Change Password
Your password must have 8 characters or more and contain 3 of the following:.
- a lower case character,
- an upper case character,
- a special character

Password Changed Successfully
Your password has been changed
- Sign in / Register
Request Username
Can't sign in? Forgot your username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username
An Exploratory Study of Students with Depression in Undergraduate Research Experiences
- Katelyn M. Cooper
- Logan E. Gin
- M. Elizabeth Barnes
- Sara E. Brownell
*Address correspondence to: Katelyn M. Cooper ( E-mail Address: [email protected] ).
Department of Biology, University of Central Florida, Orlando, FL, 32816
Search for more papers by this author
Biology Education Research Lab, Research for Inclusive STEM Education Center, School of Life Sciences, Arizona State University, Tempe, AZ 85281
Depression is a top mental health concern among undergraduates and has been shown to disproportionately affect individuals who are underserved and underrepresented in science. As we aim to create a more inclusive scientific community, we argue that we need to examine the relationship between depression and scientific research. While studies have identified aspects of research that affect graduate student depression, we know of no studies that have explored the relationship between depression and undergraduate research. In this study, we sought to understand how undergraduates’ symptoms of depression affect their research experiences and how research affects undergraduates’ feelings of depression. We interviewed 35 undergraduate researchers majoring in the life sciences from 12 research-intensive public universities across the United States who identify with having depression. Using inductive and deductive coding, we identified that students’ depression affected their motivation and productivity, creativity and risk-taking, engagement and concentration, and self-perception and socializing in undergraduate research experiences. We found that students’ social connections, experiencing failure in research, getting help, receiving feedback, and the demands of research affected students’ depression. Based on this work, we articulate an initial set of evidence-based recommendations for research mentors to consider in promoting an inclusive research experience for students with depression.
INTRODUCTION
Depression is described as a common and serious mood disorder that results in persistent feelings of sadness and hopelessness, as well as a loss of interest in activities that one once enjoyed ( American Psychiatric Association [APA], 2013 ). Additional symptoms of depression include weight changes, difficulty sleeping, loss of energy, difficulty thinking or concentrating, feelings of worthlessness or excessive guilt, and suicidality ( APA, 2013 ). While depression results from a complex interaction of psychological, social, and biological factors ( World Health Organization, 2018 ), studies have shown that increased stress caused by college can be a significant contributor to student depression ( Dyson and Renk, 2006 ).
Depression is one of the top undergraduate mental health concerns, and the rate of depression among undergraduates continues to rise ( Center for Collegiate Mental Health, 2017 ). While we cannot discern whether these increasing rates of depression are due to increased awareness or increased incidence, it is clear that is a serious problem on college campuses. The percent of U.S. college students who self-reported a diagnosis with depression was recently estimated to be about 25% ( American College Health Association, 2019 ). However, higher rates have been reported, with one study estimating that up to 84% of undergraduates experience some level of depression ( Garlow et al. , 2008 ). Depression rates are typically higher among university students compared with the general population, despite being a more socially privileged group ( Ibrahim et al. , 2013 ). Prior studies have found that depression is negatively correlated with overall undergraduate academic performance ( Hysenbegasi et al. , 2005 ; Deroma et al. , 2009 ; American College Health Association, 2019 ). Specifically, diagnosed depression is associated with half a letter grade decrease in students’ grade point average ( Hysenbegasi et al. , 2005 ), and 21.6% of undergraduates reported that depression negatively affected their academic performance within the last year ( American College Health Association, 2019 ). Provided with a list of academic factors that may be affected by depression, students reported that depression contributed to lower exam grades, lower course grades, and not completing or dropping a course.
Students in the natural sciences may be particularly at risk for depression, given that such majors are noted to be particularly stressful due to their competitive nature and course work that is often perceived to “weed students out”( Everson et al. , 1993 ; Strenta et al. , 1994 ; American College Health Association, 2019 ; Seymour and Hunter, 2019 ). Science course instruction has also been described to be boring, repetitive, difficult, and math-intensive; these factors can create an environment that can trigger depression ( Seymour and Hewitt, 1997 ; Osborne and Collins, 2001 ; Armbruster et al ., 2009 ; Ceci and Williams, 2010 ). What also distinguishes science degree programs from other degree programs is that, increasingly, undergraduate research experiences are being proposed as an essential element of a science degree ( American Association for the Advancement of Science, 2011 ; President’s Council of Advisors on Science and Technology, 2012 ; National Academies of Sciences, Engineering, and Medicine [NASEM], 2017 ). However, there is some evidence that undergraduate research experiences can add to the stress of college for some students ( Cooper et al. , 2019c ). Students can garner multiple benefits from undergraduate research, including enhanced abilities to think critically ( Ishiyama, 2002 ; Bauer and Bennett, 2003 ; Brownell et al. , 2015 ), improved student learning ( Rauckhorst et al. , 2001 ; Brownell et al. , 2015 ), and increased student persistence in undergraduate science degree programs ( Jones et al. , 2010 ; Hernandez et al. , 2018 ). Notably, undergraduate research experiences are increasingly becoming a prerequisite for entry into medical and graduate programs in science, particularly elite programs ( Cooper et al. , 2019d ). Although some research experiences are embedded into formal lab courses as course-based undergraduate research experiences (CUREs; Auchincloss et al. , 2014 ; Brownell and Kloser, 2015 ), the majority likely entail working with faculty in their research labs. These undergraduate research experiences in faculty labs are often added on top of a student’s normal course work, so they essentially become an extracurricular activity that they have to juggle with course work, working, and/or personal obligations ( Cooper et al. , 2019c ). While the majority of the literature surrounding undergraduate research highlights undergraduate research as a positive experience ( NASEM, 2017 ), studies have demonstrated that undergraduate research experiences can be academically and emotionally challenging for students ( Mabrouk and Peters, 2000 ; Seymour et al. , 2004 ; Cooper et al. , 2019c ; Limeri et al. , 2019 ). In fact, 50% of students sampled nationally from public R1 institutions consider leaving their undergraduate research experience prematurely, and about half of those students, or 25% of all students, ultimately leave their undergraduate research experience ( Cooper et al. , 2019c ). Notably, 33.8% of these individuals cited a negative lab environment and 33.3% cited negative relationships with their mentors as factors that influenced their decision about whether to leave ( Cooper et al. , 2019c ). Therefore, students’ depression may be exacerbated in challenging undergraduate research experiences, because studies have shown that depression is positively correlated with student stress ( Hish et al. , 2019 ).
While depression has not been explored in the context of undergraduate research experiences, depression has become a prominent concern surrounding graduate students conducting scientific research. A recent study that examined the “graduate student mental health crisis” ( Flaherty, 2018 ) found that work–life balance and graduate students’ relationships with their research advisors may be contributing to their depression ( Evans et al. , 2018 ). Specifically, this survey of 2279 PhD and master’s students from diverse fields of study, including the biological/physical sciences, showed that 39% of graduate students have experienced moderate to severe depression. Fifty-five percent of the graduate students with depression who were surveyed disagreed with the statement “I have good work life balance,” compared to only 21% of students with depression who agreed. Additionally, the study highlighted that more students with depression disagreed than agreed with the following statements: their advisors provided “real” mentorship, their advisors provided ample support, their advisors positively impacted their emotional or mental well-being, their advisors were assets to their careers, and they felt valued by their mentors. Another recent study identified that depression severity in biomedical doctoral students was significantly associated with graduate program climate, a perceived lack of employment opportunities, and the quality of students’ research training environment ( Nagy et al. , 2019 ). Environmental stress, academic stress, and family and monetary stress have also been shown to be predictive of depression severity in biomedical doctoral students ( Hish et al. , 2019 ). Further, one study found that self-esteem is negatively correlated and stress is positively correlated with graduate student depression; presumably research environments that challenge students’ self-esteem and induce stress are likely contributing to depressive symptoms among graduate students ( Kreger, 1995 ). While these studies have focused on graduate students, and there are certainly notable distinctions between graduate and undergraduate research, the research-related factors that affect graduate student depression, including work–life balance, relationships with mentors, research environment, stress, and self-esteem, may also be relevant to depression among undergraduates conducting research. Importantly, undergraduates in the United States have reported identical levels of depression as graduate students but are often less likely to seek mental health care services ( Wyatt and Oswalt, 2013 ), which is concerning if undergraduate research experiences exacerbate depression.
Based on the literature on the stressors of undergraduate research experiences and the literature identifying some potential causes of graduate student depression, we identified three aspects of undergraduate research that may exacerbate undergraduates’ depression. Mentoring: Mentors can be an integral part of a students’ research experience, bolstering their connections with others in the science community, scholarly productivity, and science identity, as well as providing many other benefits ( Thiry and Laursen, 2011 ; Prunuske et al. , 2013 ; Byars-Winston et al. , 2015 ; Aikens et al. , 2016 , 2017 ; Thompson et al. , 2016 ; Estrada et al. , 2018 ). However, recent literature has highlighted that poor mentoring can negatively affect undergraduate researchers ( Cooper et al. , 2019c ; Limeri et al. , 2019 ). Specifically, one study of 33 undergraduate researchers who had conducted research at 10 institutions identified seven major ways that they experienced negative mentoring, which included absenteeism, abuse of power, interpersonal mismatch, lack of career support, lack of psychosocial support, misaligned expectations, and unequal treatment ( Limeri et al. , 2019 ). We hypothesize negative mentoring experiences may be particularly harmful for students with depression, because support, particularly social support, has been shown to be important for helping individuals with depression cope with difficult circumstances ( Aneshensel and Stone, 1982 ; Grav et al. , 2012 ). Failure: Experiencing failure has been hypothesized to be an important aspect of undergraduate research experiences that may help students develop some the most distinguishing abilities of outstanding scientists, such as coping with failure, navigating challenges, and persevering ( Laursen et al. , 2010 ; Gin et al. , 2018 ; Henry et al. , 2019 ). However, experiencing failure and the stress and fatigue that often accompany it may be particularly tough for students with depression ( Aldwin and Greenberger, 1987 ; Mongrain and Blackburn, 2005 ). Lab environment: Fairness, inclusion/exclusion, and social support within one’s organizational environment have been shown to be key factors that cause people to either want to remain in the work place and be productive or to want to leave ( Barak et al. , 2006 ; Cooper et al. , 2019c ). We hypothesize that dealing with exclusion or a lack of social support may exacerbate depression for some students; patients with clinical depression react to social exclusion with more pronounced negative emotions than do individuals without clinical depression ( Jobst et al. , 2015 ). While there are likely other aspects of undergraduate research that affect student depression, we hypothesize that these factors have the potential to exacerbate negative research experiences for students with depression.
Depression has been shown to disproportionately affect many populations that are underrepresented or underserved within the scientific community, including females ( American College Health Association, 2018 ; Evans et al. , 2018 ), first-generation college students ( Jenkins et al. , 2013 ), individuals from low socioeconomic backgrounds ( Eisenberg et al. , 2007 ), members of the LGBTQ+ community ( Eisenberg et al. , 2007 ; Evans et al. , 2018 ), and people with disabilities ( Turner and Noh, 1988 ). Therefore, as the science community strives to be more diverse and inclusive ( Intemann, 2009 ), it is important that we understand more about the relationship between depression and scientific research, because negative experiences with depression in scientific research may be contributing to the underrepresentation of these groups. Specifically, more information is needed about how the research process and environment of research experiences may affect depression.
Given the high rate of depression among undergraduates, the links between depression and graduate research, the potentially challenging environment of undergraduate research, and how depression could disproportionately impact students from underserved communities, it is imperative to begin to explore the relationship between scientific research and depression among undergraduates to create research experiences that could maximize student success. In this exploratory interview study, we aimed to 1) describe how undergraduates’ symptoms of depression affect their research experiences, 2) understand how undergraduate research affects students’ feelings of depression, and 3) identify recommendations based on the literature and undergraduates’ reported experiences to promote a positive research experience for students with depression.
This study was done with an approved Arizona State University Institutional Review Board protocol #7247.
In Fall 2018, we surveyed undergraduate researchers majoring in the life sciences across 25 research-intensive (R1) public institutions across the United States (specific details about the recruitment of the students who completed the survey can be found in Cooper et al. (2019c) ). The survey asked students for their opinions about their undergraduate research experiences and their demographic information and whether they would be interested in participating in a follow-up interview related to their research experiences. For the purpose of this study, we exclusively interviewed students about their undergraduate research experiences in faculty member labs; we did not consider students’ experiences in CUREs. Of the 768 undergraduate researchers who completed the survey, 65% ( n = 496) indicated that they would be interested in participating in a follow-up interview. In Spring 2019, we emailed the 496 students, explaining that we were interested in interviewing students with depression about their experiences in undergraduate research. Our specific prompt was: “If you identify as having depression, we would be interested in hearing about your experience in undergraduate research in a 30–60 minute online interview.” We did not define depression in our email recruitment because we conducted think-aloud interviews with four undergraduates who all correctly interpreted what we meant by depression ( APA, 2013 ). We had 35 students agree to participate in the interview study. The interview participants represented 12 of the 25 R1 public institutions that were represented in the initial survey.
Student Interviews
We developed an interview script to explore our research questions. Specifically, we were interested in how students’ symptoms of depression affect their research experiences, how undergraduate research negatively affects student depression, and how undergraduate research positively affects student depression.
We recognized that mental health, and specifically depression, can be a sensitive topic to discuss with undergraduates, and therefore we tried to minimize any discomfort that the interviewees might experience during the interview. Specifically, we conducted think-aloud interviews with three graduate students who self-identified with having depression at the time of the interview. We asked them to note whether any interview questions made them uncomfortable. We also sought their feedback on questions given their experiences as persons with depression who had once engaged in undergraduate research. We revised the interview protocol after each think-aloud interview. Next, we conducted four additional think-aloud interviews with undergraduates conducting basic science or biology education research who identified with having depression to establish cognitive validity of the questions and to elicit additional feedback about any questions that might make someone uncomfortable. The questions were revised after each think-aloud interview until no question was unclear or misinterpreted by the students and we were confident that the questions minimized students’ potential discomfort ( Trenor et al. , 2011 ). A copy of the final interview script can be found in the Supplemental Material.
All interviews were individually conducted by one of two researchers (K.M.C. and L.E.G.) who conducted the think-aloud interviews together to ensure that their interviewing practices were as similar as possible. The interviews were approximately an hour long, and students received a $15 gift card for their participation.
Personal, Research, and Depression Demographics
All student demographics and information about students’ research experiences were collected using the survey distributed to students in Fall 2018. We collected personal demographics, including the participants’ gender, race/ethnicity, college generation status, transfer status, financial stability, year in college, major, and age. We also collected information about the students’ research experiences, including the length of their first research experiences, the average number of hours they spend in research per week, how they were compensated for research, who their primary mentors were, and the focus areas of their research.
In the United States, mental healthcare is disproportionately unavailable to Black and Latinx individuals, as well as those who come from low socioeconomic backgrounds ( Kataoka et al. , 2002 ; Howell and McFeeters, 2008 ; Santiago et al. , 2013 ). Therefore, to minimize a biased sample, we invited anyone who identified with having depression to participate in our study; we did not require students to be diagnosed with depression or to be treated for depression in order to participate. However, we did collect information about whether students had been formally diagnosed with depression and whether they had been treated for depression. After the interview, all participants were sent a link to a short survey that asked them if they had ever been diagnosed with depression and how, if at all, they had ever been treated for depression. A copy of these survey questions can be found in the Supplemental Material. The combined demographic information of the participants is in Table 1 . The demographics for each individual student can be found in the Supplemental Material.
a Students reported the time they had spent in research 6 months before being interviewed and only reported on the length of time of their first research experiences.
b Students were invited to report multiple ways in which they were treated for their depression; other treatments included lifestyle changes and meditation.
c Students were invited to report multiple means of compensation for their research if they had been compensated for their time in different ways.
d Students were asked whether they felt financially stable, particularly during the undergraduate research experience.
e Students reported who they work/worked with most closely during their research experiences.
f Staff members included lab coordinators or lab managers.
g Other focus areas of research included sociology, linguistics, psychology, and public health.
Interview Analysis
The initial interview analysis aimed to explore each idea that a participant expressed ( Charmaz, 2006 ) and to identify reoccurring ideas throughout the interviews. First, three authors (K.M.C., L.E.G., and S.E.B.) individually reviewed a different set of 10 interviews and took detailed analytic notes ( Birks and Mills, 2015 ). Afterward, the authors compared their notes and identified reoccurring themes throughout the interviews using open coding methods ( Saldaña, 2015 ).
Once an initial set of themes was established, two researchers (K.M.C. and L.E.G.) individually reviewed the same set of 15 randomly selected interviews to validate the themes identified in the initial analysis and to screen for any additional themes that the initial analysis may have missed. Each researcher took detailed analytic notes throughout the review of an interview, which they discussed after reviewing each interview. The researchers compared what quotes from each interview they categorized into each theme. Using constant comparison methods, they assigned quotes to each theme and constantly compared the quotes to ensure that each quote fit within the description of the theme ( Glesne and Peshkin, 1992 ). In cases in which quotes were too different from other quotes, a new theme was created. This approach allowed for multiple revisions of the themes and allowed the authors to define a final set of codes; the researchers created a final codebook with refined definitions of emergent themes (the final coding rubric can be found in the Supplemental Material). Once the final codebook was established, the researchers (K.M.C. and L.E.G.) individually coded seven additional interviews (20% of all interviews) using the coding rubric. The researchers compared their codes, and their Cohen’s κ interrater score for these seven interviews was at an acceptable level (κ = 0.88; Landis and Koch, 1977 ). One researcher (L.E.G.) coded the remaining 28 out of 35 interviews. The researchers determined that data saturation had been reached with the current sample and no further recruitment was needed ( Guest et al. , 2006 ). We report on themes that were mentioned by at least 20% of students in the interview study. In the Supplemental Material, we provide the final coding rubric with the number of participants whose interview reflected each theme ( Hannah and Lautsch, 2011 ). Reporting the number of individuals who reported themes within qualitative data can lead to inaccurate conclusions about the generalizability of the results to a broader population. These qualitative data are meant to characterize a landscape of experiences that students with depression have in undergraduate research rather than to make claims about the prevalence of these experiences ( Glesne and Peshkin, 1992 ). Because inferences about the importance of these themes cannot be drawn from these counts, they are not included in the results of the paper ( Maxwell, 2010 ). Further, the limited number of interviewees made it not possible to examine whether there were trends based on students’ demographics or characteristics of their research experiences (e.g., their specific area of study). Quotes were lightly edited for clarity by inserting clarification brackets and using ellipses to indicate excluded text. Pseudonyms were given to all students to protect their privacy.
The Effect of Depressive Symptoms on Undergraduate Research
We asked students to describe the symptoms associated with their depression. Students described experiencing anxiety that is associated with their depression; this could be anxiety that precedes their depression or anxiety that results from a depressive episode or a period of time when an individual has depression symptoms. Further, students described difficulty getting out of bed or leaving the house, feeling tired, a lack of motivation, being overly self-critical, feeling apathetic, and having difficulty concentrating. We were particularly interested in how students’ symptoms of depression affected their experiences in undergraduate research. During the think-aloud interviews that were conducted before the interview study, graduate and undergraduate students consistently described that their depression affected their motivation in research, their creativity in research, and their productivity in research. Therefore, we explicitly asked undergraduate researchers how, if at all, their depression affected these three factors. We also asked students to describe any additional ways in which their depression affected their research experiences. Undergraduate researchers commonly described five additional ways in which their depression affected their research; for a detailed description of each way students’ research was affected and for example quotes, see Table 2 . Students described that their depression negatively affected their productivity in the lab. Commonly, students described that their productivity was directly affected by a lack of motivation or because they felt less creative, which hindered the research process. Additionally, students highlighted that they were sometimes less productive because their depression sometimes caused them to struggle to engage intellectually with their research or caused them to have difficulty remembering or concentrating; students described that they could do mundane or routine tasks when they felt depressed, but that they had difficulty with more complex and intellectually demanding tasks. However, students sometimes described that even mundane tasks could be difficult when they were required to remember specific steps; for example, some students struggled recalling a protocol from memory when their depression was particularly severe. Additionally, students noted that their depression made them more self-conscious, which sometimes held them back from sharing research ideas with their mentors or from taking risks such as applying to competitive programs. In addition to being self-conscious, students highlighted that their depression caused them to be overly self-critical, and some described experiencing imposter phenomenon ( Clance and Imes, 1978 ) or feeling like they were not talented enough to be in research and were accepted into a lab by a fluke or through luck. Finally, students described that depression often made them feel less social, and they struggled to socially engage with other members of the lab when they were feeling down.
The Effect of Undergraduate Research Experiences on Student Depression
We also wanted to explore how research impacted students’ feelings of depression. Undergraduates described how research both positively and negatively affected their depression. In the following sections, we present aspects of undergraduate research and examine how each positively and/or negatively affected students’ depression using embedded student quotes to highlight the relationships between related ideas.
Lab Environment: Relationships with Others in the Lab.
Some aspects of the lab environment, which we define as students’ physical, social, or psychological research space, could be particularly beneficial for students with depression.
Specifically, undergraduate researchers perceived that comfortable and positive social interactions with others in the lab helped their depression. Students acknowledged how beneficial their relationships with graduate students and postdocs could be.
Marta: “I think always checking in on undergrads is important. It’s really easy [for us] to go a whole day without talking to anybody in the lab. But our grad students are like ‘Hey, what’s up? How’s school? What’s going on?’ (…) What helps me the most is having that strong support system. Sometimes just talking makes you feel better, but also having people that believe in you can really help you get out of that negative spiral. I think that can really help with depression.”
Kelley: “I know that anytime I need to talk to [my postdoc mentors] about something they’re always there for me. Over time we’ve developed a relationship where I know that outside of work and outside of the lab if I did want to talk to them about something I could talk to them. Even just talking to someone about hobbies and having that relationship alone is really helpful [for depression].”
In addition to highlighting the importance of developing relationships with graduate students or postdocs in the lab, students described that forming relationships with other undergraduates in the lab also helped their depression. Particularly, students described that other undergraduate researchers often validated their feelings about research, which in turn helped them realize that what they are thinking or feeling is normal, which tended to alleviate their negative thoughts. Interestingly, other undergraduates experiencing the same issues could sometimes help buffer them from perceiving that a mentor did not like them or that they were uniquely bad at research. In this article, we use the term “mentor” to refer to anyone who students referred to in the interviews as being their mentors or managing their research experiences; this includes graduate students, postdoctoral scholars, lab managers, and primary investigators (PIs).
Abby: “One of my best friends is in the lab with me. A lot of that friendship just comes from complaining about our stress with the lab and our annoyance with people in the lab. Like when we both agree like, ‘Yeah, the grad students were really off today, it wasn’t us,’ that helps. ‘It wasn’t me, it wasn’t my fault that we were having a rough day in lab; it was the grad students.’ Just being able to realize, ‘Hey, this isn’t all caused by us,’ you know? (…) We understand the stresses in the lab. We understand the details of what each other are doing in the lab, so when something doesn’t work out, we understand that it took them like eight hours to do that and it didn’t work. We provide empathy on a different level.”
Meleana: “It’s great to have solidarity in being confused about something, and it’s just that is a form of validation for me too. When we leave a lab meeting and I look at [another undergrad] I’m like, ‘Did you understand anything that they were just saying?’ And they’re like, ‘Oh, no.’ (…) It’s just really validating to hear from the other undergrads that we all seem to be struggling with the same things.”
Developing positive relationships with faculty mentors or PIs also helped alleviate some students’ depressive feelings, particularly when PIs shared their own struggles with students. This also seemed to normalize students’ concerns about their own experiences.
Alexandra: “[Talking with my PI] is helpful because he would talk about his struggles, and what he faced. A lot of it was very similar to my struggles. For example, he would say, ‘Oh, yeah, I failed this exam that I studied so hard for. I failed the GRE and I paid so much money to prepare for it.’ It just makes [my depression] better, like okay, this is normal for students to go through this. It’s not an out of this world thing where if you fail, you’re a failure and you can’t move on from it.”
Students’ relationships with others in the lab did not always positively impact their depression. Students described instances when the negative moods of the graduate students and PIs would often set the tone of the lab, which in turn worsened the mood of the undergraduate researchers.
Abby: “Sometimes [the grad students] are not in a good mood. The entire vibe of the lab is just off, and if you make a joke and it hits somebody wrong, they get all mad. It really depends on the grad students and the leadership and the mood that they’re in.”
Interviewer: “How does it affect your depression when the grad students are in a bad mood?”
Abby: “It definitely makes me feel worse. It feels like, again, that I really shouldn’t go ask them for help because they’re just not in the mood to help out. It makes me have more pressure on myself, and I have deadlines I need to meet, but I have a question for them, but they’re in a bad mood so I can’t ask. That’s another day wasted for me and it just puts more stress, which just adds to the depression.”
Additionally, some students described even more concerning behavior from research mentors, which negatively affected their depression.
Julie: “I had a primary investigator who is notorious in the department for screaming at people, being emotionally abusive, unreasonable, et cetera. (…) [He was] kind of harassing people, demeaning them, lying to them, et cetera, et cetera. (…) Being yelled at and constantly demeaned and harassed at all hours of the day and night, that was probably pretty bad for me.”
While the relationships between undergraduates and graduate, postdoc, and faculty mentors seemed to either alleviate or worsen students’ depressive symptoms, depending on the quality of the relationship, students in this study exclusively described their relationships with other undergraduates as positive for their depression. However, students did note that undergraduate research puts some of the best and brightest undergraduates in the same environment, which can result in students comparing themselves with their peers. Students described that this comparison would often lead them to feel badly about themselves, even though they would describe their personal relationship with a person to be good.
Meleana: “In just the research field in general, just feeling like I don’t really measure up to the people around me [can affect my depression]. A lot of the times it’s the beginning of a little spiral, mental spiral. There are some past undergrads that are talked about as they’re on this pedestal of being the ideal undergrads and that they were just so smart and contributed so much to the lab. I can never stop myself from wondering like, ‘Oh, I wonder if I’m having a contribution to the lab that’s similar or if I’m just another one of the undergrads that does the bare minimum and passes through and is just there.’”
Natasha: “But, on the other hand, [having another undergrad in the lab] also reminded me constantly that some people are invested in this and meant to do this and it’s not me. And that some people know a lot more than I do and will go further in this than I will.”
While students primarily expressed that their relationships with others in the lab affected their depression, some students explained that they struggled most with depression when the lab was empty; they described that they did not like being alone in the lab, because a lack of stimulation allowed their minds to be filled with negative thoughts.
Mia: “Those late nights definitely didn’t help [my depression]. I am alone, in the entire building. I’m left alone to think about my thoughts more, so not distracted by talking to people or interacting with people. I think more about how I’m feeling and the lack of progress I’m making, and the hopelessness I’m feeling. That kind of dragged things on, and I guess deepened my depression.”
Freddy: “Often times when I go to my office in the evening, that is when I would [ sic ] be prone to be more depressed. It’s being alone. I think about myself or mistakes or trying to correct mistakes or whatever’s going on in my life at the time. I become very introspective. I think I’m way too self-evaluating, way too self-deprecating and it’s when I’m alone when those things are really, really triggered. When I’m talking with somebody else, I forget about those things.”
In sum, students with depression highlighted that a lab environment full of positive and encouraging individuals was helpful for their depression, whereas isolating or competitive environments and negative interactions with others often resulted in more depressive feelings.
Doing Science: Experiencing Failure in Research, Getting Help, Receiving Feedback, Time Demands, and Important Contributions.
In addition to the lab environment, students also described that the process of doing science could affect their depression. Specifically, students explained that a large contributor to their depression was experiencing failure in research.
Interviewer: “Considering your experience in undergraduate research, what tends to trigger your feelings of depression?”
Heather: “Probably just not getting things right. Having to do an experiment over and over again. You don’t get the results you want. (…) The work is pretty meticulous and it’s frustrating when I do all this work, I do a whole experiment, and then I don’t get any results that I can use. That can be really frustrating. It adds to the stress. (…) It’s hard because you did all this other stuff before so you can plan for the research, and then something happens and all the stuff you did was worthless basically.”
Julie: “I felt very negatively about myself [when a project failed] and pretty panicked whenever something didn’t work because I felt like it was a direct reflection on my effort and/or intelligence, and then it was a big glaring personal failure.”
Students explained that their depression related to failing in research was exacerbated if they felt as though they could not seek help from their research mentors. Perceived insufficient mentor guidance has been shown to be a factor influencing student intention to leave undergraduate research ( Cooper et al. , 2019c ). Sometimes students talked about their research mentors being unavailable or unapproachable.
Michelle: “It just feels like [the graduate students] are not approachable. I feel like I can’t approach them to ask for their understanding in a certain situation. It makes [my depression] worse because I feel like I’m stuck, and that I’m being limited, and like there’s nothing I can do. So then I kind of feel like it’s my fault that I can’t do anything.”
Other times, students described that they did not seek help in fear that they would be negatively evaluated in research, which is a fear of being judged by others ( Watson and Friend, 1969 ; Weeks et al. , 2005 ; Cooper et al. , 2018 ). That is, students fear that their mentor would think negatively about them or judge them if they were to ask questions that their mentor thought they should know the answer to.
Meleana: “I would say [my depression] tends to come out more in being more reserved in asking questions because I think that comes more like a fear-based thing where I’m like, ‘Oh, I don’t feel like I’m good enough and so I don’t want to ask these questions because then my mentors will, I don’t know, think that I’m dumb or something.’”
Conversely, students described that mentors who were willing to help them alleviated their depressive feelings.
Crystal: “Yeah [my grad student] is always like, ‘Hey, I can check in on things in the lab because you’re allowed to ask me for that, you’re not totally alone in this,’ because he knows that I tend to take on all this responsibility and I don’t always know how to ask for help. He’s like, ‘You know, this is my lab too and I am here to help you as well,’ and just reminds me that I’m not shouldering this burden by myself.”
Ashlyn: “The graduate student who I work with is very kind and has a lot of patience and he really understands a lot of things and provides simple explanations. He does remind me about things and he will keep on me about certain tasks that I need to do in an understanding way, and it’s just because he’s patient and he listens.”
In addition to experiencing failure in science, students described that making mistakes when doing science also negatively affected their depression.
Abby: “I guess not making mistakes on experiments [is important in avoiding my depression]. Not necessarily that your experiment didn’t turn out to produce the data that you wanted, but just adding the wrong enzyme or messing something up like that. It’s like, ‘Oh, man,’ you know? You can get really down on yourself about that because it can be embarrassing.”
Commonly, students described that the potential for making mistakes increased their stress and anxiety regarding research; however, they explained that how other people responded to a potential mistake was what ultimately affected their depression.
Briana: “Sometimes if I made a mistake in correctly identifying an eye color [of a fly], [my PI] would just ridicule me in front of the other students. He corrected me but his method of correcting was very discouraging because it was a ridicule. It made the others laugh and I didn’t like that.”
Julie: “[My PI] explicitly [asked] if I had the dedication for science. A lot of times he said I had terrible judgment. A lot of times he said I couldn’t be trusted. Once I went to a conference with him, and, unfortunately, in front of another professor, he called me a klutz several times and there was another comment about how I never learn from my mistakes.”
When students did do things correctly, they described how important it could be for them to receive praise from their mentors. They explained that hearing praise and validation can be particularly helpful for students with depression, because their thoughts are often very negative and/or because they have low self-esteem.
Crystal: “[Something that helps my depression is] I have text messages from [my graduate student mentor] thanking me [and another undergraduate researcher] for all of the work that we’ve put in, that he would not be able to be as on track to finish as he is if he didn’t have our help.”
Interviewer: “Why is hearing praise from your mentor helpful?”
Crystal: “Because a lot of my depression focuses on everybody secretly hates you, nobody likes you, you’re going to die alone. So having that validation [from my graduate mentor] is important, because it flies in the face of what my depression tells me.”
Brian: “It reminds you that you exist outside of this negative world that you’ve created for yourself, and people don’t see you how you see yourself sometimes.”
Students also highlighted how research could be overwhelming, which negatively affected their depression. Particularly, students described that research demanded a lot of their time and that their mentors did not always seem to be aware that they were juggling school and other commitments in addition to their research. This stress exacerbated their depression.
Rose: “I feel like sometimes [my grad mentors] are not very understanding because grad students don’t take as many classes as [undergrads] do. I think sometimes they don’t understand when I say I can’t come in at all this week because I have finals and they’re like, ‘Why though?’”
Abby: “I just think being more understanding of student life would be great. We have classes as well as the lab, and classes are the priority. They forget what it’s like to be a student. You feel like they don’t understand and they could never understand when you say like, ‘I have three exams this week,’ and they’re like, ‘I don’t care. You need to finish this.’”
Conversely, some students reported that their research labs were very understanding of students’ schedules. Interestingly, these students talked most about how helpful it was to be able to take a mental health day and not do research on days when they felt down or depressed.
Marta: “My lab tech is very open, so she’ll tell us, ‘I can’t come in today. I have to take a mental health day.’ So she’s a really big advocate for that. And I think I won’t personally tell her that I’m taking a mental health day, but I’ll say, ‘I can’t come in today, but I’ll come in Friday and do those extra hours.’ And she’s like, ‘OK great, I’ll see you then.’ And it makes me feel good, because it helps me take care of myself first and then I can take care of everything else I need to do, which is amazing.”
Meleana: “Knowing that [my mentors] would be flexible if I told them that I’m crazy busy and can’t come into work nearly as much this week [helps my depression]. There is flexibility in allowing me to then care for myself.”
Interviewer: “Why is the flexibility helpful given the depression?”
Meleana: “Because sometimes for me things just take a little bit longer when I’m feeling down. I’m just less efficient to be honest, and so it’s helpful if I feel like I can only go into work for 10 hours in a week. It declutters my brain a little bit to not have to worry about all the things I have to do in work in addition the things that I need to do for school or clubs, or family or whatever.”
Despite the demanding nature of research, a subset of students highlighted that their research and research lab provided a sense of stability or familiarity that distracted them from their depression.
Freddy: “I’ll [do research] to run away from those [depressive] feelings or whatever. (…) I find sadly, I hate to admit it, but I do kind of run to [my lab]. I throw myself into work to distract myself from the feelings of depression and sadness.”
Rose: “When you’re sad or when you’re stressed you want to go to things you’re familiar with. So because lab has always been in my life, it’s this thing where it’s going to be there for me I guess. It’s like a good book that you always go back to and it’s familiar and it makes you feel good. So that’s how lab is. It’s not like the greatest thing in the world but it’s something that I’m used to, which is what I feel like a lot of people need when they’re sad and life is not going well.”
Many students also explained that research positively affects their depression because they perceive their research contribution to be important.
Ashlyn: “I feel like I’m dedicating myself to something that’s worthy and something that I believe in. It’s really important because it contextualizes those times when I am feeling depressed. It’s like, no, I do have these better things that I’m working on. Even when I don’t like myself and I don’t like who I am, which is again, depression brain, I can at least say, ‘Well, I have all these other people relying on me in research and in this area and that’s super important.’”
Jessica: “I mean, it just felt like the work that I was doing had meaning and when I feel like what I’m doing is actually going to contribute to the world, that usually really helps with [depression] because it’s like not every day you can feel like you’re doing something impactful.”
In sum, students highlighted that experiencing failure in research and making mistakes negatively contributed to depression, especially when help was unavailable or research mentors had a negative reaction. Additionally, students acknowledged that the research could be time-consuming, but that research mentors who were flexible helped assuage depressive feelings that were associated with feeling overwhelmed. Finally, research helped some students’ depression, because it felt familiar, provided a distraction from depression, and reminded students that they were contributing to a greater cause.
We believe that creating more inclusive research environments for students with depression is an important step toward broadening participation in science, not only to ensure that we are not discouraging students with depression from persisting in science, but also because depression has been shown to disproportionately affect underserved and underrepresented groups in science ( Turner and Noh, 1988 ; Eisenberg et al. , 2007 ; Jenkins et al. , 2013 ; American College Health Association, 2018 ). We initially hypothesized that three features of undergraduate research—research mentors, the lab environment, and failure—may have the potential to exacerbate student depression. We found this to be true; students highlighted that their relationships with their mentors as well as the overall lab environment could negatively affect their depression, but could also positively affect their research experiences. Students also noted that they struggled with failure, which is likely true of most students, but is known to be particularly difficult for students with depression ( Elliott et al. , 1997 ). We expand upon our findings by integrating literature on depression with the information that students provided in the interviews about how research mentors can best support students. We provide a set of evidence-based recommendations focused on mentoring, the lab environment, and failure for research mentors wanting to create more inclusive research environments for students with depression. Notably, only the first recommendation is specific to students with depression; the others reflect recommendations that have previously been described as “best practices” for research mentors ( NASEM, 2017 , 2019 ; Sorkness et al. , 2017 ) and likely would benefit most students. However, we examine how these recommendations may be particularly important for students with depression. As we hypothesized, these recommendations directly address three aspects of research: mentors, lab environment, and failure. A caveat of these recommendations is that more research needs to be done to explore the experiences of students with depression and how these practices actually impact students with depression, but our national sample of undergraduate researchers with depression can provide an initial starting point for a discussion about how to improve research experiences for these students.
Recommendations to Make Undergraduate Research Experiences More Inclusive for Students with Depression
Recognize student depression as a valid illness..
Allow students with depression to take time off of research by simply saying that they are sick and provide appropriate time for students to recover from depressive episodes. Also, make an effort to destigmatize mental health issues.
Undergraduate researchers described both psychological and physical symptoms that manifested as a result of their depression and highlighted how such symptoms prevented them from performing to their full potential in undergraduate research. For example, students described how their depression would cause them to feel unmotivated, which would often negatively affect their research productivity. In cases in which students were motivated enough to come in and do their research, they described having difficulty concentrating or engaging in the work. Further, when doing research, students felt less creative and less willing to take risks, which may alter the quality of their work. Students also sometimes struggled to socialize in the lab. They described feeling less social and feeling overly self-critical. In sum, students described that, when they experienced a depressive episode, they were not able to perform to the best of their ability, and it sometimes took a toll on them to try to act like nothing was wrong, when they were internally struggling with depression. We recommend that research mentors treat depression like any other physical illness; allowing students the chance to recover when they are experiencing a depressive episode can be extremely important to students and can allow them to maximize their productivity upon returning to research ( Judd et al. , 2000 ). Students explained that if they are not able to take the time to focus on recovering during a depressive episode, then they typically continue to struggle with depression, which negatively affects their research. This sentiment is echoed by researchers in psychiatry who have found that patients who do not fully recover from a depressive episode are more likely to relapse and to experience chronic depression ( Judd et al. , 2000 ). Students described not doing tasks or not showing up to research because of their depression but struggling with how to share that information with their research mentors. Often, students would not say anything, which caused them anxiety because they were worried about what others in the lab would say to them when they returned. Admittedly, many students understood why this behavior would cause their research mentors to be angry or frustrated, but they weighed the consequences of their research mentors’ displeasure against the consequences of revealing their depression and decided it was not worth admitting to being depressed. This aligns with literature that suggests that when individuals have concealable stigmatized identities, or identities that can be hidden and that carry negative stereotypes, such as depression, they will often keep them concealed to avoid negative judgment or criticism ( Link and Phelan, 2001 ; Quinn and Earnshaw, 2011 ; Jones and King, 2014 ; Cooper and Brownell, 2016 ; Cooper et al. , 2019b ; Cooper et al ., unpublished data ). Therefore, it is important for research mentors to be explicit with students that 1) they recognize mental illness as a valid sickness and 2) that students with mental illness can simply explain that they are sick if they need to take time off. This may be useful to overtly state on a research website or in a research syllabus, contract, or agreement if mentors use such documents when mentoring undergraduates in their lab. Further, research mentors can purposefully work to destigmatize mental health issues by explicitly stating that struggling with mental health issues, such as depression and anxiety, is common. While we do not recommend that mentors ask students directly about depression, because this can force students to share when they are not comfortable sharing, we do recommend providing opportunities for students to reveal their depression ( Chaudoir and Fisher, 2010 ). Mentors can regularly check in with students about how they’re doing, and talk openly about the importance of mental health, which may increase the chance that students may feel comfortable revealing their depression ( Chaudoir and Quinn, 2010 ; Cooper et al ., unpublished data ).
Foster a Positive Lab Environment.
Encourage positivity in the research lab, promote working in shared spaces to enhance social support among lab members, and alleviate competition among undergraduates.
Students in this study highlighted that the “leadership” of the lab, meaning graduate students, postdocs, lab managers, and PIs, were often responsible for establishing the tone of the lab; that is, if they were in a bad mood it would trickle down and negatively affect the moods of the undergraduates. Explicitly reminding lab leadership that their moods can both positively and negatively affect undergraduates may be important in establishing a positive lab environment. Further, students highlighted how they were most likely to experience negative thoughts when they were alone in the lab. Therefore, it may be helpful to encourage all lab members to work in a shared space to enhance social interactions among students and to maximize the likelihood that undergraduates have access to help when needed. A review of 51 studies in psychiatry supported our undergraduate researchers’ perceptions that social relationships positively impacted their depression; the study found that perceived emotional support (e.g., someone available to listen or give advice), perceived instrumental support (e.g., someone available to help with tasks), and large diverse social networks (e.g., being socially connected to a large number of people) were significantly protective against depression ( Santini et al. , 2015 ). Additionally, despite forming positive relationships with other undergraduates in the lab, many undergraduate researchers admitted to constantly comparing themselves with other undergraduates, which led them to feel inferior, negatively affecting their depression. Some students talked about mentors favoring current undergraduates or talking positively about past undergraduates, which further exacerbated their feelings of inferiority. A recent study of students in undergraduate research experiences highlighted that inequitable distribution of praise to undergraduates can create negative perceptions of lab environments for students (Cooper et al. , 2019). Further, the psychology literature has demonstrated that when people feel insecure in their social environments, it can cause them to focus on a hierarchical view of themselves and others, which can foster feelings of inferiority and increase their vulnerability to depression ( Gilbert et al. , 2009 ). Thus, we recommend that mentors be conscious of their behaviors so that they do not unintentionally promote competition among undergraduates or express favoritism toward current or past undergraduates. Praise is likely best used without comparison with others and not done in a public way, although more research on the impact of praise on undergraduate researchers needs to be done. While significant research has been done on mentoring and mentoring relationships in the context of undergraduate research ( Byars-Winston et al. , 2015 ; Aikens et al. , 2017 ; Estrada et al. , 2018 ; Limeri et al. , 2019 ; NASEM, 2019 ), much less has been done on the influence of the lab environment broadly and how people in nonmentoring roles can influence one another. Yet, this study indicates the potential influence of many different members of the lab, not only their mentors, on students with depression.
Develop More Personal Relationships with Undergraduate Researchers and Provide Sufficient Guidance.
Make an effort to establish more personal relationships with undergraduates and ensure that they perceive that they have access to sufficient help and guidance with regard to their research.
When we asked students explicitly how research mentors could help create more inclusive environments for undergraduate researchers with depression, students overwhelmingly said that building mentor–student relationships would be extremely helpful. Students suggested that mentors could get to know students on a more personal level by asking about their career interests or interests outside of academia. Students also remarked that establishing a more personal relationship could help build the trust needed in order for undergraduates to confide in their research mentors about their depression, which they perceived would strengthen their relationships further because they could be honest about when they were not feeling well or their mentors might even “check in” with them in times where they were acting differently than normal. This aligns with studies showing that undergraduates are most likely to reveal a stigmatized identity, such as depression, when they form a close relationship with someone ( Chaudoir and Quinn, 2010 ). Many were intimidated to ask for research-related help from their mentors and expressed that they wished they had established a better relationship so that they would feel more comfortable. Therefore, we recommend that research mentors try to establish relationships with their undergraduates and explicitly invite them to ask questions or seek help when needed. These recommendations are supported by national recommendations for mentoring ( NASEM, 2019 ) and by literature that demonstrates that both social support (listening and talking with students) and instrumental support (providing students with help) have been shown to be protective against depression ( Santini et al. , 2015 ).
Treat Undergraduates with Respect and Remember to Praise Them.
Avoid providing harsh criticism and remember to praise undergraduates. Students with depression often have low self-esteem and are especially self-critical. Therefore, praise can help calibrate their overly negative self-perceptions.
Students in this study described that receiving criticism from others, especially harsh criticism, was particularly difficult for them given their depression. Multiple studies have demonstrated that people with depression can have an abnormal or maladaptive response to negative feedback; scientists hypothesize that perceived failure on a particular task can trigger failure-related thoughts that interfere with subsequent performance ( Eshel and Roiser, 2010 ). Thus, it is important for research mentors to remember to make sure to avoid unnecessarily harsh criticisms that make students feel like they have failed (more about failure is described in the next recommendation). Further, students with depression often have low self-esteem or low “personal judgment of the worthiness that is expressed in the attitudes the individual holds towards oneself” ( Heatherton et al. , 2003 , p. 220; Sowislo and Orth, 2013 ). Specifically, a meta-analysis of longitudinal studies found that low self-esteem is predictive of depression ( Sowislo and Orth, 2013 ), and depression has also been shown to be highly related to self-criticism ( Luyten et al. , 2007 ). Indeed, nearly all of the students in our study described thinking that they are “not good enough,” “worthless,” or “inadequate,” which is consistent with literature showing that people with depression are self-critical ( Blatt et al. , 1982 ; Gilbert et al. , 2006 ) and can be less optimistic of their performance on future tasks and rate their overall performance on tasks less favorably than their peers without depression ( Cane and Gotlib, 1985 ). When we asked students what aspects of undergraduate research helped their depression, students described that praise from their mentors was especially impactful, because they thought so poorly of themselves and they needed to hear something positive from someone else in order to believe it could be true. Praise has been highlighted as an important aspect of mentoring in research for many years ( Ashford, 1996 ; Gelso and Lent, 2000 ; Brown et al. , 2009 ) and may be particularly important for students with depression. In fact, praise has been shown to enhance individuals’ motivation and subsequent productivity ( Hancock, 2002 ; Henderlong and Lepper, 2002 ), factors highlighted by students as negatively affecting their depression. However, something to keep in mind is that a student with depression and a student without depression may process praise differently. For a student with depression, a small comment that praises the student’s work may not be sufficient for the student to process that comment as praise. People with depression are hyposensitive to reward or have reward-processing deficits ( Eshel and Roiser, 2010 ); therefore, praise may affect students without depression more positively than it would affect students with depression. Research mentors should be mindful that students with depression often have a negative view of themselves, and while students report that praise is extremely important, they may have trouble processing such positive feedback.
Normalize Failure and Be Explicit about the Importance of Research Contributions.
Explicitly remind students that experiencing failure is expected in research. Also explain to students how their individual work relates to the overall project so that they can understand how their contributions are important. It can also be helpful to explain to students why the research project as a whole is important in the context of the greater scientific community.
Experiencing failure has been thought to be a potentially important aspect of undergraduate research, because it may provide students with the potential to develop integral scientific skills such as the ability to navigate challenges and persevere ( Laursen et al. , 2010 ; Gin et al. , 2018 ; Henry et al. , 2019 ). However, in the interviews, students described that when their science experiments failed, it was particularly tough for their depression. Students’ negative reaction to experiencing failure in research is unsurprising, given recent literature that has predicted that students may be inadequately prepared to approach failure in science ( Henry et al. , 2019 ). However, the literature suggests that students with depression may find experiencing failure in research to be especially difficult ( Elliott et al. , 1997 ; Mongrain and Blackburn, 2005 ; Jones et al. , 2009 ). One potential hypothesis is that students with depression may be more likely to have fixed mindsets or more likely to believe that their intelligence and capacity for specific abilities are unchangeable traits ( Schleider and Weisz, 2018 ); students with a fixed mindset have been hypothesized to have particularly negative responses to experiencing failure in research, because they are prone to quitting easily in the face of challenges and becoming defensive when criticized ( Forsythe and Johnson, 2017 ; Dweck, 2008 ). A study of life sciences undergraduates enrolled in CUREs identified three strategies of students who adopted adaptive coping mechanisms, or mechanisms that help an individual maintain well-being and/or move beyond the stressor when faced with failure in undergraduate research: 1) problem solving or engaging in strategic planning and decision making, 2) support seeking or finding comfort and help with research, and 3) cognitive restructuring or reframing a problem from negative to positive and engaging in self encouragement ( Gin et al. , 2018 ). We recommend that, when undergraduates experience failure in science, their mentors be proactive in helping them problem solve, providing help and support, and encouraging them. Students also explained that mentors sharing their own struggles as undergraduate and graduate students was helpful, because it normalized failure. Sharing personal failures in research has been recommended as an important way to provide students with psychosocial support during research ( NASEM, 2019 ). We also suggest that research mentors take time to explain to students why their tasks in the lab, no matter how small, contribute to the greater research project ( Cooper et al. , 2019a ). Additionally, it is important to make sure that students can explain how the research project as a whole is contributing to the scientific community ( Gin et al. , 2018 ). Students highlighted that contributing to something important was really helpful for their depression, which is unsurprising, given that studies have shown that meaning in life or people’s comprehension of their life experiences along with a sense of overarching purpose one is working toward has been shown to be inversely related to depression ( Steger, 2013 ).
Limitations and Future Directions
This work was a qualitative interview study intended to document a previously unstudied phenomenon: depression in the context of undergraduate research experiences. We chose to conduct semistructured interviews rather than a survey because of the need for initial exploration of this area, given the paucity of prior research. A strength of this study is the sampling approach. We recruited a national sample of 35 undergraduates engaged in undergraduate research at 12 different public R1 institutions. Despite our representative sample from R1 institutions, these findings may not be generalizable to students at other types of institutions; lab environments, mentoring structures, and interactions between faculty and undergraduate researchers may be different at other institution types (e.g., private R1 institutions, R2 institutions, master’s-granting institutions, primarily undergraduate institutions, and community colleges), so we caution against making generalizations about this work to all undergraduate research experiences. Future work could assess whether students with depression at other types of institutions have similar experiences to students at research-intensive institutions. Additionally, we intentionally did not explore the experiences of students with specific identities owing to our sample size and the small number of students in any particular group (e.g., students of a particular race, students with a graduate mentor as the primary mentor). We intend to conduct future quantitative studies to further explore how students’ identities and aspects of their research affect their experiences with depression in undergraduate research.
The students who participated in the study volunteered to be interviewed about their depression; therefore, it is possible that depression is a more salient part of these students’ identities and/or that they are more comfortable talking about their depression than the average population of students with depression. It is also important to acknowledge the personal nature of the topic and that some students may not have fully shared their experiences ( Krumpal, 2013 ), particularly those experiences that may be emotional or traumatizing ( Kahn and Garrison, 2009 ). Additionally, our sample was skewed toward females (77%). While females do make up approximately 60% of students in biology programs on average ( Eddy et al. , 2014 ), they are also more likely to report experiencing depression ( American College Health Association, 2018 ; Evans et al. , 2018 ). However, this could be because women have higher rates of depression or because males are less likely to report having depression; clinical bias, or practitioners’ subconscious tendencies to overlook male distress, may underestimate depression rates in men ( Smith et al. , 2018 ). Further, females are also more likely to volunteer to participate in studies ( Porter and Whitcomb, 2005 ); therefore, many interview studies have disproportionately more females in the data set (e.g., Cooper et al. , 2017 ). If we had been able to interview more male students, we might have identified different findings. Additionally, we limited our sample to life sciences students engaged in undergraduate research at public R1 institutions. It is possible that students in other majors may have different challenges and opportunities for students with depression, as well as different disciplinary stigmas associated with mental health.
In this exploratory interview study, we identified a variety of ways in which depression in undergraduates negatively affected their undergraduate research experiences. Specifically, we found that depression interfered with students’ motivation and productivity, creativity and risk-taking, engagement and concentration, and self-perception and socializing. We also identified that research can negatively affect depression in undergraduates. Experiencing failure in research can exacerbate student depression, especially when students do not have access to adequate guidance. Additionally, being alone or having negative interactions with others in the lab worsened students’ depression. However, we also found that undergraduate research can positively affect students’ depression. Research can provide a familiar space where students can feel as though they are contributing to something meaningful. Additionally, students reported that having access to adequate guidance and a social support network within the research lab also positively affected their depression. We hope that this work can spark conversations about how to make undergraduate research experiences more inclusive of students with depression and that it can stimulate additional research that more broadly explores the experiences of undergraduate researchers with depression.
Important note
If you or a student experience symptoms of depression and want help, there are resources available to you. Many campuses provide counseling centers equipped to provide students, staff, and faculty with treatment for depression, as well as university-dedicated crisis hotlines. Additionally, there are free 24/7 services such as Crisis Text Line, which allows you to text a trained live crisis counselor (Text “CONNECT” to 741741; Text Depression Hotline , 2019 ), and phone hotlines such as the National Suicide Prevention Lifeline at 1-800-273-8255 (TALK). You can also learn more about depression and where to find help near you through the Anxiety and Depression Association of American website: https://adaa.org ( Anxiety and Depression Association of America, 2019 ) and the Depression and Biopolar Support Alliance: http://dbsalliance.org ( Depression and Biopolar Support Alliance, 2019 ).
ACKNOWLEDGMENTS
We are extremely grateful to the undergraduate researchers who shared their thoughts and experiences about depression with us. We acknowledge the ASU LEAP Scholars for helping us create the original survey and Rachel Scott for her helpful feedback on earlier drafts of this article. L.E.G. was supported by a National Science Foundation (NSF) Graduate Fellowship (DGE-1311230) and K.M.C. was partially supported by a Howard Hughes Medical Institute (HHMI) Inclusive Excellence grant (no. 11046) and an NSF grant (no. 1644236). Any opinions, findings, conclusions, or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the NSF or HHMI.
- Aikens, M. L., Robertson, M. M., Sadselia, S., Watkins, K., Evans, M., Runyon, C. R. , … & Dolan, E. L. ( 2017 ). Race and gender differences in undergraduate research mentoring structures and research outcomes . CBE—Life Sciences Education , 16 (2), ar34. Link , Google Scholar
- Aikens, M. L., Sadselia, S., Watkins, K., Evans, M., Eby, L. T., & Dolan, E. L. ( 2016 ). A social capital perspective on the mentoring of undergraduate life science researchers: An empirical study of undergraduate–postgraduate–faculty triads . CBE—Life Sciences Education , 15 (2), ar16. Link , Google Scholar
- Aldwin, C., & Greenberger, E. ( 1987 ). Cultural differences in the predictors of depression . American Journal of Community Psychology , 15 (6), 789–813. Medline , Google Scholar
- American Association for the Advancement of Science . ( 2011 ). Vision and change in undergraduate biology education: A call to action . Retrieved November 29, 2019, from http://visionandchange.org/files/2013/11/aaas-VISchange-web1113.pdf Google Scholar
- American College Health Association . ( 2018 ). Undergraduate reference group executive summary, Fall 2018 . Retrieved November 29, 2019, from www.acha.org/documents/ncha/NCHA-II_Fall_2018_Reference_Group_Executive_Summary.pdf Google Scholar
- American College Health Association . ( 2019 ). Retrieved November 29, 2019, from NCHA-II_SPRING_2019_UNDERGRADUATE_REFERENCE_GROUP_DATA_REPORT.pdf www.acha.org/documents/ncha/NCHA-II_SPRING_2019_UNDERGRADUATE_REFERENCE_GROUP_DATA_REPORT.pdf Google Scholar
- American Psychiatric Association . ( 2013 ). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Publishing. Google Scholar
- Aneshensel, C. S., & Stone, J. D. ( 1982 ). Stress and depression: A test of the buffering model of social support . Archives of General Psychiatry , 39 (12), 1392–1396. Medline , Google Scholar
- Anxiety and Depression Association of America . ( 2019 ). Home page . Retrieved November 29, 2019, from https://adaa.org Google Scholar
- Armbruster, P., Patel, M., Johnson, E., & Weiss, M. ( 2009 ). Active learning and student-centered pedagogy improve student attitudes and performance in introductory biology . CBE—Life Sciences Education , 8 (3), 203–213. Link , Google Scholar
- Ashford, S. J. ( 1996 ). Working with doctoral students: Rhythms of Academic Life: Personal Accounts of Careers in Academia . In Front, P. J.Taylor, M. S. (Eds.), Rhythms of Academic Life: Personal Accounts of Careers in Academia (pp. 153–158). Thousand Oaks, CA: Sage. Google Scholar
- Auchincloss, L. C., Laursen, S. L., Branchaw, J. L., Eagan, K., Graham, M., Hanauer, D. I. , … & Rowland, S. ( 2014 ). Assessment of course-based undergraduate research experiences: A meeting report . CBE—Life Sciences Education , 13 (1), 29–40. Link , Google Scholar
- Barak, M. E. M., Levin, A., Nissly, J. A., & Lane, C. J. ( 2006 ). Why do they leave? Modeling child welfare workers’ turnover intentions . Children and Youth Services Review , 28 (5), 548–577. Google Scholar
- Bauer, K. W., & Bennett, J. S. ( 2003 ). Alumni perceptions used to assess undergraduate research experience . Journal of Higher Education , 74 (2), 210–230. Google Scholar
- Birks, M., & Mills, J. ( 2015 ). Grounded theory: A practical guide . Thousand Oaks, CA: Sage. Google Scholar
- Blatt, S. J., Quinlan, D. M., Chevron, E. S., McDonald, C., & Zuroff, D. ( 1982 ). Dependency and self-criticism: Psychological dimensions of depression . Journal of Consulting and Clinical Psychology , 50 (1), 113. Medline , Google Scholar
- Brown, R. T., Daly, B. P., & Leong, F. T. ( 2009 ). Mentoring in research: A developmental approach . Professional Psychology: Research and Practice , 40 (3), 306. Google Scholar
- Brownell, S. E., Hekmat-Scafe, D. S., Singla, V., Seawell, P. C., Imam, J. F. C., Eddy, S. L. , … & Cyert, M. S. ( 2015 ). A high-enrollment course-based undergraduate research experience improves student conceptions of scientific thinking and ability to interpret data . CBE—Life Sciences Education , 14 (2), ar21. Link , Google Scholar
- Brownell, S. E., & Kloser, M. J. ( 2015 ). Toward a conceptual framework for measuring the effectiveness of course-based undergraduate research experiences in undergraduate biology . Studies in Higher Education , 40 (3), 525–544. Google Scholar
- Byars-Winston, A. M., Branchaw, J., Pfund, C., Leverett, P., & Newton, J. ( 2015 ). Culturally diverse undergraduate researchers’ academic outcomes and perceptions of their research mentoring relationships . International Journal of Science Education , 37 (15), 2533–2554. Medline , Google Scholar
- Cane, D. B., & Gotlib, I. H. ( 1985 ). Depression and the effects of positive and negative feedback on expectations, evaluations, and performance . Cognitive Therapy and Research , 9 (2), 145–160. Google Scholar
- Ceci, S. J., & Williams, W. M. ( 2010 ). Sex differences in math-intensive fields . Current Directions in Psychological Science , 19 (5), 275–279. Medline , Google Scholar
- Center for Collegiate Mental Health . ( 2017 ). Center for Collegiate Mental Health 2017 Annual Report . State College, PA: Penn State Universit. Google Scholar
- Charmaz, K. ( 2006 ). Constructing grounded theory: A practical guide through qualitative research . Thousand Oaks, CA: Sage. Google Scholar
- Chaudoir, S. R., & Fisher, J. D. ( 2010 ). The disclosure processes model: Understanding disclosure decision making and postdisclosure outcomes among people living with a concealable stigmatized identity . Psychological Bulletin , 136 (2), 236. Medline , Google Scholar
- Chaudoir, S. R., & Quinn, D. M. ( 2010 ). Revealing concealable stigmatized identities: The impact of disclosure motivations and positive first-disclosure experiences on fear of disclosure and well-being . Journal of Social Issues , 66 (3), 570–584. Medline , Google Scholar
- Clance, P. R., & Imes, S. A. ( 1978 ). The imposter phenomenon in high achieving women: Dynamics and therapeutic intervention . Psychotherapy: Theory, Research & Practice , 15 (3), 241. Google Scholar
- Cooper, K. M., Ashley, M., & Brownell, S. E. ( 2017 ). A bridge to active learning: A summer bridge program helps students maximize their active-learning experiences and the active-learning experiences of others . CBE—Life Sciences Education , 16 (1), ar17. Link , Google Scholar
- Cooper, K. M., Blattman, J. N., Hendrix, T., & Brownell, S. E. ( 2019a ). The impact of broadly relevant novel discoveries on student project ownership in a traditional lab course turned CURE . CBE—Life Sciences Education , 18 (4), ar57. Link , Google Scholar
- Cooper, K. M., & Brownell, S. E. ( 2016 ). Coming out in class: Challenges and benefits of active learning in a biology classroom for LGBTQIA students . CBE—Life Sciences Education , 15 (3), ar37. https://doi.org/10.1187/cbe.16-01-0074 Link , Google Scholar
- Cooper, K. M., Brownell, S. E., & Gormally, C. C. ( 2019b ). Coming out to the class: Identifying factors that influence college biology instructor decisions about whether to reveal their LGBQ identity in class . Journal of Women and Minorities in Science and Engineering , 25 (3). Google Scholar
- Cooper, K. M., Downing, V. R., & Brownell, S. E. ( 2018 ). The influence of active learning practices on student anxiety in large-enrollment college science classrooms . International Journal of STEM Education , 5 (1), 23. Medline , Google Scholar
- Cooper, K. M., Gin, L. E., Akeeh, B., Clark, C. E., Hunter, J. S., Roderick, T. B. , … & Brownell, S. E. ( 2019c ). Factors that predict life sciences student persistence in undergraduate research experiences . PLoS ONE , 14 (8). https://doi.org/10.1371/journal.pone.0220186 Google Scholar
- Cooper, K. M., Gin, L. E., & Brownell, S. E. ( 2019d ). Diagnosing differences in what introductory biology students in a fully online and an in-person biology degree program know and do regarding medical school admission . Advances in Physiology Education , 43 (2), 221–232. Medline , Google Scholar
- Cooper, K. M., Gin, L. E., & Brownell, S. E. ( In press ). Depression as a concealable stigmatized identity: What influences whether students conceal or reveal their depression in undergraduate research experiences? International Journal of STEM Education , ( in press ). Google Scholar
- Depression and Biopolar Support Alliance . ( 2019 ). Home page . Retrieved November 28, 2019, from www.dbsalliance.org Google Scholar
- Deroma, V. M., Leach, J. B., & Leverett, J. P. ( 2009 ). The relationship between depression and college academic performance . College Student Journal , 43 (2), 325–335. Google Scholar
- Dweck, C. S. ( 2008 ). Mindset: The new psychology of success . New York, NY: Random House Digital. Google Scholar
- Dyson, R., & Renk, K. ( 2006 ). Freshmen adaptation to university life: Depressive symptoms, stress, and coping . Journal of Clinical Psychology , 62 (10), 1231–1244. Medline , Google Scholar
- Eddy, S. L., Brownell, S. E., & Wenderoth, M. P. ( 2014 ). Gender gaps in achievement and participation in multiple introductory biology classrooms . CBE—Life Sciences Education , 13 (3), 478–492. https://doi.org/10.1187/cbe.13-10-0204 Link , Google Scholar
- Eisenberg, D., Gollust, S. E., Golberstein, E., & Hefner, J. L. ( 2007 ). Prevalence and correlates of depression, anxiety, and suicidality among university students . American Journal of Orthopsychiatry , 77 (4), 534–542. Medline , Google Scholar
- Elliott, R., Sahakian, B. J., Herrod, J. J., Robbins, T. W., & Paykel, E. S. ( 1997 ). Abnormal response to negative feedback in unipolar depression: Evidence for a diagnosis specific impairment . Journal of Neurology, Neurosurgery & Psychiatry , 63 (1), 74–82. Medline , Google Scholar
- Eshel, N., & Roiser, J. P. ( 2010 ). Reward and punishment processing in depression . Biological Psychiatry , 68 (2), 118–124. Medline , Google Scholar
- Estrada, M., Hernandez, P. R., & Schultz, P. W. ( 2018 ). A longitudinal study of how quality mentorship and research experience integrate underrepresented minorities into STEM careers . CBE—Life Sciences Education , 17 (1), ar9. Link , Google Scholar
- Evans, T. M., Bira, L., Gastelum, J. B., Weiss, L. T., & Vanderford, N. L. ( 2018 ). Evidence for a mental health crisis in graduate education . Nature Biotechnology , 36 (3), 282. Medline , Google Scholar
- Everson, H. T., Tobias, S., Hartman, H., & Gourgey, A. ( 1993 ). Test anxiety and the curriculum: The subject matters . Anxiety, Stress, and Coping , 6 (1), 1–8. Google Scholar
- Flaherty, C. ( 2018 ). New study says graduate students’ mental health is a “crisis.” Retrieved November 29, 2019, from www.insidehighered.com/news/2018/03/06/new-study-says-graduate-students-mental-health-crisis Google Scholar
- Forsythe, A., & Johnson, S. ( 2017 ). Thanks, but no-thanks for the feedback . Assessment & Evaluation in Higher Education , 42 (6), 850–859. Google Scholar
- Garlow, S. J., Rosenberg, J., Moore, J. D., Haas, A. P., Koestner, B., Hendin, H., & Nemeroff, C. B. ( 2008 ). Depression, desperation, and suicidal ideation in college students: Results from the American Foundation for Suicide Prevention College Screening Project at Emory University . Depression and Anxiety , 25 (6), 482–488. Medline , Google Scholar
- Gelso, C. J., & Lent, R. W. ( 2000 ). Scientific training and scholarly productivity: The person, the training environment, and their interaction . In Brown, S. D.Lent, R. W. (Eds.), Handbook of counseling psychology (pp. 109–139). Hoboken, NJ: John Wiley & Sons Inc. Google Scholar
- Gilbert, P., Baldwin, M. W., Irons, C., Baccus, J. R., & Palmer, M. ( 2006 ). Self-criticism and self-warmth: An imagery study exploring their relation to depression . Journal of Cognitive Psychotherapy , 20 (2), 183. Google Scholar
- Gilbert, P., McEwan, K., Bellew, R., Mills, A., & Gale, C. ( 2009 ). The dark side of competition: How competitive behaviour and striving to avoid inferiority are linked to depression, anxiety, stress and self-harm . Psychology and Psychotherapy: Theory, Research and Practice , 82 (2), 123–136. Medline , Google Scholar
- Gin, L. E., Rowland, A. A., Steinwand, B., Bruno, J., & Corwin, L. A. ( 2018 ). Students who fail to achieve predefined research goals may still experience many positive outcomes as a result of CURE participation . CBE—Life Sciences Education , 17 (4), ar57. Link , Google Scholar
- Glesne, C., & Peshkin, A. ( 1992 ). Becoming qualitative researchers: An introduction . London, England, UK: Longman. Google Scholar
- Grav, S., Hellzèn, O., Romild, U., & Stordal, E. ( 2012 ). Association between social support and depression in the general population: The HUNT study, a cross-sectional survey . Journal of Clinical Nursing , 21 (1–2), 111–120. Medline , Google Scholar
- Guest, G., Bunce, A., & Johnson, L. ( 2006 ). How many interviews are enough? An experiment with data saturation and variability . Field Methods , 18 (1), 59–82. Google Scholar
- Hancock, D. R. ( 2002 ). Influencing graduate students’ classroom achievement, homework habits and motivation to learn with verbal praise . Educational Research , 44 (1), 83–95. Google Scholar
- Hannah, D. R., & Lautsch, B. A. ( 2011 ). Counting in qualitative research: Why to conduct it, when to avoid it, and when to closet it . Journal of Management Inquiry , 20 (1), 14–22. Google Scholar
- Heatherton, T. F., & Wyland, C. L. ( 2003 ). Assessing self-esteem . In Lopez, S. J.Snyder, C. R. (Eds.), Positive psychological assessment: A handbook of models and measures (pp. 219–233). Washington, DC: American Psychological Association. https://doi.org/10.1037/10612-014 . Google Scholar
- Henderlong, J., & Lepper, M. R. ( 2002 ). The effects of praise on children’s intrinsic motivation: A review and synthesis . Psychological Bulletin , 128 (5), 774. Medline , Google Scholar
- Henry, M. A., Shorter, S., Charkoudian, L., Heemstra, J. M., & Corwin, L. A. ( 2019 ). FAIL is not a four-letter word: A theoretical framework for exploring undergraduate students’ approaches to academic challenge and responses to failure in STEM learning environments . CBE—Life Sciences Education , 18 (1), ar11. Link , Google Scholar
- Hernandez, P. R., Woodcock, A., Estrada, M., & Schultz, P. W. ( 2018 ). Undergraduate research experiences broaden diversity in the scientific workforce . BioScience , 68 (3), 204–211. Google Scholar
- Hish, A. J., Nagy, G. A., Fang, C. M., Kelley, L., Nicchitta, C. V., Dzirasa, K., & Rosenthal, M. Z. ( 2019 ). Applying the stress process model to stress–burnout and stress–depression relationships in biomedical doctoral students: A cross-sectional pilot study . CBE—Life Sciences Education , 18 (4), ar51. Link , Google Scholar
- Howell, E., & McFeeters, J. ( 2008 ). Children’s mental health care: Differences by race/ethnicity in urban/rural areas . Journal of Health Care for the Poor and Underserved , 19 (1), 237–247. Medline , Google Scholar
- Hysenbegasi, A., Hass, S. L., & Rowland, C. R. ( 2005 ). The impact of depression on the academic productivity of university students . Journal of Mental Health Policy and Economics , 8 (3), 145. Medline , Google Scholar
- Ibrahim, A. K., Kelly, S. J., Adams, C. E., & Glazebrook, C. ( 2013 ). A systematic review of studies of depression prevalence in university students . Journal of Psychiatric Research , 47 (3), 391–400. Medline , Google Scholar
- Intemann, K. ( 2009 ). Why diversity matters: Understanding and applying the diversity component of the National Science Foundation’s broader impacts criterion . Social Epistemology , 23 (3–4), 249–266. Google Scholar
- Ishiyama, J. ( 2002 ). Does early participation in undergraduate research benefit social science and humanities students? College Student Journal , 36 (3), 381–387. Google Scholar
- Jenkins, S. R., Belanger, A., Connally, M. L., Boals, A., & Durón, K. M. ( 2013 ). First-generation undergraduate students’ social support, depression, and life satisfaction . Journal of College Counseling , 16 (2), 129–142. Google Scholar
- Jobst, A., Sabass, L., Palagyi, A., Bauriedl-Schmidt, C., Mauer, M. C., Sarubin, N. , … & Zill, P. ( 2015 ). Effects of social exclusion on emotions and oxytocin and cortisol levels in patients with chronic depression . Journal of Psychiatric Research , 60 , 170–177. Medline , Google Scholar
- Jones, K. P., & King, E. B. ( 2014 ). Managing concealable stigmas at work: A review and multilevel model . Journal of Management , 40 (5), 1466–1494. Google Scholar
- Jones, M. T., Barlow, A. E., & Villarejo, M. ( 2010 ). Importance of undergraduate research for minority persistence and achievement in biology . Journal of Higher Education , 81 (1), 82–115. Google Scholar
- Jones, N. P., Papadakis, A. A., Hogan, C. M., & Strauman, T. J. ( 2009 ). Over and over again: Rumination, reflection, and promotion goal failure and their interactive effects on depressive symptoms . Behaviour Research and Therapy , 47 (3), 254–259. Medline , Google Scholar
- Judd, L. L., Paulus, M. J., Schettler, P. J., Akiskal, H. S., Endicott, J., Leon, A. C. , … & Keller, M. B. ( 2000 ). Does incomplete recovery from first lifetime major depressive episode herald a chronic course of illness? American Journal of Psychiatry , 157 (9), 1501–1504. Medline , Google Scholar
- Kahn, J. H., & Garrison, A. M. ( 2009 ). Emotional self-disclosure and emotional avoidance: Relations with symptoms of depression and anxiety . Journal of Counseling Psychology , 56 (4), 573. Google Scholar
- Kataoka, S. H., Zhang, L., & Wells, K. B. ( 2002 ). Unmet need for mental health care among US children: Variation by ethnicity and insurance status . American Journal of Psychiatry , 159 (9), 1548–1555. Medline , Google Scholar
- Kreger, D. W. ( 1995 ). Self-esteem, stress, and depression among graduate students . Psychological Reports , 76 (1), 345–346. Medline , Google Scholar
- Krumpal, I. ( 2013 ). Determinants of social desirability bias in sensitive surveys: A literature review . Quality & Quantity , 47 (4), 2025–2047. Google Scholar
- Landis, J. R., & Koch, G. G. ( 1977 ). An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers . Biometrics , 33 (2), 363–374. Medline , Google Scholar
- Laursen, S., Hunter, A.-B., Seymour, E., Thiry, H., & Melton, G. ( 2010 ). Undergraduate research in the sciences: Engaging students in real science . Hoboken, NJ: Wiley. Google Scholar
- Limeri, L. B., Asif, M. Z., Bridges, B. H., Esparza, D., Tuma, T. T., Sanders, D. , … & Maltese, A. V. ( 2019 ). “Where’s my mentor?” Characterizing negative mentoring experiences in undergraduate life science research . CBE—Life Sciences Education , 18 (4), ar61. Link , Google Scholar
- Link, B. G., & Phelan, J. C. ( 2001 ). Conceptualizing stigma . Annual Review of Sociology , 27 (1), 363–385. Google Scholar
- Luyten, P., Sabbe, B., Blatt, S. J., Meganck, S., Jansen, B., De Grave, C. , … & Corveleyn, J. ( 2007 ). Dependency and self-criticism: Relationship with major depressive disorder, severity of depression, and clinical presentation . Depression and Anxiety , 24 (8), 586–596. Medline , Google Scholar
- Mabrouk, P. A., & Peters, K. ( 2000 ). Student perspectives on undergraduate research (UR) experiences in chemistry and biology . CUR Quarterly , 21 (1), 25–33. Google Scholar
- Maxwell, J. A. ( 2010 ). Using numbers in qualitative research . Qualitative Inquiry , 16 (6), 475–482. Google Scholar
- Mongrain, M., & Blackburn, S. ( 2005 ). Cognitive vulnerability, lifetime risk, and the recurrence of major depression in graduate students . Cognitive Therapy and Research , 29 (6), 747–768. Google Scholar
- Nagy, G. A., Fang, C. M., Hish, A. J., Kelly, L., Nicchitta, C. V., Dzirasa, K., & Rosenthal, M. Z. ( 2019 ). Burnout and mental health problems in biomedical doctoral students . CBE—Life Sciences Education , 18 (2), ar27. Link , Google Scholar
- National Academies of Sciences, Engineering, and Medicine (NASEM) . ( 2017 ). Undergraduate research experiences for STEM students: Successes, challenges, and opportunities . Washington, DC: National Academies Press. https://doi.org/10.17226/24622 Google Scholar
- NASEM . ( 2019 ). The science of effective mentorship in STEMM . Washington, DC: National Academies Press. Retrieved November 29, 2019, from www.nap.edu/download/25568 Google Scholar
- Osborne, J., & Collins, S. ( 2001 ). Pupils’ views of the role and value of the science curriculum: A focus-group study . International Journal of Science Education , 23 (5), 441–467. https://doi.org/10.1080/09500690010006518 Google Scholar
- Porter, S. R., & Whitcomb, M. E. ( 2005 ). Non-response in student surveys: The role of demographics, engagement and personality . Research in Higher Education , 46 (2), 127–152. Google Scholar
- President’s Council of Advisors on Science and Technology . ( 2012 ). Engage to excel: Producing one million additional college graduates with degrees in science, Technology, Engineering, and mathematics . Washington, DC: U.S. Government Office of Science and Technology. Google Scholar
- Prunuske, A. J., Wilson, J., Walls, M., & Clarke, B. ( 2013 ). Experiences of mentors training underrepresented undergraduates in the research laboratory . CBE—Life Sciences Education , 12 (3), 403–409. Link , Google Scholar
- Quinn, D. M., & Earnshaw, V. A. ( 2011 ). Understanding concealable stigmatized identities: The role of identity in psychological, physical, and behavioral outcomes . Social Issues and Policy Review , 5 (1), 160–190. Google Scholar
- Rauckhorst, W. H., Czaja, J. A., & Baxter Magolda, M. ( 2001 ). Measuring the impact of the undergraduate research experience on student intellectual development . Snowbird, UT: Project Kaleidoscope Summer Institute. Google Scholar
- Saldaña, J. ( 2015 ). The coding manual for qualitative researchers . Thousand Oaks, CA: Sage. Google Scholar
- Santiago, C. D., Kaltman, S., & Miranda, J. ( 2013 ). Poverty and mental health: How do low-income adults and children fare in psychotherapy? Journal of Clinical Psychology , 69 (2), 115–126. Medline , Google Scholar
- Santini, Z. I., Koyanagi, A., Tyrovolas, S., Mason, C., & Haro, J. M. ( 2015 ). The association between social relationships and depression: A systematic review . Journal of Affective Disorders , 175 , 53–65. Medline , Google Scholar
- Schleider, J., & Weisz, J. ( 2018 ). A single-session growth mindset intervention for adolescent anxiety and depression: 9-month outcomes of a randomized trial . Journal of Child Psychology and Psychiatry , 59 (2), 160–170. Medline , Google Scholar
- Seymour, E., & Hewitt, N. M. ( 1997 ). Talking about leaving: Why undergraduates leave the sciences . Westview Press. Google Scholar
- Seymour, E., & Hunter, A.-B. ( 2019 ). Talking about leaving revisited . New York, NY: Springer. Google Scholar
- Seymour, E., Hunter, A.-B., Laursen, S. L., & DeAntoni, T. ( 2004 ). Establishing the benefits of research experiences for undergraduates in the sciences: First findings from a three-year study . Science Education , 88 (4), 493–534. Google Scholar
- Smith, D. T., Mouzon, D. M., & Elliott, M. ( 2018 ). Reviewing the assumptions about men’s mental health: An exploration of the gender binary . American Journal of Men’s Health , 12 (1), 78–89. Medline , Google Scholar
- Sorkness, C. A., Pfund, C., Ofili, E. O., Okuyemi, K. S., Vishwanatha, J. K., Zavala, M. E. , … & Deveci, A. ( 2017 ). A new approach to mentoring for research careers: The National Research Mentoring Network . BMC Proceedings , 11 , 22. Medline , Google Scholar
- Sowislo, J. F., & Orth, U. ( 2013 ). Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies . Psychological Bulletin , 139 (1), 213. Medline , Google Scholar
- Steger, M. F. ( 2013 ). Experiencing meaning in life: Optimal functioning at the nexus of well-being, psychopathology, and spirituality . In Wong, P. T. P. (Ed.), The human quest for meaning (pp. 211–230). England, UK: Routledge. Google Scholar
- Strenta, A. C., Elliott, R., Adair, R., Matier, M., & Scott, J. ( 1994 ). Choosing and leaving science in highly selective institutions . Research in Higher Education , 35 (5), 513–547. Google Scholar
- Text Depression Hotline . ( 2019 ). Crisis text line . Retrieved November 29, 2019, from www.crisistextline.org/depression Google Scholar
- Thiry, H., & Laursen, S. L. ( 2011 ). The role of student–advisor interactions in apprenticing undergraduate researchers into a scientific community of practice . Journal of Science Education and Technology , 20 (6), 771–784. Google Scholar
- Thompson, J. J., Conaway, E., & Dolan, E. L. ( 2016 ). Undergraduate students’ development of social, cultural, and human capital in a networked research experience . Cultural Studies of Science Education , 11 (4), 959–990. Google Scholar
- Trenor, J. M., Miller, M. K., & Gipson, K. G. ( 2011 ). Utilization of a think-aloud protocol to cognitively validate a survey instrument identifying social capital resources of engineering undergraduates . 118th American Society for Engineering Education Annual Conference and Exposition, Vancouver, BC, Canada . Google Scholar
- Turner, R. J., & Noh, S. ( 1988 ). Physical disability and depression: A longitudinal analysis . Journal of Health and Social Behavior , 29 (1), 23–37. Medline , Google Scholar
- Watson, D., & Friend, R. ( 1969 ). Measurement of social-evaluative anxiety . Journal of Consulting and Clinical Psychology , 33 (4), 448. Medline , Google Scholar
- Weeks, J. W., Heimberg, R. G., Fresco, D. M., Hart, T. A., Turk, C. L., Schneier, F. R., & Liebowitz, M. R. ( 2005 ). Empirical validation and psychometric evaluation of the Brief Fear of Negative Evaluation Scale in patients with social anxiety disorder . Psychological Assessment , 17 (2), 179. Medline , Google Scholar
- World Health Organization . ( 2018 ). Depression . Retrieved November 29, 2019, from www.who.int/news-room/fact-sheets/detail/depression Google Scholar
- Wyatt, T., & Oswalt, S. B. ( 2013 ). Comparing mental health issues among undergraduate and graduate students . American Journal of Health Education , 44 (2), 96–107. Google Scholar
- Carly A. Busch ,
- Tala Araghi ,
- Jingyi He ,
- Katelyn M. Cooper , and
- Colin Harrison, Monitoring Editor
- Emma C. Goodwin ,
- Danielle Pais ,
- Logan E. Gin , and
- Derek Braun, Monitoring Editor
- Baylee A. Edwards ,
- Chloe Bowen ,
- M. Elizabeth Barnes , and
- Tati Russo-Tait, Monitoring Editor
- Sara E. Grineski ,
- Danielle X. Morales , and
- Timothy W. Collins
- Carly A. Busch , and
- Tasneem F. Mohammed ,
- Erika M. Nadile ,
- Madison L. Witt ,
- Cindy Vargas ,
- Missy Tran ,
- Joseph Gazing Wolf ,
- Danielle Brister , and
- Sehoya Cotner, Monitoring Editor
- Katelyn M. Cooper ,
- Sarah L. Eddy , and
- Coping behavior versus coping style: characterizing a measure of coping in undergraduate STEM contexts 14 February 2022 | International Journal of STEM Education, Vol. 9, No. 1
- Lisa A. Corwin ,
- Michael E. Ramsey ,
- Eric A. Vance ,
- Elizabeth Woolner ,
- Stevie Maiden ,
- Nina Gustafson and
- Joseph A. Harsh
- Erin Shortlidge, Monitoring Editor
- K. Supriya ,
- Brian Sato, Monitoring Editor
- Logan E. Gin ,
- Clark Coffman, Monitoring Editor
- Nicholas J. Wiesenthal , and
- Maryrose Weatherton and
- Elisabeth E. Schussler
- Erika Offerdahl, Monitoring Editor
- Eight Recommendations to Promote Effective Study Habits for Biology Students Enrolled in Online Courses Journal of Microbiology & Biology Education, Vol. 23, No. 1
- Fostering professional development through undergraduate research: supporting faculty mentors and student researchers 30 March 2022 | Mentoring & Tutoring: Partnership in Learning, Vol. 30, No. 2
- Jeffrey Maloy ,
- Monika B. Kwapisz , and
- Bryce E. Hughes
- Terrell Morton, Monitoring Editor
- Anxiety and depression among US college students engaging in undergraduate research during the COVID-19 pandemic 14 December 2021 | Journal of American College Health, Vol. 9
- Danielle Brister ,
- Sara E. Brownell ,
- Chade T. Claiborne ,
- Curtis Lunt ,
- Kobe M. Walker ,
- Tamiru D. Warkina ,
- Yi Zheng , and
- Rebecca Price, Monitoring Editor
- Dominant Learning Styles of Interior Design Students in Generation Z 26 July 2021 | Journal of Interior Design, Vol. 46, No. 4
- Linking Emotional Intelligence, Physical Activity and Aggression among Undergraduates 26 November 2021 | International Journal of Environmental Research and Public Health, Vol. 18, No. 23
- Advancing undergraduate synthetic biology education: insights from a Canadian iGEM student perspective Canadian Journal of Microbiology, Vol. 67, No. 10
- Frank A. Guerrero ,
- Sara E. Brownell , and
- Jennifer Momsen, Monitoring Editor
- Nicholas J. Wiesenthal ,
- Isabella Ferreira , and
- Grant Ean Gardner, Monitoring Editor
- Carolyn E. Clark ,
- Deanna B. Elliott ,
- Travis B. Roderick ,
- Rachel A. Scott ,
- Denisse Arellano ,
- Diana Ramirez ,
- Kimberly Velarde ,
- Allyson Aeschliman ,
- Sarah T. Avalle ,
- Jessica Berkheimer ,
- Rachel Campos ,
- Michael Gerbasi ,
- Sophia Hughes ,
- Julie A. Roberts ,
- Quinn M. White ,
- Ehren Wittekind ,
- Rachelle Spell, Monitoring Editor
- Christine Pfund ,
- Janet L. Branchaw ,
- Melissa McDaniels ,
- Angela Byars-Winston ,
- Steven P. Lee ,, and
- Bruce Birren
- Vladimir Anokhin ,
- MacKenzie J. Gray ,
- Daniel E. Zajic ,
- Jason E. Podrabsky , and
- Erin E. Shortlidge
- Depression as a concealable stigmatized identity: what influences whether students conceal or reveal their depression in undergraduate research experiences? 4 June 2020 | International Journal of STEM Education, Vol. 7, No. 1
Submitted: 4 November 2019 Revised: 24 February 2020 Accepted: 6 March 2020
© 2020 K. M. Cooper, L. E. Gin, et al. CBE—Life Sciences Education © 2020 The American Society for Cell Biology. This article is distributed by The American Society for Cell Biology under license from the author(s). It is available to the public under an Attribution–Noncommercial–Share Alike 3.0 Unported Creative Commons License (http://creativecommons.org/licenses/by-nc-sa/3.0).
Loading metrics
Open Access
Peer-reviewed
Research Article
Depression, anxiety and stress among high school students: A cross-sectional study in an urban municipality of Kathmandu, Nepal
Contributed equally to this work with: Anita Karki, Bipin Thapa
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Writing – original draft, Writing – review & editing
* E-mail: [email protected] (PB); [email protected] (AK)
Affiliation Central Department of Public Health, Institute of Medicine, Tribhuvan University, Kathmandu, Nepal
Roles Data curation, Formal analysis, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing
Affiliation Department of Child, Adolescent Health and Maternal Care, School of Public Health, Capital Medical University, Beijing, China
Roles Writing – review & editing
Affiliation Department of Community Medicine, Maharajgunj Medical Campus, Institute of Medicine, Tribhuvan University, Kathmandu, Nepal
Roles Conceptualization, Methodology, Supervision, Writing – review & editing
- Anita Karki,
- Bipin Thapa,
- Pranil Man Singh Pradhan,

- Published: May 31, 2022
- https://doi.org/10.1371/journal.pgph.0000516
- Peer Review
- Reader Comments
Depression and anxiety are the most widely recognized mental issues affecting youths. It is extremely important to investigate the burden and associated risk factors of these common mental disorders to combat them. Therefore, this study was undertaken with the aim to estimate the prevalence and identify factors associated with depression, anxiety, and stress among high school students in an urban municipality of Kathmandu, Nepal. A cross-sectional study was conducted among 453 students of five randomly selected high schools in Tokha Municipality of Kathmandu. Previously validated Nepali version of depression, anxiety, and stress scale (DASS-21) was used to assess the level of symptoms of depression, anxiety and stress (DAS). Multivariable logistic regression was carried out to decide statistically significant variables of symptoms of DAS at p-value<0.05. The overall prevalence of DAS was found to be 56.5% (95% CI: 51.8%, 61.1%), 55.6% (95%CI: 50.9%, 60.2%) and 32.9% (95%CI: 28.6%, 37.4%) respectively. In the multivariable model, nuclear family type, students from science or humanities faculty, presence of perceived academic stress, and being electronically bullied were found to be significantly associated with depression. Female sex, having mother with no formal education, students from science or humanities faculty and presence of perceived academic stress were significantly associated with anxiety. Likewise, female sex, currently living without parents, and presence of perceived academic stress were significantly associated with stress. Prevention and control activities such as school-based counseling services focusing to reduce and manage academic stress and electronic bullying are recommended in considering the findings of this research.
Citation: Karki A, Thapa B, Pradhan PMS, Basel P (2022) Depression, anxiety and stress among high school students: A cross-sectional study in an urban municipality of Kathmandu, Nepal. PLOS Glob Public Health 2(5): e0000516. https://doi.org/10.1371/journal.pgph.0000516
Editor: Khameer Kidia, Brigham and Women’s Hospital, UNITED STATES
Received: February 22, 2022; Accepted: May 2, 2022; Published: May 31, 2022
Copyright: © 2022 Karki et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: The data that support the findings of descriptive analysis of this study are available in Figshare with the identifier given below: https://doi.org/10.6084/m9.figshare.19203512 The data that support the findings of inferential analysis of this study are available in Figshare with the identifier given below: https://doi.org/10.6084/m9.figshare.19203491 .
Funding: The authors received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Mental disorders contribute to a huge proportion of disease burden across all societies [ 1 ]. Among them, depression, anxiety and stress are the leading causes of illness and disability among adolescents [ 2 ]. The physical, psychological, and behavioral changes that occur throughout adolescence predispose them to a variety of mental health issues [ 3 ]. Despite this, mental health and mental disorders are largely ignored and not given the same importance as physical health [ 4 ].
The existing community-based studies conducted among high school students of various parts of Nepal have reported a wide range of prevalence of symptoms of depression and anxiety. The prevalence of depressive symptoms has been reported to range from 27% to 76% [ 5 – 7 ]. Likewise, the limited studies conducted in Nepal have estimated the proportion of symptoms of anxiety to range from 10% to 57% [ 7 – 9 ]. A nationwide survey conducted in Nepal revealed the prevalence of mental distress among adolescents (13-17years) to be 5.2% [ 10 ]. The Global School Health Survey which was a nationwide survey conducted in 2015 reported anxiety among 4.6% of the students [ 11 ].
Previous studies have revealed that sex [ 12 – 16 ], staying away from home [ 17 ], grade [ 12 , 14 , 16 ], stream of study [ 18 ], academic performance and examination related issues [ 7 , 19 ], cyber bullying [ 20 ] were linked with depression. Likewise, sex [ 8 , 21 ], grade of students and type of school i.e., public or private [ 8 ], family type [ 17 ], not living with parents, educational level of parents [ 21 ] and high educational stress [ 22 ] had been the determinants of anxiety as per previous studies.
High school education is an important turning point in the life of academic students in Nepal [ 23 ]. As the educational system becomes more specialized and tough in high school, the students become more likely to experience stress at this level. This might put them at risk of developing common mental disorders such as depression, anxiety and stress (DAS). However, there is a paucity of research studies that have assessed DAS among high school students in Nepal.
Exploring the magnitude and risk factors of symptoms of DAS are very crucial to combat the burden of adolescent mental health issues [ 24 ]. However, due to limited access to psychological and psychiatric services as well as the significant social stigma associated with mental health issues, anxiety and depression in early adolescence frequently go undiagnosed and untreated, particularly in developing countries such as Nepal. Therefore, this study aimed to estimate the prevalence and identify factors associated with the symptoms of DAS among high school students in an urban municipality of Kathmandu, Nepal.
Materials and methods
Study setting, design, and population.
This was a cross-sectional survey conducted in randomly selected high schools of Tokha Municipality, Kathmandu District in province no. 3 of Nepal. The data collection period was from 27 th August to 11 th September 2019. This municipality was formed on 7 December 2014 by merging five previous villages. It has an area of 16.2 sq.km. and comprises 11 wards [ 25 , 26 ]. The municipality is rich in cultural and ethnic diversity [ 25 ]. According to Nepal government records as of 2017, there were total 218,554 students in Tokha municipality in 82 schools. High school students were the study population for this study [ 26 ]. In Nepal, high school students comprise of grade 11 and grade 12 students. The high school differs from lower schooling level since the students have the opportunity to enroll in specialized areas such as science, management, humanities and education. High school are also popularly known as 10+2 [ 27 ].
Sample size calculation and sampling technique
Sample size was estimated using the formula for cross-sectional survey [ 28 ], n = Z 2 p(1-p)/ e 2 considering the following assumptions; proportion (p) = 0.24 [ 12 ], 95% confidence level, the margin of error of 5%. The estimated proportion used for sample size calculation was based on proportion of symptoms of anxiety i.e., 24%, as reported by a similar study conducted in Manipur, India [ 12 ].
After calculation, the minimum sample size required was 280. After adjusting for design effect of 1.5 to adjust variance from cluster design and assuming non-response rate of 10%, final sample of 467 was calculated. Two-stage cluster sampling was used. A list of all high schools of Tokha municipality was obtained from the education division of the municipality. Out of twelve high schools (8 private schools and 4 public schools), five schools were randomly selected. Within each selected high school further two sections each of grades 11 and 12 were randomly selected. A total of 20 sections were selected, 4 from each selected school, and all the students from the selected sections were included in the study.
Data collection tools
A structured questionnaire was prepared based on our study objectives which was divided into three sections. The first section included information about socio-demographic, familial and academic characteristics of the students. The second section included two item question to assess socializing among the students which was based on a previous study by Vankim and Nelson [ 29 ], two questions to assess bullying among the students based on 2019 Youth Risk Behavior Survey [ 30 ] and one item question to assess perceived academic stress. The third section consisted of Depression, Anxiety and Stress Scale (DASS-21) used to assess level of symptoms of depression, anxiety and stress among the students.
DASS-21 is a psychological screening instrument capable of differentiating symptoms of DAS. Depression, anxiety, and stress are three subscales and there are 7 items in each subscale. Each item is scored on a 4-point Likert scale which ranges from 0 i.e., did not apply to me at all to 3 i.e., applied to me very much. Scores for DAS were calculated by summing the scores for the relevant items. and multiplying by two [ 31 ]. A previously validated Nepali version of DASS-21 was obtained and used for data collection. Nepali version of the DASS-21 has demonstrated adequate internal consistency and validity. However, in the validation paper, the construct validity of the tool was evaluated against life satisfaction scale and not a systematic diagnostic tool [ 32 ]. Reliability for the symptoms of DAS was tested by Cronbach alpha. Cronbach alpha values for DAS were 0.74, 0.77, and 0.74 respectively.
Data collection procedure and technique
Data was collected after obtaining permission from the municipality’s education division as well as individual high schools. The questionnaire was in both English and Nepali language and had been pre-tested among 45 high school students of neighboring municipality. Self-administered anonymous questionnaires were distributed to students in their respective classrooms and requested for participation. An orientation session was conducted for the filling the questionnaire before distribution. Written informed consent was taken from all students prior to data collection whereas additional written parental consent was obtained from students below 18 years of age. One of the investigators herself collected the data from students. After data collection, a session on depression, anxiety, and stress along with the importance of discussing it with the guardians/ teachers and asking for help was conducted.
Study variables
The study variables are described in Table 1 .
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pgph.0000516.t001
Data analysis
Compilation of data was done in EpiData 3.1 and then exported to IBM SPSS Statistics version 20 (IBM Corp., Armonk, NY) for cleaning and analysis. Descriptive analysis was performed. Frequency tables with percentages were generated for categorical variables, while mean and standard deviation (SD) were calculated for continuous variables.
Binary logistic regression was performed to identify associated factors of symptoms of DAS. Firstly, we performed univariate analysis in which each co-variate was modeled separately to determine the odds of DAS. Those variables with p-value <0.15 in univariate analysis were identified as candidate variables for multivariable logistic regression. In multivariable logistic regression, a p-value of < .05 was considered to be statistically significant and strength of association was measured using adjusted odds ratio (AOR) at 95% confidence interval.
Multicollinearity of variables was tested before entering them in the regression analysis. No problem of multicollinearity was seen among the variables (the highest observed VIF was 1.25,1.10 and 1.13 for symptoms of DAS respectively. The goodness of fit of the regression model was tested by the application of the Hosmer and Lemeshow test; the model was found to be a good fit (P >.05).
The regression model was explained by the equation:
Log [Y/ (1-Y)] = b 0 + b 1 X 1 + b 2 X 2 + b 3 X 3 … ..b n X n + e
Where Y is the expected probability for the outcome variable to occur, b 0 is the constant/intercept, b 1 through b n are the regression coefficients and the X 1 through X n are distinct independent variables and e is the error term.
Ethical approval and consent
The study protocol was approved by the Institutional Review Committee (IRC) of the Institute of Medicine, Tribhuvan University (Reference no. 23/ (6–11) 76/077). Approval to conduct this study was also obtained from the education division of Tokha Municipality (Ref: 076/077-23) and respective school authorities. A written informed consent (in the Nepali language) was obtained from the students before the data collection to assure their willingness to participate and no identifiers were listed in the questionnaire to make it anonymous and confidential. Parental consent was obtained for students who were under the age of 18. No incentives were provided.
Sociodemographic, academic and contextual characteristics of the students
The research questionnaire was distributed to a sample of 468 high school students, one of whom refused to participate in this study, with a response rate of 99.78%. Responses from 14 students were excluded due to incompleteness. This study presents the analysis on a total of 453 students.
The mean age of the students was 16.99 years (SD = ±1.12), ranging from 14 to 22 years. The proportion of female students (54.1%) was higher than male students (45.9%). Majority of the students were found to be currently living with their parents i.e., 65.8%. Around 70% of the students were from nuclear family. Regarding parent’s educational level, majority of the students responded that their father as well as mother had attained secondary level of education i.e., 31.6% and 33.3% respectively.
With regards to academic characteristics, more than two- third of students i.e., 69.5% were from private high schools while the remaining 30.5% were studying in a government or public high school. More than half i.e. (53.4%) of the students studied in grade eleven. About half of the students i.e., 50.6% were from management faculty. Only 3.8% students reported to have failed in the previous examination.
It was noted that about 60% of students perceived themselves to be stressed due to their studies. Most students were low socializing i.e., 60.9%. Around one-tenth students reported being bullied electronically in the past 12 months (10.2%). Similar proportion of students i.e., 10.4% also reported being bullied on school property in the past 12 months ( Table 2 ).
https://doi.org/10.1371/journal.pgph.0000516.t002
Level of symptoms of DAS among the students
The prevalence of symptoms of DAS was found to be 56.5% (51.8%, 61.1%), 55.6% (50.9%, 60.2%) and 32.9% (28.6%, 37.4%) respectively. About a quarter of students showed moderate level of symptoms of depression and anxiety i.e., 25.8% and 24.5% respectively. On the other hand, symptoms of mild stress were most prevalent among the students. i.e., 14.8% ( Table 3 ).
https://doi.org/10.1371/journal.pgph.0000516.t003
Factors associated with symptoms of depression
The results from multivariable logistic regression analyses for correlates of symptoms of depression are shown in Table 4 . The variables that remain in the final model were age, type of family, father’s education, mother’s education, type of school, grade, faculty, perceived academic stress, and bullied electronically as these variables had p-value less than 0.15 in the univariate model. In the final model, nuclear family type (AOR: 1.64, 95% CI: 1.06–2.52), students from science/humanities faculty (AOR: 1.58, 95% CI: 1.05–2.40), presence of perceived academic stress (AOR: 1.62, 95% CI: 1.08–2.44) and bullied electronically in past 12 months (AOR: 2.84, 95% CI: 1.34–5.99) were significantly associated with symptoms of depression.
https://doi.org/10.1371/journal.pgph.0000516.t004
Factors associated with symptoms of anxiety
The results from multivariable logistic regression analyses for correlates of symptoms of anxiety are shown in Table 5 . The variables that remained in the final model were age, sex, mother’s education, stream/ faculty, perceived academic stress, bullied electronically, and bullied on school property (p<0.15). Female sex (AOR: 1.82, 95% CI: 1.23–2.71), no formal education attained by the mother (AOR: 1.63, 95% CI: 1.08–2.47), students from science or humanities faculties (AOR: 1.50, 95% CI: 1.01–2.21), and presence of perceived academic stress (AOR: 1.93, 95% CI: 1.30–2.87), and were significantly associated with symptoms of anxiety.
https://doi.org/10.1371/journal.pgph.0000516.t005
Factors associated with symptoms of stress
The results from multivariable logistic regression analyses for main correlates of symptoms of stress are shown in Table 6 . The variables that remained in the final model were sex, current living status, grade, stream / faculty, perceived academic stress, bullied electronically and bullied on school property. In the final model, female sex (AOR: 1.54, 95% CI: 1.01–2.34), currently living without parents, (AOR: 1.70, 95% CI: 1.11–2.61), and presence of perceived academic stress (AOR: 2.11, 95% CI: 1.36–3.26) were significantly associated with stress symptoms.
https://doi.org/10.1371/journal.pgph.0000516.t006
In our study, the prevalence of depressive symptoms among high school students was found to be 56.5%. The existing community-based studies conducted among high school students of various parts of Nepal have reported a wide range of prevalence of depressive symptoms. A study by Gautam et al. reported that more than one quarter i.e., 27% of high school students in a rural setting of Nepal showed depressive symptoms [ 6 ]. Similarly, in a study conducted by Bhattarai et. al. in four schools of a metropolitan city in Nepal, it was found that more than 2/5 th i.e., 44.2% students exhibited depressive symptoms [ 5 ]. Similar proportion of depressive symptoms i.e., 41.6% was also reported by Sharma et. al in a study conducted among adolescent students of public schools of Kathmandu [ 9 ]. The prevalence estimated by these studies are lower than the findings of our study [ 5 , 6 , 9 ]. On contrary, a single high school study by Bhandari et al reported depressive symptoms among 76% students [ 7 ]. In our study, the proportion of students showing symptoms of anxiety were 55.6%. A study by Sharma et al. revealed that more than half i.e. 56.9% of public high school students showed symptoms of anxiety [ 9 ]. Another study by Bhandari et. al, also found out that nearly one out of two students i.e., 46.5% suffered from anxiety [ 8 ].These findings are in line with the findings of our study. On contrary, a study by Bhandari reported that only 10% students had mild anxiety [ 7 ]. In our study, the prevalence of stress symptoms among students was 32.9%. A study by Sharma et. al reported that more than 1/4 th students i.e., 27.5% showed symptoms of stress which corroborates with the findings of our study.
While the prevalence of symptoms of DAS reported by our study corroborates with the existing literatures in Nepal, it is exceptionally high. One possible explanation for this could be that the data was collected at the beginning of academic session. The students in the eleventh grade were undergoing sudden transition from secondary school life to high school life with regards to new friends, teachers, school environment, and change in daily schedules whereas the students in 12 th grade were awaiting results of previous board exam. This anticipation and the tremendous pressure faced by 12 th grade students for tertiary education might have contributed to the high prevalence of symptoms of DAS among 12 th grade students whereas the higher prevalence of symptoms of DAS among 11 th grade students could be possibly explained by the inability to cope with the adjustment of sudden transition from secondary to high school life. Moreover, the wide range in prevalence of DAS symptoms among these community-based studies could be attributed to the difference in the setting (rural or urban) and difference in methodology used.
Among South Asian countries, the prevalence of depression reported by our study is in line with the studies conducted in India, and Bangladesh, but slightly higher than one conducted in China and [ 13 , 17 , 33 , 34 ]. On contrary, our study has shown higher prevalence of anxiety among students as compared to study conducted in India, Sri Lanka, Vietnam and China [ 12 , 19 , 22 , 34 ].The prevalence of symptoms of stress in this study is comparable to the study from Chandigarh but higher than similar study from Manipur, India [ 12 , 17 ]. Hence, it can be suggested that there is a huge burden of DAS among high school students in South Asia. In context of Nepal, there is no standalone mental health policy. Further, there is inadequate funding allocated for mental health services along with shortage of qualified mental health professionals. In addition, there is much stigma that surrounds mental illness which acts as a barrier to seek and utilize mental health care services [ 35 ]. Due to these reasons, mental health illnesses are likely to remain untreated and continue to persist in the society. This may explain the high prevalence of DAS in our setting.
Socio-demographic characteristics and association with symptoms of DAS (depression, anxiety and stress)
In current study, it was found that females were more likely to suffer from symptoms of anxiety and stress than their male counterparts. This finding corroborates with the findings from previous studies [ 19 , 21 , 36 – 39 ]. On the contrary, a study conducted in Dang, Nepal reported that males were 1.5 times more likely to become anxious [ 8 ].One possible explanation for this is adolescent stage in girls is marked by hormonal changes as a result of various reproductive events which may have a role in the etiology of anxiety disorders [ 40 ]. Furthermore, when compared to boys, girls are more likely to be subjected to stressful situations such as sexual and domestic violence, which may make them more prone to anxiety and stress problems [ 41 ].
This study revealed that the students who live in nuclear families were more likely to exhibit depressive symptoms compared to students from joint or extended families. There are more members in a joint family system, which may provide better opportunities for adolescents to share their emotions and issues, hence providing a strong support system that may serve as a protective factor against depression which may be lacking in nuclear families [ 42 ]. Moreover, this study also found out that risks of stress symptoms was higher among students who were staying far from their parents. A similar finding was reported by Arif et al., 2019 in Uttar Pradesh, India [ 43 ]. One of the possible explanations might be that students who live without their parents may spend a substantial amount of time alone after school, which does not encourage familial intimacy [ 44 ]. As a result, they may feel alone and disconnected from their parents [ 45 ]. These adolescents may miss out on the opportunity to internalize the support they would otherwise get, leading to increased stress.
In our study, the students who reported no formal mother’s education were at greater risk of showing symptoms of anxiety. This was in accordance with other similar studies [ 38 , 46 ]. The attachment theory provides a robust foundation for understanding how parental behavior affects a child’s ability to recognize and manage stressful events throughout their lives [ 47 ]. The theory supports that the educated mother plays a stronger parenting role in the development of emotional skills and mental health outcomes in teenagers which might be protective for anxiety.
Academic characteristics and association with symptoms of DAS
In our study, the students from science or humanities faculties were more likely to have depression and anxiety as compared to management students. This was in line with other studies which showed higher proportion of depressive symptoms among science students. [ 48 ]. Generally, science students have to compete more, study longer hours and have a higher level of curriculum difficulty than management students which explains the finding. Likewise, it is believed that the humanities students have a poorer past academic performance in the secondary school, and may have chosen this stream / faculty as a secondary choice [ 49 ]. This combined with the uncertainty regarding future work prospects among humanities students may likely explain the higher prevalence of depression among humanities students.
In our study, the students who reported to be stressed due to their studies were more likely to suffer from symptoms of DAS. Several studies have documented similar findings [ 7 , 22 ]. A possible explanation might be that high school is an important stage in an individual’s academic life. However, the inability to meet the expectation of parents, teachers, and oneself in terms of academic performance can lead to overburden of stress [ 50 ]. This persistent academic related stress might accelerate the development of mood disorders such as depression, anxiety and stress among the adolescents [ 51 ].
Contextual factors and association with symptoms of DAS
In our study, the risk of depressive symptoms was higher among those students who were bullied via electronic means. Literature suggests that higher the level of cyberbullying/electronic bullying leads to higher the level of depressive symptoms among adolescents [ 52 ]. A similar study by Perren et. al demonstrated that depression was significantly associated with cyberbullying even after controlling for traditional forms of bullying [ 20 ]. The victims of cyberbullying may experience anonymous verbal or visual threats via electronic means. These repeated incidents can cause the victims to feel powerless which exacerbates the feeling of fear. This can cause significant emotional distress among victims and contribute to development of depressive symptoms [ 53 ].
Even though widely utilized in both clinical as well as research setting, DASS scales are screening tools for symptoms of depression, anxiety, and stress. Hence, they cannot be used as a modality for diagnosis. This limitation should be considered when interpreting the findings of this study. Due to its cross-sectional design, this study was unable to establish causal relationship of depression, anxiety, and stress with associated factors. Since the study tools used in this study investigate the habits and activities of the high school students in the past, recall and reporting bias are likely; however, the effect due to potential confounders have been controlled. As Nepal is a culturally diverse country, the findings of only one municipality may not be generalized to the whole country. Therefore, future studies covering a larger population of high school students employing more robust study designs such as interventional studies are recommended to get the real scenario of common mental disorders.
In conclusion, more than half of the students had depression and anxiety symptoms and nearly one third of the students had stress symptoms. Nuclear family type, students from humanities/science faculty, presence of perceived academic stress, and being bullied electronically were found to be significantly associated with symptoms of depression. Female sex, no formal mother education, students from humanities/science faculty, and presence of perceived academic stress were significantly associated with symptoms of anxiety. Likewise, symptoms of stress were significantly associated with female sex, currently living without parents, and presence of perceived academic stress.
Therefore, prevention and control activities such as school-based counseling services focusing to reduce and manage academic stress and electronic bullying faced by the students are recommended considering findings of this research.
Supporting information
S1 file. questionnaire form used in data collection..
https://doi.org/10.1371/journal.pgph.0000516.s001
Acknowledgments
We are grateful to Tokha municipality for granting permission to conduct the study. Special thank goes to the school management and teachers for their co-ordination during data collection. Lastly, we would like to thank all the study participants for their co-operation and support during the study.
- View Article
- PubMed/NCBI
- Google Scholar
- 2. Adolescent mental health. [cited 27 Jul 2021]. Available: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health
- 3. World Health Organization. Regional Office for South-East Asia. Mental health status of adolescents in South-East Asia: evidence for action. New Delhi: World Health Organization. Regional Office for South-East Asia; 2017. Available: https://apps.who.int/iris/handle/10665/254982%0A
- 9. Sharma P, Choulagai B. Stress, anxiety, and depression among adolescent students of public schools in Kathmandu. [cited 19 Mar 2022]. Available: www.jiom.com.np
- 10. Nepal Health Research Council. National Mental Health Survey, Nepal-2020. In: Nepal Health Research Council [Internet]. 2020 pp. 1–4. Available: http://nhrc.gov.np/projects/nepal-mental-health-survey-2017-2018/
- 25. Brief Introduction | Tokha Municipality, Office Of the Municipal Executive. [cited 25 Jul 2021]. Available: https://www.tokhamun.gov.np/en/node/4
- 26. Tokha Municipality Profile | Facts & Statistics–Nepal Archives. [cited 25 Jul 2021]. Available: https://www.nepalarchives.com/content/tokha-municipality-kathmandu-profile/
- 27. Nepal—Secondary Education—Level, Schools, Technical, and Training—StateUniversity.com. [cited 22 Mar 2022]. Available: https://education.stateuniversity.com/pages/1058/Nepal-SECONDARY-EDUCATION.html
- 30. 2019 State and Local Youth Risk Behavior Survey. 2019; 7. Available: https://www.cdc.gov/healthyyouth/data/yrbs/pdf/2019/2019_YRBS-Standard-HS-Questionnaire.pdf
- 35. World Health Organization (WHO). Nepal WHO Special Initiative for Mental Health Situational Assessment CONTEXT.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 17 December 2021
Anxiety and depressive symptoms in college students during the late stage of the COVID-19 outbreak: a network approach
- Wei Bai ORCID: orcid.org/0000-0001-9579-9959 1 , 2 , 3 na1 ,
- Hong Cai 1 , 2 , 3 na1 ,
- Shou Liu 4 na1 ,
- Xu Chen 5 na1 ,
- Sha Sha 5 ,
- Teris Cheung 6 ,
- Jessie Jingxia Lin ORCID: orcid.org/0000-0002-8189-8216 7 ,
- Xiling Cui 8 ,
- Chee H. Ng 9 &
- Yu-Tao Xiang ORCID: orcid.org/0000-0002-2906-0029 1 , 2 , 3
Translational Psychiatry volume 11 , Article number: 638 ( 2021 ) Cite this article
7213 Accesses
36 Citations
1 Altmetric
Metrics details
Mental health problems are common in college students even in the late stage of the coronavirus disease 2019 (COVID-19) outbreak. Network analysis is a novel approach to explore interactions of mental disorders at the symptom level. The aim of this study was to elucidate characteristics of depressive and anxiety symptoms network in college students in the late stage of the COVID-19 outbreak. A total of 3062 college students were included. The seven-item Generalized Anxiety Disorder Scale (GAD-7) and nine-item Patient Health Questionnaire (PHQ-9) were used to measure anxiety and depressive symptoms, respectively. Central symptoms and bridge symptoms were identified based on centrality and bridge centrality indices, respectively. Network stability was examined using the case-dropping procedure. The strongest direct relation was between anxiety symptoms “Nervousness” and “Uncontrollable worry”. “Fatigue” has the highest node strength in the anxiety and depression network, followed by “Excessive worry”, “Trouble relaxing”, and “Uncontrollable worry”. “Motor” showed the highest bridge strength, followed by “Feeling afraid” and “Restlessness”. The whole network was robust in both stability and accuracy tests. Central symptoms “Fatigue”, “Excessive worry”, “Trouble relaxing” and “Uncontrollable worry”, and critical bridge symptoms “Motor”, “Feeling afraid” and “Restlessness” were highlighted in this study. Targeting interventions to these symptoms may be important to effectively alleviate the overall level of anxiety and depressive symptoms in college students.
Similar content being viewed by others

Network analysis of depressive and anxiety symptoms in adolescents during the later stage of the COVID-19 pandemic

Changes in network centrality of psychopathology symptoms between the COVID-19 outbreak and after peak

Network analysis of anxiety and depressive symptoms during the COVID-19 pandemic in older adults in the United Kingdom
Introduction.
Depressive and anxiety symptoms (depression and anxiety hereafter) are common mental health problems, which are increasing globally in the past decade [ 1 ]. The presence of either depression or anxiety often increases the risk of having the other. For instance, a meta-analysis revealed that depression and anxiety are bidirectional risk factors for one another [ 2 ]. In addition, depression and anxiety often occur concurrently, such as in a study on UK college students, 29.8% of females and 13.9% of males screened positive for both anxiety and depression [ 3 ].
The coronavirus disease 2019 (COVID-19) outbreak that started in early 2020 have resulted in an increase in common depression and anxiety across many populations [ 4 , 5 , 6 ]. After the COVID-19 outbreak was largely controlled in some countries such as China, studies found that the large scale public health measures (e.g., quarantine, self-isolation, and business and school closures) resulted in long-term stress and psychological distress in many populations [ 7 , 8 ] such as college students [ 9 ]. Compared to most other subpopulations, college students are more likely to experience mental health problems [ 10 ]. The COVID-19 resurgence caused by imported cases and relevant public health measures often lead to depression and anxiety in students due to fear of immediate quarantine, delays in school opening, and switching to online teaching [ 11 ]. A recent two-wave longitudinal survey in China found that the rates of depression and anxiety among college students increased in the late stage of the COVID-19 outbreak compared to that in the early stage [ 12 ], indicating that long-term preventive measures and mental health services are important for this population even in the post-outbreak period.
In the last few years, the network analysis has been widely used in psychopathology to conceptualize and visualize patterns relevant to psychiatric disorders. In the theory of network analysis, psychiatric disorders consist of interacting symptoms [ 13 , 14 ]; accurate descriptions of these interactions are crucial to explain potential psychopathological mechanisms and develop effectively targeted intervention strategies [ 15 ]. In the visualization of the network model, each symptom of a psychiatric disorder can be viewed as a node and the association between two symptoms is viewed as an edge [ 16 ]. Compared with the traditional method of using total scale scores, network analysis is a symptom-oriented approach which can calculate indices for each node, such as centrality and predictability, representing a node’s importance and controllability in a network [ 17 , 18 ]. Calculating centrality indices could be beneficial to identify central (influential) symptoms in a psychiatric disorder, and these symptoms may be potential targets to prevention and interventions. Additionally, this novel model is useful in understanding comorbidities [ 19 ]. When an individual suffers a particular psychiatric disorder, the symptoms of this disorder may increase the risk of other disorders, which is regarded as bridge symptom in network model. The bridge symptoms in the network play an important role in maintaining and developing comorbidities, and provide hints for clinicians to prevent and treat comorbidities [ 19 ].
Researchers have explored characteristics of the anxiety and depression network in various populations. For example, “fatigue” was identified as the central and bridge symptom in migrant Filipino domestic workers, which may increase the risk of comorbidity between anxiety and depression [ 20 ]. In another psychiatric sample, “sad mood” and “worry” were the two most central symptoms in the network [ 21 ], suggesting that targeting these symptoms in treatment would be more effective. Convincing evidence has shown that patterns and features of mood disorders were influenced by socioeconomic contexts [ 22 , 23 ], suggesting that the network structure of anxiety and depressive symptoms should be examined separately across populations of different socioeconomic backgrounds.
To date, no studies have investigated how depressive and anxiety symptoms are related to each other in college students using the network model, particularly in the late stage of the COVID-19 outbreak, which gives us the impetus to conduct this study. The aim of the present study was hence to examine the associations between depressive and anxiety symptoms in Chinese college students in the late stage of the COVID-19 outbreak using network analysis.
Study settings and participants
This was a nationwide survey conducted among Chinese college students between December 27, 2020 and March 12, 2021, which was considered the late stage of the COVID-19 outbreak in China. To avoid the risk of face-to face transmission, online questionnaires were distributed using snowball sampling. The details of survey procedures have been introduced elsewhere [ 24 ]. To be eligible, participants need to be undergraduate students aged between 16 and 30 years, Chinese ethnicity, and able to understand the purpose and content of this survey. This study was approved by the Institutional Review Board (IRB) of Beijing Anding Hospital. All participants have provided electronic written informed consent; guardians provided informed consent if students were younger than 18 years.
The nine-item Patient Health Questionnaire (PHQ-9) was used to assess depressive symptoms [ 25 ]. Reference names of each item in the network analysis are presented in Table 1 . The PHQ-9 is a four-point Likert scale with each item scored from 0 (not at all) to 3 (nearly every day); higher scores indicates more severe symptoms. The Chinese version of PHQ-9 was used as it has been well validated in Chinese populations [ 26 ].
Anxiety symptoms were measured using the seven-item Generalized Anxiety Disorder (GAD-7) [ 27 ] scale and the reference names of items are shown in Table 1 . This is also a four-point Likert scale, with each item scored from 0 (not at all) to 3 (nearly every day). Higher scores indicate more severe anxiety symptoms. The Chinese version of the GAD-7 has satisfactory psychometric properties [ 28 ].
Data analysis
All analyses were conducted using the R program [ 29 ]. The network analysis was performed in three domains, including network estimation, network stability, and network comparisons.
Network estimation
In the parlance of network analysis, each item is indicated as a node and the association between two nodes is viewed as an edge. The association between each pairwise nodes was computed with partial correlation analysis, controlling for the confounding effects of all the other nodes. The least absolute shrinkage and selection operator (LASSO) was used to shrink all edges in the network and set small correlations to zero [ 30 ], which enables nodes with as few edges as necessary to be retained in the network. The extended Bayesian Information Criteria (EBIC) was adopted to choose related turning parameter so that the network was sparser and easier to interpret [ 31 ]. Due to the skewed distribution of the mean item scores, nonparametric correlations were calculated by the nonparanormal transformation [ 32 ]. The R packages bootnet (Version 1.4.3) [ 33 ] and qgraph (Version 1.6.9) [ 16 ] were used to estimate and visualize the network. In the layout of network, the thickness of edges indicates the magnitude of the association. Blue edges referred to positive associations, while red edges indicated negative ones.
To quantify the importance of each node in the network, centrality indices were computed using the function centralityPlot of the R package qgraph (Version 1.6.9) [ 16 ]. The network was usually characterized with the several centrality indices, including strength, betweenness, and closeness [ 34 ]. Previous studies demonstrated that estimations of closeness and betweenness are unreliable [ 35 , 36 ], thus, the most often used centrality index of strength was used in this study. Predictability was also measured in this study, which indicates the interconnectedness and the extent of a node associated with its neighboring nodes [ 31 ]. In the layout of the network, the area in the rings around each node represents the value of predictability, which was calculated using the function predict of R package mgm (Version 1.2-11) [ 37 ].
To assess the importance of a node in linking anxiety and depression, as recommended in previous studies [ 19 ], bridge centrality index of bridge strength was analyzed using the function bridge of the R package networktools (Version 1.2.3) [ 38 ].
Network stability
The stability of node strength and bridge strength was examined using a case-dropping bootstrap procedure. In this procedure, a growing percentage of cases was dropped from the dataset, while the centrality indices were re-estimated. A network is stable if a large proportion of sample could be excluded from dataset without observing significant changes of indices, and the stability is quantified by the Correlation Stability Coefficient (CS-C) [ 33 ]. The CS-C means the maximum cases that could be dropped from the sample, in which the centrality indices from the subsamples are correlated with the indices from the original sample at a value of r = 0.7 [ 33 ]. Generally, the value of CS-C needs to be above 0.25 and is preferably above 0.5 [ 33 ]. A nonparametric bootstrap procedure was used to assess the edge weights stability based on the 95% confidence intervals (95% CIs). Edge accuracy was assessed by 95% CIs, with a narrower CI indicating a more trustworthy network [ 33 , 39 ]. Additionally, to evaluate the differences between two edges or between two nodes strength, bootstrapped tests were conducted based on 95% CIs, which indicated that there were statistical differences between two edges or two nodes strength if zero was not included in the CIs [ 33 ]. All analyses in network stability were performed by the R package bootnet (Version 1.4.3) [ 33 ].
Network comparison
The Network Comparison Test (NCT) in the R-package NetworkComparisonTest (Version 2.2.1) was used to examine the three invariance measures (i.e., network structure invariance, edge invariance, and global strength) [ 40 ]. Network structure means the maximum difference of pairwise edges between two networks, edge invariance indicates the difference of individual edge weight between two networks, and global strength refers to the sum of all edges of each network. Holm-Bonferroni correction for multiple comparisons at the level of individual edge between two networks was adopted. Considering the moderating effect of gender [ 41 ], academic major [ 42 ] and living area [ 42 , 43 ] on anxiety and depression among college students, network structure invariance, edge invariance, and global strength were compared between different subgroups (e.g., between females and males, between health-related major and others, and between rural and urban residents) based on a permutation test ( n = 1000) [ 40 ].
Descriptive statistics
Out of the 3075 college students invited to participate, 3,062 agreed and completed the assessment, giving a response rate of 99.58%. Of the 3,062 college students included in this network, the mean age was 19.8 (standard deviation (SD) = 2.0) years, 2,068 (67.5%) were females, 1563 (51.0%) were rural residents, and 1722 (56.2%) majored in health-related subjects (Table S1 ). The mean PHQ-9 and GAD-7 rating score was 0.21 and 0.80, respectively (Table 1 ), and the distributions of the responses to PHQ-9/GAD-7 items are shown in Table S2 .
Network structure
The network of anxiety and depressive symptoms is shown in Fig. 1 and the corresponding partial correlation matric is presented in Table S3 . The edge Nervousness-Uncontrollable worry (GAD1-GAD2) shows the strongest association, followed by the edge Uncontrollable worry-Excessive worry (GAD2-GAD3), Excessive worry-Trouble relaxing (GAD3-GAD4), Restless-Feeling afraid (GAD5-GAD7), Sleep-Fatigue (PHQ3-PHQ4), Motor-Suicide (PHQ8-PHQ9), Anhedonia-Sad Mood (PHQ1-PHQ2), and Concentration-Motor (PHQ7-PHQ8).
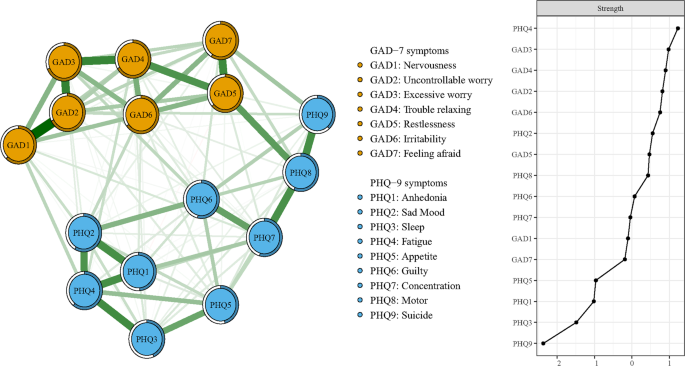
The left panel shows the visualization of the network structure; the right panel shows the value of strength in order.
In Table 1 and Fig. 1 , Fatigue (PHQ4) has the highest node strength in the anxiety and depression network among college students, followed by Excessive worry (GAD3), Trouble relaxing (GAD4), and Uncontrollable worry (GAD2). The item Excessive worry (GAD3) had the highest predictability in the network (Table 1 ) and an average of 56.3% of variance could be potentially accounted for by each node’s surrounding nodes ( M predictability = 0.563 ± 0.091). In terms of bridge symptoms, Motor (PHQ8) showed the highest bridge strength, followed by Feeling afraid (GAD7) and Restlessness (GAD5) (Fig. 2 ).
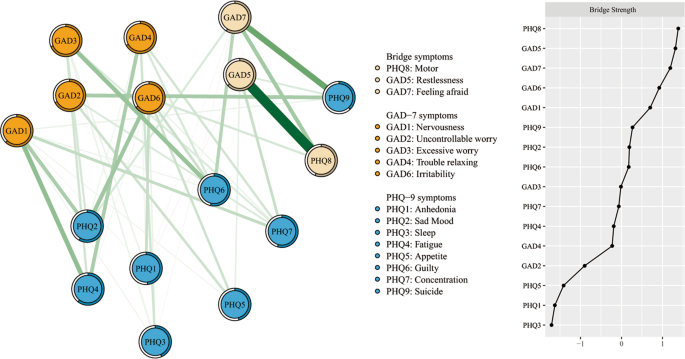
The left panel shows the visualization of the network structure of bridging symptoms; the right panel shows the value of bridge strength in order.
In Fig. 3 , the case-dropping bootstrap procedure shows that both CS-Cs of node strength and bridge strength were 0.75, which indicates that 75% of samples could be dropped, but the findings were still similar to the primary results ( r = 0.7). The results of nonparametric bootstrap procedure show that most comparisons among edge weights and node strength were statistically significant (Figs. S1 , S2 ). Additionally, bootstrapped 95% CIs were narrow, representing edges were trustworthy (Fig. S3 ).
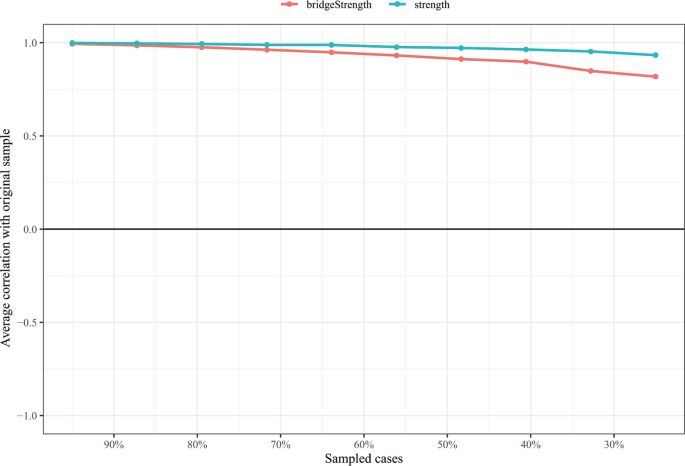
The x-axis indicates the percentage of cases of the original sample included at each step. The y-axis indicates the average of correlations between the centrality indices from the original network and the centrality indices from the networks that were re-estimated after excluding increasing percentages of cases.
Network comparisons
As shown in Fig. S4 , there was significant difference in network global strength (Urban: 7.655 vs Rural: 7.469, S = 0.186, p = 0.044) between rural and urban college students. In other two subsample comparisons, no significant differences were found in network global strength (Health-related major: 7.456 vs Other majors: 7.431, S = 0.025, p = 0.703; Females: 7.461 vs Males: 7.496, S = 0.035, p = 0.613). In terms of network structure and individual edge weight comparisons, there were also no significant differences between two networks in the three subsample comparisons.
To the best of our knowledge, this was the first study that characterized the depressive and anxiety network in Chinese college students during the late stage of the COVID-19 outbreak. All the strongest edges were within the respective disorder, while none of the strongest edges linked anxiety and depressive symptoms, which are consistent with previous findings identified in network analysis of depression and anxiety [ 15 , 20 , 21 ].
In the whole depression and anxiety network, all the top four strongest edges existed in the anxiety community, which are different from previous studies [ 15 , 20 ] where edges between depressive symptoms were the strongest in depression and anxiety network. This discrepancy may be due to different study samples; i.e., college students in this study vs. domestic workers in the Garabiles et al.’s study [ 20 ] and nursing students in the Ren et al.’s study [ 15 ]. The strongest edge in the whole depression and anxiety network was the connection between the “Nervousness” (GAD1) and “Uncontrollable worry” (GAD2), which could be due to the following reasons. Due to occasional small-scale outbreaks caused by imported cases from overseas, feelings of helplessness, fear, and apprehension were common stressors among college students [ 44 ]. Furthermore, classroom teaching may be interrupted at any time due to resurgence caused by imported cases from overseas. In switching to online learning, many college students are unable to adjust to online teaching [ 44 ], which may increase anxiety about the academic burden [ 45 ]. Apart from the influential edges within anxiety symptoms, several strong edges within depressive symptoms were observed. The edge between “Sleep” (PHQ3) and "Fatigue (PHQ4) is the strongest one, which was also the strongest edge in the depression and anxiety network study among nursing students [ 15 ]. This could be explained by the sudden change to sedentary lifestyle with reduced outdoor physical activities due to public health measures, resulting in increased fatigue [ 46 ]. Additionally, although sleep quantity could increase among the population during the lockdown, the sleep quality was often poorer [ 46 , 47 ], which could increase the risk of fatigue. Based on our findings, specific interventions that improve sleep quality and increase physical exercise may be helpful to alleviate depressive and anxiety problems.
Node index of strength may be crucial in identifying influential symptoms that activate and maintain psychopathological networks, and that are potential targets of interventions [ 15 , 39 ]. “Fatigue” (PHQ4) had the highest strength in the whole network, indicating its important role in the network of depression and anxiety. This is consistent with previous findings in nursing students [ 15 ], Filipino domestic workers [ 20 ], and patients with major depressive disorders [ 48 ]. Fatigue is common in students in the late stage of the COVID-19 outbreak, and a recent study found that the prevalence of fatigue was 67.3% (95% CI: 64.4–70.0%) in nursing students in this period [ 46 ]. Recent studies also found that fatigue in college students during the COVID-19 outbreak may be related to several factors including increased academic burden, inadequate physical activities, and poor sleep quality [ 15 , 44 , 46 , 47 ]. Moreover, compared with verbal expression, physical expression is often used as a coping strategy in Chinese societies, which may be associated with fatigue [ 15 ]. In this study, we found that certain anxiety symptoms, including “Excessive worry” (GAD3), “Trouble relaxing” (GAD4), and “Uncontrollable worry” (GAD2), also had high values of node strength, indicating these symptoms may also play important role in activating and maintaining the depression and anxiety network. This could be partly explained by the fear of contagion when students are faced with this novel and potentially fatal infectious disease, which can increase such anxiety symptoms [ 44 ]. Specific interventions could be adopted, such as cognitive behavioral therapy (CBT), applied relaxation and medications, the latter being considered for those with severe symptoms.
In this depression and anxiety network, the most influential bridge symptom was the depressive symptom of “Motor” (PHQ8), which is similar to that in a previous study in Chinese adults, where “Motor” (PHQ8) showed a high bridge centrality both during the COVID-19 peak and post-peak outbreak period [ 49 ]. In another study, the symptom of “Motor” was identified as the crucial priority due to its relation to “thought of death” in female nursing students [ 15 ], suggesting that this symptom should be a target of interventions to reduce depression and anxiety. Other influential bridge symptoms included the anxiety symptoms of “Feeling afraid” (GAD7) and “Restlessness” (GAD5), suggesting that these symptoms should also be targeted in treatment.
The predictability of each node in the network of depression and anxiety was calculated. There were no associations between predictability and mean values of each node ( r s = −0.056, p = 0.837), suggesting that certain symptoms might have a high value of predictability in the depressive and anxiety network, although these symptoms appeared less frequently [ 39 ]. On average, 56.3% of the node variance could be explained by neighboring nodes, implying that the potential sources of the remaining variance (e.g., stress and insomnia symptoms) were not included by both the PHQ-9 and GAD-7. Previous studies found that certain factors, such as gender, living area (urban/rural), and study major, were associated with depression and anxiety at the disorder level [ 41 , 42 , 43 ]. In this study, network comparison test found that compared to those from rural areas, students from urban areas had a significantly higher global strength of the network, indicating that individual symptoms in the model of urban college students were strongly inter-connected. This finding was not found in the relevant studies using network analysis and should be explored in future studies. In other comparisons (such as health-related major vs. other majors, and female vs male), no significant differences were found.
The strength of this study included the large sample size and use of the network approach to visualize depressive and anxiety symptom patterns in college students, with stable results. However, several limitations should be noted. First, the cross-sectional data collected by snowball sampling method were used to construct depressive and anxiety symptoms network structure, which could not identify the causality between individual symptoms and had limited representativeness. Therefore, the findings should be confirmed in future longitudinal studies. Second, self-reported measures were used to assess depressive and anxiety symptoms, which may have recall bias and are limited to capture clinical phenomena [ 15 ]. Third, for logistical reasons, depressive and anxiety network prior to and in the early stage of the COVID-19 pandemic were not assessed. Hence, the psychological impact of the pandemic could not be evaluated. Finally, some relevant symptoms, such as post-traumatic stress and certain somatic symptoms, were not measured, which could partly explain the relatively low predictability in the network.
In conclusion, centrality symptoms (i.e., “Fatigue”, “Excessive worry”, “Trouble relaxing” and “Uncontrollable worry”) and bridge symptoms (i.e., “Motor”, “Feeling afraid” and “Restlessness”) were identified in this network of depressive and anxiety symptoms in Chinese college students. Monitoring college students’ mental health in the late stage of the COVID-19 outbreak and targeting interventions (e.g., CBT, applied relaxation and medications) for selective symptoms are important to alleviate the overall level of anxiety and depression in this population.
Qin X, Wang S, Hsieh C-R. The prevalence of depression and depressive symptoms among adults in China: Estimation based on a National Household Survey. China Economic Rev. 2018;51:271–82. https://doi.org/10.1016/j.chieco.2016.04.001
Article Google Scholar
Jacobson NC, Newman MG. Anxiety and depression as bidirectional risk factors for one another: A meta-analysis of longitudinal studies. Psychol Bull. 2017;143:1155–1200. https://doi.org/10.1037/bul0000111
Article PubMed Google Scholar
Jenkins PE, Ducker I, Gooding R, James M, Rutter-Eley E. Anxiety and depression in a sample of UK college students: a study of prevalence, comorbidity, and quality of life. J Am Coll Health. 2020;1–7, https://doi.org/10.1080/07448481.2019.1709474 .
Zhao YJ, Jin Y, Rao WW, Li W, Zhao N, Cheung T, et al. The prevalence of psychiatric comorbidities during the SARS and COVID-19 epidemics: a systematic review and meta-analysis of observational studies. J Affect Disord. 2021;287:145–57. https://doi.org/10.1016/j.jad.2021.03.016
Article CAS PubMed PubMed Central Google Scholar
Kılınçel Ş, Kılınçel O, Muratdağı G, Aydın A, Usta MB. Factors affecting the anxiety levels of adolescents in home-quarantine during COVID-19 pandemic in Turkey. Asia Pac Psychiatry. 2021;13:e12406 https://doi.org/10.1111/appy.12406
Venugopal VC, Mohan A, Chennabasappa LK. Status of mental health and its associated factors among the general populace of India during COVID-19 pandemic. Asia Pac Psychiatry. 2020;e12412, https://doi.org/10.1111/appy.12412 .
Gu Y, Zhu Y, Xu F, Xi J, Xu G. Factors associated with mental health outcomes among patients with COVID-19 treated in the Fangcang shelter hospital in China. Asia Pac Psychiatry. 2021;13:e12443 https://doi.org/10.1111/appy.12443
Pan X, Xiao Y, Ren D, Xu ZM, Zhang Q, Yang LY, et al. Prevalence of mental health problems and associated risk factors among military healthcare workers in specialized COVID-19 hospitals in Wuhan, China: a cross-sectional survey. Asia Pac Psychiatry. 2020;e12427, https://doi.org/10.1111/appy.12427 .
Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395:e37–e38. https://doi.org/10.1016/s0140-6736(20)30309-3
Auerbach RP, Mortier P, Bruffaerts R, Alonso J, Benjet C, Cuijpers P, et al. WHO World Mental Health Surveys International College Student Project: Prevalence and distribution of mental disorders. J Abnorm Psychol. 2018;127:623–38. https://doi.org/10.1037/abn0000362
Article PubMed PubMed Central Google Scholar
Yu M, Tian F, Cui Q, Wu H. Prevalence and its associated factors of depressive symptoms among Chinese college students during the COVID-19 pandemic. BMC Psychiatry. 2021;21:66 https://doi.org/10.1186/s12888-021-03066-9
Li Y, Zhao J, Ma Z, McReynolds LS, Lin D, Chen Z, et al. Mental health among college students during the COVID-19 pandemic in China: a 2-Wave Longitudinal Survey. J Affect Disord. 2021;281:597–604. https://doi.org/10.1016/j.jad.2020.11.109
Article CAS PubMed Google Scholar
Borsboom D. A network theory of mental disorders. World Psychiatry. 2017;16:5–13. https://doi.org/10.1002/wps.20375
Hofmann SG, Curtiss J, McNally RJ. A complex network perspective on clinical science. Perspect Psychol Sci. 2016;11:597–605. https://doi.org/10.1177/1745691616639283
Ren L, Wang Y, Wu L, Wei Z, Cui LB, Wei X, et al. Network structure of depression and anxiety symptoms in Chinese female nursing students. BMC Psychiatry. 2021;21:279 https://doi.org/10.1186/s12888-021-03276-1
Epskamp S, CramerAOJ, Waldorp LJ, Schmittmann VD, Borsboom D. qgraph: network visualizations of relationships in psychometric data. J Statistical Softw. 2012;48:1.
Contreras A, Nieto I, Valiente C, Espinosa R, Vazquez C. The study of psychopathology from the network analysis perspective: a systematic review. Psychother Psychosom. 2019;88:71–83. https://doi.org/10.1159/000497425
Haslbeck JMB, Fried EI. How predictable are symptoms in psychopathological networks? A reanalysis of 18 published datasets. Psychol Med. 2017;47:2767–76. https://doi.org/10.1017/s0033291717001258
Jones PJ, Ma R, McNally RJ. Bridge centrality: a network approach to understanding comorbidity. Multivariate Behavior Res 2019;1–15, https://doi.org/10.1080/00273171.2019.1614898 .
Garabiles MR, Lao CK, Xiong Y, Hall BJ. Exploring comorbidity between anxiety and depression among migrant Filipino domestic workers: a network approach. J Affect Disord. 2019;250:85–93. https://doi.org/10.1016/j.jad.2019.02.062
Beard C, Millner AJ, Forgeard MJC, Fried EI, Hsu KJ, Treadway MT, et al. Network analysis of depression and anxiety symptom relationships in a psychiatric sample. Psychological Med. 2016;46:3359–69. https://doi.org/10.1017/S0033291716002300
Article CAS Google Scholar
Compton WM, Conway KP, Stinson FS, Grant BF. Changes in the prevalence of major depression and comorbid substance use disorders in the United States between 1991-1992 and 2001-2002. Am J Psychiatry. 2006;163:2141–7. https://doi.org/10.1176/ajp.2006.163.12.2141
Kleinman A. Culture and depression. N Engl J Med. 2004;351:951–3. https://doi.org/10.1056/NEJMp048078
Bai W, Cai H, Liu S, Liu H, Qi H, Chen X, et al. Attitudes toward COVID-19 vaccines in Chinese college students. Int J Biol Sci. 2021;17:1469–75. https://doi.org/10.7150/ijbs.58835
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Wang W, Bian Q, Zhao Y, Li X, Wang W, Du J, et al. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hospital Psychiatry. 2014;36:539–44. https://doi.org/10.1016/j.genhosppsych.2014.05.021
Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–7. https://doi.org/10.1001/archinte.166.10.1092
He XY, Li CB, Qian J, Cui HS, Wu WY. Reliability and validity of a generalized anxiety disorder scale in general hospital outpatients (in Chinese). Shanghai Arch Psychiatry. 2010;22:200–203.
R Core Team. R: A language and environment for statistical computing. 2020; https://www.R-project.org/ .
Tibshirani R. Regression shrinkage and selection via the lasso. J R Stat Soc: Ser B (Methodol). 1996;58:267–88.
Google Scholar
Haslbeck JMB, Waldorp LJ. How well do network models predict observations? On the importance of predictability in network models. Behav Res Methods. 2018;50:853–61. https://doi.org/10.3758/s13428-017-0910-x
Liu H, Han F, Yuan M, Lafferty J, Wasserman L. High-dimensional semiparametric Gaussian copula graphical models. Ann Stat. 2012;40:2293–326. 2234
Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res methods. 2018;50:195–212. https://doi.org/10.3758/s13428-017-0862-1
Opsahl T, Agneessens F, Skvoretz J. Node centrality in weighted networks: generalizing degree and shortest paths. Soc Netw. 2010;32:245–51. https://doi.org/10.1016/j.socnet.2010.03.006
Bringmann LF, Elmer T, Epskamp S, Krause RW, Schoch D, Wichers M, et al. What do centrality measures measure in psychological networks? J Abnorm Psychol. 2019;128:892–903. https://doi.org/10.1037/abn0000446
Epskamp S, Rhemtulla M, Borsboom D. Generalized network psychometrics: combining network and latent variable models. Psychometrika. 2017;82:904–27. https://doi.org/10.1007/s11336-017-9557-x
Haslbeck JMB, Waldorp LJ. mgm: estimating time-varying mixed graphical models in high-dimensional data. J Statistical Softw. 2020;93:1–46.
Payton J. Tools for identifying important nodes in networks. https://cran.r-project.org/web/packages/networktools/index.html .
Marchetti I. Hopelessness: a network analysis. Cogn Ther Res. 2019;43:611–9. https://doi.org/10.1007/s10608-018-9981-y
van Borkulo CD, Boschloo L, Kossakowski JJ, Tio P, Schoevers RA, Borsboom D, et al. Comparing network structures on three aspects: apermutation test. 2017; https://doi.org/10.13140/RG.2.2.29455.38569 .
Gao W, Ping S, Liu X. Gender differences in depression, anxiety, and stress among college students: A longitudinal study from China. J Affect Disord. 2020;263:292–300. https://doi.org/10.1016/j.jad.2019.11.121
Chang J, Yuan Y, Wang D. [Mental health status and its influencing factors among college students during the epidemic of COVID-19]. Nan fang yi ke da xue xue bao = J Southern Med Univ. 2020;40:171–6. https://doi.org/10.12122/j.issn.1673-4254.2020.02.06 .
Liu Y, Yue S, Hu X, Zhu J, Wu Z, Wang J, et al. Associations between feelings/behaviors during COVID-19 pandemic lockdown and depression/anxiety after lockdown in a sample of Chinese children and adolescents. J Affect Disord. 2021;284:98–103. https://doi.org/10.1016/j.jad.2021.02.001
Yang C, Chen A, Chen Y. College students’ stress and health in the COVID-19 pandemic: The role of academic workload, separation from school, and fears of contagion. PLoS ONE. 2021;16:e0246676 https://doi.org/10.1371/journal.pone.0246676
Hasan N, Bao Y. Impact of “e-Learning crack-up” perception on psychological distress among college students during COVID-19 pandemic: a mediating role of “fear of academic year loss”. Child Youth Serv Rev. 2020;118:105355–105355. https://doi.org/10.1016/j.childyouth.2020.105355
Liu S, Xi HT, Zhu QQ, Ji M, Zhang H, Yang BX, et al. The prevalence of fatigue among Chinese nursing students in post-COVID-19 era. PeerJ. 2021;9:e11154 https://doi.org/10.7717/peerj.11154
Benham G. Stress and sleep in college students prior to and during the COVID-19 pandemic. Stress Health. 2020; https://doi.org/10.1002/smi.3016 .
Park SC, Kim D. The centrality of depression and anxiety symptoms in major depressive disorder determined using a network analysis. J Affect Disord. 2020;271:19–26. https://doi.org/10.1016/j.jad.2020.03.078
Wang Y, Hu Z, Feng Y, Wilson A, Chen R. Changes in network centrality of psychopathology symptoms between the COVID-19 outbreak and after peak. Mol Psychiatry. 2020;25:3140–9. https://doi.org/10.1038/s41380-020-00881-6
Download references
Acknowledgements
The study was supported by the National Science and Technology Major Project for investigational new drug (2018ZX09201-014), the Beijing Municipal Science & Technology Commission (No. Z181100001518005), the University of Macau (MYRG2019-00066-FHS), and Beijing Municipal Administration of Hospitals Incubating Program (PX2018063).
Author contributions
Study design: WB, SS, YTX. Data collection, analysis and interpretation: WB, HC, XC, SL, SS. Drafting of the manuscript: WB, SS, YTX. Critical revision of the manuscript: TC, JL, XC, CHN, YTX. Approval of the final version for publication: all co-authors.
Author information
These authors contributed equally: Wei Bai, Hong Cai, Shou Liu, Xu Chen
Authors and Affiliations
Unit of Psychiatry, Department of Public Health and Medicinal Administration, & Institute of Translational Medicine, Faculty of Health Sciences, University of Macau, Macao, SAR, China
Wei Bai, Hong Cai & Yu-Tao Xiang
Centre for Cognitive and Brain Sciences, University of Macau, Macao, SAR, China
Institute of Advanced Studies in Humanities and Social Sciences, University of Macau, Macao, SAR, China
Department of Public Health, Medical College, Qinghai University, Xining, Qinghai Province, China
The National Clinical Research Center for Mental Disorders & Beijing Key Laboratory of Mental Disorders, Beijing Anding Hospital & the Advanced Innovation Center for Human Brain Protection, Capital Medical University, Beijing, China
Xu Chen & Sha Sha
School of Nursing, Hong Kong Polytechnic University, Hong Kong, SAR, China
Teris Cheung
Department of Rehabilitation Sciences, & Mental Health Research Centre, Hong Kong Polytechnic University, Hong Kong, SAR, China
Jessie Jingxia Lin
Department of Business Administration, Hong Kong Shue Yan University, Hong Kong, China
Department of Psychiatry, The Melbourne Clinic and St Vincent’s Hospital, University of Melbourne, Richmond, Victoria, Australia
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Sha Sha .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary material, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Bai, W., Cai, H., Liu, S. et al. Anxiety and depressive symptoms in college students during the late stage of the COVID-19 outbreak: a network approach. Transl Psychiatry 11 , 638 (2021). https://doi.org/10.1038/s41398-021-01738-4
Download citation
Received : 08 August 2021
Revised : 23 October 2021
Accepted : 28 October 2021
Published : 17 December 2021
DOI : https://doi.org/10.1038/s41398-021-01738-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Temporal network of experience sampling methodology identifies sleep disturbance as a central symptom in generalized anxiety disorder.
BMC Psychiatry (2024)
A network model of depressive and anxiety symptoms: a statistical evaluation
- Meng-Yi Chen
- Yu-Tao Xiang
Molecular Psychiatry (2024)
Network analysis of comorbid depression and anxiety and their associations with response style among adolescents with subthreshold depression
- Tingting Wang
Current Psychology (2024)
Changes in Mental Health and EEG Biomarkers of Undergraduates Under Different Patterns of Mindfulness
- Miaoling Luo
- Zhuangfei Chen
Brain Topography (2024)
Anxiety and Depression Symptoms among Youth Survivors of Childhood Sexual Abuse: A Network Analysis
- Yuanyuan Wang
BMC Psychology (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Open access
- Published: 11 November 2022
The relationship between depression symptoms and academic performance among first-year undergraduate students at a South African university: a cross-sectional study
- F Wagner 1 ,
- RG Wagner 2 ,
- U Kolanisi 3 ,
- LP Makuapane 1 ,
- M Masango 4 &
- FX Gómez-Olivé 2
BMC Public Health volume 22 , Article number: 2067 ( 2022 ) Cite this article
12k Accesses
11 Citations
2 Altmetric
Metrics details
Background:
South African universities face a challenge of low throughput rates, with most students failing to complete their studies within the minimum regulatory time. Literature has begun to investigate the contribution of well-being, including mental health, with depression among students being one of the most common mental disorders explored. However, locally relevant research exploring associations between depression and academic performance has been limited. This research hypothesizes that the presence of depression symptoms, when controlling for key socio-demographic factors, has an adverse impact on student academic outcomes and contributes to the delay in the academic progression of students.
The study used a cross-sectional design. Data were collected in 2019 from first-time, first-year undergraduate students using a self-administered online questionnaire. In total, 1,642 students completed the survey. The Patient Health Questionnaire-9 (PHQ-9) was used to screen for depression symptoms. Data on students’ academic performance were obtained from institutional records. Bivariate and multivariate regression analyses were used to examine associations between depression symptoms and academic performance.
Most participants (76%) successfully progressed (meeting the requirements to proceed to the second year of university study). Of the participants, 10% displayed symptoms of severe depression. The likelihood of progression delay (not meeting the academic requirements to proceed to the second year of university study) increased with the severity of depression symptoms. Moderate depression symptoms nearly doubled the adjusted odds of progression delay (aOR = 1.98, 95% CI: 1.30-3.00, p = 0.001). The likelihood of progression delay was nearly tripled by moderate severe depression symptoms (aOR = 2.70, 95% CI:1.70–4.36, p < 0.001) and severe depression symptoms (aOR = 2.59, 95% CI:1.54–4.36, p < 0.001). The model controlled for field of study, financial aid support as well as sex and race.
Conclusion:
Higher levels of depression symptoms among first-year university students are associated with a greater likelihood of progression delay and may contribute to the low throughput rates currently seen in South African universities. It is important for students, universities and government departments to recognize student mental wellness needs and how these can be met.
Peer Review reports
Mental illness is a public health priority, affecting as much as 47% of the population at some point in their lifetime [ 1 ]. Literature has identified university students as a group that is particularly vulnerable to mental illness [ 2 , 3 , 4 , 5 , 6 ]. A review on depression among university students reported that depression prevalence ranged between 6 and 54% among university students [ 6 ]. Depression is a disorder that can affect one’s overall functioning. Symptoms of depression can often include a lack of a positive outlook, high levels of anxiety, irregular sleeping patterns and reduced concentration [ 4 , 7 ]. The high prevalence of depression among university students is concerning and justifies a need to understand how depression and academic success in this population may be associated.
There is no agreed-upon definition for academic success or failure, but there is consensus that, traditionally, student academic success is represented by student retention, progression and improved throughput; while academic failure can be described as the lack of retention, progression or throughput [ 8 , 9 , 10 ]. In the South African context, universities are faced with low throughput rates, meaning that only a small percentage of students obtain their qualifications within the minimum stipulated times. This is largely due to progression delay, a consequence of students not meeting the academic requirements to progress from one academic year to the next [ 9 ]. These delays in progression are particularly significant in the South African context, where more than half of the population lives in poverty and most young people are unemployed [ 11 , 12 ]. In this context, unemployment is lowest among those with tertiary qualifications [ 12 ] and thus delays in acquiring qualifications can be devasting for students coming from poor homes, who are often expected to support their families financially upon graduation. It is therefore imperative that university student success is prioritised.
Several studies have explored factors and determinants of throughput and student success [ 13 , 14 , 15 , 16 ]. These studies found that the determinants of student success are complex, identifying high school academic achievement [ 13 , 17 ], family background [ 15 ] and the students’ ability to integrate into the different aspects of university life, including social communities and teaching and learning [ 14 ] as key determinants of academic success.
In addition to these traditional determinants, research has begun to explore the contribution of well-being, including mental health, as a potential contributor to student academic performance. This emerging research suggests that university students suffering from common mental disorders, especially anxiety and depression, are likely to perform poorly when compared to students without mental disorders [ 2 , 3 , 18 ]. A study among university students in the United States of America (USA), found that depression was not only linked to a lower grade point average (GPA), but also an increased likelihood of attrition [ 2 ]. Findings from a longitudinal cohort study in the United Arab Emirates (UAE) found that higher levels of depression predicted lower GPA scores both at baseline and follow-up [ 19 ]. Work carried out in South Africa found that students with major depressive disorder as well as those with attention deficit hyperactivity disorder (ADHD) had a higher probability of academic failure [ 3 ]. Research conducted in Australian universities found students often attributed their academic failure to poor mental health, including conditions such as anxiety and depression [ 20 ]. Evidence from students in Nigeria found depression to be inversely linked to perceived poor academic performance [ 21 ].
South African literature on depression and associations between depression and academic failure among university students has started to emerge [ 3 , 22 , 23 ]. However, findings from these studies have been based predominantly on White study participants, making it difficult to generalize these findings to more heterogenous student populations since White students are in minority in the South African higher education sector. Given this, the current research aims to close this knowledge gap while considering other important factors, such as financial aid and field of study, which may impact on progression delay. We hypothesize that the presence of depression symptoms has adverse effects on student academic outcomes and contributes to progression delay in a diverse South African university student population. The main aim of the current study was therefore to investigate the extent to which depression symptoms, when controlling for key demographic and socio-economic factors, predicted student progression delay.
The current study took place in a large research-intensive South African university. In 2019, the headcount student enrolment was around 41,000, with international students making up 9% of the student population. Female students made up 55% of the student population, and the majority of South African students attending the university were Black African (61%). The student population is culturally diverse, with the university having three official languages, English, IsiZulu and Sesotho.
The current research targeted the entire cohort of 2019 first-time, first-year undergraduate students (n = 5,912). The inclusion criteria to participate in this research, which was used to extract the sample, was as follows: being 18 years of age or older; being a first-time, first-year undergraduate student; studying full-time; completion of the Biographic Questionnaire [ 16 ], which is a baseline survey at intake; pursuing either a professional bachelor’s degree (a programme that is generally four years or longer) or a general bachelor’s degree (generally a three-year programme); and being assigned progress codes at the end of the 2019 academic year. All students provided informed consent prior to participating in the study. Students not meeting the inclusion criteria were excluded.
All students meeting the inclusion criteria were invited to participate in the study (n = 5,195). Students could only complete the survey once they had given informed consent. A total of 1,648 participants (32%) completed the survey. Six participants were not assigned progress codes at the end of the 2019 academic year, the possible reasons for this include students deregistering or awaiting the outcome of appeals. The six records were removed from the analysis, leaving a total analysis sample of 1,642 participants.
A comparison between study participants and those who did not participate in the study (non-participants) (Table 1 ) shows that non-participants were significantly older (X 2 (2, N = 5 195) = 14.95, p = 0.001), more likely to be male ((45% vs. 37%); X 2 (1, N = 5 195) = 32.31, p < 0.001), less likely to be Black African ((64% vs. 72%); X 2 (5, N = 5 195) = 28.87, p < 0.001), and were significantly more likely not to be receiving financial aid ((59% vs. 51%); X 2 (1, N = 5 195) = 27.17, p < 0.001). The participant group was significantly more likely to be from high school quintiles 1–4, and significantly more likely to be first-generation students ((47% vs. 53%); X 2 (1, N = 5 195) = 15.91, p < 0.001). There were no differences in disability status or field of study.
In the analysis sample (Table 1 ) most study participants were female (63%), Black African (72%), between the ages of 18 and 39 (median 19 years), non-first-generation students (53%), attended high school quintile 5 (33%) and reported having no special needs (98%).
Instruments
the Patient Health Questionnaire-9 (PHQ-9) was used to screen for depression symptoms using a two-week recall period [ 24 ]. The PHQ-9 has been validated and determined to give accurate accounts of the prevalence of depression symptoms [ 25 ]. Responses to each of the questionnaire items were rated on a four-point Likert scale, ranging from 0 (not at all) to 3 (nearly every day) [ 25 ]. Participants’ responses were summed and designated to one of five categories for the PHQ-9 (that is a PHQ-9 score of 0–4 denoting minimal depression symptoms; 5–9 denoting mild depression symptoms, 10–14 denoting moderate depression symptoms, 15–19 denoting moderate-severe depression symptoms, and 20–27 denoting severe depression symptoms), these categories have been used in other studies [ 26 ].
Covariates potentially influencing academic performance associations were identified in literature and included in the models. These covariates included: race (coded as Black African, Chinese, Coloured, Indian, White or Unknown), sex (coded as male or female), first-generation status (coded as 1st generation student for those first in their family to go to university), and 2nd generation or more (coded for those with family members who had attended university). A self-reported account of disability status was also included (coded as ‘yes’ for participants with self-reported disabilities and/or special needs, or ‘no’ for participants with no disabilities and/or special needs). Other covariates included field of study (coded as Commerce, Law and Management, Engineering, Health Sciences, Humanities, or Science), and financial aid from the National Student Financial Aid Scheme (NSFAS) (coded as ‘yes’, for those who were funded, or ‘no’ for those who did not receive funding).
Anxiety symptoms were measured using the GAD-7 questionnaire [ 27 ] which is a seven-item tool used to screen for anxiety symptoms. Like the PHQ-9, the GAD-7 uses a two-week recall period. Responses to each of the questionnaire items were rated on a four-point Likert scale, ranging from 0 (not at all) to 3 (nearly every day). Participants’ responses were summed and designated to one of four categories for the GAD-7 (with severity scores as follows: a score of 0–4 denoting minimal anxiety, 5–9 denoting mild anxiety, 10–14 denoting moderate anxiety and 15–21 denoting severe anxiety), these categories have been used in other studies [ 26 , 27 ].
Students’ main source of general support was also included as a variable from the question: While you are at university, who will be providing you with general support? Participants had the following response options: Both parents, Single parents, Grandparent(s) or, Guardian(s), Other family and/or friends(s), Spouse/ partner, No support. General support, in this instance, means the support given to students in general, without any particular sub-divisions.
High school socio-economic quintile was also included. South African public schools are allocated quintile categories to reflect the socio-economic status of communities surrounding the schools. Quintile 1 represents the poorest communities and quintile 5 the wealthiest [ 17 ]. In addition to the high school quintiles 1–5, was the category ‘other’. The ‘other’ category included participants from non-public high schools (private and international high schools).
Academic performance
progress codes assigned to each student at the end of the academic year were dichotomized as (i) those meeting the requirements to proceed to the second academic year of study (successful progression) and (ii) those who did not meet the academic requirements to proceed to the second year of study (progression delay). This definition has been previously used to define academic success (here defined as ‘successful progression’) and academic failure (here defined as ‘progression delay’) in similar work in South Africa [ 3 , 28 ].
Following ethics approval, as well as written permission from the university registrar, all first-time, first-year undergraduate student email addresses were extracted from the university database using the inclusion criteria stated above. Students were then invited to participate in the study via an email with a unique link to the survey. Students could only complete the survey after consenting (by clicking that they consented to take part in the study). Data collection, which took place over six weeks between July and August 2019, was in the form of a self-administered online questionnaire, which was hosted on the Research Electronic Data Capture (REDCap) web application [ 29 ]. Academic performance data (for the 2019 academic year) were requested from the university for students who completed the survey, this performance data was then linked to survey data.
Data analysis
Data were cleaned and analyzed using STATA (version 14; College Station, Texas, USA). Frequency and descriptive analyses were performed for demographic and mental health variables. Categorical variables were reported using percentages and continuous variables were reported using the median and interquartile ranges (IQR). The Mann-Whitney U test was used to compare continuous variables, while the chi-square test was used to compare categorical variables with student progression. Variables included in the logistic regression model, which used adjusted odds ratios (aOR) as a test statistic, were selected using a forwards and backwards stepwise regression, with a cut-off of p \(\le\) 0.20 used for inclusion in the model. Significance was defined at an p-value \(<\) 0.05 level in all analyses.
As shown in Table 2 , a total of 76% of students progressed successfully, while 24% experienced progression delay. A higher proportion of male students (31%) experienced progression delay, compared to female students (21%). Black African students and students from quintile 1 high schools had the highest proportion of progression delay at 27% and 33% in their respective groupings. In terms of field of study, students registered for programmes in the humanities had the lowest proportion of progression delay at 11%. There were significant differences between progression delay in the distribution by sex (X 2 (1, N = 1 642) = 20.07, p < 0.001), race (X 2 (5, N = 1 642) = 23.06, p < 0.001), high school quintile (X 2 (5, N = 1 642) = 34.89, p < 0.001) and field of study (X 2 (4, N = 1 642) = 228.20, p < 0.001).
In terms of mental health, the prevalence of severe anxiety symptoms was found to be 18% and severe depression symptoms was 10%. As shown in (Table 3 ) 29% of participants with severe anxiety symptoms experienced progression delay and 30% of participants with severe depression symptoms experienced progression delay. Finally, 27% of participants who listed having no general support experienced progression delay. The bivariate analysis indicated a high correlation between depression (X 2 (4, N = 1 642) = 22.79, p < 0.001), anxiety symptoms (X 2 (3, N = 1 642) = 12.25, p = 0.007) and progression.
The multivariate logistic regression (Table 4 ) showed that being enrolled in the Engineering field of study increased the likelihood of progression delay more than nine-fold (adjusted odds ratio (aOR) = 9.33, 95% CI: 6.35–13.72, p < 0.001) and of Science more than four-fold (aOR = 4.23, 95% CI: 2.88–6.22, p < 0.001). Furthermore, experiencing moderate depression symptoms increased the adjusted odds of progression delay almost two-fold (aOR = 1.98, 95% CI: 1.30-3.00, p = 0.001), while moderate severe symptoms of depression increased the likelihood of progression delay almost three-fold (aOR = 2.70, 95% CI:1.70–4.30, p < 0.001). Severe depression symptoms also increased the odds of progression delay almost three-fold (aOR = 2.59, 95% CI:1.54–4.35, p < 0.001). An increase in the severity of depression symptoms was also found to lead to a higher likelihood of progression delay. Anxiety symptoms did not meet the threshold to be included in the final model.
Two variables, high school quintile (quintile 5 and other) and receiving financial aid from the National Student Financial Aid Scheme (NSFAS), decreased the odds of progression delay. Participants who completed Grade 12 in well-resourced high schools (high school quintile 5), and those whose high school was classified as ‘Other’ (private and international high schools) were also significantly less likely to experience progression delay (aOR = 0.50, 95% CI:0.30–0.85, p = 0.01) and (aOR = 0.47, 95% CI:0.26–0.83, p = 0.009), respectively. Participants who received financial aid support from the NSFAS were also significantly less likely to experience progression delay (aOR = 0.67, 95% CI:0.26–0.83, p = 0.007).
The prevalence of severe anxiety symptoms was 18% and severe depression symptoms was 10%, when using standardized tools. These findings on anxiety and depression corroborate a recent South African study that found a 21% prevalence of generalized anxiety disorder and 14% prevalence of major depressive disorder among first-year university students when using a 12-month recall [ 3 ]. Findings from international literature vary with studies reporting depression and anxiety levels as high as 54% and 66%, respectively [ 6 ]. It is important to stress that the current study presents findings for anxiety and depression symptoms and not major depressive disorder or generalised anxiety disorder.
Findings from our study suggest that depression symptoms are predictive of progression delay, confirming the hypothesis underpinning this study. In fact, results indicate that moderate depression symptoms increased the odds of progression delay almost two-fold and that moderate severe and severe depression symptoms increased the adjusted odds of progression delay by three-fold. These findings align with both South African literature, which found that students experiencing major depressive disorder were almost four times more likely to perform poorly [ 3 ] and international literature from the USA and the UAE which associated low GPA scores with depression [ 18 , 19 ]. Anxiety symptoms were not significant in their association with progression delay in the logistic regression, also a common finding [ 19 , 30 , 31 ].
Common mental disorders may affect academic performance in a number of ways. One way is class attendance, which is an important contributor to academic success [ 30 ]. Evidence from universities in Australia and Jordan found that students experiencing common mental disorders, including depression, on average had higher levels of class absenteeism compared to students not experiencing mental disorders [ 20 , 32 ]. In their work, Eisenberg et al., (2009) conceptualize the impact of poor mental health on academic performance. In it they emphasize the potential impact of mental illness, including depression, in the acquisition of cognitive skills [ 2 ]. Depression symptoms, such as having low energy and difficulty concentrating [ 2 , 7 , 30 ], impact on non-cognitive skills that include persistence and motivation, which have a direct effect on cognitive function and thus the acquirement of knowledge. The presence of depression impacts on these non-cognitive skills resulting in low academic productivity, leading to potentially lower skill acquisition as reflected by lower scores [ 2 ].
It is also important to note the potential bi-directionality of the above trend. It is plausible that academic failure, including progression delay, may increase the risk of depression symptoms [ 2 ]. Other literature investigating depression, academic achievement and absenteeism, has acknowledged this [ 32 ]. Furthermore, findings from Nigeria, for instance, report that students experiencing academic failure often report feelings of anger, shame, disappointment and hopelessness [ 33 , 34 ]. Research has also highlighted the compounding effects of academic failure, including the additional financial stress of having to re-register and also the time commitment due to increased workloads, all which can have significant implications on mental health [ 34 ].
The current research also found that 24% of the first-time, first-year undergraduate university students experienced progression delay during a single year at a large South African tertiary institution. These levels are consistent with findings from a similar study which found academic failure to be 26% among first-year South African university students in the Western Cape province [ 3 ]. These findings are difficult to compare with international literature that typically measures academic performance using GPA. In terms of student success, variables such as sex, race, high school quintile and field of study have been well documented as predictors of academic success [ 13 , 17 , 35 ] and in the current research, these were also found to significantly impact academic performance. The results of our study on sex and race are supported by other research findings, both in South Africa and internationally, which indicate that female students often outperform their male counterparts [ 3 , 30 ], and that White students often attain the highest academic scores [ 13 , 30 ].
The results indicated that financial aid (NSFAS) as well as attending well-resourced high schools (quintile 5 and other) protected against progression delay. These findings are in line with literature that has demonstrated that students from well-resourced schools perform better academically than students from poorer schools [ 17 ]. Furthermore, studies have found that students with a financial need who receive financial aid were more likely to be academically successful when compared to their counterparts without any state funding [ 15 , 36 ].
Students registered in the field of study of Engineering had a probability of progression delay nine times higher than Humanities where 89% of students successfully progressed, while students registered in the Science field had an increased likelihood of progression delay by a factor of four. These findings correspond with previous research that suggests that students enrolled in science, technology, engineering and mathematics (STEM) fields, across institutions, grapple with the curriculum [ 37 ]. In fact, although enrolment in the STEM field have increased over time in South Africa, they account for the lowest university success and graduation rates [ 38 ].
Our findings highlight the important relationship between student mental health and academic progression, suggesting that student mental health should be recognized as a critical component of academic performance at universities. As such, universities should consider making provisions for mental wellness resources on campus, and build institutional cultures that promote mental wellness. However, mental health is a public health issue, and it is unreasonable to expect universities to be the sole drivers of change. We believe that the student voice is essential to reconciling the roles of both universities and the health care system in improving student academic performance.
We present original findings from a study involving first-time, first-year undergraduate students at a large South African university. Although the generalizability of the findings may be limited, our data builds on a growing body of literature demonstrating the negative impact that depression symptoms have on student academic performance, through delayed student progression and ultimately potentially low student throughput rates. It is important for students, universities as well as government departments to recognize the impact of mental health on student performance and work together to identify student’s mental health needs and how these can be met. Holistic student support programmes offered by universities should work towards fully incorporating student mental wellness activities. The current study has a number of strengths, including: a large study population; being carried out at an institution with a diverse student population; and experiencing a high response rate (32%) when compared to similar studies. To our knowledge, this is one of the largest studies, in terms of the sample size and response rate, on the African continent to explore the relationship between depression symptoms and academic performance. Studies using similar methodological approaches typically achieve response rates between 8 and 13% [ 3 , 22 , 23 ].
However, a number of limitations should also be considered when interpretating the results. The PHQ-9 is used as a screening tool for depression symptoms and is not a diagnostic clinical tool. The PHQ-9 has, however, been validated and determined to give accurate accounts of the prevalence of depression [ 25 ]. The current study was carried out at a single university, with differences delineated between study participants and non-participants, which limits the generalizability of the current findings. Furthermore, bias could have been introduced due to self-selected sampling. Finally, the cross-sectional nature of the study limits establishment of causality.
The students who participated in the current study have subsequently been invited to participate in similar research during the initial COVID-19 pandemic years (2020–2021) and the first “post-COVID-19 year” (2022). This follow-up study will help us understand the impact of the COVID-19 pandemic on the mental health of these South African students.
Data availability
The data that support the findings of this study are available from the University Registrar of the University of the Witwatersrand, Johannesburg, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the corresponding author upon reasonable request and with permission of the University Registrar of the University of the Witwatersrand, Johannesburg.
Kessler RC. The Prevalence of Mental Illness. In: Teresa L, Scheid TN, Brown, editors. A Handbook for the Study of Mental Health. Second Edi. Cambridge: Cambridge University Press; 2009. pp. 1–736.
Google Scholar
Eisenberg D, Golberstein E, Hunt JB. Mental Health and Academic Success in College. BE Journal of Economic Analysis and Policy. 2009;9.
Bantjes J, Saal W, Gericke F, Lochner C, Roos J, Auerbach RP, et al. Mental Health and Academic Failure Among First-year University Students in South Africa. South African Journal of Psychology. 2020;51.
Nsereko ND. Proliferation of university institutions in Africa: Student Academic Life and Mental Health Challenges. European Journal of Counselling Theory. 2018;2.
Schreiber B. Mental Health at Universities: Universities are Not In Loco Parentis – Students are Active Partners in Mental Health. J Student Affairs Afr. 2018;6:121–7.
Liu X-Q, Guo Y-X, Zhang W-J, Gao W-J. Influencing factors, prediction and prevention of depression in college students: A literature review. World J Psychiatry. 2022;12:860–73.
Article PubMed PubMed Central CAS Google Scholar
Bernal-Morales B, Rodríguez-Landa JF, Pulido-Criollo F. Impact of Anxiety and Depression Symptoms on Scholar Performance in High School and University Students. A Fresh Look at Anxiety Disorders. 2015. https://doi.org/10.5772/60711 .
Cele N. Big data-driven early alert systems as means of enhancing university student retention and success. South Afr J High Educ. 2021;35:56–72.
DHET (SA). Statistics on Post-School Education and Training in South Africa: 2019. Pretoria; 2021.
RSA Presidency. Twenty Year Review South Africa 1994–2014. 2014;:1–175. https://rb.gy/3wxqmq . Accessed 22 Mar 2022.
Stats SA. Poverty Trends in South Africa An examination of absolute poverty between 2006 and 2015. Pretoria; 2017.
Stats SA. Quarterly Labour Force Survey; Quarter 4:2021. Pretoria; 2022.
Bokana KG, Tewari DD. Determinants of Student Success at a South African University: An Econometric Analysis. Anthropologist. 2014;17:259–77.
Article Google Scholar
Schwartz S, Tinto V. Leaving College: Rethinking the Causes and Cures of Student Attrition. Academe. 1987;73:46.
Kuh GD, Kinzie J, Buckley JA, Bridges BK, Hayek JC. What Matters to Student Success: A Review of the Literature Commissioned Report for the National Symposium on Postsecondary Student Success: Spearheading a Dialog on Student Success. 2006.
Masango M, Muloiwa T, Wagner F, Pinheiro G. Design and Implementation of a Student Biographical Questionnaire (BQ) Online Platform for Effective Student Success. J Student Affairs Afr. 2020;8:93–110.
Burger A, Naudé L. Predictors of Academic Success in the Entry and Integration Stages of Students’. Acad Careers. 2019;22:743–55.
Fröjd SA, Nissinen ES, Pelkonen MUI, Marttunen MJ, Koivisto AM, Kaltiala-Heino R. Depression and School Performance in Middle Adolescent Boys and Girls. J Adolesc. 2008;31:485–98.
Article PubMed Google Scholar
Awadalla S, Davies EB, Glazebrook C. A longitudinal cohort study to explore the relationship between depression, anxiety and academic performance among Emirati university students. BMC Psychiatry. 2020;20:1–10.
Lawrence D, Dawson V, Houghton S, Goodsell B, Sawyer MG. Impact of Mental Disorders on Attendance at School. Aust J Educ. 2019;63:5–21.
Aluh DO, Abba A, Afosi AB. Prevalence and correlates of depression, anxiety and stress among undergraduate pharmacy students in Nigeria. Pharm Educ. 2020;20:236–48.
Mall S, Mortier P, Taljaard L, Roos J, Stein DJ, Lochner C. The Relationship Between Childhood Adversity, Recent stressors, and depression in college students Attending a South African University. BMC Psychiatry. 2018;18:63.
Article PubMed PubMed Central Google Scholar
Bantjes JR, Kagee A, McGowan T, Steel H. Symptoms of posttraumatic stress, depression, and anxiety as predictors of suicidal ideation among South African university students. J Am Coll Health. 2016;64:429–37.
Farrer LM, Gulliver A, Bennett K, Fassnacht DB, Griffiths KM. Demographic and Psychosocial Predictors of Major Depression and Generalised Anxiety Disorder in Australian University Students. BMC Psychiatry. 2016;16:1–9.
Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a Brief Depression Severity Measure. J Gen Intern Med. 2001;16:606.
Islam MdA, Barna SD, Raihan H, Khan MdNA, Hossain MdT. Depression and anxiety among university students during the COVID-19 pandemic in Bangladesh: A web-based cross-sectional survey. PLoS ONE. 2020;15:e0238162.
Spitzer RL, Kroenke K, Williams JBW, Löwe B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch Intern Med. 2006;166:1092–7.
Wagner F, Kaneli T, Masango M. Exploring the Relationship Between Food insecurity With Hunger and Academic Progression at a Large South African University. South Afr J High Educ. 2021;35:296–309.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95:103208.
Humensky J, Kuwabara SA, Fogel J, Wells C, Candidate B, Goodwin B, et al. Adolescents With Depressive Symptoms and Their Challenges With Learning in School. J School Nurs. 2010;26:377–92.
Andrews B, Wilding JM. The Relation of Depression and Anxiety to Life-stress and Achievement in Students. Br J Psychol. 2004;95:509–21.
Ruz MEA, Al-Akash HY, Jarrah S. Persistent (Anxiety and Depression) Affected Academic Achievement and Absenteeism in Nursing Students. Open Nurs J. 2018;12:171.
Erhun WO, Jegede AO, Ojelabi JA. Implications of Failure on Students who have Repeated a Class in a Faculty of Pharmacy. Curr Pharm Teach Learn. 2022;14:166–72.
Ajjawi R, Dracup M, Zacharias N, Bennett S, Boud D. Higher Education Research & Development Persisting students’ explanations of and emotional responses to academic failure. 2019. https://doi.org/10.1080/07294360.2019.1664999 .
van Zyl A, Gravett S, de Bruin G. To What Extent Do Pre-entry Attributes Predict First Year Student Academic Performance in the South African Context? South African Journal of Higher Education. 2016;26.
Maree J. Barriers to Access to and Success in Higher Education: Intervention Guide. South Afr J High Educ. 2014;29:390–411.
Case J, Marshall D, Grayson D. Mind the Gap: Science and Engineering Education at the Secondary–tertiary Interface. S Afr J Sci. 2013;109(7/8):1–5.
Stats SA. Education Series Volume V: Higher Education and Skills in South Africa, 2017. Pretoria; 2019.
Download references
Acknowledgements
The authors would like to thank the students who participated in this study.
This research project received funding from the Kresge Foundation, Grant G-1912-287858. RGW gratefully acknowledges funding from the South African National Research Foundation (119234).
Author information
Authors and affiliations.
Analytics and Institutional Research Unit (AIRU), University of the Witwatersrand, Johannesburg, South Africa
F Wagner & LP Makuapane
MRC/Wits Rural Public Health and Health Transitions Research Unit (Agincourt), School of Public Health, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
RG Wagner & FX Gómez-Olivé
Faculty of Science and Agriculture, Department of Consumer Sciences, University of Zululand, 3886, KwaDlangezwa, South Africa
Department of Institutional Planning (DIP), University of Pretoria, Pretoria, South Africa
You can also search for this author in PubMed Google Scholar
Contributions
FW, RGW and MM conceptualized the research and UK, FXG-O and FW determined the scope of the manuscript. FW, LM and MM collected the data and FW and LM analysed the data. FW drafted the first version of the manuscript, which was critically reviewed by all other authors, who then approved the final version for submission.
Corresponding author
Correspondence to F Wagner .
Ethics declarations
Ethical approval and consent to participate.
The study received ethical clearance from the University of the Witwatersrand Human Research Ethics Committee (HREC) (Medical), as well as the University of the Witwatersrand Human Research Ethics Committee (HREC) (Non-Medical), Clearance Certificates H181144; M1900627, respectively. Permission was received from the Office of the Registrar to conduct the study. All methods were carried out in accordance with the relevant guidelines and regulations. All experimental protocols were approved by a the Faculty of Health Sciences, University of the Witwatersrand, Johannesburg.
Participants were provided with the information sheet in the body of the invitation email, and were only invited to complete the survey following consent. Informed consent was obtained from all subjects. Participants were also provided with contact information for psychological counselling services available to them.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Wagner, F., Wagner, R., Kolanisi, U. et al. The relationship between depression symptoms and academic performance among first-year undergraduate students at a South African university: a cross-sectional study. BMC Public Health 22 , 2067 (2022). https://doi.org/10.1186/s12889-022-14517-7
Download citation
Received : 06 July 2022
Accepted : 01 November 2022
Published : 11 November 2022
DOI : https://doi.org/10.1186/s12889-022-14517-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- College students
- Higher education institution
- Mental health
- Progression
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An Exploratory Study of Students with Depression in Undergraduate Research Experiences
Affiliations.
- 1 Department of Biology, University of Central Florida, Orlando, FL, 32816.
- 2 Biology Education Research Lab, Research for Inclusive STEM Education Center, School of Life Sciences, Arizona State University, Tempe, AZ 85281.
- PMID: 32412838
- PMCID: PMC8697659
- DOI: 10.1187/cbe.19-11-0217
Depression is a top mental health concern among undergraduates and has been shown to disproportionately affect individuals who are underserved and underrepresented in science. As we aim to create a more inclusive scientific community, we argue that we need to examine the relationship between depression and scientific research. While studies have identified aspects of research that affect graduate student depression, we know of no studies that have explored the relationship between depression and undergraduate research. In this study, we sought to understand how undergraduates' symptoms of depression affect their research experiences and how research affects undergraduates' feelings of depression. We interviewed 35 undergraduate researchers majoring in the life sciences from 12 research-intensive public universities across the United States who identify with having depression. Using inductive and deductive coding, we identified that students' depression affected their motivation and productivity, creativity and risk-taking, engagement and concentration, and self-perception and socializing in undergraduate research experiences. We found that students' social connections, experiencing failure in research, getting help, receiving feedback, and the demands of research affected students' depression. Based on this work, we articulate an initial set of evidence-based recommendations for research mentors to consider in promoting an inclusive research experience for students with depression.
Publication types
- Research Support, Non-U.S. Gov't
- Research Support, U.S. Gov't, Non-P.H.S.
- Depression*
- Universities
Grants and funding
- HHMI/Howard Hughes Medical Institute/United States
Depression, Anxiety, Loneliness Are Peaking in College Students

Photo by Cydney Scott
Nationwide study, co-led by BU researcher Sarah Ketchen Lipson, reveals a majority of students say mental health has impacted their academic performance
Kat j. mcalpine.
A survey by a Boston University researcher of nearly 33,000 college students across the country reveals the prevalence of depression and anxiety in young people continues to increase, now reaching its highest levels, a sign of the mounting stress factors due to the coronavirus pandemic, political unrest, and systemic racism and inequality.
“Half of students in fall 2020 screened positive for depression and/or anxiety,” says Sarah Ketchen Lipson , a Boston University mental health researcher and a co–principal investigator of the nationwide survey , which was administered online during the fall 2020 semester through the Healthy Minds Network. The survey further reveals that 83 percent of students said their mental health had negatively impacted their academic performance within the past month, and that two-thirds of college students are struggling with loneliness and feeling isolated—an all-time high prevalence that reflects the toll of the pandemic and the social distancing necessary to control it.
Lipson, a BU School of Public Health assistant professor of health law, policy, and management, says the survey’s findings underscore the need for university teaching staff and faculty to put mechanisms in place that can accommodate students’ mental health needs.
“Faculty need to be flexible with deadlines and remind students that their talent is not solely demonstrated by their ability to get a top grade during one challenging semester,” Lipson says.
She adds that instructors can protect students’ mental health by having class assignments due at 5 pm, rather than midnight or 9 am, times that Lipson says can encourage students to go to bed later and lose valuable sleep to meet those deadlines.
Especially in smaller classroom settings, where a student’s absence may be more noticeable than in larger lectures, instructors who notice someone missing classes should reach out to that student directly to ask how they are doing.
“Even in larger classes, where 1:1 outreach is more difficult, instructors can send classwide emails reinforcing the idea that they care about their students not just as learners but as people, and circulating information about campus resources for mental health and wellness,” Lipson says.
And, crucially, she says, instructors must bear in mind that the burden of mental health is not the same across all student demographics. “Students of color and low-income students are more likely to be grieving the loss of a loved one due to COVID,” Lipson says. They are also “more likely to be facing financial stress.” All of these factors can negatively impact mental health and academic performance in “profound ways,” she says.
At a higher level within colleges and universities, Lipson says, administrators should focus on providing students with mental health services that emphasize prevention, coping, and resilience. The fall 2020 survey data revealed a significant “treatment gap,” meaning that many students who screen positive for depression or anxiety are not receiving mental health services.
“Often students will only seek help when they find themselves in a mental health crisis, requiring more urgent resources,” Lipson says. “But how can we create systems to foster wellness before they reach that point?” She has a suggestion: “All students should receive mental health education, ideally as part of the required curriculum.”
It’s also important to note, she says, that rising mental health challenges are not unique to the college setting—instead, the survey findings are consistent with a broader trend of declining mental health in adolescents and young adults. “I think mental health is getting worse [across the US population], and on top of that we are now gathering more data on these trends than ever before,” Lipson says. “We know mental health stigma is going down, and that’s one of the biggest reasons we are able to collect better data. People are being more open, having more dialogue about it, and we’re able to better identify that people are struggling.”
The worsening mental health of Americans, more broadly, Lipson says, could be due to a confluence of factors: the pandemic, the impact of social media, and shifting societal values that are becoming more extrinsically motivated (a successful career, making more money, getting more followers and likes), rather than intrinsically motivated (being a good member of the community).
The crushing weight of historic financial pressures is an added burden. “Student debt is so stressful,” Lipson says. “You’re more predisposed to experiencing anxiety the more debt you have. And research indicates that suicidality is directly connected to financial well-being.”
With more than 22 million young people enrolled in US colleges and universities, “and with the traditional college years of life coinciding with the age of onset for lifetime mental illnesses,” Lipson stresses that higher education is a crucial setting where prevention and treatment can make a difference.
One potential bright spot from the survey was that the stigma around mental health continues to fade. The results reveal that 94 percent of students say that they wouldn’t judge someone for seeking out help for mental health, which Lipson says is an indicator that also correlates with those students being likely to seek out help themselves during a personal crisis (although, paradoxically, almost half of students say they perceive that others may think more poorly of them if they did seek help).
“We’re harsher on ourselves and more critical of ourselves than we are with other people—we call that perceived versus personal stigma,” Lipson says. “Students need to realize, your peers are not judging you.”
Explore Related Topics:
- Community Health Sciences
- Data Sciences
- Gender Studies
- Public Policy
- Share this story
- 25 Comments Add
Former Editor, The Brink Twitter Profile

Kat J. McAlpine Profile
Comments & Discussion
Boston University moderates comments to facilitate an informed, substantive, civil conversation. Abusive, profane, self-promotional, misleading, incoherent or off-topic comments will be rejected. Moderators are staffed during regular business hours (EST) and can only accept comments written in English. Statistics or facts must include a citation or a link to the citation.
There are 25 comments on Depression, Anxiety, Loneliness Are Peaking in College Students
first of all, excellent writing! This report is extremely triggering for a few reasons. Obviously students are NOT okay at the moment, now confirmed by the student. But what does the university do about it? They micro-manage EVERY aspect of students’ life to mitigate Covid risk. Here, tell me why the university took away household table seating in the dining hall? That was one of the ONLY places on campus where students can eat with each other and actually see their friends’ faces. What type of modeling was used to make this decision and its impact on covid spread on campus. Same thing for the green badge, was there a statistical difference in case before and after students have to walk around showing that? The university’s policies are simply incentivizing off-campus, more dangerous gatherings because the university won’t facilitate anything like that on campus. Oh, and the university response? ‘you’re doing great sweetie’ type of deal – absolutely ridiculous. I know BU can’t keep this up much longer, they are losing far too much money because of Covid and less students on campus – there will be a reckoning. Students, stand up.
BU will acknowledge this but then still won’t do anything to actually help.
Great, but this school is doing absolutely nothing to help it
I appreciate this article because I feel that the issue of mental health isn’t talked about enough amongst students and just college culture in general. I don’t see any concerns coming from college faculty, at least clearly. It’s so important to talk about mental health, especially during a pandemic.
This article is definitely going in the right direction. That being said, as the other comments have also mentioned, BU needs to do MUCH more than just publishing an article telling students, “well, at least you aren’t alone.” If 83% of your student body reports their mental health affects their school work, then if not for them, at least change something for the benefit of the school’s name. To put it bluntly, this does not look good. Also referencing BU’s response to sexual harassment, BU now has a track record of acknowledging issues that significantly impact its students in an article or maybe a speech to only do NOTHING about it. Please, I implore the school to act. Act or we will.
We know mental health stigma is going down
Actually, we know support for those taught and teaching that prejudice is diminishing, though that does not mean by any stretch of the imagination it is not still being taught. It continues to be taught (often resolutely) at Boston University. The above sentence is one manner in which it continues to be taught, Passive Reference. It is also actively taught. “Perceived stigma” is another interesting Passive Reference, directed prejudices are intended by their directors to be perceived. “perceived” stigma is an obfuscation of the process whereby it is perceived. It surprises me, that so many women, eschewing “the stigma” of rape, continue to declare “the stigma” of mental illnesses. Sometimes history does not inform us. A few years ago 5 students died by suicide at a Canadian college, blamed was “the stigma” of mental illnesses, not those conveying it. When a young man at U Penn died by suicide it prompted his sister to set up a now national organization protesting “the stigma” of mental illnesses, not those conveying it. National organizations abound conveying “the stigma” of mental illnesses to eagerly awaiting audiences. Publications abound, but to my knowledge not one single publication directly addresses how it is taught or who teaches it. Nor, to my knowledge is there a campus in the US, or any English speaking country, where someone is given guidance on how to address those directing it. Whom to approach. How to resolve it. [email protected] offers no such guidance. I invite each of you to return to 1972, when a small group of personally empowered women said, “Stop directing the term stigma at rape, you have done enough harm” and take that lesson to heart: We stopped.
And I invite [email protected] to take a role in bringing about that change.
Harold A Maio, retired mental health editor
Wow – so what is BU doing about this when we have pleaded with admin and offered so many ideas and solutions to helping here since September 2020?
The silence is deafening BU.
The Well Being Project is stagnate.
The Dean is silent.
The provost says students are happy based on some survey they did just before holidays when students knew they were going home.
The Director of Mental Health says appts for mental health are down – that’s the sign everything is fine?
We are hearing the opposite and many students have just lost their faith in support from BU as well as just returning home for LFA where they have a support system.
Where are the social in person safe activities outside and inside?
Where are the RAs and their weekly activities and support of their residents or are they just there to write students up?
Where are the self-care tips and resources offered daily to students?
Where in the daily MANDATORY self-check survey of their health – are any questions about their emotional well being including their mood, stress levels, sleep and appetite?
Where is the support for faculty who are seeing these issues and trying to reach out?
Where are the therapy dogs from pre-pandemic we asked for weekly or biweekly to come outside and offer unconditional emotional support during this tough time?
Where are some campus wide concerts or comedy relief concert paid for by BU – virtually or outside so students have anything to look forward to? If it’s down to money / the $70,000 Tuition or should cover some of it or funds from housing since many were not reimbursed when they returned home for support.
Where is any work with this amazing wise resource Dr. Lipson to take any of her guidance since last summer instead of just posting it here?
Is anyone listening to the isolation and pain of so many terriers? I have heard troubling stories for months since we began our BU Parent group that is NOT monitored by the Deans office unlike others. I have helped refer and counsel families worried if they speak up there might be some retaliation. There is no retaliation just a deaf ear to making any changes to improve morale and well being of our terriers during a pandemic. And then posting this article is the ultimate hutzpah when no one has listened to Dr.Lipson / your own shining star about these issues.
Why not shine as you have with COVID testing? What if this were your family member feeling isolated and disillusioned with their dreams at BU with no outreach from BU except an occasional ZOOM message.
BU can do so much better and be the example for the rest of the nation. Why test so stringently if you will not allow any safe activities except for favorites like sports teams and band members?
Terriers are ZOOMED OUT. Don’t wait for a suicide or more depression to appear in students. It’s almost too late to be proactive / but you can try and we ask that you try hard. Be an example for other colleges.
We are not giving up on being heard. We are parents who care and love BU and know it can do better.
A lot of good points made – I wanted to touch upon when you mentioned that appointments for mental health are apparently down. As a student actively seeking mental health resources, my experience is that it has been extremely difficult to even schedule any sort of mental health appointments or counseling; we are unable to make an appointment online or in-person anymore, and the only information we are given is a phone number to call (the Behavioral Medicine number). I find this frustrating as many of us need more than just a phone conversation to help – even a zoom meeting would be helpful, but why aren’t there zoom appointments for SHS like there are for almost every other service on campus (e.g., pre-professional advising, financial aid, etc.)? I’ve noticed that the loneliness and isolation is affecting not only me but my roommates as well, who have stronger support systems and more friends on campus than I do – we’ve all been lacking motivation to do any of our work and they’ve mentioned that they feel like they need a break (spring break canceled due to pandemic concerns). Even some of my professors seem burnt out – forgetting class, getting behind on their syllabus, etc. In my opinion, BU should be more proactive in giving students resources instead of making it difficult to find said resources. Lastly, I wanted to add that I understand a lot of services are probably very different now due to the pandemic, but a single “wellness week” and emails about it do not do much to actually help students – I find it comparable to “self care” where the self care is just drinking wine and putting on a skincare mask and pushing all your real problems aside.
I agree with those who are asking for BU to do more to support students. I’m a faculty member who is trying to do my best to support my students. I’m more than willing to give extensions, modify assignments, and lower my expectations this semester. I’m checking in on students who miss class to make sure they’re okay. I’m trying to cut as much material as I can while still meeting my course learning objectives. At the same time, I don’t think it’s fair to expect faculty to do everything when it comes to students’ wellbeing. I’ve been in meetings where faculty were asked (both implicitly and explicitly) to help students make friends and socialize during class. I know faculty who are doing this in their courses (and I applaud them for their efforts), but shouldn’t Res Life and other staff at BU be providing opportunities for students to safely socialize? Sure, it’s cold, but certainly BU can be creative and think of ways to encourage students to get out of their dorms and make friends. Faculty are struggling too, and BU’s administration can help us by helping our students.
This is an excellent article, and though not surprising, it is shocking that the BU administration has not done anything to remedy this mental health crises. This is a mental health pandemic happening and it should be as high of a priority for BU as the trying to control the virus. If BU doesn’t step up and come up with a plan to address this then our students will suffer for years to come. This should have happened months ago. You can’t have a healthy individual/society if you are only concerned with physical health. It has to be a holistic approach.
Nice article I hope all instructors read this article I am one of the students sometimes fell a depression and live in the anxiety that is effectives on my life and do not have the energy to do anything particularly during what we live now
First, I would like to focus on the positive and thank BU mental health staff for being there for my son when he was in urgent need of mental health support back in the Fall semester. My call was answered right away and my son was able to speak with a professional with in 15 minutes. I was very impressed and relieved. They were there when we needed them.
On the other hand, I’m hearing from my son and all of his friends that the academic culture of rigor for the sake of rigor, grade deflation and the purposeful weeding out of students from core classes rather than supporting and helping each student succeed, not only continues but has been increased during COVID. These students have a sense that professors are concerned about online cheating so have ramped the rigor to address this. Not sure if this is real or perceived and I’m sure this is not going on in all classes as I also heard examples of supportive professors, but this is definitely a theme I am hearing from students. This style of academics is known to be outdated and ineffective, yet it continues, even at a higher level, during a pandemic.
I’m hoping this feedback can serve helpful to administration.
THANK YOU!!!! As a college student, who has survived the past year with a 4.0, attending full-time to obtain my degree in IT. I am struggling for the first time. After technology issues that set me behind four days, I really thought my instructors would understand. One of my instructors couldn’t care less. The workload is beyond overwhelming, her curriculum seems almost cruel. I graduate next month and I feel like I am losing my mind. I already suffer from severe anxiety, so the level I’m at now is almost debilitating. I have been obtaining degrees since 1998, and familiar with online learning. I’ve never had issues. This morning I received an email from her reminding me of the due date, in all bold caps, followed by some !!!! … She made it clear she is not available on the weekend, but expects us to be flexible. So my dilemma is this, I am failing my coding class now, but I don’t feel that I should be financially responsible to pay for having to retake it, as well as have it impact my financial aid and scholarships I receive for my academic performance.
Hi. I’m a BU alumna, a college professor, and mom to 4 college-aged sons. WONDERING… Do students feel there is explicit and implicit prejudice against college students as “purveyors of COVID?” I think this adds to the discomfort or enjoyment of being a college student and part of a university community. Thoughts? Thanks!
I notice that the students like to complain on here. One thing that university researchers on mental health have a difficult time assessing is knowing the familial support system (or lack thereof) students come into university life with. Psychologists will affirm that this plays a huge role in the mental health of students, at any age. Just as elementary through high schools today are expected to be the emotional, parental, physical, educational, and social supporter of each student, so too are universities being given this sort of expectation. Don’t get me wrong…I believe in striving for mental health and making resources available on campuses. However, within the communities of students – whether their friends or family – we have to realize that the internal conversation around mental health for many cultures is either non-existent or looked down upon. We can sing mental health from the rooftops all day long and hope that students are listening…..and I hope they do.
ECT/Electroshock use has been on the rise last 5 years or so and not just used for depression nor as a last resort. No FDA testing ever done of devices used or the procedure itself. Increase risk for suicide following as many cannot find help for their repeated brain injuries after consenting to this. Lawsuits taking place in the US and England around these damages covered up. See site ectjustice to learn more. Please speak out on social media so others are made aware of the truth of this practice.
People shouldn’t hesitate to ask for psychological help. I think it’s one of the main problems why people struggle mentally. Maybe, it’s a matter of self-critique, and society says sometimes that we should be strong… But when someone gets in an emotional crisis, only a professional can help. And I also never see when students/educators judge their peers/colleagues if someone contacted mental health support. I looked through the list of different affordable mental health services across English-speaking countries – https://ivypanda.com/blog/mental-health-resources – I was shocked how many problems we can have, and how many professionals exist to help with them. Maybe, it may be helpful to others too. Let’s take care of ourselves.
I tried to find the source for “83 %” of college students say their performance was negatively affected by mental health. Did you just pull that number out of thin air? I tried to go through everything I could and could not find this number anywhere in any actual published writing.
Please see page six of the report, the pie chart listed under Academic Impairment.
I think you just made up certain elements of this article and they actually have 0 foundation whatsoever. It has led me down a rabbit hole of attempting to try to find the published support for some of the claims you make. Including the 83 % figure. If you’re going to write articles that will be heavily referenced (which this is, because other idiots went on to quote this article), you should at least get the facts straight.
Please see page 6 of the report, the pie chart listed under Academic Impairment: https://healthymindsnetwork.org/wp-content/uploads/2021/02/HMS-Fall-2020-National-Data-Report.pdf
That is a misrepresentation of the data, in my opinion. Including students who reported mental health impacting their academic performance 1-2 days out of the week is insufficient to be grouped in with 83% of students. The way it is presented in this article makes it seem much more drastic than that. It should say, “28% of students felt 1-2 days out of the week had been negatively impacted by their mental health in the past month..” and report the other percentages. Not combined into one group and twisted in a sensationalistic way. I was attempting to use this information for a research paper of my own and was sent down a rabbit hole trying to find a source. Other people have cited this article, and that is your responsibility as a researcher.
Reading it because to help a friend with his assignment. He studies in FAST, Islamabad, Pakistan. If anyone of his class fellows are here, good luck to you
It is 3:12 in the morning and I just got off the phone with son. He called because he was riddled with anxiety and suffering with loneliness and a seeming inability to form meaningful connections. This is his first year at BU. He loves the University; However, in addition to the rigorous academic challenges, he is crushed by the seeming inability to form connections with others. This, on so many levels, surprises me. He is intelligent, interesting, friendly, handsome and well rounded. Upon my introduction to the University’s logistical layout, I was immediately aware that it not appear easily conducive to meeting people… As opposed to a smaller private college if you will. Clearly, BU had an obligation to address the many challenges brought about as a result of Covid. Understandable, but perhaps a bit extreme, ie: The students not being allowed to eat or congregate. Regardless, what I also observed is that there are few, if any, common rooms.. areas for students to hang out, play board games, ping pong, darts, tell jokes, b.s. and share common concerns. Or My point being, there should be multiple places (Besides sneaking into local clubs, or drinking Alone in your dorm) where kids can go..day or night. Organized events as well, aside from sports. As aforementioned, my son also found it very challenging and frustrating to contact a counselor through your service. When you do, the schedules are booked…… I have been heartbroken. Nonetheless, the consistent voice if encouragement. I want more from the school. I, like all others noted before me. More social emotional support. More access to social opportunities. More professors understanding and working with the challenges our children are struggling to navigate. In closing, it’s not just a BU crisis. I listen to very similar difficulties from many other University families…. PLEASE be more proactive. PLEASE care PLEASE help It is imperative and essential to a successful college experience and outcome. Thank you. And thank you all aforementioned
very very nice
Post a comment. Cancel reply
Your email address will not be published. Required fields are marked *
Latest from The Brink
Permanent birth control—vasectomies and tubal ligations—up following supreme court abortion ruling, explain this how do planets form, bu’s innovator of the year has pioneered devices to advance astronomy, microscopy, eye exams, bu study shows a correlation between social media use and desire for cosmetic procedures, covid-19 photo contest winners capture moments of joy, sorrow, meaning in crisis, how high-level lawsuits are disrupting climate change policies, the h5n1 bird flu is a growing threat for farm animals and humans—how serious is it, why is a bu researcher so fascinated with the diets of dung beetles, we are underestimating the health harms of climate disasters, three bu researchers elected aaas fellows, should people be fined for sleeping outside, secrets of ancient egyptian nile valley settlements found in forgotten treasure, bu electrical engineer vivek goyal named a 2024 guggenheim fellow, not having job flexibility or security can leave workers feeling depressed, anxious, and hopeless, can the bias in algorithms help us see our own, do immigrants and immigration help the economy, how do people carry such heavy loads on their heads, do alcohol ads promote underage drinking, how worried should we be about us measles outbreaks, stunning new image shows black hole’s immensely powerful magnetic field.

Kristen Bowe, APRN, C.N.P., M.S.N.
Family medicine, primary care, recent posts.

- Behavioral Health
- Children's Health (Pediatrics)
- Exercise and Fitness
- Heart Health
- Men's Health
- Neurosurgery
- Obstetrics and Gynecology
- Orthopedic Health
- Weight-loss (Bariatric) Surgery
- Women's Health


College students and depression: A guide for parents
- Balance Your Mental and Emotional Health
- Suicide Prevention

Entering or returning to college is an exciting time for young adults. Students and parents hope for memorable experiences to last a lifetime. For many students, the years at college are a time of discovery and growth.
But depression may get in the way.
The rate of depression among college students is rising. In a 2021–2022 survey of students across 133 college campuses, 44% of students reported symptoms of depression and 15% reported seriously considering suicide in the past year.
For both parents and students, knowing the risk factors and symptoms can help with the early identification and treatment of depression.
Symptoms of depression can include:
- Anxiety and panic
- Difficulty with schoolwork
- Changes in eating or sleeping patterns
- Emotional outbursts, such as tearfulness, anger or irritability
- Lack of energy or fatigue
- Loss of interest in activities, such as clubs, sports or other social commitments
- Poor self-esteem
- Sense of being overwhelmed
- Thoughts of suicide or self-harm
- Unrealistic guilt
Why are young adults struggling?
Although the problems facing college students are complex. They often feel intense pressure to succeed while still developing necessary life skills.
The rising cost of education places additional stress on students and their families. Children are being pushed to their limits as early as elementary school. As a result, their mental health and well-being are suffering.
Many middle and high school students have schedules rivaling top corporate executives, with an average day beginning at 6 a.m. and ending after 10 p.m. These demanding schedules leave many sleep deprived with little time to develop basic independent living skills, such as doing laundry, cooking meals, managing money and accessing services to meet their needs. They do this all while figuring out, "Who am I?"
These skill deficits compound as young adults go to college and face relationship challenges and heavy class schedules. They may also be living separately from their parents for the first time.
Helping children find a balance between achievement and life's demands begins at home.
Here are tips for parents and children before college:
- Set a realistic view of the big picture. Giving 100% at all times in all areas of life is unrealistic. Encourage students to focus on making the most of their college experience by forging positive relationships, creating fun memories and preparing for their future careers.
- Build independent living skills at a young age. Online resources are available to find age-appropriate chores for children to help you start the process.
- Protect downtime or unstructured time for middle and high school students. This is when students start to explore who they are.
What are the risk factors for college students?
Unfortunately, as many as 75% of students who struggle with depression are reluctant to seek help. This increases the risk of harmful outcomes, such as dropping out of college, poor academic performance, suicide and substance abuse.
College students may be exposed to many situations or risk factors that could trigger an episode of depression:
- Comparison of academic, athletic or social performance to their peers
- Drug or alcohol use
- Family history of depression
- Fears of disappointing parents because of grades or career path
- Peer relationship difficulties
- Relationship breakup
- Sexual assault
- Sexual identity adjustment difficulties
- Stressful life events
Those at highest risk for depression and anxiety are:
- Female students
- Low-income students
- Students of color
- Students who are caregivers for children or other adults
- Students who identify as LGBTQ .
What are the warning signs of suicide?
Suicide is the second-leading cause of death in young people ages 20 to 24. While the factors that lead to suicide are multifaceted, being diagnosed with a mental illness like depression increases the risk.
These behaviors may indicate that students are thinking about suicide:
- Displaying extreme mood swings
- Giving away possessions
- Increasing use of alcohol or drugs
- Ignoring class work or skipping classes
- Engaging in risky or self-destructive acts, such as using drugs or driving recklessly
- Showing anger or rage or expressing a desire to seek revenge
- Sleeping too little or too much
- Talking about suicide
- Talking about being a burden to others
- Talking about feeling trapped, hopeless or having no purpose
- Withdrawing from friends and wanting to be left alone
This is not an exhaustive list. Be alert to behavior and personality changes that can provide clues to a student's well-being.
What can parents do to help students?
Parents often worry about how their child will react if they try to talk the signs and symptoms of depression. But it's crucial to have a conversation about your concerns.
Be direct with your child. Give examples of symptoms you've noticed and explain why these examples worry you. Be patient, calm and empathetic in your communication.
Students often believe they are to blame for their mental health concerns, which can lead to defensiveness or shutting down. To reduce the stigma, help students understand it's not their fault, and many young adults experience depression.
If you have concerns, it's important to ask your students if they're considering suicide or self-harm. This won't put the idea in their heads. If your student is expressing thoughts about suicide, you must seek immediate medical attention.
Many colleges and universities provide mental health services on campus. Your child's primary care provider has resources and can refer your student to a mental health counselor. Parents and students should have hope since many effective treatments for depression exist.
Kristen Bowe is a nurse practitioner in Family Medicine in Belle Plaine and Montgomery , Minnesota.
Related Posts

- Open access
- Published: 16 May 2024
Procrastination, depression and anxiety symptoms in university students: a three-wave longitudinal study on the mediating role of perceived stress
- Anna Jochmann 1 ,
- Burkhard Gusy 1 ,
- Tino Lesener 1 &
- Christine Wolter 1
BMC Psychology volume 12 , Article number: 276 ( 2024 ) Cite this article
Metrics details
It is generally assumed that procrastination leads to negative consequences. However, evidence for negative consequences of procrastination is still limited and it is also unclear by which mechanisms they are mediated. Therefore, the aim of our study was to examine the harmful consequences of procrastination on students’ stress and mental health. We selected the procrastination-health model as our theoretical foundation and tried to evaluate the model’s assumption that trait procrastination leads to (chronic) disease via (chronic) stress in a temporal perspective. We chose depression and anxiety symptoms as indicators for (chronic) disease and hypothesized that procrastination leads to perceived stress over time, that perceived stress leads to depression and anxiety symptoms over time, and that procrastination leads to depression and anxiety symptoms over time, mediated by perceived stress.
To examine these relationships properly, we collected longitudinal data from 392 university students at three occasions over a one-year period and analyzed the data using autoregressive time-lagged panel models.
Procrastination did lead to depression and anxiety symptoms over time. However, perceived stress was not a mediator of this effect. Procrastination did not lead to perceived stress over time, nor did perceived stress lead to depression and anxiety symptoms over time.
Conclusions
We could not confirm that trait procrastination leads to (chronic) disease via (chronic) stress, as assumed in the procrastination-health model. Nonetheless, our study demonstrated that procrastination can have a detrimental effect on mental health. Further health outcomes and possible mediators should be explored in future studies.
Peer Review reports
Introduction
“Due tomorrow? Do tomorrow.”, might be said by someone who has a tendency to postpone tasks until the last minute. But can we enjoy today knowing about the unfinished task and tomorrow’s deadline? Or do we feel guilty for postponing a task yet again? Do we get stressed out because we have little time left to complete it? Almost everyone has procrastinated at some point when it came to completing unpleasant tasks, such as mowing the lawn, doing the taxes, or preparing for exams. Some tend to procrastinate more frequently and in all areas of life, while others are less inclined to do so. Procrastination is common across a wide range of nationalities, as well as socioeconomic and educational backgrounds [ 1 ]. Over the last fifteen years, there has been a massive increase in research on procrastination [ 2 ]. Oftentimes, research focuses on better understanding the phenomenon of procrastination and finding out why someone procrastinates in order to be able to intervene. Similarly, the internet is filled with self-help guides that promise a way to overcome procrastination. But why do people seek help for their procrastination? Until now, not much research has been conducted on the negative consequences procrastination could have on health and well-being. Therefore, in the following article we examine the effect of procrastination on mental health over time and stress as a possible facilitator of this relationship on the basis of the procrastination-health model by Sirois et al. [ 3 ].
Procrastination and its negative consequences
Procrastination can be defined as the tendency to voluntarily and irrationally delay intended activities despite expecting negative consequences as a result of the delay [ 4 , 5 ]. It has been observed in a variety of groups across the lifespan, such as students, teachers, and workers [ 1 ]. For example, some students tend to regularly delay preparing for exams and writing essays until the last minute, even if this results in time pressure or lower grades. Procrastination must be distinguished from strategic delay [ 4 , 6 ]. Delaying a task is considered strategic when other tasks are more important or when more resources are needed before the task can be completed. While strategic delay is viewed as functional and adaptive, procrastination is classified as dysfunctional. Procrastination is predominantly viewed as the result of a self-regulatory failure [ 7 ]. It can be understood as a trait, that is, as a cross-situational and time-stable behavioral disposition [ 8 ]. Thus, it is assumed that procrastinators chronically delay tasks that they experience as unpleasant or difficult [ 9 ]. Approximately 20 to 30% of adults have been found to procrastinate chronically [ 10 , 11 , 12 ]. Prevalence estimates for students are similar [ 13 ]. It is believed that students do not procrastinate more often than other groups. However, it is easy to examine procrastination in students because working on study tasks requires a high degree of self-organization and time management [ 14 ].
It is generally assumed that procrastination leads to negative consequences [ 4 ]. Negative consequences are even part of the definition of procrastination. Research indicates that procrastination is linked to lower academic performance [ 15 ], health impairment (e.g., stress [ 16 ], physical symptoms [ 17 ], depression and anxiety symptoms [ 18 ]), and poor health-related behavior (e.g., heavier alcohol consumption [ 19 ]). However, most studies targeting consequences of procrastination are cross-sectional [ 4 ]. For that reason, it often remains unclear whether an examined outcome is a consequence or an antecedent of procrastination, or whether a reciprocal relationship between procrastination and the examined outcome can be assumed. Additionally, regarding negative consequences of procrastination on health, it is still largely unknown by which mechanisms they are mediated. Uncovering such mediators would be helpful in developing interventions that can prevent negative health consequences of procrastination.
The procrastination-health model
The first and only model that exclusively focuses on the effect of procrastination on health and the mediators of this effect is the procrastination-health model [ 3 , 9 , 17 ]. Sirois [ 9 ] postulates three pathways: An immediate effect of trait procrastination on (chronic) disease and two mediated pathways (see Fig. 1 ).
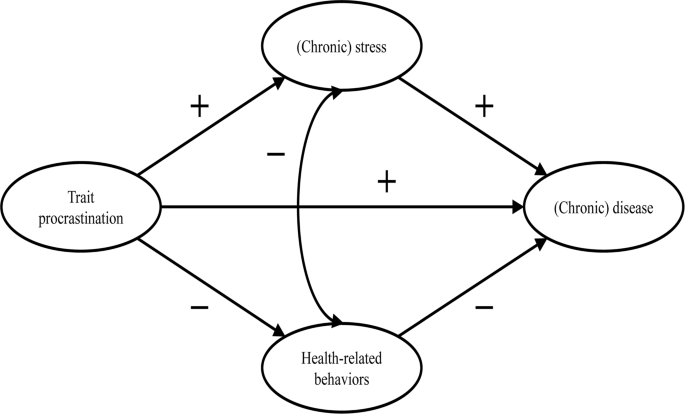
Adopted from the procrastination-health model by Sirois [ 9 ]
The immediate effect is not further explained. Research suggests that procrastination creates negative feelings, such as shame, guilt, regret, and anger [ 20 , 21 , 22 ]. The described feelings could have a detrimental effect on mental health [ 23 , 24 , 25 ].
The first mediated pathway leads from trait procrastination to (chronic) disease via (chronic) stress. Sirois [ 9 ] assumes that procrastination creates stress because procrastinators are constantly aware of the fact that they still have many tasks to complete. Stress activates the hypothalamic-pituitary-adrenocortical (HPA) system, increases autonomic nervous system arousal, and weakens the immune system, which in turn contributes to the development of diseases. Sirois [ 9 ] distinguishes between short-term and long-term effects of procrastination on health mediated by stress. She believes that, in the short term, single incidents of procrastination cause acute stress, which leads to acute health problems, such as infections or headaches. In the long term, chronic procrastination, as you would expect with trait procrastination, causes chronic stress, which leads to chronic diseases over time. There is some evidence in support of the stress-related pathway, particularly regarding short-term effects [ 3 , 17 , 26 , 27 , 28 ]. However, as we mentioned above, most of these studies are cross-sectional. Therefore, the causal direction of these effects remains unclear. To our knowledge, long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress have not yet been investigated.
The second mediated pathway leads from trait procrastination to (chronic) disease via poor health-related behavior. According to Sirois [ 9 ], procrastinators form lower intentions to carry out health-promoting behavior or to refrain from health-damaging behavior because they have a low self-efficacy of being able to care for their own health. In addition, they lack the far-sighted view that the effects of health-related behavior only become apparent in the long term. For the same reason, Sirois [ 9 ] believes that there are no short-term, but only long-term effects of procrastination on health mediated by poor health-related behavior. For example, an unhealthy diet leads to diabetes over time. The findings of studies examining the behavioral pathway are inconclusive [ 3 , 17 , 26 , 28 ]. Furthermore, since most of these studies are cross-sectional, they are not suitable for uncovering long-term effects of trait procrastination on (chronic) disease mediated by poor health-related behavior.
In summary, previous research on the two mediated pathways of the procrastination-health model mainly found support for the role of (chronic) stress in the relationship between trait procrastination and (chronic) disease. However, only short-term effects have been investigated so far. Moreover, longitudinal studies are needed to be able to assess the causal direction of the relationship between trait procrastination, (chronic) stress, and (chronic) disease. Consequently, our study is the first to examine long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress, using a longitudinal design. (Chronic) disease could be measured by a variety of different indicators (e.g., physical symptoms, diabetes, or coronary heart disease). We choose depression and anxiety symptoms as indicators for (chronic) disease because they signal mental health complaints before they manifest as (chronic) diseases. Additionally, depression and anxiety symptoms are two of the most common mental health complaints among students [ 29 , 30 ] and procrastination has been shown to be a significant predictor of depression and anxiety symptoms [ 18 , 31 , 32 , 33 , 34 ]. Until now, the stress-related pathway of the procrastination-health model with depression and anxiety symptoms as the health outcome has only been analyzed in one cross-sectional study that confirmed the predictions of the model [ 35 ].
The aim of our study is to evaluate some of the key assumptions of the procrastination-health model, particularly the relationships between trait procrastination, (chronic) stress, and (chronic) disease over time, surveyed in the following analysis using depression and anxiety symptoms.
In line with the key assumptions of the procrastination-health model, we postulate (see Fig. 2 ):
Procrastination leads to perceived stress over time.
Perceived stress leads to depression and anxiety symptoms over time.
Procrastination leads to depression and anxiety symptoms over time, mediated by perceived stress.
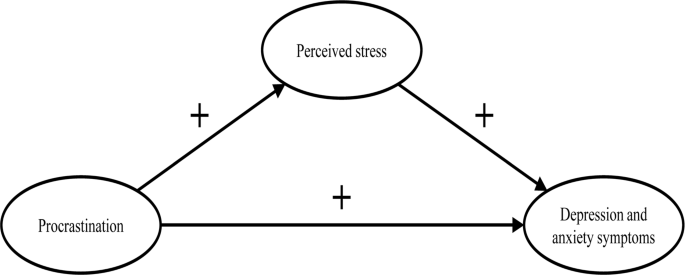
The section of the procrastination-health model we examined
Materials and methods
Our study was part of a health monitoring at a large German university Footnote 1 . Ethical approval for our study was granted by the Ethics Committee of the university’s Department of Education and Psychology. We collected the initial data in 2019. Two occasions followed, each at an interval of six months. In January 2019, we sent out 33,267 invitations to student e-mail addresses. Before beginning the survey, students provided their written informed consent to participate in our study. 3,420 students took part at the first occasion (T1; 10% response rate). Of these, 862 participated at the second (T2) and 392 at the third occasion (T3). In order to test whether dropout was selective, we compared sociodemographic and study specific characteristics (age, gender, academic semester, number of assessments/exams) as well as behavior and health-related variables (procrastination, perceived stress, depression and anxiety symptoms) between the participants of the first wave ( n = 3,420) and those who participated three times ( n = 392). Results from independent-samples t-tests and chi-square analysis showed no significant differences regarding sociodemographic and study specific characteristics (see Additional file 1: Table S1 and S2 ). Regarding behavior and health-related variables, independent-samples t-tests revealed a significant difference in procrastination between the two groups ( t (3,409) = 2.08, p < .05). The mean score of procrastination was lower in the group that participated in all three waves.
The mean age of the longitudinal respondents was 24.1 years ( SD = 5.5 years), the youngest participants were 17 years old, the oldest one was 59 years old. The majority of participants was female (74.0%), 7 participants identified neither as male nor as female (1.8%). The respondents were on average enrolled in the third year of studying ( M = 3.9; SD = 2.3). On average, the students worked about 31.2 h ( SD = 14.1) per week for their studies, and an additional 8.5 h ( SD = 8.5) for their (part-time) jobs. The average income was €851 ( SD = 406), and 4.9% of the students had at least one child. The students were mostly enrolled in philosophy and humanities (16.5%), education and psychology (15.8%), biology, chemistry, and pharmacy (12.5%), political and social sciences (10.6%), veterinary medicine (8.9%), and mathematics and computer science (7.7%).
We only used established and well evaluated instruments for our analyses.
- Procrastination
We adopted the short form of the Procrastination Questionnaire for Students (PFS-4) [ 36 ] to measure procrastination. The PFS-4 assesses procrastination at university as a largely stable behavioral disposition across situations, that is, as a trait. The questionnaire consists of four items (e.g., I put off starting tasks until the last moment.). Each item was rated on a 5-point scale ((almost) never = 1 to (almost) always = 5) for the last two weeks. All items were averaged, with higher scores indicating a greater tendency to procrastinate. The PFS-4 has been proven to be reliable and valid, showing very high correlations with other established trait procrastination scales, for example, with the German short form of the General Procrastination Scale [ 37 , 38 ]. We also proved the scale to be one-dimensional in a factor analysis, with a Cronbach’s alpha of 0.90.
Perceived stress
The Heidelberger Stress Index (HEI-STRESS) [ 39 ] is a three-item measure of current perceived stress due to studying as well as in life in general. For the first item, respondents enter a number between 0 (not stressed at all) and 100 (completely stressed) to indicate how stressed their studies have made them feel over the last four weeks. For the second and third item, respondents rate on a 5-point scale how often they feel “stressed and tense” and as how stressful they would describe their life at the moment. We transformed the second and third item to match the range of the first item before we averaged all items into a single score with higher values indicating greater perceived stress. We proved the scale to be one-dimensional and Cronbach’s alpha for our study was 0.86.
Depression and anxiety symptoms
We used the Patient Health Questionnaire-4 (PHQ-4) [ 40 ], a short form of the Patient Health Questionnaire [ 41 ] with four items, to measure depression and anxiety symptoms. The PHQ-4 contains two items from the Patient Health Questionnaire-2 (PHQ-2) [ 42 ] and the Generalized Anxiety Disorder Scale-2 (GAD-2) [ 43 ], respectively. It is a well-established screening scale designed to assess the core criteria of major depressive disorder (PHQ-2) and generalized anxiety disorder (GAD-2) according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). However, it was shown that the GAD-2 is also appropriate for screening other anxiety disorders. According to Kroenke et al. [ 40 ], the PHQ-4 can be used to assess a person’s symptom burden and impairment. We asked the participants to rate how often they have been bothered over the last two weeks by problems, such as “Little interest or pleasure in doing things”. Response options were 0 = not at all, 1 = several days, 2 = more than half the days, and 3 = nearly every day. Calculated as the sum of the four items, the total scores range from 0 to 12 with higher scores indicating more frequent depression and anxiety symptoms. The total scores can be categorized as none-to-minimal (0–2), mild (3–5), moderate (6–8), and severe (9–12) depression and anxiety symptoms. The PHQ-4 was shown to be reliable and valid [ 40 , 44 , 45 ]. We also proved the scale to be one-dimensional in a factor analysis, with a Cronbach’s alpha of 0.86.
Data analysis
To test our hypotheses, we performed structural equation modelling (SEM) using R (Version 4.1.1) with the package lavaan. All items were standardized ( M = 0, SD = 1). Due to the non-normality of some study variables and a sufficiently large sample size of N near to 400 [ 46 ], we used robust maximum likelihood estimation (MLR) for all model estimations. As recommended by Hu and Bentler [ 47 ], we assessed the models’ goodness of fit by chi-square test statistic, root mean square error of approximation (RMSEA), standardized root mean square residual (SRMR), Tucker-Lewis index (TLI), and comparative fit index (CFI). A non-significant chi-square indicates good model fit. Since chi-square is sensitive to sample size, we also evaluated fit indices less sensitive to the number of observations. RMSEA and SRMR values of 0.05 or lower as well as TLI and CFI values of 0.97 or higher indicate good model fit. RMSEA values of 0.08 or lower, SRMR values of 0.10 or lower, as well as TLI and CFI values of 0.95 or higher indicate acceptable model fit [ 48 , 49 ]. First, we conducted confirmatory factor analysis for the first occasion, defining three factors that correspond to the measures of procrastination, perceived stress, and depression and anxiety symptoms. Next, we tested for measurements invariance over time and specified the measurement model, before testing our hypotheses.
Measurement invariance over time
To test for measurement invariance over time, we defined one latent variable for each of the three occasions, corresponding to the measures of procrastination, perceived stress, and depression and anxiety symptoms, respectively. As recommended by Geiser and colleagues [ 50 ], the links between indicators and factors (i.e., factor loadings and intercepts) should be equal over measurement occasions; therefore, we added indicator specific factors. A first and least stringent step of testing measurement invariance is configural invariance (M CI ). It was examined whether the included constructs (procrastination, perceived stress, depression and anxiety symptoms) have the same pattern of free and fixed loadings over time. This means that the assignment of the indicators to the three latent factors over time is supported by the underlying data. If configural invariance was supported, restrictions for the next step of testing measurement invariance (metric or weak invariance; M MI ) were added. This means that each item contributes to the latent construct to a similar degree over time. Metric invariance was tested by constraining the factor loadings of the constructs over time. The next step of testing measurement invariance (scalar or strong invariance; M SI ) consisted of checking whether mean differences in the latent construct capture all mean differences in the shared variance of the items. Scalar invariance was tested by constraining the item intercepts over time. The constraints applied in the metric invariance model were retained [ 51 ]. For the last step of testing measurement invariance (residual or strict invariance; M RI ), the residual variables were also set equal over time. If residual invariance is supported, differences in the observed variables can exclusively be attributed to differences in the variances of the latent variables.
We used the Satorra-Bentler chi-square difference test to evaluate the superiority of a more stringent model [ 52 ]. We assumed the model with the largest number of invariance restrictions – which still has an acceptable fit and no substantial deterioration of the chi-square value – to be the final model [ 53 ]. Following previous recommendations, we considered a decrease in CFI of 0.01 and an increase in RMSEA of 0.015 as unacceptable to establish measurement invariance [ 54 ]. If a more stringent model had a significant worse chi-square value, but the model fit was still acceptable and the deterioration in model fit fell within the change criteria recommended for CFI and RMSEA values, we still considered the more stringent model to be superior.
Hypotheses testing
As recommended by Dormann et al. [ 55 ], we applied autoregressive time-lagged panel models to test our hypotheses. In the first step, we specified a model (M 0 ) that only included the stabilities of the three variables (procrastination, perceived stress, depression and anxiety symptoms) over time. In the next step (M 1 ), we added the time-lagged effects from procrastination (T1) to perceived stress (T2) and from procrastination (T2) to perceived stress (T3) as well as from perceived stress (T1) to depression and anxiety symptoms (T2) and from perceived stress (T2) to depression and anxiety symptoms (T3). Additionally, we included a direct path from procrastination (T1) to depression and anxiety symptoms (T3). If this path becomes significant, we can assume a partial mediation [ 55 ]. Otherwise, we can assume a full mediation. We compared these nested models using the Satorra-Bentler chi-square difference test and the Akaike information criterion (AIC). The chi-square difference value should either be non-significant, indicating that the proposed model including our hypotheses (M 1 ) does not have a significant worse model fit than the model including only stabilities (M 0 ), or, if significant, it should be in the direction that M 1 fits the data better than M 0 . Regarding the AIC, M 1 should have a lower value than M 0 .
Table 1 displays the means, standard deviations, internal consistencies (Cronbach’s alpha), and stabilities (correlations) of all study variables. The alpha values of procrastination, perceived stress, and depression and anxiety symptoms are classified as good (> 0.80) [ 56 ]. The correlation matrix of the manifest variables used for the analyses can be found in the Additional file 1: Table S3 .
We observed the highest test-retest reliabilities for procrastination ( r ≥ .74). The test-retest reliabilities for depression and anxiety symptoms ( r ≥ .64) and for perceived stress ( r ≥ .54) were a bit lower (see Table 1 ). The pattern of correlations shows a medium to large but positive relationship between procrastination and depression and anxiety symptoms [ 57 , 58 ]. The association between procrastination and perceived stress was small, the one between perceived stress and depression and anxiety symptoms very large (see Table 1 ).
Confirmatory factor analysis showed an acceptable to good fit (x 2 (41) = 118.618, p < .001; SRMR = 0.042; RMSEA = 0.071; TLI = 0.95; CFI = 0.97). When testing for measurement invariance over time for each construct, the residual invariance models with indicator specific factors provided good fit to the data (M RI ; see Table 2 ), suggesting that differences in the observed variables can exclusively be attributed to differences of the latent variables. We then specified and tested the measurement model of the latent constructs prior to model testing based on the items of procrastination, perceived stress, and depression and anxiety symptoms. The measurement model fitted the data well (M M ; see Table 3 ). All items loaded solidly on their respective factors (0.791 ≤ β ≤ 0.987; p < .001).
To test our hypotheses, we analyzed the two models described in the methods section.
The fit of the stability model (M 0 ) was acceptable (see Table 3 ). Procrastination was stable over time, with stabilities above 0.82. The stabilities of perceived stress as well as depression and anxiety symptoms were somewhat lower, ranging from 0.559 (T1 -> T2) to 0.696 (T2 -> T3) for perceived stress and from 0.713 (T2 -> T3) to 0.770 (T1 -> T2) for depression and anxiety symptoms, respectively.
The autoregressive mediation model (M 1 ) fitted the data significantly better than M 0 . The direct path from procrastination (T1) to depression and anxiety symptoms (T3) was significant (β = 0.16; p < .001), however, none of the mediated paths (from procrastination (T1) to perceived stress (T2) and from perceived stress (T2) to depression and anxiety symptoms (T3)) proved to be substantial. Also, the time-lagged paths from perceived stress (T1) to depression and anxiety symptoms (T2) and from procrastination (T2) to perceived stress (T3) were not substantial either (see Fig. 3 ).
To examine whether the hypothesized effects would occur over a one-year period rather than a six-months period, we specified an additional model with paths from procrastination (T1) to perceived stress (T3) and from perceived stress (T1) to depression and anxiety symptoms (T3), also including the stabilities of the three constructs as in the stability model M 0 . The model showed an acceptable fit (χ 2 (486) = 831.281, p < .001; RMSEA = 0.048; SRMR = 0.091; TLI = 0.95; CFI = 0.95), but neither of the two paths were significant.
Therefore, our hypotheses, that procrastination leads to perceived stress over time (H1) and that perceived stress leads to depression and anxiety symptoms over time (H2) must be rejected. We could only partially confirm our third hypothesis, that procrastination leads to depression and anxiety over time, mediated by perceived stress (H3), since procrastination did lead to depression and anxiety symptoms over time. However, this effect was not mediated by perceived stress.
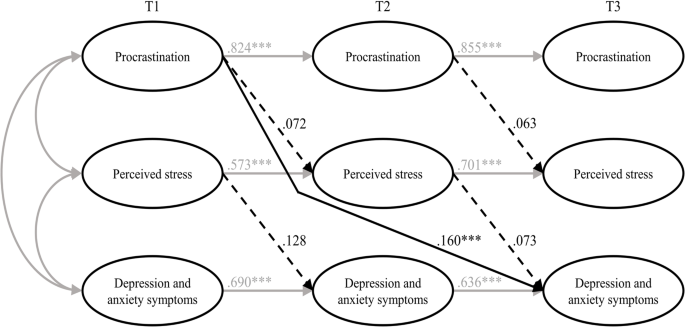
Results of the estimated model including all hypotheses (M 1 ). Note Non-significant paths are dotted. T1 = time 1; T2 = time 2; T3 = time 3. *** p < .001
To sum up, we tried to examine the harmful consequences of procrastination on students’ stress and mental health. Hence, we selected the procrastination-health model by Sirois [ 9 ] as a theoretical foundation and tried to evaluate some of its key assumptions in a temporal perspective. The author assumes that trait procrastination leads to (chronic) disease via (chronic) stress. We chose depression and anxiety symptoms as indicators for (chronic) disease and postulated, in line with the key assumptions of the procrastination-health model, that procrastination leads to perceived stress over time (H1), that perceived stress leads to depression and anxiety symptoms over time (H2), and that procrastination leads to depression and anxiety symptoms over time, mediated by perceived stress (H3). To examine these relationships properly, we collected longitudinal data from students at three occasions over a one-year period and analyzed the data using autoregressive time-lagged panel models. Our first and second hypotheses had to be rejected: Procrastination did not lead to perceived stress over time, and perceived stress did not lead to depression and anxiety symptoms over time. However, procrastination did lead to depression and anxiety symptoms over time – which is in line with our third hypothesis – but perceived stress was not a mediator of this effect. Therefore, we could only partially confirm our third hypothesis.
Our results contradict previous studies on the stress-related pathway of the procrastination-health model, which consistently found support for the role of (chronic) stress in the relationship between trait procrastination and (chronic) disease. Since most of these studies were cross-sectional, though, the causal direction of these effects remained uncertain. There are two longitudinal studies that confirm the stress-related pathway of the procrastination-health model [ 27 , 28 ], but both studies examined short-term effects (≤ 3 months), whereas we focused on more long-term effects. Therefore, the divergent findings may indicate that there are short-term, but no long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress.
Our results especially raise the question whether trait procrastination leads to (chronic) stress in the long term. Looking at previous longitudinal studies on the effect of procrastination on stress, the following stands out: At shorter study periods of two weeks [ 27 ] and four weeks [ 28 ], the effect of procrastination on stress appears to be present. At longer study periods of seven weeks [ 59 ], three months [ 28 ], six months, and twelve months, as in our study, the effect of procrastination on stress does not appear to be present. There is one longitudinal study in which procrastination was a significant predictor of stress symptoms nine months later [ 34 ]. The results of this study should be interpreted with caution, though, because the outbreak of the COVID-19 pandemic fell within the study period, which could have contributed to increased stress symptoms [ 60 ]. Unfortunately, Johansson et al. [ 34 ] did not report whether average stress symptoms increased during their study. In one of the two studies conducted by Fincham and May [ 59 ], the COVID-19 pandemic outbreak also fell within their seven-week study period. However, they reported that in their study, average stress symptoms did not increase from baseline to follow-up. Taken together, the findings suggest that procrastination can cause acute stress in the short term, for example during times when many tasks need to be completed, such as at the end of a semester, but that procrastination does not lead to chronic stress over time. It seems possible that students are able to recover during the semester from the stress their procrastination caused at the end of the previous semester. Because of their procrastination, they may also have more time to engage in relaxing activities, which could further mitigate the effect of procrastination on stress. Our conclusions are supported by an early and well-known longitudinal study by Tice and Baumeister [ 61 ], which compared procrastinating and non-procrastinating students with regard to their health. They found that procrastinators experienced less stress than their non-procrastinating peers at the beginning of the semester, but more at the end of the semester. Additionally, our conclusions are in line with an interview study in which university students were asked about the consequences of their procrastination [ 62 ]. The students reported that, due to their procrastination, they experience high levels of stress during periods with heavy workloads (e.g., before deadlines or exams). However, the stress does not last, instead, it is relieved immediately after these periods.
Even though research indicates, in line with the assumptions of the procrastination-health model, that stress is a risk factor for physical and mental disorders [ 63 , 64 , 65 , 66 ], perceived stress did not have a significant effect on depression and anxiety symptoms in our study. The relationship between stress and mental health is complex, as people respond to stress in many different ways. While some develop stress-related mental disorders, others experience mild psychological symptoms or no symptoms at all [ 67 ]. This can be explained with the help of vulnerability-stress models. According to vulnerability-stress models, mental illnesses emerge from an interaction of vulnerabilities (e.g., genetic factors, difficult family backgrounds, or weak coping abilities) and stress (e.g., minor or major life events or daily hassles) [ 68 , 69 ]. The stress perceived by the students in our sample may not be sufficient enough on its own, without the presence of other risk factors, to cause depression and anxiety symptoms. However, since we did not assess individual vulnerability and stress factors in our study, these considerations are mere speculation.
In our study, procrastination led to depression and anxiety symptoms over time, which is consistent with the procrastination-health model as well as previous cross-sectional and longitudinal evidence [ 18 , 21 , 31 , 32 , 33 , 34 ]. However, it is still unclear by which mechanisms this effect is mediated, as perceived stress did not prove to be a substantial mediator in our study. One possible mechanism would be that procrastination impairs affective well-being [ 70 ] and creates negative feelings, such as shame, guilt, regret, and anger [ 20 , 21 , 22 , 62 , 71 ], which in turn could lead to depression and anxiety symptoms [ 23 , 24 , 25 ]. Other potential mediators of the relationship between procrastination and depression and anxiety symptoms emerge from the behavioral pathway of the procrastination-health model, suggesting that poor health-related behaviors mediate the effect of trait procrastination on (chronic) disease. Although evidence for this is still scarce, the results of one cross-sectional study, for example, indicate that poor sleep quality might mediate the effect of procrastination on depression and anxiety symptoms [ 35 ].
In summary, we found that procrastination leads to depression and anxiety symptoms over time and that perceived stress is not a mediator of this effect. We could not show that procrastination leads to perceived stress over time, nor that perceived stress leads to depression and anxiety symptoms over time. For the most part, the relationships between procrastination, perceived stress, and depression and anxiety symptoms did not match the relationships between trait procrastination, (chronic) stress, and (chronic) disease as assumed in the procrastination-health model. Explanations for this could be that procrastination might only lead to perceived stress in the short term, for example, during preparations for end-of-semester exams, and that perceived stress may not be sufficient enough on its own, without the presence of other risk factors, to cause depression and anxiety symptoms. In conclusion, we could not confirm long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress, as assumed for the stress-related pathway of the procrastination-health model.
Limitations and suggestions for future research
In our study, we tried to draw causal conclusions about the harmful consequences of procrastination on students’ stress and mental health. However, since procrastination is a trait that cannot be manipulated experimentally, we have conducted an observational rather than an experimental study, which makes causal inferences more difficult. Nonetheless, a major strength of our study is that we used a longitudinal design with three waves. This made it possible to draw conclusions about the causal direction of the effects, as in hardly any other study targeting consequences of procrastination on health before [ 4 , 28 , 55 ]. Therefore, we strongly recommend using a similar longitudinal design in future studies on the procrastination-health model or on consequences of procrastination on health in general.
We chose a time lag of six months between each of the three measurement occasions to examine long-term effects of procrastination on depression and anxiety symptoms mediated by perceived stress. However, more than six months may be necessary for the hypothesized effects to occur [ 72 ]. The fact that the temporal stabilities of the examined constructs were moderate or high (0.559 ≤ β ≤ 0.854) [ 73 , 74 ] also suggests that the time lags may have been too short. The larger the time lag, the lower the temporal stabilities, as shown for depression and anxiety symptoms, for example [ 75 ]. High temporal stabilities make it more difficult to detect an effect that actually exists [ 76 ]. Nonetheless, Dormann and Griffin [ 77 ] recommend using shorter time lags of less than one year, even with high stabilities, because of other influential factors, such as unmeasured third variables. Therefore, our time lags of six months seem appropriate.
It should be discussed, though, whether it is possible to detect long-term effects of the stress-related pathway of the procrastination-health model within a total study period of one year. Sirois [ 9 ] distinguishes between short-term and long-term effects of procrastination on health mediated by stress, but does not address how long it might take for long-term effects to occur or when effects can be considered long-term instead of short-term. The fact that an effect of procrastination on stress is evident at shorter study periods of four weeks or less but in most cases not at longer study periods of seven weeks or more, as we mentioned earlier, could indicate that short-term effects occur within the time frame of one to three months, considering the entire stress-related pathway. Hence, it seems appropriate to assume that we have examined rather long-term effects, given our study period of six and twelve months. Nevertheless, it would be beneficial to use varying study periods in future studies, in order to be able to determine when effects can be considered long-term.
Concerning long-term effects of the stress-related pathway, Sirois [ 9 ] assumes that chronic procrastination causes chronic stress, which leads to chronic diseases over time. The term “chronic stress” refers to prolonged stress episodes associated with permanent tension. The instrument we used captures perceived stress over the last four weeks. Even though the perceived stress of the students in our sample was relatively stable (0.559 ≤ β ≤ 0.696), we do not know how much fluctuation occurred between each of the three occasions. However, there is some evidence suggesting that perceived stress is strongly associated with chronic stress [ 78 ]. Thus, it seems acceptable that we used perceived stress as an indicator for chronic stress in our study. For future studies, we still suggest the use of an instrument that can more accurately reflect chronic stress, for example, the Trier Inventory for Chronic Stress (TICS) [ 79 ].
It is also possible that the occasions were inconveniently chosen, as they all took place in a critical academic period near the end of the semester, just before the examination period began. We chose a similar period in the semester for each occasion for the sake of comparability. However, it is possible that, during this preparation periods, stress levels peaked and procrastinators procrastinated less because they had to catch up after delaying their work. This could have introduced bias to the data. Therefore, in future studies, investigation periods should be chosen that are closer to the beginning or in the middle of a semester.
Furthermore, Sirois [ 9 ] did not really explain her understanding of “chronic disease”. However, it seems clear that physical illnesses, such as diabetes or cardiovascular diseases, are meant. Depression and anxiety symptoms, which we chose as indicators for chronic disease, represent mental health complaints that do not have to be at the level of a major depressive disorder or an anxiety disorder, in terms of their quantity, intensity, or duration [ 40 ]. But they can be viewed as precursors to a major depressive disorder or an anxiety disorder. Therefore, given our study period of one year, it seems appropriate to use depression and anxiety symptoms as indicators for chronic disease. At longer study periods, we would expect these mental health complaints to manifest as mental disorders. Moreover, the procrastination-health model was originally designed to be applied to physical diseases [ 3 ]. Perhaps, the model assumptions are more applicable to physical diseases than to mental disorders. By applying parts of the model to mental health complaints, we have taken an important step towards finding out whether the model is applicable to mental disorders as well. Future studies should examine additional long-term health outcomes, both physical and psychological. This would help to determine whether trait procrastination has varying effects on different diseases over time. Furthermore, we suggest including individual vulnerability and stress factors in future studies in order to be able to analyze the effect of (chronic) stress on (chronic) diseases in a more differentiated way.
Regarding our sample, 3,420 students took part at the first occasion, but only 392 participated three times, which results in a dropout rate of 88.5%. At the second and third occasion, invitation e-mails were only sent to participants who had indicated at the previous occasion that they would be willing to participate in a repeat survey and provided their e-mail address. This is probably one of the main reasons for our high dropout rate. Other reasons could be that the students did not receive any incentives for participating in our study and that some may have graduated between the occasions. Selective dropout analysis revealed that the mean score of procrastination was lower in the group that participated in all three waves ( n = 392) compared to the group that participated in the first wave ( n = 3,420). One reason for this could be that those who have a higher tendency to procrastinate were more likely to procrastinate on filling out our survey at the second and third occasion. The findings of our dropout analysis should be kept in mind when interpreting our results, as lower levels of procrastination may have eliminated an effect on perceived stress or on depression and anxiety symptoms. Additionally, across all age groups in population-representative samples, the student age group reports having the best subjective health [ 80 ]. Therefore, it is possible that they are more resilient to stress and experience less impairment of well-being than other age groups. Hence, we recommend that future studies focus on other age groups as well.
It is generally assumed that procrastination leads to lower academic performance, health impairment, and poor health-related behavior. However, evidence for negative consequences of procrastination is still limited and it is also unclear by which mechanisms they are mediated. In consequence, the aim of our study was to examine the effect of procrastination on mental health over time and stress as a possible facilitator of this relationship. We selected the procrastination-health model as a theoretical foundation and used the stress-related pathway of the model, assuming that trait procrastination leads to (chronic) disease via (chronic) stress. We chose depression and anxiety symptoms as indicators for (chronic) disease and collected longitudinal data from students at three occasions over a one-year period. This allowed us to draw conclusions about the causal direction of the effects, as in hardly any other study examining consequences of procrastination on (mental) health before. Our results indicate that procrastination leads to depression and anxiety symptoms over time and that perceived stress is not a mediator of this effect. We could not show that procrastination leads to perceived stress over time, nor that perceived stress leads to depression and anxiety symptoms over time. Explanations for this could be that procrastination might only lead to perceived stress in the short term, for example, during preparations for end-of-semester exams, and that perceived stress may not be sufficient on its own, that is, without the presence of other risk factors, to cause depression and anxiety symptoms. Overall, we could not confirm long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress, as assumed for the stress-related pathway of the procrastination-health model. Our study emphasizes the importance of identifying the consequences procrastination can have on health and well-being and determining by which mechanisms they are mediated. Only then will it be possible to develop interventions that can prevent negative health consequences of procrastination. Further health outcomes and possible mediators should be explored in future studies, using a similar longitudinal design.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
University Health Report at Freie Universität Berlin.
Abbreviations
Comparative fit index
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
Generalized Anxiety Disorder Scale-2
Heidelberger Stress Index
Hypothalamic-pituitary-adrenocortical
Robust maximum likelihood estimation
Short form of the Procrastination Questionnaire for Students
Patient Health Questionnaire-2
Patient Health Questionnaire-4
Root mean square error of approximation
Structural equation modeling
Standardized root mean square residual
Tucker-Lewis index
Lu D, He Y, Tan Y, Gender S, Status. Cultural differences, Education, family size and procrastination: a sociodemographic Meta-analysis. Front Psychol. 2021. https://doi.org/10.3389/fpsyg.2021.719425 .
Article PubMed PubMed Central Google Scholar
Yan B, Zhang X. What research has been conducted on Procrastination? Evidence from a systematical bibliometric analysis. Front Psychol. 2022. https://doi.org/10.3389/fpsyg.2022.809044 .
Sirois FM, Melia-Gordon ML, Pychyl TA. I’ll look after my health, later: an investigation of procrastination and health. Pers Individ Dif. 2003;35:1167–84. https://doi.org/10.1016/S0191-8869(02)00326-4 .
Article Google Scholar
Grunschel C. Akademische Prokrastination: Eine qualitative und quantitative Untersuchung von Gründen und Konsequenzen [Unpublished doctoral dissertation]: Universität Bielefeld; 2013.
Steel P. The Nature of Procrastination: a Meta-Analytic and Theoretical Review of Quintessential Self-Regulatory failure. Psychol Bull. 2007;133:65–94. https://doi.org/10.1037/0033-2909.133.1.65 .
Article PubMed Google Scholar
Corkin DM, Yu SL, Lindt SF. Comparing active delay and procrastination from a self-regulated learning perspective. Learn Individ Differ. 2011;21:602–6. https://doi.org/10.1016/j.lindif.2011.07.005 .
Balkis M, Duru E. Procrastination, self-regulation failure, academic life satisfaction, and affective well-being: underregulation or misregulation form. Eur J Psychol Educ. 2016;31:439–59. https://doi.org/10.1007/s10212-015-0266-5 .
Schulz N. Procrastination und Planung – Eine Untersuchung zum Einfluss von Aufschiebeverhalten und Depressivität auf unterschiedliche Planungskompetenzen [Doctoral dissertation]: Westfälische Wilhelms-Universität Münster; 2007.
Sirois FM. Procrastination, stress, and Chronic Health conditions: a temporal perspective. In: Sirois FM, Pychyl TA, editors. Procrastination, Health, and well-being. London: Academic; 2016. pp. 67–92. https://doi.org/10.1016/B978-0-12-802862-9.00004-9 .
Harriott J, Ferrari JR. Prevalence of procrastination among samples of adults. Psychol Rep. 1996;78:611–6. https://doi.org/10.2466/pr0.1996.78.2.611 .
Ferrari JR, O’Callaghan J, Newbegin I. Prevalence of Procrastination in the United States, United Kingdom, and Australia: Arousal and Avoidance delays among adults. N Am J Psychol. 2005;7:1–6.
Google Scholar
Ferrari JR, Díaz-Morales JF, O’Callaghan J, Díaz K, Argumedo D. Frequent behavioral Delay tendencies by adults. J Cross Cult Psychol. 2007;38:458–64. https://doi.org/10.1177/0022022107302314 .
Day V, Mensink D, O’Sullivan M. Patterns of academic procrastination. JCRL. 2000;30:120–34. https://doi.org/10.1080/10790195.2000.10850090 .
Höcker A, Engberding M, Rist F, Prokrastination. Ein Manual Zur Behandlung Des Pathologischen Aufschiebens. 2nd ed. Göttingen: Hogrefe; 2017.
Kim KR, Seo EH. The relationship between procrastination and academic performance: a meta-analysis. Pers Individ Dif. 2015;82:26–33. https://doi.org/10.1016/j.paid.2015.02.038 .
Khalid A, Zhang Q, Wang W, Ghaffari AS, Pan F. The relationship between procrastination, perceived stress, saliva alpha-amylase level and parenting styles in Chinese first year medical students. Psychol Res Behav Manag. 2019;12:489–98. https://doi.org/10.2147/PRBM.S207430 .
Sirois FM. I’ll look after my health, later: a replication and extension of the procrastination–health model with community-dwelling adults. Pers Individ Dif. 2007;43:15–26. https://doi.org/10.1016/j.paid.2006.11.003 .
Reinecke L, Meier A, Aufenanger S, Beutel ME, Dreier M, Quiring O, et al. Permanently online and permanently procrastinating? The mediating role of internet use for the effects of trait procrastination on psychological health and well-being. New Media Soc. 2018;20:862–80. https://doi.org/10.1177/1461444816675437 .
Westgate EC, Wormington SV, Oleson KC, Lindgren KP. Productive procrastination: academic procrastination style predicts academic and alcohol outcomes. J Appl Soc Psychol. 2017;47:124–35. https://doi.org/10.1111/jasp.12417 .
Feyzi Behnagh R, Ferrari JR. Exploring 40 years on affective correlates to procrastination: a literature review of situational and dispositional types. Curr Psychol. 2022;41:1097–111. https://doi.org/10.1007/s12144-021-02653-z .
Rahimi S, Hall NC, Sticca F. Understanding academic procrastination: a longitudinal analysis of procrastination and emotions in undergraduate and graduate students. Motiv Emot. 2023. https://doi.org/10.1007/s11031-023-10010-9 .
Patrzek J, Grunschel C, Fries S. Academic procrastination: the perspective of University counsellors. Int J Adv Counselling. 2012;34:185–201. https://doi.org/10.1007/s10447-012-9150-z .
Watson D, Clark LA, Carey G. Positive and negative affectivity and their relation to anxiety and depressive disorders. J Abnorm Psychol. 1988;97:346–53. https://doi.org/10.1037//0021-843x.97.3.346 .
Cândea D-M, Szentagotai-Tătar A. Shame-proneness, guilt-proneness and anxiety symptoms: a meta-analysis. J Anxiety Disord. 2018;58:78–106. https://doi.org/10.1016/j.janxdis.2018.07.005 .
Young CM, Neighbors C, DiBello AM, Traylor ZK, Tomkins M. Shame and guilt-proneness as mediators of associations between General Causality orientations and depressive symptoms. J Soc Clin Psychol. 2016;35:357–70. https://doi.org/10.1521/jscp.2016.35.5.357 .
Stead R, Shanahan MJ, Neufeld RW. I’ll go to therapy, eventually: Procrastination, stress and mental health. Pers Individ Dif. 2010;49:175–80. https://doi.org/10.1016/j.paid.2010.03.028 .
Dow NM. Procrastination, stress, and sleep in tertiary students [Master’s thesis]: University of Canterbury; 2018.
Sirois FM, Stride CB, Pychyl TA. Procrastination and health: a longitudinal test of the roles of stress and health behaviours. Br J Health Psychol. 2023. https://doi.org/10.1111/bjhp.12658 .
Hofmann F-H, Sperth M, Holm-Hadulla RM. Psychische Belastungen Und Probleme Studierender. Psychotherapeut. 2017;62:395–402. https://doi.org/10.1007/s00278-017-0224-6 .
Liu CH, Stevens C, Wong SHM, Yasui M, Chen JA. The prevalence and predictors of mental health diagnoses and suicide among U.S. college students: implications for addressing disparities in service use. Depress Anxiety. 2019;36:8–17. https://doi.org/10.1002/da.22830 .
Aftab S, Klibert J, Holtzman N, Qadeer K, Aftab S. Schemas mediate the Link between Procrastination and Depression: results from the United States and Pakistan. J Rat-Emo Cognitive-Behav Ther. 2017;35:329–45. https://doi.org/10.1007/s10942-017-0263-5 .
Flett AL, Haghbin M, Pychyl TA. Procrastination and depression from a cognitive perspective: an exploration of the associations among Procrastinatory Automatic thoughts, rumination, and Mindfulness. J Rat-Emo Cognitive-Behav Ther. 2016;34:169–86. https://doi.org/10.1007/s10942-016-0235-1 .
Saddler CD, Sacks LA. Multidimensional perfectionism and academic procrastination: relationships with Depression in University students. Psychol Rep. 1993;73:863–71. https://doi.org/10.1177/00332941930733pt123 .
Johansson F, Rozental A, Edlund K, Côté P, Sundberg T, Onell C, et al. Associations between procrastination and subsequent Health outcomes among University students in Sweden. JAMA Netw Open. 2023. https://doi.org/10.1001/jamanetworkopen.2022.49346 .
Gusy B, Jochmann A, Lesener T, Wolter C, Blaszcyk W. „Get it done – schadet Aufschieben Der Gesundheit? Präv Gesundheitsf. 2023;18:228–33. https://doi.org/10.1007/s11553-022-00950-4 .
Glöckner-Rist A, Engberding M, Höcker A, Rist F. Prokrastinationsfragebogen für Studierende (PFS): Zusammenstellung sozialwissenschaftlicher items und Skalen. ZIS - GESIS Leibniz Institute for the Social Sciences; 2014.
Klingsieck KB, Fries S. Allgemeine Prokrastination: Entwicklung Und Validierung Einer Deutschsprachigen Kurzskala Der General Procrastination Scale (Lay, 1986). Diagnostica. 2012;58:182–93. https://doi.org/10.1026/0012-1924/a000060 .
Lay CH. At last, my research article on procrastination. J Res Pers. 1986;20:474–95. https://doi.org/10.1016/0092-6566(86)90127-3 .
Schmidt LI, Obergfell J. Zwangsjacke Bachelor?! Stressempfinden Und Gesundheit Studierender: Der Einfluss Von Anforderungen Und Entscheidungsfreiräumen Bei Bachelor- Und Diplomstudierenden Nach Karaseks Demand-Control-Modell. Saarbrücken: VDM Verlag Dr. Müller; 2011.
Kroenke K, Spitzer RL, Williams JB, Löwe B. An Ultra-brief Screening Scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50:613–21. https://doi.org/10.1016/S0033-3182(09)70864-3 .
Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ Primary Care Study. JAMA. 1999;282:1737–44. https://doi.org/10.1001/jama.282.18.1737 .
Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item Depression Screener. Med Care. 2003;41:1284–92.
Kroenke K, Spitzer RL, Williams JB, Monahan PO, Löwe B. Anxiety disorders in Primary Care: prevalence, impairment, Comorbidity, and detection. Ann Intern Med. 2007;146:317–25. https://doi.org/10.7326/0003-4819-146-5-200703060-00004 .
Khubchandani J, Brey R, Kotecki J, Kleinfelder J, Anderson J. The Psychometric properties of PHQ-4 depression and anxiety screening scale among College Students. Arch Psychiatr Nurs. 2016;30:457–62. https://doi.org/10.1016/j.apnu.2016.01.014 .
Löwe B, Wahl I, Rose M, Spitzer C, Glaesmer H, Wingenfeld K, et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disorders. 2010;122:86–95. https://doi.org/10.1016/j.jad.2009.06.019 .
Boomsma A, Hoogland JJ. The robustness of LISREL modeling revisited. In: Cudeck R, Du Toit S, Sörbom D, editors. Structural equation modeling: Present and Future: a festschrift in honor of Karl Jöreskog. Lincolnwood: Scientific Software International; 2001. pp. 139–68.
Hu L, Bentler PM. Fit indices in Covariance structure modeling: sensitivity to Underparameterized Model Misspecification. Psychol Methods. 1998;3:424–53. https://doi.org/10.1037/1082-989X.3.4.424 .
Schermelleh-Engel K, Moosbrugger H, Müller H. Evaluating the fit of structural equation models: test of significance and descriptive goodness-of-fit measures. MPR. 2003;8:23–74.
Hu L, Bentler PM. Cutoff criteria for fit indexes in Covariance structure analysis: conventional criteria Versus New Alternatives. Struct Equ Model. 1999;6:1–55. https://doi.org/10.1080/10705519909540118 .
Geiser C, Eid M, Nussbeck FW, Courvoisier DS, Cole DA. Analyzing true change in Longitudinal Multitrait-Multimethod studies: application of a Multimethod Change Model to Depression and anxiety in children. Dev Psychol. 2010;46:29–45. https://doi.org/10.1037/a0017888 .
Putnick DL, Bornstein MH. Measurement invariance conventions and reporting: the state of the art and future directions for psychological research. Dev Rev. 2016;41:71–90. https://doi.org/10.1016/j.dr.2016.06.004 .
Satorra A, Bentler PM. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66:507–14. https://doi.org/10.1007/BF02296192 .
Geiser C. Datenanalyse Mit Mplus: Eine Anwendungsorientierte Einführung. Wiesbaden: VS Verlag für Sozialwissenschaften; 2010.
Book Google Scholar
Chen F, Curran PJ, Bollen KA, Kirby J, Paxton P. An empirical evaluation of the use of fixed cutoff points in RMSEA Test Statistic in Structural equation models. Sociol Methods Res. 2008;36:462–94. https://doi.org/10.1177/0049124108314720 .
Dormann C, Zapf D, Perels F. Quer- und Längsschnittstudien in der Arbeitspsychologie [Cross-sectional and longitudinal studies in occupational psychology.]. In: Kleinbeck U, Schmidt K-H,Enzyklopädie der Psychologie [Encyclopedia of psychology]:, Themenbereich D, Serie III, Band 1, Arbeitspsychologie [Subject Area, Series D. III, Volume 1, Industrial Psychology]. Göttingen: Hogrefe Verlag; 2010. pp. 923–1001.
Nunnally JC, Bernstein IH. Psychometric theory. 3rd ed. New York: McGraw-Hill; 1994.
Gignac GE, Szodorai ET. Effect size guidelines for individual differences researchers. Pers Indiv Differ. 2016;102:74–8. https://doi.org/10.1016/j.paid.2016.06.069 .
Funder DC, Ozer DJ. Evaluating effect size in Psychological Research: sense and nonsense. Adv Methods Practices Psychol Sci. 2019;2:156–68. https://doi.org/10.1177/2515245919847202 .
Fincham FD, May RW. My stress led me to procrastinate: temporal relations between perceived stress and academic procrastination. Coll Stud J. 2021;55:413–21.
Daniali H, Martinussen M, Flaten MA. A Global Meta-Analysis of Depression, anxiety, and stress before and during COVID-19. Health Psychol. 2023;42:124–38. https://doi.org/10.1037/hea0001259 .
Tice DM, Baumeister RF. Longitudinal study of procrastination, performance, stress, and Health: the costs and benefits of Dawdling. Psychol Sci. 1997;8:454–8. https://doi.org/10.1111/j.1467-9280.1997.tb00460.x .
Schraw G, Wadkins T, Olafson L. Doing the things we do: a grounded theory of academic procrastination. J Educ Psychol. 2007;99:12–25. https://doi.org/10.1037/0022-0663.99.1.12 .
Slavich GM. Life Stress and Health: a review of conceptual issues and recent findings. Teach Psychol. 2016;43:346–55. https://doi.org/10.1177/0098628316662768 .
Phillips AC, Carroll D, Der G. Negative life events and symptoms of depression and anxiety: stress causation and/or stress generation. Anxiety Stress Coping. 2015;28:357–71. https://doi.org/10.1080/10615806.2015.1005078 .
Hammen C. Stress and depression. Annu Rev Clin Psychol. 2005;1:293–319. https://doi.org/10.1146/annurev.clinpsy.1.102803.143938 .
Blazer D, Hughes D, George LK. Stressful life events and the onset of a generalized anxiety syndrome. Am J Psychiatry. 1987;144:1178–83. https://doi.org/10.1176/ajp.144.9.1178 .
Southwick SM, Charney DS. The Science of Resilience: implications for the Prevention and Treatment of Depression. Science. 2012;338:79–82. https://doi.org/10.1126/science.1222942 .
Ingram RE, Luxton DD. Vulnerability-stress models. In: Hankin BL, Abela JR, editors. Development of psychopathology: a vulnerability-stress perspective. Thousand Oaks: Sage; 2005. pp. 32–46.
Chapter Google Scholar
Maercker A. Modelle Der Klinischen Psychologie. In: Petermann F, Maercker A, Lutz W, Stangier U, editors. Klinische psychologie – Grundlagen. Göttingen: Hogrefe; 2018. pp. 13–31.
Krause K, Freund AM. Delay or procrastination – a comparison of self-report and behavioral measures of procrastination and their impact on affective well-being. Pers Individ Dif. 2014;63:75–80. https://doi.org/10.1016/j.paid.2014.01.050 .
Grunschel C, Patrzek J, Fries S. Exploring reasons and consequences of academic procrastination: an interview study. Eur J Psychol Educ. 2013;28:841–61. https://doi.org/10.1007/s10212-012-0143-4 .
Dwyer JH. Statistical models for the social and behavioral sciences. New York: Oxford University Press; 1983.
Cohen JA, Power Primer. Psychol Bull. 1992;112:155–9. https://doi.org/10.1037//0033-2909.112.1.155 .
Ferguson CJ. An effect size primer: a Guide for clinicians and Researchers. Prof Psychol Res Pr. 2009;40:532–8. https://doi.org/10.1037/a0015808 .
Hinz A, Berth H, Kittel J, Singer S. Die zeitliche Stabilität (Test-Retest-Reliabilität) Von Angst Und Depressivität Bei Patienten Und in Der Allgemeinbevölkerung. Z Med Psychol. 2011;20:24–31. https://doi.org/10.3233/ZMP-2010-2012 .
Adachi P, Willoughby T. Interpreting effect sizes when controlling for stability effects in longitudinal autoregressive models: implications for psychological science. Eur J Dev Psychol. 2015;12:116–28. https://doi.org/10.1080/17405629.2014.963549 .
Dormann C, Griffin M. Optimal time lags in Panel studies. Psychol Methods. 2015;20:489–505. https://doi.org/10.1037/met0000041 .
Weckesser LJ, Dietz F, Schmidt K, Grass J, Kirschbaum C, Miller R. The psychometric properties and temporal dynamics of subjective stress, retrospectively assessed by different informants and questionnaires, and hair cortisol concentrations. Sci Rep. 2019. https://doi.org/10.1038/s41598-018-37526-2 .
Schulz P, Schlotz W, Becker P. TICS: Trierer Inventar Zum chronischen stress. Göttingen: Hogrefe; 2004.
Heidemann C, Scheidt-Nave C, Beyer A-K, Baumert J, Thamm R, Maier B, et al. Health situation of adults in Germany - results for selected indicators from GEDA 2019/2020-EHIS. J Health Monit. 2021;6:3–25. https://doi.org/10.25646/8459 .
Download references
Acknowledgements
Not applicable.
Open Access Funding provided by Freie Universität Berlin.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
Division of Prevention and Psychosocial Health Research, Department of Education and Psychology, Freie Universität Berlin, Habelschwerdter Allee 45, 14195, Berlin, Germany
Anna Jochmann, Burkhard Gusy, Tino Lesener & Christine Wolter
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: A.J., B.G., T.L.; methodology: B.G., A.J.; validation: B.G.; formal analysis: A.J., B.G.; investigation: C.W., T.L., B.G.; data curation: C.W., T.L., B.G.; writing–original draft preparation: A.J., B.G.; writing–review and editing: A.J., T.L., B.G., C.W.; visualization: A.J., B.G.; supervision: B.G., T.L.; project administration: C.W., T.L., B.G.; All authors contributed to the article and approved the submitted version.
Corresponding authors
Correspondence to Anna Jochmann or Burkhard Gusy .
Ethics declarations
Ethics approval and consent to participate.
This study was performed in line with the principles of the Declaration of Helsinki. Ethical approval was obtained from the Ethics Committee of the Department of Education and Psychology, Freie Universität Berlin. All methods were carried out in accordance with relevant guidelines and regulations. The participants provided their written informed consent to participate in this study.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Selective dropout analysis and correlation matrix of the manifest variables
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Jochmann, A., Gusy, B., Lesener, T. et al. Procrastination, depression and anxiety symptoms in university students: a three-wave longitudinal study on the mediating role of perceived stress. BMC Psychol 12 , 276 (2024). https://doi.org/10.1186/s40359-024-01761-2
Download citation
Received : 25 May 2023
Accepted : 02 May 2024
Published : 16 May 2024
DOI : https://doi.org/10.1186/s40359-024-01761-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Student health
- Longitudinal study
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
ORIGINAL RESEARCH article
Development of an implementation plan for a school-based multimodal approach for depression and suicide prevention in adolescents.

- 1 GGZ Oost Brabant, Boekel, Netherlands
- 2 113 Suicide Prevention, Amsterdam, Netherlands
- 3 Behavioural Science Institute, Radboud University, Nijmegen, Netherlands
- 4 Child and Adolescent Psychiatry & Psychosocial Care, Amsterdam, Netherlands
- 5 Department of Public and Occupational Health, Amsterdam UMC Location Vrije Universiteit Amsterdam, Amsterdam, Netherlands
- 6 Amsterdam Public Health Research Institute, Health Behaviors & Chronic Diseases, Amsterdam, Netherlands
- 7 Pro Persona, Nijmegen, Netherlands
Strong Teens and Resilient Minds (STORM) is a multimodal, school-based approach for depression and suicide prevention in adolescents that is currently implemented in a region in the Netherlands. The STORM approach will be implemented in new regions in the coming years. This study used the implementation mapping protocol to report on the development of the STORM implementation plan. First, a needs assessment was conducted through semi-structured interviews with stakeholders and brainstorming sessions with regional programme leaders in the two regions that started implementing STORM in 2023. This led to the identification of six main barriers to implementation: high level of demands for schools, insufficient understanding of the programme content, insufficient network collaboration, no perceived relative advantage of STORM by stakeholders, lack of attention to sustainability, and high work pressure. Second, performance and change objectives were formulated based on these barriers. For example, a performance objective for potential providers was that they felt supported by STORM. Third, implementation strategies were selected from theory and translated into practical applications through brainstorming sessions with programme leaders. The following strategies were included in the implementation plan: collaborate with similar initiatives within the region, free up time for STORM tasks, tailor strategies, identify and prepare STORM champions, and promote network weaving. Last, a plan to evaluate the implementation of STORM and the application of the STORM implementation plan was formulated. Planned evaluation research will provide more insight into the usefulness and impact of the STORM implementation plan.
Introduction
Globally, depression and suicide prevalence in adolescents is high and appears to be increasing ( 1 – 8 ). Adolescent depression is associated with poor social well-being, poor school attendance, failure to complete secondary school, depression recurrence, and the onset of other psychiatric disorders ( 9 – 12 ). Moreover, suicide is the fourth leading cause of death among adolescents aged 15–29 worldwide ( 13 ). This stresses the need to implement evidence-based depression and suicide prevention programmes.
Educational settings offer opportunities to reach a large number of adolescents, since most adolescents attend school. Several review studies have found small effects and moderate effects on students’ mental health for universal and indicated school-based depression prevention interventions, respectively ( 14 – 17 ). School-based suicide prevention interventions have shown small positive effects on suicidal ideation and behaviours ( 18 , 19 ). Katz et al. ( 20 ) and Hofstra et al. ( 21 ) have suggested combining several interventions to further increase the efficacy of depression and suicide prevention.
Such an approach has been developed in the Netherlands and is called Strong Teens and Resilient Minds (STORM) ( 22 , 23 ). Currently, the STORM approach consists of four interventions ( 22 , 23 ): (1) universal prevention through mental health lessons in schools, (2) a gatekeeper training (GKT) for school personnel to create a support network around adolescents, (3) early detection of depressive symptoms and suicidality and further assessment and referral when needed, and (4) Op Volle Kracht (OVK, which translates to “at full force”), an indicated depression prevention intervention based on cognitive behavioural group therapy. The STORM approach is science-based, and several programme components have been found to be effective ( 22 , 23 ): The GKT has been found effective at increasing knowledge of suicide prevention and confidence to discuss suicidality ( 24 ). The OVK training has been found effective at reducing depressive symptoms in adolescent ( 25 , 26 ).
Despite the existing evidence on the effectiveness of interventions for mental health promotion, prevention, and treatment, most people affected by mental health problems do not receive appropriate intervention ( 27 ). Therefore, scaling up effective prevention approaches is warranted. As part of the Dutch National Agenda Suicide Prevention 2021–2025 ( 28 ), which states national-level goals and activities in the context of suicide prevention, STORM will be scaled up to a national level. STORM is currently implemented in one region in the Netherlands that has about 250,000 inhabitants. Several new Dutch regions will be financially supported to also implement the approach in the coming years. Higher levels of implementation in various implementation outcomes, such as fidelity or dose, are related to better programme outcomes ( 29 – 31 ). This requires applying strategies that fit the context of new user settings ( 32 ). Therefore, developing an implementation plan in collaboration with stakeholders is essential to enhance the level of implementation and the potential programme outcomes.
The current study reports on the development of an implementation plan for STORM using the implementation mapping protocol, a systematic approach to developing an implementation plan by combining theory and co-creation with stakeholders in practice ( 32 ). Studies reporting on the development of an implementation plan for school-based mental health approaches in preparation for implementation are scarce. While we studied the example case of STORM, our approach to identifying these strategies and our outcomes could inform other school-based mental health approaches as well. This case is of particular interest to others, because of the complexity of STORM considering the multiple components, and because many stakeholders are involved in providing and implementing the approach.
The current study used a qualitative case study design to develop an implementation plan for STORM that was co-created with stakeholders in practice, and was guided by thematic analysis ( 33 ). The report followed the Standards for Reporting Qualitative Research formulated by O’Brien et al. ( 34 ), which was filled in and included in Supplementary File 1 . All participants in this study signed an informed consent form before participation. This study was approved by the Ethics Commission Social Sciences of Radboud University, approval number ECSW-LT-2023-2-2-33415.
The STORM approach
First, mental health lessons are offered by mental healthcare professionals in schools to improve mental health literacy. Second, schoolteachers can undergo GKT, through which they learn to identify adolescents who show signs of suicidal behaviours and how to respond to those students. Third, a screening of students’ depression and suicide risk is conducted by the Public Health Service (PHS, in Dutch: GGD) using the Childhood Depression Inventory 2 ( 35 ) and the Questionnaire Assessing Suicide and Self Injury ( 36 ). Students identified as at risk for suicide are seen within 48 h by Child and Youth Health (CYH) professionals from the PHS for further assessment and referral, if necessary. Students with elevated depressive symptoms based on the Child Depression Inventory 2 are offered the indicated depression prevention intervention called OVK, which is based on cognitive behavioural group therapy ( 23 ). This intervention is usually provided by a duo of a care professionals within the school and a care professional in the youth care domain.
An integral part of STORM is collaboration within the network of care and education for adolescents ( 22 , 23 , 37 ). There are four main partners in this network: secondary and vocational schools, municipalities, PHS, and mental health professionals. Secondary and vocational schools are the settings for all interventions that are part of STORM ( 23 ). Within a region, these schools collaborate with municipalities in educational partnerships in supporting and caring for youth ( 38 ). Also, municipalities financially facilitate the implementation of STORM in practice ( 23 ). While regions can apply for a start-up budget through the Dutch National Agenda Suicide Prevention 2021–2025 subsidised by the Ministry of Health, Welfare, and Sports ( 28 ), municipalities still have to be involved for sustained financing after 2025. A team of mental health professionals provides consultation, training and personnel for carrying out the interventions ( 23 ).
An overview of the regional STORM programme structure, including the tasks of each partner, is provided in the second and third columns of Figure 1 . Stakeholders from education, the PHS, mental health services, and municipalities collaborate in each part of the programme structure. For the current study, we defined four stakeholder categories: regional management, regional programme leaders, policymakers, and service providers. These are also indicated in the first column of Figure 1 .
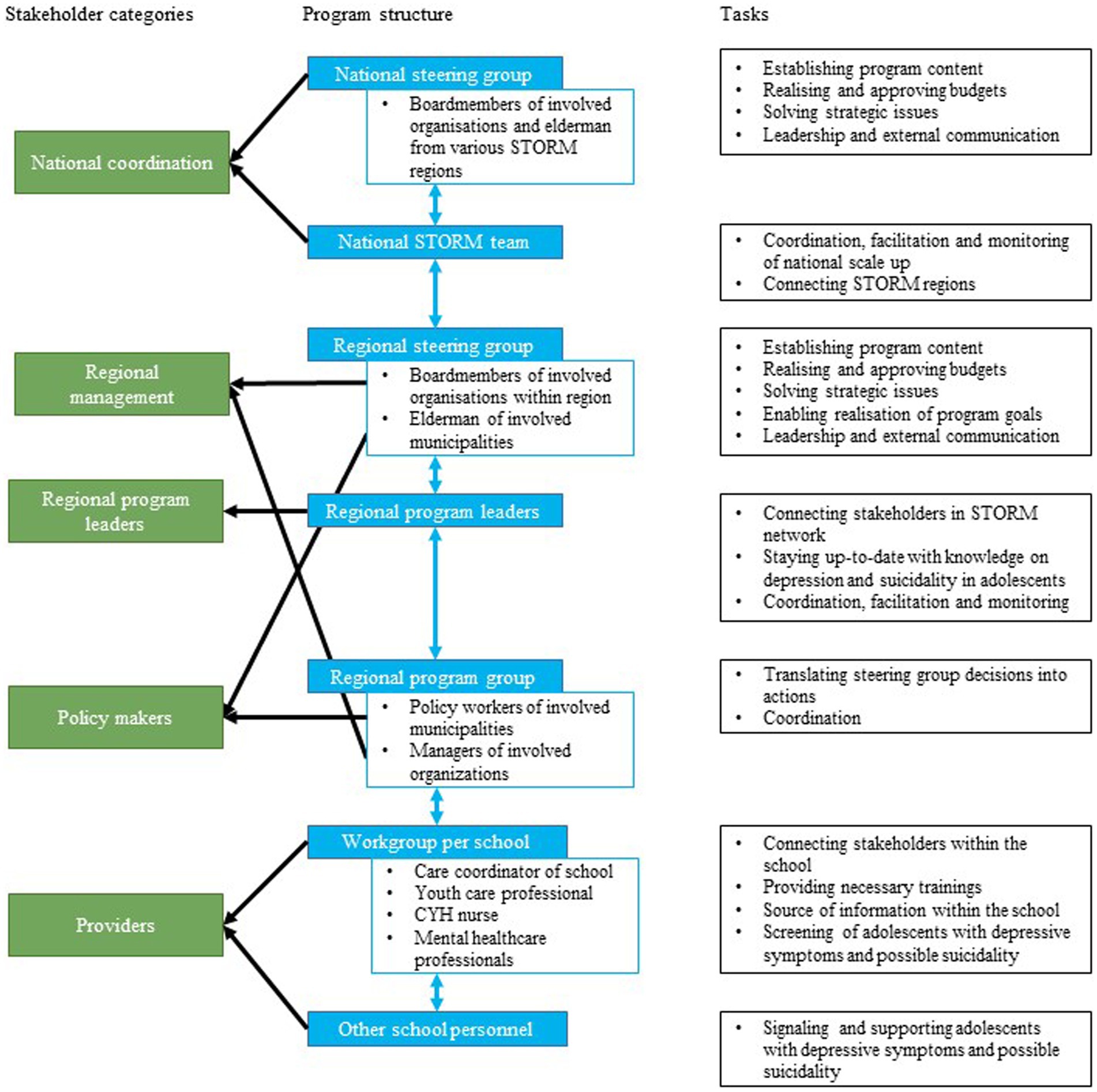
Figure 1 . Overview of regional STORM programme structure.
National scaling up of STORM
As part of the Dutch National Agenda Suicide Prevention 2021–2025 ( 28 ), STORM is being scaled-up to new regions in the Netherlands between 2021 and 2025. Interested regions could apply for a start-up implementation budget. The first two regions to receive this budget were selected in December 2022 and started implementing STORM in the academic year of 2023–2024 ( 39 ). To apply for the budget, the regions had to prepare for implementation and had thus already initiated several implementation strategies before the start of the current study. Furthermore, existing STORM regions have already introduced several implementation strategies in recent years. These strategies have already been formulated and provided to the new regions. An overview of the existing implementation strategies can be found in Supplementary File 2 . The current study seeked to identify additional strategies from the literature that can help to overcome implementation barriers.
Theoretical background
The tasks of implementation mapping (IM) described by Fernandez et al. ( 32 ) offer a systematic approach to developing an implementation plan by combining theory and co-creation with stakeholders in practice. IM has previously helped to identify implementation strategies for various preventive interventions and programmes ( 40 – 46 ). The five tasks of IM are the following: (1) conduct an implementation needs assessment to identify barriers and facilitators for implementation, (2) identify adoption and implementation outcomes, performance objectives, and change objectives, (3) select theoretical methods and design implementation strategies, (4) produce implementation protocols and materials, and (5) evaluate implementation outcomes ( 32 ).
We used the Consolidated Framework for Implementation Research (CFIR) from Damschroder et al. ( 47 ) to identify barriers to and facilitators for implementation in Task 1. The CFIR describes constructs in five domains to consider as potential barriers or facilitators. First, the innovation domain, which includes constructs related to the innovation being implemented. Second is the inner setting into which the innovation is implemented. Third is the outer setting within which the inner setting exists. The fourth domain concerns individuals and pertains to the roles and characteristics of individuals involved in the innovation being implemented. The last domain implementation process consists of constructs related to the activities and strategies used to implement the innovation ( 47 ).
For the selection of theoretical implementation strategies in Task 3, Powell, Waltz ( 48 ) compiled a list of 73 implementation strategies based on the results of the Expert Recommendations for Implementing Change (ERIC) study. Recently, this compilation has been adapted to improve its utility in educational settings in the School Implementation Strategies, Translating ERIC Resources (SISTER) Project ( 49 ). This project resulted in a list of 75 school-adapted implementation strategies. Both the ERIC and SISTER compilations guided the selection of strategies in this study.
Below, we specify our study procedures in terms of sample and recruitment, data collection, and data analysis conducted for each of the five IM tasks. An overview of our procedures for each task is described in Figure 2 .
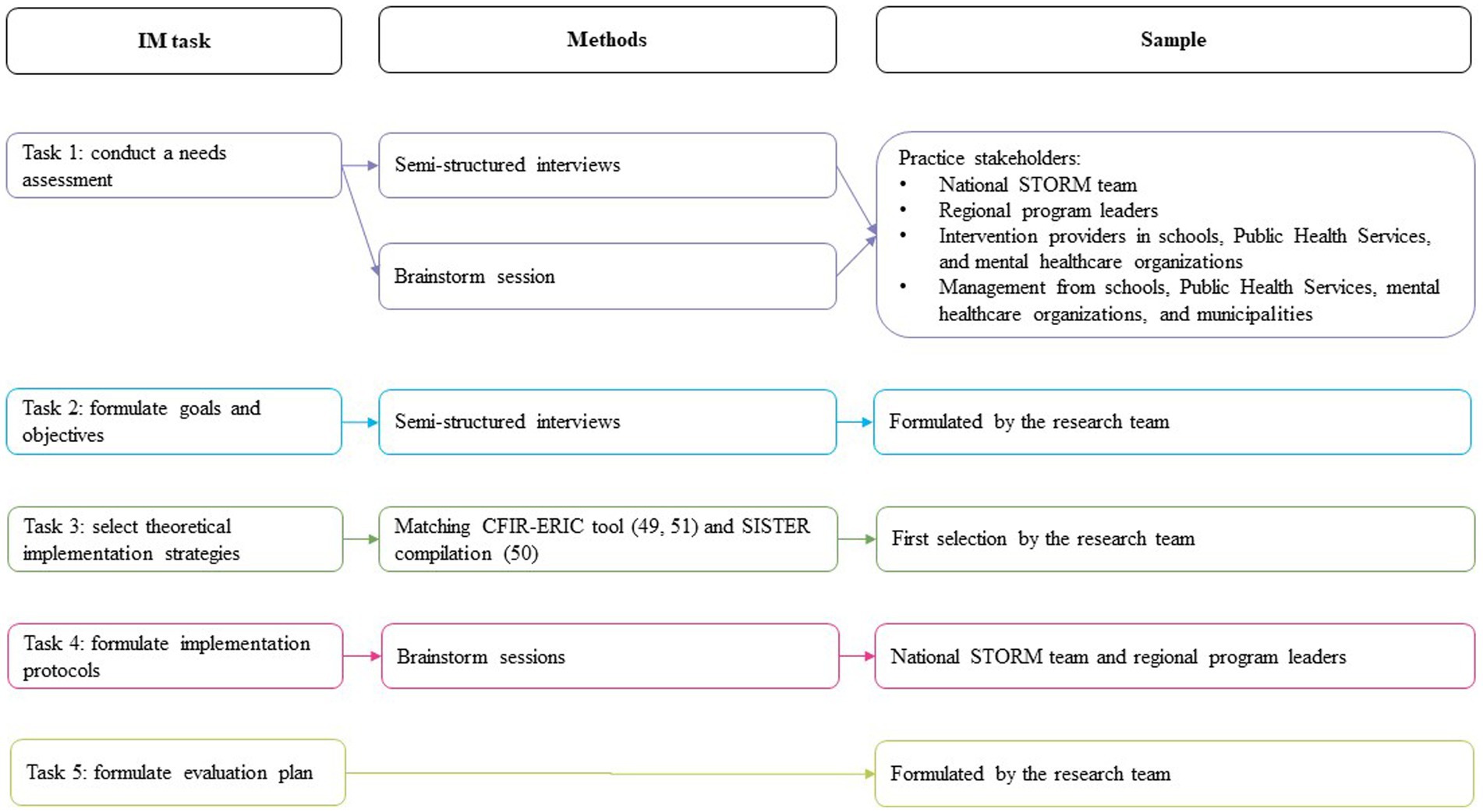
Figure 2 . Overview of procedures and sample per IM task.
Task 1: conduct a needs assessment
The needs assessment helps to identify important actors and potential barriers to and facilitators for implementation ( 32 ). For this, we conducted semi-structured interviews of approximately half an hour in February and March 2023. Study participants were selected from the region that has already implemented STORM (region 1) and two regions that were planning to implement STORM (regions 2 and 3) using purposive snowball sampling. First, we invited the national STORM team and regional programme leaders ( n = 6) for interviews. Next, they helped to identify and contact other relevant stakeholders within the regions. We aimed to represent all stakeholder groups, and reached out to management and intervention providers from schools ( n = 9), the PHS ( n = 5), mental health organisations ( n = 5), and municipalities ( n = 4). Additionally, we invited mentors from secondary schools that had already implemented STORM ( n = 2) for interviews, because mentors from secondary schools in the new regions had not yet been informed about the STORM approach. Participants were included until data saturation was reached, which meant that two researchers (KJ and CG) agreed that the last two interviews did not lead to new information. Researchers met with the national coordinators and regional programme leaders prior to the interviews to discuss which other stakeholders to include in the study. Researchers did not meet with any of the other participants prior to the interviews. The researchers’ characteristics did not influence the research questions, approach, methods, results, or transferability.
The interviews followed an interview guide based on the updated CIFR ( 47 ). The topics included STORM characteristics (example question: what is your perspective on STORM?) and barriers and facilitators (example question: what are things you think could complicate the implementation of STORM?), as well as the sub-topics Outer Setting, Inner Setting, Individuals, and Implementation Process. The full topic list is added in Supplementary File 3 . Interviews were conducted by two researchers (KJ & CG) and audio-recorded. KJ was a PhD student at the time of the study with previous experience in conducting and analysing qualitative research. CG was a bachelor student and intern at the time of the study with no previous experience in qualitative research. The recordings were transcribed verbatim. After the interviews, a short summary was sent to the participants for verification.
To draw up a codebook, three researchers (KJ, CG, and FN) analysed six of the 20 interviews using open coding in Atlas.ti. FN (PhD) has previous experience in conducting and analysing qualitative research. Two researchers (KJ & FN) ordered the codes under the five major domains of the CFIR framework ( 47 ) and then combined them into overarching codes using axial coding. The complete codebook can be found in Supplementary File 4 . Next, two researchers (KJ & CG) separately coded three transcripts, after which the coding was compared and variations in coding were discussed until both researchers agreed. Subsequently, all interview transcripts were analysed using deductive coding. Finally, the researchers analysed the coded data to identify barriers to and facilitators for the implementation of STORM in new regions.
Two researchers (KJ and FN) presented the identified barriers to four programme leaders from regions 2 and 3 and two stakeholders who had been involved in the implementation of STORM in region 1 during a brainstorming session in May 2023. We asked these participants to indicate, on a scale from 1 to 5 per barrier, whether they thought a barrier required immediate action or not using Mentimeter. The results of this brainstorming are available in Supplementary File 5 (in Dutch). Barriers that were scored higher than 3.5 were selected, while barriers that were scored lower than 2.5 were not. For barriers that were scored between 2.5 and 3.5, a group discussion determined whether the barrier was selected.
Tasks 2, 3, and 4: formulate goals, objectives, implementation strategies, and implementation protocols
We formulated performance objectives based on the most important barriers identified in Task 1. For each performance objective, we formulated change objectives across five determinants based on the example of Kang and Foster ( 46 ): knowledge, awareness, skills, outcome expectancy, and self-efficacy. We chose this example, because it was the most complete objectives matrix we found.
Next, we selected theoretical implementation strategies to achieve the change objectives. First, for determinants that match the first-version CFIR constructs ( 47 ), strategies were identified using the CFIR-ERIC tool ( 48 , 50 ). These strategies were then compared to the adapted compilation of ERIC implementation strategies for school-based implementation, SISTER ( 49 ), to identify strategies that are suitable for school-based implementation projects. Then, for determinants that did not fit the first-version CFIR constructs, suitable strategies were selected from the SISTER strategies ( 49 ).
A second round of brainstorming sessions was hosted in May 2023, one session with two national coordinators and one with four regional programme leaders. In both sessions, the main author (KJ) presented identified strategies for the selected barriers. Participants first discussed which of the identified strategies overlapped with existing implementation strategies. For the remaining strategies, participants discussed the extent to which they were realistic and relevant for practice. The implementation strategies that were considered both realistic and relevant for practice by national coordinators and regional programme leaders were selected for the implementation plan. If participants did not reach consensus about how realistic or relevant a strategy would be, the main author (KJ) made the final decision to include or exclude the strategy. A detailed description of our selection process can be found in Supplementary File 2 . Next, the selected strategies were translated into practical applications in collaboration with the programme leaders from regions 2 and 3. The applications were reported following the recommendations for reporting implementation strategies by Proctor et al. ( 51 ). The implementation strategies found in the current study were added to the STORM implementation guide developed by the national STORM team. Besides implementation strategies, this document contains a detailed description of the programme components and programme structure of STORM. All future STORM regions will be offered this guide to aid their implementation efforts.
Task 5: develop an evaluation plan
Based on the implementation plan, KJ and FN developed a plan to evaluate the implementation of STORM, as well as the application of the implementation plan in practice.
Twenty stakeholders were interviewed. Stakeholders were included until data saturation was reached. Their characteristics are presented in Table 1 . Most participants had a coordinating role in the project, followed by providers, management, and policymakers. The number of participants per organisation type were spread evenly, except for municipalities, which were represented by only two participants.
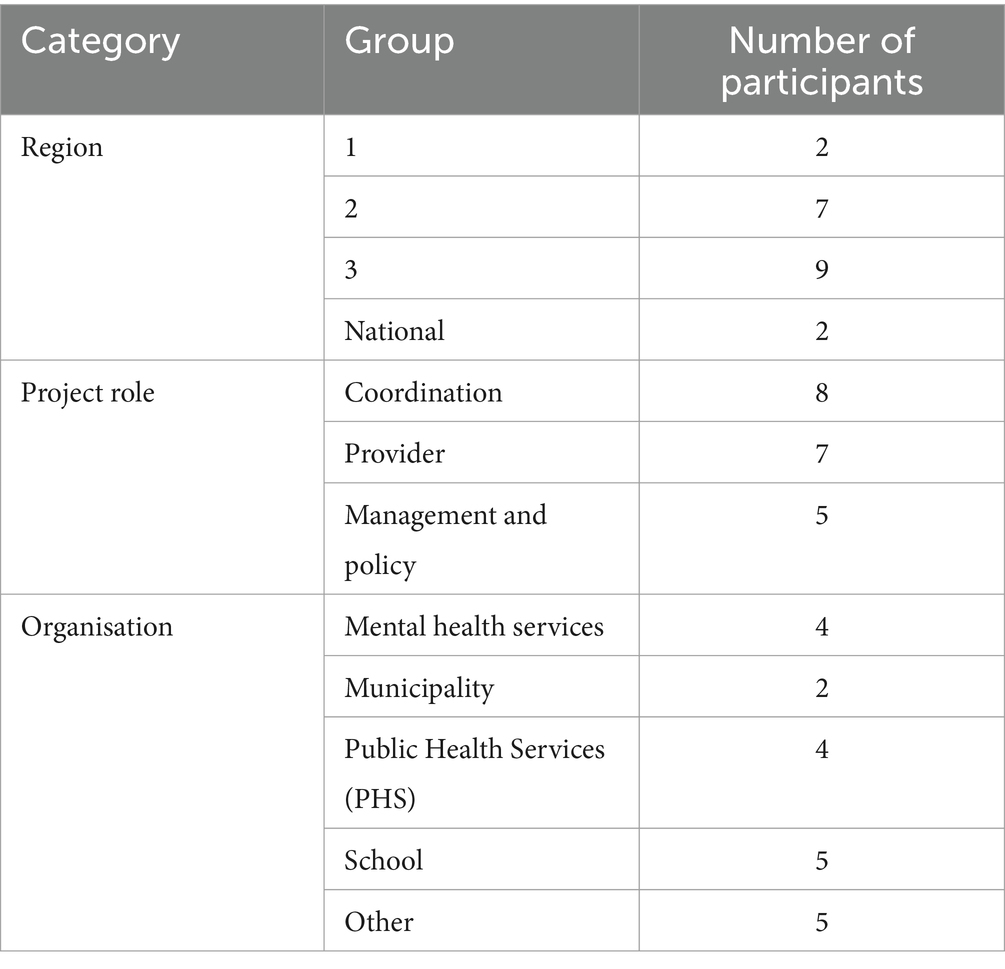
Table 1 . Participant characteristics.
We identified 21 barriers to and 13 facilitators for the implementation of STORM in new regions. An overview of all identified barriers and facilitators can be found in Supplementary File 6 . These determinants include CFIR constructs and barriers that did not match the CFIR constructs. In the first brainstorming session with programme leaders, five barriers were selected for which implementation strategies should be identified. An overview of these barriers is presented in Table 2 .
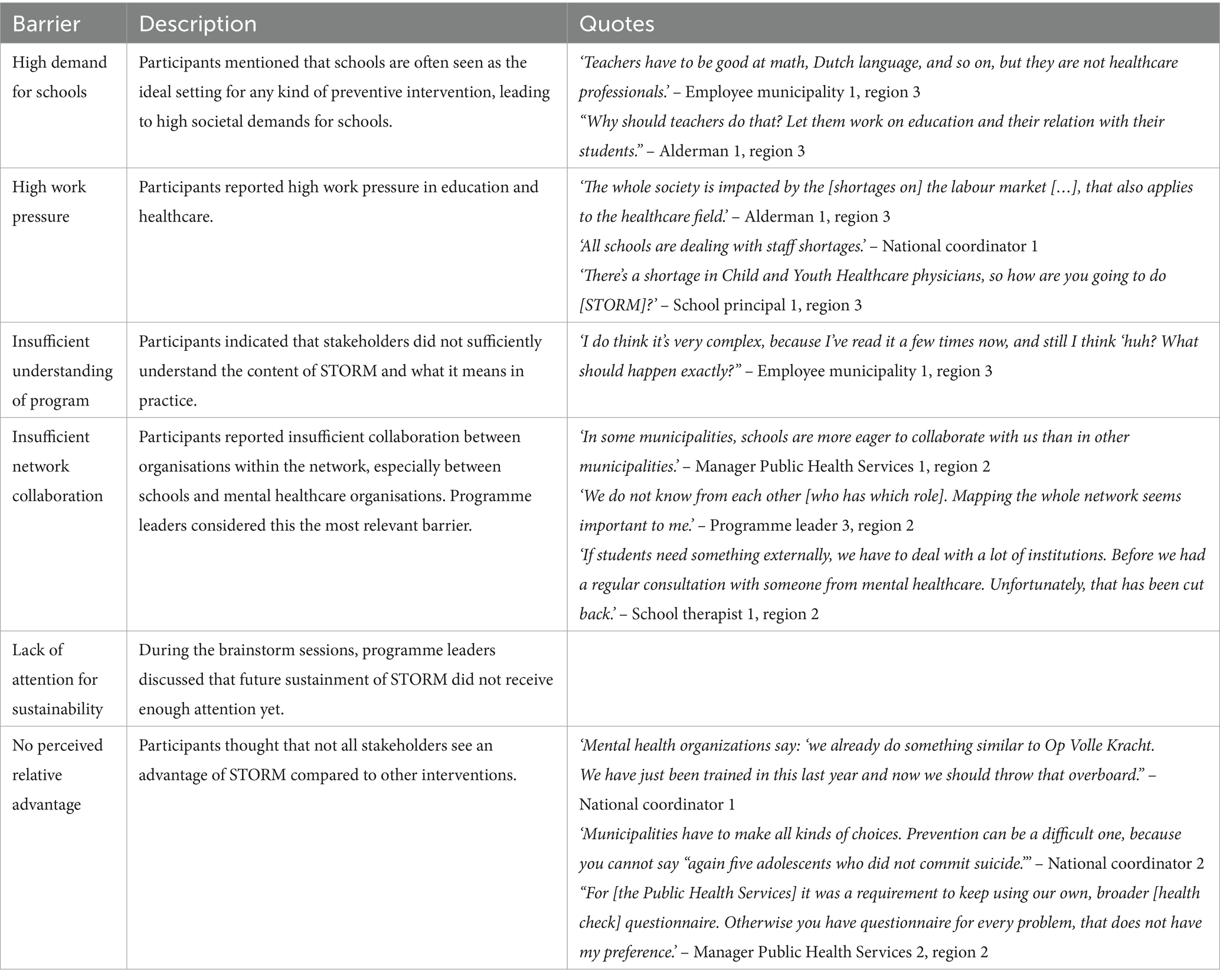
Table 2 . Barrier descriptions.
Multiple participants mentioned that schools are seen as the ideal setting for prevention, not only regarding mental health, but also for prevention of obesity or smoking. This leads to a high demand for schools. For example, one of the regional program leaders mentioned that “many societal developments are occurring and often it’s the schools who have to solve it .” Related to this, most participants recognised high work pressure in both education and healthcare as an important barrier for implementing a new approach. A school principal indicated that “it is an important theme, but honestly I do not have the people, the time, and the money to properly implement STORM.”
Another important issue raised by participants was that, at the time of the interviews, they, nor their colleagues, sufficiently understood the content of the STORM approach and what it means in practice. A school therapist mentioned, for example, that they “still need to receive a lot of information .” Moreover, participants thought that not all stakeholders saw added value in STORM compared to other interventions. A national coordinator indicated that “[organizations] struggle to de-implement [what they were already doing] to implement of STORM.”
It was also noted by some participants that network collaboration required improvement, especially between schools and mental healthcare services. A manager in mental healthcare mentioned that “education sometimes complains: ‘[mental healthcare organizations] do some test, but they never refer back to us’,” while a school therapist mentions that “collaboration [with mental healthcare organizations] does not exist in our school.”
Additional to the interview results, lack of attention to the sustainability of STORM in the current implementation efforts was identified as a barrier during the brainstorming sessions. Programme leaders felt that long-term sustainability was not receiving enough attention yet from stakeholders involved.
For each barrier selected in Task 1, we formulated performance and change objectives. The performance and change objectives are listed per stakeholder category in Table 3 . For example, a performance objective for programme leaders related to the barrier ‘insufficient network collaboration’ and was that they should stimulate the development of sustainable partnerships between involved organisations. Change objectives for this performance objective were formulated under skills (i.e., able to connect organisations within the STORM network) and self-efficacy (i.e., are confident that they are able to connect organisations within the STORM network).
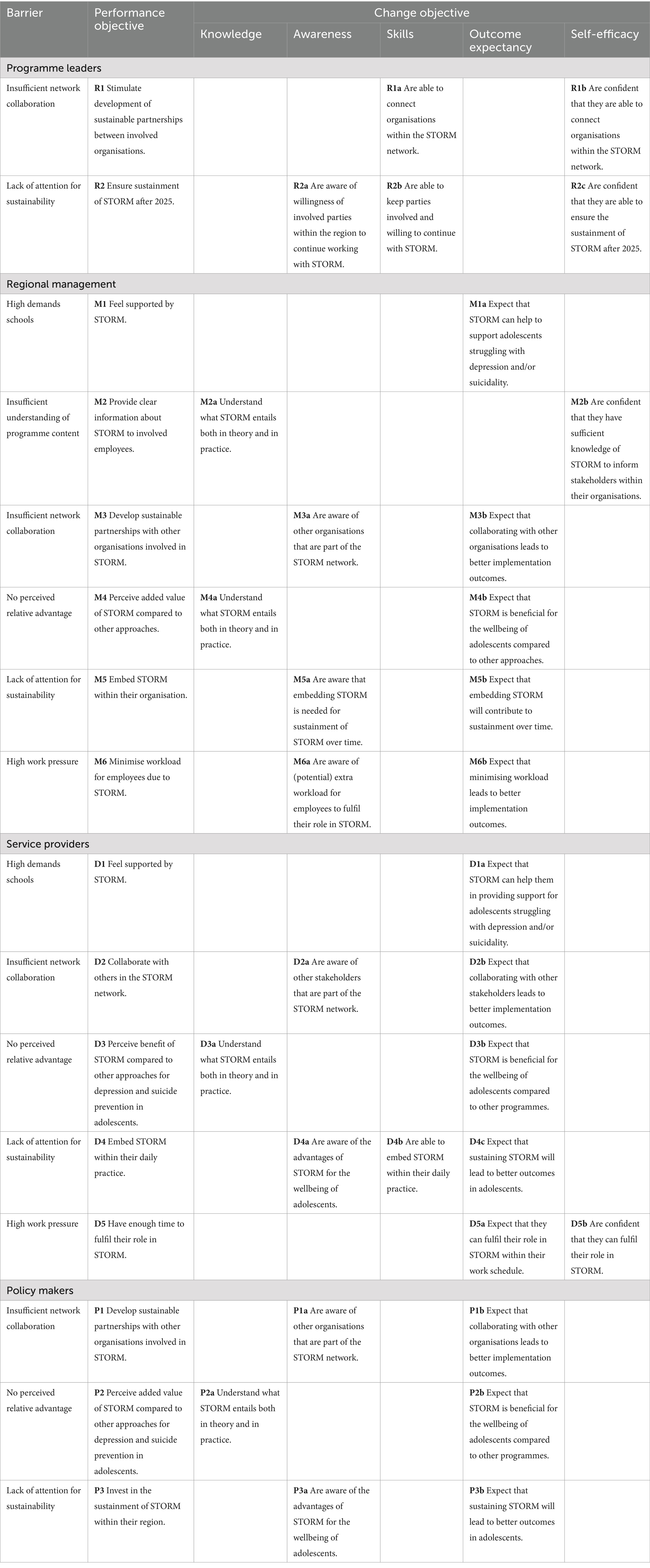
Table 3 . Matrix of change.
Not all barriers were relevant for each stakeholder category. ‘Partnerships and connections’ and ‘Sustainability’ were relevant for all categories, because all stakeholders are part of the STORM network, and the sustainable implementation of STORM should be achieved for all categories. ‘Relative advantage’ was not relevant for the programme leaders, because this is not a barrier for this stakeholder category based on the interviews. Since only the schools, the PHS, and mental healthcare organisations are involved in implementing STORM, the barriers ‘High demand for schools’ and ‘High work pressure’ were only relevant to these stakeholder categories. Finally, ‘Insufficient understanding of programme content’ was regarded as a relevant barrier for management only, because management has the final decision to participate in STORM, and thus needs to be well informed of the content.
Tasks 3 and 4
To address the performance and change objectives formulated in Task 2, 14 implementation strategies were selected using the CFIR-ERIC tool and SISTER that matched the barriers identified ( 49 , 50 ). Using the second round of brainstorming sessions with national coordinators and regional programme leaders, five implementation strategies were deemed relevant and realistic for practice: ‘pruning competing initiatives’, ‘change/alter environment’, ‘tailor strategies’, ‘identify and prepare champions’, and ‘promote network weaving’ ( 49 ). We translated these to practical applications and report on the strategies in Table 4 following the recommendations of Proctor et al. ( 51 ). The first strategy described is ‘collaborate with similar initiatives’, in which the idea is that regional program leaders actively identify other mental health school-based initiatives that are (being) implemented in their region, and look for ways to collaborate in the implementation process. The goal is to relieve the pressure on schools and minimise extra workload for service providers. Second is ‘free up time for STORM tasks’, in which organisation management allocate time to for implementing and executing STORM, while program leaders reserve budget to support organisations in doing so. Third is ‘tailor strategies’, meaning programme leaders adapt their communication style and message about STORM to the specific needs of various stakeholders, with the aim of improving adoption. Fourth is ‘identify and prepare STORM champions’, which entails both identifying and supporting individuals within involved organisations that are enthusiastic about the approach. The goal is to promote sustainment within those organisations through these individuals. Last is ‘regional network weaving’ through developing a social map of the organisations and individuals involved in STORM, and organising a joint kick-off session for those organisations and individuals.
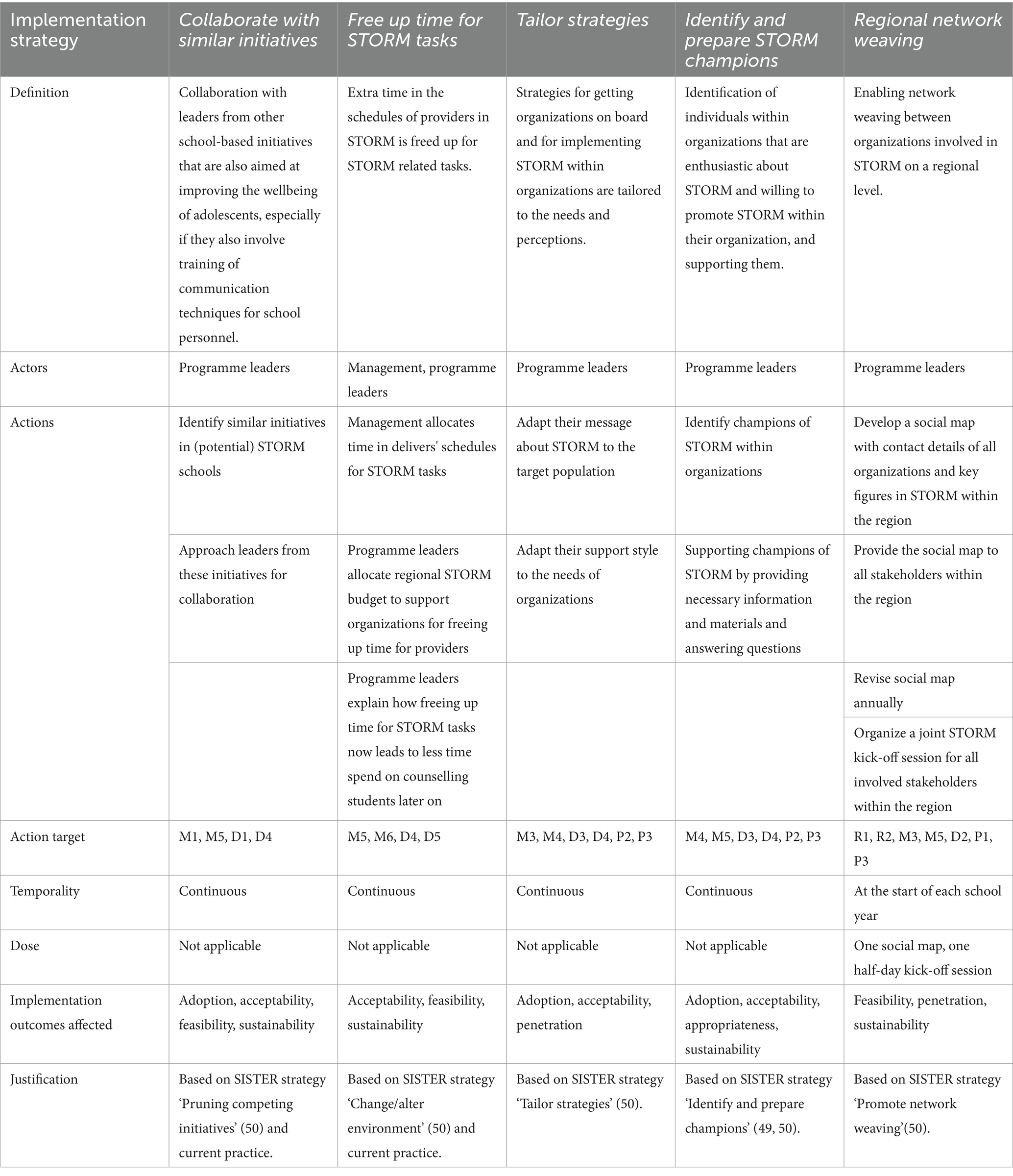
Table 4 . Implementation strategies
In the final task, we developed a plan to evaluate the implementation of STORM in the new regions, as well as the application of the implementation plan over the course of two academic years. We identified outcomes from the implementation outcomes defined by Proctor et al. ( 52 ) and process evaluation guidelines from Moore at al. ( 53 ) and Saunders et al. ( 54 ). In Table 5 , we summarise the outcomes for the implementation of STORM, including definitions, and how and when the outcomes will be measured. Providers, regional management, and policymakers will be involved in the evaluation of the implementation process through a survey and interviews at multiple time points. The measurement instruments to be used in the survey comprise a shortened version of the Acceptability of Intervention Measure, Intervention Appropriateness Measure, and Feasibility of Intervention Measure from Weiner et al. ( 55 ), and the Normalisation Measure Development Questionnaire ( 56 ). In Table 6 , we summarise the outcomes for the application of the implementation plan, including definitions of the outcomes, and how and when the outcomes will be measured. Programme leaders and programme groups (see Figure 1 ) will be involved in the evaluation through a checklist of implementation strategies and focus group sessions. Additionally, we will analyse the administrative data for both evaluations.
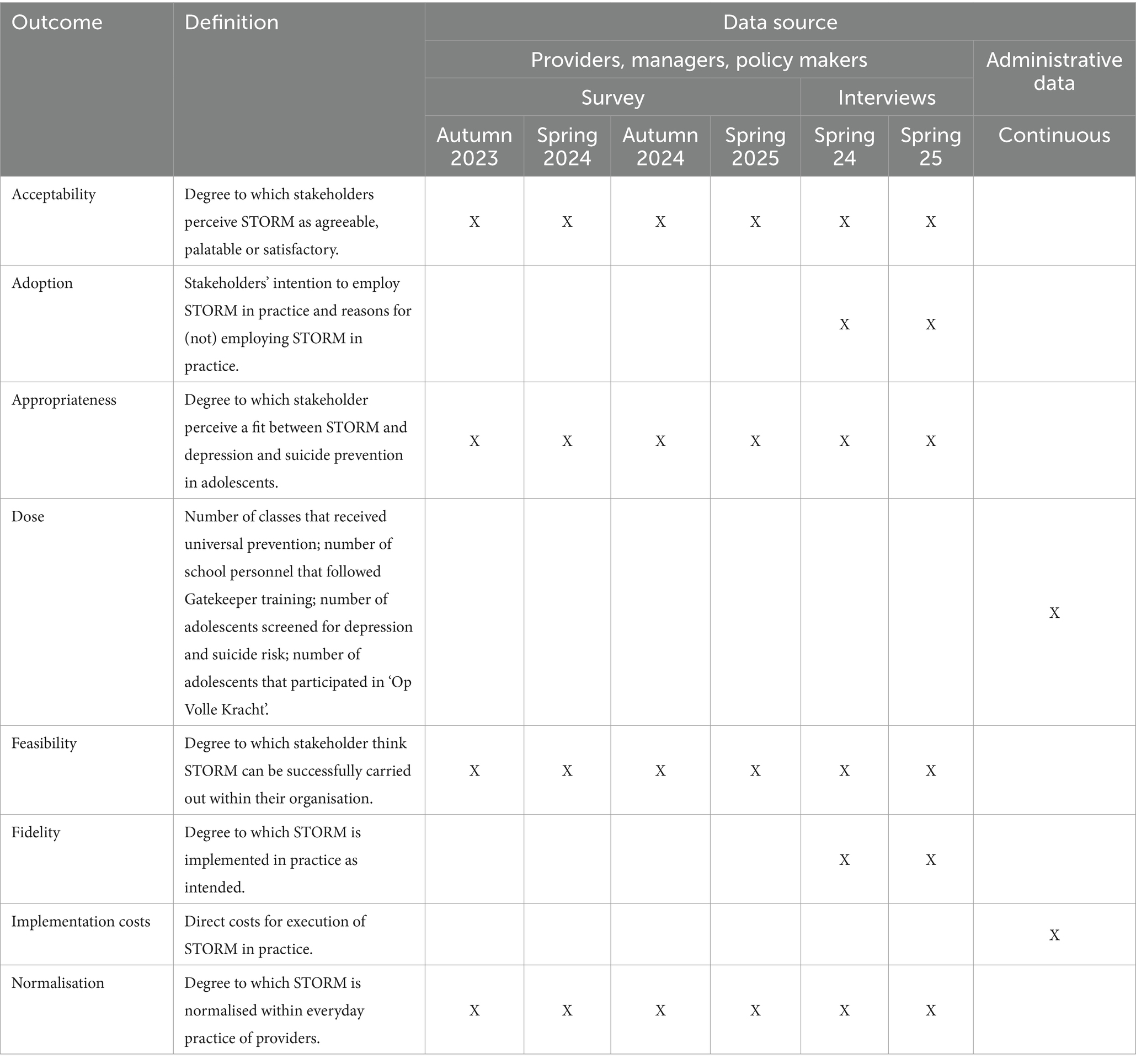
Table 5 . Evaluation plan for the implementation of STORM.
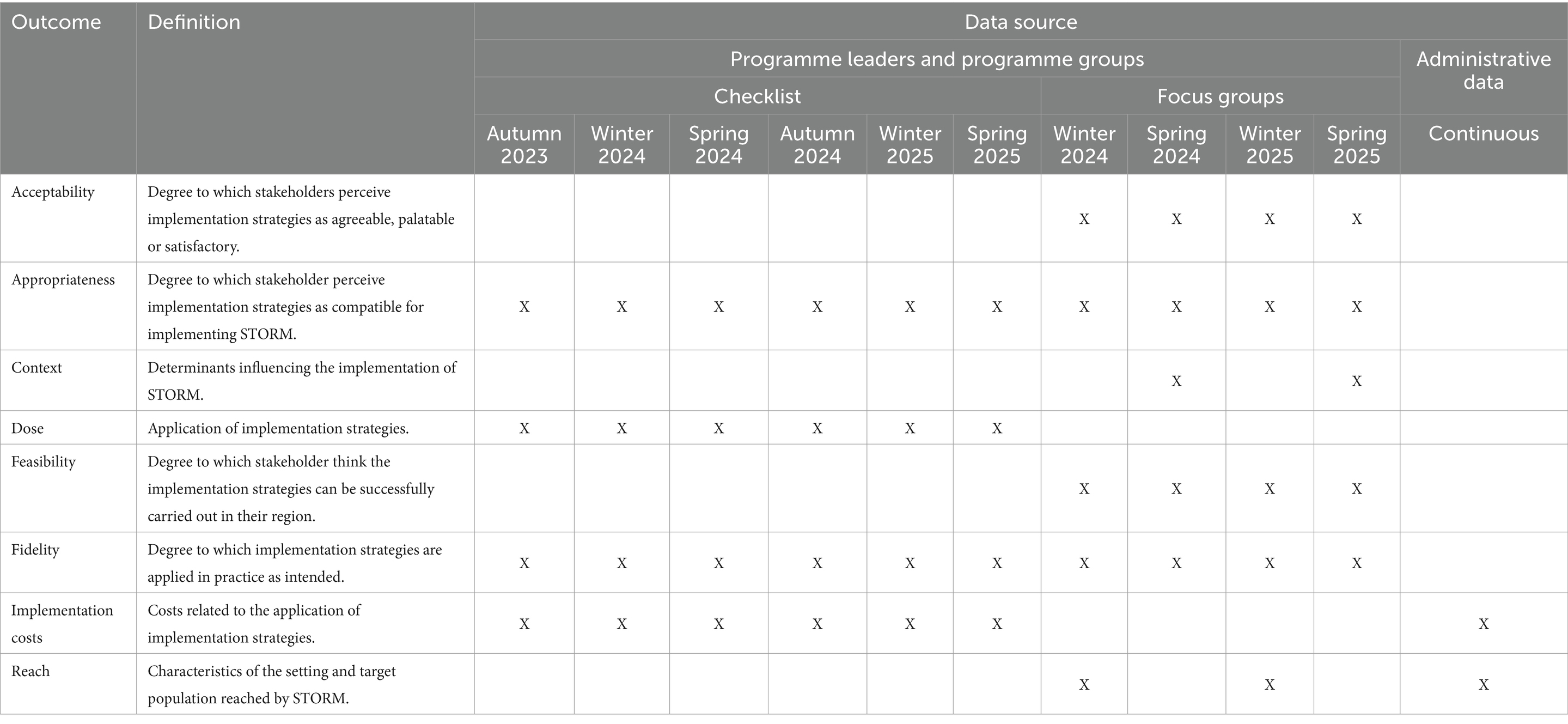
Table 6 . Evaluation plan for the application of the implementation plan.
This study aimed to develop an implementation plan for a school-based approach to depression and suicide prevention. To our knowledge, this is the first study reporting on the development of an implementation plan for school-based mental health interventions. The IM tasks from Fernandez et al. ( 32 ) helped us to combine practical needs and perceptions with theoretical strategies. We identified six main barriers to implementation, on the basis of which we formulated performance and change objectives. We found five new implementation strategies to achieve these objectives. Lastly, we developed a plan to evaluate the implementation of STORM in new regions over the course of two school years.
One of the most relevant barriers to implementation of STORM that we found was limited network collaboration within regions, while network collaboration is an essential part of the STORM approach ( 22 , 23 , 37 ). A study into determinants for the screening and subsequent referral to the OVK revealed that even in the region where STORM has been implemented for years, collaboration between organisations involved in STORM is not optimal ( 57 ). This led us to the selection of several ERIC strategies categorised under ‘develop stakeholder interrelationships’ aimed at improving network collaboration ( 58 ). The implementation evaluation will determine whether these strategies indeed helped us increase network collaboration.
Some of the identified barriers were also some of the most frequently mentioned barriers for other school-based mental health interventions ( 59 ), including ‘insufficient understanding among stakeholders of programme content’ and ‘insufficient network collaboration’. However, costs and the availability of resources, which are often reported as barriers to implementation ( 59 ), were not identified as barriers in the current study. The fact that these factors were not discussed in any of the interviews is most likely due to the implementation budget that regions receive to implement STORM ( 28 ). However, this is only a start-up budget that can only be provided to a limited number of regions. Moreover, lack of funding or financial resources was identified as a barrier to sustaining school-based mental health interventions ( 60 ). Therefore, keeping track of implementation costs is relevant and has been included as an outcome in our evaluation plan.
We selected implementation strategies based on how realistic and relevant the STORM programme leaders thought they were. In a study by Lyon et al. ( 61 ), school-based consultants who provided social, emotional, and mental health services rated the feasibility and importance of all SISTER strategies. Most strategies we selected were also rated important in this study ( 61 ). Yet, we included some strategies which were rated low on feasibility in the study from Lyon et al. ( 61 ), including ‘collaboration with similar initiatives’, ‘use advisory boards and workgroups’, and ‘promote network weaving’, because they were considered realistic and relevant by the program leaders. These different perceptions might be explained by the difference in the stakeholders involved: we spoke with programme leaders, whereas Lyon et al. ( 61 ) consulted stakeholders within schools. However, these differences might also indicate the importance of context when considering the feasibility of an implementation strategy. Our evaluation of the implementation strategies should provide more insight into this difference.
The goal of the implementation plan developed in the current study is to improve the level of implementation of STORM in new regions in the Netherlands. We selected several implementation strategies that were found in the literature to have a positive effect on programme adoption and fidelity, including ‘conduct ongoing training’, ‘identify and prepare champions’, ‘use train-the-trainer strategies’, and ‘facilitation/problem solving’ ( 62 ). Still, knowledge about the mechanisms by which implementation strategies target their linked barriers, as well as about the effectiveness of most strategies, is lacking ( 62 – 64 ). Thus, while the IM approach helped us to select strategies that are likely to positively impact the implementation of STORM, our evaluation should confirm whether our selection was accurate.
Strengths and limitations
A strength of the current study is that we systematically developed an implementation plan by following the tasks of IM ( 32 ). We did this in close collaboration with stakeholders who will implement STORM in practice, ensuring that the implementation plan matches the needs in practice. Additionally, we enhanced the credibility and transferability of our results through member checks, data and investigator triangulation, and sampling until we reached data saturation.
We recognise some limitations to our study as well. To begin, we mainly identified determinants related to the adoption and implementation of the intervention, and not to sustaining STORM over time. This is mostly likely because sustainability was not an explicit topic in our interviews and interviewees were in an early stage of pre-implementation. We discussed the lack of determinants with programme leaders and accordingly added a general determinant for sustainability. Furthermore, we reached out to multiple stakeholders and interviewed those who responded. Possibly, this led to selection bias if only participants with strong opinions about STORM, be these negative or positive, responded to our invitation. However, we asked participants to reflect on the perceptions of others in their field to minimise this bias.
Recommendations
Building on our strengths and limitations, we first recommend following the tasks of IM when developing an implementation plan, as this helped us to systematically select appropriate strategies. Furthermore, it encourages close collaboration with practice, which we found to be very helpful for developing a plan that is both achievable and relevant for practice. In doing so, we recommend including sustainability in the needs assessment to identify determinants and strategies for sustainability within the implementation plan.
Second, we recommend consulting multiple sources for the selection of implementation strategies. We found it helpful to first use the CFIR-ERIC tool to get a first idea of possible strategies, and then compare them to the SISTER strategies to identify more suitable strategies for the school context. We recommend others developing an implementation plan to consult such strategy compilations for specific intervention settings, if available.
For new STORM regions, we recommend using this implementation plan as guidance rather than a prescription. Some strategies might prove not to be as relevant and/or feasible as we originally believed. The implementation plan could also be helpful for the implementation of other school-based mental health interventions as these might encounter similar barriers. However, tailoring the implementation strategies to the specific context for these interventions is warranted.
In this study, we followed the tasks of IM, which helped us to develop a STORM implementation plan systematically and in collaboration with practice. The implementation plan offers guidance for new regions implementing STORM. Following the implementation plan could help to improve implementation outcomes and might even lead to better programme outcomes. Moreover, our approach and the strategies we identified could inform the implementation of other school-based mental health programmes, although we recommend tailoring our strategies to the specific context into which it will be implemented. Future research evaluating the implementation of STORM across the Netherlands will provide more insight into the usefulness of the implementation plan.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study was approved by the Ethics Commission Social Sciences of Radboud University, approval number ECSW-LT-2023-2-2-33415. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
KJ: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Visualization, Writing – original draft, Writing – review & editing. SR: Conceptualization, Supervision, Writing – review & editing, Writing – original draft. AP: Conceptualization, Supervision, Writing – review & editing, Writing – original draft. DC: Conceptualization, Supervision, Writing – review & editing, Writing – original draft. CG: Formal analysis, Investigation, Methodology, Writing – review & editing, Writing – original draft. LV: Investigation, Writing – review & editing, Writing – original draft. SM: Writing – review & editing, Writing – original draft. JS: Writing – review & editing, Writing – original draft. FN: Conceptualization, Formal analysis, Investigation, Methodology, Supervision, Writing – review & editing, Writing – original draft.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was funded by a subsidy of the Ministry of Health, Welfare, and Sport in the programme of the National Agenda Suicide Prevention 2021–2025.
Acknowledgments
We would like to thank the national and regional STORM teams from 113 Suicide Prevention, Groningen, Nijmegen and East Brabant for helping us to recruit study participants and for helping us select implementation strategies that are relevant for practice. We also thank all study participants for participating in an interview.
Conflict of interest
SR and DC were involved in the development of the STORM approach. SR, DC, and LV were involved in the national scale-up of STORM. LV was involved as an interview participant and was therefore not involved in revising, reading and approving the results section.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1386031/full#supplementary-material
1. Avenevoli, S, Swendsen, J, He, J-P, Burstein, M, and Merikangas, KR. Major depression in the national comorbidity survey–adolescent supplement: prevalence, correlates, and treatment. J Am Acad Child Adolesc Psychiatry . (2015) 54:37–44.e2. doi: 10.1016/j.jaac.2014.10.010
PubMed Abstract | Crossref Full Text | Google Scholar
2. Merikangas, KR, He, J-p, Burstein, M, Swanson, SA, Avenevoli, S, Cui, L, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry . (2010) 49:980–9. doi: 10.1016/j.jaac.2010.05.017
3. Mojtabai, R, Olfson, M, and Han, B. National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics . (2016) 138:1–10. doi: 10.1542/peds.2016-1878
4. Oderinde, K, Dada, M, Ogun, O, Awunor, N, Kundi, B, Ahmed, H, et al. Prevalence and predictors of depression among adolescents in Ido Ekiti, south West Nigeria. Int J Clinical Med . (2018) 9:187–202. doi: 10.4236/ijcm.2018.93017
Crossref Full Text | Google Scholar
5. Ormel, J, Raven, D, van Oort, F, Hartman, C, Reijneveld, S, Veenstra, R, et al. Mental health in Dutch adolescents: a TRAILS report on prevalence, severity, age of onset, continuity and co-morbidity of DSM disorders. Psychol Med . (2015) 45:345–60. doi: 10.1017/S0033291714001469
6. Orri, M, Scardera, S, Perret, LC, Bolanis, D, Temcheff, C, Séguin, JR, et al. Mental health problems and risk of suicidal ideation and attempts in adolescents. Pediatrics . (2020) 146:1–10. doi: 10.1542/peds.2019-3823
7. Paul, B, and Usha, V. Prevalence and predictors of depression among adolescents. Indian J Pediatr . (2021) 88:441–4. doi: 10.1007/s12098-020-03491-w
8. Uddin, R, Burton, NW, Maple, M, Khan, SR, and Khan, A. Suicidal ideation, suicide planning, and suicide attempts among adolescents in 59 low-income and middle-income countries: a population-based study. Lancet Child & Adolescent Health . (2019) 3:223–33. doi: 10.1016/S2352-4642(18)30403-6
9. Clayborne, ZM, Varin, M, and Colman, I. Systematic review and meta-analysis: adolescent depression and long-term psychosocial outcomes. J Am Acad Child Adolesc Psychiatry . (2019) 58:72–9. doi: 10.1016/j.jaac.2018.07.896
10. Finning, K, Ukoumunne, OC, Ford, T, Danielsson-Waters, E, Shaw, L, De Jager, IR, et al. The association between child and adolescent depression and poor attendance at school: a systematic review and meta-analysis. J Affect Disord . (2019) 245:928–38. doi: 10.1016/j.jad.2018.11.055
11. Verboom, CE, Sijtsema, JJ, Verhulst, FC, Penninx, BW, and Ormel, J. Longitudinal associations between depressive problems, academic performance, and social functioning in adolescent boys and girls. Dev Psychol . (2014) 50:247–57. doi: 10.1037/a0032547
12. Thapar, A, Eyre, O, Patel, V, and Brent, D. Depression in young people. Lancet (London, England) . (2022) 400:617–31. doi: 10.1016/S0140-6736(22)01012-1
13. World Health Organization . Live life: an implementation guide for suicide prevention in countries . Geneva: World Health Organization (2021).
Google Scholar
14. Caldwell, DM, Davies, SR, Thorn, JC, Palmer, JC, Caro, P, Hetrick, SE, et al. Public Health Research. School-based interventions to prevent anxiety, depression and conduct disorder in children and young people: A systematic review and network meta-analysis . Southampton (UK): NIHR Journals Library; (2021), 9, 1–284.
15. Corrieri, S, Heider, D, Conrad, I, Blume, A, König, H-H, and Riedel-Heller, SG. School-based prevention programs for depression and anxiety in adolescence: a systematic review. Health Promot Int . (2013) 29:427–41. doi: 10.1093/heapro/dat001
16. Feiss, R, Dolinger, SB, Merritt, M, Reiche, E, Martin, K, Yanes, JA, et al. A systematic review and meta-analysis of school-based stress, anxiety, and depression prevention programs for adolescents. J Youth Adolesc . (2019) 48:1668–85. doi: 10.1007/s10964-019-01085-0
17. Werner-Seidler, A, Spanos, S, Calear, AL, Perry, Y, Torok, M, O'Dea, B, et al. School-based depression and anxiety prevention programs: an updated systematic review and meta-analysis. Clin Psychol Rev . (2021) 89:102079. doi: 10.1016/j.cpr.2021.102079
18. Gijzen, MW, Rasing, SP, Creemers, DH, Engels, RC, and Smit, F. Effectiveness of school-based preventive programs in suicidal thoughts and behaviors: a meta-analysis. J Affect Disord . (2022) 298:408–20. doi: 10.1016/j.jad.2021.10.062
19. Robinson, J, Calear, AL, and Bailey, E. Suicide prevention in educational settings: a review. Australas Psychiatry . (2018) 26:132–40. doi: 10.1177/1039856218759406
20. Katz, C, Bolton, SL, Katz, LY, Isaak, C, Tilston-Jones, T, Sareen, J, et al. A systematic review of school-based suicide prevention programs. Depress Anxiety . (2013) 30:1030–45. doi: 10.1002/da.22114
21. Hofstra, E, van Nieuwenhuizen, C, Bakker, M, Özgül, D, Elfeddali, I, de Jong, SJ, et al. Effectiveness of suicide prevention interventions: a systematic review and meta-analysis. Gen Hosp Psychiatry . (2020) 63:127–40. doi: 10.1016/j.genhosppsych.2019.04.011
22. Gijzen, MW, Creemers, DH, Rasing, S, Smit, F, and Engels, RC. Evaluation of a multimodal school-based depression and suicide prevention program among Dutch adolescents: design of a cluster-randomized controlled trial. BMC Psychiatry . (2018) 18:1–12. doi: 10.1186/s12888-018-1710-2
23. Rasing, S, Spijker, J, Stikkelbroek, Y, and Creemers, D. De beste behandeling voor depressie is vroegsignalering en preventie bij jeugdigen. Tijdschr Psychiatr . (2021) 2021:111–4.
24. Terpstra, S, Beekman, A, Abbing, J, Jaken, S, Steendam, M, and Gilissen, R. Suicide prevention gatekeeper training in the Netherlands improves gatekeepers' knowledge of suicide prevention and their confidence to discuss suicidality, an observational study. BMC Public Health . (2018) 18:637. doi: 10.1186/s12889-018-5512-8
25. de Jonge-Heesen, KW, Rasing, S, Vermulst, AA, Scholte, RH, van Ettekoven, KM, Engels, RC, et al. Randomized control trial testing the effectiveness of implemented depression prevention in high-risk adolescents. BMC Med . (2020) 18:1–13. doi: 10.1186/s12916-020-01656-0
26. Wijnhoven, LA, Creemers, DH, Vermulst, AA, Scholte, RH, and Engels, RC. Randomized controlled trial testing the effectiveness of a depression prevention program (‘Op Volle Kracht’) among adolescent girls with elevated depressive symptoms. J Abnorm Child Psychol . (2014) 42:217–28. doi: 10.1007/s10802-013-9773-5
27. Herrman, H, Patel, V, Kieling, C, Berk, M, Buchweitz, C, Cuijpers, P, et al. Time for united action on depression: a lancet–world psychiatric association commission. Lancet . (2022) 399:957–1022. doi: 10.1016/S0140-6736(21)02141-3
28. 113 Suicide Prevention . Derde Landelijke Agenda Suïcidepreventie, 2021–2025 . Amsterdam: 113 Suicide Prevention (2020).
29. Durlak, JA, and DuPre, EP. Implementation matters: a review of research on the influence of implementation on program outcomes and the factors affecting implementation. Am J Community Psychol . (2008) 41:327–50. doi: 10.1007/s10464-008-9165-0
30. Seral-Cortes, M, De Miguel-Etayo, P, Zapata, P, Miguel-Berges, ML, and Moreno, LA. Effectiveness and process evaluation in obesity and type 2 diabetes prevention programs in children: a systematic review and meta-analysis. BMC Public Health . (2021) 21:348. doi: 10.1186/s12889-021-10297-8
31. Wierenga, D, Engbers, LH, Van Empelen, P, Duijts, S, Hildebrandt, VH, and Van Mechelen, W. What is actually measured in process evaluations for worksite health promotion programs: a systematic review. BMC Public Health . (2013) 13:1190. doi: 10.1186/1471-2458-13-1190
32. Fernandez, ME, Ten Hoor, GA, Van Lieshout, S, Rodriguez, SA, Beidas, RS, Parcel, G, et al. Implementation mapping: using intervention mapping to develop implementation strategies. Front Public Health . (2019) 7:158. doi: 10.3389/fpubh.2019.00158
33. Braun, V, and Clarke, V. Using thematic analysis in psychology. Qual Res Psychol . (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
34. O'Brien, BC, Harris, IB, Beckman, TJ, Reed, DA, and Cook, DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med . (2014) 89:1245–51. doi: 10.1097/ACM.0000000000000388
35. Bodden, D, Braet, C, and Stikkelbroek, Y. CDI-2 Screeningsvragenlijst voor depressie bij kinderen en jongeren . Amsterdam: Uitgeverij Hoogrefe (2016).
36. Kerkhof, A, and Huisman, A. VOZZ: Vragenlijst over Zelfdoding en Zelfbeschadiging . Houten: Bohn Stafleu van Loghum (2016).
37. de Jonge-Heesen, KW, van Ettekoven, KM, Rasing, S, Liempd, FH, Vermulst, AA, Engels, RC, et al. Evaluation of a school-based depression prevention program among adolescents with elevated depressive symptoms: study protocol of a randomized controlled trial. BMC Psychiatry . (2016) 16:1–9. doi: 10.1186/s12888-016-1119-8
38. de Haan, A, Keij, M, and Lammers, J. Handreiking bevordering mentale gezondheid jeugd . Utrecht: Trimbos Instituut & Pharos (2021).
39. Samen Minder Suïcide . Bewezen effectieve aanpak voor depressie nu voor veel jongerne in Nederland beschikbaar (2023). [cited 2023 July 7th]. Available from: https://samenmindersuicide.nl/bewezen-effectieve-aanpak/ .
40. Domlyn, AM, Crowder, C, Eisenson, H, Pollak, KI, Davis, JM, Calhoun, PS, et al. Implementation mapping for tobacco cessation in a federally qualified health center. Front Public Health . (2022) 10:908646. doi: 10.3389/fpubh.2022.908646
41. Ibekwe, LN, Walker, TJ, Ebunlomo, E, Ricks, KB, Prasad, S, Savas, LS, et al. Using implementation mapping to develop implementation strategies for the delivery of a Cancer prevention and control phone navigation program: a collaboration with 2-1-1. Health Promot Pract . (2022) 23:86–97. doi: 10.1177/1524839920957979
42. Odawara, M, Saito, J, Yaguchi-Saito, A, Fujimori, M, Uchitomi, Y, and Shimazu, T. Using implementation mapping to develop strategies for preventing non-communicable diseases in Japanese small-and medium-sized enterprises. Front Public Health . (2022) 10:873769. doi: 10.3389/fpubh.2022.873769
43. Pérez Jolles, M, Fernández, ME, Jacobs, G, De Leon, J, Myrick, L, and Aarons, GA. Using implementation mapping to develop protocols supporting the implementation of a state policy on screening children for adverse childhood experiences in a system of health centers in inland Southern California. Front Public Health . (2022) 10:876769. doi: 10.3389/fpubh.2022.876769
44. Roth, IJ, Tiedt, MK, Barnhill, JL, Karvelas, KR, Faurot, KR, Gaylord, S, et al. Feasibility of implementation mapping for integrative medical group visits. J Alt Complement Med (New York, NY) . (2021) 27:S-71–80. doi: 10.1089/acm.2020.0393
45. Thackeray, A, Waring, J, Hoogeboom, TJ, Nijhuis-van Der Sanden, MW, Hess, R, Fritz, JM, et al. Implementing a Dutch physical therapy intervention into a US health system: selecting strategies using implementation mapping. Front Public Health . (2022) 10:908484. doi: 10.3389/fpubh.2022.908484
46. Kang, E, and Foster, ER. Use of implementation mapping with community-based participatory research: development of implementation strategies of a new goal setting and goal management intervention system. Front Public Health . (2022) 10:10. doi: 10.3389/fpubh.2022.834473
47. Damschroder, LJ, Reardon, CM, Widerquist, MAO, and Lowery, J. The updated consolidated framework for implementation research based on user feedback. Implement Sci . (2022) 17:75. doi: 10.1186/s13012-022-01245-0
48. Powell, BJ, Waltz, TJ, Chinman, MJ, Damschroder, LJ, Smith, JL, Matthieu, MM, et al. A refined compilation of implementation strategies: results from the expert recommendations for implementing change (ERIC) project. Implement Sci . (2015) 10:1–14. doi: 10.1186/s13012-015-0209-1
49. Cook, CR, Lyon, AR, Locke, J, Waltz, T, and Powell, BJ. Adapting a compilation of implementation strategies to advance school-based implementation research and practice. Prev Sci . (2019) 20:914–35. doi: 10.1007/s11121-019-01017-1
50. Waltz, TJ, Powell, BJ, Fernández, ME, Abadie, B, and Damschroder, LJ. Choosing implementation strategies to address contextual barriers: diversity in recommendations and future directions. Implement Sci . (2019) 14:42. doi: 10.1186/s13012-019-0892-4
51. Proctor, EK, Powell, BJ, and McMillen, JC. Implementation strategies: recommendations for specifying and reporting. Implement Sci . (2013) 8:1–11. doi: 10.1186/1748-5908-8-139
52. Proctor, EK, Silmere, H, Raghavan, R, Hovmand, P, Aarons, G, Bunger, A, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health Ment Health Serv Res . (2011) 38:65–76. doi: 10.1007/s10488-010-0319-7
53. Moore, GF, Audrey, S, Barker, M, Bond, L, Bonell, C, Hardeman, W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ . (2015) 350:350. doi: 10.1136/bmj.h1258
54. Saunders, RP, Evans, MH, and Joshi, P. Developing a process-evaluation plan for assessing health promotion program implementation: a how-to guide. Health Promot Pract . (2005) 6:134–47. doi: 10.1177/1524839904273387
55. Weiner, BJ, Lewis, CC, Stanick, C, Powell, BJ, Dorsey, CN, Clary, AS, et al. Psychometric assessment of three newly developed implementation outcome measures. Implement Sci . (2017) 12:108. doi: 10.1186/s13012-017-0635-3
56. Vis, C, Ruwaard, J, Finch, T, Rapley, T, de Beurs, D, van Stel, H, et al. Toward an objective assessment of implementation processes for innovations in health care: psychometric evaluation of the normalization measure development (NoMAD) questionnaire among mental health care professionals. J Med Internet Res . (2019) 21:e12376. doi: 10.2196/12376
57. Braam, MWG, Rasing, SPA, Heijs, DAM, Lokkerbol, J, van Bergen, DD, Creemers, DHM, et al. Closing the gap between screening and depression prevention: a qualitative study on barriers and facilitators from the perspective of public health professionals in a school-based prevention approach. BMC Public Health . (2023) 23:884. doi: 10.1186/s12889-023-15705-9
58. Waltz, TJ, Powell, BJ, Matthieu, MM, Damschroder, LJ, Chinman, MJ, Smith, JL, et al. Use of concept mapping to characterize relationships among implementation strategies and assess their feasibility and importance: results from the expert recommendations for implementing change (ERIC) study. Implement Sci . (2015) 10:1–8. doi: 10.1186/s13012-015-0295-0
59. Richter, A, Sjunnestrand, M, Romare Strandh, M, and Hasson, H. Implementing school-based mental health services: a scoping review of the literature summarizing the factors that affect implementation. Int J Environ Res Public Health . (2022) 19:1–30. doi: 10.3390/ijerph19063489
60. March, A, Stapley, E, Hayes, D, Town, R, and Deighton, J. Barriers and facilitators to sustaining school-based mental health and wellbeing interventions: a systematic review. Int J Environ Res Public Health . (2022) 19:3587. doi: 10.3390/ijerph19063587
61. Lyon, AR, Cook, CR, Locke, J, Davis, C, Powell, BJ, and Waltz, TJ. Importance and feasibility of an adapted set of implementation strategies in schools. J Sch Psychol . (2019) 76:66–77. doi: 10.1016/j.jsp.2019.07.014
62. Baffsky, R, Ivers, R, Cullen, P, Wang, J, McGillivray, L, and Torok, M. Strategies for enhancing the implementation of universal mental health prevention programs in schools: a systematic review. Prev Sci . (2022) 24:337–52. doi: 10.1007/s11121-022-01434-9
63. Driessen, A, and Van Nassau, F. Kennisagenda Implementatie 2022: Verkenning van kennishiaten en vraagstukken op het gebied van implementatie in de gezondheidszorg in Nederland Dutch Implementation Collective (2022).
64. Lewis, CC, Klasnja, P, Lyon, AR, Powell, BJ, Lengnick-Hall, R, Buchanan, G, et al. The mechanics of implementation strategies and measures: advancing the study of implementation mechanisms. Implementation Sci Commun . (2022) 3:1–11. doi: 10.1186/s43058-022-00358-3
Keywords: implementation mapping, implementation, adolescents, prevention, depression, suicide
Citation: Jenniskens K, Rasing S, Popma A, Creemers D, Ghalit C, van Vuuren L, Mérelle S, Spijker J and van Nassau F (2024) Development of an implementation plan for a school-based multimodal approach for depression and suicide prevention in adolescents. Front. Public Health . 12:1386031. doi: 10.3389/fpubh.2024.1386031
Received: 14 February 2024; Accepted: 12 April 2024; Published: 10 May 2024.
Reviewed by:
Copyright © 2024 Jenniskens, Rasing, Popma, Creemers, Ghalit, van Vuuren, Mérelle, Spijker and van Nassau. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kristel Jenniskens, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.

Quick links
- Find a course
- Request a prospectus
Day workshop in Cognitive Behavioural Therapy effectively reduces depression in 16-18 year olds
Search the website.
14 May 2024
/7x0:1033x697/prod01/channel_3/media/middlesex-university/news-section-images/2024/Gadiel-lazcano.jpg)
- Find us on Facebook
- Find us on Twitter
- Find us on Linkedin
- Find us through email
MDX academic collaborates in mental health research for adolescents led by King’s College London
Dr Tim Weaver, Associate Professor in Mental Health Research at MDX, has collaborated in new research from the Institute of Psychiatry, Psychology & Neuroscience (IoPPN) at King’s College London released today (14 May).
The study, funded by the NIHR, has found that providing 16-18 year olds with a day-long course in Cognitive Behavioral Therapy (CBT) was both a clinically and cost-effective means of improving their mental health.
The trial, known as Brief Educational workshops in Secondary Schools Trial (BESST) and published in The Lancet Psychiatry, was successfully adapted from the DISCOVER program, which was designed to help adults manage their feelings of stress. The study has been funded by the National Institute for Health and Care Research (NIHR).
Around one in 12 young people in England currently experience anxiety or depression. Despite this, the large majority remain untreated, and almost a quarter (24%) have no contact with specialist Child and Adolescent Mental Health Services (CAMHS).
This study recruited 900 students from 57 schools in England. Half were provided with signposting to mental health services and the standard care their school would usually provide. The other half were invited to a day-long workshop on CBT coping techniques for managing mood, anxiety, and stress, and provided with follow up phone calls to help incorporate those skills into real-life situations.
Researchers found that participants who attended the workshop showed significant improvements in their depression, anxiety, wellbeing and resilience after a six-month follow up.
Dr June Brown, Associate Professor in Clinical Psychology at King’s IoPPN and the study’s lead author said: "More than half of adult mental disorders start before the age of 15, and when we approached schools, we found that there was an overwhelming number of young people actively seeking support. There is clearly an urgent need for early intervention to ensure that symptoms of poor mental health don’t persist and worsen. Our study set out to establish if there was a clinically and cost-effective way to do that at scale.
One of our main challenges was to adapt an adult therapeutic intervention which would be attractive and engaging for teenagers. In addition, previous studies have either been aimed at all students, some of whom aren’t necessarily in need of assistance, while others have taken a more targeted approach that potentially stigmatises those who might need support. Giving students the opportunity to self-refer means that we work with students who recognise that they’d like help.
Our study shows that this intervention can be delivered at low cost by mental health professionals who can bridge the gap between schools and CAMHS."
"The study shows that self-referral to a brief school-based CBT programme is an acceptable and effective intervention for promoting positive mental health outcomes amongst adolescents. If it can be widely embedded into mainstream practice this intervention could alleviate the symptoms of depression for many. Working with our project partners at King’s and elsewhere, we hope to be able to follow this trial with further research which supports wider implementation." Dr Tim Weaver , Associate Professor in Mental Health Research, Middlesex University
Professor Ben Carter, Professor of Medical Statistics at King’s IoPPN and the study’s senior author said: "Since the pandemic there is an increased need to support schools and adolescents with their mental health. While we found improvements in depression; anxiety; wellbeing; and resilience, the largest effect was seen in those students that had higher symptoms of depression at the start of the study, meaning that we reached and improved those students most vulnerable to depression."
"The ultimate success of this has laid the groundwork for these workshops to be rolled out nationwide to provide an early intervention against depression and anxiety."
Karen Crowe, Senior Tutor for the Sixth Form & Curriculum Leader for Psychology at St Nicholas Catholic High School in Cheshire said: "Our school seeks to prioritise mental wellbeing and promote strategies that improve students’ mental health. We believe it is important to teach students how to become self-regulating individuals who can manage their own stress, which is why the school fully supported the BESST trial. We value techniques that provide students with skills to resolve problems, cope better with expectations, and build confidence, so the trial’s aims perfectly complement our school’s mission and ethos."
Olivia Black, a student at St Nicholas Catholic High School who took part in the BESST trial, said: "The study gave me new ways to manage my stress and remain productive during my studies. It was such a helpful process that allowed me to develop my personal strategies for maintaining good mental health. The skills and confidence gained from this trial motivated me to help start up our 'breathing space' initiative where sixth formers support younger students with their mental health."
Image credit: Gadiel Lazcano, Unsplash
/0x57:2200x1553/prod01/channel_3/media/middlesex-university/news-section-images/2024/hmv-banner-3.png)
- 16 May 2024
/0x305:788x841/prod01/channel_3/media/Mikhaela-Rain-Roy2.jpg)
- 15 May 2024
/8x0:1033x697/prod01/channel_3/media/middlesex-university/news-section-images/2024/Manolo-Bilog.jpg)
Modal video
The Relationship Between Temporal Sense and Psychopathologies of College Students with Sensory Impairments: Mediation of Religions
- ORIGINAL PAPER
- Published: 13 May 2024
Cite this article

- Yan Dai ORCID: orcid.org/0000-0001-8938-2794 1 na1 &
- You Yu ORCID: orcid.org/0000-0002-1168-2575 1 na1
18 Accesses
Explore all metrics
Previous studies on the relationship between temporal sense and negative mental health symptoms have focused primarily on healthy college students, overlooking the role of religion. This study sought to examine the impact of religion on college students with sensory impairment and fill a gap in the research on the relationship between temporal sense and negative mental health symptoms in this population. The results were obtained from a cross sectional survey of 540 participants, including 370 hearing-impaired students and 140 visually impaired students. The survey investigated the mediating effect of religion on the relationship between temporal sense and negative mental health symptoms in impaired students. The rates of negative mental health symptoms (depression, anxiety, and stress) detected were 18.9%, 31.1%, and 2.9%, respectively. Students with different types of sensory impairments showed significant differences in their perception of time. The percentages of students with sensory impairments who attended church and practiced religion were 2.0%, 6.0%, and 1.0%, respectively. The results revealed a significant positive correlation between temporal sense and negative mental health symptoms, with religion serving as a mediating factor.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
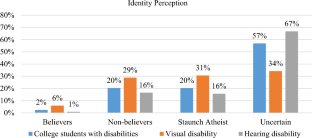
Similar content being viewed by others

Time in schizophrenia: a link between psychopathology, psychophysics and technology

Quality of Life and its Predictors among Persons with Visual Disabilities in Sri Lanka: Development of a New Measure

The Scientific Study of Life Satisfaction and Religion/Spirituality
Aneta, P., & Malgorzata, S. (2021). People with positive time perspective are more grateful and happier: Gratitude mediates the relationship between time perspective and life satisfaction. Journal of Happiness Studies, 22 (1), 113–126. https://doi.org/10.1007/s10902-020-00221-z
Article Google Scholar
Atieh, O., Hamid, H., Adeleh, S., Ameneh, M., & Saemeh, S. (2022). The relationship between observing religiousand suffering in hemodialysis patients. Journal of Religion & Health, 61 (3), 2018–2028. https://doi.org/10.1007/s10943-019-00887-7
Blewett, A. E. (1992). Abnormal subjective time experience in depression. The British Journal of Psychiatry, 161 (2), 195–200. https://doi.org/10.1192/bjp.161.2.195
Article CAS PubMed Google Scholar
Chen, C.-C., Lan, Y.-L., Chiou, S.-L., & Lin, Y.-C. (2022). The effect of emotional labor on the physical and mental health of health professionals: Emotional exhaustion has a mediating effect. Healthcare, 11 (1), 104. https://doi.org/10.3390/healthcare11010104
Article PubMed PubMed Central Google Scholar
Droitvolet, S. (2016). Time does not fly but slow down in old age. Time and Society, 28 (1), 1–23. https://doi.org/10.1177/0961463x16656852
Eskin, M., Poyrazli, S., Janghorbani, M., Bakhshi, S., Carta, M. G., Moro, M. F., Tran, U. S., Voracek, M., Mechri, A., & Aidoudi, K. (2019). The role of religion in suicidal behavior, attitudes and psychological distress among university students: A multinational study. Transcultural Psychiatry, 56 (5), 853–877. https://doi.org/10.1177/1363461518823933
Article PubMed Google Scholar
Gable, P. A., & Poole, B. D. (2012). Time flies when you’re having approach-motivated fun: effects of motivational intensity on time perception. Psychological Science, 23 (8), 879–886. https://doi.org/10.1177/0956797611435817
Gan, Y., & Fu, Q. (2022). Risk perception and coping response to covid-19 mediated by positive and negative emotions: A study on Chinese college students. PLoS ONE, 17 (1), 1–13. https://doi.org/10.1371/journal.pone.0262161
Article CAS Google Scholar
Gao, Y., Mai, H., & Kanji, L. (2020). Comparison of the development of chinese word segmentation between deaf students and deaf students. Chinese Journal of Special Education , 5 , 22–27.
Gong, X., Xie, X.-Y., Xu, R., & Luo, Y.-J. (2010). Psychometric properties of the Chinese versions of DASS-21 in Chinese college students. Chinese Journal of Clinical Psychology, 18 (4), 443–446.
Google Scholar
Hu, A., Yang, X. Y., & Luo, W. (2017). Christian identification and self-reported depression: Evidence from China. Journal for the Scientific Study of Religion, 56 (4), 765–780. https://doi.org/10.1111/jssr.12482
Iswanto, A., Zainal, A., Murodov, A., El-Ebiary, Y. A. B., & Sattarova, D. G. (2022). Studying the role of Islamic religiouson depression during COVID-19 in Malaysia. HTS Theological Studies, 78 (4), 1–6. https://doi.org/10.4102/hts.v78i4.7567
Janssen, S. M. J., Naka, M., & Friedman, W. J. (2013). Why does life appear to speed up as people get older? Time and Society, 22 (2), 274–290.
Kessler, R. C., Berglund, P., Borges, G., Nock, M., & Wang, P. S. (2005). Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990–1992 to 2001–2003. JAMA, 293 , 2487. https://doi.org/10.1001/jama.293.20.2487
Koenig, H. G., & Zaben, F. A. (2021). Psychometric validation and translation of religious and spiritual measures. Journal of Religion and Health, 60 , 3467–3483.
Lew, B., Kõlves, K., ZhangID, J., Zhizhong, W., Koenig, H. G., Yip, P. S. F., Talib, M. A., Osman, A., SiauID, C. S., Mei, C., & Chan, H. (2021). Religious affiliation and suicidality among college students in China: A cross-sectional study across six provinces. PLoS ONE, 16 (5), e0251698. https://doi.org/10.1371/journal.pone.0251698
Article CAS PubMed PubMed Central Google Scholar
Lin, Q., Jiang, Y., Sun, X., Zhang, Y., Shan, W., Zhao, J., Wang, X., Qi, Z., Sun, W., & Lu, H. (2022). Weight spectrum and executive function in adolescents: The moderating role of negative emotions. Child & Adolescent Psychiatry & Mental Health, 16 (1), 1–10. https://doi.org/10.1186/s13034-022-00468-9
Lovibond, S. (1995). Manual for the Depression Anxiety Stress Scales (2nd ed.). Psychology Foundation.
Marc, W., Tina, R., Linares, G. D., & Isabell, W. (2015). Time perspective and emotion regulation as predictors of age-related subjective passage of time. International Journal of Environmental Research and Public Health, 12 (12), 16027–16042. https://doi.org/10.3390/ijerph121215034
Paulina, B., Renata, P., King, M., & Lukasz, G. (2022). The mediating effect of negative emotions on the relationship between subjective sleep quality and paranoia-like thoughts. Journal of Psychiatric Research, 145 , 132–136. https://doi.org/10.1016/j.jpsychires.2021.12.003
RMahdi, R., Arash, D., & Farzaneh, S. (2022). Students’ negative emotions and their rational and irrational behaviors during COVID-19 outbreak. PLoS ONE, 17 (3), e0264985. https://doi.org/10.1371/journal.pone.0264985
Sun, G., Zhao, J., Tian, S., Zhang, L., & Jia, C. (2020). Psychological strain and suicidal ideation in athletes: The multiple mediating effects of hopelessness and depression. International Journal of Environmental Research and Public Health, 17 (21), 8087. https://doi.org/10.3390/ijerph17218087
Tamkeen, S., Shemaila, S., Rabia, M., & Seema, G. (2021). Belief salience, religious activities, frequency of prayer offering, religious offering preference and mental health: A study of religiosity among muslim students. Journal of Religion & Health, 60 (2), 726–735. https://doi.org/10.1007/s10943-020-01046-z
Tobias, O., Kappel, K. A., Karen, A.-R., Kaare, C., & Christian, H. N. (2021). Characteristics of Danish Centenarians’ religious beliefs: A nationwide population-based study. Journal of Religion & Health, 60 (3), 2007–2023. https://doi.org/10.1007/s10943-020-00981-1
WHO. (2020). Adolescent mental health.
Wittmann, M. R. T. G. D. L. W. I. (2015). Time perspective and emotion regulation as predictors of age-related subjective passage of time. International Journal of Environmental Research & Public Healthcare, 12 (12), 16027–16042.
Wu, A., Wang, J. Y., & Jia, C. X. (2015). Religion and completed suicide: A meta-analysis. PLoS ONE, 10 (6), e0131715. https://doi.org/10.1371/journal.pone.0131715
Yang, D., Zheng, Y., Wang, S., Wei, M., & Zhang, L. (2022). The relationship between new drug use behavior and depression, anxiety and stress in Wuhan high school students. Modern Preventive Medicine, 49 (07), 1212–1216.
Yosef, S., Chayim, R., Chynna, L., & Mairav, L. (2022). Anxiety and temporal self-appraisal: How people with anxiety evaluate themselves over time. Journal of Affective Disorders, 296 , 309–314. https://doi.org/10.1016/j.jad.2021.09.081
Yu, X., Deng, L., Lu, C., & Gao, D. (2017). Perception of Time Lapse: Concept Exploration, Questionnaire Compilation and its Reliability and Validity. Psychological Techniques and Applications, 5 , 542–552. https://doi.org/10.16842/j.cnki.issn2095-5588.2017.09.005
Zhang, Y. (2021). A study on mitigation strategies of psychological anxiety of college students under learning stress. Psychiatria Danubina, 33 , S699–S704.
Zhang, J., Zhao, S., & Liu, J. (2017). Does believing in a religion relate to individuals mental health? An initial study among Chinese college students. Int J School Cogn Psychol, 4 (4), 1–7.
Zhang, J., Lew, B., Liu, Y., Zhao, S., & Ksenia, C. (2022a). Religion, psychological strain, and Suicidality in China: A preliminary study. Omega-Journal of Death and Dying . https://doi.org/10.1177/00302228211072985
Zhang, J., Liu, Y., Hennessy, D., Zhao, S., & Ji, H. (2022). Development of the Temporal Sense Scale (TSS) for General Populations. Timing & Time Perception , 368–391.
Zhao, S., & Zhang, J. (2020). Can perception be altered by change of reference? A test of the social reference theory utilizing college students’ judgments of attractiveness. The Journal of General Psychology, 147 (4), 398–413.
Download references
Acknowledgements
The authors wish to thank all the students who participated in this project and the research associates and teachers who were involved in organizing the data collation.
The authors have not disclosed any funding.
Author information
Yan Dai and You Yu shared first authorship.
Authors and Affiliations
College of Special Education, Beijing Union University, 1 Puhuangyu Road Alley 2, Fengtai District, Beijing, China
Yan Dai & You Yu
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to You Yu .
Ethics declarations
Conflict of interest.
The authors declare no conflict of interest.
Ethical Approval
All human and animal studies have been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Dai, Y., Yu, Y. The Relationship Between Temporal Sense and Psychopathologies of College Students with Sensory Impairments: Mediation of Religions. J Relig Health (2024). https://doi.org/10.1007/s10943-024-02053-0
Download citation
Accepted : 21 April 2024
Published : 13 May 2024
DOI : https://doi.org/10.1007/s10943-024-02053-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- College students
- Sensory impairments
- Temporal sense
- Negative mental health symptoms
- Find a journal
- Publish with us
- Track your research

New Research From Clinical Psychological Science
- Clinical Psychological Science
- Obsessive Compulsive Disorder (OCD)
- Personality
- Stereotypes

Threat Appraisal and Pediatric Anxiety: Proof of Concept of a Latent-Variable Approach Rachel Bernstein, Ashley Smith, Elizabeth Kitt, Elise Cardinale, Anita Harrewijn, Rany Abend, Kalina Michalska, Daniel Pine, and Katharina Kircanski
Elevated threat appraisal is a postulated neurodevelopmental mechanism of anxiety disorders. However, laboratory-assessed threat appraisals are task-specific and subject to measurement error. We used latent-variable analysis to integrate youths’ self-reported threat appraisals across different experimental tasks; we next examined associations with pediatric anxiety and behavioral- and psychophysiological-task indices. Ninety-two youths ages 8 to 17 (M = 13.07 years, 65% female), including 51 with a primary anxiety disorder and 41 with no Axis I diagnosis, completed up to eight threat-exposure tasks. Anxiety symptoms were assessed using questionnaires and ecological momentary assessment. Appraisals both before and following threat exposures evidenced shared variance across tasks. Derived factor scores for threat appraisal were associated significantly with anxiety symptoms and variably with task indices; findings were comparable with task-specific measures and had several advantages. Results support an overarching construct of threat appraisal linked with pediatric anxiety, providing groundwork for more robust laboratory-based measurement.
Investigating a Common Structure of Personality Pathology and Attachment Madison Smith and Susan South
Critical theoretical intersections between adult insecure attachment and personality disorders (PDs) suggest that they may overlap, but a lack of empirical analysis to date has limited further interpretation. The current study used a large sample (N = 812) of undergraduates (N = 355) and adults receiving psychological treatment (N = 457) to test whether a joint hierarchical factor structure of personality pathology and insecure attachment is tenable. Results suggested that attachment and PD indicators load together on latent domains of emotional lability, detachment, and vulnerability, but antagonistic, impulsigenic, and psychosis-spectrum factors do not subsume attachment indicators. This solution was relatively consistent across treatment status but varied across gender, potentially suggesting divergent socialization of interpersonal problems. Although further tests are needed, if attachment and PDs prove to be unitary, combining them has exciting potential for providing an etiologic-developmental substrate to the classification of interpersonal dysfunction.
Does Major Depression Differentially Affect Daily Affect in Adults From Six Middle-Income Countries: China, Ghana, India, Mexico, Russian Federation, and South Africa? Vanessa Panaite and Nathan Cohen
Much of the research on how depression affects daily emotional functioning comes from Western, Educated, Industrialized, Rich, and Democratic (WEIRD) countries. In the current study, we investigated daily positive affect (PA) and negative affect (NA) and PA and NA variability in a cross-cultural sample of adults with a depression diagnosis (N = 2,487) and without a depression diagnosis (N = 31,764) from six middle-income non-WEIRD countries: China, Ghana, India, Mexico, Russian Federation, and South Africa. Across countries, adults with depression relative to adults without depression reported higher average NA and NA variability and lower average PA but higher PA variability. Findings varied between countries. Observations are discussed within the context of new theories and evidence. Implications for current knowledge and for future efforts to grow cross-cultural and non-WEIRD affective science are discussed.
Depressive Symptoms and Their Mechanisms: An Investigation of Long-Term Patterns of Interaction Through a Panel-Network Approach Asle Hoffart, Nora Skjerdingstad, René Freichel, Alessandra Mansueto, Sverre Johnson, Sacha Epskamp, and Omid V. Ebrahimi
The dynamic interaction between depressive symptoms, mechanisms proposed in the metacognitive-therapy model, and loneliness across a 9-month period was investigated. Four data waves 2 months apart were delivered by a representative population sample of 4,361 participants during the COVID-19 pandemic in Norway. Networks were estimated using the newly developed panel graphical vector-autoregression method. In the temporal network, use of substance to cope with negative feelings or thoughts positively predicted threat monitoring and depressed mood. In turn, threat monitoring positively predicted suicidal ideation. Metacognitive beliefs that thoughts and feelings are dangerous positively predicted anhedonia. Suicidal ideation positively predicted sleep problems and worthlessness. Loneliness was positively predicted by depressed mood. In turn, more loneliness predicted more control of emotions. The findings point at the theory-derived variables, threat monitoring, beliefs that thoughts and feelings are dangerous, and use of substance to cope, as potential targets for intervention to alleviate long-term depressive symptoms.
Feedback on this article? Email [email protected] or login to comment.
APS regularly opens certain online articles for discussion on our website. Effective February 2021, you must be a logged-in APS member to post comments. By posting a comment, you agree to our Community Guidelines and the display of your profile information, including your name and affiliation. Any opinions, findings, conclusions, or recommendations present in article comments are those of the writers and do not necessarily reflect the views of APS or the article’s author. For more information, please see our Community Guidelines .
Please login with your APS account to comment.

Research Briefs
Recent highlights from APS journals articles on the link between self-esteem and eating disorders, how to be liked in first encounters, the effects of stress on rigid learning, and much more.

Student Notebook: Learning Through Exposure
Ellen Finch on what therapists in training can learn from exposure therapy during a pandemic.

Video: 5 Flash Talks on Mental Health
Researchers share how their work is advancing the understanding and treatment of conditions like postpartum depression, OCD, and bipolar disorder.
Privacy Overview
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Adv Med Educ Pract
Depression and Anxiety Among Medical Students: A Brief Overview
Ahmad a mirza.
1 Department of Otolaryngology, Head and Neck Surgery, Faculty of Medicine in Rabigh, King Abdulaziz University, Jeddah, Saudi Arabia
Mukhtiar Baig
2 Department of Clinical Biochemistry/Medical Education, Faculty of Medicine in Rabigh, King Abdulaziz University, Jeddah, Saudi Arabia
Ghada M Beyari
3 Faculty of Medicine, Umm Al-Qura University, Makkah, Saudi Arabia
Mohammed Aiman Halawani
Abdulrahim a mirza.
4 Department of Surgery – Division of Urology, Ministry of National Guard - Health Affairs, Jeddah, Saudi Arabia
Depression and anxiety are highly prevalent conditions worldwide. This article reviews the extent of depression and anxiety among medical students and elucidates associated potential risk factors. In comparison to other countries, students from Middle East countries have a higher prevalence of depression. Females suffer from these conditions more commonly than males. Factors associated with these morbidities can be divided into academic and non-academic factors. There is an inconclusiveness of whether medical students experience these symptoms more commonly than their counterparts. The present review provided a cross-sectional picture of the students’ psychological well-being, which is crucial to formulate a health policy for preventive and therapeutic purposes.
Introduction
Globally, mental health among undergraudate students represents an important public health entity. University students face considerable demands in school and family, resulting in significant psychological stress that may lead to serious disorders and mental health issues such as depression and anxiety. As a result, university students’ academic performance, physical well-being and mental health may substantially worsen over the academic career and could only be detected at an advanced stage. Additionally, studies conducted among medical school graduates showed that psychological distress was associated with suboptimal quality of patient care, patient safety and professionalism. 1 , 2 The present review provides a cross-sectional picture of the current condition of the psychological well-being of medical students. In addition, it sheds light on significant predictors of depression and anxiety and helps to identify and manage major stressors in academic life.
For this narrative review, MEDLINE was searched for peer-reviewed publications in the English literature (publication period: from the inception untill 2018). We searched the grouping of Medical Subject Heading phrases: (medical students) AND (depression OR anxiety). Additional works was identified from these publications’ reference lists. Each paper was objectively reviewed and included, as applicable, based on the presentation of primary data, the quality of the methodology used, the clarity of the findings, and the dependence on the existing instruments to quantify depression and anxiety. Abundant literature is available on this topic; we included only a few important and informative research articles in this review. The ethical review committee’s approval for this report was not required, as it was a narrative review of previously published researches.
Prevalence of Depression
Depression represents a significant health problem in university populations, with about one-third of students are affected. 3 A systematic review estimated that the mean prevalence of depressive disorders in university students was 30.6%, which was considerably higher than rates reported in general populations. 3 Epidemiological data suggested that the prevalence of depression increased by 18.4% from 2005 to 2015. 4
Regional distribution showed a high frequency of depression in the Middle East with a prevalence of 31.8%, followed by North America with an incidence of 30.3%, Asia (30.1%), South America (26.8%), and Europe (20%). 5 The estimated frequency of depression or its manifestations in medical students around the world was 27.2%, according to a recent systematic review and meta-analysis. 6 Another systematic review found that the prevalence of depression varied between 6.0–66.5%. 7 An United Arab of Emirates (UAE) study examined depression and anxiety in medical students, doctors and members of the Medical College for Girls in Dubai. They found that 28.6% of medical undergraduates and 7.8% of medical staff had a high score for depression. 8 The overall frequency of depression or its symptoms among medical undergraduates ranged from 1.4% to 73.5%. 6 , 9
Difference in Gender
Regarding gender, several studies reported significant differences between males and females, whereas others did not find any significant difference. 10–15 Overall, female undergraduate students tended to have more depression than males. 16 A study conducted among university students from 23 countries found that the prevalence of depressive symptoms was 19% among male students and 22% among female students. 17 Similarly, when prevalence was stratified by gender, female medical students were found to have a higher prevalence of depression (31.5%) than males (24.2%). 5 Although females are more at risk, male students’ high rates cause a special issue since they are less willing to seek help. 3
Factors Associated with Depression
Many factors might increase students’ susceptibility to depression. These factors include changes in lifestyle, financial stressors, family relationship changes, and academic worries with post-graduation life. 3 Other possible risk factors that significantly increase the crude odds ratio (OR) of having major depressive disorder include female gender, younger age, lower-class years, living alone in a rented room, and financial difficulty. 18 Furthermore, a study highlighted some specific factors for each academic level. Notably, 1st year students reported “volume of work” and “absence of feedback” as major stressors, while 3rd year students were stressed by “fears about future capability” and “pedagogical inadequacies”. Sixth year students, on the other hand, expressed worries about “non-supportive climate” in addition to the stressors reported by the 1st and 3rd year students. 12 Other social factors were associated with a high rate of depression such as family economic status. Higher rates of depression were reported among university students from low-income families than those from high socioeconomic families. Moreover, those who lived in rural areas were likely to have a greater risk for depression than those living in urban areas. 19 Students with substance abuse, students having a family history of depression and anxiety, and those who had lost a close relative in the past year were more likely to be depressed and anxious. 20
Difference Between Medical and Non-Medical Students
Several studies evaluated the depression rate and compared medical and non-medical students. A British study compared the degree of depression in medical students with their non-medical peers and discovered that medical college students had a lower prevalence of depression generally than non-medical students. 21 In contrast, a meta-analysis indicated that the depression rate among medical students was not significantly different from non-medical students. 5 A Swedish study investigated the factors linked to depression and explored the frequency of depressive disorders at various academic levels among medical students. 12 The study demonstrated that medical students had a higher prevalence of depressive disorders compared to the general population.
The Variation Across the Academic Years
The incidence of depression was found to be varied across the academic years in medical school. First-year students had the highest prevalence of depression (33.5%), and the rates gradually decreased until year 5 (20.5%). 5 According to another study, the highest rate of depression was diagnosed in medical students of the second year. 8 A Pakistani study stated a high prevalence of depression among newly entered students (1st and 2nd year students) compared to senior students. 20 In contrast, in another study, the risk of depression was significantly higher in third-year students (39%) compared to first-year students (28.4%), besides an increased level of perceived stress among the same group. 22 A study evaluated depression, anxiety, and stress disorders among medical students and revealed that the depression levels among students at the entry of medical school were similar to the general public, then progressively worsened over the academic period. 23
Prevalence of Anxiety
The prevalence of anxiety among medical students has been reported from different regions and countries. According to a cross-sectional study carried out in Pakistan, a high prevalence of anxiety (47.7%) was found among medical students. A mild, moderate, and severe anxiety symptoms were present in 27.6%, 13.6% and 6.5% of the students, respectively. 24 In India, a study reported that 66.9% of medical undergraduates suffered from anxiety. 16 A systematic review included medical colleges across Europe and countries speaking English outside North America and found that the frequency of anxiety varied between 7.7–65.5%. 7 A Turkish study showed a high frequency of anxiety (47.1%) among medical undergraduates. 19 A high prevalence rate of anxiety was also reported among medical undergraduates in an Egyptian university (73%), and Nepal (41.1%); while relatively lower rates were reported in Brazil (37.2%) and Great Britain (31.2%). 25–28 In the Middle East region, a study showed 28.7% of medical students suffered from anxiety. 8 A Saudi study showed that the frequency of morbid anxiety was 34.9% among medical undergraduates. 29
A study carried out among medical students showed a significant gender difference with twice the rate of anxiety among females compared to males (40% versus 20%). 30 Another study in Brazil assessed and compared the frequency and severity of symptoms of anxiety among first- and sixth-year medical students. They found that females were more likely to suffer from anxiety than males. 31 In Saudi Arabia, a cross-sectional study showed a significantly higher rate of psychological morbidities, including anxiety, among premedical, 1st, 2nd and 3rd year female medical students (89.7%) than males (60%); however, no significant differences were found between gender in all other years. 32
Factors Associated with Anxiety
Several risk factors that predispose undergraduate medical students to psychological disorders, like anxiety, have been reported. A study in Pakistan described that drugs addicted students, students with a positive family history of depression and anxiety, and individuals who had lost a close relative in the past year were more prone to suffer from psychological disorders and being anxious than other individuals. 20 Another study demonstrated that students with economic difficulties were at a higher risk for such disorders. 33 In Egypt, a study estimated the frequency of depression, anxiety and stress symptoms among undergraduates in a medical college and demonstrated the relationship of such conditions with sociodemographic data. They showed that the female gender, university campus residents, pre-clinical years students, and students with lower academic accomplishment had higher scores of anxiety than other groups. 25 Other issues may cause a significant effect on medical students’ mental and emotional well-being and induce anxiety such as long working and study hours, mastering medical knowledge, competition, and inadequate time for non-academic activities. 34 , 35 Additionally, anxiety was found to be positively predicted by a family history of mental disorders. 30 A study highlighted students’ three top concerns: academic performance, the pressure to succeed, and post-graduation plans. 36 Further studies are required to determine the factors linked with mental problems such as anxiety that influence medical undergraduates’ academic achievements.
A study in Portugal reported that anxiety symptoms were significantly more prevalent among medical students than non-medical students. 37 A systematic review that included students from the USA and Canada found greater anxiety levels among medical students than the general population. 38 Similarly, a comparative study conducted among female students in Dammam University, Saudi Arabia revealed a decrease in well-being and higher levels of anxiety among medical compared to non-medical students as early as the start of the bachelor’s program. 39
Many studies compared the levels of anxiety among different academic years in medical school; one found fluctuating rates of psychological disorders, including anxiety, among students, namely 45.86% in 1st, 52.58% in 2nd, 47.14% in 3rd, 28.75% in 4th, and 45.10% in final year. 40 Besides, anxiety symptoms were found to be frequent among medical students of 2nd year (61.6%). 24 Similarly, a Brazilian study reported a higher frequency of anxiety symptoms among 1st year medical students (30.8%) than in 6th year students (9.4%). 31
Significance of the Findings and Recommendations
The present narrative review showed that the prevalence of depression and anxiety is very high. The incidence of depression ranged from 1.4% to 73.5%, and the anxiety ranged from 7.7% to 65.5% among medical students. Female medical students were more vulnerable to anxiety and depression than male students. The associated factors with depression and anxiety are female gender, economic condition, academic pressure, etc. Furthermore, the rate of depression and anxiety among medical students fluctuates across the academic years. This probably due to the difference in academia and student life from one school to another. Future research to estimate the global burden of these psychological morbidities in both developing and developed countries is of vital importance. Depression and anxiety cause hindrance to medical students’ academic career and later to their social life. It is suggested that these factors should be considered among medical students, and students should be provided psychological counseling in their early academic years. Students’ support unit should help them in alleviating their associated factors that may jeopardize their bright career.
The present paper lacks a systematic comprehensive approach that is mandated in evidence synthesis. However, the goal was to provide a brief overview of the burden and potential risk factors of psychological impairments among medical students emphasizing the importance of synthesizing a higher level of evidence.
Acknowledgments
The authors gratefully acknowledge the invaluable guidance from Prof. Waleed Milaat and Prof. Iman Ramadan, professors in the Department of Community Medicine at King Abdulaziz University, Jeddah, Saudi Arabia. This article is a part of thesis submitted for the requirements of Master of Science degree in public health conferred by Department of Community Medicine, King Abdulaziz University, Jeddah, Saudi Arabia.
Data Sharing Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
The authors declare that they have no competing interests.

IMAGES
VIDEO
COMMENTS
Depression is a top mental health concern among undergraduates and has been shown to disproportionately affect individuals who are underserved and underrepresented in science. As we aim to create a more inclusive scientific community, we argue that we need to examine the relationship between depression and scientific research. While studies have identified aspects of research that affect ...
To fill the gap in the literature, this study describes stress, anxiety, and depression symptoms for students in a public research university in Kentucky during an early phase of COVID-19 and their usage of mental health services. Results show that about 88% of students experienced moderate to severe stress, with 44% of students showing ...
In a sample of Chinese students, depression was more prevalent among medical students, followed by engineering and arts students 69. ... Despite being relevant to research involving students, the ...
INTRODUCTION. The prevalence of depression among college students has gradually increased in recent years, even exceeding that of the general public, which has become a global phenomenon[].Mounting research has focused on the topic, and the consensus is that the high prevalence of depression among college students cannot be ignored.
Globally, studies conducted on different samples of undergraduate students have identified a moderate to high prevalence of depression, anxiety and stress in this population [18,19,20,21,22,23]. Early diagnosis and management of psychological distress lead to better management and patient outcomes [ 24 ].
Depression and anxiety are the most widely recognized mental issues affecting youths. It is extremely important to investigate the burden and associated risk factors of these common mental disorders to combat them. Therefore, this study was undertaken with the aim to estimate the prevalence and identify factors associated with depression, anxiety, and stress among high school students in an ...
In all, 16 studies reported the prevalence of depression among a total of 23,469 Ph.D. students (Fig. 2; range, 10-47%).Of these, the most widely used depression scales were the PHQ-9 (9 studies ...
In addition, depression and anxiety often occur concurrently, such as in a study on UK college students, 29.8% of females and 13.9% of males screened positive for both anxiety and depression .
Abstract. Objective: Psychiatric disorders, such as depression and anxiety, can hinder academic performance among college-age individuals.Participants: Mental health among college students is a growing public health concern, with some scholars describing collegiate mental health as a crisis (Chen et al., Psychiatr Serv. 2019;70(6):442-449).Methods: This study analyzes data from four annual ...
Background: South African universities face a challenge of low throughput rates, with most students failing to complete their studies within the minimum regulatory time. Literature has begun to investigate the contribution of well-being, including mental health, with depression among students being one of the most common mental disorders explored. However, locally relevant research exploring ...
Abstract. Depression is a top mental health concern among undergraduates and has been shown to disproportionately affect individuals who are underserved and underrepresented in science. As we aim to create a more inclusive scientific community, we argue that we need to examine the relationship between depression and scientific research.
You may be experiencing depression if you've had some of the below symptoms most of the time for the last 2 weeks: ongoing feelings of sadness. being on-edge or snapping at people. low self ...
February 17, 2021. 25. Kat J. McAlpine. A survey by a Boston University researcher of nearly 33,000 college students across the country reveals the prevalence of depression and anxiety in young people continues to increase, now reaching its highest levels, a sign of the mounting stress factors due to the coronavirus pandemic, political unrest ...
The number of students seeking help at campus counseling centers increased almost 40% between 2009 and 2015 and continued to rise until the pandemic began, according to data from Penn State University's Center for Collegiate Mental Health (CCMH), a research-practice network of more than 700 college and university counseling centers (CCMH Annual Report, 2015).
Mental health issues among students. Depression is a common mood disorder, affecting around 4.5% of adults in the UK, and is characterized by persistent sadness and low mood alongside a loss of interest or pleasure in activities or social interaction (American Psychiatric Association, Citation 2013; WHO, Citation 2017).There is extensive empirical research centred around depression in ...
For many students, the years at college are a time of discovery and growth. But depression may get in the way. The rate of depression among college students is rising. In a 2021-2022 survey of students across 133 college campuses, 44% of students reported symptoms of depression and 15% reported seriously considering suicide in the past year.
University is the peak of depression, and the prevalence of depression among college students is much higher than that of ordinary people. The purpose of this research is to evaluate depression symptoms, life satisfaction, self-confidence, substance use, social adjustment, and dropout rates of the use of psychological intervention for college ...
Studies across the world have implemented various techniques to detect the level of depression among students, and most of them have demonstrated that it is a common issue. 12,19-21 In a study on international students in health-related fields, 36% were found to have symptoms of depression, and 52.63% were screened positive for anxiety ...
young students. (Kerr, 2017). Often, a breakup will precipitate about of depressive feelings. Risks of depression. related to a breakup include int rusive thoughts, difficulty c ontrolling those ...
Methods. A single author (MP) searched PubMed and Google Scholar for peer-reviewed articles published at any time in English. Search terms included academic, school, university, stress, mental health, depression, anxiety, youth, young people, resilience, stress management, stress education, substance use, sleep, drop-out, physical health with a combination of any and/or all of the preceding terms.
1 INTRODUCTION. University students are negatively impacted by poor mental health outcomes. An international study of 14,000 undergraduate students found that one in three reported at least one mental health disorder (Auerbach et al., 2018).Indeed, studies have shown that university students can be at a higher risk for increased stress, aggression, depression, and anxiety (Banu et al., 2015 ...
To examine these relationships properly, we collected longitudinal data from 392 university students at three occasions over a one-year period and analyzed the data using autoregressive time-lagged panel models. Procrastination did lead to depression and anxiety symptoms over time. However, perceived stress was not a mediator of this effect.
Introduction. Globally, depression and suicide prevalence in adolescents is high and appears to be increasing (1-8).Adolescent depression is associated with poor social well-being, poor school attendance, failure to complete secondary school, depression recurrence, and the onset of other psychiatric disorders (9-12).Moreover, suicide is the fourth leading cause of death among adolescents ...
MDX academic collaborates in mental health research for adolescents led by King's College London Dr Tim Weaver, Associate Professor in Mental Health Research at MDX, has collaborated in new research from the Institute of Psychiatry, Psychology & Neuroscience (IoPPN) at King's College London released today (14 May). The study, funded by the NIHR, has found that providing 16-18 year olds ...
The coronavirus 2019 (COVID-19) has brought significant changes to college students, but there is a lack of empirical studies regarding how the pandemic has affected student mental health among college students in the U.S. To fill the gap in the literature, this study describes stress, anxiety, and depression symptoms for students in a public research university in Kentucky during an early ...
Current research by Khan et al. on the undergraduate medical students stated that even though the high occurrence of huge depression between the students, the students GPA is unharmed. Therefore, based on given differences in various research findings, this research is supposed to find a more specific and clear answer to the shared relationship ...
Previous studies on the relationship between temporal sense and negative mental health symptoms have focused primarily on healthy college students, overlooking the role of religion. This study sought to examine the impact of religion on college students with sensory impairment and fill a gap in the research on the relationship between temporal sense and negative mental health symptoms in this ...
The results provide insights into the relations between everyday stressors and personality pathology. Stereotypes toward symptom presentations of obsessive compulsive disorder (OCD) are poorly understood. A mixed-methods, multistudy analysis of OCD stigma was conducted. In Study 1 (N = 60), participants read one of five vignettes (symmetry/just ...
To solve this problem, this paper takes mechanical engineering as the research object, and proposes a new machine-learning-driven GPA prediction approach to evaluate the academic performance of engineering students by incorporating psychological evaluation data into basic course scores. ... such as depression and anxiety, among student ...
Prevalence of Depression. Depression represents a significant health problem in university populations, with about one-third of students are affected. 3 A systematic review estimated that the mean prevalence of depressive disorders in university students was 30.6%, which was considerably higher than rates reported in general populations. 3 Epidemiological data suggested that the prevalence of ...