

BREAST CANCER CASE STUDY
Oct 01, 2014
960 likes | 5.1k Views
BREAST CANCER CASE STUDY. FRAZER BELL STUDENT BMS BSc APPLIED BIOMEDICAL SCIENCE. PATIENT HISTORY. 70 YEAR OLD FEMALE PRESENTED AT GP SURGERY 02/OCT/2012 EXAMINATION: RIGHT NIPPLE DRAWING IN & FIRM PALPABLE LUMP REFERRED TO THE BREAST CLINIC. BREAST CLINIC. ATTENDED 18/OCT/2012
Share Presentation
- receptor status
- oestrogen receptor
- staging investigations
- oestrogen receptor status
- sentinel lymph node biopsy

Presentation Transcript
BREAST CANCERCASE STUDY FRAZER BELL STUDENT BMS BSc APPLIED BIOMEDICAL SCIENCE
PATIENT HISTORY • 70 YEAR OLD FEMALE • PRESENTED AT GP SURGERY 02/OCT/2012 • EXAMINATION: RIGHT NIPPLE DRAWING IN & FIRM PALPABLE LUMP • REFERRED TO THE BREAST CLINIC
BREAST CLINIC • ATTENDED 18/OCT/2012 • EXAMINATION: INVERTED NIPPLE RETRACTION AND PALPABLE LUMP • ? PALPABLE LUMP RIGHT AXILLA • GRADED P5: MALIGNANT • FURTHER INVESTIGATIONS: MAMMOGRAM, ULTRASOUND & BREAST CORE BIOPSY
MAMMOGRAPHY • AREA OF SUSPICIOUS ABNORMALITY ON RIGHT BREAST • GRADED M4: PROBABLY MALIGNANT
ULTRASOUND • ULTRASOUND : CORRESPONDING 2CM AREA • GRADED U4: PROBABLY MALIGNANT
BIOPSY • ULTRASOUND GUIDED BREAST CORE BIOPSIES FROM THE RIGHT BREAST • ONE 13MM FIBROFATTY CORE PLUS 4 FIBROFATTY FRAGMENTS
NORMAL BREAST TISSUE
PATHOLOGY GRADED: B5b Infiltrating Breast Carcinoma
IMMUNOCYTOCHEMISTRY E-CAD NEGATIVE
RECEPTOR STATUS • OESTROGEN RECEPTOR & HER-2 STATUS • DETERMINE RECEPTOR STATUS FOR HORMONE THERAPY
OESTROGEN RECEPTOR STATUS NEGATIVE CONTROL OESTROGEN POSITIVE
PROGESTERONE REC. STATUS PROG POSITIVE NEGATIVE CONTROL
HER-2 STATUS HER2 NEGATIVE NEGATIVE CONTROL
TREATMENT PLAN • BREAST MDT MEETING • MASTECTOMY WITHOUT NEOADJUVANT TREATMENT • SENTINEL LYMPH NODE BIOPSY • SURGERY DATE 06/NOV/2012
PRE-OP ASSESSMENT • ADMITTED PRE-OP CLINIC 01/NOV/2012 • LABS TESTS: PRE-OP BLOODS • HYPERTENSIVE • MEDICAL WARD: ECG CONFIRMED LVH • SURGERY CANCELLED
TREATMENT PLAN • REDUCE BLOOD PRESSURE VIA ACE INHIBITORS • CHEST X-RAY & U/S OF KIDNEYS • STARTED ON LETROZOLE 2.5mg DAILY • BP MONITORED FORTNIGHTLY • RE-ASSESSMENT FOR SURGERY IN JANUARY
SURGERY • BP STABILISED • ADMITTED TO SURGICAL WARD 13/FEB/13 • SURGERY 25/FEB/13 • RIGHT BREAST MASTECTOMY • SENTINEL LYMPH NODE BIOPSY
MASTECTOMY • 19MM AND 7MM FIRM NODULES UPON DISSECTION • NO LYMPHOVASCULAR INVASION • 12MM CLEARANCE DEEP MARGIN
HISTOPATHOLOGY TUMOUR GRADE 2 INVASIVE LOBULAR CARCINOMA
SENTINEL LYMPH NODE • FIVE SENTINEL NODES • FOUR NEGATIVE • ONE POSITIVE DEPOSIT OF METASTATIC TUMOUR • ICC: AE1/AE3 CYTOKERATIN
SENTINEL LYMPH NODE AE1/AE3 POSITIVE H&E SENTINEL NODE
POST-OPERATIVE • GRADE 2 INVASIVE LOBULAR CARCINOMA • CLOSEST RELEVANT MARGIN 12MM • SINGLE NODE POSITIVITY • STAGING INVESTIGATIONS REQUIRED
STAGING INVESTIGATIONS • STAGING INVESTIGATIONS TO EXCLUDE METASTASES • CT SCAN - NEGATIVE • BONE SCAN - NEGATIVE
FUTURE • PATIENT DECLINED CHEMOTHERAPY • WILL ATTEND THE BEATSON CANCER CENTRE • RADIOTHERAPY TREATMENT • CONTINUE LETROZOLE
ACKNOWLEDGEMENTS • CONS. PATHOLOGIST Dr. A. W. Milne • CROSSHOUSE PATHOLOGY DEPT.
- More by User
BREAST CANCER STUDY
BREAST CANCER STUDY A STUDY OF ISSUES INVOLVING THE DIAGNOSIS OF BREAST CANCER THAT RESULT IN MEDICAL MALPRACTICE CLAIMS 2002 Breast Cancer Study Focus 450 cases involving paid claims with resolution dates no earlier than January 1, 1995 were analyzed.
749 views • 32 slides
Breast Cancer
Breast Cancer Casey and Tabitha What is it? Breast cancer is a cancerous tumor that starts from cells of the breast. The disease occurs mostly in women, but men can get breast cancer too. About 178,480 women in the United States will be found to have invasive breast cancer in 2007.
1.15k views • 9 slides
Breast Cancer. Locally Advanced and Metastatic Disease C. Legler MD FRCPC September 30, 2005. Locally Advanced and Metastatic Breast Cancer. Overview: Principles of neoadjuvant chemotherapy for locally advanced and inflammatory breast cancer Systemic therapy of metastatic breast cancer
1.93k views • 53 slides
Cervical Cancer Case Study
Cervical Cancer Case Study. Presented by: University of Guelph. Baktiar Hasan Mark Kane Melanie Laframboise Michael Maschio Andy Quigley. Objectives. To determine an appropriate model for the prediction of recurrence of cervical cancer
1.46k views • 22 slides

Breast Cancer. April 1, 2014. Introduction. Most common female cancer Accounts for 32% of all female cancer 211,300 new cases yearly and rising 40,000 deaths yearly. Gross Anatomy. Sappy’s plexus – lymphatics under areolar complex 75% of lymphatics flow to axilla. Microscopic Anatomy.
2.11k views • 33 slides
Cervical Cancer Case Study. Supervising Professor: Dr. P.D.M. Macdonald Team Members: Christine Calzonetti, Simo Goshev, Rongfang Gu, Shahidul Mohammad Islam, Amanda Lafontaine, Marcus Loreti, Maria Porco, William Volterman, Qihao Xie.
1.52k views • 17 slides
2002 Breast Cancer Study Focus . 450 cases involving paid claims with resolution dates no earlier than January 1, 1995 were analyzed.The study addresses only claims alleging a delay in the diagnosis of breast cancer.25 PIAA member companies reported information.. More than 68% of the patients repr
476 views • 32 slides

Breast Cancer. By George Rezk. What is Breast Cancer?. Breast cancer is a cancer that starts in the tissues of the breast. There are two main types of breast cancer :
717 views • 13 slides

Breast Cancer . By: Kalyn Johnson. So….What is breast cancer anyways???.
240 views • 7 slides

Breast Cancer. The Penncrest High School Medical Scholars Club. Things You probably don’t Know About Breast Cancer. -The older a woman, the more likely she is to get breast cancer -Young women can get breast cancer, even in their 20s
1.05k views • 41 slides
BREAST CANCER
BREAST CANCER. New cases (2007): 4226 (Males 30; Females 4196) Deaths (2007): 908 (Males 6; Females 902) Females 1 st for incidence, 2 nd for mortality Risk: 1 in 11 women by age 75; 1 in 9 women by age 85 1998-2007 No change in incidence rates Mortality rates 12%. BREAST CANCER.
1.15k views • 8 slides

Breast Cancer. The Penncrest High School Medical Scholars Club. 5 Things You probably don’t Know About Breast Cancer. -The older a woman, the more likely she is to get breast cancer -Young women can get breast cancer, even in their 20s
2.03k views • 51 slides
Carolina Breast Cancer Study: Breast cancer subtypes and race
Carolina Breast Cancer Study: Breast cancer subtypes and race. Robert Millikan University of North Carolina Chapel Hill, NC. Research Questions. Could breast cancer represent more than one disease? Can different subtypes of breast cancer help to explain racial disparities?.
784 views • 37 slides

Breast Cancer. By Shelby Palmer && Whitney Brosious. Sometimes, precancerous cells may be found within breast tissue. Regular healthy cells get mutated into cancer cells. They divide uncontrollably and quickly create many more or the same harmful cells.
554 views • 15 slides
Breast Cancer. Kathrina Calulut Alison Saechao. Breast Cancer. Cancer of tissues of the breast Ductal carcinoma Lobular carcinoma. Risk Factors. 1 in 8 women Age and Gender Family History Substance Abuse Childbirth Obesity. Early Symptoms. New lump or mass
769 views • 15 slides
Breast Cancer . Who Gets What Type of Surgery? Murray Pfeifer 16 th August, 2014. History of Breast Cancer Treatment. Hipppocrates (460-375BC) spoke of two cases Galen (129-200AD) Humoral theory Linked to melancholia Likened to a ‘crab’
1.33k views • 38 slides
Breast Cancer. An opportunity to save Lives. Behram Pastakia Metropolitan Washington DC USA 9 th World Zoroastrian Congress, Dubai 2009. Defining the Problem. Breast cancer strikes 1 in 8 women in their lifetime Family history can increase your risk
520 views • 24 slides
Case Study 63: Cancer of the Female Breast
Case Study 63: Cancer of the Female Breast. By Robyn Schwartz. Case Background. 46, premenopausal Dense breasts Has noticed cysts in the past Noticed new lump in upper right quadrant Did not resolve Got bigger Denied lumps in axillary. Patient history. Happily married for 21 years
1.5k views • 16 slides
Cancer Case Study Presentation
Cancer Case Study Presentation. Katrina Beining and Katie Koller 2/8/14 FN 4360. What is Cancer?. Over 100 diseases 1 Cancer can cause almost any sign or symptom depending on size/location of tumor & how it effects organs and tissues 1. Etiology. In general 1 :
236 views • 14 slides
Case Study: Radiation Therapy and Ultrasound Management of Breast Cancer
Case Study: Radiation Therapy and Ultrasound Management of Breast Cancer. hhholdorf. Radiation Therapy (also known as radiotherapy and radiation oncology) began shortly after the discovery of X-rays in 1895 by Wilhelm Rontgen.
244 views • 22 slides
Breast cancer study group
Breast cancer study group. Outline. Adjuvant endocrine therapy Systemic disease Local disease Metastatic disease. Rationale for endocrine therapy of breast cancer. Estrogen and/or progesterone receptor expression is found in 85% of breast cancers. This proportion increases with age.
855 views • 79 slides
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State
Patient Case Presentation
Patient Mrs. B.C. is a 56 year old female who is presenting to her WHNP for her annual exam. She had to cancel her appointment two months ago and didn’t reschedule until now. Her last pap smear and mammogram were normal. Today, while performing her breast exam, her nurse practitioner notices dimpling in the left breast as the patient raises her arms over her head. When the NP mentions it to Mrs. B.C. she is surprised and denies noticing it before today. A firm, non-tender, immobile nodule is palpated in the upper quadrant of her breast . The NP then asks Mrs. B.C. how frequently she is performing breast self-exams, she admits to only doing them randomly when she remembers, which is about every few months. She reports no recent or abnormal drainage from her breast. Further examination reveals palpable axillary lymph nodes.
Mrs. B.C. is about 30 pounds overweight and walks her dog around her neighborhood every morning before work and every evening when she gets home. She reports drinking a glass of white wine before bed each night. She denies any history of tobacco use. She reports use of a combination birth control pill on and off for 25 years until she reached menopause. She is not currently taking any prescription medications.
Past Medical History
- Menarche (Age 10)
- Post-menopausal (Age 53)
- No other pertinent medical history
Family History:
- Father George- deceased from stroke (75 years old), history of hypertension, CAD, HLD
- Mother Maryanne alive- 76 years old, history of dementia, osteoporosis
- Brother Michael- alive, 57 years old, history of hypertension, CAD and cardiac stent placement (54 years old)
- Sister, Michelle- alive 53 years old, history of GERD, Asthma
- Brother- Jimmy- alive 50 years old, no past medical history
Social History:
Mrs. B.C. works Monday-Friday 8am-5pm at the local dentist’s office at the front desk as a schedule coordinator. She is planning to retire in a few years. In her spare time, she is involved in various community efforts to feed the homeless and helps to prepare dinners at her local church one night a week. She also enjoys cooking and baking at home, gardening, and nature photography.
Mrs. B.C. has two children. Her oldest son, Patrick, is 21 years old and is in his final year of pre-med. He is attending a public university about 2 hours away from home where he lives year-round. As an infant, Patrick was breastfed until 18 months when he self-weaned. Her daughter, Veronica, is 19 years old and lives at home while attending the local branch campus of a state university. She is in her second year of a business degree and then plans to transfer to the main campus next year. When Veronica was an infant she had difficulty latching onto the breast due to an undiagnosed tongue and lip ties resulting in Mrs. BC exclusively pumping and bottle feeding for six months. After six months, Mrs. B.C. was having a hard time keeping up while working and her found her supply diminished. Veronica had begun eating solid foods so Mrs. B.C. switched to supplemental formula, which was a big relief.
Mrs. B.C. was married to her now ex-husband Kent for 26 years. They divorced two years ago when Veronica was a senior in high school. They have remained friends and Kent lives 25 minutes away in a condo with his girlfriend. She also has two brothers who live nearby and a sister who lives out of state. Her 7 nieces and nephews range in age from 9 years old to 26 years old. Her father, George, passed away from a sudden stroke 4 years ago. Her mother, Maryanne, has dementia and is living in a nearby memory care facility. She also has many close friends.
- Understanding Breast Cancer
- Slide Show - Slide Show
*This slide show represents a visual interpretation and is not intended to provide, nor substitute as, medical and/or clinical advice.
Breasts are made up of fatty tissue. They contain small chambers called lobules where breast milk is made. The milk travels through tiny channels called ducts to reach the nipples.
Lymph nodes are located inside your breasts and under your arms. They are connected by lymph vessels and they help your body fight disease.
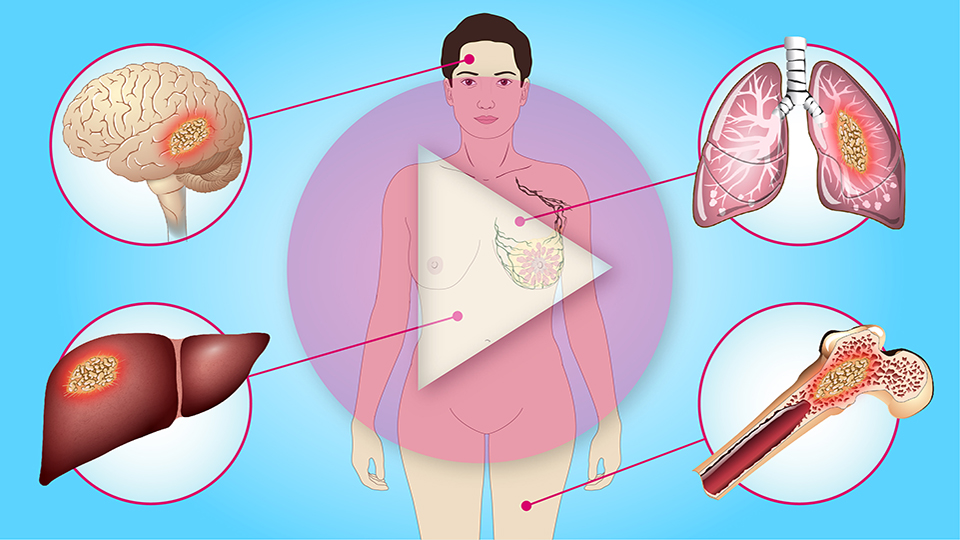
Breast cancer occurs when healthy breast cells become abnormal, grow out of control, and form tumors. Breast cancer can sometimes spread to other parts of the body.
About 1 in 8 women have a lifetime risk of getting breast cancer. For men, the risk is 1 in 1,000.
Breast cancer that develops inside the milk ducts is called “ ductal carcinoma in situ ", or DCIS . When DCIS spreads into surrounding tissue, it is called “ invasive ductal carcinoma ”, or IDC .
Abnormal cells can develop in the lobules of the breast. They are called “ lobular carcinoma in situ ", or LCIS , and are not cancer. When these cells spread into surrounding tissue, they become a cancer called “ invasive lobular carcinoma ”.
Signs of breast cancer can include:
- A lump in the breast or armpit;
- A change in breast shape or size;
- Nipple changes or discharge; and
- Skin changes, including redness, inflammation or dimpling like the skin of an orange.
Risk factors for breast cancer include:
- Dense breasts,
- Having breast cancer before, or having a parent or sibling who had it,
- Having specific, inherited gene mutations called BRCA1 and BRCA2
- Having Ashkenazi Jewish ancestry;
- Drinking more than a small amount of alcohol, and
- Being overweight or obese, especially after menopause.
Screening for breast cancer can help find cancer early and save lives.
Screening includes:
- Examining your own breasts;
- Having a healthcare provider examine them; and
- Having an X-ray of the breasts called a screening mammogram.
You can check your own breasts about the same time each month. Feel each breast and armpit and look for any of the signs of breast cancer previously discussed.
A diagnostic mammogram is used when a change is seen on a screening mammogram. It includes extra detailed images of the breast.
A breast ultrasound is often used to determine if a suspicious lump is solid or fluid-filled. A fluid-filled lump is often benign or a cyst, while a solid lump can be cancerous or a benign fibrous growth.
A breast MRI shows more detail than a mammogram, and is often used for very small masses or changes in the breast that cannot be seen by mammogram.
A breast biopsy is a test that removes a few cells or a small amount of tissue from the suspicious area in the breast. There are various types of biopsies.
A doctor called a pathologist will analyze the breast biopsy tissue by looking at the cells under a microscope and doing specific tests. Their report will let you know if you have cancer and if it grew because of estrogen, progesterone or HER2/neu protein on the cancer cell.
The results of these tests help your doctor choose the right treatment.
Doctors classify breast cancers based on how they behave. This includes:
- Non-invasive – cancer that has not spread outside the tissue where it began,
- Invasive – cancer that has spread and invaded healthy tissue,
- Recurrent – cancer that returns after it was treated, and
- Metastatic – cancer that has spread from the area where it started to other areas of the body .
Common types of breast cancer are:
- Invasive ductal carcinoma, and
- Invasive lobular cancer.
Less common types of breast cancer include:
- Inflammatory breast cancer,
- Tubular breast cancer,
- Colloid breast cancer, and
- Metaplastic breast cancer.
Triple-negative breast cancer means the tumor has no estrogen, progesterone, or HER2/neu protein receptors on its surface. Triple negative disease may have a worse outcome and often requires more intensive treatment.
Breast cancer staging is determined by the size and location of the cancer and whether it has spread to other areas in your body.
Breast cancers are graded 1 through 3, with 1 being the most similar to normal, healthy cells and 3 being the most different from normal cells and the most aggressive.
Breast cancer treatment depends on the type and stage of your cancer. You will need treatment from a cancer team specializing in different areas of medicine.
The main treatments include surgery , radiation , chemotherapy , hormone therapy , targeted therapy , and combination treatments .
Common types of surgery for breast cancer are:
- Lumpectomy (removing the tumor and a small portion of healthy normal tissue around it);
- Simple mastectomy (removing the entire breast);
- Modified radical mastectomy (removing the entire breast and lymph nodes under the arm);
- Prophylactic mastectomy (removing one or both breasts to reduce the risk of developing breast cancer);
- Mastectomy with reconstruction (reconstruction at the same time as removal of the breast);
- Sentinel lymph node biopsy (procedure to determine if one or more lymph nodes contain cancer cells); and
- Axillary node dissection (surgery to remove lymph nodes in the armpit region).
Reconstructive surgery is a procedure done to restore the appearance of the breast after a mastectomy or large tumor removal.
Radiation therapy uses radiation energy to kill cancer cells. It is mostly recommended after surgery or chemotherapy.
Chemotherapy is the use of drugs to destroy cancer cells. Chemotherapy for breast cancer is given as an IV or a pill.
Chemotherapy can be used to:
- Shrink a tumor before surgery (called neoadjuvant chemotherapy );
- Kill cancer cells after surgery (called adjuvant therapy ); and
- Control metastatic breast cancer (called palliative chemotherapy ).
Hormone therapy is given if your tumor is positive for the hormones estrogen or progesterone.
Hormone therapy is used to:
- Lower the risk of breast cancer coming back; and
- Help shrink or slow the growth of metastatic estrogen-receptor-positive breast cancers.
Tamoxifen and aromatase inhibitors are common hormone therapies for breast cancer.
Targeted therapy uses drugs or other substances to identify and fight specific types of cancer cells with less harm to normal cells.
Targeted therapies:
- Stop cancer cells from growing;
- Identify and kill cancer cells; and
- Increase the immune system’s attack on cancer cells.
HER2 is a common protein that is blocked with targeted therapy, for example trastuzumab .
Targeted therapy is often given along with chemotherapy .
Metastatic breast cancer is cancer that has spread from the breast to other areas of the body. The most common places are the liver, bones, lungs, and brain. There is no cure for metastatic breast cancer and treatment is to prolong survival.
Today , people are living 5 , 10 , or more years with metastatic breast cancer due to advances in treatment.
Metastatic breast cancer treatment may include ongoing chemotherapy, hormone therapy, targeted therapy, and new innovative medicines in clinical trials, such as immunotherapy.
Survivorship is a term used to describe any one who has had breast cancer and is still living.
As a survivor, you will have different care needs than when you were in treatment. Your cancer team and primary care doctor can help you meet these needs in the years after treatment.
It is frightening to learn you have breast cancer. However, the information available can help you receive timely, individualized, effective treatment that can give you the best chance of being cured.
Ask your doctor or cancer team if you have any questions about your treatment plan.
Slide Show - Understanding Breast Cancer
- Share with family and friends:
Click here to take our SURVEY Your feedback is important to us! We will use your feedback to develop future areas of content about breast cancer which will help other patients, caregivers and families.

Other Modules:

Understanding Breast Cancer - Screening and Diagnosis

Understanding Breast Cancer - Treatment
Understanding Metastatic Breast Cancer
Living Well with Metastatic Breast Cancer
Patient Stories:

Felicia's Story

Nicole's Story

Ruth's Story
This educational activity has been developed by American Breast Cancer Foundation and Mechanisms in Medicine Inc.
This activity is supported by an independent educational grant from Pfizer and Genentech.
This website is part of the Animated Patient ™ series developed by Mechanisms in Medicine Inc., to provide highly visual formats of learning for patients to improve their understanding, make informed decisions, and partner with their healthcare professionals for optimal outcomes.
- Terms of Use
- Technical Requirements
- © Mechanisms in Medicine Inc.
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Case Presentation on Locally Advanced breast Cancer

Related Papers
European Respiratory Journal
Annelies Rappaport
International Journal of Women's Health
Nicole Sandhu
Although much emphasis has been placed on the primary presentations of breast cancer, little focus has been placed on how systemic illnesses may affect the breast. In this article, we discuss systemic illnesses that can manifest in the breast. We summarize the clinical features, imaging, histopathology, and treatment recommendations for endocrine, vascular, systemic inflammatory, infectious, and hematologic diseases, as well as for the extramammary malignancies that can present in the breast. Despite the rarity of these manifestations of systemic disease, knowledge of these conditions is critical to the appropriate evaluation and treatment of patients presenting with breast symptoms.
Diagnostic Histopathology
Sarah Pinder
IOSR Journals
Background: Benign breast ds (BBD) are common disease affecting woman mainly. These can be diagnosed by triple assessment including clinical examination, radiological imagings, and a pathological examination. Majority of the benign lesions are not associated with an increased risk for subsequent breast cancer but some may have increased risk of malignancy like atypical hyperplasia. The main problem from women’s patient of view is fear that such a lump may be a cancer. Unlike breast cancer, benign breast diseases have often been difficult to understand, in part due to variety of names that have been used to describe the various conditions. So that clinician requires in-depth knowledge to give clear explanation about breast diseases. Making an early diagnosis and planning the treatment during initial consultations, helps in alleviating unnecessary anxiety about breast cancer and unnecessary long term follow up can be avoided. So, the need for study is to analyze the spectrum of benign breast disease. Method: A total 85 patients diagnosing as benign breast diseases under the inclusion criteria were studied during the period of Oct 2014 to March 2016; in the Dept of Surgery at People’s hospital of People’s college of medical science and research center, Bhopal. Our study objectives were A. To describe the spectrum of Benign Breast Diseases with Respect to Age of incidence, Social Demography, Duration of Symptoms, Site of lumps, Clinical features specific to conditions. B. To diagnose clinically and cytologically (FNAC) Suitable patients with benign breast disease and provide either conservative or operative treatment. C. To do histopathological examination of excised specimen for the comparisons and confirmation of cytological and clinical diagnosis. Result: Fibro adenoma was the most common benign lesion encountered (65.9%) followed by Breast Abscess 18.8% disease. Fibro adenoma was presented most often in the second and third decade (75%). Lump in the breast was the commonest presentation of BBD, Lump and Mastalgia was the second commonest symptom of BBD. There was a slight preponderance of lesions in the right breast (45.9%) as compared to left breast (44.7%), shown to be significant. Most of patients belong to middle class. 100% 0f the patients were in pre menopausal group. Majority (45.9%) of lesions were of the size 2-5 cms, 31.8% were between 6-10 cms FNAC highly reliable for fibro adenoma than for other lesions. All fibro adenomas willing for surgical procedure were managed by simple excision than follow up. All 16 cases of Breast Abscess underwent incision and drainage and simple mastectomy was done in phylloide tumors. Conclusion: In the present study BBD occupy majority of total breast diseases. Fibro adenoma was the most common benign lesion (65.9%). FNAC was highly accurate and was highly reliable for fibro adenoma than for other lesions. Triple test is a prerequisite for determining management. However all fibro adenomas willing for surgical procedure were managed by simple excision than follow up. Conservative approach is acceptable in young patients, who choose conservative management, need to be informed about the limitation of the test, advised for proper follow up, and must be assessed properly if there are symptoms and clinical changes. Breast self examination should be emphasized as a part of female adult education.
Siniša Franjić
In most women, breast pain is not severe and disappears very quickly on its own. Severe pain, which is rare, can be relieved with medication. Benign breast diseases are common in young and older women, and malignant breast diseases most commonly occur around and after menopause. Although much rarer than benign changes, breast cancers are the most common cancers in women and represent a significant health problem. When she feels pain in her breast, the woman immediately thinks she has got breast cancer. Pain is not always a symptom of cancer. This paper discusses breast cancer, as the most common type of cancer in women, but also some other breast diseases that are not so common.
The Western journal of medicine
william goodson
Sushil Kachewar
Purpose: Cystic breast lesions are a common finding in young as well as elderly females. Although, mostly benign; they can at times be malignant too. Timely diagnosis is possible with help of Fine needle aspiration cytology (FNAC). This study was carried out with the aim of studying the panorama of various cystic breast lesions on FNAC in our setup. Materials and Methods: This was a four year prospective study carried out from May 2010 to January 2014. Cystic nature of breast mass was confirmed by palpation and by sonomammography. FNAC was then performed and the smears were stained with MGG and Papanicolaou stain. Results: Out of the 72 cases that were diagnosed to be cystic breast lesions clinically or on sonomammography, 64 were found to be benign and 08 were found to be malignant on FNAC. Retrospective imaging correlation of the 08 cystic cases revealed that they were of complex cystic nature and had either thick septae(03), solid areas (04) or dense contents (01) within. This in...
Scholar Science Journals
Background: Study of pattern of benign breast disease is a challenge due to variants in occurrence and presentation in different age groups and different geographical areas. The objective is to study the clinical profile and pattern of benign breast disease and its pathological correlation. Methods: This is a prospective study of females with breast disease presenting to surgery department over a period of one year. This survey was mainly meant for studying the age distribution, to evaluate the different types of benign diseases of the breast, their mode of clinical presentation and pathology and to evaluate the various modes of management for different types of Benign Breast Diseases. Patients with obvious malignancy and males were excluded from the study. Results: A total of 100 females were included in the study. Fibroadenoma (37%) and fibroadenosis (23%) were the commonest diseases,both presenting mostly at 21-30years of age. Left side involvement was most common. The commonest presentation was breast lump which comprised 84 (84%) cases, out of which 26 (26%) had associated complaints like breast pain and nipple discharge. Conclusion: Benign breast diseases are common problems of 2nd and 3 rd decade in females and raises considerable fear of malignancy. The patients of BBDs generally present with one or more of these complaints – breast lump, breast pain or nipple discharge. All the patients with discrete breast lumps should undergo a triple assessment to make an early diagnosis.
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
IET Journal
David Sales
Genetics Research International
Hussein Sabit
Emily Mazzola
Journal of Accounting and Finance in Emerging Economies
Danish Alam
European Journal of Radiology
Lorenzo Bonomo
World applied sciences journal
Hamida Hamdi
Arquivos Brasileiros de Neurocirurgia: Brazilian Neurosurgery
laila patricia fidelis dutra
Archaeologies
Aline Vieira de Carvalho
JOURNAL OF JAPAN SOCIETY FOR HEAD AND NECK SURGERY
Akihiro Shiotani
WSI-Mitteilungen
Yolanda Grift
Journal of Morphological Sciences
Jasna Bogdanska
Cornell University - arXiv
David Menotti
J-Plantasimbiosa
Marveldani Marveldani
American Journal of Infection Control
Sara Romano-Bertrand
Ius Matrimoniale
Piotr Morciniec
Research, Society and Development
Edson Barros
Ventana Indiscreta
Isaac León Frías
Molecular and Cellular Biology
Gladys Teitelman
Frontiers in Computational Neuroscience
Yosef Yarom
KLEBER MATOS
Cardiopulmonary physical therapy journal
Christiane Perme
Natural product research
The FEBS Journal
Nathalie Caplet
Zagazig Journal of Agricultural Research
留学生文凭证书办理须知 定做康卡迪亚大学毕业证书成绩单
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches

teacher appreciation
11 templates

memorial day
12 templates
13 templates

rain forest
23 templates

amusement park
5 templates
Breast Cancer Case
Breast cancer case presentation, free google slides theme, powerpoint template, and canva presentation template.
Clinical cases are so convenient, the medical community is always grateful for the information provided. In this occasion, we at Slidesgo have decided to create this new presentation template, focused on breast cancer, so that you can raise awareness about this important topic and help everyone get to know what they can do.
The visuals of the slides are attractive so that all the attendees feel relaxed and at ease while you give your presentation. The main color of the template is, as you can see, a pastel pink, so its brightness will grab attention easily, making the presentation a dynamic experience. The illustrations contain flat colors and no outlines, and the style is very beautiful—your audience will like it for sure. The icons are related to health, the human body and medicine, so using them for your topic is a good idea. Of course, reports and cases like this ask for a good amount of data, but don’t worry. We’ve made sure this template has everything you could need, such as maps, graphs and tables. The slide design is optimized too, so you can organize your information and text in a proper manner. In fact, the typography helps a lot, since the serif font used for titles is ideal for screens. The typeface that you’ll find in body text, on the other hand, is a sans-serif one, and has semi-rounded details. Start customizing this template in Google Slides or PowerPoint and share what you have to say about a breast cancer clinical case.
Features of this template
- A clinical case presentation with pink colors and health-related fill icons
- 100% editable and easy to modify
- 26 different slides to impress your audience
- Contains easy-to-edit graphics and maps
- Includes 1000+ icons and Flaticon’s extension for customizing your slides
- Designed to be used in Google Slides, Canva, and Microsoft PowerPoint
- 16:9 widescreen format suitable for all types of screens
- Includes information about fonts, colors, and credits of the free resources used
How can I use the template?
Am I free to use the templates?
How to attribute?
Attribution required If you are a free user, you must attribute Slidesgo by keeping the slide where the credits appear. How to attribute?
Related posts on our blog.

How to Add, Duplicate, Move, Delete or Hide Slides in Google Slides

How to Change Layouts in PowerPoint

How to Change the Slide Size in Google Slides
Related presentations.

Premium template
Unlock this template and gain unlimited access

Studies Assess Impact of Cancer Risk-Reduction Measures for People with BRCA Changes
April 15, 2024 , by Carmen Phillips

People with harmful changes, or pathogenic variants, in the BRCA1 or BRCA2 genes have a substantially increased risk of breast and ovarian cancer.
For women in whom gene testing finds “harmful changes” in the BRCA1 or BRCA2 genes, leading medical groups recommend that they take specific actions to lower their chances of being diagnosed with or dying from breast and ovarian cancer.
Results from two recent large studies now add to findings from earlier studies suggesting that following those recommendations can reduce the risk of dying from these cancers.
In one of the studies, women with harmful changes in BRCA1 who got periodic breast MRI scans, known as MRI surveillance, were less likely to die of breast cancer in the ensuing years than those who did not . The same benefit wasn't seen in women with harmful BRCA2 changes, however.
The second study analyzed the impact of surgery known as a risk-reducing bilateral salpingo-oophorectomy , which involves removing both ovaries and fallopian tubes . Those with harmful BRCA1 or BRCA2 changes who had the surgery, the study found, had a lower risk of dying from ovarian cancer and breast cancer than those who didn’t.
Results from both studies were published February 29 in JAMA Oncology .
“These studies show that [these] cancer risk management strategies … can save lives,” wrote Meghna Trivedi, M.D., and Katrina Armstrong, M.D., of Columbia University Irving Medical Center in an editorial that accompanied both studies .
Nearly all participants in the studies were White, however, raising the question of what these results mean for women of other ethnic and racial backgrounds.
“We have to be careful about how we interpret the results” for people in these groups, said Goli Samimi, Ph.D., of NCI’s Division of Cancer Prevention , who was not involved in the study.
“Hopefully [these findings] are the impetus to do similar studies that focus on enrolling a diverse population of participants,” Dr. Samimi said.

Recommendations for genetic testing, MRI surveillance versus reality
Inherited changes in a host of genes can increase cancer risk. Perhaps of most concern for breast and ovarian cancer are harmful changes (often called pathogenic variants) in BRCA1 and BRCA2 .
For example, 60% to 70% of people with harmful BRCA1 or BRCA2 changes will be diagnosed with breast cancer by the time they’re in their 70s, compared with only 13% of those who don’t have such changes.
BRCA Gene Mutations: Cancer Risk & Genetic Testing
What to know about the cancer risks of, and genetic testing for, mutations of the BRCA1 and BRCA2 genes.
Because of the substantial risk linked to these inherited genetic changes, leading cancer organizations recommend that people who have them consider taking measures to reduce the likelihood of developing or dying from either of these cancers, explained Tuya Pal, M.D., of the Vanderbilt-Ingram Comprehensive Cancer Center in Tennessee, a member of the study team.
But experts on inherited cancers stress, however, that recommendations are one thing. Their use in the real world is another matter entirely. The barriers and challenges are numerous, Drs. Trivedi and Armstrong wrote.
“First and foremost, more must be done to increase the identification of” people who have harmful BRCA1 and BRCA2 changes, in the form of more genetic testing , they wrote.
The study’s lead investigator, Steven Narod, M.D., of Women’s College Hospital in Toronto, agreed. Recent studies show that genetic testing among at-risk people is increasing. But the fact remains, Dr. Narod said, that “too few people are getting tested.”
For those who are able to get tested, Dr. Pal stressed that it’s critical to get counseling first by a provider with experience in genetics and cancer risk. Such counseling can help people understand what the different test results mean for them personally, including the possible risk reduction measures.
Access to licensed genetic counselors can be an issue for some people, Dr. Samimi said. One study, for example, showed that they are largely concentrated in heavily populated areas .
Getting MRI surveillance can also be a challenge. There are barriers like transportation issues and lack of access to facilities that can perform MRI scans. And despite the recommendations from medical organizations, not all insurers cover MRI surveillance of women with harmful BRCA1 and BRCA2 changes.
Given the continued challenges around the understanding of and access to recommended risk-reduction measures, Dr. Samimi said, the more evidence to support and raise awareness about them the better.
That’s where the large international research program Dr. Narod helped initiate in the mid-1990s, called the Hereditary Breast Cancer Clinical Study Group, comes in. Known as a cohort study , it was initially planned to include just a few hundred participants. It now has nearly 20,000 people with harmful BRCA1 or BRCA2 changes.
Reductions in breast cancer deaths
The study of MRI surveillance included about 2,500 women who participate in this larger research program. About 1,750 had MRI surveillance during the study, and on average, they had five MRIs during follow-up.
Participants were followed for an average of about 9 years, and about 14% in both the MRI and non-MRI groups were diagnosed with breast cancer during the study.
Only a small number of participants died from breast cancer during the study. But among those with harmful BRCA1 changes, getting MRI surveillance was estimated to reduce the deaths from breast cancer over the following 20 years by about 3%.
The reduced likelihood of dying from breast cancer in women with harmful BRCA1 changes was also seen when the comparison was restricted to women in the nonsurveillance group who had at least one mammogram during the study period.
As for the lack of a statistical reduction in breast cancer deaths for those with BRCA2 changes, it may be largely due to two factors, Dr. Narod said: the small number of participants with these changes and who had died from breast cancer.
Surgery reduces likelihood of dying from breast, ovarian cancer
The other study included nearly 4,300 women, of whom about two-thirds had had surgery. All participants had at least a bilateral oophorectomy (removal of both ovaries) and most had a salpingo-oophorectomy (removal of both ovaries and fallopian tubes).
About 20% of all participants were diagnosed with cancer during the study period (a median follow-up of 9 years), mostly breast and ovarian cancers, and most deaths were from cancer.
The percentage of breast cancer diagnoses were very similar between those who did and didn’t have the preventive surgery, but the percentage of ovarian cancer diagnoses was markedly higher in those who didn’t get the surgery.
Overall, participants who had oophorectomy were less likely to die from any cause, which was the study’s primary measure.
For ovarian cancer specifically, about 3.5% of those who didn’t get surgery died from ovarian cancer during the study period, compared with about 0.25% of those who did have the surgery. For breast cancer, it was 2% and 1%.
More genetic testing, maximizing risk-reducing care
Both studies, Dr. Pal said, provide strong evidence about the potential benefits of MRI surveillance or a salpingo-oophorectomy. “That’s very impactful information,” she said.

Low Rates of Genetic Testing in Ovarian, Breast Cancer
Test results can guide treatment decisions, follow-up screening.
Dr. Samimi said she’s hopeful that these new findings will further increase awareness about testing among those at risk of having inherited harmful genetic changes, and inform discussions between doctors and their patients about the options for reducing that risk.
And those conversations will hopefully extend to close blood relatives of those found to have these changes, she said.
“We have to do a better job of reaching out to families about their risk,” she continued.
NCI is funding one such effort. Called Traceback , the program is focused on helping researchers identify women who have had ovarian cancer but never got tested for cancer-related genetic changes. After they are found, they and their family members will be offered a chance to be tested.
In Canada, Dr. Narod noted, there’s a study called the Screen Project that offers testing for harmful BRCA1 and BRCA2 changes to Canadian citizens aged 18 and older.
Drs. Armstrong and Trivedi stressed that there’s work to do across the board to “maximize” the care needed to prevent more breast and ovarian cancer deaths. Achieving that goal, they continued, “will require providing equitable access and [insurance] coverage” of all recommended risk-reduction actions.
Featured Posts
March 27, 2024, by Edward Winstead
March 21, 2024, by Elia Ben-Ari
March 5, 2024, by Carmen Phillips
- Biology of Cancer
- Cancer Risk
- Childhood Cancer
- Clinical Trial Results
- Disparities
- FDA Approvals
- Global Health
- Leadership & Expert Views
- Screening & Early Detection
- Survivorship & Supportive Care
- February (6)
- January (6)
- December (7)
- November (6)
- October (7)
- September (7)
- February (7)
- November (7)
- October (5)
- September (6)
- November (4)
- September (9)
- February (5)
- October (8)
- January (7)
- December (6)
- September (8)
- February (9)
- December (9)
- November (9)
- October (9)
- September (11)
- February (11)
- January (10)
- Open access
- Published: 04 May 2024
Effect of young age (below 40 years) on oncologic outcomes in Lebanese patients with breast cancer: a matched cohort study
- Eman Sbaity 1 ,
- Hani Tamim 2 ,
- Ghada El-Hajj Fuleihan 2 , 3 , 4 ,
- Jaber Abbas 1 ,
- Mariam Zahwe 5 ,
- Razan El Sayed 6 &
- Ali Shamseddine 7
BMC Cancer volume 24 , Article number: 560 ( 2024 ) Cite this article
192 Accesses
2 Altmetric
Metrics details
Developing countries have a significantly higher incidence of breast cancer in patients younger than 40 years as compared to developed countries. This study aimed to examine if young age at diagnosis is an independent prognostic factor for worse survival outcomes in breast cancer as well as the effect of age on Disease-free survival (DFS) and local recurrence free survival (LRFS) after adjusting for various tumor characteristics, local and systemic treatments.
This is a secondary analysis of prospective cohort of patients from two existing databases. We identified patients with breast cancer aged 40 years or less and we matched them to those older than 40 years. We also matched based on stage and molecular subtypes. In cohort 1, we matched at a ratio of 1:1, while in cohort 2 we matched at a ratio of 1:3.
In cohort 1, Disease-free survival (DFS) at 5 years was significantly shorter for those younger than 40 years (75.6% and 92.7% respectively; p < 0.03). On multivariate analysis, only chemotherapy was found to be significant, while age was not found to be an independent predictor of prognosis. Local recurrence free survival at 5 years was similar between both age categories. Only hormonal therapy is a significant predictor for LRFS at 5 years. In the second cohort, DFS and LRFS at 3 years were similar between those younger and those older than 40 years. On multivariate analysis, no factor including age was found to be an independent predictor of prognosis.
Data in the literature is controversial on the effect of young age on breast cancer prognosis. Our findings could not demonstrate that age is an independent prognostic factor in our population. There is a need for outcomes from larger, prospective series that have longer follow-ups and more data from our region.
Peer Review reports
Breast cancer is the most common cancer in females globally, with 2.3 million women diagnosed with breast cancer in 2020 [ 1 ]. Median age of breast cancer varies between developed countries of 41.9 years [ 2 ] compared to 44–48 years in developing countries [ 3 , 4 ]. As for Lebanon, the median age is 49.8 years [ 5 ].
Although breast cancer does not commonly occur in patients younger than 40 years of age, it is a leading cause of death from cancer in this young population. The proportion of young patients diagnosed with breast cancer is much higher in developing countries, 19-33.3% in Arab countries [ 6 , 7 , 8 , 9 ] compared to developed countries, 5–7% in the United States of America. This may be explained by different population pyramid, environmental or genetic factors [ 10 ].
Reports of breast cancers in young patients show higher proportions of adverse clinic-pathologic features, Her2 neu expression, Estrogen receptors (ER)- and progesterone receptor (PR)-negative tumors, and high-grade tumors that tend to be larger and to involve regional lymph nodes [ 11 , 12 , 13 ]. In addition, authors documented a different distribution of molecular breast cancer subtypes between young breast cancer and older population [ 14 ].
The effect of young age on oncologic outcomes is controversial in the literature. Initially, physicians attributed the worse prognosis of breast cancer at a younger age to an advanced stage of presentation, adverse pathologic subtypes, and less aggressive treatments [ 15 , 16 , 17 , 18 ]. This is supported by results from a large series of patients showing young age to be an independent risk factor for worse disease-free survival (DFS), Distant Disease-Free Survival (DDFS), and overall survival (OS) [ 18 , 19 ]. Other authors consider young age as a surrogate marker of more advanced stage or more aggressive phenotypes resulting in worse prognosis.
Due to the perception of a more aggressive disease, young breast cancer patients frequently receive total mastectomies. Thus, it is of high clinical importance to understand whether breast cancer surgery (BCS) is associated with a higher risk of local recurrence to better counsel young patients. Many large retrospective series showed a higher rate of local recurrence in BCS as compared to total mastectomy performed at a young age, but no difference in survival [ 18 , 20 , 21 , 22 , 23 , 24 , 25 ]. Thus, when indicated, BCS is still a viable option for young patients..
The aim of this cohort study is to examine if young age at diagnosis is an independent prognostic factor for worse survival outcomes in breast cancer as well as the effect of age on DFS and local recurrence free survival (LRFS) after adjusting for various tumor characteristics, local and systemic treatments received.
Methodology
Study design.
We conducted a secondary analysis of two existing prospective cohorts of breast cancer patients. We matched patients younger than 40 years to those older than 40 years at a ratio of 1:3. We matched cases based on the stage of breast cancer at presentation and molecular subtypes.
Data sources
The study is a secondary analysis of two existing databases. The first is prospectively collected data of all Lebanese non-metastatic breast cancer patients who received any part of their treatment at the American University of Beirut Medical Center (AUBMC) between the years 2011–2014 to study the difference in outcomes between the two age groups (IRB study #IM.AS.17). It includes 123 Lebanese patients (with 47 patients below the age of 40 years). The second is an IRB-approved prospectively collected database of the clinical research unit at Basile Cancer Institute at AUBMC (BIO-2018-0302), including all consecutive breast cancer patients who have presented to AUBMC from October 2014 to December 2016. Informed consent to participate in the initial studies was obtained from all participants. We performed a comparison between both datasets regarding tumor characteristics and received treatments. This revealed statistically significant differences in both populations, so we decided to analyze each cohort separately.
Eligibility criteria
We included patients with:
Non-metastatic biopsy-proven breast cancer.
Lebanese women, older than 18 years.
Received any part of their treatment or followed up at AUBMC.
We excluded:
Male breast cancer patients.
Patients with unclassified tumor.
Patients with missing data on stage or ER, PR, or Her2 NEU or staging information.
Sampling Frame
At our institution, breast cancer patients are treated by dedicated breast surgical oncologists, breast medical oncologists, and breast radiation oncologists, ensuring similar and up-to-date treatment plans based on National Comprehensive Cancer Network (NCCN) guidelines, American Society of Cancer Oncology (ASCO), and ASBS (American Society of Breast Surgery). In addition, most of these patients are discussed in the weekly Breast Tumor Board before initiation of treatments.
Outcome measures
Primary outcome:
DFS at 3 years, defined by survival without clinical or radiological evidence of recurrence of disease, whether local, distant, or both.
Secondary outcomes:
Local recurrence Free Survival at 3 years (LRFS) defined by clinical or radiological evidence of disease in the affected breast or regional nodal basin.
Overall Survival (OS) at 3 years defined from time of diagnosis till date of death or last follow up.
Distant Metastasis Free Survival (DMFS) is defined from the date of diagnosis till the date of distant metastasis or till the date of last follow up in patients who did not experience metastasis.
Effect of various tumor grade, local and systemic treatments received on DFS, LRFS, and DMFS.
Statistical analysis
We conducted all analyses using SPSS Version 24, and statistical significance was assumed at a p < 0.05. Prognostic factors were compared between the two groups using chi-square test for categorical variables and independent t-test for continuous variables. We estimated DFS, LRFS, DMFS, and OS, using Kaplan–Meier method and Log-Rank test for the different survival curves between both age categories. We then performed a univariate analysis comparing the effect of each grade of tumor, chemotherapy, Hormonal therapy, Herceptin, type of surgery, radiation therapy, and BMI on DFS, LRFS, and DMFS at three years follow up. We used Cox regression analysis to assess how survival outcomes change between both age groups after controlling for grade of tumor, chemotherapy, hormonal therapy, Herceptin therapy, surgery type, and radiation therapy. COX Regression was done using the forward and backward methods.
Description
The first cohort included 122 breast cancer patients, 77 patients above the age of 40 years, and 45 patients below or equal to 40 years. We performed 1:1 matching, where 41 breast cancer patients aged 40 or younger were matched to 41 breast cancer patients older than 40. The patients’ molecular subtypes and stages are shown in Table 1 .
Comparison of treatments received
Total mastectomy was performed only in onethird of patients above 40 years as compared to 56% of patients below 40 years with p = 0.026. Radiotherapy and chemotherapy were administered in a similar proportion for both groups without any statistical difference. A higher proportion of patients in the younger subgroup received trastuzumab as compared to the older subgroup, 30% and 12.2% respectively ( p = 0.049). Similarly, patients in the younger subgroup are more likely to receive hormonal therapy, but without reaching a statistical significance. (Table 1 )
Only one death is documented in the older subgroup, and two deaths in the younger subgroup. Local recurrence is double in the younger age group, with 6 local recurrence events (14.6%) compared to 3 local recurrence events (7.3%) in the older age group. Distant metastasis occurred more in the younger age groupin 9 patients (22%) compared to 6 (14.6%) in the older age group.
Survival analysis
DFS at 5 years : in young patients, the DFS is 75.6% compared to 92.7% in older patients with p = 0.035. In patients who received chemotherapy, DFS is lower in the younger age group,74.1% compared to 100% in those older than 40 years, with a statistically significant p -value of 0.005. Similarly, in patients who received hormonal therapy, DFS is lower in the younger subgroup of patients, at76.5% compared to 96.8%, with a p -value of 0.016. On multivariate analysis, only chemotherapy was an independent prognostic factor for DFS at 5 years. Age was not found to be an independent prognostic factor for DFS. (Table 2 )
LRFS at 5 years : among those above 40 years, the is 92.7% (3 local recurrence events) and 87.8% (5 local recurrence events) among those below or equal to 40 years ( p = 0.361).
We did not find any clinically or statistically significant difference when stratifying LRFS at 5 years according to the different loco-regional and systemic therapies. Patients who underwent partial mastectomy have an LRFS of 96.4% in the older group and 94.4% in the younger group, with no statistical significance ( p = 0.655). For those who underwent total mastectomy, LRFS is 84.6% and 82.6% in the older and younger group, respectively ( p = 0.821). In multivariate cox regression analysis, only hormonal therapy was found to be a predictor for worse LRFS at 5 years, while age was not found to be an independent prognostic factor.
OS at 5 years : in the above 40 years group, the overall survival at 5 years is 97.6% and 95.1% in the below or equal to 40 years group, with no statistical significance ( p = 0.490) (Table 3 ).
There are a total of 399 patients in cohort 2, with 55 breast cancer patients aged 40 or younger matched to 165 breast cancer patients older than 40 years, at a 1:3 ratio. In the older age group, a total of 40 patients (28%) had grade 3 breast cancer, compared to 22 patients (44%) in the younger age category with a significant p -value of 0.03 (Table 4 ).
Mastectomy was performed more frequently in the older group, but the difference is not statistically significant ;76 (46.6%) patients above 40 years underwent total mastectomy as compared to 20 (37%) patients below 40 years ( p = 0.219). For radiation therapy, 67.7% of patients over 40 years received radiotherapy, and 64.8% of patients in the younger group ( P = 0.698). Both age subgroups received chemotherapy in a similar proportion, with 74.4% of patients in the above 40 years groupand 77.4% in the below or equal to 40 years group ( p -value of 0.663). A higher proportion of patients in the younger subgroup received trastuzumab and hormonal therapy as compared to the older subgroup but without reaching statistical significance. A total of 81.3% of patients younger than 40 years received hormonal therapy compared to 69.7% of patients older than 40 years ( p = 0.119).
No deaths are documented in any subgroup. Local recurrence did not occur in the younger group, and only 1 event (0.6%) occurred in the older group. Distant metastasis occurred in 1 patient (1.8%) in the below 40 years subgroup and in 6 patients (3.6%) in the older age group.
DFS at 3-years : is slightly shorter for the younger age patient category but without reaching statistical significance (97% versus 98.2%; p = 0.621). DFS is 100% for partial mastectomy in the younger group and 97.7% (2 events) in the older group ( p = 0.346). Among patients treated with total mastectomy, DFS is 97.4% in the older group and 95% in the younger group, with no statistical significance ( p = 0.645). On multivariate Cox regression analysis for DFS at 3 years for cohort 2, no factor was found to be a significant predictor of survival.
LRFS at 3 years : local recurrence occurred only in 1 patient (99.4%) in the younger group and none in the older group. ( p = 0.537). On multivariate Cox regression analysis for cohort 2, no factor was found to be a significant predictor of survival for LRFS at 3 years.
In our first cohort, the distribution of early and advanced breast cancer was similar. In the second cohort, older breast cancer patients were more likely to be present in the early stages. This result was similar to that reported by many authors who mentioned that young patients with breast cancer present with a more aggressive clinical picture and advanced stage as compared to older patients. Cancers in the younger age group are usually detected by the patients themselves and,consequently, are often bigger in size and more advanced than the screen-detected tumors in those above 40 years [ 26 , 27 ].
We had a similar proportion of molecular subtypes in both age categories, with a slightly higher proportion of Triple negative molecular subtype in our young patient population. This is different from the proportions known for breast cancer patients. The literature reports on a difference in the distribution of breast cancer molecular subtypes between younger and older patients [ 14 , 28 ]. Variability in molecular subtyping among different populations may be due to variability in pathology reviews and different definitions to categorize the 4 subtypes, where mainly the confusion happens with deciding on luminal A and B.
Age was not found to be an independent prognostic factor in our cohort of patients, which is matched for stage and molecular subtype and after adjusting for treatments received. DFS after 5 years was statistically lower in the younger group. However, LRFS at 3 years and 5 years were not statistically different between both age categories. Nixon et al. reported similar results where young breast cancer has a higher local recurrence rate and inferior DFS [ 12 , 13 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 ]. Recurrence events in breast cancer usually happen at a median of 32 months, which falls within our follow-up period. Nevertheless, a longer follow-up is required to make a solid conclusion.
When we stratified the outcomes according to the type of surgery done, there was no significant difference in the DFS at 3 and 5 years and LRFS at 3 years in both age categories. This result was similar to the National Cancer Institute randomized study that showed similar local recurrence between both arms of treatment for BCS and total mastectomy [ 38 , 39 ]. Age was not found to be a predictor of local recurrence when total mastectomy was performed. However, in the Institut Gustave-Roussy Breast Cancer Group Distribution of local recurrence based on age grouping of less than and more than 40 years, there was a three times higher rate of local recurrence in the younger patients with BCS.
On univariate analysis of cohort 1, patients receiving radiotherapy and those below 40 years had lower 5-year DFS, but this difference was not statistically significant ( p = 0.093). We cannot compare our results to the literature because the majority of studies did not report on the use of radiation therapy after BCS, so we cannot identify those local recurrences secondary to lack of radiation. Similarly, it is not possible to discern the effect of post mastectomy radiation on preventing local recurrences.
In the strata of patients who received chemotherapy, DFS is lower in the younger age group, 74.1% compared to 100%, in those older than 40 years, with a statistically significant p -value. On multivariate analysis, only chemotherapy was an independent prognostic factor for DFS at 5 years. Age was not found to be an independent prognostic factor for DFS. Similarly, we did not find a statistically significant difference when we stratified LRFS at 5 years for the chemotherapy treatments. On the contrary, the Beadle et al. study [ 40 ] showed that local therapies did not affect the rate of local recurrence in young patients, but systemic therapy did affect it with statistical significance. This speaks about a different biology in young patients, where perhaps even in stage I, chemotherapy should be given to improve oncologic outcomes.
In the strata of patients in cohort 1, patients who received hormonal therapy had statistically significant lower DFS at 5 years in the younger subgroup of patients but not for LRFS at 5 years. On multivariate Cox regression analysis, only hormonal therapy was found to be a predictor for worse LRFS at 5 years, while age was not found to be an independent prognostic factor. ER-positive is reported in the literature to be associated with worse prognosis in the younger population. Some attribute this to the fact that young patients were not treated with hormonal therapy until recently. Consequently, the worse prognosis observed in the young population of ER-positive cancermay be due to the differential use of Tamoxifen. In addition, even after treating young breast cancer patients with Tamoxifen, there is high non-compliance. This was demonstrated by a systematic review by Murphy et al. [ 41 ].
Among those who received trastuzumab, LRFS is 100% in the older group and 83.3% in the younger group ( p = 0.315). For those who did not receive trastuzumab, LRFS is similar, with 91.7% in the older group and 89.3% in the younger group, with no statistical significance ( p = 0.629). Many studies that explored local recurrence in a large cohort of breast cancer patients included patients from the era before the introduction of trastuzumab in the treatment of Her 2 positive breast cancer. This is a major limitation of such studies because trastuzumab dramatically improved in oncologic outcomes when indicated.
Strengths and limitations
This study aimed to fill a gap in the literature where there is limited data from the modern era of effective surgery, chemotherapy, hormonal, and radiation therapy in young patients. The reported data on the effect of age on breast cancer outcomes is widely retrospective; our data is prospectively collected. Another strength of our study is matching the two age cohorts on the two most important baseline prognostic factors (stage and molecular phenotype). Data on local recurrence after BCT in young patients mainly camefrom series collected over long periods of time and did not receive the modern modalities of breast cancer treatments. Our cohort of patients is a modern cohort treated based on modern therapies.
Because there is no breast cancer national comprehensive database, we could not compare our cohort characteristics to national and thus decide on the generalizability of our results. We have a limited follow-up period for our patients, where the majority reach only 3 years of follow-up.
Data availability
The datasets analyzed in the current study are available on request from the corresponding author.
Abbreviations
Estrogen Receptors
Progesterone Receptor
Disease Free Survival
Distant Disease-Free Survival
Overall Survival
Breast Cancer Surgery
Local Recurrence Free Survival
American University of Beirut Medical Center
Human Epidermal Growth Factor Receptor 2
National Comprehensive Cancer Network
American Society of cancer Oncology
American Society of Breast Surgery
Distant Metastasis Free Survival
Breast-conserving therapy
WHO. Breast cancer 2021 [Available from: https://www.who.int/news-room/fact-sheets/detail/breast-cancer .
Dafni U, Tsourti Z, Alatsathianos I. Breast Cancer statistics in the European Union: incidence and survival across European Countries. Breast Care. 2019;14(6):344–53.
Article PubMed PubMed Central Google Scholar
Obiorah CC, Abu EK. Breast cancer in Rivers State, Nigeria: ten-year review of the Port Harcourt cancer registry. South Afr J Oncol. 2019;3.
Mehdi I, Monem EA, Bahrani BJA, Kharusi SA, Nada AM, Lawati JA, et al. Age at diagnosis of female breast cancer in Oman: issues and implications. South Asian J Cancer. 2014;03(02):101–6.
Article Google Scholar
El Saghir NS. Increased age adjusted incidence rates in younger-aged groups at presentation. In Lebanon and arab countries. Implications for screening and for europeans, australians and americans of Arabic origins. Eur J Cancer Suppl. 2004;2(3):187–8.
Bharat A, Aft RL, Gao F, Margenthaler JA. Patient and tumor characteristics associated with increased mortality in young women (≤ 40 years) with breast cancer: young women with breast Cancer. J Surg Oncol. 2009;100(3):248–51.
Article PubMed Google Scholar
Elkum N, Dermime S, Ajarim D, Al-Zahrani A, Alsayed A, Tulbah A, et al. Being 40 or younger is an independent risk factor for relapse in operable breast cancer patients: the Saudi Arabia experience. BMC Cancer. 2007;7(1):222.
AlZaman AS, Mughal SA, AlZaman YS, AlZaman ES. Correlation between hormone receptor status and age, and its prognostic implications in breast cancer patients in Bahrain. SMJ. 2016;37(1):37–42.
Peng R, Wang S, Shi Y, Liu D, Teng X, Qin T, et al. Patients 35 years old or younger with operable breast cancer are more at risk for relapse and survival: a retrospective matched case–control study. The Breast. 2011;20(6):568–73.
Chouchane L, Boussen H, Sastry KSR. Breast cancer in arab populations: molecular characteristics and disease management implications. Lancet Oncol. 2013;14(10):e417–e24.
Article CAS PubMed Google Scholar
Colleoni M, Rotmensz N, Robertson C, Orlando L, Viale G, Renne G, et al. Very young women (< 35 years) with operable breast cancer: features of disease at presentation. Ann Oncol. 2002;13(2):273–9.
Albain KS, Allred DC, Clark GM. Breast cancer outcome and predictors of outcome: are there age differentials? J Natl Cancer Inst Monogr. 1994(16):35–42.
Nixon AJ, Neuberg D, Hayes DF, Gelman R, Connolly JL, Schnitt S, et al. Relationship of patient age to pathologic features of the tumor and prognosis for patients with stage I or II breast cancer. JCO. 1994;12(5):888–94.
Article CAS Google Scholar
Azim HA, Michiels S, Bedard PL, Singhal SK, Criscitiello C, Ignatiadis M, et al. Elucidating Prognosis and Biology of breast Cancer arising in Young Women using gene expression profiling. Clin Cancer Res. 2012;18(5):1341–51.
Adami H-O, Malker B, Holmberg L, Persson I, Stone B. The relation between survival and age at diagnosis in breast Cancer. N Engl J Med. 1986;315(9):559–63.
de la Rochefordière A, Campana F, Fenton J, Vilcoq JR, Fourquet A, Asselain B, et al. Age as prognostic factor in premenopausal breast carcinoma. The Lancet. 1993;341(8852):1039–43.
Dubsky PC, Gnant MFX, Taucher S, Roka S, Kandioler D, Pichler-Gebhard B, et al. Young Age as an independent adverse prognostic factor in Premenopausal patients with breast Cancer. Clin Breast Cancer. 2002;3(1):65–72.
Oh JL, Bonnen M, Outlaw ED, Schechter NR, Perkins GH, Strom EA, et al. The impact of young age on locoregional recurrence after doxorubicin-based breast conservation therapy in patients 40 years old or younger: how young is young? Int J Radiation Oncology*Biology*Physics. 2006;65(5):1345–52.
Liedtke C, Hess KR, Karn T, Rody A, Kiesel L, Hortobagyi GN, et al. The prognostic impact of age in patients with triple-negative breast cancer. Breast Cancer Res Treat. 2013;138(2):591–9.
Recht A, Connolly JL, Schnitt SJ, Silver B, Rose MA, Love S, et al. The effect of young age on tumor recurrence in the treated breast after conservative surgery and radiotherapy. Int J Radiation Oncology*Biology*Physics. 1988;14(1):3–10.
Kurtz JM, Jacquemier J, Amalric R, Brandone H, Ayme Y, Hans D, et al. Why are local recurrences after breast-conserving therapy more frequent in younger patients? JCO. 1990;8(4):591–8.
Kurtz JM, Spitalier J-M, Amalric R, Brandone H, Ayme Y, Bressac C, et al. Mammary recurrences in women younger than forty. Int J Radiation Oncology*Biology*Physics. 1988;15(2):271–6.
Kim SH, Simkovich-Heerdt A, Tran KN, Maclean B, Borgen PI. Women 35 years of age or younger have higher Locoregional Relapse Rates after undergoing breast conservation therapy. J Am Coll Surg. 1998;187(1):1–8.
van der Sangen MJC, Poortmans PMP, Scheepers SWM, Lemaire BMD, van Berlo CLH, Tjan-Heijnen VCG, et al. Prognosis following local recurrence after breast conserving treatment in young women with early breast cancer. Eur J Surg Oncol (EJSO). 2013;39(8):892–8.
Kroman N, Holtveg H, Wohlfahrt J, Jensen M-B, Mouridsen HT, Blichert-Toft M, et al. Effect of breast-conserving therapy versus radical mastectomy on prognosis for young women with breast carcinoma. Cancer. 2004;100(4):688–93.
Ruddy KJ, Gelber S, Tamimi RM, Schapira L, Come SE, Meyer ME, et al. Breast cancer presentation and diagnostic delays in young women: breast ca Presentation in Young Women. Cancer. 2014;120(1):20–5.
Foxcroft LM, Evans EB, Porter AJ. The diagnosis of breast cancer in women younger than 40. The Breast. 2004;13(4):297–306.
Collins LC, Marotti JD, Gelber S, Cole K, Ruddy K, Kereakoglow S, et al. Pathologic features and molecular phenotype by patient age in a large cohort of young women with breast cancer. Breast Cancer Res Treat. 2012;131(3):1061–6.
Adami H-O, Malker B, Meirik O, Persson I, Bergkvist L, Stone B. Age as a prognostic factor in breast cancer. Cancer. 1985;56(4):898–902.
Fowble BL, Schultz DJ, Overmoyer B, Solin LJ, Fox K, Jardines L, et al. The influence of young age on outcome in early stage breast cancer. Int J Radiation Oncology*Biology*Physics. 1994;30(1):23–33.
Chung M, Chang HR, Bland KI, Wanebo HJ. Younger women with breast carcinoma have a poorer prognosis than older women. Cancer. 1996;77(1):97–103.
Ahn SH, Son BH, Kim SW, Kim SI, Jeong J, Ko S-S, et al. Poor outcome of hormone receptor–positive breast Cancer at very young age is due to tamoxifen resistance: Nationwide Survival Data in Korea—A Report from the Korean breast Cancer Society. JCO. 2007;25(17):2360–8.
Fredholm H, Eaker S, Frisell J, Holmberg L, Fredriksson I, Lindman H. Breast Cancer in Young women: poor survival despite intensive treatment. PLoS ONE. 2009;4(11):e7695.
Gnerlich JL, Deshpande AD, Jeffe DB, Sweet A, White N, Margenthaler JA. Elevated breast Cancer mortality in women younger than Age 40 years compared with older women is attributed to poorer survival in early-stage disease. J Am Coll Surg. 2009;208(3):341–7.
Xiong Q, Valero V, Kau V, Kau S-W, Taylor S, Smith TL, et al. Female patients with breast carcinoma age 30 years and younger have a poor prognosis: the M. D. Anderson Cancer Center experience. Cancer. 2001;92(10):2523–8.
El Saghir NS, Seoud M, Khalil MK, Charafeddine M, Salem ZK, Geara FB, et al. Effects of young age at presentation on survival in breast cancer. BMC Cancer. 2006;6(1):194.
Gajdos C, Tartter PI, Bleiweiss IJ, Bodian C, Brower ST. Stage 0 to stage III breast cancer in young women1. J Am Coll Surg. 2000;190(5):523–9.
Poggi MM, Danforth DN, Sciuto LC, Smith SL, Steinberg SM, Liewehr DJ, et al. Eighteen-year results in the treatment of early breast carcinoma with mastectomy versus breast conservation therapy: the National Cancer Institute randomized trial. Cancer. 2003;98(4):697–702.
Jacobson JA, Danforth DN, Cowan KH, d’Angelo T, Steinberg SM, Pierce L, et al. Ten-year results of a comparison of conservation with mastectomy in the treatment of stage I and II breast Cancer. N Engl J Med. 1995;332(14):907–11.
Beadle BM, Woodward WA, Tucker SL, Outlaw ED, Allen PK, Oh JL, et al. Ten-year recurrence rates in young women with breast cancer by locoregional treatment approach. Int J Radiat Oncol Biol Phys. 2009;73(3):734–44.
Murphy CC, Bartholomew LK, Carpentier MY, Bluethmann SM, Vernon SW. Adherence to adjuvant hormonal therapy among breast cancer survivors in clinical practice: a systematic review. Breast Cancer Res Treat. 2012;134(2):459–78.
Article CAS PubMed PubMed Central Google Scholar
Download references
Acknowledgements
The authors acknowledge the contribution of Ahmad Najia and Nadia Hoyek who were involved in this research under the Medical Research Volunteer Program (MRVP) at the American University of Beirut.
Author information
Authors and affiliations.
Department of Surgery, American University of Beirut Medical Center, P.O. Box: 11-0236, Riad El-Solh, Beirut, 1107 2020, Lebanon
Eman Sbaity & Jaber Abbas
Department of Internal Medicine, American University of Beirut Medical Center, Beirut, Lebanon
Hani Tamim & Ghada El-Hajj Fuleihan
Calcium Metabolism and Osteoporosis Program, American University of Beirut, Beirut, Lebanon
Ghada El-Hajj Fuleihan
Scholars in HeAlth Research Program (SHARP), American University of Beirut Medical Center, Beirut, Lebanon
Faculty of Medicine, American University of Beirut, Beirut, Lebanon
Mariam Zahwe
Center for Translational Injury Research, Department of Surgery, McGovern Medical School, University of Texas Health Science Center (UT Health), Houston, USA
Razan El Sayed
Department of Hematology/Oncology, American University of Beirut Medical Center, Beirut, Lebanon
Ali Shamseddine
You can also search for this author in PubMed Google Scholar
Contributions
Methodology: E.S, H.T, G.E, A.S; Resources: A.S, J.A; Data Curation: E.S; Data Analysis: E.S, H.T; Writing - original draft: E.S; Writing – review & editing: H.T, G.E, A.S, J.A, M.Z, R.E. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Eman Sbaity .
Ethics declarations
Ethics approval and consent to participate.
This study is a secondary analysis of two IRB-approved databases at the American University of Beirut Medical Center. All methods of the initial studies were carried out in accordance with the Declaration of Helsinki guidelines and regulations and got approved by the Institutional Review Board of the American University of Beirut Medical Center. (IRB number: IM.AS.17) (BIO-2018-0302). Informed consent to participate in the study was obtained from all participants included in the initial studies.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Sbaity, E., Tamim, H., El-Hajj Fuleihan, G. et al. Effect of young age (below 40 years) on oncologic outcomes in Lebanese patients with breast cancer: a matched cohort study. BMC Cancer 24 , 560 (2024). https://doi.org/10.1186/s12885-024-11910-w
Download citation
Received : 17 February 2023
Accepted : 22 January 2024
Published : 04 May 2024
DOI : https://doi.org/10.1186/s12885-024-11910-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Breast cancer
ISSN: 1471-2407
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Skip to content
- Skip to navigation
- Skip to footer
Enhertu demonstrated statistically significant and clinically meaningful improvement in progression-free survival in HR-positive, HER2-low metastatic breast cancer following one or more lines of endocrine therapy in DESTINY-Breast06 Phase III trial
Astrazeneca and daiichi sankyo’s enhertu also demonstrated a clinically meaningful progression-free survival improvement in patients with her2-ultralow expression .
Positive high-level results from the DESTINY-Breast06 Phase III trial showed that Enhertu (trastuzumab deruxtecan) demonstrated a statistically significant and clinically meaningful improvement in progression-free survival (PFS) compared to standard-of-care chemotherapy in the primary trial population of patients with HR-positive, HER2-low (IHC 1+ or 2+/ISH-) metastatic breast cancer following one or more lines of endocrine therapy.
A statistically significant and clinically meaningful improvement in PFS was also observed in the overall trial population (patients with HER2-low and HER2-ultralow [defined as IHC 0 with membrane staining; IHC >0<1+] metastatic breast cancer). A prespecified subgroup analysis showed the clinically meaningful improvement was consistent between patients with HER2-low and HER2-ultralow expression.
Overall survival (OS) data were not mature at the time of the analysis; however, Enhertu showed an early trend towards an OS improvement versus standard-of-care chemotherapy in patients with HER2-low metastatic breast cancer and in the overall trial population. The trial will continue as planned to further assess OS and other secondary endpoints.
Susan Galbraith, Executive Vice President, Oncology R&D, AstraZeneca, said: “DESTINY-Breast06 shows that Enhertu could become a new standard of care for patients with HER2-low and HER2-ultralow metastatic breast cancer following one or more lines of endocrine therapy. These data underscore the potential for treatment with Enhertu across the spectrum of HR-positive breast cancer, further redefining the treatment of metastatic breast cancer.”
Ken Takeshita, Global Head, R&D, Daiichi Sankyo, said: “The topline results from DESTINY-Breast06 highlight the importance of continuing to challenge current treatment paradigms and established breast cancer classifications to evolve how we treat patients with HR-positive, HER2-expressing metastatic breast cancer. Building on the practice-changing data seen in DESTINY-Breast04, these results reinforce the potential for use of Enhertu earlier in the treatment landscape and in an even broader patient population.”
Enhertu is a specifically engineered HER2-directed DXd antibody drug conjugate (ADC) discovered by Daiichi Sankyo and being jointly developed and commercialised by AstraZeneca and Daiichi Sankyo.
It is estimated that approximately 60-65% of HR-positive, HER2-negative breast cancers are HER2-low and potentially an additional 25% may be HER2-ultralow. 1,2 Endocrine therapies are widely used in the early lines of treatment for HR-positive metastatic breast cancer; however after two lines of treatment, further efficacy from endocrine therapy is often limited. 3 The current standard of care following endocrine therapy is chemotherapy, which is associated with poor response rates and outcomes. 3-6
The safety profile of Enhertu was consistent with previous breast cancer clinical trials with no new safety signals identified.
The data will be presented at a forthcoming medical meeting and shared with global regulatory authorities.
DESTINY-Breast06 DESTINY-Breast06 is a global, randomised, open-label, Phase III trial evaluating the efficacy and safety of Enhertu (5.4 mg/kg) versus investigator’s choice of chemotherapy (capecitabine, paclitaxel or nab-paclitaxel) in patients with HR-positive, HER2-low (IHC 1+ or 2+/ISH-) or HER2-ultralow (defined as IHC 0 with membrane staining; IHC >0<1+) advanced or metastatic breast cancer. Patients in the trial had no prior chemotherapy for advanced or metastatic disease and either experienced disease progression within 6 months of starting 1st-line treatment with an endocrine therapy combined with a CDK4/6 inhibitor or received at least two previous lines of endocrine therapies in the metastatic setting.
The primary endpoint is PFS in the HR-positive, HER2-low patient population as measured by blinded independent central review (BICR). Key secondary endpoints include OS in patients with HER2-low expression and PFS by BICR and OS in the overall trial population (HER2-low and HER2-ultralow). Other secondary endpoints include objective response rate, duration of response, time to first subsequent treatment or death, time to second subsequent treatment or death and safety. Analysis of the HER2-ultralow subgroup was not powered to demonstrate statistical significance.
DESTINY-Breast06 enrolled 866 patients (n=713 for HER2-low and n=153 for HER2-ultralow) at multiple sites in Asia, Europe, North America and South America. For more information about the trial, visit ClinicalTrials.gov .
Breast cancer and HER2 expression Breast cancer is the second most common cancer and one of the leading causes of cancer-related deaths worldwide. 7 More than two million breast cancer cases were diagnosed in 2022 with more than 665,000 deaths globally. 7 While survival rates are high for those diagnosed with early breast cancer, only approximately 30% of patients who are diagnosed with or progress to metastatic disease are expected to live five years after their diagnosis. 8
HR-positive, HER2-negative is the most common breast cancer subtype, accounting for approximately 70% of all breast cancers. 8 HER2 is a tyrosine kinase receptor growth-promoting protein expressed on the surface of many types of tumours, including breast cancer. 9 Patients with high levels of HER2 expression (IHC 3+ or 2+/ISH+) are classified as HER2-positive and treated with HER2-targeted therapies, representing approximately 15-20% of all breast cancers. 10 Historically, tumours that were not classified as HER2-positive were classified as HER2-negative; however, many of these tumours still carry some level of HER2 expression. 11 It is estimated that approximately 60-65% of HR-positive, HER2-negative breast cancers are HER2-low and potentially an additional 25% may be HER2-ultralow. 1,2
Prior to the approval of Enhertu in HER2-low metastatic breast cancer post chemotherapy based on the DESTINY-Breast04 trial, there were no targeted therapies approved specifically for patients with HER2-low expression. 12 There are no targeted therapies specifically approved for patients with HER2-ultralow expression.
Enhertu Enhertu is a HER2-directed ADC. Designed using Daiichi Sankyo’s proprietary DXd ADC technology, Enhertu is the lead ADC in the oncology portfolio of Daiichi Sankyo and the most advanced programme in AstraZeneca’s ADC scientific platform. Enhertu consists of a HER2 monoclonal antibody attached to a number of topoisomerase I inhibitor payloads (an exatecan derivative, DXd) via tetrapeptide-based cleavable linkers.
Enhertu (5.4 mg/kg) is approved in more than 60 countries for the treatment of adult patients with unresectable or metastatic HER2-positive (IHC 3+ or 2+/ISH+) breast cancer who have received a (or one or more) prior anti-HER2-based regimen, either in the metastatic setting or in the neoadjuvant or adjuvant setting, and have developed disease recurrence during or within six months of completing therapy based on the results from the DESTINY-Breast03 trial.
Enhertu (5.4 mg/kg) is approved in more than 60 countries for the treatment of adult patients with unresectable or metastatic HER2-low (IHC 1+ or 2+/ISH-) breast cancer who have received a prior systemic therapy in the metastatic setting or developed disease recurrence during or within six months of completing adjuvant chemotherapy based on the results from the DESTINY-Breast04 trial.
Enhertu (5.4 mg/kg) is approved in more than 35 countries for the treatment of adult patients with unresectable or metastatic NSCLC whose tumours have activating HER2 ( ERBB2 ) mutations, as detected by a locally or regionally approved test, and who have received a prior systemic therapy based on the results from the DESTINY-Lung02 trial. Continued approval in the US for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial.
Enhertu (6.4 mg/kg) is approved in more than 40 countries for the treatment of adult patients with locally advanced or metastatic HER2-positive (IHC 3+ or 2+/ISH+) gastric or gastroesophageal junction (GEJ) adenocarcinoma who have received a prior trastuzumab-based regimen based on the results from the DESTINY-Gastric01 and/or DESTINY-Gastric02 trials.
Enhertu (5.4 mg/kg) is approved in the US for the treatment of adult patients with unresectable or metastatic HER2-positive (IHC 3+) solid tumours who have received prior systemic treatment and who have no satisfactory alternative treatment options based on results from the DESTINY-PanTumor02 , DESTINY-Lung01 and DESTINY-CRC02 trials.
Enhertu development programme A comprehensive global clinical development programme is underway evaluating the efficacy and safety of Enhertu monotherapy across multiple HER2-targetable cancers. Trials in combination with other anti-cancer treatments, such as immunotherapy, also are underway.
Daiichi Sankyo collaboration AstraZeneca and Daiichi Sankyo entered into a global collaboration to jointly develop and commercialise Enhertu in March 2019 and datopotamab deruxtecan in July 2020 , except in Japan where Daiichi Sankyo maintains exclusive rights for each ADC. Daiichi Sankyo is responsible for the manufacturing and supply of Enhertu and datopotamab deruxtecan.
AstraZeneca in breast cancer Driven by a growing understanding of breast cancer biology, AstraZeneca is starting to challenge, and redefine, the current clinical paradigm for how breast cancer is classified and treated to deliver even more effective treatments to patients in need – with the bold ambition to one day eliminate breast cancer as a cause of death.
AstraZeneca has a comprehensive portfolio of approved and promising compounds in development that leverage different mechanisms of action to address the biologically diverse breast cancer tumour environment.
With Enhertu (trastuzumab deruxtecan), a HER2-directed antibody drug conjugate (ADC), AstraZeneca and Daiichi Sankyo are aiming to improve outcomes in previously treated HER2-positive and HER2-low metastatic breast cancer and are exploring its potential in earlier lines of treatment and in new breast cancer settings.
In HR-positive breast cancer, AstraZeneca continues to improve outcomes with foundational medicines Faslodex and Zoladex (goserelin) and aims to reshape the HR-positive space with first-in-class AKT inhibitor, Truqap , and next-generation SERD and potential new medicine camizestrant. AstraZeneca is also collaborating with Daiichi Sankyo to explore the potential of TROP2-directed ADC, datopotamab deruxtecan, in this setting.
PARP inhibitor Lynparza (olaparib) is a targeted treatment option that has been studied in early and metastatic breast cancer patients with an inherited BRCA mutation. AstraZeneca with MSD (Merck & Co., Inc. in the US and Canada) continue to research Lynparza in these settings and to explore its potential in earlier disease.
To bring much-needed treatment options to patients with triple-negative breast cancer, an aggressive form of breast cancer, AstraZeneca is evaluating the potential of datopotamab deruxtecan alone and in combination with immunotherapy Imfinzi (durvalumab), Truqap in combination with chemotherapy, and Imfinzi in combination with other oncology medicines, including Lynparza and Enhertu .
AstraZeneca in oncology AstraZeneca is leading a revolution in oncology with the ambition to provide cures for cancer in every form, following the science to understand cancer and all its complexities to discover, develop and deliver life-changing medicines to patients.
The Company's focus is on some of the most challenging cancers. It is through persistent innovation that AstraZeneca has built one of the most diverse portfolios and pipelines in the industry, with the potential to catalyse changes in the practice of medicine and transform the patient experience.
AstraZeneca has the vision to redefine cancer care and, one day, eliminate cancer as a cause of death.
AstraZeneca AstraZeneca (LSE/STO/Nasdaq: AZN) is a global, science-led biopharmaceutical company that focuses on the discovery, development, and commercialisation of prescription medicines in Oncology, Rare Diseases, and BioPharmaceuticals, including Cardiovascular, Renal & Metabolism, and Respiratory & Immunology. Based in Cambridge, UK, AstraZeneca operates in over 100 countries and its innovative medicines are used by millions of patients worldwide. Please visit astrazeneca.com and follow the Company on social media @AstraZeneca .
For details on how to contact the Investor Relations Team, please click here . For Media contacts, click here .
1. Denkert C, et al. Clinical and molecular characteristics of HER2-low-positive breast cancer: pooled analysis of individual patient data from four prospective, neoadjuvant clinical trials. Lancet Oncol. 2021 Aug;22(8):1151-1161.
2. Chen Z, et al. Is HER2 ultra‑low breast cancer different from HER2 null or HER2 low breast cancer? A study of 1363 patients. Breast Cancer Res Treat . 2023 Nov;202(2):313-323.
3. Manohar P, et al. Updates in endocrine therapy for metastatic breast cancer. Cancer Biol Med . 2022 Feb 15; 19(2):202–212.
4. Cortes J, et al. Eribulin monotherapy versus treatment of physician’s choice in patients with metastatic breast cancer (EMBRACE): a phase 3 open-label randomised study. Lancet. 2011;377:914-923.
5. Yuan P, et al. Eribulin mesilate versus vinorelbine in women with locally recurrent or metastatic breast cancer: A randomised clinical trial. Eur J Cancer . 2019;112:57–65.
6. Jerusalem G, et al. Everolimus Plus Exemestane vs Everolimus or Capecitabine Monotherapy for Estrogen Receptor–Positive, HER2-Negative Advanced Breast Cancer. JAMA Oncol . 2018;4(10):1367–1374.
7. Bray F, et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin . 2024 Apr 4. doi: 10.3322/caac.21834.
8. National Cancer Institute. Surveillance, Epidemiology and End Results Program. Available at: https://seer.cancer.gov/statfacts/html/breast-subtypes.html . Accessed April 2024
9. Iqbal N, et al. Human Epidermal Growth Factor Receptor 2 (HER2) in Cancers: Overexpression and Therapeutic Implications. Mol Biol Int . 2014;852748.
10. Ahn S, et al. HER2 status in breast cancer: changes in guidelines and complicating factors for interpretation. J Pathol Transl Med. 2020;54(1):34-44.
11. Sajjadi E, et al. Improving HER2 testing reproducibility in HER2-low breast cancer. Cancer Drug Resist. 2022;5(4):882-888.
12. Modi S, et al. Trastuzumab Deruxtecan in Previously Treated HER2-Low Advanced Breast Cancer. N Engl J Med. 2022;387:9-20.
Adrian Kemp Company Secretary AstraZeneca PLC
- Corporate and financial
You are now leaving AstraZeneca.com
You have selected a link that will take you to a site maintained by a third party who is solely responsible for its contents.
AstraZeneca provides this link as a service to website visitors. AstraZeneca is not responsible for the privacy policy of any third party websites. We encourage you to read the privacy policy of every website you visit.
Click ‘cancel’ to return to AstraZeneca’s site or ‘continue’ to proceed.
Important notice for users You are about to access AstraZeneca historic archive material. Any reference in these archives to AstraZeneca products or their uses may not reflect current medical knowledge and should not be used as a source of information on the present product label, efficacy data or safety data. Please refer to your approved national product label (SmPC) for current product information. I have read this warning and will not be using any of the contained product information for clinical purposes.

- Expository Essay
- Persuasive Essay
- Reflective Essay
- Argumentative Essay
- Admission Application/Essays
- Term Papers
- Essay Writing Service
- Research Proposal
- Research Papers
- Assignments
- Dissertation/Thesis proposal
- Research Paper Writer Service
- Pay For Essay Writer Help
Eloise Braun
Customer Reviews
Finished Papers
is a “rare breed” among custom essay writing services today
All the papers delivers are completely original as we check every single work for plagiarism via advanced plagiarism detection software. As a double check of the paper originality, you are free to order a full plagiarism PDF report while placing the order or afterwards by contacting our Customer Support Team.
Being tempted by low prices and promises of quick paper delivery, you may choose another paper writing service. The truth is that more often than not their words are hollow. While the main purpose of such doubtful companies is to cash in on credulity of their clients, the prime objective of is clients’ satisfaction. We do fulfill our guarantees, and if a customer believes that initial requirements were not met or there is plagiarism found and proved in paper, they can request revision or refund. However, a refund request is acceptable only within 14 days of the initial deadline.
Our paper writing service is the best choice for those who cannot handle writing assignments themselves for some reason. At , you can order custom written essays, book reviews, film reports, research papers, term papers, business plans, PHD dissertations and so forth. No matter what academic level or timeframe requested is – we will produce an excellent work for you!
Customers usually want to be informed about how the writer is progressing with their paper and we fully understand that – he who pays the piper calls the tune. Therefore, with you have a possibility to get in touch with your writer any time you have some concerns or want to give additional instructions. Our customer support staff is there for you 24/7 to answer all your questions and deal with any problems if necessary.
Of course, the best proof of the premium quality of our services is clients’ testimonials. Just take a few minutes to look through the customer feedback and you will see that what we offer is not taking a gamble.
is a company you can trust. Share the burden of academic writing with us. Your future will be in safe hands! Buy essays, buy term papers or buy research papers and economize your time, your energy and, of course, your money!
PenMyPaper: a student-friendly essay writing website
We, at PenMyPaper, are resolute in delivering you professional assistance to write any kind of academic work. Be it marketing, business, or healthcare sector, we can prepare every kind of draft efficiently, meeting all the points of the question brief. Also, we believe in 'research before drafting'. Any work without ample research and evidence will be a flawed one and thus we aim to make your drafts flawless with exclusive data and statistics. With us, you can simply relax while we do the hard work for you.

- Dissertations
- Business Plans
- PowerPoint Presentations
- Editing and Proofreading
- Annotated Bibliography
- Book Review/Movie Review
- Reflective Paper
- Company/Industry Analysis
- Article Analysis
- Custom Writing Service
- Assignment Help
- Write My Essay
- Paper Writing Help
- Write Papers For Me
- College Paper Writing Service
Emery Evans
Bennie Hawra
Customer Reviews
Eloise Braun
Customer Reviews

Standard essay helper

IMAGES
VIDEO
COMMENTS
Case study breast cancer. Jan 28, 2013 • Download as PPTX, PDF •. 75 likes • 94,154 views. Nilesh Kucha. prepared by Dr.kucha. Slideshow view. Download now. Case study breast cancer - Download as a PDF or view online for free.
Breast cancer Case Study. Dec 13, 2017 • Download as PPTX, PDF •. 9 likes • 4,054 views. Estudiante de Enfermería - Universidad de La Sabana. Case Study about de medical Center "Touching Lives". US. Education. 1 of 19.
Feb 20, 2014 • Download as PPTX, PDF •. 1,052 likes • 374,785 views. Asheer Khan. What is breast cancer types of breast cancer risk factors associated with breast cancer prevention signs and symptoms diagnosis treatment. Read more. Education. 1 of 140. Download now. Breast Cancer - Download as a PDF or view online for free.
A widely accepted evidence-based treatment approach used in patients with early HER2-positive breast cancer is surgery, followed by adjuvant therapy, for patients with clinical stage T1N0 disease ...
breast cancer case study. frazer bell student bms bsc applied biomedical science. patient history. 70 year old female presented at gp surgery 02/oct/2012 examination: right nipple drawing in & firm palpable lump referred to the breast clinic. breast clinic. attended 18/oct/2012. share presentation. embed code.
What is breast cancer? ' Breast cancer is a collection of cells in the breast tissue that grow in an uncontrolled manner. There are different types of breast cancer and different treatments. Women can have breast cancer without noticing any symptoms or changes. The main risk factors for breast cancer are: being a woman being over 50 Slide 5
Patient Case Presentation. Patient Mrs. B.C. is a 56 year old female who is presenting to her WHNP for her annual exam. She had to cancel her appointment two months ago and didn't reschedule until now. Her last pap smear and mammogram were normal. Today, while performing her breast exam, her nurse practitioner notices dimpling in the left ...
This slide show explains what breast cancer is and how it develops. You can learn about the signs and symptoms to watch for, and the factors that can increase the risk for getting breast cancer. Breast cancer screening, diagnosis, and types of breast cancer are also explained. You can also learn about the different ways that breast cancer is treated - including surgery, radiation ...
Fibroadenoma (37%) and fibroadenosis (23%) were the commonest diseases,both presenting mostly at 21-30years of age. Left side involvement was most common. The commonest presentation was breast lump which comprised 84 (84%) cases, out of which 26 (26%) had associated complaints like breast pain and nipple discharge.
Carol Edwards, a 39 year-old premenopausal woman, had a screening mammogram which revealed an abnormality in the right breast. She had no palpable masses on breast exam. A mammographically localized surgical biopsy was done and revealed a small (0.9 cm) grade III infiltrating ductal carcinoma with some associated ductal carcinoma-in-situ (DCIS ...
Background. Worldwide, male breast cancer is extremely rare, accounting for <1% of all breast tumors and <1% of all malignancies in men [1-3].Recently, the incidence of male breast cancer has increased from 1.0 per 100,000 men in the late 1970s to 1.2 per 100,000 men from 2000 to 2004 [4-7].The American Cancer Society reported a similar trend in the incidence of breast cancer in men from ...
Ironically recent studies show breast physical examination and breast self-examination to be unhelpful in reducing stage at diagnosis17 which we used to advocate to our patients initially. It is also seen that effective therapy may help lower breast cancer death rates after detection18,19 but still mortality remains high. Neoadjuvant ...
In this occasion, we at Slidesgo have decided to create this new presentation template, focused on breast cancer, so that you can raise awareness about this important topic and help everyone get to know what they can do. The visuals of the slides are attractive so that all the attendees feel relaxed and at ease while you give your presentation.
For women in whom gene testing finds "harmful changes" in the BRCA1 or BRCA2 genes, leading medical groups recommend that they take specific actions to lower their chances of being diagnosed with or dying from breast and ovarian cancer.. Results from two recent large studies now add to findings from earlier studies suggesting that following those recommendations can reduce the risk of ...
Developing countries have a significantly higher incidence of breast cancer in patients younger than 40 years as compared to developed countries. This study aimed to examine if young age at diagnosis is an independent prognostic factor for worse survival outcomes in breast cancer as well as the effect of age on Disease-free survival (DFS) and local recurrence free survival (LRFS) after ...
Preclinical evidence suggests improved breast cancer survival associated with statin use, but findings from observational studies are conflicting and remain inconclusive. The objective of this study was to assess the association between statin use after cancer diagnosis and cancer outcomes among breast cancer patients. Methods
Breast cancer and HER2 expression Breast cancer is the second most common cancer and one of the leading causes of cancer-related deaths worldwide. 7 More than two million breast cancer cases were diagnosed in 2022 with more than 665,000 deaths globally. 7 While survival rates are high for those diagnosed with early breast cancer, ...
The racial differences are especially stark with certain types of cancer, research shows.For example, Black and White women are equally likely to be diagnosed with breast cancer, but Black women ...
Case Study On Breast Cancer Slideshare | Top Writers. #5 in Global Rating. Level: College, University, High School, Master's, PHD, Undergraduate. 100% Success rate. Please note. Progressive delivery is highly recommended for your order. This additional service allows tracking the writing process of big orders as the paper will be sent to you ...
The writers of PenMyPaper establish the importance of reflective writing by explaining its pros and cons precisely to the readers. They tend to 'do my essay' by adding value to both you (enhancing your knowledge) and your paper. View Sample. 580. Finished Papers. Case Study On Breast Cancer Slideshare -.
Case Study On Breast Cancer Slideshare. 7 Customer reviews. I work with the same writer every time. He knows my preferences and always delivers as promised. It's like having a 24/7 tutor who is willing to help you no matter what. My grades improved thanks to him. That's the story. 4.8/5.
Case Study On Breast Cancer Slideshare - A standard essay helper is an expert we assign at no extra cost when your order is placed. Within minutes, after payment has been made, this type of writer takes on the job. A standard writer is the best option when you're on a budget but the deadline isn't burning. Within a couple of days, a new ...
Case Study On Breast Cancer Slideshare. Receive a Paper. ID 2644. REVIEWS HIRE. 4.7/5. User ID: 833607 / Mar 30, 2022.