Decision Making: a Theoretical Review
- Regular Article
- Published: 15 November 2021
- Volume 56 , pages 609–629, ( 2022 )

Cite this article

- Matteo Morelli 1 ,
- Maria Casagrande ORCID: orcid.org/0000-0002-4430-3367 2 &
- Giuseppe Forte 1 , 3
6471 Accesses
14 Citations
Explore all metrics
Decision-making is a crucial skill that has a central role in everyday life and is necessary for adaptation to the environment and autonomy. It is the ability to choose between two or more options, and it has been studied through several theoretical approaches and by different disciplines. In this overview article, we contend a theoretical review regarding most theorizing and research on decision-making. Specifically, we focused on different levels of analyses, including different theoretical approaches and neuropsychological aspects. Moreover, common methodological measures adopted to study decision-making were reported. This theoretical review emphasizes multiple levels of analysis and aims to summarize evidence regarding this fundamental human process. Although several aspects of the field are reported, more features of decision-making process remain uncertain and need to be clarified. Further experimental studies are necessary for understanding this process better and for integrating and refining the existing theories.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others
Ethical decision-making theory: an integrated approach.

In AI we trust? Perceptions about automated decision-making by artificial intelligence
Estimating power in (generalized) linear mixed models: An open introduction and tutorial in R
André, M., Borgquist, L., Foldevi, M., & Mölstad, S. (2002). Asking for ‘rules of thumb’: a way to discover tacit knowledge in general practice. Family Practice, 19 (6), 617–22. https://doi.org/10.1093/fampra/19.6.617
Article PubMed Google Scholar
Bechara, A., Damasio, A. R., Damasio, H., & Anderson, S. W. (1994). Insensitivity to future consequences following damage to human prefrontal cortex. Cognition, 50 (1–3), 7–15. https://doi.org/10.1016/0010-0277(94)90018-3
Bechara, A., Damasio, H., Tranel, D., & Damasio, A. R. (1997). Deciding advantageously before knowing the advantageous strategy. Science, 275 (5304), 1293–5. https://doi.org/10.1126/science.275.5304.1293
Bechara, A., Damasio, H., & Damasio, A. R. (2000a). Emotion, decision making and the orbitofrontal cortex. Cerebral cortex, 10 (3), 295–307.
Bechara, A., Tranel, D., & Damasio, H. (2000b). Characterization of the decision-making deficit of patients with ventromedial prefrontal cortex lesions. Brain, 123 (Pt 11), 2189–202. https://doi.org/10.1093/brain/123.11.2189
Bechara, A., & Damasio, A. R. (2005). The somatic marker hypothesis: a neural theory of economic decision. Games and Economic Behavior, 52, 336–372. https://doi.org/10.1016/j.geb.2004.06.010
Article Google Scholar
Blanchard, T. C., Strait, C. E., & Hayden, B. Y. (2015). Ramping ensemble activity in dorsal anterior cingulate neurons during persistent commitment to a decision. Journal of Neurophysiology, 114 (4), 2439–49. https://doi.org/10.1152/jn.00711.2015
Article PubMed PubMed Central Google Scholar
Bohanec, M. (2009). Decision making: A computer-science and information-technology viewpoint. Interdisciplinary Description of Complex Systems, 7 (2), 22–37
Google Scholar
Brand, M., Fujiwara, E., Borsutzky, S., Kalbe, E., Kessler, J., & Markowitsch, H. J. (2005). Decision-Making deficits of korsakoff patients in a new gambling task with explicit rules: associations with executive functions. Neuropsychology, 19 (3), 267–277. https://doi.org/10.1037/0894-4105.19.3.267
Broche-Pérez, Y., Jiménez, H., & Omar-Martínez, E. (2016). Neural substrates of decision-making. Neurologia, 31 (5), 319–25. https://doi.org/10.1016/j.nrl.2015.03.001
Byrnes, J. P. (2013). The nature and development of decision-making: A self-regulation model . Psychology Press
Clark, L., & Manes, F. (2004). Social and emotional decision-making following frontal lobe injury. Neurocase, 10 (5), 398–403. https://doi.org/10.1080/13554790490882799
Cummings, J. L. (1995). Anatomic and behavioral aspects of frontal-subcortical circuits a. Annals of the New York Academy of Sciences, 769 (1), 1–14
Dale, S. (2015). Heuristics and biases: The science of decision-making. Business Information Review, 32 (2), 93–99. https://doi.org/10.1177/0266382115592536
Damasio, A. R. (1996). The somatic marker hypothesis and the possible functions of the prefrontal cortex. Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences, 351 (1346), 1413–20. https://doi.org/10.1098/rstb.1996.0125
Dewberry, C., Juanchich, M., & Narendran, S. (2013). Decision-making competence in everyday life: The roles of general cognitive styles, decision-making styles and personality. Personality and Individual Differences, 55 (7), 783–788. https://doi.org/10.1016/j.paid.2013.06.012
Doya, K. (2008). Modulators of decision making. Nature Neuroscience, 11 (4), 410–6. https://doi.org/10.1038/nn2077
Dunn, B. D., Dalgleish, T., & Lawrence, A. D. (2006). The somatic marker hypothesis: a critical evaluation. Neuroscience & Biobehavioral Reviews, 30 (2), 239–71. https://doi.org/10.1016/j.neubiorev.2005.07.001
Elliott, R., Rees, G., & Dolan, R. J. (1999). Ventromedial prefrontal cortex mediates guessing. Neuropsychologia, 37 (4), 403–411
Ernst, M., Bolla, K., Mouratidis, M., Contoreggi, C., Matochik, J. A., Kurian, V., et al. (2002). Decision-making in a risk-taking task: a PET study. Neuropsychopharmacology, 26 (5), 682–91. https://doi.org/10.1016/S0893-133X(01)00414-6
Ernst, M., & Paulus, M. P. (2005). Neurobiology of decision making: a selective review from a neurocognitive and clinical perspective. Biological Psychiatry, 58 (8), 597–604. https://doi.org/10.1016/j.biopsych.2005.06.004
Evans, J. S. (2008). Dual-processing accounts of reasoning, judgment, and social cognition. Annual Review of Psychology, 59, 255–78. https://doi.org/10.1146/annurev.psych.59.103006.093629
Fellows, L. K. (2004). The cognitive neuroscience of human decision making: A review and conceptual framework. Behavioral & Cognitive Neuroscience Reviews, 3 (3), 159–72. https://doi.org/10.1177/1534582304273251
Fellows, L. K., & Farah, M. J. (2007). The role of ventromedial prefrontal cortex in decision making: judgment under uncertainty or judgment per se? Cerebral Cortex, 17 (11), 2669–74. https://doi.org/10.1093/cercor/bhl176
Fehr, E., & Camerer, C. F. (2007). Social neuroeconomics: the neural circuitry of social preferences. Trends in Cognitive Sciences, 11 (10), 419–27. https://doi.org/10.1016/j.tics.2007.09.002
Finucane, M. L., Alhakami, A., Slovic, P., & Johnson, S. M. (2000). The affect heuristic in judgments of risks and benefits. Journal of Behavioral Decision Making, 13, 1–17. https://doi.org/10.1002/(SICI)1099-0771(200001/03)13:1<1::AID-BDM333>3.0.CO;2-S
Fischhoff, B. (2010). Judgment and decision making. Wiley Interdisciplinary Reviews: Cognitive Science, 1 (5), 724–735. https://doi.org/10.1002/wcs.65
Forte, G., Favieri, F., & Casagrande, M. (2019). Heart rate variability and cognitive function: a systematic review. Frontiers in Neuroscience, 13, 710
Forte, G., Morelli, M., & Casagrande, M. (2021). Heart rate variability and decision-making: autonomic responses in making decisions. Brain Sciences, 11 (2), 243
Forte, G., Favieri, F., Oliha, E. O., Marotta, A., & Casagrande, M. (2021). Anxiety and attentional processes: the role of resting heart rate variability. Brain Sciences, 11 (4), 480
Frith, C. D., & Singer, T. (2008). The role of social cognition in decision making. Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences, 363 (1511), 3875–86. https://doi.org/10.1098/rstb.2008.0156
Galotti, K. M. (2002). Making decisions that matter: How people face important life choices . Lawrence Erlbaum Associates Publishers
Gigerenzer, G., & Gaissmaier, W. (2011). Heuristic decision making. Annual Review of Psychology, 62, 451–82. https://doi.org/10.1146/annurev-psych-120709-145346
Gigerenzer, G., & Selten, R. (Eds.). (2001). Bounded Rationality: The Adaptive Toolbox . MIT Press
Goel, V., Gold, B., Kapur, S., & Houle, S. (1998). Neuroanatomical correlates of human reasoning. Journal of Cognitive Neuroscience, 10 (3), 293–302
Gold, J. I., & Shadlen, M. N. (2007). The neural basis of decision making. Annual Review of Neuroscience, 30, 535–74. https://doi.org/10.1146/annurev.neuro.29.051605.113038
Gottlieb, J. (2007). From thought to action: the parietal cortex as a bridge between perception, action, and cognition. Neuron, 53 (1), 9–16. https://doi.org/10.1016/j.neuron.2006.12.009
Gozli, D. G. (2017). Behaviour versus performance: The veiled commitment of experimental psychology. Theory & Psychology, 27, 741–758
Gozli, D. (2019). Free Choice. Experimental Psychology and Human Agency . Springer. https://doi.org/10.1007/978-3-030-20422-8_6
Group, T. M. A. D., Fawcett, T. W., Fallenstein, B., Higginson, A. D., Houston, A. I., Mallpress, D. E., & McNamara, J. M., …. (2014). The evolution of decision rules in complex environments. Trends in Cognitive Sciences , 18 (3), 153–161
Guess, C. (2004). Decision making in individualistic and collectivistic cultures. Online Readings in Psychology and Culture , 4 (1). https://doi.org/10.9707/2307-0919.1032
Gupta, R., Koscik, T. R., Bechara, A., & Tranel, D. (2011). The amygdala and decision-making. Neuropsychologia, 49 (4), 760–6. https://doi.org/10.1016/j.neuropsychologia.2010.09.029
Heilbronner, S. R., & Hayden, B. Y. (2016). Dorsal anterior cingulate cortex: a bottom-up view. Annual Review of Neuroscience, 39, 149–70. https://doi.org/10.1146/annurev-neuro-070815-013952
Hickson, L., & Khemka, I. (2014). The psychology of decision making. International review of research in developmental disabilities (Vol 47, pp. 185–229). Academic
Johnson, J. G., & Busemeyer, J. R. (2010). Decision making under risk and uncertainty. Wiley Interdisciplinary Reviews: Cognitive Science, 1 (5), 736–749. https://doi.org/10.1002/wcs.76
Kable, J. W., & Glimcher, P. W. (2009). The neurobiology of decision: consensus and controversy. Neuron , 63 (6),733–45. https://doi.org/10.1016/j.neuron.2009.09.003
Kahneman, D. (2003). A perspective on judgment and choice. Mapping bounded rationality. American Psychologist, 58 (9), 697–720. https://doi.org/10.1037/0003-066X.58.9.697
Kahneman, D. (2011). P ensieri lenti e veloci . Trad.it. a cura di Serra, L., Arnoldo Mondadori Editore
Kahneman, D., & Tversky, A. (1979). Prospect theory: an analysis of decision under risk. Econometrica, 47 (2), 263–292
Kheramin, S., Body, S., Mobini, S., Ho, M. Y., Velázquez-Martinez, D. N., Bradshaw, C. M., et al. (2002). Effects of quinolinic acid-induced lesions of the orbital prefrontal cortex on inter-temporal choice: a quantitative analysis. Psychopharmacology (Berl), 165 (1), 9–17. https://doi.org/10.1007/s00213-002-1228-6
Lee, V. K., & Harris, L. T. (2013). How social cognition can inform social decision making. Frontiers in Neuroscience, 7, 259. https://doi.org/10.3389/fnins.2013.00259
Lerner, J. S., Li, Y., Valdesolo, P., & Kassam, K. S. (2015). Emotion and decision making. Annual Review of Psychology, 66 , 799–823
Loewenstein, G., Weber, E. U., Hsee, C. K., & Welch, N. (2001). Risk as feelings. Psychological Bulletin, 127 (2), 267–286. https://doi.org/10.1037/0033-2909.127.2.267
Mather, M. (2006). A review of decision-making processes: weighing the risks and benefits of aging. In Carstensen, L. L., & Hartel, C. R. (Eds.), & Committee on Aging Frontiers in Social Psychology, Personality, and Adult Developmental Psychology, Board on Behavioral, Cognitive, and Sensory Sciences, When I’m 64 (pp. 145–173). National Academies Press
Mazzucchi, L. (2012). La riabilitazione neuropsicologica: Premesse teoriche e applicazioni cliniche (3rd ed.). EDRA
Mishra, S. (2014). Decision-making under risk: integrating perspectives from biology, economics, and psychology. Personality and Social Psychology Review, 18 (3), 280–307. https://doi.org/10.1177/1088868314530517
Moreira, C. (2018). Unifying decision-making: a review on evolutionary theories on rationality and cognitive biases. arXiv preprint arXiv:1811.12455
Naqvi, N., Shiv, B., & Bechara, A. (2006). The role of emotion in decision making: a cognitive neuroscience perspective. Current Directions in Psychological Science, 15 (5), 260–264. https://doi.org/10.1111/j.1467-8721.2006.00448.x
O’Doherty, J. P., Buchanan, T. W., Seymour, B., & Dolan, R. J. (2006). Predictive neural coding of reward preference involves dissociable responses in human ventral midbrain and ventral striatum. Neuron, 49 (1), 157–66. https://doi.org/10.1016/j.neuron.2005.11.014
Padoa-Schioppa, C., & Assad, J. A. (2008). The representation of economic value in the orbitofrontal cortex is invariant for changes of menu. Nature Neuroscience, 11 (1), 95–102. https://doi.org/10.1038/nn2020
Palombo, D. J., Keane, M. M., & Verfaellie, M. (2015). How does the hippocampus shape decisions? Neurobiology of Learning and Memory, 125, 93–7. https://doi.org/10.1016/j.nlm.2015.08.005
Pardo-Vazquez, J. L., Padron, I., Fernandez-Rey, J., & Acuña, C. (2011). Decision-making in the ventral premotor cortex harbinger of action. Frontiers in Integrative Neuroscience, 5, 54. https://doi.org/10.3389/fnint.2011.00054
Paulus, M. P., & Yu, A. J. (2012). Emotion and decision-making: affect-driven belief systems in anxiety and depression. Trends in Cognitive Science, 16, 476–483. https://doi.org/10.1016/j.tics.2012.07.009
Payne, J. W. (1973). Alternative approaches to decision making under risk: Moments versus risk dimensions. Psychological Bulletin, 80 (6), 439–453. https://doi.org/10.1037/h0035260
Payne, J. W., Payne, J. W., Bettman, J. R., & Johnson, E. J. (1993). The adaptive decision maker . Cambridge University Press
Phelps, E. A., Lempert, K. M., & Sokol-Hessner, P. (2014). Emotion and decision making: multiple modulatory neural circuits. Annual Review of Neuroscience, 37, 263–287
Pronin, E. (2007). Perception and misperception of bias in human judgment. Trends in Cognitive Sciences, 11 (1), 37–43
Rangel, A., Camerer, C., & Read Montague, P. (2008). Neuroeconomics: The neurobiology of value-based decision-making. Nature Reviews Neuroscience, 9 (7), 545–556. https://doi.org/10.1038/nrn2357
Reyna, V. F., & Lloyd, F. J. (2006). Physician decision making and cardiac risk: Effects of knowledge, risk perception, risk tolerance, and fuzzy processing. Journal of Experimental Psychology: Applied, 12 (3), 179–195. https://doi.org/10.1037/1076-898X.12.3.179
Rilling, J. K., & Sanfey, A. G. (2011). The neuroscience of social decision-making. Annual Review of Psychology, 62, 23–48. https://doi.org/10.1146/annurev.psych.121208.131647
Robinson, D. N. (2016). Explanation and the “brain sciences". Theory & Psychology, 26 (3), 324–332
Robbins, T. W., James, M., Owen, A. M., Sahakian, B. J., McInnes, L., & Rabbitt, P. (1994). Cambridge Neuropsychological Test Automated Battery (CANTAB): a factor analytic study of a large sample of normal elderly volunteers. Dementia, 5 (5), 266–81. https://doi.org/10.1159/000106735
Rogers, R. D., Owen, A. M., Middleton, H. C., Williams, E. J., Pickard, J. D., Sahakian, B. J., et al. (1999). Choosing between small, likely rewards and large, unlikely rewards activates inferior and orbital prefrontal cortex. The Journal of Neuroscience, 19 (20), 9029–9038. https://doi.org/10.1523/JNEUROSCI.19-20-09029.1999
Rolls, E. T., & Baylis, L. L. (1994). Gustatory, olfactory, and visual convergence within the primate orbitofrontal cortex. The Journal of Neuroscience, 14 (9), 5437–52. https://doi.org/10.1523/JNEUROSCI.14-09-05437.1994
Rolls, E. T., Critchley, H. D., Browning, A. S., Hernadi, I., & Lenard, L. (1999). Responses to the sensory properties of fat of neurons in the primate orbitofrontal cortex. The Journal of Neuroscience, 19 (4), 1532–40. https://doi.org/10.1523/JNEUROSCI.19-04-01532.1999
Rosenbloom, M. H., Schmahmann, J. D., & Price, B. H. (2012). The functional neuroanatomy of decision-making. The Journal of Neuropsychiatry and Clinical Neurosciences, 24 (3), 266–77. https://doi.org/10.1176/appi.neuropsych.11060139
Rushworth, M. F., & Behrens, T. E. (2008). Choice, uncertainty and value in prefrontal and cingulate cortex. Nature Neuroscience, 11 (4), 389–97. https://doi.org/10.1038/nn2066
Sanfey, A. G. (2007). Social decision-making: insights from game theory and neuroscience. Science, 318 (5850), 598–602. https://doi.org/10.1126/science.1142996
Serra, L., Bruschini, M., Ottaviani, C., Di Domenico, C., Fadda, L., Caltagirone, C., et al. (2019). Thalamocortical disconnection affects the somatic marker and social cognition: a case report. Neurocase, 25 (1–2), 1–9. https://doi.org/10.1080/13554794.2019.1599025
Shahsavarani, A. M., & Abadi, E. A. M. (2015). The bases, principles, and methods of decision-making: A review of literature. International Journal of Medical Reviews, 2 (1), 214–225
Slovic, P., Finucane, M. L., Peters, E., & MacGregor, D. G. (2002). Rational actors or rational fools: Implications of the affect heuristic for behavioral economics. Journal of Socio-Economics, 31 (4), 329–342. https://doi.org/10.1016/S1053-5357(02)00174-9
Slovic, P., Finucane, M. L., Peters, E., & MacGregor, D. G. (2004). Risk as analysis and risk as feelings: some thoughts about affect, reason, risk, and rationality. Risk Analysis, 24, 311–322. https://doi.org/10.1111/j.0272-4332.2004.00433.x
Staerklé, C. (2015). Political Psychology. International Encyclopedia of the Social & Behavioral Sciences , 427–433. https://doi.org/10.1016/B978-0-08-097086-8.24079-8
Tremblay, S., Sharika, K. M., & Platt, M. L. (2017). Social decision-making and the brain: a comparative perspective. Trends in Cognitive Sciences, 21 (4), 265–276. https://doi.org/10.1016/j.tics.2017.01.007
Trepel, C., Fox, C. R., & Poldrack, R. A. (2005). Prospect theory on the brain? Toward a cognitive neuroscience of decision under risk. Brain Research. Cognitive Brain Research, 23 (1), 34–50. https://doi.org/10.1016/j.cogbrainres.2005.01.016
Van Der Pligt, J. (2015). Decision making, psychology of. International Encyclopedia of the Social & Behavioral Sciences, 2 (5), 917–922. https://doi.org/10.1016/B978-0-08-097086-8.24014-2
Von Neumann, J., & Morgenstern, O. (1944). Theory of games and economic behavior . Princeton University Press
Weber, E. U., & Hsee, C. K. (2000). Culture and individual judgment and decision making. Applied Psychology: An International Journal, 49, 32–61. https://doi.org/10.1111/1464-0597.00005
Weller, J. A., Levin, I. P., Shiv, B., & Bechara, A. (2009). The effects of insula damage on decision-making for risky gains and losses. Society for Neuroscience, 4 (4), 347–58. https://doi.org/10.1080/17470910902934400
Williams, D. J., & Noyes, J. M. (2007). How does our perception of risk influence decision-making? Implications for the design of risk information. Theoretical Issues in Ergonomics Science, 8, 1–35. https://doi.org/10.1080/14639220500484419
Yamada, H., Inokawa, H., Matsumoto, N., Ueda, Y., & Kimura, M. (2011). Neuronal basis for evaluating selected action in the primate striatum. European Journal of Neuroscience, 34 (3), 489–506. https://doi.org/10.1111/j.1460-9568.2011.07771.x
Download references
Author information
Authors and affiliations.
Dipartimento di Psicologia, Università di Roma “Sapienza”, Via dei Marsi. 78, 00185, Rome, Italy
Matteo Morelli & Giuseppe Forte
Dipartimento di Psicologia Dinamica, Clinica e Salute, Università di Roma “Sapienza”, Via degli Apuli, 1, 00185, Rome, Italy
Maria Casagrande
Body and Action Lab, IRCCS Fondazione Santa Lucia, Rome, Italy
Giuseppe Forte
You can also search for this author in PubMed Google Scholar
Corresponding authors
Correspondence to Maria Casagrande or Giuseppe Forte .
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Morelli, M., Casagrande, M. & Forte, G. Decision Making: a Theoretical Review. Integr. psych. behav. 56 , 609–629 (2022). https://doi.org/10.1007/s12124-021-09669-x
Download citation
Accepted : 09 November 2021
Published : 15 November 2021
Issue Date : September 2022
DOI : https://doi.org/10.1007/s12124-021-09669-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Decision making
- Neural correlates of decision making
- Decision-making tasks
- Decision-making theories
- Find a journal
- Publish with us
- Track your research
OPINION article
Decision-making in health and fitness.

- 1 Independent Researcher, Ormond Beach, FL, United States
- 2 Sports Performance Research Institute New Zealand, Auckland University of Technology, Auckland, New Zealand
Introduction
Lifestyle choices associated with food and exercise habits are fundamentally a complex decision-making process associated with many biological, social, and emotional variables. As this may be considered more difficult and time consuming, many people choose to make the simple straightforward and emotional decision influenced primarily by marketers and social media, giving consumers the perception of quick, positive predictable outcomes, even if they are inaccurate and appear too good to be true. Rather than a lack of consensus by scientists and clinicians on how to improve health and fitness, poor choices by consumers encouraged by advertisements and social trends may contribute to the continued growth of chronic illness and disability that leads to higher healthcare costs. Within this framework, modern decision-making theory may help us better understand this global problem.
Marketers selling health and fitness products and services have long since seized on our tendency to respond to advertisements that promise quick-fix solutions—especially diet and exercise fads that speak to the emotionally-run limbic system and easily grab consumer attention. Unfortunately, these initiatives often prevent people from thinking about the potential benefits and risks of using such products and services, which requires a more complex decision-making cognitive process to make the same choice. Weight loss, injury prevention , and increased energy are among the common buzzwords that quickly receive consumer's attention. Terms like fresh, natural , and local , which don't necessarily imply healthy, along with many certified organic food items, can in fact be classified as junk food. These quick-fix choices often result in postponing improved health and fitness for an individual, with wide-ranging negative outcomes; consider the current overfat pandemic with its downstream diseases and disabilities in the US, where, despite rising exercise rates, 91% of adults are now affected ( 1 , 2 ).
Since food and exercise are known to significantly influence health and fitness, and impact the development of chronic disease, disability, and premature death ( 3 ), the processes by which individuals make lifestyle choices—and their related consequences—should be an important public health concern.
Cognitive Decision-Making
Denes-Raj and Epstein ( 4 ) suggest that decision-making behavior is guided by two different cognitive processes, the first being an emotional response typical of interpersonal interactions, and the second an analytical response such as that used to solve a mathematical problem. The theory was simplified further by Amos Tversky, with Stanovich and West naming the emotional process “System 1” and the rational one “System 2” ( 5 , 6 ). Kahneman applied these ideas to economic behavior ( 7 ), with Tversky and Kahneman awarded separate Nobel prizes for their respective works. The application of System 1 and System 2 decision-making behavior in the context of health and fitness can have wide-ranging potential personal and global public health implications, and is described here as behavioral health and fitness . [ Health is defined as all areas of the body working in harmony, while fitness is the ability to perform physical activity ( 8 )].
Large numbers of people around the world attempt to regularly manage a variety of personal health and fitness routines. At its onset, this self-care process can be strongly influenced by companies selling products and services (diets, books, programs, exercise equipment) through radio and TV, online and print media, health, and fitness societies/agencies and from governmental recommendations, the latter two strongly influenced by politics and lobbying. The process is often void of individuality, encourages a one-size-fits-all notion, and can lead to dangerous herd behavior ( 9 ). These are associated with a System 1 response. Personalizing food and exercise choices require more thinking and is associated with System 2.
Characteristics of System 1 and System 2
Normally, both modes of decision-making are used in our day-to-day lives, and both have potential value. Consider System 1's first impression, an often accurate assessment of another person, place, food and physical activity. This impression may correspond to one's System 2 analysis over time. However, more often the use of images, words, sounds and other impressions in marketing, quickly sway people by enlisting System 1 to help sell unhealthy products and services.
Involving simple everyday choices that are habit- and reaction-based, usually made with little thinking, attention, or information, System 1 governs the quick decisions such as which of several doors to use when entering an office building, lanes to take on a highway, or seats to sit in at an airport. However, important decisions that can impact on immediate and long-term individual and population health and fitness are influenced if not governed by System 1 as well ( 10 ).
The System 1 process is primarily an unconscious but natural reaction, such that one's true underlying attitude or motivation for the decision is hard to come by, and the individual will likely provide one of several plausible rationalizations to justify how they made the decision. While this system is leveraged particularly well by marketers advertising products and services, it comes with the potential for strong bias and error referred to as cognitive illusions that can lead to reduced health and fitness. Fleeting first impressions appear attractive to System 1 and predominate its decision-making: Seeing a splashy colorful cover of a new diet book or a smiling lean person working out are common examples.
Relying on conscious intellect for lifestyle decision-making, System 2 requires more time to assess a particular eating plan or exercise program. In terms of self-care, it also provides an individual with the ability for ongoing monitoring of signs and symptoms that measure progress.
The more reliable and logical System 2 process can yield a personalized approach rather than a one-size-fits-all menu, and grants the ability to incorporate a planned, flexible program that can lead to improved outcomes ( 11 ). Requiring reasonable literacy, this approach offers greater autonomy, and can also reduce healthcare costs ( 12 ).
Figure 1 lists some factors associated with System 1 and System 2 decision-making.
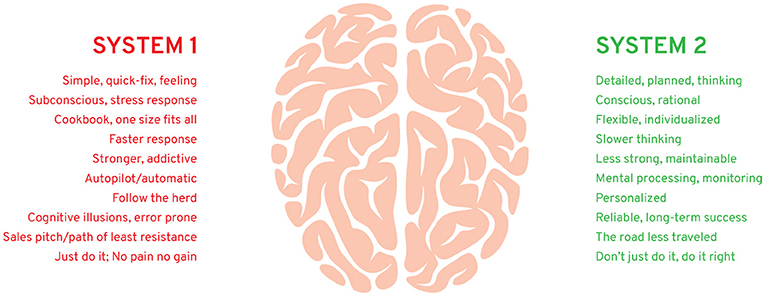
Figure 1 . Some factors associated with behavioral health and fitness.
Health practitioners can also play an important part in teaching patients about the lifestyle habits associated with their particular needs, helping them avoid making irrational or poor choices ( 3 , 13 ). However, for the benefits of health education to succeed, a high level of engagement is required. Here again, this may be impaired by society's System 1 dominance in the health and fitness arena, where consumers—patients and practitioners alike—are influenced. Unfortunately, few practitioners provide details on decision-making and modification of behavior for other related reasons: it's time-consuming, most practitioners are not knowledgeable enough, and patients are given few strategies for maintenance. Likewise, governmental recommendations are extremely simplistic, not individualized, and without encouragement.
Costs of System 1
System 1 marketing deception has been a successful business strategy for decades, selling untold numbers of health and fitness products and services that promise quick improvement that System 2 thinks is unlikely. For example, the diet industry in Europe and the United States alone has annual revenues in excess of $150 billion, and rising, yet up to two-thirds of any weight lost is regained within 1 year—and almost all is regained within 5 years, along with lost health ( 14 ).
Downstream healthcare costs continue to be high and are rising globally as well. In the US, 2014 health-care costs climbed to $3.2 trillion ( 15 ), with the Kaiser Family Foundation estimating a worldwide cumulative healthcare loss of $47 trillion between 2011 and 2030.
Examples and Misconceptions
Here, we provide two examples of how the reliance of a System 1 approach can lead to failure:
1. A person wanting to lose weight is attracted to a program claiming you can shed 10 pounds the first week. Whether initially successful or not, the diet usually fails to provide long-term results, and may cause side effects such as nutritional imbalance, metabolic impairment, and disordered eating.
2. A person wants to exercise to get into shape. Regular gym workouts encouraged by the no pain, no gain philosophy pushes the process. After a period of initial excitement, with some results realized—lost weight, more fitness—fatigue, soreness, injury, and frustration may develop causing some to give up working out. Others may become addicted to exercise, and despite pain or frustration, continue pushing through it, increasing stress hormones that impair health and fitness.
System 1-based marketing has spawned many popular misconceptions, trendy fads, and rally cries that become unhealthy social mantras. Below are two popular and very successful examples:
1. No pain, no gain . Perhaps the first social description of no-pain no-gain came from Benjamin Franklin in his writings on capitalism ( 16 ). But in the fitness arena, this rallying cry glorifies pain and the high rates of preventable injury. It overshadows the scientific consensus (System 2), considered more effective and healthy. Bill Bowerman, legendary sports coach and co-founder of Nike, said, “The idea that the harder you work, the better you're going to be is just garbage. The greatest improvement is made by the man or woman who works most intelligently.”
2. Just do it . Ironically, this popular Nike ad slogan, which appeared later in the company's evolution, communicates the System 1 message that it is enough to simply make a snap judgment to follow a certain exercise ritual without further consideration, encouraging a herd mentality ( 9 ). System 2 might think, don't just do it, do it right .
The New Players
Mobile trackers are the relatively new players in the health and fitness arena, and enlist primarily System 1 due to their emphasis on gaming and gamification. As they collect largely irrelevant data, users tend to give up on them within 6 months ( 17 ). Despite this, analysts at Morgan Stanley believe these devices will become a $1.6 trillion business in the near future ( 18 ). Indeed, the System 1 slant of mobile trackers, in the absence of more substantive and sophisticated analytics that engage System 2 thinking, may contribute to their early abandonment and demise: there is little reason to continue engaging the user through System 2 once System 1 thinking has run its course, at which point the user moves on to the next new device or program that captures the attention of System 1.
A Public Health Choice
The purpose of public health includes informing and educating the public, mobilizing community partnerships, developing policies to support health goals, and enforcing related laws and regulations ( 19 ). Despite the reality that many consumers use System 1 thinking to make unhealthy lifestyle choices, public health officials, health practitioners, policy makers, and others must work out how best to interact with an existing System 1 process to reverse this trend ( 13 , 20 ). Exploiting System 1 can help make health and fitness habitual, a process accomplished many times with whole populations reducing health-related risks through public health actions. Wide et al. ( 21 ) showed that a brief psychological intervention in young adults with a high prevalence of dental caries led to an immediate positive effect with improved oral health behaviors. The use of seatbelts has significantly reduced injury and death in vehicular accidents due to laws, high visibility enforcement, and fines, and promoting positive beliefs ( 22 ). The importance of hand washing education to help prevent infections has occurred throughout most populations ( 23 ). Promotion of self-care has also been effective in such areas as breast cancer screening behavior ( 24 ), and gestational anemia ( 25 ). While we applaud these and other public health successes, improved behavioral health and fitness promotions are urgently needed, while reducing the advertisement of unhealthy products and services to avoid drowning out the positive recommendations.
Recommendations
More specific suggestions to encourage individuals to avoid making poor diet and exercise choices can be made through two general public health approaches. First is to further restrict or ban the advertising and promotion of unhealthy products and services. This is being achieved with tobacco, and is gradually being implemented now by a ban on soda sales in some schools or junk food in some hospitals, and/or through a higher tax on unhealthy products. Second, and concurrent, is the promotion of healthy options, which can also include reductions or elimination of tax on healthy foods such as fruits and vegetables. These can be attempted through System 2 approaches but simplified sufficiently for most people to understand, implement, and maintain. This strategy may also require more creative, simple System 1-type guidelines, not unlike traditional successful marketing, to encourage easier understanding and behavioral changes. In addition:
- Public health communication messages and campaigns should be more clear and modernized; the Institute of Medicine found a major mismatch between the health information people receive and what they understand ( 26 ).
- These lifestyle recommendations should also be updated regularly as they can quickly become outdated ( 27 ). For example, the US government has just updated recommendations for physical activity for the first time in 10 years; compared with this once a decade frequency, companies promoting unhealthy products and services are bombarding consumers on a daily basis ( 28 ).
- The promotion of education strategies has already been successfully applied to individuals performing self-care for such conditions as cardiovascular disease ( 29 ) and mild cognitive impairment ( 30 ). With a sufficient level of scientific consensus in the area of diet and exercise, similar strategies regularly implemented can help people make better choices and offset ongoing System 1 misinformation campaigns.
There is no doubt that lifestyle change is difficult, one created in great part by decades of harmful System 1 marketing. This also can feed poor self-discipline in consumers. However, with the added awareness of behavioral health and fitness, combined with the help of public health actions, the process of self-care that many consumers follow could improve discipline and intellectual judgment as part of a System 2 process that more likely brings long-term success.
When it comes to making lifestyle choices, large numbers of people around the world who practice self-care are guided by System 1 thinking primarily from corporate marketing of health and fitness products and services that have potentially grave, unhealthy consequences. This may be significantly influencing the corresponding rise of chronic disease, physical impairment, lowered mental health, reduced quality of life, and healthcare costs. It is our hope that this article could help further increase public health awareness and stimulate a more detailed plan of action for effective strategies to improve and maintain health and fitness behavior, and consequently reduce mortality and morbidity of chronic disease and disability in adults and children.
Author Contributions
PM conceived the idea for the manuscript and lead the authorship process. PL edited a draft of the manuscript and contributed to the content.
Conflict of Interest Statement
PM is an independent clinical consultant, writes articles, and books that include the topics presented herein, and has a business website pertaining to health and fitness ( www.philmaffetone.com ). PL is an independent consultant, writes articles and books, and has a website pertaining to performance, health, and longevity ( www.plewsandprof.com ).
1. Maffetone PB, Rivera-Dominguez I, Laursen PB. Overfat and underfat: new terms and definitions long overdue. Front Public Health (2016) 4:279. doi: 10.3389/fpubh.2016.00279
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Maffetone PB, Laursen PB. The prevalence of overfat adults and children in the US. Front Public Health (2017) 5:290. doi: 10.3389/fpubh.2017.00290
3. Adams RJ. Improving health outcomes with better patient understanding and education. Risk Manag Healthc Policy (2010) 3:61–72. doi: 10.2147/RMHP.S7500
4. Denes-Raj V, Epstein S. Conflict between intuitive and rational processing: when people behave against their better judgment. J Pers Soc Psychol. (1994) 66:819–29. doi: 10.1037/0022-3514.66.5.819
5. Tversky A, Kahneman D. Judgment under uncertainty: Heuristics and biases. In: Kahneman D, Slovic P, Tversky A, editors. Judgment Under Uncertainty: Heuristics and Biases. New York, NY: Cambridge University Press (1982).
PubMed Abstract | Google Scholar
6. Stanovich KE, West RF. Individual differences in reasoning: implications for the rationality debate? Behav Brain Sci. (2000) 23:645–65; discussion 665–726. doi: 10.1017/S0140525X00003435
7. Kahneman D. A perspective on judgment and choice: mapping bounded rationality. Am Psychol. (2003) 58:697–720. doi: 10.1037/0003-066X.58.9.697
8. Maffetone PB, Laursen PB. Athletes: fit but unhealthy? Sports Med Open (2015) 2:24. doi: 10.1186/s40798-016-0048-x
9. Banerjee AV. A simple model of herd behavior. Q J Econ. (1992) 107:797–817. doi: 10.2307/2118364
CrossRef Full Text | Google Scholar
10. Kahneman D. Thinking, Fast and Slow. London: Penguin (2011).
Google Scholar
11. Chodosh J, Morton SC, Mojica W, Maglione M, Suttorp MJ, Hilton L, et al. Meta-analysis: chronic disease self-management programs for older adults. Ann Intern Med. (2005) 143:427–38. doi: 10.7326/0003-4819-143-6-200509200-00007
12. Anderson K, Burford O, Emmerton L. Mobile health apps to facilitate self-care: a qualitative study of user experiences. PLoS ONE (2016) 11:e0156164. doi: 10.1371/journal.pone.0156164
13. Polak L. Making health habitual. Br J Gen Pract. (2013) 63:70–1. doi: 10.3399/bjgp13X662966
14. Dulloo AG, Montani JP. Pathways from dieting to weight regain, to obesity and to the metabolic syndrome: an overview. Obes Rev. (2015) 16(Suppl. 1):1–6. doi: 10.1111/obr.12250
15. Martin AB, Hartman M, Benson J, Catlin A National Health Expenditure Accounts T. National health spending in 2014: faster growth driven by coverage expansion and prescription drug spending. Health Aff. (2016) 35:150–60. doi: 10.1377/hlthaff.2015.1194
16. Reinert SA. The way to wealth around the world: Benjamin Franklin and the Globalization of American Capitalism. Am Hist Rev . (2015) 120:61–97. doi: 10.1093/ahr/120.1.61
17. Michael A. Major Trends in the Wearable Devices Industry [Online] (2016). Available online at: http://www.wearabledevices.com/2016/01/05/major-trends-in-the-wearable-devices-industry/ (Accessed Oct 18, 2018).
18. Danova T. Just 3.3 Million Fitness Trackers Were Sold in the US in the Past Year [Online] . Business Insider (2014). Available online at: https://www.businessinsider.com/33-million-fitness-trackers-were-sold-in-the-us-in-the-past-year-2014-5 (Accessed Oct 18, 2018).
19. Stover GN, Bassett MT. Practice is the purpose of public health. Am J Public Health (2003) 93:1799–801. doi: 10.2105/AJPH.93.11.1799
20. Gardner B, Lally P, Wardle J. Making health habitual: the psychology of ‘habit-formation' and general practice. Br J Gen Pract. (2012) 62:664–6. doi: 10.3399/bjgp12X659466
21. Wide U, Hagman J, Werner H, Hakeberg M. Can a brief psychological intervention improve oral health behaviour? A randomised controlled trial. BMC Oral Health (2018) 18:163. doi: 10.1186/s12903-018-0627-y
22. Buckley L, Jones MLH, Ebert SM, Reed MP, Hallman JJ. Evaluating an intervention to improve belt fit for adult occupants: promoting positive beliefs. J Safety Res. (2018) 64:105–11. doi: 10.1016/j.jsr.2017.12.012
23. Ataee RA, Ataee MH, Mehrabi Tavana A, Salesi M. Bacteriological aspects of hand washing: a key for health promotion and infections control. Int J Prev Med. (2017) 8:16. doi: 10.4103/2008-7802.201923
24. Saei Ghare Naz M, Simbar M, Rashidi Fakari F, Ghasemi V. Effects of model-based interventions on breast cancer screening behavior of women: a systematic review. Asian Pac J Cancer Prev. (2018) 19:2031–41. doi: 10.22034/APJCP.2018.19.8.2031
25. Seshan V, Alkhasawneh E, Al Kindi S, Al Simadi FA, Arulappan J. Can gestational anemia be alleviated with increased awareness of its causes and management strategies? implications for health care services. Oman Med J. (2018) 33:322–30. doi: 10.5001/omj.2018.59
26. Nielsen-Bohlman L, Panzer AM, Kindig DA. Health Literacy: A Prescription to End Confusion . Washington, DC: The National Academies Press (2004).
27. Martinez Garcia L, Sanabria AJ, Garcia Alvarez E, Trujillo-Martin MM, Etxeandia-Ikobaltzeta I, Kotzeva A, et al. The validity of recommendations from clinical guidelines: a survival analysis. CMAJ (2014) 186:1211–9. doi: 10.1503/cmaj.140547
28. Physical Activity Guidelines for Americans (Online). President's Council on Sports, Fitness and Nutrition. U.S. Department of Health and Human Services . Available online at: https://www.hhs.gov/fitness/be-active/physical-activity-guidelines-for-americans/index.html (Accessed Nov 16, 2018).
29. Riegel B, Moser DK, Buck HG, Dickson VV, Dunbar SB, Lee CS, et al. Self-care for the prevention and management of cardiovascular disease and stroke: a scientific statement for healthcare professionals from the American Heart Association. J Am Heart Assoc. (2017) 6:e006997. doi: 10.1161/JAHA.117.006997
30. Vanoh D, Ishak IH, Shahar S, Manaf ZA, Ali NM, Noah SM. Development and assessment of a web-based intervention for educating older people on strategies promoting healthy cognition. Clin Interv Aging (2018) 13:1787–98. doi: 10.2147/CIA.S157324
Keywords: chronic disease, consumer choice behavior, emotion reactivity, system 1 and system 2, health education, diet, exercise
Citation: Maffetone PB and Laursen PB (2019) Decision-Making in Health and Fitness. Front. Public Health 7:6. doi: 10.3389/fpubh.2019.00006
Received: 25 October 2018; Accepted: 08 January 2019; Published: 23 January 2019.
Reviewed by:
Copyright © 2019 Maffetone and Laursen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Philip B. Maffetone, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- Open access
- Published: 29 March 2022
A framework of evidence-based decision-making in health system management: a best-fit framework synthesis
- Tahereh Shafaghat 1 , 2 na1 ,
- Peivand Bastani ORCID: orcid.org/0000-0002-0412-0267 1 , 3 na1 ,
- Mohammad Hasan Imani Nasab 4 ,
- Mohammad Amin Bahrami 1 ,
- Mahsa Roozrokh Arshadi Montazer 5 ,
- Mohammad Kazem Rahimi Zarchi 2 &
- Sisira Edirippulige 6
Archives of Public Health volume 80 , Article number: 96 ( 2022 ) Cite this article
11k Accesses
7 Citations
6 Altmetric
Metrics details
Scientific evidence is the basis for improving public health; decision-making without sufficient attention to evidence may lead to unpleasant consequences. Despite efforts to create comprehensive guidelines and models for evidence-based decision-making (EBDM), there isn`t any to make the best decisions concerning scarce resources and unlimited needs . The present study aimed to develop a comprehensive applied framework for EBDM.
This was a Best-Fit Framework (BFF) synthesis conducted in 2020. A comprehensive systematic review was done via six main databases including PUBMED, Scopus, Web of Science, Science Direct, EMBASE, and ProQuest using related keywords. After the evidence quality appraisal, data were extracted and analyzed via thematic analysis. Results of the thematic analysis and the concepts generated by the research team were then synthesized to achieve the best-fit framework applying Carroll et al. (2013) approach.
Four thousand six hundred thirteen studies were retrieved, and due to the full-text screening of the studies, 17 final articles were selected for extracting the components and steps of EBDM in Health System Management (HSM). After collecting, synthesizing, and categorizing key information, the framework of EBDM in HSM was developed in the form of four general scopes. These comprised inquiring, inspecting, implementing, and integrating, which included 10 main steps and 47 sub-steps.
Conclusions
The present framework provided a comprehensive guideline that can be well adapted for implementing EBDM in health systems and related organizations especially in underdeveloped and developing countries where there is usually a lag in updating and applying evidence in their decision-making process. In addition, this framework by providing a complete, well-detailed, and the sequential process can be tested in the organizational decision-making process by developed countries to improve their EBDM cycle.
Peer Review reports
Globally, there is a growing interest in using the research evidence in public health policy-making [ 1 , 2 ]. Public health systems are diverse and complex, and health policymakers face many challenges in developing and implementing policies and programs that are required to be efficient [ 1 , 3 ]. The use of scientific evidence is considered to be an effective approach in the decision-making process [ 3 , 4 , 5 ]. Due to the lack of sufficient resources, evidence-based decision-making ( EBDM) is regarded as a way to optimize costs and prevent wastes [ 6 ]. At the same time, the direct consequence of ignoring evidence is poorer health for the community [ 7 ].
Evidence suggests that health systems often fail to exploit research evidence properly, leading to inefficiencies, death or reduced quality of citizens’ lives, and a decline in productivity [ 8 ]. Decision-making in the health sector without sufficient attention to evidence may lead to a lack of effectiveness, efficiency, and fairness in health systems [ 9 ]. Instead, the advantages of EBDM include adopting cost-effective interventions, making optimal use of limited resources, increasing customer satisfaction, minimizing harm to individuals and society, achieving better health outcomes for individuals and society [ 10 , 11 ], as well as increasing the effectiveness and efficiency of public health programs [ 12 ].
Using the evidence in health systems’ policymaking is a considerable challenging issue that many developed and developing countries are facing nowadays. This is particularly important in the latter, where their health systems are in a rapid transition [ 13 ]. For instance, although in 2012, a study in European Union countries showed that health policymakers rarely had necessary structures, processes, and tools to exploit research evidence in the policy cycle [ 14 ], the condition can be worse among the developing and the underdeveloped ones. For example, evidence-based policy-making in developing countries like those located in the Middle East can have more significant impacts [ 15 , 16 ]. In such countries resources are generally scarce, so the policymakers' awareness of research evidence becomes more important [ 17 ]. In general, low and middle-income countries have fewer resources to deal with health issues and need quality evidence for efficient use of these resources [ 7 ].
Since the use of EBDM is fraught with the dilemma of most pressing needs and having the least capacity for implementation especially in developing countries [ 16 ], efforts have been made to create more comprehensive guidelines for EBDM in healthcare settings, in recent years [ 18 ]. Stakeholders are significantly interested in supporting evidence-based projects that can quickly prioritize funding allocated to health sectors to ensure the effective use of their financial resources [ 19 , 20 , 21 ]. However, it is unlikely that the implementation of EBDM in Health System Management (HSM) will follow the evidence-based medicine model [ 10 , 22 ]. On the other hand, the capacity of organizations to facilitate evidence utilization is complex and not well understood [ 22 ], and the EBDM process is not usually institutionalized within the organizational processes [ 10 ]. A study in 2005 found that few organizations support the use of research evidence in health-related decisions, globally [ 23 ]. Weis et al. (2012) also reported there is insufficient information on EBDM in local health sectors [ 12 ]. In general, it can be emphasized that relatively few organizations hold themselves accountable for using research evidence in developing health policies [ 24 ]. To the best of our knowledge, there isn`t any comprehensive global and practical model developed for EBDM in health systems/organizations management. Accordingly, the present study aimed to develop a comprehensive framework for EBDM in health system management. It can shed the light on policymakers to access a detailed practical model and enable them to apply the model in actual conditions.
This was a Best Fit Framework (BFF) synthesis conducted in 2020 to develop a comprehensive framework for EBDM in HSM. Such a framework synthesis is achieved as a combination of the relevant framework, theory, or conceptual models and particularly is applied for developing a priori framework based on deductive reasoning [ 25 ]. The BFF approach is appropriate to create conceptual models to describe or express the decisions and behaviors of individuals and groups in a particular domain. This is distinct from other methods of evidence synthesis because it employs a systematic approach to create an initial framework for synthesis based on existing frameworks, models, or theories [ 25 ] for identifying and adapting theories systematically with the rapid synthesis of evidence [ 25 , 26 ]. The initial framework can be derived from a relatively well-known model in the target field, or be formed by the integration of several existing models. The initial framework is then reduced to its key components that have shaped its concepts [ 25 ]. Indeed, the initial framework considers as the basis and it can be rebuilt, extended, or reduced based on its dimensions [ 26 ]. New concepts also emerge based on the researchers' interpretation of the evidence and ongoing comparisons of these concepts across studies [ 25 ]. This approach of synthesis possesses both positivist and interpretative perspectives; it provides the simultaneous use of the well-known strengths of both framework and evidence synthesis [ 27 ].
In order to achieve this aim the following methodological steps were conducted as follows:
Searching and selection of studies
In this step, we aimed to look for the relevant models and frameworks related to evidence-based decision-making in health systems management. The main research question was “what is the best framework for EBDM in health systems?” after defining the research question, the researchers searched for published studies on EBDM in HSM in different scientific databases with relevant keywords and constraints as inclusion and exclusion criteria from 01.01.2000 to 12.31.2020 (Table 1 ).
Inclusion and exclusion criteria
Inclusion criteria were determined as the studies that identify the components or develop a model or framework of EBDM in health organization in the form of original or review articles or dissertations, which were published in English and had a full text. The studies like book reviews, opinion articles, and commentaries that lacked a specific framework for conducting our review were excluded. During the search phase of the study, we attempted as much as possible to access studies that were not included in the search process or gray literature by reviewing the references lists of the retrieved studies or by contacting the authors of the articles or experts and querying them, as well as manually searching the related sites (Fig. 1 ).
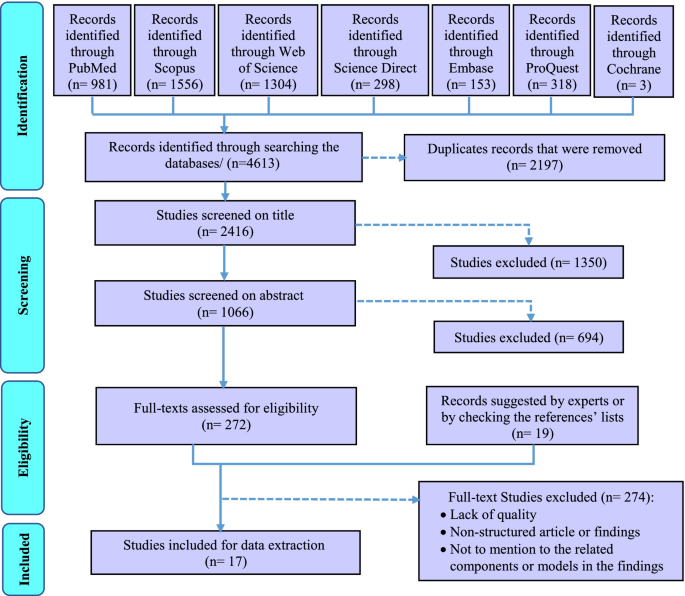
The PRISMA flowchart for selection of the studies in scoping review
Quality appraisal
The quality of the obtained studies was investigated using three tools for assessing the quality of various types of studies considering types and methods of the final include studies in systematic review. These tools were including Critical Appraisal Skills Program (CASP) for assessing the quality of qualitative researches [ 28 ], Scale for the Assessment of Narrative Review Articles (SANRA) [ 29 ], and The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers [ 30 ] (Table 3- Appendix ).
Data extraction
After searching the studies from all databases and removing duplicates, the studies were independently reviewed and screened by two members (TS and MRAM) of the research team in three phases by the title, abstract, and then the full text of the articles. At each stage of the study, the final decision to enter the study to the next stage was based on agreement and, in case of disagreement, the opinion of the third person from the research team was asked (PB). Mendeley reference manager software was used to systematically search and screen relevant studies. The data from the included studies were extracted based on the study questions and accordingly, a form of the studies’ profile including the author's name, publication year, country, study title, type of study, and its conditions were prepared in Microsoft Excel software (Table 4- Appendix ).
Synthesis and the conceptual model
In this step, a thematic analysis approach was applied to extract and analyze the data. For this purpose, first, the texts of the selected studies were read several times, and the initial qualitative codes or thematic concepts, according to the determined keywords and based on the research question, were found and labeled. Then these initial thematic codes were reviewed to achieve the final codes and they were integrated and categorized to achieve the final main themes and sub-themes, eventually. The main and the sub-themes are representative of the main and sub-steps of EBDM. At the last stage of the synthesis, the thematic analysis was finalized with 8 main themes and all the main and the sub-themes were tabulated (Table 5- Appendix ).
Creation of a new conceptual framework
For BFF synthesis in the present study, we compared the existing models and tried to find a model that fits the best. Three related models that appeared to be relatively well-suited to the purpose of this study to provide a complete, comprehensive, and practical EBDM model in HSM were found. According to the BFF instruction in Carroll et al. (2013) study [ 25 ], we decided to use all three models as the basis for the best fit because any of those models were not complete enough and we could give no one an advantage over others. Consequently, the initial model or the BFF basis was formed and the related thematic codes were classified according to the category of this basis as the main themes/steps of EBDM in HSM (Table 5- Appendix ). Then, the additional founded thematic codes were added and incorporated to this basis as the other main steps and the sub-steps of the EBDM in HSM according to the research team and some details in the form of sub-steps were added by the research team to complete the synthesized framework. Eventually, a comprehensive practical framework consisting of 10 main steps and 47 sub-steps was created with the potentiality of applying and implementing EDBM in HSM that we categorized them into four main phases (Table 6- Appendix ).
Testing the synthesis: comparison with the a priori models, dissonance and sensitivity
In order to assess the differences between the priori framework and the new conceptual framework, the authors tried to ask some experts’ opinions about the validity of the synthesized results. The group of experts has included eight specialists in the field of health system management or health policy-making. These experts have been chosen considering their previous research or experience in evidence-based decision/policy making performance/management (Table 2 ). This panel lasted in two three-hour sessions. The finalized themes and sub-themes (Table 6- Appendix ) and the new generated framework (Fig. 3 ) were provided to them before each session so that they could think and then in each meeting they discussed them. Finally, all the synthesized themes and sub-themes resulted were reviewed and confirmed by the experts.
Ethical considerations
To prevent bias, two individuals carried out all stages of the study such as screening, data extraction, and data analysis. The overall research project related to this manuscript was approved by the medical ethics conceal of the research deputy of Shiraz University of Medical Sciences with approval number IR.SUMS.REC.1396–01-07–14184, too.
The initial search across six electronic databases and the Cochrane library yielded 4613 studies. After removing duplicates, 2416 studies were assessed based on their titles. According to the abstract screening of the 1066 studies that remained after removing the irrelevant titles, 291 studies were selected and were entered into the full-text screening phase. Due to full-text screening of the studies, 17 final studies were selected for extracting the components and steps of EBDM in HSM (Fig. 1 ). The features of these studies were summarized in Table 4- Appendix (see supplementary data). Furthermore, according to the quality appraisal of the included studies, the majority of them had an acceptable level of quality. These results have been shown in Table 3- Appendix .
Results of the thematic analysis of the evidence (Table 5- Appendix ) along with the concepts proposed and added by the research team according to the focus-group discussion of the experts were shown in Table 6- Appendix . Accordingly, the main steps and related sub-steps of the EBDM process in HSM were defined and categorized.
After collecting, synthesizing, and categorizing thematic concepts, incorporating them with the initial models, and adding the additional main steps and sub-steps to the basic models, the final synthesized framework as a best-fit framework for EBDM in HSM was developed in the form of four general phases of inquiring, inspecting, implementing, and integrating and 10 main steps (Fig. 2 ). For better illustration, this framework with all the main steps and 47 sub-steps has been shown in Fig. 3 , completely.

The final synthesized framework of evidence-based decision-making in health system management
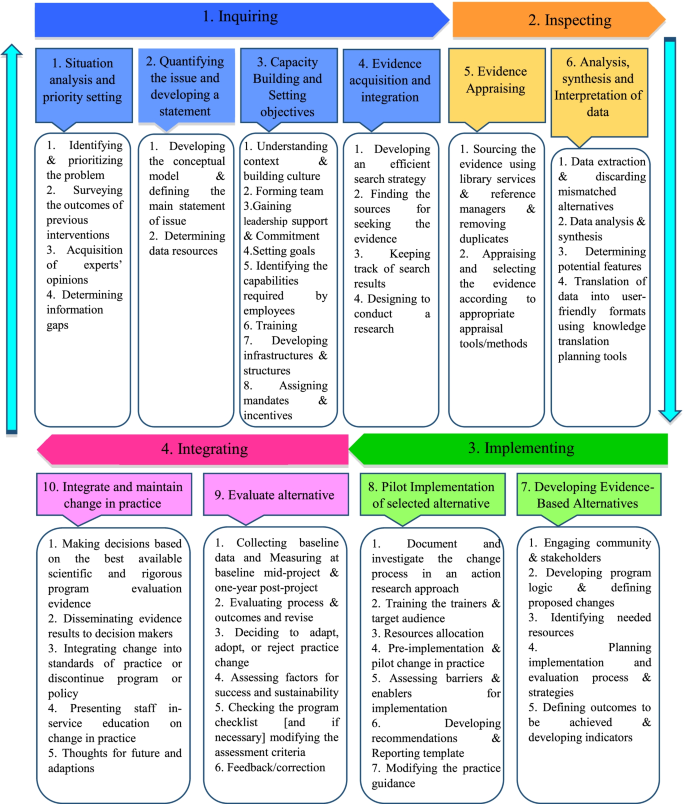
The main steps and sub-steps of the framework of EBDM in health system management
In the present study, a comprehensive framework for EBDM in HSM was developed. This model has different distinguishing characteristics than the formers. First of all, this is a comprehensive practical model that combined the strengths and the crucial components of the limited number of previous models; second, the model includes more details and complementary steps and sub-steps for full implementation of EBDM in health organizations and finally, the model is benefitted from a cyclic nature that has a priority than the linear models. Concerning the differences between the present framework and other previous models in this field, it must be said that most of the previous models related to EBDM were presented in the scope of medicine (that they were excluded from our SR according to the study objectives and exclusion criteria). A significant number of those models were proposed for the scope of public health and evidence-based practice, and only a limited number of them focused exactly on the scope of management and policy/decision making in health system organizations.
Given that the designed model is a comprehensive 10-step model, it can be used in some way at all levels of the health system and even in different countries. However, there will be a difference here, given that this framework provides a practical guide and a comprehensive guideline for applying evidence-based decision-making approach in health systems organizations, at each level of the health system in each country, this management approach can be applied depending on their existing infrastructure and the processes that are already underway (such as capacity building, planning, data collection, etc.), and at the same time, with a general guide, they can provide other infrastructure as well as the prerequisites and processes needed to make this approach much more possible and applicable.
It is true that evidence-based management is different from evidence-based medicine and even more challenging (due to lack of relevant data, greater sensitivity in data collection and their accuracy, lack of consistency and lack of transparency in the implementation of evidence-based decision-making in management rather than evidence-based medicine, etc.). Still, the general framework provided in this article can be used to help organizations that really want to act and move forward through this approach.
Furthermore, based on the findings, most of the previous studies only referred to some parts of the components and steps of the EBDM in health organizations and neglected the other parts or they were not sufficiently comprehensive [ 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 ]. Most of the previous models did not mention the necessary sub-steps, tools, and practical details for accurate and complete implementation of the EBDM, which causes the organizations that want to use these models, will be confused and cannot fully implement and complete the EBDM cycle. Among the studies that have provided a partly complete model than the other studies, were the studies by Brownson (2009), Yost (2014), and Janati (2018) [ 3 , 41 , 42 ]. Consequently, the combination of these three studies has been used as the initial framework for the best-fit synthesis in the present study.
Likewise, the models presented by Brownson (2009) and Janati (2018) were only limited to the six or seven key steps of the EBDM process, and they did not mention the details required for doing in each step, too [ 3 , 4 , 42 ]. Also, the model presented in the study of Janati (2018) was linear, and the relationships between the EBDM components were not well considered [ 42 , 43 ]; however, the model presented in this study was recursive. Also, in Yost's study (2014), despite the 7 main steps of EBDM and some details of each of the steps, the proposed process was not schematically drawn in the form of a framework and therefore the relationships between steps and sub-steps were not clear [ 41 ]. According to what was discussed, the best-fit framework makes the possibility of concentrating the fragmented models to a comprehensive one that can be fully applied and evaluated by the health systems policymakers and managers.
In the present study, the framework of EBDM in HSM was developed in the form of four general scopes of inquiring, inspecting, implementing, and integrating including 10 main steps and 47 sub-steps. These scopes were discussed as follows:
In the first step, “situation analysis and priority setting”, the most frequently cited sub-step was identifying and prioritizing the problem. Accordingly, Falzer (2009), emphasized the importance of identifying the decision-making conditions and the relevant institutions and determining their dependencies as the first steps of EBDM [ 44 ]. Aas (2012) has also cited the assessment of individuals and problem status and problem-finding as the first steps of EBDM [ 34 ]. Moreover, the necessity of identifying the existing situation and issues and prioritizing them has been emphasized as the initial steps in most management models such as environmental analysis in strategic planning [ 45 ].
Despite considering the opinions and experience of experts and managers as one of the important sources of evidence for decision-making [ 42 , 46 , 47 , 48 , 49 , 50 ], many studies did not mention this sub-step in the EBDM framework. Hence, the present authors added the acquisition of experts’ opinions as a sub-step of the first step because of its important role in achieving a comprehensive view of the overall situation.
In the second step, “quantifying the issue and developing a statement”, “Developing the conceptual model for the issue” was more addressed [ 37 , 41 , 47 ]. In addition, the authors to complete this step added the fourth sub-step, “Defining the main statement of issue”. This is because that most of the problems in health settings may have a similar value for managers and decision-makers and quantifying them can be used as a criterion for more attention or selecting the problem as the main issue to solve.
The third step, “Capacity building and setting objectives”, was not seen in many other included studies as a main step in EBDM, however, the present authors include this as a main step because without considering the appropriate objectives and preparing necessary capacities and infrastructures, entering to the next steps may become problematic. Moreover, in numerous studies, factors such as knowledge and skills of human resources, training, and the availability of the essential structures and infrastructures have been identified as facilitators of EBDM [ 51 , 52 , 53 , 54 , 55 ]. According to this justification, they are included in the present framework as sub-steps of the third step.
Considering the third step and based on the knowledge extracted from the previous studies, the three sub-steps of “understanding context and Building Culture” [ 56 , 57 ], “gaining the support and commitment of leaders” [ 39 , 57 , 58 ], and “identifying the capabilities required by employees and their skills weaknesses” [ 58 , 59 , 60 ] were the most important sub-steps in this step of EBDM framework. In this regard, Dobrow (2004) has also stated that the two essential components of any EBDM are the evidence and context of its use [ 32 ]. Furthermore, Isfeedvajani (2018) stated that to overcome barriers and persuade hospital managers and committees to apply evidence-based management and decision-making, first and foremost, creating and promoting a culture of "learning through research" was important [ 61 ].
The present findings showed that in the fourth main step, “evidence acquisition and integration”, the most important sub-step was “finding the sources for seeking the evidence” [ 39 , 40 , 41 , 60 , 62 , 63 ]. Concerning the sources for the use of evidence in decision-making in HSM, studies have cited numerous sources, most notably scientific and specialized evidence such as research, articles, academic reports, published texts, books, and clinical guidelines [ 39 , 64 , 65 ]. After scientific evidence, using the opinions and experiences of experts, colleagues, and managers [ 42 , 46 , 49 , 66 ] as well as the use of census and local level data [ 49 , 66 , 67 ], and other sources such as financial [ 67 ], political [ 42 , 49 ] and evaluations [ 49 , 68 ] data were cited.
The fifth step of the present framework, “evidence appraising”, was emphasized by previous literature; for instance, Pierson (2012) pointed to the use of library services in EBDM [ 69 ]. Appraising and selecting the evidence according to appropriate appraisal tools/methods was cited the most. International and local evidence is confirmed that ignoring these criteria can lead to serious faults in the process of decision and policy-making [ 70 , 71 ].
Furthermore, the sixth step, “analysis, synthesis, and interpretation of data”, was mentioned in many included studies [ 36 , 39 , 41 , 42 , 57 , 59 , 72 ]. This step emphasized the role of analysis and synthesis of data in the process of generation applied and useful information. It is obvious that the local interpretation according to different contexts may lead to achieving such kind of knowledge that can be used as a basis for local EBDM in HSM.
Implementing
The third scope consisted of the seventh and eighth steps of the EBDM process in HSM. In the seventh step, “developing evidence-based alternatives”, the issue of involving stakeholders in decision-making and subsequently, planning to design and implementation of the process and evaluation strategies had been focused by the previous studies [ 58 , 60 , 62 , 63 , 73 ]. Studies by Belay (2009) and Armstrong (2014) had also emphasized the need to use stakeholder and public opinion as well as local and demographic data in decision-making [ 49 , 67 ].
“Pilot-implementation of selected alternatives” was the eighth step of the framework. Some key sub-steps of this step were resources allocation [ 58 ], Pre-implementation and pilot change in practice and assessing barriers and enablers for implementation [ 40 ] that indicated the significance of testing the strategies in a pilot stage as a pre- requisition of implementing the whole alternatives. It is obvious that without attention to the pilot stage, adverse and unpleasant outcomes may occur that their correction process imposes many financial, organizational, and human costs on the originations. In addition, a study explained that one of the strategies of the decision-makers to measure the feasibility of the policy options was piloting them, which had a higher chance of being approved by the policymakers. Also, pilot implementation in smaller scales has been recommended in public health in cases of lack of sufficient evidence [ 74 ].
Integrating
This last scope consists of the ninth and tenth steps. The main sub-step of the ninth step, “evaluating alternatives”, was to evaluating process and outcomes and revise. After a successful implementation of the pilot, this step can be assured that the probable outcomes may be achieved and this evaluation will help the decision and policymakers to control the outcomes, effectively. Also, it impacts the whole target program and proposes some correcting plans through an accurate feedback process, too. Pagoto (2007) explained that a facilitator for EBDM would be an efficient and user-friendly system to assess utilization, outcomes, and perceived benefits [ 55 ].
Also, the tenth step, “integrating and maintaining change in practice”, was not considered as a major step in previous models, too, while it is important to maintain and sustain positive changes in organizational performance. In this regard, Ward (2011) also suggested several steps to maintain and sustain the widespread changes in the organization, including increasing the urgency and speed of action, forming a team, getting the right vision, negotiating for buy-in, empowerment, short-term success, not giving up and help to make a change stick [ 35 ]. Finally, the most important sub-steps that could be mentioned in this step were the dissemination of evidence results to decision-makers and the integration of changes made to existing standards and performance guidelines. Liang (2012) had also emphasized the importance of translating existing evidence into useful practices as well as disseminating them [ 47 ]. In addition, the final sub-step, “feedback and feedforward towards the EBDM framework”, was explained by the authors to complete the framework.
Some previous findings showed that about half and two-thirds of organizations do not regularly collect related data about the use of evidence, and they do not systematically evaluate the usefulness or impact of evidence use on interventions and decisions [ 75 ]. The results of a study conducted on healthcare managers at the various levels of an Iranian largest medical university showed that the status of EBDM is not appropriate. This problem was more evident among physicians who have been appointed as managers and who have less managerial and systemic attitudes [ 76 ]. Such studies, by concerning the shortcomings of current models for EBDM in HSM or even lack of a suitable and usable one, have confirmed the necessity of developing a comprehensive framework or model as a practical guide in this field. Consequently, existing and presenting such a framework can help to institutionalize the concept of EBDM in health organizations.
In contrast, results of Lavis study (2008) on organizations that supported the use of research evidence in decision-making reported that more than half of the organizations (especially institutions of health technology assessment agencies) may use the evidence in their process of decision-making [ 75 ], so applying the present framework for these organizations can be recommended, too.
Limitations
One of the limitations of the present study was the lack of access to some studies (especially gray literature) related to the subject in question that we tried to access them by manual searching and asking from some articles’ authors and experts. In addition, most of the existing studies on EBDM were limited to examining and presenting results on influencing, facilitating, or hindering factors or they only mentioned a few components in this area. Consequently, we tried to search for studies from various databases and carefully review and screen them to make sure that we did not lose any relevant data and thematic code. Also, instead of one model, we used four existing models as a basis in the BFF synthesis so that we can finally, by adding additional codes and themes obtained from other studies as well as expert opinions, provide a comprehensive model taking into account all the required steps and details. Also, the framework developed in this study is a complete conceptual model made by BFF synthesis; however, it may need some localization, according to the status and structure of each health system, for applying it.
The present framework provides a comprehensive guideline that can be well adapted for implementing EBDM in health systems and organizations especially in underdeveloped and developing countries where there is usually a lag in updating and applying evidence in their decision-making process. In addition, this framework by providing a complete, well-detailed, sequential and practical process including 10 steps and 56 sub-steps that did not exist in the incomplete related models, can be tested in the organizational decision-making process or managerial tasks by developed countries to improve their EBDM cycle, too.
Availability of data and materials
All data in a form of data extraction tables are available from the corresponding author on a reasonable request.
Abbreviations
- Evidence-based decision-making
Health System Management
Best-Fit Framework
Rychetnik L, Bauman A, Laws R, King L, Rissel C, Nutbeam D, et al. Translating research for evidence-based public health: Key concepts and future directions. J Epidemiol Community Health. 2012;66(12):1187–92.
Article Google Scholar
Nutbeam D, Boxall AM. What influences the transfer of research into health policy and practice? Observations from England and Australia. Public Health. 2008;122(8):747–53.
Brownson RC, Fielding JE, Maylahn CM. Evidence-Based Public Health: A Fundamental Concept for Public Health Practice. Annu Rev Public Health [Internet]. 2009;30(1):175–201. https://doi.org/10.1146/annurev.publhealth.031308.100134 .
Brownson RC, Gurney JG, Land GH. Evidence-based decision making in public health. J Public Heal Manag Pract [Internet]. 1999 [cited 2018 May 26];5(5):86–97. Available from: https://books.google.com/books?hl=en&lr=&id=yxRgAwAAQBAJ&oi=fnd&pg=PA133&dq=+criteria+OR+health+%22evidence+based+decision+making%22&ots=hiqVNQtF24&sig=jms9GsBfw6gz1cN2FQXzCBZvmMQ
McGinnis JM. ‘Does Proof Matter? Why Strong Evidence Sometimes Yields Weak Action.’ Am J Heal Promot. 2001;15(5):391–396. Available from: https://doi.org/10.4278/0890-1171-15.5.391 .
Majdzadeh R, Yazdizadeh B, Nedjat S, Gholami J, Ahghari S, R. M, et al. Strengthening evidence-based decision-making: Is it possible without improving health system stewardship? Health Policy Plan [Internet]. 2012 Sep 1 [cited 2018 May 15];27(6):499–504. Available from: https://doi.org/10.1093/heapol/czr072
WHO EIPNET. Using evidence and innovation to strengthen policy and practice. 2008.
Ellen ME, Léon G, Bouchard G, Lavis JN, Ouimet M, Grimshaw JM. What supports do health system organizations have in place to facilitate evidence-informed decision-making? A qualitative study. Implement Sci. 2013;8(1):84.
Oxman AD, Lavis JN, Lewin S, Fretheim A. What is evidence-informed policymaking? Health Res Policy Sys. 2009;7:1–7.
Armstrong R, Waters E, Dobbins M, Anderson L, Moore L, Petticrew M, et al. Knowledge translation strategies to improve the use of evidence in public health decision making in local government: Intervention design and implementation plan. Implement Sci [Internet]. 2013;8(1):1. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84885076767&doi=10.1186%2F1748-5908-8-121&partnerID=40&md5=dddaf4029205c63877a3e6ecf28f7762
Waters E, Armstrong R, Swinburn B, Moore L, Dobbins M, Anderson L, et al. An exploratory cluster randomised controlled trial of knowledge translation strategies to support evidence-informed decision-making in local governments (The KT4LG study). BMC Public Health [Internet]. 2011;11(1):34. Available from: http://www.biomedcentral.com/1471-2458/11/34
Imani-Nasab MH, Yazdizadeh B, Salehi M, Seyedin H, Majdzadeh R. Validity and reliability of the Evidence Utilisation in Policymaking Measurement Tool (EUPMT). Heal Res Policy Syst. 2017;15(1):1–11.
El-Jardali F, Lavis JN, Ataya N, Jamal D, Ammar W, Raouf S. Use of health systems evidence by policymakers in eastern mediterranean countries: Views, practices, and contextual influences. BMC Health Serv Res. 2012;12(1):200.
Ettelt S, Mays N. Health services research in Europe and its use for informing policy. J Health Serv Res Policy [Internet]. 2011 Jul 29 [cited 2019 Jun 29];16(2_suppl):48–60. Available from: https://doi.org/10.1258/jhsrp.2011.011004
Sutcliffe S. Evidence-Based Policymaking: What is it? How does it work? What relevance for developing countries? 2005.
Campbell DM, Redman S, Jorm L, Cooke M, Zwi AB, Rychetnik L. Increasing the use of evidence in health policy: Practice and views of policy makers and researchers. Aust New Zealand Health Policy. 2009;6(1):1–11.
WHO. Supporting the Use of Research Evidence (SURE) for Policy in African Health Systems. 2007:1–72.
Health Public Accreditation Board. Public Health Accreditation Board STANDARDS : AN OVERVIEW. 2012.
Riley WJ, Bender K, Lownik E. Public health department accreditation implementation: Transforming public health department performance. Am J Public Health. 2012;102(2):237–42.
Liebman JB. Building on Recent Advances in Evidence-Based Policymaking. 2013:36. Available from: http://www.americaachieves.org/9F42769C-3A65-4CCB-8466-E7BFD835CFE7/FinalDownload/DownloadId-0AB31816953C7B8AFBD2D15DFD39D5A8/9F42769C-3A65-4CCB-8466-E7BFD835CFE7/docs/RFA/THP_Liebman.pdf
Jacobs J a, Jones E, Gabella B a, Spring B, Brownson C. Tools for Implementing an Evidence-Based Approach in Public Health Practice. Prev Chronic Dis [Internet]. 2012;9(1):1–9. Available from: https://doi.org/10.5888/pcd9.110324
Kothari A, Edwards N, Hamel N, Judd M. Is research working for you? validating a tool to examine the capacity of health organizations to use research. Implement Sci. 2009;4(1):1–9.
Oxman AD, Bjørndal A, Becerra-Posada F, Gibson M, Block MAG, Haines A, et al. A framework for mandatory impact evaluation to ensure well informed public policy decisions. Lancet. 2010;375(9712):427–31. Available from: https://doi.org/10.1016/S0140-6736(09)61251-4
Oxman AD, Vandvik PO, Lavis JN, Fretheim A, Lewin S. SUPPORT Tools for evidence-informed health Policymaking (STP) 2: Improving how your organisation support the use of research evidence to inform policymaking. Chinese J Evidence-Based Med. 2010;10(3):247–54.
Google Scholar
Carroll C, Booth A, Leaviss J, Rick J. “ Best fit ” framework synthesis : refining the method. BMC Med Res Methodol. 2013;13(1):1 Available from: BMC Medical Research Methodology.
Carroll C, Booth A, Cooper K. A worked example of “ best fit ” framework synthesis : A systematic review of views concerning the taking of some potential chemopreventive agents. BMC Med Res Methodol. 2011;11:29.
Barnett-page E, Thomas J. Methods for the synthesis of qualitative research : a critical review. BMC Med Res Methodol 9. 2009;59:1–26.
Public Health Resource Unit. Critical Appraisal Skills Programme (CASP) making sense of evidence;10 questions to help you make sense of qualitative research. Public Health. 2006.
Baethge C, Goldbeck-Wood S, Mertens S. SANRA—a scale for the quality assessment of narrative review articles. Res Integr Peer Rev. 2019;4(1):2–8.
Hong Q, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, et al. Mixed Methods Appraisal Tool (MMAT), Version 2018. User guide. McGill [Internet]. 2018;1–11. Available from: http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/fetch/127916259/MMAT_2018_criteria-manual_2018-08-01_ENG.pdf%0Ahttp://mixedmethodsappraisaltoolpublic.pbworks.com/
Titler MG. The Iowa Model of evidence-based practice to promote quality care. 2001.
Dobrow MJ, Goel V, Upshur REG. Evidence-based health policy: context and utilisation. Soc Sci Med [Internet]. 2004;58(1):207–17. Available from: http://www.sciencedirect.com/science/article/pii/S0277953603001667
Kohatsu ND, Robinson JG, Torner JC. Evidence-based public health: An evolving concept. Am J Prev Med. 2004;27(5):417–21.
PubMed Google Scholar
Aas RW, Alexanderson K. Challenging Evidence-based Decision-making: A Hypothetical Case Study about Return to Work. Occup Ther Int. 2012 [cited 2018 May 28];19(1):28–44. Available from: https://doi.org/10.1002/oti.326
Ward M. Evidence-informed decision making in a public health setting. Healthc Manag Forum. 2011;24(1 SUPPL):S8.
Champagne F, Lemieux-Charles L, Duranceau M-F, MacKean G, Reay T. Organizational impact of evidence-informed decision making training initiatives: A case study comparison of two approaches. Implement Sci [Internet]. 2014;9(1). Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84900004312&doi=10.1186%2F1748-5908-9-53&partnerID=40&md5=df5573f17e19ef002d67cf669059aef4
Wright AL, Zammuto RF, Liesch PW, Middleton S, Hibbert P, Burke J, et al. Evidence-based Management in Practice: Opening up the Decision Process, Decision-maker and Context. Br J Manag. 2016;27(1):161–78. Available from: https://doi.org/10.1111/1467-8551.12123
Stamatakis KA, Ferreira Hino AA, Allen P, McQueen A, Jacob RR, Baker EA, et al. Results from a psychometric assessment of a new tool for measuring evidence-based decision making in public health organizations. Eval Program Plann [Internet]. 2017 Feb [cited 2018 May 16];60:17–23. Available from: http://linkinghub.elsevier.com/retrieve/pii/S014971891630009X
Harris C, Allen K, Waller C, Dyer T, Brooke V, Garrubba M, et al. Sustainability in Health care by Allocating Resources Effectively (SHARE) 7: supporting staff in evidence-based decision-making, implementation and evaluation in a local healthcare setting. BMC Health Serv Res [Internet]. 2017 Dec 21 [cited 2018 May 19];17(1):430. Available from: https://doi.org/10.1186/s12913-017-2388-8
Harris C, Garrubba M, Melder A, Voutier C, Waller C, King R, et al. Sustainability in Health care by Allocating Resources Effectively (SHARE) 8: Developing, implementing and evaluating an evidence dissemination service in a local healthcare setting. BMC Health Serv Res [Internet]. 2018;18(1). Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85042873576&doi=10.1186%2Fs12913-018-2932-1&partnerID=40&md5=2daa5bbd3ccddf299f7b9d527b6105af
Yost J, Dobbins M, Traynor R, DeCorby K, Workentine S, Greco L. Tools to support evidence-informed public health decision making. BMC Public Health [Internet]. 2014 Dec 18 [cited 2018 May 28];14(1):728. Available from: https://bmcpublichealth.biomedcentral.com/articles/ https://doi.org/10.1186/1471-2458-14-728
Janati A, Hasanpoor E, Hajebrahimi S, Sadeghi- H, Khezri A. An Evidence-Based Framework for Evidence-Based Management in Healthcare Organizations : A Delphi Study. Ethiop J Heal Sci. 2018;28(3):305–14.
Rosswurm MA, Larrabee JH. A Model for Change to Evidence-Based Practice. J Nurs Scholarsh. 1999;31(4):317–22.
Article CAS Google Scholar
Falzer PR, Garman MD. A conditional model of evidence-based decision making. J Eval Clin Pract [Internet]. 2009 Dec [cited 2018 May 19];15(6):1142–51. Available from: http://doi.wiley.com/ https://doi.org/10.1111/j.1365-2753.2009.01315.x
Ginter PM, Duncan WJ, Swayne LE. Strategic management of health care organizations. 8th Edition. Hoboken: John Wiley & Sons, Inc. 2018. p. 40.
Humphries S, Stafinski T, Mumtaz Z, Menon D. Barriers and facilitators to evidence-use in program management: a systematic review of the literature. BMC Health Serv Res [Internet]. 2014 Dec 14 [cited 2018 May 16];14(1):171. Available from: http://bmchealthservres.biomedcentral.com/articles/ https://doi.org/10.1186/1472-6963-14-171
Liang Z, Howard PF, Leggat SG, Murphy G. A framework to improve evidence-informed decision-making in health service management. Aust Heal Rev [Internet]. 2012;36(3):284–9. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84865450745&doi=10.1071%2FAH11051&partnerID=40&md5=c42d56774cd486b8df8a5e4afec33a6a
Kohn MK, Berta W, Langley A, Davis D. Evidence-based decision making in health care settings: From theory to practice [Internet]. Vol. 11, Advances in Health Care Management. Emerald Group Publishing Ltd; 215–234 p. Available from: 2011. https://doi.org/10.1108/S1474-8231(2011)0000011012 .
Armstrong R, Waters E, Moore L, Dobbins M, Pettman T, Burns C, et al. Understanding evidence: a statewide survey to explore evidence-informed public health decision-making in a local government setting. Implement Sci [Internet]. 2014;9(1):188. Available from: http://implementationscience.biomedcentral.com/articles/ https://doi.org/10.1186/s13012-014-0188-7
McDiarmid M, Sandra K, Binns M. Evidence-based administrative decision making and the Ontario hospital CEO: information needs, seeking behaviour, and access to sources. JCHLA / JABSC [Internet]. 2007 [cited 2018 May 28];28:63–72. Available from: https://ejournals.library.ualberta.ca/index.php/jchla/article/viewFile/24060/17884
Brownson RC, Allen P, Duggan K, Stamatakis KA, Erwin PC. Fostering more-effective public health by identifying administrative evidence-based practices: A review of the literature. Am J Prev Med [Internet]. 2012;43(3):309–19. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84865688888&doi=10.1016%2Fj.amepre.2012.06.006&partnerID=40&md5=a843f04e58b619ab9355a98bbfeef51a
Moussata CO. Evidence-Based Management and its Influence on the Practices of Senior Leaders of Hospitals in the Denver Metropolitan Area [Internet]. ProQuest Dissertations and Theses. [Ann Arbor]: Colorado Technical University; 2017 [cited 2018 May 19]. Available from: https://search.proquest.com/docview/1967189422?accountid=41313
Ward M, Mowat D. Creating an organizational culture for evidence-informed decision making. Healthc Manag Forum [Internet]. 2012;25(3):146–50. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84867778644&doi=10.1016%2Fj.hcmf.2012.07.005&partnerID=40&md5=42f06b7236a4a1cd6a4739c7e1900764
Sosnowy CD, Weiss LJ, Maylahn CM, Pirani SJ, Katagiri NJ. Factors affecting evidence-based decision making in local health departments. Am J Prev Med [Internet]. 2013 Dec [cited 2018 May 19];45(6):763–8. Available from: http://dx.doi.org/ https://doi.org/10.1016/j.amepre.2013.08.004
Pagoto SL, Spring B, Coups EJ, Mulvaney S. Barriers and Facilitators of Evidence-Based Practice Perceived by Behavioral Science Health Professionals. 2007;63(7):695–705.
Weiss L, Sosnowy C, Maylahn C, Katagiri N, Pirani S. Evidence-Based Decision Making in Local Health Departments Evidence-Based Decision Making in Local Health Departments. Front Public Heal Serv Syst Res. 2012;1(3):1–7.
Lester L, Haby MM, Chapman E, Kuchenmüller T. Evaluation of the performance and achievements of the WHO Evidence-informed Policy Network (EVIPNet) Europe. Heal Res policy Syst. 2020;18(1):109.
Aas RW, Alexanderson K. Challenging evidence-based decision-making: A hypothetical case study about return to work. Occup Ther Int [Internet]. 2012 Mar [cited 2018 May 28];19(1):28–44. Available from: https://doi.org/10.1002/oti.326
Daouk-Öyry L, Sahakian T, van de Vijver F. Evidence-Based Management Competency Model for Managers in Hospital Settings. Br J Manag. 2020;00:1–20.
Isfeedvajani MS. Evidence-Based Management and its Application in the Hospital Management Process. Hosp Pract Res [Internet]. 2018 [cited 2018 May 28];3(2):35–6. Available from: http://jhpr.ir/article_60533_8313dd6afa580ef2afa689e6984c8844.pdf
Armstrong R, Waters E, Moore L, Dobbins M, Pettman T, Burns C, et al. Understanding evidence: a statewide survey to explore evidence-informed public health decision-making in a local government setting. Implement Sci [Internet]. 2014 Dec 14 [cited 2018 May 28];9(1):188. Available from: https://doi.org/10.1186/s13012-014-0188-7
Uneke CJ, Sombie I, Johnson E, Uneke BI, Okolo S. Promoting the use of evidence in health policymaking in the ECOWAS region: the development and contextualization of an evidence-based policymaking guidance. Global Health [Internet]. 2020;16(1):73. Available from: http://www.embase.com/search/results?subaction=viewrecord&id=L632558076&from=export
Janati A, Hasanpoor E, Hajebrahimi S, Sadeghi-Bazargani H. Health care managers’ perspectives on the sources of evidence in evidence-based hospital management: A qualitative study in Iran. Ethiop J Health Sci [Internet]. 2017;27(6):659–68. Available from: https://www.ajol.info/index.php/ejhs/article/view/162555
Spiri WC, Kurcgant P, Pereira MV. Perception Of Nursing Middle Managers About The Evidence-Based Management. Int Arch Med [Internet]. 2017;10(February):11. Available from: http://imedicalsociety.org/ojs/index.php/iam/article/view/2311
Harris C, Allen K, Waller C, Green S, King R, Ramsey W, et al. Sustainability in Health care by Allocating Resources Effectively (SHARE) 5: developing a model for evidence-driven resource allocation in a local healthcare setting. BMC Health Serv Res. 2017;17(1):1–18.
Belay T, Mbuya N, Rajan V. Data utilization and evidence-based decision making in the health sector: survey of three Indian states [Internet]. 2009 [cited 2018 May 26]. Available from: https://openknowledge.worldbank.org/handle/10986/3161
Niedzwiedzka BM. Barriers to evidence-based decision making among Polish healthcare managers. Heal Serv Manag Res [Internet]. 2003 May 21 [cited 2018 May 19];16(2):106–15. Available from: https://doi.org/10.1258/095148403321591429
Peirson L, Ciliska D, Dobbins M, Mowat D. Building capacity for evidence informed decision making in public health: A case study of organizational change. BMC Public Health [Internet]. 2012;12(1):137. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84857132983&doi=10.1186%2F1471-2458-12-137&partnerID=40&md5=68e18844316881fb3f2662477825d441
Buffett C, Ciliska D, Thomas H. Can I Use This Evidence in my Program Decision? Assessing Applicability and Transferability of Evidence. National Collaborating Centre for Methods and Tools (NCCMT) School of Nursing, McMaster University. 2007:1–22.
Buffet C, Ciliska D, Thomas H. It worked there. Will it work here? A tool for assessing applicability and transferability of evidence (A: When considering starting a new program). National Collaborating Centre for Methods and Tools (NCCMT) School of Nursing, McMaster University. 2011;(905):1–2.
Dobbins M, Jack S, Thomas H, Kothari A. Public health decision-makers’ informational needs and preferences for receiving research evidence. Worldviews Evidence-Based Nurs. 2007;4(3):156–63.
Wright AL, Zammuto RF, Liesch PW, Middleton S, Hibbert P, Burke J, et al. Evidence-based Management in Practice: Opening up the Decision Process, Decision-maker and Context. Br J Manag [Internet]. 2016 Jan [cited 2018 May 28];27(1):161–78. Available from: https://doi.org/10.1111/1467-8551.12123
Imani-Nasab MH, Seyedin H, Yazdizadeh B, Majdzadeh R. A Qualitative Assessment of the Evidence Utilization for Health Policy-Making on the Basis of SUPPORT Tools in a Developing Country. Int J Heal Policy Manag. 2017;6(8):457–65.
Lavis JN, Paulsen EJ, Oxman AD, Moynihan R. Evidence-informed health policy 2-Survey of organizations that support the use of research evidence. Implement Sci. 2008;3:54.
Bastani P, Kavosi Z, Alipoori S, Imani-Nasab MH. Evidence- based Policy and Decision-Making among Health Managers: A Case of Shiraz Univer- sity of Medical Sciences. GMJ. 2017;6(1):30–8.
Greaves DE. Evidence-based management of Caribbean health systems: barriers and opportunities. Int J Health Governance. 2017;22(2):104–117.
Download references
Acknowledgements
This research, derived from Proposal No. 96-01-07-14184, was conducted by Mrs. Tahereh Shafaghat as part of the activities required for a Ph.D. degree in health care management at the Shiraz University of Medical Sciences. The authors wish to express their sincere gratitude to the research administration of Shiraz University of Medical Sciences for its financial and administrative support and to the English editorial board of Research Editor Institution for improving the native English language of this work.
As the overall study was an approved research project of Shiraz University of Medical Sciences and it was conducted by Mrs. Tahereh Shafaghat as part of the activities required for a Ph.D. degree in the health care management field, the Shiraz University of Medical Sciences supported this study. This study was sponsored by Shiraz University of Medical Sciences under code (96‑01‑07‑14184). The funding body was not involved in the design of the study, data collection, analysis, and interpretation, as well as in writing the manuscript.
Author information
Tahereh Shafaghat and Peivand Bastani have equal participation as first authors.
Authors and Affiliations
School of Management and Medical Informatics, Health Human Recourses Research Center, Shiraz University of Medical Sciences, Shiraz, Iran
Tahereh Shafaghat, Peivand Bastani & Mohammad Amin Bahrami
Department of Health Care Management, School of Public Health, Health Policy and Management Research Center, Shahid Saoughi University of Medical Sciences, Yazd, Iran
Tahereh Shafaghat & Mohammad Kazem Rahimi Zarchi
Faculty of Health and Behavioral Sciences, School of Dentistry, University of Queensland, QLD, 4072, Brisbane, Australia
Peivand Bastani
Social Determinants of Health Research Center, Lorestan University of Medical Sciences, Khorramabad, Iran
Mohammad Hasan Imani Nasab
Student Research Committee, School of Management and Medical Informatics, Shiraz University of Medical Sciences, Shiraz, Iran
Mahsa Roozrokh Arshadi Montazer
Faculty of Medicine, Center for Health Services Research, The University of Queensland, Brisbane, Australia
Sisira Edirippulige
You can also search for this author in PubMed Google Scholar
Contributions
PB and TSH designed the study and its overall methodology. BP also edited and finalized the article. TSH searched all the databases, with the help of MRAM retrieved the sources, scanned, and screened all the articles in 3 phases. TSH also prepared the draft of the article. MAB and MKRZ contributed to data analysis and synthesis. Also, the study was under consultation and supervision by ZK and MHIN as advisors. All the authors have read and approved the final manuscript.
Corresponding author
Correspondence to Peivand Bastani .
Ethics declarations
Ethics approval and consent to participate.
Since at this study a scoping review was conducted and then the best-fit framework synthesis was used for developing a comprehensive EBDM framework in HSM, there was no human or animal participant in this study. However, the overall research project related to this manuscript was approved by the medical ethics conceal of the research deputy of Shiraz University of Medical Sciences with approval number IR.SUMS.REC.1396–01-07–14184.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.

Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Tables 3 , 4 , 5 and 6 .
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Shafaghat, T., Bastani, P., Nasab, M.H.I. et al. A framework of evidence-based decision-making in health system management: a best-fit framework synthesis. Arch Public Health 80 , 96 (2022). https://doi.org/10.1186/s13690-022-00843-0
Download citation
Received : 30 October 2021
Accepted : 08 March 2022
Published : 29 March 2022
DOI : https://doi.org/10.1186/s13690-022-00843-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health system
- Best-fit framework synthesis
Archives of Public Health
ISSN: 2049-3258
- General enquiries: [email protected]

Teaching Critical Thinking as a Public Health Initiative
Tim Caulfield—a Law Professor at the University of Alberta and the author of Is Gwyneth Paltrow Wrong About Everything? —wants to help us get better at fighting misinformation about health.
This past Monday, Caulfield came to the Petrie-Flom Center’s Health Policy Workshop and spoke to an audience of Harvard Law students, affiliates from throughout Harvard University, and academics and community members from the Boston area.
During his fascinating and dynamic presentation, Caulfield covered a lot of ground. He discussed political polarization on Twitter, the profit-maximizing machinations (or self-delusion) of celebrities pedaling bunk health products, and evidence that false claims spread faster than true ones. All that may leave one feeling pessimistic and Caulfield would likely sympathize with your pessimism. Yet, the presentation also contained reasons to have hope.
Caulfield discussed the ways using narratives can make connections and fight misinformation, the power of consumers to initiate complaint-driven efforts to enforce truth in advertising law, and empirical research that suggests that the relevant critical thinking skills to help people make well-informed, rational decisions about their health can be taught.
This last point about teaching critical thinking stuck out to me.
I’ve just now spoke about “well-informed” and “rational” decisions. What counts as “well-informed” and “rational” will, of course, differ depending on one’s perspective and values. And it’s important that we keep this in mind when assessing the quality of the decision-making and discourse of a large population.
Yet even with these caveats in place, I take it that there are still some objective value claims we can make about some health-based decisions people make.
For example, getting your children vaccinated for measles, mumps, and rubella is a good decision , while purchasing a jade egg from Gwyneth Paltrow to put in your vagina is not (or at least not good for your health).
And if we can be doing things to help teach people how to make better, more-informed decisions about their health, for those of us interested in promoting health in the general population, this seems like an important avenue to pursue.
The study Caulfield cited was from a 2017 publication in which researchers found that primary school children (ages 10-12) in Uganda who were given nine 80-minute lessons in which they were taught about “12 concepts essential to assessing claims about treatment effects and making informed health choices” scored an average of 20 points higher than students who did not receive the instruction on a test meant to examine students’ ability to make informed, health-based decisions.
This is a hopeful finding.
In a society where people are already concerned about the population’s lack of critical thinking skills , evidence that such skills can be taught, and that they can be used to help people make better-informed decisions about their health, provides us with plenty of reason to fight for the teaching of critical thinking skills.
People are already calling for the teaching of critical thinking skills to counteract other societal issues, and courses like “ Calling Bullshit: Data Reasoning in a Digital World ” have begun cropping up online. Those of us concerned with fighting for improvements in health outcomes ought to rally behind these efforts.
If teaching critical thinking can lead to better decision-making about health, we should start treating the teaching of critical thinking as an important public health initiative.
Share this:
- Click to share on Facebook (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to print (Opens in new window)

Mark Satta is an Assistant Professor of Philosophy at Wayne State University. He holds a JD from Harvard Law School and a PhD in Philosophy from Purdue University. His research interests include First Amendment law, health law, bioethics, and epistemology. He was a 2018-2019 Student Fellow at the Petrie Flom Center, where he completed a project entitled, "Spitting at Science: HIV Criminalization Laws and the Duty to Legislate in Accordance with Current Scientific Knowledge."
One thought to “Teaching Critical Thinking as a Public Health Initiative”
“…an average of 20 points higher…” What percentage is that? And yes! Critical thinking NEEDS to be a skill that is REQUIRED to be taught in all high schools! I’d be willing to pay more in taxes to fund this.
Leave a Reply Cancel reply
You must be logged in to post a comment.
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Sign up for our newsletter

- Get started with computers
- Learn Microsoft Office
- Apply for a job
- Improve my work skills
- Design nice-looking docs
- Getting Started
- Smartphones & Tablets
- Typing Tutorial
- Online Learning
- Basic Internet Skills
- Online Safety
- Social Media
- Zoom Basics
- Google Docs
- Google Sheets
- Career Planning
- Resume Writing
- Cover Letters
- Job Search and Networking
- Business Communication
- Entrepreneurship 101
- Careers without College
- Job Hunt for Today
- 3D Printing
- Freelancing 101
- Personal Finance
- Sharing Economy
- Decision-Making
- Graphic Design
- Photography
- Image Editing
- Learning WordPress
- Language Learning
- Critical Thinking
- For Educators
- Translations
- Staff Picks
- English expand_more expand_less
Critical Thinking and Decision-Making - What is Critical Thinking?
Critical thinking and decision-making -, what is critical thinking, critical thinking and decision-making what is critical thinking.

Critical Thinking and Decision-Making: What is Critical Thinking?
Lesson 1: what is critical thinking, what is critical thinking.
Critical thinking is a term that gets thrown around a lot. You've probably heard it used often throughout the years whether it was in school, at work, or in everyday conversation. But when you stop to think about it, what exactly is critical thinking and how do you do it ?
Watch the video below to learn more about critical thinking.
Simply put, critical thinking is the act of deliberately analyzing information so that you can make better judgements and decisions . It involves using things like logic, reasoning, and creativity, to draw conclusions and generally understand things better.
This may sound like a pretty broad definition, and that's because critical thinking is a broad skill that can be applied to so many different situations. You can use it to prepare for a job interview, manage your time better, make decisions about purchasing things, and so much more.
The process
As humans, we are constantly thinking . It's something we can't turn off. But not all of it is critical thinking. No one thinks critically 100% of the time... that would be pretty exhausting! Instead, it's an intentional process , something that we consciously use when we're presented with difficult problems or important decisions.
Improving your critical thinking
In order to become a better critical thinker, it's important to ask questions when you're presented with a problem or decision, before jumping to any conclusions. You can start with simple ones like What do I currently know? and How do I know this? These can help to give you a better idea of what you're working with and, in some cases, simplify more complex issues.
Real-world applications

Let's take a look at how we can use critical thinking to evaluate online information . Say a friend of yours posts a news article on social media and you're drawn to its headline. If you were to use your everyday automatic thinking, you might accept it as fact and move on. But if you were thinking critically, you would first analyze the available information and ask some questions :
- What's the source of this article?
- Is the headline potentially misleading?
- What are my friend's general beliefs?
- Do their beliefs inform why they might have shared this?

After analyzing all of this information, you can draw a conclusion about whether or not you think the article is trustworthy.
Critical thinking has a wide range of real-world applications . It can help you to make better decisions, become more hireable, and generally better understand the world around you.

/en/problem-solving-and-decision-making/why-is-it-so-hard-to-make-decisions/content/

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
Margin Size
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

5.3: Using Critical Thinking Skills- Decision Making and Problem Solving
- Last updated
- Save as PDF
- Page ID 24260
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
Introduction
In previous lessons, you learned about characteristics of critical thinkers and information literacy. In this module, you will learn how to put those skills into action through the important processes of decision making and problem solving.
As with the process of developing information literacy, asking questions is an important part of decision making and problem solving. Thinking is born of questions. Questions wake us up. Questions alert us to hidden assumptions. Questions promote curiosity and create new distinctions. Questions open up options that otherwise go unexplored. Besides, teachers love questions.
We make decisions all the time, whether we realize it or not. Even avoiding decisions is a form of decision making. The student who puts off studying for a test until the last minute, for example, might really be saying, “I’ve decided this course is not important” or “I’ve decided not to give this course much time.”
Decisions are specific and lead to focused action. When we decide, we narrow down. We give up actions that are inconsistent with our decision.
In addition to decision making, critical thinking skills are important to solving problems. We encounter problems every single day, and having a solid process in place is important to solving them.
At the end of the lesson, you will learn how to put your critical thinking skills to use by reviewing an example of how critical thinking skills can help with making those everyday decisions.
Using Critical Thinking Skills: Asking Questions
Questions have practical power. Asking for directions can shave hours off a trip. Asking a librarian for help can save hours of research time. Asking how to address an instructor—by first name or formal title—can change your relationship with that person. Asking your academic advisor a question can alter your entire education. Asking people about their career plans can alter your career plans.
You can use the following strategies to develop questions for problem solving and decision making:
Ask questions that create possibilities. At any moment, you can ask a question that opens up a new possibility for someone.
- Suppose a friend walks up to you and says, “People just never listen to me.” You listen carefully. Then you say, “Let me make sure I understand. Who, specifically, doesn’t listen to you? And how do you know they’re not listening?”
- Another friend tells you, “I just lost my job to someone who has less experience. That should never happen.” You respond, “Wow, that’s hard. I’m sorry you lost your job. Who can help you find another job?”
- A relative seeks your advice. “My mother-in-law makes me mad,” she says. “You’re having a hard time with this person,” you say. “What does she say and do when you feel mad at her? And are there times when you don’t get mad at her?”
These kinds of questions—asked with compassion and a sense of timing—can help people move from complaining about problems to solving them.
Discover new questions. Students sometimes say, “I don’t know what questions to ask.” Consider the following ways to create questions about any subject you want to study or about any
area of your life that you want to change:
- Let your pen start moving. Sometimes you can access a deeper level of knowledge by taking out your pen, putting it on a piece of paper, and writing down questions—even before you know what to write. Don’t think. Just watch the pen move across the paper. Notice what appears. The results might be surprising.
- Ask about what’s missing . Another way to invent useful questions is to notice what’s missing from your life and then ask how to supply it. For example, if you want to take better notes, you can write, “What’s missing is skill in note taking. How can I gain more skill in taking notes?” If you always feel rushed, you can write, “What’s missing is time. How do I create enough time in my day to actually do the things that I say I want to do?”
- Pretend to be someone else. Another way to invent questions is first to think of someone you greatly respect. Then pretend you’re that person. Ask the questions you think she would ask.
- What can I do when ... an instructor calls on me in class and I have no idea what to say? When a teacher doesn’t show up for class on time? When I feel overwhelmed with assignments?
- How can I ... take the kind of courses that I want? Expand my career options? Become much more effective as a student, starting today?
- When do I ... decide on a major? Transfer to another school? Meet with an instructor to discuss an upcoming term paper?
- What else do I want to know about ... my academic plan? My career plan? My options for job hunting? My friends? My relatives? My spouse?
- Who can I ask about ... my career options? My major? My love life? My values and purpose in life?
Many times you can quickly generate questions by simply asking yourself, “What else do I want to know?” Ask this question immediately after you read a paragraph in a book or listen to someone speak.
Start from the assumption that you are brilliant. Then ask questions to unlock your brilliance.
Using Critical Thinking Skills in Decision Making
As you develop your critical thinking skills, you can apply them as you make decisions. The following suggestions can help in your decision-making process:
Recognize decisions. Decisions are more than wishes or desires. There’s a world of difference between “I wish I could be a better student” and “I will take more powerful notes, read with greater retention, and review my class notes daily.” Deciding to eat fruit for dessert instead of ice cream rules out the next trip to the ice cream store.
Establish priorities. Some decisions are trivial. No matter what the outcome, your life is not affected much. Other decisions can shape your circumstances for years. Devote more time and energy to the decisions with big outcomes.
Base decisions on a life plan. The benefit of having long-term goals for our lives is that they provide a basis for many of our daily decisions. Being certain about what we want to accomplish this year and this month makes today’s choices more clear.
Balance learning styles in decision making. To make decisions more effectively, use all four modes of learning explained in a previous lesson. The key is to balance reflection with action, and thinking with experience. First, take the time to think creatively, and generate many options. Then think critically about the possible consequences of each option before choosing one. Remember, however, that thinking is no substitute for experience. Act on your chosen option, and notice what happens. If you’re not getting the results you want, then quickly return to creative thinking to invent new options.
Choose an overall strategy. Every time you make a decision, you choose a strategy—even when you’re not aware of it. Effective decision makers can articulate and choose from among several strategies. For example:
- Find all of the available options, and choose one deliberately. Save this strategy for times when you have a relatively small number of options, each of which leads to noticeably different results.
- Find all of the available options, and choose one randomly. This strategy can be risky. Save it for times when your options are basically similar and fairness is the main issue.
- Limit the options, and then choose. When deciding which search engine to use, visit many search sites and then narrow the list down to two or three from which to choose.
Use time as an ally. Sometimes we face dilemmas—situations in which any course of action leads to undesirable consequences. In such cases, consider putting a decision on hold. Wait it out. Do nothing until the circumstances change, making one alternative clearly preferable to another.
Use intuition. Some decisions seem to make themselves. A solution pops into your mind, and you gain newfound clarity. Using intuition is not the same as forgetting about the decision or refusing to make it. Intuitive decisions usually arrive after we’ve gathered the relevant facts and faced a problem for some time.
Evaluate your decision. Hindsight is a source of insight. After you act on a decision, observe the consequences over time. Reflect on how well your decision worked and what you might have done differently.
Think of choices. This final suggestion involves some creative thinking. Consider that the word decide derives from the same roots as suicide and homicide . In the spirit of those words, a decision forever “kills” all other options. That’s kind of heavy. Instead, use the word choice , and see whether it frees up your thinking. When you choose , you express a preference for one option over others. However, those options remain live possibilities for the future. Choose for today, knowing that as you gain more wisdom and experience, you can choose again.
Using Critical Thinking Skills in Problem Solving
Think of problem solving as a process with four Ps : Define the problem , generate possibilities ,
create a plan , and perform your plan.
Step 1: Define the problem. To define a problem effectively, understand what a problem is—a mismatch between what you want and what you have. Problem solving is all about reducing the gap between these two factors.
Tell the truth about what’s present in your life right now, without shame or blame. For example: “I often get sleepy while reading my physics assignments, and after closing the book I cannot remember what I just read.”
Next, describe in detail what you want. Go for specifics: “I want to remain alert as I read about physics. I also want to accurately summarize each chapter I read.”
Remember that when we define a problem in limiting ways, our solutions merely generate new problems. As Albert Einstein said, “The world we have made is a result of the level of thinking we have done thus far. We cannot solve problems at the same level at which we created them” (Calaprice 2000).
This idea has many applications for success in school. An example is the student who struggles with note taking. The problem, she thinks, is that her notes are too sketchy. The logical solution, she decides, is to take more notes; her new goal is to write down almost everything her instructors say. No matter how fast and furiously she writes, she cannot capture all of the instructors’ comments.
Consider what happens when this student defines the problem in a new way. After more thought, she decides that her dilemma is not the quantity of her notes but their quality . She adopts a new format for taking notes, dividing her notepaper into two columns. In the right-hand column, she writes down only the main points of each lecture. In the left-hand column, she notes two or three supporting details for each point.
Over time, this student makes the joyous discovery that there are usually just three or four core ideas to remember from each lecture. She originally thought the solution was to take more notes. What really worked was taking notes in a new way.
Step 2: Generate possibilities. Now put on your creative thinking hat. Open up. Brainstorm as many possible solutions to the problem as you can. At this stage, quantity counts. As you generate possibilities, gather relevant facts. For example, when you’re faced with a dilemma about what courses to take next semester, get information on class times, locations, and instructors. If you haven’t decided which summer job offer to accept, gather information on salary, benefits, and working conditions.
Step 3: Create a plan. After rereading your problem definition and list of possible solutions, choose the solution that seems most workable. Think about specific actions that will reduce the gap between what you have and what you want. Visualize the steps you will take to make this solution a reality, and arrange them in chronological order. To make your plan even more powerful, put it in writing.
Step 4: Perform your plan. This step gets you off your chair and out into the world. Now you actually do what you have planned.
Ultimately, your skill in solving problems lies in how well you perform your plan. Through the quality of your actions, you become the architect of your own success.
When facing problems, experiment with these four Ps, and remember that the order of steps is not absolute. Also remember that any solution has the potential to create new problems. If that happens, cycle through the four Ps of problem solving again.
Critical Thinking Skills in Action: Thinking About Your Major, Part 1
One decision that troubles many students in higher education is the choice of a major. Weighing the benefits, costs, and outcomes of a possible major is an intellectual challenge. This choice is an opportunity to apply your critical thinking, decision-making, and problem-solving skills. The following suggestions will guide you through this seemingly overwhelming process.
The first step is to discover options. You can use the following suggestions to discover options for choosing your major:
Follow the fun. Perhaps you look forward to attending one of your classes and even like completing the assignments. This is a clue to your choice of major.
See whether you can find lasting patterns in the subjects and extracurricular activities that you’ve enjoyed over the years. Look for a major that allows you to continue and expand on these experiences.
Also, sit down with a stack of 3 × 5 cards and brainstorm answers to the following questions:
- What do you enjoy doing most with your unscheduled time?
- Imagine that you’re at a party and having a fascinating conversation. What is this conversation about?
- What kind of problems do you enjoy solving—those that involve people? Products? Ideas?
- What interests are revealed by your choices of reading material, television shows, and other entertainment?
- What would an ideal day look like for you? Describe where you would live, who would be with you, and what you would do throughout the day. Do any of these visions suggest a possible major?
Questions like these can uncover a “fun factor” that energizes you to finish the work of completing a major.
Consider your abilities. In choosing a major, ability counts as much as interest. In addition to considering what you enjoy, think about times and places when you excelled. List the courses that you aced, the work assignments that you mastered, and the hobbies that led to rewards or recognition. Let your choice of a major reflect a discovery of your passions and potentials.
Use formal techniques for self-discovery. Explore questionnaires and inventories that are designed to correlate your interests with specific majors. Examples include the Strong Interest Inventory and the Self-Directed Search. Your academic advisor or someone in your school’s career planning office can give you more details about these and related assessments. For some fun, take several of them and meet with an advisor to interpret the results. Remember inventories can help you gain self-knowledge, and other people can offer valuable perspectives. However, what you do with all this input is entirely up to you.
Critical Thinking Skills in Action: Thinking About Your Major, Part 2
As you review the following additional suggestions of discovering options, think about what strategies you already use in your own decision-making process. Also think about what new strategies you might try in the future.
Link to long-term goals. Your choice of a major can fall into place once you determine what you want in life. Before you choose a major, back up to a bigger picture. List your core values, such as contributing to society, achieving financial security and professional recognition, enjoying good health, or making time for fun. Also write down specific goals that you want to accomplish 5 years, 10 years, or even 50 years from today.
Many students find that the prospect of getting what they want in life justifies all of the time, money, and day-to-day effort invested in going to school. Having a major gives you a powerful incentive for attending classes, taking part in discussions, reading textbooks, writing papers, and completing other assignments. When you see a clear connection between finishing school and creating the life of your dreams, the daily tasks of higher education become charged with meaning.
Ask other people. Key people in your life might have valuable suggestions about your choice of major. Ask for their ideas, and listen with an open mind. At the same time, distance yourself from any pressure to choose a major or career that fails to interest you. If you make a choice solely on the basis of the expectations of other people, you could end up with a major or even a career you don’t enjoy.
Gather information. Check your school’s catalog or website for a list of available majors. Here is a gold mine of information. Take a quick glance, and highlight all the majors that interest you. Then talk to students who have declared these majors. Also read the descriptions of courses required for these majors. Do you get excited about the chance to enroll in them? Pay attention to your gut feelings.
Also chat with instructors who teach courses in a specific major. Ask for copies of their class syllabi. Go to the bookstore and browse the required texts. Based on all of this information, write a list of prospective majors. Discuss them with an academic advisor and someone at your school’s career-planning center.
Invent a major. When choosing a major, you might not need to limit yourself to those listed in your school catalog. Many schools now have flexible programs that allow for independent study. Through such programs, you might be able to combine two existing majors or invent an entirely new one of your own.
Consider a complementary minor. You can add flexibility to your academic program by choosing a minor to complement or contrast with your major. The student who wants to be a minister could opt for a minor in English; all of those courses in composition can help in writing sermons. Or the student with a major in psychology might choose a minor in business administration, with the idea of managing a counseling service some day. An effective choice of a minor can expand your skills and career options.
Think critically about the link between your major and your career. Your career goals might have a significant impact on your choice of major.
You could pursue a rewarding career by choosing among several different majors. Even students planning to apply for law school or medical school have flexibility in their choice of majors. In addition, after graduation, many people tend to be employed in jobs that have little relationship to their major. And you might choose a career in the future that is unrelated to any currently available major.
Critical Thinking Skills in Action: Thinking About Your Major, Part 3
Once you have discovered all of your options, you can move on to the next step in the process— making a trial choice.
Make a Trial Choice
Pretend that you have to choose a major today. Based on the options for a major that you’ve already discovered, write down the first three ideas that come to mind. Review the list for a few minutes, and then choose one.
Evaluate Your Trial Choice
When you’ve made a trial choice of major, take on the role of a scientist. Treat your choice as a hypothesis, and then design a series of experiments to evaluate and test it. For example:
- Schedule office meetings with instructors who teach courses in the major. Ask about required course work and career options in the field.
- Discuss your trial choice with an academic advisor or career counselor.
- Enroll in a course related to your possible major. Remember that introductory courses might not give you a realistic picture of the workload involved in advanced courses. Also, you might not be able to register for certain courses until you’ve actually declared a related major.
- Find a volunteer experience, internship, part-time job, or service-learning experience related to the major.
- Interview students who have declared the same major. Ask them in detail about their experiences and suggestions for success.
- Interview people who work in a field related to the major and “shadow” them—that is, spend time with those people during their workday.
- Think about whether you can complete your major given the amount of time and money that you plan to invest in higher education.
- Consider whether declaring this major would require a transfer to another program or even another school.
If your “experiments” confirm your choice of major, celebrate that fact. If they result in choosing a new major, celebrate that outcome as well.
Also remember that higher education represents a safe place to test your choice of major—and to change your mind. As you sort through your options, help is always available from administrators, instructors, advisors, and peers.
Choose Again
Keep your choice of a major in perspective. There is probably no single “correct” choice. Your unique collection of skills is likely to provide the basis for majoring in several fields.
Odds are that you’ll change your major at least once—and that you’ll change careers several times during your life. One benefit of higher education is mobility. You gain the general skills and knowledge that can help you move into a new major or career field at any time.
Viewing a major as a one-time choice that determines your entire future can raise your stress levels. Instead, look at choosing a major as the start of a continuing path that involves discovery, choice, and passionate action.
As you review this example of how you can use critical thinking to make a decision about choosing your major, think about how you will use your critical thinking to make decisions and solve problems in the future.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Perspect Med Educ
- v.7(3); 2018 Jun

Constructing critical thinking in health professional education
Renate kahlke.
Centre for Health Education Scholarship, University of British Columbia, Vancouver, Canada
Associated Data
Introduction.
Calls for enabling ‘critical thinking’ are ubiquitous in health professional education. However, there is little agreement in the literature or in practice as to what this term means and efforts to generate a universal definition have found limited traction. Moreover, the variability observed might suggest that multiplicity has value that the quest for universal definitions has failed to capture. In this study, we sought to map the multiple conceptions of critical thinking in circulation in health professional education to understand the relationships and tensions between them.
We used an inductive, qualitative approach to explore conceptions of critical thinking with educators from four health professions: medicine, nursing, pharmacy, and social work. Four participants from each profession participated in two individual in-depth semi-structured interviews, the latter of which induced reflection on a visual depiction of results generated from the first set of interviews.
Three main conceptions of critical thinking were identified: biomedical, humanist, and social justice-oriented critical thinking. ‘Biomedical critical thinking’ was the dominant conception. While each conception had distinct features, the particular conceptions of critical thinking espoused by individual participants were not stable within or between interviews.
Multiple conceptions of critical thinking likely offer educators the ability to express diverse beliefs about what ‘good thinking’ means in variable contexts. The findings suggest that any single definition of critical thinking in the health professions will be inherently contentious and, we argue, should be. Such debates, when made visible to educators and trainees, can be highly productive.
Electronic supplementary material
The online version of this article (10.1007/s40037-018-0415-z) contains supplementary material, which is available to authorized users.
What this paper adds
‘Critical thinking’ is a term commonly used across health professional education, though there is little agreement on what this means in the literature or in practice. We depart from previous work, which most often attempts to create a common definition. Instead, we offer a description of the different conceptions of critical thinking held in health professional education, illustrate their dynamic use, and discuss the tensions and affordances that this diversity brings to the field. We argue that diversity in conceptions of critical thinking can allow educators to express unique and often divergent beliefs about what ‘good thinking’ means in their contexts.
Even though the term critical thinking is ubiquitous in educational settings, there is significant disagreement about what it means to ‘think critically’ [ 1 ]. Predominantly, authors have attempted to develop consensus definitions of critical thinking that would finally put these disagreements to rest (e. g. [ 2 – 5 ]). They define critical thinking variously, but tend to focus on a rational process involving (for example) ‘interpretation, analysis, evaluation, inference, explanation, and self-regulation’ [ 2 ]. Other authors have challenged this perspective by arguing that critical thinking is a more subjective process, emphasizing the role of emotion and relationships [ 6 – 9 ]. In the tradition of critical pedagogy, critical thinking has meant critiquing ideology [ 10 – 12 ]. Last, still others have argued that critical thinking is discipline or subject-specific, meaning that critical thinking is not universal, but does have a relatively stable meaning within different disciplines [ 13 – 18 ]. However, none of these attempts to clarify the ambiguity that surrounds critical thinking have led to agreement, suggesting that each of these perspectives offers, at best, a partial explanation for the persistence of disagreements.
This is problematic in health professional education (HPE) because professional programs are mandated to educate practitioners who have a defined knowledge base and skill set. When curriculum designers, educators, researchers, or policy-makers all agree that we should teach future professionals to ‘think critically’, resting on the assumption that they also agree on what that means, they may find themselves working at cross-purposes. Moreover, the focus on a stable meaning for critical thinking, whether within a discipline or across disciplines, cannot account for the potential value of the multiplicity of definitions that exist. That is, the availability of diverse conceptions of critical thinking likely enables educators to express diverse elements of and beliefs about their work, thereby suggesting a need to explore the conceptions of critical thinking held in HPE, and the contexts that inform those conceptions.
With the historical focus on developing broad definitions of critical thinking and delineating its component skills and dispositions, little has been done either to document the diverse conceptions of this term in circulation amongst active HPE practitioners or, perhaps more importantly, to illuminate the beliefs about what constitutes ‘good thinking’ that lie behind them and the relationships between them. Perhaps clarity in our understanding of critical thinking lies in the flexibility with which it is conceptualized. This study moves away from attempting to create universal definitions of critical thinking in order to explore the tensions that surround different, converging, and competing beliefs about what critical thinking means.
In doing so, we map out conceptions of critical thinking across four health professions along with the beliefs about professional practice that underpin those conceptions. Some of these beliefs may be tied to a profession’s socialization processes and many will be tied to beliefs about ‘good thinking’ that are shared across professions, since health professionals work within shared systems [ 19 ] toward the same ultimate task of providing patient care. It is the variety of ways in which critical thinking is considered by practitioners on the whole that we wanted to understand, not the formal pronouncements of what might be listed as competencies or components of critical thinking within any one profession.
Hence, with this study, we sought to ask:
- How do educators in the health professions understand critical thinking?
- What values or beliefs inform that understanding?
To explore these questions, we adopted a qualitative research approach that focuses on how people interpret and make meaning out of their experiences and actively construct their social worlds [ 20 ].
This study uses an emergent, inductive design in an effort to be responsive to the co-construction of new and unexpected meaning between participants and researchers. While techniques derived from constructivist grounded theory [ 21 ] were employed, methods like extensive theoretical sampling (that are common to that methodology) were not maintained because this study was intended to be broadly exploratory. This ‘borrowing’ of techniques offers the ability to capitalize on the open and broad approach offered by interpretive qualitative methodology [ 20 ] while engaging selectively with the more specific tools and techniques available from constructivist grounded theory [ 22 , 23 ].
The first author has a background in sociocultural and critical theory. Data collection and early analyses were carried out as part of her dissertation in Educational Policy Studies. As a result of her background in critical theory, there was a need for reflexivity focused on limiting predisposition toward participant interpretations of critical thinking that aligned with critical theory. The senior author was trained in cognitive psychology, and contributed to the questioning of results and discussion required to ensure this reflexivity. The first author’s dissertation supervisor also provided support in this way by questioning assumptions made during the initial stages of this work.
Participants were recruited through faculty or departmental listservs for educators. Senior administrators were consulted to ensure that they were aware of and comfortable with this research taking place in their unit. In some cases, administrators identified a few key individuals who were particularly interested in education. These educators were contacted directly by the first author to request participation.
The purposive sample includes four educators from each of four diverse health professional programs ( n = 16 in total): medicine, nursing, pharmacy, and social work. All participants self-identified as being actively involved in teaching in their professional program and all were formally affiliated with either the University of Alberta (Medicine, Nursing, and Pharmacy) or the University of Calgary (Social Work). These four professions were selected to maximize diversity in approaches to critical thinking given that these professions have diverse perspectives and roles with respect to patient care. However, participants all worked in Alberta, Canada, within the same broad postsecondary education and healthcare contexts.
In addition, sampling priority was given to recruiting participants practising in a diverse range of specialties: primary care, geriatrics, paediatrics, mental health, critical care, and various consulting specialties. Specific specialties within each profession are not provided here in an effort to preserve participant anonymity. The goal was not to make conclusions about the perspective of any one group; rather, diversity in profession, practice context, gender, and years in practice was sought to increase the likelihood of illuminating diverse conceptions of critical thinking.
Data generation
Participants were invited to participate in two in-person semi-structured interviews conducted by the first author. All but one participant completed both interviews. Interviews were audio-recorded and interview guides are included in the online Electronic Supplementary Material. The first was about 1 hour in length and discussed how participants think about critical thinking in their teaching, professional practice, and other contexts. Participants were invited to bring a teaching artefact that represented how they teach critical thinking to the interview. Artefacts were used as a visual elicitation strategy to prompt discussion from a new angle [ 24 ]. Questions focused on what the participant thought about teaching critical thinking using the artefact and how they identified critical thinking (or lack thereof) in their students. Artefacts were not analyzed independently of the discussion they produced [ 25 ].
Interview 1 data were analyzed to produce a visual depiction of the aggregate terms, ideas, and relationships described by participants. The visual depiction took the form of a ‘mind map’ (see Appendix C of the Electronic Supplementary Material) that was generated using MindMup free online software [ 26 ]. In developing the mind map, we sought descriptions of participants’ views that remained as close to the data as possible, limiting interpretations and inferences. The ‘clusters’ that appear in the mind map (e. g., the cluster around ‘characteristics of the critical thinker’) represent relationships or categories commonly described when participants discussed those terms. Terms were not weighted or emphasized based on frequency of use (through font size or bolding) in an effort to allow individual participants to emphasize or deemphasize terms as they thought appropriate during the second interview.
Where there was no clear category or relationship, terms were left at the first level of the mind map, connected directly to ‘critical thinking’ at the centre. Including more connections and inferences would likely have improved the readability of the map for participants; however, we chose to include connections and exact language used by participants (even in cases where terms seemed similar) as often as possible, in an effort to limit researcher interpretation. That said, any attempt to aggregate data or to represent relationships is an act of interpretation and some inferences were made in the process, such as the distinction between descriptions about ‘characteristics’ of the critical thinker (the top left hand corner of the map) and ‘processes’ such as ‘reasoning’ or ‘examining assumptions’ (on the right side of the map). The second interview lasted approximately 45 minutes during which a visual elicitation approach invited participants to respond to the mind map.
Visual elicitation involves employing visual stimuli to generate verbal interview data. Participant-generated mind maps are often used in qualitative data collection [ 27 ], but the literature on using researcher-generated diagrams for visual elicitation is relatively thin [ 25 , 28 ]. In this study, using a researcher-generated mind map for visual elicitation offered several advantages. First, as with other forms of visual elicitation, diagrams of this kind can help participants develop candid responses and avoid rehearsed narratives [ 24 , 29 ]. For example, we used mind maps as one mechanism to reduce the tendency for participants who were familiar with the literature on critical thinking to get stuck on narrating seemingly rehearsed definitions of critical thinking. Second, we chose to use a mind map because it provided a social setting through which participants could react to language generated by others. Doing so does not allow the same degree of social negotiation inherent in focus groups, but it avoids the difficulty involved in attempts to disentangle individual from group views [ 30 ]. Third, the visual elicitation method was chosen because it offered a form of member check [ 31 ] that allowed researchers to understand the evolving nature of participants’ conceptions of critical thinking, rather than assuming that participants offer a single true conception during each and every discussion [ 32 ]. In other words, the mind map was used to prompt participants to elaborate their conception of critical thinking and locate it relative to other participants.
In interview 2, participants were asked to begin by discussing areas or terms on the mind map that resonated most with their own conception of critical thinking; they were then asked to discuss terms or concepts on the map that resonated less or with which they disagreed. They were also asked to comment on how relationships between ideas were represented through the map so that researchers could get a sense of the extent to which the relationships between the concepts depicted reflected the participants’ understanding of those relationships [ 28 ]. Participants were encouraged to disagree with portions of the map and most did actively disagree with some of the terms and relationships depicted, suggesting that the map did not come to dictate more than elicit individual interpretations [ 28 ]. Although participants were encouraged to ‘mark up’ the mind map, and the ‘marked up’ mind maps were treated as data, the primary data sources for this study were the audio-recorded interviews [ 25 ].
Participants were aware that the mind map represented aggregate data from the four health professions in the study, but were not initially told whether any of the responses came predominantly from any one profession; they did not generally seem to be attempting to associate terms with other professions. Nonetheless, interview 2 data are a mix of participants’ reactions to the ideas of others and their elaborations of their own understandings. Naturally, these data build on data generated in interview 1, and represent reactions to both the researcher interpretation of the data and to the conceptions of critical thinking offered by others. Interview 1 data tended to offer an initial, open impression of how participants think about critical thinking in their contexts. Because of these different approaches to data generation, quotes from interview 1 and 2 are labelled as ‘INT1’ or ‘INT2’, respectively.
Data analysis
Data were coded through an iterative cycle of initial and focused coding [ 33 ] with NVivo software. Initial line-by-line coding was used to develop codes that were close to the data, involving minimal abstraction. Initial codes were reviewed by the first author and dissertation supervisor to abstract categories (conceptions of critical thinking), sub-categories (features of those conceptions), and themes related to the relationships between those categories. Focused coding involved taking these categories and testing them against the data using constant comparison techniques derived from constructivist grounded theory [ 21 ]. Category development continued during the framing of this paper, and authors engaged in ongoing conversations to modify categories to better fit the data. In this process, we returned to the data to look for exceptions that did not fit any category, as well as contradictions and overlap between categories.
Interpretive sufficiency [ 34 ], in this study, occurred when no new features illustrating participants’ conceptions of critical thinking were identified. Memos were kept to track the development or elimination of initial insights or impressions. Institutional ethics approval was obtained from the University of Alberta.
Participant identities have been masked to preserve anonymity. The abbreviation ‘MD’ refers to educators in medical education, ‘NURS’ to nursing, ‘PHARM’ to pharmacy, and ‘SW’ to social work. Participants within each group were then assigned a number. For example, the code NURS3 is a unique identifier for a single participant.
Three main conceptions of critical thinking were identified, each of which will be elaborated in greater detail below: biomedical critical thinking, humanist critical thinking, and social justice-oriented critical thinking. It is important to note that these categories focus on the process and purpose of critical thinking, as defined by participants. Participant comments also spoke to the ‘characteristics’ or ‘dispositions’ of critical thinkers, such as ‘open-mindedness’ or ‘creativity’. The focus of this study, however, was on uncovering what critical thinking looks like as opposed to what a ‘critical thinker’ looks like.
The results below interweave responses from different professional groups in order to emphasize the way in which each of the three core conceptions that we have identified crosses professional boundaries. We then provide a brief discussion of the relationships between these three conceptions, emphasizing the limited extent to which these conceptions were profession-specific, and the tensions that we observed between these conceptions. In general, we also interweave results from both interviews because the discussion in interview 2 tended to reinforce the themes arising from interview 1, especially with respect to indications that different conceptions were used fluidly by individuals over time and dependent on the context being discussed. The interview from which data arose is marked after each quote and we have mentioned explicitly whenever a comment was made in specific response to the mind map presented during interview 2.
In this way, our data extend the literature on critical thinking by offering an appreciation of how each of these conceptions provide educators a different way of thinking, talking, and teaching about their work in HPE. We found that even individual participants’ conceptions of critical thinking shifted from time to time. That is, they often articulated more than one understanding of critical thinking over the course of an interview or between interviews 1 and 2. Some of these conceptions were shared by multiple participants but individual constellations of beliefs about what critical thinking means were unique and somewhat idiosyncratic. Thus, while participants’ conceptions of critical thinking were both idiosyncratic and common, they were also flexible and contextual; the meaning of critical thinking was continuously reconstructed and contested. In this way, critical thinking offered a window through which to explore how beliefs about what constitutes ‘good thinking’ in a profession are challenged in educational settings.
Biomedical critical thinking
Participants articulating a biomedical approach saw critical thinking and clinical reasoning as nearly synonymous. They emphasized a process that was rational, logical, and systematic. One participant articulated that critical thinking is ‘ to be able to reason logically’ (NURS4 INT1). Another related:
You have to kind of pull together data that’s relevant to the subject you’re dealing with. You have to interpret it, you have to analyse it, and you have to come up with some type of conclusions at the end as to how you deal with it. (PHARM3 INT1)
Participants discussing this approach agreed that critical thinking involved a systematic process of gathering and analyzing data: ‘I think [critical thinking and clinical reasoning] are the same. I think clinical reasoning is basically taking the data you have on a patient and interpreting it, and offering a treatment plan’ (MD1 INT1).
In keeping with an emphasis on the rational and logical, participants espousing this view often reacted negatively when they saw references to emotion on the mind map in interview 2: ‘as soon as you bring your emotions into the room, you’re no longer applying what I think is critical thinking’ (MD4 INT2). Participants also noted that decision-making was an important component of critical thinking: ‘ you have to make a decision. I think it’s a really important part of it’ (MD2 INT2).
For participants from pharmacy, in particular, critical thinking often meant departing from ‘rules’ that guide clinical practice in order to engage in reasoning and make situationally nuanced decisions. One pharmacist, describing a student not engaging in critical thinking, related that the student asked:
‘Have you ever seen Victoza given at 2.4 milligrams daily?’ … It’s very, you know, it’s very much yes or no. But at a deeper level, it’s actually missing things. … [There are] all these other factors that change the decision, right? … On paper there might be a regular set of values for the dose, … [but] without the rest of the background, that’s a very secondary thing. (PHARM4 INT1)
This perspective was identified as the dominant conception of critical thinking because the terms and concepts falling under this broad approach were most frequently discussed by participants; moreover, when participants discussed other conceptions of critical thinking, they were often explicitly drawing contrast to the biomedical view. While the biomedical perspective was dominant in all four groups (although primarily as a contrasting case for social workers), participants tended to occupy more than one perspective over the course of an interview. They might talk primarily about biomedical critical thinking, but also explicitly modify that perspective by drawing on the other two approaches identified: humanist critical and social justice-oriented critical thinking.
Humanist critical thinking
Participants, when adopting this view, described critical thinking as directed toward social good and oriented around positive human relationships. Humanist conceptions of critical thinking were often positioned as an alternative to the dominant biomedical perspective: ‘having to think of somebody else, at their most vulnerable, makes you know that knowledge alone, science alone, won’t get that patient to the place you want the patient to be. It won’t provide the best care’ (NURS1 INT1). In being so positioned, the humanist conception of critical thinking explicitly departed from the biomedical, which emphasized ‘setting aside’ emotion and de-emphasized the role of relationships in healthcare. In the humanist perspective, participants often discussed the purpose of critical thinking as:
Thinking about something for the betterment of yourself and the betterment of others. We’re social beings as human beings. … I think [critical thinking] has a higher purpose. … But I think that [if] critical thinking … [is] a human trait that we have or hope to have, then it has to have those components of what we are as humans. (NURS1 INT1)
Another participant emphasized that: ‘a great part of critical thinking is that human element and the consideration of ultimately what’s a good thing, a common good’ (NURS2 INT1).
In addressing the relational aspects of humanist critical thinking, participants argued that the focus on ‘hard’ sources of data, such as lab tests or imaging, in biomedical critical thinking was limiting. They were concerned that ‘hard data’ tend to be perceived as more objective and thus more important in biomedical critical thinking, compared with subjective patient narratives. They argued that the patient’s story is essential to critical thinking:
I think it doesn’t matter what kind of expert you are, you have to be able to think about patients in the context that they’re in and consider what the patient has to say, and really hear them. So I think that’s an important—that was a total lack of critical thinking in a totally, ‘I’m just going to get through this next patient to the next one’ . (MD1 INT1)
Taken together, these perspectives suggest that biomedical approaches to critical thinking fail to address the complex relational and psychosocial aspects of professional practice.
Social justice-oriented critical thinking
In social justice-oriented approaches to critical thinking participants articulated a process of examining the assumptions and biases embedded in their world. They often explicitly rejected biomedical conceptions of critical thinking as ‘ reductionistic ’ (SW3 INT1) because, in their view, these approaches fail to address the thinker’s own biases. Educators taking a social justice approach felt that: ‘critical thinking … is around things like … recognizing your own bias and recognizing the bias in the world’ (SW1 INT1). In this perspective, participants saw critical thinking as a process of analyzing and addressing the ways in which individual and societal assumptions limit possible actions and access to resources for individuals and social groups.
Unlike biomedical critical thinking and similar to the humanist view, participants articulating this conception tended to make the values and goals of critical thinking, as they conceived of it, explicit. They often contrasted their articulation of values in critical thinking with the ‘assumed’ and unarticulated values present in the biomedical perspective:
If you are not orientated in a social justice position, [critical thinking is] more about the mechanics, which is valuable as well, but … if we don’t understand the values associated with what we think, it seems to not be meaningless but there’s a piece missing or it’s assumed. The values are assumed. (SW3 INT1)
When taking this perspective, participants argued that it is necessary to understand social systems in order to think critically about individual patient cases. One educator questioned:
Why are there a disproportionate number of aboriginal inpatients than any other group? … When you start critically thinking about seeing the whole patient … there are issues related with all of society and that’s why people have more diabetes. (PHARM1 INT1)
Other participants had measured responses to this approach. One participant added to their primarily biomedical approach in order to accommodate perspectives encountered in the mind map, relating that behind their diagnostic work all physicians:
Certainly see a wide spectrum of social and economic status and cultures and things and recognizing that our system is kind of biased against certain groups as it is and knowing that but really not having a good sense of knowing even where to start deconstructing it. (MD2 INT2)
Relationships between conceptions of critical thinking
Results of this study suggest that critical thinking means a variety of things in different contexts and to different people. It might be tempting to see the three approaches outlined above as playing out along professional boundaries. Certainly, the social justice-oriented conception was more common among social work educators; the humanist approach was most common among participants from nursing; perspectives held by physician educators frequently aligned with dominant biomedical conceptions. In pharmacy, educators seemed to straddle all three perspectives, though they commonly emphasized a biomedical approach. Several participants suggested that their faculty or profession has a common understanding of critical thinking: ‘ critical thinking, for me and maybe for our faculty, is around things like … ’ (SW1 INT1).
However, while the disciplinary tendencies discussed above do appear in the data, these tendencies were not stable; participants often held more than one view on what critical thinking meant simultaneously, or shifted between perspectives. Participants also articulated approaches that were not common in their profession at certain moments, positioning themselves as ‘an outlier’, or positioning their specialty as having a different perspective than the profession as a whole, such that critical thinking might mean ‘thinking like a nurse’, or ‘thinking in geriatrics’. Further, participants’ perspectives shifted depending on the context in which they imagined critical thinking occurring.
This type of positioning and re-positioning occurred in both interviews, although they were particularly pronounced in interview 2, where participants were explicitly asked to react to different viewpoints by responding to the mind map. Examples of shifting perspectives in interview 1 occurred especially when participants from medicine shifted between biomedical and humanist conceptions. These shifts suggested a persistent tension and negotiation between characterizations of critical thinking as a rational process of data collection and analysis, and a more humanist approach that accounts for emotion and the relationship between professional and patient or family. Where participants sought to extend their notion of data beyond ‘hard data’ there is a sense of blending humanism with biomedical approaches to critical thinking. In the quote below, the participant brings together a call for a humanist relationship building with a need to gather and analyze all of the data, including important data about the patient’s experience:
I have colleagues who’ll say [to their patients]: ‘just say yes or no.’ … And it’s not very good and they’re missing stuff. So, critical thinking is—I guess it’s sort of dynamic in that you have to have time and you also have to have an interaction. (MD1 INT1)
While the participants described above negotiated between biomedical and humanist perspectives, participants primarily espousing a social justice-oriented conception of critical thinking responded to the ‘assumed’ values of the biomedical model. In talking about a problem solving-oriented biomedical approach, one participant argued that ‘ it’s important as well to have that, those foundational elements of how we think about what we think, but if we don’t understand the values associated … there’s a piece missing’ (SW3 INT1). Another stated that ‘critical thinking seems to be a neutral kind of process or—no, that can’t be true, can it?’ (SW1 INT2) with the mid-sentence shift indicating that two ways of conceptualizing critical thinking had come into conflict. This participant primarily discussed a social justice-oriented conception of critical thinking, which is not neutral, but at this moment also articulated a neutral, clinical reasoning-oriented or biomedical conception.
These relatively organic moments of negotiation certainly demonstrate a sense of conflicting values, of toggling between one perspective and another. However, they also suggest that there are ways in which these contradictions can be productively sustained. In negotiating between humanist and biomedical perspectives, educators effectively modify the dominant perspective.
In interview 2, when discussing the mind map, participants often encountered views that differed from their own. They responded either by making sense of and accommodating the new perspective, or by rejecting it. As an example of the former approach, one physician reacted to the ‘social justice-oriented’ corner of the mind map (specifically ‘examining assumptions’) by explaining how there are:
Assumptions in the background that come up for me all the time in terms of the different ways people live and want to live and how we run into it all the time … it’s always in the background and actually influencing you and until someone challenges the way you approached something, you don’t know what your assumptions are. (MD1 INT2)
As an example of a participant disagreeing with a perspective encountered in the mind map, one participant rejected social justice as an important component of critical thinking in medicine. They related that critical thinking has ‘got everything to do with reasoning, which makes sense. … Social justice has nothing to do with critical thinking’ (MD4 INT2). Interestingly, this participant also spoke at length about the link between social justice and critical thinking in the first interview, suggesting that a conception might seem ‘wrong’ when an individual is thinking and talking about it in one context, and entirely ‘right’ in another context.
Such results demonstrate that individual conceptions of critical thinking are multiple and flexible, not predetermined or stable. Educators bring certain values or perspectives into the foreground as they relate to the context under discussion, while others recede into the background. Though many participants seemed to have a primary perspective, multiple perspectives on critical thinking can co-exist and are actively negotiated by the individual.
In overview, the three broad conceptions of critical thinking offered here (biomedical, humanist, and social justice-oriented) echo approaches to critical thinking found in the critical thinking literature [ 11 , 35 – 37 ]. However, this study extends the literature in two key ways. First, our data point to ways in which different conceptions of critical thinking conflict and coalesce, within the field, within each profession, and even within individuals. Second, this tension offers an early empirical account of critical thinking in the health professions that suggests there may be benefits to maintaining flexibility in how one conceives of the concept.
The diverse conceptions of critical thinking identified all appear to have some value in HPE. It might be tempting to view each conception as a unique but stable perspective, reflecting thinking skills that are used within a particular context or value orientation. However, the multiplicity and flexibility of participants’ conceptions in this study offers some explanation as to why previous attempts to develop either generic (e. g. [ 2 , 3 , 5 ]) or discipline-specific [ 13 , 15 – 17 ] definitions and delineations of critical thinking have failed to stick.
Conceptions of critical thinking are not stable within a context or for a single educator. Educators’ conceptions of critical thinking shift within and between contexts as they navigate overlapping sets of values and beliefs. When educators take up different conceptions of critical thinking, the shifts they make are not just pragmatic; they actively negotiate the values and practices of the different communities in which they participate. Although we certainly saw hints of differences between professions, the strength of this study is that it captured the ways in which conceptions of critical thinking are not stably tied to any given profession. Critical thinking is connected to a broader idea of what ‘good thinking’—and, by extension, the ‘good professional’—looks like for each educator [ 38 ] within a given context or community.
These observations lead one to speculate about what purpose fluidity in conceptions of critical thinking might serve. Educators often have different values and goals for their profession, and, thus, it is not surprising that the meaning of critical thinking would be contested both within and across professions. Through their conceptions of critical thinking, participants contest ideas about what thinking is for in their profession—whether it should be focused on individual patient ‘problems’ or broader social issues, and the extent to which humanism is an important component of healthcare.
It is understandable that so much of the literature on critical thinking has sought to clarify a single ‘right’ definition; there is an argument for making a collective decision about what ‘good thinking’ means. Such a decision might offer clarity to interprofessional teaching and practice, or provide a foundation on which educational policy can be based. However, the critical thinking literature has long sought such a universal agreement and disagreements persist. Results of this study suggest a new approach, one that can account for multiple conceptions of critical thinking within and across health professions and practice contexts. The visual elicitation approach employed, asking participants to respond to the mind map, offered a unique perspective on the data that illuminated contradictions between conceptions held by individual participants, between participants, and between the conceptions themselves.
Such an approach offers a vehicle for thinking and talking about what kind of thinking is valued, both within and between professions. When conceptions of critical thinking are understood as flexible instead of stable, these acts of modification and contestation can be viewed as potential moments for critical self-reflection for individuals and for professional groups on the whole. Moreover, through their discussions of critical thinking, educators actively intervened to consider and assert what they value in their work.
These different conceptions might be complementary as often as they are incompatible. In fact, we would argue that ‘good thinking’ is inherently contentious (and should be) because it is such struggles over what ‘the good’ means in HPE that allow for challenges to the status quo. Advances at the heart of HPE and practice have been hard-won through deliberate reflection, discussion, action, and (often) conflict. For example, the ongoing movement toward relationship-oriented care has arguably occurred as a result of unexpected pushback regarding the limits of considering good healthcare as being entirely patient-centred. Thus, there is a need to bring unarticulated assumptions about important topics into the light so that the goals and values of educators and policy-makers can be openly discussed, even though they are unlikely to ever be fully resolved.
Strengths and limitations
This study offered a broad sample of educators from four different professions, who practised in a range of disciplinary contexts. Given that the sampling approach taken sought breadth rather than depth, the results explore a range of conceptions of critical thinking across HPE, rather than allowing strong claims about any one profession or context. The sample also focussed on conceptions of critical thinking within health professions education at specific institutions in Edmonton, Alberta. A multi-institutional study might build on these results to elaborate the extent to which each health profession has a core shared conception of critical thinking that translates across institutional settings. We expect that there may be significant differences between settings, given that what is meant by critical thinking seems to be highly contextual, even from moment to moment. Mapping aspects of context that impact how individuals and groups think about critical thinking would tell us much more about the values on which these conceptions are based.
Subsequent studies might also explore the extent to which conceptions of critical thinking among those identifying as ‘educators’ are comparable to those identifying as primarily ‘clinicians’. Although the boundary is definitely blurry, these groups engage in different kinds of work and participate in different communities, which we suspect may result in differences in how they conceive of critical thinking.
Conclusions
Rather than attempting to ‘solve’ the debate about what critical thinking should mean, this study maps the various conceptions of this term articulated by health professional educators. Educators took up biomedical, humanist, and social justice-oriented conceptions of critical thinking, and their conceptions often shifted from moment to moment or from context to context. The ‘mapping’ approach adopted to study this issue allowed for an appreciation of the ways in which educators actively modify and contest educational and professional values, even within their own thinking. Because critical thinking appears to be both value and context driven, arriving at a single right definition or taxonomy of critical thinking is unlikely to resolve deep tensions around what ‘good thinking’ in HPE means. Moreover, such an approach is unlikely to be productive. Such tensions produce challenges for shared understanding at the same time that they produce a productive space for discussion about core issues in HPE.
Caption Electronic Supplementary Material
Acknowledgements.
We thank Dr. Paul Newton for his contributions to the analysis of these data, in his role as supervisor of the dissertation work on which this manuscript is based. Thanks also to Dr. Dan Pratt for his help and support in developing this manuscript.
Support for this work was provided by the Government of Alberta (Queen Elizabeth II Graduate Scholarship), by the Social Sciences and Humanities Research Council (Doctoral Fellowship), and by the University of British Columbia (Postdoctoral Fellowship).
Biographies
PhD, is Postdoctoral Fellow in the Centre for Health Education Scholarship, University of British Columbia. This manuscript reports on doctoral research at the Department of Educational Policy Studies, University of Alberta.
PhD, is Associate Director and Senior Scientist in the Centre for Health Education Scholarship, and Professor and Director of Educational Research and Scholarship in the Department of Medicine, at the University of British Columbia.
Conflict of interest
R. Kahlke and K. Eva declare that they have no competing interests.
- Skip to primary navigation
- Skip to main content
- Skip to primary sidebar
- Skip to footer

Global Cognition
Critical thinking in decision making.
by Winston Sieck updated September 12, 2021

Critical thinking is often talked about as a stand-alone activity. Like some other individual activities, thinking critically may just feel good. Yet, critical thinking seems most useful when it aids other cognitive processes, such as applying critical thinking in decision making.
Anne Helsdingen from the Open University of the Netherlands and her colleagues studied an interesting issue about critical thinking in decision making. They wanted to know whether teaching critical thinking skills can improve judgment and decision making in general.
Helsdingen and her team define critical thinking as reasoned thinking with a purpose. They also describe some core critical thinking skills and abilities, such as being able to:
- Appreciate that your own opinions may be wrong
- Accept statements as true even when they conflict with your own views
- Temporarily adopt an initial position with which you disagree, and then reason from that starting point
A challenge, according to these researchers, is how to teach skills for critical thinking in decision making so that they transfer to new decision making problems. Transfer means being able to apply what you have learned to new tasks or new situations.
To tackle this problem, they start with a useful cognitive model of how decisions are made . Numerous researchers have worked with similar versions of the model of the years. One version is called “explanation-based decision making,” or the “story model.”
The idea is that people encounter situations. When they do, they recognize important parts of the situation from past experience. They then create a story (or explanation) about what’s going on and what will happen. They make decisions based on their story, and how things have turned out in similar stories past.
A problem with making decisions this way is that our stories tend to be less complete than we think – a failure of metacognition. We also overlook inconsistent details because we’re sucked in by the good story. According to Helsdingen, we might improve our intuitive approach by bringing critical thinking in the decision making process.
The researchers tested a method for including critical thinking in decision making. First, they explained the story model of decision making. Then, they prompted the learners to reflect on their story and thinking critically about it. Some of the questions they included to prompt critical thinking were:
- Do you have all the necessary information?
- Is there any conflict in the evidence?
- The devil’s advocate tells you that your story is wrong. Make up an alternative story. Is it more plausible than the original?
The students in the study read through cases about crimes that had been committed. Their job was to decide on the priority of each case for the police. They got feedback, so they could learn what makes cases more important in police work.
Some of the students received the critical thinking skills training while making these decisions. Others did not.
How well they made these crime decisions was not the most important thing, though. The main thing was how well they would do in a different situation after learning about critical thinking in decision making. That is, would their new skills transfer?
The researchers tested for transfer by having the students make different decisions about traffic offenses. The overall results suggested that the training on how to include critical thinking in decision making was effective. The benefits did transfer to the new decision making task.
As you come across decisions that you need to make, pay some attention to the stories you are telling yourself in the process. Use some of the ideas above and other critical thinking skills to improve your story and decision. Writing is also an excellent strategy for making good decisions . It may seem like a bit of extra work at first, but with practice will become more natural for your future decisions.
Image Credit: Critical thinking asylum
Helsdingen, A., van Gog, T., & van Merriënboer, J. (2011). The effects of practice schedule and critical thinking prompts on learning and transfer of a complex judgment task. Journal of Educational Psychology, 103 (2), 383-398 DOI: 10.1037/a0022370
About Winston Sieck
Dr. Winston Sieck is a cognitive psychologist working to advance the development of thinking skills. He is founder and president of Global Cognition, and director of Thinker Academy .
Reader Interactions
January 13, 2013 at 6:36 pm
Thanks for sharing this research and the ‘story’. We are often asked whether you can learn to be a better critical thinker – I wouldn’t be teaching it if I didn’t believe it to be the case! But it helps to have research to support this belief.
Our work is focused on critical thinking in organizational, workplace settings with all sorts of employees, including managers and executives. My experience is pretty similar to that you gave in the case; in the moment, on a particular case, the ‘decision’ may not be improved.
As the researchers and you point out, the proof is in the pudding. Can people learn and apply simple critical thinking techniques, consistently and effectively, and, does this lead to better outcomes?
We find that it can be overwhelming to try to teach too much at a clip. We boil it down to simple questions, job aids, and worksheets that can help people – especially people working on teams – to establish a common vocabulary, and create an environment that reinforces critical thinking rather than viewing it as generating conflict and controversy.
February 21, 2014 at 4:02 am
I am interested in teaching critical thinking skills to Law Enforcement, specifically to a group of people age 14 to 18 who are interested in pursuing a Law Enforcement Career (The Police Explorer Program) but then later to already established officers.
A law enforcement officer (LEO) is called upon to make decisions and wield power which effect others lives, and they are often required to do this on the spot, with a limited amount of time and information available. They make these decisions every day and I am looking for ways to sharpen their skills and help them make the best decisions possible with the information they have on hand.
I couldn’t help but notice that this study happened to be centered on LEO scenarios. I was wondering if I could adapt this study to a class for young people. Any thoughts?
Also, how could I get the specifics of this study, to include the specific scenarios used?
February 21, 2014 at 9:34 am
That sounds really interesting, Eric. I contacted Anne Helsdingen on your behalf, and shared your contact information with her.
February 28, 2016 at 11:40 pm
For the last five years I have taught CT to serving LEOs, although only slowly at first; it is a sharp departure from traditional police training. While new theories come out on how to fix a profession currently under enormous pressure, many of them have been around for 10 or 20 years whereas CT has been developed over at least 25 centuries. I would be happy to share my work and experiences to to hear of others’ work too.
- Save Your Ammo
- Publications
GC Blog Topics
- Culture & Communication
- Thinking & Deciding
- Learning Skills
- Learning Science
Online Courses
- Thinker Academy
- Study Skills Course
- For Parents
- For Teachers

COMMENTS
Relationship Between Critical Thinking and Mental Health. Associating critical thinking with mental health is not without reason, since theories of psychotherapy have long stressed a linkage between mental problems and dysfunctional thinking (Gilbert, 2003; Gambrill, 2005; Cuijpers, 2019).Proponents of cognitive behavioral therapy suggest that the interpretation by people of a situation ...
Wellness encompasses 8 mutually interdependent dimensions: physical, intellectual, emotional, social, spiritual, vocational, financial, and environmental ( Table 1) ( 1 ). Attention must be given to all the dimensions, as neglect of any one over time will adversely affect the others, and ultimately one's health, well-being, and quality of life.
In this special section of Medical Decision Making, 3 developers of evidence-based theories of medical decision making and health present their approaches: Fishbein (theory of reasoned action); Prochaska (transtheoretical model); and Reyna (fuzzy-trace theory).Spring, chair of the Evidence-Based Practice Committee of the Society for Behavioral Medicine, follows with a commentary on the 3 ...
Intellectual wellness: Just as a flexible body indicates physical health, a flexible mind indicates intellectual health. When you're intellectually healthy, you value lifelong learning, foster critical thinking, develop moral reasoning, expand worldviews, and engage in education for the pursuit of knowledge.
In Chapter 10 ("Clinical Decision Making and Risk Management"), Steven A. Sobelman and Jeffrey N. Younggren offer an important perspective on how understanding risk can enhance clinical management. Formal train-ing in decision making is not yet part of graduate curricula in behavioral and mental health programs.
There is certainly scope for improving the quality of patient decision-making (Fowler et al. 2011). The development of robust critical thinking skills is a good place to begin this improvement. Critical thinking skills are also a vital resource for the medical and health professionals who deliver our healthcare.
Definition. Clinical reasoning or professional decision-making in the health professions is a context-dependent, complex, encultured, and professional way of thinking and decision-making to guide high-quality, professionally responsible practice actions.. Contextually, clinical reasoning: Occurs within health professional practice, meaning it is governed by the purpose of enhancing health and ...
Analysis of the data indicated that critical thinking ability was significantly higher in older nurses and nurses with more than 5 years of experience. The findings of this study indicated that critical thinking ability, working years, position/title, and education level were the 4 significant predictors of nursing competence.
Decision-making is a crucial skill that has a central role in everyday life and is necessary for adaptation to the environment and autonomy. It is the ability to choose between two or more options, and it has been studied through several theoretical approaches and by different disciplines. In this overview article, we contend a theoretical review regarding most theorizing and research on ...
If the crazes of the past have faded away, we should probably view any new trends that rise up through a critical lens. Amidst this sea of health crazes, it's ultimately up to you to think critically and find the one that's effective, healthy, and right for you. Learn about why health crazes become popular and how you can use critical thinking ...
The application of System 1 and System 2 decision-making behavior in the context of health and fitness can have wide-ranging potential personal and global public health implications, and is described here as behavioral health and fitness. [ Health is defined as all areas of the body working in harmony, while fitness is the ability to perform ...
Critical thinking underlies independent and interdependent decision making. Critical thinking includes questioning, analysis, synthesis, interpretation, inference, inductive and deductive reasoning, intuition, application, and creativity 8 (p. 9). Course work or ethical experiences should provide the graduate with the knowledge and skills to:
Globally, there is a growing interest in using the research evidence in public health policy-making [1, 2].Public health systems are diverse and complex, and health policymakers face many challenges in developing and implementing policies and programs that are required to be efficient [1, 3].The use of scientific evidence is considered to be an effective approach in the decision-making process ...
In a society where people are already concerned about the population's lack of critical thinking skills, evidence that such skills can be taught, and that they can be used to help people make better-informed decisions about their health, provides us with plenty of reason to fight for the teaching of critical thinking skills.
Here are five ways to nurture your critical-thinking skills: Be a lifelong learner. Continuous learning through educational courses and professional development lets you stay current with evidence-based practice. That knowledge helps you make informed decisions in stressful moments. Practice reflection.
Clinical decision-making is a complex process involving information processing, evaluation of evidence, and application of relevant knowledge to select the appropriate interventions that provide high-quality care and reduce risk of patient harm. Decision-making can range from fast, intuitive, or heuristic to carefully reasoned, analytical, or ...
Likewise, the results of the study of Anderson et al., show that clinical judgment and critical thinking play a key role in making clinical decisions in all situations, in particular the critical and complicated conditions which prevail in pre-hospital emergency care . In the present study, the participants stated that some of their colleagues ...
Simply put, critical thinking is the act of deliberately analyzing information so that you can make better judgements and decisions. It involves using things like logic, reasoning, and creativity, to draw conclusions and generally understand things better. This may sound like a pretty broad definition, and that's because critical thinking is a ...
This chapter examines multiple thinking strategies that are needed for high-quality clinical practice. Clinical reasoning and judgment are examined in relation to other modes of thinking used by ...
Using Critical Thinking Skills in Problem Solving. Think of problem solving as a process with four Ps: Define the problem, generate possibilities, create a plan, and perform your plan. Step 1: Define the problem. To define a problem effectively, understand what a problem is—a mismatch between what you want and what you have.
Critical thinking is connected to a broader idea of what 'good thinking'—and, by extension, the 'good professional'—looks like for each educator [ 38] within a given context or community. These observations lead one to speculate about what purpose fluidity in conceptions of critical thinking might serve.
According to Helsdingen, we might improve our intuitive approach by bringing critical thinking in the decision making process. The researchers tested a method for including critical thinking in decision making. First, they explained the story model of decision making. Then, they prompted the learners to reflect on their story and thinking ...
Intellectual. _____ wellness is the ability to develop, enhance, and apply decision-making, critical thinking, and problem-solving skills. Spiritual. _____ wellness includes developing a set of core beliefs, principles, or values that give purpose, unity, and meaning to life and guide one's thoughts and actions. Wellness.