector based-vaccines that have been used to develop COVID-19 vaccines and other emerging vaccines. In the nucleic acid type vaccines, DNA or RNA representing a small section of a virus, for example, surface protein, is used as the antigen. In the case of mRNA, an encapsulating delivery system needs to be used since RNA is highly unstable and is short-lived in the body. Pfizer/BioNTech, Moderna and other COVID-19 vaccines are of this class. Research on nucleic acid (both RNA and DNA)-based vaccines have been ongoing for many decades. However, only recently RNA vaccine efforts have come to fruition and generated multiple, hugely successful mRNA vaccines for COVID-19, while no successful human DNA vaccine exists currently.
With the viral vector system, a part of the target virus is incorporated into a different virus that is harmless and nonreplicating. As a vector or carrier, adenoviruses (of human or animal origin) that cause common cold, or measles, vaccinia or other viruses may be used. Examples of this type of vaccines include Merck’s Ebola vaccine Ervebo®, which is an attenuated recombinant vesicular stomatitis viral vaccine, AstraZeneca’s and Johnson & Johnson’s COVID-19 vaccines which both use chimpanzee adenovirus viral vector while Sputnik V COVID-19 vaccine uses a human adenovirus vector, and Bavarian Nordic’s smallpox vaccine, Imvanex®, that uses a modified Vaccinia Ankara vector among other vectors.
Current vaccines and immunization programs
Recent step-wise refinements in vaccine discovery/development have led to a paradigm shift in the management of infectious diseases and vaccines are now an integral part of modern healthcare and are first-line defense to prevent human infections. In addition to inactivated or attenuated vaccine production methods, subunit, recombinant vector using short DNA/RNA fragments and polysaccharide vaccines have been developed. Sixteen childhood and adolescent vaccines 37 are now routinely administered from birth to age 4 years ( Table 1 ); most of these vaccines require multiple doses to elicit long-lasting immunity. Some of these vaccines are combination vaccines such as DTaP-HepB-IPV (diphtheria, tetanus, and acellular pertussis, hepatitis B, and inactivated poliovirus vaccine).
While many childhood vaccines provide life-long immunity, the protective effects of some vaccines decline with age, requiring additional booster shots ( Table 1 ). For example, a single dose of measles vaccine provides over 90% protection that lasts a lifetime, but booster shots are required to bring the protection to higher levels. Influenza is an exception to this; instead of booster doses, seasonal influenza vaccines are administered each year because of influenza viral shift and drift. At present, trivalent or quadrivalent seasonal influenza vaccines are available for children 6 months and older as well as adults. 38 Hunt for a universal influenza vaccine is vigorously being pursued by both vaccine industry and academia. Such efforts focus primarily on the constant regions of the virus such as the M2 protein or the stem of HA both of which have not shown mutations over the years. However, these viral domains are not very immunogenic and hence a successful universal influenza vaccine candidate is yet to be identified.
Other vaccines such as for travel vaccinations also exist and are administrated as required against many different types of pathogens ( Table 1 ). These include for example, seasonal influenza, yellow fever, rabies and zoster vaccines. WHO provides recommendations for routine immunization schedules for these 39 and each individual country adopts a schedule of vaccination from birth to adolescence; most country schedules are highly similar. As a result of vaccine hesitancy and regional conflicts (like the Yemen and Syrian wars), highly infectious vaccine-preventable diseases such as measles are on the rise in many countries including some developed countries and various public health measures have been implemented to increase mass vaccination programs (for example, mandating vaccination prior to school admission/entry).
Pandemic readiness – emerging issues with current influenza vaccines
Pandemic preparedness schemes were adopted by some countries following the 2005 bird influenza outbreak, the 2009 swine influenza pandemic and the 2014–16 Ebola outbreak. Many nations, including Australia, launched their pandemic (and biosecurity) procedures at the start of the COVID-19 pandemic. However, according to the Global Preparedness Monitoring Board (GPMB) and the WHO, no country was fully prepared or could mitigate global health emergencies like the current coronavirus outbreak. 40 , 41 The existing pandemic readiness frameworks were insufficient for the global COVID-19 pandemic caused by SARS-CoV-2; partly because most preparedness schemes were established to deal with only an influenza pandemic.
Influenza avoids our immune system due to extensive viral drift (small number of mutations in the viral gene leading to changes in key surface glycoproteins [hemagglutinin, HA, and neuraminidase, NA]) and shift (a major structural change in virus, giving rise to a new HA and/or NA, which may be categorized as a new subtype), 42 requiring vaccination annually. 43 , 44 The WHO reports that over 500,000 individuals die annually from influenza, 43–46 including high-risk groups (children, the elderly and pregnant women). The USA Centers for Disease Control and Prevention (CDC) estimated that the 2009 influenza pandemic, caused by Influenza A (H1N1pdm09 – the swine influenza), killed approximately 600,000 individuals. 47 , 48 The COVID-19 pandemic has revealed that the world was not prepared for a more virulent pandemic virus that can spread and kill rapidly and extensively.
There have been many other influenza pandemics in history such as the Russian influenza in 1889 (which killed ~1 million), Asian influenza in 1957 (~1.1 million deaths), Hong Kong influenza in 1968 (1 million casualty); with the 1918 Spanish influenza being the most deadly (50 million deaths, ~5% of the world’s population at that time). 49 Another influenza pandemic is expected by many experts, thus understanding historical and emerging influenza outbreaks might assist in dealing swiftly when another pandemic emerges.
Current influenza vaccines: element of ‘guessing’ and hit-and-miss efficacy
Current influenza vaccines consist of one influenza A strain (H1N1) and (H3N2), together with one or two influenza B virus strains that are used in either the trivalent or quadrivalent vaccines respectively. 50 There are 18 different subtypes of hemagglutinins (HA) and 11 subtypes of neuraminidases (NA) in influenza viruses. 50 Only a small number of influenza A viruses, mainly H1N1 and H3N2 subtypes, have humans as hosts.
The critical public health issue is the selection of the viral strain (subtype) for seasonal influenza vaccines as this directly affects the vaccine’s efficacy. The WHO reviews worldwide viral surveillance data to determine which strain(s) to recommend annually for different regions. Mismatch between ‘guessed’ or ‘predicted’ strains (vaccine components) and actual circulating viral strains at a particular time in a specific region results in the vaccine’s relatively poor performance. 51 While artificial intelligence (AI) and machine learning (ML) may provide better predictions of the viral strains for annual vaccines, these techniques are in their infancy. 52 Each viral strain is produced separately and mixed with the other strain(s) to yield either a trivalent or quadrivalent influenza vaccine.
Influenza vaccines are 60–85% effective in children and 30–60% in adults <65 years old. 53 In the last several decades, however, the effectiveness has fluctuated considerably and sometimes it is as low as 10%. Over the last several years, seven influenza variant strains have been observed; this rapid emergence of different strains is very concerning.
Moreover, different surfactant amounts are required to split different influenza viral strains, reflecting different intrinsic viral structural stabilities (unpublished observations from the primary author). This may result in the proportions of unsplit virus being for different strains viruses. Additionally, influenza viruses have a diverse range of HA and NA sequences and somewhat dissimilar glycosylation profiles, 54 which would affect their intrinsic stabilities and the types/amounts of protein aggregates formed. In general, however, each strain undergoes an identical manufacturing process and these critical quality attribute differences are not routinely considered during manufacturing, due to lack of sensitive methods to reliably detect virion differences. Such issues need to be understood fully to yield vaccines with high formulation stabilities. 55
Lack of sensitive in-situ methods in vaccine manufacturing
Many of the R&D issues with vaccines are known, however, regulatory agencies are slow to implement new developments. An example is the widely used Single Radial Immunodiffusion (SRID) assay, 56 developed in the 1960s, and still used to determine HA content and vaccine stability/potency. More sensitive techniques have been developed as alternatives but these are not commonly accepted either by the vaccine industry or regulatory agencies. Relying on SRID to estimate vaccine formulation stability/potency may be misleading especially for those vaccines that contain inadequately split virus; other techniques are thus urgently needed.
Lack of manufacturing controls and insufficient product characterization
Many parameters influence influenza vaccine stability including for example, flock age for egg-based vaccines, initial titer concentration, type of surfactant, initial and residual surfactant concentrations, number of filtration steps and final HA concentration. Several unanswered questions with respect to influenza vaccine development/manufacturing include:
- What other process-parameters directly affect virus yield?
- What is the relationship between viral yield and virus strain?
- Does immunosuppression have a considerable impact on yield?
- What is the temperature sensitivity of the virus yield?
- What is the effect of inoculate concentration on virus yield?
- What (and how much) growth factors and/or nutrients enhance virus growth?
- How does glycosylation (type/extent) of the virus influence yield?
- How do different surfactants (and their concentrations) interact with the virus?
- How does intrinsic virus stability influence final (finished) formulation stability?
- What type of particles are formed during manufacturing?
- Can we elucidate aggregation of HA in detail and how this affects formulation stability?
- Can we develop rapid and sensitive potency ranking/screening methods?
- How do different additives affect stability?
Understanding these vaccine formulation issues would lead to more precise control of each vaccine production step and a consistent viral yield in each vaccine batch.
Vaccine supply and demand gaps
From the current global influenza vaccine manufacturing capacity, there would be a vaccine shortage if another influenza pandemic emerged. Although cell-based influenza vaccine manufacturing platforms exist, majority of the current influenza vaccines are egg-based. The current annual capacity for producing a pandemic influenza vaccine is estimated primarily on the capacity to produce the current seasonal vaccine. The world’s annual capacity for the production of egg-based influenza vaccine is approximately 1.5 billion doses for seasonal vaccine and about 8 billion doses for a potential influenza pandemic. 57 As a result, only ~60% of the world’s population would have enough vaccine in one year if another influenza pandemic was to occur. Two billion more doses would be required to vaccinate the desired 70% of the population to confer herd immunity. 57 Limitations to pandemic influenza vaccine availability are: (i) need to plan at least 6 months ahead, (ii) availability of sufficient chicken eggs of the right quality, (iii) unpredictable viral yields, and (iv) very low viral yield per embryonated chicken egg for some viral strains. 58 , 59 These limitations also result in higher manufacturing costs, limited production volumes and unequitable vaccine distribution globally. New influenza vaccine manufacturing/formulation technologies are therefore urgently needed.
COVID-19 vaccines – a paradigm shift in vaccine development
Sars-cov-2 generated covid-19 pandemic.
Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) is the novel coronavirus ( Figure 2 ) that emerged in China in late 2019 and caused Coronavirus Disease 2019 (COVID-19) which is now a pandemic. So far (July 2021), the confirmed cases have exceeded hundred millions of cases globally and 4 millions of deaths. 60 A recent estimate found that its basic reproductive number (R 0 ) is between 3.6 and 6.1 depending on the country 61 with an incubation time of 2–14 days. More critically, asymptomatic individuals spread the virus rapidly, making SARS-CoV-2 one of the most transmissible viruses. 62–64 This was very concerning initially since there was no therapy and vaccines have only now become available. However, many countries implemented their pandemic readiness frameworks or biosecurity action procedures well before WHO’s COVID-19 pandemic declaration. However, no country was fully prepared for this pandemic, 40 , 41 especially as more virulent (delta) strains emerge.

A highly simplified representation of the SARS-CoV-2 cell cycle. (A1) Virus entry generally occurs via surface glycoprotein (Spike protein, S-protein) binding to ACE2 receptor, TMPRSS2 also has a critical role to play in this process. Detailed interactions between S protein–ACE2 are also shown (courtesy of Dr. Serdar Kuyucak, USyd (A2). The virus can also enter by endocytosis (B&C). Subsequently, uncoating of viral proteins, primary translation, polyprotein processing and transcription take place. (D). Translation and viral RNA synthesis then occur (E). Other key steps such as accessory protein-host interactions take place prior to assembly and viral maturation. (F). Finally, release of mature viruses occurs via endocytosis.
Coronaviruses on the rise
Multiple coronavirus outbreaks have occurred since the early 2000s; original SARS-CoV-1 in 2002–3, several swine coronaviruses cases, Middle East Respiratory Syndrome (MERS), and finally SARS-CoV-2 in 2019; clearly coronavirus infections are on the rise. While all these outbreaks originated from bats, intermediate hosts include civets for SARS-CoV-1, camels for MERS while the intermediate host for SARS-CoV-2 is yet to be firmly established. The virus has surface glycoproteins called Spike protein (S-protein) that play a key role in cellular attachment and entry into the host ( Figure 2 ). It is also the main target for immunity and hence many vaccines use S-protein as the antigen. SARS coronavirus is one of the largest single strand RNA viruses but unusually it has a proof-reading mechanism, so for example, compared to Influenza, it mutates more slowly. Nevertheless, it is an RNA virus, so it still mutates and different variants of SARS-CoV-2 including the UK, South Africa, India, California and Brazil variants, have appeared within a year or so. Some of these variants (like the delta variant) are more virulent and spread more rapidly but their full characteristics are yet to be fully determined. These variants are a major concern in case the immunity afforded by current vaccines do not protect individuals fully against emerging variants.
Role of regulatory agencies – approval of COVID-19 vaccines
One of the lessons learnt from history with respect to small molecule drugs and vaccines is a robust but timely approval and drug registration framework. Role of regulatory agencies in each country is generally clear and transparent; in general, the public has confidence in the drug (vaccine) approval process. Regulatory reviews of new vaccines to ensure quality, safety and efficacy has traditionally been a lengthy and slow process. Every R&D and manufacturing step, safety, efficacy and stability data must be examined prior to granting approval. Several years ago, new approval pathways were introduced in different jurisdictions to expedite approval; for example, Investigational New Drug (IND) Application, Priority Review, Breakthrough Therapy, Accelerated Approval, and Fast Track pathways by the USA’s FDA, 65–67 and PRIME ( Pri ority Me dicines) of the European Medicines Agency (EMA). 68 These pathways are generally more rapid than the traditional pathways; however, there are strict conditions for a medicine to be considered via these expediated pathways, like an unmet medical need. During this COVID-19 pandemic, however, there has been criticism of regulatory agencies for taking too long to approve a particular vaccine, especially if the same vaccine was approved in another jurisdiction. In contrast, regulatory agencies also faced criticisms about by some for approval of some vaccines too rapidly so that quality, safety, and efficacy attributes might have been compromised. What this pandemic has demonstrated though is the ability of regulatory agencies to be responsive to public demands for timely approval of vaccines in an environment where there are very few other mechanisms for controlling the pandemic.
Specific COVID-19 vaccines
As of July 2021, 21 vaccines have been authorized for emergency use in different jurisdictions and over 300 are in various stages of development. 69 , 70 Major approved vaccines, listed in Table 2 , fall into two categories: those based on established platforms, e.g., inactivated virus, and those based on novel vaccine platforms, e.g., mRNA-based vaccines. The latter can be further categorized as nucleic acid-based or viral vector-based vaccines, which are the two major classes.
Major approved COVID-19 vaccines for emergency use †
† Approvals in most countries are for Emergency Use only.
*Adapted from. 71 , 72
**Adapted from. 73–75
# Not an exhaustive list of countries.
Vaccines using novel platforms include mRNA-based vaccines (Pfizer/BioNtech and Moderna), adenovirus vector-based vaccines (AstraZeneca/Oxford University, Johnson & Johnson and Sputnik V), and protein-based (Novavax). Vaccines that have been prepared using established platforms use inactivated virus (CoronaVac TM by Sinovac, Sinopharm vaccine, and Covaxin® by Bharat Biotech). Prior to COVID-19, no vaccine on the market had utilized these novel platforms; therefore, every aspect of this vaccine development paradigm has required detailed regulatory scrutiny. The various clinical trial phases (I to IV) are traditionally designed to facilitate intense scrutiny but the design of these vaccine trials were very diverse. For example, many differences between trial protocol end-points might have existed although Pfizer, Moderna, AstraZeneca and Johnson & Johnson trials apparently had similar primary endpoints. 76 Other parameters may have affected efficacy assessments, for example, during the clinical trials of the AstraZeneca vaccine, results from different countries varied, presumably due to dosing errors.
The various phases of vaccine trials are designed to examine quality, safety, and efficacy of the product; if these attributes are sub-optimal, theoretically these would be picked up during one/more of the trial phases. This is what was observed for the University of Queensland (UQ) vaccine candidate; trials were discontinued due to an intrinsic design problem in the foundation technology. A ‘molecular clamp’ was employed to maintain the trimeric S-protein conformation, as in the actual virus, via a peptide from HIV as ‘a clamp.’ However, during phase I trials, some volunteers displayed false positive results in HIV tests and hence the trial was discontinued to prevent a potential public health distrust in the vaccine. 77
Rapid approval and use of Sputnik V vaccine in Russia, and Sinovac and Sinopharm vaccines in China, before human phase III trials were completed, have raised concerns about possible political interference in the approval processes in these countries. These controversies, however, did not hinder the early roll-out of these vaccines in many countries. 78 For example, Sinovac vaccine was used in Turkey, UAE, Indonesia, and Brazil before any peer-reviewed publications became available on clinical trial evidence. Turkey traditionally requires EMA approval for new vaccines and medications, but mass vaccination started in the country without such approval. Some of these vaccines have subsequently been shown to be safe and effective. 79
Most vaccines against SARS-CoV-2, the virus causing the COVID-19 pandemic, herald a new scientific era in vaccine discovery, development and manufacture. It is unprecedented historically that several COVID-19 vaccines have become available so rapidly for a pathogen that has initiated a pandemic within a year of its genetic sequence being determined. Vaccine development processes are generally slow, taking on average up to 10 years to develop a vaccine. In addition, many diseases including HIV AIDS do not have a vaccine, even after several decades of intense research. There are several reasons for this rapid development of COVID-19 vaccines:
- Most of the vaccine platforms (like mRNA or viral vector delivery) were already established.
- Large-scale vaccine clinical trials and large-scale manufacturing are two very expensive and risky steps in vaccine development. Significant funding from agencies like The Gates Foundation, many governments and philanthropists from around the globe added significant momentum to the discovery process.
- Some clinical trial phases were run in parallel or combined, e.g., phase I & II trials were combined or phase II trial was conducted with a large group of volunteers and overlapped with phase III trials.
- There was no shortage of volunteers for these trials in many countries.
- Rapid peer-reviewed publications (sometimes 1 week after submission) and availability of manuscripts in open access format facilitated scientific scrutiny of key findings.
- Recent prior history with human coronaviruses.
- Rapid identification of virus protein sequence including neutralization epitopes of S protein as the major antigen.
- Ability to grow SARS-CoV-2 rapidly in different cell lines and to assay the virus (and its variants) accurately and rapidly.
Some concerns have emerged about several COVID-19 vaccines related to serious but rare adverse reactions such as blood clots with low platelet numbers, thrombocytopenia syndrome 80 from AstraZeneca vaccine, resulting in public health recommendations for this vaccine in individuals over 50 years in Australia and over 30 years in the UK. With new technologies, rare but serious side- effects may only be observed once mass vaccination begins as is the case with the Astra Zeneca vaccine. Johnson & Johnson vaccine, being a vector-based vaccine is also under scrutiny for blood clots. Other ongoing concerns include lack of full efficacy against newly emerging viral variants. Another adverse event is anaphylaxis observed with Pfizer/BioNtech mRNA-based COVID-19 vaccine in individuals with prior history of severe allergies. 81 , 82
To ease global travel restrictions amid this pandemic, fresh discussions on vaccine passports have started. Some countries see such passports necessary for safe international travel and opening of borders while in some jurisdictions it is argued that mandatory vaccinations and other forced restrictions would diminish legal rights. 83
The current COVID-19 pandemic has highlighted the gap between global supply and demand for vaccines. Several European Union (EU) countries blocked export of COVID-19 vaccines that were manufactured in mainland EU 84 , 85 including a shipment to Australia. 86 Similarly, India temporarily blocked shipments of COVID-19 vaccines manufactured by Serum Institute of India because of rapidly rising COVID-19 cases in India. 87 To ensure a globally equitable and responsible access to COVID-19 vaccines, a collaboration between WHO, Gavi, the Vaccine Alliance, The Coalition for Epidemic Preparedness, CEPI and United Nations Children’s Fund, UNICEF have established COVAX, whose aim is to accelerate the development and manufacture of COVID-19 vaccines, and to guarantee fair and equitable access for every country. 88 COVAX has already delivered some vaccines to needy regions of the world; however, underdeveloped countries (who often have the greatest need) have experienced severe vaccine shortages during this COVID-19 pandemic.
What happens if annual COVID-19 vaccinations are necessary?
Vaccines against SARS-CoV-2 may stop individuals getting sick or reduce the severity of disease; however, the virus might still be prevalent in the environment. In addition, because of relatively slow mass vaccination rates, global herd immunity may not be achieved in a timely manner and more virulent variants with more extensive mutations may emerge which may lead to new strains. To make matters worse, the virus might be able to jump to another animal host. In such a scenario, annual COVID-19 vaccinations might be necessary, as with seasonal influenza vaccination. A more elegant approach might be to develop a combination influenza–COVID-19 vaccine. This is being contemplated but such a combination vaccine would require either similar or complementary platforms (either SARS-CoV-2 needs to be grown in eggs or influenza virus needs to be cultured in the same cell line as SARS-CoV-2) and would need to be in acceptable final vaccine preparations (like fully liquid and thermostable). A combination vaccine might also overcome current issues with COVID-19 vaccines (inadequate manufacturing capacity, storage, transport and delivery). A combination vaccine might also be “self-adjuvanting,” where the relatively low effectiveness of current influenza vaccines might be enhanced.
Conclusions
Vaccine development has traditionally been a slow and arduous process, but significant collaborative/targeted international research efforts and injection of substantial amounts of money have resulted in successful vaccine developments within a much shorter timespan especially during this pandemic. WHO has been listing ongoing prophylactic vaccine clinical trials since 2007; 89 trials in progress include vaccines for HIV, malaria, TB, Zika, Ebola and of course SARS-CoV-2.
Despite these remarkable vaccine discovery advancements, unwavering collaborative research is urgently needed to maintain such stepwise discoveries in vaccine development and timely commercial availability. Further advancements in vaccine discovery, development and formulation should pave the way for availability of much safer and more efficacious vaccines and restore much needed public confidence in vaccines and mass vaccination programs, as a key public health strategy, during pandemics.
1 A combination vaccine consists of several different vaccines in the same dosage form. Many childhood vaccines are combination vaccines such as VAXELIS™ (Diphtheria and Tetanus Toxoids and Acellular Pertussis, Inactivated Poliovirus, Haemophilus b Conjugate and Hepatitis B Vaccine).
2 Jean Joseph Henri Toussaint (1847–1890) was a French bacteriologist contemporary of Pasteur and worked on various infectious diseases like chicken cholera and tuberculosis. He is credited with the development of the first anthrax vaccine via chemical inactivation but during his lifetime only Pasteur received full recognition.
Disclosure of potential conflicts of interest
No potential conflict of interest was reported by the author(s).
- Work & Careers
- Life & Arts
Become an FT subscriber
Try unlimited access Only $1 for 4 weeks
Then $75 per month. Complete digital access to quality FT journalism on any device. Cancel anytime during your trial.
- Global news & analysis
- Expert opinion
- Special features
- FirstFT newsletter
- Videos & Podcasts
- Android & iOS app
- FT Edit app
- 10 gift articles per month
Explore more offers.
Standard digital.
- FT Digital Edition
Premium Digital
Print + premium digital, weekend print + standard digital, weekend print + premium digital.
Today's FT newspaper for easy reading on any device. This does not include ft.com or FT App access.
- 10 additional gift articles per month
- Global news & analysis
- Exclusive FT analysis
- Videos & Podcasts
- FT App on Android & iOS
- Everything in Standard Digital
- Premium newsletters
- Weekday Print Edition
- FT Weekend Print delivery
- Everything in Premium Digital
Essential digital access to quality FT journalism on any device. Pay a year upfront and save 20%.
- Everything in Print
Complete digital access to quality FT journalism with expert analysis from industry leaders. Pay a year upfront and save 20%.
Terms & Conditions apply
Explore our full range of subscriptions.
Why the ft.
See why over a million readers pay to read the Financial Times.
International Edition
- Share full article

We Have Tick Medications for Dogs. Why Not for People?
Certain concerns have hindered development, but several Lyme prevention drugs are currently being tested in humans.
Credit... Getty Images
Supported by

By Dana G. Smith
- April 16, 2024
Q: Every three months, I give my dog a beef-flavored chew that kills any ticks that bite her. She has also been vaccinated against Lyme disease. Why don’t these options exist for people?
“It’s funny, in Lyme disease, animals have so many more options than humans do,” said Dr. Linden Hu, a professor of immunology at Tufts University School of Medicine. That includes several Lyme vaccines, as well as oral and topical tick-prevention medications.
Safety concerns and doubts about public acceptance have hindered the development of these types of drugs for people. But with rates of Lyme and other tick-borne illnesses increasing in recent years, researchers are exploring new (and old) options, and a few are now being tested in human clinical trials.
Between 1999 and 2002, there actually was a human vaccine for Lyme disease available in the United States. The drug, called Lymerix, was approved by the Food and Drug Administration in 1998 after clinical trials deemed it safe and effective for preventing infection with Lyme-causing bacteria. It was recommended for people between the ages of 15 and 70 who were living or working in areas where Lyme disease was common.
Shortly after people started receiving the shots, reports of side effects emerged, most notably symptoms of arthritis. Federal health officials “looked at it very carefully” and didn’t find evidence that the vaccine was unsafe, said Dr. Erol Fikrig, an infectious disease expert at the Yale School of Medicine, who was involved with developing the drug.
But the reputational damage had been done. Sales of the Lyme vaccine plummeted, and in 2002, GlaxoSmithKline, which manufactured the drug, pulled it from the market.
The Lyme vaccines that currently exist for dogs are similar to the one that was developed for humans. Both vaccines work primarily by prompting the immune system to create antibodies to a protein called OspA, which is produced by the Lyme-causing bacteria that are transmitted through tick saliva. When a tick ingests a dog’s blood, the antibodies kill the bacteria residing in the tick’s gut, preventing them from causing an infection.
In recent years, the pharmaceutical companies Pfizer, Valneva and Moderna have developed two new vaccines for humans that target the same OspA protein, though other aspects of the shots have been changed from the original version, Dr. Fikrig said. Both vaccines are currently being tested in clinical trials, and results are expected in a few years.
Topical and Oral Drugs
The other main prevention methods for pet owners are topical and oral treatments. These drugs, called acaricides, get distributed through the animal’s body after they’re swallowed or applied to the skin and kill ticks, along with fleas and mites, when they bite. A major advantage is that they protect against multiple tick-borne infections, not just Lyme disease.
For many of these illnesses, a tick must remain latched onto its host for a day or two to cause an infection, said Dr. Janet Foley, a professor of medicine and epidemiology at the University of California, Davis School of Veterinary Medicine. “So as long as you can kill that tick within hours, you’ll abort the possibility of transmitting anything like Lyme disease.”
While both the oral and topical medications are toxic to ticks, they’ve largely been proven safe for dogs at the doses used. However, Dr. Hu said that to his knowledge, few thought of investigating whether humans could also use them as prophylactics against tick-borne infections until recently.
An acaricide’s “toxicity for ticks is far, far, far greater than its toxicity for mammals,” Dr. Foley said. But, she added, it’s understandable that some people may be concerned about taking a drug that suffuses the body with a toxin just in case they get bitten by a tick. “I think that there wouldn’t be much market for that for people,” Dr. Foley said, though that’s “pure speculation,” she added.
One small drug company, Tarsus Pharmaceuticals, is betting that there might be such a market. In collaboration with Dr. Hu, it is testing whether an oral acaricide used in some veterinary tick medicines, called lotilaner, is safe and effective in people. (The drug was also recently approved as an eye drop for humans , to treat eyelid inflammation caused by mites.)
“We actually are one of the few examples of bringing a medicine from the veterinary side to the human side,” said Dr. Bobak Azamian, the co-founder, chairman and chief executive of Tarsus Pharmaceuticals.
According to the company, early clinical trials of lotilaner — provided to people as a pill, not a beef-flavored chew — showed that it was about 90 percent effective at killing ticks that bit the participants both on the day they took the medication and 30 days later. No major safety concerns have surfaced during the tests, Dr. Azamian said.
Still, it will be several years, and several more rounds of clinical trials, before any of these medications might be considered for F.D.A. review. And even then, said Dr. Hu, who has also worked on the Moderna vaccine, “it’s always a wild card how people are going to feel about it.”
Dana G. Smith is a Times reporter covering personal health, particularly aging and brain health. More about Dana G. Smith
Staying Safe During Tick Season
Thanks to migrating birds and deer vasectomies, new tick species are settling in New York City. Experts are warning that this could be a particularly bad season .
More ticks mean a higher risk of contracting a Lyme infection. Here is what to do to minimize your exposure .
Lyme isn’t the only tick disease to worry about if you live in the Northeast. Babesiosis, a tick-borne illness that can cause flulike symptoms, is also on the rise .
Think you can outsmart a tick? Test your knowledge with this quiz .
The easiest way to prevent ticks is to look for them. Learn how to do a tick check after spending time outdoors .
Certain products that can help prevent a tick bite. Wirecutter recommends the best options .
Advertisement
Argument: It’s Time for the World Bank to Break With Tradition
Create an FP account to save articles to read later and in the FP mobile app.
ALREADY AN FP SUBSCRIBER? LOGIN
World Brief
- Editors’ Picks
- Africa Brief
China Brief
- Latin America Brief
South Asia Brief
Situation report.
- Flash Points
- War in Ukraine
- Israel and Hamas
- U.S.-China competition
- Biden's foreign policy
- Trade and economics
- Artificial intelligence
- Asia & the Pacific
- Middle East & Africa
Iran’s Attack on Israel—What Happens Next?
Inside the gop’s foreign policy, ones and tooze, foreign policy live.

Spring 2024 Issue
Print Archive
FP Analytics
- In-depth Special Reports
- Issue Briefs
- Power Maps and Interactive Microsites
- FP Simulations & PeaceGames
- Graphics Database
Her Power 2024
From resistance to resilience, the atlantic & pacific forum, principles of humanity under pressure, fp global health forum 2024.
By submitting your email, you agree to the Privacy Policy and Terms of Use and to receive email correspondence from us. You may opt out at any time.
Your guide to the most important world stories of the day
Essential analysis of the stories shaping geopolitics on the continent
The latest news, analysis, and data from the country each week
Weekly update on what’s driving U.S. national security policy
Evening roundup with our editors’ favorite stories of the day
One-stop digest of politics, economics, and culture
Weekly update on developments in India and its neighbors
A curated selection of our very best long reads
It’s Time for the World Bank to Break With Tradition
The bank must adopt a new model to alleviate extreme poverty..
The spring meetings of the World Bank and International Monetary Fund have little of the drama of peace negotiations. They are often dominated by technical and technocratic questions concerning the intricacies of international finance. But for the poorest people in the world, the decisions made at these meetings are matters of life and death.
Since the 1990s, the World Bank has facilitated a dramatic decline in extreme poverty globally, from more than 1 in 3 people living in extreme poverty in 1990 to less than 1 in 10 today. But fragile and conflict-affected countries, such as the Democratic Republic of the Congo and Myanmar, have seen the opposite trend: In those places, extreme poverty is growing, and by 2030, they will be home to an estimated 59 percent of all people living in extreme poverty. The convergence of conflict, climate change, and economic shocks has left more than 300 million people dependent on humanitarian aid to survive.
This week’s meetings in Washington offer an opportunity for the World Bank to bridge this gap by revamping its approach to extreme poverty. This will require more imagination than we have historically seen from the development and humanitarian communities. But if the bank can break with traditional development frameworks and improve its reach, scale, and sustainability, it will be able to better support those who need it the most.
In stable states, development economics now has a playbook beyond the Washington Consensus, marked by free market principles and deregulation; international financial institutions now support sustainable and inclusive growth models. But in crisis-affected states, where effective humanitarian action is the first step on the road to development, the World Bank’s policy agenda is much less well developed.
The World Bank itself has recognized this. The bank’s new evolution road map , led by its president, Ajay Banga, recognizes the urgent need to focus on fragility, conflict, and climate change—among other global challenges—to achieve its mission to eradicate poverty on a livable planet. But it still needs a concrete plan.
A New Multilateralism
How the United States can rejuvenate the global institutions it created.
Niger Is a Warning for the World Bank
International finance needs a new playbook for crisis as the bank convenes for its annual meetings.
The Dark Side of Climate Finance
At COP28, poor countries should be careful what they wish for.
Historically, the World Bank has relied on robust government partnerships. Yet as the landscape of poverty changes , it will need to adopt a more flexible approach. The bank should expand delivery of its services through nongovernmental partners, which can often better access communities in need. This is particularly important in crisis settings where a government may not be able to reach parts of the country.
For example, my organization, the International Rescue Committee (IRC), has successfully partnered with Gavi, the global organization that seeks to improve access to vaccines, alongside African-led civil society groups in Ethiopia, Somalia, South Sudan, and Sudan. As of February, our partnership has administered more than 1 million doses of lifesaving vaccines to children. Prior to the program, the IRC could access only 16 percent of targeted communities in the Horn of Africa. Now, we are able to reach 77 percent of those areas.
The World Bank also needs a plan to scale up its operations. This requires not just building up capacity but also reducing strains on national systems such as hospital networks, which are often stretched thin during a crisis. Humanitarian organizations such as the IRC have had success reducing acute malnutrition among children by partnering with community health workers to diagnose cases and administer treatment instead of adding to the caseload of hospitals.
It will be crucial for the bank to ensure that its programs can sustain any progress they make. This will require real, not rhetorical, localization: shifting power to local responders and building trust with them so that they can lead and deliver in aid efforts. One example of how localization can ensure that development efforts support a community’s long-term interests is the Building Resilient Communities in Somalia consortium. This program has collaborated with more than 450 communities over the past decade, and its work has been critical to avoiding famine.
Finally, the World Bank should launch a new model for its International Development Association (IDA), one of the largest sources of development finance for the world’s poorest countries. As the World Bank leadership and donors negotiate IDA replenishment this year, they should refine its finance mechanisms to be more responsive to countries’ risk, vulnerability, and accessibility to other sources of finance. For example, the IDA Crisis Response Window —which provides countries with additional resources to respond to climate, health, and economic shocks—could include better criteria to assess how fragility, conflict, and violence can compound these shocks.
More overall funding will be key to these efforts. In 2021, the last time the bank negotiated a financing package for the IDA, development partners agreed on a $93 billion package to support sustainable development in the world’s poorest countries. This year, donors should make even more ambitious pledging contributions that will put the IDA on track for tripling its size by 2030. Expanding nongovernmental partnerships will also help the bank improve disbursal and delivery of IDA funds.
The 1990s and 2000s saw one of the world’s great development success stories as hundreds of millions of people escaped extreme poverty. While the development and humanitarian communities agree on where the next success story needs to take place, that feat will not be built with the tools of the past. Luckily, we’ve already seen how humanitarian actors can drive scale, reach, and sustainability even in some of the most complex places in the world. That should be a guide for the World Bank as it seeks to chart its path for the future.
David Miliband is president and CEO of the International Rescue Committee and a former foreign secretary of the United Kingdom.
Join the Conversation
Commenting on this and other recent articles is just one benefit of a Foreign Policy subscription.
Already a subscriber? Log In .
Subscribe Subscribe
View Comments
Join the conversation on this and other recent Foreign Policy articles when you subscribe now.
Not your account? Log out
Please follow our comment guidelines , stay on topic, and be civil, courteous, and respectful of others’ beliefs.
Change your username:
I agree to abide by FP’s comment guidelines . (Required)
Confirm your username to get started.
The default username below has been generated using the first name and last initial on your FP subscriber account. Usernames may be updated at any time and must not contain inappropriate or offensive language.
Sign up for Editors' Picks
A curated selection of fp’s must-read stories..
You’re on the list! More ways to stay updated on global news:
Hezbollah Retaliates for Israel Killing Two Militant Commanders
Can israel harness its rare moment of regional support, the world’s biggest election is set to begin, russia just helped swing a european election, the moral hazard of biden’s support for israel, editors’ picks.
- 1 America Fueled the Fire in the Middle East
- 2 Why Modi Is So Popular
- 3 The New Idea of India
- 4 3 Ways Israel Could Respond to Iran
- 5 Fear and Hoarding on Ukraine’s Eastern Front
- 6 Can Israel Harness Its Rare Moment of Regional Support?
Hezbollah Strikes Israel for Deaths of Two Militant Commanders
After iran attack, can israel harness its rare moment of regional support, russia just helped swing the presidential election in slovakia, israel-iran: biden's unconditional support for israel risks regional escalation, more from foreign policy, israel is facing an iraq-like quagmire.
Six months in, there’s still no plan for after the war, U.S. officials say.
NATO Doesn’t Have Enough Troops
For the first time in decades, NATO has a plan to fight Russia. Now it just needs the forces to do it.
Biden’s ‘Coalitions of the Willing’ Foreign-Policy Doctrine
The latest flurry of U.S. diplomacy shows how the president is all about “minilateralism.”
The New Idea of India
Narendra Modi’s reign is producing a less liberal but more assured nation.
America Fueled the Fire in the Middle East
3 ways israel could respond to iran, why modi is so popular, fear and hoarding on ukraine’s eastern front, is india really the next china.
Sign up for World Brief
FP’s flagship evening newsletter guiding you through the most important world stories of the day, written by Alexandra Sharp . Delivered weekdays.

IMAGES
VIDEO
COMMENTS
The global influence of Louis Pasteur led to the expansion of the term vaccine to include a long list of treatments containing live, weakened or killed viruses, typically given in the form of an injection, to produce immunity against an infectious disease. Scientific advances in the first half of the 20th Century led to an explosion of vaccines ...
In 1872, despite enduring a stroke and the death of 2 of his daughters to typhoid, Louis Pasteur creates the first laboratory-produced vaccine: the vaccine for fowl cholera in chickens. In 1885, Louis Pasteur successfully prevents rabies through post-exposure vaccination. The treatment is controversial. Pasteur has unsuccessfully attempted to ...
Introduction "The impact of vaccination on the health of the world's peoples is hard to exaggerate. With the exception of safe water, no other modality has had such a major effect on mortality reduction and population growth" (Plotkin and Mortimer, 1988).The development of safe and efficacious vaccination against diseases that cause substantial morbidity and mortality has been one of the ...
Uptake of these vaccines in the developing world has generally been slow despite their proven efficacy and a high burden from many of the diseases that they could prevent. Uptake of hepatitis B vaccine into the routine EPI of developing countries in Africa and Asia took over 20 years, despite the fact that the hepatitis B virus is a major cause ...
The vaccine prevented an estimated 23 million deaths during this period. The first vaccine for mumps appeared in 1948, though it only produced short-lived immunity against the virus. An improved ...
Introduction and background. Although inoculation practices were started more than 500 years ago, the term vaccine was first described in the 18th century by Edward Jenner. It is derived from Vacca, a Latin word for cow. Jenner inoculated an eight-year-old boy with cowpox lesions from the hands of milkmaids in 1796.
Innovative financing expedited the introduction of the pneumococcal vaccine, enabling it to be launched in 2011, in a world-first, in rich and poor countries simultaneously. Immunisation saves millions of lives every year. We now have vaccines to prevent and control 25 infections, helping people of all ages live longer, healthier lives.
It's hard to overstate the benefits that innovative vaccines deployed in the past five decades have had on morbidity and mortality (see timeline). 1 The incidence of vaccine-preventable diseases ...
1. Immunization saves lives and protects peoples' health. Immunization keeps people healthy and has reduced the number of deaths from infectious diseases dramatically. Between 2010 and 2017, the mortality rate of children under 5 years of age declined by nearly a quarter. 1 Measles vaccines alone prevented 25.5 million deaths since 2000, and ...
Vaccines have been a part of the human fight against disease for more than 200 years. The worldwide vaccination campaign eradicated smallpox, and immunization has eliminated polio in all but a handful of countries. Childhood vaccination has substantially reduced the morbidity and mortality of infectious diseases in much of the developed world ...
The Year Vaccines Changed (Most) of the World. In 2021, the biggest vaccination drive in global history affected everything from public health to diplomacy. By Stefan Theil, a deputy editor at ...
Despite the successful development of COVID-19 vaccines, just 14 percent of the world's population is fully vaccinated against the disease and less than 30 percent has received at least one dose.
The changing face of the novel coronavirus has challenged scientists to modify existing vaccines to better tackle the changing characteristics of SARS-CoV-2. Yet, despite much talk of modified vaccines for variants, the world is still using largely the same original vaccines for initial rollouts and booster doses.
The world watched in real time, the rapid development and deployment of new life-saving vaccines in 2020 when the Covid-19 virus was infecting millions and sparked a global pandemic.
Much of the world's population had already been infected with COVID-19 by the time the Omicron variant emerged at the end of 2021, but the scale of the Omicron wave was larger than any that had come before or has happened since, and it left a global imprinting of immunity that changed the COVID-19 landscape. In this study, we simulate a South ...
Introduction. Vaccines have substantially reduced the burden of infectious diseases. An estimated 103 million cases of childhood diseases were prevented between 1924 and 2010 in the United States through vaccination (van Panhuis et al., 2013).In particular, the eradication of smallpox through vaccination in 1980 is one of the crown achievements of medicine.
Thursday, October 21, 2021. By Katelyn Silva. Robert A. Aronowitz, Walter H. and Leonore C. Annenberg Professor in the Social Sciences. The story of the COVID-19 vaccines is a winding one. Never in the world's history has a vaccine been developed and deemed safe and effective so quickly—in less than 12 months. For many, it felt like a miracle.
Vaccine Inequality Has Shut Vulnerable People Out of Plans to Save the Planet. Those with the most at stake were heard the least. ... Introducing 21 Ways COVID Changed the World.
When asked to name the feeling that best describes how they feel now that they have been vaccinated, nearly a quarter of vaccinated adults offer responses around feeling safe (24%) and relieved ...
They estimate vaccines saved 157,000 lives in England alone, and more than 470,000 across the 33 countries in Europe which were studied. Researchers called the Covid vaccines a "marvel of modern ...
US biotech Moderna has put plans to build a vaccine plant in Kenya on hold, in a sign that moves to invest in pandemic preparedness in Africa have dropped down the agenda as sales of Covid-19 jabs ...
Introduction. Vaccination has been relatively successful in preventing many childhood-related infections and saving millions of lives. Well in excess of 10 million lives were saved between mid-1960s and 2015 with viral vaccines 1, 2 such as measles, mumps, rubella, chickenpox and hepatitis A, produced from acceptable cell culture substrates. However, approximately 1.5 million children under 5 ...
Novavax is this year rolling out its second product: a malaria vaccine approved by the World Health Organization, which will help to grow its revenues from $531.4mn last year to a projected $854 ...
17 April 2024 - The report of the workshop on COVID-19 vaccine strain updates, organised by the International Coalition of Medicines Regulatory Authorities (ICMRA) and the World Health Organization (WHO) has been published today. The virtual workshop was held on 26-27 February 2024 with the aim of facilitating sharing of perspectives around the process, timing and regulatory requirements ...
When a tick ingests a dog's blood, the antibodies kill the bacteria residing in the tick's gut, preventing them from causing an infection. In recent years, the pharmaceutical companies Pfizer ...
April 15, 2024, 2:43 PM. The spring meetings of the World Bank and International Monetary Fund have little of the drama of peace negotiations. They are often dominated by technical and ...