School of Veterinary Medicine
- Graduate Program

Graduate Program Overview

The School of Veterinary Medicine offers a PhD graduate program in One Health Sciences to align with the current demand for interdisciplinary/interprofessional approach to improve public health. The program is designed to train scientists with a broader vision of One Health, interfacing animal, human, and ecological health from local and global perspectives and everything in between.
The program incorporates the One Health competency into the curriculum and evaluation. Students will demonstrate proficiencies in communication, collaboration, teamwork, leadership, systems thinking, and management while successfully addressing the current and emerging One Health challenges.
Interested students are encouraged to contact faculty at the School of Veterinary Medicine to explore potential research projects in one of the school's five areas of research excellence: One Health ; Disease Ecology, Prevention and Management ; Andragogical Scholarship ; Sustainability of Animal Agriculture ; and Molecular Mechanisms of Diseases .
Application requirements include but are not limited to:
- Education history
- Two letters of recommendation
- Personal statement
- Curriculum Vitae
- Proof of English Proficiency
Fall 2024 priority application deadline is November 30, 2023 .
The international student application deadline is March 15, 2024 .
The domestic student application deadline is May 15, 2024 .
The PhD program will be full-time, face-to-face at the School of Veterinary Medicine in Amarillo, Texas. Graduate students must complete 72 credit hours, of which 18 will be core courses and 12 will be dissertation hours. Of the remaining 42 credit hours, students will select from electives to build expertise.
Please read the PhD in One Health Sciences Texas Tech University School of Veterinary Medicine Graduate Student Handbook , to understand the program's policies and procedures.
How to Apply
- Like School of Veterinary Medicine on Facebook Like School of Veterinary Medicine on Facebook
- Follow School of Veterinary Medicine on X (twitter) Follow School of Veterinary Medicine on X (twitter)
- Subscribe to School of Veterinary Medicine on YouTube Subscribe to School of Veterinary Medicine on YouTube
- Follow School of Veterinary Medicine on Instagram Follow School of Veterinary Medicine on Instagram
You are using an outdated browser! Upgrade your browser today or install Google Chrome Frame to better experience this site.
Search form

Click "Menu" to toggle open, click "Menu" again to close
- What Is Public Health?
- Why Accreditation Matters
- Academic Departments
- Administrative Units
- Office of Information Technology
- Financial Affairs and Physical Resources
- Community, Environment & Policy
- Epidemiology and Biostatistics
- Health Promotion Sciences
- Primary Faculty
- Adjunct Faculty
- Strategic Initiatives
- Centers and Institutes
- Diversity and Inclusion
- Dean's Message
- Dean's Strategic Initiatives Fund
- Dean's Students Research Funds
- Standing Committees
- Need a Public Health Intern?
- Declaring the Public Health Major
- How to Apply for Advanced Standing
- Wellness and Health Promotion Practice (BA)
- Public Health Major (BS)
- Online Bachelors (BS)
- Addiction and Substance Use
- Aging and Population Health Minor
- Climate Change and Public Health
- Environmental and Occupational Health Minor
- Global Health Minor
- One Health Minor
- Population Health Data Science Minor
- Public Health Minor
- Wellness and Health Promotion Practice Minor
- Transfer Students
- Global Health
- Public Health Emergency and Epidemic Preparedness
- Safety Certificate
- Online Degree Curriculum
- Curriculum Information for Public Health Coursework
- Internships
- Study Abroad
- Course Schedule
- BS & MPH Environmental & Occupational Health Program
- BS & MPH in Global Health Program
- Academic Policies and Forms
- Student Services Staff
- Student Clubs and Organizations
- Public Health Ambassadors
- Meet Our Students
- Scholarships and Aid
- Academic Achievement
- Dual Degrees
- MS & PhD Programs
- Certificate Programs
- Non-Degree Seeking
- Distance Learning
- Ajman UAE Micro-Campus
- Study Abroad Programs
- Biostatistics
- Environmental Health Sciences
- Epidemiology
- Family and Child Health
- Health Behavior Health Promotion
- Health Services Administration (Phoenix & Tucson)
- Public Health Policy and Management
- Public Health Practice (Phoenix)
- Prospective Students
- Admissions Criteria & Deadlines
- How to Apply
- Admissions Information Events
- Visiting Campus
- International Students
- Tuition & Financial Assistance
- Certificate Program Admissions Criteria
- Online Team Staff
- Admitted Students
- Research Areas
- Research Projects
- Research Resources
- Research Policies
- Deans Annual Fund Application
- Student Research
- Health Services Administration
- Phoenix Campus
- Public Health Policy & Management
- Public Health Practice
- Center for Firefighter Health Collaborative Research
- Center for Health Disparities Research
- Nosotros Program
One Health Initiative
- Tucson and Pima County
- Arizona and Regional
- National and Multi-State
- International
- Community Engagement and Outreach
- IndigiWellbeing Program
- Phoenix Mobile Health Unit
- Tucson Mobile Health Unit
- Mobile Outreach Vaccination & Education (MOVE-UP)
- Ventanillas de Salud (Windows to Health)
- Rural Health Professions Program
- Street Medicine Phoenix
- Students Reach Out
- Workforce Development
- 20th Anniversary Stories
- Remembering Mel Zuckerman
- Mental Health
- Climate Change and Health
- Indigenous Health
- Digital Epidemiology
- Additional Giving Opportunities
- Ways to Give
- Scholarships
- Community Advisory Board
- Alumni Giving Circle
- Dean's Circle of Excellence
- Dalen Lecture Series
- Mel & Enid Zuckerman
- James & Priscilla Dalen
- Frank Marcus
- Barry & Janet Lang
- Kent & Liz Campbell
- Meet the Giving Team
- Dean's Annual Fund Application
- Alumni Council
- Host an Event
- Alumni Network
- Alumni Events
- Our Alumni Change the World
- Delta Omega

The more we learn, the more we understand that human health is deeply intertwined with the health of animals and the environment. The emerging field of study called One Health looks at human health in the context of these deep connections between people and the natural world, so we can find and deliver solutions that keep communities healthy.
A Global Health Challenge

To meet the health challenges of a rapidly changing world, new strategies are needed, and the One Health approach sees the complex connections between human health, animal health, and environmental health. At the Zuckerman College of Public Health, we offer a range of programs to train the next generation of One Health researchers and public health professionals. We also conduct community-engaged, cross-disciplinary One Health research to meet the global health challenges of a rapidly changing world.
Building on One Health knowledge, we find ways to apply what we learn from research, to implement programs and policies that improve health and wellness for communities that are adversely affected by health threats connected to environmental and animal health.
As ecosystems shift due to human interaction or climate change, those shifts lead to altered patterns of disease transmission. Diseases that spread between animals and people – known as zoonotic infections – are common around the globe. The recent COVID-19 pandemic stands out as the most impactful example, yet it will not be the last. A One Health work force is needed to detect, respond, and prevent infectious diseases, epidemics, and pandemics in the U.S. and around the world.
One Health Education
In the Zuckerman College of Public Health, we know how important it is to train the One Health workforce of the future. The college offers a range of degree programs with a One Health focus.
Undergraduate One Health Programs
Bs, one health track.

If you want to meet the public health challenges of the future where human, animal, and environmental health intersect, this is your path to improving global health!
Available Online and In Person
Undergraduate Minor in One Health

For students from many areas of focus, the One Health knowledge provided by this Minor provides a powerful framework to find solutions where human health, animal health, and environmental health intersect.
Available In Person
One Health Undergraduate Certificate

For the current and future public health workforce professional, this program provides knowledge and skills related to the complex interaction between human health, animal health and the environment.
Available Online
Graduate One Health Programs
Mph in one health.

For students who are ready to tackle global health challenges, this interdisciplinary concentration trains students to deploy a One Health approach to address complex public health issues.
Graduate Certificate in One Health

A distance learning program designed to meet the needs of students and professionals, the coursework provides multidisciplinary perspective and expertise in the One Health approach to find solutions for emerging health threats.
One Health Research

At the Zuckerman College of Public health, we have always understood public health within the context of social and environmental factors. Our recent public health focus on One Health affirms and enhances this approach. Our faculty, especially in the field of exposure science, have been conducting research that investigates the impacts of environmental pollution on human health for many years, working with tribes, farmworkers, firefighters, and many others in Arizona and globally.
Building on this experience and success, the college launched its new One Health Research Initiative (OHRI) in 2020 and recruited Frank von Hippel, PhD , to the Department of Community, Environment and Policy, to lead the OHRI. Frank brings a wealth of experience in One Health research, and leads research projects in the United States and globally. To engage impacted communities with the research and the outcomes, Frank employs a Community Based Participatory Research (CBPR) approach that brings community members into the process from start to finish.
New ‘One Health’ Funding for UArizona Students and Faculty
New funding opportunities for students and faculty across the university will promote One Health research.
For more than a decade, faculty in the college have been working on cross-disciplinary and community-engaged One Health research projects, both in the United States and around the globe. The OHRI now facilitates and supports many of these research projects. All our faculty involve students in their research projects so that students gain the knowledge and experience they need to lead future One Health research in public health. Our faculty who conduct One Health research include:
Mona Arora, PhD, MsPH Leila Barraza, JD, MPH Paloma Beamer, PHD Heidi Brown, PHD, MPH Stephanie Russo Carroll, DrPH, MPH Katherine Ellingson, PhD Kacey Ernst, PhD, MPH Stephanie Griffin, PhD, CIH Aminata Kilungo, PhD Kristen Pogreba-Brown, PhD, MPH Kelly Reynolds, PhD, MSPH Jonathan Sexton, PhD, MS Marc Verhougstraete, PhD
Guided by Frank’s leadership, the college has worked closely with University of Arizona Health Sciences to expand connections across the university, and engage with researchers across the state to build knowledge and capacity around the One Health approach. To build relationships and facilitate this collaborative process, the college has helped to host One Health Symposiums where researchers present and connect.

Frank von Hippel, PhD
Coming soon One Health Symposium, Spring 2023
Previous Events One Health Symposium, Fall 2022 One Health Symposium, Spring 2022

Tucson - Main Campus | 1295 N. Martin Ave. | Drachman Hall | P.O. Box 245163 | Tucson, Arizona 85724 | Fax Number: 520-626-8009 Phoenix Campus | 550 E. Van Buren Street | UA Phoenix Plaza Building 1 | Phoenix, AZ 85006 The University of Arizona | Tucson, Arizona USA 85721-0036 | Copyright 2024 © Arizona Board of Regents University Privacy Statement

- Regular Faculty
- Affiliate Faculty
- Emeritus Faculty
- Clinical Faculty
- Adjunct Faculty
- Our Mission, Vision & Values
- Serving Washington State
- Advisory Committee
- DEOHS faculty positions and fellowships
- Degree requirements
- Applying to the major
Career pathways
- Funded Research for UW Undergraduates
- Environmental Public Health Minor
- How to Apply
- Graduate degree finder
- Environmental Public Health
- Environmental Toxicology
- Individualized Track
- Infectious Diseases
- Occupational Hygiene/ Exposure Science
- Master of Science
- Master of Science: Applied
- Master of Public Health
- MPH, Occupational and Environmental Medicine
- PhD in Environmental Health Sciences
- Graduate Certificates and Concurrent Degrees
- Course Information
- Biostatistics, Epidemiologic, and Bioinformatic Training in Environmental Health
- Environmental Pathology/Toxicology Training Program
- Northwest Center for Occupational Health and Safety
- Supporting Undergraduate Research Experiences in Environmental Health (SURE-EH)
- Internship 101
- Launch your career
- Job Openings In the Field
- Student and Alumni profiles
- Contact an Adviser
- Clean Water
- Safe Workplaces
- Sustainable Communities
- Funded Projects
- Student Research
- Continuing Education
- Field Research and Consultation Group
- Environmental Health Laboratory
- Occupational & Environmental Medicine
- Pediatric Environmental Health Specialty Unit
- Teratogen Information System (TERIS)
- Alumni profiles
- Job Openings in the Field
- DEOHS Newsroom
- Environmental Health Seminar
Here you can:
Discover the links between the health of people, animals and the environments we share.
Harness your passion for improving public health. At DEOHS, you can:

Why study One Health?
One Health is a transdisciplinary approach to health issues affecting humans, animals and the rapidly changing environments we share. One Health specialists look at a range of issues—from emerging zoonotic diseases and antimicrobial resistance to climate change and food production—through the lens of creating a healthy coexistence between humans and animals in sustainable ecosystems.
Our UW Center for One Health Research , part of DEOHS, offers traineeships for the Occupational Health at the Human-Animal Interface training program, funded by the National Institute for Occupational Safety and Health.
As a student in One Health, you will:
- Choose to earn your MS, MS-Applied or PhD degree.
- Take common core courses introducing foundational concepts and skills, including: risk assessment, management and communication; assessment and management of exposures to environmental hazards; core principles of toxicology; and how to use a One Health approach to address complex challenges.
- Learn about the linkages among human, animal and environmental health; how climate change is impacting those connections; and the unique occupational health risks faced by workers who come in contact with animals. You will also choose additional courses on topics that align with your interests, such as antibiotic-resistant bacteria and genes, the microbiome and recognition and control of health and safety hazards in industrial settings.
- Complete a culminating experience (thesis or dissertation) showcasing your ability to integrate the skills you have learned to address an environmental or occupational health problem.
_0.png)
When I was researching graduate schools, the One Health program at UW stood out to me. I’ve been impressed with the support I receive from my mentors and the availability of research funding.
Madeline Benoit, MPH, One Health Read more
One Health: Student research projects
Erica Grant
Protecting gorillas by protecting people: A "One Health" approach to conservation and community health
MPH | One Health (ONE) 2018 | Peter Rabinowitz
Jose Carmona
The healthy dairy worker study: A longitudinal cohort study of dairy workers’ respiratory health
MPH | Environmental and Occupational Health (EOH) 2019 | Peter Rabinowitz
Teresa Schlanser
Compassion fatigue in lab animal medicine
MPH | One Health (ONE) 2020 | Peter Rabinowitz
Our faculty and research
_0.png)
Our study looking into whether pets can get COVID-19 aims to help people with good preventive practices to avoid transmission between people and animals.
Dr. Peter Rabinowitz, DEOHS Professor and Director, UW Center for One Health Research Read more
Research spotlight

Stopping animal-to-human disease transmission
DEOHS Professor Elaine Faustman will lead risk analysis and communication for new $100 million USAID initiative

Antibiotic resistance in orcas
Killer whales can carry antibiotic-resistant strains of E. coli , according to new UW research. Is that contributing to the decline of this endangered species?

Caring for the animal caretakers
New clinic led by DEOHS, UW Medicine focuses on animal worker health and safety
Our One Health graduates pursue careers in environmental health practice, agricultural safety, health care settings, wildlife health, climate change, academic research or consulting. Recent DEOHS graduates work as:
- Field Researcher with the Carl R. Woese Institute for Genomic Biology .
- Director, Producer and Public Health at National Pork Board .
- Research Analyst at the University of Washington .

Alumni profile
The One Health focus in DEOHS allowed me to customize my experience by focusing on animal and human health in the context of disaster preparedness.
Brianna Willis, Senior Research Specialist in the Safety and Security division of CNA , a nonprofit research and analysis organization. Read more
Online advising available
Connect with an adviser now via Zoom or phone.
Make an appointment
Explore our degrees
Master of Science in Environmental Health Sciences: Applied Complete in 15 months 52 credits and project Learn more
Master of Science in Environmental Health Sciences Complete in 2 years 62 credits and thesis Learn more
Master of Public Health in Environmental Health Sciences Complete in 2 years 65 credits and thesis or project Learn more
Doctor of Philosophy in Environmental Health Sciences Complete in 5 years 90 credits and dissertation Learn more

Texas Tech University Debuts a Very Novel PhD Program in One Health Sciences

First cohort of 25 PhD One Health Sciences at TTU-SVM (Photo Credit: Weston Brooks)
By: Brianna Kreditor, MPH
The second publicly funded Veterinary School in Texas offers a novel PhD in One Health Sciences. The School of Veterinary Medicine at Texas Tech University (TTU) was envisioned in 1971 but not realized until 2014. The school is driven by a simple purpose: “to serve veterinary educational and service needs of rural and regional communities of Texas and to provide access to affordable high-quality education”. (1,2) In addition, the school’s mission “strives to meet the current and future needs of Texas and its citizens.”
The PhD in One Health Sciences focuses on five goals of the competency-based program, and “...recognizes that current public health challenges require an inclusive version of – and interdisciplinary/interprofessional approach to – global health”. (1,2) Overall, graduates with a PhD in One Health Sciences will have a broader vision of One Health, with the goal of identifying the connection between animal, human, and ecosystem health. This is made possible through the school’s five interdisciplinary emphases that include one health; disease ecology, prevention, and management; andragogical scholarship; sustainability of animal agriculture; and molecular mechanisms of disease. (1,3)
The School of Veterinary Medicine at Texas Tech University (TTU-SVM) welcomed its inaugural class of veterinary students in Fall 2021 and debuted a PhD in One Health Sciences the following year, with the first cohort of 25 PhD One Health Sciences. (1) The One Health Sciences PhD program focuses training in the five disciplines and a competency-based approach with the goal of students demonstrating proficiency within competencies to address current and emerging One Health challenges. Now, 38 PhD students are enrolled in this ambitious program.
TTU has the unique opportunity to foster One Health training as a deep learning experience for their students, where research or electives are customized to students during the 72-credit-hour program. The program aims to enhance professional development, skills, and competencies within One Health. In addition, training experiences, such as TTU’s disaster day, offer scenarios which can be targeted using a One Health approach. Disaster day is a collaboration among the Schools of Vet Med, Pharmacy, Nursing, and the College of Medicine.
The first cohort of veterinary students will undertake a clinical rotation year in 2024, where they will obtain experiences using a hybrid, community-based approach, offering rotations both on campus and off campus with their community partners. TTU has 65 clinical partners in the state and some in New Mexico for Vet students, allowing students to rotate at a clinical site based on their interests

According to Dean Loneragan , the school has grown in just three years to be home for almost 300 students, staff, and faculty, and anticipates 400 DVM students, 75 graduate students, and 125 full-time equivalent staff and faculty. (4) As the PhD program continues to grow, TTU plans to hire faculty solely dedicated to the PhD program. Growth opportunities continue for faculty and the school, with 38 current graduate students and an incoming class of 8 graduate students in the fall
John Gibbons, MS, PhD , Program Director for One Health, noted there are opportunities to expand the program, such as the inclusion of a master program in addition to supporting a Texas Tech one health initiative that is in the planning phase.
Dean Loneragan’s area of expertise is in epidemiology and public health. His research interests include antimicrobial uses and resistance in bacteria of livestock populations, and providing more insights into the ecology of zoonotic bacteria in animals; his research profile can be found here .
John Gibbon’s area of research is focused on multifaceted approaches to address basic fertilization and early embryonic development and developing and modifying reproductive techniques.
Nguyen, T. A., Dascanio, J. J., & Loneragan, G. H. (2022). Research, discovery, and innovation: a novel PhD in One Health Sciences, American Journal of Veterinary Research, 83(11), ajvr.22.09.0163. https://doi.org/10.2460/ajvr.22.09.0163
Togami E, Gardy JL, Hansen GR, et al. Core competencies in One Health education: what are we missing? National Academy of Medicine. 2018. Accessed June 4, 2018. https://doi.org/10.31478/201806a
Brooks, Weston. (2022). Texas Tech’s Innovative Doctorate in One Health Sciences Get Final Approval. Texas Tech Today. https://today.ttu.edu/posts/2022/12/Stories/Texas-Tech-Innovative-Doctorate-in-One-Health-Sciences-Gets-Final-Approval
Inaugural cohort of students enrolled in our PhD in One Health Sciences. American Journal of Veterinary Research 83, 11; 10.2460/ajvr.22.09.0163
Loneragan, G. H., Dascanio, J. J., & Conklin, B. L. (2022). Texas Tech University School of Veterinary Medicine Driven by a Simple Purpose, Journal of the American Veterinary Medical Association, 260(14), 1777-1777. https://doi.org/10.2460/javma.22.09.0411
Roadmap to diversity: integrating holistic review principles into medical school admission processes. Association of American Medical Colleges. 2010. Accessed Aug 2022. https://www.aamc.org/services/member-capacity-building/holistic-review
Competency-based veterinary education. American Association of Veterinary Medical Colleges. 2018. Accessed Aug 2022. https://www.aavmc.org/programs/cbve/
Subscribe to the UTMB One Health Newsletter
- Health Care
- UTMB Support Areas
A cross-divisional department spanning
One Health Research Team
- Baltimore Community Outreach and Engagement Projects
- Northeast Market Patron Survey
- Evaluating the Impacts of Energy Options on Baltimore’s Air Quality
- One Health and Asthma Prevention in Baltimore
- Safer Urban Agriculture in Baltimore
- Diversity and Equity Initiatives
- Environmental Health and Engineering Student Organization (EHESO)
- Message from the Chair
- Postdoctoral Opportunity in Neuroscientist/(Neuro)toxicologist
- Postdoctoral Opportunity in Public Health Policy
- Research Assistant
- Bachelor of Science in Environmental Engineering
- Program Objectives and Outcomes
- Why Hopkins?
- Application Fee Waiver Requirements
- Areas of Focus
- Graduate Student Resources
- Jensen Fellowship
- Postdoctoral Opportunity: Toxicology Policy, Law and Regulatory Analysis
- Quotes from our EHE Alumni
- Non-Degree Programs
- EHE Research Retreat
- Geyh-Bouwer Trainee Practice Award
- Air Pollution and Cardiorespiratory Diseases
- Antimicrobial Resistance and Infectious Disease
- Biosecurity and Emerging Threats
- COVID-19 Research
- Carcinogens and Cancer
- Children's Environmental Health
- Chronic Disease Etiology and Prevention
- Community Sustainability, Resilience, and Preparedness
- Consumer Product Safety
- Energy Management and Alternative Technologies
- Environmental Chemistry, Microbiology and Ecology
- Environmental Engineering
- Environmental Epidemiology
- Environmental Inequities and Injustice
- Environmental Resource Quality
- Epigenetic Regulation in Environmental Diseases
- Food and Agricultural Systems
- Geomorphology, Geochemistry, and Hydrology
- About the Program
- Conceptual Framework
- Land Use and Energy Issues
- MPH Concentration in Global Environmental Sustainability & Health
- Projects and Research
- Recommended Reading
- Research on Land Use and Public Health
- What the Future Must Look Like
- Novel Exposure Assessment
- Risk Sciences and Public Policy
- Social and Behavioral Sciences
- Toxicology, Physiology, & Cell Biology
- Johns Hopkins University Water Institute
- Worker Health and Safety
- Teaching and Research Labs at WSE
- The INnovations to Generate Estimates of children's Soil/dust inTake (INGEST) Study
- Centers and Institutes
- Environmental Health and Engineering Doctoral Students
- Full-time Faculty Directory
- Postdoctoral Fellows
- News and Events
- Make a Gift

Meghan Frost Davis, PhD, DVM, MPH
Associate Professor Director, One Health Laboratory at Johns Hopkins University Department of Environmental Health and Engineering
As a molecular epidemiologist and an environmental microbiologist, Meghan studies the interface of bacteria and hosts to reduce microbe-mediated disease in humans and animals. Her work applies the principles of one health and microbial ecology, evaluating target microbes and bacterial genes specifically and the larger microbial community (microbiome) broadly. She also evaluates non-infection outcomes, specifically asthma, from exposure to bacterial agents and their toxic products. Designing and testing interventions to combat the rise of bacterial antimicrobial resistance and both infection and non-infection outcomes related to microbial exposures in a one health context is the goal of her research career.

Justin Edwards Research Technologist

Amanda McCormack Postdoc | 2022-

Sharmaine Miller, PhD Postdoc | 2020-

Julianna Nechin ScM Student | 2019-

Steven Sola, MSPH PhD student

Eri Togami, DVM, MPH PhD student

Kaitlin Waite, DVM MPH Postdoc | 2019-
Research Team Alumni
- 2016-20 | Alexandra Lorentz, PhD
- 2016-20 | Gabriel Innes, VMD, PhD
- 2016-18 | Christopher Nelson, RN, MPH
- 2017-18 | Maya Spaur, MHS
- 2017-18 | Zoë Johnson, Mississippi State University, MS Student
- 2017-18 | Cusi Ferradas, MPH
- 2017-18 | Raquel Serruya, MHS
- 2016-18 | Isha Pandya, ScM
- 2016-17 | Camille Effler, DVM | U.S. Army
- 2016-17 | Katie Sabella, DVM | Veterinarian
- 2016-17 | Po-Yang Tsou, MPH | Medical Resident
- 2015-16 | Kristopher Spicer
- 2015-16 | Andrea Christ
- 2015-16 | Caitlin Cotter, DVM - MPH Student | 2015-16 | CDC Epidemiology Intelligence Service
- 2014-15 | Jacqueline Ferguson | University of California, Berkeley, PhD Student
- 2014-15 | Daniel Laucks, VMD, MPH | Food and Drug Administration
- 2014-15 | Jonathan Shahbazian, BS, MPH
- 2013-14 | Emily Pieracci, DVM, MPH | CDC Epidemiology Intelligence Service
- 2012-13 | Amy Brazil, VMD, MPH | Food and Drug Administration
- 2011-12 | Sally Ann Iverson, DVM, MPH | CDC Epidemiology Intelligence Service
2017 (Summer )
- Zoë Johnson
2016 (Summer )
- Erin Beasley
- Ayanna Crear | DSIP Program
2015 (Summer )
- Isabel Jiminez-Bush | DSIP Program
- Phillip Hahn | DSIP Program
- Haley Keller
- Krista Reynolds
What's a VMD? Both a DVM and a VMD are veterinary doctoral degrees, the animal health equivalent of a MD.
- Texas Tech Today
Texas Tech's Innovative Doctorate in One Health Sciences Gets Final Approval
Weston Brooks
December 19, 2022

The newly developed doctoral program will enable students to engage, train and collaborate in One Health Sciences scholarship.
The Texas Tech University School of Veterinary Medicine in Amarillo received final approval to offer an innovative doctoral degree in One Health Sciences to help graduate students provide solutions for society's future challenges.
The program was approved by the Texas Higher Education Coordinating Board (THECB) in May 2022. The program then received final approval by the Southern Association of Colleges and Schools Commission on Colleges (SACSCOC) in December 2022.
This innovative program addresses the growing demand for interdisciplinary and interprofessional collaboration across animal, human and ecosystem health known as One Health.

for research. “Exploration of interconnectedness of human, animal and ecosystem health is at the core of the doctoral program in One Health Sciences.”
“When we collaborate across disciplines and professions, profound discoveries are made,” said Guy Loneragan , dean of the School of Veterinary Medicine. “The innovative aspect of this PhD program is that it offers broad foundational understanding of how animal, human and ecosystem health are interconnected, and also deep knowledge within a discipline. This sets our graduate students up with the tools to provide important discoveries – say in a new vaccine technology – that might be able to benefit both animals and people.”
The School of Veterinary Medicine's location is instrumental in the success of this program. It is strategically located both within the heart of Texas' animal agriculture region and adjacent to the Texas Tech University Health Sciences Center at Amarillo .
The program is built on the strength, diversity and expertise of the school's faculty members and will recruit talented scholars from around the world. Students will work alongside these experts to develop subject-matter expertise in one of the five areas of research excellence: One Health Epidemiology; Disease Ecology, Prevention and Management; Andragogical Scholarship; Sustainability of Animal Agriculture; and Molecular Mechanisms of Disease.
“I am impressed with the passion with which our first cohort of students have pursued the application of the One Health approach in working with stakeholders, developing research projects, collaborating with faculty and other students, and communicating their science with the public,” said Ryan Williams , assistant dean and associate professor of economics and public policy. “It is clear that a program with this design was desired in the United States, and that the Texas Tech University School of Veterinary Medicine is a great place for it to have been established.”
Those interested in the program can preview the Graduate Program Overview and are encouraged to apply before the priority deadline of January 15.
tags: Academics , Research , Stories , Veterinary School , Vice President for Research , provost
Texas Tech University

A new era of excellence is dawning at Texas Tech University as it stands on the cusp of being one of the nation's premier research institutions.
Research and enrollment numbers are at record levels, which cement Texas Tech's commitment to attracting and retaining quality students. In fall 2020, the university achieved a goal more than a decade in the making, reaching a total student population of more than 40,000. In 2018, the Carnegie Classification of Institutions of Higher Education again placed Texas Tech among its top doctoral universities in the nation in the “Very High Research Activity” category. Texas Tech is one of 94 public institutions nationally and 131 overall to achieve this prestigious recognition.
Quality students need top-notch faculty. Texas Tech is home to a diverse, highly revered pool of educators who excel in teaching, research and service. The university strives to foster an environment that celebrates student accomplishment above all else. Texas Tech is large enough to provide the best in facilities and academics but prides itself on being able to focus on each student individually. The momentum for excellence at Texas Tech has never been greater.
School of Veterinary Medicine

The School of Veterinary Medicine recruits and selects students with a passion to serve rural and regional communities. Its curriculum is focused on the competencies and skills necessary for success in practice types that support these communities. Texas Tech's innovative and cost-efficient model partners with the wider community of veterinary practices across the state to provide clinical, real-world experiential learning.
- Board Members
- Working at OHT
- Antimicrobial Resistance
- Communicable Disease Dynamics
- Gender, Equity, and Livelihoods
- Health and Development
- Food, Climate, and Health
- Vaccines and Immunization
- OxygenForIndia
- Noncommunicable Diseases
- North America
- Nimai Valley
PhD in Data Sciences for Global Health
- Study Abroad Program
- Internship Program
- Weekly Digest
- Peer Reviewed Articles
- Infographics
- Presentations

OHT Advisors
How to apply.

The PhD program in Data Sciences for Global Health, jointly offered by BITS Pilani and the One Health Trust (OHT), offers training in global health issues and cutting-edge research methodology with rigorous fieldwork and data analysis. This program provides full-time, advanced education in global health plus expertise in qualitative and statistical/quantitative skills leading to an interdisciplinary degree. The BITS Pilani and OHT faculty have vast research experience in infectious disease dynamics, antimicrobial resistance, vaccines and immunization, environmental health, gender equity and livelihoods, health and development, health systems, and economics.
Students will spend part of their tenure in the program at the BITS Pilani Hyderabad campus and the other period housed at the Nimai Valley Center.
Applicant Brochure (2022–2023)
If you have any questions, please contact [email protected] .

Program Curriculum and Requirements
The students must complete six core courses covering three main subjects (24 credits) during the first year. Before the end of their second year, students will defend their thesis proposal and research plan. From their third year onwards, PhD candidates will present their work at seminars, conduct fieldwork, and communicate their research outcomes through research papers that will together form a PhD dissertation. Students must maintain a minimum grade of D and CGPA of 5.50 in all semesters. Each academic year will have two semesters.
First Year (first and second semester)
The first year will involve course work in the following six core courses:
- Global Health Management I and II
- Data Sciences (including Research Methodologies) I and II
- Health Economics and Policy I and II
The coursework will help students build a strong theoretical foundation in global health and equip them with data skills. The first-year activities will take place on the BITS Pilani campus. A qualifying exam will be held at the end of the first year. Students will be promoted to the second year only if they pass at least two of their main subjects. The exam will include a written test and viva on the courses taught. BITS and OHT will jointly conduct the written exam and viva.
Second Year (third and fourth semester)
In the second year, students will draft a detailed research proposal to undertake thesis work and submit to their advisory committee for review. The students should take independent study/classes from faculty members from BITS-Pilani or OHT, in their research areas of interest (directed individual study), as they work on their research proposal and papers. A rotation method can be used to learn from various faculty members. Students are also encouraged to learn grant writing from their notional supervisor(s) and apply for research grants. At the end of each semester, students are expected to submit term papers, based on their research.
Students are strongly encouraged to find a potential advisor(s) during their second year. The main advisor will be from BITS Pilani and their co-advisor can be from OHT. Students will also choose a doctoral advisory committee (DAC) consisting of two members, from among the faculty members of BITS Pilani and OHT.
A candidacy/oral exam will be held at the end of the fourth semester. The exam will include an oral presentation on the research proposal developed in the second year. The proposal will be defended in the presence of a peer group and faculty of the concerned departments. Following the approval of the research proposal, students can then register for thesis units (maximum of 10 units per semester). A minimum of 40 thesis units should be completed to submit the thesis for examination.
Third Year through finishing the PhD program (fifth semester and beyond)
After advancing to Ph.D. candidacy, students are expected to present their progress at least twice each semester to their supervisors and DAC. Additionally, they are expected to submit progress reports to their respective DAC members at least once per semester. Students are also encouraged to present their research in seminars or conferences organized by BITS, OHT, and elsewhere.
- Field Work: Students are required to undertake field visits at OHT’s Nimai Valley Center. They may conduct quantitative or qualitative data collection corresponding to their research interests.
- Dissertation Defense: The student will prepare their thesis in consultation with their team of supervisors and present/defend to their DAC. They will be required to write three research papers, which will form their dissertation, and publish in peer-reviewed journals to graduate.
FIND OUT MORE

- Ramanan Laxminarayan
- Thomas P. Van Boeckel
- Giridara Gopal
- Deepshikha Batheja
- Geetanjali Kapoor
- Erta Kalanxhi
- Arindam Nandi
- Samantha Serrano

- Is there a fee to apply for this program?
The application fee is around INR 2,600. This is subject to revisions, and you can verify fees at https://www.bitsadmission.com/phdmain.aspx
- What is the application deadline?
The application deadline is typically in May-June with the semester starting in late July or early August. Intake for this program is yearly.
- Am I eligible to apply for this program?
We welcome applications from all professional, geographic, cultural, and socioeconomic backgrounds, with no age restriction. Meeting the minimum eligibility criteria does not guarantee admission into the program. For more information, please refer to the BITS PhD admissions prospectus.
Minimum eligibility criteria:
- ME/MTech/MPharm/MBA/MPhil/MSc/BE/BPharm or an equivalent degree: minimum of 60 percent aggregate
- MA: minimum of 55 percent aggregate
- MBBS/BDS/BVSc/MD/MDS/MVSc/BAMS/BHMS/BUMS/allied: minimum of 55 percent aggregate.
- My previous degree is from outside of India. What documents will I need to submit for registration if I am accepted?
International students will be required to provide an appropriate grade conversion to the Indian grading system, which has to meet the eligibility listed above. This will be in addition to the document checklist for the application package detailed in the BITS PhD admissions prospectus.
- Does the application process include an interview?
Shortlisted applicants will be interviewed about their knowledge of global health, data sciences, and research interests. OHT will participate in the interviewing panel. Given the diverse backgrounds of applicants, applicants are expected to be proficient in their previous degree(s) and have an aptitude for the other domains in the program. No written exam will be offered, but grades from previous degrees (transcripts), statements of purpose (SOPs), and letters of recommendation (LORs) will be considered.
- What is the expected time within which I can expect to receive a decision on my application?
You can expect to receive a decision on your application within six to eight weeks of the close of the application window.
- What is the expected length of the program?
All admitted candidates will be required to do the standard coursework in the first two semesters. Students must complete six core courses covering three main subjects (24 credits) during the first year. Before the end of their second year, students will defend their thesis proposal and research plan. From their third year on, PhD candidates will present their work at seminars, conduct fieldwork, and communicate their research outcomes through research papers that will write a PhD dissertation. PhD candidates must submit a thesis within five years to successfully complete the degree. For more information, please refer to the BITS PhD admissions prospectus. Students may take a maximum of seven years to finish their PhD due to unforeseen circumstances, with appropriate approvals from their dissertation committee.
- Is this an on-campus full-time program or a hybrid program?
This PhD is offered only as an on-campus full-time program. Students may be able to take courses online, which are offered at the other BITS campuses, as part of their degree requirements.
- Is it possible to change your supervisor after being assigned one at the time of offer of acceptance?
You will need to file a formal request for a change of supervisor and pending approval from an internal committee at BITS, you can change your assigned supervisor.
- What are the locations of the BITS Pilani campuses that offer courses applicable to this program?
You can find the addresses for each campus below:
BITS Pilani, Hyderabad Campus
Jawaharnagar, Shamirpet Mandal Medchal-Malkajgiri District Hyderabad 500078 Telangana
Google Maps
BITS Pilani, Goa Campus
NH 17B, Bypass, Road Zuarinagar, Sancoale Goa 403726
BITS Pilani, Pilani Campus
Vidya Vihar Pilani Rajasthan 333031
- What is the fee structure for this program?
The following are the details of the fees in INR payable by all students admitted to the PhD Program in the academic year 2023-2024 at BITS- Pilani, Pilani Campus/ Goa Campus/ Hyderabad Campus.
* Payable at the time of admission; # Payable at the time of thesis submission
Financial Assistance:
Full-time PhD students admitted into the PhD program are eligible to be considered for a fellowship of INR 34,000/- or INR 37,000/- per month as per intake qualifications. Consideration for a fellowship will be as per institute norms, details of which are available in the PhD brochure on the admission website. It will be obligatory on the part of every admitted full-time student to undertake eight hours (per week) of work as assigned to her/him by the institute.
- What are the potential sources of financial assistance given to PhD students?
All successfully admitted students will have financial support through one of the following sources:
- Self-funded fellowships such as UGC/CSIR NET JRF , DBT JRF/SRF , ICMR JRF/SRF , DST Inspire
- A BITS Pilani Fellowship, which will include working as a teaching assistant (TA). The stipend/scholarship is in lieu of the TA duties.
- What is the expected stipend?
All admitted students who do not have self-funded fellowships will receive a BITS Pilani Fellowship of INR 34,000/month during the first year, provided for up to five years from the date of admission. It can be enhanced to INR 37,000 per month from the second year on and to INR 40,000/42,000 per month in the third year, based on the student’s performance and output. The fellowship amount is usually aligned with the norms of the Government of India.
- If I have a self-funded fellowship such as JRF/SRF, will I still be expected to have teaching duties on the BITS campus?
Yes, you will still be required to carry out teaching assistant (TA) duties every semester you are enrolled in the program.
- As part of being a teaching assistant (TA), how many hours of classes am I expected to assist in a week?
On an average, approximately 8 hours a week.
- Does OHT provide research assistantships (RA) to complement the stipend?
Yes, OHT provides research opportunities to PhD students to earn additional income on top of their stipend.
- Does BITS or OHT provide on-campus accommodation?
Students will be expected to be at one of the BITS campuses in their first year. From the second year onwards, students are encouraged to spend time on one of the BITS campuses or OHT India campus, depending on their research area of interest. OHT will be able to provide housing on campus (expected completion: 2024/2025). Students are expected to cover their cost of stay/living at both institutions.
- Can PhD students live off-campus and attend classes?
Yes, PhD students can live off-campus and commute with their own vehicles or any other available public modes of transportation.
- Is there any accommodation for TAs assisting classes remotely?
There usually is no provision for such requests. However, temporary accommodations can be discussed on a case-by-case basis.
- Are there any qualifier exams to confirm one’s candidature as a PhD student? Are multiple attempts of the exam allowed?
Yes, apart from the semester exams for the courses a candidate is taking, candidates are expected to pass two qualifier exams to maintain their candidacy as a PhD student. Students are expected to choose a primary and a secondary research area for their thesis and to write qualifier exams in these areas. The areas can be from two different departments. The candidate should consult the DRC (Departmental Research Committee) to know about the areas offered and the exam modalities. Every student has until the end of the second year to appear for and clear their qualifier exams. A maximum of two attempts are allowed to clear qualifier exams and both the areas must be cleared together.

Eligible students may apply for the PhD program in Data Sciences for Global Health, commencing in July 2023. Online application forms will be available at from December 2022 through an extended deadline of April 30, 2023. The number of students admitted will vary based on the availability of positions in the department, funding, and the merit of applicants.
Applications to the PhD program are invited from candidates with a master’s degree in any basic science or liberal arts discipline. We also accept applications from candidates with a bachelor’s degree in medical, dental, veterinary, pharmaceutical, or alternative health sciences and engineering. Applicants from other fields are also encouraged to apply.
The minimum eligibility requirements for admission are as follows:
- ME / MTech / MPharm / MBA / MPhil: minimum of 60% aggregate
- MSc / BE / BPharm or an equivalent degree: minimum of 60% aggregate
- MA: minimum of 55% aggregate
- MBBS / BDS / BVSc / MD / MDS / MVSc / BAMS / BHMS / BUMS / allied
Applicants should submit the following:
Statement of research purpose (maximum two pages), indicating the candidate’s academic background, broad research interests, career goals, and how a PhD in Data Sciences for Global Health from BITS Pilani–OHT will advance their career goals.
Two letters of recommendation
The shortlisted applicants will be interviewed about their knowledge of global health, data sciences, and research interests. OHT will participate in the interviewing panel. There will be no written exam, but grades from previous written exams will be considered.
If you have any questions, please contact [email protected] .

Invest in a better planet for future generations. Support our work to fight drug resistance, prevent disease spillovers, and improve pandemic preparedness.
Stay Informed
Too busy to keep up with the latest scientific literature in global health? Let us summarize it for you with our weekly digest. Sign up here.
Privacy Overview

One Health Graduate Students
Graduate research assistantship awards provide an annual stipend, allowance for tuition and fees, and health insurance for graduate students focusing on One Health research. Awards are available to students throughout the University of Arizona.
One Health 2024 Graduate Research Fellowship
2024 Fellowship Description : The University of Arizona's One Health Research Initiative is seeking applications for Graduate Research Fellowships. One Health is a collaborative, multisectoral, and transdisciplinary approach with the goal of achieving optimal health outcomes recognizing the interconnections among people, animals, and their shared environment (including ecosystems, and social and built environments). These positions will begin in the fall semester of 2024. Appointments will be made for one calendar year with the possibility of applying for a second year of funding; please see below for reappointment requirements. Awards will provide an annual stipend, allowance for tuition and fees, and health insurance. Projects must have a One Health focus at the intersection of environmental health, human health, and animal health. The competition is open to projects that combine at least two of these three areas and have a plan for future growth into all three areas. Proposals must explicitly state the overall One Health problem under study, and how the current objectives fit into the overall problem. The One Health Advisory Committee is available to help students needing assistance with fitting their research objectives into the One Health framework. To request assistance, please contact Griselda Ruiz-Braun at [email protected] at least four weeks prior to the submission deadline.
Eligibility : Applicants can be US citizens, residents, or holders of an F1 visa. Applicant must be a full-time student in a University of Arizona graduate program.
Required materials:
Nomination from the principal investigator with information on: 1) Why this student is an ideal candidate for a fellowship, 2) What funding is available to the student and their research project, and 3) How the project fits with the One Health mission (no more than two pages).
Candidate’s CV including GPA in graduate coursework.
Research plan written by the candidate outlining the One Health research that the student proposes to pursue while on the fellowship (no more than one page).
A statement outlining the student’s experience and training to perform the research (no more than one page).
For students applying for a renewal of funding, a statement on achievements during the first year of funding (no more than one page).
Deadline : Monday, Feb. 12, 2024 by 5:00 pm AZ
Review Process : The One Health Advisory Committee will review the applications. The candidate will be selected based on achievement, potential impact of the proposed research, fit of the research project with the One Health mission, and the potential for future success. In accordance with the University of Arizona’s commitment to inclusive excellence , principal investigators are encouraged to nominate candidates from diverse backgrounds, especially individuals historically underrepresented in STEM fields.
For questions , contact Professor Frank von Hippel, [email protected]
Email application in ONE PDF file to: [email protected]
One Health 2023 GRA Awardees
Ma’in zaid alghzawi.

Ma’in Zaid Alghzawi was born and raised in Jordan, which faces similar water limitation challenges to those in Arizona. Knowing that alternative water resources such as treated wastewater have been increasingly used on a larger scale in the area for agricultural purposes, more environmental challenges are being faced. In addition, other concerns have been raised recently about the increased soil contaminants released from different places (e.g., As-Samra Wastewater Treatment Plant) all over the country. The unexpected flow of refugees in Jordan has a huge contribution in these concerns. Moreover, obvious symptoms of climate change in our local and global environments have also compounded the problem. Therefore, conducting PhD studies in Environmental Science-Chemistry field and investigating the fate of various types of contaminants in the environment, as well as their impacts on human health is a necessity in tackling the problem. This field would satisfy Alghzawi’s ambition of being engaged in facing the environmental challenges in Jordan and other countries. As a Ph.D. candidate in the Department of Environmental Science, he is developing expertise at the interface between soil chemistry and human health. Alghzawi joined Dr. Jon Chorover’s research group to investigate how climate and primary tailings materials interact to control the products and propagation of geochemical reactions in mine waste sites (as part of the University of Arizona Superfund Research Program) and how these processes affect the bioaccessibility of toxic metals and metalloids in simulated gastrointestinal fluid. Alghzawi has previously measured total metal(loid) concentrations down tailings weathering profiles from sites forced by a range of climate conditions using microwave-assisted acid digestion prior to ICP-MS analysis. He mentored graduate and undergraduate students interested in applying this procedure to their own analyses. With support from the One Health program, Alghzawi is initiating in vitro bioassay experiments to assess the fraction of total toxic metal(loid) concentration in tailings that is bioaccessible in stomach and intestinal fluids, as a means to improve risk assessment. Alghzawi was previously a Superfund Research Center trainee and presented a poster at the NIH/NIEHS Superfund Research Program Annual Meeting that was titled “Investigating the Transformations of Arsenic and Toxic Metals Speciation in Mine Tailings Under Different Climatic Conditions”. In 2022, Alghzawi was selected to present a poster at the SRP-35TH Anniversary Annual Meeting entitled "Climate-induced variation in toxic metal(loid)s concentration and speciation in weathered mine tailings”.
Read Research Abstract
Joshua Douglas Arnbrister

Joshua Douglas Arnbrister graduated in 2016 from Oregon State University with a bachelor’s degree in zoology. After a year working for Clackamas County Vector Control District, he attended the University of Arizona to pursue a master’s in entomology. His master’s research focused on engaging community health workers in Southern Arizona in mosquito control and surveillance. He has also been extensively involved in community outreach events and tick surveillance projects in the area of Pima County. He is currently pursuing a PhD in Entomology at the University of Arizona, focusing on flavivral ecology in Arizona and Sonora, specifically focused on dengue surveillance and factors influencing transmission.
Taylor Ann Foerster
Taylor Ann Foerster is a final year PhD candidate (ABD) in the department of communication at the University of Arizona. She holds an MS in Agricultural Education and a BS in Natural Resources (Wildlife emphasis) that inform her current research. Her research interests include the application of communication theory to inform the development of effective communication strategy, human dimensions of natural resources, and community engagement.
Stephanie Hargrave
Jenna honan.

Jenna Honan is a Scientific Analyst and PhD candidate in Environmental Health Sciences at the University of Arizona's Mel and Enid Zuckerman College of Public Health. She is a first-generation student from rural Arizona, lending a unique perspective to her studies. Her interests include contaminant fate and transport in the environment, ecological restoration, community-engaged research, policy development, ecotoxicology, and statistical modeling. Her current research areas focus on environmental and occupational exposures, including VOCs in beauty salons and autobody shops, pesticides and other toxicants on and near agricultural sites, and childhood exposures to contaminants found in soil and dust around the home. She always works with the goal of helping prevent long-term adverse health outcomes that likely follow such exposures.
Yoonhee Jung

Yoonhee Jung is a 4th year PhD student in the Environmental Health Science program at the University of Arizona. Her main research interests in her doctoral degree is Quantitative Microbial Risk Assessment (QMRA), Infectious Viruses, Indoor Environment and Intervention, Risk Perception, and Water Treatment. She studied water treatment and disinfection using advanced oxidation processes (AOP) for her bachelor's and master's degrees in the Environmental Engineering department at Yonsei University (Mirae), South Korea. She recently published her laundry QMRA research "Evaluating infection risks and importance of hand hygiene during the household laundry process using a quantitative microbial risk assessment approach" in the American journal of infection control (2023). She received the GRA scholarship for One Health research, which is "Risk-risk tradeoffs and risk-perception study associated with cleaning and disinfection (C&D) using “green” products" for the 2023-24 academic year. As a Risk assessor and Exposure scientist, she will continue working on the project to prevent pathogens and harmful chemical exposure to the public and make appropriate interventions for the indoor environment.
Sarah Leighton

Sarah Leighton is a PhD Student in Social Psychology, minoring in Human-Animal Interaction. She holds a BA in Neurobiology and Behavior from Cornell University and an MS in Human-Animal Interaction from Purdue University. Prior to pursuing her PhD, Sarah spent 10 years working at a national non-profit service dog provider, Canine Companions – first as a service dog trainer, and most recently as the National Director of Training and Client Services. She has participated on multiple expert panels and advisory committees pertaining to service dog placements including with Assistance Dogs International, American Humane, and the American Veterinary Medical Association. Sarah’s PhD research is conducted through the College of Veterinary Medicine’s OHAIRE Lab (led by Dr. Maggie O’Haire) and focuses on understanding how service dog placements influence biopsychosocial outcomes for individuals with disabilities through a One Health lens.
Tuo Liu (LT)

Tuo Liu (LT) is a Ph.D. student at the University of Arizona. He majors in Environmental Health Sciences, and minor in Biostatistics. His research interests include Metabolomics, Proteomics, Feature Selection, High-Dimensional Data Analysis and Application of Data Science tools in Public Health research He serves as a Research Associate in the Burgess Lab and the Furlong Lab and focus on the application of metabolomics & proteomics on firefighters’ occupational health improvement.
Neeraja (Neera) Setlur

Neeraja (Neera) Setlur is a 3rd year Ph.D. student in the department of Environmental Sciences. She has a bachelor’s degree in Hydrogeology from the University of Texas at Austin, and she worked as a petroleum geoscientist in ExxonMobil before beginning her Ph.D. at the University of Arizona. Her research focuses on the remediation of PFAS from contaminated water. Per and polyfluoroalkyl substances are not biodegradable and extremely hard to remove from the environment. These substances can accumulate in our bodies over time and cause several health issues including different types of cancer. Unfortunately, they are ubiquitous in our daily lives and continue to pollute our environment and bodies. Her current project tests the efficacy of an organic based polymer that can be injected into the pores of an aquifer and attract PFAS from the groundwater to stabilize it in place. The polymer in the aquifer will act as a filter so the groundwater we pump for potable water has significantly lower concentrations of PFAS.
Carrie S. Standage-Beier

Carrie S. Standage-Beier is a Nutritional Sciences Ph.D. student at the University of Arizona School of Nutritional Sciences and Wellness. She is under the mentorship of Dr. Dawn K. Coletta, an Associate Professor at the University of Arizona, with a shared appointment in the Division of Endocrinology, Department of Medicine, and Department of Physiology. Carrie’s doctoral research is funded by a One Health fellowship, which examines the intricate interplay between social determinants of health and genetic variants contributing to cardiometabolic disease among Latino participants from El Banco por Salud (Wellness Bank). This initiative stems from a collaboration between the University of Arizona’s Center for Disparities in Diabetes, Obesity, and Metabolism and Federally Qualified Health Centers, El Rio Health, and Mariposa Health in Southern Arizona. Carrie’s academic journey includes a Master of Public Health degree in Health Behavior Health Promotion from the University of Arizona, as well as a bachelor’s degree in Nutrition Dietetics from Arizona State University. Following her bachelor’s degree, Carrie completed a dietetic internship at the University of Nevada, Reno.
Ben Stansfield

Ben Stansfield is a 3rd year Genetics PhD student working in Dr. Aikseng Ooi’s laboratory. He moved from the UK in 2020 to pursue a PhD and has since been using computational biology, bioinformatic, molecular biology and chemical biology tools to analyze large genomic data sets and investigate signaling pathways in cancer. His current research focuses on developing a novel massively parallel sequencing technique that captures mutational events as they occur, to then apply it to investigate processes that drive the development of pathogenic mutations in the context of environmental exposure, human diseases, and animal health. I am also investigating the role base excision repair (BER) plays in the development of genomic mutations in the hereditary cancer syndrome, hereditary leiomyomatosis and renal cell cancer (HLRCC).
Noriko Tamari
Noriko Tamari is a PhD candidate in Epidemiology at the College of Public Health, University of Arizona. She worked as a Japan Overseas Cooperation Volunteer in Honduras, working on a project on Chagas disease control in local communities. She also worked as a clinical research coordinator in several hospitals and clinics in Tokyo, Japan. In her master's project in western Kenya, she spent seven months collecting field data on malaria infection and the number of people using bed nets. Her dissertation topic focuses on the interaction between Water, Sanitation, and Hygiene (WASH) and mosquito dynamics in western Kenya.
Chloe Thomas

Chloe Thomas is a PhD Student in Biosystems Engineering and graduate researcher in Dr. Yoon’s Biosensor Lab. Her research focuses on detecting contaminants in water using paper microfluidic chips and computer vision. She is currently designing a system utilizing this technology to detect and identify PFAS in water. She will be working with Tucson water over the course of this project to collect and test field samples from local wells. Over the summer she worked as a research engineer at Biosphere II. In this position she has worked on designing and installing remote sensing systems to aid research objectives. Prior to coming to University of Arizona, Chloe helped with sustainability projects in Argentina in underserved communities with the 100,000 Strong in the America’s grant. Chloe holds a B.S. degree in Mechanical Engineering from the University of Wisconsin – Platteville.
Sri Harsha Vishwanath

Sri Harsha Vishwanath is a third-year Ph.D. student in microbiology. His research is focused on the computational prediction of host-pathogen interactions to help find new drug targets to tackle Clostridioides difficile infection (CDI). Through a fellowship with Humane Society International, he previously tried to substitute animal models in drug testing utilizing an in silico and biological approach. He has also worked on mapping the spread of the Bluetongue Virus, a seasonal veterinary epidemic in India, through molecular epidemiological studies. His goal is to unify human health and veterinary sciences since a lot can be learned through their collaboration.
- Tools and Resources
- Customer Services
- Behavioral Science and Health Education
- Biostatistics and Data
- Disaster Preparation and Response
- Environmental Health
- Epidemiology
- Global Health
- Health Services Administration/Management
- Infectious Diseases
- Non-communicable Diseases
- Public Health Policy and Governance
- Public Health Profession
- Sexual and Reproductive Health
- Special Populations
- Theory and Methods
- Share This Facebook LinkedIn Twitter
Article contents
“one health” from concept to application in the global world.
- Maria Cristina Schneider , Maria Cristina Schneider Department of Health Surveillance, Disease Prevention and Control, Pan American Health Organization
- Claudia Munoz-Zanzi , Claudia Munoz-Zanzi Department of Public Health, University of Minnesota
- Kyung-duk Min Kyung-duk Min Department of Public Health, Seoul National University
- and Sylvain Aldighieri Sylvain Aldighieri Pan American Health Organization
- https://doi.org/10.1093/acrefore/9780190632366.013.29
- Published online: 26 April 2019
The vision that everything is connected in this world is not new. However, to respond to the current challenges that the world is facing, the integrated vision that humans, animals, and the environment are linked is more important than ever. Collaboration among multiple disciplines is crucial, and this approach is fundamental to understanding the One Health concept.
A transdisciplinary definition of One Health views animals, humans, and their shared settings or environment as linked and affected by the socioeconomic interest of humans and external pressures. A One Health concept calls for various disciplines to work together to provide new methods and tools for research and implementation of effective services to support the formulation of norms, regulations, and policies to the benefit of humanity, animals, and the environment for current and future generations. This will improve the understanding of health and disease processes as well as prediction, detection, prevention, and control of infectious hazards and other issues affecting health and well-being in the human-animal-ecosystem interface, contributing to sustainable development goals, and to improving equity in the world.
- animal-human-ecosystem interface
- multidisciplinary
- transdisciplinary
- human health and agriculture
- integrated vision
Why the “One Health” Approach Is Important
The importance of the connection among humans, animal and the environment in this world is not new. However, to respond the current challenges that the world is facing, the integrated vision that we are all linked has never been so important, and collaboration among multiple disciplines so crucial. As an introduction, this section presents a brief review of the global context and some suggestions as to why the One Health approach could be beneficial to better understanding and better performance in this setting. This section reviews the global context and describes how the One Health approach could be beneficial to better understanding and performance in this setting. 1
Demographics
The estimated world population in 2017 was 7.6 billion and is expected to reach 8.6 billion in 2030 and 9.8 billion in 2050 (United Nations, 2017 ). This trend is expected to continue, with around 83 million people being added each year, even as fertility levels continue to decline. From 2017 to 2050 , it is expected that half of the world’s population growth will be concentrated in just nine countries. In order of their expected contribution to total growth, those countries are India, Nigeria, the Democratic Republic of the Congo, Pakistan, Ethiopia, the United Republic of Tanzania, the United States, Uganda, and Indonesia. The concentration of global population growth in some less affluent countries may present a considerable challenge to their governments in implementing the United Nations’ 2030 Agenda for Sustainable Development (Box 1 ).
Why Demographics Matter in the One Health Approach
As the world’s population grows, the demand for food increases. According to the Food and Agriculture Organization of the United Nations (FAO), the human food chain continuously experiences threats from an increasing number of outbreaks of transnational animal and plant diseases and pests and food safety (FAO, 2018 ). These threats to the human food chain may impact human health, food security, livelihoods, national economies, and global markets. Although growth in demand for virtually all food commodities is expected to be less than in the previous decade, food insecurity will remain a critical global concern and the coexistence of malnutrition poses challenges in many countries (OECD & FAO, 2017 ). Trade will represent a broadly constant share of the sector’s output over the coming decade. Food imports are becoming increasingly important for food security, particularly in parts of Africa and the Middle East. In the last decade, the People’s Republic of China was the main source of growth in demand for commodities (OECD & FAO, 2017 ). From the One Health perspective, it is important to understand the production chain in this global market and secure the biosafety and biosecurity of the products.
Urbanization
Globally, more people now live in urban areas than in rural areas. In 1950 , 30% of the world’s population lived in urban areas. This rose to 54% in 2014 and is projected to be 66% by 2050 (United Nations, 2015c ). Urbanization rates vary across the world’s regions, of which the most urbanized are currently Northern America (82%), Latin America and the Caribbean (80%), and Europe (73%) as compared with Asia (48%) and Africa (40%), which combined are home to almost 90% of the world’s rural population of close to 3.4 billion (United Nations, 2015c ). Just three countries—India, China, and Nigeria—together are expected to account for 37% of the projected growth in the world’s urban population between 2014 and 2050 . Close to half of the world’s urban dwellers live in settlements of fewer than 500,000 inhabitants, while around 10% live in a megacity of at least 10 million inhabitants (United Nations, 2015c ).
Why Urbanization Matters in the One Health Approach
Higher population density, especially in poor countries, can increase contact among people and facilitate the transmission of diseases, as was seen during the Ebola outbreak in 2015 (World Health Organization (WHO), 2015 ). Rapid urbanization implies close proximity with companion animals, and specifically with rodents, as well as greater needs for sanitation and waste disposal in crowded urban settings. On the other hand, rural populations in least-developed countries rely on their animals as a protein source or to help in agriculture, and many live in areas close to forests and in close contact with wild animals.
Poverty and Income Equality
Around 10% of the global population in 2013 was living in extreme poverty (by the international definition of living on less than $1.90 per day; World Bank, 2016 ). Efforts to end extreme poverty are far from over and a number of challenges remain to achieving this main goal as those in extreme poverty often live in remote areas and fragile contexts. Even though the proportion of people living in extreme poverty globally has gradually decreased from almost 4 in 10 people in 1990 to just over 1 in 10 in 2013 , more than 767 million people are affected (World Bank). Although economic indicators suggest that more people are moving out of extreme poverty and that in some regions such as Latin America and the Caribbean the middle class is growing (World Bank, 2012 ), poverty levels are still unacceptably high.
The World Bank ( 2016 ) reported that the income gap had widened in 34 of 83 countries monitored, with incomes growing faster among the wealthiest 60% than the bottom 40%. Nonetheless, within-country inequality had decreased in many places since 2008 .
Why Poverty Matters in the One Health Approach
The first of the eight Millennium Development Goals (MDGs) defined by the United Nations ( 2015a ) was to eradicate extreme poverty and hunger by 2015 . For the developing regions as a whole, the share of undernourished people in the total population reduced from 23.3% in 1990–1992 to 12.9% in 2014–2016 . Some regions have shown fast progress, such as Latin America, parts of Asia and Africa and the Caucasus, and 72 of 129 developing countries monitored by FAO reached the MDG 1c hunger target (FAO, 2018c ). Most of these benefited from stable political conditions and economic growth, often accompanied by social protection policies that targeted vulnerable population groups. Many countries that did not reach the MDG hunger targets had experienced natural or human-induced disasters or political instability, resulting in long-term crises with increased vulnerability and food insecurity for much of the population (FAO, 2018b ).
Despite the decline in global poverty and undernourishment rates, around 815 million people are still undernourished. Economic growth is key to reducing undernourishment, but it has to be inclusive and provide opportunities for improving the livelihoods of the poor. One key to progress is to enhance the productivity and incomes of smallholder family farmers (FAO, 2018b ). The UN General Assembly in 2015 adopted the resolution of “Transforming Our World: The 2030 Agenda for Sustainable Development,” which recognized the eradication of poverty as the greatest global challenge and an indispensable requirement for sustainable development (United Nations, 2015b ). The One Health approach is crucial to reducing hunger and extreme poverty, primarily in rural populations in developing countries.
Box 1. United Nations Sustainable Development Goals
Migration and displacement.
Recent events in the Middle East and North Africa triggered a dramatic increase in migration and the number of refugees around the world, creating one of the largest humanitarian emergencies of our era. According to the UN Refugee Agency ( 2018 ), levels of displacement are the highest on record, with 65.6 million people forced from their homes. Among them are nearly 22.5 million refugees, over half of whom are under the age of 18. Thirty percent of displaced people are being hosted in Africa, 26% in the Middle East and North Africa, 17% in Europe, 16% in the Americas, and 11% in Asia and Pacific.
Why Migration and Population Displacement Matter in the One Health Approach
Displaced people often are in situations of overcrowding, inadequate sanitation, and poor access to health services, all of which create the potential for the spread of communicable diseases (Schneider et al., 2012 ). Things that displaced people need include drinking water, safe food, the means to safely prepare meals, pest control for camps, waste disposal and sanitation, and many other requisites for basic dignity in life.
Infectious Hazards and Epidemics
Studies have found that around 70% of infectious hazard threats to public health have an interface with animals (Chomel, Belotto, & Meslin, 2007 ; Schneider et al., 2011 ; Taylor, Latham, & Woolhouse, 2001 ). Taylor et al. ( 2001 ) found that an estimated 61% of human pathogens worldwide have been classified as zoonoses, a subgroup that comprises 75% of all emerging pathogens of the past decade previous to their study (Taylor et al., 2001 ). The emergence of new strains is always a possibility, as has occurred with the Ebola virus, human immunodeficiency virus (HIV), severe acute respiratory syndrome (SARS), influenza A (H5N1) with a pandemic potential, West Nile virus, and the novel influenza A (H1N1) virus (Centers for Disease Control and Prevention (CDC), 2003 ; Fraser et al., 2009 ; Jones et al., 2008 ; Webster, Peiris, Chen, & Guan, 2006 ). At the same time, very old and well-known infectious hazards such as rabies, plague, and anthrax still persist and continue to produce outbreaks and potential public health emergencies of international concern (PHEIC) and damage to animal health (Cleaveland, 2014 ; Schneider et al., 2014 ).
The World Health Organization (WHO) issued its revised International Health Regulations (IHRs) in 2005 to “help the international community prevent and respond to acute public health risks that have the potential to cross borders and threaten people worldwide” (WHO, 2008 ) (Box 2 ). A study by the Pan American Health Organization (PAHO) quantified the importance of the diseases common to animals and humans in events recorded by the Event Managements System/IHR for the Region of the Americas, and concluded that approximately 70% of events reported were within the animal–human health interface (Schneider et al., 2011 ).
Why Infectious Hazards and Epidemics Matter in the One Health Approach
Diseases have the potential to transcend geopolitical boundaries through international travel and trade. The economies and livelihoods of the entire international community can be affected by a single health crisis in one country. Three PHEICs have been declared since the implementation of the new IHR: influenza A (H1N1) in 2009 , Ebola virus in 2013 , and Zika virus in 2015 . These events occurred within the human–animal–environment interface. In some epidemics, such as influenza, animals play a major role in the interface, whereas in others such as Zika virus they are only accidental hosts. For Ebola virus, the ecosystem characteristics have been studied for several decades and are well described (Morvan, Nakouné, Deubel, & Colyn, 2000 ; Muyembe-Tamfum et al., 2012 ). Other events reported since the new IHR have also had an interface with animals or with the environment and were not classed as PHEICs, but were nonetheless also sources of much concern internationally, such as Middle East respiratory syndrome (MERS) in the Middle East (WHO, 2013 ), cholera in Haiti and Yemen (WHO, 2018 ), and yellow fever in Africa and Brazil (PAHO, 2018 ).
Box 2. International Health Regulations
The International Health Regulations (IHR) are an international legal instrument that is binding in 196 countries across the globe, including all the member states of WHO (WHO, 2016 ). The aim of the regulations is to help the international community prevent and respond to acute public health risks that have the potential to cross borders and threaten people worldwide.
For that purpose and as part of IHR implementation, WHO member states are committed to strengthening their surveillance of and ability to rapidly detect, assess, notify, and report potential public health emergencies of international concern (PHEICs) in accordance with these regulations.
PHEICs are extraordinary events— that have been determined, as provided in the IHR, to “constitute a public health risk to other States through the international spread of disease. . . and potentially require a coordinated international response” (WHO, 2016 ).
Events are identified as potential PHEICs and reported to the six WHO IHR ( 2008 ) Regional Contact Points when they fulfill at least two of the following four criteria
a serious public health event is suspected
the event is considered unusual or unexpected
there is a significant risk of international spread
the event poses a significant risk to international travel or trade (2).
Events that have been reported or detected as potential PHEICs are entered into a database known as the Event Management System, which is administered by WHO.
The IHRs, which entered into force on June 15, 2007 , require countries to report certain disease outbreaks and public health events to WHO. Building on the unique experience of WHO in global disease surveillance, alert, and response, the IHRs define the rights and obligations of countries to report public health events and establish a number of procedures that the WHO must follow in its work to uphold global public health security.
Trade, Tourism, and the Global Economy
Animal-origin food products are considered a commodity, and according to the OEDC–FAO Agricultural Outlook report ( 2017 ), global food commodity prices are projected to remain low over the next decade compared to previous peaks, as demand growth in a number of emerging economies is expected to slow down. Additional calories and protein consumption are expected to come mainly from vegetable oil, sugar, and dairy products, whereas growth in demand for meat is projected to reduce, with no new sources of demand to maintain the momentum previously generated by China.
FAO data show that milk was the highest livestock product in tonnes during 2014 (652,351,920 tonnes of cow milk and 107,764,334 of buffalo milk); followed by pig meat (115,313,734); chicken meat (100,352,826); eggs (69,790,757); and cattle meat (64,681,068 tonnes). At close to half of the world’s production, the Americas are the largest producers and exporters of cattle and chicken meat (FAO, 2018 ).
Around 10% of gross domestic product (GDP) globally comes from tourism and this has been increasing in recent years (World Bank, 2015 ). The tourism sector creates jobs and is an opportunity for developing countries with natural and cultural assets.
Why Trade, Tourism, and Global Economy Matter in the One Health Approach
For some common animal diseases, the appearance of cases in one country can have an important impact on trade related to animal products in others. This effect was observed across several countries in the case of avian influenza A (H5N1) in 2006 (Burns, van der Mensbrugghe, & Timmer, 2006 ). Although H5N1 was not detected in the Americas, there was a 40% drop in the share values of large poultry producers due to the indirect impact of the global market (Newcomb, 2008 ).
Economic losses in trade due to diseases in the animal–human interface have been estimated in billions of dollars. For example, the global economic losses from SARS were estimated to be $40–50 billion, and there was even a significant impact on the GDP of Canada and of Asian countries (Newcomb, 2008 ). Another study estimated that economic losses were in excess of $125 billion, considering the broader economic cost of some diseases affecting people and animals globally in the period 1995–2008 (Newcomb, 2008 ). The World Bank also estimated economic losses of at least $80 billion related to six zoonotic disease outbreaks between 1997 and 2009 (World Bank, 2012 ). In addition, there were high indirect costs from SARS; for example, the psychological impact on hospital workers in Canada and anxiety in affected communities in Hong Kong (Leung et al., 2004 ; Nickell et al., 2004 ).
Many of the disease outbreaks in the interface created tension in travel and tourism, even though WHO recommends not to restrict entry of people originating from affected countries. During the SARS outbreak, tourism profits fell by 15–40% in Asian countries (Newcomb, 2008 ).
Climate Change
Climate change is affecting every country, disrupting national economies, and affecting lives (United Nations, 2015a ). People are experiencing its significant impacts, which include rising sea level, changing weather patterns, and more extreme weather events. It is already costing communities and countries dearly and this will only increase, with the poorest and most vulnerable people being most affected (United Nations, 2015a ).
According to WHO, climate change affects the social and environmental determinants of health: clean air, safe drinking water, sufficient food, and secure shelter (WHO, 2017 ). Between 2030 and 2050 , climate change is expected to cause approximately 250,000 additional deaths per year from malnutrition, malaria, diarrhea, and heat stress.
Within the past decade, record-breaking and devastating rainfall events have occurred, and 2010 was ranked the wettest year on record (Coumou & Rahmstorf, 2012 ). Disasters may increase in frequency, along with an increase in the intensity of extreme weather events such as heatwaves, droughts, heavy rainfall, storms, and an expansion in areas affected by droughts and floods (Meehl et al., 2007 ).
Why Climate Change Matters in the One Health Approach
The topic of infectious diseases following natural disasters has been studied for many years in all regions of the world (Ligon, Spiegel, Le, Ververs, & Salama, 2007 ; Watson, Gayer, & Connolly, 2007 ). Rain and floods are considered primary risk factors for leptospirosis, cholera, and diarrhea outbreaks, as well as for many other communicable diseases (Schneider et al., 2012 ).
Climate-related extreme events have severe consequences for human and animal health and food and water safety and security, particularly for poor coastal and island communities and populations dependent on agriculture and natural resources (Schneider et al., 2012 ). Climate change may increase the susceptibility of animals to disease, increase the range or abundance of vectors/animal reservoirs; prolong vector transmission cycles, increase vulnerability of particular social groups and economic sectors due to extreme weather events and ecosystem stress, and impact on farming husbandry practices, including the use of veterinary drugs (Tirado, Clarke, Jaykus, & McQuatters-Gollop, 2010 ). Also, according to the FAO ( 2018a ), climate change threatens our ability to achieve global food security, eradicate poverty and achieve sustainable development. Climate change has both direct and indirect effects on agricultural productivity, including changing rainfall patterns, drought, flooding, and the geographical redistribution of pests and diseases.
History of an Integrated One Health Concept
Throughout the history of humankind, there has always been a view that humans and animals are connected. Rabies is a good example to illustrate this connection. In The Iliad , Homer referred to rabies and the malignant influence of Sirius—the dog star of the constellation Canis Major, or Orion’s dog—on the health of mankind, and compared the invincible Hector to a rabid dog (Baer, 1975 ; Schneider & Santos-Burgoa, 1994 ). Zinsstag, Schelling, Waltner-Toews, and Tanner ( 2011 ) reviewed the history of integrative thinking around human and animal health, which started with ancient healers who cared for both humans and animals. Egyptian papyri from 1800 bc describe human and animal disease and the Zhou dynasty in China ( 11th – 13th century ) had one of the earliest organizations of an integrated public health system to include medical doctors and veterinarians.
The 19th-century German physician, naturalist, anthropologist, and politician Rudolf Virchow is considered the “father of modern pathology” (Magalhaes, 2010 ). With the advance of cellular pathology came an interest in linking human and animal medicine as a form of comparative medicine, based on the discovery of similarities in the disease processes in human and animals (Zinsstag et al., 2011 ). Virchow was also an important public health professional, and he supported the idea of dividing epidemics into natural and cultural, considering the latter to be a product of disturbances experienced by society. He and his contemporaries supported the concept of a unified science (Magalhaes, 2010 ). William Osler, a Canadian physician and pathologist, was a student of Virchow’s. Osler, who is widely considered to be the father of modern medicine, brought this integrated medical thinking to North America (Cardiff, Ward, & Barthold, 2008 ). Osler’s deep interest in the linkages between human and veterinary medicine is described in his work “The Relation of Animals to Man.”
In the Americas of the late 1940s, the important role of animals in the epidemiology of zoonotic diseases was recognized, including how these diseases could spread and how they could be controlled. In 1947 , James Steele founded the Veterinary Public Health Division at the Communicable Disease Center (now Centers for Disease Control and Prevention, CDC) in the United States. This division played an important role in the public health response to diseases such as rabies, brucellosis, salmonellosis, Q fever, bovine tuberculosis, and leptospirosis. The application of veterinary science in public health was introduced to other countries in the Americas and around the world. The first “Report of the Zoonosis Commission in the Region” was published in 1947 and the Veterinary Public Health Program at PAHO was created in 1949 (WHO, 2002 ). Rabies was one of the priority zoonotic diseases for control at that time in the Americas. A joint health and agriculture surveillance system for rabies was created in the late 1960s, and cases in humans and animals (domestic and wild) in all countries of the region were reported in the same surveillance bulletin, periodically distributed by PAHO (OPS, 2018 ).
In the 1970s, Calvin Schwabe, an American veterinarian, rethought the term “one medicine” and is recognized for having coined the concept that fully recognized the close systemic interaction of humans and animals for nutrition, livelihood, and health (Zinsstag et al., 2011 ). Schwabe rearticulated concepts from Virchow in the 1964 edition of Veterinary Medicine and Human Health (Schultz, 2011 ). The concept of “one medicine” was much used by pathologists in the development of new cross-species treatments and vaccines and in other experimental studies in animals that would benefit human health.
New zoonotic diseases have been discovered continually but have not always appeared as a serious public health impact at that moment. For instance, the Zika virus first appeared in the late 1940s (Zanluca et al., 2015 ) and the Ebola virus in the 1970s (Muyembe-Tamfum et al., 2012 ), both in small villages in Africa, but it was some decades later when the diseases appeared in large cities that they became public health emergencies of international concern (WHO, 2014 , 2017 ).
In the 1990s the world experienced the emergence of new threats in the animal–human health interface, including bovine spongiform encephalopathy (BSE), or “mad cow disease,” and SARS, which had serious impact on the economy, travel, and society (Kuo, Chen, Tseng, Ju, & Huang, 2008 ; Newcomb, 2008 ; Nickell et al., 2004 ). In 2003 outbreaks of avian influenza A were reported in Asia and the disease posed a potential pandemic threat with significant economic repercussions. Trade disruption and the decline in international tourism were estimated to cause billions of dollars in global economic losses in addition to significant social impact (Kuo et al., 2008 ; Newcomb, 2008 ; Rushton, Viscarra, & Bleich, 2005 ). The constant threat of new pandemics originating in the animal–human interface demonstrates the fundamental need for intersectoral collaboration, especially in surveillance, risk management, biosafety, and communication. It was in this context that the concept of One Health emerged.
In 2004 , the Wildlife Conservation Society organized a symposium in New York City on “Building Interdisciplinary Bridges to Health in a Globalized World.” The result was a list of 12 recommendations, the Manhattan Principles, that urged world leaders, civil society, the global health community, and scientific institutions to adopt a holistic approach to the prevention and combat of epidemic/epizootic diseases and the maintenance of ecosystem integrity (CDC, 2004 ). Soon, the principles became known as the One World, One Health concept.
Many meetings and frameworks based on this approach have been organized (Box 3 ). During the 2007 International Ministerial Conference on Avian and Pandemic Influenza in New Delhi, it was recommended that a medium-term strategy be developed to address emerging infectious diseases. In response, WHO, the World Organization for Animal Health (OIE), FAO, the United Nations Children’s Fund (UNICEF), the World Bank, and the United Nations System Influenza Coordination (UNSIC) developed a multi-institutional collaboration to prevent, detect, control, manage, and eliminate diseases in the human–animal interface (FAO, OIE, & WHO, 2008 , 2010 ). This collaboration across international organizations focused on supporting member countries to minimize the burden of monitoring and reporting, maximizing support, and avoiding duplication of efforts.
Box 3. One Health Meetings
2015: 2nd Global Health Forum One Health Summit. Davos, Switzerland.
Source: http://onehealth.grforum.org/
2013: Prince Mahidol Award Conference: A World United Against Infectious Diseases; Cross-sectoral Solutions. Bangkok, Thailand.
Source: http://www.onehealthinitiative.com/publications/2013-Conference-Program.pdf
2013: One Health Central and Eastern Africa First International One Health Conference. Addis Ababa, Ethiopia.
Source: https://penaph.net/2013/07/01/first-international-ochea-one-health-conference-addis-ababa-23-27-sept-2013/
2012: One Health Summit, “One Health, One Planet, One Future.” Davos, Switzerland.
Source: http://onehealth.grforum.org
2011: High Level Technical Meeting to Address Health Risks at the Human–Animal–Ecosystems Interfaces. Mexico City, Mexico.
Source: http://apps.who.int/iris/bitstream/10665/78100/1/9789241504676_eng.pdf
2009: One World, One Health: From Ideas to Action. Winnipeg, Canada.
Source: http://www.phac-aspc.gc.ca/owoh-umus/index-eng.php
2008: The 6th International Ministerial Conference on Avian and Pandemic Influenza. Sharm el-Sheikh, Egypt.
Source: http://www.fao.org/docrep/011/aj137e/aj137e00.htm ; https://www.oie.int/doc/ged/D5894.PDF
2008: FAO–OIE–WHO with UNICEF, UNSIC, and the World Bank: A Strategic Framework for Reducing Risks of Infectious Diseases at the Animal–Human–Ecosystems Interface. Verona, Italy.
Source: ftp://ftp.fao.org/docrep/fao/011/aj137e/aj137e00.pdf
2007: International Ministerial Conference on Avian and Pandemic Influenza. New Delhi, India.
Source: http://www.fao.org/docs/eims/upload/237162/ah695e.pdf .
Since that time, other global concepts have emerged on the complex interaction between ecosystems and human health, giving rise to the terms “eco-health” or “ecosystem approaches to health.” This recognizes that well-being and health are the results of complex and dynamic interactions between people, ecosystems, and social and economic determinants (Lebel, 2003 ). Complex system approaches have been used to analyze the occurrence of zoonotic outbreaks (Schneider, 1995 ), as well as other conceptual frameworks considering the animal–human interface. In addition to supporting an interdisciplinary collaboration between human and veterinary medicine with a substantial focus on zoonoses, One Health has evolved into a broader and more holistic paradigm that includes ecological, economic, and social dimensions (Global Risk Forum, 2015 ).
The Concept
The One Health concept seeks to integrate human, animal, and environmental health for the prediction and control of diseases in the human–animal–ecosystem interface (Coker et al., 2011 ; Kaplan, Kahn, & Monath, 2009 ; Rabinowitz et al., 2013 ). It is also defined as an effort to collaborate across multiple disciplines on the local, national, and global level to achieve optimal health for people, animals, and the environment (Frank, 2008 ; Kaplan et al., 2009 ; King, 2013 ).
For Kaplan et al. ( 2009 ), the One Medicine, One Health concept recognizes a unity of purpose, irrespective of anachronistic barriers and obstructions, in which close collaboration and communication across the various disciplines of human and veterinary medicine and other sciences is a powerful strategy. This approach recognizes the need for leaders in the public, animal, and environmental health fields to conduct research, generate evidence, and guide public-policy decision makers through issues involving multiple sectors. The objective is to reduce the emergence and re-emergence of zoonotic diseases (Coker et al., 2011 ; Kakkar & Abbas, 2011 ) and other events of importance at the human–environment–animal interface.
In order to clarify the working definition of the One Health approach, the Stone Mountain Working Group specified the following principles:
It is feasible to integrate efforts in human, animal, and environmental health to predict and control certain diseases at the human–animal–ecosystem interface.
Integrated approaches that take into account human, animal, and environmental health components can improve prediction and control of certain diseases (Rabinowitz et al., 2013 ).
Boxes 4 (leptospirosis) and 5 (avian influenza) describe examples of applications of the working definition of the One Health (Rabinowitz et al., 2013 ) approach on events at the animal–human–ecosystem interface including possible suggestions for integrated action to predict, detect, prevent, and respond to the event.
Box 4. Leptospirosis as an Example of Possible Application of the Operational Concept of One Health
Box 5. avian influenza (h5n1) as an example of possible application of the operational concept of one health.
The definition of One Health as a “collaborative effort of multiple disciplines . . . to attain optimal health for humans and animals while protecting the environment” (King et al., 2008 ) is fitting, considering the importance of multidisciplinary approaches in research, education, services, and policies, which are fundamental for building solid scientific evidence for decision-making in health. However, the definition of One Health currently used by the CDC has been expanded to include the concept of “transdisciplinarity” (CDC, 2018 ). Transdisciplinarity has been defined as “efforts conducted by professionals from different disciplines working jointly to create new conceptual, methodological, and translational innovations that integrate and move beyond discipline-specific approaches to address a common problem” (Harvard Transdisciplinary Research in Energetics and Cancer Center, 2018 ). According to German philosopher Jurgen Mittelstrass ( 2011 ) transdisciplinarity “is intended to imply that cooperation will lead to an enduring and systematic scientific order that will change the outlook of subject matters and disciplines . . . it is a principle of research and science, one which becomes operative wherever it is impossible to define or attempt to solve problems within the boundaries of subjects or disciplines, or where one goes beyond such definitions” (Mittelstrass, 2011 , p. 331). Choi ( 2006 ) discussed the use of the definitions of multidisciplinarity, interdisciplinarity, and transdisciplinarity in health research, services, education, and policy (Box 6 ).
Box 6. Multidisciplinarity, Interdisciplinarity, and Transdisciplinarity Defined
Multidisciplinarity draws on knowledge from different disciplines but stays within its boundaries.
Interdisciplinarity analyzes, synthesizes and harmonizes links between disciplines into a coordinated and coherent whole.
Transdisciplinarity integrates the natural, social and health sciences in a humanities context, and transcends their traditional boundaries.
For the authors of this article, the concept of One Health is based on the integrated vision of how humans interact with animals and with the environment and how professionals in different disciplines can work side by side toward a common goal. Early work by Schneider ( 1984 ) at the local level in a community health project where physicians, nurses, veterinarians, social workers, and others were part of a health team working in close collaboration with the community in a low-income area in Brazil, provided an opportunity to learn about multidisciplinary collaboration focus in a specific community context. This was followed by other experiences in the context of rabies, from local to international level, which also were implemented using this integrated vision. This led to studies of complex systems theory (Garcia, 1986 ) and reflections on theoretical integrated frameworks that could be used to better understand the occurrence of infectious disease outbreaks in the Americas (Schneider, 1995 ).
A transdisciplinary definition of One Health views how animals, humans, and their shared settings or environment (such as ecosystem, soil, climate) are linked and are affected by the socioeconomic interest of humans (such as food production, trade, tourism) and external pressures (such as urbanization, migration, demographics). It also considers how different disciplines can together provide new methods and tools for research and implementation of effective services to support the formulation of norms, regulations, and policies to the benefit of humanity and animals, while considering the environment, for current and future generations. This approach will improve prediction, detection, prevention, and control of infectious hazards and other issues affecting health and well-being in the interface and contribute to the UN’s Sustainable Development Goals to help to improve equity in the world.
Figure 1 shows the application of the theory of complex systems to a specific real case. A critical area (“hot spot”) with a high number of human cases of leptospirosis was identified in the Central Region of Rio Grande do Sul state, Brazil (RS), and environmental and socioeconomic drivers where analyzed (Schneider et al., 2015 ). This critical area (RS Central Region) was considered as a system. Subsystems were defined to better understand the setting or context of RS: the physical/ecosystem/environmental subsystem ( P ); agro-productive subsystem ( A ); socioeconomic subsystem ( S ); and health subsystem ( H ). There are interconnections between the subsystems, such as (1) from P to A , possible interrelations could be the type of ecoregion, soil type, amount of rainfall, proximity to rivers and other natural elements that are suitable for certain types of crops (such as tobacco, rice, or corn), and the system of cattle raising (intensive or free-range); (2) from A to P , possible interrelations could be deforestation or excessive use of the soil for crop production; (3) from S to A , interrelations might include the tendency in the region for smaller-sized properties, provision of economic incentives for certain types of crops (productive process) such as tobacco, historical incentives for European immigration to the area, and easier access to land; (4) from A to S , an example of an interrelation might be that tobacco is a profitable commodity, which provides better living conditions for the people who plant and sell it than other commodities; (5) from S to H , it could be that if the majority of inhabitants of this area have higher economic standards than in other agro-productive areas they also have better conditions for lower illiteracy, higher-quality medical care, and less health inequality; (6) from H to S , if the people of this area were wealthier then they could work and live longer in general; (7) from P to H , if this ecoregion had a good climate suitable for crops and raising animals, it would facilitate good nutrition and general health. In summary, the suggested external conditions of this system in RS Central Region could be (a) the inflow of people from the immigration policies decades ago; (b) land distribution; (c) high quality agriculture work; (d) economic incentives for tobacco production; and (e) agrobusiness policies. Outgoing flow from the system could be (f) tobacco products; (g) other agricultural products; (h) trade; (i) government taxes; and (j) monetary exchange.
Figure 1. A systemic approach to leptospirosis in a “hot spot” in Rio Grande do Sul state, Brazil, using the definition for One Health suggested by the authors.
Subsystems: P, Physical/ecosystem/environment; A, Agro productive; S, Socioeconomic; H, Health system
Interrelations among the subsystems:
Between P and A: type of ecoregion, soil, rainfall, proximity to rivers
From A to P: deforestation, excessive use of the soils for plantations
Between S and A: small properties, economic incentives provided to certain types of plantations (i.e., tobacco)
From A to S: tobacco is a profitable commodity; better life conditions
From S to H: higher economic standards, high quality medical care, lower illiteracy and less health inequality
From H to S: wealthier people, longer life
From P to H: good climate suitable for crops and raising animals, good nutrition
In Figure 2 , six maps illustrate the subsystems and interrelations in RS Central Region, where the higher number of human leptospirosis cases occurred. Environmental drivers in RS Central Region found associated with leptospirosis in humans were ecoregion (Parana-Paraiba interior forest), soil type, and proximity to rivers. Socioeconomic factors included low rates of illiteracy and higher GDP, which were likely suggestive of increased healthcare access and therefore capacity for case detection, higher GDP, and lower income inequality (Gini index) associated with the extensive agricultural production in the area.
Figure 2. Environmental and socioeconomic possible drivers related to the critical areas for human leptospirosis cases in Rio Grande do Sul Central Region, Brazil. (a) Ecoregion; (b) Soil type; (c) Proximity to rivers; (d) Rates of illiteracy; (e) GDP; (f) Gini index. a and b were published in Schneider et al. ( 2015 ).

Global Applications Using the One Health Concept
To analyze the use of the One Health concept globally, a review of publications about One Health in peer-reviewed journals was performed (methodology in Box 7 ), followed by a similar internet search focusing on training being offered on this topic. In total, 955 articles were found. After excluding duplicates (168), articles considered irrelevant to One Health because they did not describe a multidisciplinary approach (515), and articles that were not found (61), 201 articles were reviewed (see Box 7 and Fig. 3 for methodology).
Box 7. Research Methodology: One Health in Peer-Reviewed Journals
A scoping review (Peterson, Pearce, Ferguson, & Langford ( 2017 ) was done to assess what is being published about One Health. This methodology was chosen in place of a systematic review because a broad search was needed on the various perspectives on One Health and to avoid limiting the search to certain types of study design or topic.
The search was performed between January and March 2017. The search strategy was as follows:
Database: PubMed, Embase
Hand searching: Google, each journal
Terms: Determined after reviewing the review paper (their search strategies)
Search terms for review paper:
PubMed: “One Health” [All Fields] AND review [pt]
Embase: “One Health” AND review
All results were organized into thematic blocks: history, concept, and application (training, research, intervention, and advocacy).
Figure 3. Flow chart of search results.
Table 1. Articles Found in the Scoping Review on One Health, by Category and Year of Publication
Source : *Number of publications until March 2017.
The number of articles about One Health increased threefold from 2012 to 2013 , when most were on the application of the concept. In almost half of the publications, the first author was located in the Americas (47.3%) followed by Europe (33.3%). The countries that published most on One Health were the United States (76 publications), the United Kingdom (20), and Australia (10). Although there were articles from all continents, the regions with the majority of One Health publications were North America and Europe (Figure 4 ).
Figure 4. Distribution of affiliations of the first authors identified in the scoping review of One Health publications.
Health Professionals and One Health
As the importance and the use of One Health approaches grows, the demand for well-trained professionals in relevant disciplines is in high demand. Globally, various academic institutions have established curricula offering graduate degrees in One Health. Veterinary medicine has been the leading discipline in introducing One Health–related training in its curriculum, probably because the veterinary public health concept was already established before the advent of the One Health concept. By expanding the concept development of training programs was simpler for veterinary science than for other disciplines. Selected examples in master’s programs in One Health include the Ross University School of Veterinary Medicine in the United States (Stroud et al., 2016 ), the Royal Veterinary College/London School of Hygiene and Tropical Medicine in the United Kingdom (Sikkema et al., 2016 ), and the Universitat Autonoma in Barcelona, Spain. In the United States, many universities have established joint programs combining a doctorate in veterinary medicine (DVM) with a master’s in public health (MPH), which are also mainstream One Health training programs (Stroud et al., 2016 ). One Health training opportunities in Asia and Africa have increased (McKenzie et al., 2016 ; Rwego et al., 2016 ), and many of the programs are established in partnership with foreign institutions, such as Massey University in New Zealand.
The Southeast Asia One Health University Network( comprises universities in Malaysia, Indonesia, Thailand, and Vietnam, and has supported One Health capacity building in various ways, such as providing scholarships for master’s programs or conference grants to attend One Health workshops.
Some academic institutions also offer nondegree short training programs, some of which include fieldwork. These programs can be found on any continent. Current training programs for One Health provide various educational opportunities for professionals from different disciplines. However, the training programs tend to be weighted toward veterinary schools.
Expectations for One Health Professionals
Core competencies for One Health professionals have been the subject of several conferences. Three working groups on essential competencies for One Health professionals were held in Bellagio, Italy (Rockefeller Foundation, 2011 ); Stone Mountain, United States (Stone Mountain Meeting Workgroups, 2011 ); and USAID/RESPOND (Global OHCC Working Group, 2013 ). The Rockefeller Foundation, CDC, and FAO, together with the University of Minnesota, sponsored a meeting in Rome to synthesize One Health Global Core Competencies. The core competency domains categorized were similar, despite the different approaches of each meeting (Frankson et al., 2016 ) (Figure 5 ). The resulting framework is not very different from the core competencies for Global Health as proposed by the Consortium of Universities for Global Health (Jogerst et al., 2015 ). Comparing both sets of core competencies, it could be suggested that the One Health core competencies tend to focus more on collaboration among diverse disciplines, while those for Global Health focus more on domains to provide skills. Both include systems thinking as a competency, referred to as strategic analysis in the Global Health core competencies: “Strategic analysis is the ability to use systems thinking to analyze a diverse range of complex and interrelated factors shaping health trends to formulate programs at the local, national, and international levels” (Jogerst et al., 2015 ). Global Health also placed more emphasis on skills to better understand the context, which include demographic and sociocultural aspects besides environmental ones (Figure 5 ).
The competencies cited in these publications from One Health groups (Frankson et al., 2016 ) are all relevant. However, one more domain could be proposed that is very close to the “systems thinking” mentioned in the publications and closer to the domain cited for Global Health professionals. We suggest the term “drivers analysis.” To define what types of collaboration are needed and also to create policies and regulations, it is necessary to understand the possible factors on a larger scale (not only individual risk factors), for example those related to the occurrence of a disease or an event.
This will imply a shift in paradigm, whereby the various disciplines transcend their traditional boundaries and create a new way to approach a common problem related to the animal–human–ecosystem interface. Studies on leptospirosis (Bacallao, 2014 ; Schneider, 2012 , 2015 ) have suggested drivers related to ecoregions, soil type, productive process (land use), and concentration of animals by property (Schneider, 2012 , 2015 ). Cases of leptospirosis were also related to socioeconomic factors, such as poverty, lack of sanitation, and poor housing conditions (Bacallao, 2014 ). Hamrick’s ( 2017 ) study on yellow fever cases in humans found association with geographic and environmental factors.
Figure 5. Comparison of One Health and Global Health core competency domains. One Health core competency domains re reframed based on descriptions in Frankson et al. ( 2016 ), and Global Health core competency domains re based on Jogerst et al. ( 2015 ).
Some natural drivers of transmission may not be modifiable (e.g., soil type) and others may be highly fluctuating (e.g. flooded areas); however, this understanding is critical in order to perform risk mapping to support health policies and to establish prevention and control actions. In the case of yellow fever, for example, a control program would consist of active surveillance in nonhuman primates, enhanced detection of human cases, human vaccination in risk areas and in occupational groups, and awareness campaigns in higher risk periods of the year, among others. Transdisciplinary teamwork is necessary to accomplish this. For example, a team that included a medical doctor, veterinarian, epidemiologist, and geographer would analyze the problem with a One Health approach and transform the data-driven recommendations into actions that may involve a public health professional to implement a vaccination campaign, a biologist to collect samples from nonhuman primates, and a communicator to prepare educational materials. Any individual working within the One Health approach does not need all of these skills, as they will likely be working within a team. Nonetheless, they will need to be able to analyze the problem with a holistic and integrated vision including an understanding of social and ecological contexts. Furthermore, it is important to see the team components as fully integrated, with common understanding, language, and goals—more than simply working in cross-discipline teams or sharing information among sectors.
Application of the One Health Concept in Research
A better understanding of the complexity of infectious diseases—in particular zoonotic infections or those with transmission drivers highly influenced by social, environmental, and ecological factors—has resulted in an increased recognition of the role of the One Health concept in research. Although not always stated as such, there has been a renewed interest in multilevel and interdisciplinary research methods (Pearce, 2013 ). Furthermore, the search for review articles on One Health in research (Box 7 ) found 15 articles that highlight a role for One Health in research. These articles discussed methods and applications and identified gaps and challenges for collaborative research across disciplines and sectors. Schurer et al. ( 2016 ) carried out a systematic review of literature on studies of parasites under a One Health approach. Criteria for One Health research should include humans, animals, and the environment. Only 30 unique publications involved work in all three areas, and most studies were cross-sectional in nature. Overall, fewer studies attempted to include an environmental component and there was a lack of application of appropriate methods in each component and the necessary statistical analysis to link all three components simultaneously. Likely barriers were listed that also apply to other research areas. These included communication in technical language and discipline-specific interactions, data sharing, synching research priorities, budget, and ensuring that team members from the various disciplines remained engaged during the entire study period.
Collaborative research can lead to progress in obtaining a mechanistic understanding of the processes behind pathogen spillover from animals to people. In the context of expansion in the demand for bush meat due to land use changes in some countries, wildlife researchers and ecologists are investigating hunting dynamics and characteristics of the wildlife hunted, as well as the impact on conservation and biodiversity. A One Health concept is applied in order to gain a full understanding of the entire process, from the ecology of the pathogen in the natural reservoir, through pathogen spillover, and public health impact. There is an increasing but still limited number of studies involving wildlife biologists and social and medical researchers investigating pathogens at the wildlife and human interface (Daszak, 2007 ). A concerted interdisciplinary research effort is needed to increase the prospects to predict spillovers of human disease potential (Morse, 2012 ). Collaborative research is also critical to evaluate the impact of animal interventions on improving public health and, depending on the disease, animal health as well. In a clear example, a randomized controlled trial showed that combined human and bovine chemotherapy for zoonotic schistosomiasis had a greater effect on human incidence than human treatment alone (Gray, 2009 ).
Life course epidemiology and the increasing recognition of the importance of the context in which populations live and work (Pearce, 1999 ) needs a One Health approach—in particular for diseases with complex transmission and in areas with difficulties regarding access and community engagement (Schurer et al., 2016 ). One example of this is in livestock-associated zoonoses, where there is limited understanding of exposure because it is difficult to quantify exposures, particularly in rural areas where people are exposed in occupational and domestic settings, and contacts and changes in contact are hard to pinpoint (Klous, 2016 ). A One Health approach to research on farms could engage farmers and their families and apply novel ways to measure exposure and outcomes in people and their animals simultaneously, while also assessing their cultural context, perceptions, and behaviors. In general, there is a need for greater incorporation of environmental and ecological context in understanding human disease processes and to evaluate interventions (Rabinowitz, 2013 ).
Mathematical models are an important tool for gaining insight on infection dynamics, assessing the impact of infections and diseases, and identifying and predicting the effect of interventions. The complexity of the life cycles and transmission processes of many pathogens of One Health relevance needs an integrated and multidisciplinary approach to develop, parameterize, and apply mathematical models for research and policy. This makes research projects that include mathematical modeling an optimal application of a One Health approach. However, modeling disease emergence at the animal–human interface is less common. For avian influenza, for example, despite the large amount of modeling work on human influenza transmission interventions and some in the transmission of zoonotic influenza within bird populations, there is limited work on modeling it within the interface (Dorjee, 2013 ). Formal involvement of social sciences throughout the modeling process has been less prominent but should be encouraged in order to help integrate and interpret data. In addition, social science, including qualitative methods, can improve models by providing a social context for the problem and more accurate recommendations for policymaking (Grant, 2016 ).
Although One Health is often thought of as involving mostly zoonotic infectious diseases, the concept is also applied to research on noncommunicable diseases. Pearce ( 2013 ) reviewed examples in which expertise from various disciplines and sectors can join efforts, for example, to understand how exposure during childhood to an environment containing microbes may protect against allergies and allergic asthma and investigate mechanisms and etiology of occupational cancer in meat workers, which some hypothesize could be related to bovine oncogenic retroviruses. Linking animal and human medicine research outside the laboratory setting, as in One Health studies in farms, can help to link benchwork and fieldwork and to foster innovation. Linking human and animal health has also been the effort behind groups investigating the health benefits of human and animal bonds (Bartges, 2017 ), such as an exercise program for obese persons and their dogs that resulted in weight loss and increased physical activity for both (Kushner, 2006 ).
The occurrence of outbreaks and the spread of pathogens with animal origin (e.g., SARS, avian influenza) led to the development and funding of collaborative networks and programs with a One Health approach (McKenzie, 2016 ). With the goal to assist with systemization and quality monitoring, a checklist for One Health Epidemiological Reporting of Evidence (COHERE) has been developed to guide the design and publication format of future One Health studies that truly integrate humans, animals, and environment (Davis, 2017 ). However, research funding for studies with a One Health approach has received less support and investigators face challenges to fit often complex and large studies into conventional research funding mechanisms. One Health research projects often need larger and longer studies in order to measure incidence and drivers of infection at the human–animal interface and even more so at the human–environment–animal interface. In addition, many zoonotic infections are endemic, have a high burden, and impact public health locally, but they do not have pandemic potential and therefore are less likely to be funding priorities. There is a great need for robust and truly interdisciplinary One Health research on these zoonotic diseases to develop effective, integrated, One Health disease-control policies (McKenzie, 2016 ).
Application of the One Health Concept in Advocacy and Interventions
With the increase in human cases of avian influenza H5N1 in 2006 in Asia and the risk of transmission to other parts of the world, eminent risk for pandemics and the importance of collaboration among sectors was obvious. Integrated vision was required in the planning of interventions: migratory wild birds could be in contact with and transmit influenza virus to backyard birds and other domestic animals and eventually to humans. Furthermore, a better understanding of the way people, produce, and trade interact are important for global security; for instance, the obvious potential risk of markets with high density of animals and low biosafety and the extensive production of birds and bird products with low biosecurity.
Official documents were communicated on the importance of intersectoral actions (PAHO, 2005 ; WHO, 2005 ). Preparedness plans for the Americas were developed with the participation of various sectors. Box 8 summarizes a joint publication by PAHO and the Inter-American Development Bank (IADB) on the importance of collaboration among sectors in the preparedness phase for the potential influenza H5N1 pandemic that never occurred. Many simulation exercises were done with intersectoral and multidisciplinary teams, with actors from different levels.
An influenza pandemic did occur in 2009 , but with another virus strain—influenza A (H1N1). Nonetheless, the joint preparedness plan was a good exercise in integrated vision and collaboration, which supported future work in responding to threats. As the first declaration of a Public Health Emergency of International Concern (PHEIC) since the new version of IHR was in place, during the H1N1 pandemic it was even more obvious that stronger collaboration was needed, with advocacy for the One Health approach to better prevent, detect, and respond to pandemic influenza and improve human, animal, and environmental health and well-being (Offeddu, 2016 ; Pappaionou, 2010 ; Simms, 2014 ). The importance of strengthening surveillance across sectors, sharing information, and new tools were among the key points mentioned in many publications (Capua, 2013 ; Levings, 2012 ; Schneider, 2007 ). The development of preparedness plans for response to pandemic influenza through collaboration across sectors was a good exercise in joint vision and effort—and for preparedness to fight any zoonotic disease emergency. However, in some regions, such as Africa, despite these years of influenza preparedness, many countries have built capacity to respond to influenza, but not yet to other zoonotic diseases (Bazeyo, 2013 ).
Box 8. Integration Between Health and Agriculture in the Preparedness Plans in Latin America
The objective of this study was to highlight the importance of and evaluate the integration between the health and agriculture sectors in preparedness plans in Latin American countries and to provide recommendations on how to fill the potential gaps.
The link between animal and human health with the emergence of pathogenic infectious diseases in the past 20 years, and recent outbreaks of zoonotic diseases, have increasingly drawn public attention to the fact that diseases move back and forth among species.
In 2006, avian influenza was considered an important global threat, when the avian H5N1 strain of the influenza virus was confirmed to have caused more them 250 cases and 150 deaths in humans. While the H5N1 virus had not yet been detected in the Americas, the health risks it represented were unknown, and the economic burden it might carry with it, made it important to prevent this pandemic.
The actors in the preparedness to a possible avian influenza pandemic, with emphasis on health and agriculture, were propelled to the forefront of the global health agenda, and many actors from the sectors of human and animal health and agriculture at different levels were working to prevent its spread and its appearance in humans, and a potential economic impact around the world.
The importance of intersectoral action in preventing and controlling zoonoses, avian influenza in particular, was defined within areas key to the interface between human and animal health, namely: in surveillance that is integrated across sectors; in adequate biosecurity (in this case, ensuring that animals and human food supplies linked to them are protected); in adequate biosafety (in this case, ensuring the protection of people in contact with the virus); and in adequate public information.
The important link between humans and animals in rabies has long been known. The application of combined surveillance, prevention, and control actions to minimize the spread of rabies has been widely recommended (PAHO, 2005 ; Schneider, 1996 ; WHO, 2013 ). One of most common examples is the importance of rabies vaccination coverage in dogs to prevent human cases (Schneider, 2007 ; Vigilato, 2013 ). The use of the One Health concept in preventing human cases of rabies from dogs is well documented globally (Cleveland, 2014 ; Fooks et al., 2014 ; Meslin, 2013 ; Rupprecht, 2015 ).
In addition, the role of the environment and wildlife such as foxes, raccoons, and other animals in rabies transmission to humans is well known, and strategic interventions, including wild-animal vaccination using baits, have been in use for many years (Rupprecht, 2008 ; Ver Cauteren et al., 2012 ) . Studying human rabies transmitted by hematophagous bats, Schneider ( 2009 ) suggested that there were two interrelated groups of factors—biological and nonbiological—as conditions to the occurrence of cases:
Biological factors include the presence of vampire bats, the existence of adequate shelter, the availability of food sources, and the presence of rabies virus in the area. Nonbiological factors include the type of human productive process and changing patterns in such activities, working and living conditions, access to rabies prophylaxis, and measures being implemented to control bat populations. (Schneider, 2009 )
The biological factors are the necessary conditions for maintaining the chain of transmission in the wildlife cycle of bat-transmitted rabies, whereas the structural changes triggered by nonbiological or social factors make the disease emerge, such as in deforestation and gold prospecting. The same rabies example was reviewed using the One Health operational concept (Rabinowitz, 2013 ) and in a publication about the One Health concept (Schneider, 2014 ).
Box 9. Rabies as an Example of Possible Application of the Operational Concept of One Health
Figure 6: Example of One Health vision: One Health in Latin America, rabies transmitted by vampire bat ( Desmodus rotundus ).
Vector-borne diseases transmitted by mosquitos, such as arbovirus, are currently in prominence, especially in the Americas. In 2016 , the WHO declared Zika virus and its complications as a PHEIC (WHO, 2017 ), while chikungunya was first recorded in the Americas at the end of 2013 (PAHO, 2013 ). Many dengue epidemics regularly occur around the world, and other arbovirus diseases are presenting new challenges (WHO, 2017 ). During 2016 and 2017 , yellow fever—another well-known arbovirus—re-emerged in some countries in Africa and in the Americas (PAHO, 2016 ; WHO, 2017 ). A study using the One Health approach analyzed human yellow fever cases and the geographic patterns and environmental factors were found to be associated with altitude, rainfall, temperature, and diversity of nonhuman primate hosts (Hamrick, 2017 ). Several studies advocate the use of the One Health approach in interventions for tickborne pathogens (Dantas-Torres, 2012 ; De Meneghi, 2016 ; Mencke, 2013 ; Vayssier-Taussat, 2015 ).
Application of the One Health Concept in Antimicrobial Resistance
Antimicrobial resistance (AMR) continues to grow in importance and can only be addressed with the One Health approach. According to King ( 2016 ),
over the past few decades, AMR has become a serious and growing global crisis. While the emergence of AMR is not surprising, the speed, scope, and impact of the problem certainly is. The evolution of AMR is now occurring at an alarming rate and is outpacing the development of new countermeasures capable of thwarting bacterial infections in people and animals. This situation threatens patient care, economic growth, public health, agriculture, and national security. (King, 2016 )
AMR occurs when microorganisms adapt after exposure to antimicrobial drugs and become ineffective so microorganisms are able to proliferate (WHO, 2018 ). For the last 70 years, antibiotics and antimicrobial agents have been an essential aspect of treating patients with infectious diseases. The drugs have been crucial in reducing illness and death (CDC, 2018 ). Nonetheless, the wide use of these drugs has come at a cost—the infectious organisms the antibiotics are designed to kill have adapted to them, making the drugs less effective (CDC, 2018 ).
In the United States, at least 2 million people become infected with bacteria that are resistant to antibiotics each year (CDC, 2018 ). In addition, at least 23,000 people die each year as a direct result of these infections (CDC, 2018 ). Patients with antimicrobial-resistant bacteria are often hospitalized longer, require additional laboratory tests, and require the use of more expensive drugs, which all adds up to a higher cost of health care (WHO, 2018 ). Multidrug resistance is also a growing concern for human health. Bacteria are developing resistance to not just one antimicrobial agent, but to several. Globally, approximately 480,000 individuals develop multidrug-resistant human tuberculosis each year, and drug resistance is also complicating the fight against HIV and malaria (WHO, 2018 ).
In addition to human health, animal health must be considered in any discussion on AMR. Across the globe, in both developing and developed countries, antibiotics are widely used in livestock and agriculture production (Ventola, 2015 ). The FAO estimates that 27 different antimicrobial classes are used in animals (FAO, 2017 ). An estimated 80% of antibiotics sold in the United States are used in animals, primarily to prevent infection, improve animal health, and promote growth, resulting in larger yields and a higher-quality end product (Bartlett, Gilbert, & Spellberg, 2013 ; Ventola, 2015 ). Unfortunately, the use of antimicrobials in livestock directly translates to the transmission of antimicrobials in the meat and animal products that humans consume. The transfer of antimicrobials to humans ultimately reduces the effectiveness of drugs for treating infection (Food and Drug Administration [FDA], 2018 ).
The transfer of antimicrobial-resistant bacteria to humans from farm animals was first noted more than 35 years ago, when high rates of antibiotic resistance were found in the intestinal flora and gut of farm animals and farmers. More recently, studies have used molecular detection methods to determine that resistant bacteria in farm animals reach consumers through meat products (Bartlett, Gilbert, & Spellberg, 2013 ; Ventola, 2015 ).
There is a growing concern that the routine use of antibiotics in food sources provides strong evolutionary pressure for potentially zoonotic bacteria to develop resistance to antibiotics commonly used to treat humans (Young et al., 2009 ). Pathogenic bacteria (e.g., Salmonella spp., Campylobacter spp.) and commensal bacteria (e.g., E. coli , Enterococcus spp.), including those carrying resistance genes, can be transmitted from animals to humans through food, by direct contact with animals, or through environmental sources such as contaminated water.
According to the WHO, AMR occurs when microorganisms adapt after exposure to antimicrobial drugs (WHO, 2018 ). Antimicrobial drugs in this case are ineffective and microorganisms are able to proliferate (WHO, 2018 ). AMR jeopardizes the effective prevention and treatment of infections caused by bacteria, parasites, viruses, and fungi. AMR is a growing threat to global public health and it is rising at an alarming rate throughout the world. New countermeasure drugs therapies are not being developed fast enough to suppress the bacterial infections in people and animals (King, 2016 ). This is a dangerous situation threatening several sectors of health including patient care, economic growth, public health, agriculture, and national security (King, 2016 ). AMR is a public health issue that can effectively be addressed only through collaboration and intersectoral partnership including but not limited to the human health, public health, and veterinary health sectors (Carnevale, 2016 ).
Given that One Health is at the intersection of human health and animal health, it must be taken into consideration in the response to AMR in both humans and animals. One Health advocates for a holistic and integrated approach involving all three domains (humans, animals, and environment) in order to establish effective AMR approaches (King, 2016 ). Thinking and acting in three domains rather than one may seem daunting, but a One Health approach to AMR will provide all stakeholders a more comprehensive perspective for intervention generation.
It was estimated that the economic impact of AMR would be $100 trillion (O’Neill, 2014 ). Previously, AMR had been considered a problem only in human public health, especially in relation to nosocomial infections, and had been relatively ignored in the veterinary and environmental sectors (Robinson et al., 2016 ). However, as the abuse of antimicrobials in domestic animal husbandry and its potential effects on the human population have become more widely understood (Robinson et al., 2016 ), the importance of the One Health approach has been highlighted.
AMR is recognized as a growing global threat, and so globally there are several initiatives and organizations devoted to raising awareness of AMR (Box 10 ). In addition, these groups are advocating for the safe use of antimicrobials in humans, animals, and the environment, in order to mitigate the effects of AMR.
Box 10. Global AMR Initiatives
Latin American Network for Antimicrobial Resistance Surveillance (RELAVRA)–PAHO. 2
Global Action Plan on AMR–WHO/FAO/OIE 3
The National Antimicrobial Resistance Monitoring System–FDA/USDA/CDC 4
Canadian Integrated Programme for Antimicrobial Resistance Surveillance 5
R&D Collaboration Hub established at the G20 Summit in 2017 6
Asian Network for Surveillance of Resistant Pathogens (ANSORP)
European Antimicrobial Resistance Surveillance Network (EARS-Net) 7
In 2014 , the White House announced the National Strategy for Combating Antibiotic-Resistant Bacteria (CARB), underscoring the need to address AMR (FDA, 2018 ). The FDA Center for Veterinary Medicine has developed a multipronged strategy designed to limit or reverse resistance arising from the use of antibiotics in food-producing animals while continuing to ensure the availability of safe and effective antibiotics for use in animals and humans (FDA, 2018 ).
The Global Antimicrobial Resistance Surveillance System supports a standardized approach to the collection, analysis, and sharing of data related to AMR at a global level to inform decision-making and drive local, national, and regional action (WHO, 2018 ). The Global Antibiotic Research and Development Partnership (GARDP) is a joint initiative of WHO and the Drugs for Neglected Diseases initiative (DNDi). GARDP encourages research and development through public–private partnerships. The goal of this partnership is to develop and deliver up to four new treatments through improvement of existing antibiotics and acceleration of the entry of new antibiotic drugs by 2023 (WHO, 2018 ).
The Global Health Security Agenda suggested AMR as one of the main action packages, emphasizing the importance of One Health approaches in developing national action plans. The UN high-level meeting on AMR held in 2016 clarified the importance of collaborative efforts in its declaration. The One Health approach in AMR has been actualized as a joint surveillance system (European Commission, 2017 ). The collaborative monitoring approach could provide details of the AMR epidemiological situation and subsequently support related research and legislation on prevention of abuse of antimicrobials.
In 2017 , the G20 summit highlighted the importance of international collaboration to address the growing AMR threat through implementation of national action plans using the One Health approach in each country. In addition, the Director-General of the WHO highlighted AMR as “the perfect example of the complex, multisectoral, multistakeholder challenges of the future, requiring more agile, strategic, innovative, and collaborative leadership.” As this is a One World issue, due to the globalization of the food systems, increasing movement of livestock, agricultural produce, and human travel (Robinson et al., 2016 ), AMR needs to be addressed as a global health priority.
Since One Health was first conceived in 2004 , a vast number of initiatives, publications, and training programs have been developed on all continents. Some have arisen around specific diseases or threats and others as a general call for the need to face complex problems from a more holistic perspective and collaborative effort among disciplines and sectors. The concept, scope, and implementation of One Health are still evolving. Nevertheless, all the concepts and examples presented in this article address the key message about One Health: At its core, One Health is based on the notion that humans, animals, and the environment are linked and are part of a large, complex, and interrelated system.
One of the major areas in the application of the One Health approach is in zoonotic infectious diseases such as avian influenza,. Shared data from human and animal surveillance programs are essential to identify the occurrence of strains and to predict their pandemic potential. Research groups working on many other zoonoses and vector-borne diseases with animals in their transmission cycle are also adopting a One Health approach and many other diseases could benefit from it.
More recently, the use of the One Health approach applied to the AMR threat has acquired high visibility. This is an urgent animal health and public health issue that can be addressed effectively only through collaboration and intersectoral partnership—including, but not limited to, the human health, public health, and veterinary health sectors (Carnevale, 2016 ).
Complex health problems that are rooted in multiple domains cannot be thoroughly investigated using compartmentalized research. One Health research needs to fully integrate other areas and actors not commonly involved in projects, such as ecologists, social scientists, mathematical modelers, and economists (Schurer et al., 2016 ). The involvement of other disciplines is needed for successful implementation and scaling up of public health interventions). however, in some instances, it may be too late to take advantage of the knowledge brought by the experts in other disciplines. One Health teams working together from the early phase of a research program can benefit from gaining a comprehensive view of the problems, generate new hypotheses, and innovate approaches based on transdisciplinary methods.
Box 11. United Nations Sustainable Development Goals and How They Can Be Supported by the One Health Approach
The UN’s Sustainable Development Goals agenda provides a perspective on the importance of the One Health approach to ensuring good health for all and reducing extreme poverty and hunger, among other goals. Box 11 provides an overview of possible applications in the pursuit of the 17 goals.
In the declaration of the last G20 Summit hold in Argentina in December of 2018 (G20, 2018 ), it was encouraged the activities of WHO, together with all relevant actors, to develop an action plan for implementation of health‐related aspects of SDGs by 2030 . Also was commend the progress made by the international community in developing and implementing National and Regional Action Plans on Anti‐Microbial Resistance (AMR) based on One‐Health approach and the need for further multisectoral action to reduce the spread of AMR. In the same paraph of the declaration it was mentioned the needs to continue to strengthen core capacities required by International Health Regulations (WHO IHR, 2008 ) for prevention, detection and response to public health emergencies. This health paragraph in the G20 declaration summarized several of the topics presented in this chapter, demonstrating the importance of the One Health approach for the current world.
Acknowledgments
The authors thank Paulo Marchiori Buss from FIOCRUZ for his great encouragement toward One Health vision and the writing of this article, Patricia Najera Hamrick from PAHO for the maps and previous collaboration in many joint works cited, Enrique Perez, Noemi Polo, and Theandra Madu from PAHO for comments on the Antimicrobial Resistance section.
- American Veterinary Medical Association . (2008). One Health: A new professional imperative . One Health Initiative Task Force.
- Ammann, W. (2013). One health, one planet, one future: Programme and Short Abstracts . Second GRF One Health Summit, Davos, Switzerland, November 17–20.
- Bacallao, J. , Schneider, M. C. , Najera, P. , Aldighieri, S. , Soto, A. , Marquiño, W. , et al. (2014). Socioeconomic factors and vulnerability to outbreaks of leptospirosis in Nicaragua. International Journal of Environmental Research and Public Health , 11 (8), 8301–8318.
- BAER, G. M. (1975). História natural de la rabia . Mexico: La Prensa Médica Mexicana.
- Bartges, J. , Kushner R. F. , Michel, K. E. , Sallis, R. , & Day, M. J. (2017). One Health solutions to obesity in people and their pets. Journal of Comparative Pathology , 156 (4), 326–333.
- Bartlett, J. G. , Gilbert, D. N. , & Spellberg, B. (2013). Seven ways to preserve the miracle of antibiotics. Clinical Infectious Diseases , 56 (10), 1445–1450.
- Bazeyo, W. , Mayega, R. W. , Nabukenya, I. , Keyyu, J. , Mamuya, S. , Tabu, S. J. , . . . Killewo, J. (2013). Institutional frameworks for management of epizoonotic emergencies in six countries in the Eastern Africa region: a situational analysis. East African Journal of Public Health , 10 (2), 387–396.
- Belotto, A. , Leanes, L. F. , Schneider, M. C. , Tamayo, H. , & Correa, E. (2005). Overview of rabies in the Americas. Virus Research , 111 (1), 5–12.
- British Veterinary Association . (2010). Promoting One Health . Veterinary Record , 166 , 702.
- Burns, A. , van der Mensbrugghe, D. , & Timmer, H. (2006). Evaluating the economic consequences of avian influenza .
- Coumou, D. , & Rahmstorf, S. (2012). A decade of weather extremes . Nature Climate Change , 2 , 491–496.
- Capua, I. (2013). Joining the dots on the emergence of pandemic influenza. Journal of Clinical Virology , 58 (2), 342–343.
- Carnevale, R. A. (2016). The importance of antibiotics for animal health . Cultures , 3 (1).
- Centers for Disease Control and Prevention . (2003). West Nile virus in the United States: Guidelines for surveillance, prevention, and control (3rd rev.). Fort Collins, CO: Author.
- Centers for Disease Control and Prevention . (2018, March 29). Antibiotic/antimicrobial resistance .
- CDC . (2004). The Manhattan Principles
- CDC . (2018). One Health .
- Chomel, B. B. , Belotto, A. , & Meslin, F. X. (2007). Wildlife, exotic pets, and emerging zoonoses. Emerging Infectious Diseases , 13 (1), 6–11.
- Claas, E. C. , Osterhaus, A. D. , Van Beek, R. , De Jong, J. C. , Rimmelzwaan, G. F. , Senne, D. A. , . . . Webster, R. G. (1998). Human influenza A H5N1 virus related to a highly pathogenic avian influenza virus. Lancet , 351 (9101), 472–477.
- Cardiff, R. D. , Ward, J. M. , & Barthold, S. W. (2008). One medicine---one pathology: are veterinary and human pathology prepared? Laboratory Investigation , 88 (1), 18–26.
- Cleaveland, S. , Lankester, F. , Townsend, S. , Lembo, T. , & Hampson, K. (2014). Rabies control and elimination: A test case for One Health. Veterinary Record , 175 (8), 188–193.
- Coker, R. , Rushton, J. , Mounier-Jack, S. , Karimuribo, E. , Lutumba, P. , Kambarage, D. , . . . Rweyemanu M. (2011). Towards a conceptual framework to support One-Health research for policy on emerging zoonoses. Lancet Infectious Diseases , 11 (4), 326–331.
- Comissão Nacional de Saúde Pública Veterinária . (2009). Veterinária. Revista CFMV , 48 , 9–14.
- Conselho Federal de Medicina Veterinária . (2012). Diagnostico CFMV. Revista CFMV , 57 , 8–18.
- Choi, B. C. , & Pak, A. W. (2006). Multidisciplinarity, interdisciplinarity and transdisciplinarity in health research, services, education and policy: 1. Definitions, objectives, and evidence of effectiveness . Clinical and Investigative Medicine , 29 (6), 351–364.
- Dantas-Torres, F. , Chomel, B. B. , & Otranto, D. (2012). Ticks and tick-borne diseases: A One Health perspective. Trends in Parasitology , 28 (10), 437–446.
- Daszak, P. , Epstein, J. H. , Kilpatrick, A. M. , Aguirre, A. A. , Karesh, W. B. , & Cunningham, A. A. (2007). Collaborative research approaches to the role of wildlife in zoonotic disease emergence. Current Topics in Microbiology and Immunology , 315 , 463–475.
- Davis, M. F. , Rankin, S. C. , Schurer, J. M. , Cole, S. , Conti, L. , & Rabinowitz, P. (2017). Checklist for One Health epidemiological reporting of evidence. One Health , 4 , 14–21.
- De Meneghi, D. , Stachurski, F. , & Adakal, H. (2016). Experiences in tick control by Acaricide in the traditional cattle sector in Zambia and Burkina Faso: Possible environmental and public health implications. Frontiers in Public Health , 4 (3), 239.
- Dorjee, S. , Poljak, Z. , Revie, C. W. , Bridgland, J. , McNab, B. , Leger, E. , & Sanchez, J. (2013). A review of simulation modelling approaches used for the spread of zoonotic influenza viruses in animal and human populations. Zoonoses Public Health , 60 (6), 383–411.
- European Commission . (2017). A European One Health action plan against antimicrobial resistance .
- FAO-OIE-WHO, UN System Influenza Coordination, UNICEF, & World Bank . (2008). Contributing to One World, One Health: A strategic framework for reducing risks of infectious diseases at the animal-human-ecosystems interface .
- FAO-OIE-WHO . (2010, April). Sharing responsibilities and coordinating global activities to address health risks at the animal-human-ecosystems interfaces: A tripartite concept note .
- Food and Agriculture Organization . (2008). Global programme for the prevention and control of H5N1 highly pathogenic avian influenza . Rome: Author.
- Food and Agricultural Organization . (2017). Strategic work of FAO for sustainable food and agriculture .
- Food and Agricultural Organization . (2018a). Climate change .
- Food and Agriculture Organization . (2018b). Food chain crisis .
- Food and Agriculture Organization . (2018c). How close are we to ZeroHunger?
- Food and Agriculture Organization (2018). Statistics .
- Food and Drug Administration . (2018). Antimicrobial resistance .
- Fooks, A. R. , Banyard, A. C. , Horton, D. L. , Johnson, N. , McElhinney, L. M. , & Jackson, A. C. (2014). Current status of rabies and prospects for elimination. Lancet , 384 (9951), 1389–1399.
- Fouchier, R. A. , Osterhaus, A. D. , & Brown, I. H. (2003). Animal influenza virus surveillance. Vaccine , 21 (16), 1754–1757.
- Frank, D. (2008). One world, one health, one medicine. Canadian Veterinary Journal , 49 (11), 1063–1065.
- Frankson, R. , Hueston, W. , Christian, K. , Olson, D. , Lee, M. , Valeri, L. , . . . Rubin, C. (2016). One Health core competency domains. Frontiers in Public Health , 4 , 192.
- Fraser, C. , Donnelly, C. A. , Cauchemez, S. , Hanage, W. P. , Van Kerkhove, M. D. , Hollingsworth, T. D. , . . . & WHO Rapid Pandemic Assessment Collaboration . (2009). Pandemic potential of a strain of influenza A (H1N1): Early findings. Science , 324 (5934), 1557–1561.
- G20 . (2018). G20 Leaders’ declaration Building consensus for fair and sustainable development . Argentina.
- Garcia R. (1986). Conceptos básicos para el estudio de sistemas complejos. In: Los Problemas del Conocimiento y la Perspectiva Ambiental del Desarrollo ( E. Leff , coord.) (pp. 45–71). México: Siglo XXI.
- Gibbs, E. P. J. (2014). The evolution of One Health: A decade of progress and challenges from the future . Veterinary Record , 174 (4), 85–91.
- Global OHCC Working Group . (2013). One Health core competency domains, subdomains, and competency examples . Washington, DC: United States Agency for International Development Respond Initiative.
- Global Risk Forum . (2015). One Health: The integrative health risk management perspective . Davos, Switzerland: Author.
- Grant, C. , Iacono, G. L. , Dzingirai, V. , Bett, B. , Winnebah, T. R. A. , & Atkinson, P. M. (2016). Moving interdisciplinary science forward: Integrating participatory modelling with mathematical modelling of zoonotic disease in Africa. Infectious Diseases of Poverty , 5 (17).
- Gray, D. J. , Williams, G. M. , Li, Y. , Chen, H. , Forsyth, S. J. , Li, R. S. , . . . McManus, D. P. (2009). A cluster-randomised intervention trial against Schistosoma japonicum in the Peoples’ Republic of China: Bovine and human transmission. PLoS ONE , 4 (6), e5900.
- Harvard Transdisciplinary Research in Energetics and Cancer Center (2018). Retrieved from https://www.hsph.harvard.edu/trec/about-us/definitions/ .
- Hamrick, P. N. , Aldighieri, S. , Machado, G. , Leonel, D. G. , Vilca, L. M. , Uriona, S. , & Schneider, M. C. (2017). Geographic patterns and environmental factors associated with human yellow fever presence in the Americas. PLOS Neglected Tropical Diseases , 11 (9), e0005897.
- Heymann, D. L. (2004). Control of communicable diseases manual (18th ed). Washington, DC: American Public Health Association.
- Intergovernmental Panel on Climate Change . (2007). Summary for policymakers. In S. Solomon , D. Qin , M. Manning , Z. Chen , M. Marquis , K. B. Averyt , . . . H. L. Miller (Eds.), Climate change 2007: Impacts, adaptation and vulnerability; Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change (pp. 7–22). Cambridge, U.K.: Cambridge University Press.
- Intergovernmental Panel on Climate Change . (2014). Climate change 2014 synthesis report: Summary for policymakers . Geneva, Switzerland: Author.
- Jogerst, K. , Callender, B. , Adams, V. , Evert, J. , Fields, E. , Hall, T. , . . . Wilson, L. L. (2015). Identifying interprofessional global health competencies for 21st-century health professionals. Annals of Global Health , 81 (2), 239–247.
- Jones, K. E. , Patel, N. G. , Levy, M. A. , Storeygard, A. , Balk, D. , Gittleman, J. L. , & Daszak P. (2008). Global trends in emerging infectious diseases. Nature , 451 (7181), 990–993.
- Kakkar, M. , & Abbas, S. S. (2011). One Health: Moving from concept to reality. Lancet Infectious Disease , 11 , 808.
- Kaplan, B. , Kahn, L. H. , & Monath, T. P. (2009). The brewing storm. Veterinaria Italiana , 45 (1), 9–18.
- Kim, S. H. , Song, J-H. , Chung, D. R. , Thamlikitkul, V. , Yang, Y. , Wang, H. , . . . (2012). Changing Trends in Antimicrobial Resistance and Serotypes of Streptococcus pneumoniae Isolates in Asian Countries: An Asian Network for Surveillance of Resistant Pathogens (ANSORP) Study . Antimicrobial Agents and Chemotherapy , 56 (3), 1418–1426.
- King, L. (2016). A One Health perspective: Curbing antimicrobial resistance . Cultures , 3 (1).
- King, L. J. , Anderson, L. R. , Blackmore, C. G. , Blackwell, M. J. , Lautner, E. A. , Marcus, L. C. , . . . Mahr, R. K. (2008). Executive summary of the AVMA One Health Initiative task force report. Journal of the American Veterinary Medical Association , 233 , 259–261.
- Klous, G. , Huss, A. , Heederik, D. J. J. , & Coutinho, R. A. (2016). Human-livestock contacts and their relationship to transmission of zoonotic pathogens: A systematic review of literature. One Health , 2 , 65–76.
- Kuo, H. I. , Chen, C. C. , Tseng, W. C. , Ju, L. F. , & Huang B. W. (2008). Assessing impacts of SARS and avian flu on international tourism demand to Asia. Tourism Management , 29 , 917–928.
- Kushner, R. F. , Blatner, D. J , Jewell, D. E. , & Rudloff, K. (2006). The PPET study: People and pets exercising together . Obesity (Silver Spring) , 14 (10), 1762–1770.
- Lebel, J. (2003). In_focus—Health: An Ecosystem Approach . Ottowa: International Development Research Centre.
- Levings, R. L. (2012). Emerging and exotic zoonotic disease preparedness and response in the United States: Coordination of the animal health component. Zoonoses and Public Health , 59 (s2), 80–94.
- Leung, G. M. , et al. (2004). The epidemiology of severe acute respiratory syndrome in the 2003 Hong Kong epidemic: an analysis of all 1755 patients . Annals of Internal Medicine , 141 (9), 662–673.
- King, L. (2013). Combating the triple threat: the need for a One Health Approach . Microbiology Spectrum , 1 (1).
- Magalhaes M. (2010). Por uma medicina científica e humanista: a atualidade da obra de Rudolf Virchow . Hist. cienc. saude-Manguinhos , 17 (2).
- McKenzie, J. S. , Dahal, R. , Kakkar, M. , Debnath, N. , Rahman, M. , Dorjee, S. , . . . Devleesschauwer, B. (2016). One Health research and training and government support for One Health in South Asia. Infection Ecology and Epidemiology , 6 , 33842.
- Melillo, J. M. , Richmond, T. , & Yohe, G. W. (2014). Climate change impacts in the United States: The third national climate assessment . Washington, DC: U.S. Global Change Research Program.
- Mencke, N. (2013). Future challenges for parasitology: Vector control and “One health” in Europe; The veterinary medicinal view on CVBDs such as tick borreliosis, rickettsiosis and canine leishmaniosis. Veterinary Parasitology , 195 (3), 256–271.
- Meslin, F. X. , & Briggs, D. J. (2013). Eliminating canine rabies, the principal source of human infection: What will it take? Antiviral Research , 98 (2), 291–296.
- Meehl, G. A. , Stocker, T. F. , Collins, W. D. , Friedlingstein, P. , Gaye, A. T. , Gregory, J. M. , Kitoh, A. , Knutti, R. , Murphy, J. M. , Noda, A. , Raper, S. C. B. , Watterson, I. G. , Weaver, A. J. , & Zhao, Z.-C. (2007). Global Climate Projections. In S. Solomon , D. Qin , M. Manning , Z. Chen , M. Marquis , K. B. Averyt , M. Tignor , & H. L. Miller (Eds.), Climate Change 2007: The Physical Science Basis. Contribution of Working Group I to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change . Cambridge, U.K. and New York, NY, USA: Cambridge University Press.
- Ministry of Health of Brazil . (1991). Fundação nacional de saúde . Brasília: FUNASA.
- Ministry of Health of Brazil . Nucleo de apoio á saude da familia (NASF) . .
- Mittelstrass, J. (2011). On Transdisciplinarity . Trames , 15 (65/60), 4, 329–338.
- Morse, S. S. , Mazet, J. A. , Woolhouse, M. , Parrish, C. R. , Carroll, D. , Karesh, W. B. , . . . Daszak, P. (2012). Prediction and prevention of the next pandemic zoonosis. Lancet , 380 , 1956–1965.
- Morvan, J. M. , Deubel, V. , Gounon, P. , et al. (2000). Forest ecosystems and Ebola virus. Bulletin de la Société de pathologie exotique , 93 (3), 172–175.
- Muyembe-Tamfum, J. J. , & Mulangu, S. , & Masumu, J. (2012). Ebola virus outbreaks in Africa: past and present . Onderstepoort Journal of Veterinary Research , 79 (2), 451.
- Najera Hamrick, P. , Aldighieri, S. , Machado, G. , Leonel, D. G. , Vilca, L. M. , Uriona, S. , & Schneider, M. C. (2017). Geographic patterns and environmental factors associated with human yellow fever presence in the Americas. PLOS Neglected Tropical Diseases , 11 (9), e0005897.
- Newcomb, J. (2008). Economic impact of selected infectious diseases . Cambridge, MA: Bio Economic Research Associates.
- Nickell, L. A. , Crighton, E. J. , Tracy, C. S. , Al-Enazy, H. , Bolaji, Y. , Hanjrah, S. , . . . Upshur, R. E. (2004). Psychosocial effects of SARS on hospital staff: Survey of a large tertiary care institution. Canadian Medical Association Journal , 170 (5), 793–798.
- OECD . (2017). Income inequality . Paris, France: Author.
- OECD & FAO . (2017). OECD-FAO agricultural outlook 2017–2026 .
- Offeddu, V. , Cowling, B. J. , & Peiris, J. M. (2016). Interventions in live poultry markets for the control of avian influenza: a systematic review. One Health , 2 , 55.
- O’Neill, J. (2014). Antimicrobial resistance: Tackling a crisis for the health and wealth of nations . London, U.K.: HM Government.
- Organización Panamericana de Salud . (2018). Sistema de Información Regional para la Vigilancia Epidemiológica de la Rabia (SIRVERA) .
- Tirado, M. C. , Clarke, R. , Jaykus, L. A. , & McQuatters-Gollop, A. (2010). Climate changes and food safety: A review . Food Research International , 43 , 1745–1765.
- PAHO (2005). PAHO strategic and operational plan for responding to pandemic influenza .
- Pan American Health Organization . (1991). Final report of the expert consultation on the care of persons exposed to rabies transmitted by vampire bats . Washington, DC: Author.
- Pan American Health Organization . (2005). PAHO strategic operational plan for responding to pandemic influenza . Washington, DC: Author.
- Pan American Health Organization . (2006, October). Rabia transmitida por murciélagos hematófagos en la Región Amazónica: Consulta de Expertos . Washington, DC: Author.
- Pan American Health Organization . (2008, August 6). Avian influenza and influenza pandemic preparedness . In Pan American Health Organization/World Health Organization 48th Directing Council, 60th Session of the Regional Committee . Washington, DC: Author.
- Pan American Health Organization . (2009). Elimination of neglected diseases and other poverty-related infections. In Pan American Health Organization/World Health Organization 144th Session of the Executive Committee, 60th Session of the Regional Committee . Washington, DC: Author.
- Pan American Health Organization . (2013). Epidemiological alert and updates: Chikungunya fever . Washington, DC: Author.
- Pan American Health Organization . (2016, April 22). Epidemiological alert and updates: Yellow fever . Washington, DC: Author.
- Pan American Health Organization . (2014). Reunión Interamericana a Nivel Ministerial, en Salud y Agricultura (RIMSA) .
- Pan American Health Organization . (2018). Yellow Fever: Epidemiological Alerts and Updates .
- Pappaioanou, M. , & Gramer, M. (2010). Lessons from pandemic H1N1 2009 to improve prevention, detection, and response to influenza pandemics from a One Health perspective. ILAR Journal , 51 (3), 268–280.
- Pearce, N. (1999). Epidemiology as a population science. International Journal of Epidemiology , 28 (5), S1015–1018.
- Pearce, N. , & Douwes, J. (2013). Research at the interface between human and veterinary health. Preventive Veterinary Medicine , 111 (3–4), 187–193.
- Peterson, J. , Pearce, P. F. , Ferguson, L. A. , & Langford, C. A. (2017). Understanding scoping reviews: Definition, purpose, and process. Journal of the American Association of Nurse Practitioners , 29 (1), 12–16.
- Rabinowitz, P. M. , Kock, R. , Kachani, M. , Kunkel, R. , Thomas, J. , Gilbert, J. , . . . Karesh, W. (2013). Toward proof of concept of a One Health approach to disease prediction and control. Emerging Infectious Diseases , 19 (12), e130265.
- Robinson, T. P. , Bu, D. P. , Carrique-Mas, J. , Fèvre, E. M. , Gilbert, M. , Grace, D. , . . . Woolhouse, M. E. J. (2016). Antibiotic resistance is the quintessential One Health issue. Transactions of the Royal Society of Tropical Medicine and Hygiene , 110 (7), 377–380.
- Robinson, T. P. , Wertheim, H. F. , Kakkar, M. , Kariuki, S. , Bu, D. , & Price, L. B. (2016). Animal production and antimicrobial resistance in the clinic. Lancet , 387 (10014), e1–e3.
- Rockefeller Foundation . (2011). Bellagio competency framework . Bellagio, Italy: Bellagio Center.
- Rupprecht, C. E. , Barrett, J. , Briggs, D. , Cliquet, F. , Fooks, A. R. , Lumlertdacha, B. , . . . Wandeler, A. (2008). Can rabies be eradicated? Developments in Biologicals , 131 , 95–121.
- Rupprecht, C. E. , & Kuzmin, I. V. (2015). Why we can prevent, control and possibly treat—but will not eradicate—rabies. Future Virology , 10 (5), 517–535.
- Rushton, J. , Viscarra, R. , Bleich, E. G. , & McLeod, A. (2005). Impact of avian influenza outbreaks in the poultry sectors of five South East Asian countries (Cambodia, Indonesia, Lao PDR, Thailand, Viet Nam) outbreak costs, responses and potential long term control. World’s Poultry Science Journal , 61 (3), 491–514.
- Rwego, I. B. , Babalobi, O. O. , Musotsi, P. , Nzietchueng, S. , Tiambo, C. K. , Kabasa, J. D. , . . . Pelican, K. (2016). One Health capacity building in sub-Saharan Africa. Infection Ecology & Epidemiology , 6 (1), 34032.
- Schneider, C. , Roca, A. , Falconi, C. , Belotto, A. , & Medici, A. (2007). Avian and human pandemic influenza: Addressing the need for integration between health and agriculture in the preparedness plans in Latin America . Washington, DC: Inter-American Development Bank, Department of Sustainable Development, Rural Development Unit.
- Schneider, M. C. (1996). Rabia humana transmitida por murciélago hematófago en Brasil: modelo de transmisión y acciones de control (Doctoral dissertation). Instituto Nacional de Salud Pública, Cuernavaca-México.
- Schneider, M. C. , Aldighieri, S. , Najera, P. , Galan, D. I. , Fisun, H. , Cosivi, O. , & Espinal, M. A. (2014). O conceito de “Uma Saúde” e sua aplicação. Rev CFMV , 62 , 18–21.
- Schneider, M. C. , Almeida, G. A. D. , Souza, L. M. , Morares, N. B. D. , & Diaz, R. C. (1996). Controle da raiva no Brasil de 1980 a 1990. Revista de Saúde Pública , 30 (2), 196–203.
- Schneider, M. C. , Belotto, A. , Ade, M. P. , & Hendricks, S. (2005). Eliminación de la rabia humana transmitida por perros en América Latina . Washington, DC: OPS.
- Schneider, M. C. , Belotto, A. , Adé, M. P. , Hendricks, S. , Leanes, L. F. , Rodrigues , . . . Correa, E. (2007). Current status of human rabies transmitted by dogs in Latin America. Cadernos de Saúde Pública , 23 (9), 2049–2063.
- Schneider, M. C. , Romijn, P. C. , Uieda, W. , Tamayo H. , Silva D. F. D. , Belotto, A. , . . . Leanes L. F. (2009). Rabies transmitted by vampire bats to humans: An emerging zoonotic disease in Latin America? Revista Panamericana de Salud Pública , 25 (3), 260–269.
- Schneider, M. C. , Tirado, M. C. , Rereddy, S. , Dugas, R. , Borda, M. I. , Peralta, E. A. , et al. (2012). Natural disasters and communicable diseases in the Americas: contribution of veterinary public health. VeterinariaItaliana , 48 (2), 193–218.
- Schneider, M. C. , Aguilera, X. P. , Smith, R. M. , Moynihan, M. J. , Barbosa da Silva, J. Jr , Aldighieri, S. , et al. (2011). Importance of animal/human health interface in potential Public Health Emergencies of International Concern in the Americas. Revista Panamericana de Salud Publica , 29 (5), 371–379.
- Schneider, M. C. , & Santos-Burgoa, C. (1994). Tratamiento contra la rabia humana: un poco de su historia. Rev Saude Publica . 28 (6), 454–463.
- Schneider, M. C. , Nájera, P. , Aldighieri, S. , Bacallao, J. , Soto, A. , Marquiño, W. , et al. (2012). Leptospirosis outbreaks in Nicaragua: identifying critical areas and exploring drivers for evidence-based planning. International Journal of Environmental Research and Public Health , 9(11), 3883–3910.
- Schneider, M. C. (1995). Reflexión sobre los modelos para el estudio de los brotes de rabia humana por murciélago . Cad. Saúde Pública [online], 11 (2), 291–304.
- Schneider, M. C. (1984). Saúde comunitária, saneamento e participação comunitária na melhoria da qualidade de vida: Relato de uma experiência. Arquivos de Medicina Preventiva , 6 , 47–54.
- Schneider, M. C. et al. (2015). Leptospirosis in Rio Grande do Sul, Brazil: An ecosystem approach in the animal-human interface. PLOS Neglected Tropical Diseases , 9 , e0004095.
- Schneider, M. C. , Nájera, P. , Aldighieri, S. , Bacallao, J. , Soto, A. , Marquiño, W. , et al. (2012). Leptospirosis outbreaks in Nicaragua: identifying critical areas and exploring drivers for evidence-based planning. International Journal of Environmental Research and Public Health , 9 (11), 3883–3910.
- Schultz M , Schantz P (2011). Photo quiz: Calvin W. Schwabe . Emerging Infectious Diseases , 17 (12), 2365–2367.
- Schurer, J. M. , Mosites, E. , Li, C. , Meschke, S. , & Rabinowitz, P. (2016). Community-based surveillance of zoonotic parasites in a “One Health” world: A systematic review. One Health , 2 , 166–174.
- Sikkema, R. , & Koopmans, M. (2016). One Health training and research activities in Western Europe. Infection Ecology & Epidemiology , 6 (1), 33703.
- Simms, L. , & Jeggo, M. (2014). Avian influenza from an ecohealth perspective. Ecohealth , 11 (1), 4–14.
- Souza, P. C. A. (2010). A inserção do médico veterinário na área de saúde. Revista CFMV , 16 (49), 5–7.
- Spiegel, P. B. , Le, P. , Ververs, M. T. , & Salama, P. (2007). Occurrence and overlap of natural disasters, complex emergencies and epidemics during the past decade (1995–2004) . Conflict and Health , 1 , 2.
- Stone Mountain Meeting Workgroups . (2011). Stone Mountain meeting newsletter . Atlanta, GA: Centers for Disease Control and Prevention.
- Stroud, C. , Kaplan, B. , Logan, J. E. , & Gray, G. C. (2016). One Health training, research, and outreach in North America. Infection Ecology & Epidemiology , 6 (1), 33680.
- Szyfres, B. , & Acha, P. (2003). Zoonoses and communicable diseases common to man and animals (Vol. 3, 3rd ed.). Washington, DC: Pan American Health Organization.
- Taylor, L. H. , Latham, S. M. , & Woolhouse, M. E. (2001). Risk factors for human disease emergence. Philosophical Transactions of the Royal Society of London B: Biological Sciences, 356( 1411), 983–989.
- UN Refugee Agency (2018). Figures at a glance .
- United Nations . (2015a, October 21). Transforming our world: The 2030 agenda for sustainable development .
- United Nations . (2017, June 21). World population prospects: The 2017 revision . Retrieved July 10, 2017, from https://www.un.org/development/desa/publications/world-population-prospects-the-2017-revision.html
- United Nations . Sustainable development goals Retrieved from.
- United Nations . (2015b). We can end poverty: Millennium development goals and beyond .
- United Nations . (2015c). Department of Economic and Social Affairs . World Urbanization Prospects The 2014 Revision.
- Vayssier-Taussat, M. , Cosson, J. F. , Degeilh, B. , Eloit, M. , Fontanet, A. , Moutailler, S. , . . . Zylbermann, P. (2015). How a multidisciplinary “One Health” approach can combat the tick-borne pathogen threat in Europe. Future Microbiology , 10 (5), 809–818.
- Ventola, C. L. (2015). The antibiotic resistance crisis. Part 1: Causes and threats. Pharmacy and Therapeutics , 40 (4), 277–283.
- Vercauteren, K. , Ellis, C. , Chipman, R. , DeLiberto, T. J. , Shwiff, S. , & Slate, D. (2012). Rabies in North America: A model of the One Health approach . In Frey S. N. (Ed.), Proceedings of the 14th WDM Conference .
- Vigilato, M. A. N. , Clavijo, A. , Knobl, T. , Silva, H. M. T. , Cosivi, O. , Schneider, M. C. , . . . Espinal, M. A. (2013). Progress towards eliminating canine rabies: Policies and perspectives from Latin America and the Caribbean. Philosophical Transactions of the Royal Society of London B: Biological Sciences , 368 (1623), 20120143.
- Watson, J. T. , Gayer, M. , & Connolly, M. A. (2007). Epidemics after natural disasters. Emerging Infectious Diseases , 13 (1), 1–5.
- Webster, R. G. , Peiris, M. , Chen, H. , & Guan, Y. (2006). H5N1 outbreaks and enzootic influenza. Emerging Infectious Diseases , 12 (1), 3–8.
- World Bank . (2012, November 13). New World Bank report finds 50 % increase in middle class in Latin America and the Caribbean over last decade .
- World Bank . (2016, October 2). Poverty: overview .
- World Bank . (2016, October 2). Tackling inequality vital to ending extreme poverty by 2030 .
- World Bank . (2017, April). Commodity markets outlook .
- World Bank . Gini index (World Bank estimate) .
- World Bank . Understanding poverty .
- World Bank . (2015). World Bank Group Forum Highlights the Economic Power of Tourism .
- World Health Organization . (2015). The human factor . Bulletin of the World Health Organization , 93 , 72–73.
- WHO . (2013). Statement on the third meeting of the iHR Emergency committee concerning middle East respiratory syndrome coronavirus (mERS-CoV) . Weekly Epidemiological Record , 40 .
- WHO . (2018). Global Health Observatory (GHO) data . Cholera.
- World Health Organization . (2002). Future Trends In Veterinary Public Health . Report of a WHO Study Group. WHO Technical Report Series 907. Geneva.
- World Health Organization (2017). Zika virus and complications: 2016 Public Health Emergency of International Concern .
- World Health Organization . (2014). Statement on the 1st meeting of the IHR Emergency Committee on the 2014 Ebola outbreak in West Africa .
- World Health Organization . (2004). Report of the WHO/FAO/OIE joint consultation on emerging zoonotic diseases/in collaboration with the Health Council of the Netherlands . Geneva, Switzerland: Author.
- World Health Organization . (2004). WHO interim recommendations for the protection of persons involved in the mass slaughter of animals potentially infected with highly pathogenic avian influenza viruses .
- World Health Organization . (2005). WHO global influenza preparedness plan .
- World Health Organization . (2008). International health regulations , 2005 .
- World Health Organization . (2009). Avian and other zoonotic influenza .
- World Health Organization . (2013). WHO Expert Consultation on Rabies . Geneva, Switzerland: World Health Organization.
- World Health Organization . (2016). International health regulations (2005) . Third edition 2016.
- World Health Organization . (2017). Emergencies preparedness, response: yellow fever .
- World Health Organization . (2017). Tool for the diagnosis and care of patients with suspected arboviral diseases .
- World Health Organization . (2017, March 27). Zika virus and complications: 2016 public health emergency of international concern .
- World Health Organization . (2017, July). Climate change and health .
- World Health Organization . (2018, February 15). Antimicrobial resistance .
- World Health Organization . (2005). FAO/OIE/WHO consultation on avian influenza and human health: Risk reduction measures in producing, marketing, and living with animals in Asia . Manila, Philippines: WHO Regional Office for the Western Pacific.
- Young, I. , Rajic, A. , Wilhelm, B. J. , Waddell, L. , Parker, S. , & McEwen, S. A. (2009). Comparison of the prevalence of bacterial enteropathogens, potentially zoonotic bacteria and bacterial resistance to antimicrobials in organic and conventional poultry, swine and beef production: a systematic review and meta-analysis. Epidemiology and Infection , 137 (9), 1217–1232.
- Zinsstag, J. , Schelling, E. , Waltner-Toews, D. , & Tanner, M. (2011). From “one medicine” to “one health” and systemic approaches to health and well-being . Preventive Veterinary Medicine , 101 (3–4), 148–156.
- Zanluca, C. et al. (2015). First report of autochthonous transmission of Zika virus in Brazil . Memórias do Instituto Oswaldo Cruz , 110 (4), 569–572.
1. Authors Maria Cristina Schneider and Sylvain Aldighieri are staff members of the Pan American Health Organization. The authors alone are responsible for the views expressed in this article and they do not necessarily represent the decisions or policies of the Pan American Health Organization.
2. http://www.paho.org/hq/index.php?option=com:topics&view=article&id=7&Itemid=40740&lang=en .
3. http://www.wpro.who.int/entity/drug_resistance/resources/global_action_plan_eng.pdf .
4. https://www.fda.gov/animalveterinary/safetyhealth/antimicrobialresistance/nationalantimicrobialresistancemonitoringsystem/ .
5. http://www.phac-aspc.gc.ca/cipars-picra/index-eng.php .
6. https://www.g20.org/gipfeldokumente/G20-leaders-declaration.pdf .
7. https://ecdc.europa.eu/en/about-us/partnerships-and-networks/disease-and-laboratory-networks/ears-net .
Related Articles
- Environmental Health Concerns from Unconventional Natural Gas Development
- Impacts of Climate Change on Workers’ Health and Safety
Printed from Oxford Research Encyclopedias, Global Public Health. Under the terms of the licence agreement, an individual user may print out a single article for personal use (for details see Privacy Policy and Legal Notice).
date: 27 March 2024
- Cookie Policy
- Privacy Policy
- Legal Notice
- Accessibility
- [66.249.64.20|185.80.151.41]
- 185.80.151.41
Character limit 500 /500
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Infect Ecol Epidemiol
The concept of health in One Health and some practical implications for research and education: what is One Health?
Henrik lerner.
1 Department of Health Care Sciences, Ersta Sköndal University College, Stockholm, Sweden
Charlotte Berg
2 Department of Animal Environment and Health, Swedish University of Agricultural Sciences, Skara, Sweden
From a strict biological point of view, humans are just one species among other species, albeit one with very special capacities, characteristics, and skills. Among scientists, it is generally acknowledged that we share many features with other animal species, which are certainly relevant when the concepts of health and disease are discussed. The term ‘One Health’ is used in many different contexts and by people with varying backgrounds. However, there appears to be some confusion as to what the term really means, and it is used in a wide range of contexts, often including or bordering concepts such as infection biology, contagious diseases, zoonotic infections, evolutionary medicine, comparative medicine, and translational medicine. Without claiming to present the one and only true interpretation, we will argue for a wide approach using the ‘umbrella’ depiction developed by One Health Sweden. We argue that this one should, compared to other demarcations, be more useful to science. We will also analyze the concept of health on different levels: individual, population, and ecosystem health, and describe how these levels inherently influence each other for both humans and animals. Both these choices are normative and have practical consequences for research and education, a way of reasoning which we develop further in this paper. Finally, we conclude that the choice of term for the approach might be normative in deciding which disciplines or parts of disciplines that may be included.
The perspective of One Health, at least considering practical regulations with the aim of improving or safeguarding animal and human health, has been traced back to ancient times [see ( 1 , 2 )].
One early record is from the Fourteen Rock Edicts (stones with regulations placed near roads) from the reign of King Ashoka (ca. 304 BC–232 BC) in India:
… everywhere has Beloved-of-the-Gods, King Piyadasi, made provision for two types of medical treatment: medical treatment for humans and medical treatment for animals. Wherever medical herbs suitable for humans or animals are not available, I have had them imported and grown. Wherever medical roots or fruits are not available I have had them imported and grown. Along roads I have had wells dug and trees planted for the benefit of humans and animals ( 3 ).
The theoretical foundations of such a One Health approach (a philosophy of One Health) have received limited discussion during history. Still, there are a few scientists who have actually taken time to do this kind of research and among those one could mention, for example, Rudolf Virchow (1821–1902), a physician, and Calvin W. Schwabe (1927–2006), a veterinarian ( 4 ). This paper will, however, not primarily deal with these historical discussions but rather present some modern thoughts on One Health, gathered from the ongoing discussion within philosophy of medicine and philosophy of veterinary medicine.
As a starting point, we will use the symbolic ‘umbrella’ recently developed by One Health Sweden in cooperation with the One Health Initiative Autonomous pro bono team, which tries to encompass all relevant aspects of the One Health movement ( Fig. 1 ). In this paper, we will analyze some aspects of the three center green circles of health. A number of scientific fields are present under the umbrella of One Health (see the top row circles): biology, human medicine, veterinary medicine, public health, environmental chemistry, and health economy, to mention some of the most important ones. Here, our discussion will in particular relate to public health, veterinary medicine, human medicine, and ecology. We will also discuss both research and education – issues not explicitly highlighted in the umbrella picture but considered implicit for all segments and topics of the whole picture.

The ‘One Health Umbrella’ developed by the networks ‘One Health Sweden’ and ‘One Health Initiative’ to illustrate the scope of the ‘One Health concept’. Available on www.onehealthinitiative.com and previously published in Ref. ( 5 ).
The paper will deal with these four topics:
- The demarcation of One Health (top row circles)
- The concept of health (center green circles)
Practical consequences for research
Practical consequences for education, the demarcation of one health.
For a demarcation of One Health, our initial starting point is the symbolic umbrella ( Fig. 1 ) developed by One Health Sweden in cooperation with the One Health Initiative autonomous pro bono team. According to this umbrella, One Health is a wide encompassing field where several disciplines could contribute. For a number of different examples of current definitions – if not demarcations – of One Health provided by different international organizations in the field, please see Gibbs ( 5 ).
Other terms have also been used for similar purposes. We therefore need to dwell a little on the different terms used to demarcate the area, terms that sometimes are perceived as more or less synonymous with One Health. These are:
- One medicine
- Comparative medicine
- Translational medicine
- Evolutionary medicine
Some authors consider the terms ‘One Medicine’, ‘One Health’ and ‘One World, One Health, One Medicine’ to be entirely synonymous ( 6 ). We will here argue that there might be a difference between them that is crucial.
Whereas the term One Medicine is mainly, although not exclusively, used in relation to transmissible or contagious zoonotic diseases, there are of course other health aspects that humans and other animal species have in common. In many cases, animals have been used as models for human diseases, and in some cases the knowledge about certain diseases or syndromes has also been transferred back to certain species of animals. This phenomenon is often referred to as ‘comparative medicine’. The shift from One Medicine to One Health partly reflects this mental shift to a broader perspective, covering not only infectious diseases but also general public health issues, comparative medicine, and ecology ( Fig. 1 ).
Comparative medicine is, by definition, based on the idea of comparing humans to one or more chosen animal species, or the other way around. Hence, it has limitations from a veterinary point of view, as veterinarians are also often interested in comparing different animal species with each other, that is, making comparisons that include several different species but not necessarily always including Homo sapiens . In the context of One Health the term ‘translational medicine’ is sometimes mentioned as well (see Fig. 1 ). The term is then used to illustrate how different knowledge in basic scientific disciplines can be ‘translated’ into new or improved therapies, procedures, diagnostic tools, or policies for individuals and populations. Translational medicine can certainly be regarded as a relevant aspect of One Health, the difference being that One Health stands for a truly multi- and interdisciplinary approach, that is, a much wider concept (see Fig. 1 ).
Recently, yet another term has been launched to illustrate the fact that humans and animals in many cases develop the same or similar health problems: ‘zoobiquity’ ( 7 ). The authors introducing this term argue that One Health is one-sided, as they perceive it as based on human medicine using insights of veterinary medicine, and not the other way around. We disregard this view (see Fig. 1 , where all disciplines are on par). What they argue for is a ‘new fusion of veterinary, human and evolutionary medicine’ ( 7 , p. 21). Furthermore, they claim: ‘We can treat the shared diseases of all animals, including humans, by taking a multispecies – that is, zoobiquitous – approach in our daily practices’ ( 7 , p. 309). The aim is again to apply a species-spanning approach to medicine, this time encompassing not only contagious diseases (infections) or other types of physical diseases (such as cancer or metabolic diseases) but also mental health, including anything from behavioral problems to addictions or depressions. One of the aims is nevertheless to integrate human and veterinary medicine and biology into an interdisciplinary approach.
‘Evolutionary medicine’ is an attempt to adopt biological ideas of macro- and microevolution, fitness and environment to medical thinking ( 8 ). Further, the advocates of evolutionary medicine seem to argue that one has to take longer timescales into consideration when thinking about health matters ( 8 , 9 ). Evolutionary medicine is then a framework explaining and contributing to the discussions of health as well as the environment from the field of biology. In the version presented by Natterson-Horowitz and Bowers ( 7 ), evolution is used to explain that some diseases have common ancestry and have existed for a long time (for example, cancer, which is traced back to dinosaurs). However, evolutionary medicine in other cases appears to be highly focused on humans and human health and disease, that is, with a surprisingly strict anthropological approach ( 10 , 11 ). We could therefore argue that the One Health concept is wider than zoobiquity, as there is no problem to include an evolutionary approach within the One Health concept.
As a conclusion, we argue that One Health is a wider concept than all the other concepts mentioned above (One Medicine, comparative medicine, translational medicine, zoobiquity, and evolutionary medicine). One Health could be used as an encompassing term to all these other concepts.
The concept of health
The concept of health could be defined on at least three different levels: the individual level, the group or population level, or the ecosystem level. At the first level, two concepts are used: animal health and human health. There is an ongoing discussion both in animal ethics and in philosophy of medicine on how to look at animals. The term ‘non-human animals’, referring to all animal species except Homo sapiens , has been used for decades ( 12 ) and is becoming increasingly common not only within animal rights groups but also in everyday colloquial usage and in scientific literature, a shift which certainly has normative connotations. The reason as to why separate humans from animals and not animals from animals is a highly normative issue. The animal kingdom shows a huge variety of life forms and to lump them together as a unity seems questionable ( 13 , 14 ). This seems especially true when it comes to the aspect of mental health ( 14 ). Another possibility that would be fruitful for One Health is to find a definition of health that is applicable to all animals including humans.
On the second level, the population level, at least two concepts might be used. In human medicine one can use public health. In veterinary medicine and biology, the terms herd health or population health could be used but for simplicity reasons; we here call it population health regardless of the species involved.
On the third level among several possible terms, we use ecosystem health. This gives us the scheme below:
- Animal health
- Human health
- Population health
- Public health
- Ecosystem health
We will here initiate an analysis of the concept of health at these three levels and we will start at the individual level.
The concept of human health has been thoroughly discussed within philosophy of medicine since the 1970s. Several categories of health definitions have been developed ranging from merely physiological interpretations to more holistic, including mental and/or social well-being ( 15 ).
The concept of animal health has been less discussed, although several categories of health definitions have been presented ( 14 , 16 ). These also range from physiological to more holistic. Still, a thorough theoretical discussion of these categories is merely absent (for a first attempt, see 14 ). There are also similarities in the categories of health between the two fields, which we will develop further below.
At the population level, the concept of health is more problematic. The concept herd health is mainly used in relation to monitoring, that is, focused on the surveillance of disease occurrence or patterns but can also indirectly involve aspects of safeguarding the microbiological quality of food of animal origin, that is, food safety ( 17 ). The first aspect is true also for human public health. It can, of course, be argued that both humans and one or more non-human animal species in many cases belong to the same multispecies population. This is particularly obvious in the case of zoonotic diseases where several species, including humans, are susceptible to infections by the same pathogen microorganisms. It is certainly valid also for a variety of other types of diseases, such as syndromes caused by environmental contamination with toxic agents, affecting both humans and animals that will then, from an epidemiological perspective, belong to a larger target population.
In these cases, the concept of health also bears a statistical component. Questions formulated here are: Is the disease absent, present, or is this even a common disease? Certain individuals within a group could be unhealthy even if the group as a whole is regarded as healthy. From a biosecurity point of view, health is often perceived as being a trait or characteristic of the group, or even a region or country. In this case, the term health merely reflects freedom from a specific transmissible disease. ‘Freedom from disease’, that is, a disease-free status, can be proven by properly designed sampling schemes and officially declared by a government or a public official, for example, to facilitate trade and travel. This aspect is, however, usually restricted to animals and animal products, that is, not applied in human medicine – at least not officially.
Still, a central argument both in theoretical discussions in human as well as animal health is that health as a concept belongs to the individual level. Lerner analyzes this further for animal health:
The claim made could further be interpreted in two ways. The concept needs to be defined so that [it] refers to the animal or the components of the animal. The concept needs to be defined so that [it] refers to the level of the animal (including the surroundings of the animal) and not to some systemic level above the animal. ( 14 , p. 76)
A similar discussion has been present in the conflict between animal ethics and environmental ethics when it comes to ascribing values. Animal ethicists claim that inherent value only can be ascribed to individuals (humans and some animals) but not to ecosystems. This is a central distinction between the now common terms biocentrism and ecocentrism ( 18 ). We will not further analyze this claim.
This implies that health at the population level such as population health or public health is rather a monitoring tool which is a statistical measure of health within a population rather than concepts of health.
On the third level of health, the ecosystem level, where the concept is ecosystem health, two ways of analyzing this concept seem to be present. Ecosystem health has been used either as a metaphor or as a defined concept of health. Definitions for ecosystem health do exist. One example of the latter is provided in Jakobsson ( 19 ).
According to Jakobsson ( 19 ), ecosystem health is a combined concept of ecosystem and health. Ecosystem refers to flora, fauna, other organisms, and the surrounding environment. Health ‘is an important indicator of the systems’ function’. ‘Ecosystem health is a comprehensive and integrated approach, which reflects the health of the living and non-living components of the land and marine world’. Jakobsson recognizes that this way of looking at health is far wider than the traditional one, and it shows links between human activity, ecological change, and health. ‘Health ultimately depends upon ecosystem services i.e. availability of fresh water, food, fuel, pollination etc.’
In Jakobsson's wide concept, health refers to something else than the individual or even population level. Using ecosystem health must be seen as an operational or instrumental definition (as an indicator for something). Nevertheless, the concept of ecosystem health has been widely discussed, and the perceptions of its limitations and the definition applied vary between different research groups ( 20 ), also in relation to the properties of health.
Not at all mentioned above, but nevertheless important, is plant health, which could be defined both at an individual and at population level ( 21 ). Plant health, or more specifically the fact that contaminated plants can act as vectors for diseases that affect humans, has been identified as important within One Health ( 22 ). Furthermore, some pathogens can negatively affect the health status of all three groups; plants, animals, and humans ( 22 ). Although certainly being included in the One Health concept, plant health is often perceived as a part of ecosystem health rather than as a separate entity, to clearly differentiate between the health of sentient beings, that is, humans and animals, on one side and other health concepts on the other. However, whether this demarcation may hold need further elaboration in the future.
This analysis gives us at hand that only health at the individual level is a true concept of health, and that health at the other levels are more a tool for the surveillance of processes or states among aggregated individuals.
So far, we have only discussed demarcation aspects of health. We will now turn to possible definitions of health and especially those that might be applicable to all animals, including humans. Among health definitions present, at least three categories of definitions might be useful in this sense: physiological ( 23 , 24 ), mental ( 15 ), or balance theories (for a wider discussion and other categories of health that might be applicable, see refs. [ 14 , 15 ]).
Choosing a definition of health is a normative issue. Different definitions of health cover different aspects of life. A physiological definition might be applicable to most species but will not cover all the aspects that are important for human health (e.g. mental health). As an example, let us develop the idea of health as balance.
At the individual level, theories of health referring to some kind of balance have been present from ancient times till present ( 25 ). The most famous have been health in terms of a humoral theory. This theory was abandoned during the 19th century in favor of better working theories, such as Rudolf Virchow's theory of health as vital cells ( 26 ). More modern versions are the theories of stress, where health is seen as a proper or valid response to stressors trying to restore a balance in the body. These theories exist both in human medicine ( 27 ) as well as veterinary medicine ( 28 ). At the population level, one could talk about populations that are in balance when it comes to population dynamics. In ecosystem research, it is also possible to use an idea of dynamic equilibrium (or balance) as a concept of ecosystem health.
The problem with balance theories, however, is that they are unable to explain states such as ‘I feel better than usual’ or ‘I am extremely healthy’ ( 25 ). A more thorough analysis than made here is needed to test these assumptions and this work has not yet been performed.
It should be stressed that One Health is not a research topic of its own but a truly multi- and interdisciplinary approach. To carry out interdisciplinary studies, basic disciplines will still be necessary. Furthermore, a One Health approach does not mean that all possible aspects of a certain disease or syndrome have to be included in each and every scientific study. Such an approach would be rather complicated and far from perspicuous. Instead, a more practical approach to One Health implies that the researchers are well aware of any correlations to other species, groups, or ecosystems, and are prepared to include such aspects whenever relevant. Not because they are forced to but because it will simply result in better science.
A One Health perspective might result in more holistic studies, as different perspectives meet when researchers from different backgrounds cooperate. In the case of work places where both animals and humans are involved, a One Health perspective might be an interdisciplinary approach on both humans and animals at the same time. One example is a study called PAWISE, comparing human well-being, animal welfare, human–animal interactions and company efficiency in abattoirs and animal laboratories ( 29 , 30 ). (Note here that this label of the project belongs to the opinion of the authors of this paper. No reference to the One Health perspective was made within that study.) Other examples are studies related to occupational health of farm workers who are exposed to microorganisms circulating among the farmed animals in question, and studies looking at the risk of human farm workers introducing pathogens into a herd of domestic animals.
Furthermore, a One Health approach may create a scientific environment where not only laboratory equipment or office space is shared by, for example, physicians, veterinarians, and microbiologists but where access to samples is shared more generously within the scientific community. In this way, biological samples (be it tissue, blood, fecal samples, effluent water, or anything else possibly relevant), which can be quite difficult, expensive, or ethically complicated to collect, can be used by several different research groups who may be interested in the same – or different – pathogens or toxins, but from different angles. The concept of ‘Open Access Publishing’ has become increasingly popular in a global society where resources are not necessarily evenly distributed. We hypothesize that ‘Open Access Bio Banks’ (though open not to the general public but to relevant research groups) will be an upcoming phenomenon in the era of One Health, where credit is given to the researchers colleting the samples but where the same samples can nevertheless be used for a multitude of scientific purposes. However, the ethical aspects of such data and sample sharing are delicate and must be handled with due care.
A practical graphic approach to use when one discuss interdisciplinarity is to implement an interdisciplinary matrix where one can see where in the research process one holds an interdisciplinary, a biology, a veterinary, or a human medicine perspective ( Fig. 2 ). By ticking boxes for each part of the scientific process, the interdisciplinary research group might get a better picture of which part is intradisciplinary and which part is interdisciplinary. This may also contribute to finding new ways to collaborate.

The interdisciplinary matrix. Researchers could mark for different aspects of the research process whether these aspects are interdisciplinary (shared) or stemming from a particular discipline.
The One Health approach can also be applied in a teaching context. When educating and training public health professionals to be, regardless of what university program they have been enrolled into, emphasising why these different disciplines inherently interact in practice is fundamental. In some parts of the world, it is currently possible to achieve a MSc degree or a PhD in One Health ( 5 ). There are an increasing number of One Health related textbooks aiming at university students in primarily medicine and veterinary medicine, with a main focus on zoonotic diseases, epidemics and toxicants ( 31 , 32 ). Initially, the focus of the One Health discussion appears to have been mainly on food-producing animals, but there is now an increasing interest in illuminating the importance of zoonoses also from a pet ownership perspective, where it is crucial that veterinarians, physicians, and other health care professionals recognize each other's expertise, a view that is reflected also in higher education ( 33 ).
Even more radical, there have been suggestions for a whole new education based on the philosophy of One Health. Calvin Schwabe presented a new curriculum that could be implemented as a new education at a veterinary school ( 34 , 35 ). Three areas of education were outlined: population, people, and biology ( 35 ). A more modern attempt to outline a combined education would place these areas, and students, in schools of public health ( 36 ). A risk of establishing such a new curriculum within the established disciplines is that we might experience a similar result as Natterson-Horowitz & Bowers ( 7 ) did when they analyzed One Health and instead proposed the term zoobiguity, that is, that one discipline would be using another one's knowledge, without any exchange in the opposite direction. Again, the interdisciplinary matrix ( Fig. 2 ) might be useful to avoid this risk. Schwabe's argument for placing the curriculum at a veterinary school was practical. He did not believe it to be possible within a human medical school, despite his own argument from historical studies that real progress seemed to be made when one treated both animals and humans ( 4 ). Following that line of thought, a new curriculum should rather be built up by truly interdisciplinary research departments, and not only by trying to make already existing departments collaborate.
Conclusions
To summarize this paper, one has to keep in mind that the philosophy of One Health still needs to be written. An attempt has been to show that the choice of term for the approach might be normative in deciding which disciplines or parts of disciplines may be included. Then, choosing a definition of health is also a normative task defining what aspects of health is important. This will have practical implications for both research as well as education for research.
Acknowledgements
The starting point for this paper was a presentation held by Henrik Lerner at the One Health network's yearly annual meeting held in Bålsta, Sweden, March 2013. Small passages of this paper belong to that presentation. The authors thank members of the Swedish One Health Network (Karin Artursson, Josef Järhult and Björn Olsen) and the One Health Initiative Autonomous pro bono team (Laura H Kahn, Bruce Kaplan, Lisa Conti, Thomas P Monath and Jack Woodall) for their valuable inputs toward the development of Fig. 1 in this paper.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.

- What is One Health?
- One Health Core Competencies
- Economic Benefits
- Roadmap to One Health
- About the Commission
- Mission, Vision, Goals, Outcomes
- Value of the Commission
- Strategic Plan
- Board of Directors
- Council Of Advisors
- Students for One Health (SOH) News
- Why Support the Commission?
- Current Actions of the One Health Commission
- About Sponsorship
- Individual Sponsorship
- Institutional Sponsorship
- Corporate Sponsorship
- List of Sponsors
- Sponsors' One Health Highlights
- Global Events Since 2001
- One Health Awareness Month
- One Health Day
- One Health Education Online Conference
- 2nd Int'l Who's Who in OH Webinar (2016)
- 1st Int'l Who's Who in OH Webinar (2014)
- Global One Health Happenings News Notes
- COVID-19 and One Health
- One Health News
- Narratives of One Health In Action
- Commission News
- Press Releases
- Bat Rabies Education Initiative
- One Health Education Initiatives - Overview
- One Health Education - US Initiative
- One Health Scholarships
- One Health Social Sciences Initiative
- One Health VBD Education Initiative
- JOIN the GLOBAL OH COMMUNITY LISTSERV
- One Health Education Resources
- One Health LIBRARY
- OH OPPORTUNITIES BULLETIN BOARD
- OH Resources for Public Health Educators
- OH Speaker Bank
- One Health Strategic Action Plans
- One Health Tools / Toolkits
- WHO's WHO in One Health
- Call for Papers
One Health Opportunities Bulletin Board
Welcome to the one health opportunities webpage.

This page has been created as a service for the global One Health Community for sharing and promoting One Health opportunities. It is only as complete and helpful as the information that is brought forward. The global One Health Community is encouraged to both submit and review announcements here.
In past years there have been challenges in making the world aware that the Commission is trying to help in this way, receiving announcement requests, and getting them posted on the Opportunities webpage in a timely manner. Starting in 2018, we are trying a more interactive, honor system-driven, series of online ‘One Health Community Bulletin Boards’ that will include links to ongoing One Health educational programs.
Anyone, from anywhere in the world, who has One Health-related employment, funding or educational opportunities to share with the One Health community can submit it directly to the online bulletin board. Required information will include the name and email address of the person submitting the posting, a (brief) description of the Opportunity, an online link if available, and contact information. If the words One Health are not found in the announcement title, a brief statement of how the opportunity relates to One Health is required in the description.
The One Health Commission reserves the right to remove any postings deemed inappropriate and the Commission is not responsible for accuracy. Postings do not reflect approval or promotion by the Commission. This is purely a service being provided for individuals and organizations working in the One Health space.
We hope this webpage will be helpful. If you have an opportunity to share, please submit it to the online bulletin board by clicking the ‘Submit/Post….’ link in the appropriate section and completing the submission form.
If you are seeking One Health-related employment, funding or educational opportunities, please click the ‘Review Posted….’ links in the Preferred section.

One Health Education Opportunities Map
This map is prepared in partnership with ISOHA. It is updated periodically ‘from’ communications and from opportunities submitted below. We know it is not yet complete. Help us share with the world One Health educational opportunities that you are aware of by submitting them to the appropriate Bulletin Board spreadsheet below. Click on ‘Submit/Post’.
Map Note: Where there are multiple opportunities at one location, pins may cover one another. After viewing ‘All’, click only on the type of program you are looking for to assure visualization.
postdocs, fellowships.

See More Student Opportunities Compiled by the International Student One Health Alliance (ISOHA)
To see Opportunities posted 2014-2017 see the old Opportunities pages .
Links to additional Higher Level One Health Educational Resources
A FROHUN (formerly USAID One Health Central and East Africa , OHCEA) One Health Course Modules
CABI One Health Resources
Conservation Medicine / One Health Programs
Bats, Ducks, and Pandemics: An Introduction to One Health Policy - (Free) by Laura Kahn. This interdisciplinary course covers diverse subjects such as basic epidemiology, public health, public policy, basic microbiology, food safety, and security, zoonotic diseases, sanitation and hygiene, antimicrobial resistance, environmental and ecosystem health, and the national and international organizations that oversee health, agriculture, and the environment. Disease outbreaks including Influenza, Q fever, and Ebola are discussed. While the course was developed and recorded before the COVID-19 pandemic, the concepts learned very much apply to it. This course emphasizes holistic, not siloed, approaches to health, and disease.
Global One Health Resources USAID
ONE HEALTH: Basics of multisectoral collaboration at the Human - Animal - Environment interface - WHO Health Security Learning Platform - 90 minute learning module
One Health Training Module - Food Sys tems
Adaptable training resources hosted by The Agriculture, Nutrition and Health (ANH) Academy . Includes four modules with PowerPoint slides, lesson plans and glossaries:
· Module 1: ANH Linkages – an introduction to the linkages between agriculture, nutrition & health
· Module 2: One Health – an introduction to the concept of One Health and how to apply a One Health approach to identifying and tackling food system challenges
· Module 3: Gender, Equity & Empowerment – provides an introduction to the concept of equity, gender and empowerment, and its linkages to agriculture, nutrition and health
· Module 4: Climate Change, Environment & Sustainability –an introduction to climate change and the environment, and linkages to agriculture, nutrition and health
One Health in Emerging Infectious Diseases” (1H-EID) Graduate Program (MSc, PhD, CE), Institut Pasteur, Paris, France
One Health Workforce Academies Resource Library, Competency Framework and Evaluation Toolkit
One Health Workforce Project Resources (U Minnesota / USAID)
One Health Workforce Training Resources
SouthEast Asia One Health University Network (SEAOHUN) RESPOND One Health Course Module s
SuperCourse: Epidemiology, the Internet and Global Health (free courses for the world, see Aflatoxins: In Search of One Health Solutions )
The Task Force for Global Health Field Epidemiology Training Program (FETP)
United Nations Sustainable Development Goals 2030 Flash Cards (Gaia Education) and Train the Multipliers Handbook
USAID One Health APP (Assessment for Planning and Performance) - Designed for use by countries but contains useful resources. Includes:
· One Health Tool Kits
· Global One Health Resources
· OH APP Resources
See a special (2016) overview of One Health Research, Training and Outreach around the world.
See Who's Who in One Health Academic Programs around the world.
Togami, E., Gardy, J.L., Hansen, G.R., Poste, G.H., Rizzo, D.M., Wilson, M.E. and Mazet, J.A.K., 2018. Core competencies in One Health education: what are we missing . NAM Perspectives, National Academy of Medicine, Washington, DC.
Allen-Scott LK, Buntain B, Hatfield JM, Meisser A, Thomas CJ. Academic Institutions and One Health: Building Capacity for Transdisciplinary Research Approaches to Address Complex Health Issues at the Animal-Human-Ecosystem Interface. Acad Med. 2015 Jul;90(7):866-71.
See Primary and Secondary (K-12) One Health Educational Resources freely available to the public.
For more information, questions, or assistance filling out this form please reach out to us!
The Charter of the One Health Commission is to 'Educate' and 'Create' networks to improve health outcomes and well-being of humans, animals and plants and to promote environmental resilience through a collaborative, global One Health approach.

CGIAR RESEARCH INITIATIVES
Ilri is actively engaged in several cgiar initiatives and platforms..
- Climate adaptation and mitigation
- Environmental health and biodiversity
- Gender, equality, youth and social inclusion
- Nutrition, health and food security
- Poverty reduction, livelihoods and jobs
- Research compliance
- Communication and knowledge management
- Intellectual property and legal unit
- Data and research methods
- Animal and human health
- Feed and forage development
- Livestock genetics
- Policies, institutions and livelihoods
- Sustainable livestock systems
- Impact at scale
- CGIAR research initiatives
- Capacity development
- Centre for tropical livestock genetics and health
- ILRI Genebank
- Kapiti research station
- Mazingira centre
- One health centre
- Poultry facility
- The CGIAR AMR hub
- Bioscience facility
- Genomics platform

International Land Coalition Rangelands Initiative: Making rangelands secure

ACTIVE Feb 2028
Emerging public health threats in africa’s drylands.
- Burkina Faso
- Explore our work in the countries
- ILRI in the media

Policies and Design Processes to Enable Transformation
- Pereira, Laura
- Vrettos, Chris
- Cramer, Laura K.
- Drimie, Scott
- Muiderman, Karlijn
- Schapendonk, Frans
- Stringer, Lindsay C.
- Veeger, Marieke
- Vervoort, Joost M.
- Wamukoya, George

Opportunities to quantify resilience of dairy cattle to environmental stressors in Sub-Saharan Africa
- Oloo, Richard Dooso
- Ekine-Dzivenu, Chinyere C.
- Ojango, Julie M.K.
- Gebreyohanes, Gebregziabher
- Mrode, Raphael A.
- Okeyo Mwai, Ally
- Chagunda, Mizeck G.G.
- Publications
- Journal articles
- Presentations
- Infographics
- Browse archive

First cohort of ILRI-based One Health PhD fellowships for African researchers announced
- Geoffrey Luis Njenga
The One Health Research, Education and Outreach Centre in Africa (OHRECA), which is supported by the Federal Ministry for Economic Cooperation and Development is happy to announce the first cohort of 2021 PhD fellowships whose research will address the health threats that face the continent using a One Health approach.
The six fellows who hail from East and West Africa, will be supported to pursue their PhD research on diverse subjects ranging from tackling the burden of emerging and re-emerging infectious disease, neglected zoonoses control, food safety and antimicrobial resistance.
The goal of the OHRECA fellowship is to build Africa’s indigenous capacity in One Health, support the growing web of One Health initiatives and develop pathways through which evidence can support policy and policy can be implemented resulting in measurable improvements to beneficiaries’ health and livelihoods.
‘OHRECA is an important centre for ILRI to build up the One Health capacity for African partners and countries to deal with complex health issues,’ said Hung Nguyen, co-leader of the Animal and Human Health program at ILRI. ‘I am glad to see this cohort of PhD students on board with OHRECA. They are all from Africa, working on key health issues in this continent and will be the champions in One Health in Africa,’ added Nguyen.
The three-year fellowships are aimed at early-career African scientists who want to better understand the link between humans, animals and the environment and how these links are integral to understanding disease dynamics, and the importance of interdisciplinary approaches to disease prevention and policy development. The fellows are expected to go on and help build national capacity in One Health in their own countries and institutions.
Bernard Bett, OHRECA team leader, noted that OHRECA will produce a cohort of well-trained professionals who will contribute to further development of One Health in their own countries when they complete the training. ‘The fellows will acquire practical skills and knowledge that are needed to manage complex health challenges in our region. To achieve these targets, OHRECA will use an apprenticeship model where each graduate fellows is attached to one or more senior scientists at the International Livestock Research Institute (ILRI) and other partner research institutions. They will then jointly implement health projects right from conception of research ideas to completion and dissemination of research findings.’
The OHRECA fellows will work with the ILRI Capacity Development unit, be assigned a mentor and receive training to enhance their capacity by building their soft skills, leadership, networks, mentoring skills and scientific research. The fellowship will also support existing as well as establish new summer schools for graduate fellows. In this journey as a cohort, the fellows will raise their awareness of working in teams and with colleagues from different disciplines towards solving current challenges in animal and human health in Africa.
Wellington Ekaya, the head of capacity development at ILRI, said ‘the greatest and yet most interesting challenge in One Health is the need for researchers to work, collaborate and communicate across disciplines and sectors. No education system is wired to produce these kinds of professionals. OHRECA offers a unique opportunity to produce uniquely skilled next-generation African professionals who will accelerate the use of One Health for improved health and wealth in the continent.’
OHRECA is working with African partners, advanced research institutes in Europe and elsewhere to build a robust pipeline of One Health leaders.
Get to know the 2021 OHRECA fellows

Nabwire Irene Mutambo
Nationality: Ugandan
Project: Gender and social-cultural research on emerging infectious diseases in northern Kenya

Maurice Karani
Nationality: Kenyan
Project: Quantifying the cost-effectiveness of control of rabies at the interface of livestock, human and wildlife ecosystem in Machakos

Abdoul Kader IIboudo
Nationality: Burkinabe
Project: Epidemiology of Crimean- Congo haemorrhagic fever in Burkina Faso using a One Health approach

Samuel Kahariri
Project: Strengthening integrated surveillance for rapid detection and response for zoonoses in Kenya

Maureen Kuboka
Project: Hazard assessment for food in the East African Community countries

Meseret Bekele
Nationality: Ethiopian
Project: Identify sustainable and scalable intervention to improve food safety in traditional markets in Ethiopia
You may also like

Integrating environmental and ecosystem health into One Health – choices, contexts and communities matter

Capacitating One Health in Eastern and Southern Africa – evidence shows appetite and pathways for institutional change
Dengue and chikungunya outbreaks in Burkina Faso: An opportunity to strengthen One Health institutions

Enhancing West African greenhouse gas research through expert exchange visits at ILRI's Mazingira Centre

ILRI and LUANAR: Shaping the future of veterinary service in Malawi

Winnie Ogutu and Patricia Koech: A convergence of purpose in Nairobi's meat safety

The annual meeting of the Taiwan Society for Risk Analysis explored risk analysis in Vietnam
Related publications.

Training report on mobile application of Farmvetcare for Sub-department of Animal Health and Livestock Production in Lao Cai Province
- Thang Nguyen
- Phuong Nguyen
- Sinh Dang-Xuan
- Unger, Fred
- Hung Nguyen-Viet
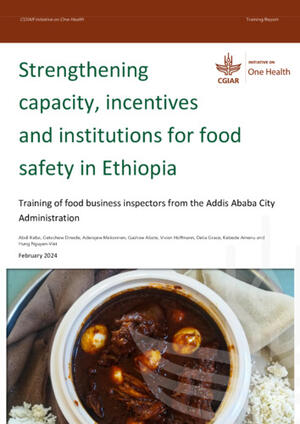
Strengthening capacity, incentives and institutions for food safety in Ethiopia: Training of food business inspectors from the Addis Ababa City Administration
- Dinede, Getachew
- Mekonnen, A.
- Abate, Gashaw Tadesse
- Hoffmann, Vivian
- Grace, Delia
- Amenu, Kebede

Incentive-based capacity building to professionalize the informal sector: the MoreMilk project
- Alonso, Silvia
Training manual for frontline animal extension service providers on antimicrobial resistance in poultry production
- Kakooza, S.
- Ayebare, D.
- Ndoboli, D.
- Mbatidde, I.
- Roesel, Kristina
- Moodley, Arshnee
Herd health management training manual for animal health care workers
- Hasahya, Emmanuel
- Doyle, Rebecca
- Ouma, Emily A.
- Dione, Michel M.
Dairy herd health and welfare management training report: Bahir Dar Zuria District, Amhara Region, Ethiopia
- Lemma, Mamusha
- Temesgen, Wudu
Related Projects

ACTIVE Dec 2025
Improving human health through sustainable value chains in human-animal-environmental interactions using ict in vietnam (ict4health).

ACTIVE Nov 2025
Capacitating one health in eastern and southern africa (cohesa).

ACTIVE Sep 2025
Agroecology and safe food system transitions in southeast asia (asset).

- Schools & departments

The MSc One Health is an innovative, transdisciplinary programme that will equip and inspire you to work across disciplines to address complex health challenges.

Why study this programme?
One Health sits at the interface between human, animal and ecosystem health. This fast-evolving subject area is well suited to preparing professionals looking to tackle the wide range of complex health challenges of the 21st Century.
One Health has become widely established as an effective approach to managing the health of humans, animals, plants and the ecosystems on which they depend. The covid-19 pandemic has demonstrated the need for this more holistic and integrated approach to health across all species, addressing the ecological, environmental, sociological and economic determinants of health.
The Royal (Dick) School of Veterinary Studies is a world leader in veterinary education, research, and clinical practice. We provide outstanding postgraduate education, drawing together the University of Edinburgh’s interdisciplinary expertise with a proven track record to deliver first-class teaching in One Health.
This programme seeks to develop the career potential for professionals and contribute to the delivery of health for all. Studying this programme will provide you with a strong theoretical foundation to pursue a career in this emerging field of study. You will acquire many transferable skills and the opportunity to develop a network of like-minded professionals.
Global Health Academy
This programme is affiliated with the University's Global Health Academy
We place a strong emphasis on developing your self-awareness as a reflective practitioner and future One Health professional. We work to achieve this through journaling, reflective writing and other awareness-based activities alongside opportunities to work with experienced coaching professionals. Students are able to explore their potential and future contribution, their values, strengths and talents.
There are many and diverse prospects for employment depending on where you want to work. Graduates will be prepared for employment in the following areas:
Industry: Clinical research organisation, pharmaceutical companies, consultancy
Research: Universities, research institutions; PhD
Education: Universities, colleges
Organisations: World Health Organization (WHO), World Organisation for Animal Health (OIE), Food and Agriculture Organization (FAO)
Government departments
Non-profit organisations
Read about what MSc One Health graduate Kelvin Momanyi went on to do after studying with us
The Programme is currently developing a blog to showcase how past and current students have benefited from the programme.
One Health and Conservation Medicine blog
Employment links
Links to online employment resources.
Queen's Careers Advisory Service
New Scientist
New Scientist Careers Website
Academic Posts
Science Careers
Inside Careers
Qualification
MSc, PGDip, PGCert, PPD
Online distance learning
The online, part-time format of our teaching is particularly suited to students with busy lives. The flexible learning environment can be adapted to suit individual needs and online study allows you to study at a location that is convenient for you.
The School has been teaching online taught postgraduate programmes since 2008 and online learning is treated as seriously as in-person. Our digital teaching platform has a dedicated e-learning team to ensure the teaching runs smoothly and students have access to support and welfare staff throughout their studies.
This programme is supported by an experienced team of a programme director, co-ordinator, administrator and course leaders and each student is provided with a personal tutor.
Key features of the programme are pre-recorded lectures that you can view at any time, study guides, textbook and journal excerpts and interactive online discussions, enabling students from a range of disciplines to bring their unique perspectives to build a community of online students.
How online learning work at University of Edinburgh
The MSc programme begins in September and runs part-time over a period of 3-6 years. The programme is delivered using a blend of online learning methods, supported by the University’s award-winning online learning environments.
Students enrolling onto standalone short courses may have start dates throughout the academic year.
The programme is structured to allow sequential progression from short courses* to Certificate, Diploma and MSc phases however, there are several earlier exit points.
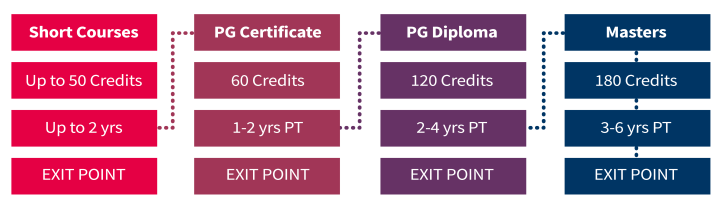
Students can opt to take time out from learning if work or family life are impacted too much. It is also possible to pay per course** to help spread the cost of your studies.
* also referred to as the Postgraduate Professional Development (PPD) scheme
** The University uses the terminology 'course', and sometimes 'module', to refer to the individual components that make up a degree programme
Certificate and Diploma
The Certificate phase comprises four compulsory courses from within the programme (see Content tab).
The Diploma phase comprises a selection of courses totaling 60 credits from within the programme (see Content tab).
Masters (MSc)
The dissertation element gives students the opportunity to further develop scientific skills and apply scientific theory, in a less structured learning environment.
The dissertation is designed to advance your understanding of the processes and planning involved in undertaking research and to develop your scientific written communication skills, research ethics, statistics and the principle of good research practice.
This is a self-directed course but you are supported by an allocated subject-specific expert supervisor, statistician and experienced researchers from within the programme team. You are also encouraged, where appropriate, to work closely with senior staff at your home institution.
20 credit courses (elsewhere often called ‘modules’) are delivered in 2 blocks of 5 weeks of study plus 1 week of independent study and reflection time in between.
10 credit courses are delivered over a period of 5 weeks. The majority of the lecture material is pre-recorded so that it can be watched at any time.
Each 10 credits represents 100 hours of study time and a time commitment of 20hrs per week.
Certificate
Students are strongly recommended to take the Innovative Approaches to Health Challenges Across Disciplines course.
* This course is compulsory for students progressing to the dissertation.
The dissertation may be submitted in either in a traditional dissertation format (10-14,000 words) or in the format of a scientific publication. The assessment for this will be 80% Dissertation, 10% Reflective Account and 10% Presentation.
Supervision for this element of the programme will be provided by existing research staff and subject experts currently employed by the University of Edinburgh. Candidates will also be encouraged, where appropriate, to work closely with senior staff at their home institutions.
Students will be required to submit a proposal that demonstrates an appropriate level of critical analysis, academic knowledge and reflection, depending on the choice made, prior to progression to the Master’s year.
Credit-bearing standalone short courses
The Postgraduate Professional Development (PPD) scheme is aimed at working professionals who want to advance their knowledge through postgraduate-level learning, without the time, or financial commitment, of a full award.
You may take a maximum of 50 credits worth of courses over two years and gain a University of Edinburgh postgraduate award of academic credit.
You can also choose to continue your studies after one year and put credits towards a postgraduate Certificate, Diploma or full Masters degree. Any time spent taking courses through the PPD scheme will be deducted from the amount of time you have left to complete the higher award.
To view the short courses available within the PPD scheme and details on how to apply, please visit the credit-bearing standalone short courses page.
Testimonials
More testimonials from One Health students
Teaching team
We have a number of internationally recognised experts in their field contributing to the teaching of many aspects of the programme.
Entry requirements
Graduates with a UK 2:1 honours degree, or its international equivalent, in a relevant subject area such as medicine, biomedical science, veterinary medicine, biological or life science, environmental or social science, ecosystem health or economics.
We may also consider candidates below a 2:1 or a degree in another discipline where they can demonstrate significant relevant experience. Candidates are encouraged to contact the Programme Team for further guidance.
To discuss your eligibility for the programme, please contact [email protected]
English language requirements
If English is not your first language, we will also need to see evidence of your English language proficiency before we can offer you a place.
English language requirements
Fees and funding
Tuition fees
Please note that you can pay for the programme on a course (module) basis. Each course is 20 credits and the dissertation year is equivalent to 60 credits.
Tuition fees for online learning
Tuition fee discount for some of our former graduates
Alternative Guide to Postgraduate Funding
The University of Edinburgh subscribes to a funding database specifically for those looking for funding to support postgraduate studies. The guide contains a huge database of funding opportunities, comprehensive guidance and tools to help you prepare a winning grant application including.
The Alternative Guide to Postgraduate Funding Online
Scholarship information
It is recommended that you conduct your own research on this, but you can refer to the University Scholarship website to view suggestions on Scholarships.
Online distance learning scholarships
Mastercard Foundation Scholars Program
There are up to 15 Mastercard Scholars Foundation scholarships available for postgraduate study for selected programmes (including MSc One Health) at the University of Edinburgh.
Mastercard Foundation Scholars Program - information for candidates
ITA Scotland
Get up to £200 towards the cost of a training course with an SDS Individual Training Account (ITA).
You could use the money to build the skills you need for a job. Or get some training to take your career to the next level. Whatever you want to do, there is a wide range of ITA approved courses on offer.
ITA Scotland
UK government postgraduate loans
If you are planning to study with us, you could be eligible for a postgraduate loan towards your fees. From this year, online programmes are also eligible for this funding (please note, restrictions apply)
This funding is available for UK nationals, those with settled status, and in some cases, EU nationals not resident in the UK.
Learn more about postgraduate loans and submit your application
Find out more and apply
Online application form
Applications must be submitted through the University’s online application service, EUCLID. Offers cannot be made without a fully completed online application.
Apply for this degree
Register interest
If you would like more information about this programme, please complete a webform to register your interest.
Register interest
Poster download
Download a copy of the programme poster
Equality and Diversity
The University has a strong and long-standing commitment to equality, diversity and inclusion and to promoting a positive culture which celebrates difference, challenges prejudice and ensures fairness.
Find out more
You might also be interested in:
Global Food Security and Nutrition
Food Safety
- Dean’s Welcome
- Advisory Council
- STAR Committee
- Leadership Team
- Strategic Plan
- Commitment to Diversity, Equity, and Inclusion
- Graduate Students
- Affiliate Faculty
- Emeriti Faculty
- Visiting Scholars
- CFWE Employment
- Celebrating 75 Years of Forestry & Wildlife Sciences
- Current News
- CFWE Newsletter
- Newsletter Archive
- Events Calendar
- Update Your Information
- FWE Building Room Directory
- CFWE Facilities
- Photo Gallery
- Virtual Tour
- Sustainable Development Goals (SDGs)
- Environmental Conservation and Management
- Geospatial and Environmental Informatics
- Natural Resources Management
- Parks and Recreation Management
- Sustainable Biomaterials and Packaging
- Wildlife Ecology and Management
- Wildlife Enterprise Management
- Wildlife Sciences Pre-Vet
- Explore CFWE Majors
- Graduate Degrees
- Online Graduate Programs
- Pathways to Auburn
- Cooperative Transfer Programs
- Path to the Plains Concurrent Enrollment Program
- Undergraduate Student Services
- Academic Advising & Resources
- Transfer Student Assistance
- Graduate Student Services
- Faculty Directory
- Request Information
- Dean’s List
- Student Life
- Student News
- Diversity, Equity, and Inclusion Initiatives
- Student Internship Experiences
- Student Testimonials
- Forest, Environment and Wildlife Leadership (FEWL) Academy
- Summer Practicum
- Study Abroad
- Clubs and Organizations
- Undergraduate Research Positions
- CFWE Volunteer Opportunities
- Careers & Internships
- Wildlife Sciences
- Ecosystems & Society
- Research Assistantships and Other Positions
- Undergraduate Research Opportunities
- Faculty Resources & Support
- Center for Natural Resources Management on Military Lands
- Cooperative Ecosystem Studies Unit (CESU)
- The McCrary Institute
- Research Centers & Cooperatives
- Faculty & Research Staff
- Journal Editors
- Research News
- Kreher Preserve & Nature Center
- Solon Dixon Forestry Education Center
- Crooked Oaks
- Facilities & Outdoor Classrooms
- Continuing Education
- Seminars & Workshops
- Outreach Fact Sheet
- Outreach News
- CFWE Extension Directory
- Statewide Extension Directory
- Forestry, Wildlife, and Natural Resources Extension Blog
- CFWE Extension Impact Report
- Extension Program Calendar
- W. Kelly Mosley Environmental Awards
- Extension FAQ
- Contact CFWE Extension
- Alumni & Friends News
- Outstanding Alumni
- Philanthropy in Action
- Update Your Profile
- Invest in the CFWE
- Giving Opportunities
- War Eagle Woods
- Woodlands & Wildlife Society
- Compass Circle Young Alumni Giving Society
- Tigers United
- Endowed Professorships
- Undergraduate Student Awards and Scholarships
- Graduate Student Awards and Fellowships
- Career and Internship Opportunities
- Current Students
- Future Students
- Request Info
Home » Online Professional Graduate Certificate Programs » One-Health
Latin American teacher with a group of young students at an animal farm feeding the goats – lifestyle concepts
The One-Health concept is based on the premise that health-related interactions among people, animals, and the environment profoundly influence disease risk, transmission, and prediction efforts. There are estimates that 60% and 75% of human infectious diseases and emerging human diseases, respectively, have their source in domestic or wild animals ( http://www.oie.int/for-the-media/onehealth ). These are called zoonotic diseases and include rabies, West Nile virus, Rift Valley fever, and brucellosis, among others. In some cases, animal health can serve as a warning for human disease transmission, as demonstrated by the West Nile virus, or where mortality of West Nile virus-infected birds may trigger awareness of human risks.
While human-animal-environmental interactions have long been recognized as being important, some powerful drivers of change are increasingly causing volatility among people, animals, and environmental linkages. These drivers include climate change, population growth, land use/cover changes, and alterations in disease vector ecology. According to the CDC, climate change and other environmental factors have caused many diseases to emerge and re-emerge. Consequently, it is crucial to educate and inform people to the greatest extent possible regarding the One-Health concept and those factors that continuously cause variation in the interacting processes among people, animals, and the environment.
Key Learning Outcomes
The Auburn University One-Health online graduate program clearly represents an area of crucial need and importance within our state, nationally, and globally.
Students completing the graduate certificate program will be:
- Recognized for their education and new skill sets and be afforded new professional opportunities in the public and private sectors
- Knowledgeable regarding relationships between One-Health concepts and many other professions such as urban planning, engineering, natural resource management, etc.
- Competent in the fundamentals of One-Health concepts
- Able to articulate to audiences linkages between One-Health concepts and challenging technical problems related to the environment
The Auburn One-Health certificate program utilizes expertise from the College of Forestry, Wildlife and Environment, the College of Veterinary Medicine, and the School of Public Health at the University of Alabama at Birmingham.
Requirements
To obtain a One-Health graduate certificate from Auburn University, students must complete fifteen (15) credit hours of online coursework.
*Tentative; contact CFWE or course schedule for confirmation
To participate in the One-Health certificate program, students must apply to Auburn University ( http://graduate.auburn.edu/ ). Graduate Record Examination (GRE) scores are not required.
Entrance to the certificate program and AU Graduate School requires a 2.75 GPA. However, exceptions can be made if sufficient justification for the exception is provided to the CFWE Graduate Program Office.
Graduate certificate applicants must submit the online application to be admitted as a non-degree student, pay the online application fee ($60 or $70 domestic vs. international, respectively), and submit transcripts. They must submit an official transcript for the highest degree they currently hold. International applicants must also submit an English proficiency score.
Students enrolled in our program may elect to apply to the UAB School of Public Health as a non-degree student at a fee of $40, a status which will allow them to take HCOP 601Q Health Economics (link to syllabus). The UAB credit can be transferred to Auburn University, where the credit will count toward the completion of the certificate.
Students may enroll three times yearly to begin their coursework in the spring, summer, or fall semesters. All application materials must be received no later than 45 days before the first day of class of the semester. For deadlines and other details, visit http://graduate.auburn.edu/prospective-students/general-admission-requirements/ .
The One Health graduate certificate program requires 15 credit hours at $546 per credit hour for Auburn University courses. UAB course fees can be found online at https://www.uab.edu/cost-aid/cost/detailed-tuition-fees#graduate . Please be aware that students pursuing graduate certificates are not eligible for financial aid.
Need help getting started?
For guidance regarding curriculum choices, admissions policies, and deadlines, please contact Dr. Jessica Daniel at [email protected] or (334) 844-1077 or submit a request for information about our online programs.
Specific questions concerning the One-Health certificate and courses can be addressed to Dr. Aniruddha Belsare at [email protected] or (334) 844-1037).
Now Accepting Applications
Through distance education and online learning, our expert faculty prepare students to address complex natural resources-related topics and issues that are highly impactful to our society and environment. Our curriculum is convenient and flexible for students of diverse academic backgrounds who wish to advance professionally.
Quick Facts
- Earn a certificate in less than 3 years
- Only 15 credit hours required
- Credit may be applied to Master’s of Natural Resources Graduate Degree ( MNR Non-thesis )
- No GRE required for enrollment
- Enrollment open spring, summer and fall!
Quick Links
- About One-Health
- One Health Graduate Certificate Brochure
- Graduate Study
- Auburn Graduate School
- Student Resources
- Sustainable Development Goal 3: Good Health & Well-being
Link to School of Forestry and Wildlife Sciences Facebook page

Link to School of Forestry and Wildlife Sciences Twitter profile

Link to School of Forestry and Wildlife Sciences Instagram profile

Link to School of Forestry and Wildlife Sciences Linked In page

Link to School of Forestry and Wildlife Sciences Flicker page

Link to School of Forestry and Wildlife Sciences YouTube channel

Link to email School of Forestry and Wildlife Sciences
Working with Nature for Society’s Well Being
- CFWE Intranet
- Alabama Cooperative Extension System
- Alabama Cooperative Experiment Station
- Alabama Cooperative Fish and Wildlife Research Unit
- Auburn University
- Office of Development
- Office of Communications & Marketing
- People Finder
Website Feedback Webmaster Privacy Copyright Accessibility AUAccess
Page Last Updated: Feb 26, 2024 @ 2:59 pm
Dr. Janaki R.R. Alavalapati, Dean
School of Forestry & Wildlife Sciences Auburn University 3301 Forestry and Wildlife Building 602 Duncan Drive Auburn, Alabama 36849-3418
Phone: 334-844-1004 Email: [email protected]
Dear Auburn Family,
It is my pleasure to welcome you to the 75th Anniversary Celebration of the School of Forestry and Wildlife Sciences at Auburn University!
Thank you for visiting our website in observance of this important anniversary. We hope you’ll enjoy learning about the history of Auburn’s forestry and wildlife sciences programs within the interactive timeline and photo archive of the School’s significant milestones and achievements.
As you’ll discover, forestry first became a stand-alone program in what was then known as the School of Agriculture in 1946. Since that time, Auburn has produced thousands of well-qualified graduates, provided citizens with science-based solutions to improve their quality of life and developed solutions to some of society’s most complex natural resource challenges.
In honor of this occasion, the School has published Arthur L. Slotkin’s 75 Years of Forestry and Wildlife Sciences at Auburn University . Through personal interviews and in-depth research, Mr. Slotkin has created a detailed chronology that will take readers on a journey through time to discover how Auburn’s forestry and wildlife programs evolved to become the present-day School of Forestry and Wildlife Sciences.
The School will commemorate its 75th anniversary from March 2021 through 2022. Throughout the year, we will invite our faculty, students, alumni, and friends to join us in celebrating the School’s rich history of teaching, research, and extension through a series of virtual and in-person *events, including:
- 7 for 75 Virtual Speaker Series: Accomplished alumni and industry leaders representing our diverse programs will discuss a wide range of topics from land management to current and future technology to stakeholder engagement.
- Dean’s Q & A and Alumni Breakout Sessions: Deans past and present will share their personal stories of the major milestones that occurred during their tenure. As part of these virtual roundtable discussions, we will host breakout sessions for alumni to socialize and reminisce about their time at Auburn.
- 75th Anniversary Events: Faculty, staff, and students will celebrate the anniversary with alumni and friends during the School’s annual events, including the student awards banquet, graduate research symposium, and alumni homecoming barbeque.
- 75th Anniversary Gala: The anniversary celebrations will conclude with a signature gala in the spring of 2022 at the Gogue Performing Arts Center. To feature a distinguished keynote speaker, guests will also enjoy dinner, musical entertainment, a complimentary book signing with Arthur Slotkin, and a short documentary of the 75-year history of forestry and wildlife sciences at Auburn University.
In addition to this exciting calendar of events, we invite our alumni to share their Auburn experience by submitting stories, photos, and other memorabilia to our website that will be shared online with fellow alumni during the anniversary celebration year.
On behalf of the faculty and staff, we look forward to commemorating this milestone anniversary with you in honor of 75 years of forestry and wildlife Sciences at Auburn University!
Events are subject to change in compliance with Auburn University’s COVID-19 safety protocols.
About the Program
The Summer Program in Epidemiology aims to provide undergraduates with a comprehensive understanding of the vital link between mathematics, quantitative methods, and public health, helping them realize their interest in pursuing Epidemiology at a career or academic level. Through interactive coursework and hands-on experiences, participants develop analytical skills, track trends, identify risk factors, and devise effective public health strategies. Held in *Boston over six weeks, the program emphasizes quantitative proficiency and practical application through data analysis and strategy development. By gaining a solid understanding of statistical methods and epidemiological principles, interns are equipped for meaningful contributions to public health research, policy-making, and professional roles.
* Location may be subject to change at the discretion of The Department of Epidemiology
During the program, interns will:
- Attend Introduction to Epidemiology and Biostatistics courses.
- Participate in faculty roundtables.
- Engage in writing-intensive courses.
- Take part in an R boot camp.
- Attend ODI workshops.
- Receive support from alumni mentors.
- Collaborate on research projects with faculty and postdocs.
- Deliver presentations to faculty, staff, current students, and fellow interns to share the conclusions of their research projects.
- Network with Harvard faculty and community members.
- Cultivate a peer social network through active engagement in various events and gatherings.
News from the School

Bethany Kotlar, PhD '24, studies how children fare when they're born to incarcerated mothers

Soccer, truffles, and exclamation points: Dean Baccarelli shares his story

Health care transformation in Africa highlighted at conference

COVID, four years in

- Seeking Patient Care?
- Faculty Directory
- Manuel J Arana Rosainz

Manuel J. Arana Rosainz, M.D., Ph.D.
Department: Pathology and Laboratory Medicine
Education & Training
2002: universidad de ciencias médicas de la habana (higher institute of medical sciences of havana), havana, cuba, 1983: universidad de ciencias médicas de la habana (higher institute of medical sciences of havana), havana, cuba, post graduate training, 2021: cedars-sinai medical center, los angeles, ca, 2020: university of texas health science center at houston mcgovern medical school, houston, tx, licensures and certifications, state of florida, national institute of hematology and immunology, national hospital, honors & awards, no result found, teaching interests, research interests, publications.

- Global navigation
- Site navigation
School of Public Health – Bloomington Bulletin 2024-2025
- IU Bulletins
- Undergraduate
- Policies & Procedures
- Departments & Centers
- Organizations & Services
- Online Graduate Certificate in Safety Management
- Graduate Certificates
- Public Health Certificate
- Addiction Intervention Certificate
- Environmental Health Major
- Epidemiology Major
- Biostatistics Major
- Joint Graduate Degrees
- Master of Public Health Degree (M.P.H.), Public Health Administration Major
- Master of Public Health Degree (M.P.H.), Environmental Health Major
- Master of Public Health Degree (M.P.H.), Epidemiology Major (Note: courses offered online are synchronous)
- Master of Science in Kinesiology Degree (M.S.K.), Kinesiology Major
- Online Master of Public Health Degree (M.P.H.), Environmental Health Major
- Online Master of Public Health Degree (M.P.H.), Epidemiology Major (Note: Courses offered online are synchronous)
- Online Master of Public Health Degree (M.P.H.), Public Health Administration Major
- Public Health Administration Major(MPH)- Health Behavior Major PhD
- MSAHS Nutrition MS – Dietetics BS
- Accelerated Programs
- Advising & Registration
- Financial Aid, Awards & Scholarships
Graduate Academic Programs
Master's degree programs, master of science (m.s.) in environmental and occupational health degree, description of program, degree requirements, special opportunities.
The Master of Science (M.S.) in Environmental and Occupational Health is a research-focused degree, designed to be completed in two years, with either a thesis or a graduate research project that is typically completed during the final year in the program. The M.S. in Environmental and Occupational Health degree will provide graduate students with training in important analytic and technical skills and cutting-edge research methods in environmental and occupational health. Students who graduate from this program will be prepared to enter the job market, where there are a wide range of opportunities in environmental health and related fields. Furthermore, this degree will prepare students to enter advanced graduate programs focused on research in environmental, occupational and other public health disciplines (PhD, DrPH), as well as other health-related academic and professional disciplines (MD, DO, DVM).
A minimum of 30 credit hours is required to complete this degree program. A minimum 3.0 cumulative grade point average (GPA) is required for graduation. A minimum grade of C is required in each course.
Public Health Foundations Requirement (0 credits) All new master's degree students must complete the Public Health Foundations online course no later than the end of their first semester of graduate study. Complete details and registration information for this course can be found iu.instructure.com/enroll/MNG3L6
Environmental and Occupational Health Core: (15 credits)
Complete each of the following courses (12 cr.):
- SPH-E 651 Epidemiology (3 cr.)
- SPH-Q 501 Introduction to Statistics in Public Health (or equivalent)
- SPH-V 541 Environmental Health (3 cr.)
- SPH-V 692 Research in Environmental Health (3 cr.)
Environmental and Occupational Health Electives: (9 credits)
Complete 9 credits from the following courses (15 cr.):
- SPH-V 542 Principles of Toxicology (3 cr.)
- SPH-V 545 Exposure Assessment and Control (3 cr.)
- SPH-V 546 Risk Assessment, Policy, and Toxic Regulations (3 cr.)
- SPH-V 522 Global Environmental Health Issues (3 cr.)
- SPH-V 548 Environmental and Occupational Epidemiology (3 cr.)
- SPH-V 549 Public Health Biology (3 cr.)
- SPH-V 532 Foundations of Global Environmental Health (3 cr.)
- SPH-V 533 Human Health Assessment Methods in Global Settings (3 cr.)
- SPH-V 633 Field Research Methods in Global Environmental Health (3 cr.)
- SPH-V 635 Interdisciplinary Field Research in Global Environmental Health (3 cr.)
- SPH-V 691 Readings in Environmental Health
- SPH-V 5__ Other advisor approved Environmental and Occupational Health course at the 500-level or higher (3 cr.)
Required Research Option: (3-6 credits)
Complete one of the following courses:
- SPH-V 599 Masters Thesis (6 cr.)
OR
- SPH-V 598 Graduate Research Project in Environmental and Occupational Health (3 cr.)
Multidisciplinary Electives: (3-6 credits)
Complete between 3 and 6 credits from the following courses, or from the Environmental and Occupational Health Electives above in addition to the required 9 credits above:
- SPH-E 653 Chronic Disease Epidemiology (3 cr.)
- SPH-E 655 Infectious Disease Epidemiology (3 cr.)
- SPH-E 658 Intermediate Epidemiology (3 cr.)
- SPH-E 659 Intermediate Epidemiological Methods (3 cr.)
- SPH-Q 502 Introduction to Statistics in Public Health (3 cr.)
- SPH-Q 602 Multivariate Statistical Analysis (3 cr.)
- SPH-V 625 Integrated Models for Environmental Health Research (3 cr.)
- SPH-V 650 Special Topics in Environmental Health (3 cr.)
- SPEA-E 536 Environmental Chemistry (3 cr.)
- SPEA-E 539 Aquatic Chemistry (3 cr.)
- SPEA-E 542 Hazardous Materials (3 cr.)
- SPEA-E 543 Environmental Management (3 cr.)
- SPEA-E 552 Environmental Engineering (3 cr.)
- SPEA-E 560 Environmental Risk Analysis (3 cr.)
- SPEA-E 562 Solid and Hazardous Waste Management (3 cr.)
- SPEA-E 564 Organic Pollutant Environmental Chemicals and Fate (3 cr.)
- BIOC-B 501 Integrated Biochemistry (3 cr.)
- BIOC-B 530 Macromolecular Structure/Function (1.5 cr.)
- BIOC-B 531 Biomolecular Analysis/Interact (1.5 cr.)
- BIOC-B 580 Intro to Biochemical Research (3 cr.)
- BIOL-M 550 Microbiology (3 cr.)
- EAS-G 576 Climate Change Science (3 cr.)
- GEOG-G 535 Environmental Remote Sensing (3 cr.)
- Others courses as approved by the faculty advisor (3 cr.)
The Department of Environmental and Occupational Health is committed to promoting and protecting the health and well-being of human populations. Our department is comprised of diverse faculty who are engaged in multidisciplinary research, teaching and service in Indiana and globally. The research of faculty within the Department of Environmental and Occupational Health is broadly focused on understanding how environmental risks impact human health. We seek to provide students with the necessary skills and knowledge in toxicology, occupational health, and global environmental health to solve environmental health challenges locally and globally.
The M.S. in Environmental and Occupational Health degree will serve both a national and a state labor market need. The job outlook for environmental health scientists and specialists is strong. The Bureau of Labor Statistics estimates an approximate 11% increase in employment of environmental scientists and specialists from 2014 to 2024 ( bls.gov/ooh/life-physical-and-social-science/environmental-scientists-and-specialists.htm ). The Indiana Department of Workforce Development (DWD) estimates an 17.7% increase in jobs for environmental scientists and specialists, and a 16.4% increase in jobs for environmental science and protection technicians between now and 2024.
Students who graduate with an M.S. in Environmental and Occupational Health degree will be prepared to enter the job market where there are a wide range of opportunities. Individuals holding an M.S. in Environmental and Occupational Health degree are employed in virtually every sector of the workforce, including:
- State and local health departments, for example the Indiana State Health Department or Marion County Health Department
- Federal government agencies such as the Environmental Protection Agency, National Institutes of Health, Department of Health and Human Services, and the Centers for Disease Control and Prevention
- Pharmaceutical and chemical companies such as Cook, Bristol-Myers Squibb, Chevron Corporation, Corteva Agroscience, Dupont, and Eli Lilly
- International agencies and organizations such as the World Health Organization, Pan American Health Organization, United Nations Environment Programme, and World Bank
- Consulting firms
- National and global organizations such as the Bill and Melinda Gates Foundation, Kaiser Foundation, CARE, Save the Children, UNICEF, and the World Health Organization
- Academia, including medical centers and biomedical research laboratories
The research-intensive M.S. in Environmental and Occupational Health prepares students to enter advanced graduate programs focused on research in environmental, occupational, and other public health disciplines, (Ph.D., Dr.P.H.), environmental science, biology, and health-related professions.
Academic Bulletins
- Indiana University
- IU Bloomington
Copyright © 2024 The Trustees of Indiana University , Copyright Complaints

“Opposite of a Hack”: Bodybuilder With PhD in Sports Physiology Bashes Rich Piana’s Viral 8-Hour Arm Workout for All the Right Reasons
Late bodybuilding icon Rich Piana earned equal measures of fame and notoriety. Although the bodybuilder passed away in 2017, one of his particular workouts has served along with his legacy. Even today’s fitness influencers like the Tren Twins have tried Rich Piana’s eight-hour arm workout. However, exercise scientist Dr. Mike Israetel didn’t seem impressed with the viral workout.
From the very beginning of the clip, Israetel was sarcastic about the clip where Rich Piana shared the particulars of the eight-hour arm workout. The late bodybuilder said that the “deep dark secret” to his massive arms was the eight-hour arm workout. However, Israetel answered if it was a “deep, dark secret,” Rich Piana wouldn’t be sharing it online.
Rich Piana revealed the workout as a secret hack for insane arm growth. The bodybuilder claimed his eight-hour workout would add an inch to your arm in 24 hours. Dr. Mike Israetel disagreed with this statement and openly criticized Piana. “You know, I would call an eight-hour arm workout the opposite of a hack. A hack is a shortcut,” stated Israetel.
However, the Ph.D. holder in exercise physiology wasn’t done treating Piana’s words with sarcasm. “It says it consists of 16 mini-workouts every half hour, for eight hours straight,” said the bodybuilding coach. However, he paused and stressed the words “every half hour,” and “straight” to highlight that the eight-hour arm workout lasted for four hours with 30-minute rests.
After this point, Mike Israetel simply burst into laughter and gave up. “I thought this was a meme,” said the exercise scientist because he couldn’t take Piana’s advice on preparing 16 protein shakes seriously. However, Rich Piana didn’t design the eight-hour arm workout as a meme. He was serious and shared all the particulars one would need.
Read More | “This Is Too Much”: Exercise Scientist Reacts to Rich Piana’s Extremely Painful Chest Workout
Rich Piana explained how to attempt the workout
In his clip, Rich Piana laid out a plan for those interested in attempting the workout. Undertaking such a long workout would require you to fuel your body, so Piana recommended what you should eat. “The morning of the workout, get up, and have a huge breakfast,” recommended Piana. That’s because anyone training every half hour would burn through calories.
He also recommended making 16 protein shakes. Rich Piana said the shakes should contain a “Little bit of protein, some simple sugars, and a little bit of carbs.” The bodybuilding icon explained that the workout followed Arnold Schwarzenegger’s philosophy of shocking the muscle to grow.
Read More | “Big No No for Recovery”: Exercise Scientist Unravels Consequences of Alcohol on Your Fitness Journey
While Rich Piana promised incredible results, Mike Israetel didn’t seem convinced. Unfortunately, even those who have tried it have not reported the insane hypertrophy that Piana promised.
The post “Opposite of a Hack”: Bodybuilder With PhD in Sports Physiology Bashes Rich Piana’s Viral 8-Hour Arm Workout for All the Right Reasons appeared first on EssentiallySports .

IMAGES
VIDEO
COMMENTS
The PhD in Public Health, One Health concentration will require a minimum of 90 post-baccalaureate credit hours. The One Health concentration is a research-oriented health degree that emphasizes working across public health, veterinary health, and environmental health disciplines to tackle difficult health problems. This program is designed to bridge the gap between various areas of…
The international student application deadline is March 15, 2024. The domestic student application deadline is May 15, 2024. The PhD program will be full-time, face-to-face at the School of Veterinary Medicine in Amarillo, Texas. Graduate students must complete 72 credit hours, of which 18 will be core courses and 12 will be dissertation hours.
This Wellcome Trust 4-year PhD programme in One Health Models of Disease combines key training in experimental techniques, bioethics and social sciences, to apply new 'One Health' models of neurodegenerative, cardiovascular, developmental, and infectious diseases of humans and animals. The application window for entry in October 2024 is NOW CLOSED.
Building on this experience and success, the college launched its new One Health Research Initiative (OHRI) in 2020 and recruited Frank von Hippel, PhD, to the Department of Community, Environment and Policy, to lead the OHRI. Frank brings a wealth of experience in One Health research, and leads research projects in the United States and globally.
As a student in One Health, you will: Choose to earn your MS, MS-Applied or PhD degree. Take common core courses introducing foundational concepts and skills, including: risk assessment, management and communication; assessment and management of exposures to environmental hazards; core principles of toxicology; and how to use a One Health approach to address complex challenges.
A $5,000 USD Dr. Gregory D. Bossart Memorial One Health Scholarship is available to a graduate student doing research in wildlife biology, epidemiology, veterinary, medical, public health, basic or social sciences or other program focusing on the interconnection between people, animals, plants, and their shared environment using a One Health framework.
(1) The One Health Sciences PhD program focuses training in the five disciplines and a competency-based approach with the goal of students demonstrating proficiency within competencies to address current and emerging One Health challenges. Now, 38 PhD students are enrolled in this ambitious program.
4-year PhD Studentship: Antimicrobial resistance dynamics and antimicrobial use in wildlife rehabilitation facilities in the United Kingdom. University of Bristol Bristol Veterinary School. Antimicrobial resistance (AMR) is one of the greatest global public health threats of the 21st century (Prestinaci et al. 2015).
Meghan Frost Davis, PhD, DVM, MPH. Associate Professor. Director, One Health Laboratory at Johns Hopkins University. Department of Environmental Health and Engineering. As a molecular epidemiologist and an environmental microbiologist, Meghan studies the interface of bacteria and hosts to reduce microbe-mediated disease in humans and animals.
The Texas Tech University School of Veterinary Medicine in Amarillo received final approval to offer an innovative doctoral degree in One Health Sciences to help graduate students provide solutions for society's future challenges. The program was approved by the Texas Higher Education Coordinating Board (THECB) in May 2022.
The PhD program in Data Sciences for Global Health, jointly offered by BITS Pilani and the One Health Trust (OHT), offers training in global health issues and cutting-edge research methodology with rigorous fieldwork and data analysis. This program provides full-time, advanced education in global health plus expertise in qualitative and ...
Fig. 1. Location of known academic One Health training, research, and outreach programs in North America as of August 2016. Blue stars denote universities that offer formal One Health, academic credit-earning programs, including Undergraduate majors/minors as well as Certificate, Masters, or PhD programs.
2024 Fellowship Description: The University of Arizona's One Health Research Initiative is seeking applications for Graduate Research Fellowships.One Health is a collaborative, multisectoral, and transdisciplinary approach with the goal of achieving optimal health outcomes recognizing the interconnections among people, animals, and their shared environment (including ecosystems, and social and ...
Globally, various academic institutions have established curricula offering graduate degrees in One Health. Veterinary medicine has been the leading discipline in introducing One Health-related training in its curriculum, probably because the veterinary public health concept was already established before the advent of the One Health concept. ...
The One Health MSc aims to provide interested professionals with the knowledge, skills and awareness required to work within a One Health framework that recognises the importance of interdisciplinary working and the interrelatedness of human, animal and environmental health. Graduates from our programme can expect to enhance their prospects in:
In some parts of the world, it is currently possible to achieve a MSc degree or a PhD in One Health . There are an increasing number of One Health related textbooks aiming at university students in primarily medicine and veterinary medicine, with a main focus on zoonotic diseases, epidemics and toxicants (31, 32).
One Health in Emerging Infectious Diseases" (1H-EID) Graduate Program (MSc, PhD, CE), Institut Pasteur, Paris, France . One Health Workforce Academies Resource Library, Competency Framework and Evaluation Toolkit . One Health Workforce Project Resources (U Minnesota / USAID) One Health Workforce Training Resources
The One Health Master's Degree (OHM) educates students to use a constructionist approach to address issues in the Circumpolar North that are at the intersection of human, animal, and environmental health. Graduates of the program will be able to engage key stakeholders to develop and implement realistic management plans that can be ...
Geoffrey Luis Njenga. The One Health Research, Education and Outreach Centre in Africa (OHRECA), which is supported by the Federal Ministry for Economic Cooperation and Development is happy to announce the first cohort of 2021 PhD fellowships whose research will address the health threats that face the continent using a One Health approach.
Ecosystem Health. 10. One Health Policy. 10. and either Applied Veterinary Epidemiology or Applied Epidemiology and Public Health or Applied Epidemiology and Surveillance for Conservation Medicine. 20. Elective Courses (select 20-40 credits from the following list of courses) Credits. Innovative Approaches to Health Challenges Across Disciplines.
Specific questions concerning the One-Health certificate and courses can be addressed to Dr. Aniruddha Belsare at [email protected] or (334) 844-1037). Earn a One-Health Certificate online from The School of Forestry & Wildlife Sciences. Urban planning, natural resource management, and more.
The Summer Program in Epidemiology aims to provide undergraduates with a comprehensive understanding of the vital link between mathematics, quantitative methods, and public health, helping them realize their interest in pursuing Epidemiology at a career or academic level. Through interactive coursework and hands-on experiences, participants ...
The cost of a doctorate in healthcare administration varies widely. Programs on our list range from $234 to over $1,000 per credit. Most degrees require 54 to 62 credits, totaling about $14,500 to ...
Official website for the University of Miami Leonard M. Miller School of Medicine
The M.S. in Environmental and Occupational Health degree will serve both a national and a state labor market need. The job outlook for environmental health scientists and specialists is strong. The Bureau of Labor Statistics estimates an approximate 11% increase in employment of environmental scientists and specialists from 2014 to 2024 ( bls ...
The MHA program, located in the University of Memphis CEPH-accredited School of Public Health, is a full graduate member of the Association of University Programs in Health Administration (AUPHA), and belongs to ACHE's Higher Education Network (HEN). ... HADM 7209 Quantitative Methods in Health Services; HADM 7101 Day One; Summer 1. HADM 7190 ...
Late bodybuilding icon Rich Piana earned equal measures of fame and notoriety. Although the bodybuilder passed away in 2017, one of his particular workouts has served along with his legacy. Even ...