An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Environmental and Health Impacts of Air Pollution: A Review
Ioannis manisalidis, elisavet stavropoulou, agathangelos stavropoulos, eugenia bezirtzoglou.
- Author information
- Article notes
- Copyright and License information
Edited by: Ethel Eljarrat, Institute of Environmental Assessment and Water Research (CSIC), Spain
Reviewed by: Fei Li, Zhongnan University of Economics and Law, China; M. Jahangir Alam, University of Houston, United States
*Correspondence: Ioannis Manisalidis [email protected]
Elisavet Stavropoulou [email protected]
This article was submitted to Environmental Health, a section of the journal Frontiers in Public Health
†These authors have contributed equally to this work
Received 2019 Oct 17; Accepted 2020 Jan 17; Collection date 2020.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
One of our era's greatest scourges is air pollution, on account not only of its impact on climate change but also its impact on public and individual health due to increasing morbidity and mortality. There are many pollutants that are major factors in disease in humans. Among them, Particulate Matter (PM), particles of variable but very small diameter, penetrate the respiratory system via inhalation, causing respiratory and cardiovascular diseases, reproductive and central nervous system dysfunctions, and cancer. Despite the fact that ozone in the stratosphere plays a protective role against ultraviolet irradiation, it is harmful when in high concentration at ground level, also affecting the respiratory and cardiovascular system. Furthermore, nitrogen oxide, sulfur dioxide, Volatile Organic Compounds (VOCs), dioxins, and polycyclic aromatic hydrocarbons (PAHs) are all considered air pollutants that are harmful to humans. Carbon monoxide can even provoke direct poisoning when breathed in at high levels. Heavy metals such as lead, when absorbed into the human body, can lead to direct poisoning or chronic intoxication, depending on exposure. Diseases occurring from the aforementioned substances include principally respiratory problems such as Chronic Obstructive Pulmonary Disease (COPD), asthma, bronchiolitis, and also lung cancer, cardiovascular events, central nervous system dysfunctions, and cutaneous diseases. Last but not least, climate change resulting from environmental pollution affects the geographical distribution of many infectious diseases, as do natural disasters. The only way to tackle this problem is through public awareness coupled with a multidisciplinary approach by scientific experts; national and international organizations must address the emergence of this threat and propose sustainable solutions.
Keywords: air pollution, environment, health, public health, gas emission, policy
Approach to the Problem
The interactions between humans and their physical surroundings have been extensively studied, as multiple human activities influence the environment. The environment is a coupling of the biotic (living organisms and microorganisms) and the abiotic (hydrosphere, lithosphere, and atmosphere).
Pollution is defined as the introduction into the environment of substances harmful to humans and other living organisms. Pollutants are harmful solids, liquids, or gases produced in higher than usual concentrations that reduce the quality of our environment.
Human activities have an adverse effect on the environment by polluting the water we drink, the air we breathe, and the soil in which plants grow. Although the industrial revolution was a great success in terms of technology, society, and the provision of multiple services, it also introduced the production of huge quantities of pollutants emitted into the air that are harmful to human health. Without any doubt, the global environmental pollution is considered an international public health issue with multiple facets. Social, economic, and legislative concerns and lifestyle habits are related to this major problem. Clearly, urbanization and industrialization are reaching unprecedented and upsetting proportions worldwide in our era. Anthropogenic air pollution is one of the biggest public health hazards worldwide, given that it accounts for about 9 million deaths per year ( 1 ).
Without a doubt, all of the aforementioned are closely associated with climate change, and in the event of danger, the consequences can be severe for mankind ( 2 ). Climate changes and the effects of global planetary warming seriously affect multiple ecosystems, causing problems such as food safety issues, ice and iceberg melting, animal extinction, and damage to plants ( 3 , 4 ).
Air pollution has various health effects. The health of susceptible and sensitive individuals can be impacted even on low air pollution days. Short-term exposure to air pollutants is closely related to COPD (Chronic Obstructive Pulmonary Disease), cough, shortness of breath, wheezing, asthma, respiratory disease, and high rates of hospitalization (a measurement of morbidity).
The long-term effects associated with air pollution are chronic asthma, pulmonary insufficiency, cardiovascular diseases, and cardiovascular mortality. According to a Swedish cohort study, diabetes seems to be induced after long-term air pollution exposure ( 5 ). Moreover, air pollution seems to have various malign health effects in early human life, such as respiratory, cardiovascular, mental, and perinatal disorders ( 3 ), leading to infant mortality or chronic disease in adult age ( 6 ).
National reports have mentioned the increased risk of morbidity and mortality ( 1 ). These studies were conducted in many places around the world and show a correlation between daily ranges of particulate matter (PM) concentration and daily mortality. Climate shifts and global planetary warming ( 3 ) could aggravate the situation. Besides, increased hospitalization (an index of morbidity) has been registered among the elderly and susceptible individuals for specific reasons. Fine and ultrafine particulate matter seems to be associated with more serious illnesses ( 6 ), as it can invade the deepest parts of the airways and more easily reach the bloodstream.
Air pollution mainly affects those living in large urban areas, where road emissions contribute the most to the degradation of air quality. There is also a danger of industrial accidents, where the spread of a toxic fog can be fatal to the populations of the surrounding areas. The dispersion of pollutants is determined by many parameters, most notably atmospheric stability and wind ( 6 ).
In developing countries ( 7 ), the problem is more serious due to overpopulation and uncontrolled urbanization along with the development of industrialization. This leads to poor air quality, especially in countries with social disparities and a lack of information on sustainable management of the environment. The use of fuels such as wood fuel or solid fuel for domestic needs due to low incomes exposes people to bad-quality, polluted air at home. It is of note that three billion people around the world are using the above sources of energy for their daily heating and cooking needs ( 8 ). In developing countries, the women of the household seem to carry the highest risk for disease development due to their longer duration exposure to the indoor air pollution ( 8 , 9 ). Due to its fast industrial development and overpopulation, China is one of the Asian countries confronting serious air pollution problems ( 10 , 11 ). The lung cancer mortality observed in China is associated with fine particles ( 12 ). As stated already, long-term exposure is associated with deleterious effects on the cardiovascular system ( 3 , 5 ). However, it is interesting to note that cardiovascular diseases have mostly been observed in developed and high-income countries rather than in the developing low-income countries exposed highly to air pollution ( 13 ). Extreme air pollution is recorded in India, where the air quality reaches hazardous levels. New Delhi is one of the more polluted cities in India. Flights in and out of New Delhi International Airport are often canceled due to the reduced visibility associated with air pollution. Pollution is occurring both in urban and rural areas in India due to the fast industrialization, urbanization, and rise in use of motorcycle transportation. Nevertheless, biomass combustion associated with heating and cooking needs and practices is a major source of household air pollution in India and in Nepal ( 14 , 15 ). There is spatial heterogeneity in India, as areas with diverse climatological conditions and population and education levels generate different indoor air qualities, with higher PM 2.5 observed in North Indian states (557–601 μg/m 3 ) compared to the Southern States (183–214 μg/m 3 ) ( 16 , 17 ). The cold climate of the North Indian areas may be the main reason for this, as longer periods at home and more heating are necessary compared to in the tropical climate of Southern India. Household air pollution in India is associated with major health effects, especially in women and young children, who stay indoors for longer periods. Chronic obstructive respiratory disease (CORD) and lung cancer are mostly observed in women, while acute lower respiratory disease is seen in young children under 5 years of age ( 18 ).
Accumulation of air pollution, especially sulfur dioxide and smoke, reaching 1,500 mg/m3, resulted in an increase in the number of deaths (4,000 deaths) in December 1952 in London and in 1963 in New York City (400 deaths) ( 19 ). An association of pollution with mortality was reported on the basis of monitoring of outdoor pollution in six US metropolitan cities ( 20 ). In every case, it seems that mortality was closely related to the levels of fine, inhalable, and sulfate particles more than with the levels of total particulate pollution, aerosol acidity, sulfur dioxide, or nitrogen dioxide ( 20 ).
Furthermore, extremely high levels of pollution are reported in Mexico City and Rio de Janeiro, followed by Milan, Ankara, Melbourne, Tokyo, and Moscow ( 19 ).
Based on the magnitude of the public health impact, it is certain that different kinds of interventions should be taken into account. Success and effectiveness in controlling air pollution, specifically at the local level, have been reported. Adequate technological means are applied considering the source and the nature of the emission as well as its impact on health and the environment. The importance of point sources and non-point sources of air pollution control is reported by Schwela and Köth-Jahr ( 21 ). Without a doubt, a detailed emission inventory must record all sources in a given area. Beyond considering the above sources and their nature, topography and meteorology should also be considered, as stated previously. Assessment of the control policies and methods is often extrapolated from the local to the regional and then to the global scale. Air pollution may be dispersed and transported from one region to another area located far away. Air pollution management means the reduction to acceptable levels or possible elimination of air pollutants whose presence in the air affects our health or the environmental ecosystem. Private and governmental entities and authorities implement actions to ensure the air quality ( 22 ). Air quality standards and guidelines were adopted for the different pollutants by the WHO and EPA as a tool for the management of air quality ( 1 , 23 ). These standards have to be compared to the emissions inventory standards by causal analysis and dispersion modeling in order to reveal the problematic areas ( 24 ). Inventories are generally based on a combination of direct measurements and emissions modeling ( 24 ).
As an example, we state here the control measures at the source through the use of catalytic converters in cars. These are devices that turn the pollutants and toxic gases produced from combustion engines into less-toxic pollutants by catalysis through redox reactions ( 25 ). In Greece, the use of private cars was restricted by tracking their license plates in order to reduce traffic congestion during rush hour ( 25 ).
Concerning industrial emissions, collectors and closed systems can keep the air pollution to the minimal standards imposed by legislation ( 26 ).
Current strategies to improve air quality require an estimation of the economic value of the benefits gained from proposed programs. These proposed programs by public authorities, and directives are issued with guidelines to be respected.
In Europe, air quality limit values AQLVs (Air Quality Limit Values) are issued for setting off planning claims ( 27 ). In the USA, the NAAQS (National Ambient Air Quality Standards) establish the national air quality limit values ( 27 ). While both standards and directives are based on different mechanisms, significant success has been achieved in the reduction of overall emissions and associated health and environmental effects ( 27 ). The European Directive identifies geographical areas of risk exposure as monitoring/assessment zones to record the emission sources and levels of air pollution ( 27 ), whereas the USA establishes global geographical air quality criteria according to the severity of their air quality problem and records all sources of the pollutants and their precursors ( 27 ).
In this vein, funds have been financing, directly or indirectly, projects related to air quality along with the technical infrastructure to maintain good air quality. These plans focus on an inventory of databases from air quality environmental planning awareness campaigns. Moreover, pollution measures of air emissions may be taken for vehicles, machines, and industries in urban areas.
Technological innovation can only be successful if it is able to meet the needs of society. In this sense, technology must reflect the decision-making practices and procedures of those involved in risk assessment and evaluation and act as a facilitator in providing information and assessments to enable decision makers to make the best decisions possible. Summarizing the aforementioned in order to design an effective air quality control strategy, several aspects must be considered: environmental factors and ambient air quality conditions, engineering factors and air pollutant characteristics, and finally, economic operating costs for technological improvement and administrative and legal costs. Considering the economic factor, competitiveness through neoliberal concepts is offering a solution to environmental problems ( 22 ).
The development of environmental governance, along with technological progress, has initiated the deployment of a dialogue. Environmental politics has created objections and points of opposition between different political parties, scientists, media, and governmental and non-governmental organizations ( 22 ). Radical environmental activism actions and movements have been created ( 22 ). The rise of the new information and communication technologies (ICTs) are many times examined as to whether and in which way they have influenced means of communication and social movements such as activism ( 28 ). Since the 1990s, the term “digital activism” has been used increasingly and in many different disciplines ( 29 ). Nowadays, multiple digital technologies can be used to produce a digital activism outcome on environmental issues. More specifically, devices with online capabilities such as computers or mobile phones are being used as a way to pursue change in political and social affairs ( 30 ).
In the present paper, we focus on the sources of environmental pollution in relation to public health and propose some solutions and interventions that may be of interest to environmental legislators and decision makers.
Sources of Exposure
It is known that the majority of environmental pollutants are emitted through large-scale human activities such as the use of industrial machinery, power-producing stations, combustion engines, and cars. Because these activities are performed at such a large scale, they are by far the major contributors to air pollution, with cars estimated to be responsible for approximately 80% of today's pollution ( 31 ). Some other human activities are also influencing our environment to a lesser extent, such as field cultivation techniques, gas stations, fuel tanks heaters, and cleaning procedures ( 32 ), as well as several natural sources, such as volcanic and soil eruptions and forest fires.
The classification of air pollutants is based mainly on the sources producing pollution. Therefore, it is worth mentioning the four main sources, following the classification system: Major sources, Area sources, Mobile sources, and Natural sources.
Major sources include the emission of pollutants from power stations, refineries, and petrochemicals, the chemical and fertilizer industries, metallurgical and other industrial plants, and, finally, municipal incineration.
Indoor area sources include domestic cleaning activities, dry cleaners, printing shops, and petrol stations.
Mobile sources include automobiles, cars, railways, airways, and other types of vehicles.
Finally, natural sources include, as stated previously, physical disasters ( 33 ) such as forest fire, volcanic erosion, dust storms, and agricultural burning.
However, many classification systems have been proposed. Another type of classification is a grouping according to the recipient of the pollution, as follows:
Air pollution is determined as the presence of pollutants in the air in large quantities for long periods. Air pollutants are dispersed particles, hydrocarbons, CO, CO 2 , NO, NO 2 , SO 3 , etc.
Water pollution is organic and inorganic charge and biological charge ( 10 ) at high levels that affect the water quality ( 34 , 35 ).
Soil pollution occurs through the release of chemicals or the disposal of wastes, such as heavy metals, hydrocarbons, and pesticides.
Air pollution can influence the quality of soil and water bodies by polluting precipitation, falling into water and soil environments ( 34 , 36 ). Notably, the chemistry of the soil can be amended due to acid precipitation by affecting plants, cultures, and water quality ( 37 ). Moreover, movement of heavy metals is favored by soil acidity, and metals are so then moving into the watery environment. It is known that heavy metals such as aluminum are noxious to wildlife and fishes. Soil quality seems to be of importance, as soils with low calcium carbonate levels are at increased jeopardy from acid rain. Over and above rain, snow and particulate matter drip into watery ' bodies ( 36 , 38 ).
Lastly, pollution is classified following type of origin:
Radioactive and nuclear pollution , releasing radioactive and nuclear pollutants into water, air, and soil during nuclear explosions and accidents, from nuclear weapons, and through handling or disposal of radioactive sewage.
Radioactive materials can contaminate surface water bodies and, being noxious to the environment, plants, animals, and humans. It is known that several radioactive substances such as radium and uranium concentrate in the bones and can cause cancers ( 38 , 39 ).
Noise pollution is produced by machines, vehicles, traffic noises, and musical installations that are harmful to our hearing.
The World Health Organization introduced the term DALYs. The DALYs for a disease or health condition is defined as the sum of the Years of Life Lost (YLL) due to premature mortality in the population and the Years Lost due to Disability (YLD) for people living with the health condition or its consequences ( 39 ). In Europe, air pollution is the main cause of disability-adjusted life years lost (DALYs), followed by noise pollution. The potential relationships of noise and air pollution with health have been studied ( 40 ). The study found that DALYs related to noise were more important than those related to air pollution, as the effects of environmental noise on cardiovascular disease were independent of air pollution ( 40 ). Environmental noise should be counted as an independent public health risk ( 40 ).
Environmental pollution occurs when changes in the physical, chemical, or biological constituents of the environment (air masses, temperature, climate, etc.) are produced.
Pollutants harm our environment either by increasing levels above normal or by introducing harmful toxic substances. Primary pollutants are directly produced from the above sources, and secondary pollutants are emitted as by-products of the primary ones. Pollutants can be biodegradable or non-biodegradable and of natural origin or anthropogenic, as stated previously. Moreover, their origin can be a unique source (point-source) or dispersed sources.
Pollutants have differences in physical and chemical properties, explaining the discrepancy in their capacity for producing toxic effects. As an example, we state here that aerosol compounds ( 41 – 43 ) have a greater toxicity than gaseous compounds due to their tiny size (solid or liquid) in the atmosphere; they have a greater penetration capacity. Gaseous compounds are eliminated more easily by our respiratory system ( 41 ). These particles are able to damage lungs and can even enter the bloodstream ( 41 ), leading to the premature deaths of millions of people yearly. Moreover, the aerosol acidity ([H+]) seems to considerably enhance the production of secondary organic aerosols (SOA), but this last aspect is not supported by other scientific teams ( 38 ).
Climate and Pollution
Air pollution and climate change are closely related. Climate is the other side of the same coin that reduces the quality of our Earth ( 44 ). Pollutants such as black carbon, methane, tropospheric ozone, and aerosols affect the amount of incoming sunlight. As a result, the temperature of the Earth is increasing, resulting in the melting of ice, icebergs, and glaciers.
In this vein, climatic changes will affect the incidence and prevalence of both residual and imported infections in Europe. Climate and weather affect the duration, timing, and intensity of outbreaks strongly and change the map of infectious diseases in the globe ( 45 ). Mosquito-transmitted parasitic or viral diseases are extremely climate-sensitive, as warming firstly shortens the pathogen incubation period and secondly shifts the geographic map of the vector. Similarly, water-warming following climate changes leads to a high incidence of waterborne infections. Recently, in Europe, eradicated diseases seem to be emerging due to the migration of population, for example, cholera, poliomyelitis, tick-borne encephalitis, and malaria ( 46 ).
The spread of epidemics is associated with natural climate disasters and storms, which seem to occur more frequently nowadays ( 47 ). Malnutrition and disequilibration of the immune system are also associated with the emerging infections affecting public health ( 48 ).
The Chikungunya virus “took the airplane” from the Indian Ocean to Europe, as outbreaks of the disease were registered in Italy ( 49 ) as well as autochthonous cases in France ( 50 ).
An increase in cryptosporidiosis in the United Kingdom and in the Czech Republic seems to have occurred following flooding ( 36 , 51 ).
As stated previously, aerosols compounds are tiny in size and considerably affect the climate. They are able to dissipate sunlight (the albedo phenomenon) by dispersing a quarter of the sun's rays back to space and have cooled the global temperature over the last 30 years ( 52 ).
Air Pollutants
The World Health Organization (WHO) reports on six major air pollutants, namely particle pollution, ground-level ozone, carbon monoxide, sulfur oxides, nitrogen oxides, and lead. Air pollution can have a disastrous effect on all components of the environment, including groundwater, soil, and air. Additionally, it poses a serious threat to living organisms. In this vein, our interest is mainly to focus on these pollutants, as they are related to more extensive and severe problems in human health and environmental impact. Acid rain, global warming, the greenhouse effect, and climate changes have an important ecological impact on air pollution ( 53 ).
Particulate Matter (PM) and Health
Studies have shown a relationship between particulate matter (PM) and adverse health effects, focusing on either short-term (acute) or long-term (chronic) PM exposure.
Particulate matter (PM) is usually formed in the atmosphere as a result of chemical reactions between the different pollutants. The penetration of particles is closely dependent on their size ( 53 ). Particulate Matter (PM) was defined as a term for particles by the United States Environmental Protection Agency ( 54 ). Particulate matter (PM) pollution includes particles with diameters of 10 micrometers (μm) or smaller, called PM 10 , and extremely fine particles with diameters that are generally 2.5 micrometers (μm) and smaller.
Particulate matter contains tiny liquid or solid droplets that can be inhaled and cause serious health effects ( 55 ). Particles <10 μm in diameter (PM 10 ) after inhalation can invade the lungs and even reach the bloodstream. Fine particles, PM 2.5 , pose a greater risk to health ( 6 , 56 ) ( Table 1 ).
Penetrability according to particle size.
Multiple epidemiological studies have been performed on the health effects of PM. A positive relation was shown between both short-term and long-term exposures of PM 2.5 and acute nasopharyngitis ( 56 ). In addition, long-term exposure to PM for years was found to be related to cardiovascular diseases and infant mortality.
Those studies depend on PM 2.5 monitors and are restricted in terms of study area or city area due to a lack of spatially resolved daily PM 2.5 concentration data and, in this way, are not representative of the entire population. Following a recent epidemiological study by the Department of Environmental Health at Harvard School of Public Health (Boston, MA) ( 57 ), it was reported that, as PM 2.5 concentrations vary spatially, an exposure error (Berkson error) seems to be produced, and the relative magnitudes of the short- and long-term effects are not yet completely elucidated. The team developed a PM 2.5 exposure model based on remote sensing data for assessing short- and long-term human exposures ( 57 ). This model permits spatial resolution in short-term effects plus the assessment of long-term effects in the whole population.
Moreover, respiratory diseases and affection of the immune system are registered as long-term chronic effects ( 58 ). It is worth noting that people with asthma, pneumonia, diabetes, and respiratory and cardiovascular diseases are especially susceptible and vulnerable to the effects of PM. PM 2.5 , followed by PM 10 , are strongly associated with diverse respiratory system diseases ( 59 ), as their size permits them to pierce interior spaces ( 60 ). The particles produce toxic effects according to their chemical and physical properties. The components of PM 10 and PM 2.5 can be organic (polycyclic aromatic hydrocarbons, dioxins, benzene, 1-3 butadiene) or inorganic (carbon, chlorides, nitrates, sulfates, metals) in nature ( 55 ).
Particulate Matter (PM) is divided into four main categories according to type and size ( 61 ) ( Table 2 ).
Types and sizes of particulate Matter (PM).
Gas contaminants include PM in aerial masses.
Particulate contaminants include contaminants such as smog, soot, tobacco smoke, oil smoke, fly ash, and cement dust.
Biological Contaminants are microorganisms (bacteria, viruses, fungi, mold, and bacterial spores), cat allergens, house dust and allergens, and pollen.
Types of Dust include suspended atmospheric dust, settling dust, and heavy dust.
Finally, another fact is that the half-lives of PM 10 and PM 2.5 particles in the atmosphere is extended due to their tiny dimensions; this permits their long-lasting suspension in the atmosphere and even their transfer and spread to distant destinations where people and the environment may be exposed to the same magnitude of pollution ( 53 ). They are able to change the nutrient balance in watery ecosystems, damage forests and crops, and acidify water bodies.
As stated, PM 2.5 , due to their tiny size, are causing more serious health effects. These aforementioned fine particles are the main cause of the “haze” formation in different metropolitan areas ( 12 , 13 , 61 ).
Ozone Impact in the Atmosphere
Ozone (O 3 ) is a gas formed from oxygen under high voltage electric discharge ( 62 ). It is a strong oxidant, 52% stronger than chlorine. It arises in the stratosphere, but it could also arise following chain reactions of photochemical smog in the troposphere ( 63 ).
Ozone can travel to distant areas from its initial source, moving with air masses ( 64 ). It is surprising that ozone levels over cities are low in contrast to the increased amounts occuring in urban areas, which could become harmful for cultures, forests, and vegetation ( 65 ) as it is reducing carbon assimilation ( 66 ). Ozone reduces growth and yield ( 47 , 48 ) and affects the plant microflora due to its antimicrobial capacity ( 67 , 68 ). In this regard, ozone acts upon other natural ecosystems, with microflora ( 69 , 70 ) and animal species changing their species composition ( 71 ). Ozone increases DNA damage in epidermal keratinocytes and leads to impaired cellular function ( 72 ).
Ground-level ozone (GLO) is generated through a chemical reaction between oxides of nitrogen and VOCs emitted from natural sources and/or following anthropogenic activities.
Ozone uptake usually occurs by inhalation. Ozone affects the upper layers of the skin and the tear ducts ( 73 ). A study of short-term exposure of mice to high levels of ozone showed malondialdehyde formation in the upper skin (epidermis) but also depletion in vitamins C and E. It is likely that ozone levels are not interfering with the skin barrier function and integrity to predispose to skin disease ( 74 ).
Due to the low water-solubility of ozone, inhaled ozone has the capacity to penetrate deeply into the lungs ( 75 ).
Toxic effects induced by ozone are registered in urban areas all over the world, causing biochemical, morphologic, functional, and immunological disorders ( 76 ).
The European project (APHEA2) focuses on the acute effects of ambient ozone concentrations on mortality ( 77 ). Daily ozone concentrations compared to the daily number of deaths were reported from different European cities for a 3-year period. During the warm period of the year, an observed increase in ozone concentration was associated with an increase in the daily number of deaths (0.33%), in the number of respiratory deaths (1.13%), and in the number of cardiovascular deaths (0.45%). No effect was observed during wintertime.
Carbon Monoxide (CO)
Carbon monoxide is produced by fossil fuel when combustion is incomplete. The symptoms of poisoning due to inhaling carbon monoxide include headache, dizziness, weakness, nausea, vomiting, and, finally, loss of consciousness.
The affinity of carbon monoxide to hemoglobin is much greater than that of oxygen. In this vein, serious poisoning may occur in people exposed to high levels of carbon monoxide for a long period of time. Due to the loss of oxygen as a result of the competitive binding of carbon monoxide, hypoxia, ischemia, and cardiovascular disease are observed.
Carbon monoxide affects the greenhouses gases that are tightly connected to global warming and climate. This should lead to an increase in soil and water temperatures, and extreme weather conditions or storms may occur ( 68 ).
However, in laboratory and field experiments, it has been seen to produce increased plant growth ( 78 ).
Nitrogen Oxide (NO 2 )
Nitrogen oxide is a traffic-related pollutant, as it is emitted from automobile motor engines ( 79 , 80 ). It is an irritant of the respiratory system as it penetrates deep in the lung, inducing respiratory diseases, coughing, wheezing, dyspnea, bronchospasm, and even pulmonary edema when inhaled at high levels. It seems that concentrations over 0.2 ppm produce these adverse effects in humans, while concentrations higher than 2.0 ppm affect T-lymphocytes, particularly the CD8+ cells and NK cells that produce our immune response ( 81 ).It is reported that long-term exposure to high levels of nitrogen dioxide can be responsible for chronic lung disease. Long-term exposure to NO 2 can impair the sense of smell ( 81 ).
However, systems other than respiratory ones can be involved, as symptoms such as eye, throat, and nose irritation have been registered ( 81 ).
High levels of nitrogen dioxide are deleterious to crops and vegetation, as they have been observed to reduce crop yield and plant growth efficiency. Moreover, NO 2 can reduce visibility and discolor fabrics ( 81 ).
Sulfur Dioxide (SO 2 )
Sulfur dioxide is a harmful gas that is emitted mainly from fossil fuel consumption or industrial activities. The annual standard for SO 2 is 0.03 ppm ( 82 ). It affects human, animal, and plant life. Susceptible people as those with lung disease, old people, and children, who present a higher risk of damage. The major health problems associated with sulfur dioxide emissions in industrialized areas are respiratory irritation, bronchitis, mucus production, and bronchospasm, as it is a sensory irritant and penetrates deep into the lung converted into bisulfite and interacting with sensory receptors, causing bronchoconstriction. Moreover, skin redness, damage to the eyes (lacrimation and corneal opacity) and mucous membranes, and worsening of pre-existing cardiovascular disease have been observed ( 81 ).
Environmental adverse effects, such as acidification of soil and acid rain, seem to be associated with sulfur dioxide emissions ( 83 ).
Lead is a heavy metal used in different industrial plants and emitted from some petrol motor engines, batteries, radiators, waste incinerators, and waste waters ( 84 ).
Moreover, major sources of lead pollution in the air are metals, ore, and piston-engine aircraft. Lead poisoning is a threat to public health due to its deleterious effects upon humans, animals, and the environment, especially in the developing countries.
Exposure to lead can occur through inhalation, ingestion, and dermal absorption. Trans- placental transport of lead was also reported, as lead passes through the placenta unencumbered ( 85 ). The younger the fetus is, the more harmful the toxic effects. Lead toxicity affects the fetal nervous system; edema or swelling of the brain is observed ( 86 ). Lead, when inhaled, accumulates in the blood, soft tissue, liver, lung, bones, and cardiovascular, nervous, and reproductive systems. Moreover, loss of concentration and memory, as well as muscle and joint pain, were observed in adults ( 85 , 86 ).
Children and newborns ( 87 ) are extremely susceptible even to minimal doses of lead, as it is a neurotoxicant and causes learning disabilities, impairment of memory, hyperactivity, and even mental retardation.
Elevated amounts of lead in the environment are harmful to plants and crop growth. Neurological effects are observed in vertebrates and animals in association with high lead levels ( 88 ).
Polycyclic Aromatic Hydrocarbons(PAHs)
The distribution of PAHs is ubiquitous in the environment, as the atmosphere is the most important means of their dispersal. They are found in coal and in tar sediments. Moreover, they are generated through incomplete combustion of organic matter as in the cases of forest fires, incineration, and engines ( 89 ). PAH compounds, such as benzopyrene, acenaphthylene, anthracene, and fluoranthene are recognized as toxic, mutagenic, and carcinogenic substances. They are an important risk factor for lung cancer ( 89 ).
Volatile Organic Compounds(VOCs)
Volatile organic compounds (VOCs), such as toluene, benzene, ethylbenzene, and xylene ( 90 ), have been found to be associated with cancer in humans ( 91 ). The use of new products and materials has actually resulted in increased concentrations of VOCs. VOCs pollute indoor air ( 90 ) and may have adverse effects on human health ( 91 ). Short-term and long-term adverse effects on human health are observed. VOCs are responsible for indoor air smells. Short-term exposure is found to cause irritation of eyes, nose, throat, and mucosal membranes, while those of long duration exposure include toxic reactions ( 92 ). Predictable assessment of the toxic effects of complex VOC mixtures is difficult to estimate, as these pollutants can have synergic, antagonistic, or indifferent effects ( 91 , 93 ).
Dioxins originate from industrial processes but also come from natural processes, such as forest fires and volcanic eruptions. They accumulate in foods such as meat and dairy products, fish and shellfish, and especially in the fatty tissue of animals ( 94 ).
Short-period exhibition to high dioxin concentrations may result in dark spots and lesions on the skin ( 94 ). Long-term exposure to dioxins can cause developmental problems, impairment of the immune, endocrine and nervous systems, reproductive infertility, and cancer ( 94 ).
Without any doubt, fossil fuel consumption is responsible for a sizeable part of air contamination. This contamination may be anthropogenic, as in agricultural and industrial processes or transportation, while contamination from natural sources is also possible. Interestingly, it is of note that the air quality standards established through the European Air Quality Directive are somewhat looser than the WHO guidelines, which are stricter ( 95 ).
Effect of Air Pollution on Health
The most common air pollutants are ground-level ozone and Particulates Matter (PM). Air pollution is distinguished into two main types:
Outdoor pollution is the ambient air pollution.
Indoor pollution is the pollution generated by household combustion of fuels.
People exposed to high concentrations of air pollutants experience disease symptoms and states of greater and lesser seriousness. These effects are grouped into short- and long-term effects affecting health.
Susceptible populations that need to be aware of health protection measures include old people, children, and people with diabetes and predisposing heart or lung disease, especially asthma.
As extensively stated previously, according to a recent epidemiological study from Harvard School of Public Health, the relative magnitudes of the short- and long-term effects have not been completely clarified ( 57 ) due to the different epidemiological methodologies and to the exposure errors. New models are proposed for assessing short- and long-term human exposure data more successfully ( 57 ). Thus, in the present section, we report the more common short- and long-term health effects but also general concerns for both types of effects, as these effects are often dependent on environmental conditions, dose, and individual susceptibility.
Short-term effects are temporary and range from simple discomfort, such as irritation of the eyes, nose, skin, throat, wheezing, coughing and chest tightness, and breathing difficulties, to more serious states, such as asthma, pneumonia, bronchitis, and lung and heart problems. Short-term exposure to air pollution can also cause headaches, nausea, and dizziness.
These problems can be aggravated by extended long-term exposure to the pollutants, which is harmful to the neurological, reproductive, and respiratory systems and causes cancer and even, rarely, deaths.
The long-term effects are chronic, lasting for years or the whole life and can even lead to death. Furthermore, the toxicity of several air pollutants may also induce a variety of cancers in the long term ( 96 ).
As stated already, respiratory disorders are closely associated with the inhalation of air pollutants. These pollutants will invade through the airways and will accumulate at the cells. Damage to target cells should be related to the pollutant component involved and its source and dose. Health effects are also closely dependent on country, area, season, and time. An extended exposure duration to the pollutant should incline to long-term health effects in relation also to the above factors.
Particulate Matter (PMs), dust, benzene, and O 3 cause serious damage to the respiratory system ( 97 ). Moreover, there is a supplementary risk in case of existing respiratory disease such as asthma ( 98 ). Long-term effects are more frequent in people with a predisposing disease state. When the trachea is contaminated by pollutants, voice alterations may be remarked after acute exposure. Chronic obstructive pulmonary disease (COPD) may be induced following air pollution, increasing morbidity and mortality ( 99 ). Long-term effects from traffic, industrial air pollution, and combustion of fuels are the major factors for COPD risk ( 99 ).
Multiple cardiovascular effects have been observed after exposure to air pollutants ( 100 ). Changes occurred in blood cells after long-term exposure may affect cardiac functionality. Coronary arteriosclerosis was reported following long-term exposure to traffic emissions ( 101 ), while short-term exposure is related to hypertension, stroke, myocardial infracts, and heart insufficiency. Ventricle hypertrophy is reported to occur in humans after long-time exposure to nitrogen oxide (NO 2 ) ( 102 , 103 ).
Neurological effects have been observed in adults and children after extended-term exposure to air pollutants.
Psychological complications, autism, retinopathy, fetal growth, and low birth weight seem to be related to long-term air pollution ( 83 ). The etiologic agent of the neurodegenerative diseases (Alzheimer's and Parkinson's) is not yet known, although it is believed that extended exposure to air pollution seems to be a factor. Specifically, pesticides and metals are cited as etiological factors, together with diet. The mechanisms in the development of neurodegenerative disease include oxidative stress, protein aggregation, inflammation, and mitochondrial impairment in neurons ( 104 ) ( Figure 1 ).
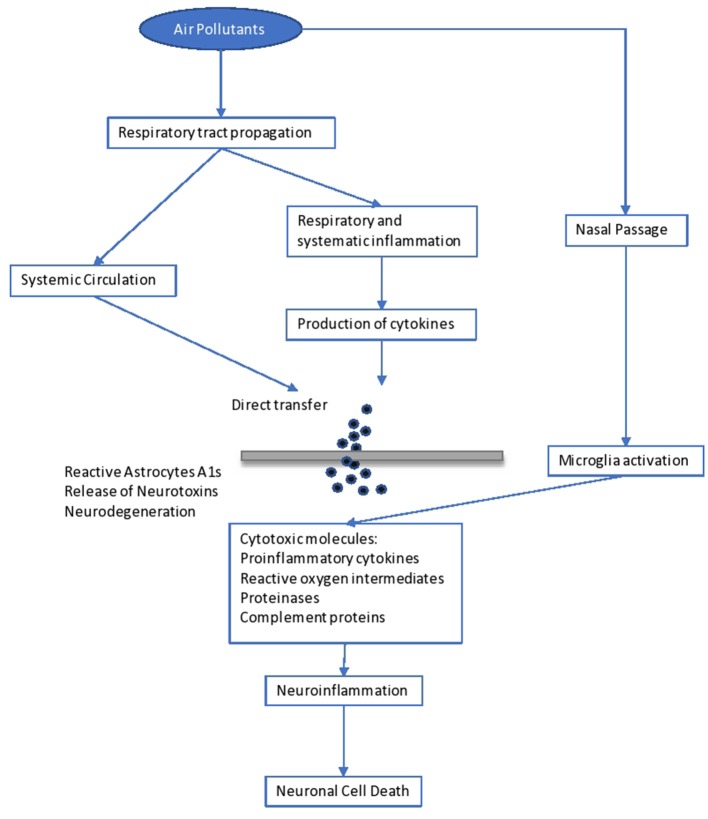
Impact of air pollutants on the brain.
Brain inflammation was observed in dogs living in a highly polluted area in Mexico for a long period ( 105 ). In human adults, markers of systemic inflammation (IL-6 and fibrinogen) were found to be increased as an immediate response to PNC on the IL-6 level, possibly leading to the production of acute-phase proteins ( 106 ). The progression of atherosclerosis and oxidative stress seem to be the mechanisms involved in the neurological disturbances caused by long-term air pollution. Inflammation comes secondary to the oxidative stress and seems to be involved in the impairment of developmental maturation, affecting multiple organs ( 105 , 107 ). Similarly, other factors seem to be involved in the developmental maturation, which define the vulnerability to long-term air pollution. These include birthweight, maternal smoking, genetic background and socioeconomic environment, as well as education level.
However, diet, starting from breast-feeding, is another determinant factor. Diet is the main source of antioxidants, which play a key role in our protection against air pollutants ( 108 ). Antioxidants are free radical scavengers and limit the interaction of free radicals in the brain ( 108 ). Similarly, genetic background may result in a differential susceptibility toward the oxidative stress pathway ( 60 ). For example, antioxidant supplementation with vitamins C and E appears to modulate the effect of ozone in asthmatic children homozygous for the GSTM1 null allele ( 61 ). Inflammatory cytokines released in the periphery (e.g., respiratory epithelia) upregulate the innate immune Toll-like receptor 2. Such activation and the subsequent events leading to neurodegeneration have recently been observed in lung lavage in mice exposed to ambient Los Angeles (CA, USA) particulate matter ( 61 ). In children, neurodevelopmental morbidities were observed after lead exposure. These children developed aggressive and delinquent behavior, reduced intelligence, learning difficulties, and hyperactivity ( 109 ). No level of lead exposure seems to be “safe,” and the scientific community has asked the Centers for Disease Control and Prevention (CDC) to reduce the current screening guideline of 10 μg/dl ( 109 ).
It is important to state that impact on the immune system, causing dysfunction and neuroinflammation ( 104 ), is related to poor air quality. Yet, increases in serum levels of immunoglobulins (IgA, IgM) and the complement component C3 are observed ( 106 ). Another issue is that antigen presentation is affected by air pollutants, as there is an upregulation of costimulatory molecules such as CD80 and CD86 on macrophages ( 110 ).
As is known, skin is our shield against ultraviolet radiation (UVR) and other pollutants, as it is the most exterior layer of our body. Traffic-related pollutants, such as PAHs, VOCs, oxides, and PM, may cause pigmented spots on our skin ( 111 ). On the one hand, as already stated, when pollutants penetrate through the skin or are inhaled, damage to the organs is observed, as some of these pollutants are mutagenic and carcinogenic, and, specifically, they affect the liver and lung. On the other hand, air pollutants (and those in the troposphere) reduce the adverse effects of ultraviolet radiation UVR in polluted urban areas ( 111 ). Air pollutants absorbed by the human skin may contribute to skin aging, psoriasis, acne, urticaria, eczema, and atopic dermatitis ( 111 ), usually caused by exposure to oxides and photochemical smoke ( 111 ). Exposure to PM and cigarette smoking act as skin-aging agents, causing spots, dyschromia, and wrinkles. Lastly, pollutants have been associated with skin cancer ( 111 ).
Higher morbidity is reported to fetuses and children when exposed to the above dangers. Impairment in fetal growth, low birth weight, and autism have been reported ( 112 ).
Another exterior organ that may be affected is the eye. Contamination usually comes from suspended pollutants and may result in asymptomatic eye outcomes, irritation ( 112 ), retinopathy, or dry eye syndrome ( 113 , 114 ).
Environmental Impact of Air Pollution
Air pollution is harming not only human health but also the environment ( 115 ) in which we live. The most important environmental effects are as follows.
Acid rain is wet (rain, fog, snow) or dry (particulates and gas) precipitation containing toxic amounts of nitric and sulfuric acids. They are able to acidify the water and soil environments, damage trees and plantations, and even damage buildings and outdoor sculptures, constructions, and statues.
Haze is produced when fine particles are dispersed in the air and reduce the transparency of the atmosphere. It is caused by gas emissions in the air coming from industrial facilities, power plants, automobiles, and trucks.
Ozone , as discussed previously, occurs both at ground level and in the upper level (stratosphere) of the Earth's atmosphere. Stratospheric ozone is protecting us from the Sun's harmful ultraviolet (UV) rays. In contrast, ground-level ozone is harmful to human health and is a pollutant. Unfortunately, stratospheric ozone is gradually damaged by ozone-depleting substances (i.e., chemicals, pesticides, and aerosols). If this protecting stratospheric ozone layer is thinned, then UV radiation can reach our Earth, with harmful effects for human life (skin cancer) ( 116 ) and crops ( 117 ). In plants, ozone penetrates through the stomata, inducing them to close, which blocks CO 2 transfer and induces a reduction in photosynthesis ( 118 ).
Global climate change is an important issue that concerns mankind. As is known, the “greenhouse effect” keeps the Earth's temperature stable. Unhappily, anthropogenic activities have destroyed this protecting temperature effect by producing large amounts of greenhouse gases, and global warming is mounting, with harmful effects on human health, animals, forests, wildlife, agriculture, and the water environment. A report states that global warming is adding to the health risks of poor people ( 119 ).
People living in poorly constructed buildings in warm-climate countries are at high risk for heat-related health problems as temperatures mount ( 119 ).
Wildlife is burdened by toxic pollutants coming from the air, soil, or the water ecosystem and, in this way, animals can develop health problems when exposed to high levels of pollutants. Reproductive failure and birth effects have been reported.
Eutrophication is occurring when elevated concentrations of nutrients (especially nitrogen) stimulate the blooming of aquatic algae, which can cause a disequilibration in the diversity of fish and their deaths.
Without a doubt, there is a critical concentration of pollution that an ecosystem can tolerate without being destroyed, which is associated with the ecosystem's capacity to neutralize acidity. The Canada Acid Rain Program established this load at 20 kg/ha/yr ( 120 ).
Hence, air pollution has deleterious effects on both soil and water ( 121 ). Concerning PM as an air pollutant, its impact on crop yield and food productivity has been reported. Its impact on watery bodies is associated with the survival of living organisms and fishes and their productivity potential ( 121 ).
An impairment in photosynthetic rhythm and metabolism is observed in plants exposed to the effects of ozone ( 121 ).
Sulfur and nitrogen oxides are involved in the formation of acid rain and are harmful to plants and marine organisms.
Last but not least, as mentioned above, the toxicity associated with lead and other metals is the main threat to our ecosystems (air, water, and soil) and living creatures ( 121 ).
In 2018, during the first WHO Global Conference on Air Pollution and Health, the WHO's General Director, Dr. Tedros Adhanom Ghebreyesus, called air pollution a “silent public health emergency” and “the new tobacco” ( 122 ).
Undoubtedly, children are particularly vulnerable to air pollution, especially during their development. Air pollution has adverse effects on our lives in many different respects.
Diseases associated with air pollution have not only an important economic impact but also a societal impact due to absences from productive work and school.
Despite the difficulty of eradicating the problem of anthropogenic environmental pollution, a successful solution could be envisaged as a tight collaboration of authorities, bodies, and doctors to regularize the situation. Governments should spread sufficient information and educate people and should involve professionals in these issues so as to control the emergence of the problem successfully.
Technologies to reduce air pollution at the source must be established and should be used in all industries and power plants. The Kyoto Protocol of 1997 set as a major target the reduction of GHG emissions to below 5% by 2012 ( 123 ). This was followed by the Copenhagen summit, 2009 ( 124 ), and then the Durban summit of 2011 ( 125 ), where it was decided to keep to the same line of action. The Kyoto protocol and the subsequent ones were ratified by many countries. Among the pioneers who adopted this important protocol for the world's environmental and climate “health” was China ( 3 ). As is known, China is a fast-developing economy and its GDP (Gross Domestic Product) is expected to be very high by 2050, which is defined as the year of dissolution of the protocol for the decrease in gas emissions.
A more recent international agreement of crucial importance for climate change is the Paris Agreement of 2015, issued by the UNFCCC (United Nations Climate Change Committee). This latest agreement was ratified by a plethora of UN (United Nations) countries as well as the countries of the European Union ( 126 ). In this vein, parties should promote actions and measures to enhance numerous aspects around the subject. Boosting education, training, public awareness, and public participation are some of the relevant actions for maximizing the opportunities to achieve the targets and goals on the crucial matter of climate change and environmental pollution ( 126 ). Without any doubt, technological improvements makes our world easier and it seems difficult to reduce the harmful impact caused by gas emissions, we could limit its use by seeking reliable approaches.
Synopsizing, a global prevention policy should be designed in order to combat anthropogenic air pollution as a complement to the correct handling of the adverse health effects associated with air pollution. Sustainable development practices should be applied, together with information coming from research in order to handle the problem effectively.
At this point, international cooperation in terms of research, development, administration policy, monitoring, and politics is vital for effective pollution control. Legislation concerning air pollution must be aligned and updated, and policy makers should propose the design of a powerful tool of environmental and health protection. As a result, the main proposal of this essay is that we should focus on fostering local structures to promote experience and practice and extrapolate these to the international level through developing effective policies for sustainable management of ecosystems.
Author Contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Conflict of Interest
IM is employed by the company Delphis S.A. The remaining authors declare that the present review paper was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
- 1. WHO Air Pollution. WHO. Available online at: http://www.who.int/airpollution/en/ (accessed October 5, 2019).
- 2. Moores FC. Climate change and air pollution: exploring the synergies and potential for mitigation in industrializing countries. Sustainability. (2009) 1:43–54. 10.3390/su1010043 [ DOI ] [ Google Scholar ]
- 3. USGCRP (2009). Global Climate Change Impacts in the United States. In: Karl TR, Melillo JM, Peterson TC, editors. Climate Change Impacts by Sectors: Ecosystems. New York, NY: United States Global Change Research Program. Cambridge University Press. [ Google Scholar ]
- 4. Marlon JR, Bloodhart B, Ballew MT, Rolfe-Redding J, Roser-Renouf C, Leiserowitz A, et al. (2019). How hope and doubt affect climate change mobilization. Front. Commun. 4:20 10.3389/fcomm.2019.00020 [ DOI ] [ Google Scholar ]
- 5. Eze IC, Schaffner E, Fischer E, Schikowski T, Adam M, Imboden M, et al. Long- term air pollution exposure and diabetes in a population-based Swiss cohort. Environ Int. (2014) 70:95–105. 10.1016/j.envint.2014.05.014 [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Kelishadi R, Poursafa P. Air pollution and non-respiratory health hazards for children. Arch Med Sci. (2010) 6:483–95. 10.5114/aoms.2010.14458 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. Manucci PM, Franchini M. Health effects of ambient air pollution in developing countries. Int J Environ Res Public Health. (2017) 14:1048 10.3390/ijerph14091048 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 8. Burden of Disease from Ambient and Household Air Pollution. Available online: http://who.int/phe/health_topics/outdoorair/databases/en/ (accessed August 15, 2017).
- 9. Hashim D, Boffetta P. Occupational and environmental exposures and cancers in developing countries. Ann Glob Health. (2014) 80:393–411. 10.1016/j.aogh.2014.10.002 [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. Guo Y, Zeng H, Zheng R, Li S, Pereira G, Liu Q, et al. The burden of lung cancer mortality attributable to fine particles in China. Total Environ Sci. (2017) 579:1460–6. 10.1016/j.scitotenv.2016.11.147 [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Hou Q, An XQ, Wang Y, Guo JP. An evaluation of resident exposure to respirable particulate matter and health economic loss in Beijing during Beijing 2008 Olympic Games. Sci Total Environ. (2010) 408:4026–32. 10.1016/j.scitotenv.2009.12.030 [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. Kan H, Chen R, Tong S. Ambient air pollution, climate change, and population health in China. Environ Int. (2012) 42:10–9. 10.1016/j.envint.2011.03.003 [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Burroughs Peña MS, Rollins A. Environmental exposures and cardiovascular disease: a challenge for health and development in low- and middle-income countries. Cardiol Clin. (2017) 35:71–86. 10.1016/j.ccl.2016.09.001 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 14. Kankaria A, Nongkynrih B, Gupta S. Indoor air pollution in india: implications on health and its control. Indian J Comm Med. 39:203–7. 10.4103/0970-0218.143019 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 15. Parajuli I, Lee H, Shrestha KR. Indoor air quality and ventilation assessment of rural mountainous households of Nepal. Int J Sust Built Env. (2016) 5:301–11. 10.1016/j.ijsbe.2016.08.003 [ DOI ] [ Google Scholar ]
- 16. Saud T, Gautam R, Mandal TK, Gadi R, Singh DP, Sharma SK. Emission estimates of organic and elemental carbon from household biomass fuel used over the Indo-Gangetic Plain (IGP), India. Atmos Environ. (2012) 61:212–20. 10.1016/j.atmosenv.2012.07.030 [ DOI ] [ Google Scholar ]
- 17. Singh DP, Gadi R, Mandal TK, Saud T, Saxena M, Sharma SK. Emissions estimates of PAH from biomass fuels used in rural sector of Indo-Gangetic Plains of India. Atmos Environ. (2013) 68:120–6. 10.1016/j.atmosenv.2012.11.042 [ DOI ] [ Google Scholar ]
- 18. Dherani M, Pope D, Mascarenhas M, Smith KR, Weber M BN. Indoor air pollution from unprocessed solid fuel use and pneumonia risk in children aged under five years: a systematic review and meta-analysis. Bull World Health Organ. (2008) 86:390–4. 10.2471/BLT.07.044529 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 19. Kassomenos P, Kelessis A, Petrakakis M, Zoumakis N, Christides T, Paschalidou AK. Air Quality assessment in a heavily-polluted urban Mediterranean environment through Air Quality indices. Ecol Indic. (2012) 18:259–68. 10.1016/j.ecolind.2011.11.021 [ DOI ] [ Google Scholar ]
- 20. Dockery DW, Pope CA, Xu X, Spengler JD, Ware JH, Fay ME, et al. An association between air pollution and mortality in six U.S. cities. N Engl J Med. (1993) 329:1753–9. 10.1056/NEJM199312093292401 [ DOI ] [ PubMed ] [ Google Scholar ]
- 21. Schwela DH, Köth-Jahr I. Leitfaden für die Aufstellung von Luftreinhalteplänen [Guidelines for the Implementation of Clean Air Implementation Plans]. Landesumweltamt des Landes Nordrhein Westfalen. State Environmental Service of the State of North Rhine-Westphalia (1994). [ Google Scholar ]
- 22. Newlands M. Environmental Activism, Environmental Politics, and Representation: The Framing of the British Environmental Activist Movement. Ph.D. thesis. University of East London, United Kingdom (2015). [ Google Scholar ]
- 23. NEPIS (National Service Center for Environmental Publications) US EPA (Environmental Protection Agency) (2017). Available online at: https://www.epa.gov/clean-air-act-overview/air-pollution-current-and-future-challenges (accessed August 15, 2017).
- 24. NRC (National Research Council) Available online at: https://www.nap.edu/read/10728/chapter/1,2014 (accessed September 17, 2019).
- 25. Bull A. Traffic Congestion: The Problem and How to Deal With It. Santiago: Nationes Unidas, Cepal; (2003). [ Google Scholar ]
- 26. Spiegel J, Maystre LY. Environmental Pollution Control, Part VII - The Environment, Chapter 55, Encyclopedia of Occupational Health and Safety. Available online at: http://www.ilocis.org/documents/chpt55e.htm (accessed September 17, 2019).
- 27. European Community Reports Assessment of the Effectiveness of European Air Quality Policies and Measures: Case Study 2; Comparison of the EU and US Air Quality Standards and Planning Requirements. (2004). Available online at: https://ec.europa.eu/environment/archives/cafe/activities/pdf/case_study2.pdf (accessed September 22, 2019).
- 28. Gibson R, Ward S. Parties in the digital age; a review. J Represent Democracy. (2009) 45:87–100. 10.1080/00344890802710888 [ DOI ] [ Google Scholar ]
- 29. Kaun A, Uldam J. Digital activism: after the hype. New Media Soc. (2017) 20:2099–106. 10.1177/14614448177319 [ DOI ] [ Google Scholar ]
- 30. Sivitanides M, Shah V. The era of digital activism. In: 2011 Conference for Information Systems Applied Research(CONISAR) Proceedings Wilmington North Carolina, USA. Available online at: https://www.arifyildirim.com/ilt510/marcos.sivitanides.vivek.shah.pdf (accessed September 22, 2019).
- 31. Möller L, Schuetzle D, Autrup H. Future research needs associated with the assessment of potential human health risks from exposure to toxic ambient air pollutants. Environ Health Perspect. (1994) 102(Suppl. 4):193–210. 10.1289/ehp.94102s4193 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 32. Jacobson MZ, Jacobson PMZ. Atmospheric Pollution: History, Science, and Regulation. Cambridge University Press (2002). p. 206 10.1256/wea.243.02 [ DOI ] [ Google Scholar ]
- 33. Stover RH. Flooding of soil for disease control. In: Mulder D, editor. Chapter 3. Developments in Agricultural and Managed Forest Ecology. Elsevier (1979). p. 19–28. Available online at: http://www.sciencedirect.com/science/article/pii/B9780444416926500094 10.1016/B978-0-444-41692-6.50009-4 (accessed July 1, 2019). [ DOI ]
- 34. Maipa V, Alamanos Y, Bezirtzoglou E. Seasonal fluctuation of bacterial indicators in coastal waters. Microb Ecol Health Dis. (2001) 13:143–6. 10.1080/089106001750462687 [ DOI ] [ Google Scholar ]
- 35. Bezirtzoglou E, Dimitriou D, Panagiou A. Occurrence of Clostridium perfringens in river water by using a new procedure. Anaerobe. (1996) 2:169–73. 10.1006/anae.1996.0022 [ DOI ] [ Google Scholar ]
- 36. Kjellstrom T, Lodh M, McMichael T, Ranmuthugala G, Shrestha R, Kingsland S. Air and Water Pollution: Burden and Strategies for Control. DCP, Chapter 43. 817–32 p. Available online at: https://www.dcp-3.org/sites/default/files/dcp2/DCP43.pdf (accessed September 17, 2017).
- 37. Pathak RK, Wang T, Ho KF, Lee SC. Characteristics of summertime PM2.5 organic and elemental carbon in four major Chinese cities: implications of high acidity for water- soluble organic carbon (WSOC). Atmos Environ. (2011) 45:318–25. 10.1016/j.atmosenv.2010.10.021 [ DOI ] [ Google Scholar ]
- 38. Bonavigo L, Zucchetti M, Mankolli H. Water radioactive pollution and related environmental aspects. J Int Env Appl Sci. (2009) 4:357–63 [ Google Scholar ]
- 39. World Health Organization (WHO) Preventing Disease Through Healthy Environments: Towards an Estimate of the Environmental Burden of Disease. 1106 p. Available online at: https://www.who.int/quantifying_ehimpacts/publications/preventingdisease.pdf (accessed September 22, 2019).
- 40. Stansfeld SA. Noise effects on health in the context of air pollution exposure. Int J Environ Res Public Health. (2015) 12:12735–60. 10.3390/ijerph121012735 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 41. Ethical Unicorn. Everything You Need To Know About Aerosols & Air Pollution. (2019). Available online at: https://ethicalunicorn.com/2019/04/29/everything-you-need-to-know-about-aerosols-air-pollution/ (accessed October 4, 2019).
- 42. Colbeck I, Lazaridis M. Aerosols and environmental pollution. Sci Nat. (2009) 97:117–31. 10.1007/s00114-009-0594-x [ DOI ] [ PubMed ] [ Google Scholar ]
- 43. Incecik S, Gertler A, Kassomenos P. Aerosols and air quality. Sci Total Env. (2014) 355, 488–9. 10.1016/j.scitotenv.2014.04.012 [ DOI ] [ PubMed ] [ Google Scholar ]
- 44. D'Amato G, Pawankar R, Vitale C, Maurizia L. Climate change and air pollution: effects on respiratory allergy. Allergy Asthma Immunol Res. (2016) 8:391–5. 10.4168/aair.2016.8.5.391 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 45. Bezirtzoglou C, Dekas K, Charvalos E. Climate changes, environment and infection: facts, scenarios and growing awareness from the public health community within Europe. Anaerobe. (2011) 17:337–40. 10.1016/j.anaerobe.2011.05.016 [ DOI ] [ PubMed ] [ Google Scholar ]
- 46. Castelli F, Sulis G. Migration and infectious diseases. Clin Microbiol Infect. (2017) 23:283–9. 10.1016/j.cmi.2017.03.012 [ DOI ] [ PubMed ] [ Google Scholar ]
- 47. Watson JT, Gayer M, Connolly MA. Epidemics after natural disasters. Emerg Infect Dis. (2007) 13:1–5. 10.3201/eid1301.060779 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 48. Fenn B. Malnutrition in Humanitarian Emergencies. Available online at: https://www.who.int/diseasecontrol_emergencies/publications/idhe_2009_london_malnutrition_fenn.pdf . (accessed August 15, 2017).
- 49. Lindh E, Argentini C, Remoli ME, Fortuna C, Faggioni G, Benedetti E, et al. The Italian 2017 outbreak Chikungunya virus belongs to an emerging Aedes albopictus –adapted virus cluster introduced from the Indian subcontinent. Open Forum Infect Dis. (2019) 6:ofy321. 10.1093/ofid/ofy321 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 50. Calba C, Guerbois-Galla M, Franke F, Jeannin C, Auzet-Caillaud M, Grard G, Pigaglio L, Decoppet A, et al. Preliminary report of an autochthonous chikungunya outbreak in France, July to September 2017. Eur Surveill. (2017) 22:17-00647. 10.2807/1560-7917.ES.2017.22.39.17-00647 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 51. Menne B, Murray V. Floods in the WHO European Region: Health Effects and Their Prevention. Copenhagen: WHO; Weltgesundheits organisation, Regionalbüro für Europa; (2013). Available online at: http://www.euro.who.int/data/assets/pdf_file/0020/189020/e96853.pdf (accessed 15 August 2017). [ Google Scholar ]
- 52. Schneider SH. The greenhouse effect: science and policy. Science. (1989) 243:771–81. 10.1126/science.243.4892.771 [ DOI ] [ PubMed ] [ Google Scholar ]
- 53. Wilson WE, Suh HH. Fine particles and coarse particles: concentration relationships relevant to epidemiologic studies. J Air Waste Manag Assoc. (1997) 47:1238–49. 10.1080/10473289.1997.10464074 [ DOI ] [ PubMed ] [ Google Scholar ]
- 54. US EPA (US Environmental Protection Agency) (2018). Available online at: https://www.epa.gov/pm-pollution/particulate-matter-pm-basics (accessed September 22, 2018).
- 55. Cheung K, Daher N, Kam W, Shafer MM, Ning Z, Schauer JJ, et al. Spatial and temporal variation of chemical composition and mass closure of ambient coarse particulate matter (PM10–2.5) in the Los Angeles area. Atmos Environ. (2011) 45:2651–62. 10.1016/j.atmosenv.2011.02.066 [ DOI ] [ Google Scholar ]
- 56. Zhang L, Yang Y, Li Y, Qian ZM, Xiao W, Wang X, et al. Short-term and long-term effects of PM2.5 on acute nasopharyngitis in 10 communities of Guangdong, China. Sci Total Env. (2019) 688:136–42. 10.1016/j.scitotenv.2019.05.470. [ DOI ] [ PubMed ] [ Google Scholar ]
- 57. Kloog I, Ridgway B, Koutrakis P, Coull BA, Schwartz JD. Long- and short-term exposure to PM2.5 and mortality using novel exposure models, Epidemiology. (2013) 24:555–61. 10.1097/EDE.0b013e318294beaa [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 58. New Hampshire Department of Environmental Services Current and Forecasted Air Quality in New Hampshire. Environmental Fact Sheet (2019). Available online at: https://www.des.nh.gov/organization/commissioner/pip/factsheets/ard/documents/ard-16.pdf (accessed September 22, 2019).
- 59. Kappos AD, Bruckmann P, Eikmann T, Englert N, Heinrich U, Höppe P, et al. Health effects of particles in ambient air. Int J Hyg Environ Health. (2004) 207:399–407. 10.1078/1438-4639-00306 [ DOI ] [ PubMed ] [ Google Scholar ]
- 60. Boschi N. (Ed.). Defining an educational framework for indoor air sciences education. In: Education and Training in Indoor Air Sciences. Luxembourg: Springer Science & Business Media; (2012). 245 p. [ Google Scholar ]
- 61. Heal MR, Kumar P, Harrison RM. Particles, air quality, policy and health. Chem Soc Rev. (2012) 41:6606–30. 10.1039/c2cs35076a [ DOI ] [ PubMed ] [ Google Scholar ]
- 62. Bezirtzoglou E, Alexopoulos A. Ozone history and ecosystems: a goliath from impacts to advance industrial benefits and interests, to environmental and therapeutical strategies. In: Ozone Depletion, Chemistry and Impacts. (2009). p. 135–45. [ Google Scholar ]
- 63. Villányi V, Turk B, Franc B, Csintalan Z. Ozone Pollution and its Bioindication. In: Villányi V, editor. Air Pollution. London: Intech Open; (2010). 10.5772/10047 [ DOI ] [ Google Scholar ]
- 64. Massachusetts Department of Public Health Massachusetts State Health Assessment. Boston, MA (2017). Available online at: https://www.mass.gov/files/documents/2017/11/03/2017%20MA%20SHA%20final%20compressed.pdf (accessed October 30, 2017).
- 65. Lorenzini G, Saitanis C. Ozone: A Novel Plant “Pathogen.” In: Sanitá di, Toppi L, Pawlik-Skowrońska B, editors. Abiotic Stresses in Plant Springer Link (2003). p. 205–29. 10.1007/978-94-017-0255-3_8 [ DOI ] [ Google Scholar ]
- 66. Fares S, Vargas R, Detto M, Goldstein AH, Karlik J, Paoletti E, et al. Tropospheric ozone reduces carbon assimilation in trees: estimates from analysis of continuous flux measurements. Glob Change Biol. (2013) 19:2427–43. 10.1111/gcb.12222 [ DOI ] [ PubMed ] [ Google Scholar ]
- 67. Harmens H, Mills G, Hayes F, Jones L, Norris D, Fuhrer J. Air Pollution and Vegetation. ICP Vegetation Annual Report 2006/2007. (2012) [ Google Scholar ]
- 68. Emberson LD, Pleijel H, Ainsworth EA, den Berg M, Ren W, Osborne S, et al. Ozone effects on crops and consideration in crop models. Eur J Agron. (2018) 100:19–34. 10.1016/j.eja.2018.06.002 [ DOI ] [ Google Scholar ]
- 69. Alexopoulos A, Plessas S, Ceciu S, Lazar V, Mantzourani I, Voidarou C, et al. Evaluation of ozone efficacy on the reduction of microbial population of fresh cut lettuce ( Lactuca sativa ) and green bell pepper ( Capsicum annuum ). Food Control. (2013) 30:491–6. 10.1016/j.foodcont.2012.09.018 [ DOI ] [ Google Scholar ]
- 70. Alexopoulos A, Plessas S, Kourkoutas Y, Stefanis C, Vavias S, Voidarou C, et al. Experimental effect of ozone upon the microbial flora of commercially produced dairy fermented products. Int J Food Microbiol. (2017) 246:5–11. 10.1016/j.ijfoodmicro.2017.01.018 [ DOI ] [ PubMed ] [ Google Scholar ]
- 71. Maggio A, Fagnano M. Ozone damages to mediterranean crops: physiological responses. Ital J Agron. (2008) 13–20. 10.4081/ija.2008.13 [ DOI ] [ Google Scholar ]
- 72. McCarthy JT, Pelle E, Dong K, Brahmbhatt K, Yarosh D, Pernodet N. Effects of ozone in normal human epidermal keratinocytes. Exp Dermatol. (2013) 22:360–1. 10.1111/exd.12125 [ DOI ] [ PubMed ] [ Google Scholar ]
- 73. WHO Health Risks of Ozone From Long-Range Transboundary Air Pollution. Available online at: http://www.euro.who.int/data/assets/pdf_file/0005/78647/E91843.pdf (accessed August 15, 2019).
- 74. Thiele JJ, Traber MG, Tsang K, Cross CE, Packer L. In vivo exposure to ozone depletes vitamins C and E and induces lipid peroxidation in epidermal layers of murine skin. Free Radic Biol Med. (1997) 23:365–91. 10.1016/S0891-5849(96)00617-X [ DOI ] [ PubMed ] [ Google Scholar ]
- 75. Hatch GE, Slade R, Harris LP, McDonnell WF, Devlin RB, Koren HS, et al. Ozone dose and effect in humans and rats. A comparison using oxygen- 18 labeling and bronchoalveolar lavage. Am J Respir Crit Care Med. (1994) 150:676–83. 10.1164/ajrccm.150.3.8087337 [ DOI ] [ PubMed ] [ Google Scholar ]
- 76. Lippmann M. Health effects of ozone. A critical review. JAPCA. (1989) 39:672–95. 10.1080/08940630.1989.10466554 [ DOI ] [ PubMed ] [ Google Scholar ]
- 77. Gryparis A, Forsberg B, Katsouyanni K, Analitis A, Touloumi G, Schwartz J, et al. Acute effects of ozone on mortality from the “air pollution and health: a European approach” project. Am J Respir Crit Care Med. (2004) 170:1080–7. 10.1164/rccm.200403-333OC [ DOI ] [ PubMed ] [ Google Scholar ]
- 78. Soon W, Baliunas SL, Robinson AB, Robinson ZW. Environmental effects of increased atmospheric carbon dioxide. Climate Res. (1999) 13:149–64 10.1260/0958305991499694 [ DOI ] [ Google Scholar ]
- 79. Richmont-Bryant J, Owen RC, Graham S, Snyder M, McDow S, Oakes M, et al. Estimation of on-road NO2 concentrations, NO2/NOX ratios, and related roadway gradients from near-road monitoring data. Air Qual Atm Health. (2017) 10:611–25. 10.1007/s11869-016-0455-7 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 80. Hesterberg TW, Bunn WB, McClellan RO, Hamade AK, Long CM, Valberg PA. Critical review of the human data on short-term nitrogen dioxide (NO 2 ) exposures: evidence for NO2 no-effect levels. Crit Rev Toxicol. (2009) 39:743–81. 10.3109/10408440903294945 [ DOI ] [ PubMed ] [ Google Scholar ]
- 81. Chen T-M, Gokhale J, Shofer S, Kuschner WG. Outdoor air pollution: nitrogen dioxide, sulfur dioxide, and carbon monoxide health effects. Am J Med Sci. (2007) 333:249–56. 10.1097/MAJ.0b013e31803b900f [ DOI ] [ PubMed ] [ Google Scholar ]
- 82. US EPA. Table of Historical SO 2 NAAQS, Sulfur US EPA. Available online at: https://www3.epa.gov/ttn/naaqs/standards/so2/s_so2_history.html (accessed October 5, 2019).
- 83. WHO Regional Office of Europe (2000). Available online at: https://euro.who.int/_data/assets/pdf_file/0020/123086/AQG2ndEd_7_4Sulfuroxide.pdf
- 84. Pruss-Ustun A, Fewrell L, Landrigan PJ, Ayuso-Mateos JL. Lead exposure. Comparative Quantification of Health Risks. World Health Organization. p. 1495–1542. Available online at: https://www.who.int/publications/cra/chapters/volume2/1495-1542.pdf?ua=1
- 85. Goyer RA. Transplacental transport of lead. Environ Health Perspect. (1990) 89:101–5. 10.1289/ehp.9089101 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 86. National Institute of Environmental Health Sciences (NIH) Lead and Your Health. (2013). 1–4 p. Available online at: https://www.niehs.nih.gov/health/materials/lead_and_your_health_508.pdf (accessed September 17, 2019).
- 87. Farhat A, Mohammadzadeh A, Balali-Mood M, Aghajanpoor-Pasha M, Ravanshad Y. Correlation of blood lead level in mothers and exclusively breastfed infants: a study on infants aged less than six months. Asia Pac J Med Toxicol. (2013) 2:150–2. [ Google Scholar ]
- 88. Assi MA, Hezmee MNM, Haron AW, Sabri MYM, Rajion MA. The detrimental effects of lead on human and animal health. Vet World. (2016) 9:660–71. 10.14202/vetworld.2016.660-671 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 89. Abdel-Shafy HI, Mansour MSM. A review on polycyclic aromatic hydrocarbons: source, environmental impact, effect on human health and remediation. Egypt J Pet. (2016) 25:107–23. 10.1016/j.ejpe.2015.03.011 [ DOI ] [ Google Scholar ]
- 90. Kumar A, Singh BP, Punia M, Singh D, Kumar K, Jain VK. Assessment of indoor air concentrations of VOCs and their associated health risks in the library of Jawaharlal Nehru University, New Delhi. Environ Sci Pollut Res Int. (2014) 21:2240–8. 10.1007/s11356-013-2150-7 [ DOI ] [ PubMed ] [ Google Scholar ]
- 91. Molhave L, Clausen G, Berglund B, Ceaurriz J, Kettrup A, Lindvall T, et al. Total Volatile Organic Compounds (TVOC) in Indoor Air Quality Investigations. Indoor Air. 7:225–240. 10.1111/j.1600-0668.1997.00002.x [ DOI ] [ Google Scholar ]
- 92. Gibb T. Indoor Air Quality May be Hazardous to Your Health. MSU Extension. Available online at: https://www.canr.msu.edu/news/indoor_air_quality_may_be_hazardous_to_your_health (accessed October 5, 2019).
- 93. Ebersviller S, Lichtveld K, Sexton KG, Zavala J, Lin Y-H, Jaspers I, et al. Gaseous VOCs rapidly modify particulate matter and its biological effects – Part 1: simple VOCs and model PM. Atmos Chem Phys Discuss. (2012) 12:5065–105. 10.5194/acpd-12-5065-2012 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 94. WHO (World Health Organization) . Dioxins and Their Effects on Human Health. Available online at: https://www.who.int/news-room/fact-sheets/detail/dioxins-and-their-effects-on-human-health (accessed October 5, 2019).
- 95. EEA (European Environmental Agency) Air Quality Standards to the European Union and WHO. Available online at: https://www.eea.europa.eu/themes/data-and-maps/figures/air-quality-standards-under-the
- 96. Nakano T, Otsuki T. [Environmental air pollutants and the risk of cancer]. (Japanese). Gan To Kagaku Ryoho. (2013) 40:1441–5. [ PubMed ] [ Google Scholar ]
- 97. Kurt OK, Zhang J, Pinkerton KE. Pulmonary health effects of air pollution. Curr Opin Pulm Med. (2016) 22:138–43. 10.1097/MCP.0000000000000248 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 98. Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet. (2014) 383:1581–92. 10.1016/S0140-6736(14)60617-6 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 99. Jiang X-Q, Mei X-D, Feng D. Air pollution and chronic airway diseases: what should people know and do? J Thorac Dis. (2016) 8:E31–40. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 100. Bourdrel T, Bind M-A, Béjot Y, Morel O, Argacha J-F. Cardiovascular effects of air pollution. Arch Cardiovasc Dis. (2017) 110:634–42. 10.1016/j.acvd.2017.05.003 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 101. Hoffmann B, Moebus S, Möhlenkamp S, Stang A, Lehmann N, Dragano N, et al. Residential exposure to traffic is associated with coronary atherosclerosis. Circulation. (2007) 116:489–496. 10.1161/CIRCULATIONAHA.107.693622 [ DOI ] [ PubMed ] [ Google Scholar ]
- 102. Katholi RE, Couri DM. Left ventricular hypertrophy: major risk factor in patients with hypertension: update and practical clinical applications. Int J Hypertens. (2011) 2011:495349. 10.4061/2011/495349 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 103. Leary PJ, Kaufman JD, Barr RG, Bluemke DA, Curl CL, Hough CL, et al. Traffic- related air pollution and the right ventricle. the multi-ethnic study of atherosclerosis. Am J Respir Crit Care Med. (2014) 189:1093–100. 10.1164/rccm.201312-2298OC [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 104. Genc S, Zadeoglulari Z, Fuss SH, Genc K. The adverse effects of air pollution on the nervous system. J Toxicol. (2012) 2012:782462. 10.1155/2012/782462 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 105. Calderon-Garciduenas L, Azzarelli B, Acuna H, et al. Air pollution and brain damage. Toxicol Pathol. (2002) 30:373–89. 10.1080/01926230252929954 [ DOI ] [ PubMed ] [ Google Scholar ]
- 106. Rückerl R, Greven S, Ljungman P, Aalto P, Antoniades C, Bellander T, et al. Air pollution and inflammation (interleukin-6, C-reactive protein, fibrinogen) in myocardial infarction survivors. Environ Health Perspect. (2007) 115:1072–80. 10.1289/ehp.10021 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 107. Peters A, Veronesi B, Calderón-Garcidueñas L, Gehr P, Chen LC, Geiser M, et al. Translocation and potential neurological effects of fine and ultrafine particles a critical update. Part Fibre Toxicol. (2006) 3:13–8. 10.1186/1743-8977-3-13 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 108. Kelly FJ. Dietary antioxidants and environmental stress. Proc Nutr Soc. (2004) 63:579–85. 10.1079/PNS2004388 [ DOI ] [ PubMed ] [ Google Scholar ]
- 109. Bellinger DC. Very low lead exposures and children's neurodevelopment. Curr Opin Pediatr. (2008) 20:172–7. 10.1097/MOP.0b013e3282f4f97b [ DOI ] [ PubMed ] [ Google Scholar ]
- 110. Balbo P, Silvestri M, Rossi GA, Crimi E, Burastero SE. Differential role of CD80 and CD86 on alveolar macrophages in the presentation of allergen to T lymphocytes in asthma. Clin Exp Allergy J Br Soc Allergy Clin Immunol. (2001) 31:625–36. 10.1046/j.1365-2222.2001.01068.x [ DOI ] [ PubMed ] [ Google Scholar ]
- 111. Drakaki E, Dessinioti C, Antoniou C. Air pollution and the skin. Front Environ Sci Eng China. (2014) 15:2–8. 10.3389/fenvs.2014.00011 [ DOI ] [ Google Scholar ]
- 112. Weisskopf MG, Kioumourtzoglou M-A, Roberts AL. Air pollution and autism spectrum disorders: causal or confounded? Curr Environ Health Rep. (2015) 2:430–9. 10.1007/s40572-015-0073-9 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 113. Mo Z, Fu Q, Lyu D, Zhang L, Qin Z, Tang Q, et al. Impacts of air pollution on dry eye disease among residents in Hangzhou, China: a case-crossover study. Environ Pollut. (2019) 246:183–9. 10.1016/j.envpol.2018.11.109 [ DOI ] [ PubMed ] [ Google Scholar ]
- 114. Klopfer J. Effects of environmental air pollution on the eye. J Am Optom Assoc. (1989) 60:773–8. [ PubMed ] [ Google Scholar ]
- 115. Ashfaq A, Sharma P. Environmental effects of air pollution and application of engineered methods to combat the problem. J Indust Pollut Control. (2012) 29. [ Google Scholar ]
- 116. Madronich S, de Gruijl F. Skin cancer and UV radiation. Nature. (1993) 366:23–9. 10.1038/366023a0 [ DOI ] [ PubMed ] [ Google Scholar ]
- 117. Teramura A. Effects of UV-B radiation on the growth and yield of crop plants. Physiol Plant. (2006) 58:415–27. 10.1111/j.1399-3054.1983.tb04203.x [ DOI ] [ Google Scholar ]
- 118. Singh E, Tiwari S, Agrawal M. Effects of elevated ozone on photosynthesis and stomatal conductance of two soybean varieties: a case study to assess impacts of one component of predicted global climate change. Plant Biol Stuttg Ger. (2009) 11(Suppl. 1):101–8. 10.1111/j.1438-8677.2009.00263.x [ DOI ] [ PubMed ] [ Google Scholar ]
- 119. Manderson L. How global Warming is Adding to the Health Risks of Poor People. The Conversation. University of the Witwatersrand. Available online at: http://theconversation.com/how-global-warming-is-adding-to-the-health-risks-of-poor-people-109520 (accessed October 5, 2019).
- 120. Ministers of Energy and Environment Federal/Provincial/Territorial Ministers of Energy and Environment (Canada), editor. The Canada-Wide Acid Rain Strategy for Post-2000. Halifax: The Ministers; (1999). 11 p. [ Google Scholar ]
- 121. Zuhara S, Isaifan R. The impact of criteria air pollutants on soil and water: a review. (2018) 278–84. 10.30799/jespr.133.18040205 [ DOI ] [ Google Scholar ]
- 122. WHO . First WHO Global Conference on Air Pollution and Health. (2018). Available online at: https://www.who.int/airpollution/events/conference/en/ (accessed October 6, 2019).
- 123. What is the Kyoto Protocol? UNFCCC. Available online at: https://unfccc.int/kyoto__protocol (accessed October 6, 2019).
- 124. CopenhagenClimate Change Conference (UNFCCC). Available online at: https://unfccc.int/process-and-meetings/conferences/past-conferences/copenhagen-climate-change-conference-december-2009/copenhagen-climate-change-conference-december-2009 (accessed October 6, 2019).
- 125. Durban Climate Change Conference,. UNFCCC (2011). Available online at: https://unfccc.int/process-and-meetings/conferences/past-conferences/copenhagen-climate-change-conference-december-2009/copenhagen-climate-change-conference-december-2009 (accessed October 6, 2019).
- 126. Paris Climate Change Agreement,. (2016). Available online at: https://unfccc.int/process-and-meetings/the-paris-agreement/the-paris-agreement
- View on publisher site
- PDF (689.0 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
REVIEW article
Environmental and health impacts of air pollution: a review.

- 1 Delphis S.A., Kifisia, Greece
- 2 Laboratory of Hygiene and Environmental Protection, Faculty of Medicine, Democritus University of Thrace, Alexandroupolis, Greece
- 3 Centre Hospitalier Universitaire Vaudois (CHUV), Service de Médicine Interne, Lausanne, Switzerland
- 4 School of Social and Political Sciences, University of Glasgow, Glasgow, United Kingdom
One of our era's greatest scourges is air pollution, on account not only of its impact on climate change but also its impact on public and individual health due to increasing morbidity and mortality. There are many pollutants that are major factors in disease in humans. Among them, Particulate Matter (PM), particles of variable but very small diameter, penetrate the respiratory system via inhalation, causing respiratory and cardiovascular diseases, reproductive and central nervous system dysfunctions, and cancer. Despite the fact that ozone in the stratosphere plays a protective role against ultraviolet irradiation, it is harmful when in high concentration at ground level, also affecting the respiratory and cardiovascular system. Furthermore, nitrogen oxide, sulfur dioxide, Volatile Organic Compounds (VOCs), dioxins, and polycyclic aromatic hydrocarbons (PAHs) are all considered air pollutants that are harmful to humans. Carbon monoxide can even provoke direct poisoning when breathed in at high levels. Heavy metals such as lead, when absorbed into the human body, can lead to direct poisoning or chronic intoxication, depending on exposure. Diseases occurring from the aforementioned substances include principally respiratory problems such as Chronic Obstructive Pulmonary Disease (COPD), asthma, bronchiolitis, and also lung cancer, cardiovascular events, central nervous system dysfunctions, and cutaneous diseases. Last but not least, climate change resulting from environmental pollution affects the geographical distribution of many infectious diseases, as do natural disasters. The only way to tackle this problem is through public awareness coupled with a multidisciplinary approach by scientific experts; national and international organizations must address the emergence of this threat and propose sustainable solutions.
Approach to the Problem
The interactions between humans and their physical surroundings have been extensively studied, as multiple human activities influence the environment. The environment is a coupling of the biotic (living organisms and microorganisms) and the abiotic (hydrosphere, lithosphere, and atmosphere).
Pollution is defined as the introduction into the environment of substances harmful to humans and other living organisms. Pollutants are harmful solids, liquids, or gases produced in higher than usual concentrations that reduce the quality of our environment.
Human activities have an adverse effect on the environment by polluting the water we drink, the air we breathe, and the soil in which plants grow. Although the industrial revolution was a great success in terms of technology, society, and the provision of multiple services, it also introduced the production of huge quantities of pollutants emitted into the air that are harmful to human health. Without any doubt, the global environmental pollution is considered an international public health issue with multiple facets. Social, economic, and legislative concerns and lifestyle habits are related to this major problem. Clearly, urbanization and industrialization are reaching unprecedented and upsetting proportions worldwide in our era. Anthropogenic air pollution is one of the biggest public health hazards worldwide, given that it accounts for about 9 million deaths per year ( 1 ).
Without a doubt, all of the aforementioned are closely associated with climate change, and in the event of danger, the consequences can be severe for mankind ( 2 ). Climate changes and the effects of global planetary warming seriously affect multiple ecosystems, causing problems such as food safety issues, ice and iceberg melting, animal extinction, and damage to plants ( 3 , 4 ).
Air pollution has various health effects. The health of susceptible and sensitive individuals can be impacted even on low air pollution days. Short-term exposure to air pollutants is closely related to COPD (Chronic Obstructive Pulmonary Disease), cough, shortness of breath, wheezing, asthma, respiratory disease, and high rates of hospitalization (a measurement of morbidity).
The long-term effects associated with air pollution are chronic asthma, pulmonary insufficiency, cardiovascular diseases, and cardiovascular mortality. According to a Swedish cohort study, diabetes seems to be induced after long-term air pollution exposure ( 5 ). Moreover, air pollution seems to have various malign health effects in early human life, such as respiratory, cardiovascular, mental, and perinatal disorders ( 3 ), leading to infant mortality or chronic disease in adult age ( 6 ).
National reports have mentioned the increased risk of morbidity and mortality ( 1 ). These studies were conducted in many places around the world and show a correlation between daily ranges of particulate matter (PM) concentration and daily mortality. Climate shifts and global planetary warming ( 3 ) could aggravate the situation. Besides, increased hospitalization (an index of morbidity) has been registered among the elderly and susceptible individuals for specific reasons. Fine and ultrafine particulate matter seems to be associated with more serious illnesses ( 6 ), as it can invade the deepest parts of the airways and more easily reach the bloodstream.
Air pollution mainly affects those living in large urban areas, where road emissions contribute the most to the degradation of air quality. There is also a danger of industrial accidents, where the spread of a toxic fog can be fatal to the populations of the surrounding areas. The dispersion of pollutants is determined by many parameters, most notably atmospheric stability and wind ( 6 ).
In developing countries ( 7 ), the problem is more serious due to overpopulation and uncontrolled urbanization along with the development of industrialization. This leads to poor air quality, especially in countries with social disparities and a lack of information on sustainable management of the environment. The use of fuels such as wood fuel or solid fuel for domestic needs due to low incomes exposes people to bad-quality, polluted air at home. It is of note that three billion people around the world are using the above sources of energy for their daily heating and cooking needs ( 8 ). In developing countries, the women of the household seem to carry the highest risk for disease development due to their longer duration exposure to the indoor air pollution ( 8 , 9 ). Due to its fast industrial development and overpopulation, China is one of the Asian countries confronting serious air pollution problems ( 10 , 11 ). The lung cancer mortality observed in China is associated with fine particles ( 12 ). As stated already, long-term exposure is associated with deleterious effects on the cardiovascular system ( 3 , 5 ). However, it is interesting to note that cardiovascular diseases have mostly been observed in developed and high-income countries rather than in the developing low-income countries exposed highly to air pollution ( 13 ). Extreme air pollution is recorded in India, where the air quality reaches hazardous levels. New Delhi is one of the more polluted cities in India. Flights in and out of New Delhi International Airport are often canceled due to the reduced visibility associated with air pollution. Pollution is occurring both in urban and rural areas in India due to the fast industrialization, urbanization, and rise in use of motorcycle transportation. Nevertheless, biomass combustion associated with heating and cooking needs and practices is a major source of household air pollution in India and in Nepal ( 14 , 15 ). There is spatial heterogeneity in India, as areas with diverse climatological conditions and population and education levels generate different indoor air qualities, with higher PM 2.5 observed in North Indian states (557–601 μg/m 3 ) compared to the Southern States (183–214 μg/m 3 ) ( 16 , 17 ). The cold climate of the North Indian areas may be the main reason for this, as longer periods at home and more heating are necessary compared to in the tropical climate of Southern India. Household air pollution in India is associated with major health effects, especially in women and young children, who stay indoors for longer periods. Chronic obstructive respiratory disease (CORD) and lung cancer are mostly observed in women, while acute lower respiratory disease is seen in young children under 5 years of age ( 18 ).
Accumulation of air pollution, especially sulfur dioxide and smoke, reaching 1,500 mg/m3, resulted in an increase in the number of deaths (4,000 deaths) in December 1952 in London and in 1963 in New York City (400 deaths) ( 19 ). An association of pollution with mortality was reported on the basis of monitoring of outdoor pollution in six US metropolitan cities ( 20 ). In every case, it seems that mortality was closely related to the levels of fine, inhalable, and sulfate particles more than with the levels of total particulate pollution, aerosol acidity, sulfur dioxide, or nitrogen dioxide ( 20 ).
Furthermore, extremely high levels of pollution are reported in Mexico City and Rio de Janeiro, followed by Milan, Ankara, Melbourne, Tokyo, and Moscow ( 19 ).
Based on the magnitude of the public health impact, it is certain that different kinds of interventions should be taken into account. Success and effectiveness in controlling air pollution, specifically at the local level, have been reported. Adequate technological means are applied considering the source and the nature of the emission as well as its impact on health and the environment. The importance of point sources and non-point sources of air pollution control is reported by Schwela and Köth-Jahr ( 21 ). Without a doubt, a detailed emission inventory must record all sources in a given area. Beyond considering the above sources and their nature, topography and meteorology should also be considered, as stated previously. Assessment of the control policies and methods is often extrapolated from the local to the regional and then to the global scale. Air pollution may be dispersed and transported from one region to another area located far away. Air pollution management means the reduction to acceptable levels or possible elimination of air pollutants whose presence in the air affects our health or the environmental ecosystem. Private and governmental entities and authorities implement actions to ensure the air quality ( 22 ). Air quality standards and guidelines were adopted for the different pollutants by the WHO and EPA as a tool for the management of air quality ( 1 , 23 ). These standards have to be compared to the emissions inventory standards by causal analysis and dispersion modeling in order to reveal the problematic areas ( 24 ). Inventories are generally based on a combination of direct measurements and emissions modeling ( 24 ).
As an example, we state here the control measures at the source through the use of catalytic converters in cars. These are devices that turn the pollutants and toxic gases produced from combustion engines into less-toxic pollutants by catalysis through redox reactions ( 25 ). In Greece, the use of private cars was restricted by tracking their license plates in order to reduce traffic congestion during rush hour ( 25 ).
Concerning industrial emissions, collectors and closed systems can keep the air pollution to the minimal standards imposed by legislation ( 26 ).
Current strategies to improve air quality require an estimation of the economic value of the benefits gained from proposed programs. These proposed programs by public authorities, and directives are issued with guidelines to be respected.
In Europe, air quality limit values AQLVs (Air Quality Limit Values) are issued for setting off planning claims ( 27 ). In the USA, the NAAQS (National Ambient Air Quality Standards) establish the national air quality limit values ( 27 ). While both standards and directives are based on different mechanisms, significant success has been achieved in the reduction of overall emissions and associated health and environmental effects ( 27 ). The European Directive identifies geographical areas of risk exposure as monitoring/assessment zones to record the emission sources and levels of air pollution ( 27 ), whereas the USA establishes global geographical air quality criteria according to the severity of their air quality problem and records all sources of the pollutants and their precursors ( 27 ).
In this vein, funds have been financing, directly or indirectly, projects related to air quality along with the technical infrastructure to maintain good air quality. These plans focus on an inventory of databases from air quality environmental planning awareness campaigns. Moreover, pollution measures of air emissions may be taken for vehicles, machines, and industries in urban areas.
Technological innovation can only be successful if it is able to meet the needs of society. In this sense, technology must reflect the decision-making practices and procedures of those involved in risk assessment and evaluation and act as a facilitator in providing information and assessments to enable decision makers to make the best decisions possible. Summarizing the aforementioned in order to design an effective air quality control strategy, several aspects must be considered: environmental factors and ambient air quality conditions, engineering factors and air pollutant characteristics, and finally, economic operating costs for technological improvement and administrative and legal costs. Considering the economic factor, competitiveness through neoliberal concepts is offering a solution to environmental problems ( 22 ).
The development of environmental governance, along with technological progress, has initiated the deployment of a dialogue. Environmental politics has created objections and points of opposition between different political parties, scientists, media, and governmental and non-governmental organizations ( 22 ). Radical environmental activism actions and movements have been created ( 22 ). The rise of the new information and communication technologies (ICTs) are many times examined as to whether and in which way they have influenced means of communication and social movements such as activism ( 28 ). Since the 1990s, the term “digital activism” has been used increasingly and in many different disciplines ( 29 ). Nowadays, multiple digital technologies can be used to produce a digital activism outcome on environmental issues. More specifically, devices with online capabilities such as computers or mobile phones are being used as a way to pursue change in political and social affairs ( 30 ).
In the present paper, we focus on the sources of environmental pollution in relation to public health and propose some solutions and interventions that may be of interest to environmental legislators and decision makers.
Sources of Exposure
It is known that the majority of environmental pollutants are emitted through large-scale human activities such as the use of industrial machinery, power-producing stations, combustion engines, and cars. Because these activities are performed at such a large scale, they are by far the major contributors to air pollution, with cars estimated to be responsible for approximately 80% of today's pollution ( 31 ). Some other human activities are also influencing our environment to a lesser extent, such as field cultivation techniques, gas stations, fuel tanks heaters, and cleaning procedures ( 32 ), as well as several natural sources, such as volcanic and soil eruptions and forest fires.
The classification of air pollutants is based mainly on the sources producing pollution. Therefore, it is worth mentioning the four main sources, following the classification system: Major sources, Area sources, Mobile sources, and Natural sources.
Major sources include the emission of pollutants from power stations, refineries, and petrochemicals, the chemical and fertilizer industries, metallurgical and other industrial plants, and, finally, municipal incineration.
Indoor area sources include domestic cleaning activities, dry cleaners, printing shops, and petrol stations.
Mobile sources include automobiles, cars, railways, airways, and other types of vehicles.
Finally, natural sources include, as stated previously, physical disasters ( 33 ) such as forest fire, volcanic erosion, dust storms, and agricultural burning.
However, many classification systems have been proposed. Another type of classification is a grouping according to the recipient of the pollution, as follows:
Air pollution is determined as the presence of pollutants in the air in large quantities for long periods. Air pollutants are dispersed particles, hydrocarbons, CO, CO 2 , NO, NO 2 , SO 3 , etc.
Water pollution is organic and inorganic charge and biological charge ( 10 ) at high levels that affect the water quality ( 34 , 35 ).
Soil pollution occurs through the release of chemicals or the disposal of wastes, such as heavy metals, hydrocarbons, and pesticides.
Air pollution can influence the quality of soil and water bodies by polluting precipitation, falling into water and soil environments ( 34 , 36 ). Notably, the chemistry of the soil can be amended due to acid precipitation by affecting plants, cultures, and water quality ( 37 ). Moreover, movement of heavy metals is favored by soil acidity, and metals are so then moving into the watery environment. It is known that heavy metals such as aluminum are noxious to wildlife and fishes. Soil quality seems to be of importance, as soils with low calcium carbonate levels are at increased jeopardy from acid rain. Over and above rain, snow and particulate matter drip into watery ' bodies ( 36 , 38 ).
Lastly, pollution is classified following type of origin:
Radioactive and nuclear pollution , releasing radioactive and nuclear pollutants into water, air, and soil during nuclear explosions and accidents, from nuclear weapons, and through handling or disposal of radioactive sewage.
Radioactive materials can contaminate surface water bodies and, being noxious to the environment, plants, animals, and humans. It is known that several radioactive substances such as radium and uranium concentrate in the bones and can cause cancers ( 38 , 39 ).
Noise pollution is produced by machines, vehicles, traffic noises, and musical installations that are harmful to our hearing.
The World Health Organization introduced the term DALYs. The DALYs for a disease or health condition is defined as the sum of the Years of Life Lost (YLL) due to premature mortality in the population and the Years Lost due to Disability (YLD) for people living with the health condition or its consequences ( 39 ). In Europe, air pollution is the main cause of disability-adjusted life years lost (DALYs), followed by noise pollution. The potential relationships of noise and air pollution with health have been studied ( 40 ). The study found that DALYs related to noise were more important than those related to air pollution, as the effects of environmental noise on cardiovascular disease were independent of air pollution ( 40 ). Environmental noise should be counted as an independent public health risk ( 40 ).
Environmental pollution occurs when changes in the physical, chemical, or biological constituents of the environment (air masses, temperature, climate, etc.) are produced.
Pollutants harm our environment either by increasing levels above normal or by introducing harmful toxic substances. Primary pollutants are directly produced from the above sources, and secondary pollutants are emitted as by-products of the primary ones. Pollutants can be biodegradable or non-biodegradable and of natural origin or anthropogenic, as stated previously. Moreover, their origin can be a unique source (point-source) or dispersed sources.
Pollutants have differences in physical and chemical properties, explaining the discrepancy in their capacity for producing toxic effects. As an example, we state here that aerosol compounds ( 41 – 43 ) have a greater toxicity than gaseous compounds due to their tiny size (solid or liquid) in the atmosphere; they have a greater penetration capacity. Gaseous compounds are eliminated more easily by our respiratory system ( 41 ). These particles are able to damage lungs and can even enter the bloodstream ( 41 ), leading to the premature deaths of millions of people yearly. Moreover, the aerosol acidity ([H+]) seems to considerably enhance the production of secondary organic aerosols (SOA), but this last aspect is not supported by other scientific teams ( 38 ).
Climate and Pollution
Air pollution and climate change are closely related. Climate is the other side of the same coin that reduces the quality of our Earth ( 44 ). Pollutants such as black carbon, methane, tropospheric ozone, and aerosols affect the amount of incoming sunlight. As a result, the temperature of the Earth is increasing, resulting in the melting of ice, icebergs, and glaciers.
In this vein, climatic changes will affect the incidence and prevalence of both residual and imported infections in Europe. Climate and weather affect the duration, timing, and intensity of outbreaks strongly and change the map of infectious diseases in the globe ( 45 ). Mosquito-transmitted parasitic or viral diseases are extremely climate-sensitive, as warming firstly shortens the pathogen incubation period and secondly shifts the geographic map of the vector. Similarly, water-warming following climate changes leads to a high incidence of waterborne infections. Recently, in Europe, eradicated diseases seem to be emerging due to the migration of population, for example, cholera, poliomyelitis, tick-borne encephalitis, and malaria ( 46 ).
The spread of epidemics is associated with natural climate disasters and storms, which seem to occur more frequently nowadays ( 47 ). Malnutrition and disequilibration of the immune system are also associated with the emerging infections affecting public health ( 48 ).
The Chikungunya virus “took the airplane” from the Indian Ocean to Europe, as outbreaks of the disease were registered in Italy ( 49 ) as well as autochthonous cases in France ( 50 ).
An increase in cryptosporidiosis in the United Kingdom and in the Czech Republic seems to have occurred following flooding ( 36 , 51 ).
As stated previously, aerosols compounds are tiny in size and considerably affect the climate. They are able to dissipate sunlight (the albedo phenomenon) by dispersing a quarter of the sun's rays back to space and have cooled the global temperature over the last 30 years ( 52 ).
Air Pollutants
The World Health Organization (WHO) reports on six major air pollutants, namely particle pollution, ground-level ozone, carbon monoxide, sulfur oxides, nitrogen oxides, and lead. Air pollution can have a disastrous effect on all components of the environment, including groundwater, soil, and air. Additionally, it poses a serious threat to living organisms. In this vein, our interest is mainly to focus on these pollutants, as they are related to more extensive and severe problems in human health and environmental impact. Acid rain, global warming, the greenhouse effect, and climate changes have an important ecological impact on air pollution ( 53 ).
Particulate Matter (PM) and Health
Studies have shown a relationship between particulate matter (PM) and adverse health effects, focusing on either short-term (acute) or long-term (chronic) PM exposure.
Particulate matter (PM) is usually formed in the atmosphere as a result of chemical reactions between the different pollutants. The penetration of particles is closely dependent on their size ( 53 ). Particulate Matter (PM) was defined as a term for particles by the United States Environmental Protection Agency ( 54 ). Particulate matter (PM) pollution includes particles with diameters of 10 micrometers (μm) or smaller, called PM 10 , and extremely fine particles with diameters that are generally 2.5 micrometers (μm) and smaller.
Particulate matter contains tiny liquid or solid droplets that can be inhaled and cause serious health effects ( 55 ). Particles <10 μm in diameter (PM 10 ) after inhalation can invade the lungs and even reach the bloodstream. Fine particles, PM 2.5 , pose a greater risk to health ( 6 , 56 ) ( Table 1 ).
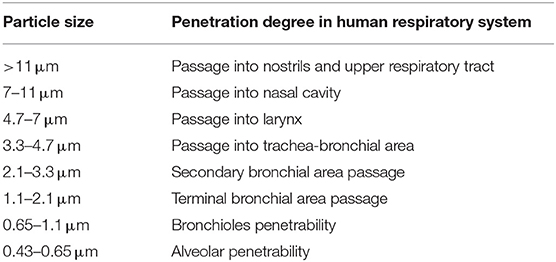
Table 1 . Penetrability according to particle size.
Multiple epidemiological studies have been performed on the health effects of PM. A positive relation was shown between both short-term and long-term exposures of PM 2.5 and acute nasopharyngitis ( 56 ). In addition, long-term exposure to PM for years was found to be related to cardiovascular diseases and infant mortality.
Those studies depend on PM 2.5 monitors and are restricted in terms of study area or city area due to a lack of spatially resolved daily PM 2.5 concentration data and, in this way, are not representative of the entire population. Following a recent epidemiological study by the Department of Environmental Health at Harvard School of Public Health (Boston, MA) ( 57 ), it was reported that, as PM 2.5 concentrations vary spatially, an exposure error (Berkson error) seems to be produced, and the relative magnitudes of the short- and long-term effects are not yet completely elucidated. The team developed a PM 2.5 exposure model based on remote sensing data for assessing short- and long-term human exposures ( 57 ). This model permits spatial resolution in short-term effects plus the assessment of long-term effects in the whole population.
Moreover, respiratory diseases and affection of the immune system are registered as long-term chronic effects ( 58 ). It is worth noting that people with asthma, pneumonia, diabetes, and respiratory and cardiovascular diseases are especially susceptible and vulnerable to the effects of PM. PM 2.5 , followed by PM 10 , are strongly associated with diverse respiratory system diseases ( 59 ), as their size permits them to pierce interior spaces ( 60 ). The particles produce toxic effects according to their chemical and physical properties. The components of PM 10 and PM 2.5 can be organic (polycyclic aromatic hydrocarbons, dioxins, benzene, 1-3 butadiene) or inorganic (carbon, chlorides, nitrates, sulfates, metals) in nature ( 55 ).
Particulate Matter (PM) is divided into four main categories according to type and size ( 61 ) ( Table 2 ).
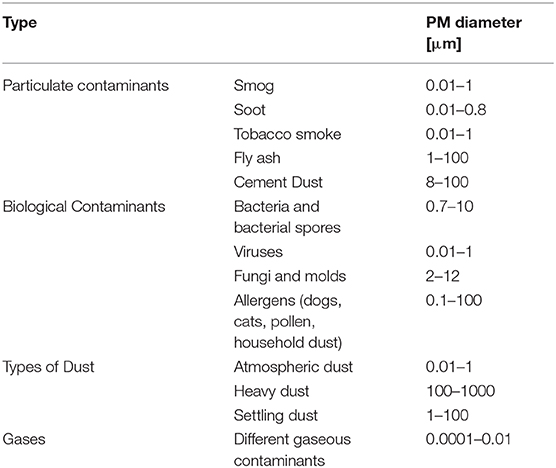
Table 2 . Types and sizes of particulate Matter (PM).
Gas contaminants include PM in aerial masses.
Particulate contaminants include contaminants such as smog, soot, tobacco smoke, oil smoke, fly ash, and cement dust.
Biological Contaminants are microorganisms (bacteria, viruses, fungi, mold, and bacterial spores), cat allergens, house dust and allergens, and pollen.
Types of Dust include suspended atmospheric dust, settling dust, and heavy dust.
Finally, another fact is that the half-lives of PM 10 and PM 2.5 particles in the atmosphere is extended due to their tiny dimensions; this permits their long-lasting suspension in the atmosphere and even their transfer and spread to distant destinations where people and the environment may be exposed to the same magnitude of pollution ( 53 ). They are able to change the nutrient balance in watery ecosystems, damage forests and crops, and acidify water bodies.
As stated, PM 2.5 , due to their tiny size, are causing more serious health effects. These aforementioned fine particles are the main cause of the “haze” formation in different metropolitan areas ( 12 , 13 , 61 ).
Ozone Impact in the Atmosphere
Ozone (O 3 ) is a gas formed from oxygen under high voltage electric discharge ( 62 ). It is a strong oxidant, 52% stronger than chlorine. It arises in the stratosphere, but it could also arise following chain reactions of photochemical smog in the troposphere ( 63 ).
Ozone can travel to distant areas from its initial source, moving with air masses ( 64 ). It is surprising that ozone levels over cities are low in contrast to the increased amounts occuring in urban areas, which could become harmful for cultures, forests, and vegetation ( 65 ) as it is reducing carbon assimilation ( 66 ). Ozone reduces growth and yield ( 47 , 48 ) and affects the plant microflora due to its antimicrobial capacity ( 67 , 68 ). In this regard, ozone acts upon other natural ecosystems, with microflora ( 69 , 70 ) and animal species changing their species composition ( 71 ). Ozone increases DNA damage in epidermal keratinocytes and leads to impaired cellular function ( 72 ).
Ground-level ozone (GLO) is generated through a chemical reaction between oxides of nitrogen and VOCs emitted from natural sources and/or following anthropogenic activities.
Ozone uptake usually occurs by inhalation. Ozone affects the upper layers of the skin and the tear ducts ( 73 ). A study of short-term exposure of mice to high levels of ozone showed malondialdehyde formation in the upper skin (epidermis) but also depletion in vitamins C and E. It is likely that ozone levels are not interfering with the skin barrier function and integrity to predispose to skin disease ( 74 ).
Due to the low water-solubility of ozone, inhaled ozone has the capacity to penetrate deeply into the lungs ( 75 ).
Toxic effects induced by ozone are registered in urban areas all over the world, causing biochemical, morphologic, functional, and immunological disorders ( 76 ).
The European project (APHEA2) focuses on the acute effects of ambient ozone concentrations on mortality ( 77 ). Daily ozone concentrations compared to the daily number of deaths were reported from different European cities for a 3-year period. During the warm period of the year, an observed increase in ozone concentration was associated with an increase in the daily number of deaths (0.33%), in the number of respiratory deaths (1.13%), and in the number of cardiovascular deaths (0.45%). No effect was observed during wintertime.
Carbon Monoxide (CO)
Carbon monoxide is produced by fossil fuel when combustion is incomplete. The symptoms of poisoning due to inhaling carbon monoxide include headache, dizziness, weakness, nausea, vomiting, and, finally, loss of consciousness.
The affinity of carbon monoxide to hemoglobin is much greater than that of oxygen. In this vein, serious poisoning may occur in people exposed to high levels of carbon monoxide for a long period of time. Due to the loss of oxygen as a result of the competitive binding of carbon monoxide, hypoxia, ischemia, and cardiovascular disease are observed.
Carbon monoxide affects the greenhouses gases that are tightly connected to global warming and climate. This should lead to an increase in soil and water temperatures, and extreme weather conditions or storms may occur ( 68 ).
However, in laboratory and field experiments, it has been seen to produce increased plant growth ( 78 ).
Nitrogen Oxide (NO 2 )
Nitrogen oxide is a traffic-related pollutant, as it is emitted from automobile motor engines ( 79 , 80 ). It is an irritant of the respiratory system as it penetrates deep in the lung, inducing respiratory diseases, coughing, wheezing, dyspnea, bronchospasm, and even pulmonary edema when inhaled at high levels. It seems that concentrations over 0.2 ppm produce these adverse effects in humans, while concentrations higher than 2.0 ppm affect T-lymphocytes, particularly the CD8+ cells and NK cells that produce our immune response ( 81 ).It is reported that long-term exposure to high levels of nitrogen dioxide can be responsible for chronic lung disease. Long-term exposure to NO 2 can impair the sense of smell ( 81 ).
However, systems other than respiratory ones can be involved, as symptoms such as eye, throat, and nose irritation have been registered ( 81 ).
High levels of nitrogen dioxide are deleterious to crops and vegetation, as they have been observed to reduce crop yield and plant growth efficiency. Moreover, NO 2 can reduce visibility and discolor fabrics ( 81 ).
Sulfur Dioxide (SO 2 )
Sulfur dioxide is a harmful gas that is emitted mainly from fossil fuel consumption or industrial activities. The annual standard for SO 2 is 0.03 ppm ( 82 ). It affects human, animal, and plant life. Susceptible people as those with lung disease, old people, and children, who present a higher risk of damage. The major health problems associated with sulfur dioxide emissions in industrialized areas are respiratory irritation, bronchitis, mucus production, and bronchospasm, as it is a sensory irritant and penetrates deep into the lung converted into bisulfite and interacting with sensory receptors, causing bronchoconstriction. Moreover, skin redness, damage to the eyes (lacrimation and corneal opacity) and mucous membranes, and worsening of pre-existing cardiovascular disease have been observed ( 81 ).
Environmental adverse effects, such as acidification of soil and acid rain, seem to be associated with sulfur dioxide emissions ( 83 ).
Lead is a heavy metal used in different industrial plants and emitted from some petrol motor engines, batteries, radiators, waste incinerators, and waste waters ( 84 ).
Moreover, major sources of lead pollution in the air are metals, ore, and piston-engine aircraft. Lead poisoning is a threat to public health due to its deleterious effects upon humans, animals, and the environment, especially in the developing countries.
Exposure to lead can occur through inhalation, ingestion, and dermal absorption. Trans- placental transport of lead was also reported, as lead passes through the placenta unencumbered ( 85 ). The younger the fetus is, the more harmful the toxic effects. Lead toxicity affects the fetal nervous system; edema or swelling of the brain is observed ( 86 ). Lead, when inhaled, accumulates in the blood, soft tissue, liver, lung, bones, and cardiovascular, nervous, and reproductive systems. Moreover, loss of concentration and memory, as well as muscle and joint pain, were observed in adults ( 85 , 86 ).
Children and newborns ( 87 ) are extremely susceptible even to minimal doses of lead, as it is a neurotoxicant and causes learning disabilities, impairment of memory, hyperactivity, and even mental retardation.
Elevated amounts of lead in the environment are harmful to plants and crop growth. Neurological effects are observed in vertebrates and animals in association with high lead levels ( 88 ).
Polycyclic Aromatic Hydrocarbons(PAHs)
The distribution of PAHs is ubiquitous in the environment, as the atmosphere is the most important means of their dispersal. They are found in coal and in tar sediments. Moreover, they are generated through incomplete combustion of organic matter as in the cases of forest fires, incineration, and engines ( 89 ). PAH compounds, such as benzopyrene, acenaphthylene, anthracene, and fluoranthene are recognized as toxic, mutagenic, and carcinogenic substances. They are an important risk factor for lung cancer ( 89 ).
Volatile Organic Compounds(VOCs)
Volatile organic compounds (VOCs), such as toluene, benzene, ethylbenzene, and xylene ( 90 ), have been found to be associated with cancer in humans ( 91 ). The use of new products and materials has actually resulted in increased concentrations of VOCs. VOCs pollute indoor air ( 90 ) and may have adverse effects on human health ( 91 ). Short-term and long-term adverse effects on human health are observed. VOCs are responsible for indoor air smells. Short-term exposure is found to cause irritation of eyes, nose, throat, and mucosal membranes, while those of long duration exposure include toxic reactions ( 92 ). Predictable assessment of the toxic effects of complex VOC mixtures is difficult to estimate, as these pollutants can have synergic, antagonistic, or indifferent effects ( 91 , 93 ).
Dioxins originate from industrial processes but also come from natural processes, such as forest fires and volcanic eruptions. They accumulate in foods such as meat and dairy products, fish and shellfish, and especially in the fatty tissue of animals ( 94 ).
Short-period exhibition to high dioxin concentrations may result in dark spots and lesions on the skin ( 94 ). Long-term exposure to dioxins can cause developmental problems, impairment of the immune, endocrine and nervous systems, reproductive infertility, and cancer ( 94 ).
Without any doubt, fossil fuel consumption is responsible for a sizeable part of air contamination. This contamination may be anthropogenic, as in agricultural and industrial processes or transportation, while contamination from natural sources is also possible. Interestingly, it is of note that the air quality standards established through the European Air Quality Directive are somewhat looser than the WHO guidelines, which are stricter ( 95 ).
Effect of Air Pollution on Health
The most common air pollutants are ground-level ozone and Particulates Matter (PM). Air pollution is distinguished into two main types:
Outdoor pollution is the ambient air pollution.
Indoor pollution is the pollution generated by household combustion of fuels.
People exposed to high concentrations of air pollutants experience disease symptoms and states of greater and lesser seriousness. These effects are grouped into short- and long-term effects affecting health.
Susceptible populations that need to be aware of health protection measures include old people, children, and people with diabetes and predisposing heart or lung disease, especially asthma.
As extensively stated previously, according to a recent epidemiological study from Harvard School of Public Health, the relative magnitudes of the short- and long-term effects have not been completely clarified ( 57 ) due to the different epidemiological methodologies and to the exposure errors. New models are proposed for assessing short- and long-term human exposure data more successfully ( 57 ). Thus, in the present section, we report the more common short- and long-term health effects but also general concerns for both types of effects, as these effects are often dependent on environmental conditions, dose, and individual susceptibility.
Short-term effects are temporary and range from simple discomfort, such as irritation of the eyes, nose, skin, throat, wheezing, coughing and chest tightness, and breathing difficulties, to more serious states, such as asthma, pneumonia, bronchitis, and lung and heart problems. Short-term exposure to air pollution can also cause headaches, nausea, and dizziness.
These problems can be aggravated by extended long-term exposure to the pollutants, which is harmful to the neurological, reproductive, and respiratory systems and causes cancer and even, rarely, deaths.
The long-term effects are chronic, lasting for years or the whole life and can even lead to death. Furthermore, the toxicity of several air pollutants may also induce a variety of cancers in the long term ( 96 ).
As stated already, respiratory disorders are closely associated with the inhalation of air pollutants. These pollutants will invade through the airways and will accumulate at the cells. Damage to target cells should be related to the pollutant component involved and its source and dose. Health effects are also closely dependent on country, area, season, and time. An extended exposure duration to the pollutant should incline to long-term health effects in relation also to the above factors.
Particulate Matter (PMs), dust, benzene, and O 3 cause serious damage to the respiratory system ( 97 ). Moreover, there is a supplementary risk in case of existing respiratory disease such as asthma ( 98 ). Long-term effects are more frequent in people with a predisposing disease state. When the trachea is contaminated by pollutants, voice alterations may be remarked after acute exposure. Chronic obstructive pulmonary disease (COPD) may be induced following air pollution, increasing morbidity and mortality ( 99 ). Long-term effects from traffic, industrial air pollution, and combustion of fuels are the major factors for COPD risk ( 99 ).
Multiple cardiovascular effects have been observed after exposure to air pollutants ( 100 ). Changes occurred in blood cells after long-term exposure may affect cardiac functionality. Coronary arteriosclerosis was reported following long-term exposure to traffic emissions ( 101 ), while short-term exposure is related to hypertension, stroke, myocardial infracts, and heart insufficiency. Ventricle hypertrophy is reported to occur in humans after long-time exposure to nitrogen oxide (NO 2 ) ( 102 , 103 ).
Neurological effects have been observed in adults and children after extended-term exposure to air pollutants.
Psychological complications, autism, retinopathy, fetal growth, and low birth weight seem to be related to long-term air pollution ( 83 ). The etiologic agent of the neurodegenerative diseases (Alzheimer's and Parkinson's) is not yet known, although it is believed that extended exposure to air pollution seems to be a factor. Specifically, pesticides and metals are cited as etiological factors, together with diet. The mechanisms in the development of neurodegenerative disease include oxidative stress, protein aggregation, inflammation, and mitochondrial impairment in neurons ( 104 ) ( Figure 1 ).
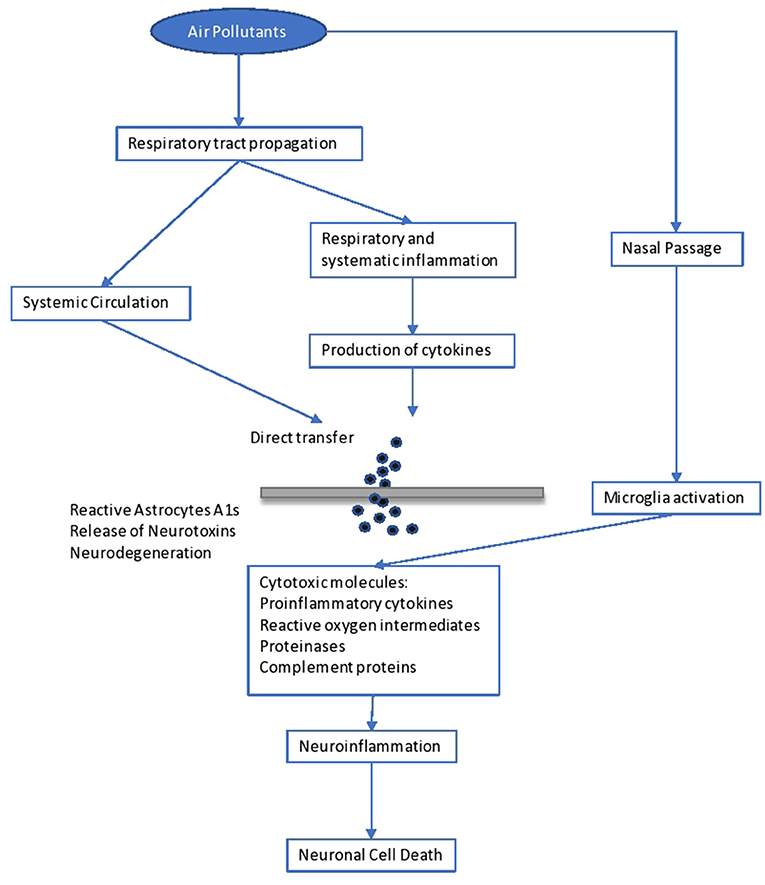
Figure 1 . Impact of air pollutants on the brain.
Brain inflammation was observed in dogs living in a highly polluted area in Mexico for a long period ( 105 ). In human adults, markers of systemic inflammation (IL-6 and fibrinogen) were found to be increased as an immediate response to PNC on the IL-6 level, possibly leading to the production of acute-phase proteins ( 106 ). The progression of atherosclerosis and oxidative stress seem to be the mechanisms involved in the neurological disturbances caused by long-term air pollution. Inflammation comes secondary to the oxidative stress and seems to be involved in the impairment of developmental maturation, affecting multiple organs ( 105 , 107 ). Similarly, other factors seem to be involved in the developmental maturation, which define the vulnerability to long-term air pollution. These include birthweight, maternal smoking, genetic background and socioeconomic environment, as well as education level.
However, diet, starting from breast-feeding, is another determinant factor. Diet is the main source of antioxidants, which play a key role in our protection against air pollutants ( 108 ). Antioxidants are free radical scavengers and limit the interaction of free radicals in the brain ( 108 ). Similarly, genetic background may result in a differential susceptibility toward the oxidative stress pathway ( 60 ). For example, antioxidant supplementation with vitamins C and E appears to modulate the effect of ozone in asthmatic children homozygous for the GSTM1 null allele ( 61 ). Inflammatory cytokines released in the periphery (e.g., respiratory epithelia) upregulate the innate immune Toll-like receptor 2. Such activation and the subsequent events leading to neurodegeneration have recently been observed in lung lavage in mice exposed to ambient Los Angeles (CA, USA) particulate matter ( 61 ). In children, neurodevelopmental morbidities were observed after lead exposure. These children developed aggressive and delinquent behavior, reduced intelligence, learning difficulties, and hyperactivity ( 109 ). No level of lead exposure seems to be “safe,” and the scientific community has asked the Centers for Disease Control and Prevention (CDC) to reduce the current screening guideline of 10 μg/dl ( 109 ).
It is important to state that impact on the immune system, causing dysfunction and neuroinflammation ( 104 ), is related to poor air quality. Yet, increases in serum levels of immunoglobulins (IgA, IgM) and the complement component C3 are observed ( 106 ). Another issue is that antigen presentation is affected by air pollutants, as there is an upregulation of costimulatory molecules such as CD80 and CD86 on macrophages ( 110 ).
As is known, skin is our shield against ultraviolet radiation (UVR) and other pollutants, as it is the most exterior layer of our body. Traffic-related pollutants, such as PAHs, VOCs, oxides, and PM, may cause pigmented spots on our skin ( 111 ). On the one hand, as already stated, when pollutants penetrate through the skin or are inhaled, damage to the organs is observed, as some of these pollutants are mutagenic and carcinogenic, and, specifically, they affect the liver and lung. On the other hand, air pollutants (and those in the troposphere) reduce the adverse effects of ultraviolet radiation UVR in polluted urban areas ( 111 ). Air pollutants absorbed by the human skin may contribute to skin aging, psoriasis, acne, urticaria, eczema, and atopic dermatitis ( 111 ), usually caused by exposure to oxides and photochemical smoke ( 111 ). Exposure to PM and cigarette smoking act as skin-aging agents, causing spots, dyschromia, and wrinkles. Lastly, pollutants have been associated with skin cancer ( 111 ).
Higher morbidity is reported to fetuses and children when exposed to the above dangers. Impairment in fetal growth, low birth weight, and autism have been reported ( 112 ).
Another exterior organ that may be affected is the eye. Contamination usually comes from suspended pollutants and may result in asymptomatic eye outcomes, irritation ( 112 ), retinopathy, or dry eye syndrome ( 113 , 114 ).
Environmental Impact of Air Pollution
Air pollution is harming not only human health but also the environment ( 115 ) in which we live. The most important environmental effects are as follows.
Acid rain is wet (rain, fog, snow) or dry (particulates and gas) precipitation containing toxic amounts of nitric and sulfuric acids. They are able to acidify the water and soil environments, damage trees and plantations, and even damage buildings and outdoor sculptures, constructions, and statues.
Haze is produced when fine particles are dispersed in the air and reduce the transparency of the atmosphere. It is caused by gas emissions in the air coming from industrial facilities, power plants, automobiles, and trucks.
Ozone , as discussed previously, occurs both at ground level and in the upper level (stratosphere) of the Earth's atmosphere. Stratospheric ozone is protecting us from the Sun's harmful ultraviolet (UV) rays. In contrast, ground-level ozone is harmful to human health and is a pollutant. Unfortunately, stratospheric ozone is gradually damaged by ozone-depleting substances (i.e., chemicals, pesticides, and aerosols). If this protecting stratospheric ozone layer is thinned, then UV radiation can reach our Earth, with harmful effects for human life (skin cancer) ( 116 ) and crops ( 117 ). In plants, ozone penetrates through the stomata, inducing them to close, which blocks CO 2 transfer and induces a reduction in photosynthesis ( 118 ).
Global climate change is an important issue that concerns mankind. As is known, the “greenhouse effect” keeps the Earth's temperature stable. Unhappily, anthropogenic activities have destroyed this protecting temperature effect by producing large amounts of greenhouse gases, and global warming is mounting, with harmful effects on human health, animals, forests, wildlife, agriculture, and the water environment. A report states that global warming is adding to the health risks of poor people ( 119 ).
People living in poorly constructed buildings in warm-climate countries are at high risk for heat-related health problems as temperatures mount ( 119 ).
Wildlife is burdened by toxic pollutants coming from the air, soil, or the water ecosystem and, in this way, animals can develop health problems when exposed to high levels of pollutants. Reproductive failure and birth effects have been reported.
Eutrophication is occurring when elevated concentrations of nutrients (especially nitrogen) stimulate the blooming of aquatic algae, which can cause a disequilibration in the diversity of fish and their deaths.
Without a doubt, there is a critical concentration of pollution that an ecosystem can tolerate without being destroyed, which is associated with the ecosystem's capacity to neutralize acidity. The Canada Acid Rain Program established this load at 20 kg/ha/yr ( 120 ).
Hence, air pollution has deleterious effects on both soil and water ( 121 ). Concerning PM as an air pollutant, its impact on crop yield and food productivity has been reported. Its impact on watery bodies is associated with the survival of living organisms and fishes and their productivity potential ( 121 ).
An impairment in photosynthetic rhythm and metabolism is observed in plants exposed to the effects of ozone ( 121 ).
Sulfur and nitrogen oxides are involved in the formation of acid rain and are harmful to plants and marine organisms.
Last but not least, as mentioned above, the toxicity associated with lead and other metals is the main threat to our ecosystems (air, water, and soil) and living creatures ( 121 ).
In 2018, during the first WHO Global Conference on Air Pollution and Health, the WHO's General Director, Dr. Tedros Adhanom Ghebreyesus, called air pollution a “silent public health emergency” and “the new tobacco” ( 122 ).
Undoubtedly, children are particularly vulnerable to air pollution, especially during their development. Air pollution has adverse effects on our lives in many different respects.
Diseases associated with air pollution have not only an important economic impact but also a societal impact due to absences from productive work and school.
Despite the difficulty of eradicating the problem of anthropogenic environmental pollution, a successful solution could be envisaged as a tight collaboration of authorities, bodies, and doctors to regularize the situation. Governments should spread sufficient information and educate people and should involve professionals in these issues so as to control the emergence of the problem successfully.
Technologies to reduce air pollution at the source must be established and should be used in all industries and power plants. The Kyoto Protocol of 1997 set as a major target the reduction of GHG emissions to below 5% by 2012 ( 123 ). This was followed by the Copenhagen summit, 2009 ( 124 ), and then the Durban summit of 2011 ( 125 ), where it was decided to keep to the same line of action. The Kyoto protocol and the subsequent ones were ratified by many countries. Among the pioneers who adopted this important protocol for the world's environmental and climate “health” was China ( 3 ). As is known, China is a fast-developing economy and its GDP (Gross Domestic Product) is expected to be very high by 2050, which is defined as the year of dissolution of the protocol for the decrease in gas emissions.
A more recent international agreement of crucial importance for climate change is the Paris Agreement of 2015, issued by the UNFCCC (United Nations Climate Change Committee). This latest agreement was ratified by a plethora of UN (United Nations) countries as well as the countries of the European Union ( 126 ). In this vein, parties should promote actions and measures to enhance numerous aspects around the subject. Boosting education, training, public awareness, and public participation are some of the relevant actions for maximizing the opportunities to achieve the targets and goals on the crucial matter of climate change and environmental pollution ( 126 ). Without any doubt, technological improvements makes our world easier and it seems difficult to reduce the harmful impact caused by gas emissions, we could limit its use by seeking reliable approaches.
Synopsizing, a global prevention policy should be designed in order to combat anthropogenic air pollution as a complement to the correct handling of the adverse health effects associated with air pollution. Sustainable development practices should be applied, together with information coming from research in order to handle the problem effectively.
At this point, international cooperation in terms of research, development, administration policy, monitoring, and politics is vital for effective pollution control. Legislation concerning air pollution must be aligned and updated, and policy makers should propose the design of a powerful tool of environmental and health protection. As a result, the main proposal of this essay is that we should focus on fostering local structures to promote experience and practice and extrapolate these to the international level through developing effective policies for sustainable management of ecosystems.
Author Contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Conflict of Interest
IM is employed by the company Delphis S.A.
The remaining authors declare that the present review paper was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. WHO. Air Pollution . WHO. Available online at: http://www.who.int/airpollution/en/ (accessed October 5, 2019).
Google Scholar
2. Moores FC. Climate change and air pollution: exploring the synergies and potential for mitigation in industrializing countries. Sustainability . (2009) 1:43–54. doi: 10.3390/su1010043
CrossRef Full Text | Google Scholar
3. USGCRP (2009). Global Climate Change Impacts in the United States. In: Karl TR, Melillo JM, Peterson TC, editors. Climate Change Impacts by Sectors: Ecosystems . New York, NY: United States Global Change Research Program. Cambridge University Press.
4. Marlon JR, Bloodhart B, Ballew MT, Rolfe-Redding J, Roser-Renouf C, Leiserowitz A, et al. (2019). How hope and doubt affect climate change mobilization. Front. Commun. 4:20. doi: 10.3389/fcomm.2019.00020
5. Eze IC, Schaffner E, Fischer E, Schikowski T, Adam M, Imboden M, et al. Long- term air pollution exposure and diabetes in a population-based Swiss cohort. Environ Int . (2014) 70:95–105. doi: 10.1016/j.envint.2014.05.014
PubMed Abstract | CrossRef Full Text | Google Scholar
6. Kelishadi R, Poursafa P. Air pollution and non-respiratory health hazards for children. Arch Med Sci . (2010) 6:483–95. doi: 10.5114/aoms.2010.14458
7. Manucci PM, Franchini M. Health effects of ambient air pollution in developing countries. Int J Environ Res Public Health . (2017) 14:1048. doi: 10.3390/ijerph14091048
8. Burden of Disease from Ambient and Household Air Pollution . Available online: http://who.int/phe/health_topics/outdoorair/databases/en/ (accessed August 15, 2017).
9. Hashim D, Boffetta P. Occupational and environmental exposures and cancers in developing countries. Ann Glob Health . (2014) 80:393–411. doi: 10.1016/j.aogh.2014.10.002
10. Guo Y, Zeng H, Zheng R, Li S, Pereira G, Liu Q, et al. The burden of lung cancer mortality attributable to fine particles in China. Total Environ Sci . (2017) 579:1460–6. doi: 10.1016/j.scitotenv.2016.11.147
11. Hou Q, An XQ, Wang Y, Guo JP. An evaluation of resident exposure to respirable particulate matter and health economic loss in Beijing during Beijing 2008 Olympic Games. Sci Total Environ . (2010) 408:4026–32. doi: 10.1016/j.scitotenv.2009.12.030
12. Kan H, Chen R, Tong S. Ambient air pollution, climate change, and population health in China. Environ Int . (2012) 42:10–9. doi: 10.1016/j.envint.2011.03.003
13. Burroughs Peña MS, Rollins A. Environmental exposures and cardiovascular disease: a challenge for health and development in low- and middle-income countries. Cardiol Clin . (2017) 35:71–86. doi: 10.1016/j.ccl.2016.09.001
14. Kankaria A, Nongkynrih B, Gupta S. Indoor air pollution in india: implications on health and its control. Indian J Comm Med . 39:203–7. doi: 10.4103/0970-0218.143019
15. Parajuli I, Lee H, Shrestha KR. Indoor air quality and ventilation assessment of rural mountainous households of Nepal. Int J Sust Built Env . (2016) 5:301–11. doi: 10.1016/j.ijsbe.2016.08.003
16. Saud T, Gautam R, Mandal TK, Gadi R, Singh DP, Sharma SK. Emission estimates of organic and elemental carbon from household biomass fuel used over the Indo-Gangetic Plain (IGP), India. Atmos Environ . (2012) 61:212–20. doi: 10.1016/j.atmosenv.2012.07.030
17. Singh DP, Gadi R, Mandal TK, Saud T, Saxena M, Sharma SK. Emissions estimates of PAH from biomass fuels used in rural sector of Indo-Gangetic Plains of India. Atmos Environ . (2013) 68:120–6. doi: 10.1016/j.atmosenv.2012.11.042
18. Dherani M, Pope D, Mascarenhas M, Smith KR, Weber M BN. Indoor air pollution from unprocessed solid fuel use and pneumonia risk in children aged under five years: a systematic review and meta-analysis. Bull World Health Organ . (2008) 86:390–4. doi: 10.2471/BLT.07.044529
19. Kassomenos P, Kelessis A, Petrakakis M, Zoumakis N, Christides T, Paschalidou AK. Air Quality assessment in a heavily-polluted urban Mediterranean environment through Air Quality indices. Ecol Indic . (2012) 18:259–68. doi: 10.1016/j.ecolind.2011.11.021
20. Dockery DW, Pope CA, Xu X, Spengler JD, Ware JH, Fay ME, et al. An association between air pollution and mortality in six U.S. cities. N Engl J Med . (1993) 329:1753–9. doi: 10.1056/NEJM199312093292401
21. Schwela DH, Köth-Jahr I. Leitfaden für die Aufstellung von Luftreinhalteplänen [Guidelines for the Implementation of Clean Air Implementation Plans]. Landesumweltamt des Landes Nordrhein Westfalen. State Environmental Service of the State of North Rhine-Westphalia (1994).
22. Newlands M. Environmental Activism, Environmental Politics, and Representation: The Framing of the British Environmental Activist Movement . Ph.D. thesis. University of East London, United Kingdom (2015).
23. NEPIS (National Service Center for Environmental Publications) US EPA (Environmental Protection Agency) (2017). Available online at: https://www.epa.gov/clean-air-act-overview/air-pollution-current-and-future-challenges (accessed August 15, 2017).
24. NRC (National Research Council). Available online at: https://www.nap.edu/read/10728/chapter/1,2014 (accessed September 17, 2019).
25. Bull A. Traffic Congestion: The Problem and How to Deal With It . Santiago: Nationes Unidas, Cepal (2003).
26. Spiegel J, Maystre LY. Environmental Pollution Control, Part VII - The Environment, Chapter 55, Encyclopedia of Occupational Health and Safety . Available online at: http://www.ilocis.org/documents/chpt55e.htm (accessed September 17, 2019).
27. European Community Reports. Assessment of the Effectiveness of European Air Quality Policies and Measures: Case Study 2; Comparison of the EU and US Air Quality Standards and Planning Requirements. (2004). Available online at: https://ec.europa.eu/environment/archives/cafe/activities/pdf/case_study2.pdf (accessed September 22, 2019).
28. Gibson R, Ward S. Parties in the digital age; a review. J Represent Democracy . (2009) 45:87–100. doi: 10.1080/00344890802710888
29. Kaun A, Uldam J. Digital activism: after the hype. New Media Soc. (2017) 20:2099–106. doi: 10.1177/14614448177319
30. Sivitanides M, Shah V. The era of digital activism. In: 2011 Conference for Information Systems Applied Research(CONISAR) Proceedings Wilmington North Carolina, USA . Available online at: https://www.arifyildirim.com/ilt510/marcos.sivitanides.vivek.shah.pdf (accessed September 22, 2019).
31. Möller L, Schuetzle D, Autrup H. Future research needs associated with the assessment of potential human health risks from exposure to toxic ambient air pollutants. Environ Health Perspect . (1994) 102(Suppl. 4):193–210. doi: 10.1289/ehp.94102s4193
32. Jacobson MZ, Jacobson PMZ. Atmospheric Pollution: History, Science, and Regulation. Cambridge University Press (2002). p. 206. doi: 10.1256/wea.243.02
33. Stover RH. Flooding of soil for disease control. In: Mulder D, editor. Chapter 3. Developments in Agricultural and Managed Forest Ecology . Elsevier (1979). p. 19–28. Available online at: http://www.sciencedirect.com/science/article/pii/B9780444416926500094 doi: 10.1016/B978-0-444-41692-6.50009-4 (accessed July 1, 2019).
34. Maipa V, Alamanos Y, Bezirtzoglou E. Seasonal fluctuation of bacterial indicators in coastal waters. Microb Ecol Health Dis . (2001) 13:143–6. doi: 10.1080/089106001750462687
35. Bezirtzoglou E, Dimitriou D, Panagiou A. Occurrence of Clostridium perfringens in river water by using a new procedure. Anaerobe . (1996) 2:169–73. doi: 10.1006/anae.1996.0022
36. Kjellstrom T, Lodh M, McMichael T, Ranmuthugala G, Shrestha R, Kingsland S. Air and Water Pollution: Burden and Strategies for Control. DCP, Chapter 43. 817–32 p. Available online at: https://www.dcp-3.org/sites/default/files/dcp2/DCP43.pdf (accessed September 17, 2017).
37. Pathak RK, Wang T, Ho KF, Lee SC. Characteristics of summertime PM2.5 organic and elemental carbon in four major Chinese cities: implications of high acidity for water- soluble organic carbon (WSOC). Atmos Environ . (2011) 45:318–25. doi: 10.1016/j.atmosenv.2010.10.021
38. Bonavigo L, Zucchetti M, Mankolli H. Water radioactive pollution and related environmental aspects. J Int Env Appl Sci . (2009) 4:357–63
39. World Health Organization (WHO). Preventing Disease Through Healthy Environments: Towards an Estimate of the Environmental Burden of Disease . 1106 p. Available online at: https://www.who.int/quantifying_ehimpacts/publications/preventingdisease.pdf (accessed September 22, 2019).
40. Stansfeld SA. Noise effects on health in the context of air pollution exposure. Int J Environ Res Public Health . (2015) 12:12735–60. doi: 10.3390/ijerph121012735
41. Ethical Unicorn. Everything You Need To Know About Aerosols & Air Pollution. (2019). Available online at: https://ethicalunicorn.com/2019/04/29/everything-you-need-to-know-about-aerosols-air-pollution/ (accessed October 4, 2019).
42. Colbeck I, Lazaridis M. Aerosols and environmental pollution. Sci Nat . (2009) 97:117–31. doi: 10.1007/s00114-009-0594-x
43. Incecik S, Gertler A, Kassomenos P. Aerosols and air quality. Sci Total Env . (2014) 355, 488–9. doi: 10.1016/j.scitotenv.2014.04.012
44. D'Amato G, Pawankar R, Vitale C, Maurizia L. Climate change and air pollution: effects on respiratory allergy. Allergy Asthma Immunol Res . (2016) 8:391–5. doi: 10.4168/aair.2016.8.5.391
45. Bezirtzoglou C, Dekas K, Charvalos E. Climate changes, environment and infection: facts, scenarios and growing awareness from the public health community within Europe. Anaerobe . (2011) 17:337–40. doi: 10.1016/j.anaerobe.2011.05.016
46. Castelli F, Sulis G. Migration and infectious diseases. Clin Microbiol Infect . (2017) 23:283–9. doi: 10.1016/j.cmi.2017.03.012
47. Watson JT, Gayer M, Connolly MA. Epidemics after natural disasters. Emerg Infect Dis . (2007) 13:1–5. doi: 10.3201/eid1301.060779
48. Fenn B. Malnutrition in Humanitarian Emergencies . Available online at: https://www.who.int/diseasecontrol_emergencies/publications/idhe_2009_london_malnutrition_fenn.pdf . (accessed August 15, 2017).
49. Lindh E, Argentini C, Remoli ME, Fortuna C, Faggioni G, Benedetti E, et al. The Italian 2017 outbreak Chikungunya virus belongs to an emerging Aedes albopictus –adapted virus cluster introduced from the Indian subcontinent. Open Forum Infect Dis. (2019) 6:ofy321. doi: 10.1093/ofid/ofy321
50. Calba C, Guerbois-Galla M, Franke F, Jeannin C, Auzet-Caillaud M, Grard G, Pigaglio L, Decoppet A, et al. Preliminary report of an autochthonous chikungunya outbreak in France, July to September 2017. Eur Surveill . (2017) 22:17-00647. doi: 10.2807/1560-7917.ES.2017.22.39.17-00647
51. Menne B, Murray V. Floods in the WHO European Region: Health Effects and Their Prevention . Copenhagen: WHO; Weltgesundheits organisation, Regionalbüro für Europa (2013). Available online at: http://www.euro.who.int/data/assets/pdf_file/0020/189020/e96853.pdf (accessed 15 August 2017).
52. Schneider SH. The greenhouse effect: science and policy. Science . (1989) 243:771–81. doi: 10.1126/science.243.4892.771
53. Wilson WE, Suh HH. Fine particles and coarse particles: concentration relationships relevant to epidemiologic studies. J Air Waste Manag Assoc . (1997) 47:1238–49. doi: 10.1080/10473289.1997.10464074
54. US EPA (US Environmental Protection Agency) (2018). Available online at: https://www.epa.gov/pm-pollution/particulate-matter-pm-basics (accessed September 22, 2018).
55. Cheung K, Daher N, Kam W, Shafer MM, Ning Z, Schauer JJ, et al. Spatial and temporal variation of chemical composition and mass closure of ambient coarse particulate matter (PM10–2.5) in the Los Angeles area. Atmos Environ . (2011) 45:2651–62. doi: 10.1016/j.atmosenv.2011.02.066
56. Zhang L, Yang Y, Li Y, Qian ZM, Xiao W, Wang X, et al. Short-term and long-term effects of PM2.5 on acute nasopharyngitis in 10 communities of Guangdong, China. Sci Total Env. (2019) 688:136–42. doi: 10.1016/j.scitotenv.2019.05.470.
57. Kloog I, Ridgway B, Koutrakis P, Coull BA, Schwartz JD. Long- and short-term exposure to PM2.5 and mortality using novel exposure models, Epidemiology . (2013) 24:555–61. doi: 10.1097/EDE.0b013e318294beaa
58. New Hampshire Department of Environmental Services. Current and Forecasted Air Quality in New Hampshire . Environmental Fact Sheet (2019). Available online at: https://www.des.nh.gov/organization/commissioner/pip/factsheets/ard/documents/ard-16.pdf (accessed September 22, 2019).
59. Kappos AD, Bruckmann P, Eikmann T, Englert N, Heinrich U, Höppe P, et al. Health effects of particles in ambient air. Int J Hyg Environ Health . (2004) 207:399–407. doi: 10.1078/1438-4639-00306
60. Boschi N (Ed.). Defining an educational framework for indoor air sciences education. In: Education and Training in Indoor Air Sciences . Luxembourg: Springer Science & Business Media (2012). 245 p.
61. Heal MR, Kumar P, Harrison RM. Particles, air quality, policy and health. Chem Soc Rev . (2012) 41:6606–30. doi: 10.1039/c2cs35076a
62. Bezirtzoglou E, Alexopoulos A. Ozone history and ecosystems: a goliath from impacts to advance industrial benefits and interests, to environmental and therapeutical strategies. In: Ozone Depletion, Chemistry and Impacts. (2009). p. 135–45.
63. Villányi V, Turk B, Franc B, Csintalan Z. Ozone Pollution and its Bioindication. In: Villányi V, editor. Air Pollution . London: Intech Open (2010). doi: 10.5772/10047
64. Massachusetts Department of Public Health. Massachusetts State Health Assessment . Boston, MA (2017). Available online at: https://www.mass.gov/files/documents/2017/11/03/2017%20MA%20SHA%20final%20compressed.pdf (accessed October 30, 2017).
65. Lorenzini G, Saitanis C. Ozone: A Novel Plant “Pathogen.” In: Sanitá di Toppi L, Pawlik-Skowrońska B, editors. Abiotic Stresses in Plant Springer Link (2003). p. 205–29. doi: 10.1007/978-94-017-0255-3_8
66. Fares S, Vargas R, Detto M, Goldstein AH, Karlik J, Paoletti E, et al. Tropospheric ozone reduces carbon assimilation in trees: estimates from analysis of continuous flux measurements. Glob Change Biol . (2013) 19:2427–43. doi: 10.1111/gcb.12222
67. Harmens H, Mills G, Hayes F, Jones L, Norris D, Fuhrer J. Air Pollution and Vegetation . ICP Vegetation Annual Report 2006/2007. (2012)
68. Emberson LD, Pleijel H, Ainsworth EA, den Berg M, Ren W, Osborne S, et al. Ozone effects on crops and consideration in crop models. Eur J Agron . (2018) 100:19–34. doi: 10.1016/j.eja.2018.06.002
69. Alexopoulos A, Plessas S, Ceciu S, Lazar V, Mantzourani I, Voidarou C, et al. Evaluation of ozone efficacy on the reduction of microbial population of fresh cut lettuce ( Lactuca sativa ) and green bell pepper ( Capsicum annuum ). Food Control . (2013) 30:491–6. doi: 10.1016/j.foodcont.2012.09.018
70. Alexopoulos A, Plessas S, Kourkoutas Y, Stefanis C, Vavias S, Voidarou C, et al. Experimental effect of ozone upon the microbial flora of commercially produced dairy fermented products. Int J Food Microbiol . (2017) 246:5–11. doi: 10.1016/j.ijfoodmicro.2017.01.018
71. Maggio A, Fagnano M. Ozone damages to mediterranean crops: physiological responses. Ital J Agron . (2008) 13–20. doi: 10.4081/ija.2008.13
72. McCarthy JT, Pelle E, Dong K, Brahmbhatt K, Yarosh D, Pernodet N. Effects of ozone in normal human epidermal keratinocytes. Exp Dermatol . (2013) 22:360–1. doi: 10.1111/exd.12125
73. WHO. Health Risks of Ozone From Long-Range Transboundary Air Pollution . Available online at: http://www.euro.who.int/data/assets/pdf_file/0005/78647/E91843.pdf (accessed August 15, 2019).
74. Thiele JJ, Traber MG, Tsang K, Cross CE, Packer L. In vivo exposure to ozone depletes vitamins C and E and induces lipid peroxidation in epidermal layers of murine skin. Free Radic Biol Med. (1997) 23:365–91. doi: 10.1016/S0891-5849(96)00617-X
75. Hatch GE, Slade R, Harris LP, McDonnell WF, Devlin RB, Koren HS, et al. Ozone dose and effect in humans and rats. A comparison using oxygen- 18 labeling and bronchoalveolar lavage. Am J Respir Crit Care Med . (1994) 150:676–83. doi: 10.1164/ajrccm.150.3.8087337
76. Lippmann M. Health effects of ozone. A critical review. JAPCA . (1989) 39:672–95. doi: 10.1080/08940630.1989.10466554
77. Gryparis A, Forsberg B, Katsouyanni K, Analitis A, Touloumi G, Schwartz J, et al. Acute effects of ozone on mortality from the “air pollution and health: a European approach” project. Am J Respir Crit Care Med . (2004) 170:1080–7. doi: 10.1164/rccm.200403-333OC
78. Soon W, Baliunas SL, Robinson AB, Robinson ZW. Environmental effects of increased atmospheric carbon dioxide. Climate Res . (1999) 13:149–64 doi: 10.1260/0958305991499694
79. Richmont-Bryant J, Owen RC, Graham S, Snyder M, McDow S, Oakes M, et al. Estimation of on-road NO2 concentrations, NO2/NOX ratios, and related roadway gradients from near-road monitoring data. Air Qual Atm Health . (2017) 10:611–25. doi: 10.1007/s11869-016-0455-7
80. Hesterberg TW, Bunn WB, McClellan RO, Hamade AK, Long CM, Valberg PA. Critical review of the human data on short-term nitrogen dioxide (NO 2 ) exposures: evidence for NO2 no-effect levels. Crit Rev Toxicol . (2009) 39:743–81. doi: 10.3109/10408440903294945
81. Chen T-M, Gokhale J, Shofer S, Kuschner WG. Outdoor air pollution: nitrogen dioxide, sulfur dioxide, and carbon monoxide health effects. Am J Med Sci . (2007) 333:249–56. doi: 10.1097/MAJ.0b013e31803b900f
82. US EPA. Table of Historical SO 2 NAAQS, Sulfur US EPA . Available online at: https://www3.epa.gov/ttn/naaqs/standards/so2/s_so2_history.html (accessed October 5, 2019).
83. WHO Regional Office of Europe (2000). Available online at: https://euro.who.int/_data/assets/pdf_file/0020/123086/AQG2ndEd_7_4Sulfuroxide.pdf
84. Pruss-Ustun A, Fewrell L, Landrigan PJ, Ayuso-Mateos JL. Lead exposure. Comparative Quantification of Health Risks . World Health Organization. p. 1495–1542. Available online at: https://www.who.int/publications/cra/chapters/volume2/1495-1542.pdf?ua=1
PubMed Abstract | Google Scholar
85. Goyer RA. Transplacental transport of lead. Environ Health Perspect . (1990) 89:101–5. doi: 10.1289/ehp.9089101
86. National Institute of Environmental Health Sciences (NIH). Lead and Your Health . (2013). 1–4 p. Available online at: https://www.niehs.nih.gov/health/materials/lead_and_your_health_508.pdf (accessed September 17, 2019).
87. Farhat A, Mohammadzadeh A, Balali-Mood M, Aghajanpoor-Pasha M, Ravanshad Y. Correlation of blood lead level in mothers and exclusively breastfed infants: a study on infants aged less than six months. Asia Pac J Med Toxicol . (2013) 2:150–2.
88. Assi MA, Hezmee MNM, Haron AW, Sabri MYM, Rajion MA. The detrimental effects of lead on human and animal health. Vet World . (2016) 9:660–71. doi: 10.14202/vetworld.2016.660-671
89. Abdel-Shafy HI, Mansour MSM. A review on polycyclic aromatic hydrocarbons: source, environmental impact, effect on human health and remediation. Egypt J Pet . (2016) 25:107–23. doi: 10.1016/j.ejpe.2015.03.011
90. Kumar A, Singh BP, Punia M, Singh D, Kumar K, Jain VK. Assessment of indoor air concentrations of VOCs and their associated health risks in the library of Jawaharlal Nehru University, New Delhi. Environ Sci Pollut Res Int . (2014) 21:2240–8. doi: 10.1007/s11356-013-2150-7
91. Molhave L, Clausen G, Berglund B, Ceaurriz J, Kettrup A, Lindvall T, et al. Total Volatile Organic Compounds (TVOC) in Indoor Air Quality Investigations. Indoor Air . 7:225–240. doi: 10.1111/j.1600-0668.1997.00002.x
92. Gibb T. Indoor Air Quality May be Hazardous to Your Health . MSU Extension. Available online at: https://www.canr.msu.edu/news/indoor_air_quality_may_be_hazardous_to_your_health (accessed October 5, 2019).
93. Ebersviller S, Lichtveld K, Sexton KG, Zavala J, Lin Y-H, Jaspers I, et al. Gaseous VOCs rapidly modify particulate matter and its biological effects – Part 1: simple VOCs and model PM. Atmos Chem Phys Discuss . (2012) 12:5065–105. doi: 10.5194/acpd-12-5065-2012
94. WHO (World Health Organization). Dioxins and Their Effects on Human Health. Available online at: https://www.who.int/news-room/fact-sheets/detail/dioxins-and-their-effects-on-human-health (accessed October 5, 2019).
95. EEA (European Environmental Agency). Air Quality Standards to the European Union and WHO . Available online at: https://www.eea.europa.eu/themes/data-and-maps/figures/air-quality-standards-under-the
96. Nakano T, Otsuki T. [Environmental air pollutants and the risk of cancer]. (Japanese). Gan To Kagaku Ryoho . (2013) 40:1441–5.
97. Kurt OK, Zhang J, Pinkerton KE. Pulmonary health effects of air pollution. Curr Opin Pulm Med . (2016) 22:138–43. doi: 10.1097/MCP.0000000000000248
98. Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet . (2014) 383:1581–92. doi: 10.1016/S0140-6736(14)60617-6
99. Jiang X-Q, Mei X-D, Feng D. Air pollution and chronic airway diseases: what should people know and do? J Thorac Dis . (2016) 8:E31–40.
100. Bourdrel T, Bind M-A, Béjot Y, Morel O, Argacha J-F. Cardiovascular effects of air pollution. Arch Cardiovasc Dis . (2017) 110:634–42. doi: 10.1016/j.acvd.2017.05.003
101. Hoffmann B, Moebus S, Möhlenkamp S, Stang A, Lehmann N, Dragano N, et al. Residential exposure to traffic is associated with coronary atherosclerosis. Circulation . (2007) 116:489–496. doi: 10.1161/CIRCULATIONAHA.107.693622
102. Katholi RE, Couri DM. Left ventricular hypertrophy: major risk factor in patients with hypertension: update and practical clinical applications. Int J Hypertens . (2011) 2011:495349. doi: 10.4061/2011/495349
103. Leary PJ, Kaufman JD, Barr RG, Bluemke DA, Curl CL, Hough CL, et al. Traffic- related air pollution and the right ventricle. the multi-ethnic study of atherosclerosis. Am J Respir Crit Care Med . (2014) 189:1093–100. doi: 10.1164/rccm.201312-2298OC
104. Genc S, Zadeoglulari Z, Fuss SH, Genc K. The adverse effects of air pollution on the nervous system. J Toxicol . (2012) 2012:782462. doi: 10.1155/2012/782462
105. Calderon-Garciduenas L, Azzarelli B, Acuna H, et al. Air pollution and brain damage. Toxicol Pathol. (2002) 30:373–89. doi: 10.1080/01926230252929954
106. Rückerl R, Greven S, Ljungman P, Aalto P, Antoniades C, Bellander T, et al. Air pollution and inflammation (interleukin-6, C-reactive protein, fibrinogen) in myocardial infarction survivors. Environ Health Perspect . (2007) 115:1072–80. doi: 10.1289/ehp.10021
107. Peters A, Veronesi B, Calderón-Garcidueñas L, Gehr P, Chen LC, Geiser M, et al. Translocation and potential neurological effects of fine and ultrafine particles a critical update. Part Fibre Toxicol . (2006) 3:13–8. doi: 10.1186/1743-8977-3-13
108. Kelly FJ. Dietary antioxidants and environmental stress. Proc Nutr Soc . (2004) 63:579–85. doi: 10.1079/PNS2004388
109. Bellinger DC. Very low lead exposures and children's neurodevelopment. Curr Opin Pediatr . (2008) 20:172–7. doi: 10.1097/MOP.0b013e3282f4f97b
110. Balbo P, Silvestri M, Rossi GA, Crimi E, Burastero SE. Differential role of CD80 and CD86 on alveolar macrophages in the presentation of allergen to T lymphocytes in asthma. Clin Exp Allergy J Br Soc Allergy Clin Immunol . (2001) 31:625–36. doi: 10.1046/j.1365-2222.2001.01068.x
111. Drakaki E, Dessinioti C, Antoniou C. Air pollution and the skin. Front Environ Sci Eng China . (2014) 15:2–8. doi: 10.3389/fenvs.2014.00011
112. Weisskopf MG, Kioumourtzoglou M-A, Roberts AL. Air pollution and autism spectrum disorders: causal or confounded? Curr Environ Health Rep . (2015) 2:430–9. doi: 10.1007/s40572-015-0073-9
113. Mo Z, Fu Q, Lyu D, Zhang L, Qin Z, Tang Q, et al. Impacts of air pollution on dry eye disease among residents in Hangzhou, China: a case-crossover study. Environ Pollut . (2019) 246:183–9. doi: 10.1016/j.envpol.2018.11.109
114. Klopfer J. Effects of environmental air pollution on the eye. J Am Optom Assoc . (1989) 60:773–8.
115. Ashfaq A, Sharma P. Environmental effects of air pollution and application of engineered methods to combat the problem. J Indust Pollut Control . (2012) 29.
116. Madronich S, de Gruijl F. Skin cancer and UV radiation. Nature . (1993) 366:23–9. doi: 10.1038/366023a0
117. Teramura A. Effects of UV-B radiation on the growth and yield of crop plants. Physiol Plant . (2006) 58:415–27. doi: 10.1111/j.1399-3054.1983.tb04203.x
118. Singh E, Tiwari S, Agrawal M. Effects of elevated ozone on photosynthesis and stomatal conductance of two soybean varieties: a case study to assess impacts of one component of predicted global climate change. Plant Biol Stuttg Ger . (2009) 11(Suppl. 1):101–8. doi: 10.1111/j.1438-8677.2009.00263.x
119. Manderson L. How global Warming is Adding to the Health Risks of Poor People . The Conversation. University of the Witwatersrand. Available online at: http://theconversation.com/how-global-warming-is-adding-to-the-health-risks-of-poor-people-109520 (accessed October 5, 2019).
120. Ministers of Energy and Environment. Federal/Provincial/Territorial Ministers of Energy and Environment (Canada), editor. The Canada-Wide Acid Rain Strategy for Post-2000 . Halifax: The Ministers (1999). 11 p.
121. Zuhara S, Isaifan R. The impact of criteria air pollutants on soil and water: a review. (2018) 278–84. doi: 10.30799/jespr.133.18040205
122. WHO. First WHO Global Conference on Air Pollution and Health. (2018). Available online at: https://www.who.int/airpollution/events/conference/en/ (accessed October 6, 2019).
123. What is the Kyoto Protocol? UNFCCC . Available online at: https://unfccc.int/kyoto__protocol (accessed October 6, 2019).
124. CopenhagenClimate Change Conference (UNFCCC) . Available online at: https://unfccc.int/process-and-meetings/conferences/past-conferences/copenhagen-climate-change-conference-december-2009/copenhagen-climate-change-conference-december-2009 (accessed October 6, 2019).
125. Durban Climate Change Conference,. UNFCCC (2011). Available online at: https://unfccc.int/process-and-meetings/conferences/past-conferences/copenhagen-climate-change-conference-december-2009/copenhagen-climate-change-conference-december-2009 (accessed October 6, 2019).
126. Paris Climate Change Agreement,. (2016). Available online at: https://unfccc.int/process-and-meetings/the-paris-agreement/the-paris-agreement
Keywords: air pollution, environment, health, public health, gas emission, policy
Citation: Manisalidis I, Stavropoulou E, Stavropoulos A and Bezirtzoglou E (2020) Environmental and Health Impacts of Air Pollution: A Review. Front. Public Health 8:14. doi: 10.3389/fpubh.2020.00014
Received: 17 October 2019; Accepted: 17 January 2020; Published: 20 February 2020.
Reviewed by:
Copyright © 2020 Manisalidis, Stavropoulou, Stavropoulos and Bezirtzoglou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ioannis Manisalidis, giannismanisal@gmail.com ; Elisavet Stavropoulou, elisabeth.stavropoulou@gmail.com
† These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
The effect of air-pollution and weather exposure on mortality and hospital admission and implications for further research: A systematic scoping review
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation School of Geography and Sustainable Development, University of St Andrews, Scotland, United Kingdom
Roles Conceptualization, Funding acquisition, Supervision, Writing – review & editing
Affiliation School of Medicine, University of St Andrews, Scotland, United Kingdom
Roles Methodology, Validation
Affiliation Department of Landscape Design and Ecosystem Management, American University of Beirut, Beirut, Lebanon
Roles Conceptualization, Funding acquisition, Investigation, Supervision, Writing – review & editing
- Mary Abed Al Ahad,
- Frank Sullivan,
- Urška Demšar,
- Maya Melhem,

- Published: October 29, 2020
- https://doi.org/10.1371/journal.pone.0241415
- Peer Review
- Reader Comments
Air-pollution and weather exposure beyond certain thresholds have serious effects on public health. Yet, there is lack of information on wider aspects including the role of some effect modifiers and the interaction between air-pollution and weather. This article aims at a comprehensive review and narrative summary of literature on the association of air-pollution and weather with mortality and hospital admissions; and to highlight literature gaps that require further research.
We conducted a scoping literature review. The search on two databases (PubMed and Web-of-Science) from 2012 to 2020 using three conceptual categories of “environmental factors”, “health outcomes”, and “Geographical region” revealed a total of 951 records. The narrative synthesis included all original studies with time-series, cohort, or case cross-over design; with ambient air-pollution and/or weather exposure; and mortality and/or hospital admission outcomes.
The final review included 112 articles from which 70 involved mortality, 30 hospital admission, and 12 studies included both outcomes. Air-pollution was shown to act consistently as risk factor for all-causes, cardiovascular, respiratory, cerebrovascular and cancer mortality and hospital admissions. Hot and cold temperature was a risk factor for wide range of cardiovascular, respiratory, and psychiatric illness; yet, in few studies, the increase in temperature reduced the risk of hospital admissions for pulmonary embolism, angina pectoris, chest, and ischemic heart diseases. The role of effect modification in the included studies was investigated in terms of gender, age, and season but not in terms of ethnicity.
Air-pollution and weather exposure beyond certain thresholds affect human health negatively. Effect modification of important socio-demographics such as ethnicity and the interaction between air-pollution and weather is often missed in the literature. Our findings highlight the need of further research in the area of health behaviour and mortality in relation to air-pollution and weather, to guide effective environmental health precautionary measures planning.
Citation: Abed Al Ahad M, Sullivan F, Demšar U, Melhem M, Kulu H (2020) The effect of air-pollution and weather exposure on mortality and hospital admission and implications for further research: A systematic scoping review. PLoS ONE 15(10): e0241415. https://doi.org/10.1371/journal.pone.0241415
Editor: Chon-Lin Lee, National Sun Yat-sen University, TAIWAN
Received: June 23, 2020; Accepted: October 15, 2020; Published: October 29, 2020
Copyright: © 2020 Abed Al Ahad et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting Information files.
Funding: This review is part of a PhD project that is funded by the St Leonard’s PhD scholarship, University of St Andrews, Scotland, United Kingdom. The open access publication fees were funded by the University of St Andrews Libraries, Scotland, United Kingdom.
Competing interests: The authors declare that they have no conflict of interest.
Introduction
Air-pollution and weather exposure beyond region-specific thresholds have serious effects on the public health [ 1 , 2 ]. Worldwide, population growth, increased urbanization, economic and industrial growth, intense energy consumption, high usage of transportation vehicles, improved living standards, and changing lifestyles and consumption patterns for at least the last 100 years have resulted in increased emissions of air pollutants including greenhouse gases; and fluctuations in ambient temperature and other weather variables [ 3 , 4 ].
Ambient air-pollution consists of a range of pollutants including particulate matters with diameters of less than 10 μm (PM10) and less than 2.5 μm (PM2.5), nitrogen oxides (NOx) including nitrogen dioxide (NO2), Sulphur dioxide (SO2), Carbon monoxide (CO), and Ozone (O3) that have been associated with a range of different acute and chronic health conditions [ 5 , 6 ].
Weather exposure in terms of changing temperature, relative humidity, rainfall and other weather patterns can cause a wide range of acute illness and result in deaths especially among vulnerable populations who lack adequate physiological and behavioural responses to weather fluctuations [ 7 , 8 ]. Age (elderly and children vs adults), sex, socioeconomic factors (poverty, education, and ethnicity among others), pre-existing chronic diseases, use of certain medications, and environmental conditions such as the absence of central heating increase individual’s susceptibility to environmental exposures [ 1 , 9 , 10 ]. Research has shown that hospital admissions and mortality increase when weather exposure exceed certain thresholds with lags up to 20 days [ 11 – 14 ].
Most of the literature has shown positive correlations of air-pollution and/or exposure to weather variables beyond region-specific thresholds with all-cause and cause-specific mortality and/or hospital admission especially related to respiratory and cardiovascular diseases [ 14 – 21 ]. Though, there is a lack of information on wider aspects including the role of some effect modifiers such as ethnicity and the interaction between air-pollution and weather factors. Literature has shown that ethnic minorities often live in more disadvantaged, highly populated urban communities with poor housing conditions and higher levels of air pollution exposure [ 22 – 24 ]. This results in poorer health and higher risk for chronic health problems with time. Similar to ethnicity, the interaction between air-pollution and weather variables in relation to health outcomes is often missed in the literature despite its importance in minimizing biased estimations. Air pollutants are highly reactive, and their formation is either catalysed or slowed down based on the existing weather conditions. For example, the presence of sunlight catalyses the formation of ozone pollutant resulting in higher ozone concentrations during the summer [ 25 ].
In this context, a thorough literature review is needed to map the available literature and highlight areas that require further research and investigation. Not to mention that further understanding of the effect of air-pollution and weather exposure on mortality and hospital admission is needed to achieve better environmental and health system planning, organization, resources allocation, and interventions. This article aims to provide a comprehensive review and narrative summary (not numerical estimate) of literature on the association of air-pollution and weather with mortality and hospital admissions; and to shed the light on areas that require further research. As far as we are aware, this is the first literature review examining the effect of multiple exposures (air-pollution and weather) on multiple outcomes (mortality and hospital admissions). We chose to focus our scoping literature review on countries that are part of the single European Union (EU) market (Austria, Belgium, Bulgaria, Croatia, Republic of Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Netherlands, Poland, Portugal, Romania, Slovakia, Slovenia, Spain and Sweden, Norway, and Switzerland) and United Kingdom (UK) because these countries exhibit similar socio-economic, environmental, and health policies; minimizing the contextual differences in the effect of air-pollution and weather on mortality and hospital admission. Literature examining the effect of air-pollution and/or weather on mortality and hospital admissions in countries outside the EU and UK will be used for comparison purposes.
Materials and methods
Search strategy and database sources.
To ensure methodological reliability, we carried out our scoping literature review according to the “Preferred Reporting Items for Systematic Reviews and Meta-Analyses for scoping reviews” (PRISMA-ScR) guidelines ( S1 Checklist ) [ 26 ].
A literature search was performed on the 6 th of February 2020 using “PubMed” and “Web of Science” database sources that cover health, medical, and environmental literature. We attempted to assess the effects of air-pollution and weather events on mortality and hospital admission in Europe by searching original research articles published in peer-reviewed journals in the last 8 years (between 06/02/2012 and 06/02/2020 inclusive). We chose to review research published in the last 8 years because in March 2007, the European Union (EU) Heads of State and Government endorsed an “integrated climate change and energy strategy” that will come into action post the expiry of Kyoto Protocol targets in 2012 and that aims to combat climate change and weather fluctuations and cut air-pollution emissions to 30% below the 1990 levels [ 27 ].
Our search strategy was divided into three conceptual categories: “environmental factors”, “health outcomes”, and “Geographical region”. The “Environmental factors” refers to air-pollution, including PM10, PM2.5, NO2, SO2, CO, and O3 air pollutants and to weather variables, including air temperature, rainfall, wind, relative humidity, and vapour pressure. The “health outcomes” include hospital admissions and mortality and the “Geographical region” refers to the EU countries and UK. For each conceptual category, a set of “MeSH” and “All Fields” terms joined by the Boolean operator “OR” were developed. Later, the three conceptual categories’ search terms were joined using the Boolean operator “AND”. Our search strategy excluded the “influenza infections”, as these are considered confounders rather than outcomes for air-pollution and weather exposure. For more details about the search codes used to navigate PubMed and Web of Science search engines, please refer to S1 Table .
To minimize finding irrelevant literature, our search was limited to the following categories in the “Web of Science” search engine: environmental sciences, public environmental occupational health, medicine general internal, environmental studies, multidisciplinary sciences, geosciences multidisciplinary, respiratory system, geography physical, geography, cardiac cardiovascular systems, urban studies, healthcare sciences services, peripheral vascular disease, medicine research experimental, emergency medicine, critical care medicine, health policy services, primary healthcare, social sciences biomedical, and demography. Grey literature, non-English language articles, conference abstracts, books, reports, masters and PhD dissertations, and unpublished studies were excluded from this review.
Inclusion and exclusion criteria
To determine the studies that would be included in this scoping review, a set of inclusion and exclusion criteria were developed for the procedure of title, keyword, and abstract screening.
The inclusion criteria involved original quantitative research studies conducted in the EU and UK; that included at least one analysis where mortality and/or hospital admission was the outcome and where one or more of the following exposures were investigated: 1) ambient air pollutants including PM10, PM2.5, CO, NO2/NOx, SO2, and O3; 2) weather exposures including temperature, rainfall, wind, humidity, and pressure; and 3) extreme weather events including heat waves, cold spells, and droughts. Due to the large amount of literature on this topic and to allow comparable results between the studies, this review was limited to cohort, time-series, and case-crossover/self-controlled quantitative study designs where hazard ratios (HR), relative risks (RR), odd ratios (OR), or percentage increase were reported for quantifying the factors associated with mortality and hospital admission. These three study designs allow a temporal follow up to evaluate the effect of time varying exposures (air-pollution and weather) on the mortality and hospital admission health outcomes.
The exclusion criteria included the following:
- Methodological studies
- Original data studies that investigated the effect of ambient air-pollution and/or weather on mortality and/or hospital admission in countries outside the EU market and UK
- Articles studying the effect of indoor air-pollution on mortality and hospital admission
- Studies examining air-pollution and weather exposure on animals and plants
- Studies on occupational air-pollution exposure
- Non-English language articles
- Mortality and/or hospital admission projections and forecasting studies
- Protocol and letter to editor papers
- Qualitative research studies
- All types of literature reviews including but not limited to narrative, scoping, and systematic literature reviews
Screening and data abstraction
Our search strategy revealed 487 articles from the “PubMed” database and 517 articles from the “Web of Science” database. These articles were exported to the citation manager software “Endnote” where 53 duplicates were identified and removed resulting in a total of 951 articles ( Fig 1 ). Using the titles, key words, and abstracts, the 951 articles were screened for relevance according to the inclusion and exclusion criteria, explained in the previous section only by first author (MA). To ensure a rigorous and reliable application of the inclusion and exclusion criteria in the screening process, a second researcher (MM) screened independently a sample of 20% of the titles and abstracts of the 951 identified records. Disagreements between the two researchers were resolved through discussion until consensus was reached. All the studies that met the inclusion criteria (n = 149 articles) were retrieved for full text screening by MA. Following the full text screening phase, an additional 37 articles were excluded by MA resulting in a total of 112 articles to be included in the final narrative synthesis ( Fig 1 ).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0241415.g001
For narrative synthesis, the following information was retrieved from the 112 articles:
- Study design
- Location of the study population
- The outcome of interest
- Sample size
- Exposure variables
- The confounders adjusted for
- The assessed exposure time and the lags considered
- The exposure assessment method
- The statistical/modelling approach
- The relative risks (RR)/incident relative risks (IRR)/odd ratios (OR)/hazard ratios (HR) with their respective confidence intervals or the percentage increase that quantify the association between the outcome of interest (mortality and/or hospital admission) and the exposures (air-pollution and/or weather events).
Ethical approval
Not applicable for this scoping literature review as it only includes descriptive narrative analysis of 112 published articles.
A total of 112 studies ( S2 Table ) were included in the final narrative review from which 70 involved the mortality outcome, 30 the hospital admission outcome, and 12 studies included both health outcomes ( Table 1 ). Most of the studies used the time-series study design (n = 74, 66%) with Poisson models for data analysis, while minority of the reviewed studies employed the case-crossover design (n = 19, 17%) with conditional logistic regression for data analysis, and the cohort design (n = 18, 16%) with Cox hazard regression for data analysis ( Table 1 ).
https://doi.org/10.1371/journal.pone.0241415.t001
Most of the studies examined all-cause, cardiovascular and respiratory disease mortality and hospital admission outcomes while some studies tried to focus more directly on certain types of specific diseases such as psychiatric disorders including mania and depression, pulmonary embolism, myocardial infarction, stroke, ischemic heart disease, arrhythmias, atrial fibrillation, heart failure, cerebrovascular disease, chronic obstructive pulmonary disease (COPD), lung cancer, and diabetes ( Table 1 ).
Table 1 shows the descriptive statistics of the included articles. S2 Table summarise the characteristics of the included studies in more details by the type of investigated health outcome. S3 Table demonstrate the included article’s reported associations in terms of coefficients with 95% confidence intervals between air-pollution and/or weather exposure and mortality and/or hospital admission outcomes.
The effect of air-pollution on mortality and hospital admission
In this review, six air pollutants (PM2.5, PM10, O3, CO, SO2, and NO2/NOx) were identified as causes of increased rates of mortality and hospital admissions. Each pollutant affects a range of diseases, most commonly, cardiovascular, respiratory, and cerebrovascular diseases. Some of the health effects can be immediate while others might appear after several days of initial exposure ( Fig 2 ).
https://doi.org/10.1371/journal.pone.0241415.g002
The effect of particulate matter pollutants on mortality and hospital admission.
Particulate matter is a heterogeneous mixtures of liquid droplets and solid particles suspended in the air that can result either from natural resources (windblown Saharan and non-Saharan dust, volcano ashes, forest fires, pollen, etc…) or from man-made activities including industrial processes, transportation vehicle smoke, burning of fossil fuels, extensive energy usage, combustion processes, and grinding and mining industries [ 28 ]. Due to its size, mass composition, and chemical components, particulate matter with larger diameter (PM10) will be deposited in nasal cavities and upper airways while particulate matter with smaller diameter (PM2.5) may penetrate more deeply the respiratory system reaching the alveoli and blood stream, carrying with them various toxic substances [ 29 ]. This in turn will cause health problems in humans such as asthma, irregular heartbeat, nonfatal heart attacks, decreased lung function, coughing and difficulty breathing symptoms [ 30 ].
Our review showed that PM10 air-pollution is positively associated with a range of cardiovascular and respiratory diseases mortality and hospital admission outcomes ( Fig 3A and S3 Table ). Fischer et al. (2015) showed an elevated hazard of 1.06 (95% CI = 1.04 to 1.08) for cardiovascular disease mortality for every 10 μg/m3 increase in PM10 pollution in the Netherlands [ 31 ]. Likewise, PM10 pollution acted as a risk factor for respiratory diseases mortality (HR = 1.11, 95%CI = 1.08 to 1.15; RR = 1.056, 95%CI = 1.043 to 1.069) [ 21 , 32 ] and hospital admission (%increase = 0.69, 95% CI = 0.20 to 1.19) [ 20 ].
https://doi.org/10.1371/journal.pone.0241415.g003
Air-pollution with PM2.5 exhibited a similar effect on human health as that of PM10 ( Fig 3B and S3 Table ). Nevertheless, PM2.5 was shown to have a greater risk on human health as compared to PM10 due to its smaller diameter size allowing more deep penetration into the respiratory system [ 33 ]. In France, Sanyal et al. (2018) showed an increased risk of 1.11 and 1.02 for all-cause hospital admission and moratality respectively per 10 μg/m3 increase in PM2.5 pollutant [ 32 ].
The effect of ozone pollution on mortality and hospital admission.
Contrary to particulate matter pollution, the effect of ozone on mortality and hospital admission did not show a consistent effect. In some studies, ozone acted as a protective factor agianst mortality and hospital admission, while in other studies it showed increased risk or no association with mortality and hospital admissions ( Fig 3C and S3 Table ). This is related to the fact that ozone is a highly reactive pollutant and its formation is related to the presence of sunlight [ 25 ]. In a cohort study conducted by Carey et al. (2013) in England, ozone acted as a protective factor agianst all-cause mortality (HR = 0.96, 95%CI = 0.93 to 0.98), cardiovascular mortality (HR = 0.96, 95%CI = 0.94 to 0.98), respiratory mortality (HR = 0.93, 95%CI = 0.90 to 0.96), and lung cancer mortality (HR = 0.94, 95%CI = 0.90 to 0.98) [ 21 ]. However, ozone acted as a risk factor in some of the reviewed studies leading up to 2% increase in all-cause mortality per interquartile range increase of ozone concentration [ 34 – 37 ].
The effect of nitrogen oxides pollution on mortality and hospital admission.
Similar to other air pollutants, this review showed that exposure to nitrogen dioxide and nitrogen oxides pollution can cause many types of diseases resulting in increased risk for all-cause mortality and hospital admission [ 25 , 32 , 38 , 39 ] ( Fig 3D and S3 Table ). A study conducted in Belgium showed a 3.5% increase in cardiovascular hospital admission as well as 4.5% and 4.9% increase in ischemic stroke and haemorrhagic stroke hospital admissions respectively for each 10 μg/m3 increase in NO2 [ 40 ].
The effect of sulphur dioxide pollution on mortality and hospital admission.
Sulphur dioxide air-pollution is mainly caused from industrial processes and power plants that involve burning of fossil fuel. Exposure to SO2 pollution can cause mild health effects including eyes, nose, and throat irritations as well as severe health effects such as bronchial spasms and deaths due to respiratory insufficiency [ 41 ].
The effect of sulphur dioxide (SO2) on mortality and hospital admission was investigated in only 12 out of the 112 reviewed studies. Exposure to SO2 air-pollution was found to increase the risk for all-cause, cardiovascular, and respiratory mortality [ 21 , 39 , 42 ] ( Fig 3E and S3 Table ).
The effect of carbon monoxide pollution on mortality and hospital admission.
Carbon monoxide results from incomplete combustion of fossil fuels. Carbon monoxide is dangerous for human beings since it possess the ability to bind to haemoglobin resulting in reduction of the red blood cells to carry oxygen to cells [ 41 ].
Only 10 out of the 112 reviewed studies investigated the association of carbon monoxide (CO) with mortality and hospital admission. The majority of these studies showed that carbon monoxide exposure can cause a number of cardiovascular and respiratory health problems ( Fig 3F and S3 Table ). Exposure to carbon monoxide pollution resulted in increased odds for pulmonary embolism hospital admission [ 43 ]. Additionally, Renzi et al. (2017) showed that all-cause mortality increases by 0.12% for every 1 mg/m3 increase in CO [ 39 ]. On the contrary, carbon monoxide acted as a protective factor against chest disease hospital admission among patients with sickle cell anaemia in one of the reviewed studies [ 44 ]. This association was explained by the fact that carbon monoxide can bind to haemoglobin which enhances the affinity of other binding sites for oxygen in addition to reducing vasoconstriction and inflammation; suggesting a beneficial effect rather than risk factor for patients with sickle cell disease [ 44 ].
The effect of air temperature on mortality and hospital admission
Exposure to hot or cold temperature beyond region-specific thresholds exhibits a range of direct and indirect effects on human health. The direct effects include hyperthermia or heat stress during hot temperature exposures and hypothermia and ischemic stroke during cold temperature exposures [ 45 ]. Besides the direct effects, small fluctuations in temperature across time can result in indirect effects on the respiratory and cardiovascular systems of the body [ 45 ].
Most of the reviewed articles that studied the effect of weather exposure on mortality and hospital admission focused on air temperature exposure with lags ranging from 0 days up to 5 weeks for cold temperatures and from 0 days up to 25 days for hot temperatures. The reviewed studies examined the effect of cold temperature, hot temperature, and air temperature increase on a range of diseases, most commonly, cardiovascular, respiratory, and psychiatric disorders. Table 2 below shows the definitions of “cold temperature”, “hot temperature”, and “air temperature increase” classifications derived from the reviewed studies.
https://doi.org/10.1371/journal.pone.0241415.t002
Cold temperature acted as a risk factor for several types of mortality and hospital admission outcomes ( Fig 4A and S3 Table ). Nevertheless, cold temperature was a protective factor only in one of the reviwed studies for all-cause mortality at lag 0 (RR = 0.99, 95%CI = 0.985 to 0.995); yet cold temperature acted as a risk factor for all-cause mortality in the same study at lag of 14 days with a relative risk of 1.003 emphasizing the delayed effect of cold temperature on mortality [ 46 ].
https://doi.org/10.1371/journal.pone.0241415.g004
Similar to cold temperature, hot temperature also acted as a risk factor in most of the reviewed studies for a number of mortality and hospital admission outcomes ( Fig 4B and S3 Table ). On the other hand, hot temperatures were associated with reductions in hospital admission rates for ischemic heart disease (RR = 0.74, 95%CI = 0.55 to 0.99) in a study conducted by Bijelovic et al. (2017) and for all-cause hospital admissions (RR = 0.961, 95% CI = 0.956 to 0.967) and cardiovascular hospital admissions (RR = 0.975, 95% CI = 0.957 to 0.993) in a study conducted by Monteiro et al. (2013) [ 47 , 48 ].
Some studies examined the effect of increasing temperature across the whole year on mortality and hospital admission. More than half of these studies showed a significant positive association between the increasing temperature and the mortality and hospital admission outcomes ( Fig 4C and S3 Table ).
The effect of other weather exposures on mortality and hospital admission
Similar to the temperature, weather exposures that include humidity, rainfall, sunshine, snowcover, air pressure, daylight, wind speed and wind direction with lags ranging from 0 up to 7 days were found to affect a range of diseases, most commonly, cardiovascular, respiratory, and psychiatric disorders ( S3 Table ).
Weather variables that showed significant positive assciations with hospital admission included: a rainfall effect on psychiatric hospital admission [ 49 ], sunshine and daylight effects on hospital trauma [ 50 ] and psychaitric admissions [ 51 ], wind speed effects on chest disease hospital admission [ 44 ], and air pressure effects on mania and depression hospital admission [ 49 ].
It is worth mentioning that sunshine showed inconsistency in its effect on psychaitric hospital admission, acting as a risk factor in a Danish study [ 52 ] while acting as a protective factor in a study conducted in Ireland [ 49 ].
The adjustments and effect modifications for the association of air-pollution and weather exposure with mortality and hospital admission
Most of the reviewed studies stratified and adjusted their analysis by age and gender [ 25 , 40 , 51 , 53 – 61 ]. Socio-economic deprivation, education attainment, income level, marital status, and occupational class were considered as confounders or effect modifiers in some of the reviewed studies [ 25 , 58 , 62 – 66 ]. However, only one study considered ethnicity to act as an effect modifier in the association between all-cause mortality and “summer smog” days defined as having maximum temperature of 25°C and PM10 pollutant oncentration of 50 μg/m3 [ 62 ]. And only two studies investigating the effect of air-pollution on all-cause and cardiovascular mortality in England adjusted for ethnicity in their multivariate regresison models [ 67 , 68 ].
Some of the studies that examined the effect of air-pollution on mortality and hospital admission accounted for air temperature effect in their analysis [ 35 , 40 , 46 ]. Likewise, some of the reviewed articles that studied the association of weather exposure to mortality and hospital admission considered the effect of air-pollution in their analysis [ 34 , 65 , 69 – 72 ].
Other variables considered to affect the relationship of air-pollution and/or weather exposure with mortality and/or hospital admission included: weekend and holiday effect, population decrease during the summer, influenza epidemics, season, day of the week, and tobacco smoke [ 25 , 40 , 46 , 54 , 56 , 73 – 79 ].
In this scoping review of 112 articles, we aimed to examine the effect of (1) air pollution, (2) temperature, and (3) other weather exposures on mortality and hospital admission outcomes.
The first part of the review showed that air-pollution acted consistently as a risk factor for all-cause, cardiovascular, respiratory, cerebrovascular and cancer mortality and hospital admission in the EU and UK which is in line with the findings of studies conducted in other regions of the world [ 80 – 84 ]. For instance, elevated risks of cardiovascular and respiratory diseases mortality were reported in Istanbul-Turkey for every 10 μg/m3 increase in PM10, SO2 and NO2 pollutants [ 85 ]. An exception was ozone (O3) air-pollution which showed inconsistent association with mortality and hospital admission. Two explanations were offered in the literature for the negative association between health outcomes and ozone pollution. The first explanation is related to the fact that ozone is a highly seasonal pollutant since its formation is catalysed by sunlight rendering higher ozone concentrations in the summer as compared to winter season. Thus, ozone effect on health outcomes should be analysed by accounting for the season effect [ 21 ]. In the continental United States, a 49% higher risk in all-cause mortality was shown for every 10 ppb increase in ozone during the warm-season [ 86 ]. The second explanation is related to the high reactivity of ozone leading to the formation of other pollutants such as NO2 and particulate matter. Therefore, ozone is negatively correlated with other air pollutants and its effect on health outcomes should be analysed as a combined effect of O3 and NO2 (known as Ox effect) [ 25 ].
Additionally, our scoping review showed that the effect of particulate matter (PM10 and PM2.5) pollution on mortality and hospital admission is more studied in the literature as compared to the other air pollutants. This could be related to the more pronounced effects of particulate matter exposure on health which is corroborated by many studies across the world [ 81 , 87 ]. Despite the fact that PM10 particles are deposited in the nasal cavities and upper airways, PM2.5 may penetrate deep into the lung tissues (reaching the alveoli and bloodstream) and irritate the respiratory airways causing various respiratory and cardiovascular problems [ 29 , 30 , 88 ].
Similar to air pollution, the second part of this review showed that hot and cold temperature exposures beyond region-specific thresholds are risk factors for a wide range of respiratory, cardiovascular (including: ischemic heart disease, myocardial infarction, pulmonary embolism, stroke, heart failure, and COPD), and psychiatric (including: mania and depression) illness in the EU and UK. These findings are corroborated by a wide body of literature from across the world [ 89 – 97 ]. In India, cold temperatures below 13.8°C were associated with increased risk of 6.3% for all-cause mortality, 27.2% for stroke mortality, 9.7% for ischemic heart disease mortality, and 6.5% for respiratory diseases mortality [ 92 ]. In Istanbul-Turkey, 23 days of exposure to hot temperature above 22.8°C was associated with a total of 419 excess deaths [ 90 ]. In Korea, hot temperature days of 25°C compared to 15°C were significantly associated with a 4.5% increase in cardiovascular hospitalizations [ 98 ].
It is worth to point out that the effect of cold temperature on health is more delayed (up to 5 weeks) in comparison to the more immediate effects of hot temperature (up to 25 days). Similar study in Northeast-Asia showed a delayed risk of cold temperature on mortality after 5 to 11 days, yet a more immediate effect of hot temperature on mortality after 1 to 3 days in each of Taiwan, Korea, and Japan countries [ 91 ].
Although exposure to hot or cold temperature can affect the health negatively, our scoping review showed that in few studies, the increase in temperature reduced the risk of hospital admissions for some types of cardiovascular diseases; mainly for pulmonary embolism, angina pectoris, chest, and ischemic heart diseases. This could be explained by the fact that hot temperature can cause immediate increase in cardiovascular mortality rates; whereby many cases might pass directly to the death state without passing through the hospital admission state resulting in lower hospital admission rates [ 47 ].
The third part of this scoping review presented the studies that examined the effects of other weather exposures such as relative humidity, barometric pressure, rainfall, and wind speed on mortality and hospital admission outcomes. These weather exposures were found to affect significantly only hospital admission. No significant effect was noted with respect to the mortality outcome. The weather exposures acted as a risk factor for psychiatric disorders (including depression and Mania), chest disease, and trauma hospital admissions. This was corroborated by evidence from countries outside the EU as well [ 99 – 101 ]. Yet in some of the reviewed studies, weather exposures acted as a protective factor for some types of psychiatric and cardiovascular disorders. The significant negative association between ischemic heart disease hospital admission and humidity in one of the reviewed studies was explained by the fact that people in general and the elderly specifically reduce their activities during high humidity and temperature periods. This is mainly due to the lack of the body’s ability to perspire, which in turn reduces their risk of cardiovascular complications [ 48 ]. As for the protective effect of some weather exposures on psychiatric hospital admissions, similar findings were presented in Iran; with a negative association between barometric pressure and schizophrenia hospital admissions and rainy days and bipolar hospital admissions [ 101 ].
In addition to the association of air pollution and weather exposure with mortality and hospital admission outcomes, our review aimed to present the individual, socio-economic, and environmental factors that play an important role in modifying the latter association. The effect modifiers identified in this scoping review included: pre-existing health conditions, age, gender, educational attainment, wealth or income or socio-economic deprivation, occupation, marital status, tobacco smoking, season, day of the week, holidays, and influenza epidemics.
Individuals with pre-existing chronic health conditions face increased susceptibility toward air-pollution and weather exposure related mortality and hospital admission [ 52 , 54 , 78 , 102 ].
Older people are more vulnerable to the health effects associated with air-pollution, hot or cold temperatures, and other weather variables [ 54 , 56 , 103 – 105 ]. This is due to the physiological degeneration of the human body with increasing age. Aging affects the normal function of the body organs resulting in many chronic cardiovascular, urinary, and respiratory health conditions. This reduces the ability of older people to adapt to increased concentrations of air pollutants and changing weather conditions [ 103 , 105 , 106 ]. Moreover, old age people have lower immunity and antioxidant defence as compared to young people placing them at a higher risk [ 107 ]. Many older people also have reduced mobility and mental abilities which delay their access to healthcare leading to severe health complications and death [ 108 ].
As for gender, our review revealed inconsistency regarding its modification effect on the association between air-pollution and weather exposure and mortality and hospital admission health outcomes. Nevertheless, most of the reviewed studies have found that females have higher risks of mortality and/or hospital admission after exposure to air-pollution and/or weather fluctuations beyond region-specific thresholds including hot and cold temperatures [ 9 , 47 , 57 , 58 , 65 , 78 , 109 – 112 ]. Whereas some studies found higher risks of mortality and/or hospital admissions among males in relation to air-pollution and/or weather exposure [ 25 , 40 , 42 , 59 , 70 , 113 , 114 ]. One explanation for this might be due to the physiological differences between males and females. Females have smaller lung size, yet higher airways reactivity making them more susceptible to air-pollution health effects as compared to males [ 42 , 115 ]. Likewise, higher pulse rates and smaller heart size relative to the human body in females as compared to males render females more vulnerable to the health effects of air-pollution and hot or cold temperature exposures [ 115 ]. Moreover, females exhibit more fluctuations in hormone levels due to pregnancy, menstrual cycle and menopause periods which may place them at a higher health risk upon exposure to air-pollution and weather variations [ 115 ]. The different lifestyle, socio-economic position, and occupation type between males and females may also lead to different levels and duration of air-pollution and weather exposure [ 62 , 109 , 116 – 118 ]. However, it is worth mentioning that the effect modification of gender in the association of air-pollution and weather exposure with mortality and hospital admission outcomes is believed to be confounded by age since in many of the reviewed studies, higher risks were found among old aged females (age>65 years old) [ 47 , 57 , 61 , 78 , 112 ] and old aged males (age >70 years old) [ 114 ]. This confounding effect could be reduced either by assessing the combined effect modification of age and gender through an interaction term or by stratifying the analysis according to both the age groups and gender.
Wealth and socio-economic deprivation were also considered by some of the reviewed studies as an effect modifier in the relationship of air-pollution and weather with mortality and hospital admission. In general, the absence of wealth and presence of socio-economic deprivation increase the risk of exposure to air-pollution and weather variations resulting in elevated mortality and hospital admission rates in Europe [ 62 , 66 , 76 ] and in other parts of the world including New Zealand [ 22 ], United States of America [ 119 ], and Chile [ 120 ].
Educational attainment was also considered by some of the reviewed studies as an effect modifier, with higher risks detected among individuals with lower educational attainment [ 25 , 63 , 64 , 121 , 122 ]. Despite the consideration of age, gender, education, and wealth effect in the association of air-pollution and weather with mortality and hospital admissions in Europe, our scoping review revealed the lack of investigation into the role of other important socio-demographics such as ethnicity. Research has extensively shown that ethnic minorities live in more disadvantaged communities and have lower socio-economic status as well as poor housing conditions. This results in higher risk for chronic health problems associated with higher exposure on one hand and with lower access to quality healthcare on the other hand [ 22 – 24 ].
Finally, it is worth to note that most of the reviewed studies with a time-series or case-crossover design adjusted their analysis for the season effect [ 40 , 46 , 52 , 54 , 60 , 71 , 73 , 74 , 123 , 124 ]. It is well established that air-pollution, temperature, and other weather variables vary with seasons [ 125 – 127 ]. Not to mention that the emission, formation, and dispersion of air pollutants is affected by seasonal weather variations which in turn affects the individual exposure levels [ 128 ]. Outdoor activities and daily habits (eg. Window ventilation of houses) might also vary depending on the season which reflect changes in the level and duration of individual exposure to air-pollution and weather changes [ 129 ].
Despite the value of this scoping literature review, it has some limitations. First, the employed search strategy was limited to original articles published in peer reviewed journals which might have led to the omission of unpublished work or articles that were published in non-indexed journals. Nevertheless, our search strategy involved navigation through two databases which enables a good catch of major published studies addressing the effect of air-pollution and weather exposure on mortality and hospital admission. Second, limiting our inclusion criteria only to English language articles might have resulted in missing some research written in other languages. However, as most of the literature worldwide is published in the English language, we believe that no major papers have been excluded. Third, this review was limited only to quantitative research which would have led to missing out other type of important research including opinion research pieces and letters to editor as well as qualitative research studies. Opinion research pieces and letters to editor provide a critical appraisal/discussion for the findings of original studies which warrant future research development. Qualitative studies provide an overview about the effect of air-pollution or weather variations on human health from the perspective of lay people rather than relying only on objective census/statistics numbers as in quantitative research. Forth, due to resources limitations, title and abstract screening as well as data abstraction were done only by one researcher (MA). Nevertheless, a second researcher performed title and abstract screening for a random sample of 20% of the retrieved records. Given the high consensus between the two researchers, we are confident of the exact application of the inclusion and exclusion criteria. Our goal from this literature review was not to produce a numerical estimate but rather to give a narrative summary on the effect of air-pollution/weather on mortality/hospital admission. Hence, missing some studies would not be a major concern for this scoping review.
Literature gaps and implications for future research
This scoping review helped us to identify literature gaps that require further research.
First, this review revealed the extensive research carried out to determine the effect of air-pollution on human health. Yet, due to the high correlation between air pollutants and the issue of collinearity in multivariate models, most of the studies examined the effect of single pollutants on mortality and hospital admission outcomes. Nevertheless, the issue of correlation between air pollutants is highly contextual and it depends on the study settings including the season and the specific geographical area. Hence, future researchers should try to examine the effect of multi-pollutants on mortality and/or hospital admission in one model, where strong correlations between the air pollutants are absent.
Second, the majority of studies examined the direct effects of air-pollution and weather exposure on mortality and hospital admission without considering the role of certain effect modifiers. The examined effect modifiers considered mostly by the literature involve age, gender, education, socio-economic deprivation, and season. Therefore, there is a lack of evidence regarding the modifying effect of other individual factors such as previous disease conditions and ethnicity which affect the person’s health vulnerability. Indeed, future research is needed to find out the reasons behind elevated individual’s susceptibility to the detrimental effects of air-pollution and weather variations in certain groups of population.
Third, our review showed that most of the studies either investigated the effect of air-pollution or the effect of weather on mortality and hospital admission. The formation and dispersion of air pollutants depends highly on the existing atmospheric conditions such as temperature, humidity, and wind speed [ 130 ]. Therefore, future studies should consider examining the effect of both, weather conditions and air-pollution, on human health through interaction terms or adjustments in the analysis models.
Fourth, although extensive research has been performed to study the effect of particulate matter and nitrogen oxides pollution on human health, there was a lack of research with respect to other air pollutants including carbon monoxide, ozone, and sulphur dioxide. This might be due to the absence of rigorous and reliable measurements of these pollutants or due to the complexity of analysing the effect of these pollutants.
Fifth, literature is more focused on examining the effect of temperature on mortality and hospital admission, placing less emphasis on other weather exposures. Hence, future research should shift the focus toward other weather exposures such as wind speed, rainfall, humidity, snow cover, daylight, and air pressure.
Sixth, there was a lack of research examining the effect of air-pollution and weather on hospital admission. Mortality was the major outcome in most of the reviewed studies due to the ease of data access governed by less ethical considerations. Additionally, analysis is more straightforward given that it occurs only once in an individual’s life. Thus, it is recommended for future research to consider the impact of air-pollution and weather variables on hospital admission on its own and in combination with mortality through multistate modelling.
Finally, the majority of studies in this field employ the time-series design which uses aggregated mortality and hospital admission data linked to environmental exposures at the local authorities or municipalities level. Research that uses aggregated data neglect the physiological and socio-economic differences among individuals. Additionally, assigning air-pollution and weather exposure based on wide geographies overlook the small geographical exposure differences biasing the drawn estimates. Therefore, there is a need for cohort research studies that utilize individual level data linked to air-pollution and weather exposure at small geographical spatial resolution (eg. Postcodes).
In summary, our scoping review showed that air-pollution and weather exposure beyond certain thresholds lead to various impacts on human health, most commonly cardiovascular and respiratory problems, resulting in increased rates of mortality and hospital admission. Yet, further research is needed given that the effect modification of important socio-demographics such as ethnicity and the interaction between air-pollution and weather is often missed in the literature. Understanding this should give enough evidence to the policy makers to plan and act accordingly aiming to reduce the effects of air pollution and weather variations on the public health. Additionally, research should focus on projecting future health behaviour and mortality patterns in relation to air pollution and weather variations, in order to guide effective environmental and health precautionary measures planning.
Supporting information
S1 checklist. prisma checklist followed for this systematic scoping review data searching, screening, and abstraction..
https://doi.org/10.1371/journal.pone.0241415.s001
S1 Table. The search codes used in PubMed and Web of Science databases for this scoping literature review.
https://doi.org/10.1371/journal.pone.0241415.s002
S2 Table. A detailed summary of the characteristics of the 112 studies included in this scoping review by the type of investigated health outcome.
https://doi.org/10.1371/journal.pone.0241415.s003
S3 Table. A detailed summary of the reported associations between air pollution and/or weather exposures and mortality and/or hospital admission outcomes in the 112 reviewed studies in terms of coefficients and 95% confidence intervals.
https://doi.org/10.1371/journal.pone.0241415.s004
Acknowledgments
The authors would like to thank the University of St Andrews Library services for helping in developing the search codes used in this scoping literature review.
- View Article
- PubMed/NCBI
- Google Scholar
- 3. World-Bank. Cities and Climate Change: An Urgent Agenda. Washington DC: The World Bank; 2010.
- 5. WHO. Ambient (outdoor) air pollution: World health organization (WHO); 2018 [Available from: https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health
- 27. European-Commission. EU action against climate change: Leading global action to 2020 and beyond Luxembourg: Office for Official Publications of the European Communities; 2009. Contract No.: KH-78-09-725-EN-C.
- 41. Samet J, Jaakkola J. The epidemiologic approach In Air pollution and health (Holgate ST, Samet JM, Koren HS and Maynard RL, Eds.). Academic Press, London; 1999.
Advertisement
Ambient air pollution and its influence on human health and welfare: an overview
- Review Article
- Published: 03 May 2020
- Volume 27 , pages 24815–24830, ( 2020 )
Cite this article

- Alsaid Ahmed Almetwally 1 ,
- May Bin-Jumah 2 &
- Ahmed A. Allam 3
8690 Accesses
167 Citations
43 Altmetric
Explore all metrics
Human health is closely related to his environment. The influence of exposure to air pollutants on human health and well-being has been an interesting subject and gained much volume of research over the last 50 years. In general, polluted air is considered one of the major factors leading to many diseases such as cardiovascular and respiratory disease and lung cancer for the people. Besides, air pollution adversely affects the animals and deteriorates the plant environment. The overarching objective of this review is to explore the previous researches regarding the causes and sources of air pollution, how to control it and its detrimental effects on human health. The definition of air pollution and its sources were introduced extensively. Major air pollutants and their noxious effects were detailed. Detrimental impacts of air pollution on human health and well-being were also presented.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
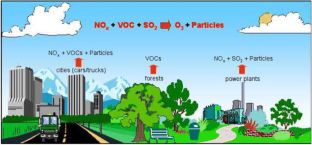
Similar content being viewed by others
Air Pollution Exposure Studies Related to Human Health

Air Pollution and Health Effects

Health impacts of air pollution in China
Explore related subjects.
- Environmental Chemistry
Abou Rafee S et al (2017) Contributions of mobile, stationary and biogenic sources to air pollution in the Amazon rainforest: a numerical study with the WRF-Chem model. Atmos Chem Phys 17:7977–7995. https://doi.org/10.5194/acp-17-7977-2017
Article CAS Google Scholar
Altshuller AP (1956) Thermodynamic considerations in the interactions of nitrogen oxides and oxy-acids in the atmosphere. Journal of the Air Pollution Control Association 6:97–100. https://doi.org/10.1080/00966665.1956.10467740
Alves C, Ferraz C (2005) Effects of air pollution on emergency admissions for chronic obstructive pulmonary diseases in Oporto, Portugal. Int J Environ Pollut 23:42–64. https://doi.org/10.1504/IJEP.2005.006395
Appannagari RR (2017) Environmental pollution causes and consequences: a study 3
Arbex MA, de Souza Conceicao GM, Cendon SP, Arbex FF, Lopes AC, Moyses EP, Santiago SL, Saldiva PHN, Pereira LAA, Braga ALF (2009) Urban air pollution and chronic obstructive pulmonary disease-related emergency department visits. J Epidemiol Community Health 63:777–783. https://doi.org/10.1136/jech.2008.078360
Armenta, MdlgaS (2016) The quality of air vol 73. Comprehensive analytical chemistry. Elsevier
Arroyave C, Morcillo M (1995) The effect of nitrogen oxides in atmospheric corrosion of metals. Corros Sci 37:293–305. https://doi.org/10.1016/0010-938X(94)00136-T
Association AL (2013) American Lung Association State of the Air 2013 - Health Effects of Ozone and Particle Pollution American Lung Association
Azari AA, Barney NP (2013) Conjunctivitis: a systematic review of diagnosis and treatment. Jama 310:1721–1729. https://doi.org/10.1001/jama.2013.280318
Article Google Scholar
Babayemi J, Ogundiran M, Osibanjo O (2016) Overview of environmental hazards and health effects of pollution in developing countries: a case study of Nigeria. Environmental Hazards and Health Effects of Pollution Environmental Quality Management 26:51–71. https://doi.org/10.1002/tqem.21480
Balmes JR (2019) Household air pollution from domestic combustion of solid fuels and health. J Allergy Clin Immunol 143:1979–1987. https://doi.org/10.1016/j.jaci.2019.04.016
Bao X, Tian X, Yang C, Li Y, Hu Y (2019) Association between ambient air pollution and hospital admission for epilepsy in Eastern China. Epilepsy Res 152:52–58. https://doi.org/10.1016/j.eplepsyres.2019.02.012
Berg AT, Altalib HH, Devinsky O (2017) Psychiatric and behavioral comorbidities in epilepsy: a critical reappraisal. Epilepsia 58:1123–1130. https://doi.org/10.1111/epi.13766
Berglind N (2017) Cardiovascular and respiratory effects of air pollution- application of different observational study designs and analysis approaches. Larolinska Institutet
Bermejo-Orduna R, McBride JR, Shiraishi K, Elustondo D, Lasheras E, Santamaria JM (2014) Biomonitoring of traffic-related nitrogen pollution using Letharia vulpina (L.) hue in the Sierra Nevada, California. Sci Total Environ 490:205–212. https://doi.org/10.1016/j.scitotenv.2014.04.119
Bernstein JA, Alexis N, Barnes C, Bernstein IL, Nel A, Peden D, Diaz-Sanchez D, Tarlo SM, Williams PB, Bernstein JA (2004) Health effects of air pollution. J Allergy Clin Immunol 114:1116–1123. https://doi.org/10.1016/j.jaci.2004.08.030
Bian Y, Huang Z, Ou J, Zhong Z, Xu Y, Zhang Z, Xiao X, Ye X, Wu Y, Yin X, Li C, Chen L, Shao M, Zheng J (2019) Evolution of anthropogenic air pollutant emissions in Guangdong Province, China, from 2006 to 2015. Atmos Chem Phys 19:11701–11719. https://doi.org/10.5194/acp-19-11701-2019
Bloom B, Jones LI, Freeman G (2013) Summary health statistics for U.S. children: National Health Interview Survey, 2012 Vital Health Stat 10:1-81
Brook RD (2008) Cardiovascular effects of air pollution. Clin Sci (Lond) 115:175–187. https://doi.org/10.1042/cs20070444
Brook RD, Jerrett M, Brook JR, Bard RL, Finkelstein MM (2008) The relationship between diabetes mellitus and traffic-related air pollution. J Occup Environ Med 50:32–38. https://doi.org/10.1097/JOM.0b013e31815dba70
Brown TP, Rushton L, Mugglestone MA, Meechan DF (2003) Health effects of a sulphur dioxide air pollution episode. J Public Health 25:369–371. https://doi.org/10.1093/pubmed/fdg083
Cai J, Zhao A, Zhao J, Chen R, Wang W, Ha S, Xu X, Kan H (2014) Acute effects of air pollution on asthma hospitalization in Shanghai, China. Environ Pollut 191:139–144. https://doi.org/10.1016/j.envpol.2014.04.028
Cakmak S, Dales RE, Vidal CB (2010) Air pollution and hospitalization for epilepsy in Chile. Environ Int 36:501–505. https://doi.org/10.1016/j.envint.2010.03.008
Carmichael GR et al (2009) Asian aerosols: current and year 2030 distributions and implications to human health and regional climate change. Environ Sci Technol 43:5811–5817. https://doi.org/10.1021/es8036803
Chang T, Zivin J, Gross T, Neidell M (2019) The effect of pollution on worker productivity: evidence from call center workers in China. Am Econ J Appl Econ 11:151–172. https://doi.org/10.1257/app.20160436
Chen X (2018) A spatial and temporal analysis of the socioeconomic factors associated with breast cancer in Illinois using geographically weighted generalized linear regression. Journal of Geovisualization and Spatial Analysis:2. https://doi.org/10.1007/s41651-017-0011-5
Choe SA, Kauderer S, Eliot MN, Glazer KB, Kingsley SL, Carlson L, Awad YA, Schwartz JD, Savitz DA, Wellenius GA (2018) Air pollution, land use, and complications of pregnancy. Sci Total Environ 645:1057–1064. https://doi.org/10.1016/j.scitotenv.2018.07.237
Chuang KJ, Yan YH, Chiu SY, Cheng TJ (2011) Long-term air pollution exposure and risk factors for cardiovascular diseases among the elderly in Taiwan Occup Environ Med 68:64–68. doi: https://doi.org/10.1136/oem.2009.052704
Combes A, Franchineau G (2019) Fine particle environmental pollution and cardiovascular diseases. Metabolism 100:153944. https://doi.org/10.1016/j.metabol.2019.07.008
Coppola A et al (2016) Psychiatric comorbidities in patients from seven families with autosomal dominant cortical tremor, myoclonus, and epilepsy. Epilepsy Behav 56:38–43. https://doi.org/10.1016/j.yebeh.2015.12.038
Cui L, Conway GA, Jin L, Zhou J, Zhang J, Li X, Zhou L, Li T, Zhang J (2017) Increase in medical emergency calls and calls for central nervous system symptoms during a severe air pollution event, January 2013, Jinan City. China Epidemiology 28(Suppl 1):S67–s73. https://doi.org/10.1097/ede.0000000000000739
D'Amato G et al (2015) Meteorological conditions, climate change, new emerging factors, and asthma and related allergic disorders. A statement of the World Allergy Organization World Allergy Organ J 8:25. https://doi.org/10.1186/s40413-015-0073-0
Dai W, Gao J, Cao G, Ouyang F (2013) Chemical composition and source identification of PM2.5 in the suburb of Shenzhen. China Atmospheric Research 122:391–400. https://doi.org/10.1016/j.atmosres.2012.12.004
Dauchet L, Hulo S, Cherot-Kornobis N, Matran R, Amouyel P, Edme JL, Giovannelli J (2018) Short-term exposure to air pollution: associations with lung function and inflammatory markers in non-smoking, healthy adults. Environ Int 121:610–619. https://doi.org/10.1016/j.envint.2018.09.036
de Prado BP, Mercader EMH, Pujol J, Sunyer J, Mortamais M (2018) The effects of air pollution on the brain: a review of studies interfacing environmental epidemiology and neuroimaging. Curr Environ Health Rep 5:351–364. https://doi.org/10.1007/s40572-018-0209-9
Demetriou CA et al (2012) Biomarkers of ambient air pollution and lung cancer: a systematic review. Occup Environ Med 69:619–627. https://doi.org/10.1136/oemed-2011-100566
Demetriou CA, Vineis P (2015) Carcinogenicity of ambient air pollution: use of biomarkers, lessons learnt and future directions. J Thorac Dis 7:67–95. https://doi.org/10.3978/j.issn.2072-1439.2014.12.31
Ebenstein A, Lavy V, Roth S (2016) The long-run economic consequences of high-stakes examinations: evidence from transitory variation in pollution American Economic Journal: Applied Economics 8. doi: https://doi.org/10.1257/app.20150213 , 65
EEA (2008) EU-27 emission of carbon monoxide, 2006
Europe WHOROf (2013) Health effects of particulate matter. Policy implications for countries in Eastern Europe, Caucasus and Central Asia Copenhagen. W.H. Organization
Ezeh GC (2012) Characterization of PM10 and PM2.5 particulates sizes collected in Ikoyi Lagos, Nigeria Toxicological and environmental chemistry v. 94:pp. 884–894-2012 v.2094 no.2015. doi: https://doi.org/10.1080/02772248.2012.674133
Falcon-Rodriguez CI, Osornio-Vargas AR, Sada-Ovalle I, Segura-Medina P (2016) Aeroparticles, composition, and lung diseases. Front Immunol 7:3. https://doi.org/10.3389/fimmu.2016.00003
Faustini A, Rapp R, Forastiere F (2014) Nitrogen dioxide and mortality: review and meta-analysis of long-term studies. Eur Respir J 44:744–753. https://doi.org/10.1183/09031936.00114713
Fisher RS, van Emde BW, Blume W, Elger C, Genton P, Lee P, Engel J Jr (2005) Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia 46:470–472. https://doi.org/10.1111/j.0013-9580.2005.66104.x
Fluegge K, Fluegge K (2017) Air pollution and risk of hospitalization for epilepsy: the role of farm use of nitrogen fertilizers and emissions of the agricultural air pollutant, nitrous oxide. Arq Neuropsiquiatr 75:614–619. https://doi.org/10.1590/0004-282x20170107
Fujita EM, Campbell DE, Arnott WP, Johnson T, Ollison W (2014) Concentrations of mobile source air pollutants in urban microenvironments. J Air Waste Manage Assoc 64:743–758. https://doi.org/10.1080/10962247.2013.872708
Fuzzi S et al (2015) Particulate matter, air quality and climate: lessons learned and future needs. Atmos Chem Phys 15:8217–8299. https://doi.org/10.5194/acp-15-8217-2015
Garba Ibrahim, Dakasku ISi, Hassan Galadima Kurkushe (2018) Review on the Influence of Primary Air Pollutants upon Human Health. International Research Journal of Engineering and Technology (IRJET) 5
Gauderman WJ et al (2015) Association of improved air quality with lung development in children. N Engl J Med 372:905–913. https://doi.org/10.1056/NEJMoa1414123
Ghorani-Azam A, Riahi-Zanjani B, Balali-Mood M (2016) Effects of air pollution on human health and practical measures for prevention in Iran Journal of research in medical sciences. The Official Journal of Isfahan University of Medical Sciences 21:65. https://doi.org/10.4103/1735-1995.189646
Gourdji S (2018) Review of plants to mitigate particulate matter, ozone as well as nitrogen dioxide air pollutants and applicable recommendations for green roofs in Montreal. Quebec Environmental Pollution 241:378–387. https://doi.org/10.1016/j.envpol.2018.05.053
Greenberg N, Carel RS, Derazne E, Bibi H, Shpriz M, Tzur D, Portnov BA (2016) Different effects of long-term exposures to SO2 and NO2 air pollutants on asthma severity in young adults. J Toxicol Environ Health A 79:342–351. https://doi.org/10.1080/15287394.2016.1153548
Guo H, Chen M (2018) Short-term effect of air pollution on asthma patient visits in Shanghai area and assessment of economic costs. Ecotoxicol Environ Saf 161:184–189. https://doi.org/10.1016/j.ecoenv.2018.05.089
Hamra GB, Laden F, Cohen AJ, Raaschou-Nielsen O, Brauer M, Loomis D (2015) Lung cancer and exposure to nitrogen dioxide and traffic: a systematic review and meta-analysis. Environ Health Perspect 123:1107–1112. https://doi.org/10.1289/ehp.1408882
Hanna R, Oliva P (2015) The effect of pollution on labor supply: Evidence from a natural experiment in Mexico City. J Public Econ 122:68–79. https://doi.org/10.1016/j.jpubeco.2014.10.004
Hao J, Yang Z, Huang S, Yang W, Zhu Z, Tian L, Lu Y, Xiang H, Liu S (2019) The association between short-term exposure to ambient air pollution and the incidence of mumps in Wuhan, China: A time-series study. Environ Res 177:108660. https://doi.org/10.1016/j.envres.2019.108660
Hehua Z, Qing C, Shanyan G, Qijun W, Yuhong Z (2017) The impact of prenatal exposure to air pollution on childhood wheezing and asthma: A systematic review. Environ Res 159:519–530. https://doi.org/10.1016/j.envres.2017.08.038
Hendryx M, Luo J, Chojenta C, Byles JE (2019) Air pollution exposures from multiple point sources and risk of incident chronic obstructive pulmonary disease (COPD) and asthma. Environ Res 179:108783. https://doi.org/10.1016/j.envres.2019.108783
Heyes A, Zhu M (2019) Air pollution as a cause of sleeplessness: social media evidence from a panel of Chinese cities. J Environ Econ Manag 98:102247. https://doi.org/10.1016/j.jeem.2019.07.002
Ho YC, Su BH, Su HJ, Chang HL, Lin CY, Chen H, Chen KT (2015) The association between the incidence of mumps and meteorological parameters in Taiwan. Hum Vaccin Immunother 11:1406–1412. https://doi.org/10.1080/21645515.2015.1029687
Hoek G, Krishnan RM, Beelen R, Peters A, Ostro B, Brunekreef B, Kaufman JD (2013) Long-term air pollution exposure and cardio- respiratory mortality: a review. Environ Health 12:43. https://doi.org/10.1186/1476-069x-12-43
Hu W, Li Y, Han W, Xue L, Zhang W, Ma W, Bi P (2018) Meteorological factors and the incidence of mumps in Fujian Province, China, 2005–2013. Non-linear effects Science of the Total Environment 619:1286–1298. https://doi.org/10.1016/j.scitotenv.2017.11.108
Huang J, Meng X, Zheng Z, Gao Y (2019) Effect of multi-pollutant state of ozone and sulfur dioxide on atmospheric corrosivity map of Guangdong Province. Environ Pollut 251:885–891. https://doi.org/10.1016/j.envpol.2019.05.073
Huebert B, Vitousek P, Sutton J, Elias T, Heath J, Coeppicus S, Howell S, Blomquist B (1999) Volcano fixes nitrogen into plant-available forms. Biogeochemistry 47:111–118. https://doi.org/10.1023/a:1006276011055
Hviid A, Rubin S, Muhlemann K (2008) Mumps. Lancet 371:932–944. https://doi.org/10.1016/s0140-6736(08)60419-5
Janghorbani M, Momeni F, Mansourian M (2014) Systematic review and metaanalysis of air pollution exposure and risk of diabetes. Eur J Epidemiol 29:231–242. https://doi.org/10.1007/s10654-014-9907-2
Janssen NA et al (2011) Black carbon as an additional indicator of the adverse health effects of airborne particles compared with PM10 and PM2.5. Environ Health Perspect 119:1691–1699. https://doi.org/10.1289/ehp.1003369
Jeong CH et al (2011) Receptor model based identification of PM2.5 sources in Canadian cities. Atmospheric Pollution Research 2:158–171. https://doi.org/10.5094/APR.2011.021
Jorcano A et al (2019) Prenatal and postnatal exposure to air pollution and emotional and aggressive symptoms in children from 8 European birth cohorts. Environ Int 131:104927. https://doi.org/10.1016/j.envint.2019.104927
Karimi B, Shokrinezhad B, Samadi S (2019) Mortality and hospitalizations due to cardiovascular and respiratory diseases associated with air pollution in Iran: A systematic review and meta-analysis. Atmos Environ 198:438–447. https://doi.org/10.1016/j.atmosenv.2018.10.063
Kayode S, John aKF (2013) Air Pollution by carbon monoxide (CO) poisonous gas in lagos area southwestern nigeria. Atmospheric and Climate Sciences 3:510–514. https://doi.org/10.4236/acs.2013.34053
Kelly FJ, Fussell JC (2015) Air pollution and public health: emerging hazards and improved understanding of risk. Environ Geochem Health 37:631–649. https://doi.org/10.1007/s10653-015-9720-1
Khallaf MK (2011) The impact of air pollution on health, economy, environment and agricultural sources. In Tech Publishing, Rijeka
Khreis H, Ramani T, de Hoogh K, Mueller N, Rojas-Rueda D, Zietsman J, Nieuwenhuijsen MJ (2019) Traffic-related air pollution and the local burden of childhood asthma in Bradford, UK. International Journal of Transportation Science and Technology 8:116–128. https://doi.org/10.1016/j.ijtst.2018.07.003
Kibble A, Harrison R (2005) Point sources of air pollution. Occupational medicine (Oxford, England) 55:425–431. https://doi.org/10.1093/occmed/kqi138
Kim KH, Jahan SA, Kabir E (2013) A review on human health perspective of air pollution with respect to allergies and asthma. Environ Int 59:41–52. https://doi.org/10.1016/j.envint.2013.05.007
Knibbs LD et al (2018) The Australian Child Health and Air Pollution Study (ACHAPS): a national population-based cross-sectional study of long-term exposure to outdoor air pollution, asthma, and lung function. Environ Int 120:394–403. https://doi.org/10.1016/j.envint.2018.08.025
Ko F, Hui D (2011) Air pollution and chronic obstructive pulmonary disease. Respirology (Carlton, Vic) 17:395–401. https://doi.org/10.1111/j.1440-1843.2011.02112.x
Ko FW et al (2007) Effects of air pollution on asthma hospitalization rates in different age groups in Hong Kong. Clin Exp Allergy 37:1312–1319. https://doi.org/10.1111/j.1365-2222.2007.02791.x
Komarnisky LA, Christopherson RJ, Basu TK (2003) Sulfur: its clinical and toxicologic aspects. Nutrition 19:54–61. https://doi.org/10.1016/s0899-9007(02)00833-x
Kulhánová I et al (2018) The fraction of lung cancer incidence attributable to fine particulate air pollution in France: impact of spatial resolution of air pollution models. Environ Int 121:1079–1086. https://doi.org/10.1016/j.envint.2018.09.055
Lang JD, Taylor DC, Kasper BS (2018) Stress, seizures, and epilepsy: patient narratives. Epilepsy Behav 80:163–172. https://doi.org/10.1016/j.yebeh.2018.01.005
Leibowitz HM (2000) The red eye. N Engl J Med 343:345–351. https://doi.org/10.1056/nejm200008033430507
Levy H, Horowitz L, Schwarzkopf M, Ming Y, Golaz JC, Naik V, Ramaswamy V (2013) The roles of aerosol direct and indirect effects in past and future climate. J Geophys Res-Atmos:118, 4532. https://doi.org/10.1002/jgrd.50192
Li D, Wang JB, Yu ZB, Lin HB, Chen K (2019a) Air pollution exposures and blood pressure variation in type-2 diabetes mellitus patients: a retrospective cohort study in China. Ecotoxicol Environ Saf 171:206–210. https://doi.org/10.1016/j.ecoenv.2018.12.069
Li H, Cai J, Chen R, Zhao Z, Ying Z, Wang L, Chen J, Hao K, Kinney PL, Chen H, Kan H (2017a) Particulate matter exposure and stress hormone levels: a randomized. double-blind, crossover trial of air purification circulation 136:618–627. https://doi.org/10.1161/circulationaha.116.026796
Li R et al (2017b) Epidemiological characteristics and spatial-temporal clusters of mumps in Shandong Province, China, 2005–2014. Sci Rep 7:46328. https://doi.org/10.1038/srep46328
Li Z, Xu X, Thompson LA, Gross HE, Shenkman EA, DeWalt DA, Huang IC (2019b) Longitudinal effect of ambient air pollution and pollen exposure on asthma control: The Patient-Reported Outcomes Measurement Information System (PROMIS) Pediatric Asthma Study. Acad Pediatr 19:615–623. https://doi.org/10.1016/j.acap.2019.03.010
Lichter A, Pestel N, Sommer E (2017) Productivity effects of air pollution: evidence from professional soccer. Labour Econ 48:54–66. https://doi.org/10.1016/j.labeco.2017.06.002
Liu C, Yin P, Chen R, Meng X, Wang L, Niu Y, Lin Z, Liu Y, Liu J, Qi J, You J, Kan H, Zhou M (2018) Ambient carbon monoxide and cardiovascular mortality: a nationwide time-series analysis in 272 cities in China. The Lancet Planetary Health 2:e12–e18. https://doi.org/10.1016/S2542-5196(17)30181-X
Lu JG, Lee JJ, Gino F, Galinsky AD (2018) Polluted morality: air pollution predicts criminal activity and unethical behavior. Psychol Sci 29:340–355. https://doi.org/10.1177/0956797617735807
Lu P, Zhang Y, Xia G, Zhang W, Li S, Guo Y (2019) Short-term exposure to air pollution and conjunctivitis outpatient visits: A multi-city study in China. Environ Pollut 254:113030. https://doi.org/10.1016/j.envpol.2019.113030
Ma Y, Yang S, Zhou J, Yu Z, Zhou J (2018) Effect of ambient air pollution on emergency room admissions for respiratory diseases in Beijing, China. Atmos Environ 191:320–327. https://doi.org/10.1016/j.atmosenv.2018.08.027
Macdonald B, Denmead O, White I, Melville M (2004) Natural sulfur dioxide emissions from sulfuric soils. Atmos Environ 38:1473–1480. https://doi.org/10.1016/j.atmosenv.2003.12.005
Mao M, Zhang X, Yin Y (2018) Particulate matter and gaseous pollutions in three metropolises along the Chinese Yangtze River: situation and implications. Int J Environ Res Public Health 15:1102. https://doi.org/10.3390/ijerph15061102
Marais EA et al (2018) Nitrogen oxides in the global upper troposphere: interpreting cloud-sliced NO2 observations from the OMI satellite instrument. Atmos Chem Phys 18:17017–17027. https://doi.org/10.5194/acp-18-17017-2018
Martinez-Rivera C, Garcia-Olive I, Stojanovic Z, Radua J, Ruiz Manzano J, Abad-Capa J (2019) Association between air pollution and asthma exacerbations in Badalona, Barcelona (Spain), 2008-2016 Med Clin (Barc) 152:333–338. doi:10.1016/j.medcli.2018.06.027
Meng Z, Qin G, Zhang B, Geng H, Bai Q, Bai W, Liu C (2003) Oxidative damage of sulfur dioxide inhalation on lungs and hearts of mice. Environ Res 93:285–292. https://doi.org/10.1016/s0013-9351(03)00045-8
Miller KA, Siscovick DS, Sheppard L, Shepherd K, Sullivan JH, Anderson GL, Kaufman JD (2007) Long-term exposure to air pollution and incidence of cardiovascular events in women. N Engl J Med 356:447–458. https://doi.org/10.1056/NEJMoa054409
Mills NL et al (2009) Adverse cardiovascular effects of air pollution. Nat Clin Pract Cardiovasc Med 6:36–44. https://doi.org/10.1038/ncpcardio1399
Morrow GL, Abbott RL (1998) Conjunctivitis. Am Fam Physician 57:735–746
CAS Google Scholar
Mukherjee A (2002) Perspectives of the silent majority: air pollution, livelihood and food security. Ashgate Publishing Limited, Hampshire, England
Murphy SR, Schelegle ES, Miller LA, Hyde DM, Van Winkle LS (2013) Ozone exposure alters serotonin and serotonin receptor expression in the developing lung. Toxicol Sci 134:168–179. https://doi.org/10.1093/toxsci/kft090
Murray CJ, Lopez AD (1997) Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study Lancet 349:1498–1504. doi: https://doi.org/10.1016/s0140-6736(96)07492-2
Nriagu JO (2011) Encyclopedia of environmental health
Nriagu JO (2019) Encyclopedia of environmental health
Moses K. Onabowale and Oyediran K. Owoade (2015) Assessment residential indoor outdoor airborne particulate matter in Ibadan, Southwestern Nigeria Donnish J Physical Sci 1:1–7
Organization WH (2014) 7 million premature deaths annually linked to air pollution. WHO
Orok U (2015) Contamination and health risk assessment of suspended particulate matter (SPM) in Uyo, Niger Delta, Nigeria Journal of Scientific Research and Reports 6:276–286. doi: https://doi.org/10.9734/JSRR/2015/16296
Padula AM, Yang W, Lurmann FW, Balmes J, Hammond SK, Shaw GM (2019) Prenatal exposure to air pollution, maternal diabetes and preterm birth. Environ Res 170:160–167. https://doi.org/10.1016/j.envres.2018.12.031
Pangaribuan M, Chuang K-J, Chuang H-C (2019) Association between exposures to air pollution and biomarkers of cardiovascular disease in Northern Taiwan. Atmospheric Pollution Research 10:1250–1259. https://doi.org/10.1016/j.apr.2019.02.008
Park M, Luo S, Kwon J, Stock TH, Delclos G, Kim H, Yun-Chul H (2013) Effects of air pollution on asthma hospitalization rates in different age groups in metropolitan cities of Korea. Air Qual Atmos Health:6, 551. https://doi.org/10.1007/s11869-013-0195-x
Phosri A, Ueda K, Phung VLH, Tawatsupa B, Honda A, Takano H (2019) Effects of ambient air pollution on daily hospital admissions for respiratory and cardiovascular diseases in Bangkok, Thailand. Sci Total Environ 651:1144–1153. https://doi.org/10.1016/j.scitotenv.2018.09.183
Pope CA, 3rd, Burnett RT, Thurston GD, Thun MJ, Calle EE, Krewski D, Godleski JJ (2004) Cardiovascular mortality and long-term exposure to particulate air pollution: epidemiological evidence of general pathophysiological pathways of disease Circulation 109:71–77. doi: https://doi.org/10.1161/01.Cir.0000108927.80044.7f
Puett RC et al (2019) Inflammation and acute traffic-related air pollution exposures among a cohort of youth with type 1 diabetes. Environ Int 132:105064. https://doi.org/10.1016/j.envint.2019.105064
Radovic NI, Bozic K, Duric AP, Vodopic S, Radulovic L, Vujisic S (2017) Health-related quality of life in adolescents with epilepsy in Montenegro. Epilepsy Behav 76:105–109. https://doi.org/10.1016/j.yebeh.2017.07.009
Rahmat M, Maulina W, Rustami E, Azis M, Budiarti DR, Seminar KB, Yuwono AS, Alatas H (2013) Performance in real condition of photonic crystal sensor based NO2 gas monitoring system. Atmos Environ 79:480–485. https://doi.org/10.1016/j.atmosenv.2013.05.057
Rincon M, Irvin CG (2012) Role of IL-6 in asthma and other inflammatory pulmonary diseases. Int J Biol Sci 8:1281–1290. https://doi.org/10.7150/ijbs.4874
Robertson D (2006) Health effects of increase in concentration of carbon dioxide in the atmosphere Current Science 90
Rosa IdMA (2015) The Impact of Transportation Construction Projects and Activities on Emissions., North Carolina State University
Sager L (2019) Estimating the effect of air pollution on road safety using atmospheric temperature inversions. J Environ Econ Manag 98:102250. https://doi.org/10.1016/j.jeem.2019.102250
Samek L, Stegowski Z, Styszko K, Furman L, Fiedor J (2018) Seasonal contribution of assessed sources to submicron and fine particulate matter in a Central European urban area. Environ Pollut 241:406–411. https://doi.org/10.1016/j.envpol.2018.05.082
Schumann U, Huntrieser H (2007) The global lightning-induced nitrogen oxides source. Atmos Chem Phys 7:3823–3907. https://doi.org/10.5194/acp-7-3823-2007
Seok B, Helmig D, Ganzeveld L, Williams MW, Vogel CS (2013) Dynamics of nitrogen oxides and ozone above and within a mixed hardwood forest in northern Michigan. Atmos Chem Phys 13:7301–7320. https://doi.org/10.5194/acp-13-7301-2013
Shahadin MS, Ab Mutalib NS, Latif MT, Greene CM, Hassan T (2018) Challenges and future direction of molecular research in air pollution-related lung cancers. Lung Cancer 118:69–75. https://doi.org/10.1016/j.lungcan.2018.01.016
Shyam Bihari Sharma SJ, Praveen Khirwadkar, and Sunisha Kulkarni (2013) The effects of air pollution on the environment and human health Indian Journal of Research in Pharmacy and Biotechnology 1:391–396
Singh A, Trevick S (2016) The Epidemiology of Global Epilepsy. Neurol Clin 34:837–847. https://doi.org/10.1016/j.ncl.2016.06.015
Skalska K, Miller J, Ledakowicz S (2010) Trends in NOx abatement: a review. Sci Total Environ 408:3976–3989. https://doi.org/10.1016/j.scitotenv.2010.06.001
Song P, Liu Y, Yu X, Wu J, Poon AN, Demaio A, Wang W, Rudan I, Chan KY (2017) Prevalence of epilepsy in China between 1990 and 2015: a systematic review and meta-analysis. J Glob Health 7:020706. https://doi.org/10.7189/jogh.07-020706
Srivastava RK, Hall RE, Khan S, Culligan K, Lani BW (2005) Nitrogen oxides emission control options for coal-fired electric utility boilers. J Air Waste Manage Assoc 55:1367–1388. https://doi.org/10.1080/10473289.2005.10464736
Svensson JE, Johansson LG (1993) A laboratory study of the effect of ozone, nitrogen dioxide, and sulfur dioxide on the atmospheric corrosion of zinc. J Electrochem Soc 140:2210–2216
Tajudin M et al (2019) Risk of concentrations of major air pollutants on the prevalence of cardiovascular and respiratory diseases in urbanized area of Kuala Lumpur. Malaysia Ecotoxicol Environ Saf 171:290–300. https://doi.org/10.1016/j.ecoenv.2018.12.057
Tamayo T, Rathmann W, Krämer U, Sugiri D, Grabert M, Holl RW (2014) Is particle pollution in outdoor air associated with metabolic control in type 2 diabetes? PLoS One 9:–e91639. https://doi.org/10.1371/journal.pone.0091639
Tamayo T, Rathmann W, Stahl-Pehe A, Landwehr S, Sugiri D, Krämer U, Hermann J, Holl RW, Rosenbauer J (2016) No adverse effect of outdoor air pollution on HbA1c in children and young adults with type 1 diabetes. Int J Hyg Environ Health 219:349–355. https://doi.org/10.1016/j.ijheh.2016.02.002
Tian L, Qiu H, Pun VC, Ho KF, Chan CS, Yu IT (2015) Carbon monoxide and stroke: a time series study of ambient air pollution and emergency hospitalizations. Int J Cardiol 201:4–9. https://doi.org/10.1016/j.ijcard.2015.07.099
Tikuisis P, Kane DM, McLellan TM, Buick F (1985) Fairburn SM (1992) Rate of formation of carboxyhemoglobin in exercising humans exposed to carbon monoxide. J Appl Physiol 72:1311–1319. https://doi.org/10.1152/jappl.1992.72.4.1311
Tofield A (2017) Air pollution and traffic noise effect on blood pressure. Eur Heart J 38:71–72. https://doi.org/10.1093/eurheartj/ehw607
Townsend CL, Maynard RL (2002) Effects on health of prolonged exposure to low concentrations of carbon monoxide. Occup Environ Med 59:708–711. https://doi.org/10.1136/oem.59.10.708
Tsangari H, Paschalidou AK, Kassomenos AP, Vardoulakis S, Heaviside C, Georgiou KE, Yamasaki EN (2016) Extreme weather and air pollution effects on cardiovascular and respiratory hospital admissions in Cyprus. Sci Total Environ 542:247–253. https://doi.org/10.1016/j.scitotenv.2015.10.106
Venditti CC, Smith GN (2014) Involvement of the heme oxygenase system in the development of preeclampsia and as a possible therapeutic target. Womens Health (Lond) 10:623–643. https://doi.org/10.2217/whe.14.54
Wang N, Mengersen K, Tong S, Kimlin M, Zhou M, Wang L, Yin P, Xu Z, Cheng J, Zhang Y, Hu W (2019) Short-term association between ambient air pollution and lung cancer mortality. Environ Res 179:108748. https://doi.org/10.1016/j.envres.2019.108748
Weinstock B, Niki H (1972) Carbon monoxide balance in nature. Science 176:290–292. https://doi.org/10.1126/science.176.4032.290
Wong IC, Ng YK, Lui VW (2014) Cancers of the lung, head and neck on the rise: perspectives on the genotoxicity of air pollution Chin J Cancer 33:476–480. doi: https://doi.org/10.5732/cjc.014.10093
World Health Organization O, Environmental Health T (2006) WHO Air quality guidelines for particulate matter, ozone, nitrogen dioxide and sulfur dioxide : global update 2005 : summary of risk assessment. World Health Organization, Geneva
World Health Organization. Regional Office for E (2003) Health aspects of air pollution with particulate matter, ozone and nitrogen dioxide : report on a WHO working group, Bonn, Germany 13-15 January 2003. Copenhagen : WHO Regional Office for Europe
Xu C, Fan YN, Kan HD, Chen RJ, Liu JH, Li YF, Zhang Y, Ji AL, Cai TJ (2016) The novel relationship between urban air pollution and epilepsy: a time series study. PLoS One 11:e0161992–e0161992. https://doi.org/10.1371/journal.pone.0161992
Yan Y, Li Y, Sun M, Wu Z (2019) Primary pollutants and air quality analysis for urban air in China: evidence from Shanghai. Sustainability 11:2319
Zhang H, Dong H, Ren M, Liang Q, Shen X, Wang Q, Yu L, Lin H, Luo Q, Chen W, Knibbs LD, Jalaludin B, Wang Q, Huang C (2020) Ambient air pollution exposure and gestational diabetes mellitus in Guangzhou, China: a prospective cohort study. Sci Total Environ 699:134390. https://doi.org/10.1016/j.scitotenv.2019.134390
Zhang X, Zhang X, Chen X (2017) Happiness in the air: how does a dirty sky affect mental health and subjective well-being? J Environ Econ Manag 85:81–94. https://doi.org/10.1016/j.jeem.2017.04.001
Zhao CN, Xu Z, Wu GC, Mao YM, Liu LN, Qian-Wu, Dan YL, Tao SS, Zhang Q, Sam NB, Fan YG, Zou YF, Ye DQ, Pan HF (2019a) Emerging role of air pollution in autoimmune diseases. Autoimmun Rev 18:607–614. https://doi.org/10.1016/j.autrev.2018.12.010
Zhao Y, Hu J, Tan Z, Liu T, Zeng W, Li X, Huang C, Wang S, Huang Z, Ma W (2019b) Ambient carbon monoxide and increased risk of daily hospital outpatient visits for respiratory diseases in Dongguan, China. Sci Total Environ 668:254–260. https://doi.org/10.1016/j.scitotenv.2019.02.333
Zhu F et al (2019) The short-term effects of air pollution on respiratory diseases and lung cancer mortality in Hefei: a time-series analysis. Respir Med 146:57–65. https://doi.org/10.1016/j.rmed.2018.11.019
Zivin JG, Neidell M (2012a) The impact of pollution on worker productivity. Am Econ Rev 102:3652–3673
Zivin JG, Neidell M (2012b) The impact of pollution on worker productivity. Am Econ Rev 102:3652–3673. https://doi.org/10.1257/aer.102.7.3652
Download references

Acknowledgements
This research was funded by the Deanship of scientific research at Princess Nourah bint Abdulrahman University through the fast-track research funding program.
Author information
Authors and affiliations.
Textile Engineering Department, Textile Research Division, National Research Centre, Dokki, Cairo, Egypt
Alsaid Ahmed Almetwally
Biology Department, College of Science, Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia
May Bin-Jumah
Department of Zoology, Faculty of Science, Beni-Suef University, Beni-Suef, 65211, Egypt
Ahmed A. Allam
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Alsaid Ahmed Almetwally .
Additional information
Responsible editor: Lotfi Aleya
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Almetwally, A.A., Bin-Jumah, M. & Allam, A.A. Ambient air pollution and its influence on human health and welfare: an overview. Environ Sci Pollut Res 27 , 24815–24830 (2020). https://doi.org/10.1007/s11356-020-09042-2
Download citation
Received : 09 January 2020
Accepted : 23 April 2020
Published : 03 May 2020
Issue Date : July 2020
DOI : https://doi.org/10.1007/s11356-020-09042-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Air pollution
- Major air pollutants
- Human health
- Harmful effects
- Cardiovascular disease
- Respiratory disease
- Find a journal
- Publish with us
- Track your research
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Air pollution and health prevention: A document of reflection
Calidad del aire ambiente y prevención de la salud: un documento de reflexión, emilio bouza, francisco vargas, bernardino alcázar, teresa álvarez, ángel asensio, gloria cruceta, diego gracia, jesús guinea, miguel angel gil, cristina linares, patricia muñoz, eduardo olier, paulino pastor, maría luisa pedro-botet, xavier querol, javier tovar, isabel urrutia, felipe villar, esteban palomo.
- Author information
- Article notes
- Copyright and License information
Correspondence: Emilio Bouza, Servicio de Microbiología Clínica y Enfermedades Infecciosas del Hospital General Universitario Gregorio Marañón, Universidad Complutense. CIBERES. Ciber de Enfermedades Respiratorias. Madrid E-mail: [email protected]
Received 2021 Dec 12; Accepted 2022 Jan 10; Issue date 2022.
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0)( https://creativecommons.org/licenses/by-nc/4.0/ ).
Ambient air quality, pollution and its implication on health is a topic of enormous importance that is normally dealt with by major specialists in their particular areas of interest. In general, it is not discussed from multidisciplinary approaches or with a language that can reach everyone. For this reason, the Health Sciences Foundation, from its prevention area, has formulated a series of questions to people with very varied competences in the area of ambient air quality in order to obtain a global panorama of the problem and its elements of measurement and control. The answers have been produced by specialists in each subject and have been subjected to a general discussion that has allowed conclusions to be reached on each point. The subject was divided into three main blocks: external ambient air, internal ambient air, mainly in the work-place, and hospital ambient air and the consequences of its poor control. Along with the definitions of each area and the indicators of good and bad quality, some necessary solutions have been pointed out. We have tried to know the current legislation on this problem and the competences of the different administrations on it. Despite its enormous importance, ambient air quality and health is not usually a topic of frequent presence in the general media and we have asked about the causes of this. Finally, the paper addresses a series of reflections from the perspective of ethics and very particularly in the light of the events that the present pandemic raises. This work aims to provide objective data and opinions that will enable non-specialists in the field to gain a better understanding of this worrying reality.
Keywords: Ambient air, quality, public health, nosocomial infection, invasive aspergillosis, measurement systems, respiratory infections
La calidad del aire ambiente y su implicación en la salud es un tema de enorme importancia que normalmente es tratado por grandes especialistas en sus particulares áreas de interés. En general, no es discutido desde enfoques multidisciplinares ni con un lenguaje que pueda llegar a todos. Por ese motivo, la Fundación de Ciencias de la Salud desde su área de prevención, ha formulado una serie de preguntas a personas con competencias muy variadas en el área de la calidad del aire ambiente para obtener un panorama global del problema y de sus elementos de medida y control. Las respuestas han sido producidas por especialistas en cada tema y han sido sometidas a una discusión general que ha permitido alcanzar conclusiones en cada punto. El tema ha sido dividido en tres grandes bloques: el aire ambiente externo, el aire ambiente interno, principal-mente en el medio laboral, y el aire ambiente hospitalario y las consecuencias de su mal control. Junto con las definiciones de cada área y los indicadores de buena y mala calidad, se ha apuntado a algunas necesarias soluciones. Hemos tratado de conocer la legislación vigente sobre este problema y las competencias de las distintas administraciones sobre el mismo. Pese a su enorme importancia, la calidad del aire ambiente y la salud no suele ser un tema de frecuente presencia en los medios de comunicación generales y hemos preguntado sobre las causas de ello. Finalmente, el documento aborda una serie de reflexiones desde la perspectiva de la ética y muy particularmente a la luz de los acontecimientos que la presente pandemia plantea. Este trabajo pretende aportar datos objetivos y opinión que permitan a los no especialistas en el tema conocer mejor esta preocupante realidad.
Keywords: Aire ambiente, calidad, salud pública, infección nosocomial, aspergilosis invasora, sistemas de medición, infecciones respiratorias
INTRODUCTION
Air quality is a subject of unquestionable interest for the population, for health authorities, for scientists and technicians involved in one way or another and, consequently, for the political world. However, its complexity, its multiple technical aspects and the different approaches to this subject from different fields mean that an overall view is often lacking. The quality of external ambient air does not necessarily follow the same parameters as in the working environment, and hospital air problems have specific consequences that are not always understood from outside the healthcare world.
Very often, experts in one of these aspects ignore the quality parameters and the consequences of their lack of control in areas other than their own.
For this reason, the Health Sciences Foundation, from its area of prevention, has motivated a multidisciplinary meeting so that different experts in some of the many facets of air quality control, could answer questions, apparently elementary, but not always known by all, that would help to better understand this issue and its very serious implications for the health of all.
The different authors responded in writing to the questions posed to them, shared the information with the rest of the participants and conclusions were reached after the discussion of each topic.
The following document is the result of these activities and we have divided it into 3 thematic areas: ambient air in the community, ambient air in the workplace and ambient air in the hospital environment.
FIRST BLOCK: AMBIENT AIR IN THE COMMUNITY
What is the relationship between outdoor air pollution, disease and mortality, bernardino alcázar navarrete.
Environmental pollution is a global threat that has high impacts on human health and ecosystems, with emissions and concentrations that have been progressively increasing in recent years around the world. Air pollution is currently considered the most important environmental risk factor for human health and is a leading cause of premature death and disease [ 1 - 3 ]. In Europe, air quality remains below the level considered optimal in many areas despite efforts to reduce emissions and air pollutants [ 4 ].
The effects of air pollution on human health include primarily premature deaths from cardiovascular disease, including ischemic heart disease and cerebrovascular disease, followed by deaths due to respiratory disease and lung cancer. In addition, both short- and long-term exposure to air pollution can lead to reduced lung function, increased individual susceptibility to respiratory infections, and aggravation of bronchial asthma. On the other hand, exposure to environmental pollutants is associated with negative impacts on fertility, pregnancy, newborns, and children.
Different studies have shown a consistent association between levels of environmental pollution and all-cause mortality and also specific mortality due to cardiovascular or respiratory disease, both in the short and in the medium and long term. In an international study involving more than 600 cities around the world, exposure to 10 μg increases in mean suspended particulate matter (PM) concentrations [ 5 ] was associated in the short term with an increase in overall, cardiovascular and respiratory mortality. Similarly, increases of the same magnitude in mean daily PM were also associated with increases in overall, cardiovascular and respiratory mortality.
Air pollution is also associated with increases in long-term mortality in the European population. Within the ESCAPE (European Cohort Study for the Effects of Environmental Pollution) initiative, this effect was analyzed using data from 22 European cohorts, with an average follow-up of 13.9 years, showing an effect of PM on mortality (7% increased risk of death per 5 μg/mm 3 ). These effects were also observable if data were selected from participants with exposure levels below the thresholds recommended by the authorities [ 4 ].
In Spain, the most recent available data indicate that 15.3% of the Spanish urban population is exposed to levels of ozone (O 3 ) above the EU recommended standard, 3.6% of the population is exposed to levels of nitrogen dioxide (NO 2 ) above the recommended standard and 0.1% is exposed to excessive levels of PM. It is true that exposure to these environmental pollutants has undergone a progressive decrease in the last decade thanks to the efforts of different governments, but there is still work to be done.
According to the data consulted for 2018, estimates tell us that in Spain there were 23,000 premature deaths due to exposure to PM, 6,800 premature deaths attributable to NO 2 and 1,800 deaths attributable to O 3 , which would give us a total of 31,600 premature deaths attributable to environmental pollution in a year.
In addition to these data, environmental pollution, as previously mentioned, is responsible for the loss of years of life derived from its effects both in the short and long term. It was estimated for 2018 a loss of more than 350,000 years of life in the Spanish population attributable to environmental pollution, derived from 254,700 years of life lost due to PM, 75,400 years of life lost due to NO 2 and 20,600 years of life lost due to O 3 . In population-adjusted terms, these losses would be 573, 170 and 46 years of life/100,000 inhabitants for PM, NO 2 and O 3 , respectively.
CONCLUSION:
The impact of environmental pollution on the health of the population is indisputable, both in the short and long term, with increases in mortality due mainly to cardiovascular and respiratory causes, in addition to other health effects that can have repercussions on the quality and duration of life .
HOW DO WE DEFINE WHAT IS AN OUTDOOR AIR OF GOOD QUALITY? WHAT ARE THE CRITICAL PARAMETERS IN OUTDOOR AMBIENT AIR QUALITY CONTROL? WHAT MEASURES SHOULD BE TAKEN TO IMPROVE OUTDOOR AIR QUALITY?
Xavier querol carceller.
An air pollutant is any substance present in the air that may have harmful effects on human health, the environment or property of any nature. The increase in the concentration of atmospheric pollutants in outdoor ambient air (street, parks, industrial, rural, and remote areas) causes deterioration of air quality. This deterioration occurs at different scales. Thus, in cities, emissions of urban, industrial, and domestic pollutants have an impact on air quality in the same area where they are emitted. On the other hand, cities and rural and remote areas can see their ambient air deteriorated by the transport of pollutants produced tens, hundreds or even thousands of kilometers away. Examples include tropospheric ozone, acid rain or incursions of Saharan dust masses. The critical WHO normative target pollutants are particulate matter (PM 10 and PM 2.5 ), nitrogen dioxide (NO 2 ), tropospheric ozone (O 3 ) and Benzo(a) pyrene (BaP). Any pollutant that has a WHO normative reference value should be kept below the reference values.
The latest study on “The global burden of disease”, published in The Lancet, concludes that exposure to polluted air is the fourth leading risk factor for mortality on a global scale, behind high blood pressure, smoking and inadequate diet. This impact also has another associated economic effect, estimated by the World Bank at 4% of global GDP [ 5 , 6 ].
The European Environment Agency [ 7 ] quantifies the annual premature deaths in the European Union due to exposure to PM2.5 at 374,000, and recalls that in 1990 this impact reached one million. The same Agency states that 74% of the European population breathed outdoor air that exceeded the WHO guideline value for this pollutant. The maximum levels of NO 2 are not complied with in some of our cities and the Agency estimates that 54,000 premature deaths per year are attributable to its impact on health. With regard to O 3 levels, 70% of the Spanish territory does not comply with the normative target values for human health and 99% of the population of the Europe of -28 breathes outdoor air with concentrations above the WHO guideline level. Finally, BaP is highly carcinogenic, and its levels have increased with the use of agricultural, domestic and residential biomass burning.
In a typical Spanish city, road traffic contributes 70% of the NO 2 breathed by its citizens. And within the traffic about 90% of this contribution is due to diesel vehicles, especially those prior to 2019. In the case of PM 2.5 , road traffic is also responsible for 30% of the PM 2.5 and PM 10 we breathe, and not only because of exhaust pipes, but also because of brake and wheel wear. Industry can still contribute 20% of PM, construction sites 10%, ports 5%, .... In the case of BaP, the highest levels recorded in Spain are from rural areas with high domestic-residential and/or agricultural biomass burning. Finally, O 3 is the most complex pollutant. It is secondary (not emitted by emission sources but formed in the atmosphere from reactions between NO 2 and volatile organic compounds), so to reduce its levels it is necessary to act on its precursors, although knowing how to do this is still scientifically and politically complex. In addition, there are unregulated pollutants, such as ultra-fine particles (those smaller than 0.1 microns) and black carbon (the product of the imperfect combustion of fossil fuels or biomass), which have a high impact on health and, in the opinion of a large part of science, deserve to be regulated. In both cases their main source in urban areas is road traffic.
To improve air quality, the most environmentally advanced cities (Scandinavian, Swiss, Canadian, Australian) have for years implemented measures that have enabled them to record the lowest pollution levels in the urban world, but also in rural areas, where air quality problems can also occur. It is important to note that air quality is a characteristic of a society, and that the most cultured and advanced societies have the best conditions in this regard.
In the case of NO 2 , measures have focused on reducing the number of metropolitan vehicles circulating by means of [ 8 ]
well-developed, fast, economical and comfortable metropolitan and urban public transport;
reduction of the number of urban vehicles circulating through urban tolls and restriction of outdoor parking to residents only;
low emission zones that do not allow the circulation of the most polluting older vehicles and favor the most eco-efficient ones;
efficient logistics of urban distribution of goods and cabs (reducing the number of trips through intelligent logistics, night-time deliveries, hybridization and electrification of vehicles, ....); and
urban redesign to gain space for the vehicle in favor of green and pedestrian areas, and to separate traffic from hospitals, schools, primary care centers, geriatric centers, playgrounds, etc.)
For PM 2.5 these measures may be partially effective, but measures have also been taken on industrial emissions, ports, airports, construction-demolition and domestic and residential emissions. Thus, for both PM 2.5 and BaP, low emission certification for biomass boilers and the use of certified biomass (natural origin, low humidity and ash) is mandatory [ 9 ].
For O 3 the situation is more complex [ 10 , 11 ], measures should be taken not only at the urban level but also at the regional, national and European levels, in terms of reducing emissions of precursors (NO 2 from traffic, industry and electricity generation mainly) and volatile organic compounds (traffic and industry mainly, but also from the use of cleaning products, paints, resins, ....).
The critical pollutants are suspended particulate matter (PM 10 , and PM 2.5 ), nitrogen dioxide (NO 2 ), tropospheric ozone (O 3 ) and Benzo(a)pyrene (BaP) .
Control measures have focused on reducing the number of metropolitan vehicles circulating, but measures have also been taken on industrial emissions, ports, airports, construction-demolition and domestic and residential emissions .
HOW DOES AIR POLLUTION AFFECT MORE THAN JUST CARDIOVASCULAR AND RESPIRATORY DISEASES? IS THERE A RELATIONSHIP BETWEEN COVID-19 AND AIR POLLUTION? WHY IS NOISE POLLUTION NOT CONSIDERED AS PART OF AIR POLLUTION?
Cristina linares gil.
According to the World Health Organization (WHO), 90% of the world’s population currently lives in areas where environmental pollution levels acceptable for health protection are exceeded [ 12 ]. Historically, air pollution has been linked to respiratory and cardiovascular health problems, but every day more and more studies are published on the impact on other organs. In 2013, the IARC (International Agency for Research on Cancer) classified air pollution as a major carcinogen [ 13 ] and in 2018 a review study was already published with data from different cohorts in Europe linking air pollution to breast cancer [ 14 ], especially with NO 2 . Other studies [ 15 ] have also pointed out that there is an association between PM 2.5 concentrations and mortality from cancer of any origin and especially in the upper digestive tract. Pollution is also related to endocrine diseases such as diabetes. The study by Alderete et al. [ 16 ] summarizes the scientific evidence that air pollution is a new risk factor for various metabolic dysfunctions and type 2 diabetes.
At the behavioral level, air pollution is also related to the risk of anxiety and depression. A study conducted in Barcelona, between 2013-2014, shows increased cases of depression and use of medications such as benzodiazepines and antidepressants as the levels of exposure to air pollutants increase [ 17 ]. Air pollution has also been linked to cognitive ability in adults. A review of studies linking air pollution and Parkinson’s disease establishes that exposure to NO 2 , CO and O 3 may increase the risk of Parkinson’s disease [ 18 ] and a study carried out in Madrid shows that hospital admissions for Alzheimer’s disease increase in relation to PM 2.5 concentrations [ 19 ].
Of particular importance is the impact of air pollution on children’s health. There is growing evidence that exposure to air pollutants during periods of fetal life and infancy can have very long-term effects. Health impacts occur even at lower pollutant concentrations than in adults [ 20 ] because of the vulnerability of the accelerated cellular growth that occurs at this stage for the formation of the nervous, reproductive and endocrine systems [ 21 ] among others; as well as the fact that the physiological pathways are metabolically more immature and the mechanisms of elimination of exogenous compounds from the organism are also less developed and less effective. Exposure of children to O 3 and PM is associated with an increased likelihood of bronchitis and other respiratory diseases in the postnatal stage, while intrauterine exposure to nitrogen dioxide and particulate matter has significant negative effects on fetal growth and anthropometric parameters at birth [ 22 , 23 ]. On the other hand, COVID-19 and the mobility limitations established to try to contain its spread during the period of confinement in Spain, have led to a decrease in pollutant emissions. This reduction has been of more than 50% in NO 2 emissions and almost 20% in PM 10 emission [ 24 ]. As to whether air pollution may be a risk factor in the transmission of the SARS-CoV-2 virus, two hypotheses are currently being considered, both of which are complementary:
a) It is being investigated whether the polluting particles themselves are capable of viably transporting the new virus, as has been demonstrated in previous studies with other types of biological material: bacteria, viruses, fungi and pollen grains [ 25 ]. The explanation for this mechanism can be found in recent research according to which particulate matter may act as a vector for the spread of the disease [ 26 - 28 ]; places with higher concentrations of PM 10 would be associated with regions with a higher number of COVID-19 cases. This same study, but more extended, has found traces of SARS-CoV-2 RNA in PM samples measured in both industrial and urban environments. The hypothesis is based on the fact that aerosol particles containing the virus of between 0.1 and 1μm can travel farther when bound to pollutant particles of up to 10μm as the resulting particle is larger and less dense than a respiratory droplet, so it could increase its residence time in the atmosphere.
b) The second hypothesis focuses on the increased cardio-respiratory vulnerability of people who are regularly exposed to high levels of pollution in cities. According to the WHO, 1 in 7 patients with COVID-19 suffer respiratory difficulties and other serious complications [ 29 ] and to date, factors associated with COVID-19 mortality include: advanced age (higher risk in >65 years) and the presence of comorbidities, including hypertension, diabetes, cardiovascular and cerebrovascular disease. Also documented in relation to this new disease are: vascular inflammation, myocarditis and cardiac arrhythmias.
Finally, it is important to note that air pollution includes both traditional chemical air pollution and pollen pollution as well as thermal, light, electromagnetic and, of course, noise pollution. Although when air pollution is almost always referred to as chemical pollution, in an urban environment and from the point of view of its impact on health, chemical pollution is just as important as noise pollution [ 30 ].
Environmental pollution is a major carcinogen, is a risk factor for various metabolic dysfunctions such as type 2 diabetes, increases the risk of anxiety and depression, and influences fetal and neonatal health .
It was initially hypothesized that particulate matter could act as a viable transport vector for SARS-CoV-2, although recent research does not appear to support this hypothesis. It is important to note that air pollution includes both traditional chemical and pollen pollution as well as thermal, light, electromagnetic and noise pollution .
HOW IS THE DETECTOR NETWORK IN SPAIN? ARE THERE DIFFERENCES BY AUTONOMOUS COMMUNITIES? IS IT SUFFICIENT?
Miguel angel gil amigot.
The Network of Environmental Pollutant Detectors in Spain is based on a system of monitoring stations equipped with sensors and automatic analyzers distributed in representative locations by zones affected by air quality. This zoning serves to group areas with similar characteristics or homogeneous behavior in relation to air quality and environmental pollutant thresholds [ 31 ].
The determination of the different zones and the location of each control and monitoring station is the responsibility of the Autonomous Communities (CCAA). In addition to the network controlled by the Autonomous Communities, there are two other types of monitoring networks. On the one hand, the state network managed by the Spanish Meteorological Agency (AEMET), which is responsible for measuring air quality in remote rural environments and aims to obtain information on transboundary and background pollution in order to comply with current regulations [ 32 ]. On the other hand, the network of detectors controlled by local entities or municipalities is developed in order to monitor the main pollutants in certain locations.
In addition to the air quality homogeneity criteria, the air quality legislation, Royal Decree 102/2011 on air quality improvement, requires the Autonomous Regions to justify the division of the zones considering a certain population density and a common ecosystem in each one of them. As an example, the Autonomous Community of Aragon follows a methodology for zoning its territory [ 33 ]. On the one hand, the historical air quality data from the detector stations is studied, comparing the data from different stations, the meteorological factors of each area and the topography of the territory. Once the data for the territory has been obtained, measures are taken to ensure that the characteristics in terms of air quality and geography are the same in each area and to delimit as far as possible the areas where there is a high level of concentration (since the restrictions required by law are greater).
All the monitoring stations of the regional and local network in Spain measure the concentrations of gaseous pollutants (NO 2 , O 3 , CO...) and particulate matter (PM 2.5 , PM 10 ) in the air that are harmful to health and the environment. It is a monitoring network with more than 600 fixed measurement stations in which a wide variety of pollutants are recorded and controlled to estimate the risks and associate the effects on health resulting from exposure to various pollutants in each area of the Spanish territory [ 34 - 36 ].
Stations can be classified by type of area and by type of main pollutant influencing the site. In relation to the type of area, the station can be urban, if it is placed in areas that are continuously built-up; suburban, if it is in places where there is no continuous building and there are separations from lakes, forests, parks...; or rural, when it does not meet any of the previous criteria. On the other hand, in relation to the type of pollutant influencing the zone, it can be classified as a traffic station, if the main pollutant in the zone is vehicle emissions; industrial, when the emission comes from industry; or background, when no predominant emission is detected.
The reason why each zone is evaluated by means of a number of stations and a type of station determined by each Autonomous Community is justified by the impossibility of measuring air quality at all points of the territory. In line with this reasoning, it is true that the location of the monitoring and control stations in each area of Spain can be a determining factor in the measurement of the levels of certain pollutants. That is to say, it is not the same to place a traffic station very close to one of the busiest and most congested roads in a large city where it is obvious that very high concentrations of pollutants will be registered (for example, NO 2 emissions from vehicles will be directly registered in these stations), than to build the station in a place further away from traffic and high congestion in that same city. Since there is no specific standard related to the exact location of station placement, it is very difficult to reflect the reality of variations in pollutant exposure levels.
Finally, it should be noted that although each Autonomous Community divides its territory into air quality assessment zones, in the end, Spanish legislation requires a series of criteria for the division of the zones. It is true that in the most populated and busiest cities in Spain, where the highest levels of pollution are detected, i.e. Madrid, Barcelona and Valencia, a greater number of control stations are concentrated and more rigorous action plans and protocols are developed to obtain the values allowed by law.
The air quality monitoring network in the national territory is correctly distributed in cities and towns and it is sufficiently sophisticated for the detection of environmental pollutants. They send, in real-time, the results recorded for the preparation of evaluation reports and implementation of plans for the reduction of pollutants in the environment, although it is true, that there is room for improvement at least as far as unification of criteria is concerned .
WHAT DISEASES ARE DIRECTLY RELATED TO AIR POLLUTION?
Recent work indicates that the health impact attributable to air pollution is substantially higher than previously assumed, and estimates excess mortality attributed to air pollution at 790,000 deaths per year in Europe alone ( Figure 1 ). Although air pollutants can damage virtually every organ in the human body, it is cardiovascular and respiratory diseases that cause the most deaths. It is estimated that around 500,000 lung cancer deaths and 1.6 million COPD deaths worldwide can be attributed to air pollution. In Spain, it is estimated that there are more than 5,000 deaths per year from ischemic heart disease, more than 2,000 from strokes, almost 3,000 from COPD, 1,216 from pulmonary neoplasms and more than 1,000 from lower respiratory tract infections that would not occur if we did not breathe polluted air.
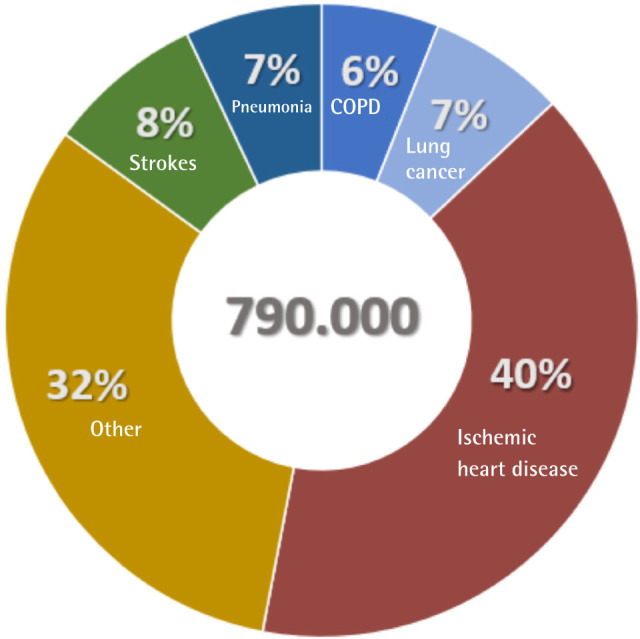
Deaths per year in Europe due to air pollution
COPD is characterized by persistent airflow limitation associated with chronic inflammation of the airways and lungs in response to exposure to particles and gases. Active smoking remains the main risk factor, but other factors are increasingly well known, such as occupational exposures, infections and the role of air pollution. COPD is the fourth leading cause of death both in Spain and worldwide, and it is estimated that in the coming years it will climb one more place in this fateful ranking [ 37 ]. Worldwide prevalence is estimated at 11.7% with very high underdiagnosis rates that may exceed 70%.
COPD patients are more vulnerable to the effects of air pollution. The main mechanisms underlying the adverse health effects of environmental exposure to pollutants are related to oxidative stress and inflammation. Apart from the fact that particulate matter can move into the bloodstream and create vascular dysfunction with potential systemic effects that de-compensate the frequent cardiovascular comorbidities of these patients, oxidative stress related to air pollutants can directly damage the airway epithelium and alter the immune response. At present, there is sufficient scientific evidence to consider environmental pollution as a direct cause of COPD. This is reflected in the favorable positioning of the main clinical practice guidelines for the management of COPD, both national and international [ 38 - 40 ] . Ambient concentrations of particulate matter (PM) and nitrogen dioxide (NO 2 ) have been associated with an increased prevalence of COPD. For example, a higher year-round average PM 2.5 concentration has been associated with an increased prevalence of COPD with an adjusted odds ratio (OR) of 2.4 for concentrations between 35 and 75 μg/m 3 and 2.5 for concentrations above 75 μg/m 3 , respectively, compared with the lower limit of 35 μg/m 3 . However, this etiological role is even more evident if we consider indoor air pollution. We spend about 90% of our time indoors, so the atmosphere in these spaces is very important for our health. Some 3 billion people cook and heat their homes with open fires and stoves burning biomass (wood, animal dung or agricultural waste) and charcoal. This practice occurs mainly in developing countries. Each year, more than 4 million people die prematurely from diseases attributable to household air pollution and COPD accounts for 20% of these deaths. Thus, environmental pollutants become the main cause of COPD in some regions of the world among certain population groups, such as women with limited economic resources in some areas of Southeast Asia.
Environmental pollution has also been recognized as a precipitating factor in COPD exacerbations, which accelerate the deterioration of respiratory function, contribute to increased mortality and significantly increase healthcare costs. In the case of the COVID pandemic, we know that SARS-CoV-2 is spread through the air by so-called Flugge droplets. Particles smaller than 5μ can remain in the air even for hours and spread far away. Some authors have described that PM can both increase transmission distance and infectivity in the aerosol with a “booster” effect.
The impact that air pollution has on the extent and prognosis of COVID-19 remains to be elucidated. In a recent study conducted in China between January and February 2020 they observed a positive association between two-week PM 2.5 , PM 10 , NO 2 and O 3 levels and confirmed new cases of COVID-19. The authors observed that each 10g/m 3 (lag 0-14 days) increase in these pollutants was associated with an increase in new confirmed cases of 2.24%, 1.76%, 6.94%, and 4.76%, respectively.
Italy was another of the major victims of the beginning of this pandemic in Europe. Several Italian authors have stressed that the high spread of COVID in some areas of Northern Italy could be linked to environmental conditions. In addition, the suspended particles, composed of solid and liquid particles, allow the virus to float in the air for longer and over longer distances. In fact, the spread of SARS-CoV-2 infection is found to increase in areas with higher relative humidity while it decreases in warmer climates.
Ambient air pollution is estimated to cause 790,000 deaths per year in Europe. In addition to cardiovascular diseases, the relationship between environmental pollution and Chronic Obstructive Pulmonary Disease is essential. There is also speculation about the relationship between environmental pollutants and a better vehiculation of SARS-CoV-2 particles over longer distances .
SECOND BLOCK: INDOOR AMBIENT AIR QUALITY IN THE WORKING ENVIRONMENT
How do we define indoor environmental quality what is the effect of aerosols on sars-cov-2 transmission what measures are most effective in reducing aerosols, francisco vargas marcos.
Indoor Environmental Quality (IQ) is defined in the Une 171330:2008 Standard [ 41 ] as “Indoor environmental conditions, appropriate to the user and the activity, defined by the levels of chemical and microbiological contamination and by the values of physical factors”. Without good IAC, the risk of numerous diseases such as COVID-19 increases. We spend between 80-90% of our time in indoor environments for work, home, education, sports or leisure. During the COVID-19 pandemic this percentage has risen and has highlighted the importance of living in healthier and safer enclosed spaces that prevent airborne transmission of SAR-CoV-2. Humans generate aerosols or bioaerosols that have been defined elsewhere [ 42 ]. It can be stated that SARS-CoV-2 is viable as an aerogenic pathogen continuously emitted with respiration. Its quantity increases when we suffer from respiratory diseases and when we force our voice when speaking, singing or shouting. For these reasons, the transmission of respiratory diseases inside poorly ventilated enclosed spaces can be up to 20 times higher than outdoor transmission. Since the beginning of the pandemic, numerous studies have been published that have observed an increase in the number of outbreaks of COVID-19 caused by aerosols carrying the virus in restaurants, gyms, boats, buses, choirs and other enclosed places with poor ventilation. Several experimental tests on fluid dynamics, aerosol physico-chemistry, permanence, SARS-CoV-2 viability, infective capacity (16 hours), have alerted to the importance of aerosol transmission and the need to apply prevention and control measures in closed, poorly ventilated and crowded spaces [ 43 - 46 ].
This evidence challenged the classical routes of transmission of respiratory diseases accepted by WHO and the scientific community. New knowledge on respiratory emission dynamics indicates that respiratory droplets can reach, under specific conditions, 7-8 meters. Their acceptance has important implications for improving respiratory protection mask design, social distancing recommendations, prevention strategies in air conditioning installations and other public health recommendations.
But to prevent airborne SARS-CoV-2 transmission, the first step was for health authorities, agencies and organizations to accept the published evidence on the role of aerosols in COVID-19 transmission, overcoming political fears of public reaction, the media, opinion polls and social networks. It is clear that there has been a delay in recognizing the impact of air on COVID-19 transmission and in making decisions on the most effective measures for implementation.
Legitimate and justified calls have been published to evaluate how the pandemic has been managed, to learn from mistakes, to provide the necessary resources for research, to improve epidemiological surveillance systems and public health services. However, it should be noted that it is common for too much time to elapse between the publication of solid evidence, its majority acceptance by the scientific community and finally its application by the competent authorities in Public Health or health professionals with respect to a preventive measure, drug, medical or surgical technique.
One of the first articles published in our country calling for airway prevention measures was a review of scientific evidence on the transmission of SARS-CoV-2 by respiratory droplets, contaminated objects and aerosols [ 47 ]. This document served as the basis for the Ministry of Health to promote the drafting of a technical document containing the Recommendations for the operation and maintenance of air conditioning and ventilation systems to prevent the spread of SARS-CoV-2 [ 48 ].
The ECDC [ 49 ], WHO [ 50 ] and American CDC [ 51 ] have accepted the evidence of SARS-CoV-2 transmission via aerosols, proposed measures to reduce the risk of exposure to aerosols and described the role played by heating, ventilation and air conditioning systems. In the light of the new evidence, they admit the possibility that in certain indoor environments with many people who do not keep a safe distance, without facial protection, in closed and poorly ventilated spaces, airborne transmission combined with droplet (large) and contact transmission may occur.
Subsequently, the Spanish Ministry of Health published a technical document supported by experts and several SSCCs specialized in aerosols that recognizes the importance of airborne transmission and proposes prevention measures [ 52 ].
Summary of recommendations for the prevention of SARS-CoV-2 transmission by aerosols .
Preventive measures to avoid SARS-CoV-2 virus transmission should follow a combined strategy of protective measures, so that the combined use of more than one measure achieves better protection. No single protective measure is 100% effective on its own in preventing transmission. At present, the scientific evidence on the effectiveness of each measure in relation to SARS-CoV-2 is still limited and must be weighed against the risks and feasibility associated with its implementation. Figure 2 summarizes the measures for the prevention of SARS-CoV-2 transmission.
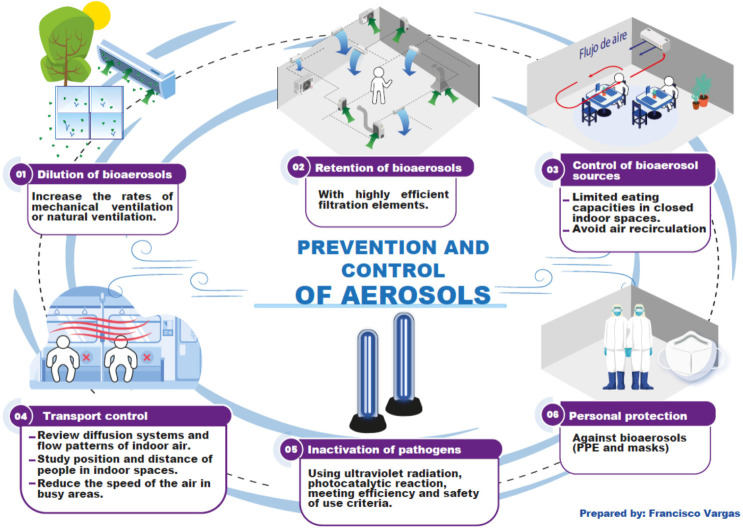
Prevention and control of pathogen transmission by aerosols.
1. Dilution of bioaerosols .
Increase ventilation rates with mechanical ventilation equipment or natural ventilation by opening windows.
2. Retention of bioaerosols .
Use of filtration elements with high filtration efficiency.
3. Control of sources of bioaerosols .
Reduce occupancy rates and time spent in the premises. Maintain interpersonal distance.
Avoid recirculation of air in air conditioning equipment.
Use of face masks in enclosed areas when social distancing measures cannot be applied.
4. Control of bioaerosol transport .
Control of the air diffusion system and indoor air flow patterns.
Study the position and distance of people in indoor premises. Avoid air flows coming from another person.
Reduce air velocity in the occupied area. Avoid air currents between people in the breathing zone.
5. Inactivation of pathogens in bioaerosols .
Use of germicidal equipment of physical action that can contribute to reinforce the hygiene of the indoor environment. With two conditions for their use:
- Scientific evidence of the effectiveness of the system against SARS-CoV-2 virus.
- The dose applied and the residues resulting from its application do not pose any risk to people.
6. Personal protection against bioaerosols .
Use masks with adequate filtration capacity to avoid transmission from/to other persons. Use of PPE in the work environment.
Indoor Environmental Quality (IQ) is defined in the Une 171330:2008 Standard. Since the onset of the COVID-19 pandemic, numerous studies have been published that have noted an increase in the number of COVID-19 outbreaks caused by aerosols in restaurants, gyms, boats, buses, choirs, and other enclosed places with poor ventilation. The Spanish Ministry of Health published a document proposing measures to prevent the transmission of SARS-CoV-2 by aerosols .
WHAT IS THE RELATIONSHIP BETWEEN OUTDOOR AND INDOOR POLLUTION? WHAT ARE, BROADLY SPEAKING, THE MEASURES TO MAINTAIN HEALTHY AIR IN THE WORK ENVIRONMENT? CAN THESE MEASURES BE APPLIED TO COVID-19 PREVENTION?
Teresa álvarez bayona.
WHO estimates that 3.8 million deaths occur annually from diseases attributable to indoor air pollution often caused by the use of inefficient solid fuels [ 53 ]. In countries such as Spain, people spend between 60% and 80% of their time indoors [ 54 ] and the effects of polluted indoor air accumulate in the body regardless of where the pollution occurs. CO 2 is a pollutant that serves as an indicator of indoor air quality associated with human activity. Its use requires reference to the outdoor concentration [ 55 ] since in reality, outdoor air is neither “clean” nor “fresh”.
The technical measures for the control of indoor air will be aimed at controlling the risks related to the environment: reduce the emission of the source, prevent or reduce its spread through the air and, finally, act on people. When the source cannot be eliminated, nor can the emission be reduced, it is necessary to screen the source. It is a measure whose objective is to interpose a physical barrier that reduces the emission of the pollutant into the air [ 56 ].
The next group of measures is aimed at acting on the environment. The most effective measure is ventilation, whether natural, mechanical or mixed. The objective is that, indoors, the “polluted” air is renewed at an adequate rate. As the most effective and cheapest ventilation is natural ventilation, preferably cross ventilation, it should be chosen whenever it is feasible and sufficient [ 57 ]. Sometimes, the programming and adjustments of the air conditioning systems should be directed to a greater contribution of outside air flow. The use of appropriate filters for the recirculated air fraction and their maintenance are other key aspects [ 57 ].
The latest technical measures in the preventive field are aimed at acting directly on the worker. Many of them coincide with the measures aimed at controlling the source, since the workers to be protected must also be considered as possible sources.
Focusing on the throbbing problem of SARS-CoV, this virus identified in 2019 belongs to the Coronaviridae family [ 58 ] and its transmission route and behavior is similar to that of other viruses of the same family [ 59 ]. It is transmitted by nasopharyngeal secretions through droplets of more than 5 microns and by aerosols from human respiration [ 60 ]. In other words, if the focus is avoided, the “contamination” is eliminated. The most direct way is to prevent people from coming to the workplace, for example, by teleworking. As this is not always possible, exposure should be reduced, even if the risk is not eliminated, and measures should be taken to distance and minimize contact. In this case, the barrier is the mask, and the better its efficiency and fit, the lower the emission of aerosols into the environment. There are autonomous governments that have made it compulsory to wear the mask at all times in the workplace [ 61 ].
Some studies suggesting the viability of SARS-CoV-2 in aerosol form during three hours [ 58 ]. This is the reason for recommendations such as ventilating before entering workstations. But not all spaces have windows or elements that ensure proper air renewal. One situation that occurred at the beginning of the pandemic was to consider fans that remove air as a substitute. Their effect is the opposite: instead of providing “clean” air, they recirculate and concentrate pollutants including aerosols. In these cases, it is necessary to resort to mechanical ventilation, which is more expensive and requires specialized expertise. In the case of SARS-CoV-2, distances of 2 meters will be sufficient to avoid droplets, but this is not the case for aerosols. The aerosol has a medium-dependent aerodynamics influenced by temperature, humidity, and air speed. Thus, increasing the relative humidity above 40% affects its aerodynamics in the sense that it favors the precipitation of aerosols and, therefore, hinders their propagation [ 59 ].
All these technical measures to control the transmission of the virus through the air do not work unless the behavior of workers is also changed. In medium- and low-risk companies, the main causes of virus transmission have probably been coffee outings, retirement parties or other social events. For employee awareness to be successful, information must be coherent and adjusted to the level of knowledge of the recipient so that the worker can apply common sense. Unfortunately, these days, this task has been made more difficult due to the contradictory media over-information that has made the general population’s opinion on such a specialized and delicate aspect as this one.
WHO estimates that 3.8 million deaths occur annually from diseases attributable to indoor air pollution frequently caused by the use of inefficient solid fuels. Technical measures for indoor air control should be aimed at eliminating or controlling sources of pollutants, decreasing their spread through the air, and increasing and improving ventilation and air renewal, sometimes including the programming and adjustment of air conditioning systems and the use of appropriate filters. SARS-CoV-2 can remain viable in aerosols for three or more hours and therefore distancing and ventilation measures are recommended .
WHAT IS BEING DONE TO REDUCE AIR POLLUTION FROM INDUSTRY, ARE THERE FEASIBLE PLANS, AND CAN RENEWABLE ENERGIES HELP IMPROVE AIR QUALITY?
Paulino pastor pérez.
When we talk about indoor environmental quality, we often reflect that we spend 90% of our time indoors, to better visualize the magnitude of this exposure, let us consider that for a 55 year old person, this means 50 years in an indoor environment, divided between residential, work and leisure exposure, therefore, it is clear that enclosed spaces are the main source of exposure to air pollution.
Indoor air quality is conditioned by outdoor air quality, since the first measure to improve it is to ventilate with fresh outdoor air, the problem is that this air does not always meet the thermal or purity conditions (absence of pollutants) to produce an effective improvement of indoor air, so it is necessary to condition and treat the air by purification and filtration systems before introducing it into indoor environments.
Improving indoor air quality usually involves an energy cost, and that paradoxically produces pollution outside, especially if we do it through energy from fossil fuels, so it is essential to work on the decarbonization of our buildings in such a way that we end up achieving the necessary indoor air quality and thermal comfort without compromising the quality of outdoor air.
Fortunately, renewable energies, in generation (solar, thermal, biomass, etc.) as well as the improvement in the forms of energy consumption (aerothermal, geothermal, etc.) and the reduction of the energy demand of buildings through improvements in the envelope and others, are allowing us to approach a point of balance between healthiness and comfort indoors and neutrality in terms of emissions to the atmosphere by the building stock.
Nowadays, building owners, mainly office buildings, are starting to devote more and more resources to achieving sustainable buildings (environmental certifications such as LEED or BREEAM), but in recent years the importance of healthy and comfortable buildings (WELL certification) is also being emphasized.
The environmental trend in the tertiary sector is clear; however, other building sectors are not yet in line with this trend. Residential buildings, industrial buildings, logistics centers, hotels, transportation centers and even shopping centers are still far from starting the decarbonization process on a massive scale.
If we compare the real estate sector with other energy-intensive areas such as transport (electric vehicles), we can be sure that it is still far behind. The recent incentive plans by the administration will most probably help technologies to start to be implemented, because currently the technology exists, but the main barrier is the availability of financial resources for the rehabilitation of buildings.
Improving indoor air quality usually involves an energy cost, and that paradoxically produces pollution outside, especially if it is done through energy from fossil fuels .
It is essential to work on decarbonization by progressing towards environmental certifications such as LEED, BREEAM or WELL .
WHAT IS THE CURRENT SITUATION OF LEGIONELLOSIS IN SPAIN? ARE SUFFICIENT MEASURES BEING TAKEN FOR ITS PREVENTION? WHAT DOES THE LEGISLATION ESTABLISH?
Legionella spp . is an intracellular aerobic Gram-negative bacillus that causes pneumonia in both community and hospital settings in the form of sporadic cases or outbreaks. The Legionellaceae family has more than 60 species and more than 70 serogroups of which L. pneumophila sg 1 stands out in both the aquatic reservoir and in human pathology.
The term legionellosis refers to the clinical manifestations caused by this microorganism and includes mostly the pneumonic form and, less frequently, a febrile form without pneumonia or “Pontiac fever”. The most commonly accepted mechanism of transmission to humans is the inhalation of aerosols emanating from colonized water, sanitary or from cooling systems (cooling towers and cogeneration) although exceptionally aspiration is described after oropharyngeal colonization in hospitalized patients with dysphagia.
According to data published by the European Centre for Disease Control (ECDC), a total of 30 countries reported 11,343 cases of legionellosis in 2018 to the European Surveillance system, representing an incidence of 2.2 cases/100,000 inhabitants, the highest recorded in recent years. Among the countries that have declared the most cases, France, Germany, Italy and Spain stand out. In Spain, the number of cases declared in 2018 was 1,513 and the incidence was 3.3 cases per 100,000 inhabitants. In the Spanish territory, cases and outbreaks are monitored by the autonomous communities and notified through the National Epidemiological Surveillance Network (RENAVE) to the National Epidemiological Center of the ISCIII.
Legionellosis mortality in Europe stood at 8% in 2018 and 32 outbreaks have been reported in that year accounting for between 2 and 11 affected per outbreak and of which only 6 have originated in hospital environment.
Climate change, the aging of the population, the eventual deterioration of buildings and their water distribution systems and a greater awareness and sensitivity of countries towards the diagnosis and reporting of legionellosis cases to the ECDC undoubtedly justify the increase in cases and incidence of this disease in Europe.
Current legislation does not provide for any action on air quality in the case of legionellosis and, on the contrary, on the design, operation and maintenance phase of water systems that are the source of Legionella infection in humans. In the case of health centers, the ventilation system should be closed, as a measure to stop the possible entry through the windows of aerosols generated outside in facilities at risk for legionellosis. If the hospital has central air conditioners, the humidification, heating (for heating) and cooling (for cooling) chambers should be monitored, since a failure in these systems could lead to the passage of aerosols possibly contaminated by Legionella into the distribution air of the hospital rooms [ 62 - 67 ].
Aerosol-borne microorganisms of the genus Legionella are a cause of pneumonic and non-pneumonic infections both inside and outside hospitals. Their prevention is focused on avoiding and treating the colonization of water reservoirs from which aerosols that reach the airway of people can be generated .
WHAT ARE THE HEALTH, SOCIAL AND ECONOMIC COSTS OF POLLUTED INDOOR AIR?
Eduardo olier arenas.
In 2013, the World Bank and the University of Washington’s Institute for Health Metrics and Evaluation estimated that indoor air pollution alone led to wealth losses of around $1.5 billion [ 68 ].
There are few studies on the socio-economic effects of indoor air pollution in developing countries. France, however, is one of the countries that have understood the importance of this type of pollution and its harmful social and economic effects. Perhaps not much attention has been paid to this problem because the economic effects of pollution constitute “negative externalities”: an economic concept that is difficult to account for in many cases. As a prelude to what follows, we will say that an economic externality is one in which the costs of producing or consuming a good or service, or the benefits of doing so, are not reflected in market prices. In other words, these are side effects that occur when an economic activity does not take into account the costs or benefits that it itself produces. And, in this case, pollution, being a negative externality, causes economic consequences that are difficult to estimate, as it is difficult to evaluate the corresponding market prices.
Indoor air pollution is a fact that has been little studied in general, since more emphasis and effort is placed on policies aimed at mitigating the effects of climate change and, in particular, the effects produced by greenhouse gases. So much so that the current 750 billion euro Next Generation EU Program, approved by the European Council on July 21, 2020, has been approved by the European Council on July 21, 2020 [ 69 ], The issue of indoor air pollution is a long-standing economic problem that Ronald Coase, winner of the Nobel Prize in Economics, highlighted as early as 1960 when he discussed the harmful effects of certain factories whose emissions were damaging to the health of the population.
The issue of pollution is an old economic problem that Ronald Coase, winner of the Nobel Prize in Economics, brought to light as early as 1960 when he discussed the harmful effects caused by certain factories, whose emissions were damaging the health of the inhabitants of nearby towns and cities [ 70 ]. Coase refuted those economists who sought to solve this problem by taxing polluting industries, since the real problem to be solved — Coase — understood — had to focus on avoiding pollution, not on accepting it by applying a tax treatment; since, in reality, it is a problem related to the social cost of the damage produced, which should consider whether the cost of pollution is greater or lesser than the problem caused by it [ 70 ]. This issue can be extended to all the problems related to the pillars of the welfare state enjoyed by advanced countries, which is none other than the analysis between economic efficiency and the problem of equity between those who pollute and those who suffer such effects [ 71 ].
This is a circumstance that, in general, does not take into account its full dimension, since the problem is usually alleviated with fiscal or financial solutions through the well-known emissions markets created under the Kyoto Agreements [ 72 ]. In what follows, without being exhaustive, we will give some ideas on the socioeconomic problem of indoor air pollution which, in Spain, by the way, has not been an issue that has attracted much attention to date.
The main pollutants in indoor spaces come mainly from three sources: (i) chemical pollutants (volatile organic compounds, nitrogen oxides, carbon monoxide, aromatic hydrocarbons, etc.); (ii) bio-pollutants (molds, dust mites, pets, pollen, cockroaches, etc.); (iii) suspended particles and fibers (asbestos, artificial mineral fibers, inert particles, etc.)[ 73 ]. The philosophy behind this criterion, however, focuses on solving the problem by taxing the supposedly polluting companies, i.e., imposing a tax according to the level of the economic externality produced, which requires knowledge of the type of pollutant and its effects on the environment, in addition to determining the polluting agent. Once again, this mechanism tries to solve pollution problems with new taxes, for which fiscal criteria are imposed with ex-ante criteria, instead of carrying out ex-post analyses, which are necessary to know in detail the undesirable effects of pollution, where they come from and what measures should be taken to avoid them.
With regard to the economic impact of indoor air pollutants, at least two aspects must be considered: (i) the opportunity cost, related to the loss of economic activity due to the illness of workers or, in extreme cases, the loss of human lives, and (ii) the direct cost of pollution on the public or private economy, which is related to the marginal cost that governments or companies have to bear because of pollution; that is, the additional costs that they have to assume due to the polluting event. A circumstance also dealt with by Ronald Coase in his day, which gave rise to the so-called Coase Theorem, according to which, in the absence of monetary transactions, as in the case we are dealing with, private and public costs coincide [ 74 ]; It is understood that the market alone will not be able to accommodate the two extremes, and it will be up to the regulator, i.e., the corresponding government, to provide an equitable solution to the problem, in order to find the optimum point between efficiency and equity, apart from the simple application of new taxes. Figure 3 shows the equity vs. efficiency scheme [ 71 ].
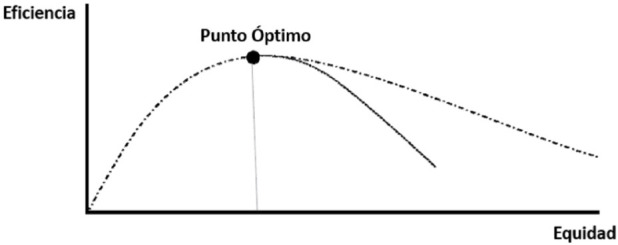
Search for tax equity
One way of expressing the socioeconomic cost produced by indoor air pollution takes the following form for the case of the public costs associated with it:
W = ΔCE + ΔG x (1 + α)
where: W is the socioeconomic cost; ΔCE the variation of costs due to loss of human lives, degradation of quality of life or production losses; (1 + α) the negative impact on public finances; and ΔG the variation of other concepts such as: retirement or disability pensions, investments in research, added health expenses, etc.; with “x” as multiplication sign [ 75 ]. This study, led by Guillaume Boulanger, also shows the health effects of a number of pollutants (benzene, radon, carbon monoxide, tobacco smoke, etc.) in France in 2004: 19,879 deaths, with an impact on morbidity of 26,046 people, and a total cost of 19,443 million euros to the public purse. In addition, a report by the European Parliament [ 76 ] reference a study estimating, for 26 European Union countries, a loss of 700,000 years of “healthy life” due to indoor air pollution [ 77 ], with a distribution of the produced harm by different particles as it is shown in Figure 4 . The risk, as shown here, is greater in the case of microparticles coming from outdoors, so that outdoor pollution is also harmful indoors, with a higher incidence in people suffering from some type of respiratory diseases or dysfunction, both young and old, and, in current times, especially in people suffering from the coronavirus pandemic (COVID-19).
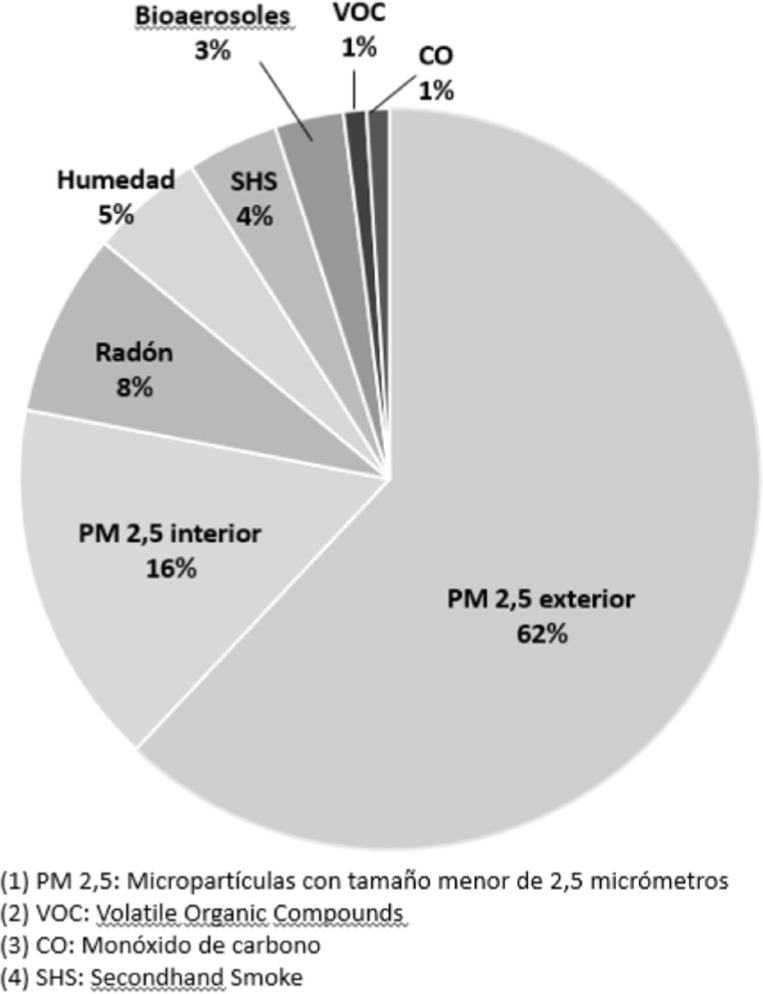
Influence of different particles in interior spaces.
Indoor air pollution is an understudied fact in general, as more emphasis and effort is placed on policies aimed at mitigating the effects of climate change and, in particular, the effects produced by greenhouse gases and outdoor pollution. Indoor air pollution alone leads to wealth losses of around $1.5 billion. In addition to the opportunity cost of lost economic activity due to worker illness or, in extreme cases, loss of human life, there is the direct cost of pollution to the public or private economy, which is related to the marginal cost borne by governments or companies as a result of pollution .
WHAT IS THE RELATIONSHIP BETWEEN AIR POLLUTION AND CLIMATE CHANGE, AND WHAT ARE THE IMPLICATIONS FOR THE HEALTH SECTOR?
Felipe villar álvarez.
Air pollution and climate change are the two main environmental problems. Both are closely related, but they are not the same. Just as the definition of the former has been well defined above, we can say that climate change, according to the WHO, is a statistically significant variation in the mean state of the climate or its variability, persisting over an extended period of time (usually decades or longer). Climate change is due to natural internal processes or external forcings, and to persistent anthropogenic changes in the composition of the atmosphere. The United Nations Framework Convention on Climate Change defines climate change as “a change of climate that is attributed directly or indirectly to human activity that alters the composition of the global atmosphere and that is in addition to natural climate variability observed over comparable time periods”. PM 2.5 can come from all kinds of combustion, such as from automobiles, factories, wood and agricultural burning, or other activities, and can also affect the climate. Primary pollutants such as soot can absorb heat, thereby increasing local temperatures [ 78 ], and secondary aerosols such as sulfate particles cool the climate and contribute to aerosol-cloud interactions [ 79 , 80 ]. Near-surface ozone is another secondary pollutant formed by the interaction of precursor compounds with sunlight, including ultraviolet radiation [ 81 ]. The rate of formation depends on temperature. Because of this, ozone increases on hot, cloudless days [ 82 ]. On the other hand, wind and dry deposition can reduce their levels [ 83 ]. This near-surface ozone formation is the result of chemical reactions that depend on emissions of ozone precursors from natural and anthropogenic sources. The main precursors include several primary and other secondary pollutants such as volatile organic compounds (VOCs), methane (CH 4 ) and carbon monoxide (CO), which react with the hydroxyl radical (OH) to ultimately produce ground-level ozone. In addition, the formation of hydroxyl radicals is associated with CH 4 , another greenhouse gas [ 84 ].
Global warming of the planet is accelerated by the emission of greenhouse gases caused by human activities. The main ones are carbon dioxide (CO 2 ), CH 4 and nitrogen oxide (N 2 O). The two main effects of climate change on air quality are the amplification of atmospheric chemistry and the degradation of air removal processes [ 83 ]. These will affect primary and secondary pollutants. Rising temperatures, with consequent changes in plant metabolism, will alter emissions of VOCs and secondary organic aerosols, leading to changes in secondary particulate matter levels [ 85 ]. Climate change may lead to more forest fires, dust storms and transport of dust particles, which may change the annual average concentrations of PM 2.5 in ± 1 μ g/m 3 [ 81 ].
Climate change and air pollution can affect each other’s health directly or indirectly. Air particles, especially from combustion, and gases such as ozone can increase cardiopulmonary mortality and hospitalizations, and are related to respiratory diseases such as asthma, chronic bronchitis or rhinitism [ 86 , 87 ].
Other diseases associated with air pollution include rheumatic diseases, neurodegenerative diseases, diabetes, premature birth, and cognitive impairment [ 86 , 87 ]. On the other hand, primary and secondary pollutants can drive climate change, which in turn affects public health through, for example, more extreme temperatures [ 88 ]. Secondary pollutants such as ozone can also affect crop yields which, in combination with climate change, can affect food safety and public health [ 89 , 90 ].
The direct impacts of climate change, such as the spread of vector-borne diseases, higher temperatures, droughts, severe storms and floods, as well as the mass migration of climate refugees, have consequences for health, through an increase in infectious, cardiovascular, respiratory, mental or allergic diseases, and even the onset of malnutrition. These will disproportionately affect the most vulnerable and marginalized populations, and will increase in intensity over time [ 91 ].
Each country’s healthcare sector releases greenhouse gases and contributes to carbon emissions through energy consumption, transportation, and the manufacture, use and disposal of products [ 91 ]. The climate footprint of the health sector is equivalent to 4.4% of global net emissions (1.6 gigatons of CO 2 equivalent) [ 92 ]. Emissions emanating directly from health facilities make up 17% of the sector’s global footprint, while indirect emissions from purchased energy sources such as electricity, steam, cooling and heating account for another 12%. The majority of emissions (71%) come from the health sector supply chain [ 91 ].
Air pollution and climate change are closely related and share the same main culprit: the burning of fossil fuels. Finding solutions to reduce air pollution and climate change requires joint actions through clean energy to reduce air emissions, reduce mortality and disease occurrence, and reduce health care costs .
THIRD BLOCK: AMBIENT AIR AS A CAUSE OF HOSPITAL AND HEALTH CENTER-ACQUIRED DISEASE
What do we mean by healthy ambient air in hospitals and healthcare centers.
We could define a healthy air environment in healthcare facilities as one that provides comfortable activity and safe conditions for both patients and workers or visitors [ 93 ].
Comfort and safety criteria will often overlap. Comfort will depend on parameters such as temperature, humidity and air velocity and safety will cover aspects from the point of view of protection against harmful biological, physical or chemical agents.
In the healthcare environment, of all the risks associated with ambient air, and leaving aside the risks common to other workplaces, biological risks are the most important. And these risks will be proportional to the vulnerability of the patients. Therefore, the maintenance of good air quality will in many cases be an important non-pharmacological strategy for the prevention of infections and the maintenance of health [ 94 ].
Heating, ventilation and air conditioning (HVAC) activities, in addition to their primary purpose of providing a comfortable and safe environment for patients and others, play a fundamental role in preventing patient infection [ 95 , 96 ]. The essential functions of HVAC systems include heating and cooling, humidification and dehumidification, ventilation and air distribution, and filtering to remove dust particles and biological contaminants such as fungi, viruses or bacteria from the air. These air conditioning functions are important for the prevention of contamination and cross-contamination, and for the protection of both patients and workers [ 97 ].
Numerous diseases are related to poor air quality management in hospitals. From filamentous fungal infections ( Aspergillus ,...) to the transmission of bacteria ( Enterobacteriaceae , non-fermentative Gram-negative, Gram-positive, Legionella ,...), mycobacteria (tuberculosis,...) or viruses (RSV, varicella, influenza, rhinovirus, coronavirus,...).
Patients with severe immunosuppression, those undergoing surgery, and those housed in Intensive Care Units will be very vulnerable groups of patients to airborne biological agents. Therefore, it will be in the rooms where these patients are housed where air safety conditions must be more stringent.
When we need to create a special protective environment for patients at very high risk of infection, we must ensure that the quality of the ambient air is ultra-clean by means of very high efficiency filtration (High Efficiency Particulate Air filter, or HEPA filters) and by ensuring that the pressure inside the room is positive so that when the doors are opened, air currents entering the room from the potentially contaminated outside are prevented.
On the other hand, we must ensure that patients with airborne infections are housed in controlled environments that prevent contagion to other patients or workers. This is the case of infections caused by microorganisms that can generally be sent to the environment from the respiratory tree of infected patients, and which, depending on the type of vehicle (size of the exhaled particles) and the viability and survival of the agents, can contaminate patients or professionals. In these cases, HVAC systems must be adapted to contain and purify the agents, creating conditions of airtightness, negative pressure, purification and exhaustive air renewal.
The most complex situation occurs when we must accommodate in a protective environment patients who in turn can be infectious for others in which case the HVAC systems must ensure through intermediate chambers between the patient’s room and the corridors, a positive pressure for the patient and in turn positive between the corridor in front of the intermediate chamber.
Another important section in the environmental safety of healthcare facilities is related to airborne physical or chemical noxious agents such as dusts, gases and irritants that must be addressed by measures including containment or elimination of the emitting source, filtration or purification.
Finally, while the mechanism of transmission of infections by contact is the most frequent, that of airborne transmission is more difficult to control, and one where engineering sciences play an important role in limiting the spread of microorganisms.
We understand healthy hospital air to be that which provides comfortable activity and adequate safety conditions for both patients and workers or visitors. The risks of hospital air for patients will be proportional to their vulnerability .
WHAT TYPES OF AMBIENT AIR PROTECTION LEVELS SHOULD BE IN PLACE IN HOSPITALS AND HEALTHCARE FACILITIES? ARE THERE SPECIAL MEASURES TO PREVENT COVID-19?
Gloria cruceta arboles.
If there is a building or space where air quality becomes the main protagonist of our health, it is in hospitals and healthcare centers. Immunosuppressed patients are susceptible to airborne infections from microorganisms (bacteria, fungi, viruses...) that may be common in the general environment, but that can cause nosocomial infection in sick persons, with an often irreversible impact.
The protection of the ambient air in hospitals is achieved through three fundamental means, which are:
1-Ventilation.
2-Filtration.
3-Purification.
The combination of these elements must be studied in function of the patient’s needs required by the patient, the intervention to be performed, or the complementary actions to be carried out.
Ventilation is very important as it dilutes the contaminants, whether chemical or biological, and there are regulations in this regard, in RD 1027/2007, RITE, which categorizes air quality in healthcare centers as IDA 1, which means maximum ventilation.
Filtration is essential to limit the passage of particles, knowing that microorganisms are always suspended in them, it is basic to restrict their propagation in the air. In hospitals there are controlled environment rooms, which, in order to protect the patient, are equipped with high efficiency HEPA filtration, being able to retain up to 99.95% of the particles. These rooms, especially for immunocompromised patients, surgical areas, areas for the preparation of parenteral drugs, etc., should have HEPA filtration and must also have a pressure differential to ensure that the air always goes from the cleanest to the most contaminated area.
Current regulations require that the design of the controlled environment areas be adapted to the needs of control and protection, establishing a classification, according to the danger that exists for the patient to be contaminated, from a slight risk to a very high risk. Likewise, It also establishes the obligation of annual validation and qualification of these rooms, contained in the UNE 171340:2020 Standard.
The combination of these elements and other purification elements, such as photocatalysis, electrostatic filtration and photocatalysis, electrostatic filtration or UV lamps, increase the efficiency of the systems and installations, to the point of providing systems and installations air free of microorganisms, to the treated areas in healthcare facilities [ 98 - 104 ].
In the case of SARS CoV-2, it is another biological agent that can be transmitted through airborne aerosols and, therefore, as with the other microorganisms, the three aforementioned protection mechanisms mentioned above are applicable to it [ 105 - 109 ].
Antibiotics and corticosteroids are frequently used in patients with COVID, and a new form of invasive aspergillosis called COVID-Associated Pulmonary Aspergillosis (CAPA) has been described [ 110 - 113 ]. It is recommended in some of these patients, isolation from adjacent areas and the use of supportive air purification equipment with high-efficiency HEPA filters, ultraviolet radiation lamps, and electrostatic filtration.
Immunosuppressed patients admitted to hospitals are susceptible to contracting infections through the air, by different microorganisms (bacteria, fungi, viruses...) that can be common in the general environment, but that can produce in very sick people a nosocomial infection, with an impact, in many occasions irreversible .
The protection of the ambient air in hospitals is achieved through three fundamental ventilation, filtration and purification .
WHAT ARE THE MAIN AIRBORNE FUNGI THAT ARE POTENTIALLY PATHOGENIC TO HUMAN HEALTH?
Invasive mycoses are serious opportunistic infections caused by fungi in hospitalized patients with varying degrees of immunosuppression. In general terms, the fungal kingdom is composed of yeasts and filamentous fungi or molds, the latter group being a series of species that multiply and proliferate by means of spores. These spores are airborne, and their accidental inhalation by high-risk patients can trigger the development of invasive mycoses that generally affect the lung locally
and in some cases spread to other deep organs. This phenomenon is especially relevant in the hospital environment, which is where patients reside at times of increased risk for the development of invasive mycoses [ 114 - 117 ].
Considering the air as its natural vehicle, any spore-producing filamentous fungal species can be detected in the air. Without protective measures, the spores present in the air of the hospital environment will be a reflection of what is occurring in the street air [ 118 , 119 ].
It is estimated that there are about 4 million species of fungi in nature, although only a few dozen are of clinical interest, being the species belonging to the genera Aspergillus , species of Mucorales, Fusarium, Scedosporium and Pseudoallescheria , the most relevant filamentous fungi. Aspergillus fumigatus is by far the filamentous fungus causing the greatest number of serious mycoses, known as invasive aspergillosis.
The main filamentous fungi present in ambient air and capable of causing invasive mycoses in hospitalized immunocompromised patients are the various species belonging to the genera Aspergillus, Mucorales, Fusarium, Scedosporium and Pseudoallescheria .
WHAT PARAMETERS SHOULD BE MEASURED AND WHERE IN HOSPITALS AND HEALTHCARE CENTERS TO DEFINE THE QUALITY OF THEIR AMBIENT AIR? WHAT DOES OUR LEGISLATION SAY? IS IT HOMOGENEOUS IN ALL THE AUTONOMOUS COMMUNITIES?
There is a relationship between the acquisition of invasive mycoses and the presence of filamentous fungal spores in the patient’s environment. Indirect data suggest this relationship come from the disproportionate occurrence of aspergillosis cases in the form of hospital outbreaks when activities leading to high levels of spores in the air, such as renovation work, take place near areas where high-risk patients reside [ 120 ]. Similarly, the location of these same patients in areas equipped with high-efficiency HEPA protection is associated with fewer cases [ 121 ]. The most direct and clear evidence comes from the demonstration by means of molecular typing of the presence of the microorganism causing the infection in the air of the patient’s environment [ 122 , 123 ].
Particulate counters are a quick and simple method to monitor the presence of airborne particles, but they simply alert of the presence of airborne particles, without discriminating between fungal spores or other particles (dust, pollen, etc.). For the specific detection of filamentous fungal spores, it is necessary to resort to the culture of air samples, which involves the aspiration of specific volumes of air and their subsequent culture in special media, identification, and calculation of spores per cubic meter of air sampled (CFU/m 3 ). The spore load tolerated in the air will depend on the level of protection of the sampled area. While in street air spore levels of up to 10 5 CFU/m 3 are accepted, in unprotected areas of the hospital environment the presence of >25 CFU/m 3 has been defined as a risk threshold, while in those protected with HEPA filters the fungal levels should be 0 CFU/m 3 [ 124 ]. The regulations applicable to the hospital setting have not been very specific and are based on guides developed specifically for the design of operating rooms or of wider application in the hospital (Guía Práctica para el Diseño y Mantenimiento de la climatización en Quirófanos del Insalud; 1996 and Guía INSALUD 99 Verificación de Bioseguridad ambiental frente a hongos oportunistas; 1999). Therefore, in the absence of specific regulations, the centers where this type of sampling is carried out base their policy on the recommendations of scientific documents. Current scientific recommendations recommend air monitoring in rooms/protected areas, operating rooms, critical-burn patient units and oncohematology units [ 124 ]. CDC (Centers for Diseases Control and Prevention) recommendations recommend hospital air sampling both during periods of high risk due to construction work and periodic sampling to determine air quality, the effectiveness of barrier measures, or the condition of air conditioning systems [ 62 ]. Hospital centers such as the Gregorio Marañón Hospital apply a monthly sampling policy in protected environment areas, quarterly sampling in unprotected environment areas, and whenever there are high risk activities (construction sites) or within a hospital outbreak of invasive aspergillosis. This evaluates the integrity of filters, the detection of unknown spore niches, detects abnormally high levels of spores, and generates awareness of the problem among all hospital personnel responsible for air quality.
Hospital ambient air quality is usually measured generally by particle counters and more specifically by counting per cubic meter the number of filamentous fungal spores. Acceptable quantities are different in different environments and in the case of operating rooms and neutropenic patient rooms a zero count is intended. Legislation on this aspect is not common either internationally or in Spain .
WHAT ARE THE MAIN DISEASES THAT CAN BE ACQUIRED IN A HOSPITAL DUE TO THE PRESENCE OF INADEQUATE AMBIENT AIR?
Patricia muñoz garcía.
Air is the medium through which a large number of infections are acquired, both inside and outside hospitals. This risk is especially high in hospitals and healthcare centers where fragile patients with a high risk of infection are concentrated, such as immunocompromised patients, elderly, operated, intubated patients, etc. These patients can acquire an infection either because of a general hospital air quality problem, to which this review is dedicated, or because of a specific failure of isolation and prevention of transmission of microorganisms from another patient, a visitor or a sick worker. Examples of these latter situations are the nosocomial transmission of respiratory infections such as influenza, chickenpox, respiratory syncytial virus, or even COVID-19 [ 113 , 125 , 126 ]. These cases must be recognized and avoided, since they cause significant morbidity and mortality.
However, as we were saying, the subject that concerns us are the diseases acquired by poor care of the aeration systems, which can constitute a hospital responsibility. Although this problem can cause different infections, the most paradigmatic is invasive aspergillosis, the most important clinical characteristics of which I will briefly describe. Aspergillosis is the name given to diseases caused by filamentous fungi of the genus Aspergillus, which is a ubiquitous microorganism that can be isolated from soil and dust and is universally distributed. It is characterized by producing small conidia, which, given their size, can be easily inhaled reaching the lung and paranasal sinuses, from where they can spread to any organ. The infection can also be acquired by direct inoculation in operated patients, when Aspergillus is in the air of an operating room [ 127 ].
Acute invasive aspergillosis usually affects immunocom-promised patients, although the types of patients affected are becoming increasingly diverse [ 128 ]. The most frequent underlying diseases are hematological diseases (leukemia, lymphoma, progenitor transplantation), which account for almost 60% of cases in some series [ 129 ]. It is also described in other immunocompromised patients (solid organ transplants, HIV, high doses of steroids, solid tumors, etc.) and in patients with fulminant hepatic failure, advanced cirrhotics, critically mal-nourished patients, major burns, etc.
As the microorganism penetrates through the air, the most frequent invasive clinical forms in immunocompromised patients are pulmonary aspergillosis and rhinosinusitis. Less frequent are airway aspergillosis (obstructive bronchial, invasive tracheobronchitis, ulcerative or pseudomembranous), primary cutaneous, central nervous system (CNS) and disseminated aspergillosis. The invasiveness of the fungus is due to its great angioinvasive capacity and it can spread both by contiguity and by hematogenous route to organs distant from the primary infection, such as the CNS, liver, spleen, kidneys, prostate, etc. [ 130 ].
Pulmonary aspergillosis may begin asymptomatically and be a radiological finding or be accompanied by cough, fever, dyspnea, chest pain and hemoptysis. It is advisable to perform whenever possible a high-resolution chest CT scan, which usually provides more data than plain radiography and is a requirement in international diagnostic criteria [ 131 ]. The radiological manifestations considered suggestive of pulmonary aspergillosis are nodular lesions with or without a surrounding attenuation halo - halo sign (early), ca vitations and the air meniscus or crescent sign (later). However, aspergillosis can have other radiological presentations, especially in populations other than neutropenic patients. Early treatment (patients with halo or crescent sign) has been associated with longer survival than when treatment is initiated already with cavitation.
Tracheobronchial forms are more frequent in lung transplant recipients. Accepted clinical criteria require fibrobronchoscopy in which tracheobronchial ulcers, nodules, pseudomembranes, plaques or eschar should be observed. The diagnosis of sinusitis requires its radiological demonstration together with at least one of the following clinical data: acute localized pain sometimes radiating to the eye, nasal ulcer with black eschar or paranasal extension of the infection beyond the bony barriers and sometimes affecting the orbit.
The forms of invasive aspergillosis that appear in nonimmunosuppressed patients associated with tissue damage, surgery or presence of foreign material are also extraordinarily important due to their clinical and legal significance. Some examples are post-surgical or post-traumatic keratitis or endophthalmitis, skin infections in burn patients, wound or surgical area infections, and those related to the placement of prosthetic valves, dialysis or central venous catheters, pacemakers, etc. [ 132 - 134 ].
Mortality of this infection is very high (around 60%), reaching more than 80% in very immunosuppressed patients, with CNS involvement or disseminated infection. At present, somewhat more satisfactory figures are obtained partly due to earlier detection and treatment with better tolerated and highly effective drugs.
The paradigm of infection conveyed by poor quality ambient air in a hospital is Invasive Pulmonary Aspergillosis. It occurs in very vulnerable patients and with relatively small exposures, as in the case of neutropenic onco-haematological patients. On the other hand, it can occur in immunocompetent patients with massive exposures or by direct exposure of deep tissues and organs to ambient air, as in the case of infections acquired during extracorporeal surgery .
CAN ZERO INCIDENCE OF HOSPITAL-ACQUIRED INVASIVE MYCOSES BE ACHIEVED?
The ambition to achieve zero incidence in various nosocomial infections is embodied in well-structured and ambitious campaigns, which have significantly reduced the incidence of catheter-related bacteremia, pneumonia in mechanically ventilated patients, surgical wound infections and even infections due to multi-resistant bacteria. It is therefore legitimate and very pertinent to try to approach zero incidence of hospital-acquired invasive mycoses.
As with many other infections, invasive mycoses diagnosed in the hospital may have been acquired in the community (food, plants, unfiltered air, dust) or in the hospital, and within the hospital, either in the area where the patient is admitted or during their movements around the center for tests or interventions. It is therefore difficult to establish the place of acquisition of aspergillosis [ 135 ]. On the other hand, there are many environmental factors (climate, wind, rain, vegetation, etc.) that can influence an increase in the number of specific cases. In addition, the problem is exacerbated by the fact that the incubation period of the disease is not well defined and depends on the immune status of the patient, the route of acquisition and the concentration of spores to which the patient has been exposed. We describe a well-documented case in which the time of infection could be determined and establish an incubation period of 15-20 days for our patient [ 122 ].
Despite these considerations and difficulties, it is imperative to try to detect hospital-acquired cases and prevent them through the strict implementation of general and specific measures. General measures include, among others, the following recommendations: Transfer of high-risk patients to a protected area distant from the construction or remodeling site and avoid exposure to plants, showers, contaminated food, etc; Keep doors and windows closed in areas with high-risk patients; Use of N95 masks by high-risk patients when leaving protected areas; Optimal isolation of construction sites with impermeable barriers; Reducing traffic through affected areas; Routine environmental measurements and in case of suspected nosocomial episode, to ensure that they do not exceed the levels allowed in each area; Optimal cleaning of surfaces with wet wipes and immediate removal of debris. Careful recording of filter changes; Follow-up of possible infections in patients at risk of IA; Regular meetings with all involved (infectious diseases, microbiology, preventive, hospital management, affected services, engineering) [ 124 , 136 - 140 ].
Specific measures include the administration of antifungal prophylaxis to patients at risk. This measure has to be directed only to patients with a very high risk, either because of their baseline conditions, or because they have been exposed to high levels of spores in the hospital, given that we are going to administer potentially toxic drugs to people who do not yet have the disease. But it is worth it, because these measures work.
As an example, I will give our experience with aspergillosis in a cardiac transplant program. In this population group the recommendation was to give prophylaxis to all patients, but we observed that, as long as there were no massive environmental exposures, only patients with certain risk factors suffered from aspergillosis. We defined which factors increased the risk and the duration of the increased risk in relation to each of the factors. With this we designed a prevention protocol in which we only administered prophylaxis to that particular group of patients and only for the minimum time necessary. In this way we managed to reduce the incidence of aspergillosis in our transplant program to zero for several years, with a very important impact on the overall survival of our patients and with good tolerance [ 141 , 142 ] . Figure 5 shows that in several years of the program there was not a single case, neither nosocomial nor community. Subsequently, a new nosocomial airborne contamination led to the appearance of nosocomial cases [ 132 ], which later disappeared again.
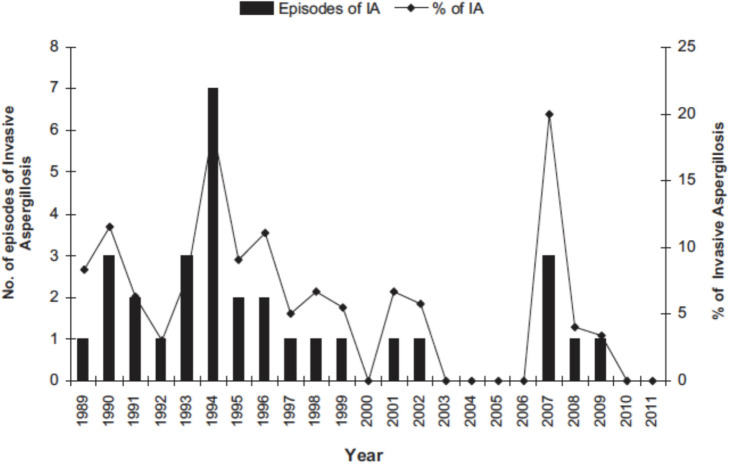
Annual distribution of cases of invasive aspergillosis in heart transplant recipients.
It is necessary to insist on the need to be rigorous and exquisite in the observance of all prevention recommendations, including the measurement of spores in hospital air. We must be exemplary in the observance of the law on “zero tolerance” of spores in protected air (operating rooms, hematology) and not exceeding reasonable levels (25 ufc/m 3 ) in unprotected air [ 143 ]. This extraordinary care will mean that, unlike in many centers, we will not have to regret cases acquired in the operating room, which often complicate cardiac surgeries and lead to high mortality. Finally, if the episode could not be prevented, it is necessary to diagnose and treat it promptly and record it for subsequent analysis by all parties involved.
Zero incidence of systemic mycoses in the hospital environment should be a reasonable goal and involves the implementation of a series of measures to protect the ambient air and sometimes also antifungal prophylaxis measures. We are not aware of the stable achievement of this objective, but the measures that have been tried have been associated with a clear decrease in the number of episodes .
WHAT IS THE CURRENT SYSTEM FOR MEASURING CONTAMINANTS, IS IT EFFECTIVE, AND WHAT MEASURES ARE MOST EFFECTIVE TO ENSURE GREATER SAFETY AND PREVENT DISEASE IN HOSPITALS AND HEALTH CENTERS?
The Ministry for Ecological Transition and Demographic Challenge (MITECO) is the body in charge of collecting all the information and making an evaluation report annually regarding the values recorded in the environmental pollutant monitoring stations in each Autonomous Community (C.A.). This information is evaluated in relation to the legislation in force in Spain (Royal Decree 102/2011) which was constituted from the Directive 2008/50/EC on ambient air quality and a cleaner atmosphere in Europe. The evaluation is carried out according to the following criteria: the classification of the zone in relation to pollutant levels is determined by the highest value of each pollutant detected in the stations belonging to the zone [ 144 , 145 ].
The legislation establishes limit values that all Autonomous Regions must comply with in their air quality measurement zones. In the event that any Autonomous Region exceeds the legal limit values for a certain pollutant, it must take the necessary measures to reduce it to a permitted level. In addition, the legislation sets national target values for all Autonomous Regions to take measures and achieve a reduction of certain pollutants (PM 2.5 , O 3 , Cd...) for the specified year [ 146 ].
The World Health Organization (WHO) conducts global and European studies to analyze the impact of pollution on the health of the population. According to the results obtained, it is estimated that air pollution causes 3.2% of the world’s illnesses and some 3.1 million premature deaths per year. The effects of pollution on health are mainly related to respiratory and cardiovascular diseases and cancer of the respiratory system. In Spain, the National Center for Environmental Health (CNSA) is the body in charge of controlling air pollution and carrying out studies to contribute to the protection of people’s health.
Due to the great impact of air pollution on people’s health, healthcare centers, hospitals and health centers must adopt measures to control the indoor air quality level (IDA) of the centers. The air circulating inside healthcare facilities can be loaded with both small particles and gases from outside air and infectious bacteria and viruses exhaled by patients suffering from respiratory infections in the facility itself. Air conditioning and air ducts in healthcare facilities are essential elements for controlling the quality of the air that enters the facility and circulates within the hospital. In the case of air conditioning, the air coming from outside is filtered and acclimatized in the Air Handling Units (AHUs) and circulates through the air ducts to the different rooms. In the most sensitive areas of hospitals where the air quality must be optimal, i.e. in operating theaters and controlled environment rooms, current legislation regarding air conditioning requires compliance with certain requirements: a number of filtration stages, the application of filters with a high level of efficiency (HEPA filters), a permitted microorganism concentration and a minimum number of air renewals per hour.
In the rest of the hospital spaces, consultations, bedrooms, meeting rooms, general services, etc., less demanding requirements must be met in terms of air quality. From the point of view of the facilities, there are a series of important measures to be considered and adopted for the control of pollution in healthcare centers, as well as the use of the Air Treatment Units (AHU) and their maintenance, i.e. cleaning of the air conditioning units and air distribution ducts of the air driven by the AHUs, replacement of pre-filters and medium and high efficiency filters and checking the correct operation of the air conditioning system. In addition, continuous air renewal in all indoor spaces and window openings for supplementary ventilation are effective measures to reduce the transmission of respiratory infections.
The most effective measures to ensure the quality of hospital ambient air is the establishment of filters in areas of maximum risk and for the protection of the most vulnerable patients .
WHAT ROLE CAN THE MEDIA PLAY IN THE DISSEMINATION AND AWARENESS OF THE GENERAL PUBLIC ABOUT THE PROBLEM OF AMBIENT AIR QUALITY AND IN PARTICULAR ABOUT PEOPLE WITH SOME TYPE OF RESPIRATORY DISEASE?
Javier tovar garcía.
Having established the importance and relevance of this problem for the present and future health of citizens, as well as its enormous repercussions on the sustainability of health-care systems, we point out a group of considerations on the role that the media and journalism can and should play to mitigate these considerable effects and risks.
The media have a social responsibility to develop through good informative practices, distribution and dissemination capacity to reach the population, rigor and truthfulness of the contents and informative work to inform about the relationship between Health and Environment.
The role of the media in raising public awareness in order to value both the defense of health and a healthy environment is a crucial and essential part of their tasks.
Both health and environmental issues have acquired enormous importance for decades in the general and specialized media, beyond the very intense and specific media impact that the COVID-19 pandemic has generated since March 2020.
The conjunction of these two factors, preservation of a sustainable environment (in this case focused on achieving clean air) and the defense of health and well-being as a citizen’s right, already has a certain presence in the media through news, reports, reports, debates, interviews and other types of journalistic content.
The Health/Sanitation and Environment sections occupy places in the newsrooms, although not with the resources and people that society demands; in addition, these departments have seen their staffs reduced as a result of the economic crisis that, since 2008, affected the media, both in the loss of revenue, the effects of the technological revolution and the bankruptcy of the business model.
It is necessary that, in the organization, structure and planing of media content strategies, the Environment and Health sections be strengthened and move towards greater coordination in order to offer joint informative production works that link and connect, with greater depth and breadth, the binomial Health/Environment.
In my opinion, the media have among their informative tasks to expose, both from the news and from the dissemination, rigorous, complete and contrasted, clear and truthful contents, of the reality that focuses and surrounds environmental pollution and its effects on health.
Issues, among others, such as environmental and health policies, and the connection between them; the denunciation of polluting situations of risk to health; the opinion of experts on this casuistry; the work, research and reports of both public and private organizations and institutions; giving a voice to those who suffer most directly from these problems; and other contents of social relevance, with specifics, examples, cases and stories that show and demonstrate the damage to health.
They must also complement the contents generated by the actors in the sector with their own initiative to offer quality information to society which, in turn, helps to alleviate the hoaxes and misinformation that are also produced in this area.
The protection of those who are especially harmed by air pollution, such as children, the elderly or people with respiratory diseases, must involve an added effort through content that gives visibility to reprehensible situations, measures or actions.
While it is true that the issue at hand, unlike other social or health problems, does not remain relegated or cornered in the media, I believe it is the responsibility of the media to increase its presence in prominent places on the journalistic agenda and in information showcases.
In addition, the media must be demanding in monitoring the actions of public authorities on the risks of pollution and its effect on health; monitoring compliance with standards and the strategies of industry and companies to collaborate in cleaner air, both in public and private spaces, workplaces, academics, hospitals or health centers, to give some examples.
It is also the role of the media to inject awareness and responsibility in citizens so that they commit, within the scope of their actions and decisions, to achieve clean air in homes and cities.
The media must help to get out of the certain social numbness that leads the citizenship not to be really aware of the enormous health risks of breathing, day after day, unhealthy air that prevents our organism from functioning in a healthy way, and that acts as a kind of invisible killer that is difficult to detect and control .
WHAT ETHICAL ASPECTS WOULD YOU HIGHLIGHT? WHAT REFLECTIONS FROM THE PERSPECTIVE OF ETHICS ARE RAISED IN THIS PANDEMIC?
Diego gracia guillén.
The current pandemic is new not only because it is produced by an agent different from all those known to date, but also because it is posing a new and unprecedented challenge to the health system. The latter was prepared to deal with epidemics of short duration, sudden onset and rapid end. In fact, that is what the term “epidemic” means. Dêmos is the Greek word for population, and epí is a prefix meaning over or through. To the essence of epidemic diseases belongs that they are transient and usually brief. In this they differ from endemic diseases, those in which the disease remains in a population for very long periods of time, reaching a certain degree of equilibrium between the germ and the populations it affects. The paradigmatic example of this is malaria, which has been so endemic in certain areas of the planet that its inhabitants have ended up developing certain genetic mutations that allow it to coexist with the parasite, as is the case of the modification of the hemoglobin cell that protects against malaria, even though it produces another disease, sickle cell anemia.
Epidemic diseases are characterized by their great aggressiveness, so that they affect very high percentages of the population, killing a large number of people and immunizing the rest. The immunity acquired during the epidemic prevents the germ from finding a place to reproduce, resulting in its disappearance.
All this is well known in medicine and something for which health systems, and with them advanced societies in general, are prepared. Crises are acute situations that require special measures, not only in health care but also in politics, economics, etc. The latter, for example, are aimed at maintaining economic activity by means of public subsidies to private companies and to workers who lose their jobs during the quarantine period, which in epidemics is, by definition, supposed to be short.
The current epidemic has two characteristics that make it peculiar. Firstly, it is a global epidemic, since it is the first, or one of the first, of the so-called “era of globalization” in which we find ourselves. The second characteristic is that it is lasting much longer than a classic epidemic. To such an extent that it is becoming so prolonged that it is beginning to have features more typical of endemics. This is something for which no one was prepared, neither the health system nor economic theory. When a pandemic begins to present symptoms typical of endemic diseases, as is the case in the present one, the social system as a whole enters into crisis. It was assumed that the advances in science, and more specifically in medicine, made the emergence of a phenomenon such as the one described impossible. As a result, what has happened has come as a surprise to everyone, and not exactly a pleasant one.
Medicine has played a fundamental role in the chronification of this epidemic. Left to its natural course, this disease would have very quickly infected a large part of the world’s population, and after killing a certain percentage and immunizing the rest, it would have disappeared. That is the natural history of an epidemic disease. Chronification is the consequence of the preventive measures put in place by the political authorities in application of the principles of the preventivists. These measures undoubtedly save many lives, but at the price of delaying the immunization of the population, which is thus susceptible to infection for much longer, until all or most of the population is immunized, or until all or most of them are artificially vaccinated. The problem is that, in a pandemic, immunization has to reach all or most of the inhabitants of the earth, which poses all kinds of challenges for which our society is at present poorly and ill-prepared. The big question is whether the lessons learned during this crisis by the social system as a whole, and particularly by the health system, will serve to correct the enormous number of dysfunctions identified, or not. And this at all levels, from the local to the global.
The return to the “new normal” has become a slogan. Nothing could be more dangerous than this. If there is one thing we have to learn from this crisis, it is that we cannot go back to the past, so that this pandemic passes like a bad dream. We cannot go back to the past, because that will mean that we have learned nothing from this, which will leave the problems unresolved. This is not just about the profound reforms that the healthcare system requires. If what we are talking about is hygiene and public health, then many things have to change in people’s habits and in the culture of society. Epidemic diseases are due to the Darwinian principle of the struggle for life of the different animal species, but they are also due to the disruption of ecological balances. Historical epidemiology is a good witness to this cause. And the belief, so widespread today, that the human being is the king of creation and that everything else is at his service, so that he can use and abuse nature as he pleases, is a very serious error. Whoever does not treat nature, even inanimate nature, with respect, there is no reason to think that he will treat human beings with respect. And what is said about people is also true for companies and governments.
This crisis must be understood as a first warning that the path humanity is following is not correct, that it needs to be rectified, and that this must be rapid and profound. Otherwise, the warnings will follow one after the other, and they will become more and more serious.
Ethics is the study of the correctness or incorrectness of the habits and customs of human beings. The present health crisis is not a mere fortuitous event, but a consequence of the way in which human beings are depredating nature and altering its equilibrium. It is necessary to promote a new culture of respect for nature and its balances, if only because it is the environment in which human life, our own life, is possible. In the face of a predatory culture, it is necessary to promote another based on respect and the maintenance of equilibrium. If this is not done, this pandemic will have been only a first warning, after which others, probably more serious, will follow .
TRANSPARENCY DECLARATION
For transparency purposes, we inform you that GSK has collaborated in the financing of this publication. Its contents reflect the authors’ own opinions, criteria, conclusions and/ or findings, which may not necessarily coincide with those of GSK. GSK always recommends the use of its products in accordance with the data sheet approved by the health authorities.
- 1. Pope CA, 3rd, Ezzati M, Dockery DW. Fine particulate air pollution and life expectancies in the United States: the role of influential observations. J Air Waste Manag Assoc. 2013;63(2):129-32. DOI: 10.1080/10962247.2013.760353. [ DOI ] [ PubMed ] [ Google Scholar ]
- 2. Pope CA, 3rd. Air pollution and health-good news and bad. N Engl J Med. 2004;351(11):1132-4. DOI: 10.1056/NEJMe048182. [ DOI ] [ PubMed ] [ Google Scholar ]
- 3. Liu C, Chen R, Sera F, Vicedo-Cabrera AM, Guo Y, Tong S, et al. Ambient Particulate Air Pollution and Daily Mortality in 652 Cities. N Engl J Med. 2019;381(8):705-15. DOI: 10.1056/NEJMoa1817364. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 4. European Enviroment Agency . Air quality in Europe- 2020 report.. Disponible en https://www.eeaeuropaeu/publications/air-quality-in-europe-2020-report (Access April 20, 2021). 2020.
- 5. Beelen R, Raaschou-Nielsen O, Stafoggia M, Andersen ZJ, Weinmayr G, Hoffmann B, et al. Effects of long-term exposure to air pollution on natural-cause mortality: an analysis of 22 European cohorts within the multicentre ESCAPE project. Lancet. 2014;383(9919):785-95. DOI: 10.1016/s0140-6736(13)62158-3 [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Zhang Z, Zeng Y, Zheng N, Luo L, Xiao H, Xiao H. Fossil fuel-related emissions were the major source of NH(3) pollution in urban cities of northern China in the autumn of 2017. Environ Pollut. 2020;256:113428. DOI: 10.1016/j.envpol.2019.113428 [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. European Environment Agency . Air quality in Europe — 2020. Report 09/2020. 164 pp. Available at: https://www.eeaeuropaeu/publications/air-quality-in-europe-2020-report . 2020. [ Google Scholar ]
- 8. Querol X. Alcance y propuestas de actuación de los planes de mejora de la calidad del aire. 2018. In: X. Q, editor. La calidad del aire en las ciudades Un reto mundial Madrid: Fundación Naturgy, 147-166. https://www.fundacionnaturgy.org/publicacion/libro-la-calidaddel-aire-las-ciudades-reto-mundial/ ; [ Google Scholar ]
- 9. AIRUSE . Medidas para la mejora de la calidad del aire urbano. 2018. AIRUSE-LIFE+, AXA-Foundation http://www.cleanaircitiesnet/es/
- 10. Monks PS, Archibald AT, Colette A, Cooper O, Coyle M, Derwent R, et al. Tropospheric ozone and its precursors from the urban to the global scale from air quality to short-lived climate forcer. Atmos Chem Phys. 2015; 15:8889–973. [ Google Scholar ]
- 11. Millán MM, Sanz MJ, Salvador R, Mantilla E. Atmospheric dynamics and ozone cycles related to nitrogen deposition in the western Mediterranean. Environ Pollut. 2002;118(2):167-86. DOI: 10.1016/s0269-7491(01)00311-6. [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. World Health Organization . 9 out of 10 people worldwide breathe polluted air, but more countries are taking action. 2018. Available at: https://www.whoint/news/item/02-05-2018-9-out-of-10-people-worldwide-breathe-polluted-air-but-more-countries-are-taking-action .
- 13. Straif K, Cohen A, Samet J. IARC Scientific Publication 161. 2013. http://publicationsiarcfr/Book-And-Report-Series/Iarc-Scientific-Publications/Air-Pollution-And-Cancer-2013 .
- 14. Schmidt CW. Air Pollution and Breast Cancer in Postmenopausal Women: Evidence across Cohorts. Environ Health Perspect. 2018;126(3):34001. DOI: 10.1289/ehp3200. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 15. Wong CM, Tsang H, Lai HK, Thomas GN, Lam KB, Chan KP, et al. Cancer Mortality Risks from Long-term Exposure to Ambient Fine Particle. Cancer Epidemiol Biomarkers Prev. 2016;25(5):839-45. DOI: 10.1158/1055-9965.Epi-15-0626. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 16. Alderete TL, Chen Z, Toledo-Corral CM, Contreras ZA, Kim JS, Habre R, et al. Ambient and Traffic-Related Air Pollution Exposures as Novel Risk Factors for Metabolic Dysfunction and Type 2 Diabetes. Curr Epidemiol Rep. 2018;5(2):79-91. DOI: 10.1007/s40471-018-0140-5. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 17. Vert C, Sánchez-Benavides G, Martínez D, Gotsens X, Gramunt N, Cirach M, et al. Effect of long-term exposure to air pollution on anxiety and depression in adults: A cross-sectional study. Int J Hyg Environ Health. 2017;220(6):1074-80. DOI: 10.1016/j.ijheh.2017.06.009. [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Hu CY, Fang Y, Li FL, Dong B, Hua XG, Jiang W, et al. Association between ambient air pollution and Parkinson’s disease: Systematic review and meta-analysis. Environ Res. 2019;168:448-59. DOI: 10.1016/j.envres.2018.10.008. [ DOI ] [ PubMed ] [ Google Scholar ]
- 19. Culqui DR, Linares C, Ortiz C, Carmona R, Díaz J. Association between environmental factors and emergency hospital admissions due to Alzheimer’s disease in Madrid. Sci Total Environ. 2017;592:451-7. DOI: 10.1016/j.scitotenv.2017.03.089. [ DOI ] [ PubMed ] [ Google Scholar ]
- 20. Weiss B, Landrigan PJ. The developing brain and the environment: an introduction. Environ Health Perspect. 2000;108 Suppl 3(Suppl 3):373-4. DOI: 10.1289/ehp.00108s3373. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 21. Bruckner JV. Differences in sensitivity of children and adults to chemical toxicity: the NAS panel report. Regul Toxicol Pharmacol. 2000;31(3):280-5. DOI: 10.1006/rtph.2000.1393. [ DOI ] [ PubMed ] [ Google Scholar ]
- 22. Pedersen M, Giorgis-Allemand L, Bernard C, Aguilera I, Andersen AM, Ballester F, et al. Ambient air pollution and low birthweight: a European cohort study (ESCAPE). Lancet Respir Med. 2013;1(9):695-704. DOI: 10.1016/s2213-2600(13)70192-9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 23. Arroyo V, Díaz J, Ortiz C, Carmona R, Sáez M, Linares C. Short term effect of air pollution, noise and heat waves on preterm births in Madrid (Spain). Environ Res. 2016;145:162-8. DOI: 10.1016/j.envres.2015.11.034. [ DOI ] [ PubMed ] [ Google Scholar ]
- 24. Acción. Ee. [Informe] Efectos de la crisis de la COVID-19 en la calidad del aire urbano en España 10/12/2020 | 2020. Informes. Available at: https://www.ecologistasenaccionorg/140177/informeefectos-de-la-crisis-de-la-covid-19-en-la-calidad-del-aire-urbano-en-espana/ .
- 25. American Chemical Society (ACS) . Air pollutants could boost potency of common airborne allergens. 2015. Available at:: https://www.acsorg/content/acs/en/pressroom/newsreleases/2015/march/air-pollutants-could-boostpotency-of-common-airborne-allergenshtml .
- 26. Setti L, Passarini F, De Gennaro G, Barbieri P, Licen S, Perrone MG, et al. Potential role of particulate matter in the spreading of COVID-19 in Northern Italy: first observational study based on initial epidemic diffusion. BMJ Open. 2020;10(9):e039338. DOI: 10.1136/bmjopen-2020-039338. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 27. Setti L, Passarini F, De Gennaro G, Barbieri P, Pallavicini A, Ruscio M, et al. Searching for SARS-COV-2 on Particulate Matter: A Possible Early Indicator of COVID-19 Epidemic Recurrence. Int J Environ Res Public Health. 2020;17(9). DOI: 10.3390/ijerph17092986. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 28. Setti L, Passarini F, De Gennaro G, Barbieri P, Perrone MG, Borelli M, et al. SARS-Cov-2RNA found on particulate matter of Bergamo in Northern Italy: First evidence. Environ Res. 2020;188:109754. DOI: 10.1016/j.envres.2020.109754. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 29. World Health Organization . Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). 2020. Available at: https://www.whoint/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf
- 30. Linares C, Sánchez-Martínez G, J. D.. ¿Influyen el clima y la contaminación atmosférica en la transmisión e incidencia de la nueva enfermedad COVID19?. . Revista DIECISIETE. 2020; Nº 3. Madrid. ISSN DOI: 10.36852/2695-4427_2020_03.03. [ DOI ] [ Google Scholar ]
- 31. Subdirección General de Aire Limpio y Sostenibilidad Industrial del Ministerio para la Transición Ecológica y el Reto Demográfico. SnGdALySIdMplTnEgyeR. Informe de vigilancia de la contaminación de fondo 2019. Available at: https://www.mitecogobes/images/es/vigilanciacontaminacionfondo2019-emep_tcm30-510613.pdf .
- 32. Querol X. La calidad del aire en las ciudades. Un reto mundial. Fundación gas natural fenosa 2018; Available at: http://www.fundacionnaturgy.org/wp-content/uploads/2018/06/calidad-del-airereto-mundial.pdf .
- 33. Gobierno de Aragón. Calidad del aire en Aragón. Zonificación de la calidad del aire en la Comunidad de Aragón. 2020. Available at: https://aragonairearagones/zonificacion .
- 34. Ministerio para la Transición Ecológica y el Reto Demográfico . Ín-dice de la calidad del aire en España. 2021. Available at: https://www.miteco.gob.es/es/calidad-y-evaluacion-ambiental/temas/atmosfera-y-calidad-del-aire/calidad-del-aire/ICA.aspx .
- 35. Dirección General de Biodiversidad y Calidad Ambiental . I Programa Nacional de Control de la Contaminación Atmosférica . 2019. Available at: https://ec.europa.eu/environment/air/pdf/reduction_napcp/ES%20final%20NAPCP%203Oct2019.pdf
- 36. Dominici F, Peng RD, Barr CD, Bell ML. Protecting human health from air pollution: shifting from a single-pollutant to a multipollutant approach. Epidemiology. 2010;21(2):187-94. DOI: 10.1097/EDE.0b013e3181cc86e8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 37. Bouza E, Alvar A, Almagro P, Alonso T, Ancochea J, Barbé F, et al. Chronic obstructive pulmonary disease (COPD) in Spain and the different aspects of its social impact: a multidisciplinary opinion document. Rev Esp Quimioter. 2020;33(1):49-67. DOI: 10.37201/req/2064.2019. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 38. Miravitlles M, Soler-Cataluña JJ, Calle M, Molina J, Almagro P, Quintano JA, et al. Spanish Guidelines for Management of Chronic Obstructive Pulmonary Disease (GesEPOC) 2017. Pharmacological Treatment of Stable Phase. Arch Bronconeumol. 2017;53(6):324-35. DOI: 10.1016/j.arbres.2017.03.018. [ DOI ] [ PubMed ] [ Google Scholar ]
- 39. Pleguezuelos E, Gimeno-Santos E, Hernández C, Mata MDC, Palacios L, Piñera P, et al. Recommendations on non-Pharmacological Treatment in Chronic Obstructive Pulmonary Disease From the Spanish COPD Guidelines (GesEPOC 2017). Arch Bronconeumol (Engl Ed). 2018;54(11):568-75. DOI: 10.1016/j.arbres.2018.06.001. [ DOI ] [ PubMed ] [ Google Scholar ]
- 40. Vogelmeier CF, Criner GJ, Martinez FJ, Anzueto A, Barnes PJ, Bour-beau J, et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease 2017 Report. GOLD Executive Summary. Am J Respir Crit Care Med. 2017;195(5):557-82. DOI: 10.1164/rccm.201701-0218PP. [ DOI ] [ PubMed ] [ Google Scholar ]
- 41. Instituto Nacional de Seguridad e Higiene en el Trabajo, Ruiz Ruiz L, Peñahora García Sanz M. Calidad del aire. Definiciones de las fracciones de los tamaños de partículas para el muestreo asociado a problemas de salud. Centro Nacional de Nuevas Tecnologías. Available at: https://www.aenorcom/normas-y-libros/buscador-denormas/une/?c=N0007129 . 2021.
- 42. Waron and Willeke . Aerosol. Bioaerosol In: Interscience W, editor. Aerosol Measurement: Principles, Techniques, and Applications. New York. 2001. p. 1065. [ Google Scholar ]
- 43. Morawska L, Milton DK. It Is Time to Address Airborne Transmission of Coronavirus Disease 2019 (COVID-19). Clin Infect Dis. 2020;71(9):2311-3. DOI: 10.1093/cid/ciaa939. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 44. Bourouiba L. Turbulent Gas Clouds and Respiratory Pathogen Emissions: Potential Implications for Reducing Transmission of COVID-19. Jama. 2020;323(18):1837-8. DOI: 10.1001/jama.2020.4756. [ DOI ] [ PubMed ] [ Google Scholar ]
- 45. Morawska L, Tang JW, Bahnfleth W, Bluyssen PM, Boerstra A, Buonanno G, et al. How can airborne transmission of COVID-19 indoors be minimised? Environ Int. 2020;142:105832. DOI: 10.1016/j.envint.2020.105832. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 46. Fears AC, Klimstra WB, Duprex P, Hartman A, Weaver SC, Plante KC, et al. Comparative dynamic aerosol efficiencies of three emergent coronaviruses and the unusual persistence of SARS-CoV-2 in aerosol suspensions. medRxiv. 2020. DOI: 10.1101/2020.04.13.20063784. [ DOI ] [ Google Scholar ]
- 47. Vargas Marcos F, Ruiz de Adana M, Marín Rodríguez I, S. MG. Transmisión del SARS-CoV-2 por gotas respiratorias, objetos contaminados y aerosoles (vía aérea). Revisión de evidencias 2020. Available at: https://www.sanidadambientalcom/wp-content/uploads/2020/09/Transmisi%C3%B3n-del-SARS-CoV-2-por-gotas-respiratoriasobjetos-contaminados-y-aerosoles.pdf .
- 48. Ministerio de Sanidad . Recomendaciones de operación y mantenimiento nde los sistemas de climatización y ventilación de edificios y locales para la prevención de la propagación de SARS-CoV-2. 2020. Available at: https://www.mscbsgobes/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/Recomendaciones_de_operacion_y_mantenimiento.pdf .
- 49. European Center for Disease Prevention and Control . Heating, ventilation and air.conditioning systems in the context of COVID.19: November 2020 Available at: https://www.ecdceuropaeu/en/publications-data/heating-ventilation-air-conditioning-systems-covid-19 .
- 50. W.H.O . Transmission of SARSCoV-2: implications for infection prevention precautions Scientific Brief 9 July 2020. COVID-19: Infection prevention and control /WASH[10 de junio 2020]. Available at: https://www.whoint/publications/i/item/modes-of-transmission-of-viruscausing-covid-19-implications-for-ipc-precaution-recommendations .
- 51. CDC . Scientific Brief: SARS-CoV-2 and Potential Airborne Transmission. Available at: https://www.mscbsgobes/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/COVID19_Aerosolespdf . 2020.
- 52. Ministerio de Sanidad . Documento técnico. Evaluación del riesgo de la transmisión de SAR-CoV-2 mediante aerosoles. Medias de prevención y recomendaciones. 2020. Available at: https://www.mscbsgobes/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/COVID19_Aerosoles.pdf ..
- 53. W.H.O . Contaminación del aire de interiores y salud. Available at: https://www.whoint/es/news-room/fact-sheets/detail/household-air-pollution-and-health . 2018.
- 54. Instituto Nacional de Seguridad e Higiene en el Trabajo. Ruiz L, Peñahora M. CALIDAD DEL AMBIENTE INTERIOR. Available at: https://www.insstes/documents/94886/509319/CalidadambinteriorDTECAIpdf/6f7cfa1c-215d-4f56-9e39-2869a23d8892 . Accedido en 2021:1-22. [ Google Scholar ]
- 55. Instituto Nacional de Seguridad e Higiene en el Trabajo. Berernguer MJ, Bernal F. NTP 549: El dióxido de carbono en la evaluación de la calidad del aire interior. Available at: https://www.insstes/documents/94886/327064/ntp_549pdf/e9364a82-6f1b-4590-90e0-1d08b22e1074 . 2000:1-6. [ Google Scholar ]
- 56. Instituto Nacional de Seguridad e Higiene en el Trabajo. Álvarez T, Peñahora M, Martín I. CALIDAD DE AMBIENTE INTERIOR EN OFICINAS Identificación, análisis y priorización de actuación frente al riesgo. 2015:1-80. Available at: https://www.insstes/documents/94886/96076/CAI+en+oficinaspdf/cf678a1a-ac21-40a7-9c31-a22efe5428d3?t=1526555136853 . [ Google Scholar ]
- 57. Instituto Nacional de Seguridad e Higiene en el Trabajo (INSST) . La ventilación como medida preventiva frente al Coronavirus SARS-CoV-2. 2021:1-17. Available at: https://www.insst.es/documents/94886/712877/La+ventilaci%C3%83%C6%92%C3%86%E2%80%99%C3%83%E2%80%A0%C3%A2%E2%82%AC%E2%84%A2%C3%83%C6%92%C3%A2%E2%82%AC%C5%A1%C3%83%E2%80%9A%C3%82%C2%B3n+como+medida+preventiva+frente+al+coronavirus+SARS-CoV-2.pdf/7d80e9f3-2b44-7e37-8af2-7ab105621070?t=1613134710733 . [ Google Scholar ]
- 58. MInisterio de Sanidad. Nuevo coronavirus 2019-nCoV. Informe Técnico. 2020:1-20. Available at: https://www.mscbsgobes/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/20200210_ITCoronavirus.pdf . [ Google Scholar ]
- 59. Instituto Nacional de Seguridad e Higiene en el Trabajo (INSST) . Marqués F. La pandemia de la COVID-19: lecciones aprendidas para la seguridad y salud del futuro. 2020;103:6-19.Available at: https://www.insstes/documents/94886/712877/La+pandemia+de+la+COVID19+lecciones+aprendidas+para+la+seguridad+y+salud+del+futuro+SST+103+2020/88af9d05-95fc-4ee5-bba2-c7719d245f2a . [ Google Scholar ]
- 60. Ministerio de Sanidad. Evaluación del riesgo de la transmisión de SARS-CoV-2 mediante aerosoles. Medias de prevención y recomendaciones. Documento técnico. 2020:1-43. Available at: https://www.mscbsgobes/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/COVID19_Aerosoles.pdf . [ Google Scholar ]
- 61. Boletín Oficial del País Vasco . DECRETO 38/2020, de 6 de noviembre, del Lehendakari, de modificación del Decreto 36/2020, de 26 de octubre, por el que se determinan medidas específicas de prevención, en el ámbito de la declaración del estado de alarma, como consecuencia de la evolución de la situación epidemiológica y para contener la propagación de infecciones causadas por el SARS-CoV-2. 2020;Boletín 221:1-4. Available at: https://www.legeguneaeuskadieus/eli/es-pv/d/2020/11/06/38/dof/spa/html/webleg00-contfich/es/ . [ Google Scholar ]
- 62. Sehulster L, Chinn RY, Cdc, Hicpac. Guidelines for environmental infection control in health-care facilities. Recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee (HICPAC). MMWR Recomm Rep. 2003;52(RR-10):1-42. [ PubMed ] [ Google Scholar ]
- 63. Sociedad Española de Medicina Preventiva SPeHS, INSALUD . Recomendaciones para la Verificación de la Bioseguridad Ambiental (BSA) respecto a Hongos Oportunistas. 2000:1-16. Available at: https://www.sempsphcom/images/stories/recursos/pdf/protocolos/2012/108_Bioseguridad_Ambiental_frente_a_Hongos.pdf . [ Google Scholar ]
- 64. Ezpeleta-Baquedano C, Barrios-Andrés JL, Delgado-Iribarren A. Control microbiológico ambiental. Enferm Infecc Microbiol Clin. 2013;31(6):396-401. [ DOI ] [ PubMed ] [ Google Scholar ]
- 65. European Center for Disease Prevention and Control . Legionnaires’ disease. Annual Epidemiological Report for 2018. Surveillance report. 2020:1-8. Available at: https://www.ecdceuropaeu/sites/default/files/documents/AER_for_2018_Legionnaires.pdf . [ Google Scholar ]
- 66. Red Nacional de Vigilancia Epidemiológica . Informe semanal de vigilancia epidemiológica en España. 2021;2:1-12. Available at: https://www.isciiies/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Boletines/Documents/Boletin_Epidemiologico_en_red/boletines%20en%20red%202021/IS_N%C2%BA2-210112_WEB.pdf . [ Google Scholar ]
- 67. UNE NE . Prevención y control de la proliferación y diseminación de Legionella en instalaciones. Norma Española. UNE 100030. Abril 2017. 2017:1-6. Available at: https://www.uneorg/encuentra-tunorma/busca-tu-norma/norma?c=N0058186 . [ Google Scholar ]
- 68. Group. WB . The cost of air pollution : strengthening the economic case for action. 2016. Available at: https://documentsworldbankorg/en/publication/documents-reports/documentdetail/781521473177013155/the-cost-of-air-pollution-strengthening-the-economic-case-for-action .
- 69. Consejo Europeo . Reunión extraordinaria del Consejo Europeo (17 a 21 de julio de 2020). Conclusiones. 2020;EUCO 10/20 1-68. Available at: https://www.consiliumeuropaeu/media/45124/210720-euco-final-conclusions-es.pdf .
- 70. Coase RH. The Problem of Social Cost. The Journal of Law and Economics. 1960;3:1-44. [ Google Scholar ]
- 71. Olier E. Welfare Economics, Welfare State and the Real Economy. AESTIMATIO, The IEB International Journal of Finance. 2014;8:160-83. [ Google Scholar ]
- 72. Nations U. A Kyoto Protocol to the United Nations Framework Convention on Climate Change. Available at: https://treatiesunorg/Pages/ViewDetailsaspx?src=TREATY&mtdsg_no=XXVII-7-a&chapter=27&clang=_en . 1997:1-7. [ Google Scholar ]
- 73. Agence nationale de sécurité sanitaire de l’alimentation, de l’environnement et du travail . Étude exploratoire du coût socioéconomique des polluants de l’air intérieur. Rapport d’étude. Available at: https://www.anses.fr/fr/system/files/AUT-Ra-CoutAirInterieurSHS2014.pdf .
- 74. Coase RH. The Firm, the Market, and the Law. University of Chicago Press. 1988:1-226. [ Google Scholar ]
- 75. Boulanger G, Bayeux T, Mandin C, Kirchner S, Vergriette B, PerneletJoly V, et al. Socio-economic costs of indoor air pollution: A tentative estimation for some pollutants of health interest in France. Environ Int. 2017;104:14-24. DOI: 10.1016/j.envint.2017.03.025. [ DOI ] [ PubMed ] [ Google Scholar ]
- 76. Brunekreef B, et al. Air pollution and COVID-19. 2021;PE 658.216:1-66. Available at: https://www.europarleuropaeu/RegData/etudes/STUD/2021/658216/IPOL_STU(2021)658216_EN.pdf . [ Google Scholar ]
- 77. Asikainen A, Carrer P, Kephalopoulos S, Fernandes Ede O, Wargocki P, Hanninen O. Reducing burden of disease from residential indoor air exposures in Europe (HEALTHVENT project). Environ Health. 2016;15 Suppl 1:35. DOI: 10.1186/s12940-016-0101-8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 78. Bond TC, Doherty SJ, Fahey DW, Forster PM, Berntsen T, DeAngelo BJ, et al. Bounding the role of black carbon in the climate system: a scientific assessment. J Geophys Res Atmos. 2013;118(11):5380-552. DOI: 10.1002/jgrd.50171. [ DOI ] [ Google Scholar ]
- 79. Myhre G, Shindell D, Bréon F-M, Collins W, Fuglestvedt J, Huang J, et al. Anthropogenic and natural radiative forcing. Cambridge University Press. 2014:659-740. DOI: 10.1017/CBO9781107415324.018. [ DOI ] [ Google Scholar ]
- 80. Shindell DT, Lamarque J-F, Schulz M, Flanner M, Jiao C, Chin M, et al. Radiative forcing in the ACCMIP historical and future climate simulations. Atmos Chem Phys. 2013;13(6):2939-74. DOI: 10.5194/acp-13-2939-2013. [ DOI ] [ Google Scholar ]
- 81. Jacob DJ, Winner DA. Effect of climate change on air quality. Atmospheric Environment. 2009;43(1):51-63. [ Google Scholar ]
- 82. Sillman S, P.J. S. Impact of temperature on oxidant photochemistry in urban, polluted rural and remote environments. 100(D6):11497–508. J Geophys Res Atmos. 1995;100(D6):11497-508. DOI: 10.1029/94JD02146. [ DOI ] [ Google Scholar ]
- 83. Fiore AM, Naik V, Leibensperger EM. Air quality and climate connections. J Air Waste Manag Assoc. 2015;65(6):645–85. DOI: 10.1080/10962247.2015.1040526. [ DOI ] [ PubMed ] [ Google Scholar ]
- 84. Fiore AM. Atmospheric chemistry: no equatorial divide for a cleansing radical. 2014;513(7517):176–8. Nature. 2014;513(7517):176-8. DOI: 10.1038/513176a. [ DOI ] [ PubMed ] [ Google Scholar ]
- 85. Carslaw KS, Boucher O, Spracklen DV, Mann GW, Rae JGL, Woodward S, et al. A review of natural aerosol interactions and feedbacks within the Earth system. Atmos Chem Phys. 2010;10(4):1701-37. DOI: doi.org/ 10.5194/acp-10-1701-2010. [ DOI ] [ Google Scholar ]
- 86. Orru H, Ebi KL, Forsberg B. The Interplay of Climate Change and Air Pollution on Health. Curr Environ Health Rep. 2017;4(4):504-13. DOI: 10.1007/s40572-017-0168-6. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 87. Olsson D, Mogren I, Forsberg B. Air pollution exposure in early pregnancy and adverse pregnancy outcomes: a register-based cohort study. BMJ Open. 2013;3(2). DOI: 10.1136/bmjopen-2012-001955. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 88. Bunker A, Wildenhain J, Vandenbergh A, Henschke N, Rocklov J, Hajat S, et al. Effects of Air Temperature on Climate-Sensitive Mortality and Morbidity Outcomes in the Elderly; a Systematic Review and Meta-analysis of Epidemiological Evidence. EBioMedicine. 2016;6:258-68. DOI: 10.1016/j.ebiom.2016.02.034. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 89. Patz JA, Frumkin H, Holloway T, Vimont DJ, Haines A. Climate change: challenges and opportunities for global health. JAMA. 2014;312(15):1565-80. DOI: 10.1001/jama.2014.13186 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 90. McGrath JM, Betzelberger AM, Wang S, Shook E, Zhu XG, Long SP, et al. An analysis of ozone damage to historical maize and soybean yields in the United States. Proc Natl Acad Sci U S A. 2015;112(46):14390-5. DOI: 10.1073/pnas.1509777112. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 91. (HCWH) HCWH, ARUP. 2019:1-48. Available at: https://www.arupcom/perspectives/publications/research/section/healthcares-climate-footprint . [ Google Scholar ]
- 92. Pichler PP, Jaccard IS, Weisz U, Weisz H. International comparison of health care carbon footprints.14:064004. Environ Res Lett. 2019;14:1-8.35340667 [ Google Scholar ]
- 93. Saran S, Gurjar M, Baronia A, Sivapurapu V, Ghosh PS, Raju GM, et al. Heating, ventilation and air conditioning (HVAC) in intensive care unit. Crit Care. 2020;24(1):194. DOI: 10.1186/s13054-020-02907-5. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 94. Curtis LT. Prevention of hospital-acquired infections: review of non-pharmacological interventions. J Hosp Infect. 2008;69(3):204-19. DOI: 10.1016/j.jhin.2008.03.018. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 95. Bartley JM, Olmsted RN, Haas J. Current views of health care design and construction: practical implications for safer, cleaner environments. Am J Infect Control. 2010;38(5 Suppl 1):S1-12. DOI: 10.1016/j.ajic.2010.04.195. [ DOI ] [ PubMed ] [ Google Scholar ]
- 96. McDowall R. Fundamentals of HVAC systems, 1st edition.. 2006:223. [ Google Scholar ]
- 97. Luongo JC, Fennelly KP, Keen JA, Zhai ZJ, Jones BW, Miller SL. Role of mechanical ventilation in the airborne transmission of infectious agents in buildings. Indoor Air. 2016;26(5):666-78. DOI: 10.1111/ina.12267. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 98. Eames I, Tang JW, Li Y, Wilson P. Airborne transmission of disease in hospitals. J R Soc Interface. 2009;6 Suppl 6:S697-702. DOI: 10.1098/rsif.2009.0407.focus. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 99. UNE NE . UNE 100713. Instalaciones de Acondicionamiento de Aire en Hospitales. 2005. Available at: https://www.uneorg/encuentratu-norma/busca-tu-norma/norma/?c=N0034264 .
- 100. UNE NE . UNE 171330-1:2008. Calidad ambiental en interiores. Parte 1: Diagnóstico de calidad ambiental interior. Available at: https://www.enuneorg/encuentra-tu-norma/busca-tu-norma/norma/?c=N0041499 . 2008. [ Google Scholar ]
- 101. UNE NE . UNE 171330-2:2014. Calidad ambiental en interiores. Parte 2: Procedimientos de inspección de calidad ambiental interior. 2014. Available at: https://www.uneorg/encuentra-tu-norma/busca-tu-norma/norma?c=N0054187 . [ Google Scholar ]
- 102. UNE NE . UNE 171340:2020. Validación y Cualificación de salas de ambiente controlado en hospitales. 2020. Available at: https://www.uneorg/encuentra-tu-norma/busca-tu-norma/norma?c=N0064465 . [ Google Scholar ]
- 103. UNE NE . UNE-EN ISO 14644-1:2016. Salas limpias y locales anexos controlados. Parte 1: Clasificación de la limpieza del aire mediante la concentración de partículas. (ISO 14644-1:2015). 2016. Available at: https://www.uneorg/encuentra-tu-norma/busca-tu-norma/norma?c=N0057435 . [ Google Scholar ]
- 104. UNE NE . UNE-EN ISO 16890-1:2017. Filtros de aire utilizados en ventilación general. Parte 1: Especificaciones técnicas, requisitos y clasificación según eficiencia basado en la materia particulada (PM). (ISO 16890-1:2016). 2017. Available at: https://www.uneorg/encuentra-tu-norma/busca-tu-norma/norma/?c=N0058514 . [ Google Scholar ]
- 105. Liu Y, Ning Z, Chen Y, Guo M, Liu Y, Gali NK, et al. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature. 2020;582(7813):557-60. DOI: 10.1038/s41586-020-2271-3 [ DOI ] [ PubMed ] [ Google Scholar ]
- 106. Razzini K, Castrica M, Menchetti L, Maggi L, Negroni L, Orfeo NV, et al. SARS-CoV-2 RNA detection in the air and on surfaces in the COVID-19 ward of a hospital in Milan, Italy. Sci Total Environ. 2020;742:140540. DOI: 10.1016/j.scitotenv.2020.140540 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 107. Ministerio de Sanidad. Prevención y control de la infección en el manejo de pacientes con COVID-19. Documento Técnico. Versión 20 de mayo de 2020. 2020:1-18. Available at: https://medicostenerifees/wp-content/uploads/2020/05/Documento_Control_Infeccion.pdf . [ Google Scholar ]
- 108. (WHO) WHO . Infection prevention and control during health care when novel coronavirus (nCoV) infection is suspected. 2020:1-5. Available at: https://www.whoint/publications/i/item/10665-331495 . [ Google Scholar ]
- 109. European Center for Disease Prevention and Control . Infection prevention and control and preparedness for COVID-19 in health-care settings. Fourth update. Technical Report. 2020:1-13. Available at: https://www.ecdceuropaeu/sites/default/files/documents/Infection-prevention-and-control-in-healthcare-settings-COVID-19_4th_update.pdf . [ Google Scholar ]
- 110. Lai CC, Yu WL. COVID-19 associated with pulmonary aspergillosis: A literature review. J Microbiol Immunol Infect. 2021;54(1):46-53. DOI: 10.1016/j.jmii.2020.09.004. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 111. Koehler P, Bassetti M, Chakrabarti A, Chen SCA, Colombo AL, Hoenigl M, et al. Defining and managing COVID-19-associated pulmonary aspergillosis: the 2020 ECMM/ISHAM consensus criteria for research and clinical guidance. Lancet Infect Dis. 2020. DOI: 10.1016/s1473-3099(20)30847-1. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 112. Verweij PE, Gangneux JP, Bassetti M, Brüggemann RJM, Cornely OA, Koehler P, et al. Diagnosing COVID-19-associated pulmonary aspergillosis. Lancet Microbe. 2020;1(2):e53-e5. DOI: 10.1016/s2666-5247(20)30027-6. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 113. Machado M, Valerio M, Álvarez-Uría A, Olmedo M, Veintimilla C, Padilla B, et al. Invasive pulmonary aspergillosis in the COVID-19 era: An expected new entity. Mycoses. 2021;64(2):132-43. DOI: 10.1111/myc.13213. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 114. Cornely OA, Alastruey-Izquierdo A, Arenz D, Chen SCA, Dannaoui E, Hochhegger B, et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019;19(12):e405-e21. DOI: 10.1016/s1473-3099(19)30312-3. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 115. Cornely OA, Arikan-Akdagli S, Dannaoui E, Groll AH, Lagrou K, Chakrabarti A, et al. ESCMID and ECMM joint clinical guidelines for the diagnosis and management of mucormycosis 2013. Clin Micro-biol Infect. 2014;20 Suppl 3:5-26. DOI: 10.1111/1469-0691.12371. [ DOI ] [ PubMed ] [ Google Scholar ]
- 116. Tortorano AM, Richardson M, Roilides E, van Diepeningen A, Caira M, Munoz P, et al. ESCMID and ECMM joint guidelines on diagnosis and management of hyalohyphomycosis: Fusarium spp., Scedosporium spp. and others. Clin Microbiol Infect. 2014;20 Suppl 3:27-46. DOI: 10.1111/1469-0691.12465. [ DOI ] [ PubMed ] [ Google Scholar ]
- 117. Garcia-Vidal C, Alastruey-Izquierdo A, Aguilar-Guisado M, Carratalà J, Castro C, Fernández-Ruiz M, et al. Executive summary of clinical practice guideline for the management of invasive diseases caused by Aspergillus: 2018 Update by the GEMICOMED-SEIMC/REIPI. Enferm Infecc Microbiol Clin (Engl Ed). 2019;37(8):535-41. DOI: 10.1016/j.eimc.2018.03.018. [ DOI ] [ PubMed ] [ Google Scholar ]
- 118. Peláez T, Muñoz P, Guinea J, Valerio M, Giannella M, Klaassen CH, et al. Outbreak of invasive aspergillosis after major heart surgery caused by spores in the air of the intensive care unit. Clin Infect Dis. 2012;54(3):e24-31. DOI: 10.1093/cid/cir771. [ DOI ] [ PubMed ] [ Google Scholar ]
- 119. Muñoz P, Guinea J, Peláez T, Durán C, Blanco JL, Bouza E. Nosocomial invasive aspergillosis in a heart transplant patient acquired during a break in the HEPA air filtration system. Transpl Infect Dis. 2004;6(1):50-4. DOI: 10.1111/j.1399-3062.2004.00047. [ DOI ] [ PubMed ] [ Google Scholar ]
- 120. Vonberg RP, Gastmeier P. Nosocomial aspergillosis in outbreak settings. J Hosp Infect. 2006;63(3):246-54. DOI: 10.1016/j.jhin.2006.02.014. [ DOI ] [ PubMed ] [ Google Scholar ]
- 121. Benet T, Nicolle MC, Thiebaut A, Piens MA, Nicolini FE, Thomas X, et al. Reduction of invasive aspergillosis incidence among immunocompromised patients after control of environmental exposure. Clin Infect Dis. 2007;45(6):682-6. DOI: 10.1086/521378. [ DOI ] [ PubMed ] [ Google Scholar ]
- 122. Munoz P, Guinea J, Pelaez T, Duran C, Blanco JL, Bouza E. Nosocomial invasive aspergillosis in a heart transplant patient acquired during a break in the HEPA air filtration system. Transpl Infect Dis. 2004;6(1):50-4. DOI: 10.1111/j.1399-3062.2004.00047. [ DOI ] [ PubMed ] [ Google Scholar ]
- 123. Guinea J, Garcia de Viedma D, Pelaez T, Escribano P, Munoz P, Meis JF, et al. Molecular epidemiology of Aspergillus fumigatus: an in-depth genotypic analysis of isolates involved in an outbreak of invasive aspergillosis. J Clin Microbiol. 2011;49(10):3498-503. DOI: 10.1128/JCM.01159-11. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 124. Ruiz-Camps I, Aguado JM, Almirante B, Bouza E, Ferrer-Barbera CF, Len O, et al. Guidelines for the prevention of invasive mould diseases caused by filamentous fungi by the Spanish Society of Infectious Diseases and Clinical Microbiology (SEIMC). Clin Microbiol Infect. 2011;17 Suppl 2:1-24. DOI: 10.1111/j.1469-0691.2011.03477. [ DOI ] [ PubMed ] [ Google Scholar ]
- 125. Javaid W, Ehni J, Gonzalez-Reiche AS, Carreno JM, Hirsch E, Tan J, et al. Real-Time Investigation of a Large Nosocomial Influenza A Outbreak Informed by Genomic Epidemiology. Clin Infect Dis. 2020. DOI: 10.1093/cid/ciaa1781. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 126. Carter B, Collins JT, Barlow-Pay F, Rickard F, Bruce E, Verduri A, et al. Nosocomial COVID-19 infection: examining the risk of mortality. The COPE-Nosocomial Study (COVID in Older PEople). J Hosp Infect. 2020;106(2):376-84. DOI: 10.1016/j.jhin.2020.07.013. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 127. Jensen J, Guinea J, Torres-Narbona M, Munoz P, Pelaez T, Bouza E. Post-surgical invasive aspergillosis: an uncommon and under-appreciated entity. J Infect. 2010;60(2):162-7. DOI: 10.1016/j.jinf.2009.11.005. [ DOI ] [ PubMed ] [ Google Scholar ]
- 128. Garnaud C, Brenier-Pinchart MP, Thiebaut-Bertrand A, Hamidfar R, Quesada JL, Bosseray A, et al. Seven-year surveillance of nosocomial invasive aspergillosis in a French University Hospital. J Infect. 2012;65(6):559-67. DOI: 10.1016/j.jinf.2012.08.006. [ DOI ] [ PubMed ] [ Google Scholar ]
- 129. Lee LD, Hachem RY, Berkheiser M, Hackett B, Jiang Y, Raad, II. Hospital environment and invasive aspergillosis in patients with hematologic malignancy. Am J Infect Control. 2012;40(3):247-9. DOI: 10.1016/j.ajic.2011.03.031. [ DOI ] [ PubMed ] [ Google Scholar ]
- 130. Valerio M, Fernandez-Cruz A, Fernandez-Yanez J, Palomo J, Guinea J, Duran R, et al. Prostatic aspergillosis in a heart transplant recipient: case report and review. J Heart Lung Transplant. 2009;28(6):638-46. DOI: 10.1016/j.healun.2009.03.002. [ DOI ] [ PubMed ] [ Google Scholar ]
- 131. Ullmann AJ, Aguado JM, Arikan-Akdagli S, Denning DW, Groll AH, Lagrou K, et al. Diagnosis and management of Aspergillus diseases: executive summary of the 2017 ESCMID-ECMM-ERS guideline. Clin Microbiol Infect. 2018;24 Suppl 1:e1-e38. DOI: 10.1016/j.cmi.2018.01.002. [ DOI ] [ PubMed ] [ Google Scholar ]
- 132. Pelaez T, Munoz P, Guinea J, Valerio M, Giannella M, Klaassen CH, et al. Outbreak of invasive aspergillosis after major heart surgery caused by spores in the air of the intensive care unit. Clin Infect Dis. 2012;54(3):e24-31. DOI: 10.1093/cid/cir771. [ DOI ] [ PubMed ] [ Google Scholar ]
- 133. Gonzales Zamora JA, Henry Z, Gultekin SH. Central Nervous System Aspergillosis: An Unexpected Complication following Neurosurgery. Diseases. 2018;6(2). DOI: 10.3390/diseases6020046. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 134. Asare KA, Jahng M, Pincus JL, Massie L, Lee SA. Sternal osteomyelitis caused by Aspergillus fumigatus following cardiac surgery: Case and review. Med Mycol Case Rep. 2012;2:4-6. DOI: 10.1016/j.mmcr.2012.12.003. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 135. Nicolle MC, Benet T, Vanhems P. Aspergillosis: nosocomial or community-acquired? Med Mycol. 2011;49 Suppl 1:S24-9. DOI: 10.3109/13693786.2010.509335. [ DOI ] [ PubMed ] [ Google Scholar ]
- 136. Partridge-Hinckley K, Liddell GM, Almyroudis NG, Segal BH. Infection control measures to prevent invasive mould diseases in hematopoietic stem cell transplant recipients. Mycopathologia. 2009;168(6):329-37. DOI: 10.1007/s11046-009-9247-z. [ DOI ] [ PubMed ] [ Google Scholar ]
- 137. Haiduven D. Nosocomial aspergillosis and building construction. Med Mycol. 2009;47 Suppl 1:S210-6. DOI: 10.1080/13693780802247694. [ DOI ] [ PubMed ] [ Google Scholar ]
- 138. Kauffmann-Lacroix C, Bousseau A, Dalle F, Brenier-Pinchart MP, Delhaes L, Machouart M, et al. [Prevention of fungal infections related to the water supply in French hospitals: proposal for standardization of methods]. Presse Med. 2008;37(5 Pt 1):751-9. DOI: 10.1016/j.lpm.2007.09.015. [ DOI ] [ PubMed ] [ Google Scholar ]
- 139. Munoz P, Burillo A, Bouza E. Environmental surveillance and other control measures in the prevention of nosocomial fungal infections. Clin Microbiol Infect. 2001;7 Suppl 2:38-45. DOI: 10.1111/j.1469-0691.2001.tb00008. [ DOI ] [ PubMed ] [ Google Scholar ]
- 140. Troiano G, Sacco C, Donato R, Pini G, Niccolini F, Nante N. Demolition activities in a healthcare facility: results from a fungal surveillance after extraordinary preventive measures. Public Health. 2019;175:145-7. DOI: 10.1016/j.puhe.2019.07.012. [ DOI ] [ PubMed ] [ Google Scholar ]
- 141. Munoz P, Rodriguez C, Bouza E, Palomo J, Yanez JF, Dominguez MJ, et al. Risk factors of invasive aspergillosis after heart transplantation: protective role of oral itraconazole prophylaxis. Am J Transplant. 2004;4(4):636-43. DOI: 10.1111/j.1600-6143.2004.00390. [ DOI ] [ PubMed ] [ Google Scholar ]
- 142. Munoz P, Ceron I, Valerio M, Palomo J, Villa A, Eworo A, et al. Invasive aspergillosis among heart transplant recipients: a 24-year perspective. J Heart Lung Transplant. 2014;33(3):278-88. DOI: 10.1016/j.healun.2013.11.003. [ DOI ] [ PubMed ] [ Google Scholar ]
- 143. Guinea J, Pelaez T, Alcala L, Bouza E. Outdoor environmental levels of Aspergillus spp. conidia over a wide geographical area. Med Mycol. 2006;44(4):349-56. DOI: 10.1080/13693780500488939. [ DOI ] [ PubMed ] [ Google Scholar ]
- 144. Demográfico MMplTEyeR. Evaluación de l calidad del aire en España. 2019:1-246. Available at: https://www.mitecogobes/images/es/informeevaluacioncalidadaireespana2019_tcm30-510616.pdf . [ Google Scholar ]
- 145. Ministerio de la Presidencia RclCyMD, Estado Jd. Ley 34/2007, de 15 de noviembre, de calidad del aire y protección de la atmósfera. Boletín Oficial del Estado BOE. 2007.
- 146. Organización Mundial de la Salud . Contaminación del aire. Available at: https://www.whoint/ipcs/assessment/public_health/air_pollution/es/ .
- View on publisher site
- PDF (1.3 MB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
JavaScript appears to be disabled on this computer. Please click here to see any active alerts .
Research on Health Effects from Air Pollution
Decades of research have shown that air pollutants such as ozone and particulate matter (PM) increase the amount and seriousness of lung and heart disease and other health problems. More investigation is needed to further understand the role poor air quality plays in causing detrimental effects to health and increased disease, especially in vulnerable populations. Children, the elderly, and people living in areas with high levels of air pollution are especially susceptible.
Results from these investigations are used to support the nation's air quality standards under the Clean Air Act and contribute to improvements in public health.
On this page:
Health Effects of Air Pollutants on Vulnerable Populations
Long-term and short-term effects from exposure to air pollutants.
- Multipollutant Exposures and Changes in Environmental Conditions
- Leveraging Big Data for Innovations in Health Science
Health Effects of Wildfire Smoke
Public health intervention and communications strategies, integrated science assessments for air pollutants.

Research has shown that some people are more susceptible than others to air pollutants. These groups include children, pregnant women, older adults, and individuals with pre-existing heart and lung disease. People in low socioeconomic neighborhoods and communities may be more vulnerable to air pollution because of many factors. Proximity to industrial sources of air pollution, underlying health problems, poor nutrition, stress, and other factors can contribute to increased health impacts in these communities.
There is a need for greater understanding of the factors that may influence whether a population or age group is at increased risk of health effects from air pollution. In addition, advances to analytical approaches used to study the health effects from air pollution will improve exposure estimates for healthy and at-risk groups.
The research by EPA scientists and others inform the required reviews of the primary National Ambient Air Quality Standards (NAAQS), which is done with the development of Integrated Science Assessments (ISAs). These ISAs are mandated by Congress every five years to assess the current state of the science on criteria air pollutants and determine if the standards provide adequate protection to public health.
Research is focused on addressing four areas:
- Identifying and characterizing whether there are key reproductive factors and critical stages of development that are impacted by air pollution exposures;
- Determining the role of acute and chronic sociodemographic factors in air pollution health disparities;
- Understanding how diet modifies responses to air pollution;
- Evaluating long-term lifestyle and chronic disease effects on air pollution-induced respiratory and cardiovascular responses
A multi-disciplinary team of investigators is coordinating epidemiological, human observational, and basic toxicological research to assess the effects of air pollution in at-risk populations and develop strategies to protect these populations, particularly those with pre-existing disease. The results from these products will improve risk assessments by clarifying the role of modifying factors such as psychosocial stress (e.g. noise) and diet, and determining the impact of individual susceptibility on the relationship between air pollutant exposures and health.
Related Links
- Healthy Heart Research
- Integrated Science Assessments
- Criteria Air Pollutants

People can experience exposure to varying concentrations of air pollution. Poor air quality can impact individuals for a short period of time during the day, or more frequently during a given day. Exposure to pollutants can also occur over multiple days, weeks or months due to seasonal air pollution, such as increased ozone during the summer or particulate matter from woodstoves during the winter.
The health impact of air pollution exposure depends on the duration and concentrations, and the health status of the affected populations. Studies are needed to increase knowledge of the exposure duration and the possible cumulative increase in risk.
The research is focused on three main areas:
- Short-term peak exposures, such as wildfires, traffic-related sources, or other episodic events;
- Intermittent and cumulative exposures;
- Mechanisms underlying the exposure risks
Researchers are evaluating the health responses of intermittent multiple days versus one-day air pollution exposure in controlled human exposure, animal, and in vitro models and associated cellular and molecular mechanisms. They are employing population-based models and electronic health records to assess the health effects of short-term and long-term exposures and identifying populations at greatest risk of health effects. The work is improving our understanding of the possible cumulative effects of multiple short-term peak exposures and the relationship of these exposures to longer-term exposures and risks.
Multipollutant Exposures and Changes in Environmental Conditions

EPA research is providing information to understand how individuals may respond to two or more pollutants or mixtures and how environmental conditions may impact air quality. While risk estimates for exposure to individual criteria air pollutants such as PM and ozone are well established, the acute and cumulative effects of combinations of pollutants is not well understood. In addition, research is needed to determine how changes in the environment affect both pollutant formation and subsequent responsiveness to exposures in healthy and susceptible individuals.
The research is focused on three specific questions:
- What is the role of temperature and photochemical aging on the health impact of wildfire smoke and air pollution mixtures?
- What is the effect of changing environmental conditions (i.e., temperature and humidity) on responsiveness to air pollution?
- Does prior pollutant exposure modify responsiveness to subsequent exposures?
The integrated, multi-disciplinary research includes:
- Epidemiologic analyses of environmental influences on morbidity and mortality in populations,
- Simulations of changing environmental conditions in multi-pollutant formation in atmospheric chamber studies coupled with clinical and toxicological assessments in healthy and at-risk populations,
- Evaluation of pre-exposure as a modifying effect on subsequent exposures
The results are revealing how changes in environmental conditions affect pollutant formation and subsequent health impact in at-risk populations. The research findings are informing EPA’s Integrated Science Assessments for criteria air pollutants and assisting with future regulatory decisions on the National Ambient Air Quality Standards (NAAQS).
Leveraging Big Data for Innovations in Health Science

EPA is at the cutting edge of health science, using electronic health records, novel data systems, tissue-like advanced cellular models, molecular approaches, and animal models to evaluate the health impacts of air pollution. Researchers are using these powerful new techniques to identify factors that may increase sensitivity and vulnerability to air pollution effects.
The research is building capacity for future risk assessment and regulatory analyses that go beyond traditional lines of evidence to more clearly define populations and lifestages at increased risk of health effects from air pollution.
To continue to protect public health from poor air quality, researchers must consider new epidemiological, toxicological and clinical approaches to understand the health risks of poor air quality and the biological mechanisms responsible for these risks. At the center of these new research approaches is an explosion of data availability and methodological approaches for handling large clinical and molecular datasets, also known as "big data."
While data of increasing size, depth, and complexity have accelerated research for many industries and scientific fields, big data is sometimes less recognized for the impacts it is having on environmental health studies. Increasingly, researchers are able to examine vulnerable populations with unprecedented precision and detail while also evaluating hundreds of thousands of molecular biomarkers in order to understand biological mechanisms associated with exposure.
- Development of the InTelligence And Machine LEarning (TAME) Toolkit for Introductory Data Science, Chemical-Biological Analyses, Predictive Modeling, and Database Mining for Environmental Health Research (Journal Article)

Larger and more intense wildfires are creating the potential for greater smoke production and chronic exposures in the United States, particularly in the West. Wildfires increase air pollution in surrounding areas and can affect regional air quality.
The health effects of wildfire smoke can range from eye and respiratory tract irritation to more serious disorders, including reduced lung function, exacerbation of asthma and heart failure, and premature death. Children, pregnant women, and the elderly are especially vulnerable to smoke exposure. Emissions from wildfires are known to cause increased visits to hospitals and clinics by those exposed to smoke.
It is important to more fully understand the human health effects associated with short- and long-term exposures to smoke from wildfires as well as prescribed fires, together referred to as wildland fires. EPA is conducting research to advance understanding of the health effects from different types of fires as well as combustion phases. Researchers want to know:
- What is the full extent of health effects from smoke exposure?
- Who is most at risk?
- Are there differences in health effects from different wildfire fuel types or combustion phases (burning versus flaming)?
- What strategies and approaches are most effective in protecting public health?
- What are the environmental, social and economic impacts of wildfire emissions?
- Wildland Fire Research
- Smoke-Ready Toolbox for Wildfires
- Smoke Sense Project and App

Many communities throughout the United States face challenges in providing advice to residents about how best to protect their health when they are exposed to elevated concentrations of air pollutants from motor vehicle and industrial emissions and other sources of combustion, including wildland fire smoke.
Researchers are studying intervention strategies to reduce the health impacts from exposure to air pollution as well as ways to effectively communicate these health risks. To translate the science for use in public health communication and community empowerment, EPA is collaborating with other federal agencies, such as the Centers for Disease Control and Prevention (CDC) and the National Heart, Lung, and Blood Institute (NHLBI), and state and local agencies and tribes. The objectives are to identify ways to lower air pollution exposure or mitigate the biological responses at individual, community or ecosystem levels, and ultimately evaluate whether such interventions have benefits as measured by indicators of health, well-being or economics.
Studies are evaluating the interactions between behavior and social and economic factors to more thoroughly understand how these factors may influence health and well-being outcomes, which can inform effective and consistent health risk messaging.
- Healthy Heart Toolkit and Research
- Video: Air Quality Impacts on Public Health

EPA sets National Ambient Air Quality Standards (NAAQS) for six principal criteria air pollutants —nitrogen oxides, sulfur oxides, particulate matter, carbon monoxide, ozone and lead—all of which have been shown to be harmful to public health and the environment.
The Agency’s Integrated Science Assessments (ISAs) form the scientific foundation for the review of the NAAQS standards by providing the primary (human health-based) assessments and secondary (welfare-based, e.g. ecology, visibility, materials) assessments. The ISAs are assessments of the state of the science on the criteria pollutants. They are conducted as mandated under the Clean Air Act.
Air Research

Children play on the shore of Manila Bay in the Philippines, which is polluted by plastic waste.
- ENVIRONMENT
The world's plastic pollution crisis, explained
Much of the planet is swimming in discarded plastic, which is harming animal and possibly human health. Can it be cleaned up?
Plastic pollution has become one of the most pressing environmental issues , as rapidly increasing production of disposable plastic products overwhelms the world’s ability to deal with them. Plastic pollution is most visible in developing Asian and African nations, where garbage collection systems are often inefficient or nonexistent. But the developed world, especially in countries with low recycling rates , also has trouble properly collecting discarded plastics. Plastic trash has become so ubiquitous it has prompted efforts to write a global treaty negotiated by the United Nations.
Why was plastic invented?
Plastics made from fossil fuels are just over a century old. Belgian chemist Leo Baekeland created the first fully synthetic plastic in 1907. Production and development of thousands of new plastic products accelerated after World War II , so transforming the modern age that life without plastics would be unrecognizable today. In plastic, inventors found a light, durable material that can be used in everything from transportation to medicine.
Plastics revolutionized medicine with life-saving devices, made space travel possible, lightened cars and jets—saving fuel and pollution—and saved lives with helmets, incubators, and equipment for clean drinking water.
The conveniences plastics offer, however, led to a throw-away culture that reveals the material’s dark side: today, single-use plastics account for 40 percent of the plastic produced every year. Many of these products, such as plastic bags and food wrappers, have a lifespan of mere minutes to hours, yet they may persist in the environment for hundreds of years.
That's why some governments have taken steps to limit or ban the use of plastic bags. Most recently, California passed legislation to ban all plastic bags by 2026.
Plastics by the numbers
Some key facts:
YEAR-LONG ADVENTURE for every explorer on your list
Half of all plastics ever manufactured have been made in the last 20 years.
- Production increased exponentially, from 2.3 million tons in 1950 to 448 million tons by 2015. Production is expected to double by 2050.
- Every year, about eight million tons of plastic waste escapes into the oceans from coastal nations. That’s the equivalent of setting five garbage bags full of trash on every foot of coastline around the world.
- Plastics often contain additives making them stronger, more flexible, and durable. But many of these additives can extend the life of products if they become litter, with some estimates ranging to at least 400 years to break down.
How plastics move around the world
Most of the plastic trash in the oceans, Earth’s last sink, flows from land. Trash is also carried to sea by major rivers , which act as conveyor belts, picking up more and more trash as they move downstream. Once at sea, much of the plastic trash remains in coastal waters. But once caught up in ocean currents, it can be transported around the world.
On Henderson Island , an uninhabited atoll in the Pitcairn Group isolated halfway between Chile and New Zealand, scientists found plastic items from Russia, the United States, Europe, South America, Japan, and China. They were carried to the South Pacific by the South Pacific gyre, a circular ocean current.
Microplastics—a new health threat
Once at sea, sunlight, wind, and wave action break down plastic waste into small particles, often less than one-fifth of an inch across. These so-called microplastics are spread throughout the water column and have been found in every corner of the globe, from Mount Everest, the highest peak, to the Mariana Trench , the deepest trough.
You May Also Like

Marine pollution, explained

The world’s nations agree to fix the plastic waste crisis

The Haunting Art of Plastic Pollution
Microplastics are breaking down further into smaller and smaller pieces. Plastic microfibers, meanwhile, have been found in municipal drinking water systems and drifting through the air.
It's no surprise then that scientists have found microplastics in people. The tiny particles are in our blood, lungs, and even in feces . Exactly how much microplastics might be harming human health is a question scientists are urgently trying to answer.
Learn more about the microplastics in our bodies and how much do they harm us.
Harm to wildlife
Millions of animals are killed by plastics every year, from birds to fish to other marine organisms. Nearly 2,100 species , including endangered ones, are known to have been affected by plastics. Nearly every species of seabird eats plastics.
Most of the deaths to animals are caused by entanglement or starvation. Seals, whales , turtles, and other animals are strangled by abandoned fishing gear or discarded six-pack rings . Microplastics have been found in more than 100 aquatic species, including fish, shrimp, and mussels destined for our dinner plates. In many cases, these tiny bits pass through the digestive system and are expelled without consequence. But plastics have also been found to have blocked digestive tracts or pierced organs, causing death. Stomachs so packed with plastics reduce the urge to eat, causing starvation.
Plastics have been consumed by land-based animals, including elephants, hyenas, zebras, tigers, camels, cattle, and other large mammals, in some cases causing death .
Tests have also confirmed liver and cell damage and disruptions to reproductive systems , prompting some species, such as oysters, to produce fewer eggs. New research shows that larval fish are eating nanofibers in the first days of life, raising new questions about the effects of plastics on fish populations.
Stopping plastic pollution
Once in the ocean, it is difficult—if not impossible—to retrieve plastic waste. Mechanical systems, such as Mr. Trash Wheel , a litter interceptor in Maryland’s Baltimore Harbor, can be effective at picking up large pieces of plastic, such as foam cups and food containers, from inland waters. But once plastics break down into microplastics and drift throughout the water column in the open ocean, they are virtually impossible to recover.
The solution is to prevent plastic waste from entering rivers and seas in the first place, many scientists and conservationists say. This could be accomplished with improved waste management systems and recycling , better product design that takes into account the short life of disposable packaging, and a reduction in manufacturing of unnecessary single-use plastics.
Related Topics
- WATER POLLUTION
- TOXIC WASTE

How a dramatic win in plastic waste case may curb ocean pollution

In a first, microplastic particles have been linked to heart disease

How do you solve a problem like glitter?

‘Forever chemicals’ are hiding in your kitchen. Here’s where—and what you can do

Biodegradable plastic exists—but it’s not cheap
- Terms of Use
- Privacy Policy
- Your US State Privacy Rights
- Children's Online Privacy Policy
- Interest-Based Ads
- About Nielsen Measurement
- Do Not Sell or Share My Personal Information
- Nat Geo Home
- Attend a Live Event
- Book a Trip
- Inspire Your Kids
- Shop Nat Geo
- Visit the D.C. Museum
- Learn About Our Impact
- Support Our Mission
- Advertise With Us
- Customer Service
- Renew Subscription
- Manage Your Subscription
- Work at Nat Geo
- Sign Up for Our Newsletters
- Contribute to Protect the Planet
Copyright © 1996-2015 National Geographic Society Copyright © 2015-2024 National Geographic Partners, LLC. All rights reserved
Natural Environment Research Council (NERC)
NERC is the driving force of investment in environmental science.

NERC content
- Funding, assessment and award management
- Strategy, remit and programmes
- People, skills and fellowships
- Innovation and collaboration
- Investments, impacts and engagement
- Research centres, facilities and resources
- Register for NERC newsletters

Announcing ‘Explore our planet’ public event

Transforming environmental science with the power of AI

24 October 2024
Landscape review supports NERC’s low-carbon science vision

22 October 2024
UKRI seeks your views in our 2024 stakeholder perception survey

8 October 2024
New investments will drive understanding of our planet
View all NERC news
Funding opportunities
Pre-announcement: future leaders fellowships: round 10.
Funding to support ambitious research and innovation across UK Research and Innovation (UKRI)’s remit. You must be an early career researcher or innovator who is either:
- looking to establish or transition to independence
- developing your own original and ambitious plans within a commercial setting
UKRI Future Leaders Fellowships Renewal Meeting 11 (Invite only)
Future Leaders Fellowship (FLF) award holders have the opportunity to extend their four-year fellowship by up to a further three years. The renewal funding will continue to support the development of a fellow and further the fellow’s work to undertake adventurous, ambitious programmes that tackle difficult and novel challenges.
View all NERC opportunities
Natural Environment Research Council (NERC) Polaris House, North Star Avenue, Swindon, SN2 1EU
Connect with NERC
Subscribe to ukri emails.
Keep up to date with funding, news and events, and a weekly newsletter.
There are no upcoming NERC events at this time.
View all events
This is the website for UKRI: our seven research councils, Research England and Innovate UK. Let us know if you have feedback or would like to help improve our online products and services .

IMAGES
VIDEO
COMMENTS
Moreover, air pollution seems to have various malign health effects in early human life, such as respiratory, cardiovascular, mental, and perinatal disorders (3), leading to infant mortality or chronic disease in adult age (6). National reports have mentioned the increased risk of morbidity and mortality (1).
Abstract. Air pollution is a pressing global environmental challenge with far-reaching consequences for human health and well-being. This research paper presents an extensive examination of air ...
There is much evidence that both acute and chronic exposure to air pollution, especially coarse and fine particulates, increases the morbidity and mortality of the population (Liu et al., 2019; Sanyal et al., 2018).The World Health Organization (WHO) estimates 4.2 million deaths every year as a result of exposure to ambient (outdoor) air pollution (WHO, 2018), which makes air pollution the ...
INTRODUCTION. Air pollution is a major problem of recent decades, which has a serious toxicological impact on human health and the environment. The sources of pollution vary from small unit of cigarettes and natural sources such as volcanic activities to large volume of emission from motor engines of automobiles and industrial activities.[1,2] Long-term effects of air pollution on the onset of ...
Paper Context. Main findings: Among 95 studies assessing health risk perception of air pollution, only nine studies used standardised scales. Added knowledge: There was considerable variation in the scales measuring the multiple dimensions of risk perception for air pollution, which makes comparison among the studies difficult. Global health impact for policy and action: This review highlights ...
Despite progress in many countries, air pollution, and especially fine particulate matter air pollution (PM2.5) remains a global health threat: over 6 million premature cardiovascular and respiratory deaths/yr. have been attributed to household and outdoor air pollution. In this viewpoint, we identify present gaps in air pollution monitoring and regulation, and how they could be strengthened ...
Two large bodies of evidence in air pollution research support a rethinking of current practices in evaluating the health effects of air pollution for prevention and policy: In September 2021, the World Health Organization (WHO) substantially reinforced its Air Quality Guidelines for clean air by reducing the recommended annual levels of PM 2.5 from 10 μg/m 3 to 5 μg/m 3 and those of NO 2 ...
The roles of air pollution and climate change in individual-level patient care are increasingly recognized. While air pollution has contributed to morbidity and mortality before these cases, the past 2 years brought the first cases in which individual deaths were officially linked with air pollution: in the death of a 9-year-old girl who suffered from asthma in the United Kingdom in whom ...
Clean air is a fundamental requirement for the existence of life on earth. However, with the rapid rate of economic development, globalization, and increasing energy demand, large amount of emissions and waste are generated, leading to severe air pollution. This paper surveys the literature to provide an overview of the impact of air pollution on various aspects of human life. The impact is ...
The Lancet Commission on pollution and health reported that pollution was responsible for 9 million premature deaths in 2015, making it the world's largest environmental risk factor for disease and premature death. We have now updated this estimate using data from the Global Burden of Diseases, Injuriaes, and Risk Factors Study 2019. We find that pollution remains responsible for approximately ...
Air pollution poses a major threat to global health (Cattani-Cavalieri et al., 2020).The World Health Organisation (WHO) air quality data shows 99% of the world's population inhale high levels of pollutants, and as a result of poor air quality an estimated 4.2 million people die each year, with the majority death (91%) from low- and middle-income countries (World Health Organisation, 2021).
Air Pollution and Its Destructive Impact on Human Health Deepa Verma Assistant Professor in Zoology Government Science college, Sikar (Raj) ABSTRACT Air pollution is a huge problem in the modern, industrialized world because of the devastating toxicological effects it has on people and the planet. Air pollution comes from a variety of sources ...
Moreover, air pollution seems to have various malign health effects in early human life, such as respiratory, cardiovascular, mental, and perinatal disorders (3), leading to infant mortality or chronic disease in adult age (6). National reports have mentioned the increased risk of morbidity and mortality (1).
Ambient air pollution is a complex mixture of particles and gases. Their concentrations and composition vary from place to place, depending on what sources are present, weather conditions, and how they mix in the atmosphere (Chow, 1995).Over the past several decades, numerous studies have documented associations between ambient air pollution and mortality and morbidity (Hoek et al., 2013 ...
Background Air-pollution and weather exposure beyond certain thresholds have serious effects on public health. Yet, there is lack of information on wider aspects including the role of some effect modifiers and the interaction between air-pollution and weather. This article aims at a comprehensive review and narrative summary of literature on the association of air-pollution and weather with ...
Air pollution has several adverse environmental effects and is regarded as a major global public health concern (Manisalidis et al. 2020). ... reviewing the sources and health effects of indoor air pollution in households" ... Trend analysis of indoor air research worldwide revealed a quantum jump of 2.8 times in the number of publications ...
Human health is closely related to his environment. The influence of exposure to air pollutants on human health and well-being has been an interesting subject and gained much volume of research over the last 50 years. In general, polluted air is considered one of the major factors leading to many diseases such as cardiovascular and respiratory disease and lung cancer for the people. Besides ...
According to the results obtained, it is estimated that air pollution causes 3.2% of the world's illnesses and some 3.1 million premature deaths per year. The effects of pollution on health are mainly related to respiratory and cardiovascular diseases and cancer of the respiratory system.
Decades of research have shown that air pollutants such as ozone and particulate matter (PM) increase the amount and seriousness of lung and heart disease and other health problems. More investigation is needed to further understand the role poor air quality plays in causing detrimental effects to health and increased disease, especially in ...
Health and the environment: addressing the health impact of air pollution (WHA68.8) Health and the environment: draft road map for an enhanced global response to the adverse health effects of air pollution: report by the Secretariat (A69/18) Health, environment and climate change: report by the Director-General (A71/10)
The United Nations defines climate change as a long-term shift in temperatures and weather patterns. As the global climate continues to experience considerable shifts and changes, there is a significant wide range of impacts on human health (IPCC., 2021).Climate change is more than merely a worldwide issue but is a major worry that is a great menace to human health and the most significant ...
The presence of impurities in an atmosphere that affect Nature of the environment including. Human Health are known as air pollution, i t reduce the life quality or interfere with the normal ...
New research shows that larval fish are eating nanofibers in the first days of life, raising new questions about the effects of plastics on fish populations. Stopping plastic pollution
Investments, impacts and engagement; Research centres, facilities and resources; Register for NERC newsletters; Highlights. Announcing 'Explore our planet' public event. Transforming environmental science with the power of AI. News. 24 October 2024. Landscape review supports NERC's low-carbon science vision.